User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
test publish
test for unpublish
test for unpublish
test for unpublish
Is SNRI Treatment of Fibromyalgia Working? Look at Sleep Patterns
Not a morning person? For patients with fibromyalgia, the answer to that question could be a clue about their treatment response with a serotonin and norepinephrine reuptake inhibitor (SNRI), suggested a new cross-sectional study published in Rheumatology International.
Compared with patients who had 30% or more pain relief after 8 or more weeks on an SNRI (duloxetine, venlafaxine, or milnacipran), those with less pain relief reported rougher mornings and worse sleep overall. Morningness, morning affect, diurnal dysrhythmia, anytime wakeability, overall sleep quality, subjective sleep quality and disturbances, sleep medication use, and daytime dysfunction were all predictors of nonresponse to SNRI treatment.
“The observed chronobiological characteristics of patients resistant to SNRI treatment are important because they can be targeted with adjunctive circadian interventions, ie, morning light therapy, in order to normalize circadian rhythms and improve sleep, and in effect, overcome the resistance to treatment and alleviate [the] patient’s pain,” said study author Anna Julia Krupa, MD, a psychiatrist and research assistant in the Department of Affective Disorders at Jagiellonian University Medical College, Kraków, Poland.
Fibromyalgia symptoms like sleep disturbance, low mood, fatigue, stiffness, cognitive impairment, and anxiety are often interlinked in positive feedback loops, meaning that the presence of one symptom (ie, sleep problems or depression) exacerbates the other (ie, pain or anxiety), Dr. Krupa said. While SNRIs can reduce pain, anxiety, and depression, they don’t directly improve sleep. Sometimes, pain relief smooths out minor sleep problems, but not always.
“Therefore, if circadian rhythm disruptions and sleep problems are significant, they may constitute a factor which limits SNRI effects on pain in people with fibromyalgia,” Dr. Krupa said.
With 60 patients with fibromyalgia (30 responsive to treatment and 30 nonresponsive to treatment) and 30 healthy controls, this was a small study, noted Daniel G. Arkfeld, MD, DDS, a rheumatologist and associate professor of clinical medicine at Keck School of Medicine, University of Southern California, Los Angeles. However, “sleep is probably one of the most difficult things in fibromyalgia, and it definitely needs to be targeted.”
Decades of research suggest that important neurochemicals, like growth hormone, are released in deep sleep. “We know that sleep disturbances and time frame and release of neurochemicals [are] all super important in fibromyalgia,” he said.
Side effects of medication could be another factor at play here. As with any drug, the side effects of SNRIs vary widely from person to person, but palpitations, tremulousness, and insomnia are common, said Daniel J. Clauw, MD, professor of anesthesiology, internal medicine/rheumatology, and psychiatry and director of the Chronic Pain & Fatigue Research Center at the University of Michigan, Ann Arbor.
“SNRIs are often ‘activating’ because of the increase in norepinephrine,” Dr. Clauw said. “This is often helpful for symptoms such as fatigue and memory problems — but could worsen sleep.”
That’s why he always recommends that patients take an SNRI in the morning, not at night. Try that and the following tips to help patients with fibromyalgia sleep better and feel better, too.
Start with the basics. It’s worth reminding patients about the tried-and-true tips like going to bed and waking up at the same time every day and keeping your bedroom quiet and dark. “Patients should first try ‘sleep hygiene’ strategies,” said Dr. Clauw. “If that doesn’t help then cognitive-behavioral therapy (CBT) for insomnia can be very helpful.”
A systematic review and meta-analysis showed that CBT for insomnia helped patients with fibromyalgia improve sleep quality, pain, anxiety, and depression compared with nonpharmacologic treatments. And if that doesn’t help? “If need be, they can try nonbenzodiazepine hypnotic drugs, eg, tricyclics or gabapentinoids taken at bedtime,” said Dr. Clauw.
Help them fall in love with exercise. A personalized approach to exercise can help patients with fibromyalgia feel better, suggested a study review in Clinical and Experimental Rheumatology. Exercise can also help reset the circadian clock. Morning activity helps night owls get on an earlier schedule, suggested a study review published in Physical Activity and Nutrition.
Consider yoga, tai chi, or qigong. A study review published in Seminars in Arthritis and Rheumatism suggested mind-body and combined exercises help improve sleep for people with fibromyalgia, while aerobic or strength training alone does not. One explanation is that mind-body exercises might do more than other types to tamp down sympathetic-excitatory overactivation in fibromyalgia, the researchers said. Use this handy guide from the European Pain Federation to help you start the exercise conversation.
Talk about sleep alongside other aspects of fibromyalgia. Psychoeducation for fibromyalgia often includes information about the distinction between acute and chronic pain, the nature of fibromyalgia syndrome, disease-contributing factors, safe and effective treatments, symptoms and characteristics, and coping strategies, according to a study review in the journal Behavioral Sciences. “As a psychiatrist and someone who often consults patients with fibromyalgia, I would also add the information about links between pain and mood, anxiety as well as sleep,” said Dr. Krupa.
Try morning light. Use light to shift circadian rhythms, suggested Dr. Krupa. People who struggle in the morning might benefit from 30-60 minutes of morning light therapy immediately after waking using a 10,000-lux light box or light glasses, as suggested by a study review from the University of Michigan.
Help them get off the night shift. “Fibromyalgia patients probably shouldn’t work the night shift and throw their circadian rhythm off,” said Dr. Arkfeld. Depending on a patient’s work and financial circumstances, a job change might not be possible, but consider writing a note to the patient’s employer asking them to switch the patient to the day shift. Dr. Arkfeld said this approach has worked for some of his patients.
Refer them for a sleep study. Many patients with fibromyalgia have obstructive sleep apnea or other sleep disorders that require additional intervention. “Sleep studies are important to kind of define the actual sleep problem that’s occurring as well, whether it’s the stage for interruption of sleep or sleep apnea or wakefulness,” said Dr. Arkfeld.
The study was funded by Jagiellonian University Medical College. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Not a morning person? For patients with fibromyalgia, the answer to that question could be a clue about their treatment response with a serotonin and norepinephrine reuptake inhibitor (SNRI), suggested a new cross-sectional study published in Rheumatology International.
Compared with patients who had 30% or more pain relief after 8 or more weeks on an SNRI (duloxetine, venlafaxine, or milnacipran), those with less pain relief reported rougher mornings and worse sleep overall. Morningness, morning affect, diurnal dysrhythmia, anytime wakeability, overall sleep quality, subjective sleep quality and disturbances, sleep medication use, and daytime dysfunction were all predictors of nonresponse to SNRI treatment.
“The observed chronobiological characteristics of patients resistant to SNRI treatment are important because they can be targeted with adjunctive circadian interventions, ie, morning light therapy, in order to normalize circadian rhythms and improve sleep, and in effect, overcome the resistance to treatment and alleviate [the] patient’s pain,” said study author Anna Julia Krupa, MD, a psychiatrist and research assistant in the Department of Affective Disorders at Jagiellonian University Medical College, Kraków, Poland.
Fibromyalgia symptoms like sleep disturbance, low mood, fatigue, stiffness, cognitive impairment, and anxiety are often interlinked in positive feedback loops, meaning that the presence of one symptom (ie, sleep problems or depression) exacerbates the other (ie, pain or anxiety), Dr. Krupa said. While SNRIs can reduce pain, anxiety, and depression, they don’t directly improve sleep. Sometimes, pain relief smooths out minor sleep problems, but not always.
“Therefore, if circadian rhythm disruptions and sleep problems are significant, they may constitute a factor which limits SNRI effects on pain in people with fibromyalgia,” Dr. Krupa said.
With 60 patients with fibromyalgia (30 responsive to treatment and 30 nonresponsive to treatment) and 30 healthy controls, this was a small study, noted Daniel G. Arkfeld, MD, DDS, a rheumatologist and associate professor of clinical medicine at Keck School of Medicine, University of Southern California, Los Angeles. However, “sleep is probably one of the most difficult things in fibromyalgia, and it definitely needs to be targeted.”
Decades of research suggest that important neurochemicals, like growth hormone, are released in deep sleep. “We know that sleep disturbances and time frame and release of neurochemicals [are] all super important in fibromyalgia,” he said.
Side effects of medication could be another factor at play here. As with any drug, the side effects of SNRIs vary widely from person to person, but palpitations, tremulousness, and insomnia are common, said Daniel J. Clauw, MD, professor of anesthesiology, internal medicine/rheumatology, and psychiatry and director of the Chronic Pain & Fatigue Research Center at the University of Michigan, Ann Arbor.
“SNRIs are often ‘activating’ because of the increase in norepinephrine,” Dr. Clauw said. “This is often helpful for symptoms such as fatigue and memory problems — but could worsen sleep.”
That’s why he always recommends that patients take an SNRI in the morning, not at night. Try that and the following tips to help patients with fibromyalgia sleep better and feel better, too.
Start with the basics. It’s worth reminding patients about the tried-and-true tips like going to bed and waking up at the same time every day and keeping your bedroom quiet and dark. “Patients should first try ‘sleep hygiene’ strategies,” said Dr. Clauw. “If that doesn’t help then cognitive-behavioral therapy (CBT) for insomnia can be very helpful.”
A systematic review and meta-analysis showed that CBT for insomnia helped patients with fibromyalgia improve sleep quality, pain, anxiety, and depression compared with nonpharmacologic treatments. And if that doesn’t help? “If need be, they can try nonbenzodiazepine hypnotic drugs, eg, tricyclics or gabapentinoids taken at bedtime,” said Dr. Clauw.
Help them fall in love with exercise. A personalized approach to exercise can help patients with fibromyalgia feel better, suggested a study review in Clinical and Experimental Rheumatology. Exercise can also help reset the circadian clock. Morning activity helps night owls get on an earlier schedule, suggested a study review published in Physical Activity and Nutrition.
Consider yoga, tai chi, or qigong. A study review published in Seminars in Arthritis and Rheumatism suggested mind-body and combined exercises help improve sleep for people with fibromyalgia, while aerobic or strength training alone does not. One explanation is that mind-body exercises might do more than other types to tamp down sympathetic-excitatory overactivation in fibromyalgia, the researchers said. Use this handy guide from the European Pain Federation to help you start the exercise conversation.
Talk about sleep alongside other aspects of fibromyalgia. Psychoeducation for fibromyalgia often includes information about the distinction between acute and chronic pain, the nature of fibromyalgia syndrome, disease-contributing factors, safe and effective treatments, symptoms and characteristics, and coping strategies, according to a study review in the journal Behavioral Sciences. “As a psychiatrist and someone who often consults patients with fibromyalgia, I would also add the information about links between pain and mood, anxiety as well as sleep,” said Dr. Krupa.
Try morning light. Use light to shift circadian rhythms, suggested Dr. Krupa. People who struggle in the morning might benefit from 30-60 minutes of morning light therapy immediately after waking using a 10,000-lux light box or light glasses, as suggested by a study review from the University of Michigan.
Help them get off the night shift. “Fibromyalgia patients probably shouldn’t work the night shift and throw their circadian rhythm off,” said Dr. Arkfeld. Depending on a patient’s work and financial circumstances, a job change might not be possible, but consider writing a note to the patient’s employer asking them to switch the patient to the day shift. Dr. Arkfeld said this approach has worked for some of his patients.
Refer them for a sleep study. Many patients with fibromyalgia have obstructive sleep apnea or other sleep disorders that require additional intervention. “Sleep studies are important to kind of define the actual sleep problem that’s occurring as well, whether it’s the stage for interruption of sleep or sleep apnea or wakefulness,” said Dr. Arkfeld.
The study was funded by Jagiellonian University Medical College. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Not a morning person? For patients with fibromyalgia, the answer to that question could be a clue about their treatment response with a serotonin and norepinephrine reuptake inhibitor (SNRI), suggested a new cross-sectional study published in Rheumatology International.
Compared with patients who had 30% or more pain relief after 8 or more weeks on an SNRI (duloxetine, venlafaxine, or milnacipran), those with less pain relief reported rougher mornings and worse sleep overall. Morningness, morning affect, diurnal dysrhythmia, anytime wakeability, overall sleep quality, subjective sleep quality and disturbances, sleep medication use, and daytime dysfunction were all predictors of nonresponse to SNRI treatment.
“The observed chronobiological characteristics of patients resistant to SNRI treatment are important because they can be targeted with adjunctive circadian interventions, ie, morning light therapy, in order to normalize circadian rhythms and improve sleep, and in effect, overcome the resistance to treatment and alleviate [the] patient’s pain,” said study author Anna Julia Krupa, MD, a psychiatrist and research assistant in the Department of Affective Disorders at Jagiellonian University Medical College, Kraków, Poland.
Fibromyalgia symptoms like sleep disturbance, low mood, fatigue, stiffness, cognitive impairment, and anxiety are often interlinked in positive feedback loops, meaning that the presence of one symptom (ie, sleep problems or depression) exacerbates the other (ie, pain or anxiety), Dr. Krupa said. While SNRIs can reduce pain, anxiety, and depression, they don’t directly improve sleep. Sometimes, pain relief smooths out minor sleep problems, but not always.
“Therefore, if circadian rhythm disruptions and sleep problems are significant, they may constitute a factor which limits SNRI effects on pain in people with fibromyalgia,” Dr. Krupa said.
With 60 patients with fibromyalgia (30 responsive to treatment and 30 nonresponsive to treatment) and 30 healthy controls, this was a small study, noted Daniel G. Arkfeld, MD, DDS, a rheumatologist and associate professor of clinical medicine at Keck School of Medicine, University of Southern California, Los Angeles. However, “sleep is probably one of the most difficult things in fibromyalgia, and it definitely needs to be targeted.”
Decades of research suggest that important neurochemicals, like growth hormone, are released in deep sleep. “We know that sleep disturbances and time frame and release of neurochemicals [are] all super important in fibromyalgia,” he said.
Side effects of medication could be another factor at play here. As with any drug, the side effects of SNRIs vary widely from person to person, but palpitations, tremulousness, and insomnia are common, said Daniel J. Clauw, MD, professor of anesthesiology, internal medicine/rheumatology, and psychiatry and director of the Chronic Pain & Fatigue Research Center at the University of Michigan, Ann Arbor.
“SNRIs are often ‘activating’ because of the increase in norepinephrine,” Dr. Clauw said. “This is often helpful for symptoms such as fatigue and memory problems — but could worsen sleep.”
That’s why he always recommends that patients take an SNRI in the morning, not at night. Try that and the following tips to help patients with fibromyalgia sleep better and feel better, too.
Start with the basics. It’s worth reminding patients about the tried-and-true tips like going to bed and waking up at the same time every day and keeping your bedroom quiet and dark. “Patients should first try ‘sleep hygiene’ strategies,” said Dr. Clauw. “If that doesn’t help then cognitive-behavioral therapy (CBT) for insomnia can be very helpful.”
A systematic review and meta-analysis showed that CBT for insomnia helped patients with fibromyalgia improve sleep quality, pain, anxiety, and depression compared with nonpharmacologic treatments. And if that doesn’t help? “If need be, they can try nonbenzodiazepine hypnotic drugs, eg, tricyclics or gabapentinoids taken at bedtime,” said Dr. Clauw.
Help them fall in love with exercise. A personalized approach to exercise can help patients with fibromyalgia feel better, suggested a study review in Clinical and Experimental Rheumatology. Exercise can also help reset the circadian clock. Morning activity helps night owls get on an earlier schedule, suggested a study review published in Physical Activity and Nutrition.
Consider yoga, tai chi, or qigong. A study review published in Seminars in Arthritis and Rheumatism suggested mind-body and combined exercises help improve sleep for people with fibromyalgia, while aerobic or strength training alone does not. One explanation is that mind-body exercises might do more than other types to tamp down sympathetic-excitatory overactivation in fibromyalgia, the researchers said. Use this handy guide from the European Pain Federation to help you start the exercise conversation.
Talk about sleep alongside other aspects of fibromyalgia. Psychoeducation for fibromyalgia often includes information about the distinction between acute and chronic pain, the nature of fibromyalgia syndrome, disease-contributing factors, safe and effective treatments, symptoms and characteristics, and coping strategies, according to a study review in the journal Behavioral Sciences. “As a psychiatrist and someone who often consults patients with fibromyalgia, I would also add the information about links between pain and mood, anxiety as well as sleep,” said Dr. Krupa.
Try morning light. Use light to shift circadian rhythms, suggested Dr. Krupa. People who struggle in the morning might benefit from 30-60 minutes of morning light therapy immediately after waking using a 10,000-lux light box or light glasses, as suggested by a study review from the University of Michigan.
Help them get off the night shift. “Fibromyalgia patients probably shouldn’t work the night shift and throw their circadian rhythm off,” said Dr. Arkfeld. Depending on a patient’s work and financial circumstances, a job change might not be possible, but consider writing a note to the patient’s employer asking them to switch the patient to the day shift. Dr. Arkfeld said this approach has worked for some of his patients.
Refer them for a sleep study. Many patients with fibromyalgia have obstructive sleep apnea or other sleep disorders that require additional intervention. “Sleep studies are important to kind of define the actual sleep problem that’s occurring as well, whether it’s the stage for interruption of sleep or sleep apnea or wakefulness,” said Dr. Arkfeld.
The study was funded by Jagiellonian University Medical College. The authors had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM RHEUMATOLOGY INTERNATIONAL
The Digital Side Effects
On July 19, what was supposed to be a harmless software upgrade brought down a huge chunk of the health care, banking, flight, and travel systems.
While my dinky little practice wasn’t affected, several of my patients were in other ways. Tests that had to be rescheduled, flights canceled ... inconveniences, but not life altering.
Things are allegedly fixed (at least until next time) but there may be fallout down the road. People who had delayed medical procedures could have a different prognosis depending on what the results showed when they were done. Hopefully this won’t happen.
But it’s a reminder of how vulnerable our whole world is to disruption of the internet, not to mention the power grid and software systems. Paper is time consuming, and takes up a lot of space, but as long as you have a decent pen and enough light to read it you’re fine.
I’m not saying we should go back to paper. It’s more expensive in the long run, takes up shelf and closet space, kills trees, has to be shredded after a time, and turns yellow around the edges. It also makes it a pain to copy and transfer records. With paper I wouldn’t be able to take all my charts with me to refer to when I leave town on a busman’s holiday. The benefits of digital far outstrip paper or we wouldn’t have switched in the first place.
But it’s still kind of scary to realize how much we depend on software to keep things running smoothly. The events of July 19 were unintentional. Someone looking to cause real trouble could do worse — and there are plenty out there who would love to — and we’re putting our faith in companies like CrowdStrike to protect us from them.
But, on the flip side, we’re asking others to do the same. We often use the phrase “trust me, I’m a doctor,” in jest, but the point is there. People come to us because we have knowledge and training they don’t, and they’re hoping we can help them. We spent a lot of time getting to the point where we can hang up a sign that says so. And we, like everyone else, are not infallible.
We’re individuals, not machines. Both are fallible, though in different ways. In CrowdStrike’s case the machines didn’t fail, they just did what the humans told them to do. Which didn’t work.
The bottom line is that even the most well-meaning will make mistakes.
But it’s still pretty scary because, even unintentionally, there will be a next time. And between now and then our world will become even more dependent on these systems. None of us want to go back to the preconnected era, it’s too much a part of our daily lives.
Like the long list of potential side effects on any drug we prescribe, it’s a trade-off that we’ve accepted. And at this point we aren’t going back.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
On July 19, what was supposed to be a harmless software upgrade brought down a huge chunk of the health care, banking, flight, and travel systems.
While my dinky little practice wasn’t affected, several of my patients were in other ways. Tests that had to be rescheduled, flights canceled ... inconveniences, but not life altering.
Things are allegedly fixed (at least until next time) but there may be fallout down the road. People who had delayed medical procedures could have a different prognosis depending on what the results showed when they were done. Hopefully this won’t happen.
But it’s a reminder of how vulnerable our whole world is to disruption of the internet, not to mention the power grid and software systems. Paper is time consuming, and takes up a lot of space, but as long as you have a decent pen and enough light to read it you’re fine.
I’m not saying we should go back to paper. It’s more expensive in the long run, takes up shelf and closet space, kills trees, has to be shredded after a time, and turns yellow around the edges. It also makes it a pain to copy and transfer records. With paper I wouldn’t be able to take all my charts with me to refer to when I leave town on a busman’s holiday. The benefits of digital far outstrip paper or we wouldn’t have switched in the first place.
But it’s still kind of scary to realize how much we depend on software to keep things running smoothly. The events of July 19 were unintentional. Someone looking to cause real trouble could do worse — and there are plenty out there who would love to — and we’re putting our faith in companies like CrowdStrike to protect us from them.
But, on the flip side, we’re asking others to do the same. We often use the phrase “trust me, I’m a doctor,” in jest, but the point is there. People come to us because we have knowledge and training they don’t, and they’re hoping we can help them. We spent a lot of time getting to the point where we can hang up a sign that says so. And we, like everyone else, are not infallible.
We’re individuals, not machines. Both are fallible, though in different ways. In CrowdStrike’s case the machines didn’t fail, they just did what the humans told them to do. Which didn’t work.
The bottom line is that even the most well-meaning will make mistakes.
But it’s still pretty scary because, even unintentionally, there will be a next time. And between now and then our world will become even more dependent on these systems. None of us want to go back to the preconnected era, it’s too much a part of our daily lives.
Like the long list of potential side effects on any drug we prescribe, it’s a trade-off that we’ve accepted. And at this point we aren’t going back.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
On July 19, what was supposed to be a harmless software upgrade brought down a huge chunk of the health care, banking, flight, and travel systems.
While my dinky little practice wasn’t affected, several of my patients were in other ways. Tests that had to be rescheduled, flights canceled ... inconveniences, but not life altering.
Things are allegedly fixed (at least until next time) but there may be fallout down the road. People who had delayed medical procedures could have a different prognosis depending on what the results showed when they were done. Hopefully this won’t happen.
But it’s a reminder of how vulnerable our whole world is to disruption of the internet, not to mention the power grid and software systems. Paper is time consuming, and takes up a lot of space, but as long as you have a decent pen and enough light to read it you’re fine.
I’m not saying we should go back to paper. It’s more expensive in the long run, takes up shelf and closet space, kills trees, has to be shredded after a time, and turns yellow around the edges. It also makes it a pain to copy and transfer records. With paper I wouldn’t be able to take all my charts with me to refer to when I leave town on a busman’s holiday. The benefits of digital far outstrip paper or we wouldn’t have switched in the first place.
But it’s still kind of scary to realize how much we depend on software to keep things running smoothly. The events of July 19 were unintentional. Someone looking to cause real trouble could do worse — and there are plenty out there who would love to — and we’re putting our faith in companies like CrowdStrike to protect us from them.
But, on the flip side, we’re asking others to do the same. We often use the phrase “trust me, I’m a doctor,” in jest, but the point is there. People come to us because we have knowledge and training they don’t, and they’re hoping we can help them. We spent a lot of time getting to the point where we can hang up a sign that says so. And we, like everyone else, are not infallible.
We’re individuals, not machines. Both are fallible, though in different ways. In CrowdStrike’s case the machines didn’t fail, they just did what the humans told them to do. Which didn’t work.
The bottom line is that even the most well-meaning will make mistakes.
But it’s still pretty scary because, even unintentionally, there will be a next time. And between now and then our world will become even more dependent on these systems. None of us want to go back to the preconnected era, it’s too much a part of our daily lives.
Like the long list of potential side effects on any drug we prescribe, it’s a trade-off that we’ve accepted. And at this point we aren’t going back.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
Light Therapy, Phototherapy, Photobiomodulation: New Ways to Heal With Light
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
Navigating Election Anxiety: How Worry Affects the Brain
Once again, America is deeply divided before a national election, with people on each side convinced of the horrors that will be visited upon us if the other side wins.
’Tis the season — and regrettably, not to be jolly but to be worried.
As a neuroscientist, I am especially aware of the deleterious mental and physical impact of chronic worry on our citizenry. That’s because worry is not “all in your head.” We modern humans live in a world of worry which appears to be progressively growing.
Flight or Fight
Worry stems from the brain’s rather remarkable ability to foresee and reflexively respond to threat. Our “fight or flight” brain machinery probably arose in our vertebrate ancestors more than 300 million years ago. The fact that we have machinery akin to that possessed by lizards or tigers or shrews is testimony to its crucial contribution to our species’ survival.
As the phrase “fight or flight” suggests, a brain that senses trouble immediately biases certain body and brain functions. As it shifts into a higher-alert mode, it increases the energy supplies in our blood and supports other changes that facilitate faster and stronger reactions, while it shuts down less essential processes which do not contribute to hiding, fighting, or running like hell.
This hyperreactive response is initiated in the amygdala in the anterior brain, which identifies “what’s happening” as immediately or potentially threatening. The now-activated amygdala generates a response in the hypothalamus that provokes an immediate increase of adrenaline and cortisol in the body, and cortisol and noradrenaline in the brain. Both sharply speed up our physical and neurologic reactivity. In the brain, that is achieved by increasing the level of excitability of neurons across the forebrain. Depending on the perceived level of threat, an excitable brain will be just a little or a lot more “on alert,” just a little or a lot faster to respond, and just a little or a lot better at remembering the specific “warning” events that trigger this lizard-brain response.
Alas, this machinery was designed to be engaged every so often when a potentially dangerous surprise arises in life. When the worry and stress are persistent, the brain experiences a kind of neurologic “burn-out” of its fight versus flight machinery.
Dangers of Nonstop Anxiety and Stress
A consistently stressed-out brain turns down its production and release of noradrenaline, and the brain becomes less attentive, less engaged. This sets the brain on the path to an anxiety (and then a depressive) disorder, and, in the longer term, to cognitive losses in memory and executive control systems, and to emotional distortions that can lead to substance abuse or other addictions.
Our political distress is but one source of persistent worry and stress. Worry is a modern plague. The head counts of individuals seeking psychiatric or psychological health are at an all-time high in the United States. Near-universal low-level stressors, such as 2 years of COVID, insecurities about the changing demands of our professional and private lives, and a deeply divided body politic are unequivocally affecting American brain health.
The brain also collaborates in our body’s response to stress. Its regulation of hormonal responses and its autonomic nervous system’s mediated responses contribute to elevated blood sugar levels, to craving high-sugar foods, to elevated blood pressure, and to weaker immune responses. This all contributes to higher risks for cardiovascular and other dietary- and immune system–related disease. And ultimately, to shorter lifespans.
Strategies to Address Neurologic Changes Arising From Chronic Stress
There are many things you can try to bring your worry back to a manageable (and even productive) level.
- Engage in a “reset” strategy several times a day to bring your amygdala and locus coeruleus back under control. It takes a minute (or five) of calm, positive meditation to take your brain to a happy, optimistic place. Or use a mindfulness exercise to quiet down that overactive amygdala.
- Talk to people. Keeping your worries to yourself can compound them. Hashing through your concerns with a family member, friend, professional coach, or therapist can help put them in perspective and may allow you to come up with strategies to identify and neurologically respond to your sources of stress.
- Exercise, both physically and mentally. Do what works for you, whether it’s a run, a long walk, pumping iron, playing racquetball — anything that promotes physical release. Exercise your brain too. Engage in a project or activity that is mentally demanding. Personally, I like to garden and do online brain exercises. There’s nothing quite like yanking out weeds or hitting a new personal best at a cognitive exercise for me to notch a sense of accomplishment to counterbalance the unresolved issues driving my worry.
- Accept the uncertainty. Life is full of uncertainty. To paraphrase from Yale theologian Reinhold Niebuhr’s “Serenity Prayer”: Have the serenity to accept what you cannot help, the courage to change what you can, and the wisdom to recognize one from the other.
And, please, be assured that you’ll make it through this election season.
Dr. Merzenich, professor emeritus, Department of Neuroscience, University of California San Francisco, disclosed ties with Posit Science. He is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app.
A version of this article appeared on Medscape.com.
Once again, America is deeply divided before a national election, with people on each side convinced of the horrors that will be visited upon us if the other side wins.
’Tis the season — and regrettably, not to be jolly but to be worried.
As a neuroscientist, I am especially aware of the deleterious mental and physical impact of chronic worry on our citizenry. That’s because worry is not “all in your head.” We modern humans live in a world of worry which appears to be progressively growing.
Flight or Fight
Worry stems from the brain’s rather remarkable ability to foresee and reflexively respond to threat. Our “fight or flight” brain machinery probably arose in our vertebrate ancestors more than 300 million years ago. The fact that we have machinery akin to that possessed by lizards or tigers or shrews is testimony to its crucial contribution to our species’ survival.
As the phrase “fight or flight” suggests, a brain that senses trouble immediately biases certain body and brain functions. As it shifts into a higher-alert mode, it increases the energy supplies in our blood and supports other changes that facilitate faster and stronger reactions, while it shuts down less essential processes which do not contribute to hiding, fighting, or running like hell.
This hyperreactive response is initiated in the amygdala in the anterior brain, which identifies “what’s happening” as immediately or potentially threatening. The now-activated amygdala generates a response in the hypothalamus that provokes an immediate increase of adrenaline and cortisol in the body, and cortisol and noradrenaline in the brain. Both sharply speed up our physical and neurologic reactivity. In the brain, that is achieved by increasing the level of excitability of neurons across the forebrain. Depending on the perceived level of threat, an excitable brain will be just a little or a lot more “on alert,” just a little or a lot faster to respond, and just a little or a lot better at remembering the specific “warning” events that trigger this lizard-brain response.
Alas, this machinery was designed to be engaged every so often when a potentially dangerous surprise arises in life. When the worry and stress are persistent, the brain experiences a kind of neurologic “burn-out” of its fight versus flight machinery.
Dangers of Nonstop Anxiety and Stress
A consistently stressed-out brain turns down its production and release of noradrenaline, and the brain becomes less attentive, less engaged. This sets the brain on the path to an anxiety (and then a depressive) disorder, and, in the longer term, to cognitive losses in memory and executive control systems, and to emotional distortions that can lead to substance abuse or other addictions.
Our political distress is but one source of persistent worry and stress. Worry is a modern plague. The head counts of individuals seeking psychiatric or psychological health are at an all-time high in the United States. Near-universal low-level stressors, such as 2 years of COVID, insecurities about the changing demands of our professional and private lives, and a deeply divided body politic are unequivocally affecting American brain health.
The brain also collaborates in our body’s response to stress. Its regulation of hormonal responses and its autonomic nervous system’s mediated responses contribute to elevated blood sugar levels, to craving high-sugar foods, to elevated blood pressure, and to weaker immune responses. This all contributes to higher risks for cardiovascular and other dietary- and immune system–related disease. And ultimately, to shorter lifespans.
Strategies to Address Neurologic Changes Arising From Chronic Stress
There are many things you can try to bring your worry back to a manageable (and even productive) level.
- Engage in a “reset” strategy several times a day to bring your amygdala and locus coeruleus back under control. It takes a minute (or five) of calm, positive meditation to take your brain to a happy, optimistic place. Or use a mindfulness exercise to quiet down that overactive amygdala.
- Talk to people. Keeping your worries to yourself can compound them. Hashing through your concerns with a family member, friend, professional coach, or therapist can help put them in perspective and may allow you to come up with strategies to identify and neurologically respond to your sources of stress.
- Exercise, both physically and mentally. Do what works for you, whether it’s a run, a long walk, pumping iron, playing racquetball — anything that promotes physical release. Exercise your brain too. Engage in a project or activity that is mentally demanding. Personally, I like to garden and do online brain exercises. There’s nothing quite like yanking out weeds or hitting a new personal best at a cognitive exercise for me to notch a sense of accomplishment to counterbalance the unresolved issues driving my worry.
- Accept the uncertainty. Life is full of uncertainty. To paraphrase from Yale theologian Reinhold Niebuhr’s “Serenity Prayer”: Have the serenity to accept what you cannot help, the courage to change what you can, and the wisdom to recognize one from the other.
And, please, be assured that you’ll make it through this election season.
Dr. Merzenich, professor emeritus, Department of Neuroscience, University of California San Francisco, disclosed ties with Posit Science. He is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app.
A version of this article appeared on Medscape.com.
Once again, America is deeply divided before a national election, with people on each side convinced of the horrors that will be visited upon us if the other side wins.
’Tis the season — and regrettably, not to be jolly but to be worried.
As a neuroscientist, I am especially aware of the deleterious mental and physical impact of chronic worry on our citizenry. That’s because worry is not “all in your head.” We modern humans live in a world of worry which appears to be progressively growing.
Flight or Fight
Worry stems from the brain’s rather remarkable ability to foresee and reflexively respond to threat. Our “fight or flight” brain machinery probably arose in our vertebrate ancestors more than 300 million years ago. The fact that we have machinery akin to that possessed by lizards or tigers or shrews is testimony to its crucial contribution to our species’ survival.
As the phrase “fight or flight” suggests, a brain that senses trouble immediately biases certain body and brain functions. As it shifts into a higher-alert mode, it increases the energy supplies in our blood and supports other changes that facilitate faster and stronger reactions, while it shuts down less essential processes which do not contribute to hiding, fighting, or running like hell.
This hyperreactive response is initiated in the amygdala in the anterior brain, which identifies “what’s happening” as immediately or potentially threatening. The now-activated amygdala generates a response in the hypothalamus that provokes an immediate increase of adrenaline and cortisol in the body, and cortisol and noradrenaline in the brain. Both sharply speed up our physical and neurologic reactivity. In the brain, that is achieved by increasing the level of excitability of neurons across the forebrain. Depending on the perceived level of threat, an excitable brain will be just a little or a lot more “on alert,” just a little or a lot faster to respond, and just a little or a lot better at remembering the specific “warning” events that trigger this lizard-brain response.
Alas, this machinery was designed to be engaged every so often when a potentially dangerous surprise arises in life. When the worry and stress are persistent, the brain experiences a kind of neurologic “burn-out” of its fight versus flight machinery.
Dangers of Nonstop Anxiety and Stress
A consistently stressed-out brain turns down its production and release of noradrenaline, and the brain becomes less attentive, less engaged. This sets the brain on the path to an anxiety (and then a depressive) disorder, and, in the longer term, to cognitive losses in memory and executive control systems, and to emotional distortions that can lead to substance abuse or other addictions.
Our political distress is but one source of persistent worry and stress. Worry is a modern plague. The head counts of individuals seeking psychiatric or psychological health are at an all-time high in the United States. Near-universal low-level stressors, such as 2 years of COVID, insecurities about the changing demands of our professional and private lives, and a deeply divided body politic are unequivocally affecting American brain health.
The brain also collaborates in our body’s response to stress. Its regulation of hormonal responses and its autonomic nervous system’s mediated responses contribute to elevated blood sugar levels, to craving high-sugar foods, to elevated blood pressure, and to weaker immune responses. This all contributes to higher risks for cardiovascular and other dietary- and immune system–related disease. And ultimately, to shorter lifespans.
Strategies to Address Neurologic Changes Arising From Chronic Stress
There are many things you can try to bring your worry back to a manageable (and even productive) level.
- Engage in a “reset” strategy several times a day to bring your amygdala and locus coeruleus back under control. It takes a minute (or five) of calm, positive meditation to take your brain to a happy, optimistic place. Or use a mindfulness exercise to quiet down that overactive amygdala.
- Talk to people. Keeping your worries to yourself can compound them. Hashing through your concerns with a family member, friend, professional coach, or therapist can help put them in perspective and may allow you to come up with strategies to identify and neurologically respond to your sources of stress.
- Exercise, both physically and mentally. Do what works for you, whether it’s a run, a long walk, pumping iron, playing racquetball — anything that promotes physical release. Exercise your brain too. Engage in a project or activity that is mentally demanding. Personally, I like to garden and do online brain exercises. There’s nothing quite like yanking out weeds or hitting a new personal best at a cognitive exercise for me to notch a sense of accomplishment to counterbalance the unresolved issues driving my worry.
- Accept the uncertainty. Life is full of uncertainty. To paraphrase from Yale theologian Reinhold Niebuhr’s “Serenity Prayer”: Have the serenity to accept what you cannot help, the courage to change what you can, and the wisdom to recognize one from the other.
And, please, be assured that you’ll make it through this election season.
Dr. Merzenich, professor emeritus, Department of Neuroscience, University of California San Francisco, disclosed ties with Posit Science. He is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app.
A version of this article appeared on Medscape.com.
AHS White Paper Guides Treatment of Posttraumatic Headache in Youth
The guidance document, the first of its kind, covers risk factors for prolonged recovery, along with pharmacologic and nonpharmacologic management strategies, and supports an emphasis on multidisciplinary care, lead author Carlyn Patterson Gentile, MD, PhD, attending physician in the Division of Neurology at Children’s Hospital of Philadelphia in Pennsylvania, and colleagues reported.
“There are no guidelines to inform the management of posttraumatic headache in youth, but multiple studies have been conducted over the past 2 decades,” the authors wrote in Headache. “This white paper aims to provide a thorough review of the current literature, identify gaps in knowledge, and provide a road map for [posttraumatic headache] management in youth based on available evidence and expert opinion.”
Clarity for an Underrecognized Issue
According to Russell Lonser, MD, professor and chair of neurological surgery at Ohio State University, Columbus, the white paper is important because it offers concrete guidance for health care providers who may be less familiar with posttraumatic headache in youth.
“It brings together all of the previous literature ... in a very well-written way,” Dr. Lonser said in an interview. “More than anything, it could reassure [providers] that they shouldn’t be hunting down potentially magical cures, and reassure them in symptomatic management.”
Meeryo C. Choe, MD, associate clinical professor of pediatric neurology at UCLA Health in Calabasas, California, said the paper also helps shine a light on what may be a more common condition than the public suspects.
“While the media focuses on the effects of concussion in professional sports athletes, the biggest population of athletes is in our youth population,” Dr. Choe said in a written comment. “Almost 25 million children participate in sports throughout the country, and yet we lack guidelines on how to treat posttraumatic headache which can often develop into persistent postconcussive symptoms.”
This white paper, she noted, builds on Dr. Gentile’s 2021 systematic review, introduces new management recommendations, and aligns with the latest consensus statement from the Concussion in Sport Group.
Risk Factors
The white paper first emphasizes the importance of early identification of youth at high risk for prolonged recovery from posttraumatic headache. Risk factors include female sex, adolescent age, a high number of acute symptoms following the initial injury, and social determinants of health.
“I agree that it is important to identify these patients early to improve the recovery trajectory,” Dr. Choe said.
Identifying these individuals quickly allows for timely intervention with both pharmacologic and nonpharmacologic therapies, Dr. Gentile and colleagues noted, potentially mitigating persistent symptoms. Clinicians are encouraged to perform thorough initial assessments to identify these risk factors and initiate early, personalized management plans.
Initial Management of Acute Posttraumatic Headache
For the initial management of acute posttraumatic headache, the white paper recommends a scheduled dosing regimen of simple analgesics. Ibuprofen at a dosage of 10 mg/kg every 6-8 hours (up to a maximum of 600 mg per dose) combined with acetaminophen has shown the best evidence for efficacy. Provided the patient is clinically stable, this regimen should be initiated within 48 hours of the injury and maintained with scheduled dosing for 3-10 days.
If effective, these medications can subsequently be used on an as-needed basis. Careful usage of analgesics is crucial, the white paper cautions, as overadministration can lead to medication-overuse headaches, complicating the recovery process.
Secondary Treatment Options
In cases where first-line oral medications are ineffective, the AHS white paper outlines several secondary treatment options. These include acute intravenous therapies such as ketorolac, dopamine receptor antagonists, and intravenous fluids. Nerve blocks and oral corticosteroid bridges may also be considered.
The white paper stresses the importance of individualized treatment plans that consider the specific needs and responses of each patient, noting that the evidence supporting these approaches is primarily derived from retrospective studies and case reports.
“Patient preferences should be factored in,” said Sean Rose, MD, pediatric neurologist and codirector of the Complex Concussion Clinic at Nationwide Children’s Hospital, Columbus, Ohio.
Supplements and Preventive Measures
For adolescents and young adults at high risk of prolonged posttraumatic headache, the white paper suggests the use of riboflavin and magnesium supplements. Small randomized clinical trials suggest that these supplements may aid in speeding recovery when administered for 1-2 weeks within 48 hours of injury.
If significant headache persists after 2 weeks, a regimen of riboflavin 400 mg daily and magnesium 400-500 mg nightly can be trialed for 6-8 weeks, in line with recommendations for migraine prevention. Additionally, melatonin at a dose of 3-5 mg nightly for an 8-week course may be considered for patients experiencing comorbid sleep disturbances.
Targeted Preventative Therapy
The white paper emphasizes the importance of targeting preventative therapy to the primary headache phenotype.
For instance, patients presenting with a migraine phenotype, or those with a personal or family history of migraines, may be most likely to respond to medications proven effective in migraine prevention, such as amitriptyline, topiramate, and propranolol.
“Most research evidence [for treating posttraumatic headache in youth] is still based on the treatment of migraine,” Dr. Rose pointed out in a written comment.
Dr. Gentile and colleagues recommend initiating preventive therapies 4-6 weeks post injury if headaches are not improving, occur more than 1-2 days per week, or significantly impact daily functioning.
Specialist Referrals and Physical Activity
Referral to a headache specialist is advised for patients who do not respond to first-line acute and preventive therapies. Specialists can offer advanced diagnostic and therapeutic options, the authors noted, ensuring a comprehensive approach to managing posttraumatic headache.
The white paper also recommends noncontact, sub–symptom threshold aerobic physical activity and activities of daily living after an initial 24-48 hour period of symptom-limited cognitive and physical rest. Engaging in these activities may promote faster recovery and help patients gradually return to their normal routines.
“This has been a shift in the concussion treatment approach over the last decade, and is one of the most important interventions we can recommend as physicians,” Dr. Choe noted. “This is where pediatricians and emergency department physicians seeing children acutely can really make a difference in the recovery trajectory for a child after a concussion. ‘Cocoon therapy’ has been proven not only to not work, but be detrimental to recovery.”
Nonpharmacologic Interventions
Based on clinical assessment, nonpharmacologic interventions may also be considered, according to the white paper. These interventions include cervico-vestibular therapy, which addresses neck and balance issues, and cognitive-behavioral therapy, which helps manage the psychological aspects of chronic headache. Dr. Gentile and colleagues highlighted the potential benefits of a collaborative care model that incorporates these nonpharmacologic interventions alongside pharmacologic treatments, providing a holistic approach to posttraumatic headache management.
“Persisting headaches after concussion are often driven by multiple factors,” Dr. Rose said. “Multidisciplinary concussion clinics can offer multiple treatment approaches such as behavioral, physical therapy, exercise, and medication options.”
Unmet Needs
The white paper concludes by calling for high-quality prospective cohort studies and placebo-controlled, randomized, controlled trials to further advance the understanding and treatment of posttraumatic headache in children.
Dr. Lonser, Dr. Choe, and Dr. Rose all agreed.
“More focused treatment trials are needed to gauge efficacy in children with headache after concussion,” Dr. Rose said.
Specifically, Dr. Gentile and colleagues underscored the need to standardize data collection via common elements, which could improve the ability to compare results across studies and develop more effective treatments. In addition, research into the underlying pathophysiology of posttraumatic headache is crucial for identifying new therapeutic targets and clinical and biological markers that can personalize patient care.
They also stressed the importance of exploring the impact of health disparities and social determinants on posttraumatic headache outcomes, aiming to develop interventions that are equitable and accessible to all patient populations.The white paper was approved by the AHS, and supported by the National Institutes of Health/National Institute of Neurological Disorders and Stroke K23 NS124986. The authors disclosed relationships with Eli Lilly, Pfizer, Amgen, and others. The interviewees disclosed no conflicts of interest.
The guidance document, the first of its kind, covers risk factors for prolonged recovery, along with pharmacologic and nonpharmacologic management strategies, and supports an emphasis on multidisciplinary care, lead author Carlyn Patterson Gentile, MD, PhD, attending physician in the Division of Neurology at Children’s Hospital of Philadelphia in Pennsylvania, and colleagues reported.
“There are no guidelines to inform the management of posttraumatic headache in youth, but multiple studies have been conducted over the past 2 decades,” the authors wrote in Headache. “This white paper aims to provide a thorough review of the current literature, identify gaps in knowledge, and provide a road map for [posttraumatic headache] management in youth based on available evidence and expert opinion.”
Clarity for an Underrecognized Issue
According to Russell Lonser, MD, professor and chair of neurological surgery at Ohio State University, Columbus, the white paper is important because it offers concrete guidance for health care providers who may be less familiar with posttraumatic headache in youth.
“It brings together all of the previous literature ... in a very well-written way,” Dr. Lonser said in an interview. “More than anything, it could reassure [providers] that they shouldn’t be hunting down potentially magical cures, and reassure them in symptomatic management.”
Meeryo C. Choe, MD, associate clinical professor of pediatric neurology at UCLA Health in Calabasas, California, said the paper also helps shine a light on what may be a more common condition than the public suspects.
“While the media focuses on the effects of concussion in professional sports athletes, the biggest population of athletes is in our youth population,” Dr. Choe said in a written comment. “Almost 25 million children participate in sports throughout the country, and yet we lack guidelines on how to treat posttraumatic headache which can often develop into persistent postconcussive symptoms.”
This white paper, she noted, builds on Dr. Gentile’s 2021 systematic review, introduces new management recommendations, and aligns with the latest consensus statement from the Concussion in Sport Group.
Risk Factors
The white paper first emphasizes the importance of early identification of youth at high risk for prolonged recovery from posttraumatic headache. Risk factors include female sex, adolescent age, a high number of acute symptoms following the initial injury, and social determinants of health.
“I agree that it is important to identify these patients early to improve the recovery trajectory,” Dr. Choe said.
Identifying these individuals quickly allows for timely intervention with both pharmacologic and nonpharmacologic therapies, Dr. Gentile and colleagues noted, potentially mitigating persistent symptoms. Clinicians are encouraged to perform thorough initial assessments to identify these risk factors and initiate early, personalized management plans.
Initial Management of Acute Posttraumatic Headache
For the initial management of acute posttraumatic headache, the white paper recommends a scheduled dosing regimen of simple analgesics. Ibuprofen at a dosage of 10 mg/kg every 6-8 hours (up to a maximum of 600 mg per dose) combined with acetaminophen has shown the best evidence for efficacy. Provided the patient is clinically stable, this regimen should be initiated within 48 hours of the injury and maintained with scheduled dosing for 3-10 days.
If effective, these medications can subsequently be used on an as-needed basis. Careful usage of analgesics is crucial, the white paper cautions, as overadministration can lead to medication-overuse headaches, complicating the recovery process.
Secondary Treatment Options
In cases where first-line oral medications are ineffective, the AHS white paper outlines several secondary treatment options. These include acute intravenous therapies such as ketorolac, dopamine receptor antagonists, and intravenous fluids. Nerve blocks and oral corticosteroid bridges may also be considered.
The white paper stresses the importance of individualized treatment plans that consider the specific needs and responses of each patient, noting that the evidence supporting these approaches is primarily derived from retrospective studies and case reports.
“Patient preferences should be factored in,” said Sean Rose, MD, pediatric neurologist and codirector of the Complex Concussion Clinic at Nationwide Children’s Hospital, Columbus, Ohio.
Supplements and Preventive Measures
For adolescents and young adults at high risk of prolonged posttraumatic headache, the white paper suggests the use of riboflavin and magnesium supplements. Small randomized clinical trials suggest that these supplements may aid in speeding recovery when administered for 1-2 weeks within 48 hours of injury.
If significant headache persists after 2 weeks, a regimen of riboflavin 400 mg daily and magnesium 400-500 mg nightly can be trialed for 6-8 weeks, in line with recommendations for migraine prevention. Additionally, melatonin at a dose of 3-5 mg nightly for an 8-week course may be considered for patients experiencing comorbid sleep disturbances.
Targeted Preventative Therapy
The white paper emphasizes the importance of targeting preventative therapy to the primary headache phenotype.
For instance, patients presenting with a migraine phenotype, or those with a personal or family history of migraines, may be most likely to respond to medications proven effective in migraine prevention, such as amitriptyline, topiramate, and propranolol.
“Most research evidence [for treating posttraumatic headache in youth] is still based on the treatment of migraine,” Dr. Rose pointed out in a written comment.
Dr. Gentile and colleagues recommend initiating preventive therapies 4-6 weeks post injury if headaches are not improving, occur more than 1-2 days per week, or significantly impact daily functioning.
Specialist Referrals and Physical Activity
Referral to a headache specialist is advised for patients who do not respond to first-line acute and preventive therapies. Specialists can offer advanced diagnostic and therapeutic options, the authors noted, ensuring a comprehensive approach to managing posttraumatic headache.
The white paper also recommends noncontact, sub–symptom threshold aerobic physical activity and activities of daily living after an initial 24-48 hour period of symptom-limited cognitive and physical rest. Engaging in these activities may promote faster recovery and help patients gradually return to their normal routines.
“This has been a shift in the concussion treatment approach over the last decade, and is one of the most important interventions we can recommend as physicians,” Dr. Choe noted. “This is where pediatricians and emergency department physicians seeing children acutely can really make a difference in the recovery trajectory for a child after a concussion. ‘Cocoon therapy’ has been proven not only to not work, but be detrimental to recovery.”
Nonpharmacologic Interventions
Based on clinical assessment, nonpharmacologic interventions may also be considered, according to the white paper. These interventions include cervico-vestibular therapy, which addresses neck and balance issues, and cognitive-behavioral therapy, which helps manage the psychological aspects of chronic headache. Dr. Gentile and colleagues highlighted the potential benefits of a collaborative care model that incorporates these nonpharmacologic interventions alongside pharmacologic treatments, providing a holistic approach to posttraumatic headache management.
“Persisting headaches after concussion are often driven by multiple factors,” Dr. Rose said. “Multidisciplinary concussion clinics can offer multiple treatment approaches such as behavioral, physical therapy, exercise, and medication options.”
Unmet Needs
The white paper concludes by calling for high-quality prospective cohort studies and placebo-controlled, randomized, controlled trials to further advance the understanding and treatment of posttraumatic headache in children.
Dr. Lonser, Dr. Choe, and Dr. Rose all agreed.
“More focused treatment trials are needed to gauge efficacy in children with headache after concussion,” Dr. Rose said.
Specifically, Dr. Gentile and colleagues underscored the need to standardize data collection via common elements, which could improve the ability to compare results across studies and develop more effective treatments. In addition, research into the underlying pathophysiology of posttraumatic headache is crucial for identifying new therapeutic targets and clinical and biological markers that can personalize patient care.
They also stressed the importance of exploring the impact of health disparities and social determinants on posttraumatic headache outcomes, aiming to develop interventions that are equitable and accessible to all patient populations.The white paper was approved by the AHS, and supported by the National Institutes of Health/National Institute of Neurological Disorders and Stroke K23 NS124986. The authors disclosed relationships with Eli Lilly, Pfizer, Amgen, and others. The interviewees disclosed no conflicts of interest.
The guidance document, the first of its kind, covers risk factors for prolonged recovery, along with pharmacologic and nonpharmacologic management strategies, and supports an emphasis on multidisciplinary care, lead author Carlyn Patterson Gentile, MD, PhD, attending physician in the Division of Neurology at Children’s Hospital of Philadelphia in Pennsylvania, and colleagues reported.
“There are no guidelines to inform the management of posttraumatic headache in youth, but multiple studies have been conducted over the past 2 decades,” the authors wrote in Headache. “This white paper aims to provide a thorough review of the current literature, identify gaps in knowledge, and provide a road map for [posttraumatic headache] management in youth based on available evidence and expert opinion.”
Clarity for an Underrecognized Issue
According to Russell Lonser, MD, professor and chair of neurological surgery at Ohio State University, Columbus, the white paper is important because it offers concrete guidance for health care providers who may be less familiar with posttraumatic headache in youth.
“It brings together all of the previous literature ... in a very well-written way,” Dr. Lonser said in an interview. “More than anything, it could reassure [providers] that they shouldn’t be hunting down potentially magical cures, and reassure them in symptomatic management.”
Meeryo C. Choe, MD, associate clinical professor of pediatric neurology at UCLA Health in Calabasas, California, said the paper also helps shine a light on what may be a more common condition than the public suspects.
“While the media focuses on the effects of concussion in professional sports athletes, the biggest population of athletes is in our youth population,” Dr. Choe said in a written comment. “Almost 25 million children participate in sports throughout the country, and yet we lack guidelines on how to treat posttraumatic headache which can often develop into persistent postconcussive symptoms.”
This white paper, she noted, builds on Dr. Gentile’s 2021 systematic review, introduces new management recommendations, and aligns with the latest consensus statement from the Concussion in Sport Group.
Risk Factors
The white paper first emphasizes the importance of early identification of youth at high risk for prolonged recovery from posttraumatic headache. Risk factors include female sex, adolescent age, a high number of acute symptoms following the initial injury, and social determinants of health.
“I agree that it is important to identify these patients early to improve the recovery trajectory,” Dr. Choe said.
Identifying these individuals quickly allows for timely intervention with both pharmacologic and nonpharmacologic therapies, Dr. Gentile and colleagues noted, potentially mitigating persistent symptoms. Clinicians are encouraged to perform thorough initial assessments to identify these risk factors and initiate early, personalized management plans.
Initial Management of Acute Posttraumatic Headache
For the initial management of acute posttraumatic headache, the white paper recommends a scheduled dosing regimen of simple analgesics. Ibuprofen at a dosage of 10 mg/kg every 6-8 hours (up to a maximum of 600 mg per dose) combined with acetaminophen has shown the best evidence for efficacy. Provided the patient is clinically stable, this regimen should be initiated within 48 hours of the injury and maintained with scheduled dosing for 3-10 days.
If effective, these medications can subsequently be used on an as-needed basis. Careful usage of analgesics is crucial, the white paper cautions, as overadministration can lead to medication-overuse headaches, complicating the recovery process.
Secondary Treatment Options
In cases where first-line oral medications are ineffective, the AHS white paper outlines several secondary treatment options. These include acute intravenous therapies such as ketorolac, dopamine receptor antagonists, and intravenous fluids. Nerve blocks and oral corticosteroid bridges may also be considered.
The white paper stresses the importance of individualized treatment plans that consider the specific needs and responses of each patient, noting that the evidence supporting these approaches is primarily derived from retrospective studies and case reports.
“Patient preferences should be factored in,” said Sean Rose, MD, pediatric neurologist and codirector of the Complex Concussion Clinic at Nationwide Children’s Hospital, Columbus, Ohio.
Supplements and Preventive Measures
For adolescents and young adults at high risk of prolonged posttraumatic headache, the white paper suggests the use of riboflavin and magnesium supplements. Small randomized clinical trials suggest that these supplements may aid in speeding recovery when administered for 1-2 weeks within 48 hours of injury.
If significant headache persists after 2 weeks, a regimen of riboflavin 400 mg daily and magnesium 400-500 mg nightly can be trialed for 6-8 weeks, in line with recommendations for migraine prevention. Additionally, melatonin at a dose of 3-5 mg nightly for an 8-week course may be considered for patients experiencing comorbid sleep disturbances.
Targeted Preventative Therapy
The white paper emphasizes the importance of targeting preventative therapy to the primary headache phenotype.
For instance, patients presenting with a migraine phenotype, or those with a personal or family history of migraines, may be most likely to respond to medications proven effective in migraine prevention, such as amitriptyline, topiramate, and propranolol.
“Most research evidence [for treating posttraumatic headache in youth] is still based on the treatment of migraine,” Dr. Rose pointed out in a written comment.
Dr. Gentile and colleagues recommend initiating preventive therapies 4-6 weeks post injury if headaches are not improving, occur more than 1-2 days per week, or significantly impact daily functioning.
Specialist Referrals and Physical Activity
Referral to a headache specialist is advised for patients who do not respond to first-line acute and preventive therapies. Specialists can offer advanced diagnostic and therapeutic options, the authors noted, ensuring a comprehensive approach to managing posttraumatic headache.
The white paper also recommends noncontact, sub–symptom threshold aerobic physical activity and activities of daily living after an initial 24-48 hour period of symptom-limited cognitive and physical rest. Engaging in these activities may promote faster recovery and help patients gradually return to their normal routines.
“This has been a shift in the concussion treatment approach over the last decade, and is one of the most important interventions we can recommend as physicians,” Dr. Choe noted. “This is where pediatricians and emergency department physicians seeing children acutely can really make a difference in the recovery trajectory for a child after a concussion. ‘Cocoon therapy’ has been proven not only to not work, but be detrimental to recovery.”
Nonpharmacologic Interventions
Based on clinical assessment, nonpharmacologic interventions may also be considered, according to the white paper. These interventions include cervico-vestibular therapy, which addresses neck and balance issues, and cognitive-behavioral therapy, which helps manage the psychological aspects of chronic headache. Dr. Gentile and colleagues highlighted the potential benefits of a collaborative care model that incorporates these nonpharmacologic interventions alongside pharmacologic treatments, providing a holistic approach to posttraumatic headache management.
“Persisting headaches after concussion are often driven by multiple factors,” Dr. Rose said. “Multidisciplinary concussion clinics can offer multiple treatment approaches such as behavioral, physical therapy, exercise, and medication options.”
Unmet Needs
The white paper concludes by calling for high-quality prospective cohort studies and placebo-controlled, randomized, controlled trials to further advance the understanding and treatment of posttraumatic headache in children.
Dr. Lonser, Dr. Choe, and Dr. Rose all agreed.
“More focused treatment trials are needed to gauge efficacy in children with headache after concussion,” Dr. Rose said.
Specifically, Dr. Gentile and colleagues underscored the need to standardize data collection via common elements, which could improve the ability to compare results across studies and develop more effective treatments. In addition, research into the underlying pathophysiology of posttraumatic headache is crucial for identifying new therapeutic targets and clinical and biological markers that can personalize patient care.
They also stressed the importance of exploring the impact of health disparities and social determinants on posttraumatic headache outcomes, aiming to develop interventions that are equitable and accessible to all patient populations.The white paper was approved by the AHS, and supported by the National Institutes of Health/National Institute of Neurological Disorders and Stroke K23 NS124986. The authors disclosed relationships with Eli Lilly, Pfizer, Amgen, and others. The interviewees disclosed no conflicts of interest.
FROM HEADACHE
New First-Line Therapies for Migraine Prevention
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 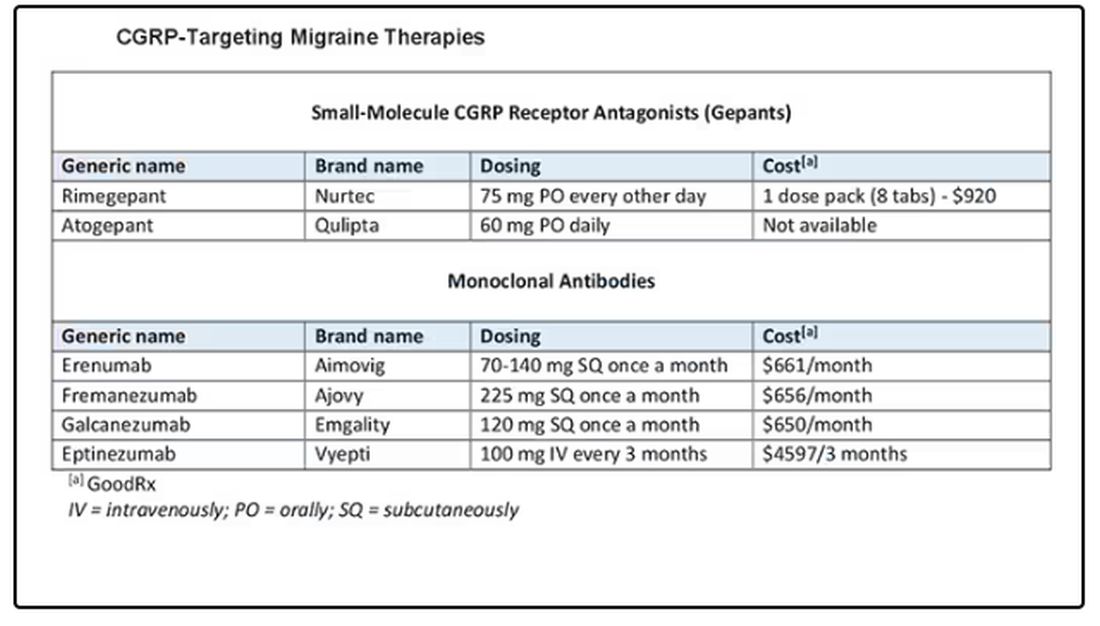
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 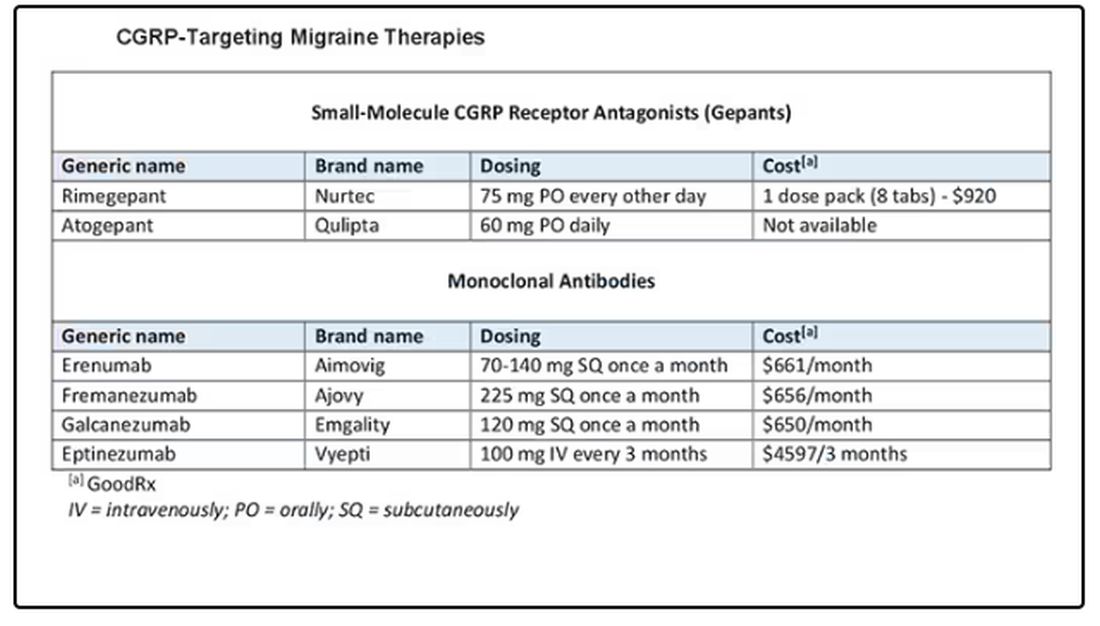
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Today I am going to talk about the position statement from the American Headache Society (AHS) “Calcitonin gene-related peptide [CGRP]–targeting therapies are a first-line option for the prevention of migraine”. This update is of critical importance because about three fourths of people with migraine get their care from a primary care clinician, not from a neurologist or a headache specialist. CGRP-targeting therapies have transformed migraine care at the specialty level, but many in primary care are not yet familiar with this class of medicines. Until this new statement was released, CGRPs were not viewed as first-line agents for migraine. That has now changed.
Two main types of therapy for people with migraine headache are: (1) acute or abortive therapy (when a headache develops, it is treated), and (2) preventive therapy. Preventive therapy is typically used when the patient has headaches on 4 or more days per month. Preventive therapy is aimed at reducing the frequency and severity of headaches. About 40% of patients with migraine qualify for preventive therapy, but only a minority are receiving it.
The armamentarium for preventive therapy of migraines had not changed in a long time — until now. First-line preventive therapy has traditionally consisted of three classes of agents: beta-blockers, tricyclic antidepressants, and topiramate. These medicines were developed for different therapeutic purposes, yet they work for migraines. These drugs may have off-target effects that can make them difficult to tolerate.
Based on new evidence, candesartan — an angiotensin receptor blocker (ARB) — is now also a first-line drug for migraine. This is good news, because ARBs are a drug class that we have a lot of experience with, are easy to use, and could be an excellent choice for people with concomitant hypertension or chronic kidney disease. The serotonin-norepinephrine reuptake inhibitors (venlafaxine and duloxetine) are also considered first-line agents for migraine treatment.
In the AHS’s new position statement, the two main drug classes are small-molecule CGRP receptor antagonists and monoclonal antibodies.
The role of the neuropeptide CGRP in migraine was originally discovered after finding that blood levels of CGRP were elevated during migraine attacks. This led to the discovery of agents that blocked CGRP, initially for acute treatment of migraine, and then for preventive therapy. Multiple clinical studies show the CGRP targeting therapies to be as or even more effective than traditional first-line agents at decreasing the number of migraine days per month.
The efficacy and safety of these agents have been demonstrated in both randomized trials and in real-world studies. Other important positive endpoints include fewer days of migraine, reduced acute medication use, and improvements in many quality-of-life outcomes. Studies also have shown that CGRP-targeting therapies are well tolerated and safe, with very few serious adverse events.
Furthermore, studies have shown the CGRP targeting therapies are effective in individuals who have failed multiple other first-line therapies. They fit now both as first-line agents and as agents that can be used in difficult-to-treat patients as well as in patients who struggle with acute medication overuse, which is often very challenging.
To quote from the AHS statement,
Side effects are uncommon and can include hypertension, constipation, and Raynaud phenomenon.
The position statement is strong and is based on a lot of evidence and clinical experience. CGRP-targeting therapies are now first-line agents for the prevention of migraine headache. We should learn more about and begin to feel comfortable using this class of agents because they stand to benefit our patients greatly. I’d suggest looking at the table below and picking one new agent to become familiar with so that you can add that agent to your toolbox. 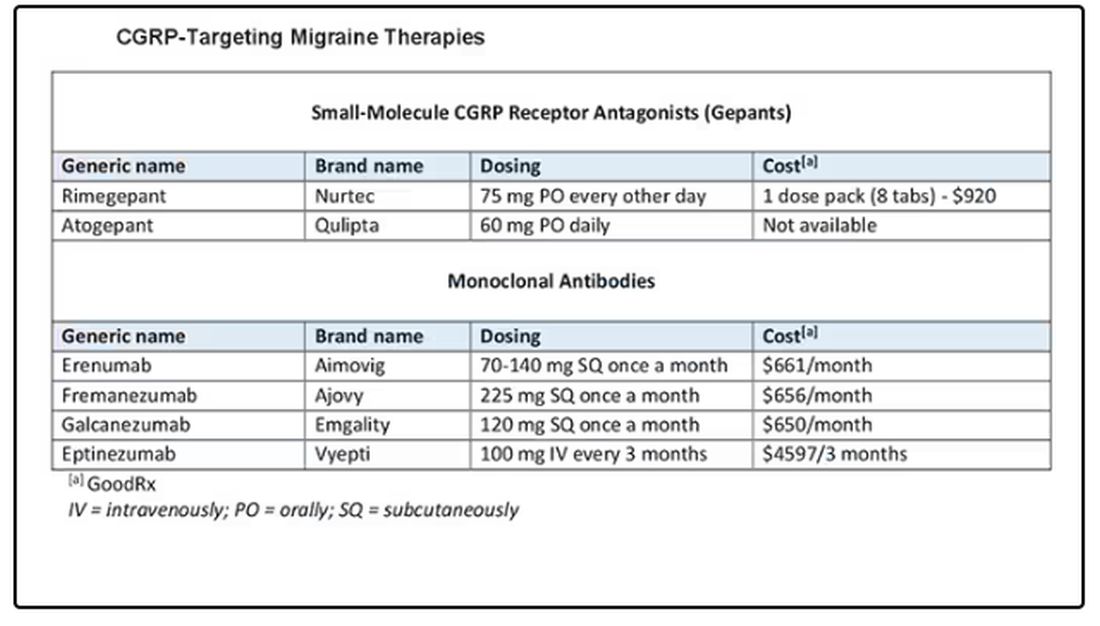
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, Pennsylvania, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, Bayer, and Teva.
A version of this article appeared on Medscape.com.
Immunotherapy May Be Overused in Dying Patients With Cancer
Chemotherapy has fallen out of favor for treating cancer toward the end of life. The toxicity is too high, and the benefit, if any, is often too low.
Immunotherapy, however, has been taking its place.
This means “there are patients who are getting immunotherapy who shouldn’t,” said Yale University, New Haven, Connecticut, surgical oncologist Sajid Khan, MD, senior investigator on a recent study that highlighted the growing use of these agents in patients’ last month of life.
What’s driving this trend, and how can oncologists avoid overtreatment with immunotherapy at the end of life?
The N-of-1 Patient
With immunotherapy at the end of life, “each of us has had our N-of-1” where a patient bounces back with a remarkable and durable response, said Don Dizon, MD, a gynecologic oncologist at Brown University, Providence, Rhode Island.
He recalled a patient with sarcoma who did not respond to chemotherapy. But after Dr. Dizon started her on immunotherapy, everything turned around. She has now been in remission for 8 years and counting.
The possibility of an unexpected or remarkable responder is seductive. And the improved safety of immunotherapy over chemotherapy adds to the allure.
Meanwhile, patients are often desperate. It’s rare for someone to be ready to stop treatment, Dr. Dizon said. Everybody “hopes that they’re going to be the exceptional responder.”
At the end of the day, the question often becomes: “Why not try immunotherapy? What’s there to lose?”
This thinking may be prompting broader use of immunotherapy in late-stage disease, even in instances with no Food and Drug Administration indication and virtually no supportive data, such as for metastatic ovarian cancer, Dr. Dizon said.
Back to Earth
The problem with the hopeful approach is that end-of-life turnarounds with immunotherapy are rare, and there’s no way at the moment to predict who will have one, said Laura Petrillo, MD, a palliative care physician at Massachusetts General Hospital, Boston.
Even though immunotherapy generally comes with fewer adverse events than chemotherapy, catastrophic side effects are still possible.
Dr. Petrillo recalled a 95-year-old woman with metastatic cancer who was largely asymptomatic.
She had a qualifying mutation for a checkpoint inhibitor, so her oncologist started her on one. The patient never bounced back from the severe colitis the agent caused, and she died of complications in the hospital.
Although such reactions with immunotherapy are uncommon, less serious problems caused by the agents can still have a major impact on a person’s quality of life. Low-grade diarrhea, for instance, may not sound too bad, but in a patient’s daily life, it can translate to six or more episodes a day.
Even with no side effects, prescribing immunotherapy can mean that patients with limited time left spend a good portion of it at an infusion clinic instead of at home. These patients are also less likely to be referred to hospice and more likely to be admitted to and die in the hospital.
And with treatments that can cost $20,000 per dose, financial toxicity becomes a big concern.
In short, some of the reasons why chemotherapy is not recommended at the end of life also apply to immunotherapy, Dr. Petrillo said.
Prescribing Decisions
Recent research highlights the growing use of immunotherapy at the end of life.
Dr. Khan’s retrospective study found, for instance, that the percentage of patients starting immunotherapy in the last 30 days of life increased by about fourfold to fivefold over the study period for the three cancers analyzed — stage IV melanoma, lung, and kidney cancers.
Among the population that died within 30 days, the percentage receiving immunotherapy increased over the study periods — 0.8%-4.3% for melanoma, 0.9%-3.2% for NSCLC, and 0.5%-2.6% for kidney cell carcinoma — prompting the conclusion that immunotherapy prescriptions in the last month of life are on the rise.
Prescribing immunotherapy in patients who ultimately died within 1 month occurred more frequently at low-volume, nonacademic centers than at academic or high-volume centers, and outcomes varied by practice setting.
Patients had better survival outcomes overall when receiving immunotherapy at academic or high-volume centers — a finding Dr. Khan said is worth investigating further. Possible explanations include better management of severe immune-related side effects at larger centers and more caution when prescribing immunotherapy to “borderline” candidates, such as those with several comorbidities.
Importantly, given the retrospective design, Dr. Khan and colleagues already knew which patients prescribed immunotherapy died within 30 days of initiating treatment.
More specifically, 5192 of 71,204 patients who received immunotherapy (7.3%) died within a month of initiating therapy, while 66,012 (92.7%) lived beyond that point.
The study, however, did not assess how the remaining 92.7% who lived beyond 30 days fared on immunotherapy and the differences between those who lived less than 30 days and those who survived longer.
Knowing the outcome of patients at the outset of the analysis still leaves open the question of when immunotherapy can extend life and when it can’t for the patient in front of you.
To avoid overtreating at the end of life, it’s important to have “the same standard that you have for giving chemotherapy. You have to treat it with the same respect,” said Moshe Chasky, MD, a community medical oncologist with Alliance Cancer Specialists in Philadelphia, Pennsylvania. “You can’t just be throwing” immunotherapy around “at the end of life.”
While there are no clear predictors of risk and benefit, there are some factors to help guide decisions.
As with chemotherapy, Dr. Petrillo said performance status is key. Dr. Petrillo and colleagues found that median overall survival with immune checkpoint inhibitors for advanced non–small cell lung cancer was 14.3 months in patients with an Eastern Cooperative Oncology Group performance score of 0-1 but only 4.5 months with scores of ≥ 2.
Dr. Khan also found that immunotherapy survival is, unsurprisingly, worse in patients with high metastatic burdens and more comorbidities.
“You should still consider immunotherapy for metastatic melanoma, non–small cell lung cancer, and renal cell carcinoma,” Dr. Khan said. The message here is to “think twice before using” it, especially in comorbid patients with widespread metastases.
“Just because something can be done doesn’t always mean it should be done,” he said.
At Yale, when Dr. Khan works, immunotherapy decisions are considered by a multidisciplinary tumor board. At Mass General, immunotherapy has generally moved to the frontline setting, and the hospital no longer prescribes checkpoint inhibitors to hospitalized patients because the cost is too high relative to the potential benefit, Dr. Petrillo explained.
Still, with all the uncertainties about risk and benefit, counseling patients is a challenge. Dr. Dizon called it “the epitome of shared decision-making.”
Dr. Petrillo noted that it’s critical not to counsel patients based solely on the anecdotal patients who do surprisingly well.
“It’s hard to mention that and not have that be what somebody anchors on,” she said. But that speaks to “how desperate people can feel, how hopeful they can be.”
Dr. Khan, Dr. Petrillo, and Dr. Chasky all reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Chemotherapy has fallen out of favor for treating cancer toward the end of life. The toxicity is too high, and the benefit, if any, is often too low.
Immunotherapy, however, has been taking its place.
This means “there are patients who are getting immunotherapy who shouldn’t,” said Yale University, New Haven, Connecticut, surgical oncologist Sajid Khan, MD, senior investigator on a recent study that highlighted the growing use of these agents in patients’ last month of life.
What’s driving this trend, and how can oncologists avoid overtreatment with immunotherapy at the end of life?
The N-of-1 Patient
With immunotherapy at the end of life, “each of us has had our N-of-1” where a patient bounces back with a remarkable and durable response, said Don Dizon, MD, a gynecologic oncologist at Brown University, Providence, Rhode Island.
He recalled a patient with sarcoma who did not respond to chemotherapy. But after Dr. Dizon started her on immunotherapy, everything turned around. She has now been in remission for 8 years and counting.
The possibility of an unexpected or remarkable responder is seductive. And the improved safety of immunotherapy over chemotherapy adds to the allure.
Meanwhile, patients are often desperate. It’s rare for someone to be ready to stop treatment, Dr. Dizon said. Everybody “hopes that they’re going to be the exceptional responder.”
At the end of the day, the question often becomes: “Why not try immunotherapy? What’s there to lose?”
This thinking may be prompting broader use of immunotherapy in late-stage disease, even in instances with no Food and Drug Administration indication and virtually no supportive data, such as for metastatic ovarian cancer, Dr. Dizon said.
Back to Earth
The problem with the hopeful approach is that end-of-life turnarounds with immunotherapy are rare, and there’s no way at the moment to predict who will have one, said Laura Petrillo, MD, a palliative care physician at Massachusetts General Hospital, Boston.
Even though immunotherapy generally comes with fewer adverse events than chemotherapy, catastrophic side effects are still possible.
Dr. Petrillo recalled a 95-year-old woman with metastatic cancer who was largely asymptomatic.
She had a qualifying mutation for a checkpoint inhibitor, so her oncologist started her on one. The patient never bounced back from the severe colitis the agent caused, and she died of complications in the hospital.
Although such reactions with immunotherapy are uncommon, less serious problems caused by the agents can still have a major impact on a person’s quality of life. Low-grade diarrhea, for instance, may not sound too bad, but in a patient’s daily life, it can translate to six or more episodes a day.
Even with no side effects, prescribing immunotherapy can mean that patients with limited time left spend a good portion of it at an infusion clinic instead of at home. These patients are also less likely to be referred to hospice and more likely to be admitted to and die in the hospital.
And with treatments that can cost $20,000 per dose, financial toxicity becomes a big concern.
In short, some of the reasons why chemotherapy is not recommended at the end of life also apply to immunotherapy, Dr. Petrillo said.
Prescribing Decisions
Recent research highlights the growing use of immunotherapy at the end of life.
Dr. Khan’s retrospective study found, for instance, that the percentage of patients starting immunotherapy in the last 30 days of life increased by about fourfold to fivefold over the study period for the three cancers analyzed — stage IV melanoma, lung, and kidney cancers.
Among the population that died within 30 days, the percentage receiving immunotherapy increased over the study periods — 0.8%-4.3% for melanoma, 0.9%-3.2% for NSCLC, and 0.5%-2.6% for kidney cell carcinoma — prompting the conclusion that immunotherapy prescriptions in the last month of life are on the rise.
Prescribing immunotherapy in patients who ultimately died within 1 month occurred more frequently at low-volume, nonacademic centers than at academic or high-volume centers, and outcomes varied by practice setting.
Patients had better survival outcomes overall when receiving immunotherapy at academic or high-volume centers — a finding Dr. Khan said is worth investigating further. Possible explanations include better management of severe immune-related side effects at larger centers and more caution when prescribing immunotherapy to “borderline” candidates, such as those with several comorbidities.
Importantly, given the retrospective design, Dr. Khan and colleagues already knew which patients prescribed immunotherapy died within 30 days of initiating treatment.
More specifically, 5192 of 71,204 patients who received immunotherapy (7.3%) died within a month of initiating therapy, while 66,012 (92.7%) lived beyond that point.
The study, however, did not assess how the remaining 92.7% who lived beyond 30 days fared on immunotherapy and the differences between those who lived less than 30 days and those who survived longer.
Knowing the outcome of patients at the outset of the analysis still leaves open the question of when immunotherapy can extend life and when it can’t for the patient in front of you.
To avoid overtreating at the end of life, it’s important to have “the same standard that you have for giving chemotherapy. You have to treat it with the same respect,” said Moshe Chasky, MD, a community medical oncologist with Alliance Cancer Specialists in Philadelphia, Pennsylvania. “You can’t just be throwing” immunotherapy around “at the end of life.”
While there are no clear predictors of risk and benefit, there are some factors to help guide decisions.
As with chemotherapy, Dr. Petrillo said performance status is key. Dr. Petrillo and colleagues found that median overall survival with immune checkpoint inhibitors for advanced non–small cell lung cancer was 14.3 months in patients with an Eastern Cooperative Oncology Group performance score of 0-1 but only 4.5 months with scores of ≥ 2.
Dr. Khan also found that immunotherapy survival is, unsurprisingly, worse in patients with high metastatic burdens and more comorbidities.
“You should still consider immunotherapy for metastatic melanoma, non–small cell lung cancer, and renal cell carcinoma,” Dr. Khan said. The message here is to “think twice before using” it, especially in comorbid patients with widespread metastases.
“Just because something can be done doesn’t always mean it should be done,” he said.
At Yale, when Dr. Khan works, immunotherapy decisions are considered by a multidisciplinary tumor board. At Mass General, immunotherapy has generally moved to the frontline setting, and the hospital no longer prescribes checkpoint inhibitors to hospitalized patients because the cost is too high relative to the potential benefit, Dr. Petrillo explained.
Still, with all the uncertainties about risk and benefit, counseling patients is a challenge. Dr. Dizon called it “the epitome of shared decision-making.”
Dr. Petrillo noted that it’s critical not to counsel patients based solely on the anecdotal patients who do surprisingly well.
“It’s hard to mention that and not have that be what somebody anchors on,” she said. But that speaks to “how desperate people can feel, how hopeful they can be.”
Dr. Khan, Dr. Petrillo, and Dr. Chasky all reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Chemotherapy has fallen out of favor for treating cancer toward the end of life. The toxicity is too high, and the benefit, if any, is often too low.
Immunotherapy, however, has been taking its place.
This means “there are patients who are getting immunotherapy who shouldn’t,” said Yale University, New Haven, Connecticut, surgical oncologist Sajid Khan, MD, senior investigator on a recent study that highlighted the growing use of these agents in patients’ last month of life.
What’s driving this trend, and how can oncologists avoid overtreatment with immunotherapy at the end of life?
The N-of-1 Patient
With immunotherapy at the end of life, “each of us has had our N-of-1” where a patient bounces back with a remarkable and durable response, said Don Dizon, MD, a gynecologic oncologist at Brown University, Providence, Rhode Island.
He recalled a patient with sarcoma who did not respond to chemotherapy. But after Dr. Dizon started her on immunotherapy, everything turned around. She has now been in remission for 8 years and counting.
The possibility of an unexpected or remarkable responder is seductive. And the improved safety of immunotherapy over chemotherapy adds to the allure.
Meanwhile, patients are often desperate. It’s rare for someone to be ready to stop treatment, Dr. Dizon said. Everybody “hopes that they’re going to be the exceptional responder.”
At the end of the day, the question often becomes: “Why not try immunotherapy? What’s there to lose?”
This thinking may be prompting broader use of immunotherapy in late-stage disease, even in instances with no Food and Drug Administration indication and virtually no supportive data, such as for metastatic ovarian cancer, Dr. Dizon said.
Back to Earth
The problem with the hopeful approach is that end-of-life turnarounds with immunotherapy are rare, and there’s no way at the moment to predict who will have one, said Laura Petrillo, MD, a palliative care physician at Massachusetts General Hospital, Boston.
Even though immunotherapy generally comes with fewer adverse events than chemotherapy, catastrophic side effects are still possible.
Dr. Petrillo recalled a 95-year-old woman with metastatic cancer who was largely asymptomatic.
She had a qualifying mutation for a checkpoint inhibitor, so her oncologist started her on one. The patient never bounced back from the severe colitis the agent caused, and she died of complications in the hospital.
Although such reactions with immunotherapy are uncommon, less serious problems caused by the agents can still have a major impact on a person’s quality of life. Low-grade diarrhea, for instance, may not sound too bad, but in a patient’s daily life, it can translate to six or more episodes a day.
Even with no side effects, prescribing immunotherapy can mean that patients with limited time left spend a good portion of it at an infusion clinic instead of at home. These patients are also less likely to be referred to hospice and more likely to be admitted to and die in the hospital.
And with treatments that can cost $20,000 per dose, financial toxicity becomes a big concern.
In short, some of the reasons why chemotherapy is not recommended at the end of life also apply to immunotherapy, Dr. Petrillo said.
Prescribing Decisions
Recent research highlights the growing use of immunotherapy at the end of life.
Dr. Khan’s retrospective study found, for instance, that the percentage of patients starting immunotherapy in the last 30 days of life increased by about fourfold to fivefold over the study period for the three cancers analyzed — stage IV melanoma, lung, and kidney cancers.
Among the population that died within 30 days, the percentage receiving immunotherapy increased over the study periods — 0.8%-4.3% for melanoma, 0.9%-3.2% for NSCLC, and 0.5%-2.6% for kidney cell carcinoma — prompting the conclusion that immunotherapy prescriptions in the last month of life are on the rise.
Prescribing immunotherapy in patients who ultimately died within 1 month occurred more frequently at low-volume, nonacademic centers than at academic or high-volume centers, and outcomes varied by practice setting.
Patients had better survival outcomes overall when receiving immunotherapy at academic or high-volume centers — a finding Dr. Khan said is worth investigating further. Possible explanations include better management of severe immune-related side effects at larger centers and more caution when prescribing immunotherapy to “borderline” candidates, such as those with several comorbidities.
Importantly, given the retrospective design, Dr. Khan and colleagues already knew which patients prescribed immunotherapy died within 30 days of initiating treatment.
More specifically, 5192 of 71,204 patients who received immunotherapy (7.3%) died within a month of initiating therapy, while 66,012 (92.7%) lived beyond that point.
The study, however, did not assess how the remaining 92.7% who lived beyond 30 days fared on immunotherapy and the differences between those who lived less than 30 days and those who survived longer.
Knowing the outcome of patients at the outset of the analysis still leaves open the question of when immunotherapy can extend life and when it can’t for the patient in front of you.
To avoid overtreating at the end of life, it’s important to have “the same standard that you have for giving chemotherapy. You have to treat it with the same respect,” said Moshe Chasky, MD, a community medical oncologist with Alliance Cancer Specialists in Philadelphia, Pennsylvania. “You can’t just be throwing” immunotherapy around “at the end of life.”
While there are no clear predictors of risk and benefit, there are some factors to help guide decisions.
As with chemotherapy, Dr. Petrillo said performance status is key. Dr. Petrillo and colleagues found that median overall survival with immune checkpoint inhibitors for advanced non–small cell lung cancer was 14.3 months in patients with an Eastern Cooperative Oncology Group performance score of 0-1 but only 4.5 months with scores of ≥ 2.
Dr. Khan also found that immunotherapy survival is, unsurprisingly, worse in patients with high metastatic burdens and more comorbidities.
“You should still consider immunotherapy for metastatic melanoma, non–small cell lung cancer, and renal cell carcinoma,” Dr. Khan said. The message here is to “think twice before using” it, especially in comorbid patients with widespread metastases.
“Just because something can be done doesn’t always mean it should be done,” he said.
At Yale, when Dr. Khan works, immunotherapy decisions are considered by a multidisciplinary tumor board. At Mass General, immunotherapy has generally moved to the frontline setting, and the hospital no longer prescribes checkpoint inhibitors to hospitalized patients because the cost is too high relative to the potential benefit, Dr. Petrillo explained.
Still, with all the uncertainties about risk and benefit, counseling patients is a challenge. Dr. Dizon called it “the epitome of shared decision-making.”
Dr. Petrillo noted that it’s critical not to counsel patients based solely on the anecdotal patients who do surprisingly well.
“It’s hard to mention that and not have that be what somebody anchors on,” she said. But that speaks to “how desperate people can feel, how hopeful they can be.”
Dr. Khan, Dr. Petrillo, and Dr. Chasky all reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
How Clinicians Can Help Patients Navigate Psychedelics/Microdosing
Peter Grinspoon, MD, has some advice for clinicians when patients ask questions about microdosing of psychedelics: Keep the lines of communication open — and don’t be judgmental.
“If you’re dismissive or critical or sound like you’re judging them, then the patients just clam up,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and a primary care physician at Massachusetts General Hospital, both in Boston.
Psychedelic drugs are still illegal in the majority of states despite the growth of public interest in and use of these substances. That growth is evidenced by a flurry of workshops, reports, law enforcement seizures, and pressure by Congressional members for the Food and Drug Administration to approve new psychedelic drugs, just in the past year.
A recent study in JAMA Health Forum showed a nearly 14-fold increase in Google searches — from 7.9 to 105.6 per 10 million nationwide — for the term “microdosing” and related wording, between 2015 and 2023.
Two states — Oregon and Colorado — have decriminalized certain psychedelic drugs and are in various stages of establishing regulations and centers for prospective clients. Almost two dozen localities, like Ann Arbor, Michigan, have decriminalized psychedelic drugs. A handful of states have active legislation to decriminalize use, while others have bills that never made it out of committee.
But no definitive studies have reported that microdosing produces positive mental effects at a higher rate than placebo, according to Dr. Grinspoon. So
“We’re in this renaissance where everybody is idealizing these medications, as opposed to 20 years ago when we were in the war on drugs and everybody was dismissing them,” Dr. Grinspoon said. “The truth is somewhere in between.”
The Science
Microdosing is defined as taking doses of 1/5 to 1/20 of the conventional recreational amount, which might include a dried psilocybin mushroom, lysergic acid diethylamide, or 3,4-methylenedioxymethamphetamine. But even that much may be neither effective nor safe.
Dr. Grinspoon said clinicians should tell patients that psychedelics may cause harm, although the drugs are relatively nontoxic and are not addictive. An illegally obtained psilocybin could cause negative reactions, especially if the drug has been adulterated with other substances and if the actual dose is higher than what was indicated by the seller.
He noted that people have different reactions to psychedelics, just as they have to prescription medications. He cited one example of a woman who microdosed and could not sleep for 2 weeks afterward. Only recently have randomized, double-blinded studies begun on benefits and harms.
Researchers have also begun investigating whether long-term microdosing of psilocybin could lead to valvular heart disease (VHD), said Kevin Yang, MD, a psychiatry resident at the University of California San Diego School of Medicine. A recent review of evidence concluded that microdosing various psychedelics over a period of months can lead to drug-induced VHD.
“It’s extremely important to emphasize with patients that not only do we not know if it works or not, we also don’t really know how safe it is,” Dr. Yang said.
Dr. Yang also said clinicians should consider referring patients to a mental health professional, and especially those that may have expertise in psychedelic therapies.
One of those experts is Rachel Yehuda, PhD, director of the Center for Psychedelic Psychotherapy and Trauma Research at Icahn School of Medicine at Mount Sinai in New York City. She said therapists should be able to assess the patient’s perceived need for microdosing and “invite reflections about why current approaches are falling short.”
“I would also not actively discourage it either but remain curious until both of you have a better understanding of the reasons for seeking this out and potential alternative strategies for obtaining more therapeutic benefits,” she said. “I think it is really important to study the effects of both micro- and macrodosing of psychedelics but not move in advance of the data.”
Navigating Legality
Recent ballot measures in Oregon and Colorado directed the states to develop regulated and licensed psilocybin-assisted therapy centers for legal “trips.” Oregon’s first center was opened in 2023, and Colorado is now developing its own licensing model.
According to the Oregon Health Authority, the centers are not medical facilities, and prescription or referral from a medical professional is not required.
The Oregon Academy of Family Physicians (OAFP) has yet to release guidance to clinicians on how to talk to their patients about these drugs or potential interest in visiting a licensed therapy center.
However, Betsy Boyd-Flynn, executive director of OAFP, said the organization is working on continuing medical education for what the average family physician needs to know if a patient asks about use.
“We suspect that many of our members have interest and want to learn more,” she said.
Dr. Grinspoon said clinicians should talk with patients about legality during these conversations.
“The big question I get is: ‘I really want to try microdosing, but how do I obtain the mushrooms?’ ” he said. “You can’t really as a physician tell them to do anything illegal. So you tell them to be safe, be careful, and to use their judgment.”
Patients who want to pursue microdosing who do not live in Oregon have two legal and safe options, Dr. Grinspoon said: Enroll in a clinical study or find a facility in a state or country — such as Oregon or Jamaica — that offers microdosing with psilocybin.
Clinicians also should warn their patients that the consequences of obtaining illicit psilocybin could exacerbate the mental health stresses they are seeking to alleviate.
“It’s going to get worse if they get tangled up with law enforcement or take something that’s contaminated and they get real sick,” he said.
Lisa Gillespie contributed reporting to this story. A version of this article appeared on Medscape.com.
Peter Grinspoon, MD, has some advice for clinicians when patients ask questions about microdosing of psychedelics: Keep the lines of communication open — and don’t be judgmental.
“If you’re dismissive or critical or sound like you’re judging them, then the patients just clam up,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and a primary care physician at Massachusetts General Hospital, both in Boston.
Psychedelic drugs are still illegal in the majority of states despite the growth of public interest in and use of these substances. That growth is evidenced by a flurry of workshops, reports, law enforcement seizures, and pressure by Congressional members for the Food and Drug Administration to approve new psychedelic drugs, just in the past year.
A recent study in JAMA Health Forum showed a nearly 14-fold increase in Google searches — from 7.9 to 105.6 per 10 million nationwide — for the term “microdosing” and related wording, between 2015 and 2023.
Two states — Oregon and Colorado — have decriminalized certain psychedelic drugs and are in various stages of establishing regulations and centers for prospective clients. Almost two dozen localities, like Ann Arbor, Michigan, have decriminalized psychedelic drugs. A handful of states have active legislation to decriminalize use, while others have bills that never made it out of committee.
But no definitive studies have reported that microdosing produces positive mental effects at a higher rate than placebo, according to Dr. Grinspoon. So
“We’re in this renaissance where everybody is idealizing these medications, as opposed to 20 years ago when we were in the war on drugs and everybody was dismissing them,” Dr. Grinspoon said. “The truth is somewhere in between.”
The Science
Microdosing is defined as taking doses of 1/5 to 1/20 of the conventional recreational amount, which might include a dried psilocybin mushroom, lysergic acid diethylamide, or 3,4-methylenedioxymethamphetamine. But even that much may be neither effective nor safe.
Dr. Grinspoon said clinicians should tell patients that psychedelics may cause harm, although the drugs are relatively nontoxic and are not addictive. An illegally obtained psilocybin could cause negative reactions, especially if the drug has been adulterated with other substances and if the actual dose is higher than what was indicated by the seller.
He noted that people have different reactions to psychedelics, just as they have to prescription medications. He cited one example of a woman who microdosed and could not sleep for 2 weeks afterward. Only recently have randomized, double-blinded studies begun on benefits and harms.
Researchers have also begun investigating whether long-term microdosing of psilocybin could lead to valvular heart disease (VHD), said Kevin Yang, MD, a psychiatry resident at the University of California San Diego School of Medicine. A recent review of evidence concluded that microdosing various psychedelics over a period of months can lead to drug-induced VHD.
“It’s extremely important to emphasize with patients that not only do we not know if it works or not, we also don’t really know how safe it is,” Dr. Yang said.
Dr. Yang also said clinicians should consider referring patients to a mental health professional, and especially those that may have expertise in psychedelic therapies.
One of those experts is Rachel Yehuda, PhD, director of the Center for Psychedelic Psychotherapy and Trauma Research at Icahn School of Medicine at Mount Sinai in New York City. She said therapists should be able to assess the patient’s perceived need for microdosing and “invite reflections about why current approaches are falling short.”
“I would also not actively discourage it either but remain curious until both of you have a better understanding of the reasons for seeking this out and potential alternative strategies for obtaining more therapeutic benefits,” she said. “I think it is really important to study the effects of both micro- and macrodosing of psychedelics but not move in advance of the data.”
Navigating Legality
Recent ballot measures in Oregon and Colorado directed the states to develop regulated and licensed psilocybin-assisted therapy centers for legal “trips.” Oregon’s first center was opened in 2023, and Colorado is now developing its own licensing model.
According to the Oregon Health Authority, the centers are not medical facilities, and prescription or referral from a medical professional is not required.
The Oregon Academy of Family Physicians (OAFP) has yet to release guidance to clinicians on how to talk to their patients about these drugs or potential interest in visiting a licensed therapy center.
However, Betsy Boyd-Flynn, executive director of OAFP, said the organization is working on continuing medical education for what the average family physician needs to know if a patient asks about use.
“We suspect that many of our members have interest and want to learn more,” she said.
Dr. Grinspoon said clinicians should talk with patients about legality during these conversations.
“The big question I get is: ‘I really want to try microdosing, but how do I obtain the mushrooms?’ ” he said. “You can’t really as a physician tell them to do anything illegal. So you tell them to be safe, be careful, and to use their judgment.”
Patients who want to pursue microdosing who do not live in Oregon have two legal and safe options, Dr. Grinspoon said: Enroll in a clinical study or find a facility in a state or country — such as Oregon or Jamaica — that offers microdosing with psilocybin.
Clinicians also should warn their patients that the consequences of obtaining illicit psilocybin could exacerbate the mental health stresses they are seeking to alleviate.
“It’s going to get worse if they get tangled up with law enforcement or take something that’s contaminated and they get real sick,” he said.
Lisa Gillespie contributed reporting to this story. A version of this article appeared on Medscape.com.
Peter Grinspoon, MD, has some advice for clinicians when patients ask questions about microdosing of psychedelics: Keep the lines of communication open — and don’t be judgmental.
“If you’re dismissive or critical or sound like you’re judging them, then the patients just clam up,” said Dr. Grinspoon, a professor of medicine at Harvard Medical School and a primary care physician at Massachusetts General Hospital, both in Boston.
Psychedelic drugs are still illegal in the majority of states despite the growth of public interest in and use of these substances. That growth is evidenced by a flurry of workshops, reports, law enforcement seizures, and pressure by Congressional members for the Food and Drug Administration to approve new psychedelic drugs, just in the past year.
A recent study in JAMA Health Forum showed a nearly 14-fold increase in Google searches — from 7.9 to 105.6 per 10 million nationwide — for the term “microdosing” and related wording, between 2015 and 2023.
Two states — Oregon and Colorado — have decriminalized certain psychedelic drugs and are in various stages of establishing regulations and centers for prospective clients. Almost two dozen localities, like Ann Arbor, Michigan, have decriminalized psychedelic drugs. A handful of states have active legislation to decriminalize use, while others have bills that never made it out of committee.
But no definitive studies have reported that microdosing produces positive mental effects at a higher rate than placebo, according to Dr. Grinspoon. So
“We’re in this renaissance where everybody is idealizing these medications, as opposed to 20 years ago when we were in the war on drugs and everybody was dismissing them,” Dr. Grinspoon said. “The truth is somewhere in between.”
The Science
Microdosing is defined as taking doses of 1/5 to 1/20 of the conventional recreational amount, which might include a dried psilocybin mushroom, lysergic acid diethylamide, or 3,4-methylenedioxymethamphetamine. But even that much may be neither effective nor safe.
Dr. Grinspoon said clinicians should tell patients that psychedelics may cause harm, although the drugs are relatively nontoxic and are not addictive. An illegally obtained psilocybin could cause negative reactions, especially if the drug has been adulterated with other substances and if the actual dose is higher than what was indicated by the seller.
He noted that people have different reactions to psychedelics, just as they have to prescription medications. He cited one example of a woman who microdosed and could not sleep for 2 weeks afterward. Only recently have randomized, double-blinded studies begun on benefits and harms.
Researchers have also begun investigating whether long-term microdosing of psilocybin could lead to valvular heart disease (VHD), said Kevin Yang, MD, a psychiatry resident at the University of California San Diego School of Medicine. A recent review of evidence concluded that microdosing various psychedelics over a period of months can lead to drug-induced VHD.
“It’s extremely important to emphasize with patients that not only do we not know if it works or not, we also don’t really know how safe it is,” Dr. Yang said.
Dr. Yang also said clinicians should consider referring patients to a mental health professional, and especially those that may have expertise in psychedelic therapies.
One of those experts is Rachel Yehuda, PhD, director of the Center for Psychedelic Psychotherapy and Trauma Research at Icahn School of Medicine at Mount Sinai in New York City. She said therapists should be able to assess the patient’s perceived need for microdosing and “invite reflections about why current approaches are falling short.”
“I would also not actively discourage it either but remain curious until both of you have a better understanding of the reasons for seeking this out and potential alternative strategies for obtaining more therapeutic benefits,” she said. “I think it is really important to study the effects of both micro- and macrodosing of psychedelics but not move in advance of the data.”
Navigating Legality
Recent ballot measures in Oregon and Colorado directed the states to develop regulated and licensed psilocybin-assisted therapy centers for legal “trips.” Oregon’s first center was opened in 2023, and Colorado is now developing its own licensing model.
According to the Oregon Health Authority, the centers are not medical facilities, and prescription or referral from a medical professional is not required.
The Oregon Academy of Family Physicians (OAFP) has yet to release guidance to clinicians on how to talk to their patients about these drugs or potential interest in visiting a licensed therapy center.
However, Betsy Boyd-Flynn, executive director of OAFP, said the organization is working on continuing medical education for what the average family physician needs to know if a patient asks about use.
“We suspect that many of our members have interest and want to learn more,” she said.
Dr. Grinspoon said clinicians should talk with patients about legality during these conversations.
“The big question I get is: ‘I really want to try microdosing, but how do I obtain the mushrooms?’ ” he said. “You can’t really as a physician tell them to do anything illegal. So you tell them to be safe, be careful, and to use their judgment.”
Patients who want to pursue microdosing who do not live in Oregon have two legal and safe options, Dr. Grinspoon said: Enroll in a clinical study or find a facility in a state or country — such as Oregon or Jamaica — that offers microdosing with psilocybin.
Clinicians also should warn their patients that the consequences of obtaining illicit psilocybin could exacerbate the mental health stresses they are seeking to alleviate.
“It’s going to get worse if they get tangled up with law enforcement or take something that’s contaminated and they get real sick,” he said.
Lisa Gillespie contributed reporting to this story. A version of this article appeared on Medscape.com.
Anxiety Linked to a Threefold Increased Risk for Dementia
TOPLINE:
, new research shows.
METHODOLOGY:
- A total of 2132 participants aged 55-85 years (mean age, 76 years) were recruited from the Hunter Community Study. Of these, 53% were women.
- Participants were assessed over three different waves, 5 years apart. Demographic and health-related data were captured at wave 1.
- Researchers used the Kessler Psychological Distress Scale (K10) to measure anxiety at two points: Baseline (wave 1) and first follow-up (wave 2), with a 5-year interval between them. Anxiety was classified as chronic if present during both waves, resolved if only present at wave 1, and new if only appearing at wave 2.
- The primary outcome, incident all-cause dementia, during the follow-up period (maximum 13 years after baseline) was identified using the International Classification of Disease-10 codes.
TAKEAWAY:
- Out of 2132 cognitively healthy participants, 64 developed dementia, with an average time to diagnosis of 10 years. Chronic anxiety was linked to a 2.8-fold increased risk for dementia, while new-onset anxiety was associated with a 3.2-fold increased risk (P = .01).
- Participants younger than 70 years with chronic anxiety had a 4.6-fold increased risk for dementia (P = .03), and those with new-onset anxiety had a 7.2 times higher risk for dementia (P = .004).
- There was no significant risk for dementia in participants with anxiety that had resolved.
- Investigators speculated that individuals with anxiety were more likely to engage in unhealthy lifestyle behaviors, such as poor diet and smoking, which can lead to cardiovascular disease — a condition strongly associated with dementia.
IN PRACTICE:
“This prospective cohort study used causal inference methods to explore the role of anxiety in promoting the development of dementia,” lead author Kay Khaing, MMed, The University of Newcastle, Australia, wrote in a press release. “The findings suggest that anxiety may be a new risk factor to target in the prevention of dementia and also indicate that treating anxiety may reduce this risk.”
SOURCE:
Kay Khaing, MMed, of The University of Newcastle, Australia, led the study, which was published online in the Journal of the American Geriatrics Society.
LIMITATIONS:
Anxiety was measured using K10, which assessed symptoms experienced in the most recent 4 weeks, raising concerns about its accuracy over the entire observation period. The authors acknowledged that despite using a combination of the total K10 score and the anxiety subscale, the overlap of anxiety and depression might not be fully disentangled, leading to residual confounding by depression. Additionally, 33% of participants were lost to follow-up, and those lost had higher anxiety rates at baseline, potentially leading to missing cases of dementia and affecting the effect estimate.
DISCLOSURES:
This study did not report any funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
, new research shows.
METHODOLOGY:
- A total of 2132 participants aged 55-85 years (mean age, 76 years) were recruited from the Hunter Community Study. Of these, 53% were women.
- Participants were assessed over three different waves, 5 years apart. Demographic and health-related data were captured at wave 1.
- Researchers used the Kessler Psychological Distress Scale (K10) to measure anxiety at two points: Baseline (wave 1) and first follow-up (wave 2), with a 5-year interval between them. Anxiety was classified as chronic if present during both waves, resolved if only present at wave 1, and new if only appearing at wave 2.
- The primary outcome, incident all-cause dementia, during the follow-up period (maximum 13 years after baseline) was identified using the International Classification of Disease-10 codes.
TAKEAWAY:
- Out of 2132 cognitively healthy participants, 64 developed dementia, with an average time to diagnosis of 10 years. Chronic anxiety was linked to a 2.8-fold increased risk for dementia, while new-onset anxiety was associated with a 3.2-fold increased risk (P = .01).
- Participants younger than 70 years with chronic anxiety had a 4.6-fold increased risk for dementia (P = .03), and those with new-onset anxiety had a 7.2 times higher risk for dementia (P = .004).
- There was no significant risk for dementia in participants with anxiety that had resolved.
- Investigators speculated that individuals with anxiety were more likely to engage in unhealthy lifestyle behaviors, such as poor diet and smoking, which can lead to cardiovascular disease — a condition strongly associated with dementia.
IN PRACTICE:
“This prospective cohort study used causal inference methods to explore the role of anxiety in promoting the development of dementia,” lead author Kay Khaing, MMed, The University of Newcastle, Australia, wrote in a press release. “The findings suggest that anxiety may be a new risk factor to target in the prevention of dementia and also indicate that treating anxiety may reduce this risk.”
SOURCE:
Kay Khaing, MMed, of The University of Newcastle, Australia, led the study, which was published online in the Journal of the American Geriatrics Society.
LIMITATIONS:
Anxiety was measured using K10, which assessed symptoms experienced in the most recent 4 weeks, raising concerns about its accuracy over the entire observation period. The authors acknowledged that despite using a combination of the total K10 score and the anxiety subscale, the overlap of anxiety and depression might not be fully disentangled, leading to residual confounding by depression. Additionally, 33% of participants were lost to follow-up, and those lost had higher anxiety rates at baseline, potentially leading to missing cases of dementia and affecting the effect estimate.
DISCLOSURES:
This study did not report any funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
, new research shows.
METHODOLOGY:
- A total of 2132 participants aged 55-85 years (mean age, 76 years) were recruited from the Hunter Community Study. Of these, 53% were women.
- Participants were assessed over three different waves, 5 years apart. Demographic and health-related data were captured at wave 1.
- Researchers used the Kessler Psychological Distress Scale (K10) to measure anxiety at two points: Baseline (wave 1) and first follow-up (wave 2), with a 5-year interval between them. Anxiety was classified as chronic if present during both waves, resolved if only present at wave 1, and new if only appearing at wave 2.
- The primary outcome, incident all-cause dementia, during the follow-up period (maximum 13 years after baseline) was identified using the International Classification of Disease-10 codes.
TAKEAWAY:
- Out of 2132 cognitively healthy participants, 64 developed dementia, with an average time to diagnosis of 10 years. Chronic anxiety was linked to a 2.8-fold increased risk for dementia, while new-onset anxiety was associated with a 3.2-fold increased risk (P = .01).
- Participants younger than 70 years with chronic anxiety had a 4.6-fold increased risk for dementia (P = .03), and those with new-onset anxiety had a 7.2 times higher risk for dementia (P = .004).
- There was no significant risk for dementia in participants with anxiety that had resolved.
- Investigators speculated that individuals with anxiety were more likely to engage in unhealthy lifestyle behaviors, such as poor diet and smoking, which can lead to cardiovascular disease — a condition strongly associated with dementia.
IN PRACTICE:
“This prospective cohort study used causal inference methods to explore the role of anxiety in promoting the development of dementia,” lead author Kay Khaing, MMed, The University of Newcastle, Australia, wrote in a press release. “The findings suggest that anxiety may be a new risk factor to target in the prevention of dementia and also indicate that treating anxiety may reduce this risk.”
SOURCE:
Kay Khaing, MMed, of The University of Newcastle, Australia, led the study, which was published online in the Journal of the American Geriatrics Society.
LIMITATIONS:
Anxiety was measured using K10, which assessed symptoms experienced in the most recent 4 weeks, raising concerns about its accuracy over the entire observation period. The authors acknowledged that despite using a combination of the total K10 score and the anxiety subscale, the overlap of anxiety and depression might not be fully disentangled, leading to residual confounding by depression. Additionally, 33% of participants were lost to follow-up, and those lost had higher anxiety rates at baseline, potentially leading to missing cases of dementia and affecting the effect estimate.
DISCLOSURES:
This study did not report any funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.







