User login
US Experience With Infliximab Biosimilars Suggests Need for More Development Incentives
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Light Therapy, Phototherapy, Photobiomodulation: New Ways to Heal With Light
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
A surprising therapy is showing promise for chronic pain, vision loss, and muscle recovery, among other conditions.
It’s not a pill, an injection, or surgery.
It’s light.
Yes, light. The thing that appears when you open the curtains, flip a switch, or strike a match.
Light illuminates our world and helps us see. Early human trials suggest it may help us heal in new ways as well.
“Phototherapy is still in its infancy,” said Mohab Ibrahim, MD, PhD, a professor of anesthesiology at the University of Arizona, Tucson, who studies the effects of light on chronic pain. “There are so many questions, a lot of things we do not understand yet. But that’s where it gets interesting. What we can conclude is that different colors of light can influence different biological functions.”
This growing field goes by several names. Light therapy. Phototherapy. Photobiomodulation.
It leverages known effects of light on human health — such as skin exposure to ultraviolet light producing vitamin D or blue light’s power to regulate human body clocks — to take light as medicine in surprising new directions.
New Science, Old Idea
The science is young, but the concept of using light to restore health is thousands of years old.
Hippocrates prescribed sunbathing to patients at his medical center on the Greek island of Kos in 400 BC. Florence Nightingale promoted sunshine, along with fresh air, as prerequisites for recovery in hospitals during the Civil War. A Danish doctor, Niels Finsen, won the Nobel Prize in 1903 for developing ultraviolet lamps to treat a tuberculosis-related skin condition. And worried parents of the 1930s sat their babies in front of mercury arc lamps, bought at the drugstore, to discourage rickets.
Today, light therapy is widely used in medicine for newborn jaundice, psoriasis, and seasonal affective disorder and in light-activated treatments for cancers of the esophagus and lungs, as well as for actinic keratosis, a skin condition that can lead to cancer.
But researchers are finding that light may be capable of far more, particularly in conditions with few treatment options or where available drugs have unwanted side effects.
How Red Light Could Restore Vision
When 100 midlife and older adults, aged 53-91, with the dry form of age-related macular degeneration (AMD) were treated with an experimental red-light therapy or a sham therapy, the light treatment group showed signs of improved vision, as measured on a standard eye chart.
Volunteers received the therapy three times a week for 3-5 weeks, every 4 months for 2 years. By the study’s end, 67% of those treated with light could read an additional five letters on the chart, and 20% could read 10 or more. About 7% developed geographic atrophy — the most advanced, vision-threatening stage of dry AMD — compared with 24% in the sham group.
The study, called LIGHTSITE III, was conducted at 10 ophthalmology centers across the United States. The device they used — the Valeda Light Delivery System from medical device company LumiThera — is available in Europe and now being reviewed by the Food and Drug Administration (FDA).
Exposure to red light at the wavelengths used in the study likely revitalizes failing mitochondria — the power plants inside cells — so they produce more energy, the researchers say.
“This is the first therapy for dry AMD that’s actually shown a benefit in improving vision,” said study coauthor Richard Rosen, MD, chair of ophthalmology at the Icahn School of Medicine at Mount Sinai and chief of Retinal Services at the New York Eye and Ear Infirmary in New York City. “Supplements called AREDS can reduce progression, and in wet AMD we can improve vision loss with injections. But in dry AMD, none of the treatments studied in the past have improved it.”
AMD develops when the eyes can’t break down natural by-products, which glom together as clumps of protein called drusen. Drusen can lodge under the retina, eventually damaging tissue.
“Retinal epithelial cells, a single layer of cells that cares for the photoreceptors in the eyes, are there for life,” Dr. Rosen said. “They have a tremendous capacity to repair themselves, but things [such as aging and smoking] get in the way.”
“I’m proposing,” Dr. Rosen said, “that by boosting energy levels in cells [with red light], we’re improving normal repair mechanisms.”
Lab studies support this idea.
In a 2017 mouse study from the University College London Institute of Ophthalmology in England, retinal function improved by 25% in old mice exposed to red light. And a 2019 study from the Ophthalmological Research Foundation, Oviedo, Spain, found that exposure to blue light harmed the mitochondria in retina cells, while red light somewhat counteracted the losses.
If cleared by the FDA — which the company anticipated could happen in 2024 — LumiThera’s light delivery device will likely be most useful in the beginning stages of dry AMD, Dr. Rosen said. “I think treatment of early dry AMD will be huge.”
Eventually, light therapy may also be valuable in treating or managing glaucoma and diabetic retinopathy.
For now, Dr. Rosen recommended that clinicians and consumers with AMD skip over-the-counter (OTC) red-light therapy devices currently on the market.
“We don’t know what kind of light the devices produce,” he said. “The wavelengths can vary. The eyes are delicate. Experimenting on your own may be hazardous to your vision.”
Green Light for Pain Relief
On his way to the pharmacy to pick up pain relievers for a headache, Dr. Ibrahim passed Gene C. Reid Park in Tucson. Recalling how his brother eased headaches by sitting in his backyard, Dr. Ibrahim pulled over.
“Reid Park is probably one of the greenest areas of Tucson,” said Dr. Ibrahim, who also serves as medical director of the Comprehensive Center for Pain & Addiction at Banner-University Medical Center Phoenix in Arizona. “I spent a half hour or 40 minutes there, and my headache felt better.”
Being outdoors in a green space may be soothing for lots of reasons, like the quiet or the fresh air. But there’s also sunlight reflected off and shining through greenery. The experience inspired Dr. Ibrahim to take a closer look at the effects of green light on chronic pain.
In his 2021 study of 29 people with migraines, participants reported that, after daily exposure to green light for 10 weeks, the number of days per month when they had headaches fell from 7.9 to 2.4 for those who had episodic migraines and from 22.3 to 9.4 for those with chronic migraines. In another 2021 study, 21 people with fibromyalgia who had green light therapy for 10 weeks said their average, self-reported pain intensity fell from 8.4 to 4.9 on a 10-point scale used at the University of Arizona’s pain clinic.
Volunteers in both studies got their light therapy at home, switching on green LED lights while they listened to music, read a book, relaxed, or exercised for 1 or 2 hours daily. The lights were within their field of vision, but they did not look directly at them.
Dr. Ibrahim now has funding from the Department of Defense and Department of Veterans Affairs to find out why green light alters pain perception.
“What we know is that the visual system is connected to certain areas of the brain that also modulate pain,” he said. “We are trying to understand the connection.”
Padma Gulur, MD, a professor of anesthesiology and population health and director of Pain Management Strategy and Opioid Surveillance at Duke University, Durham, North Carolina, saw similar results in a 2023 study of 45 people with fibromyalgia. But instead of using a light source, volunteers wore glasses with clear, green, or blue lenses for 4 hours a day.
After 2 weeks, 33% in the green lens group reduced their use of opioids by 10% or more, compared with 11% in the blue lens group and 8% who wore clear lenses. Previous studies have found green light affects levels of the feel-good brain chemical serotonin and stimulates the body’s own opioid system, the authors noted.
“Green light helps your body control and reduce pain,” Dr. Gulur said. It “seems to help with pain relief by affecting the body’s natural pain management system. This effect appears to play a crucial role in antinociception — reducing the sensation of pain; antiallodynia — preventing normal, nonpainful stimuli from causing pain; and antihyperalgesia — reducing heightened sensitivity to pain.”
Light therapy could help pain patients reduce their dose of opioids or even forgo the drugs altogether, Dr. Gulur said. “It is our hope this will become a useful adjuvant therapy to manage pain.”
In the University of Arizona studies, some patients on green-light therapy stopped their medications completely. Even if they didn’t, other benefits appeared. “They had improved quality of life, decreased depression and anxiety, and improved sleep,” Dr. Ibrahim said.
But not just any green light or green-tinted glasses will work, both researchers said. “We have found there are specific frequencies of green light that give this benefit,” Dr. Gulur said. “OTC products may not be helpful for that reason.”
While Dr. Ibrahim said it could be possible for healthcare practitioners and consumers to consult his studies and put together an inexpensive green-light device at home while carefully following the protocol participants used in the studies , it would first be a good idea for patients to talk with their family doctor or a pain specialist.
“A headache is not always just a headache,” Dr. Ibrahim said. “It could be some other abnormality that needs diagnosis and treatment. If you have long-lasting pain or pain that’s getting worse, it’s always better to discuss it with your physician.”
Helping Muscles Recover With Red Light
Intense exercise — whether it’s a sprint at the end of a morning run, an extra set of biceps curls, or a weekend of all-day DIY home improvement projects — can temporarily damage muscle, causing soreness, inflammation, and even swelling. Phototherapy with red and near-infrared light is widely used by sports trainers, physical therapists, and athletes to aid in recovery. It may even work better than a trendy plunge in an ice bath, according to a 2019 Texas State University review.
But how does it work? Jamie Ghigiarelli, PhD, professor of Allied Health & Kinesiology at Hofstra University in Hempstead, New York, looked closely at signs of inflammation and muscle damage in 12 athletes to find out.
Study participants overtaxed their muscles with rounds of chin-ups, high-speed sprints, and repeated bench presses. Afterward, they relaxed in a full-body red-light therapy bed or in a similar bed without lights.
The results, published in 2020, showed that blood levels of creatine kinase — an enzyme that’s elevated by muscle damage — were 18% lower 1-3 days after exercising for the light-bed group than for the control group.
“Photobiomodulation seems to help with muscle recovery,” Dr. Ghigiarelli said.
Red light at wavelengths from 650 to 820 nm can enter muscle cells, where it is absorbed by mitochondria and boosts their energy production, he said. At the time of his research, some exercise science researchers and athletes thought using light therapy before an event might also increase athletic performance, but according to Dr. Ghigiarelli, that use has not panned out.
Handheld red light and near-infrared light devices for muscle recovery are widely available, but it’s important to do your homework before buying one.
“You want to choose a device with the right energy production — the right wavelength of light, the right power — to be safe and effective,” he said.
For details, he recommends consulting a 2019 paper in The Brazilian Journal of Physical Therapy called “Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: Current evidence and future directions.”
The paper, from the Laboratory of Phototherapy and Innovative Technologies in Health at the Universidade Nove de Julho in Sao Paulo, Brazil, recommends that for small muscle groups like the biceps or triceps, use red-light lasers or LED devices with a wavelength of 640 nm for red light or 950 nm for infrared light, at a power of 50-200 mW per diode for single-probe device types, at a dose of 20-60 J, given 5-10 minutes after exercise.
A version of this article appeared on Medscape.com.
Management, Evaluation of Chronic Itch in Older Adults
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024
Advantages of a Pediatric Rheumatology/Dermatology Clinic Evaluated
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Study Finds Differences in Side Effect Profiles With Two Oral Psoriasis Therapies
TOPLINE:
, according to a retrospective comparison using US Food and Drug Administration (FDA) data.
METHODOLOGY:
- To evaluate the adverse events associated with apremilast, an oral phosphodiesterase-4 (PDE4) inhibitor, and deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor, data were drawn from the FDA’s Adverse Event Reporting System database.
- The Medex_UIMA_1.8.3 system was used to standardize drug names, and MedDRA terminology was used to encode, categorize, and localize signals.
- AE event signals were grouped by skin and subcutaneous tissue disorders, gastrointestinal disorders, infections and infestations, and nervous system disorders.
TAKEAWAY:
- There were 95,734 AE reports for apremilast and 760 AE reports for deucravacitinib, and AEs were found to be significant over time.
- The more common cutaneous AEs were psoriasis recurrence and acne (associated with apremilast) and skin burning and erythema (associated with deucravacitinib).
- The more common gastrointestinal AEs were diarrhea and nausea (apremilast) and mouth ulceration (deucravacitinib).
- Deucravacitinib-related pruritus and rash, as well as apremilast-related tension headache, were more common in women than men; deucravacitinib-related skin burning was more common in men.
IN PRACTICE:
The results “can help the doctors to choose the right treatment options based on the baseline characteristics of different patients,” said Yuanyuan Xu, a graduate student in the Department of Dermatology, Sichuan University, Chengdu, China.
SOURCE:
Mr. Xu presented the study as a poster at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2024 annual meeting.
LIMITATIONS:
The study was retrospective and cannot prove causality, and there were far fewer AE reports related to deucravacitinib, likely because the drug was introduced more recently.
DISCLOSURES:
The study received no funding, and the authors had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a retrospective comparison using US Food and Drug Administration (FDA) data.
METHODOLOGY:
- To evaluate the adverse events associated with apremilast, an oral phosphodiesterase-4 (PDE4) inhibitor, and deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor, data were drawn from the FDA’s Adverse Event Reporting System database.
- The Medex_UIMA_1.8.3 system was used to standardize drug names, and MedDRA terminology was used to encode, categorize, and localize signals.
- AE event signals were grouped by skin and subcutaneous tissue disorders, gastrointestinal disorders, infections and infestations, and nervous system disorders.
TAKEAWAY:
- There were 95,734 AE reports for apremilast and 760 AE reports for deucravacitinib, and AEs were found to be significant over time.
- The more common cutaneous AEs were psoriasis recurrence and acne (associated with apremilast) and skin burning and erythema (associated with deucravacitinib).
- The more common gastrointestinal AEs were diarrhea and nausea (apremilast) and mouth ulceration (deucravacitinib).
- Deucravacitinib-related pruritus and rash, as well as apremilast-related tension headache, were more common in women than men; deucravacitinib-related skin burning was more common in men.
IN PRACTICE:
The results “can help the doctors to choose the right treatment options based on the baseline characteristics of different patients,” said Yuanyuan Xu, a graduate student in the Department of Dermatology, Sichuan University, Chengdu, China.
SOURCE:
Mr. Xu presented the study as a poster at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2024 annual meeting.
LIMITATIONS:
The study was retrospective and cannot prove causality, and there were far fewer AE reports related to deucravacitinib, likely because the drug was introduced more recently.
DISCLOSURES:
The study received no funding, and the authors had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a retrospective comparison using US Food and Drug Administration (FDA) data.
METHODOLOGY:
- To evaluate the adverse events associated with apremilast, an oral phosphodiesterase-4 (PDE4) inhibitor, and deucravacitinib, an oral tyrosine kinase 2 (TYK2) inhibitor, data were drawn from the FDA’s Adverse Event Reporting System database.
- The Medex_UIMA_1.8.3 system was used to standardize drug names, and MedDRA terminology was used to encode, categorize, and localize signals.
- AE event signals were grouped by skin and subcutaneous tissue disorders, gastrointestinal disorders, infections and infestations, and nervous system disorders.
TAKEAWAY:
- There were 95,734 AE reports for apremilast and 760 AE reports for deucravacitinib, and AEs were found to be significant over time.
- The more common cutaneous AEs were psoriasis recurrence and acne (associated with apremilast) and skin burning and erythema (associated with deucravacitinib).
- The more common gastrointestinal AEs were diarrhea and nausea (apremilast) and mouth ulceration (deucravacitinib).
- Deucravacitinib-related pruritus and rash, as well as apremilast-related tension headache, were more common in women than men; deucravacitinib-related skin burning was more common in men.
IN PRACTICE:
The results “can help the doctors to choose the right treatment options based on the baseline characteristics of different patients,” said Yuanyuan Xu, a graduate student in the Department of Dermatology, Sichuan University, Chengdu, China.
SOURCE:
Mr. Xu presented the study as a poster at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2024 annual meeting.
LIMITATIONS:
The study was retrospective and cannot prove causality, and there were far fewer AE reports related to deucravacitinib, likely because the drug was introduced more recently.
DISCLOSURES:
The study received no funding, and the authors had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Risk of MACE Comparable Among Biologic Classes for Psoriasis, PsA
TOPLINE:
a database analysis finds.
METHODOLOGY:
- Data from the TriNetX health records database included 32,758 patients treated with TNF inhibitors (TNFi, 62.9%), interleukin-17 inhibitors (IL-17i, 15.4%), IL-23i (10.7%), and IL-12i/IL-23i (10.7%).
- The researchers calculated time-dependent risk for MACE using multinomial Cox proportional hazard ratios. The reference was TNFi exposure.
- Subset analyses compared MACE in patients with and without existing cardiovascular disease.
TAKEAWAY:
- Compared with TNFi use, there was no difference in the incidence of MACE events in the IL-17i, IL-23i, or IL-12i/IL-23i group.
- There were also no significant differences between biologic groups in the incidence of congestive heart failure, myocardial infarction, or cerebral vascular accident/stroke.
IN PRACTICE:
Despite some concern about increased risk for MACE with TNFi use, this study suggests no special risk for patients with psoriasis or PsA associated with TNFi vs other biologics. “Given our results, as it pertains to MACE, prescribers shouldn’t favor any one biologic class over another,” said lead investigator Shikha Singla, MD, medical director of the Psoriatic Arthritis Program at Medical College of Wisconsin in Milwaukee, Wisconsin.
SOURCE:
Bonit Gill, MD, a second-year fellow at Medical College of Wisconsin, presented the study as a poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
LIMITATIONS:
The study’s retrospective nature makes it impossible to prove causation and the patients included in the study were from Wisconsin, which may limit generalizability.
DISCLOSURES:
Dr. Gill had no relevant financial disclosures. Other study authors participated in trials or consulted for AbbVie, AstraZeneca, Novartis, Eli Lilly, Janssen, and UCB.
A version of this article first appeared on Medscape.com.
TOPLINE:
a database analysis finds.
METHODOLOGY:
- Data from the TriNetX health records database included 32,758 patients treated with TNF inhibitors (TNFi, 62.9%), interleukin-17 inhibitors (IL-17i, 15.4%), IL-23i (10.7%), and IL-12i/IL-23i (10.7%).
- The researchers calculated time-dependent risk for MACE using multinomial Cox proportional hazard ratios. The reference was TNFi exposure.
- Subset analyses compared MACE in patients with and without existing cardiovascular disease.
TAKEAWAY:
- Compared with TNFi use, there was no difference in the incidence of MACE events in the IL-17i, IL-23i, or IL-12i/IL-23i group.
- There were also no significant differences between biologic groups in the incidence of congestive heart failure, myocardial infarction, or cerebral vascular accident/stroke.
IN PRACTICE:
Despite some concern about increased risk for MACE with TNFi use, this study suggests no special risk for patients with psoriasis or PsA associated with TNFi vs other biologics. “Given our results, as it pertains to MACE, prescribers shouldn’t favor any one biologic class over another,” said lead investigator Shikha Singla, MD, medical director of the Psoriatic Arthritis Program at Medical College of Wisconsin in Milwaukee, Wisconsin.
SOURCE:
Bonit Gill, MD, a second-year fellow at Medical College of Wisconsin, presented the study as a poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
LIMITATIONS:
The study’s retrospective nature makes it impossible to prove causation and the patients included in the study were from Wisconsin, which may limit generalizability.
DISCLOSURES:
Dr. Gill had no relevant financial disclosures. Other study authors participated in trials or consulted for AbbVie, AstraZeneca, Novartis, Eli Lilly, Janssen, and UCB.
A version of this article first appeared on Medscape.com.
TOPLINE:
a database analysis finds.
METHODOLOGY:
- Data from the TriNetX health records database included 32,758 patients treated with TNF inhibitors (TNFi, 62.9%), interleukin-17 inhibitors (IL-17i, 15.4%), IL-23i (10.7%), and IL-12i/IL-23i (10.7%).
- The researchers calculated time-dependent risk for MACE using multinomial Cox proportional hazard ratios. The reference was TNFi exposure.
- Subset analyses compared MACE in patients with and without existing cardiovascular disease.
TAKEAWAY:
- Compared with TNFi use, there was no difference in the incidence of MACE events in the IL-17i, IL-23i, or IL-12i/IL-23i group.
- There were also no significant differences between biologic groups in the incidence of congestive heart failure, myocardial infarction, or cerebral vascular accident/stroke.
IN PRACTICE:
Despite some concern about increased risk for MACE with TNFi use, this study suggests no special risk for patients with psoriasis or PsA associated with TNFi vs other biologics. “Given our results, as it pertains to MACE, prescribers shouldn’t favor any one biologic class over another,” said lead investigator Shikha Singla, MD, medical director of the Psoriatic Arthritis Program at Medical College of Wisconsin in Milwaukee, Wisconsin.
SOURCE:
Bonit Gill, MD, a second-year fellow at Medical College of Wisconsin, presented the study as a poster at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
LIMITATIONS:
The study’s retrospective nature makes it impossible to prove causation and the patients included in the study were from Wisconsin, which may limit generalizability.
DISCLOSURES:
Dr. Gill had no relevant financial disclosures. Other study authors participated in trials or consulted for AbbVie, AstraZeneca, Novartis, Eli Lilly, Janssen, and UCB.
A version of this article first appeared on Medscape.com.
Mysteries Persist About Tissue Resident Memory T Cells in Psoriasis
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
FROM GRAPPA 2024
Debate: Should Dermatologists or Rheumatologists Manage Musculoskeletal Symptoms in Patients With Psoriasis?
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
FROM GRAPPA 2024
Pyzchiva Receives FDA Approval as Third Ustekinumab Biosimilar
The Food and Drug Administration has approved ustekinumab-ttwe (Pyzchiva) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions.
In addition, the agency “provisionally determined” that the medication would be interchangeable with the reference product but that designation would not take hold until the interchangeability exclusivity period for the first approved biosimilar ustekinumab-auub (Wezlana) expires, according to a press release. This designation would, depending on state law, allow a pharmacist to substitute the biosimilar for the reference product without involving the prescribing clinician. It’s unclear when ustekinumab-auub’s interchangeability exclusivity ends.
Ustekinumab-ttwe, a human interleukin (IL)-12 and IL-23 antagonist, is indicated for the treatment of:
- Moderate to severe plaque psoriasis in adults and pediatric patients aged 6 years or older who are candidates for phototherapy or systemic therapy
- Active psoriatic arthritis in adults and pediatric patients aged 6 years or older with moderately to severely active Crohn’s disease or ulcerative colitis
It is administered via subcutaneous injection in 45 mg/0.5 mL and 90 mg/mL prefilled syringes or via intravenous infusion in 130 mg/26 mL (5 mg/mL) single-dose vial.
Developed by Samsung Bioepis, ustekinumab-ttwe will be commercialized by Sandoz in the United States. Besides ustekinumab-auub, the other ustekinumab biosimilar is ustekinumab-aekn (Selarsdi).
Ustekinumab-ttwe is expected to launch in February 2025 “in accordance with the settlement and license agreement with Janssen Biotech,” which manufacturers the reference product, Sandoz said. The other approved ustekinumab biosimilars will launch within a similar time frame.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved ustekinumab-ttwe (Pyzchiva) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions.
In addition, the agency “provisionally determined” that the medication would be interchangeable with the reference product but that designation would not take hold until the interchangeability exclusivity period for the first approved biosimilar ustekinumab-auub (Wezlana) expires, according to a press release. This designation would, depending on state law, allow a pharmacist to substitute the biosimilar for the reference product without involving the prescribing clinician. It’s unclear when ustekinumab-auub’s interchangeability exclusivity ends.
Ustekinumab-ttwe, a human interleukin (IL)-12 and IL-23 antagonist, is indicated for the treatment of:
- Moderate to severe plaque psoriasis in adults and pediatric patients aged 6 years or older who are candidates for phototherapy or systemic therapy
- Active psoriatic arthritis in adults and pediatric patients aged 6 years or older with moderately to severely active Crohn’s disease or ulcerative colitis
It is administered via subcutaneous injection in 45 mg/0.5 mL and 90 mg/mL prefilled syringes or via intravenous infusion in 130 mg/26 mL (5 mg/mL) single-dose vial.
Developed by Samsung Bioepis, ustekinumab-ttwe will be commercialized by Sandoz in the United States. Besides ustekinumab-auub, the other ustekinumab biosimilar is ustekinumab-aekn (Selarsdi).
Ustekinumab-ttwe is expected to launch in February 2025 “in accordance with the settlement and license agreement with Janssen Biotech,” which manufacturers the reference product, Sandoz said. The other approved ustekinumab biosimilars will launch within a similar time frame.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved ustekinumab-ttwe (Pyzchiva) as a biosimilar to ustekinumab (Stelara) for the treatment of multiple inflammatory conditions.
In addition, the agency “provisionally determined” that the medication would be interchangeable with the reference product but that designation would not take hold until the interchangeability exclusivity period for the first approved biosimilar ustekinumab-auub (Wezlana) expires, according to a press release. This designation would, depending on state law, allow a pharmacist to substitute the biosimilar for the reference product without involving the prescribing clinician. It’s unclear when ustekinumab-auub’s interchangeability exclusivity ends.
Ustekinumab-ttwe, a human interleukin (IL)-12 and IL-23 antagonist, is indicated for the treatment of:
- Moderate to severe plaque psoriasis in adults and pediatric patients aged 6 years or older who are candidates for phototherapy or systemic therapy
- Active psoriatic arthritis in adults and pediatric patients aged 6 years or older with moderately to severely active Crohn’s disease or ulcerative colitis
It is administered via subcutaneous injection in 45 mg/0.5 mL and 90 mg/mL prefilled syringes or via intravenous infusion in 130 mg/26 mL (5 mg/mL) single-dose vial.
Developed by Samsung Bioepis, ustekinumab-ttwe will be commercialized by Sandoz in the United States. Besides ustekinumab-auub, the other ustekinumab biosimilar is ustekinumab-aekn (Selarsdi).
Ustekinumab-ttwe is expected to launch in February 2025 “in accordance with the settlement and license agreement with Janssen Biotech,” which manufacturers the reference product, Sandoz said. The other approved ustekinumab biosimilars will launch within a similar time frame.
A version of this article appeared on Medscape.com.
Need a Wood Lamp Alternative? Grab Your Smartphone
Practice Gap
The Wood lamp commonly is used as a diagnostic tool for pigmentary skin conditions (eg, vitiligo) or skin conditions that exhibit fluorescence (eg, erythrasma).1 Recently, its diagnostic efficacy has extended to scabies, in which it unveils a distinctive wavy, bluish-white, linear fluorescence upon illumination.2
Functionally, the Wood lamp operates by subjecting phosphors to UV light within the wavelength range of 320 to 400 nm, inducing fluorescence in substances such as collagen and elastin. In the context of vitiligo, this process manifests as a preferential chalk white fluorescence in areas lacking melanin.1
Despite its demonstrated effectiveness, the Wood lamp is not without limitations. It comes with a notable financial investment ranging from $70 to $500, requires periodic maintenance such as light bulb replacements, and can be unwieldy.3 Furthermore, its reliance on a power source poses a challenge in settings where immediate access to convenient power outlets is limited, such as inpatient and rural dermatology clinics. These limitations underscore the need for alternative solutions and innovations to address challenges and ensure accessibility in diverse health care environments.
The Tools
Free smartphone applications (apps), such as Ultraviolet Light-UV Lamp by AppBrain or Blacklight UV Light Simulator by That Smile, can simulate UV light and functionally serve as a Wood lamp.
The Technique
UV light apps use LED or organic LED screen pixels to emit a blue light equivalent at 467 nm.4 Although these apps are not designed specifically for dermatologic uses, they are mostly free, widely available for Android and iPhone users, and portable. Importantly, they can demonstrate good performance in visualizing vitiligo, as shown in Figure 1—albeit perhaps not reaching the same level as the Wood lamp (Figure 2).
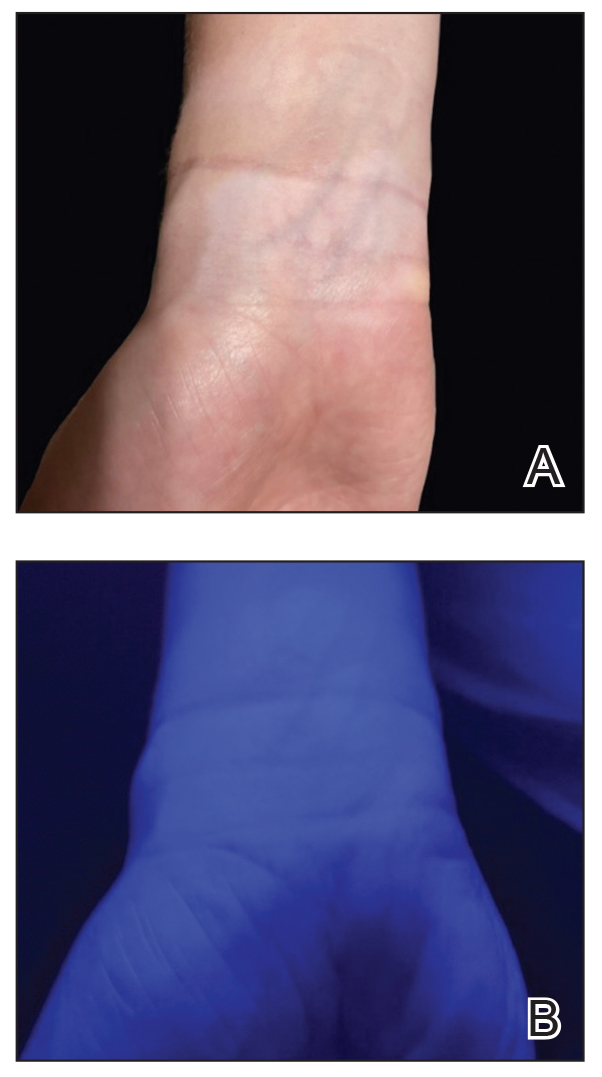
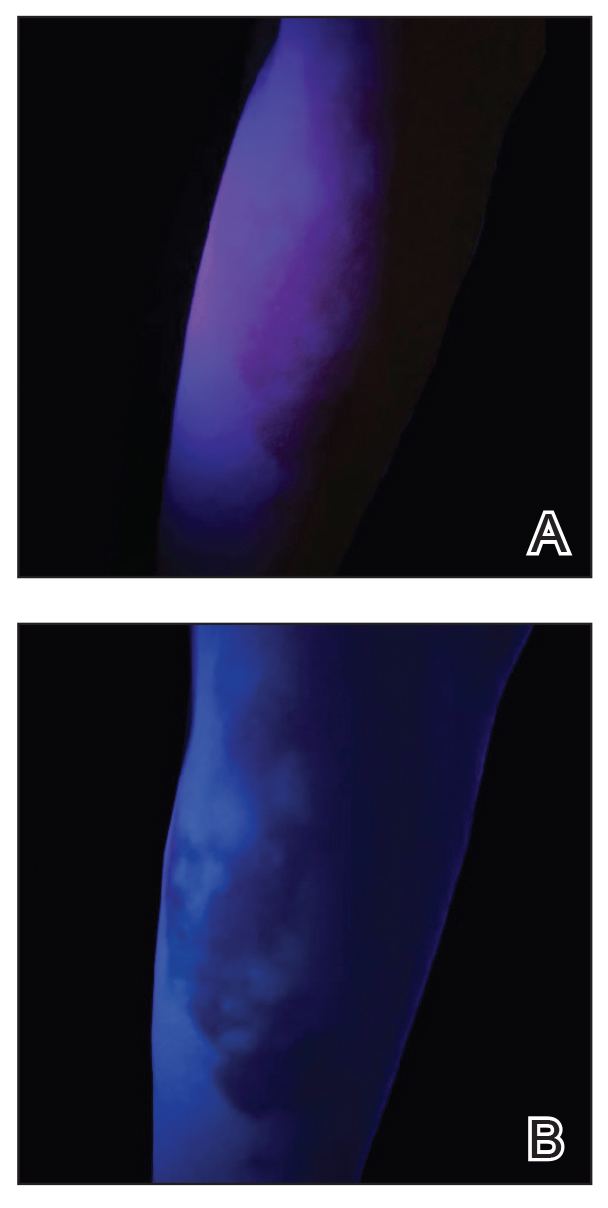
Because these UV light apps are not regulated and their efficacy for medical use has not been firmly established, the Wood lamp remains the gold standard. Therefore, we propose the use of UV light apps in situations when a Wood lamp is not available or convenient, such as in rural, inpatient, or international health care settings.
Practice Implications
Exploring and adopting these free alternatives can contribute to improved accessibility and diagnostic capabilities in diverse health care environments, particularly for communities facing financial constraints. Continued research and validation of these apps in clinical settings will be essential to establish their reliability and effectiveness in enhancing diagnostic practices.
- Dyer JM, Foy VM. Revealing the unseen: a review of Wood’s lamp in dermatology. J Clin Aesthet Dermatol. 2022;15:25-30.
- Scanni G. Facilitations in the clinical diagnosis of human scabies through the use of ultraviolet light (UV-scab scanning): a case-series study. Trop Med Infect Dis. 2022;7:422. doi:10.3390/tropicalmed7120422
- USA Medical and Surgical Supplies. Top 9 medical diagnostic applications for a Woods lamp. February 26, 2019. Accessed May 20, 2024.
- Huang Y, Hsiang E-L, Deng M-Y, et al. Mini-led, micro-led and OLED displays: present status and future perspectives. Light Sci Appl. 2020;9:105. doi:10.1038/s41377-020-0341-9
Practice Gap
The Wood lamp commonly is used as a diagnostic tool for pigmentary skin conditions (eg, vitiligo) or skin conditions that exhibit fluorescence (eg, erythrasma).1 Recently, its diagnostic efficacy has extended to scabies, in which it unveils a distinctive wavy, bluish-white, linear fluorescence upon illumination.2
Functionally, the Wood lamp operates by subjecting phosphors to UV light within the wavelength range of 320 to 400 nm, inducing fluorescence in substances such as collagen and elastin. In the context of vitiligo, this process manifests as a preferential chalk white fluorescence in areas lacking melanin.1
Despite its demonstrated effectiveness, the Wood lamp is not without limitations. It comes with a notable financial investment ranging from $70 to $500, requires periodic maintenance such as light bulb replacements, and can be unwieldy.3 Furthermore, its reliance on a power source poses a challenge in settings where immediate access to convenient power outlets is limited, such as inpatient and rural dermatology clinics. These limitations underscore the need for alternative solutions and innovations to address challenges and ensure accessibility in diverse health care environments.
The Tools
Free smartphone applications (apps), such as Ultraviolet Light-UV Lamp by AppBrain or Blacklight UV Light Simulator by That Smile, can simulate UV light and functionally serve as a Wood lamp.
The Technique
UV light apps use LED or organic LED screen pixels to emit a blue light equivalent at 467 nm.4 Although these apps are not designed specifically for dermatologic uses, they are mostly free, widely available for Android and iPhone users, and portable. Importantly, they can demonstrate good performance in visualizing vitiligo, as shown in Figure 1—albeit perhaps not reaching the same level as the Wood lamp (Figure 2).
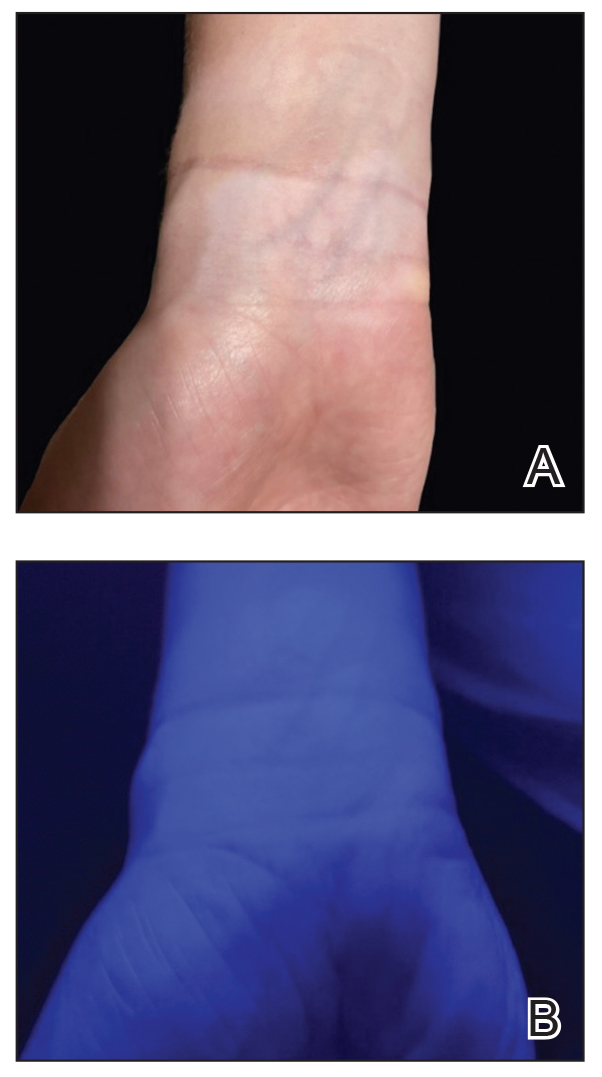
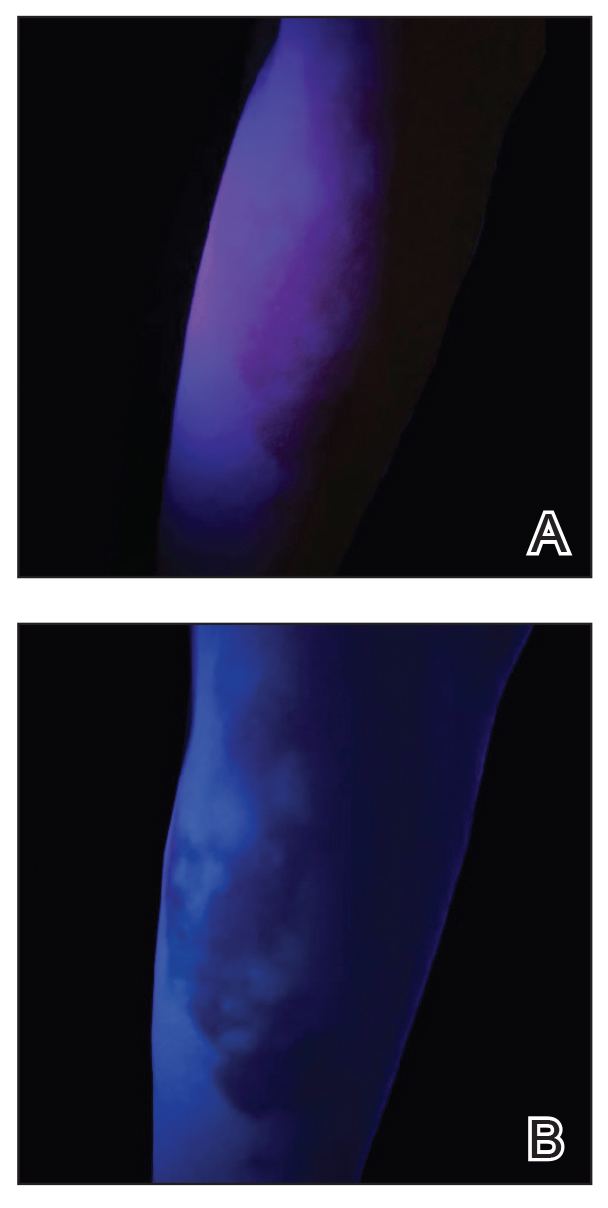
Because these UV light apps are not regulated and their efficacy for medical use has not been firmly established, the Wood lamp remains the gold standard. Therefore, we propose the use of UV light apps in situations when a Wood lamp is not available or convenient, such as in rural, inpatient, or international health care settings.
Practice Implications
Exploring and adopting these free alternatives can contribute to improved accessibility and diagnostic capabilities in diverse health care environments, particularly for communities facing financial constraints. Continued research and validation of these apps in clinical settings will be essential to establish their reliability and effectiveness in enhancing diagnostic practices.
Practice Gap
The Wood lamp commonly is used as a diagnostic tool for pigmentary skin conditions (eg, vitiligo) or skin conditions that exhibit fluorescence (eg, erythrasma).1 Recently, its diagnostic efficacy has extended to scabies, in which it unveils a distinctive wavy, bluish-white, linear fluorescence upon illumination.2
Functionally, the Wood lamp operates by subjecting phosphors to UV light within the wavelength range of 320 to 400 nm, inducing fluorescence in substances such as collagen and elastin. In the context of vitiligo, this process manifests as a preferential chalk white fluorescence in areas lacking melanin.1
Despite its demonstrated effectiveness, the Wood lamp is not without limitations. It comes with a notable financial investment ranging from $70 to $500, requires periodic maintenance such as light bulb replacements, and can be unwieldy.3 Furthermore, its reliance on a power source poses a challenge in settings where immediate access to convenient power outlets is limited, such as inpatient and rural dermatology clinics. These limitations underscore the need for alternative solutions and innovations to address challenges and ensure accessibility in diverse health care environments.
The Tools
Free smartphone applications (apps), such as Ultraviolet Light-UV Lamp by AppBrain or Blacklight UV Light Simulator by That Smile, can simulate UV light and functionally serve as a Wood lamp.
The Technique
UV light apps use LED or organic LED screen pixels to emit a blue light equivalent at 467 nm.4 Although these apps are not designed specifically for dermatologic uses, they are mostly free, widely available for Android and iPhone users, and portable. Importantly, they can demonstrate good performance in visualizing vitiligo, as shown in Figure 1—albeit perhaps not reaching the same level as the Wood lamp (Figure 2).
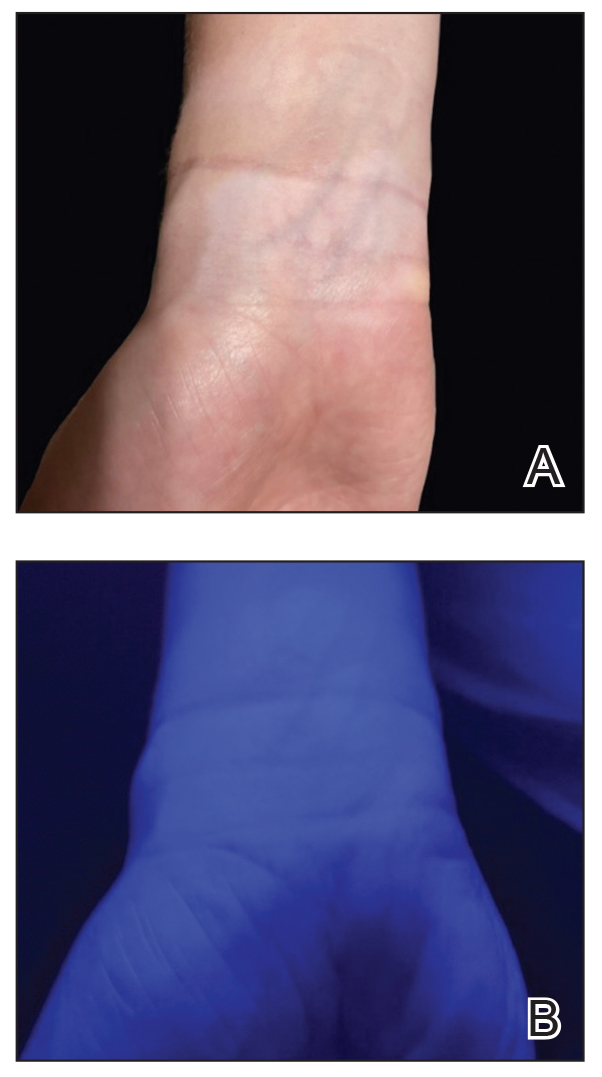
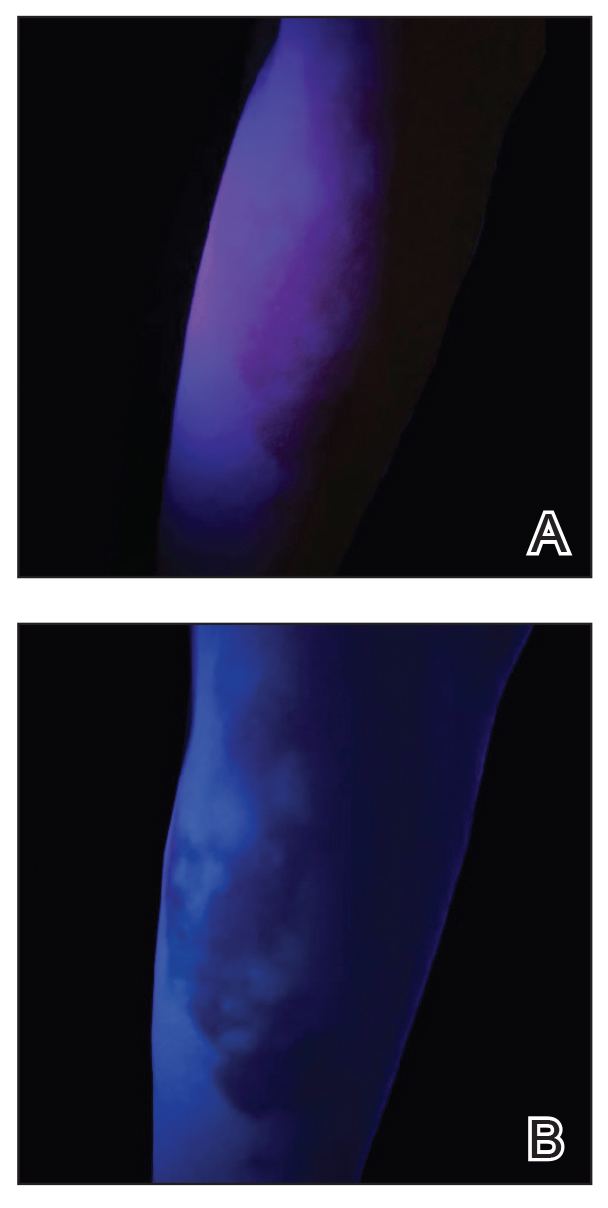
Because these UV light apps are not regulated and their efficacy for medical use has not been firmly established, the Wood lamp remains the gold standard. Therefore, we propose the use of UV light apps in situations when a Wood lamp is not available or convenient, such as in rural, inpatient, or international health care settings.
Practice Implications
Exploring and adopting these free alternatives can contribute to improved accessibility and diagnostic capabilities in diverse health care environments, particularly for communities facing financial constraints. Continued research and validation of these apps in clinical settings will be essential to establish their reliability and effectiveness in enhancing diagnostic practices.
- Dyer JM, Foy VM. Revealing the unseen: a review of Wood’s lamp in dermatology. J Clin Aesthet Dermatol. 2022;15:25-30.
- Scanni G. Facilitations in the clinical diagnosis of human scabies through the use of ultraviolet light (UV-scab scanning): a case-series study. Trop Med Infect Dis. 2022;7:422. doi:10.3390/tropicalmed7120422
- USA Medical and Surgical Supplies. Top 9 medical diagnostic applications for a Woods lamp. February 26, 2019. Accessed May 20, 2024.
- Huang Y, Hsiang E-L, Deng M-Y, et al. Mini-led, micro-led and OLED displays: present status and future perspectives. Light Sci Appl. 2020;9:105. doi:10.1038/s41377-020-0341-9
- Dyer JM, Foy VM. Revealing the unseen: a review of Wood’s lamp in dermatology. J Clin Aesthet Dermatol. 2022;15:25-30.
- Scanni G. Facilitations in the clinical diagnosis of human scabies through the use of ultraviolet light (UV-scab scanning): a case-series study. Trop Med Infect Dis. 2022;7:422. doi:10.3390/tropicalmed7120422
- USA Medical and Surgical Supplies. Top 9 medical diagnostic applications for a Woods lamp. February 26, 2019. Accessed May 20, 2024.
- Huang Y, Hsiang E-L, Deng M-Y, et al. Mini-led, micro-led and OLED displays: present status and future perspectives. Light Sci Appl. 2020;9:105. doi:10.1038/s41377-020-0341-9




