User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
How Common Is Pediatric Emergency Mistriage?
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.
“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.
“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.
“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
FROM JAMA PEDIATRICS
SUNY Downstate Emergency Medicine Doc Charged With $1.5M Fraud
In a case that spotlights the importance of comprehensive financial controls in medical offices,
Michael Lucchesi, MD, who had served as chairman of Emergency Medicine at SUNY Downstate Medical Center in New York City, was arraigned on July 9 and pleaded not guilty. Dr. Lucchesi’s attorney, Earl Ward, did not respond to messages from this news organization, but he told the New York Post that “the funds he used were not stolen funds.”
Dr. Lucchesi, who’s in his late 60s, faces nine counts of first- and second-degree grand larceny, first-degree falsifying business records, and third-degree criminal tax fraud. According to a press statement from the district attorney of Kings County, which encompasses the borough of Brooklyn, Dr. Lucchesi is accused of using his clinical practice’s business card for cash advances (about $115,000), high-end pet care ($176,000), personal travel ($348,000), gym membership and personal training ($109,000), catering ($52,000), tuition payments for his children ($46,000), and other expenses such as online shopping, flowers, liquor, and electronics.
Most of the alleged pet care spending — $120,000 — went to the Green Leaf Pet Resort, which has two locations in New Jersey, including one with “56 acres of nature and lots of tail wagging.” Some of the alleged spending on gym membership was at the New York Sports Clubs chain, where monthly membership tops out at $139.99.
The alleged spending occurred between 2016 and 2023 and was discovered by SUNY Downstate during an audit. Dr. Lucchesi reportedly left his position at the hospital, where he made $399,712 in 2022 as a professor, according to public records.
“As a high-ranking doctor at this vital healthcare institution, this defendant was entrusted with access to significant funds, which he allegedly exploited, stealing more than 1 million dollars to pay for a lavish lifestyle,” District Attorney Eric Gonzalez said in a statement.
SUNY Downstate is in a fight for its life amid efforts by New York Governor Kathy Hochul to shut it down. According to The New York Times, it is the only state-run hospital in New York City.
Dr. Lucchesi, who had previously served as the hospital’s chief medical officer and acting head, was released without bail. His next court date is September 25, 2024.
Size of Alleged Theft Is ‘Very Unusual’
David P. Weber, JD, DBA, a professor and fraud specialist at Salisbury University, Salisbury, Maryland, told this news organization that the fraudulent use of a business or purchase credit card is a form of embezzlement and “one of the most frequently seen types of frauds against organizations.”
William J. Kresse, JD, MSA, CPA/CFF, who studies fraud at Governors State University in University Park, Illinois, noted in an interview with this news organization that the high amount of alleged fraud in this case is “very unusual,” as is the period it is said to have occurred (over 6 years).
Mr. Kresse highlighted a 2024 report by the Association of Certified Fraud Examiners, which found that the median fraud loss in healthcare, on the basis of 117 cases, is $100,000. The most common form of fraud in the industry is corruption (47%), followed by billing (38%), noncash theft such as inventory (22%), and expense reimbursement (21%).
The details of the current case suggest that “SUNY Downstate had weak or insufficient internal controls to prevent this type of fraud,” Salisbury University’s Mr. Weber said. “However, research also makes clear that the tenure and position of the perpetrator play a significant role in the size of the fraud. Internal controls are supposed to apply to all employees, but the higher in the organization the perpetrator is, the easier it can be to engage in fraud.”
Even Small Medical Offices Can Act to Prevent Fraud
What can be done to prevent this kind of fraud? “Each employee should be required to submit actual receipts or scanned copies, and the reimbursement requests should be reviewed and inputted by a separate department or office of the organization to ensure that the expenses are legitimate,” Mr. Weber said. “In addition, all credit card statements should be available for review by the organization either simultaneously with the bill going to the employee or available for audit or review at any time without notification to the employee. Expenses that are in certain categories should be prohibited automatically and coded to the card so such a charge is rejected by the credit card bank.”
Smaller businesses — like many medical practices — may not have the manpower to handle these roles. In that case, Mr. Weber said, “The key is segregation or separation of duties. The bookkeeper cannot be the person receiving the bank statements, the payments from patients, and the invoices from vendors. There needs to be at least one other person in the loop to have some level of control.”
One strategy, he said, “is that the practice should institute a policy that only the doctor or owner of the practice can receive the mail, not the bookkeeper. Even if the practice leader does not actually review the bank statements, simply opening them before handing them off to the bookkeeper can provide a level of deterrence [since] the employee may get caught if someone else is reviewing the bank statements.”
A version of this article first appeared on Medscape.com.
In a case that spotlights the importance of comprehensive financial controls in medical offices,
Michael Lucchesi, MD, who had served as chairman of Emergency Medicine at SUNY Downstate Medical Center in New York City, was arraigned on July 9 and pleaded not guilty. Dr. Lucchesi’s attorney, Earl Ward, did not respond to messages from this news organization, but he told the New York Post that “the funds he used were not stolen funds.”
Dr. Lucchesi, who’s in his late 60s, faces nine counts of first- and second-degree grand larceny, first-degree falsifying business records, and third-degree criminal tax fraud. According to a press statement from the district attorney of Kings County, which encompasses the borough of Brooklyn, Dr. Lucchesi is accused of using his clinical practice’s business card for cash advances (about $115,000), high-end pet care ($176,000), personal travel ($348,000), gym membership and personal training ($109,000), catering ($52,000), tuition payments for his children ($46,000), and other expenses such as online shopping, flowers, liquor, and electronics.
Most of the alleged pet care spending — $120,000 — went to the Green Leaf Pet Resort, which has two locations in New Jersey, including one with “56 acres of nature and lots of tail wagging.” Some of the alleged spending on gym membership was at the New York Sports Clubs chain, where monthly membership tops out at $139.99.
The alleged spending occurred between 2016 and 2023 and was discovered by SUNY Downstate during an audit. Dr. Lucchesi reportedly left his position at the hospital, where he made $399,712 in 2022 as a professor, according to public records.
“As a high-ranking doctor at this vital healthcare institution, this defendant was entrusted with access to significant funds, which he allegedly exploited, stealing more than 1 million dollars to pay for a lavish lifestyle,” District Attorney Eric Gonzalez said in a statement.
SUNY Downstate is in a fight for its life amid efforts by New York Governor Kathy Hochul to shut it down. According to The New York Times, it is the only state-run hospital in New York City.
Dr. Lucchesi, who had previously served as the hospital’s chief medical officer and acting head, was released without bail. His next court date is September 25, 2024.
Size of Alleged Theft Is ‘Very Unusual’
David P. Weber, JD, DBA, a professor and fraud specialist at Salisbury University, Salisbury, Maryland, told this news organization that the fraudulent use of a business or purchase credit card is a form of embezzlement and “one of the most frequently seen types of frauds against organizations.”
William J. Kresse, JD, MSA, CPA/CFF, who studies fraud at Governors State University in University Park, Illinois, noted in an interview with this news organization that the high amount of alleged fraud in this case is “very unusual,” as is the period it is said to have occurred (over 6 years).
Mr. Kresse highlighted a 2024 report by the Association of Certified Fraud Examiners, which found that the median fraud loss in healthcare, on the basis of 117 cases, is $100,000. The most common form of fraud in the industry is corruption (47%), followed by billing (38%), noncash theft such as inventory (22%), and expense reimbursement (21%).
The details of the current case suggest that “SUNY Downstate had weak or insufficient internal controls to prevent this type of fraud,” Salisbury University’s Mr. Weber said. “However, research also makes clear that the tenure and position of the perpetrator play a significant role in the size of the fraud. Internal controls are supposed to apply to all employees, but the higher in the organization the perpetrator is, the easier it can be to engage in fraud.”
Even Small Medical Offices Can Act to Prevent Fraud
What can be done to prevent this kind of fraud? “Each employee should be required to submit actual receipts or scanned copies, and the reimbursement requests should be reviewed and inputted by a separate department or office of the organization to ensure that the expenses are legitimate,” Mr. Weber said. “In addition, all credit card statements should be available for review by the organization either simultaneously with the bill going to the employee or available for audit or review at any time without notification to the employee. Expenses that are in certain categories should be prohibited automatically and coded to the card so such a charge is rejected by the credit card bank.”
Smaller businesses — like many medical practices — may not have the manpower to handle these roles. In that case, Mr. Weber said, “The key is segregation or separation of duties. The bookkeeper cannot be the person receiving the bank statements, the payments from patients, and the invoices from vendors. There needs to be at least one other person in the loop to have some level of control.”
One strategy, he said, “is that the practice should institute a policy that only the doctor or owner of the practice can receive the mail, not the bookkeeper. Even if the practice leader does not actually review the bank statements, simply opening them before handing them off to the bookkeeper can provide a level of deterrence [since] the employee may get caught if someone else is reviewing the bank statements.”
A version of this article first appeared on Medscape.com.
In a case that spotlights the importance of comprehensive financial controls in medical offices,
Michael Lucchesi, MD, who had served as chairman of Emergency Medicine at SUNY Downstate Medical Center in New York City, was arraigned on July 9 and pleaded not guilty. Dr. Lucchesi’s attorney, Earl Ward, did not respond to messages from this news organization, but he told the New York Post that “the funds he used were not stolen funds.”
Dr. Lucchesi, who’s in his late 60s, faces nine counts of first- and second-degree grand larceny, first-degree falsifying business records, and third-degree criminal tax fraud. According to a press statement from the district attorney of Kings County, which encompasses the borough of Brooklyn, Dr. Lucchesi is accused of using his clinical practice’s business card for cash advances (about $115,000), high-end pet care ($176,000), personal travel ($348,000), gym membership and personal training ($109,000), catering ($52,000), tuition payments for his children ($46,000), and other expenses such as online shopping, flowers, liquor, and electronics.
Most of the alleged pet care spending — $120,000 — went to the Green Leaf Pet Resort, which has two locations in New Jersey, including one with “56 acres of nature and lots of tail wagging.” Some of the alleged spending on gym membership was at the New York Sports Clubs chain, where monthly membership tops out at $139.99.
The alleged spending occurred between 2016 and 2023 and was discovered by SUNY Downstate during an audit. Dr. Lucchesi reportedly left his position at the hospital, where he made $399,712 in 2022 as a professor, according to public records.
“As a high-ranking doctor at this vital healthcare institution, this defendant was entrusted with access to significant funds, which he allegedly exploited, stealing more than 1 million dollars to pay for a lavish lifestyle,” District Attorney Eric Gonzalez said in a statement.
SUNY Downstate is in a fight for its life amid efforts by New York Governor Kathy Hochul to shut it down. According to The New York Times, it is the only state-run hospital in New York City.
Dr. Lucchesi, who had previously served as the hospital’s chief medical officer and acting head, was released without bail. His next court date is September 25, 2024.
Size of Alleged Theft Is ‘Very Unusual’
David P. Weber, JD, DBA, a professor and fraud specialist at Salisbury University, Salisbury, Maryland, told this news organization that the fraudulent use of a business or purchase credit card is a form of embezzlement and “one of the most frequently seen types of frauds against organizations.”
William J. Kresse, JD, MSA, CPA/CFF, who studies fraud at Governors State University in University Park, Illinois, noted in an interview with this news organization that the high amount of alleged fraud in this case is “very unusual,” as is the period it is said to have occurred (over 6 years).
Mr. Kresse highlighted a 2024 report by the Association of Certified Fraud Examiners, which found that the median fraud loss in healthcare, on the basis of 117 cases, is $100,000. The most common form of fraud in the industry is corruption (47%), followed by billing (38%), noncash theft such as inventory (22%), and expense reimbursement (21%).
The details of the current case suggest that “SUNY Downstate had weak or insufficient internal controls to prevent this type of fraud,” Salisbury University’s Mr. Weber said. “However, research also makes clear that the tenure and position of the perpetrator play a significant role in the size of the fraud. Internal controls are supposed to apply to all employees, but the higher in the organization the perpetrator is, the easier it can be to engage in fraud.”
Even Small Medical Offices Can Act to Prevent Fraud
What can be done to prevent this kind of fraud? “Each employee should be required to submit actual receipts or scanned copies, and the reimbursement requests should be reviewed and inputted by a separate department or office of the organization to ensure that the expenses are legitimate,” Mr. Weber said. “In addition, all credit card statements should be available for review by the organization either simultaneously with the bill going to the employee or available for audit or review at any time without notification to the employee. Expenses that are in certain categories should be prohibited automatically and coded to the card so such a charge is rejected by the credit card bank.”
Smaller businesses — like many medical practices — may not have the manpower to handle these roles. In that case, Mr. Weber said, “The key is segregation or separation of duties. The bookkeeper cannot be the person receiving the bank statements, the payments from patients, and the invoices from vendors. There needs to be at least one other person in the loop to have some level of control.”
One strategy, he said, “is that the practice should institute a policy that only the doctor or owner of the practice can receive the mail, not the bookkeeper. Even if the practice leader does not actually review the bank statements, simply opening them before handing them off to the bookkeeper can provide a level of deterrence [since] the employee may get caught if someone else is reviewing the bank statements.”
A version of this article first appeared on Medscape.com.
How Drones Are Reducing Emergency Response Times
The drones are coming.
Starting in September, if someone in Clemmons, North Carolina, calls 911 to report a cardiac arrest, the first responder on the scene may be a drone carrying an automated external defibrillator, or AED.
“The idea is for the drone to get there several minutes before first responders,” such as an emergency medical technician or an ambulance, said Daniel Crews, a spokesperson for the sheriff’s office in Forsyth County, where Clemmons is located. The sheriff’s office is partnering on the project with local emergency services, the Clinical Research Institute at Duke University, and the drone consulting firm Hovecon. “The ultimate goal is to save lives and improve life expectancy for someone experiencing a cardiac episode,” Mr. Crews said.
The Forsyth County program is one of a growing number of efforts by public safety and healthcare organizations across the country to use drones to speed up lifesaving treatment in situations in which every second counts.
More than 356,000 people have a cardiac arrest outside of a hospital setting every year in the United States, according to the American Heart Association. Most people are at home when it happens, and about 90% die because they don’t get immediate help from first responders or bystanders. Every minute that passes without medical intervention decreases the odds of survival by 10%.
“We’ve never been able to move the needle for cardiac arrest in private settings, and this technology could meet that need,” said Monique Anderson Starks, MD, a cardiologist and associate professor of medicine at Duke University. Dr. Starks is leading pilot studies in Forsyth County and James City County, Virginia, to test whether drone AED delivery can improve treatment response times. The work is funded by a 4-year grant from the American Heart Association.
Dr. Starks said she believes the drone-delivered AEDs in the pilot study could reduce the time to treatment by 4 minutes compared with first responders.
Unlike a heart attack, which occurs when blood flow to the heart is blocked, a cardiac arrest happens when a heart malfunction causes it to stop beating, typically because of an arrhythmia or an electrical problem. Eighty percent of cardiac arrests start as heart attacks. The only way to get the heart restarted is with CPR and a defibrillator.
In Forsyth County, a drone pilot from the sheriff’s department will listen in on 911 calls. If there’s a suspected cardiac arrest, the pilot can dispatch the drone even before emergency medical services are contacted. The drone, which weighs 22 pounds and can travel 60 mph, will fly to the location and hover 125 feet in the air before lowering an AED to the ground on a winch. The AED provides simple verbal instructions; the 911 dispatcher on the phone can also help a bystander use the AED.
Eventually there will be six drone bases in Forsyth and James City counties, Dr. Starks said.
While the technology is promising and research has often found that drones arrive faster than first responders, there’s little conclusive evidence that drones improve health outcomes.
A Swedish study published in The Lancet in 2023 compared the response times between drones and ambulances for suspected cardiac arrest in 58 deployments in an area of about 200,000 people. It found that drones beat the ambulance to the scene two thirds of the time, by a median of 3 minutes and 14 seconds.
In the United States, most programs are just getting started, and they are exploring the use of drones to also provide remedies for drug overdoses and major trauma or potential drowning rescues.
In Florida, Tampa General Hospital, Manatee County, and Archer First Response Systems, or AFRS, began a program in May to deliver AEDs, a tourniquet, and Narcan, a nasal spray that can reverse an opioid overdose. The program initially covers a 7-square-mile area, and EMS dispatchers deploy the drones, which are monitored by drone pilots.
There were nearly 108,000 drug overdose deaths in the United States in 2022, according to the National Institute on Drug Abuse.
As of early July, the Tampa program hadn’t yet deployed any drones, said Gordon Folkes, the founder and chief executive of AFRS, which develops and deploys emergency drone logistics systems. One request in June to send a drone to an overdose couldn’t be fulfilled because of a violent thunderstorm, Mr. Folkes said. In the testing area, which covers about 7,000 residents, Mr. Folkes estimates that 10-15 drones might be deployed each year.
“The bread and butter for these systems is suburban areas” like Manatee County that are well-populated and where the drones have the advantage of being able to avoid traffic congestion, Mr. Folkes said.
There are other uses for drones in medical emergencies. The New York Police Department plans to drop emergency flotation devices to struggling swimmers at local beaches. In Chula Vista, California, a police drone was able to pinpoint the location of a burning car, and then officers pulled the driver out, said Sgt. Tony Molina.
Rescue personnel have used drones to locate people who wander away from nursing homes, said James Augustine, a spokesperson for the American College of Emergency Physicians who is the medical director for the International Association of Fire Chiefs.
In the United States, one hurdle for drone programs is that the Federal Aviation Administration typically requires that drones be operated within the operators’ visual line of sight. In May, when Congress passed the FAA reauthorization bill, it gave the FAA 4 months to issue a notice of proposed rule-making on drone operations beyond the visual line of sight.
“The FAA is focused on developing standard rules to make [Beyond Visual Line of Sight] operations routine, scalable, and economically viable,” said Rick Breitenfeldt, an FAA spokesperson.
Some civil liberties groups are concerned that the FAA’s new rules may not provide enough protection from drone cameras for people on the ground.
Jay Stanley, a senior policy analyst at the American Civil Liberties Union, acknowledged the benefits of using drones in emergency situations but said there are issues that need to be addressed.
“The concern is that the FAA is going to significantly loosen the reins of drones without any significant privacy protections,” he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.
The drones are coming.
Starting in September, if someone in Clemmons, North Carolina, calls 911 to report a cardiac arrest, the first responder on the scene may be a drone carrying an automated external defibrillator, or AED.
“The idea is for the drone to get there several minutes before first responders,” such as an emergency medical technician or an ambulance, said Daniel Crews, a spokesperson for the sheriff’s office in Forsyth County, where Clemmons is located. The sheriff’s office is partnering on the project with local emergency services, the Clinical Research Institute at Duke University, and the drone consulting firm Hovecon. “The ultimate goal is to save lives and improve life expectancy for someone experiencing a cardiac episode,” Mr. Crews said.
The Forsyth County program is one of a growing number of efforts by public safety and healthcare organizations across the country to use drones to speed up lifesaving treatment in situations in which every second counts.
More than 356,000 people have a cardiac arrest outside of a hospital setting every year in the United States, according to the American Heart Association. Most people are at home when it happens, and about 90% die because they don’t get immediate help from first responders or bystanders. Every minute that passes without medical intervention decreases the odds of survival by 10%.
“We’ve never been able to move the needle for cardiac arrest in private settings, and this technology could meet that need,” said Monique Anderson Starks, MD, a cardiologist and associate professor of medicine at Duke University. Dr. Starks is leading pilot studies in Forsyth County and James City County, Virginia, to test whether drone AED delivery can improve treatment response times. The work is funded by a 4-year grant from the American Heart Association.
Dr. Starks said she believes the drone-delivered AEDs in the pilot study could reduce the time to treatment by 4 minutes compared with first responders.
Unlike a heart attack, which occurs when blood flow to the heart is blocked, a cardiac arrest happens when a heart malfunction causes it to stop beating, typically because of an arrhythmia or an electrical problem. Eighty percent of cardiac arrests start as heart attacks. The only way to get the heart restarted is with CPR and a defibrillator.
In Forsyth County, a drone pilot from the sheriff’s department will listen in on 911 calls. If there’s a suspected cardiac arrest, the pilot can dispatch the drone even before emergency medical services are contacted. The drone, which weighs 22 pounds and can travel 60 mph, will fly to the location and hover 125 feet in the air before lowering an AED to the ground on a winch. The AED provides simple verbal instructions; the 911 dispatcher on the phone can also help a bystander use the AED.
Eventually there will be six drone bases in Forsyth and James City counties, Dr. Starks said.
While the technology is promising and research has often found that drones arrive faster than first responders, there’s little conclusive evidence that drones improve health outcomes.
A Swedish study published in The Lancet in 2023 compared the response times between drones and ambulances for suspected cardiac arrest in 58 deployments in an area of about 200,000 people. It found that drones beat the ambulance to the scene two thirds of the time, by a median of 3 minutes and 14 seconds.
In the United States, most programs are just getting started, and they are exploring the use of drones to also provide remedies for drug overdoses and major trauma or potential drowning rescues.
In Florida, Tampa General Hospital, Manatee County, and Archer First Response Systems, or AFRS, began a program in May to deliver AEDs, a tourniquet, and Narcan, a nasal spray that can reverse an opioid overdose. The program initially covers a 7-square-mile area, and EMS dispatchers deploy the drones, which are monitored by drone pilots.
There were nearly 108,000 drug overdose deaths in the United States in 2022, according to the National Institute on Drug Abuse.
As of early July, the Tampa program hadn’t yet deployed any drones, said Gordon Folkes, the founder and chief executive of AFRS, which develops and deploys emergency drone logistics systems. One request in June to send a drone to an overdose couldn’t be fulfilled because of a violent thunderstorm, Mr. Folkes said. In the testing area, which covers about 7,000 residents, Mr. Folkes estimates that 10-15 drones might be deployed each year.
“The bread and butter for these systems is suburban areas” like Manatee County that are well-populated and where the drones have the advantage of being able to avoid traffic congestion, Mr. Folkes said.
There are other uses for drones in medical emergencies. The New York Police Department plans to drop emergency flotation devices to struggling swimmers at local beaches. In Chula Vista, California, a police drone was able to pinpoint the location of a burning car, and then officers pulled the driver out, said Sgt. Tony Molina.
Rescue personnel have used drones to locate people who wander away from nursing homes, said James Augustine, a spokesperson for the American College of Emergency Physicians who is the medical director for the International Association of Fire Chiefs.
In the United States, one hurdle for drone programs is that the Federal Aviation Administration typically requires that drones be operated within the operators’ visual line of sight. In May, when Congress passed the FAA reauthorization bill, it gave the FAA 4 months to issue a notice of proposed rule-making on drone operations beyond the visual line of sight.
“The FAA is focused on developing standard rules to make [Beyond Visual Line of Sight] operations routine, scalable, and economically viable,” said Rick Breitenfeldt, an FAA spokesperson.
Some civil liberties groups are concerned that the FAA’s new rules may not provide enough protection from drone cameras for people on the ground.
Jay Stanley, a senior policy analyst at the American Civil Liberties Union, acknowledged the benefits of using drones in emergency situations but said there are issues that need to be addressed.
“The concern is that the FAA is going to significantly loosen the reins of drones without any significant privacy protections,” he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.
The drones are coming.
Starting in September, if someone in Clemmons, North Carolina, calls 911 to report a cardiac arrest, the first responder on the scene may be a drone carrying an automated external defibrillator, or AED.
“The idea is for the drone to get there several minutes before first responders,” such as an emergency medical technician or an ambulance, said Daniel Crews, a spokesperson for the sheriff’s office in Forsyth County, where Clemmons is located. The sheriff’s office is partnering on the project with local emergency services, the Clinical Research Institute at Duke University, and the drone consulting firm Hovecon. “The ultimate goal is to save lives and improve life expectancy for someone experiencing a cardiac episode,” Mr. Crews said.
The Forsyth County program is one of a growing number of efforts by public safety and healthcare organizations across the country to use drones to speed up lifesaving treatment in situations in which every second counts.
More than 356,000 people have a cardiac arrest outside of a hospital setting every year in the United States, according to the American Heart Association. Most people are at home when it happens, and about 90% die because they don’t get immediate help from first responders or bystanders. Every minute that passes without medical intervention decreases the odds of survival by 10%.
“We’ve never been able to move the needle for cardiac arrest in private settings, and this technology could meet that need,” said Monique Anderson Starks, MD, a cardiologist and associate professor of medicine at Duke University. Dr. Starks is leading pilot studies in Forsyth County and James City County, Virginia, to test whether drone AED delivery can improve treatment response times. The work is funded by a 4-year grant from the American Heart Association.
Dr. Starks said she believes the drone-delivered AEDs in the pilot study could reduce the time to treatment by 4 minutes compared with first responders.
Unlike a heart attack, which occurs when blood flow to the heart is blocked, a cardiac arrest happens when a heart malfunction causes it to stop beating, typically because of an arrhythmia or an electrical problem. Eighty percent of cardiac arrests start as heart attacks. The only way to get the heart restarted is with CPR and a defibrillator.
In Forsyth County, a drone pilot from the sheriff’s department will listen in on 911 calls. If there’s a suspected cardiac arrest, the pilot can dispatch the drone even before emergency medical services are contacted. The drone, which weighs 22 pounds and can travel 60 mph, will fly to the location and hover 125 feet in the air before lowering an AED to the ground on a winch. The AED provides simple verbal instructions; the 911 dispatcher on the phone can also help a bystander use the AED.
Eventually there will be six drone bases in Forsyth and James City counties, Dr. Starks said.
While the technology is promising and research has often found that drones arrive faster than first responders, there’s little conclusive evidence that drones improve health outcomes.
A Swedish study published in The Lancet in 2023 compared the response times between drones and ambulances for suspected cardiac arrest in 58 deployments in an area of about 200,000 people. It found that drones beat the ambulance to the scene two thirds of the time, by a median of 3 minutes and 14 seconds.
In the United States, most programs are just getting started, and they are exploring the use of drones to also provide remedies for drug overdoses and major trauma or potential drowning rescues.
In Florida, Tampa General Hospital, Manatee County, and Archer First Response Systems, or AFRS, began a program in May to deliver AEDs, a tourniquet, and Narcan, a nasal spray that can reverse an opioid overdose. The program initially covers a 7-square-mile area, and EMS dispatchers deploy the drones, which are monitored by drone pilots.
There were nearly 108,000 drug overdose deaths in the United States in 2022, according to the National Institute on Drug Abuse.
As of early July, the Tampa program hadn’t yet deployed any drones, said Gordon Folkes, the founder and chief executive of AFRS, which develops and deploys emergency drone logistics systems. One request in June to send a drone to an overdose couldn’t be fulfilled because of a violent thunderstorm, Mr. Folkes said. In the testing area, which covers about 7,000 residents, Mr. Folkes estimates that 10-15 drones might be deployed each year.
“The bread and butter for these systems is suburban areas” like Manatee County that are well-populated and where the drones have the advantage of being able to avoid traffic congestion, Mr. Folkes said.
There are other uses for drones in medical emergencies. The New York Police Department plans to drop emergency flotation devices to struggling swimmers at local beaches. In Chula Vista, California, a police drone was able to pinpoint the location of a burning car, and then officers pulled the driver out, said Sgt. Tony Molina.
Rescue personnel have used drones to locate people who wander away from nursing homes, said James Augustine, a spokesperson for the American College of Emergency Physicians who is the medical director for the International Association of Fire Chiefs.
In the United States, one hurdle for drone programs is that the Federal Aviation Administration typically requires that drones be operated within the operators’ visual line of sight. In May, when Congress passed the FAA reauthorization bill, it gave the FAA 4 months to issue a notice of proposed rule-making on drone operations beyond the visual line of sight.
“The FAA is focused on developing standard rules to make [Beyond Visual Line of Sight] operations routine, scalable, and economically viable,” said Rick Breitenfeldt, an FAA spokesperson.
Some civil liberties groups are concerned that the FAA’s new rules may not provide enough protection from drone cameras for people on the ground.
Jay Stanley, a senior policy analyst at the American Civil Liberties Union, acknowledged the benefits of using drones in emergency situations but said there are issues that need to be addressed.
“The concern is that the FAA is going to significantly loosen the reins of drones without any significant privacy protections,” he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.
‘Alarming’ Rise in Mental Health Hospital Admissions Involving Methamphetamine
new research showed. Investigators found that between 2008 and 2020, such admissions increased by more than 10-fold.
“Overall, our results show an alarming increase in mental health disorder–related hospitalizations with concurrent methamphetamine use from 2008 to 2020,” wrote the investigators, led by Diensn Xing, Department of Medicine, Louisiana State University Health Sciences Center, Shreveport.
“These results are especially concerning because these hospitalizations outpace hospitalizations for methamphetamine use alone or mental health disorders alone,” they added.
The study was published online in Nature Mental Health .
Action Needed
Mental illness and methamphetamine use are both growing health problems. The investigators pointed out that methamphetamine use can cause serious harm to an individual’s mental, emotional, and social well-being and can significantly alter the brain.
They added that long-term methamphetamine users can exhibit “extreme anxiety, confusion, troubled sleep, mood changes, and aggressive behavior.” In addition, use of the drug can cause psychotic side effects such as paranoia, hallucinations, delusions, and suicidality.
The investigators noted that, to date, no studies have examined the combined effects of both diseases or characterized national trends over more than 10 years.
The researchers analyzed US mental health–related trends in methamphetamine users from 2008 to 2020. In particular, they wanted to characterize which demographic and geographic groups might be affected by both of these diseases because people with mental illness and co-occurring methamphetamine use are an “intersectional group” that is “doubly vulnerable to suicide and overdose death due to the synergistic effects of methamphetamine and mental health disorders.”
The investigators evaluated US trends in mental health disorder–related hospital admissions (MHD-HAs) and compared them with mental health admissions that involved concurrent methamphetamine use (MHD-HA-MUs) between 2008 and 2020.
Using data from the largest US inpatient care database, which encompasses more than 7 million hospital stays annually, they examined close to 4 million weighted hospital admissions and found more than a 10-fold increase in MHD-HA-MUs, compared with a 1.4-fold increase in MHD-HAs.
MHD-HA-MUs increased significantly among men (13-fold), non-Hispanic Black patients (39-fold), and those aged 41-64 years (16-fold). In the southern United States, MHD-HA-MUs increased 24-fold, larger than in any other region in the United States.
“Overall, the data suggest that there are synergistic effects with methamphetamine use and mental health disorder, highlighting this patient group’s unique needs, requiring distinct action,” the researchers wrote.
They proposed several interventions, including public education about substance use disorders, mental illness, and the effects of stigma. They also suggested decreasing criminal penalties for those with substance use disorders and improving healthcare delivery for this patient population.
This work was supported by the National Institutes of Health and an award from the National Institute of General Medical Sciences. The study authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research showed. Investigators found that between 2008 and 2020, such admissions increased by more than 10-fold.
“Overall, our results show an alarming increase in mental health disorder–related hospitalizations with concurrent methamphetamine use from 2008 to 2020,” wrote the investigators, led by Diensn Xing, Department of Medicine, Louisiana State University Health Sciences Center, Shreveport.
“These results are especially concerning because these hospitalizations outpace hospitalizations for methamphetamine use alone or mental health disorders alone,” they added.
The study was published online in Nature Mental Health .
Action Needed
Mental illness and methamphetamine use are both growing health problems. The investigators pointed out that methamphetamine use can cause serious harm to an individual’s mental, emotional, and social well-being and can significantly alter the brain.
They added that long-term methamphetamine users can exhibit “extreme anxiety, confusion, troubled sleep, mood changes, and aggressive behavior.” In addition, use of the drug can cause psychotic side effects such as paranoia, hallucinations, delusions, and suicidality.
The investigators noted that, to date, no studies have examined the combined effects of both diseases or characterized national trends over more than 10 years.
The researchers analyzed US mental health–related trends in methamphetamine users from 2008 to 2020. In particular, they wanted to characterize which demographic and geographic groups might be affected by both of these diseases because people with mental illness and co-occurring methamphetamine use are an “intersectional group” that is “doubly vulnerable to suicide and overdose death due to the synergistic effects of methamphetamine and mental health disorders.”
The investigators evaluated US trends in mental health disorder–related hospital admissions (MHD-HAs) and compared them with mental health admissions that involved concurrent methamphetamine use (MHD-HA-MUs) between 2008 and 2020.
Using data from the largest US inpatient care database, which encompasses more than 7 million hospital stays annually, they examined close to 4 million weighted hospital admissions and found more than a 10-fold increase in MHD-HA-MUs, compared with a 1.4-fold increase in MHD-HAs.
MHD-HA-MUs increased significantly among men (13-fold), non-Hispanic Black patients (39-fold), and those aged 41-64 years (16-fold). In the southern United States, MHD-HA-MUs increased 24-fold, larger than in any other region in the United States.
“Overall, the data suggest that there are synergistic effects with methamphetamine use and mental health disorder, highlighting this patient group’s unique needs, requiring distinct action,” the researchers wrote.
They proposed several interventions, including public education about substance use disorders, mental illness, and the effects of stigma. They also suggested decreasing criminal penalties for those with substance use disorders and improving healthcare delivery for this patient population.
This work was supported by the National Institutes of Health and an award from the National Institute of General Medical Sciences. The study authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research showed. Investigators found that between 2008 and 2020, such admissions increased by more than 10-fold.
“Overall, our results show an alarming increase in mental health disorder–related hospitalizations with concurrent methamphetamine use from 2008 to 2020,” wrote the investigators, led by Diensn Xing, Department of Medicine, Louisiana State University Health Sciences Center, Shreveport.
“These results are especially concerning because these hospitalizations outpace hospitalizations for methamphetamine use alone or mental health disorders alone,” they added.
The study was published online in Nature Mental Health .
Action Needed
Mental illness and methamphetamine use are both growing health problems. The investigators pointed out that methamphetamine use can cause serious harm to an individual’s mental, emotional, and social well-being and can significantly alter the brain.
They added that long-term methamphetamine users can exhibit “extreme anxiety, confusion, troubled sleep, mood changes, and aggressive behavior.” In addition, use of the drug can cause psychotic side effects such as paranoia, hallucinations, delusions, and suicidality.
The investigators noted that, to date, no studies have examined the combined effects of both diseases or characterized national trends over more than 10 years.
The researchers analyzed US mental health–related trends in methamphetamine users from 2008 to 2020. In particular, they wanted to characterize which demographic and geographic groups might be affected by both of these diseases because people with mental illness and co-occurring methamphetamine use are an “intersectional group” that is “doubly vulnerable to suicide and overdose death due to the synergistic effects of methamphetamine and mental health disorders.”
The investigators evaluated US trends in mental health disorder–related hospital admissions (MHD-HAs) and compared them with mental health admissions that involved concurrent methamphetamine use (MHD-HA-MUs) between 2008 and 2020.
Using data from the largest US inpatient care database, which encompasses more than 7 million hospital stays annually, they examined close to 4 million weighted hospital admissions and found more than a 10-fold increase in MHD-HA-MUs, compared with a 1.4-fold increase in MHD-HAs.
MHD-HA-MUs increased significantly among men (13-fold), non-Hispanic Black patients (39-fold), and those aged 41-64 years (16-fold). In the southern United States, MHD-HA-MUs increased 24-fold, larger than in any other region in the United States.
“Overall, the data suggest that there are synergistic effects with methamphetamine use and mental health disorder, highlighting this patient group’s unique needs, requiring distinct action,” the researchers wrote.
They proposed several interventions, including public education about substance use disorders, mental illness, and the effects of stigma. They also suggested decreasing criminal penalties for those with substance use disorders and improving healthcare delivery for this patient population.
This work was supported by the National Institutes of Health and an award from the National Institute of General Medical Sciences. The study authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE MENTAL HEALTH
Giving Cash to Improve Health
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
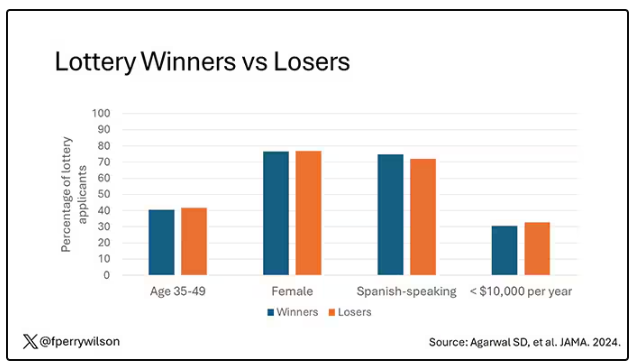
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
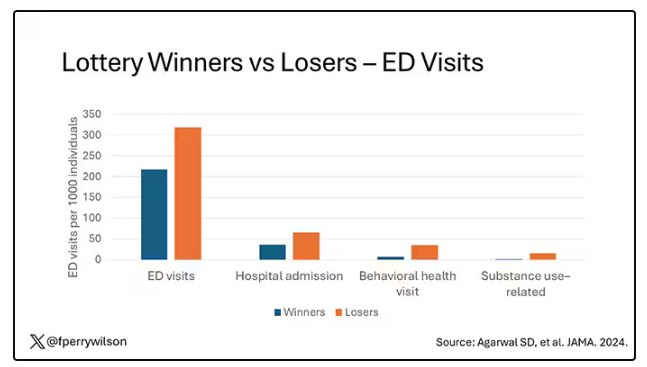
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
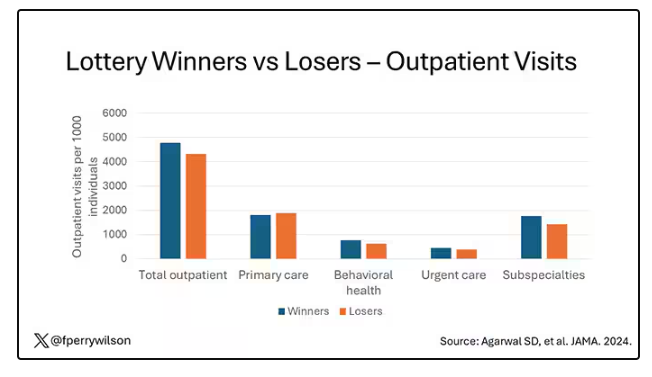
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
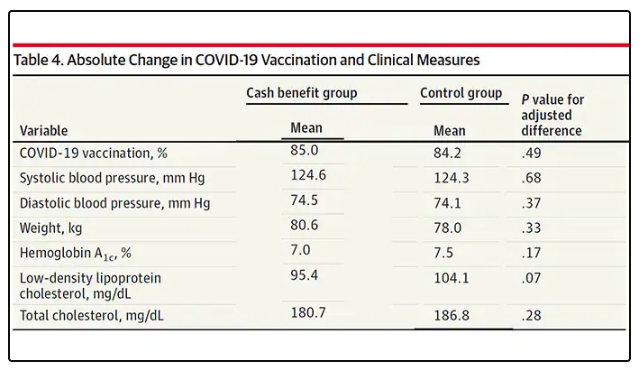
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Doctor on Death Row: Ahmad Reza Djalali Begins Hunger Strike
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Healthcare Workers Face Gender-Based Violence
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the world, healthcare workers experience workplace violence, which can differ by gender, seniority, and the type of workplace, according to a recent study.
An analysis found that men were more likely to report physical violence, while women were more likely to face nonphysical violence, such as verbal abuse, sexual harassment, and bullying.
“Our study was sparked by the increasing research on workplace violence in healthcare settings. Yet, there’s less empirical data about workplace violence based on gender, its effects on individuals and the collective workforce, and its subsequent impact on patient care and healthcare organizations,” study author Basnama Ayaz, a PhD candidate in nursing at the University of Toronto, told this news organization.
“Workplace violence in healthcare settings is a critical issue that requires attention and action from all stakeholders, including individual providers, healthcare and other institutions, policymakers, and the community,” she said. “By recognizing the problem and implementing evidence-based solutions, we can create safer work environments that protect healthcare workers and improve quality care for patients and organizational effectiveness.”
The study was published online in PLOS Global Public Health.
Widespread and Severe
Although women represent most of the healthcare workforce worldwide, hierarchical structures tend to reflect traditional gender norms, where men hold leadership positions and women serve in front-line care roles, said Ms. Ayaz. Women are often marginalized, and their concerns dismissed, which can exacerbate their vulnerability to gender-based workplace violence, she added.
To better understand these imbalances on a global scale, the investigators conducted a scoping review of the prevalence of and risk factors for gender-based workplace violence in healthcare settings. Participants included physicians, nurses, and midwives, between 2010 and 2024. Although the authors acknowledged that gender-based workplace violence affects the full gender spectrum, only a handful of studies included information about nonbinary personnel, so the review focused on men and women.
Among 226 studies, half focused on physicians, 22% focused on nurses, and 28% included physicians, nurses, midwives, and other medical workers. About 64% of studies reported a higher prevalence of all forms of workplace violence for women, including sexual violence, verbal abuse, discrimination, bullying, and physical violence, while 17% reported a higher prevalence for men.
Overall, across most countries, men experienced more physical violence than did women, and women experienced more verbal abuse, sexual harassment, and bullying. Female nurses were particularly likely to experience violence.
Healthcare workers were also more likely to experience violence if they were younger, less experienced, had a lower professional status, or were part of a minority group based on ethnicity, nationality, culture, or language. These factors were sensitive to gender, “reflecting women’s structural disadvantages in the workplace,” wrote the authors.
As a result of workplace violence, women were more likely to report changes in mental health and social behaviors, as well as dissatisfaction, burnout, and changes in their career goals.
The research team identified various factors linked to violent episodes. In clinical settings where most perpetrators were patients and their relatives, abuse and violence could be related to overcrowding, waiting time, and heavy workloads for healthcare providers. When supervisors or colleagues were the perpetrators, workplace violence appeared to be more likely with long hours, night shifts, and certain clinical settings, such as emergency departments, psychiatric settings, operating rooms, and maternity wards, said Ms. Ayaz. Sexual or gender harassment toward women was more prevalent in male-dominated surgical specialties.
“We were surprised by the extent and severity of workplace violence that healthcare workers face around the globe based on gender,” she said. “One aspect that stood out was the significant role that organizational culture and support systems play either in mitigating or exacerbating these incidents, particularly the power structures between and within professions.”
For instance, trainees in lower hierarchical positions often face a higher risk for violence, especially gender-based harassment, she said. Many times, they feel they can’t report these incidents to trainers or managers, who may also be the perpetrators, she added.
Addressing Systemic Issues
In 2002, the World Health Organization, International Council of Nurses, and other major medical and labor groups worldwide launched a program focused on ways to eliminate workplace violence in healthcare settings. Since 2020, the call for a solution has grown louder as clinicians, nurses, and other health professionals faced more physical and verbal violence during the COVID-19 pandemic, often leading to burnout.
“Workplace violence is very important because it is more prevalent in healthcare workers than in many other settings and is on the rise,” said Karen Abrams, MD, assistant professor of psychiatry at the University of Toronto. Dr. Abrams, who wasn’t involved with this study, has researched physicians’ experiences of stalking by patients.
Workplace violence “can affect physical and mental health and lead to burnout, depression, anxiety, and symptoms of PTSD,” said Dr. Abrams. “It can affect one’s sleep and concentration and, therefore, ability to perform one’s job.”
Dr. Ayaz and colleagues suggested recommendations to improve gender-based workplace violence, noting the complex and multifaceted aspects of enhancing current policies, fortifying institutional capacities to respond, and implementing tailored interventions. Changes are needed at various levels, including at the healthcare system and provincial, territorial, and national levels, she said.
In Canada, for instance, lawmakers passed a bill in 2021 that amended the national criminal code to make intimidation or bullying a healthcare worker punishable by as many as 10 years in prison. The changes also required courts to consider more serious penalties for offenders who target healthcare workers aggressively.
But more needs to be done, medical professional groups say. The Canadian Nurses Association and Canadian Federation of Nurses Unions, as well as provincial groups, have called for a pan-Canadian violence-prevention framework, targeted funding for violence prevention infrastructure, and an update to the nation’s health human resources strategy to address severe staffing shortages across the country.
“Canada needs a bold vision for the future of our healthcare. Amid an ongoing staffing crisis, the cracks in our public healthcare systems have only grown deeper and wider, with too many going without the care they need when they need it,” Linda Silas, president of the Canadian Federation of Nurses Unions, told this news organization.
“Access to care relies on safe staffing. Years of unsafe working conditions and insufficient staffing are pushing nurses out of our public healthcare system,” she said. “Working collaboratively, we can make healthcare jobs the best jobs in our communities.”
The authors received no specific funding for the study. Ms. Ayaz, Dr. Abrams, and Ms. Silas reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
US 911 System Is Nearing Its Own Emergency
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Just after lunchtime on June 18, Massachusetts’ leaders discovered that the statewide 911 system was down.
A scramble to handle the crisis was on.
Police texted out administrative numbers that callers could use, Boston Mayor Michelle Wu gave outage updates at a press conference outlining plans for the Celtics’ championship parade, and local officials urged people to summon help by pulling red fire alarm boxes.
About 7 million people went roughly 2 hours with no 911 service. Such crashes have become more of a feature than a bug in the nation’s fragmented emergency response system.
While some states, cities, and counties have already modernized their systems or have made plans to upgrade, many others are lagging.
911 is typically supported by fees tacked on to phone bills, but state and local governments also tap general funds or other resources.
“Now there are haves and have-nots,” said Jonathan Gilad, vice president of government affairs at the National Emergency Number Association (NENA), which represents 911 first responders. “Next-generation 911 shouldn’t be for people who happen to have an emergency in a good location.”
Meanwhile, federal legislation that could steer billions of dollars into modernizing the patchwork 911 system remains waylaid in Congress.
“This is a national security imperative,” said George Kelemen, executive director of the Industry Council for Emergency Response Technologies, a trade association that represents companies that provide hardware and software to the emergency response industry.
“In a crisis — a school shooting or a house fire or, God forbid, a terrorist attack — people call 911 first,” he said. “The system can’t go down.”
The United States debuted a single, universal 911 emergency number in February 1968 to simplify crisis response. But instead of a seamless national program, the 911 response network has evolved into a massive puzzle of many interlocking pieces. There are more than 6,000 911 call centers to handle an estimated 240 million emergency calls each year, according to federal data. More than three-quarters of call centers experienced outages in the prior 12 months, according to a survey in February by NENA, which sets standards and advocates for 911, and Carbyne, a provider of public safety technology solutions.
In April, widespread 911 outages affected millions in Nebraska, Nevada, South Dakota, and Texas. The shutdown was blamed on workers’ severing a fiber line while installing a light pole.
In February, tens of thousands of people in areas of California, Georgia, Illinois, Texas, and other states lost cellphone service, including some 911 services, from an outage.
And in June, Verizon agreed to pay a $1.05 million fine to settle a Federal Communications Commission (FCC) probe into a December 2022 outage that affected 911 calls in Alabama, Florida, Georgia, North Carolina, South Carolina, and Tennessee.
The fires that raced across the Hawaiian island of Maui in August 2023 highlighted the critical importance of 911 systems. Dispatchers there fielded more than 4,500 contacts, meaning calls and texts, on Aug. 8, the day the fires broke out, compared with about 400 on a typical day, said Davlynn Racadio, emergency services dispatch coordinator in Maui County.
“We’re dying out here,” one caller told 911 operators.
But some cell towers faltered because of widespread service outages, according to county officials. Maui County in May filed a lawsuit against four telecommunications companies, saying they failed to inform dispatchers about the outages.
“If 911 calls came in with no voice, we would send text messages,” Ms. Racadio said. “The state is looking at upgrading our system. Next-generation 911 would take us even further into the future.”
Florida, Illinois, Montana, and Oklahoma passed legislation in 2023 to advance or fund modernized 911 systems, according to the National Conference of State Legislatures. The upgrades include replacing analog 911 infrastructure with digital, Internet-based systems.
Instead of just fielding calls, next-generation systems can pinpoint a caller’s location, accept texts, and enable residents in a crisis to send videos and images to dispatchers. While outages can still occur, modernized systems often include more redundancy to minimize the odds of a shutdown, Mr. Gilad said.
Lawmakers have looked at modernizing 911 systems by tapping revenue the FCC gets from auctioning off the rights to transmit signals over specific bands of the electromagnetic spectrum.
But the U.S. Senate, in March 2023, for the first time allowed a lapse of the FCC’s authority to auction spectrum bands.
Legislation that would allocate almost $15 billion in grants from auction proceeds to speed deployment of next-generation 911 in every state unanimously passed the House Energy and Commerce Committee in May 2023. The bill, HR 3565, sponsored by Rep. Cathy McMorris Rodgers (R-Wash.), would also extend the FCC’s auction authority.
Other bills have been introduced by various lawmakers, including one in March from Sen. Ted Cruz (R-Texas) and legislation from Sen. Maria Cantwell (D-Wash.) to extend the auction authority. For now, neither effort has advanced. Nine former FCC chairs wrote lawmakers in February, urging them to make 911 upgrades a national priority. They suggested Congress tap unspent federal COVID-19 money.
“Whatever the funding source, the need is urgent and the time to act is now,” they wrote.
Ajit Pai, who served as chair of the FCC from 2017 to 2021, said outages often occur in older, legacy systems.
“The fact that the FCC doesn’t have authority to auction spectrum is a real hindrance now,” Mr. Pai said in an interview. “You may never need to call 911, but it can make the difference between life and death. We need more of an organized effort at the federal level because 911 is so decentralized.”
Meanwhile, some safety leaders are making backup plans for 911 outages or conducting investigations into their causes. In Massachusetts, a firewall designed to prevent hacking led to the recent 2-hour outage, according to the state 911 department.
“Outages bring to everyone’s attention that we rely on 911 and we don’t think about how we really rely on it until something happens,” said April Heinze, chief of 911 operations at NENA.
Mass General Brigham, a health system in the Boston area, sent out emergency alerts when the outage happened letting clinics and smaller practices know how to find their 10-digit emergency numbers. In the wake of the outage, it plans to keep the backup numbers next to phones at those facilities.
“Two hours can be a long time,” said Paul Biddinger, chief preparedness and continuity officer at the health system.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Primary Care Internal Medicine Is Dead
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.
Editor’s Note: This piece was originally published in Dr. Glasser’s bimonthly column in The Jolt, a nonprofit online news organization based in Olympia, Washington. She was inspired to write her story after meeting Christine Laine, MD, one of three female physician presenters at the Sommer Lectures in Portland, Oregon, in May 2024. The article has been edited lightly from the original.
Primary care internal medicine — the medical field I chose, loved, and practiced for four decades — is dead.
The grief and shock I feel about this is personal and transpersonal. The loss of internists (internal medicine physicians) practicing primary care is a major loss to us all.
From the 1970s to roughly 2020, there were three groups of primary care physicians: family practice, pediatricians, and internists. In their 3-year residencies (after 4 years of medical school), pediatricians trained to care for children and adolescents; internists for adults; and FPs for children, adults, and women and pregnancy. Family practitioners are the most general of the generalists, whereas the others’ training involves comprehensive care of complex patients in their age groups.
How and when the field of primary care internal medicine flourished is my story.
I was one of those kids who was hyperfocused on science, math, and the human body. By the end of high school, I was considering medicine for my career.
To learn more, I volunteered at the local hospital. In my typical style, I requested not to be one of those candy stripers serving drinks on the wards. Instead, they put me in the emergency department, where I would transport patients and clean the stretchers. There I was free to watch whatever was going on if I did not interfere with the staff. On my first shift, a 20-year-old drowning victim arrived by ambulance. I watched the entire unsuccessful resuscitation and as shocked and saddened as I was, I knew (in the way only a headstrong 18-year-old can) that medicine was for me.
It was a fortuitous time to graduate as a female pre-med student.
In 1975, our country was in the midst of the women’s movement and a national effort to train primary care physicians. I was accepted to my state medical school. The University of Massachusetts Medical School had been established a few years earlier, with its main purpose to train primary care physicians and spread them around the state (especially out of the Boston metropolitan area). The curriculum was designed to expose students to primary care from year one. I was assigned to shadow a general practice physician in inner-city Springfield who saw over 50 patients a day! The patients knew they could see and afford him, so they crammed into his waiting room until their name was called in order of their arrival. No appointments necessary. His chart notes were a few scribbled sentences. I didn’t see myself in that practice exactly, but his work ethic and dedication inspired me.
Over half of our graduating class chose to train in primary care specialties, and most stayed in-state. It turned out to be a good bet on the part of the government of Massachusetts.
When I applied for residency in 1980, several internal medicine programs had a focus on primary care, which was my goal. I matched at Providence St. Vincent Hospital in Portland, Oregon, and moved across the country to the Pacific Northwest, never to look back. There, my attendings were doctors like I wanted to be: primary care internists in the community, not in academia. It was the perfect choice and an excellent training program.
In 1984, I hung out my private practice internal medicine shingle in Hillsboro, Oregon, across the street from the community hospital. My primary care internal medicine colleagues and I shared weekend calls and admitted and cared for our patients in the hospital, and when they were discharged. That is now called “continuity of care.” It was a time when we ate in the doctors’ lounge together, met in hallways, and informally consulted each other about our patients. These were called “curbside consults.” They were invaluable to our ability to provide comprehensive care to our patients in primary care, led to fewer specialty referrals, and were free. That would now be called interprofessional communication and collegiality.
“Burnout” was not a word you heard. We were busy and happy doing what we had spent 12 years of our precious youth to prepare for.
What did internists offer to primary care? That also is part of my story.
When I moved to Olympia, I took a position in the women’s health clinic at the American Lake Veterans Administration Medical Center.
We were a small group: two family practice doctors, three nurse practitioners, and me, the only internist. Many of our patients were sick and complex. Two of the nurse practitioners (NPs) asked me to take their most complicated patients. Being comfortable with complexity as an internist, I said yes.
One of the NPs was inappropriately hired, as she had experience in women’s health. She came to me freaked out: “Oh my God, I have no idea how to manage COPD!” The other wanted simpler patients. I don’t blame them for the patient transfers. NPs typically have 3 years of training before they practice, in contrast to primary care physicians’ 8.
Guess who made friends with the custodian, staying until 8 p.m. most evenings, and who left by 5:30 p.m.
What was I doing in those extra hours? I was trudging through clerical, yet important, tasks my medical assistant and transcriptionist used to do in private practice. In the 30 minutes allotted for the patient, I needed to focus entirely on them and their multiple complex medical problems.
What is lost with the death of primary care internal medicine?
At the recent Sommer Memorial Lectures in Portland, Steven D. Freer, MD, the current director of the residency program where I trained, has not had a single of his eight annual internal medicine graduates choose primary care in several years. Half (two of four) of those in my year did: One went to Tillamook, an underserved area on the Oregon coast, and I to Hillsboro.
Why are they not choosing primary care? As when the University of Massachusetts Medical School was established, a shortage of primary care physicians persists and probably is more severe than it was in the 1970s. Massachusetts was proactive. We are already years behind catching up. The shortage is no longer in rural areas alone.
Christine Laine, MD, who is editor in chief of Annals of Internal Medicine and spoke at the Sommer Memorial Lectures, lives in Philadelphia. Even there, she has lost her own primary care internal medicine physician and cannot find another primary care physician (much less an internist) for herself.
Washington State, where I live, scores a D grade for our primary care staffing statewide.
Is there hope for the future of primary care in general? Or for the restoration of primary care internal medicine?
Maybe. I was relieved to hear from Dr. Freer and Dr. Laine that efforts are beginning to revive the field.
Just like internists’ patients, the potential restoration of the field will be complex and multilayered. It will require new laws, policies, residency programs, and incentives for students, including debt reduction. Administrative burdens will need to be reduced; de-corporatization and restoring healthcare leadership to those with in-depth medical training will need to be a part of the solution as well.
Let’s all hope the new resuscitation efforts will be successful for the field of primary care in general and primary care internal medicine specifically. It will be good for healthcare and for your patients!
Many work for large systems in which they feel powerless to effect change.
Dr. Glasser is a retired internal medicine physician in Olympia, Washington. She can be reached at drdebra@theJOLTnews.com.
A version of this article appeared on Medscape.com.