User login
Factors linked with increased VTE risk in COVID outpatients
Though VTE risk is well studied and significant in those hospitalized with COVID, little is known about the risk in the outpatient setting, said the authors of the new research published online in JAMA Network Open.
The study was conducted at two integrated health care delivery systems in northern and southern California. Data were gathered from the Kaiser Permanente Virtual Data Warehouse and electronic health records.
Nearly 400,000 patients studied
Researchers, led by Margaret Fang, MD, with the division of hospital medicine, University of California, San Francisco, identified 398,530 outpatients with COVID-19 from Jan. 1, 2020, through Jan. 31, 2021.
VTE risk was low overall for ambulatory COVID patients.
“It is a reassuring study,” Dr. Fang said in an interview.
The researchers found that the risk is highest in the first 30 days after COVID-19 diagnosis (unadjusted rate, 0.58; 95% confidence interval, 0.51-0.67 per 100 person-years vs. 0.09; 95% CI, 0.08-0.11 per 100 person-years after 30 days).
Factors linked with high VTE risk
They also found that several factors were linked with a higher risk of blood clots in the study population, including being at least 55 years old; being male; having a history of blood clots or thrombophilia; and a body mass index (BMI) of at least 30 kg/m2.
The authors write, “These findings may help identify subsets of patients with COVID-19 who could benefit from VTE preventive strategies and more intensive short-term surveillance.”
Are routine anticoagulants justified?
Previously, randomized clinical trials have found that hospitalized patients with moderate COVID-19 may benefit from therapeutically dosed heparin anticoagulants but that therapeutic anticoagulation had no net benefit – and perhaps could even harm – patients who were critically ill with COVID.
“[M]uch less is known about the optimal thromboprophylaxis strategy for people with milder presentations of COVID-19 who do not require hospitalization,” they write.
Mild COVID VTE risk similar to general population
The authors note that rates of blood clots linked with COVID-19 are not much higher than the average blood clot rate in the general population, which is about 0.1-0.2 per 100 person-years.
Therefore, the results don’t justify routine administration of anticoagulation given the costs, inconvenience, and bleeding risks, they acknowledge.
Dr. Fang told this publication that it’s hard to know what to tell patients, given the overall low VTE risk. She said their study wasn’t designed to advise when to give prophylaxis.
Physicians should inform patients of their higher risk
“We should tell our patients who fall into these risk categories that blood clot is a concern after the development of COVID, especially in those first 30 days. And some people might benefit from increased surveillance,” Dr. Fang said.
”I think this study would support ongoing studies that look at whether selected patients benefit from VTE prophylaxis, for example low-dose anticoagulants,” she said.
Dr. Fang said the subgroup factors they found increased risk of blood clots for all patients, not just COVID-19 patients. It’s not clear why factors such as being male may increase blood clot risk, though that is consistent with previous literature, but higher risk with higher BMI might be related to a combination of inflammation or decreased mobility, she said.
Unanswered questions
Robert H. Hopkins Jr., MD, says the study helps answer a couple of important questions – that the VTE risk in nonhospitalized COVID-19 patients is low and when and for which patients risk may be highest.
However, there are several unanswered questions that argue against routine initiation of anticoagulants, notes the professor of internal medicine and pediatrics chief, division of general internal medicine, at University of Arkansas for Medical Sciences, Little Rock.
One is the change in the COVID variant landscape.
“We do not know whether rates of VTE are same or lower or higher with current circulating variants,” Dr. Hopkins said.
The authors acknowledge this as a limitation. Study data predate Omicron and subvariants, which appear to lower clinical severity, so it’s unclear whether VTE risk is different in this Omicron era.
Dr. Hopkins added another unknown: “We do not know whether vaccination affects rates of VTE in ambulatory breakthrough infection.”
Dr. Hopkins and the authors also note the lack of a control group in the study, to better compare risk.
Coauthor Dr. Prasad reports consultant fees from EpiExcellence LLC outside the submitted work. Coauthor Dr. Go reports grants paid to the division of research, Kaiser Permanente Northern California, from CSL Behring, Novartis, Bristol Meyers Squibb/Pfizer Alliance, and Janssen outside the submitted work.
The research was funded through Patient-Centered Outcomes Research Institute.
Dr. Hopkins reports no relevant financial relationships.
Though VTE risk is well studied and significant in those hospitalized with COVID, little is known about the risk in the outpatient setting, said the authors of the new research published online in JAMA Network Open.
The study was conducted at two integrated health care delivery systems in northern and southern California. Data were gathered from the Kaiser Permanente Virtual Data Warehouse and electronic health records.
Nearly 400,000 patients studied
Researchers, led by Margaret Fang, MD, with the division of hospital medicine, University of California, San Francisco, identified 398,530 outpatients with COVID-19 from Jan. 1, 2020, through Jan. 31, 2021.
VTE risk was low overall for ambulatory COVID patients.
“It is a reassuring study,” Dr. Fang said in an interview.
The researchers found that the risk is highest in the first 30 days after COVID-19 diagnosis (unadjusted rate, 0.58; 95% confidence interval, 0.51-0.67 per 100 person-years vs. 0.09; 95% CI, 0.08-0.11 per 100 person-years after 30 days).
Factors linked with high VTE risk
They also found that several factors were linked with a higher risk of blood clots in the study population, including being at least 55 years old; being male; having a history of blood clots or thrombophilia; and a body mass index (BMI) of at least 30 kg/m2.
The authors write, “These findings may help identify subsets of patients with COVID-19 who could benefit from VTE preventive strategies and more intensive short-term surveillance.”
Are routine anticoagulants justified?
Previously, randomized clinical trials have found that hospitalized patients with moderate COVID-19 may benefit from therapeutically dosed heparin anticoagulants but that therapeutic anticoagulation had no net benefit – and perhaps could even harm – patients who were critically ill with COVID.
“[M]uch less is known about the optimal thromboprophylaxis strategy for people with milder presentations of COVID-19 who do not require hospitalization,” they write.
Mild COVID VTE risk similar to general population
The authors note that rates of blood clots linked with COVID-19 are not much higher than the average blood clot rate in the general population, which is about 0.1-0.2 per 100 person-years.
Therefore, the results don’t justify routine administration of anticoagulation given the costs, inconvenience, and bleeding risks, they acknowledge.
Dr. Fang told this publication that it’s hard to know what to tell patients, given the overall low VTE risk. She said their study wasn’t designed to advise when to give prophylaxis.
Physicians should inform patients of their higher risk
“We should tell our patients who fall into these risk categories that blood clot is a concern after the development of COVID, especially in those first 30 days. And some people might benefit from increased surveillance,” Dr. Fang said.
”I think this study would support ongoing studies that look at whether selected patients benefit from VTE prophylaxis, for example low-dose anticoagulants,” she said.
Dr. Fang said the subgroup factors they found increased risk of blood clots for all patients, not just COVID-19 patients. It’s not clear why factors such as being male may increase blood clot risk, though that is consistent with previous literature, but higher risk with higher BMI might be related to a combination of inflammation or decreased mobility, she said.
Unanswered questions
Robert H. Hopkins Jr., MD, says the study helps answer a couple of important questions – that the VTE risk in nonhospitalized COVID-19 patients is low and when and for which patients risk may be highest.
However, there are several unanswered questions that argue against routine initiation of anticoagulants, notes the professor of internal medicine and pediatrics chief, division of general internal medicine, at University of Arkansas for Medical Sciences, Little Rock.
One is the change in the COVID variant landscape.
“We do not know whether rates of VTE are same or lower or higher with current circulating variants,” Dr. Hopkins said.
The authors acknowledge this as a limitation. Study data predate Omicron and subvariants, which appear to lower clinical severity, so it’s unclear whether VTE risk is different in this Omicron era.
Dr. Hopkins added another unknown: “We do not know whether vaccination affects rates of VTE in ambulatory breakthrough infection.”
Dr. Hopkins and the authors also note the lack of a control group in the study, to better compare risk.
Coauthor Dr. Prasad reports consultant fees from EpiExcellence LLC outside the submitted work. Coauthor Dr. Go reports grants paid to the division of research, Kaiser Permanente Northern California, from CSL Behring, Novartis, Bristol Meyers Squibb/Pfizer Alliance, and Janssen outside the submitted work.
The research was funded through Patient-Centered Outcomes Research Institute.
Dr. Hopkins reports no relevant financial relationships.
Though VTE risk is well studied and significant in those hospitalized with COVID, little is known about the risk in the outpatient setting, said the authors of the new research published online in JAMA Network Open.
The study was conducted at two integrated health care delivery systems in northern and southern California. Data were gathered from the Kaiser Permanente Virtual Data Warehouse and electronic health records.
Nearly 400,000 patients studied
Researchers, led by Margaret Fang, MD, with the division of hospital medicine, University of California, San Francisco, identified 398,530 outpatients with COVID-19 from Jan. 1, 2020, through Jan. 31, 2021.
VTE risk was low overall for ambulatory COVID patients.
“It is a reassuring study,” Dr. Fang said in an interview.
The researchers found that the risk is highest in the first 30 days after COVID-19 diagnosis (unadjusted rate, 0.58; 95% confidence interval, 0.51-0.67 per 100 person-years vs. 0.09; 95% CI, 0.08-0.11 per 100 person-years after 30 days).
Factors linked with high VTE risk
They also found that several factors were linked with a higher risk of blood clots in the study population, including being at least 55 years old; being male; having a history of blood clots or thrombophilia; and a body mass index (BMI) of at least 30 kg/m2.
The authors write, “These findings may help identify subsets of patients with COVID-19 who could benefit from VTE preventive strategies and more intensive short-term surveillance.”
Are routine anticoagulants justified?
Previously, randomized clinical trials have found that hospitalized patients with moderate COVID-19 may benefit from therapeutically dosed heparin anticoagulants but that therapeutic anticoagulation had no net benefit – and perhaps could even harm – patients who were critically ill with COVID.
“[M]uch less is known about the optimal thromboprophylaxis strategy for people with milder presentations of COVID-19 who do not require hospitalization,” they write.
Mild COVID VTE risk similar to general population
The authors note that rates of blood clots linked with COVID-19 are not much higher than the average blood clot rate in the general population, which is about 0.1-0.2 per 100 person-years.
Therefore, the results don’t justify routine administration of anticoagulation given the costs, inconvenience, and bleeding risks, they acknowledge.
Dr. Fang told this publication that it’s hard to know what to tell patients, given the overall low VTE risk. She said their study wasn’t designed to advise when to give prophylaxis.
Physicians should inform patients of their higher risk
“We should tell our patients who fall into these risk categories that blood clot is a concern after the development of COVID, especially in those first 30 days. And some people might benefit from increased surveillance,” Dr. Fang said.
”I think this study would support ongoing studies that look at whether selected patients benefit from VTE prophylaxis, for example low-dose anticoagulants,” she said.
Dr. Fang said the subgroup factors they found increased risk of blood clots for all patients, not just COVID-19 patients. It’s not clear why factors such as being male may increase blood clot risk, though that is consistent with previous literature, but higher risk with higher BMI might be related to a combination of inflammation or decreased mobility, she said.
Unanswered questions
Robert H. Hopkins Jr., MD, says the study helps answer a couple of important questions – that the VTE risk in nonhospitalized COVID-19 patients is low and when and for which patients risk may be highest.
However, there are several unanswered questions that argue against routine initiation of anticoagulants, notes the professor of internal medicine and pediatrics chief, division of general internal medicine, at University of Arkansas for Medical Sciences, Little Rock.
One is the change in the COVID variant landscape.
“We do not know whether rates of VTE are same or lower or higher with current circulating variants,” Dr. Hopkins said.
The authors acknowledge this as a limitation. Study data predate Omicron and subvariants, which appear to lower clinical severity, so it’s unclear whether VTE risk is different in this Omicron era.
Dr. Hopkins added another unknown: “We do not know whether vaccination affects rates of VTE in ambulatory breakthrough infection.”
Dr. Hopkins and the authors also note the lack of a control group in the study, to better compare risk.
Coauthor Dr. Prasad reports consultant fees from EpiExcellence LLC outside the submitted work. Coauthor Dr. Go reports grants paid to the division of research, Kaiser Permanente Northern California, from CSL Behring, Novartis, Bristol Meyers Squibb/Pfizer Alliance, and Janssen outside the submitted work.
The research was funded through Patient-Centered Outcomes Research Institute.
Dr. Hopkins reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Digital rectal exam fails as screening tool for prostate cancer
, say investigators reporting the PROBASE study.
The study compared risk-adapted screening measures in men who had prostate-specific antigen (PSA) measured at age 45 with those who had PSA measurements plus DRE at age 50.
The results show that as a solitary screening tool, 99% of DREs did not raise suspicion for prostate cancer, and among the 57 cases where DRE did raise suspicion, only three men were found to have cancer, all of which were low-grade, reported Agne Krilaviciute, PhD, from the German Cancer Research Center in Heidelberg, and colleagues.
“We also see that the cancer detection rate by PSA is four times higher compared to the DRE detection. Around 18% of the tumors are located in the part of the prostate where DRE cannot detect them,” she said in an oral presentation at the European Association of Urology Congress.
The investigators found that the majority of prostate cancers that occurred in this relatively young population were International Society of Urological Pathology grade 1 (Gleason score 3 + 3 = 6) or grade 2 (Gleason 3 + 4 = 7). DRE yields positive results in only about 12% of cases of ISUP grade 1 or 2, they noted.
“We conclude that DRE as a solitary screening test does not lead to a significant PCa [prostate cancer] detection rate in young men,” Dr. Krilaviciute said.
Falling by the wayside
The study adds to the growing body of evidence that DRE may not be especially helpful as either a screening tool or when used in active surveillance of men with prostate cancer.
An international consensus panel found that DRE could be safely skipped for active surveillance when MRI and other more accurate and objective measures, such as biomarkers, are available.
A prostate cancer expert who was not involved in the PROBASE study told this news organization that when he was in medical school, it would have been considered a serious lapse of practice not to perform a DRE, but that things have changed considerably over the past several years.
“We have PSA now, we have technology with MRI, and the yield of digital rectal examination is very low,” commented Julio Pow-Sang, MD, chief of the genitourinary oncology program at Moffitt Cancer Center in Tampa, Fla.
“Empirically, it’s very rare to find positive cancer through rectal exam in this day and age of PSA,” he said, adding that the examination itself is highly subjective, with varying results depending on the skills of the particular examiner.
“I think that in time, with good studies like this, digital rectal exam specifically for prostate cancer is going to slowly fade away,” Dr. Pow-Sang said.
PROBASE results
PROBASE was a randomized screening study enrolling men at age 45 to test a risk-adapted screening strategy using a baseline PSA value with the additional offer of DRE in a large subcohort of participants.
The study was conducted in Germany, and the authors note that the “German statutory early detection program recommends DRE as a stand-alone screening test starting annually at age 45.”
The PROBASE investigators enrolled 46,495 men from February 2014 through December 2019.
Among the first 23,194 men enrolled, 6,537 underwent DRE at enrollment without a study PSA test.
In this group, 6,480 DREs (99%) were not suspicious for cancer, and 57 (1%) were. Of those with suspected prostate cancer, 37 underwent biopsy and 20 did not. Of those biopsied, only two were found to have prostate cancer. This translated into a cancer detection rate of 0.03% for DRE.
After a median of 6.6 years of follow-up, only one additional case of ISUP grade 2 prostate cancer was detected among the 6,357 men who had DREs at enrollment, translating into a prostate cancer detection rate of .05%.
The investigators also looked at men who suspicious DRE findings at baseline. They assumed that a DRE-detectable tumor at age 45 would still be manifest 5 years later and should be detectable with PSA at age 50. Of the 57 men with initially suspicious findings, 11 returned for PSA screening but refused biopsy, and of this group only one had an elevated PSA level. He then underwent biopsy, but the findings were negative.
Of those who underwent biopsy on the basis of DRE, 16 had prostatitis, 14 had benign prostatic hyperplasia, 1 had high-grade prostatic intraepithelial neoplasia, 1 had atypical small acinar proliferation, and 3 had equivocal findings.
In total, the investigators found 24 tumors among men screened with DRE. Of these, 3 occurred in men with results deemed suspicious and 21 were in men with unsuspicious digital exams. All of the tumors were ISUP grade 1, 2, or 3 tumors.
Among 245 men who had biopsies for a PSA level equal to or higher than 3 ng/mL, primarily Prostate Imaging Reporting and Data System (PI-RADS) 3-5 tumors, DRE findings at the time of biopsy were unsuspicious in about 82% of cases, Dr. Krilaviciute said.
“We also used MRI data to determine what proportion of tumors would be potentially detectable by DRE. We estimated that around 18% of tumors are located in the upper part of the prostate, which is not detectable by DRE,” she said. “Even excluding those tumors, still the DRE detection rate is low in palpable tumors.”
Although DRE performed better in higher-grade tumors, 80% of the tumors in the PROBASE participants were ISUP grade 1 or 2 and were likely to be undetected by DRE, she added.
“In Germany, the recommendations for the screening still include 45-year-olds to go with annual DRE. The PROBASE trial allowed us to evaluate for the first time what was the diagnostic performance for DRE at such a young age, and we see that 99% of men undergoing DRE have no suspicious findings, and among the 1% of suspicious findings having cancers extremely unlikely,” she said.
The study was supported by Deutsche Krebshilfe (German Cancer Aid). Dr. Krilaviciute and Dr. Pow-Sang reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
, say investigators reporting the PROBASE study.
The study compared risk-adapted screening measures in men who had prostate-specific antigen (PSA) measured at age 45 with those who had PSA measurements plus DRE at age 50.
The results show that as a solitary screening tool, 99% of DREs did not raise suspicion for prostate cancer, and among the 57 cases where DRE did raise suspicion, only three men were found to have cancer, all of which were low-grade, reported Agne Krilaviciute, PhD, from the German Cancer Research Center in Heidelberg, and colleagues.
“We also see that the cancer detection rate by PSA is four times higher compared to the DRE detection. Around 18% of the tumors are located in the part of the prostate where DRE cannot detect them,” she said in an oral presentation at the European Association of Urology Congress.
The investigators found that the majority of prostate cancers that occurred in this relatively young population were International Society of Urological Pathology grade 1 (Gleason score 3 + 3 = 6) or grade 2 (Gleason 3 + 4 = 7). DRE yields positive results in only about 12% of cases of ISUP grade 1 or 2, they noted.
“We conclude that DRE as a solitary screening test does not lead to a significant PCa [prostate cancer] detection rate in young men,” Dr. Krilaviciute said.
Falling by the wayside
The study adds to the growing body of evidence that DRE may not be especially helpful as either a screening tool or when used in active surveillance of men with prostate cancer.
An international consensus panel found that DRE could be safely skipped for active surveillance when MRI and other more accurate and objective measures, such as biomarkers, are available.
A prostate cancer expert who was not involved in the PROBASE study told this news organization that when he was in medical school, it would have been considered a serious lapse of practice not to perform a DRE, but that things have changed considerably over the past several years.
“We have PSA now, we have technology with MRI, and the yield of digital rectal examination is very low,” commented Julio Pow-Sang, MD, chief of the genitourinary oncology program at Moffitt Cancer Center in Tampa, Fla.
“Empirically, it’s very rare to find positive cancer through rectal exam in this day and age of PSA,” he said, adding that the examination itself is highly subjective, with varying results depending on the skills of the particular examiner.
“I think that in time, with good studies like this, digital rectal exam specifically for prostate cancer is going to slowly fade away,” Dr. Pow-Sang said.
PROBASE results
PROBASE was a randomized screening study enrolling men at age 45 to test a risk-adapted screening strategy using a baseline PSA value with the additional offer of DRE in a large subcohort of participants.
The study was conducted in Germany, and the authors note that the “German statutory early detection program recommends DRE as a stand-alone screening test starting annually at age 45.”
The PROBASE investigators enrolled 46,495 men from February 2014 through December 2019.
Among the first 23,194 men enrolled, 6,537 underwent DRE at enrollment without a study PSA test.
In this group, 6,480 DREs (99%) were not suspicious for cancer, and 57 (1%) were. Of those with suspected prostate cancer, 37 underwent biopsy and 20 did not. Of those biopsied, only two were found to have prostate cancer. This translated into a cancer detection rate of 0.03% for DRE.
After a median of 6.6 years of follow-up, only one additional case of ISUP grade 2 prostate cancer was detected among the 6,357 men who had DREs at enrollment, translating into a prostate cancer detection rate of .05%.
The investigators also looked at men who suspicious DRE findings at baseline. They assumed that a DRE-detectable tumor at age 45 would still be manifest 5 years later and should be detectable with PSA at age 50. Of the 57 men with initially suspicious findings, 11 returned for PSA screening but refused biopsy, and of this group only one had an elevated PSA level. He then underwent biopsy, but the findings were negative.
Of those who underwent biopsy on the basis of DRE, 16 had prostatitis, 14 had benign prostatic hyperplasia, 1 had high-grade prostatic intraepithelial neoplasia, 1 had atypical small acinar proliferation, and 3 had equivocal findings.
In total, the investigators found 24 tumors among men screened with DRE. Of these, 3 occurred in men with results deemed suspicious and 21 were in men with unsuspicious digital exams. All of the tumors were ISUP grade 1, 2, or 3 tumors.
Among 245 men who had biopsies for a PSA level equal to or higher than 3 ng/mL, primarily Prostate Imaging Reporting and Data System (PI-RADS) 3-5 tumors, DRE findings at the time of biopsy were unsuspicious in about 82% of cases, Dr. Krilaviciute said.
“We also used MRI data to determine what proportion of tumors would be potentially detectable by DRE. We estimated that around 18% of tumors are located in the upper part of the prostate, which is not detectable by DRE,” she said. “Even excluding those tumors, still the DRE detection rate is low in palpable tumors.”
Although DRE performed better in higher-grade tumors, 80% of the tumors in the PROBASE participants were ISUP grade 1 or 2 and were likely to be undetected by DRE, she added.
“In Germany, the recommendations for the screening still include 45-year-olds to go with annual DRE. The PROBASE trial allowed us to evaluate for the first time what was the diagnostic performance for DRE at such a young age, and we see that 99% of men undergoing DRE have no suspicious findings, and among the 1% of suspicious findings having cancers extremely unlikely,” she said.
The study was supported by Deutsche Krebshilfe (German Cancer Aid). Dr. Krilaviciute and Dr. Pow-Sang reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
, say investigators reporting the PROBASE study.
The study compared risk-adapted screening measures in men who had prostate-specific antigen (PSA) measured at age 45 with those who had PSA measurements plus DRE at age 50.
The results show that as a solitary screening tool, 99% of DREs did not raise suspicion for prostate cancer, and among the 57 cases where DRE did raise suspicion, only three men were found to have cancer, all of which were low-grade, reported Agne Krilaviciute, PhD, from the German Cancer Research Center in Heidelberg, and colleagues.
“We also see that the cancer detection rate by PSA is four times higher compared to the DRE detection. Around 18% of the tumors are located in the part of the prostate where DRE cannot detect them,” she said in an oral presentation at the European Association of Urology Congress.
The investigators found that the majority of prostate cancers that occurred in this relatively young population were International Society of Urological Pathology grade 1 (Gleason score 3 + 3 = 6) or grade 2 (Gleason 3 + 4 = 7). DRE yields positive results in only about 12% of cases of ISUP grade 1 or 2, they noted.
“We conclude that DRE as a solitary screening test does not lead to a significant PCa [prostate cancer] detection rate in young men,” Dr. Krilaviciute said.
Falling by the wayside
The study adds to the growing body of evidence that DRE may not be especially helpful as either a screening tool or when used in active surveillance of men with prostate cancer.
An international consensus panel found that DRE could be safely skipped for active surveillance when MRI and other more accurate and objective measures, such as biomarkers, are available.
A prostate cancer expert who was not involved in the PROBASE study told this news organization that when he was in medical school, it would have been considered a serious lapse of practice not to perform a DRE, but that things have changed considerably over the past several years.
“We have PSA now, we have technology with MRI, and the yield of digital rectal examination is very low,” commented Julio Pow-Sang, MD, chief of the genitourinary oncology program at Moffitt Cancer Center in Tampa, Fla.
“Empirically, it’s very rare to find positive cancer through rectal exam in this day and age of PSA,” he said, adding that the examination itself is highly subjective, with varying results depending on the skills of the particular examiner.
“I think that in time, with good studies like this, digital rectal exam specifically for prostate cancer is going to slowly fade away,” Dr. Pow-Sang said.
PROBASE results
PROBASE was a randomized screening study enrolling men at age 45 to test a risk-adapted screening strategy using a baseline PSA value with the additional offer of DRE in a large subcohort of participants.
The study was conducted in Germany, and the authors note that the “German statutory early detection program recommends DRE as a stand-alone screening test starting annually at age 45.”
The PROBASE investigators enrolled 46,495 men from February 2014 through December 2019.
Among the first 23,194 men enrolled, 6,537 underwent DRE at enrollment without a study PSA test.
In this group, 6,480 DREs (99%) were not suspicious for cancer, and 57 (1%) were. Of those with suspected prostate cancer, 37 underwent biopsy and 20 did not. Of those biopsied, only two were found to have prostate cancer. This translated into a cancer detection rate of 0.03% for DRE.
After a median of 6.6 years of follow-up, only one additional case of ISUP grade 2 prostate cancer was detected among the 6,357 men who had DREs at enrollment, translating into a prostate cancer detection rate of .05%.
The investigators also looked at men who suspicious DRE findings at baseline. They assumed that a DRE-detectable tumor at age 45 would still be manifest 5 years later and should be detectable with PSA at age 50. Of the 57 men with initially suspicious findings, 11 returned for PSA screening but refused biopsy, and of this group only one had an elevated PSA level. He then underwent biopsy, but the findings were negative.
Of those who underwent biopsy on the basis of DRE, 16 had prostatitis, 14 had benign prostatic hyperplasia, 1 had high-grade prostatic intraepithelial neoplasia, 1 had atypical small acinar proliferation, and 3 had equivocal findings.
In total, the investigators found 24 tumors among men screened with DRE. Of these, 3 occurred in men with results deemed suspicious and 21 were in men with unsuspicious digital exams. All of the tumors were ISUP grade 1, 2, or 3 tumors.
Among 245 men who had biopsies for a PSA level equal to or higher than 3 ng/mL, primarily Prostate Imaging Reporting and Data System (PI-RADS) 3-5 tumors, DRE findings at the time of biopsy were unsuspicious in about 82% of cases, Dr. Krilaviciute said.
“We also used MRI data to determine what proportion of tumors would be potentially detectable by DRE. We estimated that around 18% of tumors are located in the upper part of the prostate, which is not detectable by DRE,” she said. “Even excluding those tumors, still the DRE detection rate is low in palpable tumors.”
Although DRE performed better in higher-grade tumors, 80% of the tumors in the PROBASE participants were ISUP grade 1 or 2 and were likely to be undetected by DRE, she added.
“In Germany, the recommendations for the screening still include 45-year-olds to go with annual DRE. The PROBASE trial allowed us to evaluate for the first time what was the diagnostic performance for DRE at such a young age, and we see that 99% of men undergoing DRE have no suspicious findings, and among the 1% of suspicious findings having cancers extremely unlikely,” she said.
The study was supported by Deutsche Krebshilfe (German Cancer Aid). Dr. Krilaviciute and Dr. Pow-Sang reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM EAU 2023
Urine test predicts future bladder cancer 12 years before symptoms
an international team of researchers claims.
The test, if validated in further studies, has the potential to serve as a cancer screening tool for individuals at elevated risk for bladder cancer due to genetics, smoking, or from environmental exposures to known carcinogens, and it could help to reduce the frequency of unnecessary cystoscopies, say urologists who were not involved in the research.
The test involved was performed using a next-generation sequencing assay (UroAmp, Convergent Genomics, based in San Francisco) that identifies mutations in 60 genes associated with bladder cancer. New research reported at the annual congress of the European Association of Urology described the screening model that focused on 10 key genes covered in the assay.
In training and validation cohorts, the urinary comprehensive genomic profiling test accurately predicted future bladder cancer in 66% of patient urine samples, including some that had been collected more than a decade prior to being tested, reported Florence Le Calvez-Kelm, PhD, MSc, from the International Agency for Research on Cancer, Lyon, France.
“Our results provide first evidence from a population-based cohort study of preclinical urothelial cancer detection with urinary comprehensive genomic profiling,” she told the meeting.
The results were consistent both in individuals with known risk factors for bladder cancer who were undergoing cystoscopy and in those with no evidence of disease, she said.
“Research of this nature is very encouraging, as it shows that our ability to identify molecular alterations in liquid biopsies such as urine that might indicate cancer is constantly improving,” commented Joost Boormans, MD, PhD, a urologist at the Erasmus University Medical Center, Rotterdam, Netherlands, and a member of the EAU Scientific Congress Office.
“While we do need to develop more accurate diagnostics, it’s unlikely that we’ll have a mass screening program for bladder cancer in the near future,” he continued. “Where a urine test for genetic mutations could show its value is in reducing cystoscopies and scans in bladder cancer patients who are being monitored for recurrence, as well as those referred for blood in their urine. A simple urine test would be far easier for patients to undergo than invasive procedures or scans, as well as being less costly for health services.”
Dr. Le Calvez-Kelm and colleagues had previously shown that promoter mutations in the gene encoding for the enzyme telomerase reverse transcriptase (TERT) identified in urine were “promising noninvasive biomarkers” for early detection of bladder cancer.
They found that TERT mutations in urine could predict which patients were likely to develop urothelial cancer with 48% sensitivity and 100% specificity.
In the study presented at EAU23, they hypothesized that uCGP of DNA in urine could offer enhanced sensitivity for early detection of urothelial cancer.
They first used the 60-gene assay to create a training set using urine samples from 46 patients with de novo urothelial cancer, 40 with recurrent cancer, and 140 healthy controls.
They then tested the model in two validation cohorts. The first validation cohort consisted of samples from 22 patients with de novo cancer, 48 with recurrent urothelial cancer, and 96 controls from a case-control study conducted at Massachusetts General Hospital, Boston, and Ohio State University, Columbus.
The second validation cohort included 29 patients from the prospective Golestan Cohort Study who subsequently developed urothelial cancer, with 98 controls.
In all, 10 genes were identified as optimal for inclusion in a screening model, which was trained to an overall sensitivity of 88% and a 97% sensitivity for high-grade tumors, with a specificity of 94%.
In the MGH/OSU validation cohort the sensitivity of the models was 71%, and the specificity was 94%. In the Golestan cohort, the sensitivity was 66%, with a specificity of 94%. This compared favorably with the performance of the TERT-only screening model, which, as noted before, had a sensitivity of 48%, albeit with 100% specificity.
“Interestingly, when we broke down the analysis according to the lag time between urine collection and diagnosis, sensitivity increased as the time to diagnosis decreased, so the closer we got to the diagnosis, the higher was the sensitivity,” Dr. Le Calvez-Kelm said.
When the analysis was limited to urothelial cancers diagnosed within 7 years of sample collection, the sensitivity for detecting preclinical cancer improved to 86%, compared with 57% for a test of TERT promoter mutations alone.
Among the patients in the Golestan cohort, uCGP-predicted positive results were associated with a more than eightfold higher risk for worse cancer-free survival, compared with uCGP-predicted negatives (hazard ratio 8.5, P < .0001).
“Of course, further studies are needed to validate this finding and to assess the clinical utility in other longitudinal cohorts,” Dr. Le Calvez-Kelm concluded.
A version of this article first appeared on Medscape.com.
an international team of researchers claims.
The test, if validated in further studies, has the potential to serve as a cancer screening tool for individuals at elevated risk for bladder cancer due to genetics, smoking, or from environmental exposures to known carcinogens, and it could help to reduce the frequency of unnecessary cystoscopies, say urologists who were not involved in the research.
The test involved was performed using a next-generation sequencing assay (UroAmp, Convergent Genomics, based in San Francisco) that identifies mutations in 60 genes associated with bladder cancer. New research reported at the annual congress of the European Association of Urology described the screening model that focused on 10 key genes covered in the assay.
In training and validation cohorts, the urinary comprehensive genomic profiling test accurately predicted future bladder cancer in 66% of patient urine samples, including some that had been collected more than a decade prior to being tested, reported Florence Le Calvez-Kelm, PhD, MSc, from the International Agency for Research on Cancer, Lyon, France.
“Our results provide first evidence from a population-based cohort study of preclinical urothelial cancer detection with urinary comprehensive genomic profiling,” she told the meeting.
The results were consistent both in individuals with known risk factors for bladder cancer who were undergoing cystoscopy and in those with no evidence of disease, she said.
“Research of this nature is very encouraging, as it shows that our ability to identify molecular alterations in liquid biopsies such as urine that might indicate cancer is constantly improving,” commented Joost Boormans, MD, PhD, a urologist at the Erasmus University Medical Center, Rotterdam, Netherlands, and a member of the EAU Scientific Congress Office.
“While we do need to develop more accurate diagnostics, it’s unlikely that we’ll have a mass screening program for bladder cancer in the near future,” he continued. “Where a urine test for genetic mutations could show its value is in reducing cystoscopies and scans in bladder cancer patients who are being monitored for recurrence, as well as those referred for blood in their urine. A simple urine test would be far easier for patients to undergo than invasive procedures or scans, as well as being less costly for health services.”
Dr. Le Calvez-Kelm and colleagues had previously shown that promoter mutations in the gene encoding for the enzyme telomerase reverse transcriptase (TERT) identified in urine were “promising noninvasive biomarkers” for early detection of bladder cancer.
They found that TERT mutations in urine could predict which patients were likely to develop urothelial cancer with 48% sensitivity and 100% specificity.
In the study presented at EAU23, they hypothesized that uCGP of DNA in urine could offer enhanced sensitivity for early detection of urothelial cancer.
They first used the 60-gene assay to create a training set using urine samples from 46 patients with de novo urothelial cancer, 40 with recurrent cancer, and 140 healthy controls.
They then tested the model in two validation cohorts. The first validation cohort consisted of samples from 22 patients with de novo cancer, 48 with recurrent urothelial cancer, and 96 controls from a case-control study conducted at Massachusetts General Hospital, Boston, and Ohio State University, Columbus.
The second validation cohort included 29 patients from the prospective Golestan Cohort Study who subsequently developed urothelial cancer, with 98 controls.
In all, 10 genes were identified as optimal for inclusion in a screening model, which was trained to an overall sensitivity of 88% and a 97% sensitivity for high-grade tumors, with a specificity of 94%.
In the MGH/OSU validation cohort the sensitivity of the models was 71%, and the specificity was 94%. In the Golestan cohort, the sensitivity was 66%, with a specificity of 94%. This compared favorably with the performance of the TERT-only screening model, which, as noted before, had a sensitivity of 48%, albeit with 100% specificity.
“Interestingly, when we broke down the analysis according to the lag time between urine collection and diagnosis, sensitivity increased as the time to diagnosis decreased, so the closer we got to the diagnosis, the higher was the sensitivity,” Dr. Le Calvez-Kelm said.
When the analysis was limited to urothelial cancers diagnosed within 7 years of sample collection, the sensitivity for detecting preclinical cancer improved to 86%, compared with 57% for a test of TERT promoter mutations alone.
Among the patients in the Golestan cohort, uCGP-predicted positive results were associated with a more than eightfold higher risk for worse cancer-free survival, compared with uCGP-predicted negatives (hazard ratio 8.5, P < .0001).
“Of course, further studies are needed to validate this finding and to assess the clinical utility in other longitudinal cohorts,” Dr. Le Calvez-Kelm concluded.
A version of this article first appeared on Medscape.com.
an international team of researchers claims.
The test, if validated in further studies, has the potential to serve as a cancer screening tool for individuals at elevated risk for bladder cancer due to genetics, smoking, or from environmental exposures to known carcinogens, and it could help to reduce the frequency of unnecessary cystoscopies, say urologists who were not involved in the research.
The test involved was performed using a next-generation sequencing assay (UroAmp, Convergent Genomics, based in San Francisco) that identifies mutations in 60 genes associated with bladder cancer. New research reported at the annual congress of the European Association of Urology described the screening model that focused on 10 key genes covered in the assay.
In training and validation cohorts, the urinary comprehensive genomic profiling test accurately predicted future bladder cancer in 66% of patient urine samples, including some that had been collected more than a decade prior to being tested, reported Florence Le Calvez-Kelm, PhD, MSc, from the International Agency for Research on Cancer, Lyon, France.
“Our results provide first evidence from a population-based cohort study of preclinical urothelial cancer detection with urinary comprehensive genomic profiling,” she told the meeting.
The results were consistent both in individuals with known risk factors for bladder cancer who were undergoing cystoscopy and in those with no evidence of disease, she said.
“Research of this nature is very encouraging, as it shows that our ability to identify molecular alterations in liquid biopsies such as urine that might indicate cancer is constantly improving,” commented Joost Boormans, MD, PhD, a urologist at the Erasmus University Medical Center, Rotterdam, Netherlands, and a member of the EAU Scientific Congress Office.
“While we do need to develop more accurate diagnostics, it’s unlikely that we’ll have a mass screening program for bladder cancer in the near future,” he continued. “Where a urine test for genetic mutations could show its value is in reducing cystoscopies and scans in bladder cancer patients who are being monitored for recurrence, as well as those referred for blood in their urine. A simple urine test would be far easier for patients to undergo than invasive procedures or scans, as well as being less costly for health services.”
Dr. Le Calvez-Kelm and colleagues had previously shown that promoter mutations in the gene encoding for the enzyme telomerase reverse transcriptase (TERT) identified in urine were “promising noninvasive biomarkers” for early detection of bladder cancer.
They found that TERT mutations in urine could predict which patients were likely to develop urothelial cancer with 48% sensitivity and 100% specificity.
In the study presented at EAU23, they hypothesized that uCGP of DNA in urine could offer enhanced sensitivity for early detection of urothelial cancer.
They first used the 60-gene assay to create a training set using urine samples from 46 patients with de novo urothelial cancer, 40 with recurrent cancer, and 140 healthy controls.
They then tested the model in two validation cohorts. The first validation cohort consisted of samples from 22 patients with de novo cancer, 48 with recurrent urothelial cancer, and 96 controls from a case-control study conducted at Massachusetts General Hospital, Boston, and Ohio State University, Columbus.
The second validation cohort included 29 patients from the prospective Golestan Cohort Study who subsequently developed urothelial cancer, with 98 controls.
In all, 10 genes were identified as optimal for inclusion in a screening model, which was trained to an overall sensitivity of 88% and a 97% sensitivity for high-grade tumors, with a specificity of 94%.
In the MGH/OSU validation cohort the sensitivity of the models was 71%, and the specificity was 94%. In the Golestan cohort, the sensitivity was 66%, with a specificity of 94%. This compared favorably with the performance of the TERT-only screening model, which, as noted before, had a sensitivity of 48%, albeit with 100% specificity.
“Interestingly, when we broke down the analysis according to the lag time between urine collection and diagnosis, sensitivity increased as the time to diagnosis decreased, so the closer we got to the diagnosis, the higher was the sensitivity,” Dr. Le Calvez-Kelm said.
When the analysis was limited to urothelial cancers diagnosed within 7 years of sample collection, the sensitivity for detecting preclinical cancer improved to 86%, compared with 57% for a test of TERT promoter mutations alone.
Among the patients in the Golestan cohort, uCGP-predicted positive results were associated with a more than eightfold higher risk for worse cancer-free survival, compared with uCGP-predicted negatives (hazard ratio 8.5, P < .0001).
“Of course, further studies are needed to validate this finding and to assess the clinical utility in other longitudinal cohorts,” Dr. Le Calvez-Kelm concluded.
A version of this article first appeared on Medscape.com.
FROM EAU23
Three surprising studies on exercise restriction and an exercise sweet spot
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Catheterized urine color change
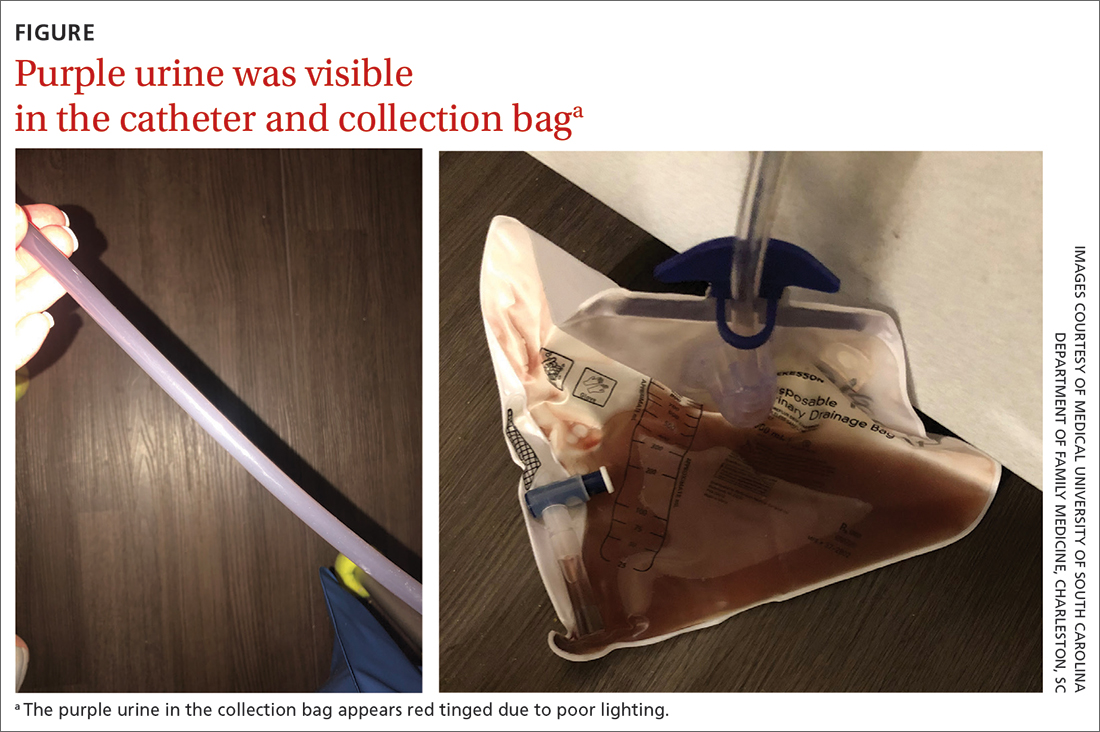
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
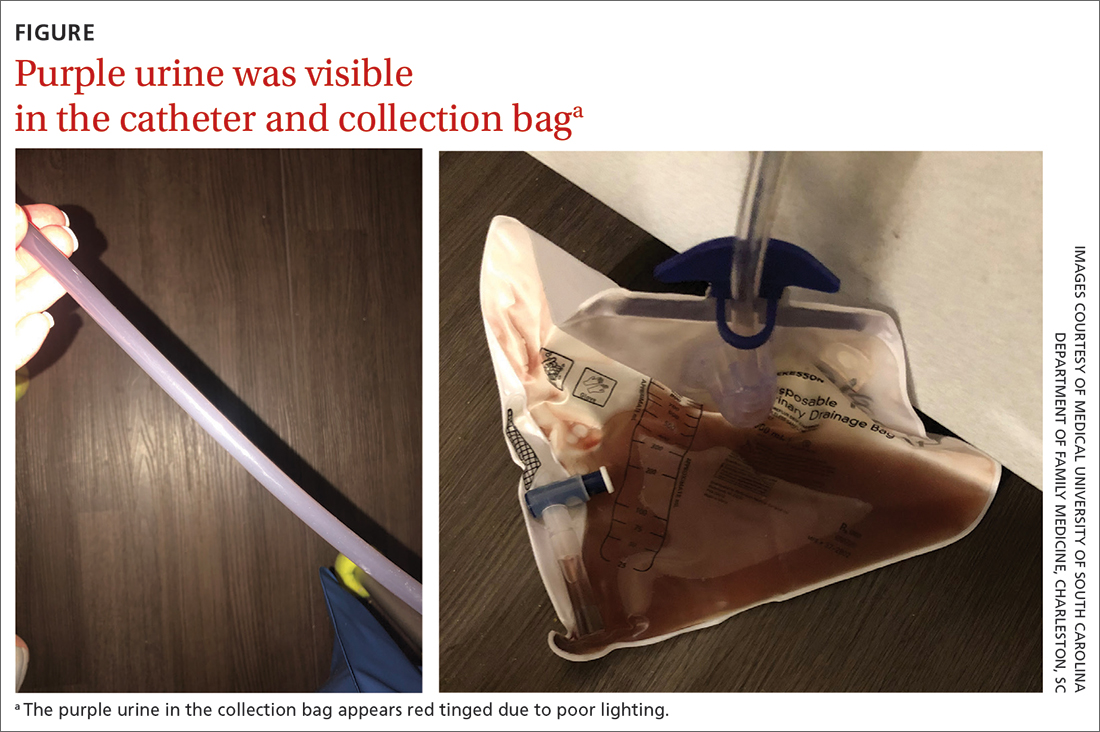
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
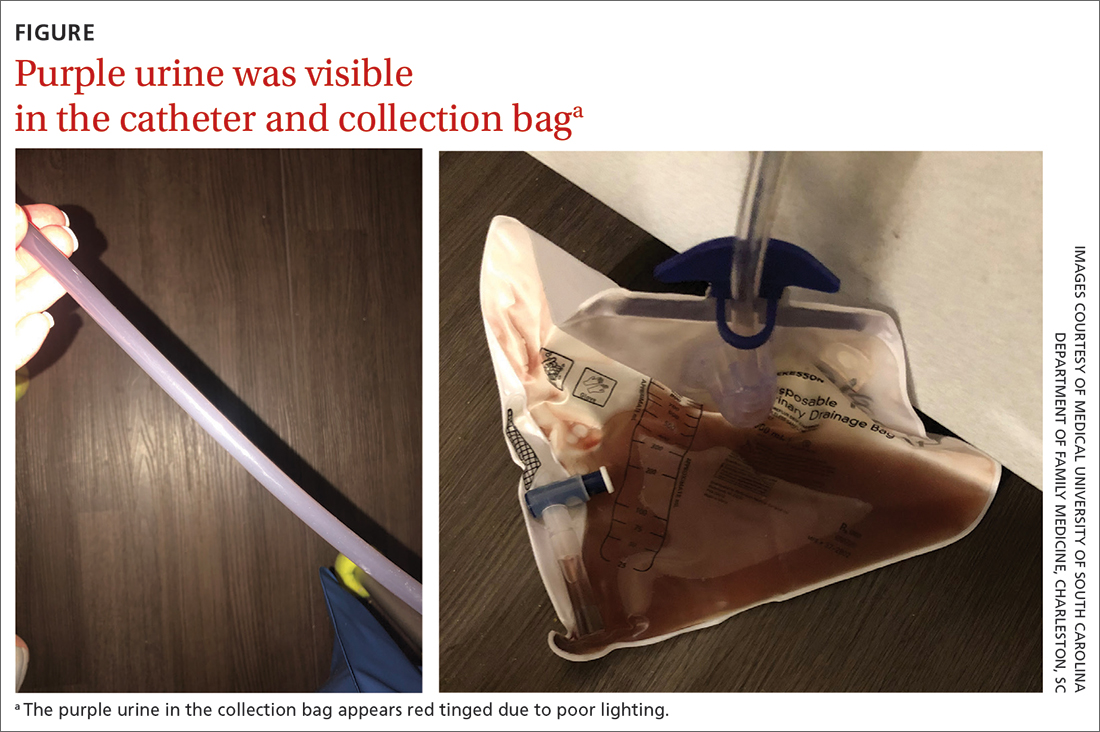
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
USPSTF recommends against routine herpes screening for asymptomatic teens and adults
Asymptomatic adults, teens, and pregnant women with no known history or symptoms of herpes infection need not undergo routine screening, according to the latest recommendation from the U.S. Preventive Services Task Force.
The 2023 recommendation reaffirms the conclusion from 2016, wrote Carol M. Mangione, MD, of the University of California, Los Angeles, and members of the task force.
“Currently, routine serologic screening for genital herpes is limited by the low predictive value of the widely available serologic screening tests and the expected high rate of false-positive results likely to occur with routine screening of asymptomatic persons in the U.S.,” the authors said.
In the recommendation, published in JAMA, the authors affirmed with moderate certainty and a grade D recommendation that the risks of routine screening for herpes simplex virus (HSV) in asymptomatic individuals outweigh the benefits.
The task force found no new evidence on the accuracy of serologic screening tests, the benefits of early detection and treatment, or on the harms of screening and treatment since the 2016 review of 17 studies in 19 publications, with data from more than 9,000 individuals.
Studies of the accuracy of serologic screening for herpes simplex virus-2 in the 2016 report mainly reflect populations with higher HSV-2 prevalence and are of limited applicability to the U.S. primary care population, the authors wrote. Evidence from the 2016 review also showed limited and inconsistent support for the early identification and treatment of HSV-2 in asymptomatic individuals, including those who were pregnant.
No new evidence has emerged since 2016 regarding harms of screening or treating genital herpes in asymptomatic individuals, the authors noted. “Based on previous evidence, the USPSTF estimated that using the widely available serologic tests for HSV-2, nearly 1 of every 2 diagnoses in the general U.S. primary care population could be false,” they said. The task force also concluded that the low accuracy of the current tests could prompt unnecessary treatment for individuals with false-positive diagnoses, as well as social and emotional harm for these individuals.
During a period of public comment from Aug. 16, 2022, to Sept. 12, 2022, individuals expressed concerns that the recommendation against routine screening showed a disinclination to take herpes seriously, and concerns that asymptomatic individuals could transmit the infection to sexual partners, the authors said. However, the estimated seroprevalence of HSV-1 and HSV-2 has declined in recent decades, and other comments supported the USPSTF’s analysis of the evidence and noted their consistency with current clinical practice.
The task force noted that research gaps remain and recognized the need to improve screening and treatment of genital herpes to prevent symptomatic episodes and transmission. Specifically, the USPSTF recommendation calls for more research to assess the accuracy of screening tests, to enroll more study participants from populations disproportionately affected by HSV, to examine the effect of behavioral counseling, and to clarify associations between HSV and pregnancy outcomes. In addition, the task force called for research to create an effective vaccine to prevent genital HSV infection and to develop a cure.
Targeted screening makes sense for now
“Given the frequency and severity of the range of diseases seen with HSV and the large proportion of persons who are asymptomatic, identifying carriers through type-specific serologic screening has long been considered a plausible strategy,” Mark D. Pearlman, MD, of the University of Michigan, Ann Arbor, wrote in an accompanying editorial.
However, accuracy of the currently available serology screening tests is low, and the adverse social and psychological effects and the impact on relationships for many asymptomatic individuals who test positive and may be incorrectly identified as infected remains a concern, said Dr. Pearlman.
Although some may be disagree about the value of routine serotesting for HSV-2 in asymptomatic individuals, other strategies can reduce the spread of infection and help those infected, he said.
Many experts continue to recommend targeted serotesting to high-risk populations, such as pregnant women whose nonpregnant partner is known to have genital or oral herpes and whose own infection status or serostatus is uncertain, said Dr. Pearlman. Other targeted strategies include screening individuals with recurrent or atypical genital symptoms and negative polymerase chain reaction assay or culture results, a clinical herpes diagnosis without laboratory confirmation, or those at increased risk because of a high number of sexual partners or a history of HIV infection, he said.
“Of note, the current CDC STI guidelines and ACOG both concur with the USPSTF that routine screening in the general population or routine screening during pregnancy are not recommended,” Dr. Pearlman said. Meanwhile, research efforts continue to help reduce the impact of HSV disease and development of a more effective testing methodology “might tip the balance in favor of routine screening” in the future, he emphasized.
The recommendations were supported by the Agency for Healthcare Research and Quality. The members of the task force received reimbursement for travel and an honorarium but had no other relevant financial conflicts to disclose. Dr. Pearlman had no financial conflicts to disclose.
Asymptomatic adults, teens, and pregnant women with no known history or symptoms of herpes infection need not undergo routine screening, according to the latest recommendation from the U.S. Preventive Services Task Force.
The 2023 recommendation reaffirms the conclusion from 2016, wrote Carol M. Mangione, MD, of the University of California, Los Angeles, and members of the task force.
“Currently, routine serologic screening for genital herpes is limited by the low predictive value of the widely available serologic screening tests and the expected high rate of false-positive results likely to occur with routine screening of asymptomatic persons in the U.S.,” the authors said.
In the recommendation, published in JAMA, the authors affirmed with moderate certainty and a grade D recommendation that the risks of routine screening for herpes simplex virus (HSV) in asymptomatic individuals outweigh the benefits.
The task force found no new evidence on the accuracy of serologic screening tests, the benefits of early detection and treatment, or on the harms of screening and treatment since the 2016 review of 17 studies in 19 publications, with data from more than 9,000 individuals.
Studies of the accuracy of serologic screening for herpes simplex virus-2 in the 2016 report mainly reflect populations with higher HSV-2 prevalence and are of limited applicability to the U.S. primary care population, the authors wrote. Evidence from the 2016 review also showed limited and inconsistent support for the early identification and treatment of HSV-2 in asymptomatic individuals, including those who were pregnant.
No new evidence has emerged since 2016 regarding harms of screening or treating genital herpes in asymptomatic individuals, the authors noted. “Based on previous evidence, the USPSTF estimated that using the widely available serologic tests for HSV-2, nearly 1 of every 2 diagnoses in the general U.S. primary care population could be false,” they said. The task force also concluded that the low accuracy of the current tests could prompt unnecessary treatment for individuals with false-positive diagnoses, as well as social and emotional harm for these individuals.
During a period of public comment from Aug. 16, 2022, to Sept. 12, 2022, individuals expressed concerns that the recommendation against routine screening showed a disinclination to take herpes seriously, and concerns that asymptomatic individuals could transmit the infection to sexual partners, the authors said. However, the estimated seroprevalence of HSV-1 and HSV-2 has declined in recent decades, and other comments supported the USPSTF’s analysis of the evidence and noted their consistency with current clinical practice.
The task force noted that research gaps remain and recognized the need to improve screening and treatment of genital herpes to prevent symptomatic episodes and transmission. Specifically, the USPSTF recommendation calls for more research to assess the accuracy of screening tests, to enroll more study participants from populations disproportionately affected by HSV, to examine the effect of behavioral counseling, and to clarify associations between HSV and pregnancy outcomes. In addition, the task force called for research to create an effective vaccine to prevent genital HSV infection and to develop a cure.
Targeted screening makes sense for now
“Given the frequency and severity of the range of diseases seen with HSV and the large proportion of persons who are asymptomatic, identifying carriers through type-specific serologic screening has long been considered a plausible strategy,” Mark D. Pearlman, MD, of the University of Michigan, Ann Arbor, wrote in an accompanying editorial.
However, accuracy of the currently available serology screening tests is low, and the adverse social and psychological effects and the impact on relationships for many asymptomatic individuals who test positive and may be incorrectly identified as infected remains a concern, said Dr. Pearlman.
Although some may be disagree about the value of routine serotesting for HSV-2 in asymptomatic individuals, other strategies can reduce the spread of infection and help those infected, he said.
Many experts continue to recommend targeted serotesting to high-risk populations, such as pregnant women whose nonpregnant partner is known to have genital or oral herpes and whose own infection status or serostatus is uncertain, said Dr. Pearlman. Other targeted strategies include screening individuals with recurrent or atypical genital symptoms and negative polymerase chain reaction assay or culture results, a clinical herpes diagnosis without laboratory confirmation, or those at increased risk because of a high number of sexual partners or a history of HIV infection, he said.
“Of note, the current CDC STI guidelines and ACOG both concur with the USPSTF that routine screening in the general population or routine screening during pregnancy are not recommended,” Dr. Pearlman said. Meanwhile, research efforts continue to help reduce the impact of HSV disease and development of a more effective testing methodology “might tip the balance in favor of routine screening” in the future, he emphasized.
The recommendations were supported by the Agency for Healthcare Research and Quality. The members of the task force received reimbursement for travel and an honorarium but had no other relevant financial conflicts to disclose. Dr. Pearlman had no financial conflicts to disclose.
Asymptomatic adults, teens, and pregnant women with no known history or symptoms of herpes infection need not undergo routine screening, according to the latest recommendation from the U.S. Preventive Services Task Force.
The 2023 recommendation reaffirms the conclusion from 2016, wrote Carol M. Mangione, MD, of the University of California, Los Angeles, and members of the task force.
“Currently, routine serologic screening for genital herpes is limited by the low predictive value of the widely available serologic screening tests and the expected high rate of false-positive results likely to occur with routine screening of asymptomatic persons in the U.S.,” the authors said.
In the recommendation, published in JAMA, the authors affirmed with moderate certainty and a grade D recommendation that the risks of routine screening for herpes simplex virus (HSV) in asymptomatic individuals outweigh the benefits.
The task force found no new evidence on the accuracy of serologic screening tests, the benefits of early detection and treatment, or on the harms of screening and treatment since the 2016 review of 17 studies in 19 publications, with data from more than 9,000 individuals.
Studies of the accuracy of serologic screening for herpes simplex virus-2 in the 2016 report mainly reflect populations with higher HSV-2 prevalence and are of limited applicability to the U.S. primary care population, the authors wrote. Evidence from the 2016 review also showed limited and inconsistent support for the early identification and treatment of HSV-2 in asymptomatic individuals, including those who were pregnant.
No new evidence has emerged since 2016 regarding harms of screening or treating genital herpes in asymptomatic individuals, the authors noted. “Based on previous evidence, the USPSTF estimated that using the widely available serologic tests for HSV-2, nearly 1 of every 2 diagnoses in the general U.S. primary care population could be false,” they said. The task force also concluded that the low accuracy of the current tests could prompt unnecessary treatment for individuals with false-positive diagnoses, as well as social and emotional harm for these individuals.
During a period of public comment from Aug. 16, 2022, to Sept. 12, 2022, individuals expressed concerns that the recommendation against routine screening showed a disinclination to take herpes seriously, and concerns that asymptomatic individuals could transmit the infection to sexual partners, the authors said. However, the estimated seroprevalence of HSV-1 and HSV-2 has declined in recent decades, and other comments supported the USPSTF’s analysis of the evidence and noted their consistency with current clinical practice.
The task force noted that research gaps remain and recognized the need to improve screening and treatment of genital herpes to prevent symptomatic episodes and transmission. Specifically, the USPSTF recommendation calls for more research to assess the accuracy of screening tests, to enroll more study participants from populations disproportionately affected by HSV, to examine the effect of behavioral counseling, and to clarify associations between HSV and pregnancy outcomes. In addition, the task force called for research to create an effective vaccine to prevent genital HSV infection and to develop a cure.
Targeted screening makes sense for now
“Given the frequency and severity of the range of diseases seen with HSV and the large proportion of persons who are asymptomatic, identifying carriers through type-specific serologic screening has long been considered a plausible strategy,” Mark D. Pearlman, MD, of the University of Michigan, Ann Arbor, wrote in an accompanying editorial.
However, accuracy of the currently available serology screening tests is low, and the adverse social and psychological effects and the impact on relationships for many asymptomatic individuals who test positive and may be incorrectly identified as infected remains a concern, said Dr. Pearlman.
Although some may be disagree about the value of routine serotesting for HSV-2 in asymptomatic individuals, other strategies can reduce the spread of infection and help those infected, he said.
Many experts continue to recommend targeted serotesting to high-risk populations, such as pregnant women whose nonpregnant partner is known to have genital or oral herpes and whose own infection status or serostatus is uncertain, said Dr. Pearlman. Other targeted strategies include screening individuals with recurrent or atypical genital symptoms and negative polymerase chain reaction assay or culture results, a clinical herpes diagnosis without laboratory confirmation, or those at increased risk because of a high number of sexual partners or a history of HIV infection, he said.
“Of note, the current CDC STI guidelines and ACOG both concur with the USPSTF that routine screening in the general population or routine screening during pregnancy are not recommended,” Dr. Pearlman said. Meanwhile, research efforts continue to help reduce the impact of HSV disease and development of a more effective testing methodology “might tip the balance in favor of routine screening” in the future, he emphasized.
The recommendations were supported by the Agency for Healthcare Research and Quality. The members of the task force received reimbursement for travel and an honorarium but had no other relevant financial conflicts to disclose. Dr. Pearlman had no financial conflicts to disclose.
FROM JAMA
Can a hormone shot rescue low libido?
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
New cancer data spark outcry from patient advocates
The American Cancer Society on Jan. 13 revealed what it called “alarming” news about prostate cancer: After 2 decades of decline, the number of men diagnosed with the disease in the United States rose by 15% from 2014 to 2019.
“Most concerning,” according to the group’s CEO Karen Knudsen, PhD, MBA, is that the increase is being driven by diagnoses of advanced disease.
“Since 2011, the diagnosis of advanced-stage (regional- or distant-stage) prostate cancer has increased by 4%-5% annually and the proportion of men diagnosed with distant-stage disease has doubled,” said Dr. Knudsen at a press conference concerning the figures. “These findings underscore the importance of understanding and reducing this trend.”
The increase, which works out to be an additional 99,000 cases of prostate cancer, did not take the ACS by surprise; the group has been predicting a jump in diagnoses of the disease, which is the most common cancer in men after skin cancer, and the second most common cause of cancer death for that group.
The ACS announced a new action plan, “Improving Mortality from Prostate Cancer Together” – or IMPACT – to address the rise, especially in Black men, and to curb the increasing rate of advanced, difficult-to-treat cases.
“We must address these shifts in prostate cancer, especially in the Black community, since the incidence of prostate cancer in Black men is 70% higher than in White men and prostate cancer mortality rates in Black men are approximately two to four times higher than those in every other racial and ethnic group,” William Dahut, MD, PhD, chief scientific officer for the ACS, said at the press conference.
A study published in JAMA Network Open challenged that claim, finding that, after controlling for socioeconomic factors, race does not appear to be a significant predictor of mortality for prostate cancer.
Dr. Dahut said in an interview that IMPACT “is still [in the] early days for this initiative and more details will be coming out soon.”
Charles Ryan, MD, CEO of the Prostate Cancer Foundation, the world’s largest prostate cancer research charity, called IMPACT “extremely important work. Highlighting the disparities can only serve to benefit all men with prostate cancer, especially Black men.”
Bold action ... or passivity?
Overall cancer mortality has dropped 33% since 1991, averting an estimated 3.8 million deaths, according to ACS. But the story for prostate cancer is different.
The society and advocates had warned as recently as 2 years ago that prostate cancer was poised to rise again, especially advanced cases that may be too late to treat.
Leaders in the prostate cancer advocacy community praised the ACS plan for IMPACT, but some expressed frustration over what they said was ACS’ passivity in the face of long-anticipated increases in cases of the disease.
“I think prostate cancer was not high on their agenda,” said Rick Davis, founder of AnCan, which offers several support groups for patients with prostate cancer. “It’s good to see ACS get back into the prostate cancer game.”
Mr. Davis and patient advocate Darryl Mitteldorf, LCSW, founder of Malecare, another prostate support organization, said ACS dropped patient services for prostate cancer patients a decade ago and has not been a vocal supporter of screening for levels of prostate-specific antigen (PSA) to detect prostate cancer early.
“Early detection is supposed to be their goal,” Mr. Davis said.
In 2012, the U.S. Preventive Services Task Force recommended against PSA screening, giving it a D-rating. The move prompted attacks on the task force from most advocates and many urologists.
Following this criticism, the task force recommended shared decision-making between patient and doctor, while giving PSA screening a C-rating. Now, the ACS recommends men in general at age 50 discuss prostate cancer screening with their doctor and that Black men do the same at age 45.
Mr. Mitteldorf said ACS “owes prostate cancer patients an explanation and analysis of its response to the USPTF’s downgrade of PSA testing and how that response might be related to death and instance rates.”
Mr. Mitteldorf added that male patients lost key support from ACS when the group dismantled its Man to Man group for prostate cancer patients and its Brother to Brother group for Blacks in particular.
Dr. Dahut said Man to Man “sunsetted” and was turned over to any local organization that chose to offer it. He said longtime staff didn’t have “a lot of information about [the demise of] Brother to Brother.”
For Mr. Davis, those smaller cuts add up to a much larger insult.
“Today, in 2023, ACS continues to poke a finger in the eyes of prostate cancer patients,” he said. “Since 2010, they have not given us any respect. ACS dumped its support.”
He pointed to the group’s funding priorities, noting that outlays for prostate cancer have consistently lagged behind those for breast cancer.
The ACS spent $25.3 million on breast cancer research and $6.7 million for prostate cancer in 2018, and in 2023 will designate $126.5 for breast cancer research and $43.9 million for prostate cancer.
ACS has earmarked $62 million this year for lung cancer programs and $61 million for colorectal cancer.
“Parity between breast cancer and prostate cancer would be a good start in sizing the IMPACT program,” Mr. Davis said. “After all, breast cancer and prostate cancer are hardly different in numbers today.”
Dr. Dahut denied any gender bias in research funding. He said the group makes funding decisions “based on finding the most impactful science regardless of tumor type. Our mission includes funding every cancer, every day; thus, we generally do not go into our funding cycle with any set-asides for a particular cancer.”
Mr. Davis also said the ACS data suggest the growing number of prostate cancer cases is even worse than the group has said. Although the society cites a 3% annual increase in prostate cancer diagnoses from 2014 to 2019, since 2019 the annual increase is a much more dramatic 16%. Meanwhile, the number of new cases of the disease is projected to rise from 175,000 per year in 2019 to 288,000 this year.
Dr. Dahut said the society used the 2014-2019 time frame for technical reasons, separating confirmed cases in the earlier period from estimated cases in recent years.
“We discourage comparing projected cases over time because these cases are model-based and subject to fluctuations,” Dr. Dahut said.
A version of this article originally appeared on Medscape.com.
The American Cancer Society on Jan. 13 revealed what it called “alarming” news about prostate cancer: After 2 decades of decline, the number of men diagnosed with the disease in the United States rose by 15% from 2014 to 2019.
“Most concerning,” according to the group’s CEO Karen Knudsen, PhD, MBA, is that the increase is being driven by diagnoses of advanced disease.
“Since 2011, the diagnosis of advanced-stage (regional- or distant-stage) prostate cancer has increased by 4%-5% annually and the proportion of men diagnosed with distant-stage disease has doubled,” said Dr. Knudsen at a press conference concerning the figures. “These findings underscore the importance of understanding and reducing this trend.”
The increase, which works out to be an additional 99,000 cases of prostate cancer, did not take the ACS by surprise; the group has been predicting a jump in diagnoses of the disease, which is the most common cancer in men after skin cancer, and the second most common cause of cancer death for that group.
The ACS announced a new action plan, “Improving Mortality from Prostate Cancer Together” – or IMPACT – to address the rise, especially in Black men, and to curb the increasing rate of advanced, difficult-to-treat cases.
“We must address these shifts in prostate cancer, especially in the Black community, since the incidence of prostate cancer in Black men is 70% higher than in White men and prostate cancer mortality rates in Black men are approximately two to four times higher than those in every other racial and ethnic group,” William Dahut, MD, PhD, chief scientific officer for the ACS, said at the press conference.
A study published in JAMA Network Open challenged that claim, finding that, after controlling for socioeconomic factors, race does not appear to be a significant predictor of mortality for prostate cancer.
Dr. Dahut said in an interview that IMPACT “is still [in the] early days for this initiative and more details will be coming out soon.”
Charles Ryan, MD, CEO of the Prostate Cancer Foundation, the world’s largest prostate cancer research charity, called IMPACT “extremely important work. Highlighting the disparities can only serve to benefit all men with prostate cancer, especially Black men.”
Bold action ... or passivity?
Overall cancer mortality has dropped 33% since 1991, averting an estimated 3.8 million deaths, according to ACS. But the story for prostate cancer is different.
The society and advocates had warned as recently as 2 years ago that prostate cancer was poised to rise again, especially advanced cases that may be too late to treat.
Leaders in the prostate cancer advocacy community praised the ACS plan for IMPACT, but some expressed frustration over what they said was ACS’ passivity in the face of long-anticipated increases in cases of the disease.
“I think prostate cancer was not high on their agenda,” said Rick Davis, founder of AnCan, which offers several support groups for patients with prostate cancer. “It’s good to see ACS get back into the prostate cancer game.”
Mr. Davis and patient advocate Darryl Mitteldorf, LCSW, founder of Malecare, another prostate support organization, said ACS dropped patient services for prostate cancer patients a decade ago and has not been a vocal supporter of screening for levels of prostate-specific antigen (PSA) to detect prostate cancer early.
“Early detection is supposed to be their goal,” Mr. Davis said.
In 2012, the U.S. Preventive Services Task Force recommended against PSA screening, giving it a D-rating. The move prompted attacks on the task force from most advocates and many urologists.
Following this criticism, the task force recommended shared decision-making between patient and doctor, while giving PSA screening a C-rating. Now, the ACS recommends men in general at age 50 discuss prostate cancer screening with their doctor and that Black men do the same at age 45.
Mr. Mitteldorf said ACS “owes prostate cancer patients an explanation and analysis of its response to the USPTF’s downgrade of PSA testing and how that response might be related to death and instance rates.”
Mr. Mitteldorf added that male patients lost key support from ACS when the group dismantled its Man to Man group for prostate cancer patients and its Brother to Brother group for Blacks in particular.
Dr. Dahut said Man to Man “sunsetted” and was turned over to any local organization that chose to offer it. He said longtime staff didn’t have “a lot of information about [the demise of] Brother to Brother.”
For Mr. Davis, those smaller cuts add up to a much larger insult.
“Today, in 2023, ACS continues to poke a finger in the eyes of prostate cancer patients,” he said. “Since 2010, they have not given us any respect. ACS dumped its support.”
He pointed to the group’s funding priorities, noting that outlays for prostate cancer have consistently lagged behind those for breast cancer.
The ACS spent $25.3 million on breast cancer research and $6.7 million for prostate cancer in 2018, and in 2023 will designate $126.5 for breast cancer research and $43.9 million for prostate cancer.
ACS has earmarked $62 million this year for lung cancer programs and $61 million for colorectal cancer.
“Parity between breast cancer and prostate cancer would be a good start in sizing the IMPACT program,” Mr. Davis said. “After all, breast cancer and prostate cancer are hardly different in numbers today.”
Dr. Dahut denied any gender bias in research funding. He said the group makes funding decisions “based on finding the most impactful science regardless of tumor type. Our mission includes funding every cancer, every day; thus, we generally do not go into our funding cycle with any set-asides for a particular cancer.”
Mr. Davis also said the ACS data suggest the growing number of prostate cancer cases is even worse than the group has said. Although the society cites a 3% annual increase in prostate cancer diagnoses from 2014 to 2019, since 2019 the annual increase is a much more dramatic 16%. Meanwhile, the number of new cases of the disease is projected to rise from 175,000 per year in 2019 to 288,000 this year.
Dr. Dahut said the society used the 2014-2019 time frame for technical reasons, separating confirmed cases in the earlier period from estimated cases in recent years.
“We discourage comparing projected cases over time because these cases are model-based and subject to fluctuations,” Dr. Dahut said.
A version of this article originally appeared on Medscape.com.
The American Cancer Society on Jan. 13 revealed what it called “alarming” news about prostate cancer: After 2 decades of decline, the number of men diagnosed with the disease in the United States rose by 15% from 2014 to 2019.
“Most concerning,” according to the group’s CEO Karen Knudsen, PhD, MBA, is that the increase is being driven by diagnoses of advanced disease.
“Since 2011, the diagnosis of advanced-stage (regional- or distant-stage) prostate cancer has increased by 4%-5% annually and the proportion of men diagnosed with distant-stage disease has doubled,” said Dr. Knudsen at a press conference concerning the figures. “These findings underscore the importance of understanding and reducing this trend.”
The increase, which works out to be an additional 99,000 cases of prostate cancer, did not take the ACS by surprise; the group has been predicting a jump in diagnoses of the disease, which is the most common cancer in men after skin cancer, and the second most common cause of cancer death for that group.
The ACS announced a new action plan, “Improving Mortality from Prostate Cancer Together” – or IMPACT – to address the rise, especially in Black men, and to curb the increasing rate of advanced, difficult-to-treat cases.
“We must address these shifts in prostate cancer, especially in the Black community, since the incidence of prostate cancer in Black men is 70% higher than in White men and prostate cancer mortality rates in Black men are approximately two to four times higher than those in every other racial and ethnic group,” William Dahut, MD, PhD, chief scientific officer for the ACS, said at the press conference.
A study published in JAMA Network Open challenged that claim, finding that, after controlling for socioeconomic factors, race does not appear to be a significant predictor of mortality for prostate cancer.
Dr. Dahut said in an interview that IMPACT “is still [in the] early days for this initiative and more details will be coming out soon.”
Charles Ryan, MD, CEO of the Prostate Cancer Foundation, the world’s largest prostate cancer research charity, called IMPACT “extremely important work. Highlighting the disparities can only serve to benefit all men with prostate cancer, especially Black men.”
Bold action ... or passivity?
Overall cancer mortality has dropped 33% since 1991, averting an estimated 3.8 million deaths, according to ACS. But the story for prostate cancer is different.
The society and advocates had warned as recently as 2 years ago that prostate cancer was poised to rise again, especially advanced cases that may be too late to treat.
Leaders in the prostate cancer advocacy community praised the ACS plan for IMPACT, but some expressed frustration over what they said was ACS’ passivity in the face of long-anticipated increases in cases of the disease.
“I think prostate cancer was not high on their agenda,” said Rick Davis, founder of AnCan, which offers several support groups for patients with prostate cancer. “It’s good to see ACS get back into the prostate cancer game.”
Mr. Davis and patient advocate Darryl Mitteldorf, LCSW, founder of Malecare, another prostate support organization, said ACS dropped patient services for prostate cancer patients a decade ago and has not been a vocal supporter of screening for levels of prostate-specific antigen (PSA) to detect prostate cancer early.
“Early detection is supposed to be their goal,” Mr. Davis said.
In 2012, the U.S. Preventive Services Task Force recommended against PSA screening, giving it a D-rating. The move prompted attacks on the task force from most advocates and many urologists.
Following this criticism, the task force recommended shared decision-making between patient and doctor, while giving PSA screening a C-rating. Now, the ACS recommends men in general at age 50 discuss prostate cancer screening with their doctor and that Black men do the same at age 45.
Mr. Mitteldorf said ACS “owes prostate cancer patients an explanation and analysis of its response to the USPTF’s downgrade of PSA testing and how that response might be related to death and instance rates.”
Mr. Mitteldorf added that male patients lost key support from ACS when the group dismantled its Man to Man group for prostate cancer patients and its Brother to Brother group for Blacks in particular.
Dr. Dahut said Man to Man “sunsetted” and was turned over to any local organization that chose to offer it. He said longtime staff didn’t have “a lot of information about [the demise of] Brother to Brother.”
For Mr. Davis, those smaller cuts add up to a much larger insult.
“Today, in 2023, ACS continues to poke a finger in the eyes of prostate cancer patients,” he said. “Since 2010, they have not given us any respect. ACS dumped its support.”
He pointed to the group’s funding priorities, noting that outlays for prostate cancer have consistently lagged behind those for breast cancer.
The ACS spent $25.3 million on breast cancer research and $6.7 million for prostate cancer in 2018, and in 2023 will designate $126.5 for breast cancer research and $43.9 million for prostate cancer.
ACS has earmarked $62 million this year for lung cancer programs and $61 million for colorectal cancer.
“Parity between breast cancer and prostate cancer would be a good start in sizing the IMPACT program,” Mr. Davis said. “After all, breast cancer and prostate cancer are hardly different in numbers today.”
Dr. Dahut denied any gender bias in research funding. He said the group makes funding decisions “based on finding the most impactful science regardless of tumor type. Our mission includes funding every cancer, every day; thus, we generally do not go into our funding cycle with any set-asides for a particular cancer.”
Mr. Davis also said the ACS data suggest the growing number of prostate cancer cases is even worse than the group has said. Although the society cites a 3% annual increase in prostate cancer diagnoses from 2014 to 2019, since 2019 the annual increase is a much more dramatic 16%. Meanwhile, the number of new cases of the disease is projected to rise from 175,000 per year in 2019 to 288,000 this year.
Dr. Dahut said the society used the 2014-2019 time frame for technical reasons, separating confirmed cases in the earlier period from estimated cases in recent years.
“We discourage comparing projected cases over time because these cases are model-based and subject to fluctuations,” Dr. Dahut said.
A version of this article originally appeared on Medscape.com.
Atrial fibrillation: Sex differences and modifiable risk factors
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
New osteoporosis guideline says start with a bisphosphonate
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
FROM THE ANNALS OF INTERNAL MEDICINE
