User login
French warn of upsurge in pneumococcal meningitis
MALMO, SWEDEN – A French national study has documented a sharp increase in pneumococcal meningitis since 2015 in children under age 15 years.
The culprit has been identified as serotype 24F, which is not covered by the infant 13-valent conjugate pneumococcal vaccine (PCV13), Naim Ouldali, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The rapid emergence of serotype 24F has been accompanied by a disturbing change in its penicillin susceptibility. Indeed, penicillin resistance was present in only 18% of serotype 24F isolates in France during 2000-2014, then jumped to 74% during 2015-2016, according to Dr. Ouldali of René Descartes University in Paris.
“PCV13 has strongly reduced the pneumococcal meningitis burden in children, but its benefit now seems to be jeopardized, at least in France. So serum 24F could become a major concern in the coming years because of its characteristics. And now the question is, is this emergence an epidemic phenomenon or not? And if it’s confirmed in future studies and in other countries, probably it should drive the development of next-generation PCV formulations,” he said.
Dr. Ouldali presented a population-based interrupted time-series analysis of a nationwide prospective survey conducted in France during 2001-2016. He noted that the Cochrane Collaboration has deemed this study design second only to the randomized controlled trial in terms of quality of evidence.
The study, which included 227 French pediatric wards and 168 microbiology departments, identified 1,778 children under age 15 years with pneumococcal meningitis. This is believed to be more than 60% of all cases that occurred in the country during the study years.
The purpose of the study was to determine the impact of implementation of routine PCV13 as part of the national vaccine strategy. Rates of PCV13 coverage in French children are very high: in excess of 90% during 2015 to 2016.
Implementation of PCV13 led to a dramatic 38% reduction in the monthly incidence of pneumococcal meningitis, from 0.12 cases per 100,000 children before PCV13 to a low of 0.07 cases per 100,000 in December 2014. But after that the rate rebounded sharply, by 2.3% per month during 2015-2016, to a high of 0.13 cases per 100,000 per month by the end of 2016. Drilling down into the data, Dr. Ouldali and his coinvestigators learned that the resurgence of pneumococcal meningitis was due largely to the emergence of serotype 24F.
“This serotype is of particular concern because of two characteristics: First, it is already known to have a high disease potential – one of the highest, along with serotype 12F – and second, this rapid emergence was accompanied by a change in its penicillin susceptibility,” he noted.
Most of the French rebound in pneumococcal meningitis has occurred in children under 2 years of age. Of note, German investigators also have recently reported a rebound in invasive pneumococcal disease in German children under 16 years of age. Non-PCV13 serotypes accounted for 84% of all invasive pneumococcal disease during 2015-2016, with serotypes 10A and 24F leading the way. As in France, most of the resurgence has involved children less than 2 years old. However, unlike in France, most of the German increase has been in nonmeningitis forms of invasive pneumococcal disease (Vaccine. 2018 Jan 25;36[4]:572-7).
In response to a question from a concerned audience member, Dr. Ouldali said that while the penicillin susceptibility of serotype 24F has taken a sharp turn for the worse, cephalosporin susceptibility has not.
“To date, we have not seen any cephalosporin-resistant strains. To date, there is no need to use vancomycin,” he said.
Dr. Ouldali said the next step he and his colleagues plan to take is to see if there is a clonal expansion or a particular underlying genetic pattern which could explain the explosive emergence of 24F.
The study was funded by a research grant from Pfizer and by the French Pediatric Infectious Diseases Group.
MALMO, SWEDEN – A French national study has documented a sharp increase in pneumococcal meningitis since 2015 in children under age 15 years.
The culprit has been identified as serotype 24F, which is not covered by the infant 13-valent conjugate pneumococcal vaccine (PCV13), Naim Ouldali, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The rapid emergence of serotype 24F has been accompanied by a disturbing change in its penicillin susceptibility. Indeed, penicillin resistance was present in only 18% of serotype 24F isolates in France during 2000-2014, then jumped to 74% during 2015-2016, according to Dr. Ouldali of René Descartes University in Paris.
“PCV13 has strongly reduced the pneumococcal meningitis burden in children, but its benefit now seems to be jeopardized, at least in France. So serum 24F could become a major concern in the coming years because of its characteristics. And now the question is, is this emergence an epidemic phenomenon or not? And if it’s confirmed in future studies and in other countries, probably it should drive the development of next-generation PCV formulations,” he said.
Dr. Ouldali presented a population-based interrupted time-series analysis of a nationwide prospective survey conducted in France during 2001-2016. He noted that the Cochrane Collaboration has deemed this study design second only to the randomized controlled trial in terms of quality of evidence.
The study, which included 227 French pediatric wards and 168 microbiology departments, identified 1,778 children under age 15 years with pneumococcal meningitis. This is believed to be more than 60% of all cases that occurred in the country during the study years.
The purpose of the study was to determine the impact of implementation of routine PCV13 as part of the national vaccine strategy. Rates of PCV13 coverage in French children are very high: in excess of 90% during 2015 to 2016.
Implementation of PCV13 led to a dramatic 38% reduction in the monthly incidence of pneumococcal meningitis, from 0.12 cases per 100,000 children before PCV13 to a low of 0.07 cases per 100,000 in December 2014. But after that the rate rebounded sharply, by 2.3% per month during 2015-2016, to a high of 0.13 cases per 100,000 per month by the end of 2016. Drilling down into the data, Dr. Ouldali and his coinvestigators learned that the resurgence of pneumococcal meningitis was due largely to the emergence of serotype 24F.
“This serotype is of particular concern because of two characteristics: First, it is already known to have a high disease potential – one of the highest, along with serotype 12F – and second, this rapid emergence was accompanied by a change in its penicillin susceptibility,” he noted.
Most of the French rebound in pneumococcal meningitis has occurred in children under 2 years of age. Of note, German investigators also have recently reported a rebound in invasive pneumococcal disease in German children under 16 years of age. Non-PCV13 serotypes accounted for 84% of all invasive pneumococcal disease during 2015-2016, with serotypes 10A and 24F leading the way. As in France, most of the resurgence has involved children less than 2 years old. However, unlike in France, most of the German increase has been in nonmeningitis forms of invasive pneumococcal disease (Vaccine. 2018 Jan 25;36[4]:572-7).
In response to a question from a concerned audience member, Dr. Ouldali said that while the penicillin susceptibility of serotype 24F has taken a sharp turn for the worse, cephalosporin susceptibility has not.
“To date, we have not seen any cephalosporin-resistant strains. To date, there is no need to use vancomycin,” he said.
Dr. Ouldali said the next step he and his colleagues plan to take is to see if there is a clonal expansion or a particular underlying genetic pattern which could explain the explosive emergence of 24F.
The study was funded by a research grant from Pfizer and by the French Pediatric Infectious Diseases Group.
MALMO, SWEDEN – A French national study has documented a sharp increase in pneumococcal meningitis since 2015 in children under age 15 years.
The culprit has been identified as serotype 24F, which is not covered by the infant 13-valent conjugate pneumococcal vaccine (PCV13), Naim Ouldali, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The rapid emergence of serotype 24F has been accompanied by a disturbing change in its penicillin susceptibility. Indeed, penicillin resistance was present in only 18% of serotype 24F isolates in France during 2000-2014, then jumped to 74% during 2015-2016, according to Dr. Ouldali of René Descartes University in Paris.
“PCV13 has strongly reduced the pneumococcal meningitis burden in children, but its benefit now seems to be jeopardized, at least in France. So serum 24F could become a major concern in the coming years because of its characteristics. And now the question is, is this emergence an epidemic phenomenon or not? And if it’s confirmed in future studies and in other countries, probably it should drive the development of next-generation PCV formulations,” he said.
Dr. Ouldali presented a population-based interrupted time-series analysis of a nationwide prospective survey conducted in France during 2001-2016. He noted that the Cochrane Collaboration has deemed this study design second only to the randomized controlled trial in terms of quality of evidence.
The study, which included 227 French pediatric wards and 168 microbiology departments, identified 1,778 children under age 15 years with pneumococcal meningitis. This is believed to be more than 60% of all cases that occurred in the country during the study years.
The purpose of the study was to determine the impact of implementation of routine PCV13 as part of the national vaccine strategy. Rates of PCV13 coverage in French children are very high: in excess of 90% during 2015 to 2016.
Implementation of PCV13 led to a dramatic 38% reduction in the monthly incidence of pneumococcal meningitis, from 0.12 cases per 100,000 children before PCV13 to a low of 0.07 cases per 100,000 in December 2014. But after that the rate rebounded sharply, by 2.3% per month during 2015-2016, to a high of 0.13 cases per 100,000 per month by the end of 2016. Drilling down into the data, Dr. Ouldali and his coinvestigators learned that the resurgence of pneumococcal meningitis was due largely to the emergence of serotype 24F.
“This serotype is of particular concern because of two characteristics: First, it is already known to have a high disease potential – one of the highest, along with serotype 12F – and second, this rapid emergence was accompanied by a change in its penicillin susceptibility,” he noted.
Most of the French rebound in pneumococcal meningitis has occurred in children under 2 years of age. Of note, German investigators also have recently reported a rebound in invasive pneumococcal disease in German children under 16 years of age. Non-PCV13 serotypes accounted for 84% of all invasive pneumococcal disease during 2015-2016, with serotypes 10A and 24F leading the way. As in France, most of the resurgence has involved children less than 2 years old. However, unlike in France, most of the German increase has been in nonmeningitis forms of invasive pneumococcal disease (Vaccine. 2018 Jan 25;36[4]:572-7).
In response to a question from a concerned audience member, Dr. Ouldali said that while the penicillin susceptibility of serotype 24F has taken a sharp turn for the worse, cephalosporin susceptibility has not.
“To date, we have not seen any cephalosporin-resistant strains. To date, there is no need to use vancomycin,” he said.
Dr. Ouldali said the next step he and his colleagues plan to take is to see if there is a clonal expansion or a particular underlying genetic pattern which could explain the explosive emergence of 24F.
The study was funded by a research grant from Pfizer and by the French Pediatric Infectious Diseases Group.
REPORTING FROM ESPID 2018
Key clinical point:
Major finding: The incidence of pneumococcal meningitis in French children jumped by 2.3% per month during 2015-2016.
Study details: This population-based interrupted time-series analysis included all 1,778 cases of pneumococcal meningitis in children under age 15 years during 2001-2016 in 227 French pediatric wards.
Disclosures: The study was funded by a grant from Pfizer and by the French Pediatric Infectious Diseases Group.
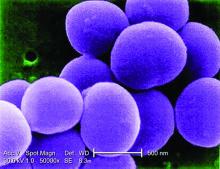
Four syndromes suggest life-threatening PVL-positive S. aureus infection
MALMO, SWEDEN – Methicillin-resistant Staphylococcus aureus gets the blame in the Americas as the main cause of a great wave of community-acquired severe invasive staphylococcal infections in children and adolescents during the past nearly 2 decades, but many European pediatric infectious disease specialists believe that Panton-Valentine leukocidin (PVL), a frequent co-traveler with MRSA, is the true bad actor.
“The American literature focused first on MRSA, but we’ve seen very similar, very severe cases with MSSA [methicillin-susceptible S. aureus] PVL-positive and MRSA PVL-positive infections,” Pablo Rojo, MD, PhD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
“It is only because at the beginning there were so many MRSA cases in the States that they thought that was the driver of the disease. It is still unclear. There is still a discussion. But I wanted to bring you my opinion and that of many other authors that it’s mostly PVL-associated,” added Dr. Rojo of Complutense University in Madrid.
He was senior author of a multinational European and Israeli prospective study of risk factors associated with the severity of invasive community-acquired S. aureus infections in children, with invasive infection being defined as hospitalization for an infection with S. aureus isolated from a normally sterile body site such as blood, bone, or cerebrospinal fluid, or S. aureus pneumonia. They identified 152 affected children, 17% of whom had severe community-acquired invasive S. aureus, defined by death or admission to a pediatric intensive care unit due to respiratory failure or hemodynamic instability.
The prevalence of PVL-positive S. aureus infection in the overall invasive infection group was 19%, while 8% of the isolates were MRSA. while MRSA was not associated with a significantly increased risk. The other independent risk factors for severe outcome were pneumonia, with an adjusted 13-fold increased risk, and leukopenia at admission, with an associated 18-fold risk (Clin Microbiol Infect. 2016 Jul;22[7]:643.e1-6.).
Of note, the virulence of PVL stems from the pore-forming toxin’s ability to lyse white blood cells. Because a leukocyte count is always available once a patient reaches the ED, severe leukopenia as defined by a count of less than 3,000 cells/mm3 at admission becomes a useful early marker of the likely severity of any case of S. aureus invasive disease, according to Dr. Rojo.
He highlighted four key syndromes involving severe invasive S. aureus infection in previously healthy children and adolescents that entail a high likelihood of being PVL positive and should cause physicians to run – not walk – to start appropriate empiric therapy. He also described the treatment regimen that he and other European thought leaders recommend for severe PVL-positive S. aureus invasive infections.
The microbiologic diagnosis of PVL can be made by ELISA (enzyme-linked immunoassay) to detect the toxin in an S. aureus isolate, by a rapid monoclonal antibody test, or by polymerase chain reaction to detect PVL genes in an S. aureus isolate. But don’t wait for test results to initiate treatment because these are high-mortality syndromes, he advised.
“Many people tell me, ‘My lab doesn’t have a way to diagnose PVL.’ And it’s true, it’s not available in real life at many hospitals. My message to you is that you don’t need to wait for a microbiological diagnosis or the results to come back from a sample you have sent to the reference lab in the main referral center. We can base our diagnosis and decision to treat on clinical grounds if we focus on these four very uncommon syndromes involving invasive S. aureus infection. I think if you have any child with these symptoms you have to manage them on the assumption that PVL is present,” said Dr. Rojo, principal investigator of the European Project on Invasive S. aureus Pediatric Infections.
The four key syndromes
The four syndromes are severe S. aureus pneumonia, S. aureus bone and joint infections with multiple foci, S. aureus osteomyelitis complicated by deep vein thrombosis, and invasive S. aureus infection plus shock.
- Severe S. aureus pneumonia. Investigators at Claude Bernard University in Lyon, France, have done extensive pioneering work on severe PVL-positive S. aureus invasive infections in children. In an early paper, they highlighted the characteristics that distinguish severe PVL-positive pneumonia: it typically occurs in previously healthy children and adolescents without underlying comorbid conditions, and it is often preceded by a influenza-like syndrome followed by an acute severe pneumonia with hemoptysis. Mortality was very high in this early series, with nearly half of the patients being dead within the first several days after admission (Lancet. 2002 Mar 2;359[9308]:753-9).
- Severe osteomyelitis. Investigators at Baylor College of Medicine, Houston, were among the first to observe that osteomyelitis caused by PVL-positive strains of S. aureus are associated with more severe local disease, with multiple affected areas, bigger abscesses, a greater systemic inflammatory response, and more surgeries required compared with osteomyelitis caused by PVL-negative S. aureus (Pediatrics. 2006 Feb;117[2]:433-40).
- Osteomyelitis with deep vein thrombosis. When a child hospitalized for acute hematogenous osteomyelitis due to S. aureus develops difficulty breathing, that’s a red flag for a severe PVL-positive infection involving deep vein thrombosis. Indeed, investigators at the Leeds (England) General Infirmary have reported that deep vein thrombosis in the setting of S. aureus osteomyelitis is associated with a greater than eightfold increased likelihood of a PVL-positive infection (Br J Hosp Med [Lond]. 2015 Jan;76[1]:18-24). Also, patients with PVL-positive osteomyelitis and deep vein thrombosis are prone to formation of septic emboli.
- Osteomyelitis with septic shock. The Lyon group compared outcomes in 14 pediatric patients with PVL-positive S. aureus osteomyelitis and a control group of 17 patients with PVL-negative disease. All 14 PVL-positive patients had severe sepsis and 6 of them had septic shock. In contrast, none of the controls did. Median duration of hospitalization was 46 days in the PVL-positive group, compared with 13 days in controls (Pediatr Infect Dis J. 2007 Nov;26[11]:1042-8).
Treatment
No randomized trials exist to guide treatment, but Dr. Rojo recommends the protocol utilized by the Lyon group: a bactericidal antibiotic – vancomycin or a beta-lactam – to take on the S. aureus, coupled with a ribosomally active antibiotic – clindamycin or linezolid – to suppress the PVL toxin’s virulence expression. The French group cites both in vitro and in vivo evidence that clindamycin and linezolid in their standard dosing have such an antitoxin effect (Clin Microbiol Rev. 2017 Oct;30[4]:887-917).
In addition, Dr. Rojo recommends utilizing any of the commercially available intravenous immunoglobulin (IVIG) products on the basis of work by investigators at Vanderbilt University in Nashville, Tenn., who have demonstrated that these products contain functional neutralizing antibodies against S. aureus leukocidins. This observation provides a likely explanation for anecdotal reports of improved outcomes in IVIG-treated patients with toxin-associated staphylococcal disease (Antimicrob Agents Chemother. 2017 Oct 24;61[11]. pii: e00968-17).
Challenged as to when specifically he would use IVIG in light of the global shortage of immunoglobulins, Dr. Rojo replied: “Not in every invasive S. aureus infection, but in serious infections that are PVL positive. I think if you have a child with one of these four syndromes who is in a pediatric ICU, you should use it. I mean, the mortality is around 30% in healthy children, so you would not stop from giving it. The risk of giving IVIG is very low, no side effects, so I highly recommend it for these severe cases.”
He reported having no financial conflicts.
MALMO, SWEDEN – Methicillin-resistant Staphylococcus aureus gets the blame in the Americas as the main cause of a great wave of community-acquired severe invasive staphylococcal infections in children and adolescents during the past nearly 2 decades, but many European pediatric infectious disease specialists believe that Panton-Valentine leukocidin (PVL), a frequent co-traveler with MRSA, is the true bad actor.
“The American literature focused first on MRSA, but we’ve seen very similar, very severe cases with MSSA [methicillin-susceptible S. aureus] PVL-positive and MRSA PVL-positive infections,” Pablo Rojo, MD, PhD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
“It is only because at the beginning there were so many MRSA cases in the States that they thought that was the driver of the disease. It is still unclear. There is still a discussion. But I wanted to bring you my opinion and that of many other authors that it’s mostly PVL-associated,” added Dr. Rojo of Complutense University in Madrid.
He was senior author of a multinational European and Israeli prospective study of risk factors associated with the severity of invasive community-acquired S. aureus infections in children, with invasive infection being defined as hospitalization for an infection with S. aureus isolated from a normally sterile body site such as blood, bone, or cerebrospinal fluid, or S. aureus pneumonia. They identified 152 affected children, 17% of whom had severe community-acquired invasive S. aureus, defined by death or admission to a pediatric intensive care unit due to respiratory failure or hemodynamic instability.
The prevalence of PVL-positive S. aureus infection in the overall invasive infection group was 19%, while 8% of the isolates were MRSA. while MRSA was not associated with a significantly increased risk. The other independent risk factors for severe outcome were pneumonia, with an adjusted 13-fold increased risk, and leukopenia at admission, with an associated 18-fold risk (Clin Microbiol Infect. 2016 Jul;22[7]:643.e1-6.).
Of note, the virulence of PVL stems from the pore-forming toxin’s ability to lyse white blood cells. Because a leukocyte count is always available once a patient reaches the ED, severe leukopenia as defined by a count of less than 3,000 cells/mm3 at admission becomes a useful early marker of the likely severity of any case of S. aureus invasive disease, according to Dr. Rojo.
He highlighted four key syndromes involving severe invasive S. aureus infection in previously healthy children and adolescents that entail a high likelihood of being PVL positive and should cause physicians to run – not walk – to start appropriate empiric therapy. He also described the treatment regimen that he and other European thought leaders recommend for severe PVL-positive S. aureus invasive infections.
The microbiologic diagnosis of PVL can be made by ELISA (enzyme-linked immunoassay) to detect the toxin in an S. aureus isolate, by a rapid monoclonal antibody test, or by polymerase chain reaction to detect PVL genes in an S. aureus isolate. But don’t wait for test results to initiate treatment because these are high-mortality syndromes, he advised.
“Many people tell me, ‘My lab doesn’t have a way to diagnose PVL.’ And it’s true, it’s not available in real life at many hospitals. My message to you is that you don’t need to wait for a microbiological diagnosis or the results to come back from a sample you have sent to the reference lab in the main referral center. We can base our diagnosis and decision to treat on clinical grounds if we focus on these four very uncommon syndromes involving invasive S. aureus infection. I think if you have any child with these symptoms you have to manage them on the assumption that PVL is present,” said Dr. Rojo, principal investigator of the European Project on Invasive S. aureus Pediatric Infections.
The four key syndromes
The four syndromes are severe S. aureus pneumonia, S. aureus bone and joint infections with multiple foci, S. aureus osteomyelitis complicated by deep vein thrombosis, and invasive S. aureus infection plus shock.
- Severe S. aureus pneumonia. Investigators at Claude Bernard University in Lyon, France, have done extensive pioneering work on severe PVL-positive S. aureus invasive infections in children. In an early paper, they highlighted the characteristics that distinguish severe PVL-positive pneumonia: it typically occurs in previously healthy children and adolescents without underlying comorbid conditions, and it is often preceded by a influenza-like syndrome followed by an acute severe pneumonia with hemoptysis. Mortality was very high in this early series, with nearly half of the patients being dead within the first several days after admission (Lancet. 2002 Mar 2;359[9308]:753-9).
- Severe osteomyelitis. Investigators at Baylor College of Medicine, Houston, were among the first to observe that osteomyelitis caused by PVL-positive strains of S. aureus are associated with more severe local disease, with multiple affected areas, bigger abscesses, a greater systemic inflammatory response, and more surgeries required compared with osteomyelitis caused by PVL-negative S. aureus (Pediatrics. 2006 Feb;117[2]:433-40).
- Osteomyelitis with deep vein thrombosis. When a child hospitalized for acute hematogenous osteomyelitis due to S. aureus develops difficulty breathing, that’s a red flag for a severe PVL-positive infection involving deep vein thrombosis. Indeed, investigators at the Leeds (England) General Infirmary have reported that deep vein thrombosis in the setting of S. aureus osteomyelitis is associated with a greater than eightfold increased likelihood of a PVL-positive infection (Br J Hosp Med [Lond]. 2015 Jan;76[1]:18-24). Also, patients with PVL-positive osteomyelitis and deep vein thrombosis are prone to formation of septic emboli.
- Osteomyelitis with septic shock. The Lyon group compared outcomes in 14 pediatric patients with PVL-positive S. aureus osteomyelitis and a control group of 17 patients with PVL-negative disease. All 14 PVL-positive patients had severe sepsis and 6 of them had septic shock. In contrast, none of the controls did. Median duration of hospitalization was 46 days in the PVL-positive group, compared with 13 days in controls (Pediatr Infect Dis J. 2007 Nov;26[11]:1042-8).
Treatment
No randomized trials exist to guide treatment, but Dr. Rojo recommends the protocol utilized by the Lyon group: a bactericidal antibiotic – vancomycin or a beta-lactam – to take on the S. aureus, coupled with a ribosomally active antibiotic – clindamycin or linezolid – to suppress the PVL toxin’s virulence expression. The French group cites both in vitro and in vivo evidence that clindamycin and linezolid in their standard dosing have such an antitoxin effect (Clin Microbiol Rev. 2017 Oct;30[4]:887-917).
In addition, Dr. Rojo recommends utilizing any of the commercially available intravenous immunoglobulin (IVIG) products on the basis of work by investigators at Vanderbilt University in Nashville, Tenn., who have demonstrated that these products contain functional neutralizing antibodies against S. aureus leukocidins. This observation provides a likely explanation for anecdotal reports of improved outcomes in IVIG-treated patients with toxin-associated staphylococcal disease (Antimicrob Agents Chemother. 2017 Oct 24;61[11]. pii: e00968-17).
Challenged as to when specifically he would use IVIG in light of the global shortage of immunoglobulins, Dr. Rojo replied: “Not in every invasive S. aureus infection, but in serious infections that are PVL positive. I think if you have a child with one of these four syndromes who is in a pediatric ICU, you should use it. I mean, the mortality is around 30% in healthy children, so you would not stop from giving it. The risk of giving IVIG is very low, no side effects, so I highly recommend it for these severe cases.”
He reported having no financial conflicts.
MALMO, SWEDEN – Methicillin-resistant Staphylococcus aureus gets the blame in the Americas as the main cause of a great wave of community-acquired severe invasive staphylococcal infections in children and adolescents during the past nearly 2 decades, but many European pediatric infectious disease specialists believe that Panton-Valentine leukocidin (PVL), a frequent co-traveler with MRSA, is the true bad actor.
“The American literature focused first on MRSA, but we’ve seen very similar, very severe cases with MSSA [methicillin-susceptible S. aureus] PVL-positive and MRSA PVL-positive infections,” Pablo Rojo, MD, PhD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
“It is only because at the beginning there were so many MRSA cases in the States that they thought that was the driver of the disease. It is still unclear. There is still a discussion. But I wanted to bring you my opinion and that of many other authors that it’s mostly PVL-associated,” added Dr. Rojo of Complutense University in Madrid.
He was senior author of a multinational European and Israeli prospective study of risk factors associated with the severity of invasive community-acquired S. aureus infections in children, with invasive infection being defined as hospitalization for an infection with S. aureus isolated from a normally sterile body site such as blood, bone, or cerebrospinal fluid, or S. aureus pneumonia. They identified 152 affected children, 17% of whom had severe community-acquired invasive S. aureus, defined by death or admission to a pediatric intensive care unit due to respiratory failure or hemodynamic instability.
The prevalence of PVL-positive S. aureus infection in the overall invasive infection group was 19%, while 8% of the isolates were MRSA. while MRSA was not associated with a significantly increased risk. The other independent risk factors for severe outcome were pneumonia, with an adjusted 13-fold increased risk, and leukopenia at admission, with an associated 18-fold risk (Clin Microbiol Infect. 2016 Jul;22[7]:643.e1-6.).
Of note, the virulence of PVL stems from the pore-forming toxin’s ability to lyse white blood cells. Because a leukocyte count is always available once a patient reaches the ED, severe leukopenia as defined by a count of less than 3,000 cells/mm3 at admission becomes a useful early marker of the likely severity of any case of S. aureus invasive disease, according to Dr. Rojo.
He highlighted four key syndromes involving severe invasive S. aureus infection in previously healthy children and adolescents that entail a high likelihood of being PVL positive and should cause physicians to run – not walk – to start appropriate empiric therapy. He also described the treatment regimen that he and other European thought leaders recommend for severe PVL-positive S. aureus invasive infections.
The microbiologic diagnosis of PVL can be made by ELISA (enzyme-linked immunoassay) to detect the toxin in an S. aureus isolate, by a rapid monoclonal antibody test, or by polymerase chain reaction to detect PVL genes in an S. aureus isolate. But don’t wait for test results to initiate treatment because these are high-mortality syndromes, he advised.
“Many people tell me, ‘My lab doesn’t have a way to diagnose PVL.’ And it’s true, it’s not available in real life at many hospitals. My message to you is that you don’t need to wait for a microbiological diagnosis or the results to come back from a sample you have sent to the reference lab in the main referral center. We can base our diagnosis and decision to treat on clinical grounds if we focus on these four very uncommon syndromes involving invasive S. aureus infection. I think if you have any child with these symptoms you have to manage them on the assumption that PVL is present,” said Dr. Rojo, principal investigator of the European Project on Invasive S. aureus Pediatric Infections.
The four key syndromes
The four syndromes are severe S. aureus pneumonia, S. aureus bone and joint infections with multiple foci, S. aureus osteomyelitis complicated by deep vein thrombosis, and invasive S. aureus infection plus shock.
- Severe S. aureus pneumonia. Investigators at Claude Bernard University in Lyon, France, have done extensive pioneering work on severe PVL-positive S. aureus invasive infections in children. In an early paper, they highlighted the characteristics that distinguish severe PVL-positive pneumonia: it typically occurs in previously healthy children and adolescents without underlying comorbid conditions, and it is often preceded by a influenza-like syndrome followed by an acute severe pneumonia with hemoptysis. Mortality was very high in this early series, with nearly half of the patients being dead within the first several days after admission (Lancet. 2002 Mar 2;359[9308]:753-9).
- Severe osteomyelitis. Investigators at Baylor College of Medicine, Houston, were among the first to observe that osteomyelitis caused by PVL-positive strains of S. aureus are associated with more severe local disease, with multiple affected areas, bigger abscesses, a greater systemic inflammatory response, and more surgeries required compared with osteomyelitis caused by PVL-negative S. aureus (Pediatrics. 2006 Feb;117[2]:433-40).
- Osteomyelitis with deep vein thrombosis. When a child hospitalized for acute hematogenous osteomyelitis due to S. aureus develops difficulty breathing, that’s a red flag for a severe PVL-positive infection involving deep vein thrombosis. Indeed, investigators at the Leeds (England) General Infirmary have reported that deep vein thrombosis in the setting of S. aureus osteomyelitis is associated with a greater than eightfold increased likelihood of a PVL-positive infection (Br J Hosp Med [Lond]. 2015 Jan;76[1]:18-24). Also, patients with PVL-positive osteomyelitis and deep vein thrombosis are prone to formation of septic emboli.
- Osteomyelitis with septic shock. The Lyon group compared outcomes in 14 pediatric patients with PVL-positive S. aureus osteomyelitis and a control group of 17 patients with PVL-negative disease. All 14 PVL-positive patients had severe sepsis and 6 of them had septic shock. In contrast, none of the controls did. Median duration of hospitalization was 46 days in the PVL-positive group, compared with 13 days in controls (Pediatr Infect Dis J. 2007 Nov;26[11]:1042-8).
Treatment
No randomized trials exist to guide treatment, but Dr. Rojo recommends the protocol utilized by the Lyon group: a bactericidal antibiotic – vancomycin or a beta-lactam – to take on the S. aureus, coupled with a ribosomally active antibiotic – clindamycin or linezolid – to suppress the PVL toxin’s virulence expression. The French group cites both in vitro and in vivo evidence that clindamycin and linezolid in their standard dosing have such an antitoxin effect (Clin Microbiol Rev. 2017 Oct;30[4]:887-917).
In addition, Dr. Rojo recommends utilizing any of the commercially available intravenous immunoglobulin (IVIG) products on the basis of work by investigators at Vanderbilt University in Nashville, Tenn., who have demonstrated that these products contain functional neutralizing antibodies against S. aureus leukocidins. This observation provides a likely explanation for anecdotal reports of improved outcomes in IVIG-treated patients with toxin-associated staphylococcal disease (Antimicrob Agents Chemother. 2017 Oct 24;61[11]. pii: e00968-17).
Challenged as to when specifically he would use IVIG in light of the global shortage of immunoglobulins, Dr. Rojo replied: “Not in every invasive S. aureus infection, but in serious infections that are PVL positive. I think if you have a child with one of these four syndromes who is in a pediatric ICU, you should use it. I mean, the mortality is around 30% in healthy children, so you would not stop from giving it. The risk of giving IVIG is very low, no side effects, so I highly recommend it for these severe cases.”
He reported having no financial conflicts.
EXPERT ANALYSIS FROM ESPID 2018
DTPa-HBV-IPV/Hib in infancy maintains lasting immune memory against HBV in teens
MALMO, SWEDEN – Four doses of hexavalent diphtheria-tetanus-acellular pertussis-hepatitis B-inactivated poliovirus/Haemophilus influenza type b vaccine given in infancy provides reassuringly long-lasting immune memory against hepatitis B among 14- to 15-year-olds, Tino F. Schwarz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented the fourth and final study in a series evaluating the antibody persistence and immune memory against hepatitis B (HBV) in recipients of the complete four-dose series of hexavalent DTPa-HBV-IPV/Hib vaccine in infancy. Because exposure to HBV can increase during adolescence, it was essential to determine whether antibody persistence is maintained, explained Dr. Schwarz of Juliusspital Hospital in Wurzburg, Germany.
“As expected, we saw a decrease in anti-HBs [hepatitis B surface antigen] antibody levels over the years, with persistent seroprotection in 85% of children at age 4-5 years, 72% at 7-8 years, 61% at 12-13 years, and now 54% of adolescents at 14-15 years. But we could demonstrate a very strong anamnestic response in the trial. This is good information. It clearly shows that, in patients who are exposed to hepatitis B, we can certainly guarantee that they are protected. It’s a good result for public health. The vaccine is a very robust vaccine which induces a very strong response over the years. It can be boosted, but from an immunologic point of view it is not required,” he said.
The multicenter study included 268 adolescents aged 14-15 years who had received the four-dose hexavalent vaccine series in infancy. Their antibody persistence against anti-HBs was measured, then measured once again 1 month after receiving a challenge dose of monovalent HBV vaccine.
Prechallenge, 105 of the teens were seronegative, 144 were seroprotected as defined by an anti-HBs concentration of at least 10 mIU/mL, and 19 had low seropositivity marked by an antibody level of 6 to less than 10 mIU/mL. Yet 1 month after the booster, which was intended to mimic the impact of real-world exposure to HBV, 83% of the initially seronegative subjects had an anti-HBs concentration of 10 mIU/mL or more, and 67% of them had a level of at least 100 mIU/mL.
“We saw a clear fantastic anamnestic response,” Dr. Schwarz declared.
Overall, 93% of study participants seroconverted, and 87% of them had anti-HBs titers of 100 mIU/mL, “which is the level we’d like to achieve in vaccinees,” he observed.
The booster monovalent HBV vaccine was well tolerated, with one-third of subjects complaining of mild local injection site pain and 30% noting fatigue. But in response to a question posed by session chair Ronald de Groot, MD, emeritus professor of pediatrics at Radboud University in Nijmegen, the Netherlands, Dr. Schwarz said these study results indicate there’s no need for routine boosting in healthy adolescents such as those in the trial. Immunocompromised individuals might be a different story, but they weren’t investigated.
But what about in physicians and surgeons, where protection against HBV infection is essential? Dr. de Groot asked.
“In Germany, we require a titer of 100 mIU/mL or more in medical staff, but we’re quite alone in Europe. Other countries do not require booster vaccination for medical staff. The data we’ve shown here is quite reassuring: If you get exposed, you in effect get a booster. It’s complicated to test surgeons in their offices; better to just rely on the anamnestic response that we’ve demonstrated,” Dr. Schwarz replied.
He reported serving as a consultant to GlaxoSmithKline, which funded the study, as well as to Pfizer and Sanofi Pasteur.
MALMO, SWEDEN – Four doses of hexavalent diphtheria-tetanus-acellular pertussis-hepatitis B-inactivated poliovirus/Haemophilus influenza type b vaccine given in infancy provides reassuringly long-lasting immune memory against hepatitis B among 14- to 15-year-olds, Tino F. Schwarz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented the fourth and final study in a series evaluating the antibody persistence and immune memory against hepatitis B (HBV) in recipients of the complete four-dose series of hexavalent DTPa-HBV-IPV/Hib vaccine in infancy. Because exposure to HBV can increase during adolescence, it was essential to determine whether antibody persistence is maintained, explained Dr. Schwarz of Juliusspital Hospital in Wurzburg, Germany.
“As expected, we saw a decrease in anti-HBs [hepatitis B surface antigen] antibody levels over the years, with persistent seroprotection in 85% of children at age 4-5 years, 72% at 7-8 years, 61% at 12-13 years, and now 54% of adolescents at 14-15 years. But we could demonstrate a very strong anamnestic response in the trial. This is good information. It clearly shows that, in patients who are exposed to hepatitis B, we can certainly guarantee that they are protected. It’s a good result for public health. The vaccine is a very robust vaccine which induces a very strong response over the years. It can be boosted, but from an immunologic point of view it is not required,” he said.
The multicenter study included 268 adolescents aged 14-15 years who had received the four-dose hexavalent vaccine series in infancy. Their antibody persistence against anti-HBs was measured, then measured once again 1 month after receiving a challenge dose of monovalent HBV vaccine.
Prechallenge, 105 of the teens were seronegative, 144 were seroprotected as defined by an anti-HBs concentration of at least 10 mIU/mL, and 19 had low seropositivity marked by an antibody level of 6 to less than 10 mIU/mL. Yet 1 month after the booster, which was intended to mimic the impact of real-world exposure to HBV, 83% of the initially seronegative subjects had an anti-HBs concentration of 10 mIU/mL or more, and 67% of them had a level of at least 100 mIU/mL.
“We saw a clear fantastic anamnestic response,” Dr. Schwarz declared.
Overall, 93% of study participants seroconverted, and 87% of them had anti-HBs titers of 100 mIU/mL, “which is the level we’d like to achieve in vaccinees,” he observed.
The booster monovalent HBV vaccine was well tolerated, with one-third of subjects complaining of mild local injection site pain and 30% noting fatigue. But in response to a question posed by session chair Ronald de Groot, MD, emeritus professor of pediatrics at Radboud University in Nijmegen, the Netherlands, Dr. Schwarz said these study results indicate there’s no need for routine boosting in healthy adolescents such as those in the trial. Immunocompromised individuals might be a different story, but they weren’t investigated.
But what about in physicians and surgeons, where protection against HBV infection is essential? Dr. de Groot asked.
“In Germany, we require a titer of 100 mIU/mL or more in medical staff, but we’re quite alone in Europe. Other countries do not require booster vaccination for medical staff. The data we’ve shown here is quite reassuring: If you get exposed, you in effect get a booster. It’s complicated to test surgeons in their offices; better to just rely on the anamnestic response that we’ve demonstrated,” Dr. Schwarz replied.
He reported serving as a consultant to GlaxoSmithKline, which funded the study, as well as to Pfizer and Sanofi Pasteur.
MALMO, SWEDEN – Four doses of hexavalent diphtheria-tetanus-acellular pertussis-hepatitis B-inactivated poliovirus/Haemophilus influenza type b vaccine given in infancy provides reassuringly long-lasting immune memory against hepatitis B among 14- to 15-year-olds, Tino F. Schwarz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented the fourth and final study in a series evaluating the antibody persistence and immune memory against hepatitis B (HBV) in recipients of the complete four-dose series of hexavalent DTPa-HBV-IPV/Hib vaccine in infancy. Because exposure to HBV can increase during adolescence, it was essential to determine whether antibody persistence is maintained, explained Dr. Schwarz of Juliusspital Hospital in Wurzburg, Germany.
“As expected, we saw a decrease in anti-HBs [hepatitis B surface antigen] antibody levels over the years, with persistent seroprotection in 85% of children at age 4-5 years, 72% at 7-8 years, 61% at 12-13 years, and now 54% of adolescents at 14-15 years. But we could demonstrate a very strong anamnestic response in the trial. This is good information. It clearly shows that, in patients who are exposed to hepatitis B, we can certainly guarantee that they are protected. It’s a good result for public health. The vaccine is a very robust vaccine which induces a very strong response over the years. It can be boosted, but from an immunologic point of view it is not required,” he said.
The multicenter study included 268 adolescents aged 14-15 years who had received the four-dose hexavalent vaccine series in infancy. Their antibody persistence against anti-HBs was measured, then measured once again 1 month after receiving a challenge dose of monovalent HBV vaccine.
Prechallenge, 105 of the teens were seronegative, 144 were seroprotected as defined by an anti-HBs concentration of at least 10 mIU/mL, and 19 had low seropositivity marked by an antibody level of 6 to less than 10 mIU/mL. Yet 1 month after the booster, which was intended to mimic the impact of real-world exposure to HBV, 83% of the initially seronegative subjects had an anti-HBs concentration of 10 mIU/mL or more, and 67% of them had a level of at least 100 mIU/mL.
“We saw a clear fantastic anamnestic response,” Dr. Schwarz declared.
Overall, 93% of study participants seroconverted, and 87% of them had anti-HBs titers of 100 mIU/mL, “which is the level we’d like to achieve in vaccinees,” he observed.
The booster monovalent HBV vaccine was well tolerated, with one-third of subjects complaining of mild local injection site pain and 30% noting fatigue. But in response to a question posed by session chair Ronald de Groot, MD, emeritus professor of pediatrics at Radboud University in Nijmegen, the Netherlands, Dr. Schwarz said these study results indicate there’s no need for routine boosting in healthy adolescents such as those in the trial. Immunocompromised individuals might be a different story, but they weren’t investigated.
But what about in physicians and surgeons, where protection against HBV infection is essential? Dr. de Groot asked.
“In Germany, we require a titer of 100 mIU/mL or more in medical staff, but we’re quite alone in Europe. Other countries do not require booster vaccination for medical staff. The data we’ve shown here is quite reassuring: If you get exposed, you in effect get a booster. It’s complicated to test surgeons in their offices; better to just rely on the anamnestic response that we’ve demonstrated,” Dr. Schwarz replied.
He reported serving as a consultant to GlaxoSmithKline, which funded the study, as well as to Pfizer and Sanofi Pasteur.
REPORTING FROM ESPID 2018
Key clinical point:
Major finding: Ninety-three percent of recipients of four doses of hexavalent DTPa-HBV-IPV/Hib vaccine in infancy were seroprotected against HBV at age 14-15 years.
Study details: This was a prospective study of antibody persistence and immune memory in 268 teens aged 14-15 before and 1 month after receiving a booster challenge HBV monovalent vaccine.
Disclosures: The presenter reported serving as a consultant to GlaxoSmithKline, which funded the study, as well as to Pfizer and Sanofi Pasteur.
Skip ultrasound in acute UTI in small children
MALMO, SWEDEN – Ultrasound of the kidneys and urinary tract in the acute phase of a first urinary tract infection in young children has an unacceptably high false-positive rate, Magdalena Okarska-Napierala, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“Sonography performed 2 weeks after treatment initiation seems to be more reliable,” said Dr. Okarska-Napierala, a pediatrician at the Medical University of Warsaw Children’s Hospital.
Broad agreement exists that imaging is warranted in all children with a first urinary tract infection (UTI), because this infection can be the first signal of a structural abnormality of the kidneys or urinary tract. Abdominal ultrasound is the first-choice imaging modality in this setting because it is noninvasive, widely available, and inexpensive. But there remains controversy – and guidelines differ – regarding when to perform the ultrasound in children with UTI who respond well to therapy. This was the impetus for Dr. Okarska-Napierala and her coinvestigators to launch a prospective, single-center study examining the issue.
“The theory beneath it is the possibility that diffuse inflammation affects the ultrasound picture of the kidneys and urinary tract and may give us false-positive results, so we shouldn’t base our decisions on those results,” she explained.
This theory has been provisionally confirmed by the preliminary results of the study, which is continuing to enroll patients.
To date, the study includes 48 children, mean age 10.4 months, hospitalized for their first UTI. Participation was restricted to patients with no known congenital abnormalities of the kidneys or urinary tract and who were not on antibiotics at enrollment. Of the 48 children, 44 had an Escherichia coli infection. The predominant treatment was a second-generation cephalosporin for a median of 10 days.
On day 1 of treatment all patients underwent an ultrasound exam evaluating kidney size, anterior-posterior renal pelvis diameter, and the urinary tract based upon a grading system for urinary tract dilation developed by multidisciplinary consensus (J Pediatr Urol. 2014 Dec;10[6]:982-98). The ultrasound exam was repeated 2 weeks later, and again 2 weeks after that.
The most striking findings were a significantly increased kidney size and more prevalent urinary tract dilation on the day 1 ultrasound exam than on repeat ultrasound 2 weeks later. The average length of the left and right kidneys was 67.0 and 64.5 mm, respectively, on day 1, dropping off to 64.3 and 62.0 mm at 2 weeks, with a smaller and statistically nonsignificant further drop-off to 61.9 and 60.0 mm on the week 4 ultrasound.
“We saw a strong correlation between initial kidney size and CRP [C-reactive protein] value: The higher the CRP you have initially, the bigger the kidneys. It’s an interesting finding, but not so very practical. The only practical conclusion is that if we perform ultrasound at this stage and the child has big kidneys, it doesn’t mean anything. We have to check it again later,” she said.
Also, the number of renal units with urinary tract dilation went from 29 on day 1 ultrasound to 20 at 2 weeks and 19 at 4 weeks. Of the 48 children, 28 had urinary tract dilation on day 1, compared with 18 at 2 weeks and 16 at 4 weeks.
“If we look at this practically, if we base our decision on the day 1 ultrasound we would qualify half of all children for voiding cystourethrography, which is harmful, but if we wait 2 weeks to do the ultrasound we would reduce this number by six children. So I think we can call this a clinically significant difference,” she continued.
Of the 48 children, 11 have undergone voiding cystourethrography, revealing 2 mild cases of vesicoureteral reflux, which is the most common congenital abnormality of the urinary tract.
“I would like to emphasize that there is no real benefit in performing an ultrasound exam in children in this acute phase of infection. And there is harm in that we have to repeat the exam later, the parents are worried, the doctor is worried,” Dr. Okarska-Napierala concluded.
She reported having no relevant financial conflicts, and the study was conducted free of commercial support.
MALMO, SWEDEN – Ultrasound of the kidneys and urinary tract in the acute phase of a first urinary tract infection in young children has an unacceptably high false-positive rate, Magdalena Okarska-Napierala, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“Sonography performed 2 weeks after treatment initiation seems to be more reliable,” said Dr. Okarska-Napierala, a pediatrician at the Medical University of Warsaw Children’s Hospital.
Broad agreement exists that imaging is warranted in all children with a first urinary tract infection (UTI), because this infection can be the first signal of a structural abnormality of the kidneys or urinary tract. Abdominal ultrasound is the first-choice imaging modality in this setting because it is noninvasive, widely available, and inexpensive. But there remains controversy – and guidelines differ – regarding when to perform the ultrasound in children with UTI who respond well to therapy. This was the impetus for Dr. Okarska-Napierala and her coinvestigators to launch a prospective, single-center study examining the issue.
“The theory beneath it is the possibility that diffuse inflammation affects the ultrasound picture of the kidneys and urinary tract and may give us false-positive results, so we shouldn’t base our decisions on those results,” she explained.
This theory has been provisionally confirmed by the preliminary results of the study, which is continuing to enroll patients.
To date, the study includes 48 children, mean age 10.4 months, hospitalized for their first UTI. Participation was restricted to patients with no known congenital abnormalities of the kidneys or urinary tract and who were not on antibiotics at enrollment. Of the 48 children, 44 had an Escherichia coli infection. The predominant treatment was a second-generation cephalosporin for a median of 10 days.
On day 1 of treatment all patients underwent an ultrasound exam evaluating kidney size, anterior-posterior renal pelvis diameter, and the urinary tract based upon a grading system for urinary tract dilation developed by multidisciplinary consensus (J Pediatr Urol. 2014 Dec;10[6]:982-98). The ultrasound exam was repeated 2 weeks later, and again 2 weeks after that.
The most striking findings were a significantly increased kidney size and more prevalent urinary tract dilation on the day 1 ultrasound exam than on repeat ultrasound 2 weeks later. The average length of the left and right kidneys was 67.0 and 64.5 mm, respectively, on day 1, dropping off to 64.3 and 62.0 mm at 2 weeks, with a smaller and statistically nonsignificant further drop-off to 61.9 and 60.0 mm on the week 4 ultrasound.
“We saw a strong correlation between initial kidney size and CRP [C-reactive protein] value: The higher the CRP you have initially, the bigger the kidneys. It’s an interesting finding, but not so very practical. The only practical conclusion is that if we perform ultrasound at this stage and the child has big kidneys, it doesn’t mean anything. We have to check it again later,” she said.
Also, the number of renal units with urinary tract dilation went from 29 on day 1 ultrasound to 20 at 2 weeks and 19 at 4 weeks. Of the 48 children, 28 had urinary tract dilation on day 1, compared with 18 at 2 weeks and 16 at 4 weeks.
“If we look at this practically, if we base our decision on the day 1 ultrasound we would qualify half of all children for voiding cystourethrography, which is harmful, but if we wait 2 weeks to do the ultrasound we would reduce this number by six children. So I think we can call this a clinically significant difference,” she continued.
Of the 48 children, 11 have undergone voiding cystourethrography, revealing 2 mild cases of vesicoureteral reflux, which is the most common congenital abnormality of the urinary tract.
“I would like to emphasize that there is no real benefit in performing an ultrasound exam in children in this acute phase of infection. And there is harm in that we have to repeat the exam later, the parents are worried, the doctor is worried,” Dr. Okarska-Napierala concluded.
She reported having no relevant financial conflicts, and the study was conducted free of commercial support.
MALMO, SWEDEN – Ultrasound of the kidneys and urinary tract in the acute phase of a first urinary tract infection in young children has an unacceptably high false-positive rate, Magdalena Okarska-Napierala, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“Sonography performed 2 weeks after treatment initiation seems to be more reliable,” said Dr. Okarska-Napierala, a pediatrician at the Medical University of Warsaw Children’s Hospital.
Broad agreement exists that imaging is warranted in all children with a first urinary tract infection (UTI), because this infection can be the first signal of a structural abnormality of the kidneys or urinary tract. Abdominal ultrasound is the first-choice imaging modality in this setting because it is noninvasive, widely available, and inexpensive. But there remains controversy – and guidelines differ – regarding when to perform the ultrasound in children with UTI who respond well to therapy. This was the impetus for Dr. Okarska-Napierala and her coinvestigators to launch a prospective, single-center study examining the issue.
“The theory beneath it is the possibility that diffuse inflammation affects the ultrasound picture of the kidneys and urinary tract and may give us false-positive results, so we shouldn’t base our decisions on those results,” she explained.
This theory has been provisionally confirmed by the preliminary results of the study, which is continuing to enroll patients.
To date, the study includes 48 children, mean age 10.4 months, hospitalized for their first UTI. Participation was restricted to patients with no known congenital abnormalities of the kidneys or urinary tract and who were not on antibiotics at enrollment. Of the 48 children, 44 had an Escherichia coli infection. The predominant treatment was a second-generation cephalosporin for a median of 10 days.
On day 1 of treatment all patients underwent an ultrasound exam evaluating kidney size, anterior-posterior renal pelvis diameter, and the urinary tract based upon a grading system for urinary tract dilation developed by multidisciplinary consensus (J Pediatr Urol. 2014 Dec;10[6]:982-98). The ultrasound exam was repeated 2 weeks later, and again 2 weeks after that.
The most striking findings were a significantly increased kidney size and more prevalent urinary tract dilation on the day 1 ultrasound exam than on repeat ultrasound 2 weeks later. The average length of the left and right kidneys was 67.0 and 64.5 mm, respectively, on day 1, dropping off to 64.3 and 62.0 mm at 2 weeks, with a smaller and statistically nonsignificant further drop-off to 61.9 and 60.0 mm on the week 4 ultrasound.
“We saw a strong correlation between initial kidney size and CRP [C-reactive protein] value: The higher the CRP you have initially, the bigger the kidneys. It’s an interesting finding, but not so very practical. The only practical conclusion is that if we perform ultrasound at this stage and the child has big kidneys, it doesn’t mean anything. We have to check it again later,” she said.
Also, the number of renal units with urinary tract dilation went from 29 on day 1 ultrasound to 20 at 2 weeks and 19 at 4 weeks. Of the 48 children, 28 had urinary tract dilation on day 1, compared with 18 at 2 weeks and 16 at 4 weeks.
“If we look at this practically, if we base our decision on the day 1 ultrasound we would qualify half of all children for voiding cystourethrography, which is harmful, but if we wait 2 weeks to do the ultrasound we would reduce this number by six children. So I think we can call this a clinically significant difference,” she continued.
Of the 48 children, 11 have undergone voiding cystourethrography, revealing 2 mild cases of vesicoureteral reflux, which is the most common congenital abnormality of the urinary tract.
“I would like to emphasize that there is no real benefit in performing an ultrasound exam in children in this acute phase of infection. And there is harm in that we have to repeat the exam later, the parents are worried, the doctor is worried,” Dr. Okarska-Napierala concluded.
She reported having no relevant financial conflicts, and the study was conducted free of commercial support.
REPORTING FROM ESPID 2018
Key clinical point:
Major finding: Average left kidney length dropped from 67.0 mm on treatment day 1 to 64.3 mm 2 weeks later.
Study details: This interim report from an ongoing, prospective, single-center study included 48 children up to age 3 years who were hospitalized for their first urinary tract infection.
Disclosures: The presenter reported no relevant financial conflicts.
Reducing risk of febrile convulsion after first dose of MMRV
MALMO, SWEDEN – Giving a combined MMR vaccine and a varicella vaccine separately on the same day in children with personal or family history of febrile convulsions while utilizing the more convenient MMRV vaccine in those without such a history showed promise as a means of reducing the overall risk of febrile convulsions attributable to vaccination, Corinne Willame said at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a post hoc analysis of an enormous, German observational study that demonstrated an increased risk of hospitalization for febrile convulsions 5-12 days after receiving the first dose of the Priorix-Tetra MMRV vaccine, with no alternative plausible cause of the convulsions (Vaccine. 2014 Feb 3;32[6]:645-50).
The original study was conducted in more than 180,000 children under the age of 5 years, 90% of whom were 11- 23 months. The increased risk associated with MMRV, compared with MMR alone or MMR plus V separately on the same day, was similar in magnitude to what had previously been reported for the ProQuad MMRV vaccine, suggesting a class effect for the quadrivalent vaccines.
Because genetic predisposition is known to be associated with increased risk of febrile convulsions, Ms. Willame of GlaxoSmithKline in Wavre, Belgium, and her coinvestigators conducted an exploratory analysis investigating whether the presence of a personal or first-degree family history of febrile convulsions impacted the risk of developing febrile convulsions following a first dose of MMRV, compared with MMR alone or MMR and V administered separately on the same day. They found that indeed it did, according to Ms. Willame.
They analyzed the data in multiple ways. The first scenario compared the risk of febrile convulsions in 74,631 children 5-12 days after receiving the MMRV vaccine with a roughly equal number of children who received the MMR vaccine. Study subjects were matched for age, sex, month of vaccination, and insurance provider. The febrile convulsion incidence rate was 6.03 cases per 10,000 children in MMRV recipients and 2.55 per 10,000 in those who got MMR. Then they reanalyzed the data after subtracting all children with a baseline personal history of febrile convulsions from the pool of MMRV recipients: The febrile convulsion rate in the MMRV group dropped to 5.27 cases per 10,000.
Next, they did the same analysis in more than 64,000 matched children who got either MMRV or MMR plus V separately. For the whole cohort of MMRV recipients, the febrile convulsion rate was 6.53 cases per 10,000 vaccine recipients, dropping to 5.95 per 10,000 if children with a personal history of febrile convulsions were removed. The relative risk of febrile convulsions was 150% greater in the overall MMRV group than with MMR plus V, but only 58% greater when the children with a personal history of febrile seizures were excluded from the MMRV population.
Unfortunately, the parent study didn’t record whether a history of febrile convulsions was present in first-degree family members. The investigators therefore turned to the published literature on the subject and constructed conditional probability analyses based upon a 20%-40% likelihood of a positive family history in children with a personal history, and a 5% likelihood in those children without such a history. In this scenario, when children with a personal or hypothetical family history of febrile convulsions were subtracted from the MMRV group, the result was a febrile convulsion incidence rate of 3.27-4.41 cases per 10,000 MMRV recipients in the comparison with MMR and 3.63-4.95 per 10,000 in the comparison with MMR plus V.
Ms. Willame emphasized that her analysis must be considered hypothesis generating because it’s post hoc and relies upon published estimates of the prevalence of a positive family history of febrile convulsions. The febrile convulsion risk differences she found with the different vaccination strategies should be confirmed in studies that collect family history data of febrile seizures at an individual level.
Her study was funded by her employer, GlaxoSmithKline.
MALMO, SWEDEN – Giving a combined MMR vaccine and a varicella vaccine separately on the same day in children with personal or family history of febrile convulsions while utilizing the more convenient MMRV vaccine in those without such a history showed promise as a means of reducing the overall risk of febrile convulsions attributable to vaccination, Corinne Willame said at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a post hoc analysis of an enormous, German observational study that demonstrated an increased risk of hospitalization for febrile convulsions 5-12 days after receiving the first dose of the Priorix-Tetra MMRV vaccine, with no alternative plausible cause of the convulsions (Vaccine. 2014 Feb 3;32[6]:645-50).
The original study was conducted in more than 180,000 children under the age of 5 years, 90% of whom were 11- 23 months. The increased risk associated with MMRV, compared with MMR alone or MMR plus V separately on the same day, was similar in magnitude to what had previously been reported for the ProQuad MMRV vaccine, suggesting a class effect for the quadrivalent vaccines.
Because genetic predisposition is known to be associated with increased risk of febrile convulsions, Ms. Willame of GlaxoSmithKline in Wavre, Belgium, and her coinvestigators conducted an exploratory analysis investigating whether the presence of a personal or first-degree family history of febrile convulsions impacted the risk of developing febrile convulsions following a first dose of MMRV, compared with MMR alone or MMR and V administered separately on the same day. They found that indeed it did, according to Ms. Willame.
They analyzed the data in multiple ways. The first scenario compared the risk of febrile convulsions in 74,631 children 5-12 days after receiving the MMRV vaccine with a roughly equal number of children who received the MMR vaccine. Study subjects were matched for age, sex, month of vaccination, and insurance provider. The febrile convulsion incidence rate was 6.03 cases per 10,000 children in MMRV recipients and 2.55 per 10,000 in those who got MMR. Then they reanalyzed the data after subtracting all children with a baseline personal history of febrile convulsions from the pool of MMRV recipients: The febrile convulsion rate in the MMRV group dropped to 5.27 cases per 10,000.
Next, they did the same analysis in more than 64,000 matched children who got either MMRV or MMR plus V separately. For the whole cohort of MMRV recipients, the febrile convulsion rate was 6.53 cases per 10,000 vaccine recipients, dropping to 5.95 per 10,000 if children with a personal history of febrile convulsions were removed. The relative risk of febrile convulsions was 150% greater in the overall MMRV group than with MMR plus V, but only 58% greater when the children with a personal history of febrile seizures were excluded from the MMRV population.
Unfortunately, the parent study didn’t record whether a history of febrile convulsions was present in first-degree family members. The investigators therefore turned to the published literature on the subject and constructed conditional probability analyses based upon a 20%-40% likelihood of a positive family history in children with a personal history, and a 5% likelihood in those children without such a history. In this scenario, when children with a personal or hypothetical family history of febrile convulsions were subtracted from the MMRV group, the result was a febrile convulsion incidence rate of 3.27-4.41 cases per 10,000 MMRV recipients in the comparison with MMR and 3.63-4.95 per 10,000 in the comparison with MMR plus V.
Ms. Willame emphasized that her analysis must be considered hypothesis generating because it’s post hoc and relies upon published estimates of the prevalence of a positive family history of febrile convulsions. The febrile convulsion risk differences she found with the different vaccination strategies should be confirmed in studies that collect family history data of febrile seizures at an individual level.
Her study was funded by her employer, GlaxoSmithKline.
MALMO, SWEDEN – Giving a combined MMR vaccine and a varicella vaccine separately on the same day in children with personal or family history of febrile convulsions while utilizing the more convenient MMRV vaccine in those without such a history showed promise as a means of reducing the overall risk of febrile convulsions attributable to vaccination, Corinne Willame said at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a post hoc analysis of an enormous, German observational study that demonstrated an increased risk of hospitalization for febrile convulsions 5-12 days after receiving the first dose of the Priorix-Tetra MMRV vaccine, with no alternative plausible cause of the convulsions (Vaccine. 2014 Feb 3;32[6]:645-50).
The original study was conducted in more than 180,000 children under the age of 5 years, 90% of whom were 11- 23 months. The increased risk associated with MMRV, compared with MMR alone or MMR plus V separately on the same day, was similar in magnitude to what had previously been reported for the ProQuad MMRV vaccine, suggesting a class effect for the quadrivalent vaccines.
Because genetic predisposition is known to be associated with increased risk of febrile convulsions, Ms. Willame of GlaxoSmithKline in Wavre, Belgium, and her coinvestigators conducted an exploratory analysis investigating whether the presence of a personal or first-degree family history of febrile convulsions impacted the risk of developing febrile convulsions following a first dose of MMRV, compared with MMR alone or MMR and V administered separately on the same day. They found that indeed it did, according to Ms. Willame.
They analyzed the data in multiple ways. The first scenario compared the risk of febrile convulsions in 74,631 children 5-12 days after receiving the MMRV vaccine with a roughly equal number of children who received the MMR vaccine. Study subjects were matched for age, sex, month of vaccination, and insurance provider. The febrile convulsion incidence rate was 6.03 cases per 10,000 children in MMRV recipients and 2.55 per 10,000 in those who got MMR. Then they reanalyzed the data after subtracting all children with a baseline personal history of febrile convulsions from the pool of MMRV recipients: The febrile convulsion rate in the MMRV group dropped to 5.27 cases per 10,000.
Next, they did the same analysis in more than 64,000 matched children who got either MMRV or MMR plus V separately. For the whole cohort of MMRV recipients, the febrile convulsion rate was 6.53 cases per 10,000 vaccine recipients, dropping to 5.95 per 10,000 if children with a personal history of febrile convulsions were removed. The relative risk of febrile convulsions was 150% greater in the overall MMRV group than with MMR plus V, but only 58% greater when the children with a personal history of febrile seizures were excluded from the MMRV population.
Unfortunately, the parent study didn’t record whether a history of febrile convulsions was present in first-degree family members. The investigators therefore turned to the published literature on the subject and constructed conditional probability analyses based upon a 20%-40% likelihood of a positive family history in children with a personal history, and a 5% likelihood in those children without such a history. In this scenario, when children with a personal or hypothetical family history of febrile convulsions were subtracted from the MMRV group, the result was a febrile convulsion incidence rate of 3.27-4.41 cases per 10,000 MMRV recipients in the comparison with MMR and 3.63-4.95 per 10,000 in the comparison with MMR plus V.
Ms. Willame emphasized that her analysis must be considered hypothesis generating because it’s post hoc and relies upon published estimates of the prevalence of a positive family history of febrile convulsions. The febrile convulsion risk differences she found with the different vaccination strategies should be confirmed in studies that collect family history data of febrile seizures at an individual level.
Her study was funded by her employer, GlaxoSmithKline.
REPORTING FROM ESPID 2018
Key clinical point: The increased risk of febrile seizures associated with MMRV vaccine can probably be reduced by administering the MMR and varicella vaccines separately on the same day in children with a personal or family history of febrile seizures.
Major finding: The incidence rate of febrile seizures 5-12 days post MMRV vaccination was reduced from 6.53 to 3.63-4.95 cases per 10,000 vaccine recipients.
Study details: This was a post hoc analysis of an observational study of more than 180,000 German children.
Disclosures: The study was sponsored by GlaxoSmithKline and presented by a company employee.
European experts envy U.S. pediatric flu vaccination approach
MALMO, SWEDEN – When American physicians think about health care in Europe, what typically comes to mind are government-funded, single-payer national health services with cradle-to-grave coverage of essential services, a strong public health bent, and perhaps some queuing.
“It’s complicated. There is no common strategic approach,” Hanna Nohynek, MD, PhD, observed at a session on childhood immunization against flu held during the annual meeting of the European Society for Paediatric Infectious Diseases.
“In real life, influenza coverage among [European] children is either not known or quite low. Impact assessments in children are done in only a few countries,” said Dr. Nohynek, chief physician in the infectious diseases control and vaccinations unit of the National Institute for Health and Welfare in Helsinki, Finland.
“The only country doing as well coverage-wise as the U.S. is the U.K., with rates of 50%-65%. In Finland it’s less than 40%,” according to Dr. Nohynek.
“We have 28 countries today in the E.U. [European Union], and we have 28 different recommendations in Europe. So where do we go from here? It’s really not easy,” observed session cochair Alberticus Osterhaus, DVM, PhD, emeritus professor of virology at Erasmus University in Rotterdam, the Netherlands.
For all the oft-cited shortcomings of health care in the United States, That’s why Jon S. Abramson, MD, a former chair of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP), was invited to explain how the U.S. strategy was accomplished.
The U.S. approach
The current U.S. policy, implemented in 2010, is to recommend an annual flu shot for all persons older than 6 months of age.
Influenza vaccination has been part of the U.S. public health program since 1960. Children aged 6-23 months, as well as their household contacts and women who will be pregnant during flu season, were added in 2004. In 2006, the flu vaccine recommendation was expanded to include children aged 6-59 months as a result of persuasive data showing that the rate of flu-associated hospitalizations and deaths in children up to 4 years old was second only to the rate in the elderly population.
The rationale for expanding the recommendation to include all school-age children and adolescents stemmed from evidence that the highest average flu-related illness rate in the United States was in that age group, which confirmed that schools are a powerful vector for the spread of influenza. Vaccinating this age-group also was seen as having an indirect benefit for their household contacts.
The current policy of recommending vaccination of everyone over age 6 months was adopted because it checked off a lot of boxes: “It’s a single recommendation, easy to apply; it eliminates the need to look for indications and risk factors; it increases vaccination coverage rates; annual vaccination is safe and effective; and flu-related morbidity and mortality occur in all age groups,” Dr. Abramson continued.
The rate of influenza vaccine coverage in pregnant women has improved over time from less than 15% to about 50%. To place that in perspective, however, the rate in Argentina is 95%, the pediatrician noted.
“We’re doing better in children than we are in adults in terms of seasonal coverage rates,” he added. “In 2015, it was 59%, versus 42% in adults.”
Dr. Abramson said there remains some skepticism in the United States regarding the effectiveness of flu vaccines in preventing flu-related illness. That’s because of the difficulty in communicating that vaccine effectiveness varies from year to year, sometimes substantially, depending upon two factors: the transmission characteristics of the circulating strains and how well the vaccines match up against those strains.
“I think we have to learn to live with that. I don’t think we’ll see a universal flu vaccine that we can give once every 10 years,” he said.
“The bottom line is, even if a vaccine is only 50% efficacious overall, we’re still impacting huge numbers,” the pediatrician added.
Dr. Abramson cited a CDC estimate that, for the 2012-2013 season, where the vaccine was 49% efficacious, the result of vaccination was 6.6 million fewer cases of influenza-associated illnesses nationally, 3.2 million fewer flu-associated medical visits, and 79,000 hospitalizations avoided.
“I think we have a fairly good program in the United States. We’re doing well in children. We certainly could be doing better. Not having FluMist for the past 2 seasons probably hurt us some,” according to Dr. Abramson.
The FluMist experience
The FluMist episode is viewed by many European pediatric infectious disease experts as a debacle. Europeans eager to develop a pan-European strategy for seasonal immunization against influenza in children and adolescents viewed the U.S. FluMist episode with dismay. For the 2016-2017 and 2017-2018 flu seasons, the ACIP recommended against FluMist, a previously approved intranasally administered quadrivalent live attenuated virus vaccine, on the basis of a single study showing subpar effectiveness against influenza A H1NI. Then at its October 2017 meeting, ACIP reversed itself and reinstated FluMist for the 2018-2019 season after viewing data from Finland and several other countries demonstrating that, in countries where it hadn’t been taken off the market, the vaccine had performed as well as injectable inactivated influenza vaccines in the 2016-2017 flu season.
“I think from the European side, it’s been a bit of a sorry spectacle,” commented Dr. Osterhaus, referring to the ACIP’s waffling. After all, authorities in Canada and European countries where FluMist was available had looked at the same data that caused ACIP to derecommend the vaccine but hadn’t found it convincing.
“We’re very happy to see ACIP has reinstated the vaccine,” Dr. Nohynek said.
Dr. Abramson declined to defend the ACIP decision to drop FluMist.
“From my standpoint, knowing that influenza B kills more children than A does, if I had been on the ACIP committee – and I’m not anymore – that would not have been my vote,” he said. “Whatever you want to say about the live attenuated influenza vaccine, about how good it is against some A strains or not, it’s better than other vaccines against influenza B. And the death rate is higher from B than A in children, although that is not true in adults.”
Plus, FluMist was an important option for people avoiding immunization because they dislike shots.
“The vast majority of deaths due to flu in children in 2010-2016 have been in kids who didn’t get vaccinated,” he noted.
Dr. Nohynek said the Finnish real-world experience recorded in comprehensive national registries for the 2017-2018 flu season – a bad year for vaccine/virus mismatch in Europe – confirmed Dr. Abramson’s comments about the superiority of quadrivalent live attenuated influenza vaccine against influenza B. Among 54,611 Finnish children aged 24-35 months, the laboratory-confirmed vaccine effectiveness of trivalent inactivated virus vaccine, with 9% coverage, was 4.5% for influenza A and 12.2% for influenza B. In contrast, the vaccine effectiveness for the intranasal quadrivalent live attenuated influenza vaccine was 32% for A and a whopping 80% for B.
“It’s quite amazing, at least to me, to see figures like this in real world data,” she commented.
Session cochair Adam Finn, MD, PhD, said he has found it instructive to take a closer look at the U.K. data for the past several flu seasons.
“We’ve seen greater control of the epidemic in Scotland and Northern Ireland, where coverage in primary school kids was higher, in the 60%-70% area, and lower in England and Wales, where it was more like 50%. So we’re beginning to think that’s the kind of level of annual coverage in children we might need to suppress an epidemic. I think that’s a really important message that people should understand: We’re not looking for 95% coverage,” observed Dr. Finn, aprofessor of pediatrics at the University of Bristol (England).
Vaccine effectiveness will improve
Dr. Osterhaus predicted better times are coming in terms of vaccine effectiveness. Vaccine production times will become shorter as recombinant technologies replace the traditional lengthy chicken egg-based vaccine production; as a result, there will be less drift-associated mismatch. Improved surveillance, including the ability to follow strain mobility patterns and population-based antibody landscapes, are another important advance.
“We’ve always been looking at one side of the coin: the virus. Once or twice a year eminent gray people sitting together in Geneva at WHO decide which strains should be selected for the next vaccine. But if you know what antibodies are present in the population, this can be quite important information as well,” he said.
Dr. Nohynek reported receiving research funding from GlaxoSmithKline and Pfizer. The other speakers reported having no relevant financial conflicts of interest.
MALMO, SWEDEN – When American physicians think about health care in Europe, what typically comes to mind are government-funded, single-payer national health services with cradle-to-grave coverage of essential services, a strong public health bent, and perhaps some queuing.
“It’s complicated. There is no common strategic approach,” Hanna Nohynek, MD, PhD, observed at a session on childhood immunization against flu held during the annual meeting of the European Society for Paediatric Infectious Diseases.
“In real life, influenza coverage among [European] children is either not known or quite low. Impact assessments in children are done in only a few countries,” said Dr. Nohynek, chief physician in the infectious diseases control and vaccinations unit of the National Institute for Health and Welfare in Helsinki, Finland.
“The only country doing as well coverage-wise as the U.S. is the U.K., with rates of 50%-65%. In Finland it’s less than 40%,” according to Dr. Nohynek.
“We have 28 countries today in the E.U. [European Union], and we have 28 different recommendations in Europe. So where do we go from here? It’s really not easy,” observed session cochair Alberticus Osterhaus, DVM, PhD, emeritus professor of virology at Erasmus University in Rotterdam, the Netherlands.
For all the oft-cited shortcomings of health care in the United States, That’s why Jon S. Abramson, MD, a former chair of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP), was invited to explain how the U.S. strategy was accomplished.
The U.S. approach
The current U.S. policy, implemented in 2010, is to recommend an annual flu shot for all persons older than 6 months of age.
Influenza vaccination has been part of the U.S. public health program since 1960. Children aged 6-23 months, as well as their household contacts and women who will be pregnant during flu season, were added in 2004. In 2006, the flu vaccine recommendation was expanded to include children aged 6-59 months as a result of persuasive data showing that the rate of flu-associated hospitalizations and deaths in children up to 4 years old was second only to the rate in the elderly population.
The rationale for expanding the recommendation to include all school-age children and adolescents stemmed from evidence that the highest average flu-related illness rate in the United States was in that age group, which confirmed that schools are a powerful vector for the spread of influenza. Vaccinating this age-group also was seen as having an indirect benefit for their household contacts.
The current policy of recommending vaccination of everyone over age 6 months was adopted because it checked off a lot of boxes: “It’s a single recommendation, easy to apply; it eliminates the need to look for indications and risk factors; it increases vaccination coverage rates; annual vaccination is safe and effective; and flu-related morbidity and mortality occur in all age groups,” Dr. Abramson continued.
The rate of influenza vaccine coverage in pregnant women has improved over time from less than 15% to about 50%. To place that in perspective, however, the rate in Argentina is 95%, the pediatrician noted.
“We’re doing better in children than we are in adults in terms of seasonal coverage rates,” he added. “In 2015, it was 59%, versus 42% in adults.”
Dr. Abramson said there remains some skepticism in the United States regarding the effectiveness of flu vaccines in preventing flu-related illness. That’s because of the difficulty in communicating that vaccine effectiveness varies from year to year, sometimes substantially, depending upon two factors: the transmission characteristics of the circulating strains and how well the vaccines match up against those strains.
“I think we have to learn to live with that. I don’t think we’ll see a universal flu vaccine that we can give once every 10 years,” he said.
“The bottom line is, even if a vaccine is only 50% efficacious overall, we’re still impacting huge numbers,” the pediatrician added.
Dr. Abramson cited a CDC estimate that, for the 2012-2013 season, where the vaccine was 49% efficacious, the result of vaccination was 6.6 million fewer cases of influenza-associated illnesses nationally, 3.2 million fewer flu-associated medical visits, and 79,000 hospitalizations avoided.
“I think we have a fairly good program in the United States. We’re doing well in children. We certainly could be doing better. Not having FluMist for the past 2 seasons probably hurt us some,” according to Dr. Abramson.
The FluMist experience
The FluMist episode is viewed by many European pediatric infectious disease experts as a debacle. Europeans eager to develop a pan-European strategy for seasonal immunization against influenza in children and adolescents viewed the U.S. FluMist episode with dismay. For the 2016-2017 and 2017-2018 flu seasons, the ACIP recommended against FluMist, a previously approved intranasally administered quadrivalent live attenuated virus vaccine, on the basis of a single study showing subpar effectiveness against influenza A H1NI. Then at its October 2017 meeting, ACIP reversed itself and reinstated FluMist for the 2018-2019 season after viewing data from Finland and several other countries demonstrating that, in countries where it hadn’t been taken off the market, the vaccine had performed as well as injectable inactivated influenza vaccines in the 2016-2017 flu season.
“I think from the European side, it’s been a bit of a sorry spectacle,” commented Dr. Osterhaus, referring to the ACIP’s waffling. After all, authorities in Canada and European countries where FluMist was available had looked at the same data that caused ACIP to derecommend the vaccine but hadn’t found it convincing.
“We’re very happy to see ACIP has reinstated the vaccine,” Dr. Nohynek said.
Dr. Abramson declined to defend the ACIP decision to drop FluMist.
“From my standpoint, knowing that influenza B kills more children than A does, if I had been on the ACIP committee – and I’m not anymore – that would not have been my vote,” he said. “Whatever you want to say about the live attenuated influenza vaccine, about how good it is against some A strains or not, it’s better than other vaccines against influenza B. And the death rate is higher from B than A in children, although that is not true in adults.”
Plus, FluMist was an important option for people avoiding immunization because they dislike shots.
“The vast majority of deaths due to flu in children in 2010-2016 have been in kids who didn’t get vaccinated,” he noted.
Dr. Nohynek said the Finnish real-world experience recorded in comprehensive national registries for the 2017-2018 flu season – a bad year for vaccine/virus mismatch in Europe – confirmed Dr. Abramson’s comments about the superiority of quadrivalent live attenuated influenza vaccine against influenza B. Among 54,611 Finnish children aged 24-35 months, the laboratory-confirmed vaccine effectiveness of trivalent inactivated virus vaccine, with 9% coverage, was 4.5% for influenza A and 12.2% for influenza B. In contrast, the vaccine effectiveness for the intranasal quadrivalent live attenuated influenza vaccine was 32% for A and a whopping 80% for B.
“It’s quite amazing, at least to me, to see figures like this in real world data,” she commented.
Session cochair Adam Finn, MD, PhD, said he has found it instructive to take a closer look at the U.K. data for the past several flu seasons.
“We’ve seen greater control of the epidemic in Scotland and Northern Ireland, where coverage in primary school kids was higher, in the 60%-70% area, and lower in England and Wales, where it was more like 50%. So we’re beginning to think that’s the kind of level of annual coverage in children we might need to suppress an epidemic. I think that’s a really important message that people should understand: We’re not looking for 95% coverage,” observed Dr. Finn, aprofessor of pediatrics at the University of Bristol (England).
Vaccine effectiveness will improve
Dr. Osterhaus predicted better times are coming in terms of vaccine effectiveness. Vaccine production times will become shorter as recombinant technologies replace the traditional lengthy chicken egg-based vaccine production; as a result, there will be less drift-associated mismatch. Improved surveillance, including the ability to follow strain mobility patterns and population-based antibody landscapes, are another important advance.
“We’ve always been looking at one side of the coin: the virus. Once or twice a year eminent gray people sitting together in Geneva at WHO decide which strains should be selected for the next vaccine. But if you know what antibodies are present in the population, this can be quite important information as well,” he said.
Dr. Nohynek reported receiving research funding from GlaxoSmithKline and Pfizer. The other speakers reported having no relevant financial conflicts of interest.
MALMO, SWEDEN – When American physicians think about health care in Europe, what typically comes to mind are government-funded, single-payer national health services with cradle-to-grave coverage of essential services, a strong public health bent, and perhaps some queuing.
“It’s complicated. There is no common strategic approach,” Hanna Nohynek, MD, PhD, observed at a session on childhood immunization against flu held during the annual meeting of the European Society for Paediatric Infectious Diseases.
“In real life, influenza coverage among [European] children is either not known or quite low. Impact assessments in children are done in only a few countries,” said Dr. Nohynek, chief physician in the infectious diseases control and vaccinations unit of the National Institute for Health and Welfare in Helsinki, Finland.
“The only country doing as well coverage-wise as the U.S. is the U.K., with rates of 50%-65%. In Finland it’s less than 40%,” according to Dr. Nohynek.
“We have 28 countries today in the E.U. [European Union], and we have 28 different recommendations in Europe. So where do we go from here? It’s really not easy,” observed session cochair Alberticus Osterhaus, DVM, PhD, emeritus professor of virology at Erasmus University in Rotterdam, the Netherlands.
For all the oft-cited shortcomings of health care in the United States, That’s why Jon S. Abramson, MD, a former chair of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP), was invited to explain how the U.S. strategy was accomplished.
The U.S. approach
The current U.S. policy, implemented in 2010, is to recommend an annual flu shot for all persons older than 6 months of age.
Influenza vaccination has been part of the U.S. public health program since 1960. Children aged 6-23 months, as well as their household contacts and women who will be pregnant during flu season, were added in 2004. In 2006, the flu vaccine recommendation was expanded to include children aged 6-59 months as a result of persuasive data showing that the rate of flu-associated hospitalizations and deaths in children up to 4 years old was second only to the rate in the elderly population.
The rationale for expanding the recommendation to include all school-age children and adolescents stemmed from evidence that the highest average flu-related illness rate in the United States was in that age group, which confirmed that schools are a powerful vector for the spread of influenza. Vaccinating this age-group also was seen as having an indirect benefit for their household contacts.
The current policy of recommending vaccination of everyone over age 6 months was adopted because it checked off a lot of boxes: “It’s a single recommendation, easy to apply; it eliminates the need to look for indications and risk factors; it increases vaccination coverage rates; annual vaccination is safe and effective; and flu-related morbidity and mortality occur in all age groups,” Dr. Abramson continued.
The rate of influenza vaccine coverage in pregnant women has improved over time from less than 15% to about 50%. To place that in perspective, however, the rate in Argentina is 95%, the pediatrician noted.
“We’re doing better in children than we are in adults in terms of seasonal coverage rates,” he added. “In 2015, it was 59%, versus 42% in adults.”
Dr. Abramson said there remains some skepticism in the United States regarding the effectiveness of flu vaccines in preventing flu-related illness. That’s because of the difficulty in communicating that vaccine effectiveness varies from year to year, sometimes substantially, depending upon two factors: the transmission characteristics of the circulating strains and how well the vaccines match up against those strains.
“I think we have to learn to live with that. I don’t think we’ll see a universal flu vaccine that we can give once every 10 years,” he said.
“The bottom line is, even if a vaccine is only 50% efficacious overall, we’re still impacting huge numbers,” the pediatrician added.
Dr. Abramson cited a CDC estimate that, for the 2012-2013 season, where the vaccine was 49% efficacious, the result of vaccination was 6.6 million fewer cases of influenza-associated illnesses nationally, 3.2 million fewer flu-associated medical visits, and 79,000 hospitalizations avoided.
“I think we have a fairly good program in the United States. We’re doing well in children. We certainly could be doing better. Not having FluMist for the past 2 seasons probably hurt us some,” according to Dr. Abramson.
The FluMist experience
The FluMist episode is viewed by many European pediatric infectious disease experts as a debacle. Europeans eager to develop a pan-European strategy for seasonal immunization against influenza in children and adolescents viewed the U.S. FluMist episode with dismay. For the 2016-2017 and 2017-2018 flu seasons, the ACIP recommended against FluMist, a previously approved intranasally administered quadrivalent live attenuated virus vaccine, on the basis of a single study showing subpar effectiveness against influenza A H1NI. Then at its October 2017 meeting, ACIP reversed itself and reinstated FluMist for the 2018-2019 season after viewing data from Finland and several other countries demonstrating that, in countries where it hadn’t been taken off the market, the vaccine had performed as well as injectable inactivated influenza vaccines in the 2016-2017 flu season.
“I think from the European side, it’s been a bit of a sorry spectacle,” commented Dr. Osterhaus, referring to the ACIP’s waffling. After all, authorities in Canada and European countries where FluMist was available had looked at the same data that caused ACIP to derecommend the vaccine but hadn’t found it convincing.
“We’re very happy to see ACIP has reinstated the vaccine,” Dr. Nohynek said.
Dr. Abramson declined to defend the ACIP decision to drop FluMist.
“From my standpoint, knowing that influenza B kills more children than A does, if I had been on the ACIP committee – and I’m not anymore – that would not have been my vote,” he said. “Whatever you want to say about the live attenuated influenza vaccine, about how good it is against some A strains or not, it’s better than other vaccines against influenza B. And the death rate is higher from B than A in children, although that is not true in adults.”
Plus, FluMist was an important option for people avoiding immunization because they dislike shots.
“The vast majority of deaths due to flu in children in 2010-2016 have been in kids who didn’t get vaccinated,” he noted.
Dr. Nohynek said the Finnish real-world experience recorded in comprehensive national registries for the 2017-2018 flu season – a bad year for vaccine/virus mismatch in Europe – confirmed Dr. Abramson’s comments about the superiority of quadrivalent live attenuated influenza vaccine against influenza B. Among 54,611 Finnish children aged 24-35 months, the laboratory-confirmed vaccine effectiveness of trivalent inactivated virus vaccine, with 9% coverage, was 4.5% for influenza A and 12.2% for influenza B. In contrast, the vaccine effectiveness for the intranasal quadrivalent live attenuated influenza vaccine was 32% for A and a whopping 80% for B.
“It’s quite amazing, at least to me, to see figures like this in real world data,” she commented.
Session cochair Adam Finn, MD, PhD, said he has found it instructive to take a closer look at the U.K. data for the past several flu seasons.
“We’ve seen greater control of the epidemic in Scotland and Northern Ireland, where coverage in primary school kids was higher, in the 60%-70% area, and lower in England and Wales, where it was more like 50%. So we’re beginning to think that’s the kind of level of annual coverage in children we might need to suppress an epidemic. I think that’s a really important message that people should understand: We’re not looking for 95% coverage,” observed Dr. Finn, aprofessor of pediatrics at the University of Bristol (England).
Vaccine effectiveness will improve
Dr. Osterhaus predicted better times are coming in terms of vaccine effectiveness. Vaccine production times will become shorter as recombinant technologies replace the traditional lengthy chicken egg-based vaccine production; as a result, there will be less drift-associated mismatch. Improved surveillance, including the ability to follow strain mobility patterns and population-based antibody landscapes, are another important advance.
“We’ve always been looking at one side of the coin: the virus. Once or twice a year eminent gray people sitting together in Geneva at WHO decide which strains should be selected for the next vaccine. But if you know what antibodies are present in the population, this can be quite important information as well,” he said.
Dr. Nohynek reported receiving research funding from GlaxoSmithKline and Pfizer. The other speakers reported having no relevant financial conflicts of interest.
EXPERT ANALYSIS FROM ESPID 2018
Bivalent HPV vaccine brings no significant increase in 38 potential adverse outcomes
MALMO, SWEDEN – in a nationwide, retrospective cohort study.
“Anxiety and fear regarding adverse events are still very much alive and are associated with lack of acceptance of HPV vaccination,” Jozica Skufca, DVM, MIPH, observed while presenting the study findings at the annual meeting of the European Society for Paediatric Infectious Diseases.
“These results contribute valid evidence to combat public skepticism, anxiety, fears of adverse events, and possible opposition to HPV vaccination and consequently can contribute to increase HPV vaccination coverage in Finland as well as elsewhere,” added Dr. Skufca, who conducted this research while at the Finnish National Institute for Health and Welfare but is now an epidemiologist at P95, a privately held epidemiology and pharmacovigilance consulting firm in Heverlee, Belgium.
Finland introduced the bivalent HPV vaccine known as Cervarix, which is directed against HPV types 16 and 18, into the nation’s vaccination program in November 2013. The target population were girls aged 11-13 years, with catch-up vaccination at ages 14-15 years until 2015.
Dr. Skufca utilized Finland’s comprehensive system of national health care registries to conduct a study of all 240,605 Finnish girls aged 11-15 years who were eligible for the bivalent HPV vaccine from November 2013 to December 2016. Only 56% of the target population, or 134,615 girls, were actually vaccinated. All were subsequently followed for more than a year.
The investigators compared vaccinated and unvaccinated groups in terms of the subsequent rates of 38 selected outcomes of national and international interest. These included celiac disease, chronic fatigue syndrome, type 1 diabetes, Guillain-Barré syndrome, postural orthostatic tachycardia syndrome, ulcerative colitis, venous thromboembolism, psoriasis, vitiligo, scleroderma, autism, poyarteritis nodosa, asthma, Raynaud’s disease, systemic lupus erythematosus, Bell’s palsy, polycystic ovaries, juvenile arthritis, Hashimoto’s disease, and many others.
HPV vaccination rates varied considerably between hospital districts, so the results were adjusted for that potential confounder. Risks also were adjusted for the number of hospital visits 1-2 years prior to vaccination, because healthier girls – those with fewer hospital visits – turned out to be more likely to get vaccinated.
The study’s main result was that HPV vaccination wasn’t associated with a significantly higher risk of any of the 38 adverse outcomes. To the contrary, vaccination was associated with significantly reduced risk of several of them: The risk of chronic fatigue syndrome was reduced by 25%, epilepsy and recurrent seizures were reduced by 28%, the risk of Henoch-Schönlein purpura was an adjusted 52% lower in children vaccinated against HPV, and the risk of malaise and fatigue was reduced by 24%.
Dr. Skufca drew particular attention to the 400% increased risk of Guillain-Barré syndrome in vaccinated children. While this may look impressive, it wasn’t a statistically significant difference. Guillain-Barré was a rare event, with only six cases occurring during 186,934 person-years of follow-up of vaccinated individuals and a single case in unvaccinated girls. Two cases occurred within 180 days after vaccination, for an adjusted 200% increase in risk, which was nonsignificant.
Another two cases occurred more than 365 days postvaccination, for a whopping 3100% increased risk, compared with unvaccinated children; however, this too was a nonstatistically significant finding, with extraordinarily broad confidence intervals of 1.59-652.4. And there is no plausible mechanism to account for a true association between HPV vaccination and a complication, such as this, occurring more than 1 year later. It appeared to be a matter of chance, she added.
However, session cochair Ron Dagan, MD, commented that vaccine skeptics won’t find the Guillain-Barré findings reassuring.
“With HPV vaccination, there are a lot of issues related to mass perception. You say it’s not statistically significant, but some people will say, ‘Forget about the statistics – look at the confidence intervals, the risk could be more than 600 times increased.’ How do you answer this? It’s not easy, especially when we’re talking about a vaccine which has a strong adjuvant,” said Dr. Dagan, director of the pediatric infectious disease unit at Soroka University Medical Center and professor of pediatrics and infectious diseases at the Ben-Gurion University of the Negev, both in Beer-Sheva, Israel.
“I completely agree, how to communicate results to the public is one of the most challenging things. They don’t understand about statistics,” Dr. Skufca replied.
The ball is now in the court of the Finnish health ministry, she added. These study results are brand new. Ministry officials are now going over the details and developing a strategy to communicate the results to the media, the public, and affected families.
The study was funded by the Finnish National Institute for Health and Welfare. Dr. Skufca reported receiving research grants from GlaxoSmithKline and Pfizer.
MALMO, SWEDEN – in a nationwide, retrospective cohort study.
“Anxiety and fear regarding adverse events are still very much alive and are associated with lack of acceptance of HPV vaccination,” Jozica Skufca, DVM, MIPH, observed while presenting the study findings at the annual meeting of the European Society for Paediatric Infectious Diseases.
“These results contribute valid evidence to combat public skepticism, anxiety, fears of adverse events, and possible opposition to HPV vaccination and consequently can contribute to increase HPV vaccination coverage in Finland as well as elsewhere,” added Dr. Skufca, who conducted this research while at the Finnish National Institute for Health and Welfare but is now an epidemiologist at P95, a privately held epidemiology and pharmacovigilance consulting firm in Heverlee, Belgium.
Finland introduced the bivalent HPV vaccine known as Cervarix, which is directed against HPV types 16 and 18, into the nation’s vaccination program in November 2013. The target population were girls aged 11-13 years, with catch-up vaccination at ages 14-15 years until 2015.
Dr. Skufca utilized Finland’s comprehensive system of national health care registries to conduct a study of all 240,605 Finnish girls aged 11-15 years who were eligible for the bivalent HPV vaccine from November 2013 to December 2016. Only 56% of the target population, or 134,615 girls, were actually vaccinated. All were subsequently followed for more than a year.
The investigators compared vaccinated and unvaccinated groups in terms of the subsequent rates of 38 selected outcomes of national and international interest. These included celiac disease, chronic fatigue syndrome, type 1 diabetes, Guillain-Barré syndrome, postural orthostatic tachycardia syndrome, ulcerative colitis, venous thromboembolism, psoriasis, vitiligo, scleroderma, autism, poyarteritis nodosa, asthma, Raynaud’s disease, systemic lupus erythematosus, Bell’s palsy, polycystic ovaries, juvenile arthritis, Hashimoto’s disease, and many others.
HPV vaccination rates varied considerably between hospital districts, so the results were adjusted for that potential confounder. Risks also were adjusted for the number of hospital visits 1-2 years prior to vaccination, because healthier girls – those with fewer hospital visits – turned out to be more likely to get vaccinated.
The study’s main result was that HPV vaccination wasn’t associated with a significantly higher risk of any of the 38 adverse outcomes. To the contrary, vaccination was associated with significantly reduced risk of several of them: The risk of chronic fatigue syndrome was reduced by 25%, epilepsy and recurrent seizures were reduced by 28%, the risk of Henoch-Schönlein purpura was an adjusted 52% lower in children vaccinated against HPV, and the risk of malaise and fatigue was reduced by 24%.
Dr. Skufca drew particular attention to the 400% increased risk of Guillain-Barré syndrome in vaccinated children. While this may look impressive, it wasn’t a statistically significant difference. Guillain-Barré was a rare event, with only six cases occurring during 186,934 person-years of follow-up of vaccinated individuals and a single case in unvaccinated girls. Two cases occurred within 180 days after vaccination, for an adjusted 200% increase in risk, which was nonsignificant.
Another two cases occurred more than 365 days postvaccination, for a whopping 3100% increased risk, compared with unvaccinated children; however, this too was a nonstatistically significant finding, with extraordinarily broad confidence intervals of 1.59-652.4. And there is no plausible mechanism to account for a true association between HPV vaccination and a complication, such as this, occurring more than 1 year later. It appeared to be a matter of chance, she added.
However, session cochair Ron Dagan, MD, commented that vaccine skeptics won’t find the Guillain-Barré findings reassuring.
“With HPV vaccination, there are a lot of issues related to mass perception. You say it’s not statistically significant, but some people will say, ‘Forget about the statistics – look at the confidence intervals, the risk could be more than 600 times increased.’ How do you answer this? It’s not easy, especially when we’re talking about a vaccine which has a strong adjuvant,” said Dr. Dagan, director of the pediatric infectious disease unit at Soroka University Medical Center and professor of pediatrics and infectious diseases at the Ben-Gurion University of the Negev, both in Beer-Sheva, Israel.
“I completely agree, how to communicate results to the public is one of the most challenging things. They don’t understand about statistics,” Dr. Skufca replied.
The ball is now in the court of the Finnish health ministry, she added. These study results are brand new. Ministry officials are now going over the details and developing a strategy to communicate the results to the media, the public, and affected families.
The study was funded by the Finnish National Institute for Health and Welfare. Dr. Skufca reported receiving research grants from GlaxoSmithKline and Pfizer.
MALMO, SWEDEN – in a nationwide, retrospective cohort study.
“Anxiety and fear regarding adverse events are still very much alive and are associated with lack of acceptance of HPV vaccination,” Jozica Skufca, DVM, MIPH, observed while presenting the study findings at the annual meeting of the European Society for Paediatric Infectious Diseases.
“These results contribute valid evidence to combat public skepticism, anxiety, fears of adverse events, and possible opposition to HPV vaccination and consequently can contribute to increase HPV vaccination coverage in Finland as well as elsewhere,” added Dr. Skufca, who conducted this research while at the Finnish National Institute for Health and Welfare but is now an epidemiologist at P95, a privately held epidemiology and pharmacovigilance consulting firm in Heverlee, Belgium.
Finland introduced the bivalent HPV vaccine known as Cervarix, which is directed against HPV types 16 and 18, into the nation’s vaccination program in November 2013. The target population were girls aged 11-13 years, with catch-up vaccination at ages 14-15 years until 2015.
Dr. Skufca utilized Finland’s comprehensive system of national health care registries to conduct a study of all 240,605 Finnish girls aged 11-15 years who were eligible for the bivalent HPV vaccine from November 2013 to December 2016. Only 56% of the target population, or 134,615 girls, were actually vaccinated. All were subsequently followed for more than a year.
The investigators compared vaccinated and unvaccinated groups in terms of the subsequent rates of 38 selected outcomes of national and international interest. These included celiac disease, chronic fatigue syndrome, type 1 diabetes, Guillain-Barré syndrome, postural orthostatic tachycardia syndrome, ulcerative colitis, venous thromboembolism, psoriasis, vitiligo, scleroderma, autism, poyarteritis nodosa, asthma, Raynaud’s disease, systemic lupus erythematosus, Bell’s palsy, polycystic ovaries, juvenile arthritis, Hashimoto’s disease, and many others.
HPV vaccination rates varied considerably between hospital districts, so the results were adjusted for that potential confounder. Risks also were adjusted for the number of hospital visits 1-2 years prior to vaccination, because healthier girls – those with fewer hospital visits – turned out to be more likely to get vaccinated.
The study’s main result was that HPV vaccination wasn’t associated with a significantly higher risk of any of the 38 adverse outcomes. To the contrary, vaccination was associated with significantly reduced risk of several of them: The risk of chronic fatigue syndrome was reduced by 25%, epilepsy and recurrent seizures were reduced by 28%, the risk of Henoch-Schönlein purpura was an adjusted 52% lower in children vaccinated against HPV, and the risk of malaise and fatigue was reduced by 24%.
Dr. Skufca drew particular attention to the 400% increased risk of Guillain-Barré syndrome in vaccinated children. While this may look impressive, it wasn’t a statistically significant difference. Guillain-Barré was a rare event, with only six cases occurring during 186,934 person-years of follow-up of vaccinated individuals and a single case in unvaccinated girls. Two cases occurred within 180 days after vaccination, for an adjusted 200% increase in risk, which was nonsignificant.
Another two cases occurred more than 365 days postvaccination, for a whopping 3100% increased risk, compared with unvaccinated children; however, this too was a nonstatistically significant finding, with extraordinarily broad confidence intervals of 1.59-652.4. And there is no plausible mechanism to account for a true association between HPV vaccination and a complication, such as this, occurring more than 1 year later. It appeared to be a matter of chance, she added.
However, session cochair Ron Dagan, MD, commented that vaccine skeptics won’t find the Guillain-Barré findings reassuring.
“With HPV vaccination, there are a lot of issues related to mass perception. You say it’s not statistically significant, but some people will say, ‘Forget about the statistics – look at the confidence intervals, the risk could be more than 600 times increased.’ How do you answer this? It’s not easy, especially when we’re talking about a vaccine which has a strong adjuvant,” said Dr. Dagan, director of the pediatric infectious disease unit at Soroka University Medical Center and professor of pediatrics and infectious diseases at the Ben-Gurion University of the Negev, both in Beer-Sheva, Israel.
“I completely agree, how to communicate results to the public is one of the most challenging things. They don’t understand about statistics,” Dr. Skufca replied.
The ball is now in the court of the Finnish health ministry, she added. These study results are brand new. Ministry officials are now going over the details and developing a strategy to communicate the results to the media, the public, and affected families.
The study was funded by the Finnish National Institute for Health and Welfare. Dr. Skufca reported receiving research grants from GlaxoSmithKline and Pfizer.
REPORTING FROM ESPID 2018
Key clinical point: Human papillomavirus vaccination poses no significant increased risk of numerous potential adverse outcomes.
Major finding: There was no significantly increased risk of any of 38 potential adverse outcomes in girls aged 11-15 years following administration of a bivalent HPV vaccine.
Study details: This was a retrospective cohort study including more than 240,000 Finnish girls eligible for HPV vaccination following its introduction into the national immunization program.
Disclosures: The study was sponsored by the Finnish National Institute for Health and Welfare. The presenter reported receiving research grants from GlaxoSmithKline and Pfizer.
How to identify DVT faster in pediatric osteomyelitis
MALMO, SWEDEN – Early identification of deep vein thrombosis in children with acute hematogenous osteomyelitis is critical given the need to plan anticoagulation management around the high likelihood that such patients will undergo multiple surgeries, Lawson A.B. Copley, MD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
He and his coinvestigators have identified a handful of risk factors helpful in expediting recognition of deep vein thrombosis (DVT) in children with suspected invasive infection of the musculoskeletal system.
“To improve the rate and timing of identification of DVT, we recommend performing early screening ultrasound on all children with these risk factors who are suspected of having acute hematogenous osteomyelitis,” declared Dr. Copley, professor of orthopaedic surgery and pediatrics at the University of Texas, Dallas.
Delayed diagnosis of DVT in the setting of acute hematogenous osteomyelitis (AHO) is common. Indeed, in a review of the experience at Children’s Medical Center Dallas during 2012-2014, the average time delay from ICU admission in patients suspected of having AHO to identification of DVT by ultrasound was 6.3 days.
“We’ve changed some things on the basis of that study in order to accelerate that timeline,” he explained.
Their major change was to identify actionable risk factors for DVT. This was accomplished by conducting a retrospective study of the EHR of nearly 902,000 Texas children during 2008-2016.
The study demonstrated that children with AHO complicated by DVT are, from the get-go, very different from AHO patients without DVT. They have higher illness severity of illness, are more likely to be admitted to the ICU, are prone to methicillin-resistant Staphylococcus aureus infection with prolonged bacteremia, and are much more likely to undergo multiple surgeries. Moreover, children with AHO and DVT differed substantially from other children with DVT: The dual diagnosis children lacked comorbid conditions, were prone to septic pulmonary emboli, didn’t develop postthrombotic syndrome marked by chronic venous stasis and ulcerations, and had invariably negative coagulopathy workups.
“There is no need, we feel, to perform a hypercoagulopathy workup in children with AHO complicated by DVT,” Dr. Copley said.
Drilling deeper into the data, he and his coinvestigators identified 224 new cases of DVT in the study population, for a prevalence of 2.5 per 10,000 children, along with 466 children with AHO. A total of 6% of children with AHO had DVT, and 12.1% of all children with DVT had AHO. The researchers then compared the demographics, laboratory parameters, and treatment in three cohorts: the 196 children with DVT without AHO, 28 with both AHO and DVT, and 438 with AHO without DVT.
Through this analysis, they came up with a list of risk factors warranting early screening ultrasound in children suspected of having AHO:
- An initial C-reactive protein level above 8 mg/dL, which was present in all 28 dual diagnosis children.
- ICU admission, which occurred in 19 of 28 (68%) children.
- A severity of illness score of at least 7 on a 10-point scale during the first several days in the hospital, present in 27 of the 28 children. The severity of illness scale was developed and validated by Dr. Copley and coworkers (J Pediatr Orthop. 2016 Oct 12. doi: 10.1097/BPO.0000000000000879).
- Bacteremia in the initial blood culture, present in 23 of 28 patients (82%).
- Just under 90% of the children with AHO and DVT had methicillin-resistant S. aureus, compared with 20% of those with AHO without DVT.
- Septic pulmonary emboli visualized on chest x-ray, a complication that occurred in 64% of the dual diagnosis group versus just 1% of patients with DVT without AHO.
- A band percentage of white blood cells greater than 1.5%, present in 86% of children with AHO and DVT.
More than 90% of children with AHO and DVT underwent surgery, with a mean of 2.7 surgeries per child, in contrast to the group with AHO without DVT, 55% of whom had surgery, with a mean of 0.7 surgeries per child.
Of note, there was no significant difference in the occurrence of pulmonary embolism between children with DVT without AHO versus those with DVT and AHO, with a rate of about 10% in both groups.
Dr. Copley reported having no relevant financial conflicts.
MALMO, SWEDEN – Early identification of deep vein thrombosis in children with acute hematogenous osteomyelitis is critical given the need to plan anticoagulation management around the high likelihood that such patients will undergo multiple surgeries, Lawson A.B. Copley, MD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
He and his coinvestigators have identified a handful of risk factors helpful in expediting recognition of deep vein thrombosis (DVT) in children with suspected invasive infection of the musculoskeletal system.
“To improve the rate and timing of identification of DVT, we recommend performing early screening ultrasound on all children with these risk factors who are suspected of having acute hematogenous osteomyelitis,” declared Dr. Copley, professor of orthopaedic surgery and pediatrics at the University of Texas, Dallas.
Delayed diagnosis of DVT in the setting of acute hematogenous osteomyelitis (AHO) is common. Indeed, in a review of the experience at Children’s Medical Center Dallas during 2012-2014, the average time delay from ICU admission in patients suspected of having AHO to identification of DVT by ultrasound was 6.3 days.
“We’ve changed some things on the basis of that study in order to accelerate that timeline,” he explained.
Their major change was to identify actionable risk factors for DVT. This was accomplished by conducting a retrospective study of the EHR of nearly 902,000 Texas children during 2008-2016.
The study demonstrated that children with AHO complicated by DVT are, from the get-go, very different from AHO patients without DVT. They have higher illness severity of illness, are more likely to be admitted to the ICU, are prone to methicillin-resistant Staphylococcus aureus infection with prolonged bacteremia, and are much more likely to undergo multiple surgeries. Moreover, children with AHO and DVT differed substantially from other children with DVT: The dual diagnosis children lacked comorbid conditions, were prone to septic pulmonary emboli, didn’t develop postthrombotic syndrome marked by chronic venous stasis and ulcerations, and had invariably negative coagulopathy workups.
“There is no need, we feel, to perform a hypercoagulopathy workup in children with AHO complicated by DVT,” Dr. Copley said.
Drilling deeper into the data, he and his coinvestigators identified 224 new cases of DVT in the study population, for a prevalence of 2.5 per 10,000 children, along with 466 children with AHO. A total of 6% of children with AHO had DVT, and 12.1% of all children with DVT had AHO. The researchers then compared the demographics, laboratory parameters, and treatment in three cohorts: the 196 children with DVT without AHO, 28 with both AHO and DVT, and 438 with AHO without DVT.
Through this analysis, they came up with a list of risk factors warranting early screening ultrasound in children suspected of having AHO:
- An initial C-reactive protein level above 8 mg/dL, which was present in all 28 dual diagnosis children.
- ICU admission, which occurred in 19 of 28 (68%) children.
- A severity of illness score of at least 7 on a 10-point scale during the first several days in the hospital, present in 27 of the 28 children. The severity of illness scale was developed and validated by Dr. Copley and coworkers (J Pediatr Orthop. 2016 Oct 12. doi: 10.1097/BPO.0000000000000879).
- Bacteremia in the initial blood culture, present in 23 of 28 patients (82%).
- Just under 90% of the children with AHO and DVT had methicillin-resistant S. aureus, compared with 20% of those with AHO without DVT.
- Septic pulmonary emboli visualized on chest x-ray, a complication that occurred in 64% of the dual diagnosis group versus just 1% of patients with DVT without AHO.
- A band percentage of white blood cells greater than 1.5%, present in 86% of children with AHO and DVT.
More than 90% of children with AHO and DVT underwent surgery, with a mean of 2.7 surgeries per child, in contrast to the group with AHO without DVT, 55% of whom had surgery, with a mean of 0.7 surgeries per child.
Of note, there was no significant difference in the occurrence of pulmonary embolism between children with DVT without AHO versus those with DVT and AHO, with a rate of about 10% in both groups.
Dr. Copley reported having no relevant financial conflicts.
MALMO, SWEDEN – Early identification of deep vein thrombosis in children with acute hematogenous osteomyelitis is critical given the need to plan anticoagulation management around the high likelihood that such patients will undergo multiple surgeries, Lawson A.B. Copley, MD, said at the annual meeting of the European Society for Paediatric Infectious Diseases.
He and his coinvestigators have identified a handful of risk factors helpful in expediting recognition of deep vein thrombosis (DVT) in children with suspected invasive infection of the musculoskeletal system.
“To improve the rate and timing of identification of DVT, we recommend performing early screening ultrasound on all children with these risk factors who are suspected of having acute hematogenous osteomyelitis,” declared Dr. Copley, professor of orthopaedic surgery and pediatrics at the University of Texas, Dallas.
Delayed diagnosis of DVT in the setting of acute hematogenous osteomyelitis (AHO) is common. Indeed, in a review of the experience at Children’s Medical Center Dallas during 2012-2014, the average time delay from ICU admission in patients suspected of having AHO to identification of DVT by ultrasound was 6.3 days.
“We’ve changed some things on the basis of that study in order to accelerate that timeline,” he explained.
Their major change was to identify actionable risk factors for DVT. This was accomplished by conducting a retrospective study of the EHR of nearly 902,000 Texas children during 2008-2016.
The study demonstrated that children with AHO complicated by DVT are, from the get-go, very different from AHO patients without DVT. They have higher illness severity of illness, are more likely to be admitted to the ICU, are prone to methicillin-resistant Staphylococcus aureus infection with prolonged bacteremia, and are much more likely to undergo multiple surgeries. Moreover, children with AHO and DVT differed substantially from other children with DVT: The dual diagnosis children lacked comorbid conditions, were prone to septic pulmonary emboli, didn’t develop postthrombotic syndrome marked by chronic venous stasis and ulcerations, and had invariably negative coagulopathy workups.
“There is no need, we feel, to perform a hypercoagulopathy workup in children with AHO complicated by DVT,” Dr. Copley said.
Drilling deeper into the data, he and his coinvestigators identified 224 new cases of DVT in the study population, for a prevalence of 2.5 per 10,000 children, along with 466 children with AHO. A total of 6% of children with AHO had DVT, and 12.1% of all children with DVT had AHO. The researchers then compared the demographics, laboratory parameters, and treatment in three cohorts: the 196 children with DVT without AHO, 28 with both AHO and DVT, and 438 with AHO without DVT.
Through this analysis, they came up with a list of risk factors warranting early screening ultrasound in children suspected of having AHO:
- An initial C-reactive protein level above 8 mg/dL, which was present in all 28 dual diagnosis children.
- ICU admission, which occurred in 19 of 28 (68%) children.
- A severity of illness score of at least 7 on a 10-point scale during the first several days in the hospital, present in 27 of the 28 children. The severity of illness scale was developed and validated by Dr. Copley and coworkers (J Pediatr Orthop. 2016 Oct 12. doi: 10.1097/BPO.0000000000000879).
- Bacteremia in the initial blood culture, present in 23 of 28 patients (82%).
- Just under 90% of the children with AHO and DVT had methicillin-resistant S. aureus, compared with 20% of those with AHO without DVT.
- Septic pulmonary emboli visualized on chest x-ray, a complication that occurred in 64% of the dual diagnosis group versus just 1% of patients with DVT without AHO.
- A band percentage of white blood cells greater than 1.5%, present in 86% of children with AHO and DVT.
More than 90% of children with AHO and DVT underwent surgery, with a mean of 2.7 surgeries per child, in contrast to the group with AHO without DVT, 55% of whom had surgery, with a mean of 0.7 surgeries per child.
Of note, there was no significant difference in the occurrence of pulmonary embolism between children with DVT without AHO versus those with DVT and AHO, with a rate of about 10% in both groups.
Dr. Copley reported having no relevant financial conflicts.
REPORTING FROM ESPID 2018
Key clinical point: Osteomyelitis patients with deep vein thrombosis are much sicker than those without DVT.
Major finding:
Study details: This was a retrospective study of the medical records of more than 900,000 Texas children.
Disclosures: Dr. Copley reported having no relevant financial conflicts.
Immunogenicity of two-dose Gardasil 9 persists at 36 months
MALMO, SWEDEN – Robust human papillomavirus antibody responses persist through 36 months in boys and girls who received two doses of the 9-valent HPV vaccine known as Gardasil 9 at age 9-14 years, according to an open-label randomized immunogenicity study conducted in 15 countries.
This is reassuring news supportive of regulatory decisions made in 2016/2017 to license the more convenient two-dose schedule in the United States, European Union, Canada, and other countries, Rosybel Drury, PhD, observed in reporting the results at the annual meeting of the European Society for Paediatric Infectious Diseases.
Moreover, HPV type-specific antibody levels at 36 months post vaccination in boys and girls who received two doses were similar to or greater than in the 36-month follow-up of adolescent and young adult females who received three doses at ages 16-26 years.
“This result supports the bridging of efficacy findings in young women receiving three doses to girls and boys receiving two doses,” according to Dr. Drury, a vaccine scientist at Merck Sharp & Dohme in Lyon, France.
She presented an update of a five-cohort study including roughly 1,500 recipients of either two doses of the 9-valent HPV vaccine given 6 or 12 months apart or three doses administered at 0, 2, and 6 months. Four cohorts were composed of 9- to 14-year-olds. The fifth consisted of adolescent girls and young women who got three doses of Gardasil 9 over the course of 6 months at ages 16-26 years. The previous report from this major study provided only short-term data based upon measurements of immunogenicity obtained 1 month after the last dose of vaccine (JAMA. 2016 Dec. 13;316(22):2411-21).
Anti-HPV geometric mean titers were highest 1 month after completing a two- or three-dose series, dropped off sharply during the next 6-12 months, then declined more slowly through 36 months.
While the demonstration of persistent immunogenicity over 3 years of follow-up was reassuring overall, there was a potential hitch: Significantly lower antibody levels for some HPV types were observed in girls who received two doses of the vaccine than in those who got three. Specifically, levels of anti-HPV antibodies to HPV types 18, 31, 45, and 52 were significantly lower in the girls who got two doses of the 9-valent HPV vaccine than in those who got three doses at the same age. Antibody levels directed against HPV types 6, 11, 16, 33, and 58 were similar in the two patient populations.
“The clinical significance of this finding remains unknown,” Dr. Drury said.
Challenged as to why the study didn’t include a single-dose vaccine arm, which would be the preferred preventive strategy in low-income countries where the burden of anogenital cancers and warts due to HPV is greatest, she replied that while there is great interest in this approach, and some modeling studies suggest it would be beneficial, the study she presented was designed to evaluate immunogenicity over time, not clinical efficacy, which needs to be assessed before single-dose public health programs are implemented.
The study was funded by Merck and presented by a company employee.
MALMO, SWEDEN – Robust human papillomavirus antibody responses persist through 36 months in boys and girls who received two doses of the 9-valent HPV vaccine known as Gardasil 9 at age 9-14 years, according to an open-label randomized immunogenicity study conducted in 15 countries.
This is reassuring news supportive of regulatory decisions made in 2016/2017 to license the more convenient two-dose schedule in the United States, European Union, Canada, and other countries, Rosybel Drury, PhD, observed in reporting the results at the annual meeting of the European Society for Paediatric Infectious Diseases.
Moreover, HPV type-specific antibody levels at 36 months post vaccination in boys and girls who received two doses were similar to or greater than in the 36-month follow-up of adolescent and young adult females who received three doses at ages 16-26 years.
“This result supports the bridging of efficacy findings in young women receiving three doses to girls and boys receiving two doses,” according to Dr. Drury, a vaccine scientist at Merck Sharp & Dohme in Lyon, France.
She presented an update of a five-cohort study including roughly 1,500 recipients of either two doses of the 9-valent HPV vaccine given 6 or 12 months apart or three doses administered at 0, 2, and 6 months. Four cohorts were composed of 9- to 14-year-olds. The fifth consisted of adolescent girls and young women who got three doses of Gardasil 9 over the course of 6 months at ages 16-26 years. The previous report from this major study provided only short-term data based upon measurements of immunogenicity obtained 1 month after the last dose of vaccine (JAMA. 2016 Dec. 13;316(22):2411-21).
Anti-HPV geometric mean titers were highest 1 month after completing a two- or three-dose series, dropped off sharply during the next 6-12 months, then declined more slowly through 36 months.
While the demonstration of persistent immunogenicity over 3 years of follow-up was reassuring overall, there was a potential hitch: Significantly lower antibody levels for some HPV types were observed in girls who received two doses of the vaccine than in those who got three. Specifically, levels of anti-HPV antibodies to HPV types 18, 31, 45, and 52 were significantly lower in the girls who got two doses of the 9-valent HPV vaccine than in those who got three doses at the same age. Antibody levels directed against HPV types 6, 11, 16, 33, and 58 were similar in the two patient populations.
“The clinical significance of this finding remains unknown,” Dr. Drury said.
Challenged as to why the study didn’t include a single-dose vaccine arm, which would be the preferred preventive strategy in low-income countries where the burden of anogenital cancers and warts due to HPV is greatest, she replied that while there is great interest in this approach, and some modeling studies suggest it would be beneficial, the study she presented was designed to evaluate immunogenicity over time, not clinical efficacy, which needs to be assessed before single-dose public health programs are implemented.
The study was funded by Merck and presented by a company employee.
MALMO, SWEDEN – Robust human papillomavirus antibody responses persist through 36 months in boys and girls who received two doses of the 9-valent HPV vaccine known as Gardasil 9 at age 9-14 years, according to an open-label randomized immunogenicity study conducted in 15 countries.
This is reassuring news supportive of regulatory decisions made in 2016/2017 to license the more convenient two-dose schedule in the United States, European Union, Canada, and other countries, Rosybel Drury, PhD, observed in reporting the results at the annual meeting of the European Society for Paediatric Infectious Diseases.
Moreover, HPV type-specific antibody levels at 36 months post vaccination in boys and girls who received two doses were similar to or greater than in the 36-month follow-up of adolescent and young adult females who received three doses at ages 16-26 years.
“This result supports the bridging of efficacy findings in young women receiving three doses to girls and boys receiving two doses,” according to Dr. Drury, a vaccine scientist at Merck Sharp & Dohme in Lyon, France.
She presented an update of a five-cohort study including roughly 1,500 recipients of either two doses of the 9-valent HPV vaccine given 6 or 12 months apart or three doses administered at 0, 2, and 6 months. Four cohorts were composed of 9- to 14-year-olds. The fifth consisted of adolescent girls and young women who got three doses of Gardasil 9 over the course of 6 months at ages 16-26 years. The previous report from this major study provided only short-term data based upon measurements of immunogenicity obtained 1 month after the last dose of vaccine (JAMA. 2016 Dec. 13;316(22):2411-21).
Anti-HPV geometric mean titers were highest 1 month after completing a two- or three-dose series, dropped off sharply during the next 6-12 months, then declined more slowly through 36 months.
While the demonstration of persistent immunogenicity over 3 years of follow-up was reassuring overall, there was a potential hitch: Significantly lower antibody levels for some HPV types were observed in girls who received two doses of the vaccine than in those who got three. Specifically, levels of anti-HPV antibodies to HPV types 18, 31, 45, and 52 were significantly lower in the girls who got two doses of the 9-valent HPV vaccine than in those who got three doses at the same age. Antibody levels directed against HPV types 6, 11, 16, 33, and 58 were similar in the two patient populations.
“The clinical significance of this finding remains unknown,” Dr. Drury said.
Challenged as to why the study didn’t include a single-dose vaccine arm, which would be the preferred preventive strategy in low-income countries where the burden of anogenital cancers and warts due to HPV is greatest, she replied that while there is great interest in this approach, and some modeling studies suggest it would be beneficial, the study she presented was designed to evaluate immunogenicity over time, not clinical efficacy, which needs to be assessed before single-dose public health programs are implemented.
The study was funded by Merck and presented by a company employee.
REPORTING FROM ESPID 2018
Key clinical point:
Major finding: HPV type-specific antibody responses to two doses given at age 9-14 years were as good as or better than in 16- to 26-year-olds who got three doses.
Study details: This prospective open-label immunogenicity study included roughly 1,500 subjects in 15 countries who received either two or three doses of the 9-valent HPV vaccine.
Disclosures: The study was funded by Merck and presented by a company employee.
Norovirus vaccine appears promising in children
MALMO, SWEDEN – in an interim analysis of an ongoing phase 2 study, Taisei Masuda, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The randomized, double-blind, multinational trial remains blinded because follow-up is continuing, so – to the disappointment of the ESPID audience – there are as yet no data on duration of antibody persistence or clinical efficacy.
However, an earlier phase 2 study in 420 healthy participants aged 18-64 years showed that the Takeda vaccine elicited persistent immune responses 1 year post vaccination and that higher antibody levels correlated with a reduced frequency of moderate to severe vomiting and diarrheal illness following oral challenge with norovirus (Clin Vaccine Immunol. 2015 Aug;22[8]:923-9). Follow-up will continue in order to learn how long the protective immune response lasts in adults, according to Dr. Masuda, of Takeda Pharmaceuticals in Zurich.
The bivalent Takeda vaccine is the first candidate vaccine to reach the randomized trial stage. An oral vaccine in tablet form under development by Vaxart, a San Francisco Bay Area biotech company, recently completed preliminary phase 1 studies.
Dr. Masuda explained that the Takeda vaccine contains virus-like particle antigens from norovirus strains GI.1 and GII.4c, which together account for the majority of human norovirus illness. These virus-like particles are formed on the outer surface of the virus. Of note, virus-like particle–based vaccines against hepatitis B and human papillomavirus have won regulatory approval in the United States, Europe, and elsewhere.
He presented data on 120 healthy subjects aged 1 year to less than 4 years old and another 120 aged 4 years to less than 9 years. They are part of a larger phase 2 study of 840 children as young as age 6 weeks. This was a dose-finding study, so participants received various doses of the vaccine on day 1 and either a second dose or a saline injection 28 days later. The vaccine, which contains aluminum hydroxide to enhance immunogenicity, comes in prefilled syringes.
At 57 days of follow-up in this interim analysis, protective seroresponse rates as defined by at least a fourfold increase in histo-blood group antigen–blocking titers approached 100%. In the older group, this was typically achieved with a single dose of vaccine. However, the younger group of children generally derived further benefit from a second dose, according to Dr. Masuda.
In terms of safety concerns, he said no serious adverse events occurred in the study and no one withdrew from the trial because of vaccine-related side effects. The overall safety picture was the same in the two age groups. The incidence of fever of 38° C or higher was similar after administration of vaccine and placebo. Injection site pain occurred in one-quarter of younger vaccine recipients, in 38%-63% of those aged 4 years or older, and in 17%-22% who got placebo injections. Those and other local and systemic adverse events were mostly mild and transient. Their incidence and severity weren’t related to vaccine dosage.
In sum, Dr. Masuda deemed the safety profile “clinically acceptable.”
Session chair Karina Butler, MD, of Temple Street Children’s University Hospital, Dublin, raised the question of how might this vaccine, which may require two doses in younger children, fit into an already crowded pediatric immunization schedule – will parents and physicians embrace it?
Dr. Masuda replied that noroviruses are the No. 1 cause of acute gastroenteritis worldwide and there is a clamor for development of effective vaccines to protect the groups that bear the greatest burden of disease, including children, the elderly, military personnel, cruise ship vacationers, and others who experience crowded conditions. He expressed confidence that a safe and effective vaccine will be in high demand.
“In the future, we’ll look at the possibility of a combination vaccine,” he added.
In response to audience questions, Dr. Masuda said that in adult studies higher levels of immunogenicity have been achieved after vaccination, compared with natural infection; however, there are as yet no pediatric data on that score. Also, investigators have seen evidence of cross-reactivity to the vaccine in some but not all naturally circulating nonvaccine strains.
The vaccine formulation being carried forward into advanced clinical trials in adults is 15 mcg of GI.1/50 mcg of GII.4c (J Infect Dis. 2018 Jan 30;217[4]:597-607).
The phase 2 study presented by Dr. Masuda was supported by the U.S. Army.
MALMO, SWEDEN – in an interim analysis of an ongoing phase 2 study, Taisei Masuda, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The randomized, double-blind, multinational trial remains blinded because follow-up is continuing, so – to the disappointment of the ESPID audience – there are as yet no data on duration of antibody persistence or clinical efficacy.
However, an earlier phase 2 study in 420 healthy participants aged 18-64 years showed that the Takeda vaccine elicited persistent immune responses 1 year post vaccination and that higher antibody levels correlated with a reduced frequency of moderate to severe vomiting and diarrheal illness following oral challenge with norovirus (Clin Vaccine Immunol. 2015 Aug;22[8]:923-9). Follow-up will continue in order to learn how long the protective immune response lasts in adults, according to Dr. Masuda, of Takeda Pharmaceuticals in Zurich.
The bivalent Takeda vaccine is the first candidate vaccine to reach the randomized trial stage. An oral vaccine in tablet form under development by Vaxart, a San Francisco Bay Area biotech company, recently completed preliminary phase 1 studies.
Dr. Masuda explained that the Takeda vaccine contains virus-like particle antigens from norovirus strains GI.1 and GII.4c, which together account for the majority of human norovirus illness. These virus-like particles are formed on the outer surface of the virus. Of note, virus-like particle–based vaccines against hepatitis B and human papillomavirus have won regulatory approval in the United States, Europe, and elsewhere.
He presented data on 120 healthy subjects aged 1 year to less than 4 years old and another 120 aged 4 years to less than 9 years. They are part of a larger phase 2 study of 840 children as young as age 6 weeks. This was a dose-finding study, so participants received various doses of the vaccine on day 1 and either a second dose or a saline injection 28 days later. The vaccine, which contains aluminum hydroxide to enhance immunogenicity, comes in prefilled syringes.
At 57 days of follow-up in this interim analysis, protective seroresponse rates as defined by at least a fourfold increase in histo-blood group antigen–blocking titers approached 100%. In the older group, this was typically achieved with a single dose of vaccine. However, the younger group of children generally derived further benefit from a second dose, according to Dr. Masuda.
In terms of safety concerns, he said no serious adverse events occurred in the study and no one withdrew from the trial because of vaccine-related side effects. The overall safety picture was the same in the two age groups. The incidence of fever of 38° C or higher was similar after administration of vaccine and placebo. Injection site pain occurred in one-quarter of younger vaccine recipients, in 38%-63% of those aged 4 years or older, and in 17%-22% who got placebo injections. Those and other local and systemic adverse events were mostly mild and transient. Their incidence and severity weren’t related to vaccine dosage.
In sum, Dr. Masuda deemed the safety profile “clinically acceptable.”
Session chair Karina Butler, MD, of Temple Street Children’s University Hospital, Dublin, raised the question of how might this vaccine, which may require two doses in younger children, fit into an already crowded pediatric immunization schedule – will parents and physicians embrace it?
Dr. Masuda replied that noroviruses are the No. 1 cause of acute gastroenteritis worldwide and there is a clamor for development of effective vaccines to protect the groups that bear the greatest burden of disease, including children, the elderly, military personnel, cruise ship vacationers, and others who experience crowded conditions. He expressed confidence that a safe and effective vaccine will be in high demand.
“In the future, we’ll look at the possibility of a combination vaccine,” he added.
In response to audience questions, Dr. Masuda said that in adult studies higher levels of immunogenicity have been achieved after vaccination, compared with natural infection; however, there are as yet no pediatric data on that score. Also, investigators have seen evidence of cross-reactivity to the vaccine in some but not all naturally circulating nonvaccine strains.
The vaccine formulation being carried forward into advanced clinical trials in adults is 15 mcg of GI.1/50 mcg of GII.4c (J Infect Dis. 2018 Jan 30;217[4]:597-607).
The phase 2 study presented by Dr. Masuda was supported by the U.S. Army.
MALMO, SWEDEN – in an interim analysis of an ongoing phase 2 study, Taisei Masuda, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
The randomized, double-blind, multinational trial remains blinded because follow-up is continuing, so – to the disappointment of the ESPID audience – there are as yet no data on duration of antibody persistence or clinical efficacy.
However, an earlier phase 2 study in 420 healthy participants aged 18-64 years showed that the Takeda vaccine elicited persistent immune responses 1 year post vaccination and that higher antibody levels correlated with a reduced frequency of moderate to severe vomiting and diarrheal illness following oral challenge with norovirus (Clin Vaccine Immunol. 2015 Aug;22[8]:923-9). Follow-up will continue in order to learn how long the protective immune response lasts in adults, according to Dr. Masuda, of Takeda Pharmaceuticals in Zurich.
The bivalent Takeda vaccine is the first candidate vaccine to reach the randomized trial stage. An oral vaccine in tablet form under development by Vaxart, a San Francisco Bay Area biotech company, recently completed preliminary phase 1 studies.
Dr. Masuda explained that the Takeda vaccine contains virus-like particle antigens from norovirus strains GI.1 and GII.4c, which together account for the majority of human norovirus illness. These virus-like particles are formed on the outer surface of the virus. Of note, virus-like particle–based vaccines against hepatitis B and human papillomavirus have won regulatory approval in the United States, Europe, and elsewhere.
He presented data on 120 healthy subjects aged 1 year to less than 4 years old and another 120 aged 4 years to less than 9 years. They are part of a larger phase 2 study of 840 children as young as age 6 weeks. This was a dose-finding study, so participants received various doses of the vaccine on day 1 and either a second dose or a saline injection 28 days later. The vaccine, which contains aluminum hydroxide to enhance immunogenicity, comes in prefilled syringes.
At 57 days of follow-up in this interim analysis, protective seroresponse rates as defined by at least a fourfold increase in histo-blood group antigen–blocking titers approached 100%. In the older group, this was typically achieved with a single dose of vaccine. However, the younger group of children generally derived further benefit from a second dose, according to Dr. Masuda.
In terms of safety concerns, he said no serious adverse events occurred in the study and no one withdrew from the trial because of vaccine-related side effects. The overall safety picture was the same in the two age groups. The incidence of fever of 38° C or higher was similar after administration of vaccine and placebo. Injection site pain occurred in one-quarter of younger vaccine recipients, in 38%-63% of those aged 4 years or older, and in 17%-22% who got placebo injections. Those and other local and systemic adverse events were mostly mild and transient. Their incidence and severity weren’t related to vaccine dosage.
In sum, Dr. Masuda deemed the safety profile “clinically acceptable.”
Session chair Karina Butler, MD, of Temple Street Children’s University Hospital, Dublin, raised the question of how might this vaccine, which may require two doses in younger children, fit into an already crowded pediatric immunization schedule – will parents and physicians embrace it?
Dr. Masuda replied that noroviruses are the No. 1 cause of acute gastroenteritis worldwide and there is a clamor for development of effective vaccines to protect the groups that bear the greatest burden of disease, including children, the elderly, military personnel, cruise ship vacationers, and others who experience crowded conditions. He expressed confidence that a safe and effective vaccine will be in high demand.
“In the future, we’ll look at the possibility of a combination vaccine,” he added.
In response to audience questions, Dr. Masuda said that in adult studies higher levels of immunogenicity have been achieved after vaccination, compared with natural infection; however, there are as yet no pediatric data on that score. Also, investigators have seen evidence of cross-reactivity to the vaccine in some but not all naturally circulating nonvaccine strains.
The vaccine formulation being carried forward into advanced clinical trials in adults is 15 mcg of GI.1/50 mcg of GII.4c (J Infect Dis. 2018 Jan 30;217[4]:597-607).
The phase 2 study presented by Dr. Masuda was supported by the U.S. Army.
REPORTING FROM ESPID 2018
Key clinical point: Hope runs high that an effective norovirus vaccine is in the works.
Major finding: Protective seroresponse rates against the two chief disease-causing strains of norovirus were seen in nearly 100% of vaccinated children aged 1-8 years.
Study details: This is an ongoing prospective, multicenter, double-blind, phase 2 randomized trial including 840 children.
Disclosures: The study was supported by the U.S. Army and presented by an employee of Takeda Pharmaceuticals.