User login
Catheterized urine color change
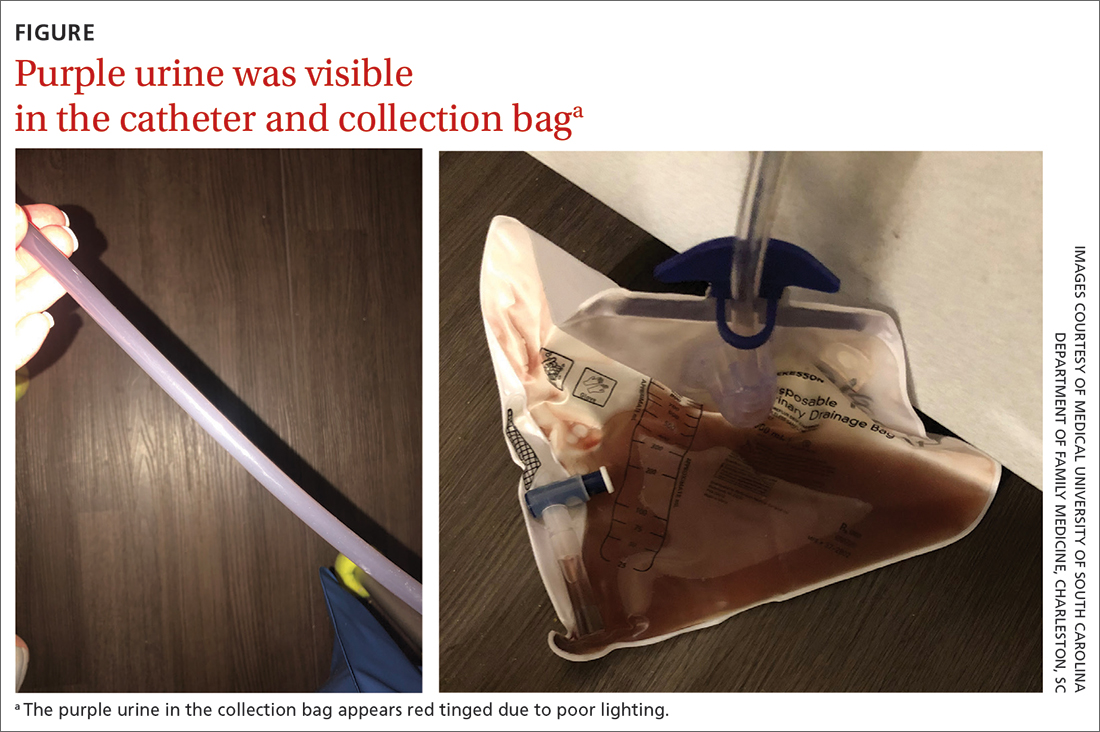
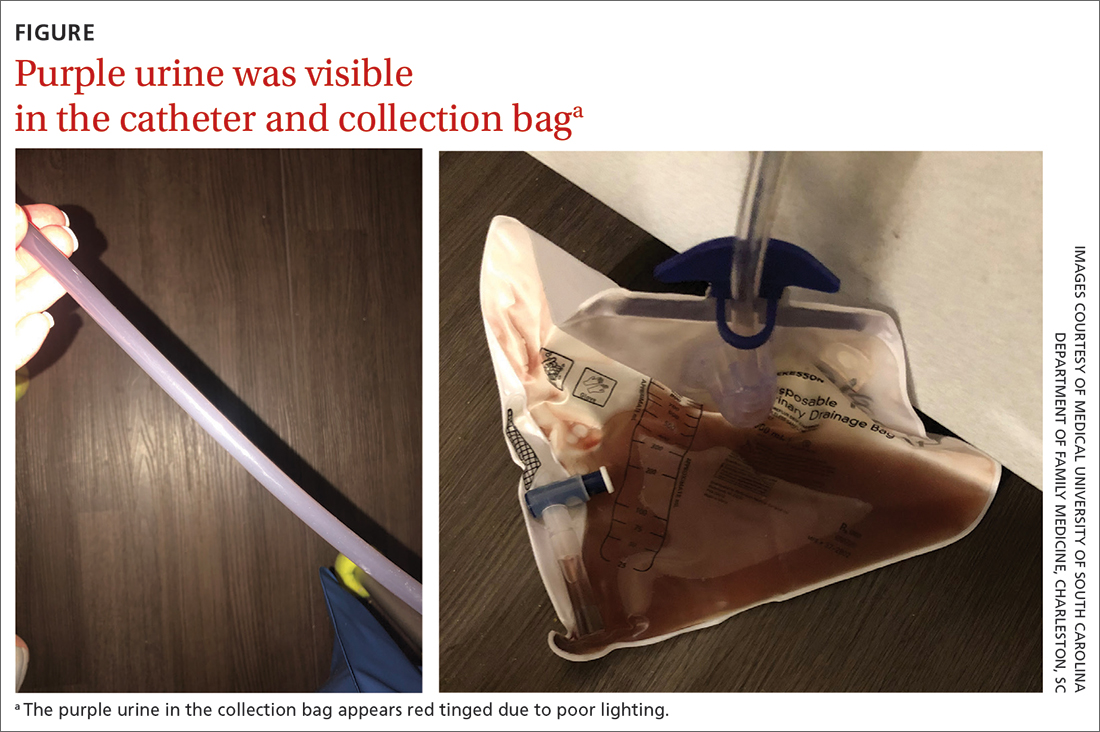
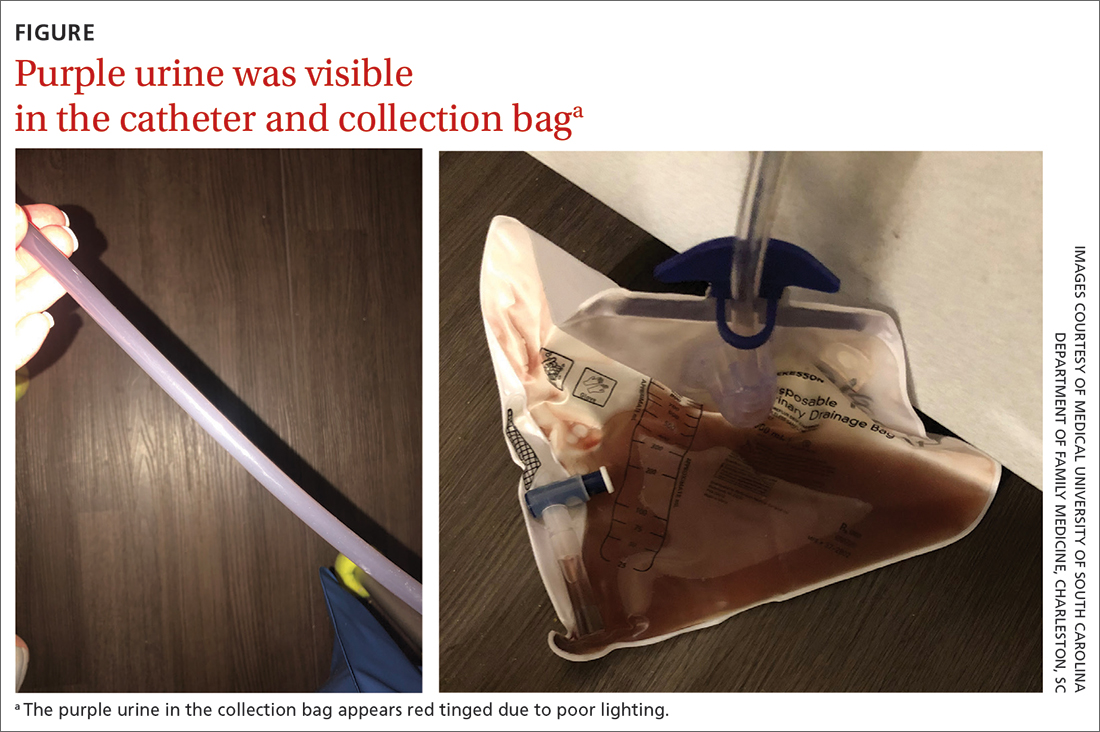
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Purple urine bag syndrome
The diagnosis of purple urine bag syndrome (PUBS) was made based on the patient’s clinical presentation and medical history. PUBS is generally a benign condition that can occur in patients who have urinary catheters for prolonged periods of time and urinary tract infections (UTIs), often with constipation.1
PUBS was first described in the literature in 1978.2 Its prevalence has been estimated to be 9.8% in long-term wards and higher in patients with chronic catheters.3-5 PUBS is reported more often in institutionalized older women, although it has been documented in men as well.1 Risk factors include having a chronic indwelling urinary catheter; alkaline urine; the use of plastic, polyvinylchloride urine bags3; chronic constipation6; renal failure4,5; and dementia.1 In many cases, patients with PUBS have been found to have stable vitals and lack systemic symptoms, such as fever, that could indicate an infection.1,5
The pathogenesis of PUBS has been associated with tryptophan.3 Gut bacteria metabolize tryptophan to indole, which is converted to indoxyl sulfate in the liver.3,7 Then certain bacteria associated with UTIs, including Pseudomonas, Escherichia coli, Proteus mirabilis, Providencia spp, Enterococcus faecalis, and Klebsiella,5-7 which contain indoxyl phosphatase and sulfatase enzymes, can convert indoxyl sulfate into indirubin (red) and indigo (blue) compounds; this results in a purple hue in the urine seen in a Foley catheter and bag.
Differential is generally limited to medication and food consumption
Clinical presentation and a detailed history and review of medication and/or food ingestion may distinguish PUBS from other conditions.
Medications and foods, such as rifampicin or beets, may discolor urine and need to be ruled out as a cause with a thorough history.3
Cyanide toxicity in those taking vitamin B12can result in purple-tinged urine.8 Signs and symptoms can alsoinclude reddening of the skin, dyspnea, nausea, headache, erythema at the injection site, and a modest increase in blood pressure.8
Identify the infection and treat as needed
There have been some case reports regarding the progression of PUBS to Fournier gangrene,4 but such cases are rare and associated with immunocompromised patients.9 PUBS is generally a benign condition associated with UTIs. Management involves identifying the underlying infection, treating with antibiotics if indicated (ie, patient is symptomatic or immunocompromised),3 providing proper treatment of constipation if needed, and replacing the Foley catheter.4 Some studies suggest that simply exchanging the catheter may resolve PUBS, particularly in asymptomatic patients.5
In light of his complicated urologic history, our patient was treated with a 10-day course of renally dosed intravenous cefepime (500 mg every 24 hours based on calculated creatine clearance of 21 mL/min) and Foley exchange. The patient’s urine color returned to normal after Foley exchange and 24 hours of antibiotics. His kidney function continued to improve and normalized by the time he was discharged from the facility approximately 2 weeks later.
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
1. Goyal A, Vikas G, Jindal J. Purple urine bag syndrome: series of nine cases and review of literature. J Clin Diagn Res. 2018;12:PR01-PR03. doi: 10.7860/JCDR/2018/34951.12202
2. Barlow GB, Dickson JAS. Purple urine bags. Lancet. 1978;28:220-221. doi: 10.1016/S0140-6736(78)90667-0
3. Richardson-May J. Single case of purple urine bag syndrome in an elderly woman with stroke. BMJ Case Rep. 2016;2016:bcr2016215465. doi: 10.1136/bcr-2016-215465
4. Khan F, Chaudhry MA, Qureshi N, et al. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi: 10.4061/2011/419213
5. Ben-Chetrit E, Munter G. Purple urine. JAMA. 2012;307:193-194. doi: 10.1001/jama.2011.1997
6. Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2:104-105. doi: 10.4103/2249-4863.109970
7. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152-2156. doi: 10.1128/jcm.26.10.2152-2156.1988
8. Hudson M, Cashin BV, Matlock AG, et al. A man with purple urine. Hydroxocobalamin-induced chromaturia. Clin Toxicol (Phila). 2012;50:77. doi: 10.3109/15563650.2011.626782
9. Tasi Y-M, Huang M-S, Yang C-J, et al. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27:895-897. doi: 10.1016/j.ajem.2009.01.030
