User login
Did Statin Decision-Making Just Get Harder?
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
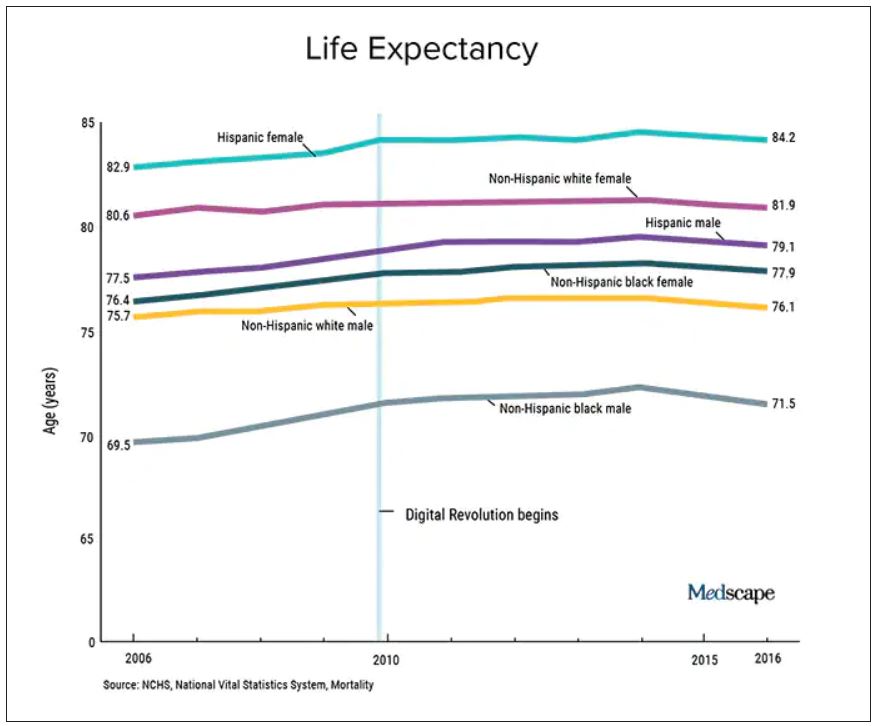
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The new American Heart Association Predicting Risk of cardiovascular disease EVENTs (PREVENT) equation outperforms the standard pooled cohort equation (PCE). But there is a problem. A big one, actually.
The new score incorporates kidney function and social situation, and it eliminates race from the estimate. It was derived from larger, more modern datasets and can be applied to younger adults.
Two luminaries in preventive cardiology recently called the PREVENT calculator a “substantial improvement over the PCE in terms of accuracy and precision of risk estimates over the entire population and within demographic subgroups.”
Now to the Problem of PREVENT vs PCE
A recent study comparing PREVENT and PCE found that the PREVENT equation would assign lower 10-year risks to millions of US adults.
The authors estimated that the more accurate calculator would result in an estimated 14 million adults no longer reaching the statin eligibility risk threshold of 7.5% over 10 years. Nearly 3 million adults would also not reach the threshold for blood pressure therapy.
Because statins and blood pressure drugs reduce cardiac events, the authors further estimated that more than 100,000 excess myocardial infarctions (MIs) would occur if the PREVENT equation was used along with the current risk thresholds for statin eligibility.
The change in eligibility induced by PREVENT would affect more men than women and a greater proportion of Black adults than White adults.
The Tension of Arbitrary Thresholds
Modern cardiac therapeutics are amazing, but it’s still better to prevent an event than to treat it.
Statin drugs reduce cardiac risk by about 20%-25% at all absolute risks. American experts chose a 10-year risk of 7.5% as the threshold where statin benefit exceed risk. The USPSTF chose 10%. But the thresholds are arbitrary and derived only by opinion.
If your frame is population health, the more patients who take statins, the fewer cardiac events there will be. Anything that reduces statin use increases cardiac events.
The tension occurs because a more accurate equation decreases the number of people who meet eligibility for primary prevention therapy and therefore increases the number of cardiac events.
I write from the perspective of both a clinician and a possible patient. As a clinician, patients often ask me whether they should take a statin. (Sadly, most have not had a risk-based discussion with their clinician. But that is another column.)
The incidence of MI or stroke in a population has no effect on either of these scenarios. I see three broad categories of patients: minimizers, maximizers, and those in between.
I am a minimizer. I don’t worry much about heart disease. First, I won’t ignore symptoms, and I know that we have great treatments. Second, my wife, Staci, practiced hospice and palliative care medicine, and this taught me that worrying about one specific disease is folly. In the next decade, I, like anyone my age, could have many other bad things happen: cancer, trauma, infection, etc. Given these competing risks for serious disease, a PREVENT-calculated risk of 4% or a PCE-calculated risk of 8% makes no difference. I don’t like pills, and, with risks in this range, I decline statin drugs.
Then there are the maximizers. This person wants to avoid heart disease. Maybe they have family or friends who had terrible cardiac events. This person will maximize everything to avoid heart disease. The calculated 10-year risk makes little difference to a maximizer. Whether it is 4% or 8% matters not. They will take a statin or blood pressure drugs to reduce risk to as low as possible.
There are people between minimizers and maximizers. I am not sure that there are that many truly undecided people, but I challenge you to translate a difference of a few percent over a decade to them. I feel comfortable with numbers but struggle to sort out these small absolute differences over such a long time frame.
Other Issues With Risk-Based Decisions
Venk Murthy, MD, PhD, from the University of Michigan, wrote on X about two other issues with a risk-based decision. One is that it does not consider life-years lost. If a 50-year-old person has a fatal MI, that counts as one event. But in life-years lost, that one event is much worse than a fatal MI in a 79-year-old. Cardiac prevention, therefore, may have a greater effect in lower-risk younger people.
Another point Dr. Murthy made is that risk and benefit are driven by many different preferences and rare events. Minimizers and maximizers come to the decision with widely disparate preferences. Risk-based decisions treat patients as if they were automatons who make decisions based simply on calculated probabilities. Clinicians know how untrue that is.
Conclusion
If you carry forward the logic of being disturbed by the estimate of more MIs using the PREVENT score, then you could justify putting statins in the water — because that would reduce population estimates of MIs.
I am not disturbed by the PREVENT score. Clinicians treat individuals, not populations. Individuals want a more accurate score. They don’t need expert-based thresholds. Clinician and patient can discuss the evidence and come up with an agreeable decision, one that is concordant with a person’s goals. The next patient may have a different decision despite seeing the same evidence.
The tension created by this comparative study exposes the gap between population health and basic clinical care. I don’t think clinicians need to worry about populations.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Pulsed Field Ablation for AF: Are US Electrophysiologists Too Easily Impressed?
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
It dominated 2024’s heart rhythm meetings, and it dominates my private electrophysiologist chat groups. My Google alert for “AF ablation” most often includes notices on PFA and the expansion of the atrial fibrillation ablation market.
Yet, the excitement does not match the empirical data.
Despite having strong brains, electrophysiologists adopt new things as if we were emotional shoppers. Our neighbor buys a sports car and we think we need the same car. Left atrial appendage occlusion and subcutaneous defibrillators were past examples.
The most recent example of soft thinking (especially in the United States) is the enthusiasm and early adoption of first-generation PFA systems for the treatment of AF.
Readers of cardiac news (including some of my patients) might think PFA has solved the AF puzzle. It has not.
A true breakthrough in AF would be to find its cause. PFA is simply another way to destroy (ablate) cardiac myocytes. PFA uses electrical energy (think shocks) to create pores in the cell membranes of myocytes. It’s delivered through various types of catheters.
The main theoretical advantage of PFA is cardioselectivity, which is possible because myocytes have lower thresholds for irreversible electroporation than surrounding tissues. The dose of electrical energy that ablates cardiac tissue does not affect surrounding tissues. Cardioselectivity decreases the chance of the most feared complication of standard AF ablation, thermal damage to the esophagus, which is often fatal. The esophagus lies immediately behind the posterior wall of the left atrium and can be inadvertently injured during thermal ablation.
The challenge in assessing this potential advantage is that thermal esophageal damage is, thankfully, exceedingly rare. Its incidence is in the range of 1 in 10,000 AF ablations. But it might be even lower than that in contemporary practice, because knowledge of esophageal injury has led to innovations that probably have reduced its incidence even further.
Proponents of PFA would rightly point to the fact that not having to worry about esophageal injury allows operators to add posterior wall ablation to the normal pulmonary vein isolation lesion set. This ability, they would argue, is likely to improve AF ablation outcomes. The problem is that the strongest and most recent trial of posterior wall isolation (with radiofrequency ablation) did not show better outcomes. A more recent observational analysis also showed no benefit to posterior wall isolation (using PFA) over pulmonary vein isolation alone.
What About PFA Efficacy?
I’ve long spoken and written about the lack of progress in AF ablation. In 1998, the first report on ablation of AF showed a 62% arrhythmia-free rate. Two decades later, in the carefully chosen labs treating patients in the CABANA trial, arrhythmia-free rates after AF ablation remain unchanged. We have improved our speed and ability to isolate pulmonary veins, but this has not increased our success in eliminating AF. The reason, I believe, is that we have made little to no progress in understanding the pathophysiology of AF.
The Food and Drug Administration regulatory trial called ADVENT randomly assigned more than 600 patients to thermal ablation or PFA, and the primary endpoint of ablation success was nearly identical. Single-center studies, observational registries, and single-arm studies have all shown similar efficacy of PFA and thermal ablation.
Proponents of PFA might argue that these early studies used first-generation PFA systems, and iteration will lead to better efficacy. Perhaps, but we’ve had 20 years of iteration of thermal ablation, and its efficacy has not budged.
What About PFA Safety?
In the ADVENT randomized trial, safety results were similar, though the one death, caused by cardiac perforation and tamponade, occurred in the PFA arm. In the MANIFEST-17K multinational survey of PFA ablation, safety events were in the range reported with thermal ablation. PFA still involves placing catheters in the heart, and complications such as tamponade, stroke, and vascular damage occur.
The large MANIFEST-17K survey also exposed two PFA-specific complications: coronary artery spasm, which can occur when PFA is delivered close to coronary arteries; and hemolysis-related kidney failure — severe enough to require dialysis in five patients. Supporters of PFA speculate that hemolysis occurs because electrical energy within the atrium can shred red blood cells. Their solution is to strive for good contact and use hydration. The irony of this latter fix is that one of the best advances in thermal ablation has been catheters that deliver less fluid and less need for diuresis after the procedure.
No PFA study has shown a decreased incidence of thermal damage to the esophagus with PFA ablation. Of course, this is because it is such a low-incidence event.
One of my concerns with PFA is brain safety. PFA creates substantial microbubbles in the left atrium, which can then travel north to the brain. In a small series from ADVENT, three patients had brain lesions after PFA vs none with thermal ablation. PFA proponents wrote that brain safety was important to study, but few patients have been systematically studied with brain MRI scans. Asymptomatic brain lesions have been noted after many arterial procedures. The clinical significance of these is not known. As a new technology, and one that creates substantial microbubbles in the left atrium, I agree with the PFA proponents that brain safety should be thoroughly studied — before widespread adoption.
What About Speed and Cost?
Observational studies from European labs report fast procedure times. I have seen PFA procedures in Europe; they’re fast — typically under an hour. A standard thermal ablation takes me about 60-70 minutes.
I am not sure that US operators can duplicate European procedural times. In the ADVENT regulatory trial, the mean procedure time was 105 minutes and that was in experienced US centers. While this still represents early experience with PFA, the culture of US AF ablation entails far more mapping and extra catheters than I have seen used in European labs.
Cost is a major issue. It’s hard to sort out exact costs in the United States, but a PFA catheter costs approximately threefold more than a standard ablation catheter. A recent study from Liverpool, England, found that PFA ablation was faster but more expensive than standard thermal ablation because of higher PFA equipment prices. For better or worse, US patients are not directly affected by the higher procedural costs. But the fact remains that PFA adds more costs to the healthcare system.
What Drives the Enthusiasm for First-Generation PFA?
So why all the enthusiasm? It’s surely not the empirical data. Evidence thus far shows no obvious advantage in safety or efficacy. European use of PFA does seem to reduce procedure time. But in many electrophysiology labs in the United States, the rate-limiting step for AF ablation is not time in the lab but having enough staff to turn rooms around.
The main factor driving early acceptance of PFA relates to basic human nature. It is the fear of missing out. Marketing works on consumers, and it surely works on doctors. Companies that make PFA systems sponsor key opinion leaders to discuss PFA. These companies have beautiful booths in the expo of our meetings; they host dinners and talks. When a hospital in a city does PFA, the other hospitals feel the urge to keep up. It’s hard to be a Top Person in electrophysiology and not be a PFA user.
One of my favorite comments came from a key opinion leader. He told me that he advised his administration to buy a PFA system, promote that they have it, and keep it in the closet until better systems are released.
Iteration in the medical device field is tricky. There are negatives to being too harsh on first-generation systems. Early cardiac resynchronization tools, for instance, were horrible. Now CRT is transformative in selected patients with heart failure.
It’s possible (but not certain) that electrical ablative therapy will iterate and surpass thermal ablation in the future. Maybe.
But for now, the enthusiasm for PFA far outstrips its evidence. Until better evidence emerges, I will be a slow adopter. And I hope that our field gathers evidence before widespread adoption makes it impossible to do proper studies.
Dr. Mandrola, clinical electrophysiologist, Baptist Medical Associates, Louisville, Kentucky, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Is Red Meat Healthy? Multiverse Analysis Has Lessons Beyond Meat
Observational studies on red meat consumption and lifespan are prime examples of attempts to find signal in a sea of noise.
Randomized controlled trials are the best way to sort cause from mere correlation. But these are not possible in most matters of food consumption. So, we look back and observe groups with different exposures.
My most frequent complaint about these nonrandom comparison studies has been the chance that the two groups differ in important ways, and it’s these differences — not the food in question — that account for the disparate outcomes.
But selection biases are only one issue. There is also the matter of analytic flexibility. Observational studies are born from large databases. Researchers have many choices in how to analyze all these data.
A few years ago, Brian Nosek, PhD, and colleagues elegantly showed that analytic choices can affect results. His Many Analysts, One Data Set study had little uptake in the medical community, perhaps because he studied a social science question.
Multiple Ways to Slice the Data
Recently, a group from McMaster University, led by Dena Zeraatkar, PhD, has confirmed the analytic choices problem, using the question of red meat consumption and mortality.
Their idea was simple: Because there are many plausible and defensible ways to analyze a dataset, we should not choose one method; rather, we should choose thousands, combine the results, and see where the truth lies.
You might wonder how there could be thousands of ways to analyze a dataset. I surely did.
The answer stems from the choices that researchers face. For instance, there is the selection of eligible participants, the choice of analytic model (logistic, Poisson, etc.), and covariates for which to adjust. Think exponents when combining possible choices.
Dr. Zeraatkar and colleagues are research methodologists, so, sadly, they are comfortable with the clunky name of this approach: specification curve analysis. Don’t be deterred. It means that they analyze the data in thousands of ways using computers. Each way is a specification. In the end, the specifications give rise to a curve of hazard ratios for red meat and mortality. Another name for this approach is multiverse analysis.
For their paper in the Journal of Clinical Epidemiology, aptly named “Grilling the Data,” they didn’t just conjure up the many analytic ways to study the red meat–mortality question. Instead, they used a published systematic review of 15 studies on unprocessed red meat and early mortality. The studies included in this review reported 70 unique ways to analyze the association.
Is Red Meat Good or Bad?
Their first finding was that this analysis yielded widely disparate effect estimates, from 0.63 (reduced risk for early death) to 2.31 (a higher risk). The median hazard ratio was 1.14 with an interquartile range (IQR) of 1.02-1.23. One might conclude from this that eating red meat is associated with a slightly higher risk for early mortality.
Their second step was to calculate how many ways (specifications) there were to analyze the data by totaling all possible combinations of choices in the 70 ways found in the systematic review.
They calculated a total of 10 quadrillion possible unique analyses. A quadrillion is 1 with 15 zeros. Computing power cannot handle that amount of analyses yet. So, they generated 20 random unique combinations of covariates, which narrowed the number of analyses to about 1400. About 200 of these were excluded due to implausibly wide confidence intervals.
Voilà. They now had about 1200 different ways to analyze a dataset; they chose an NHANES longitudinal cohort study from 2007-2014. They deemed each of the more than 1200 approaches plausible because they were derived from peer-reviewed papers written by experts in epidemiology.
Specification Curve Analyses Results
Each analysis (or specification) yielded a hazard ratio for red meat exposure and death.
- The median HR was 0.94 (IQR, 0.83-1.05) for the effect of red meat on all-cause mortality — ie, not significant.
- The range of hazard ratios was large. They went from 0.51 — a 49% reduced risk for early mortality — to 1.75: a 75% increase in early mortality.
- Among all analyses, 36% yielded hazard ratios above 1.0 and 64% less than 1.0.
- As for statistical significance, defined as P ≤.05, only 4% (or 48 specifications) met this threshold. Zeraatkar reminded me that this is what you’d expect if unprocessed red meat has no effect on longevity.
- Of the 48 analyses deemed statistically significant, 40 indicated that red meat consumption reduced early death and eight indicated that eating red meat led to higher mortality.
- Nearly half the analyses yielded unexciting point estimates, with hazard ratios between 0.90 and 1.10.
Paradigm Changing
As a user of evidence, I find this a potentially paradigm-changing study. Observational studies far outnumber randomized trials. For many medical questions, observational data are all we have.
Now think about every observational study published. The authors tell you — post hoc — which method they used to analyze the data. The key point is that it is one method.
Dr. Zeraatkar and colleagues have shown that there are thousands of plausible ways to analyze the data, and this can lead to very different findings. In the specific question of red meat and mortality, their many analyses yielded a null result.
Now imagine other cases where the researchers did many analyses of a dataset and chose to publish only the significant ones. Observational studies are rarely preregistered, so a reader cannot know how a result would vary depending on analytic choices. A specification curve analysis of a dataset provides a much broader picture. In the case of red meat, you see some significant results, but the vast majority hover around null.
What about the difficulty in analyzing a dataset 1000 different ways? Dr. Zeraatkar told me that it is harder than just choosing one method, but it’s not impossible.
The main barrier to adopting this multiverse approach to data, she noted, was not the extra work but the entrenched belief among researchers that there is a best way to analyze data.
I hope you read this paper and think about it every time you read an observational study that finds a positive or negative association between two things. Ask: What if the researchers were as careful as Dr. Zeraatkar and colleagues and did multiple different analyses? Would the finding hold up to a series of plausible analytic choices?
Nutritional epidemiology would benefit greatly from this approach. But so would any observational study of an exposure and outcome. I suspect that the number of “positive” associations would diminish. And that would not be a bad thing.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Observational studies on red meat consumption and lifespan are prime examples of attempts to find signal in a sea of noise.
Randomized controlled trials are the best way to sort cause from mere correlation. But these are not possible in most matters of food consumption. So, we look back and observe groups with different exposures.
My most frequent complaint about these nonrandom comparison studies has been the chance that the two groups differ in important ways, and it’s these differences — not the food in question — that account for the disparate outcomes.
But selection biases are only one issue. There is also the matter of analytic flexibility. Observational studies are born from large databases. Researchers have many choices in how to analyze all these data.
A few years ago, Brian Nosek, PhD, and colleagues elegantly showed that analytic choices can affect results. His Many Analysts, One Data Set study had little uptake in the medical community, perhaps because he studied a social science question.
Multiple Ways to Slice the Data
Recently, a group from McMaster University, led by Dena Zeraatkar, PhD, has confirmed the analytic choices problem, using the question of red meat consumption and mortality.
Their idea was simple: Because there are many plausible and defensible ways to analyze a dataset, we should not choose one method; rather, we should choose thousands, combine the results, and see where the truth lies.
You might wonder how there could be thousands of ways to analyze a dataset. I surely did.
The answer stems from the choices that researchers face. For instance, there is the selection of eligible participants, the choice of analytic model (logistic, Poisson, etc.), and covariates for which to adjust. Think exponents when combining possible choices.
Dr. Zeraatkar and colleagues are research methodologists, so, sadly, they are comfortable with the clunky name of this approach: specification curve analysis. Don’t be deterred. It means that they analyze the data in thousands of ways using computers. Each way is a specification. In the end, the specifications give rise to a curve of hazard ratios for red meat and mortality. Another name for this approach is multiverse analysis.
For their paper in the Journal of Clinical Epidemiology, aptly named “Grilling the Data,” they didn’t just conjure up the many analytic ways to study the red meat–mortality question. Instead, they used a published systematic review of 15 studies on unprocessed red meat and early mortality. The studies included in this review reported 70 unique ways to analyze the association.
Is Red Meat Good or Bad?
Their first finding was that this analysis yielded widely disparate effect estimates, from 0.63 (reduced risk for early death) to 2.31 (a higher risk). The median hazard ratio was 1.14 with an interquartile range (IQR) of 1.02-1.23. One might conclude from this that eating red meat is associated with a slightly higher risk for early mortality.
Their second step was to calculate how many ways (specifications) there were to analyze the data by totaling all possible combinations of choices in the 70 ways found in the systematic review.
They calculated a total of 10 quadrillion possible unique analyses. A quadrillion is 1 with 15 zeros. Computing power cannot handle that amount of analyses yet. So, they generated 20 random unique combinations of covariates, which narrowed the number of analyses to about 1400. About 200 of these were excluded due to implausibly wide confidence intervals.
Voilà. They now had about 1200 different ways to analyze a dataset; they chose an NHANES longitudinal cohort study from 2007-2014. They deemed each of the more than 1200 approaches plausible because they were derived from peer-reviewed papers written by experts in epidemiology.
Specification Curve Analyses Results
Each analysis (or specification) yielded a hazard ratio for red meat exposure and death.
- The median HR was 0.94 (IQR, 0.83-1.05) for the effect of red meat on all-cause mortality — ie, not significant.
- The range of hazard ratios was large. They went from 0.51 — a 49% reduced risk for early mortality — to 1.75: a 75% increase in early mortality.
- Among all analyses, 36% yielded hazard ratios above 1.0 and 64% less than 1.0.
- As for statistical significance, defined as P ≤.05, only 4% (or 48 specifications) met this threshold. Zeraatkar reminded me that this is what you’d expect if unprocessed red meat has no effect on longevity.
- Of the 48 analyses deemed statistically significant, 40 indicated that red meat consumption reduced early death and eight indicated that eating red meat led to higher mortality.
- Nearly half the analyses yielded unexciting point estimates, with hazard ratios between 0.90 and 1.10.
Paradigm Changing
As a user of evidence, I find this a potentially paradigm-changing study. Observational studies far outnumber randomized trials. For many medical questions, observational data are all we have.
Now think about every observational study published. The authors tell you — post hoc — which method they used to analyze the data. The key point is that it is one method.
Dr. Zeraatkar and colleagues have shown that there are thousands of plausible ways to analyze the data, and this can lead to very different findings. In the specific question of red meat and mortality, their many analyses yielded a null result.
Now imagine other cases where the researchers did many analyses of a dataset and chose to publish only the significant ones. Observational studies are rarely preregistered, so a reader cannot know how a result would vary depending on analytic choices. A specification curve analysis of a dataset provides a much broader picture. In the case of red meat, you see some significant results, but the vast majority hover around null.
What about the difficulty in analyzing a dataset 1000 different ways? Dr. Zeraatkar told me that it is harder than just choosing one method, but it’s not impossible.
The main barrier to adopting this multiverse approach to data, she noted, was not the extra work but the entrenched belief among researchers that there is a best way to analyze data.
I hope you read this paper and think about it every time you read an observational study that finds a positive or negative association between two things. Ask: What if the researchers were as careful as Dr. Zeraatkar and colleagues and did multiple different analyses? Would the finding hold up to a series of plausible analytic choices?
Nutritional epidemiology would benefit greatly from this approach. But so would any observational study of an exposure and outcome. I suspect that the number of “positive” associations would diminish. And that would not be a bad thing.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Observational studies on red meat consumption and lifespan are prime examples of attempts to find signal in a sea of noise.
Randomized controlled trials are the best way to sort cause from mere correlation. But these are not possible in most matters of food consumption. So, we look back and observe groups with different exposures.
My most frequent complaint about these nonrandom comparison studies has been the chance that the two groups differ in important ways, and it’s these differences — not the food in question — that account for the disparate outcomes.
But selection biases are only one issue. There is also the matter of analytic flexibility. Observational studies are born from large databases. Researchers have many choices in how to analyze all these data.
A few years ago, Brian Nosek, PhD, and colleagues elegantly showed that analytic choices can affect results. His Many Analysts, One Data Set study had little uptake in the medical community, perhaps because he studied a social science question.
Multiple Ways to Slice the Data
Recently, a group from McMaster University, led by Dena Zeraatkar, PhD, has confirmed the analytic choices problem, using the question of red meat consumption and mortality.
Their idea was simple: Because there are many plausible and defensible ways to analyze a dataset, we should not choose one method; rather, we should choose thousands, combine the results, and see where the truth lies.
You might wonder how there could be thousands of ways to analyze a dataset. I surely did.
The answer stems from the choices that researchers face. For instance, there is the selection of eligible participants, the choice of analytic model (logistic, Poisson, etc.), and covariates for which to adjust. Think exponents when combining possible choices.
Dr. Zeraatkar and colleagues are research methodologists, so, sadly, they are comfortable with the clunky name of this approach: specification curve analysis. Don’t be deterred. It means that they analyze the data in thousands of ways using computers. Each way is a specification. In the end, the specifications give rise to a curve of hazard ratios for red meat and mortality. Another name for this approach is multiverse analysis.
For their paper in the Journal of Clinical Epidemiology, aptly named “Grilling the Data,” they didn’t just conjure up the many analytic ways to study the red meat–mortality question. Instead, they used a published systematic review of 15 studies on unprocessed red meat and early mortality. The studies included in this review reported 70 unique ways to analyze the association.
Is Red Meat Good or Bad?
Their first finding was that this analysis yielded widely disparate effect estimates, from 0.63 (reduced risk for early death) to 2.31 (a higher risk). The median hazard ratio was 1.14 with an interquartile range (IQR) of 1.02-1.23. One might conclude from this that eating red meat is associated with a slightly higher risk for early mortality.
Their second step was to calculate how many ways (specifications) there were to analyze the data by totaling all possible combinations of choices in the 70 ways found in the systematic review.
They calculated a total of 10 quadrillion possible unique analyses. A quadrillion is 1 with 15 zeros. Computing power cannot handle that amount of analyses yet. So, they generated 20 random unique combinations of covariates, which narrowed the number of analyses to about 1400. About 200 of these were excluded due to implausibly wide confidence intervals.
Voilà. They now had about 1200 different ways to analyze a dataset; they chose an NHANES longitudinal cohort study from 2007-2014. They deemed each of the more than 1200 approaches plausible because they were derived from peer-reviewed papers written by experts in epidemiology.
Specification Curve Analyses Results
Each analysis (or specification) yielded a hazard ratio for red meat exposure and death.
- The median HR was 0.94 (IQR, 0.83-1.05) for the effect of red meat on all-cause mortality — ie, not significant.
- The range of hazard ratios was large. They went from 0.51 — a 49% reduced risk for early mortality — to 1.75: a 75% increase in early mortality.
- Among all analyses, 36% yielded hazard ratios above 1.0 and 64% less than 1.0.
- As for statistical significance, defined as P ≤.05, only 4% (or 48 specifications) met this threshold. Zeraatkar reminded me that this is what you’d expect if unprocessed red meat has no effect on longevity.
- Of the 48 analyses deemed statistically significant, 40 indicated that red meat consumption reduced early death and eight indicated that eating red meat led to higher mortality.
- Nearly half the analyses yielded unexciting point estimates, with hazard ratios between 0.90 and 1.10.
Paradigm Changing
As a user of evidence, I find this a potentially paradigm-changing study. Observational studies far outnumber randomized trials. For many medical questions, observational data are all we have.
Now think about every observational study published. The authors tell you — post hoc — which method they used to analyze the data. The key point is that it is one method.
Dr. Zeraatkar and colleagues have shown that there are thousands of plausible ways to analyze the data, and this can lead to very different findings. In the specific question of red meat and mortality, their many analyses yielded a null result.
Now imagine other cases where the researchers did many analyses of a dataset and chose to publish only the significant ones. Observational studies are rarely preregistered, so a reader cannot know how a result would vary depending on analytic choices. A specification curve analysis of a dataset provides a much broader picture. In the case of red meat, you see some significant results, but the vast majority hover around null.
What about the difficulty in analyzing a dataset 1000 different ways? Dr. Zeraatkar told me that it is harder than just choosing one method, but it’s not impossible.
The main barrier to adopting this multiverse approach to data, she noted, was not the extra work but the entrenched belief among researchers that there is a best way to analyze data.
I hope you read this paper and think about it every time you read an observational study that finds a positive or negative association between two things. Ask: What if the researchers were as careful as Dr. Zeraatkar and colleagues and did multiple different analyses? Would the finding hold up to a series of plausible analytic choices?
Nutritional epidemiology would benefit greatly from this approach. But so would any observational study of an exposure and outcome. I suspect that the number of “positive” associations would diminish. And that would not be a bad thing.
Dr. Mandrola, a clinical electrophysiologist at Baptist Medical Associates, Louisville, Kentucky, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Is AFib ablation the fifth pillar in heart failure care? CASTLE-HTx
Recorded Aug. 28, 2023. This transcript has been edited for clarity.
John M. Mandrola, MD: I’m here at the European Society of Cardiology meeting, and I’m very excited to have two colleagues whom I met at the Western Atrial Fibrillation Symposium (Western AFib) and who presented the CASTLE-HTx study. This is Christian Sohns and Philipp Sommer, and the CASTLE-HTx study is very exciting.
Before I get into that, I really want to introduce the concept of atrial fibrillation in heart failure. I like to say that there are two big populations of patients with atrial fibrillation, and the vast majority can be treated slowly with reassurance and education. There is a group of patients who have heart failure who, when they develop atrial fibrillation, can degenerate rapidly. The CASTLE-HTx study looked at catheter ablation versus medical therapy in patients with advanced heart failure.
Christian, why don’t you tell us the top-line results and what you found.
CASTLE-HTx key findings
Christian Sohns, MD, PhD: Thanks, first of all, for mentioning this special cohort of patients in end-stage heart failure, which is very important. The endpoint of the study was a composite of death from any cause or left ventricular assist device (LVAD) implantation and heart transplantation. These are very hard, strong clinical endpoints, not the rate of rehospitalization or something like that.
Catheter ablation was superior to medical therapy alone in terms of this composite endpoint. That was driven by cardiovascular death and all-cause mortality, which highlights the fact that you should always consider atrial fibrillation ablation in the end-stage heart failure cohort. The findings were driven by the fact that we saw left ventricular reverse remodeling and the reduction of atrial fibrillation in these patients.
Dr. Mandrola: Tell me about how it came about. It was conducted at your center. Who were these patients?
Philipp Sommer, MD: As one of the biggest centers for heart transplantations all over Europe, with roughly 100 transplants per year, we had many patients being referred to our center with the questions of whether those patients are eligible for a heart transplantation. Not all of the patients in our study were listed for a transplant, but all of them were admitted in that end-stage heart failure status to evaluate their eligibility for transplant.
If we look at the baseline data of those patients, they had an ejection fraction of 29%. They had a 6-minute walk test as a functional capacity parameter of around 300 m. Approximately two thirds of them were New York Heart Association class III and IV, which is significantly worse than what we saw in the previous studies dealing with heart failure patients.
I think overall, if you also look at NT-proBNP levels, this is a really sick patient population where some people might doubt if they should admit and refer those patients for an ablation procedure. Therefore, it’s really interesting and fascinating to see the results.
Dr. Mandrola: I did read in the manuscript, and I heard from you, that these were recruited as outpatients. So they were stable outpatients who were referred to the center for consideration of an LVAD or transplant?
Dr. Sohns: The definition of stability is very difficult in these patients because they have hospital stays, they have a history of drug therapy, and they have a history of interventions also behind them – not atrial fibrillation ablation, but others. I think these patients are referred because the referring physicians are done with the case. They can no longer offer any option to the patients other than surgical treatment, assist device, pump implantation, or transplantation.
If you look at the guidelines, they do not comment on atrial fibrillation ablation in this cohort of patients. Also, they have different recommendations between the American societies and the European societies regarding what is end-stage heart failure and how to treat these patients. Therefore, it was a big benefit of CASTLE-HTx that we randomized a cohort of patients with advanced end-stage heart failure.
How can AFib ablation have such big, early effects?
Dr. Mandrola: These are very clinically significant findings, with large effect sizes and very early separation of the Kaplan-Meier curves. How do you explain how dramatic an effect that is, and how early of an effect?
Dr. Sommer: That’s one of the key questions at the end of the day. I think our job basically was to provide the data and to ensure that the data are clean and that it’s all perfectly done. The interpretation of these data is really kind of difficult, although we do not have the 100% perfect and obvious explanation why the curves separated so early. Our view on that is that we are talking about a pretty fragile patient population, so little differences like having a tachyarrhythmia of 110 day in, day out or being in sinus rhythm of 60 can make a huge difference. That’s obviously pretty early.
The one that remains in tachyarrhythmia will deteriorate and will require an LVAD after a couple of months, and the one that you may keep in sinus rhythm, even with reduced atrial fibrillation burden – not zero, but reduced atrial fibrillation burden – and improved LV function, all of a sudden this patient will still remain on a low level of being stable, but he or she will remain stable and will not require any surgical interventions for the next 1.5-2 years. If we can manage to do this, just postponing the natural cause of the disease, I think that is a great benefit for the patient.
Dr. Mandrola: One of the things that comes up in our center is that I look at some of these patients and think, there’s no way I can put this patient under general anesthetic and do all of this. Your ablation procedure wasn’t that extensive, was it?
Dr. Sohns: On the one hand, no. On the other hand, yes. You need to take into consideration that it has been performed by experienced physicians with experience in heart failure treatment and atrial fibrillation in heart transplantation centers, though it›s not sure that we can transfer these results one-to-one to all other centers in the world.
It is very clear that we have almost no major complications in these patients. We were able to do these ablation procedures without general anesthesia. We have 60% of patients who had pulmonary vein isolation only and 40% of patients who have PVI and additional therapy. We have a procedure duration of almost 90 minutes during radiofrequency ablation.
We have different categories. When you talk about the different patient cohorts, we also see different stages of myocardial tissue damage, which will be part of another publication for sure. It is, in part, surprising how normal some of the atria were despite having a volume of 180 mL, but they had no fibrosis. That was very interesting.
Dr. Mandrola: How did the persistent vs paroxysmal atrial fibrillation sort out? Were these mostly patients with persistent atrial fibrillation?
Dr. Sommer: Two-thirds were persistent. It would be expected in this patient population that you would not find so many paroxysmal cases. I think it›s very important what Christian was just mentioning that when we discussed the trial design, we were anticipating problems with the sedation, for example. With the follow-up of those procedures, would they decompensate because of the fluid that you have to deliver during such a procedure.
We were quite surprised at the end of the day that the procedures were quite straightforward. Fortunately, we had no major complications. I think there were four complications in the 100 ablated patients. I think we were really positive about how the procedures turned out.
I should mention that one of the exclusion criteria was a left atrial diameter of about 60 mm. The huge ones may be very diseased, and maybe the hopeless ones were excluded from the study. Below 60 mm, we did the ablation.
Rhythm control
Dr. Mandrola: One of my colleagues, who is even more skeptical than me, wanted me to ask you, why wouldn’t you take a patient with persistent atrial fibrillation who had heart failure and just cardiovert and use amiodarone and try and maintain sinus rhythm that way?
Dr. Sohns: It is important to mention that 50% of the patients have already had amiodarone before they were randomized and enrolled for the trial. It might bring you a couple of minutes or a couple of hours [of relief], but the patients would get recurrence.
It was very interesting also, and this is in line with the data from Jason Andrade, who demonstrated that we were able to reduce the percentage of patients with persistent atrial fibrillation to paroxysmal. We did a down-staging of the underlying disease. This is not possible with cardioversion or drugs, for example.
Dr. Sommer: What I really like about that question and that comment is the idea that rhythm control in this subset of patients obviously has a role and an importance. It may be a cardioversion initially, giving amiodarone if they didn’t have that before, and you can keep the patient in sinus rhythm with this therapy, I think we’re reaching the same goal.
I think the critical point to get into the mind of physicians who treat heart failure is that sinus rhythm is beneficial, however you get there. Ablation, of course, as in other studies, is the most powerful tool to get there. Cardioversion can be a really good thing to do; you just have to think about it and consider it.
Dr. Mandrola: I do want to say to everybody that there is a tension sometimes between the heart failure community and the electrophysiology community. I think the ideal situation is that we work together, because I think that we can help with the maintenance of sinus rhythm. The control group mortality at 1 year was 20%, and I’ve heard people say that that’s not advanced heart failure. Advanced heart failure patients have much higher mortality than that. My colleague who is a heart failure specialist was criticizing a selection bias in picking the best patients. How would you answer that?
Dr. Sohns: There are data available from Eurotransplant, for example, that the waiting list mortality is 18%, so I think we are almost in line with this 20% mortality in this conservative group. You cannot generalize it. All these patients have different histories. We have 60% dilated cardiomyopathy and 40% ischemic cardiomyopathy. I think it is a very representative group in contrast to your friend who suggests that it is not.
Dr. Sommer: What I like about the discussion is that some approach us to say that the mortality in the control group is much too high – like, what are you doing with those patients that you create so many endpoints? Then others say that it’s not high enough because that is not end-stage heart failure. Come on! We have a patient cohort that is very well described and very well characterized.
If the label is end-stage heart failure, advanced heart failure, or whatever, they are sicker than the patients that we had in earlier trials. The patients that we treated were mostly excluded from all other trials. We opened the door. We found a clear result. I think everyone can see whatever you like to see.
Dr. Mandrola: What would your take-home message be after having done this trial design, the trial was conducted in your single center, and you come up with these amazing results? What would your message be to the whole community?
Dr. Sohns: Taking into consideration how severely sick these patients are, I can just repeat it: They are one step away from death, more or less, or from surgical intervention that can prolong their life. You should also consider that there are options like atrial fibrillation ablation that can buy time, postpone the natural course, or even in some patients replace the destination therapy. Therefore, in my opinion the next guidelines should recommend that every patient should carefully be checked for sinus rhythm before bringing these patients into the environment of transplantation.
Dr. Sommer: My interpretation is that we have to try to bring into physicians’ minds that besides a well-established and well-documented effect of drug therapy with the fabulous four, we may now have the fabulous five, including an ablation option for patients with atrial fibrillation.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. Dr. Sohns is deputy director of the Heart and Diabetes Center NRW, Ruhr University Bochum, Bad Oeynhausen, Germany. Dr. Sommer is professor of cardiology at the Heart and Diabetes Center NRW. Dr. Mandrola reported no conflicts of interest. Dr. Sohns reported receiving research funding from Else Kröner–Fresenius–Stiftung. Dr. Sommer reported consulting with Abbott, Biosense Webster, Boston Scientific, and Medtronic USA.
A version of this article first appeared on Medscape.com.
Recorded Aug. 28, 2023. This transcript has been edited for clarity.
John M. Mandrola, MD: I’m here at the European Society of Cardiology meeting, and I’m very excited to have two colleagues whom I met at the Western Atrial Fibrillation Symposium (Western AFib) and who presented the CASTLE-HTx study. This is Christian Sohns and Philipp Sommer, and the CASTLE-HTx study is very exciting.
Before I get into that, I really want to introduce the concept of atrial fibrillation in heart failure. I like to say that there are two big populations of patients with atrial fibrillation, and the vast majority can be treated slowly with reassurance and education. There is a group of patients who have heart failure who, when they develop atrial fibrillation, can degenerate rapidly. The CASTLE-HTx study looked at catheter ablation versus medical therapy in patients with advanced heart failure.
Christian, why don’t you tell us the top-line results and what you found.
CASTLE-HTx key findings
Christian Sohns, MD, PhD: Thanks, first of all, for mentioning this special cohort of patients in end-stage heart failure, which is very important. The endpoint of the study was a composite of death from any cause or left ventricular assist device (LVAD) implantation and heart transplantation. These are very hard, strong clinical endpoints, not the rate of rehospitalization or something like that.
Catheter ablation was superior to medical therapy alone in terms of this composite endpoint. That was driven by cardiovascular death and all-cause mortality, which highlights the fact that you should always consider atrial fibrillation ablation in the end-stage heart failure cohort. The findings were driven by the fact that we saw left ventricular reverse remodeling and the reduction of atrial fibrillation in these patients.
Dr. Mandrola: Tell me about how it came about. It was conducted at your center. Who were these patients?
Philipp Sommer, MD: As one of the biggest centers for heart transplantations all over Europe, with roughly 100 transplants per year, we had many patients being referred to our center with the questions of whether those patients are eligible for a heart transplantation. Not all of the patients in our study were listed for a transplant, but all of them were admitted in that end-stage heart failure status to evaluate their eligibility for transplant.
If we look at the baseline data of those patients, they had an ejection fraction of 29%. They had a 6-minute walk test as a functional capacity parameter of around 300 m. Approximately two thirds of them were New York Heart Association class III and IV, which is significantly worse than what we saw in the previous studies dealing with heart failure patients.
I think overall, if you also look at NT-proBNP levels, this is a really sick patient population where some people might doubt if they should admit and refer those patients for an ablation procedure. Therefore, it’s really interesting and fascinating to see the results.
Dr. Mandrola: I did read in the manuscript, and I heard from you, that these were recruited as outpatients. So they were stable outpatients who were referred to the center for consideration of an LVAD or transplant?
Dr. Sohns: The definition of stability is very difficult in these patients because they have hospital stays, they have a history of drug therapy, and they have a history of interventions also behind them – not atrial fibrillation ablation, but others. I think these patients are referred because the referring physicians are done with the case. They can no longer offer any option to the patients other than surgical treatment, assist device, pump implantation, or transplantation.
If you look at the guidelines, they do not comment on atrial fibrillation ablation in this cohort of patients. Also, they have different recommendations between the American societies and the European societies regarding what is end-stage heart failure and how to treat these patients. Therefore, it was a big benefit of CASTLE-HTx that we randomized a cohort of patients with advanced end-stage heart failure.
How can AFib ablation have such big, early effects?
Dr. Mandrola: These are very clinically significant findings, with large effect sizes and very early separation of the Kaplan-Meier curves. How do you explain how dramatic an effect that is, and how early of an effect?
Dr. Sommer: That’s one of the key questions at the end of the day. I think our job basically was to provide the data and to ensure that the data are clean and that it’s all perfectly done. The interpretation of these data is really kind of difficult, although we do not have the 100% perfect and obvious explanation why the curves separated so early. Our view on that is that we are talking about a pretty fragile patient population, so little differences like having a tachyarrhythmia of 110 day in, day out or being in sinus rhythm of 60 can make a huge difference. That’s obviously pretty early.
The one that remains in tachyarrhythmia will deteriorate and will require an LVAD after a couple of months, and the one that you may keep in sinus rhythm, even with reduced atrial fibrillation burden – not zero, but reduced atrial fibrillation burden – and improved LV function, all of a sudden this patient will still remain on a low level of being stable, but he or she will remain stable and will not require any surgical interventions for the next 1.5-2 years. If we can manage to do this, just postponing the natural cause of the disease, I think that is a great benefit for the patient.
Dr. Mandrola: One of the things that comes up in our center is that I look at some of these patients and think, there’s no way I can put this patient under general anesthetic and do all of this. Your ablation procedure wasn’t that extensive, was it?
Dr. Sohns: On the one hand, no. On the other hand, yes. You need to take into consideration that it has been performed by experienced physicians with experience in heart failure treatment and atrial fibrillation in heart transplantation centers, though it›s not sure that we can transfer these results one-to-one to all other centers in the world.
It is very clear that we have almost no major complications in these patients. We were able to do these ablation procedures without general anesthesia. We have 60% of patients who had pulmonary vein isolation only and 40% of patients who have PVI and additional therapy. We have a procedure duration of almost 90 minutes during radiofrequency ablation.
We have different categories. When you talk about the different patient cohorts, we also see different stages of myocardial tissue damage, which will be part of another publication for sure. It is, in part, surprising how normal some of the atria were despite having a volume of 180 mL, but they had no fibrosis. That was very interesting.
Dr. Mandrola: How did the persistent vs paroxysmal atrial fibrillation sort out? Were these mostly patients with persistent atrial fibrillation?
Dr. Sommer: Two-thirds were persistent. It would be expected in this patient population that you would not find so many paroxysmal cases. I think it›s very important what Christian was just mentioning that when we discussed the trial design, we were anticipating problems with the sedation, for example. With the follow-up of those procedures, would they decompensate because of the fluid that you have to deliver during such a procedure.
We were quite surprised at the end of the day that the procedures were quite straightforward. Fortunately, we had no major complications. I think there were four complications in the 100 ablated patients. I think we were really positive about how the procedures turned out.
I should mention that one of the exclusion criteria was a left atrial diameter of about 60 mm. The huge ones may be very diseased, and maybe the hopeless ones were excluded from the study. Below 60 mm, we did the ablation.
Rhythm control
Dr. Mandrola: One of my colleagues, who is even more skeptical than me, wanted me to ask you, why wouldn’t you take a patient with persistent atrial fibrillation who had heart failure and just cardiovert and use amiodarone and try and maintain sinus rhythm that way?
Dr. Sohns: It is important to mention that 50% of the patients have already had amiodarone before they were randomized and enrolled for the trial. It might bring you a couple of minutes or a couple of hours [of relief], but the patients would get recurrence.
It was very interesting also, and this is in line with the data from Jason Andrade, who demonstrated that we were able to reduce the percentage of patients with persistent atrial fibrillation to paroxysmal. We did a down-staging of the underlying disease. This is not possible with cardioversion or drugs, for example.
Dr. Sommer: What I really like about that question and that comment is the idea that rhythm control in this subset of patients obviously has a role and an importance. It may be a cardioversion initially, giving amiodarone if they didn’t have that before, and you can keep the patient in sinus rhythm with this therapy, I think we’re reaching the same goal.
I think the critical point to get into the mind of physicians who treat heart failure is that sinus rhythm is beneficial, however you get there. Ablation, of course, as in other studies, is the most powerful tool to get there. Cardioversion can be a really good thing to do; you just have to think about it and consider it.
Dr. Mandrola: I do want to say to everybody that there is a tension sometimes between the heart failure community and the electrophysiology community. I think the ideal situation is that we work together, because I think that we can help with the maintenance of sinus rhythm. The control group mortality at 1 year was 20%, and I’ve heard people say that that’s not advanced heart failure. Advanced heart failure patients have much higher mortality than that. My colleague who is a heart failure specialist was criticizing a selection bias in picking the best patients. How would you answer that?
Dr. Sohns: There are data available from Eurotransplant, for example, that the waiting list mortality is 18%, so I think we are almost in line with this 20% mortality in this conservative group. You cannot generalize it. All these patients have different histories. We have 60% dilated cardiomyopathy and 40% ischemic cardiomyopathy. I think it is a very representative group in contrast to your friend who suggests that it is not.
Dr. Sommer: What I like about the discussion is that some approach us to say that the mortality in the control group is much too high – like, what are you doing with those patients that you create so many endpoints? Then others say that it’s not high enough because that is not end-stage heart failure. Come on! We have a patient cohort that is very well described and very well characterized.
If the label is end-stage heart failure, advanced heart failure, or whatever, they are sicker than the patients that we had in earlier trials. The patients that we treated were mostly excluded from all other trials. We opened the door. We found a clear result. I think everyone can see whatever you like to see.
Dr. Mandrola: What would your take-home message be after having done this trial design, the trial was conducted in your single center, and you come up with these amazing results? What would your message be to the whole community?
Dr. Sohns: Taking into consideration how severely sick these patients are, I can just repeat it: They are one step away from death, more or less, or from surgical intervention that can prolong their life. You should also consider that there are options like atrial fibrillation ablation that can buy time, postpone the natural course, or even in some patients replace the destination therapy. Therefore, in my opinion the next guidelines should recommend that every patient should carefully be checked for sinus rhythm before bringing these patients into the environment of transplantation.
Dr. Sommer: My interpretation is that we have to try to bring into physicians’ minds that besides a well-established and well-documented effect of drug therapy with the fabulous four, we may now have the fabulous five, including an ablation option for patients with atrial fibrillation.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. Dr. Sohns is deputy director of the Heart and Diabetes Center NRW, Ruhr University Bochum, Bad Oeynhausen, Germany. Dr. Sommer is professor of cardiology at the Heart and Diabetes Center NRW. Dr. Mandrola reported no conflicts of interest. Dr. Sohns reported receiving research funding from Else Kröner–Fresenius–Stiftung. Dr. Sommer reported consulting with Abbott, Biosense Webster, Boston Scientific, and Medtronic USA.
A version of this article first appeared on Medscape.com.
Recorded Aug. 28, 2023. This transcript has been edited for clarity.
John M. Mandrola, MD: I’m here at the European Society of Cardiology meeting, and I’m very excited to have two colleagues whom I met at the Western Atrial Fibrillation Symposium (Western AFib) and who presented the CASTLE-HTx study. This is Christian Sohns and Philipp Sommer, and the CASTLE-HTx study is very exciting.
Before I get into that, I really want to introduce the concept of atrial fibrillation in heart failure. I like to say that there are two big populations of patients with atrial fibrillation, and the vast majority can be treated slowly with reassurance and education. There is a group of patients who have heart failure who, when they develop atrial fibrillation, can degenerate rapidly. The CASTLE-HTx study looked at catheter ablation versus medical therapy in patients with advanced heart failure.
Christian, why don’t you tell us the top-line results and what you found.
CASTLE-HTx key findings
Christian Sohns, MD, PhD: Thanks, first of all, for mentioning this special cohort of patients in end-stage heart failure, which is very important. The endpoint of the study was a composite of death from any cause or left ventricular assist device (LVAD) implantation and heart transplantation. These are very hard, strong clinical endpoints, not the rate of rehospitalization or something like that.
Catheter ablation was superior to medical therapy alone in terms of this composite endpoint. That was driven by cardiovascular death and all-cause mortality, which highlights the fact that you should always consider atrial fibrillation ablation in the end-stage heart failure cohort. The findings were driven by the fact that we saw left ventricular reverse remodeling and the reduction of atrial fibrillation in these patients.
Dr. Mandrola: Tell me about how it came about. It was conducted at your center. Who were these patients?
Philipp Sommer, MD: As one of the biggest centers for heart transplantations all over Europe, with roughly 100 transplants per year, we had many patients being referred to our center with the questions of whether those patients are eligible for a heart transplantation. Not all of the patients in our study were listed for a transplant, but all of them were admitted in that end-stage heart failure status to evaluate their eligibility for transplant.
If we look at the baseline data of those patients, they had an ejection fraction of 29%. They had a 6-minute walk test as a functional capacity parameter of around 300 m. Approximately two thirds of them were New York Heart Association class III and IV, which is significantly worse than what we saw in the previous studies dealing with heart failure patients.
I think overall, if you also look at NT-proBNP levels, this is a really sick patient population where some people might doubt if they should admit and refer those patients for an ablation procedure. Therefore, it’s really interesting and fascinating to see the results.
Dr. Mandrola: I did read in the manuscript, and I heard from you, that these were recruited as outpatients. So they were stable outpatients who were referred to the center for consideration of an LVAD or transplant?
Dr. Sohns: The definition of stability is very difficult in these patients because they have hospital stays, they have a history of drug therapy, and they have a history of interventions also behind them – not atrial fibrillation ablation, but others. I think these patients are referred because the referring physicians are done with the case. They can no longer offer any option to the patients other than surgical treatment, assist device, pump implantation, or transplantation.
If you look at the guidelines, they do not comment on atrial fibrillation ablation in this cohort of patients. Also, they have different recommendations between the American societies and the European societies regarding what is end-stage heart failure and how to treat these patients. Therefore, it was a big benefit of CASTLE-HTx that we randomized a cohort of patients with advanced end-stage heart failure.
How can AFib ablation have such big, early effects?
Dr. Mandrola: These are very clinically significant findings, with large effect sizes and very early separation of the Kaplan-Meier curves. How do you explain how dramatic an effect that is, and how early of an effect?
Dr. Sommer: That’s one of the key questions at the end of the day. I think our job basically was to provide the data and to ensure that the data are clean and that it’s all perfectly done. The interpretation of these data is really kind of difficult, although we do not have the 100% perfect and obvious explanation why the curves separated so early. Our view on that is that we are talking about a pretty fragile patient population, so little differences like having a tachyarrhythmia of 110 day in, day out or being in sinus rhythm of 60 can make a huge difference. That’s obviously pretty early.
The one that remains in tachyarrhythmia will deteriorate and will require an LVAD after a couple of months, and the one that you may keep in sinus rhythm, even with reduced atrial fibrillation burden – not zero, but reduced atrial fibrillation burden – and improved LV function, all of a sudden this patient will still remain on a low level of being stable, but he or she will remain stable and will not require any surgical interventions for the next 1.5-2 years. If we can manage to do this, just postponing the natural cause of the disease, I think that is a great benefit for the patient.
Dr. Mandrola: One of the things that comes up in our center is that I look at some of these patients and think, there’s no way I can put this patient under general anesthetic and do all of this. Your ablation procedure wasn’t that extensive, was it?
Dr. Sohns: On the one hand, no. On the other hand, yes. You need to take into consideration that it has been performed by experienced physicians with experience in heart failure treatment and atrial fibrillation in heart transplantation centers, though it›s not sure that we can transfer these results one-to-one to all other centers in the world.
It is very clear that we have almost no major complications in these patients. We were able to do these ablation procedures without general anesthesia. We have 60% of patients who had pulmonary vein isolation only and 40% of patients who have PVI and additional therapy. We have a procedure duration of almost 90 minutes during radiofrequency ablation.
We have different categories. When you talk about the different patient cohorts, we also see different stages of myocardial tissue damage, which will be part of another publication for sure. It is, in part, surprising how normal some of the atria were despite having a volume of 180 mL, but they had no fibrosis. That was very interesting.
Dr. Mandrola: How did the persistent vs paroxysmal atrial fibrillation sort out? Were these mostly patients with persistent atrial fibrillation?
Dr. Sommer: Two-thirds were persistent. It would be expected in this patient population that you would not find so many paroxysmal cases. I think it›s very important what Christian was just mentioning that when we discussed the trial design, we were anticipating problems with the sedation, for example. With the follow-up of those procedures, would they decompensate because of the fluid that you have to deliver during such a procedure.
We were quite surprised at the end of the day that the procedures were quite straightforward. Fortunately, we had no major complications. I think there were four complications in the 100 ablated patients. I think we were really positive about how the procedures turned out.
I should mention that one of the exclusion criteria was a left atrial diameter of about 60 mm. The huge ones may be very diseased, and maybe the hopeless ones were excluded from the study. Below 60 mm, we did the ablation.
Rhythm control
Dr. Mandrola: One of my colleagues, who is even more skeptical than me, wanted me to ask you, why wouldn’t you take a patient with persistent atrial fibrillation who had heart failure and just cardiovert and use amiodarone and try and maintain sinus rhythm that way?
Dr. Sohns: It is important to mention that 50% of the patients have already had amiodarone before they were randomized and enrolled for the trial. It might bring you a couple of minutes or a couple of hours [of relief], but the patients would get recurrence.
It was very interesting also, and this is in line with the data from Jason Andrade, who demonstrated that we were able to reduce the percentage of patients with persistent atrial fibrillation to paroxysmal. We did a down-staging of the underlying disease. This is not possible with cardioversion or drugs, for example.
Dr. Sommer: What I really like about that question and that comment is the idea that rhythm control in this subset of patients obviously has a role and an importance. It may be a cardioversion initially, giving amiodarone if they didn’t have that before, and you can keep the patient in sinus rhythm with this therapy, I think we’re reaching the same goal.
I think the critical point to get into the mind of physicians who treat heart failure is that sinus rhythm is beneficial, however you get there. Ablation, of course, as in other studies, is the most powerful tool to get there. Cardioversion can be a really good thing to do; you just have to think about it and consider it.
Dr. Mandrola: I do want to say to everybody that there is a tension sometimes between the heart failure community and the electrophysiology community. I think the ideal situation is that we work together, because I think that we can help with the maintenance of sinus rhythm. The control group mortality at 1 year was 20%, and I’ve heard people say that that’s not advanced heart failure. Advanced heart failure patients have much higher mortality than that. My colleague who is a heart failure specialist was criticizing a selection bias in picking the best patients. How would you answer that?
Dr. Sohns: There are data available from Eurotransplant, for example, that the waiting list mortality is 18%, so I think we are almost in line with this 20% mortality in this conservative group. You cannot generalize it. All these patients have different histories. We have 60% dilated cardiomyopathy and 40% ischemic cardiomyopathy. I think it is a very representative group in contrast to your friend who suggests that it is not.
Dr. Sommer: What I like about the discussion is that some approach us to say that the mortality in the control group is much too high – like, what are you doing with those patients that you create so many endpoints? Then others say that it’s not high enough because that is not end-stage heart failure. Come on! We have a patient cohort that is very well described and very well characterized.
If the label is end-stage heart failure, advanced heart failure, or whatever, they are sicker than the patients that we had in earlier trials. The patients that we treated were mostly excluded from all other trials. We opened the door. We found a clear result. I think everyone can see whatever you like to see.
Dr. Mandrola: What would your take-home message be after having done this trial design, the trial was conducted in your single center, and you come up with these amazing results? What would your message be to the whole community?
Dr. Sohns: Taking into consideration how severely sick these patients are, I can just repeat it: They are one step away from death, more or less, or from surgical intervention that can prolong their life. You should also consider that there are options like atrial fibrillation ablation that can buy time, postpone the natural course, or even in some patients replace the destination therapy. Therefore, in my opinion the next guidelines should recommend that every patient should carefully be checked for sinus rhythm before bringing these patients into the environment of transplantation.
Dr. Sommer: My interpretation is that we have to try to bring into physicians’ minds that besides a well-established and well-documented effect of drug therapy with the fabulous four, we may now have the fabulous five, including an ablation option for patients with atrial fibrillation.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. Dr. Sohns is deputy director of the Heart and Diabetes Center NRW, Ruhr University Bochum, Bad Oeynhausen, Germany. Dr. Sommer is professor of cardiology at the Heart and Diabetes Center NRW. Dr. Mandrola reported no conflicts of interest. Dr. Sohns reported receiving research funding from Else Kröner–Fresenius–Stiftung. Dr. Sommer reported consulting with Abbott, Biosense Webster, Boston Scientific, and Medtronic USA.
A version of this article first appeared on Medscape.com.
The most important study from ESC: FRAIL-AF
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Are fish oils on the hook for AFib risk?
Questions about omega-3 fatty acid supplements come up often in the atrial fibrillation (AFib) clinic.
The story begins with the simple observation that populations who eat lots of oily fish have fewer coronary events. This correlation provoked great interest in concentrating fish oils in pill form and studying their use to promote health.
OMENI secondary analysis
Peder Myhre, MD, and colleagues recently published a secondary analysis of the OMENI trial looking at both the risk and possible causes of AFib in the omega-3 group.
The OMENI trial randomly assigned slightly more than 1,000 older patients (mean age, 75 years) post–myocardial infarction to either 1.8 g/d of fish oil supplements versus placebo for 2 years. The supplements comprised 930 mg of eicosapentaenoic acid (EPA) and 660 mg of docosahexaenoic acid (DHA). The main trial reported no difference in a composite primary endpoint of MI, revascularization, stroke, death, or hospitalization for heart failure.
The secondary analysis explored the 75% of patients in the main trial who had no history of AFib. It looked at how many in each group developed either true clinical AFib or what the authors called micro-AFib, defined as short bursts of irregular atrial activity lasting seconds.
The sub-analysis had three main findings: Patients in the supplement arm had a 90% higher rate of AFib or micro-AFib, compared with patients on placebo, EPA had the strongest effect on the association, and there was a graded risk for AFib with increasing serum EPA levels.
The authors raised the possibility that more micro-AFib might be a possible mediator of AFib risk.
Trials of low-dose EPA and DHA
First, the low-dose trials. In the ASCEND trial from 2018, more than 15,000 patients with diabetes were randomly assigned to either 1 g of omega-3 fatty acids (460-mg EPA and 380-mg DHA) or mineral oil.
The trial was neutral. After 7.4 years, the primary endpoint of MI, stroke, transient ischemic attack, or cardiovascular death occurred in 8.9% of the supplement group versus 9.2% of the placebo arm.The incidence of AFib was higher in the omega-3 group but did not reach statistical significance (2.1% vs. 1.7% for placebo; hazard ratio, 1.23; 95% confidence interval, 0.98-1.54).
Another neutral CV trial, VITAL, specifically studied the effects of marine omega-3 pills (460-mg EPA and 380-mg DHA) in older adults without heart disease, cancer, or AFib. After slightly more than 5 years, AFib occurred at a similar rate in the active arm and placebo arms (3.7% vs. 3.4% for placebo; HR, 1.09; 95% CI, 0.96-1.24; P = .19)
Trials of very high-dose marine omega-3s
Next came trials of higher doses in higher-risk populations.
In 2020, JAMA published the STRENGTH trial, which compared 4 g/d of a carboxylic acid formulation of EPA and DHA with a corn oil placebo in more than 13,000 patients who either had established atherosclerotic CV disease (ASCVD) or were at high risk for ASCVD.
The trial was terminated early because of futility and a signal of increased AFib risk in the supplement arm.
Nearly the same number of patients in the supplement versus placebo arm experienced a primary composite endpoint of major adverse cardiac events: 12.0% versus 12.2%, respectively.
AFib was a tertiary endpoint in this trial. An increase in investigator-reported new-onset AFib was observed in the omega-3 group: 2.2% vs. 1.3% for corn oil (HR, 1.69; 95% CI, 1.29-2.21; nominal P < .001).
The REDUCE-IT trial randomly assigned more than 8,000 patients who had ASCVD or diabetes and high ASCVD risk and elevated triglyceride levels to either 4 g of icosapent ethyl daily, a concentrated form of EPA, or a mineral oil placebo.
After nearly 5 years, there was a 4.8% absolute risk reduction in the primary endpoint of CV death, MI, stroke, revascularization, or unstable angina with icosapent ethyl. An increase in atherogenic biomarkers in the mineral oil placebo complicated interpretation of this trial.
Hospitalization for AFib or flutter occurred in 3.1% of the active arm versus 2.1% of the mineral oil group (P = .004).
Meta-analysis of marine omega-3 supplement trials
In 2021, Baris Gencer and colleagues performed a meta-analysis of these five trials plus 2 more (GISSI-HF and RP) looking specifically at risk for AFib. Their final analysis included more than 81,000 patients followed for nearly 5 years.
Omega 3 fatty acid supplements associated with a 25% increase in the risk for AFib (HR, 1.25; 95% CI, 1.07-1.46P =.013). Exploring further, they noted a dose-dependent relationship. Most of the increased risk occurred in trials that tested greater than 1 g/d.
Summary
When faced with surprise findings, I like to think things through.
First about plausibility. Omega-3 fatty acids clearly exert electrophysiologic effects on cardiac cells, an increase in AFib risk is plausible. The exact underlying mechanism may be unknown, but exact mechanisms are less important than actual clinical effects (see sodium-glucose cotransporter 2 inhibitors).
What about causality? Factors supporting causality include plausibility, consistency of increased AFib risk in multiple studies, and a dose-response relationship.
I see multiple clinical implications of this observation.
The first is the power of the randomized trial to inform practice. If we relied only on observational evidence, we might have assumed that since high fish consumption in populations associated with lower rates of cardiac events, fish oil supplementation would also reduce cardiac events. Other than the outlier trial, REDUCE-IT, with its mineral oil placebo, the preponderance of the randomized controlled trial evidence does not support fish oils for the reduction of CV events.
Randomized controlled trials also exposed the AFib risk. This would have been difficult to sort out in nonrandom observational studies.
Another underappreciated lesson is the notion that drugs, including supplements, can have off-target effects.
Consider the case of statin drugs. It is widely assumed that statins reduce cardiac events by lowering low-density lipoprotein cholesterol (LDL-C). Yet, statins became a mainstay not because of LDL-C lowering but because multiple trials found that this class of drugs reduced cardiac events without increasing adverse effects.
Omega-3 fatty acids reduce triglyceride levels, but this is not enough to adopt the use of these pills. The lack of consistent reduction in CV events and the off-target signal of AFib risk argue against routine use of fish-oil pills.
I will close with uncertainty. Though there is plausibility and multiple reasons to infer causality of marine omega-3s in increasing AFib risk, the effect size remains unknown.
In an editorial accompanying the recent meta-analysis, epidemiologist Michelle Samuel, MPH, PhD, and electrophysiologist Stanley Nattel, MD, cautioned readers on a technical but important point. It concerns the matter of competing risks, such as death, in the analysis of AFib risk, meaning that patients who died may have developed AFib had they lived. They provide a detailed explanation in the open access article, but the take-home is that the exact effect size is difficult to quantify without patient-level original data.
No matter. I find the signal of increased AFib risk an important one to use at the bedside.
Intermittent AFib has an unpredictable natural history. It often resolves as mysteriously as it arises. When patients take fish-oil supplements, I cite these studies, note the lack of CV protection, then I recommend stopping the pills.
This allows for one of the most important interventions in AFib care: time.
Dr. Mandrola is a clinical electrophysiologist with Baptist Medical Associates, Louisville, Ky. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Questions about omega-3 fatty acid supplements come up often in the atrial fibrillation (AFib) clinic.
The story begins with the simple observation that populations who eat lots of oily fish have fewer coronary events. This correlation provoked great interest in concentrating fish oils in pill form and studying their use to promote health.
OMENI secondary analysis
Peder Myhre, MD, and colleagues recently published a secondary analysis of the OMENI trial looking at both the risk and possible causes of AFib in the omega-3 group.
The OMENI trial randomly assigned slightly more than 1,000 older patients (mean age, 75 years) post–myocardial infarction to either 1.8 g/d of fish oil supplements versus placebo for 2 years. The supplements comprised 930 mg of eicosapentaenoic acid (EPA) and 660 mg of docosahexaenoic acid (DHA). The main trial reported no difference in a composite primary endpoint of MI, revascularization, stroke, death, or hospitalization for heart failure.
The secondary analysis explored the 75% of patients in the main trial who had no history of AFib. It looked at how many in each group developed either true clinical AFib or what the authors called micro-AFib, defined as short bursts of irregular atrial activity lasting seconds.
The sub-analysis had three main findings: Patients in the supplement arm had a 90% higher rate of AFib or micro-AFib, compared with patients on placebo, EPA had the strongest effect on the association, and there was a graded risk for AFib with increasing serum EPA levels.
The authors raised the possibility that more micro-AFib might be a possible mediator of AFib risk.
Trials of low-dose EPA and DHA
First, the low-dose trials. In the ASCEND trial from 2018, more than 15,000 patients with diabetes were randomly assigned to either 1 g of omega-3 fatty acids (460-mg EPA and 380-mg DHA) or mineral oil.
The trial was neutral. After 7.4 years, the primary endpoint of MI, stroke, transient ischemic attack, or cardiovascular death occurred in 8.9% of the supplement group versus 9.2% of the placebo arm.The incidence of AFib was higher in the omega-3 group but did not reach statistical significance (2.1% vs. 1.7% for placebo; hazard ratio, 1.23; 95% confidence interval, 0.98-1.54).
Another neutral CV trial, VITAL, specifically studied the effects of marine omega-3 pills (460-mg EPA and 380-mg DHA) in older adults without heart disease, cancer, or AFib. After slightly more than 5 years, AFib occurred at a similar rate in the active arm and placebo arms (3.7% vs. 3.4% for placebo; HR, 1.09; 95% CI, 0.96-1.24; P = .19)
Trials of very high-dose marine omega-3s
Next came trials of higher doses in higher-risk populations.
In 2020, JAMA published the STRENGTH trial, which compared 4 g/d of a carboxylic acid formulation of EPA and DHA with a corn oil placebo in more than 13,000 patients who either had established atherosclerotic CV disease (ASCVD) or were at high risk for ASCVD.
The trial was terminated early because of futility and a signal of increased AFib risk in the supplement arm.
Nearly the same number of patients in the supplement versus placebo arm experienced a primary composite endpoint of major adverse cardiac events: 12.0% versus 12.2%, respectively.
AFib was a tertiary endpoint in this trial. An increase in investigator-reported new-onset AFib was observed in the omega-3 group: 2.2% vs. 1.3% for corn oil (HR, 1.69; 95% CI, 1.29-2.21; nominal P < .001).
The REDUCE-IT trial randomly assigned more than 8,000 patients who had ASCVD or diabetes and high ASCVD risk and elevated triglyceride levels to either 4 g of icosapent ethyl daily, a concentrated form of EPA, or a mineral oil placebo.
After nearly 5 years, there was a 4.8% absolute risk reduction in the primary endpoint of CV death, MI, stroke, revascularization, or unstable angina with icosapent ethyl. An increase in atherogenic biomarkers in the mineral oil placebo complicated interpretation of this trial.
Hospitalization for AFib or flutter occurred in 3.1% of the active arm versus 2.1% of the mineral oil group (P = .004).
Meta-analysis of marine omega-3 supplement trials
In 2021, Baris Gencer and colleagues performed a meta-analysis of these five trials plus 2 more (GISSI-HF and RP) looking specifically at risk for AFib. Their final analysis included more than 81,000 patients followed for nearly 5 years.
Omega 3 fatty acid supplements associated with a 25% increase in the risk for AFib (HR, 1.25; 95% CI, 1.07-1.46P =.013). Exploring further, they noted a dose-dependent relationship. Most of the increased risk occurred in trials that tested greater than 1 g/d.
Summary
When faced with surprise findings, I like to think things through.
First about plausibility. Omega-3 fatty acids clearly exert electrophysiologic effects on cardiac cells, an increase in AFib risk is plausible. The exact underlying mechanism may be unknown, but exact mechanisms are less important than actual clinical effects (see sodium-glucose cotransporter 2 inhibitors).
What about causality? Factors supporting causality include plausibility, consistency of increased AFib risk in multiple studies, and a dose-response relationship.
I see multiple clinical implications of this observation.
The first is the power of the randomized trial to inform practice. If we relied only on observational evidence, we might have assumed that since high fish consumption in populations associated with lower rates of cardiac events, fish oil supplementation would also reduce cardiac events. Other than the outlier trial, REDUCE-IT, with its mineral oil placebo, the preponderance of the randomized controlled trial evidence does not support fish oils for the reduction of CV events.
Randomized controlled trials also exposed the AFib risk. This would have been difficult to sort out in nonrandom observational studies.
Another underappreciated lesson is the notion that drugs, including supplements, can have off-target effects.
Consider the case of statin drugs. It is widely assumed that statins reduce cardiac events by lowering low-density lipoprotein cholesterol (LDL-C). Yet, statins became a mainstay not because of LDL-C lowering but because multiple trials found that this class of drugs reduced cardiac events without increasing adverse effects.
Omega-3 fatty acids reduce triglyceride levels, but this is not enough to adopt the use of these pills. The lack of consistent reduction in CV events and the off-target signal of AFib risk argue against routine use of fish-oil pills.
I will close with uncertainty. Though there is plausibility and multiple reasons to infer causality of marine omega-3s in increasing AFib risk, the effect size remains unknown.
In an editorial accompanying the recent meta-analysis, epidemiologist Michelle Samuel, MPH, PhD, and electrophysiologist Stanley Nattel, MD, cautioned readers on a technical but important point. It concerns the matter of competing risks, such as death, in the analysis of AFib risk, meaning that patients who died may have developed AFib had they lived. They provide a detailed explanation in the open access article, but the take-home is that the exact effect size is difficult to quantify without patient-level original data.
No matter. I find the signal of increased AFib risk an important one to use at the bedside.
Intermittent AFib has an unpredictable natural history. It often resolves as mysteriously as it arises. When patients take fish-oil supplements, I cite these studies, note the lack of CV protection, then I recommend stopping the pills.
This allows for one of the most important interventions in AFib care: time.
Dr. Mandrola is a clinical electrophysiologist with Baptist Medical Associates, Louisville, Ky. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Questions about omega-3 fatty acid supplements come up often in the atrial fibrillation (AFib) clinic.
The story begins with the simple observation that populations who eat lots of oily fish have fewer coronary events. This correlation provoked great interest in concentrating fish oils in pill form and studying their use to promote health.
OMENI secondary analysis
Peder Myhre, MD, and colleagues recently published a secondary analysis of the OMENI trial looking at both the risk and possible causes of AFib in the omega-3 group.
The OMENI trial randomly assigned slightly more than 1,000 older patients (mean age, 75 years) post–myocardial infarction to either 1.8 g/d of fish oil supplements versus placebo for 2 years. The supplements comprised 930 mg of eicosapentaenoic acid (EPA) and 660 mg of docosahexaenoic acid (DHA). The main trial reported no difference in a composite primary endpoint of MI, revascularization, stroke, death, or hospitalization for heart failure.
The secondary analysis explored the 75% of patients in the main trial who had no history of AFib. It looked at how many in each group developed either true clinical AFib or what the authors called micro-AFib, defined as short bursts of irregular atrial activity lasting seconds.
The sub-analysis had three main findings: Patients in the supplement arm had a 90% higher rate of AFib or micro-AFib, compared with patients on placebo, EPA had the strongest effect on the association, and there was a graded risk for AFib with increasing serum EPA levels.
The authors raised the possibility that more micro-AFib might be a possible mediator of AFib risk.
Trials of low-dose EPA and DHA
First, the low-dose trials. In the ASCEND trial from 2018, more than 15,000 patients with diabetes were randomly assigned to either 1 g of omega-3 fatty acids (460-mg EPA and 380-mg DHA) or mineral oil.
The trial was neutral. After 7.4 years, the primary endpoint of MI, stroke, transient ischemic attack, or cardiovascular death occurred in 8.9% of the supplement group versus 9.2% of the placebo arm.The incidence of AFib was higher in the omega-3 group but did not reach statistical significance (2.1% vs. 1.7% for placebo; hazard ratio, 1.23; 95% confidence interval, 0.98-1.54).
Another neutral CV trial, VITAL, specifically studied the effects of marine omega-3 pills (460-mg EPA and 380-mg DHA) in older adults without heart disease, cancer, or AFib. After slightly more than 5 years, AFib occurred at a similar rate in the active arm and placebo arms (3.7% vs. 3.4% for placebo; HR, 1.09; 95% CI, 0.96-1.24; P = .19)
Trials of very high-dose marine omega-3s
Next came trials of higher doses in higher-risk populations.
In 2020, JAMA published the STRENGTH trial, which compared 4 g/d of a carboxylic acid formulation of EPA and DHA with a corn oil placebo in more than 13,000 patients who either had established atherosclerotic CV disease (ASCVD) or were at high risk for ASCVD.
The trial was terminated early because of futility and a signal of increased AFib risk in the supplement arm.
Nearly the same number of patients in the supplement versus placebo arm experienced a primary composite endpoint of major adverse cardiac events: 12.0% versus 12.2%, respectively.
AFib was a tertiary endpoint in this trial. An increase in investigator-reported new-onset AFib was observed in the omega-3 group: 2.2% vs. 1.3% for corn oil (HR, 1.69; 95% CI, 1.29-2.21; nominal P < .001).
The REDUCE-IT trial randomly assigned more than 8,000 patients who had ASCVD or diabetes and high ASCVD risk and elevated triglyceride levels to either 4 g of icosapent ethyl daily, a concentrated form of EPA, or a mineral oil placebo.
After nearly 5 years, there was a 4.8% absolute risk reduction in the primary endpoint of CV death, MI, stroke, revascularization, or unstable angina with icosapent ethyl. An increase in atherogenic biomarkers in the mineral oil placebo complicated interpretation of this trial.
Hospitalization for AFib or flutter occurred in 3.1% of the active arm versus 2.1% of the mineral oil group (P = .004).
Meta-analysis of marine omega-3 supplement trials
In 2021, Baris Gencer and colleagues performed a meta-analysis of these five trials plus 2 more (GISSI-HF and RP) looking specifically at risk for AFib. Their final analysis included more than 81,000 patients followed for nearly 5 years.
Omega 3 fatty acid supplements associated with a 25% increase in the risk for AFib (HR, 1.25; 95% CI, 1.07-1.46P =.013). Exploring further, they noted a dose-dependent relationship. Most of the increased risk occurred in trials that tested greater than 1 g/d.
Summary
When faced with surprise findings, I like to think things through.
First about plausibility. Omega-3 fatty acids clearly exert electrophysiologic effects on cardiac cells, an increase in AFib risk is plausible. The exact underlying mechanism may be unknown, but exact mechanisms are less important than actual clinical effects (see sodium-glucose cotransporter 2 inhibitors).
What about causality? Factors supporting causality include plausibility, consistency of increased AFib risk in multiple studies, and a dose-response relationship.
I see multiple clinical implications of this observation.
The first is the power of the randomized trial to inform practice. If we relied only on observational evidence, we might have assumed that since high fish consumption in populations associated with lower rates of cardiac events, fish oil supplementation would also reduce cardiac events. Other than the outlier trial, REDUCE-IT, with its mineral oil placebo, the preponderance of the randomized controlled trial evidence does not support fish oils for the reduction of CV events.
Randomized controlled trials also exposed the AFib risk. This would have been difficult to sort out in nonrandom observational studies.
Another underappreciated lesson is the notion that drugs, including supplements, can have off-target effects.
Consider the case of statin drugs. It is widely assumed that statins reduce cardiac events by lowering low-density lipoprotein cholesterol (LDL-C). Yet, statins became a mainstay not because of LDL-C lowering but because multiple trials found that this class of drugs reduced cardiac events without increasing adverse effects.
Omega-3 fatty acids reduce triglyceride levels, but this is not enough to adopt the use of these pills. The lack of consistent reduction in CV events and the off-target signal of AFib risk argue against routine use of fish-oil pills.
I will close with uncertainty. Though there is plausibility and multiple reasons to infer causality of marine omega-3s in increasing AFib risk, the effect size remains unknown.
In an editorial accompanying the recent meta-analysis, epidemiologist Michelle Samuel, MPH, PhD, and electrophysiologist Stanley Nattel, MD, cautioned readers on a technical but important point. It concerns the matter of competing risks, such as death, in the analysis of AFib risk, meaning that patients who died may have developed AFib had they lived. They provide a detailed explanation in the open access article, but the take-home is that the exact effect size is difficult to quantify without patient-level original data.
No matter. I find the signal of increased AFib risk an important one to use at the bedside.
Intermittent AFib has an unpredictable natural history. It often resolves as mysteriously as it arises. When patients take fish-oil supplements, I cite these studies, note the lack of CV protection, then I recommend stopping the pills.
This allows for one of the most important interventions in AFib care: time.
Dr. Mandrola is a clinical electrophysiologist with Baptist Medical Associates, Louisville, Ky. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Three surprising studies on exercise restriction and an exercise sweet spot
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
LIVE HCM: Surprising result No. 1
Rachel Lampert, MD, from Yale University, New Haven, Conn., presented results of the LIVE-HCM observational study of vigorous exercise in more than 1,600 patients with hypertrophic cardiomyopathy (40% female). The investigators aimed to determine whether engagement in vigorous exercise, including competitive sports, is associated with increased risk for life-threatening ventricular arrhythmia and/or mortality in patients with HCM.
Because of the myocardial disease, HCM comes with a risk for ventricular arrhythmia. Prevailing wisdom held that vigorous exercise in these patients would be hazardous. It was all expert opinion; there were no data. Now there are.
Dr. Lampert and colleagues recruited patients from 42 international HCM centers. Patients self-enrolled and the researchers created three groups based on self-reported levels of exercise – vigorous, moderate, and sedentary. The main comparison was between vigorous versus nonvigorous exercisers (including moderate and sedentary). The two groups were mostly matched on baseline characteristics and typical of patients with HCM.
The primary endpoint was a composite of death, resuscitated cardiac arrest, syncope likely caused by an arrhythmia, or an appropriate shock from an ICD.
The event rates were low in all groups and almost identical in vigorous versus nonvigorous exercisers. Sub-group analyses found no increased risk in HCM patients who identified as competitive athletes.
Dr. Lampert said these data “do not support universal restriction of vigorous exercise in patients with HCM.”
Return to play: Surprising result No. 2
Undergraduate student Katherine Martinez from Loyola University, Chicago, presented an observational analysis of 76 elite athletes with genetic heart disease who gained a return-to-play approval from four expert centers in the United States.
The three-step, return-to-play protocol from these specialized centers deserves emphasis. First was the initial evaluation, including two ECGs, 24-hour ECG monitor, echocardiography, and treadmill exercise testing. Second was a discussion between clinicians and patients regarding the athlete’s situation. The third step was to inform coaches and staff of the team and instruct athletes to obtain a personal AED, stay replenished with electrolytes, avoid QT-prolonging drugs, and continue with annual follow-up.
Slightly more than half of these patients had HCM and almost a third had long QT syndrome. Nearly one-third had an ICD implant and 22 were women.
Of the 76 athletes, 73 chose to return to play; however, 4 of these remained disqualified because of their team’s decision. Of the remaining 69, only 3 had one or more breakthrough cardiac events during 200 patient-years of follow-up.
These comprised one male Division I basketball player with HCM who had an ICD shock while moving furniture; another male Division 1 hockey player with long QT syndrome who was taking beta-blockers experienced syncope while coming off the bench and while cooking; and a third male professional hockey player with HCM, on beta-blockers, had syncope without exertion.
The authors concluded that when there was careful evaluation by experts and shared decision-making, a specific plan to return to sport can be put into place for the highest-level athletes.
Masters@Heart: Surprising result No. 3
Ruben De Bosscher MD, PhD, from KU Leuven (Belgium), presented the Masters@Heart study on behalf of a Belgian team of researchers. The question they asked was whether lifelong endurance exercise is associated with more coronary atherosclerosis than standard “normal” exercise levels.
That question brings up the paradox of exercise, which is that numerous observational studies find that exercise strongly associates with lower rates of cardiovascular events, but imaging studies also report high rates of coronary artery calcium in endurance athletes, especially in those who have run multiple marathons.
Masters@Heart investigators sought to explore this paradox by performing detailed coronary imaging in three groups – lifelong athletes, late-onset athletes (after age 30 years), and super-healthy controls. Through advertisements they obtained about 1,100 middle-aged male volunteers (mean age, 55 years). Of these, 605 men were selected at random to participate to reduce the chance of enrolling people who responded to the ads because of health concerns.
Investigators assigned those selected based on self-report of exercise. The control group was notable for their good health: they were free of any risk factors, took (almost) no meds, exercised regularly but not excessively (about 3 hours per week) and had a VO2 max of 122% of predicted.
The groups were well matched on baseline characteristics. Cycling predominated as the exercise of choice (this is a Belgian study after all). All patients had an extensive evaluation including coronary CT imaging.
European Heart Journal published the provocative results.
- Lifelong exercisers had a significantly higher CAC burden than controls, which confirms previous work.
- Lifelong exercisers had a higher percentage of multiple coronary plaques, plaques of at least 50%, and proximal plaques.
- There were no significant differences in the mixture of plaque types in the three groups. About two thirds of the plaques in each group were calcified and the remainder were deemed noncalcified or mixed.
- When looking only at noncalcified plaques, lifelong exercisers tended to have a higher prevalence of multiple plaques, plaques of at least 50%, and proximal plaques.
- So named “vulnerable” plaques were extremely infrequent in all three groups.
The authors concluded that lifelong endurance sport relative to a generic healthy lifestyle was not associated with more favorable coronary plaque composition.
Comments
Each of these three studies provided data where there was none. That is always a good thing.
The major theme from the first two studies is that expert opinion was too cautious. Doctors have long held the idea that patients with genetic heart disease, especially hypertrophic cardiomyopathy, are vulnerable, fragile even, when it comes to vigorous sport.
This new evidence upends this belief, as long as return to sport occurs in the setting of robust patient education and expert evaluation and surveillance.
Paternalism in prohibiting participation in sport because of genetic heart disease has joined the long list of medical reversals.
Masters@Heart provides a slightly different message. It finds that lifelong high-level exercise does not prevent coronary atherosclerosis in men. And, more provocatively, if replicated, might even show that long-term exposure to the biochemical, inflammatory, or hormonal effects of endurance training may actually be atherogenic. Like all good science, these findings raise more questions to explore in the realm of atherogenesis.
Two of the main limitations of the Belgian study was that the control arm was quite healthy; had the comparison arm been typical of sedentary controls in say, the Southeastern United States, the coronary lesions found in longtime exercisers may have looked more favorable. The more significant limitation is the lack of outcomes. Images of coronary arteries remain a surrogate marker. It’s possible that, like statins, higher levels of exercise may stabilize plaque and actually lower the risk for events.
The Belgian authors suggest – as many have – a J-curve of exercise benefits, wherein too little exercise is clearly bad, but too much exercise may also increase risk. In other words, for maximizing health, there may be a Goldilocks amount of exercise.
The problem with this idea comes in its pragmatic translation. The number of lifelong high-level, middle-aged endurance athletes that cite heart health reasons for their affliction is ... almost zero. Nearly everyone I have met in the endurance sport fraternity harbors no notion that racing a bike or running multiple marathons per year is a healthy endeavor.
Paternalism, therefore, would also fall in the realm of limiting lifelong exercise in addicted middle-aged athletes.
Via email, sports cardiologist Michael Emery, MD, reiterated the main immediate message from Masters@Heart: “Exercise does not make you immune from heart disease (which is a message a lot of athletes need to hear honestly).”
I for one cannot give up on endurance exercise. I won’t likely race anymore but I am like the lab rat who needs to run on the wheel. Whether this affects my coronary plaque burden matters not to me.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Taking cardiac pacing from boring to super cool
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.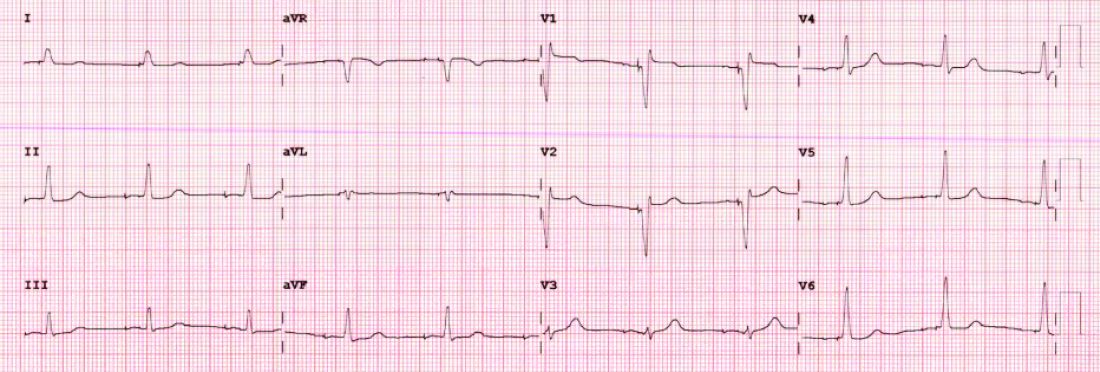
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.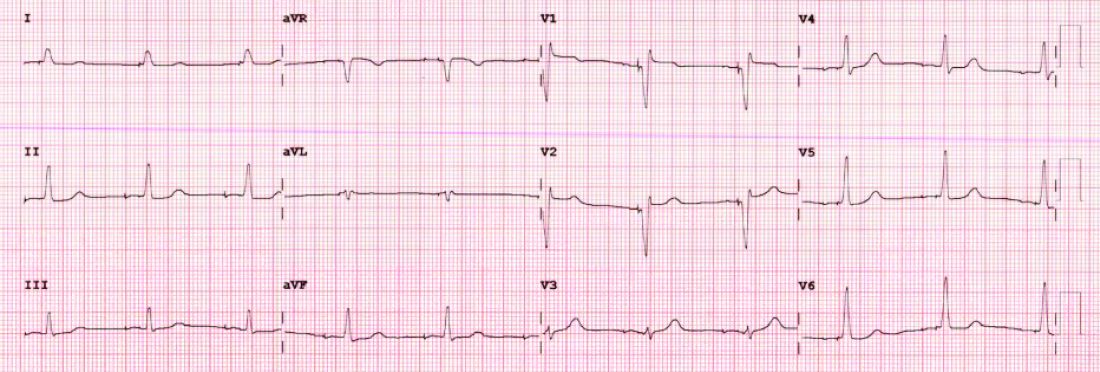
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.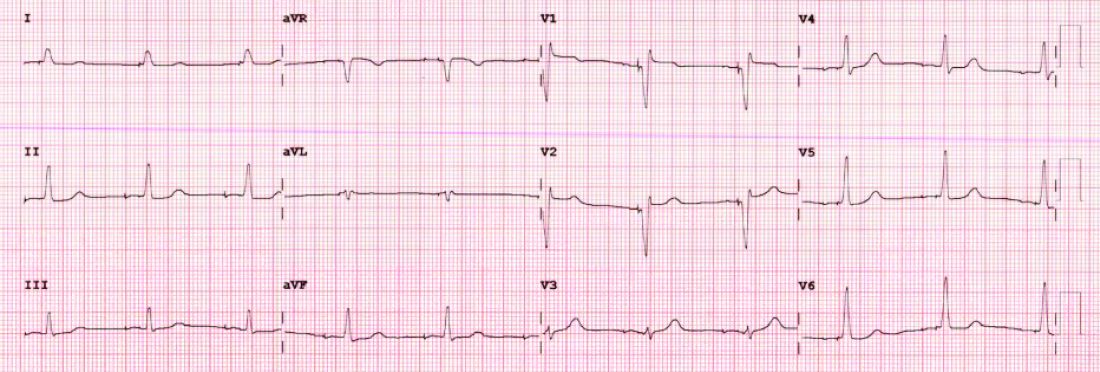
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Why is vitamin D hype so impervious to evidence?
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
This doc still supports NP/PA-led care ... with caveats
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.
Two years ago, I argued that independent care from nurse practitioners (NPs) and physician assistants (PAs) would not have ill effects on health outcomes. To the surprise of no one, NPs and PAs embraced the argument; physicians clobbered it.
My case had three pegs: One was that medicine isn’t rocket science and clinicians control a lot less than we think we do. The second peg was that technology levels the playing field of clinical care. High-sensitivity troponin assays, for instance, make missing MI a lot less likely. The third peg was empirical: Studies have found little difference in MD versus non–MD-led care. Looking back, I now see empiricism as the weakest part of the argument because the studies had so many limitations.
I update this viewpoint now because health care is increasingly delivered by NPs and PAs. And there are two concerning trends regarding NP education and experience. First is that nurses are turning to advanced practitioner training earlier in their careers – without gathering much bedside experience. And these training programs are increasingly likely to be online, with minimal hands-on clinical tutoring.
Education and experience pop in my head often. Not every day, but many days I think back to my lucky 7 years in Indiana learning under the supervision of master clinicians – at a time when trainees were allowed the leeway to make decisions ... and mistakes. Then, when I joined private practice, I continued to learn from experienced practitioners.
It would be foolish to argue that training and experience aren’t important.
But here’s the thing:
I will make three points: First, I will bolster two of my old arguments as to why we shouldn’t be worried about non-MD clinicians, then I will propose some ideas to increase confidence in NP and PA care.
Health care does not equal health
On the matter of how much clinicians affect outcomes, a recently published randomized controlled trial performed in India found that subsidizing insurance care led to increased utilization of hospital services but had no significant effect on health outcomes. This follows the RAND and Oregon Health Insurance studies in the United States, which largely reported similar results.
We should also not dismiss the fact that – despite the massive technology gains over the past half-century in digital health and artificial intelligence and increased use of quality measures, new drugs and procedures, and mega-medical centers – the average lifespan of Americans is flat to declining (in most ethnic and racial groups). Worse than no gains in longevity, perhaps, is that death from diseases like dementia and Parkinson’s disease are on the rise.
A neutral Martian would look down and wonder why all this health care hasn’t translated to longer and better lives. The causes of this paradox remain speculative, and are for another column, but the point remains that – on average – more health care is clearly not delivering more health. And if that is true, one may deduce that much of U.S. health care is marginal when it comes to affecting major outcomes.
It’s about the delta
Logos trumps pathos. Sure, my physician colleagues can tell scary anecdotes of bad outcomes caused by an inexperienced NP or PA. I would counter that by saying I have sat on our hospital’s peer review committee for 2 decades, including the era before NPs or PAs were practicing, and I have plenty of stories of physician errors. These include, of course, my own errors.
Logos: We must consider the difference between non–MD-led care and MD-led care.
My arguments from 2020 remain relevant today. Most medical problems are not engineering puzzles. Many, perhaps most, patients fall into an easy protocol – say, chest pain, dyspnea, or atrial fibrillation. With basic training, a motivated serious person quickly gains skill in recognizing and treating everyday problems.
And just 2 years on, technology further levels the playing field. Consider radiology in 2022 – it’s easy to take for granted the speed of the CT scan, the fidelity of the MRI, and the easy access to both in the U.S. hospital system. Less experienced clinicians have never had more tools to assist with diagnostics and therapeutics.
The expansion of team-based care has also mitigated the effects of inexperience. It took Americans longer than Canadians to figure out how helpful pharmacists could be. Pharmacists in my hospital now help us dose complicated medicines and protect us against prescribing errors.
Then there is the immediate access to online information. Gone are the days when you had to memorize long-QT syndromes. Book knowledge – that I spent years acquiring – now comes in seconds. The other day an NP corrected me. I asked, Are you sure? Boom, she took out her phone and showed me the evidence.
In sum, if it were even possible to measure the clinical competence of care from NP and PA versus physicians, there would be two bell-shaped curves with a tremendous amount of overlap. And that overlap would steadily increase as a given NP or PA gathered experience. (The NP in our electrophysiology division has more than 25 years’ experience in heart rhythm care, and it is common for colleagues to call her before one of us docs. Rightly so.)
Three basic proposals regarding NP and PA care
To ensure quality of care, I have three proposals.
It has always seemed strange to me that an NP or PA can flip from one field to another without a period of training. I can’t just change practice from electrophysiology to dermatology without doing a residency. But NPs and PAs can.
My first proposal would be that NPs and PAs spend a substantial period of training in a field before practice – a legit apprenticeship. The duration of this period is a matter of debate, but it ought to be standardized.
My second proposal is that, if physicians are required to pass certification exams, so should NPs. (PAs have an exam every 10 years.) The exam should be the same as (or very similar to) the physician exam, and it should be specific to their field of practice.
While I have argued (and still feel) that the American Board of Internal Medicine brand of certification is dubious, the fact remains that physicians must maintain proficiency in their field. Requiring NPs and PAs to do the same would help foster specialization. And while I can’t cite empirical evidence, specialization seems super-important. We have NPs at my hospital who have been in the same area for years, and they exude clinical competence.
Finally, I have come to believe that the best way for nearly any clinician to practice medicine is as part of a team. (The exception being primary care in rural areas where there are clinician shortages.)
On the matter of team care, I’ve practiced for a long time, but nearly every day I run situations by a colleague; often this person is an NP. The economist Friedrich Hayek proposed that dispersed knowledge always outpaces the wisdom of any individual. That notion pertains well to the increasing complexities and specialization of modern medical practice.
A person who commits to learning one area of medicine, enjoys helping people, asks often for help, and has the support of colleagues is set up to be a successful clinician – whether the letters after their name are APRN, PA, DO, or MD.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky. He did not report any relevant financial disclosures. A version of this article first appeared on Medscape.com.