User login
PCPs play a small part in low-value care spending
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.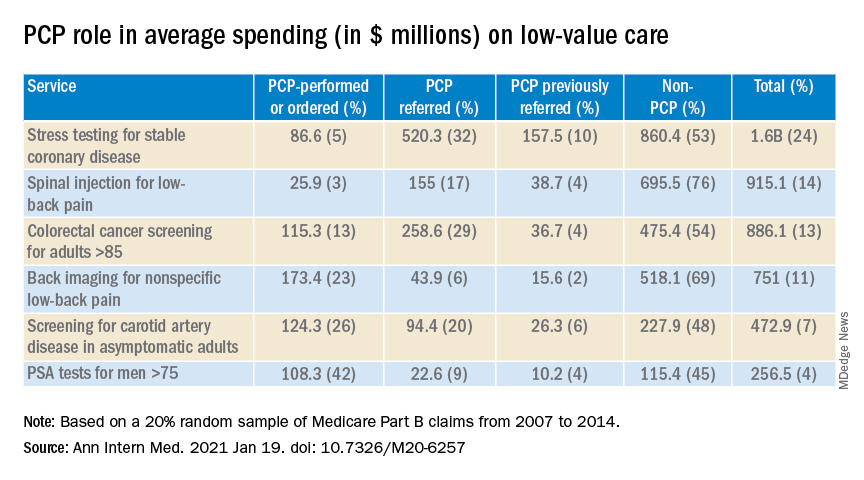
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.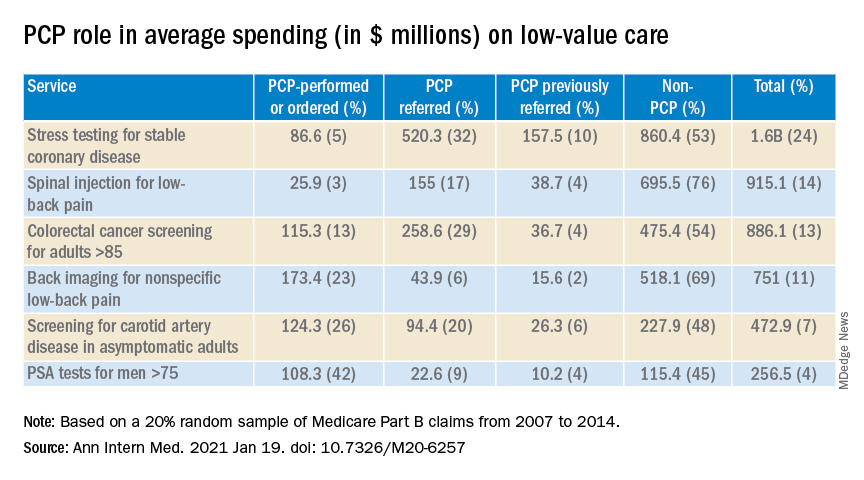
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.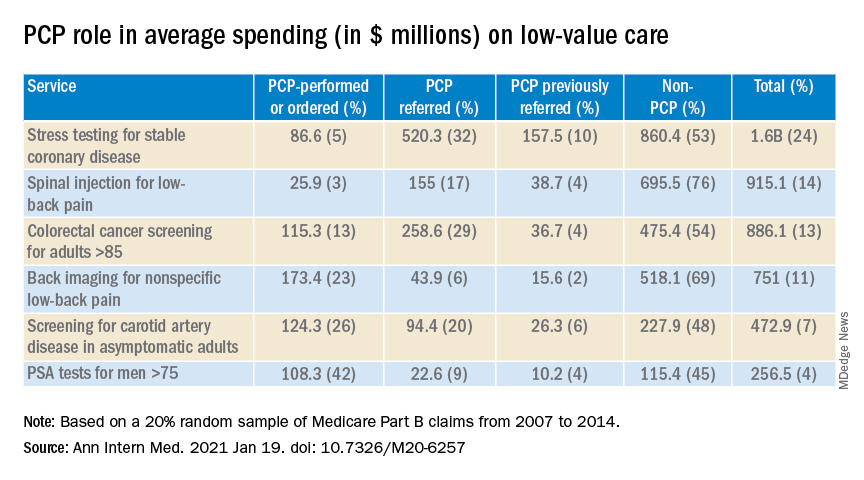
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How to predict successful colonoscopy malpractice lawsuits
Malpractice lawsuits related to colonoscopy continue to pose challenges for practitioners, and a new analysis reveals that errors related to sedation are more likely to be awarded to plaintiffs. Primary care physicians and surgeons are often codefendants, which emphasizes the importance of interdisciplinary care in colonoscopy.
Cases involving informed consent were more likely to be ruled for the defendant, while those tied to medication error favored the plaintiff, according to an analysis of cases from the Westlaw legal database. The study, led by Krishan S. Patel and Sushil Ahlawat of Rutgers New Jersey Medical School, Newark, was published in the Journal of Clinical Gastroenterology.
According to the authors, 55% of physicians face a malpractice suit at some point in their careers, and gastroenterology ranks as the sixth most common specialty named in malpractice suits. Every year, about 13% of gastroenterologists confront malpractice allegations, and colonoscopy is the most common reason.
The researchers searched the Westlaw legal database for malpractice cases involving colonoscopy or sigmoidoscopy, identifying 305 cases between 1980 and 2017. The average patient age was 54.9 years, and 52.8% of cases were brought by female patients. The most cases were from New York (21.0%), followed by California (13.4%), Pennsylvania (13.1%), Massachusetts (12.5%), and New Jersey (7.9%). Gastroenterologists were named in 71.1% of cases, internists in 25.6%, and surgeons in 14.8%.
A little more than half (51.8%) of cases were ruled in favor of the defendant, and 25% for the plaintiff; 17% were settled, and 6% had a mixed outcome. Payouts ranged from $30,000 to $500,000,000, with a median of $995,000.
There were multiple causes of litigation listed in 83.6% of cases. The most frequent causes were delayed treatment (65.9%), delayed diagnosis (65.6%), procedural error/negligence (44.3%), and failure to refer/reorder tests (25.6%).
Of 135 cases alleging procedural negligence, 90 (67%) named perforation. Among 79 cases that cited a failure to refer and order appropriate tests, 97% claimed the defendant missed a cancerous lesion. In cases alleging missed cancers, 31% were in the cecum, and 23% in the anus.
A logistic regression analysis of factors associated with a verdict for the defendant found “lack of informed consent” to be an independent predictor of defendant verdict (odds ratio, 4.05; P = .004). “Medication error” was associated with reduced defendant success (OR, 0.17; P=.023). There were nonsignificant trends between reduced odds of a verdict for the defendant and lawsuits that named “delay in diagnosis” (OR, 0.35; P = .060) and “failure to refer” (OR, 0.51; P = .074).
The authors sound a dire note about the number of malpractice suits brought against gastroenterologists, but Lawrence Kosinski, MD, is more sanguine. He notes that gastroenterologists have low insurance premiums, compared with other specialties, but recognizes that colonoscopies are a significant source of risk.
Dr. Kosinski, who is chief medical officer at SonarMD and formerly a managing partner at the Illinois Gastroenterology Group, said in an interview that the study is revealing. “It comes out in the article: Acts of omission are more dangerous to the physician than acts of commission. Not finding that cancer, not acting on that malignant polyp, not pursuing it, is much more likely to get you in trouble than taking it off and perforating a colon,” said Dr. Kosinski, who was not involved in the study.
To gastroenterologists seeking to reduce their risks, he offered advice: You shouldn’t assume that the patient has read the information provided. Risks of anesthesia and the procedure should be directly communicated. It’s also important to document the procedure, including pictures of the cecum and rectal retroflexion. Finally, don’t rush. “This isn’t a race. Clean the colon, make sure you don’t miss something. If that person pops up in 3 years with a cancer, someone may go after you,” said Dr. Kosinski.
No source of funding was disclosed. Dr. Kosinski has no relevant financial disclosures.
Malpractice lawsuits related to colonoscopy continue to pose challenges for practitioners, and a new analysis reveals that errors related to sedation are more likely to be awarded to plaintiffs. Primary care physicians and surgeons are often codefendants, which emphasizes the importance of interdisciplinary care in colonoscopy.
Cases involving informed consent were more likely to be ruled for the defendant, while those tied to medication error favored the plaintiff, according to an analysis of cases from the Westlaw legal database. The study, led by Krishan S. Patel and Sushil Ahlawat of Rutgers New Jersey Medical School, Newark, was published in the Journal of Clinical Gastroenterology.
According to the authors, 55% of physicians face a malpractice suit at some point in their careers, and gastroenterology ranks as the sixth most common specialty named in malpractice suits. Every year, about 13% of gastroenterologists confront malpractice allegations, and colonoscopy is the most common reason.
The researchers searched the Westlaw legal database for malpractice cases involving colonoscopy or sigmoidoscopy, identifying 305 cases between 1980 and 2017. The average patient age was 54.9 years, and 52.8% of cases were brought by female patients. The most cases were from New York (21.0%), followed by California (13.4%), Pennsylvania (13.1%), Massachusetts (12.5%), and New Jersey (7.9%). Gastroenterologists were named in 71.1% of cases, internists in 25.6%, and surgeons in 14.8%.
A little more than half (51.8%) of cases were ruled in favor of the defendant, and 25% for the plaintiff; 17% were settled, and 6% had a mixed outcome. Payouts ranged from $30,000 to $500,000,000, with a median of $995,000.
There were multiple causes of litigation listed in 83.6% of cases. The most frequent causes were delayed treatment (65.9%), delayed diagnosis (65.6%), procedural error/negligence (44.3%), and failure to refer/reorder tests (25.6%).
Of 135 cases alleging procedural negligence, 90 (67%) named perforation. Among 79 cases that cited a failure to refer and order appropriate tests, 97% claimed the defendant missed a cancerous lesion. In cases alleging missed cancers, 31% were in the cecum, and 23% in the anus.
A logistic regression analysis of factors associated with a verdict for the defendant found “lack of informed consent” to be an independent predictor of defendant verdict (odds ratio, 4.05; P = .004). “Medication error” was associated with reduced defendant success (OR, 0.17; P=.023). There were nonsignificant trends between reduced odds of a verdict for the defendant and lawsuits that named “delay in diagnosis” (OR, 0.35; P = .060) and “failure to refer” (OR, 0.51; P = .074).
The authors sound a dire note about the number of malpractice suits brought against gastroenterologists, but Lawrence Kosinski, MD, is more sanguine. He notes that gastroenterologists have low insurance premiums, compared with other specialties, but recognizes that colonoscopies are a significant source of risk.
Dr. Kosinski, who is chief medical officer at SonarMD and formerly a managing partner at the Illinois Gastroenterology Group, said in an interview that the study is revealing. “It comes out in the article: Acts of omission are more dangerous to the physician than acts of commission. Not finding that cancer, not acting on that malignant polyp, not pursuing it, is much more likely to get you in trouble than taking it off and perforating a colon,” said Dr. Kosinski, who was not involved in the study.
To gastroenterologists seeking to reduce their risks, he offered advice: You shouldn’t assume that the patient has read the information provided. Risks of anesthesia and the procedure should be directly communicated. It’s also important to document the procedure, including pictures of the cecum and rectal retroflexion. Finally, don’t rush. “This isn’t a race. Clean the colon, make sure you don’t miss something. If that person pops up in 3 years with a cancer, someone may go after you,” said Dr. Kosinski.
No source of funding was disclosed. Dr. Kosinski has no relevant financial disclosures.
Malpractice lawsuits related to colonoscopy continue to pose challenges for practitioners, and a new analysis reveals that errors related to sedation are more likely to be awarded to plaintiffs. Primary care physicians and surgeons are often codefendants, which emphasizes the importance of interdisciplinary care in colonoscopy.
Cases involving informed consent were more likely to be ruled for the defendant, while those tied to medication error favored the plaintiff, according to an analysis of cases from the Westlaw legal database. The study, led by Krishan S. Patel and Sushil Ahlawat of Rutgers New Jersey Medical School, Newark, was published in the Journal of Clinical Gastroenterology.
According to the authors, 55% of physicians face a malpractice suit at some point in their careers, and gastroenterology ranks as the sixth most common specialty named in malpractice suits. Every year, about 13% of gastroenterologists confront malpractice allegations, and colonoscopy is the most common reason.
The researchers searched the Westlaw legal database for malpractice cases involving colonoscopy or sigmoidoscopy, identifying 305 cases between 1980 and 2017. The average patient age was 54.9 years, and 52.8% of cases were brought by female patients. The most cases were from New York (21.0%), followed by California (13.4%), Pennsylvania (13.1%), Massachusetts (12.5%), and New Jersey (7.9%). Gastroenterologists were named in 71.1% of cases, internists in 25.6%, and surgeons in 14.8%.
A little more than half (51.8%) of cases were ruled in favor of the defendant, and 25% for the plaintiff; 17% were settled, and 6% had a mixed outcome. Payouts ranged from $30,000 to $500,000,000, with a median of $995,000.
There were multiple causes of litigation listed in 83.6% of cases. The most frequent causes were delayed treatment (65.9%), delayed diagnosis (65.6%), procedural error/negligence (44.3%), and failure to refer/reorder tests (25.6%).
Of 135 cases alleging procedural negligence, 90 (67%) named perforation. Among 79 cases that cited a failure to refer and order appropriate tests, 97% claimed the defendant missed a cancerous lesion. In cases alleging missed cancers, 31% were in the cecum, and 23% in the anus.
A logistic regression analysis of factors associated with a verdict for the defendant found “lack of informed consent” to be an independent predictor of defendant verdict (odds ratio, 4.05; P = .004). “Medication error” was associated with reduced defendant success (OR, 0.17; P=.023). There were nonsignificant trends between reduced odds of a verdict for the defendant and lawsuits that named “delay in diagnosis” (OR, 0.35; P = .060) and “failure to refer” (OR, 0.51; P = .074).
The authors sound a dire note about the number of malpractice suits brought against gastroenterologists, but Lawrence Kosinski, MD, is more sanguine. He notes that gastroenterologists have low insurance premiums, compared with other specialties, but recognizes that colonoscopies are a significant source of risk.
Dr. Kosinski, who is chief medical officer at SonarMD and formerly a managing partner at the Illinois Gastroenterology Group, said in an interview that the study is revealing. “It comes out in the article: Acts of omission are more dangerous to the physician than acts of commission. Not finding that cancer, not acting on that malignant polyp, not pursuing it, is much more likely to get you in trouble than taking it off and perforating a colon,” said Dr. Kosinski, who was not involved in the study.
To gastroenterologists seeking to reduce their risks, he offered advice: You shouldn’t assume that the patient has read the information provided. Risks of anesthesia and the procedure should be directly communicated. It’s also important to document the procedure, including pictures of the cecum and rectal retroflexion. Finally, don’t rush. “This isn’t a race. Clean the colon, make sure you don’t miss something. If that person pops up in 3 years with a cancer, someone may go after you,” said Dr. Kosinski.
No source of funding was disclosed. Dr. Kosinski has no relevant financial disclosures.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
CRC risk in young adults: Not as high as previously reported
Implications for CRC screening.
New estimates for the risk of CRC in young adults, which differentiate colorectal adenocarcinoma from other types, are reported in a study published Dec. 15, 2020, in Annals of Internal Medicine.
They are important because this finding has implications for CRC screening, say a trio of experts in an accompanying editorial.
Reports of an increase in the incidence of CRC in younger adults have led to changes in screening for this cancer in the United States. The age for starting CRC screening has been lowered to 45 years (instead of 50 years) in recommendations issued in 2018 by the American Cancer Society, and also more recently in preliminary recommendations from the U.S. Preventive Services Task Force.
However, that 2018 ACS recommendation to lower the starting age to 45 years was based to a large extent on a report of a higher incidence of CRC in younger adults from a 2017 study that used the SEER (Surveillance, Epidemiology, and End Results) database).
But that SEER-based study considered “colorectal cancer” as a homogeneous group defined by topology, the editorialists pointed out.
The new study, the editorialists said, uses that same SEER database but has “disentangled colorectal adenocarcinoma, the target for screening, from other histologic CRC types, including neuroendocrine (carcinoid) tumors, for which screening is not recommended.”
The study authors explained that adenocarcinoma is a target for prevention through screening because it arises from precancerous polyps. Those growths can be detected and removed before cancer develops. That doesn’t apply to carcinoid tumors, which are frequently incidental findings on flexible sigmoidoscopy or colonoscopy.
These carcinoid tumors typically are indolent, with a better prognosis than most other cancer types, the editorialists added. “Most likely, the majority of carcinoid tumors identified by screening represent incidental findings with little health benefit from detection. In fact, many may be characterized as overdiagnosed tumors, which by definition increase the burden and harms of screening without the balance of additional benefit.”
This new analysis showed that 4%-20% of the lesions previously described as CRC were not adenocarcinoma but carcinoid tumors, the editorialists pointed out.
This figure rose even higher in the subgroup of findings pertaining to the rectum, the colonic segment with the largest reported increase in early-onset CRC. Here, up to 34% of lesions (depending on patient age) were carcinoid tumors rather than adenocarcinoma, they noted.
The three editorialists – Michael Bretthauer, MD, PhD, and Mette Kalager, MD, PhD, both of the University of Oslo, and David Weinberg, MD, MSc, of Fox Chase Cancer Center, Philadelphia – call for action based on the new findings.
“The ACS’s 2018 estimate of about 7,000 new CRC cases among persons aged 45-49 years in the United States (the justification for screening) needs to be adjusted downward on the basis of the new evidence,” the trio wrote.
They conclude that “caution is warranted when promoting the benefits of CRC screening for persons younger than 50 years.”
However, the senior author of the new study, Jordan Karlitz, MD, of Tulane University, New Orleans, strongly disagreed.
Contrary to the editorialists, Dr. Karlitz said in an interview that he and his colleagues firmly believe that colorectal cancer screening for average-risk patients should begin at age 45 and that their new research, despite its clarification about carcinoid tumors, provides evidence for that.
“There are a number of other studies that support screening at age 45 as well,” he said. “This [new] finding supports the presence of a large preclinical colorectal cancer case burden in patients in their 40s that is ultimately uncovered with screening initiation at age 50. Many of these cancers could be prevented or diagnosed at an earlier stage with screening at age 45.”
“This is the first study to analyze early-onset colorectal cancer by specific histologic subtype,” Dr. Karlitz also pointed out.
“Although colorectal carcinoids are increasing at a faster rate than adenocarcinomas, adenocarcinomas constitute the overwhelming majority of colorectal cancers in people in their 40s and are also steadily increasing, which has implications for beginning screening at age 45,” he said.
Adenocarcinomas also make up the “overwhelming majority” of colorectal cancers in patients under 50 overall and “are the main driving force behind the increased colorectal cancer burden we are seeing in young patients,” Dr. Karlitz added.
Furthermore, “modeling studies on which the USPSTF screening recommendations were based [which recommended starting at age 45] were confined to adenocarcinoma, thus excluding carcinoids from their analysis,” he said.
Steepest changes in adenocarcinomas in younger groups
In their study, Dr. Karlitz and colleagues assessed the incidence rates of early colorectal cancer, using SEER data from 2000 to 2016, and stratifying the data by histologic subtype (primarily adenocarcinoma and carcinoid tumors), age group (20-29, 30-39, 40-49, and 50-54 years), and subsite.
A total of 123,143 CRC cases were identified in 119,624 patients between the ages of 20-54 years during that time period.
The absolute incidence rates in the younger age groups (20-29 and 30-39 years) were very low, compared with those aged 40-49 and 50-54 years.
The greatest 3-year average annual incident rate changes in adenocarcinoma (2000-2002 vs. 2014-2016) for any age group or subsite were for rectal-only cases in the 20-29 years group (+39%), as well as rectal-only cases in those aged 30-39 years (+39%), and colon-only cases in the age 30-39 group (+20%).
There was also significant increase in rectal-only adenocarcinoma in individuals aged 50-54 years (+10%). A statistically significant increase in the annual percentage change for adenocarcinomas was observed for all age groups, except for colon-only cases in the 20-29 years group (0.7%) and for both colorectal (0.2%) and colon-only cases (–0.1%) in those aged 50-54 years.
Even though the absolute carcinoid tumor incidence rates were lower than for adenocarcinoma in all age groups and subsites, a statistically significant increase was observed in the 3-year average annual incidence rate of combined-site colorectal carcinoid tumors in all age groups from 2000–2002 and 2014–2016. This increase was largely the result of increases in rectal carcinoid tumors, the authors note.
The authors also highlighted the results in the 40- to 49-year age group “because of differing opinions on whether to begin average-risk screening at age 45 or 50 years.”
They reported that rates of rectal and colon adenocarcinoma are increasing “substantially,” whether measured by changes in 3-year average annual incidence rate or by annual percentage changes. The change in average annual incidence rate of colon-only adenocarcinoma for persons aged 40-49 years was 13% (12.21 to 13.85 per 100,000), and that of rectal adenocarcinoma was 16% (7.50 to 8.72 per 100,000). Corresponding annual percentage changes were 0.8% and 1.2%, respectively. “These significant increases in adenocarcinoma incident rates add to the debate over earlier screening at age 45 years,” they commented.
Calls for next steps
The editorialists emphasize restraint when promoting the benefits of colorectal screening for persons younger than 50 years.
They point out that the USPSTF released a provisional update of its CRC screening recommendations about lowering the age to initiate screening to 45 years, as reported by this news organization.
“No new empirical evidence has been found since the USPSTF update in 2016 to inform the effectiveness of screening in persons younger than 50 years,” they write, adding that similar to the American Cancer Society in 2018, the task force has relied exclusively on modeling studies.
This new data from Dr. Karlitz and colleagues “should prompt the modelers to recalculate their estimates of benefits and harms of screening,” they suggested. “Revisiting the model would also allow competing forms of CRC screening to be compared in light of new risk assumptions.
“Previous assumptions that screening tests are equally effective in younger and older patients and that screening adherence will approach 100% may also be reconsidered,” the editorialist commented.
The study authors concluded somewhat differently.
“In conclusion, adenocarcinoma rates increased in many early-onset subgroups but showed no significant increase in others, including colon-only cases in persons aged 20-29 and 50-54 years,” the investigators wrote.
They also observed that “rectal carcinoid tumors are increasing in young patients and may have a substantial impact on overall CRC incident rates.”
Those findings on rectal carcinoid tumors “underscore the importance of assessing histologic CRC subtypes independently,” the researchers said.
This new approach, of which the current study is a first effort, “may lead to a better understanding of the drivers of temporal changes in overall CRC incidence and a more accurate measurement of the outcomes of adenocarcinoma risk reduction efforts, and can guide future research.”
The study had no outside funding. Dr. Karlitz reported personal fees from Exact Sciences, personal fees from Myriad Genetics, and other fees from Gastro Girl and GI OnDEMAND, outside the submitted work. Dr. Bretthauer reports grants from Norwegian Research Council, grants from Norwegian Cancer Society for research in colorectal cancer screening. Dr. Weinberg and Dr. Kalager have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Implications for CRC screening.
Implications for CRC screening.
New estimates for the risk of CRC in young adults, which differentiate colorectal adenocarcinoma from other types, are reported in a study published Dec. 15, 2020, in Annals of Internal Medicine.
They are important because this finding has implications for CRC screening, say a trio of experts in an accompanying editorial.
Reports of an increase in the incidence of CRC in younger adults have led to changes in screening for this cancer in the United States. The age for starting CRC screening has been lowered to 45 years (instead of 50 years) in recommendations issued in 2018 by the American Cancer Society, and also more recently in preliminary recommendations from the U.S. Preventive Services Task Force.
However, that 2018 ACS recommendation to lower the starting age to 45 years was based to a large extent on a report of a higher incidence of CRC in younger adults from a 2017 study that used the SEER (Surveillance, Epidemiology, and End Results) database).
But that SEER-based study considered “colorectal cancer” as a homogeneous group defined by topology, the editorialists pointed out.
The new study, the editorialists said, uses that same SEER database but has “disentangled colorectal adenocarcinoma, the target for screening, from other histologic CRC types, including neuroendocrine (carcinoid) tumors, for which screening is not recommended.”
The study authors explained that adenocarcinoma is a target for prevention through screening because it arises from precancerous polyps. Those growths can be detected and removed before cancer develops. That doesn’t apply to carcinoid tumors, which are frequently incidental findings on flexible sigmoidoscopy or colonoscopy.
These carcinoid tumors typically are indolent, with a better prognosis than most other cancer types, the editorialists added. “Most likely, the majority of carcinoid tumors identified by screening represent incidental findings with little health benefit from detection. In fact, many may be characterized as overdiagnosed tumors, which by definition increase the burden and harms of screening without the balance of additional benefit.”
This new analysis showed that 4%-20% of the lesions previously described as CRC were not adenocarcinoma but carcinoid tumors, the editorialists pointed out.
This figure rose even higher in the subgroup of findings pertaining to the rectum, the colonic segment with the largest reported increase in early-onset CRC. Here, up to 34% of lesions (depending on patient age) were carcinoid tumors rather than adenocarcinoma, they noted.
The three editorialists – Michael Bretthauer, MD, PhD, and Mette Kalager, MD, PhD, both of the University of Oslo, and David Weinberg, MD, MSc, of Fox Chase Cancer Center, Philadelphia – call for action based on the new findings.
“The ACS’s 2018 estimate of about 7,000 new CRC cases among persons aged 45-49 years in the United States (the justification for screening) needs to be adjusted downward on the basis of the new evidence,” the trio wrote.
They conclude that “caution is warranted when promoting the benefits of CRC screening for persons younger than 50 years.”
However, the senior author of the new study, Jordan Karlitz, MD, of Tulane University, New Orleans, strongly disagreed.
Contrary to the editorialists, Dr. Karlitz said in an interview that he and his colleagues firmly believe that colorectal cancer screening for average-risk patients should begin at age 45 and that their new research, despite its clarification about carcinoid tumors, provides evidence for that.
“There are a number of other studies that support screening at age 45 as well,” he said. “This [new] finding supports the presence of a large preclinical colorectal cancer case burden in patients in their 40s that is ultimately uncovered with screening initiation at age 50. Many of these cancers could be prevented or diagnosed at an earlier stage with screening at age 45.”
“This is the first study to analyze early-onset colorectal cancer by specific histologic subtype,” Dr. Karlitz also pointed out.
“Although colorectal carcinoids are increasing at a faster rate than adenocarcinomas, adenocarcinomas constitute the overwhelming majority of colorectal cancers in people in their 40s and are also steadily increasing, which has implications for beginning screening at age 45,” he said.
Adenocarcinomas also make up the “overwhelming majority” of colorectal cancers in patients under 50 overall and “are the main driving force behind the increased colorectal cancer burden we are seeing in young patients,” Dr. Karlitz added.
Furthermore, “modeling studies on which the USPSTF screening recommendations were based [which recommended starting at age 45] were confined to adenocarcinoma, thus excluding carcinoids from their analysis,” he said.
Steepest changes in adenocarcinomas in younger groups
In their study, Dr. Karlitz and colleagues assessed the incidence rates of early colorectal cancer, using SEER data from 2000 to 2016, and stratifying the data by histologic subtype (primarily adenocarcinoma and carcinoid tumors), age group (20-29, 30-39, 40-49, and 50-54 years), and subsite.
A total of 123,143 CRC cases were identified in 119,624 patients between the ages of 20-54 years during that time period.
The absolute incidence rates in the younger age groups (20-29 and 30-39 years) were very low, compared with those aged 40-49 and 50-54 years.
The greatest 3-year average annual incident rate changes in adenocarcinoma (2000-2002 vs. 2014-2016) for any age group or subsite were for rectal-only cases in the 20-29 years group (+39%), as well as rectal-only cases in those aged 30-39 years (+39%), and colon-only cases in the age 30-39 group (+20%).
There was also significant increase in rectal-only adenocarcinoma in individuals aged 50-54 years (+10%). A statistically significant increase in the annual percentage change for adenocarcinomas was observed for all age groups, except for colon-only cases in the 20-29 years group (0.7%) and for both colorectal (0.2%) and colon-only cases (–0.1%) in those aged 50-54 years.
Even though the absolute carcinoid tumor incidence rates were lower than for adenocarcinoma in all age groups and subsites, a statistically significant increase was observed in the 3-year average annual incidence rate of combined-site colorectal carcinoid tumors in all age groups from 2000–2002 and 2014–2016. This increase was largely the result of increases in rectal carcinoid tumors, the authors note.
The authors also highlighted the results in the 40- to 49-year age group “because of differing opinions on whether to begin average-risk screening at age 45 or 50 years.”
They reported that rates of rectal and colon adenocarcinoma are increasing “substantially,” whether measured by changes in 3-year average annual incidence rate or by annual percentage changes. The change in average annual incidence rate of colon-only adenocarcinoma for persons aged 40-49 years was 13% (12.21 to 13.85 per 100,000), and that of rectal adenocarcinoma was 16% (7.50 to 8.72 per 100,000). Corresponding annual percentage changes were 0.8% and 1.2%, respectively. “These significant increases in adenocarcinoma incident rates add to the debate over earlier screening at age 45 years,” they commented.
Calls for next steps
The editorialists emphasize restraint when promoting the benefits of colorectal screening for persons younger than 50 years.
They point out that the USPSTF released a provisional update of its CRC screening recommendations about lowering the age to initiate screening to 45 years, as reported by this news organization.
“No new empirical evidence has been found since the USPSTF update in 2016 to inform the effectiveness of screening in persons younger than 50 years,” they write, adding that similar to the American Cancer Society in 2018, the task force has relied exclusively on modeling studies.
This new data from Dr. Karlitz and colleagues “should prompt the modelers to recalculate their estimates of benefits and harms of screening,” they suggested. “Revisiting the model would also allow competing forms of CRC screening to be compared in light of new risk assumptions.
“Previous assumptions that screening tests are equally effective in younger and older patients and that screening adherence will approach 100% may also be reconsidered,” the editorialist commented.
The study authors concluded somewhat differently.
“In conclusion, adenocarcinoma rates increased in many early-onset subgroups but showed no significant increase in others, including colon-only cases in persons aged 20-29 and 50-54 years,” the investigators wrote.
They also observed that “rectal carcinoid tumors are increasing in young patients and may have a substantial impact on overall CRC incident rates.”
Those findings on rectal carcinoid tumors “underscore the importance of assessing histologic CRC subtypes independently,” the researchers said.
This new approach, of which the current study is a first effort, “may lead to a better understanding of the drivers of temporal changes in overall CRC incidence and a more accurate measurement of the outcomes of adenocarcinoma risk reduction efforts, and can guide future research.”
The study had no outside funding. Dr. Karlitz reported personal fees from Exact Sciences, personal fees from Myriad Genetics, and other fees from Gastro Girl and GI OnDEMAND, outside the submitted work. Dr. Bretthauer reports grants from Norwegian Research Council, grants from Norwegian Cancer Society for research in colorectal cancer screening. Dr. Weinberg and Dr. Kalager have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New estimates for the risk of CRC in young adults, which differentiate colorectal adenocarcinoma from other types, are reported in a study published Dec. 15, 2020, in Annals of Internal Medicine.
They are important because this finding has implications for CRC screening, say a trio of experts in an accompanying editorial.
Reports of an increase in the incidence of CRC in younger adults have led to changes in screening for this cancer in the United States. The age for starting CRC screening has been lowered to 45 years (instead of 50 years) in recommendations issued in 2018 by the American Cancer Society, and also more recently in preliminary recommendations from the U.S. Preventive Services Task Force.
However, that 2018 ACS recommendation to lower the starting age to 45 years was based to a large extent on a report of a higher incidence of CRC in younger adults from a 2017 study that used the SEER (Surveillance, Epidemiology, and End Results) database).
But that SEER-based study considered “colorectal cancer” as a homogeneous group defined by topology, the editorialists pointed out.
The new study, the editorialists said, uses that same SEER database but has “disentangled colorectal adenocarcinoma, the target for screening, from other histologic CRC types, including neuroendocrine (carcinoid) tumors, for which screening is not recommended.”
The study authors explained that adenocarcinoma is a target for prevention through screening because it arises from precancerous polyps. Those growths can be detected and removed before cancer develops. That doesn’t apply to carcinoid tumors, which are frequently incidental findings on flexible sigmoidoscopy or colonoscopy.
These carcinoid tumors typically are indolent, with a better prognosis than most other cancer types, the editorialists added. “Most likely, the majority of carcinoid tumors identified by screening represent incidental findings with little health benefit from detection. In fact, many may be characterized as overdiagnosed tumors, which by definition increase the burden and harms of screening without the balance of additional benefit.”
This new analysis showed that 4%-20% of the lesions previously described as CRC were not adenocarcinoma but carcinoid tumors, the editorialists pointed out.
This figure rose even higher in the subgroup of findings pertaining to the rectum, the colonic segment with the largest reported increase in early-onset CRC. Here, up to 34% of lesions (depending on patient age) were carcinoid tumors rather than adenocarcinoma, they noted.
The three editorialists – Michael Bretthauer, MD, PhD, and Mette Kalager, MD, PhD, both of the University of Oslo, and David Weinberg, MD, MSc, of Fox Chase Cancer Center, Philadelphia – call for action based on the new findings.
“The ACS’s 2018 estimate of about 7,000 new CRC cases among persons aged 45-49 years in the United States (the justification for screening) needs to be adjusted downward on the basis of the new evidence,” the trio wrote.
They conclude that “caution is warranted when promoting the benefits of CRC screening for persons younger than 50 years.”
However, the senior author of the new study, Jordan Karlitz, MD, of Tulane University, New Orleans, strongly disagreed.
Contrary to the editorialists, Dr. Karlitz said in an interview that he and his colleagues firmly believe that colorectal cancer screening for average-risk patients should begin at age 45 and that their new research, despite its clarification about carcinoid tumors, provides evidence for that.
“There are a number of other studies that support screening at age 45 as well,” he said. “This [new] finding supports the presence of a large preclinical colorectal cancer case burden in patients in their 40s that is ultimately uncovered with screening initiation at age 50. Many of these cancers could be prevented or diagnosed at an earlier stage with screening at age 45.”
“This is the first study to analyze early-onset colorectal cancer by specific histologic subtype,” Dr. Karlitz also pointed out.
“Although colorectal carcinoids are increasing at a faster rate than adenocarcinomas, adenocarcinomas constitute the overwhelming majority of colorectal cancers in people in their 40s and are also steadily increasing, which has implications for beginning screening at age 45,” he said.
Adenocarcinomas also make up the “overwhelming majority” of colorectal cancers in patients under 50 overall and “are the main driving force behind the increased colorectal cancer burden we are seeing in young patients,” Dr. Karlitz added.
Furthermore, “modeling studies on which the USPSTF screening recommendations were based [which recommended starting at age 45] were confined to adenocarcinoma, thus excluding carcinoids from their analysis,” he said.
Steepest changes in adenocarcinomas in younger groups
In their study, Dr. Karlitz and colleagues assessed the incidence rates of early colorectal cancer, using SEER data from 2000 to 2016, and stratifying the data by histologic subtype (primarily adenocarcinoma and carcinoid tumors), age group (20-29, 30-39, 40-49, and 50-54 years), and subsite.
A total of 123,143 CRC cases were identified in 119,624 patients between the ages of 20-54 years during that time period.
The absolute incidence rates in the younger age groups (20-29 and 30-39 years) were very low, compared with those aged 40-49 and 50-54 years.
The greatest 3-year average annual incident rate changes in adenocarcinoma (2000-2002 vs. 2014-2016) for any age group or subsite were for rectal-only cases in the 20-29 years group (+39%), as well as rectal-only cases in those aged 30-39 years (+39%), and colon-only cases in the age 30-39 group (+20%).
There was also significant increase in rectal-only adenocarcinoma in individuals aged 50-54 years (+10%). A statistically significant increase in the annual percentage change for adenocarcinomas was observed for all age groups, except for colon-only cases in the 20-29 years group (0.7%) and for both colorectal (0.2%) and colon-only cases (–0.1%) in those aged 50-54 years.
Even though the absolute carcinoid tumor incidence rates were lower than for adenocarcinoma in all age groups and subsites, a statistically significant increase was observed in the 3-year average annual incidence rate of combined-site colorectal carcinoid tumors in all age groups from 2000–2002 and 2014–2016. This increase was largely the result of increases in rectal carcinoid tumors, the authors note.
The authors also highlighted the results in the 40- to 49-year age group “because of differing opinions on whether to begin average-risk screening at age 45 or 50 years.”
They reported that rates of rectal and colon adenocarcinoma are increasing “substantially,” whether measured by changes in 3-year average annual incidence rate or by annual percentage changes. The change in average annual incidence rate of colon-only adenocarcinoma for persons aged 40-49 years was 13% (12.21 to 13.85 per 100,000), and that of rectal adenocarcinoma was 16% (7.50 to 8.72 per 100,000). Corresponding annual percentage changes were 0.8% and 1.2%, respectively. “These significant increases in adenocarcinoma incident rates add to the debate over earlier screening at age 45 years,” they commented.
Calls for next steps
The editorialists emphasize restraint when promoting the benefits of colorectal screening for persons younger than 50 years.
They point out that the USPSTF released a provisional update of its CRC screening recommendations about lowering the age to initiate screening to 45 years, as reported by this news organization.
“No new empirical evidence has been found since the USPSTF update in 2016 to inform the effectiveness of screening in persons younger than 50 years,” they write, adding that similar to the American Cancer Society in 2018, the task force has relied exclusively on modeling studies.
This new data from Dr. Karlitz and colleagues “should prompt the modelers to recalculate their estimates of benefits and harms of screening,” they suggested. “Revisiting the model would also allow competing forms of CRC screening to be compared in light of new risk assumptions.
“Previous assumptions that screening tests are equally effective in younger and older patients and that screening adherence will approach 100% may also be reconsidered,” the editorialist commented.
The study authors concluded somewhat differently.
“In conclusion, adenocarcinoma rates increased in many early-onset subgroups but showed no significant increase in others, including colon-only cases in persons aged 20-29 and 50-54 years,” the investigators wrote.
They also observed that “rectal carcinoid tumors are increasing in young patients and may have a substantial impact on overall CRC incident rates.”
Those findings on rectal carcinoid tumors “underscore the importance of assessing histologic CRC subtypes independently,” the researchers said.
This new approach, of which the current study is a first effort, “may lead to a better understanding of the drivers of temporal changes in overall CRC incidence and a more accurate measurement of the outcomes of adenocarcinoma risk reduction efforts, and can guide future research.”
The study had no outside funding. Dr. Karlitz reported personal fees from Exact Sciences, personal fees from Myriad Genetics, and other fees from Gastro Girl and GI OnDEMAND, outside the submitted work. Dr. Bretthauer reports grants from Norwegian Research Council, grants from Norwegian Cancer Society for research in colorectal cancer screening. Dr. Weinberg and Dr. Kalager have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Geography and behaviors linked to early-onset colorectal cancer survival in U.S. women
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
FROM CLINICAL AND TRANSLATIONAL GASTROENTEROLOGY
Statins may lower risk of colorectal cancer
Statin use may significantly lower the risk of colorectal cancer (CRC) in patients with or without inflammatory bowel disease (IBD), based on a meta-analysis and systematic review.
In more than 15,000 patients with IBD, statin use was associated with a 60% reduced risk of CRC, reported lead author Kevin N. Singh, MD, of NYU Langone Medical Center in New York, and colleagues.
“Statin use has been linked with a risk reduction for cancers including hepatocellular carcinoma, breast, gastric, pancreatic, and biliary tract cancers, but data supporting the use of statins for chemoprevention against CRC is conflicting,” Dr. Singh said during a virtual presentation at the annual meeting of the American College of Gastroenterology.
He noted a 2014 meta-analysis by Lytras and colleagues that reported a 9% CRC risk reduction in statin users who did not have IBD. In patients with IBD, data are scarce, according to Dr. Singh.
To further explore the relationship between statin use and CRC in patients without IBD, the investigators analyzed data from 52 studies, including 8 randomized clinical trials, 17 cohort studies, and 27 case-control studies. Of the 11,459,306 patients involved, approximately 2 million used statins and roughly 9 million did not.
To evaluate the same relationship in patients with IBD, the investigators conducted a separate meta-analysis involving 15,342 patients from 5 observational studies, 1 of which was an unpublished abstract. In the 4 published studies, 1,161 patients used statins while 12,145 did not.
In the non-IBD population, statin use was associated with a 20% reduced risk of CRC (pooled odds ratio, 0.80; 95% confidence interval, 0.73-0.88; P less than .001). In patients with IBD, statin use was associated with a 60% CRC risk reduction (pooled OR, 0.40; 95% CI, 0.19-0.86, P = .019).
Dr. Singh noted “significant heterogeneity” in both analyses (I2 greater than 75), most prominently in the IBD populations, which he ascribed to “differences in demographic features, ethnic groups, and risk factors for CRC.”
While publication bias was absent from the non-IBD analysis, it was detected in the IBD portion of the study. Dr. Singh said that selection bias may also have been present in the IBD analysis, due to exclusive use of observational studies.
“Prospective trials are needed to confirm the risk reduction of CRC in the IBD population, including whether the effects of statins differ between ulcerative colitis and Crohn’s disease patients,” Dr. Singh said.
Additional analyses are underway, he added, including one that will account for the potentially confounding effect of aspirin use.
According to David E. Kaplan, MD, of the University of Pennsylvania, Philadelphia, “The finding that statins are associated with reduced CRC in IBD provides additional support for the clinical importance of the antineoplastic effects of statins. This effect has been strongly observed in liver cancer, and is pending prospective validation.”
Dr. Kaplan also offered some mechanistic insight into why statins have an anticancer effect, pointing to “the centrality of cholesterol biosynthesis for development and/or progression of malignancy.”
The investigators and Dr. Kaplan reported no relevant conflicts of interest.
Statin use may significantly lower the risk of colorectal cancer (CRC) in patients with or without inflammatory bowel disease (IBD), based on a meta-analysis and systematic review.
In more than 15,000 patients with IBD, statin use was associated with a 60% reduced risk of CRC, reported lead author Kevin N. Singh, MD, of NYU Langone Medical Center in New York, and colleagues.
“Statin use has been linked with a risk reduction for cancers including hepatocellular carcinoma, breast, gastric, pancreatic, and biliary tract cancers, but data supporting the use of statins for chemoprevention against CRC is conflicting,” Dr. Singh said during a virtual presentation at the annual meeting of the American College of Gastroenterology.
He noted a 2014 meta-analysis by Lytras and colleagues that reported a 9% CRC risk reduction in statin users who did not have IBD. In patients with IBD, data are scarce, according to Dr. Singh.
To further explore the relationship between statin use and CRC in patients without IBD, the investigators analyzed data from 52 studies, including 8 randomized clinical trials, 17 cohort studies, and 27 case-control studies. Of the 11,459,306 patients involved, approximately 2 million used statins and roughly 9 million did not.
To evaluate the same relationship in patients with IBD, the investigators conducted a separate meta-analysis involving 15,342 patients from 5 observational studies, 1 of which was an unpublished abstract. In the 4 published studies, 1,161 patients used statins while 12,145 did not.
In the non-IBD population, statin use was associated with a 20% reduced risk of CRC (pooled odds ratio, 0.80; 95% confidence interval, 0.73-0.88; P less than .001). In patients with IBD, statin use was associated with a 60% CRC risk reduction (pooled OR, 0.40; 95% CI, 0.19-0.86, P = .019).
Dr. Singh noted “significant heterogeneity” in both analyses (I2 greater than 75), most prominently in the IBD populations, which he ascribed to “differences in demographic features, ethnic groups, and risk factors for CRC.”
While publication bias was absent from the non-IBD analysis, it was detected in the IBD portion of the study. Dr. Singh said that selection bias may also have been present in the IBD analysis, due to exclusive use of observational studies.
“Prospective trials are needed to confirm the risk reduction of CRC in the IBD population, including whether the effects of statins differ between ulcerative colitis and Crohn’s disease patients,” Dr. Singh said.
Additional analyses are underway, he added, including one that will account for the potentially confounding effect of aspirin use.
According to David E. Kaplan, MD, of the University of Pennsylvania, Philadelphia, “The finding that statins are associated with reduced CRC in IBD provides additional support for the clinical importance of the antineoplastic effects of statins. This effect has been strongly observed in liver cancer, and is pending prospective validation.”
Dr. Kaplan also offered some mechanistic insight into why statins have an anticancer effect, pointing to “the centrality of cholesterol biosynthesis for development and/or progression of malignancy.”
The investigators and Dr. Kaplan reported no relevant conflicts of interest.
Statin use may significantly lower the risk of colorectal cancer (CRC) in patients with or without inflammatory bowel disease (IBD), based on a meta-analysis and systematic review.
In more than 15,000 patients with IBD, statin use was associated with a 60% reduced risk of CRC, reported lead author Kevin N. Singh, MD, of NYU Langone Medical Center in New York, and colleagues.
“Statin use has been linked with a risk reduction for cancers including hepatocellular carcinoma, breast, gastric, pancreatic, and biliary tract cancers, but data supporting the use of statins for chemoprevention against CRC is conflicting,” Dr. Singh said during a virtual presentation at the annual meeting of the American College of Gastroenterology.
He noted a 2014 meta-analysis by Lytras and colleagues that reported a 9% CRC risk reduction in statin users who did not have IBD. In patients with IBD, data are scarce, according to Dr. Singh.
To further explore the relationship between statin use and CRC in patients without IBD, the investigators analyzed data from 52 studies, including 8 randomized clinical trials, 17 cohort studies, and 27 case-control studies. Of the 11,459,306 patients involved, approximately 2 million used statins and roughly 9 million did not.
To evaluate the same relationship in patients with IBD, the investigators conducted a separate meta-analysis involving 15,342 patients from 5 observational studies, 1 of which was an unpublished abstract. In the 4 published studies, 1,161 patients used statins while 12,145 did not.
In the non-IBD population, statin use was associated with a 20% reduced risk of CRC (pooled odds ratio, 0.80; 95% confidence interval, 0.73-0.88; P less than .001). In patients with IBD, statin use was associated with a 60% CRC risk reduction (pooled OR, 0.40; 95% CI, 0.19-0.86, P = .019).
Dr. Singh noted “significant heterogeneity” in both analyses (I2 greater than 75), most prominently in the IBD populations, which he ascribed to “differences in demographic features, ethnic groups, and risk factors for CRC.”
While publication bias was absent from the non-IBD analysis, it was detected in the IBD portion of the study. Dr. Singh said that selection bias may also have been present in the IBD analysis, due to exclusive use of observational studies.
“Prospective trials are needed to confirm the risk reduction of CRC in the IBD population, including whether the effects of statins differ between ulcerative colitis and Crohn’s disease patients,” Dr. Singh said.
Additional analyses are underway, he added, including one that will account for the potentially confounding effect of aspirin use.
According to David E. Kaplan, MD, of the University of Pennsylvania, Philadelphia, “The finding that statins are associated with reduced CRC in IBD provides additional support for the clinical importance of the antineoplastic effects of statins. This effect has been strongly observed in liver cancer, and is pending prospective validation.”
Dr. Kaplan also offered some mechanistic insight into why statins have an anticancer effect, pointing to “the centrality of cholesterol biosynthesis for development and/or progression of malignancy.”
The investigators and Dr. Kaplan reported no relevant conflicts of interest.
FROM ACG 2020
Now USPSTF also suggests start CRC screening at age 45
that is open for public comment.
“This is the only change that was made,” said task force member Michael Barry, MD, director of the Informed Medical Decisions Program in the Health Decision Sciences Center at Massachusetts General Hospital, Boston.
The recommendation is that all adults aged 45-75 years be screened for CRC.
This is an “A” recommendation for adults aged 50-75 and a “B” recommendation for adults aged 45-49. Dr. Barry explained that the reason for this difference is that the benefit is smaller for the 45- to 49-years age group. “But there’s not much difference between A and B from a practical standpoint,” he explained.
For adults aged 76-85, the benefits and harms of screening need to be weighed against the individual’s overall health and personal circumstances. This is a “C” recommendation.
Barry emphasized that the USPSTF document is not final. The draft recommendation and supporting evidence is posted on the task force website and will be available for public comments until Nov. 23.
Mounting pressure
The move comes after mounting evidence of an increase in CRC among younger adults and mounting pressure to lower the starting age.
Two years ago, the American Cancer Society (ACS) revised its own screening guidelines and lowered the starting age to 45 years. Soon afterward, a coalition of 22 public health and patient advocacy groups joined the ACS in submitting a letter to the USPSTF asking that the task force reconsider its 2016 guidance (which recommends starting at age 50 years).
The starting age for screening is an important issue, commented Judy Yee, MD, chair of radiology at the Albert Einstein College of Medicine and the Montefiore Health System in New York and chair of the Colon Cancer Committee of the American College of Radiology.
“Right now it is very confusing to physicians and to the public,” Dr. Yee said in an interview at that time. “The USPSTF and the ACS differ as far as the age to begin screening, and insurers may not cover the cost of colorectal cancer screening before age 50.”
Dr. Barry said that the Task Force took notice of recent data showing an increase in the incidence of CRC among younger adults. “The risk now for age 45 to 49 is pretty similar to the risk for people in their early 50s. So in some ways, today’s late 40-year-olds are like yesterday’s 50-year-olds,” he commented.
The task force used simulation models that confirmed what the epidemiologic data suggested and “that we could prevent some additional colorectal cancer deaths by starting screening at age 45,” he said.
The rest of the new draft recommendation is similar to the 2016 guidelines, in which the task force says there is convincing evidence that CRC screening substantially reduces disease-related mortality. However, it does not recommend any one screening approach over another. It recommends both direct visualization, such as colonoscopy, as well as noninvasive stool-based tests. It does not recommend serum tests, urine tests, or capsule endoscopy because there is not yet enough evidence about the benefits and harms of these tests.
“The right test is the one a patient will do,” Dr. Barry commented.
Defining populations
CRC in young adults made the news in August 2020 when Chadwick Boseman, known for his role as King T’Challa in Marvel’s “Black Panther,” died of colon cancer. Diagnosed in 2016, he was only 43 years old.
“The recent passing of Chadwick Boseman is tragic, and our thoughts are with his loved ones during this difficult time,” said Dr. Barry. “As a Black man, the data show that Chadwick was at higher risk for developing colorectal cancer.”
Unfortunately, there is currently not enough evidence that screening Black men younger than 45 could help prevent tragic deaths such as Chadwick’s, he commented. “The task force is calling for more research on colorectal cancer screening in Black adults,” he added.
Limit screening to those at higher risk
In contrast to the USPSTF and ACS guidelines, which recommend screening for CRC for everyone over a certain age, a set of recommendations developed by an international panel of experts suggests screening only for individuals who are at higher risk for CRC.
As previously reported, these guidelines suggest restricting screening to adults whose cumulative cancer risk is 3% or more in the next 15 years, the point at which the balance between benefits and harms favors screening.
The authors, led by Lise Helsingen, MD, Clinical Effectiveness Research Group, University of Oslo, said “the optimal choice for each person requires shared decision-making.”
Such a risk-based approach is “increasingly regarded as the most appropriate way to discuss cancer screening.” That approach is already used in prostate and lung cancer screening, they noted.
A version of this article originally appeared on Medscape.com.
Clinicians and researchers have actively debated the pros and cons of lowering the screening age to 45 years since 2018, when the American Cancer Society released its colorectal cancer (CRC) screening guidelines. The most compelling argument in support of lowering the screening age is that recent data from Surveillance Epidemiology and End Results (SEER) show that the CRC incidence rates in 45- to 50-year-olds are similar to rates seen in 50- to 54-year-olds about 20 years ago, when the first guidelines to initiate screening at age 50 were widely established. Termed early-onset CRC (EOCRC), the underlying reasons for this increase are not completely understood, and while the absolute numbers of EOCRC cases are smaller than in older age groups, modeling studies show that screening this age group is both efficient and effective.
Over the last 20 years we have made major strides in reducing the incidence and mortality from CRC in ages 50 years and older, and now we must rise to the challenge of delivering CRC screening to this younger group in order to see similar dividends over time and curb the rising incidence curve of EOCRC. And we must do so without direct evidence to guide us as to the magnitude of the benefit of screening this younger group, the best modality to use, or tools to risk stratify who is likely to benefit from screening in this group. We must also be careful not to worsen racial and geographic disparities in CRC screening, which already exist for African Americans, Native Americans, and other minorities and rural residents. Finally, even though the goal posts are changing, our target remains to get to 80% screening rates for all age groups, and not neglect the currently underscreened 50- to 75-year-olds, who are at a much higher risk of CRC than their younger counterparts.
Aasma Shaukat, MD, MPH, is an investigator, Center for Care Delivery and Outcomes Research, section chief and staff physician, GI section, Minneapolis VA Health Care System; staff physician, Fairview University of Minnesota Medical Center, Minneapolis; and professor, University of Minnesota department of medicine, division of gastroenterology, Minneapolis. She has no conflicts of interest.
Clinicians and researchers have actively debated the pros and cons of lowering the screening age to 45 years since 2018, when the American Cancer Society released its colorectal cancer (CRC) screening guidelines. The most compelling argument in support of lowering the screening age is that recent data from Surveillance Epidemiology and End Results (SEER) show that the CRC incidence rates in 45- to 50-year-olds are similar to rates seen in 50- to 54-year-olds about 20 years ago, when the first guidelines to initiate screening at age 50 were widely established. Termed early-onset CRC (EOCRC), the underlying reasons for this increase are not completely understood, and while the absolute numbers of EOCRC cases are smaller than in older age groups, modeling studies show that screening this age group is both efficient and effective.
Over the last 20 years we have made major strides in reducing the incidence and mortality from CRC in ages 50 years and older, and now we must rise to the challenge of delivering CRC screening to this younger group in order to see similar dividends over time and curb the rising incidence curve of EOCRC. And we must do so without direct evidence to guide us as to the magnitude of the benefit of screening this younger group, the best modality to use, or tools to risk stratify who is likely to benefit from screening in this group. We must also be careful not to worsen racial and geographic disparities in CRC screening, which already exist for African Americans, Native Americans, and other minorities and rural residents. Finally, even though the goal posts are changing, our target remains to get to 80% screening rates for all age groups, and not neglect the currently underscreened 50- to 75-year-olds, who are at a much higher risk of CRC than their younger counterparts.
Aasma Shaukat, MD, MPH, is an investigator, Center for Care Delivery and Outcomes Research, section chief and staff physician, GI section, Minneapolis VA Health Care System; staff physician, Fairview University of Minnesota Medical Center, Minneapolis; and professor, University of Minnesota department of medicine, division of gastroenterology, Minneapolis. She has no conflicts of interest.
Clinicians and researchers have actively debated the pros and cons of lowering the screening age to 45 years since 2018, when the American Cancer Society released its colorectal cancer (CRC) screening guidelines. The most compelling argument in support of lowering the screening age is that recent data from Surveillance Epidemiology and End Results (SEER) show that the CRC incidence rates in 45- to 50-year-olds are similar to rates seen in 50- to 54-year-olds about 20 years ago, when the first guidelines to initiate screening at age 50 were widely established. Termed early-onset CRC (EOCRC), the underlying reasons for this increase are not completely understood, and while the absolute numbers of EOCRC cases are smaller than in older age groups, modeling studies show that screening this age group is both efficient and effective.
Over the last 20 years we have made major strides in reducing the incidence and mortality from CRC in ages 50 years and older, and now we must rise to the challenge of delivering CRC screening to this younger group in order to see similar dividends over time and curb the rising incidence curve of EOCRC. And we must do so without direct evidence to guide us as to the magnitude of the benefit of screening this younger group, the best modality to use, or tools to risk stratify who is likely to benefit from screening in this group. We must also be careful not to worsen racial and geographic disparities in CRC screening, which already exist for African Americans, Native Americans, and other minorities and rural residents. Finally, even though the goal posts are changing, our target remains to get to 80% screening rates for all age groups, and not neglect the currently underscreened 50- to 75-year-olds, who are at a much higher risk of CRC than their younger counterparts.
Aasma Shaukat, MD, MPH, is an investigator, Center for Care Delivery and Outcomes Research, section chief and staff physician, GI section, Minneapolis VA Health Care System; staff physician, Fairview University of Minnesota Medical Center, Minneapolis; and professor, University of Minnesota department of medicine, division of gastroenterology, Minneapolis. She has no conflicts of interest.
that is open for public comment.
“This is the only change that was made,” said task force member Michael Barry, MD, director of the Informed Medical Decisions Program in the Health Decision Sciences Center at Massachusetts General Hospital, Boston.
The recommendation is that all adults aged 45-75 years be screened for CRC.
This is an “A” recommendation for adults aged 50-75 and a “B” recommendation for adults aged 45-49. Dr. Barry explained that the reason for this difference is that the benefit is smaller for the 45- to 49-years age group. “But there’s not much difference between A and B from a practical standpoint,” he explained.
For adults aged 76-85, the benefits and harms of screening need to be weighed against the individual’s overall health and personal circumstances. This is a “C” recommendation.
Barry emphasized that the USPSTF document is not final. The draft recommendation and supporting evidence is posted on the task force website and will be available for public comments until Nov. 23.
Mounting pressure
The move comes after mounting evidence of an increase in CRC among younger adults and mounting pressure to lower the starting age.
Two years ago, the American Cancer Society (ACS) revised its own screening guidelines and lowered the starting age to 45 years. Soon afterward, a coalition of 22 public health and patient advocacy groups joined the ACS in submitting a letter to the USPSTF asking that the task force reconsider its 2016 guidance (which recommends starting at age 50 years).
The starting age for screening is an important issue, commented Judy Yee, MD, chair of radiology at the Albert Einstein College of Medicine and the Montefiore Health System in New York and chair of the Colon Cancer Committee of the American College of Radiology.
“Right now it is very confusing to physicians and to the public,” Dr. Yee said in an interview at that time. “The USPSTF and the ACS differ as far as the age to begin screening, and insurers may not cover the cost of colorectal cancer screening before age 50.”
Dr. Barry said that the Task Force took notice of recent data showing an increase in the incidence of CRC among younger adults. “The risk now for age 45 to 49 is pretty similar to the risk for people in their early 50s. So in some ways, today’s late 40-year-olds are like yesterday’s 50-year-olds,” he commented.
The task force used simulation models that confirmed what the epidemiologic data suggested and “that we could prevent some additional colorectal cancer deaths by starting screening at age 45,” he said.
The rest of the new draft recommendation is similar to the 2016 guidelines, in which the task force says there is convincing evidence that CRC screening substantially reduces disease-related mortality. However, it does not recommend any one screening approach over another. It recommends both direct visualization, such as colonoscopy, as well as noninvasive stool-based tests. It does not recommend serum tests, urine tests, or capsule endoscopy because there is not yet enough evidence about the benefits and harms of these tests.
“The right test is the one a patient will do,” Dr. Barry commented.
Defining populations
CRC in young adults made the news in August 2020 when Chadwick Boseman, known for his role as King T’Challa in Marvel’s “Black Panther,” died of colon cancer. Diagnosed in 2016, he was only 43 years old.
“The recent passing of Chadwick Boseman is tragic, and our thoughts are with his loved ones during this difficult time,” said Dr. Barry. “As a Black man, the data show that Chadwick was at higher risk for developing colorectal cancer.”
Unfortunately, there is currently not enough evidence that screening Black men younger than 45 could help prevent tragic deaths such as Chadwick’s, he commented. “The task force is calling for more research on colorectal cancer screening in Black adults,” he added.
Limit screening to those at higher risk
In contrast to the USPSTF and ACS guidelines, which recommend screening for CRC for everyone over a certain age, a set of recommendations developed by an international panel of experts suggests screening only for individuals who are at higher risk for CRC.
As previously reported, these guidelines suggest restricting screening to adults whose cumulative cancer risk is 3% or more in the next 15 years, the point at which the balance between benefits and harms favors screening.
The authors, led by Lise Helsingen, MD, Clinical Effectiveness Research Group, University of Oslo, said “the optimal choice for each person requires shared decision-making.”
Such a risk-based approach is “increasingly regarded as the most appropriate way to discuss cancer screening.” That approach is already used in prostate and lung cancer screening, they noted.
A version of this article originally appeared on Medscape.com.
that is open for public comment.
“This is the only change that was made,” said task force member Michael Barry, MD, director of the Informed Medical Decisions Program in the Health Decision Sciences Center at Massachusetts General Hospital, Boston.
The recommendation is that all adults aged 45-75 years be screened for CRC.
This is an “A” recommendation for adults aged 50-75 and a “B” recommendation for adults aged 45-49. Dr. Barry explained that the reason for this difference is that the benefit is smaller for the 45- to 49-years age group. “But there’s not much difference between A and B from a practical standpoint,” he explained.
For adults aged 76-85, the benefits and harms of screening need to be weighed against the individual’s overall health and personal circumstances. This is a “C” recommendation.
Barry emphasized that the USPSTF document is not final. The draft recommendation and supporting evidence is posted on the task force website and will be available for public comments until Nov. 23.
Mounting pressure
The move comes after mounting evidence of an increase in CRC among younger adults and mounting pressure to lower the starting age.
Two years ago, the American Cancer Society (ACS) revised its own screening guidelines and lowered the starting age to 45 years. Soon afterward, a coalition of 22 public health and patient advocacy groups joined the ACS in submitting a letter to the USPSTF asking that the task force reconsider its 2016 guidance (which recommends starting at age 50 years).
The starting age for screening is an important issue, commented Judy Yee, MD, chair of radiology at the Albert Einstein College of Medicine and the Montefiore Health System in New York and chair of the Colon Cancer Committee of the American College of Radiology.
“Right now it is very confusing to physicians and to the public,” Dr. Yee said in an interview at that time. “The USPSTF and the ACS differ as far as the age to begin screening, and insurers may not cover the cost of colorectal cancer screening before age 50.”
Dr. Barry said that the Task Force took notice of recent data showing an increase in the incidence of CRC among younger adults. “The risk now for age 45 to 49 is pretty similar to the risk for people in their early 50s. So in some ways, today’s late 40-year-olds are like yesterday’s 50-year-olds,” he commented.
The task force used simulation models that confirmed what the epidemiologic data suggested and “that we could prevent some additional colorectal cancer deaths by starting screening at age 45,” he said.
The rest of the new draft recommendation is similar to the 2016 guidelines, in which the task force says there is convincing evidence that CRC screening substantially reduces disease-related mortality. However, it does not recommend any one screening approach over another. It recommends both direct visualization, such as colonoscopy, as well as noninvasive stool-based tests. It does not recommend serum tests, urine tests, or capsule endoscopy because there is not yet enough evidence about the benefits and harms of these tests.
“The right test is the one a patient will do,” Dr. Barry commented.
Defining populations
CRC in young adults made the news in August 2020 when Chadwick Boseman, known for his role as King T’Challa in Marvel’s “Black Panther,” died of colon cancer. Diagnosed in 2016, he was only 43 years old.
“The recent passing of Chadwick Boseman is tragic, and our thoughts are with his loved ones during this difficult time,” said Dr. Barry. “As a Black man, the data show that Chadwick was at higher risk for developing colorectal cancer.”
Unfortunately, there is currently not enough evidence that screening Black men younger than 45 could help prevent tragic deaths such as Chadwick’s, he commented. “The task force is calling for more research on colorectal cancer screening in Black adults,” he added.
Limit screening to those at higher risk
In contrast to the USPSTF and ACS guidelines, which recommend screening for CRC for everyone over a certain age, a set of recommendations developed by an international panel of experts suggests screening only for individuals who are at higher risk for CRC.
As previously reported, these guidelines suggest restricting screening to adults whose cumulative cancer risk is 3% or more in the next 15 years, the point at which the balance between benefits and harms favors screening.
The authors, led by Lise Helsingen, MD, Clinical Effectiveness Research Group, University of Oslo, said “the optimal choice for each person requires shared decision-making.”
Such a risk-based approach is “increasingly regarded as the most appropriate way to discuss cancer screening.” That approach is already used in prostate and lung cancer screening, they noted.
A version of this article originally appeared on Medscape.com.
Colorectal cancer screening guidelines: How to make best use of all of them
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
The recent death of “Black Panther” star Chadwick Boseman has resulted in colorectal cancer (CRC) screening guidelines receiving more attention. Mr. Boseman was diagnosed with Stage 3 CRC in 2016 and underwent treatment. He passed away 4 years later at the young age of 44.
Mr. Boseman’s death has highlighted two important concerns about current screening guidelines for CRC. These include racial disparities in patients with colon cancer and the fact that more younger patients are getting this disease.
There are at least three different sets of CRC screening recommendations from different trusted professional organizations that primary care physicians must decide how to follow. These organizations each published their guidelines indicating review of the best available evidence. On first glance there is discrepancy between these guidelines, but a closer look at them reveals they have a lot of similarities.
The U.S. Multi-Society Task Force of Colorectal Cancer (MSTF), which represents the American College of Gastroenterology, the American Gatroenterological Association, and the American Society for Gastrointestinal Endoscopy, is one of the organizations that offers guidelines. The MSTF recommends CRC screening for non-African American average risked persons at the age of 50 years (strong recommendation; moderate quality evidence). The first-tier options for this recommendation are to have a colonoscopy every 10 years or annual fecal immunochemial test. Additionally, the MSTF recommends beginning screening of African Americans at age 45 years (weak recommendation; very-low-quality evidence). This recommendation cites higher incidence rates, earlier mean age at onset, higher proportion of cancers before age 50 years and late-stage presentation. The MSTF indicates that the increased rate of CRC at an earlier age in African Americans is caused by a combination of biologic and societal factors, but do not point to what those are. This earlier screening is not backed by evidence that it in fact improves morbidity or mortality outcomes. The MSTF also address screening among high-risk individuals. Those with first degree relatives with CRC or advanced adenomas diagnosed before the age of 60 years should be screened beginning at age 40 years or 10 years younger than the age the relative was diagnosed, whichever comes first, according to the MSTF recommendations. These individuals should have a colonoscopy every 5 years, the MSTF says. Those with first degree relatives with CRC or advanced adenomas diagnosed at older than 60 years should have CRC beginning at 40 years, though with the same testing intervals as average-risk individuals.1
The American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), however, endorse the guidelines set forth by the United States Preventive Services Task Force (USPSTF). These guidelines were published in 2016 in the JAMA and notably are currently under review. These guidelines recommend routine screening for those at average risk at the age of 50 years. In the publication of these guidelines, the increasing incidence of CRC in those under 50 was acknowledged. It is however stated that the modest benefit of earlier diagnosis made via screening is not better than the increased risk of increased lifetime colonoscopy.2
The publication specifically addresses the disparity among Black adults who have the highest incidence and mortality rates in comparison with other racial/ethnic groups. These guidelines specifically state that there are higher rates of colon cancer among black adults. They however clarify that they think it is because of decreased screening and treatment in this group. When compared with other groups and the screening and treatment is controlled for, there is no longer a difference. Lowering the age for starting screening, therefore, won’t help resolve the disparity because the higher cases in Black adults has resulted from not enough Black adults being screened at the recommended age of 50, according to the USPSTF recommendation statement. As such, rather than changing the age of screening for Black adults, this publication recommends efforts to ensure that screening, follow-up, and treatment are received.
The USPSTF specifically did not include adults with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC. They instead refer to other professional organizations for these recommendations.2
The American Cancer Society (ACS) also had a separate guideline published in CA: A Cancer Journal for Clinicians. It provides a qualified recommendation that CRC screening begin at age 45 years for those with average risk. The guideline also includes a strong recommendation for CRC screening beginning at age 50 years. The qualified recommendation for the younger age group is based on the incidence of colorectal cancer being similar between those aged 45-49 and those aged 50-54 years. The ACS also hypothesized that screening at an earlier age will decrease the disparity among population groups with a higher burden. Importantly, this updated guideline prioritized incidence reduction rather than mortality reduction. The ACS also stressed the need for a multipronged approach to mitigate barriers to CRC screening at the individual, provider, organizational, and policy levels. Similar to the USPSTF, the ACS did not address the screening of those with known disorders that have a genetic predisposition to CRC or those with a first degree relative with CRC.3
In all of the publications discussing CRC screening guidelines, it is stressed that there is not sufficient uptake of any of these recommendations. Rather than conduct earlier screening, in my opinion, we should focus on programmatic ways to ensure that the existing screening recommendations are followed. This is a space in which we can help affect the disparity seen among population groups.
The most important screening test is the one that patients are willing to use. Primary care physicians can use any of these guidelines to have conversations with patients about risk and when to start screening. Although these guidelines may seem to be different from each other, each one includes strong recommendations with the same information.
Additional studies should be done to determine the benefits and harms of screening in patients with known risk factors such as obesity, cigarette smoking, diabetes, high consumption of alcohol, high consumption of red meat and processed food, inactivity, and low intake of dietary fiber, fruits, and vegetables. It is possible that the higher burden of disease among Black adults is related to societal factors leading to increased obesity and dietary habits that increase rates of CRC.
Primary care physicians would be better served by a tool that allows for risk stratification to help guide early screening for all patients. For certain patients, such a tool might result in them qualifying for screening that begins at a later age than the current guidelines recommend. Finally, primary care physicians must remember that these are just the guidelines for screening for CRC. They all specifically exclude patients experiencing any symptoms. As such, patients with unexplained bleeding, anemia, weight loss, and other symptoms should be evaluated fully, including being considered for colonoscopy to diagnose CRC. Primary care physicians should use these guidelines to screen their asymptomatic patients and should ensure that they provide evaluation of any of the symptoms of CRC.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is also program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on editorial advisory board of Family Practice News.
References
1. Rex DK et al. Gastrointest Endosc. 2017;86(1):18-33.
2. US Preventive Services Task Force. JAMA. 2016;315(23):2564-2575.
3. Wolf AMD et al. CA Cancer J Clin. 2018 Jul;68(4):250-281.
Delayed cancer screening could cause increase in deaths, study says
Delays in colorectal cancer screening due to the COVID-19 pandemic could lead to higher rates of advanced-stage cancer and death, according to a new study.
When compared with a delay of less than three months, the longer delay seen this year may result in an 11.9% increase in death rates.
“Across the globe, health care systems are facing serious difficulties while dealing with COVID-19, and it is imperative that support is given to the public and patients throughout the crisis, including for high-impact diseases such as colorectal cancer,” Luigi Ricciardiello, the lead study author and a professor at the University of Bologna in Italy, said in a statement.
Ricciardiello and colleagues presented their research on Monday at UEG Week Virtual 2020, an international conference for gastroenterologists. The study will be published in the UEG Journal .
The researchers created a model to forecast the effects of delayed cancer screening during 2020. A “moderate” delay of 7-12 months caused a 3% increase in advanced-stage colon cancer, and a long delay of more than 12 months caused a 7% increase in advanced cancer.
Based on a survival rate of 5 years for stage 3 or stage 4 colorectal cancer, the death rate would increase nearly 12% when screening is delayed for more than a year, as compared with less than three months of delay.
The research team found similar results when forecasting advanced-stage cancer and deaths earlier this year. In a paper published in Clinical Gastroenterology and Hepatology in early September, they projected that deaths could increase 12% if screening is delayed for more than a year.
Throughout the pandemic, screening programs have been delayed in many countries, particularly across Europe.
“Healthcare authorities need to act urgently on how they reorganise activities during COVID-19, without compromising the diagnosis of other high-impact diseases like this research shows,” Ricciardiello said.
United European Gastroenterology, a professional medical organization for digestive health specialists, has called for policymakers to implement colon cancer screening programs across the European Union. Annually, more than 375,000 new cases are diagnosed across the EU, and more than 170,000 people die from colorectal cancer, according to a UEG report.
“Early-stage diagnosis of colorectal cancer is crucial — it’s far easier to treat and enhances optimal patient outcomes,” Ricciardiello said. “It is therefore essential that vital diagnosis tools, like screening programmes, continue and help to prevent mortality rates from rising even further.”
This article first appeared on Medscape.com.
Delays in colorectal cancer screening due to the COVID-19 pandemic could lead to higher rates of advanced-stage cancer and death, according to a new study.
When compared with a delay of less than three months, the longer delay seen this year may result in an 11.9% increase in death rates.
“Across the globe, health care systems are facing serious difficulties while dealing with COVID-19, and it is imperative that support is given to the public and patients throughout the crisis, including for high-impact diseases such as colorectal cancer,” Luigi Ricciardiello, the lead study author and a professor at the University of Bologna in Italy, said in a statement.
Ricciardiello and colleagues presented their research on Monday at UEG Week Virtual 2020, an international conference for gastroenterologists. The study will be published in the UEG Journal .
The researchers created a model to forecast the effects of delayed cancer screening during 2020. A “moderate” delay of 7-12 months caused a 3% increase in advanced-stage colon cancer, and a long delay of more than 12 months caused a 7% increase in advanced cancer.
Based on a survival rate of 5 years for stage 3 or stage 4 colorectal cancer, the death rate would increase nearly 12% when screening is delayed for more than a year, as compared with less than three months of delay.
The research team found similar results when forecasting advanced-stage cancer and deaths earlier this year. In a paper published in Clinical Gastroenterology and Hepatology in early September, they projected that deaths could increase 12% if screening is delayed for more than a year.
Throughout the pandemic, screening programs have been delayed in many countries, particularly across Europe.
“Healthcare authorities need to act urgently on how they reorganise activities during COVID-19, without compromising the diagnosis of other high-impact diseases like this research shows,” Ricciardiello said.
United European Gastroenterology, a professional medical organization for digestive health specialists, has called for policymakers to implement colon cancer screening programs across the European Union. Annually, more than 375,000 new cases are diagnosed across the EU, and more than 170,000 people die from colorectal cancer, according to a UEG report.
“Early-stage diagnosis of colorectal cancer is crucial — it’s far easier to treat and enhances optimal patient outcomes,” Ricciardiello said. “It is therefore essential that vital diagnosis tools, like screening programmes, continue and help to prevent mortality rates from rising even further.”
This article first appeared on Medscape.com.
Delays in colorectal cancer screening due to the COVID-19 pandemic could lead to higher rates of advanced-stage cancer and death, according to a new study.
When compared with a delay of less than three months, the longer delay seen this year may result in an 11.9% increase in death rates.
“Across the globe, health care systems are facing serious difficulties while dealing with COVID-19, and it is imperative that support is given to the public and patients throughout the crisis, including for high-impact diseases such as colorectal cancer,” Luigi Ricciardiello, the lead study author and a professor at the University of Bologna in Italy, said in a statement.
Ricciardiello and colleagues presented their research on Monday at UEG Week Virtual 2020, an international conference for gastroenterologists. The study will be published in the UEG Journal .
The researchers created a model to forecast the effects of delayed cancer screening during 2020. A “moderate” delay of 7-12 months caused a 3% increase in advanced-stage colon cancer, and a long delay of more than 12 months caused a 7% increase in advanced cancer.
Based on a survival rate of 5 years for stage 3 or stage 4 colorectal cancer, the death rate would increase nearly 12% when screening is delayed for more than a year, as compared with less than three months of delay.
The research team found similar results when forecasting advanced-stage cancer and deaths earlier this year. In a paper published in Clinical Gastroenterology and Hepatology in early September, they projected that deaths could increase 12% if screening is delayed for more than a year.
Throughout the pandemic, screening programs have been delayed in many countries, particularly across Europe.
“Healthcare authorities need to act urgently on how they reorganise activities during COVID-19, without compromising the diagnosis of other high-impact diseases like this research shows,” Ricciardiello said.
United European Gastroenterology, a professional medical organization for digestive health specialists, has called for policymakers to implement colon cancer screening programs across the European Union. Annually, more than 375,000 new cases are diagnosed across the EU, and more than 170,000 people die from colorectal cancer, according to a UEG report.
“Early-stage diagnosis of colorectal cancer is crucial — it’s far easier to treat and enhances optimal patient outcomes,” Ricciardiello said. “It is therefore essential that vital diagnosis tools, like screening programmes, continue and help to prevent mortality rates from rising even further.”
This article first appeared on Medscape.com.
CRC risk: Raised by meat/alcohol, lowered by aspirin/NSAIDs
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AGA Clinical Practice Update: Young adult–onset colorectal cancer diagnosis and management
The rising incidence of colorectal cancer in adults younger than 50 years heightens the need to evaluate the colon and rectum of any patient, regardless of age, who presents with symptoms such as rectal bleeding, weight loss, abdominal pain, iron-deficiency anemia, or changes in bowel habits, according to a new American Gastroenterological Association clinical practice update.
In addition to receiving cancer staging or being referred to an oncologist, newly diagnosed patients should be counseled about both germline genetic testing and fertility preservation, wrote Lisa A. Boardman, MD, of Mayo Clinic in Rochester, Minn., with associates in Clinical Gastroenterology and Hepatology. “Clinicians should present the role of fertility preservation prior to [administering] cancer-directed therapy, including surgery, pelvic radiation, or chemotherapy.”
It remains unclear why the incidence of young adult–onset colorectal cancer is rising, but the trend is not limited to the United States. Implicated risk factors include inflammatory bowel disease, prior irradiation, harboring a pathogenic germline mutation for a known hereditary cancer syndrome, and having a first- or second-degree relative with colorectal cancer. Indeed, the odds of developing young adult–onset disease are nearly 4 times higher if a parent has colorectal cancer and nearly 12 times higher if a sibling is affected.
For newly diagnosed young adults, it is important to collect a family cancer history but vital, regardless of history, to discuss targeted or multiplex germline mutation testing. Detecting hereditary colorectal cancer syndromes is crucial because their nature informs surgical options for treatment. “Roughly one in five young adult–onset colorectal cancers will be caused by a germline mutation, and among those with a detectable hereditary condition, half of those patients with young adult–onset colorectal cancer will have Lynch syndrome,” the experts noted. For these patients (who have mutations involving MSH2, EPCAM, MLH1, MSH6, and PMS2), ileorectostomy (IRA) for colorectal cancer should be considered.
For patients with the classic subtype of familial adenomatous polyposis, ileal pouch anal anastomosis is recommended after the polyp burden can no longer be managed endoscopically, although initial IRA with subsequent conversion to IPAA is an option for women of child-bearing age, according to the clinical practice update. Patients with the attenuated subtype of familial adenomatous polyposis should consider IRA or colectomy if colorectal cancer develops or if the polyp burden exceeds endoscopic control. In contrast, colectomy is the only type of surgery recommended for patients with serrated polyposis syndrome requiring surgical treatment.
Finally, clinicians should offer only screening for hereditary cancer syndromes if young adults cancer have been diagnosed with a hereditary colorectal cancer syndrome. “For patients with sporadic young adult–onset colorectal cancer, extracolonic screening and colorectal cancer surveillance intervals are the same as for patients with older adult–onset colorectal cancer,” the experts wrote. For young patients without an apparent underlying genetic syndrome, molecular studies may eventually help tailor treatment options, “but at this point, more extensive surgery or more aggressive chemotherapy cannot be recommended. As cancer treatments evolve to use patient tumor specific therapeutics, our management of patients with young adult–onset colorectal cancer will improve.”
Dr. Boardman and associates reported having no relevant conflicts of interest.
SOURCE: Boardman LA et al. Clin Gastroenterol Hepatol. 2020 Jun 7. doi: 10.1016/j.cgh.2020.05.058.
The rising incidence of colorectal cancer in adults younger than 50 years heightens the need to evaluate the colon and rectum of any patient, regardless of age, who presents with symptoms such as rectal bleeding, weight loss, abdominal pain, iron-deficiency anemia, or changes in bowel habits, according to a new American Gastroenterological Association clinical practice update.
In addition to receiving cancer staging or being referred to an oncologist, newly diagnosed patients should be counseled about both germline genetic testing and fertility preservation, wrote Lisa A. Boardman, MD, of Mayo Clinic in Rochester, Minn., with associates in Clinical Gastroenterology and Hepatology. “Clinicians should present the role of fertility preservation prior to [administering] cancer-directed therapy, including surgery, pelvic radiation, or chemotherapy.”
It remains unclear why the incidence of young adult–onset colorectal cancer is rising, but the trend is not limited to the United States. Implicated risk factors include inflammatory bowel disease, prior irradiation, harboring a pathogenic germline mutation for a known hereditary cancer syndrome, and having a first- or second-degree relative with colorectal cancer. Indeed, the odds of developing young adult–onset disease are nearly 4 times higher if a parent has colorectal cancer and nearly 12 times higher if a sibling is affected.
For newly diagnosed young adults, it is important to collect a family cancer history but vital, regardless of history, to discuss targeted or multiplex germline mutation testing. Detecting hereditary colorectal cancer syndromes is crucial because their nature informs surgical options for treatment. “Roughly one in five young adult–onset colorectal cancers will be caused by a germline mutation, and among those with a detectable hereditary condition, half of those patients with young adult–onset colorectal cancer will have Lynch syndrome,” the experts noted. For these patients (who have mutations involving MSH2, EPCAM, MLH1, MSH6, and PMS2), ileorectostomy (IRA) for colorectal cancer should be considered.
For patients with the classic subtype of familial adenomatous polyposis, ileal pouch anal anastomosis is recommended after the polyp burden can no longer be managed endoscopically, although initial IRA with subsequent conversion to IPAA is an option for women of child-bearing age, according to the clinical practice update. Patients with the attenuated subtype of familial adenomatous polyposis should consider IRA or colectomy if colorectal cancer develops or if the polyp burden exceeds endoscopic control. In contrast, colectomy is the only type of surgery recommended for patients with serrated polyposis syndrome requiring surgical treatment.
Finally, clinicians should offer only screening for hereditary cancer syndromes if young adults cancer have been diagnosed with a hereditary colorectal cancer syndrome. “For patients with sporadic young adult–onset colorectal cancer, extracolonic screening and colorectal cancer surveillance intervals are the same as for patients with older adult–onset colorectal cancer,” the experts wrote. For young patients without an apparent underlying genetic syndrome, molecular studies may eventually help tailor treatment options, “but at this point, more extensive surgery or more aggressive chemotherapy cannot be recommended. As cancer treatments evolve to use patient tumor specific therapeutics, our management of patients with young adult–onset colorectal cancer will improve.”
Dr. Boardman and associates reported having no relevant conflicts of interest.
SOURCE: Boardman LA et al. Clin Gastroenterol Hepatol. 2020 Jun 7. doi: 10.1016/j.cgh.2020.05.058.
The rising incidence of colorectal cancer in adults younger than 50 years heightens the need to evaluate the colon and rectum of any patient, regardless of age, who presents with symptoms such as rectal bleeding, weight loss, abdominal pain, iron-deficiency anemia, or changes in bowel habits, according to a new American Gastroenterological Association clinical practice update.
In addition to receiving cancer staging or being referred to an oncologist, newly diagnosed patients should be counseled about both germline genetic testing and fertility preservation, wrote Lisa A. Boardman, MD, of Mayo Clinic in Rochester, Minn., with associates in Clinical Gastroenterology and Hepatology. “Clinicians should present the role of fertility preservation prior to [administering] cancer-directed therapy, including surgery, pelvic radiation, or chemotherapy.”
It remains unclear why the incidence of young adult–onset colorectal cancer is rising, but the trend is not limited to the United States. Implicated risk factors include inflammatory bowel disease, prior irradiation, harboring a pathogenic germline mutation for a known hereditary cancer syndrome, and having a first- or second-degree relative with colorectal cancer. Indeed, the odds of developing young adult–onset disease are nearly 4 times higher if a parent has colorectal cancer and nearly 12 times higher if a sibling is affected.
For newly diagnosed young adults, it is important to collect a family cancer history but vital, regardless of history, to discuss targeted or multiplex germline mutation testing. Detecting hereditary colorectal cancer syndromes is crucial because their nature informs surgical options for treatment. “Roughly one in five young adult–onset colorectal cancers will be caused by a germline mutation, and among those with a detectable hereditary condition, half of those patients with young adult–onset colorectal cancer will have Lynch syndrome,” the experts noted. For these patients (who have mutations involving MSH2, EPCAM, MLH1, MSH6, and PMS2), ileorectostomy (IRA) for colorectal cancer should be considered.
For patients with the classic subtype of familial adenomatous polyposis, ileal pouch anal anastomosis is recommended after the polyp burden can no longer be managed endoscopically, although initial IRA with subsequent conversion to IPAA is an option for women of child-bearing age, according to the clinical practice update. Patients with the attenuated subtype of familial adenomatous polyposis should consider IRA or colectomy if colorectal cancer develops or if the polyp burden exceeds endoscopic control. In contrast, colectomy is the only type of surgery recommended for patients with serrated polyposis syndrome requiring surgical treatment.
Finally, clinicians should offer only screening for hereditary cancer syndromes if young adults cancer have been diagnosed with a hereditary colorectal cancer syndrome. “For patients with sporadic young adult–onset colorectal cancer, extracolonic screening and colorectal cancer surveillance intervals are the same as for patients with older adult–onset colorectal cancer,” the experts wrote. For young patients without an apparent underlying genetic syndrome, molecular studies may eventually help tailor treatment options, “but at this point, more extensive surgery or more aggressive chemotherapy cannot be recommended. As cancer treatments evolve to use patient tumor specific therapeutics, our management of patients with young adult–onset colorectal cancer will improve.”
Dr. Boardman and associates reported having no relevant conflicts of interest.
SOURCE: Boardman LA et al. Clin Gastroenterol Hepatol. 2020 Jun 7. doi: 10.1016/j.cgh.2020.05.058.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY




