User login
American College of Chest Physicians (ACCP): Annual International Scientific Assembly (CHEST 2013)
Imaging techniques target bronchial thermoplasty
CHICAGO – CHICAGO - Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It's off-label at this point, but I think this is where we're going with this therapy," Dr. Mario Castro, FCCP, said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro's colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have asignificantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Dr. Castro's team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT, to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they're asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I've done up to around 140-150 activations, just because they've had an extensive bronchial tree that I needed to treat." … If you have a nonresponder, even 5 years out, I wouldn't treat because I think smooth muscle is probably not their main problem."
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
Dr. Eric Gartman, FCCP, comments: Severe asthma patients are a heterogenous population, and any modality that augments our ability to discriminate the best treatment option for an individual patient is eagerly welcomed.
As this field of research matures, we may begin to tailor our therapies more effectively to those who will benefit most.
CHICAGO – CHICAGO - Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It's off-label at this point, but I think this is where we're going with this therapy," Dr. Mario Castro, FCCP, said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro's colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have asignificantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Dr. Castro's team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT, to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they're asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I've done up to around 140-150 activations, just because they've had an extensive bronchial tree that I needed to treat." … If you have a nonresponder, even 5 years out, I wouldn't treat because I think smooth muscle is probably not their main problem."
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
Dr. Eric Gartman, FCCP, comments: Severe asthma patients are a heterogenous population, and any modality that augments our ability to discriminate the best treatment option for an individual patient is eagerly welcomed.
As this field of research matures, we may begin to tailor our therapies more effectively to those who will benefit most.
CHICAGO – CHICAGO - Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It's off-label at this point, but I think this is where we're going with this therapy," Dr. Mario Castro, FCCP, said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro's colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have asignificantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Dr. Castro's team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT, to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they're asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I've done up to around 140-150 activations, just because they've had an extensive bronchial tree that I needed to treat." … If you have a nonresponder, even 5 years out, I wouldn't treat because I think smooth muscle is probably not their main problem."
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
Dr. Eric Gartman, FCCP, comments: Severe asthma patients are a heterogenous population, and any modality that augments our ability to discriminate the best treatment option for an individual patient is eagerly welcomed.
As this field of research matures, we may begin to tailor our therapies more effectively to those who will benefit most.
Emerging imaging techniques target bronchial thermoplasty
CHICAGO – Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It’s off-label at this point, but I think this is where we’re going with this therapy," Dr. Mario Castro said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI images allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro’s colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have a significantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Biopredictors of bronchial thermoplasty response are also being evaluated in a prospective study of patients with severe refractory asthma, led by Dr. Castro, currently recruiting approximately 190 patients at five U.S. sites (NCT01185275).
Dr. Castro’s team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they’re asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I’ve done up to around 140-150 activations, just because they’ve had an extensive bronchial tree that I needed to treat. ... If you have a nonresponder, even 5 years out, I wouldn’t treat because I think smooth muscle is probably not their main problem," he added.
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
CHICAGO – Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It’s off-label at this point, but I think this is where we’re going with this therapy," Dr. Mario Castro said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI images allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro’s colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have a significantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Biopredictors of bronchial thermoplasty response are also being evaluated in a prospective study of patients with severe refractory asthma, led by Dr. Castro, currently recruiting approximately 190 patients at five U.S. sites (NCT01185275).
Dr. Castro’s team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they’re asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I’ve done up to around 140-150 activations, just because they’ve had an extensive bronchial tree that I needed to treat. ... If you have a nonresponder, even 5 years out, I wouldn’t treat because I think smooth muscle is probably not their main problem," he added.
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
CHICAGO – Advanced imaging techniques may play an increasing role in targeting the delivery of bronchial thermoplasty in severe, uncontrolled asthma.
"It’s off-label at this point, but I think this is where we’re going with this therapy," Dr. Mario Castro said at the annual meeting of the American College of Chest Physicians. "Perhaps we can do a better job to target this therapy, just like phenotyping our patients [for novel biologic agents]."
Reconstruction of the airway and parenchyma using diagnostic software during an inspiratory computed tomography (CT) scan allows clinicians to measure all of the lung airways in a systematic way, said Dr. Castro, director of the asthma and airway translational research unit, Washington University School of Medicine, St. Louis.
In the case of a 50-year-old patient with severe persistent asthma, the technique revealed a clearly remodeled airway with a 63% average wall area, but also areas of great heterogeneity in all segmental airways. "What we find is that some airways are remodeled more than others," Dr. Castro said.
The university also now images its patients by combining inhaled hyperpolarized helium gas with magnetic resonance imaging from the apex all the way to the base of the lung. A color algorithm CT mask imposed on the MRI images allows the team to quantify ventilation defects before and after bronchial thermoplasty.
Earlier this year, Dr. Castro’s colleague, Dr. Ajay Sheshadri, reported that patients with severe asthma have a significantly higher baseline ventilation defect percentage (VDP) than healthy subjects (mean 24.4% vs. 3.5%; P = .003). VDP improved by about 7% overall after bronchial thermoplasty (P = .10), with some patients having a marked improvement in VDP, while others did not, Dr. Castro said.
Baseline characteristics were analyzed in an effort to identify responders, and "we were very surprised to find that sputum eosinophilia was the one that trended best in predicting a change in ventilation defect score," he added.
Biopredictors of bronchial thermoplasty response are also being evaluated in a prospective study of patients with severe refractory asthma, led by Dr. Castro, currently recruiting approximately 190 patients at five U.S. sites (NCT01185275).
Dr. Castro’s team is also using xenon gas instead of helium with MRI, because it is more readily available and less expensive. Other groups are using confocal CT to evaluate airways for bronchial thermoplasty, he noted.
Dr. Castro stressed that 13 years of cumulative experience have shown that bronchial thermoplasty is safe and effective, but that careful initial evaluation of candidates remains essential. The American Thoracic Society and European Respiratory Society are expected to release new guidelines early next year for the initial evaluation of all severe asthmatics that recommend six tests, including blood work, spirometry, immunoglobulin E assessment with skin prick tests or an immunoabsorbent assay, and multidetector CT to evaluate for other conditions mimicking asthma.
"With this basic evaluation in our center, we find about one out of every three patients are really not pure asthma; they’re asthma mixed with significant bronchiectasis or no asthma at all, or they have underlying emphysema from prior smoke exposure," said Dr. Castro. "So it is very important that we take a step back with these patients and look."
During a discussion following the presentation, Dr. Castro said he would use bronchial thermoplasty to treat patients with incomplete reversibility of airflow obstruction, but does not advocate repeat treatments because of the potential for additional injury.
"What we do advocate is that we extensively treat all the airways that we can access, and that you treat with continuous therapies," he said. "The average activations in the lower, lower [airway] is around 60, but in some cases I’ve done up to around 140-150 activations, just because they’ve had an extensive bronchial tree that I needed to treat. ... If you have a nonresponder, even 5 years out, I wouldn’t treat because I think smooth muscle is probably not their main problem," he added.
Dr. Castro reported research support, lecturing, and consulting for numerous firms including Boston Scientific, maker of the Alair bronchial thermoplasty system.
AT CHEST 2013
Riociguat benefits persist in pulmonary hypertension
CHICAGO – Patients with chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension maintained benefits with riociguat at 1 year in two long-term extension studies.
Riociguat (Adempas) is the first drug approved for chronic thromboembolic pulmonary hypertension (CTEPH) and the first to show sustained benefits in 6-minute walk distance and functional class in this setting, Dr. Gérald Simonneau said in a late-breaking session at the annual meeting of the American College of Chest Physicians.
The oral soluble guanylate cyclase stimulator was approved in the United States in October 2013 to treat CTEPH and pulmonary arterial hypertension (PAH) based on the phase III CHEST-1 and PATENT-1 studies.
CHEST-1 randomized 261 patients with inoperable CTEPH or persistent pulmonary hypertension after endarterectomy to placebo or riociguat up to 2.5 mg three times daily for 16 weeks.
In all, 237 patients entered CHEST-2, and were either maintained on their optimum riociguat dose, up to 2.5 mg three times daily, or switched to riociguat titrated up to 2.5 mg three times daily. Only 8% of patients required additional PAH drugs at 1 year.
Patients maintained on riociguat gained only 15 m on the 6-minute walk test at 1 year, but added 66 m overall from baseline, said Dr. Simonneau, head of pneumology and intensive care medicine at Hôpital Kremlin Bicêtre, University of Paris-Sud, Le Kremlin-Bicêtre, France.
Patients switching from placebo to riociguat gained 37 m in the walk test at 1 year, but only 45 m from baseline.
WHO functional class improved in about 15% of patients in the riociguat maintenance arm and about 30% of those switched from placebo, he reported.
Freedom from clinical worsening at years 1 and 2 were 88% and 80%, with estimated overall survival rates of 97% and 94%.
During a discussion of the results, Dr. Simonneau observed that the 2-year overall survival rate for CTEPH patients is approximately 92% for patients treated surgically, but only about 70% for those receiving traditional medical therapy.
Adverse events
One fatal pulmonary hemorrhage occurred during CHEST-2, but it was not considered related to the study drug, said Dr. Simonneau, who noted that riociguat's label includes a warning about the risk of pulmonary bleeding events.
Two fatal pulmonary hemorrhages occurred in PATENT-2, and one was related to riociguat, Dr. Lewis Rubin reported during the same session. A third serious pulmonary hemorrhage occurred that was considered related to riociguat, but it resolved.
Hemoptysis was another serious adverse event (SAE) of "interest and concern" in both pulmonary arterial hypertension and CTEPH patients, said Dr. Rubin of the University of California, San Diego. Two patients (1%) had serious hemoptysis in PATENT-1, with seven additional events occurring in the extension phase (2%). All but one case resolved, five were moderate, and no cases were considered related to the study drug, although this could not be entirely excluded.
"The outcome of pulmonary bleeding-related SAEs was, in general, resolved in most cases, and there does not appear to be an association between dose of riociguat used and the occurrence of hemoptysis," said Dr. Rubin. However, "we need some further clarification on the mechanism responsible," he added.
Six serious hemoptysis events occurred in the two CHEST studies (three each), and one patient required bronchial artery embolization. All patients were receiving anticoagulants and none of these events was considered related to the study drug, Dr. Simonneau said.
Overall, 100 (42%) patients in CHEST-2 had a serious AE, and 12 were considered related to riociguat. SAEs were reported in 204 patients (52%) in PATENT-2, with 7% considered study drug related. Syncope was the most common adverse event (2%).
PATENT study
PATENT-1 randomized 443 patients with PAH to placebo or riociguat titrated to 1.5 mg or 2.5 mg three times daily. In all, 98% of patients (434) entered PATENT-2 and received riociguat titrated up to 2.5 mg three times daily. Notably, 54% of patients were on additional PAH medications at 1 year (97% of those pretreated with riociguat and 11% of controls).
Six-minute walk distances increased from a mean of 400 m at the close of PATENT-1 to 417 m in patients initially given the maximum dose of riociguat, for a gain of 17 m; from 406 to 417 m in those initially capped at riociguat 1.5 mg; and from 390 to 426 m in the former placebo group, Dr. Rubin said.
WHO functional class improved by approximately 10% in all three arms.
Freedom from clinical worsening at 1 and 2 years was 88% and 77%, with overall survival estimated at 97% and 93%, he said.
CHEST-2 and PATENT-2 are supported by Bayer Healthcare, maker of riociguat. Dr. Simonneau and Dr. Lewis reported financial relationships with several drug companies including Bayer.
CHICAGO – Patients with chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension maintained benefits with riociguat at 1 year in two long-term extension studies.
Riociguat (Adempas) is the first drug approved for chronic thromboembolic pulmonary hypertension (CTEPH) and the first to show sustained benefits in 6-minute walk distance and functional class in this setting, Dr. Gérald Simonneau said in a late-breaking session at the annual meeting of the American College of Chest Physicians.
The oral soluble guanylate cyclase stimulator was approved in the United States in October 2013 to treat CTEPH and pulmonary arterial hypertension (PAH) based on the phase III CHEST-1 and PATENT-1 studies.
CHEST-1 randomized 261 patients with inoperable CTEPH or persistent pulmonary hypertension after endarterectomy to placebo or riociguat up to 2.5 mg three times daily for 16 weeks.
In all, 237 patients entered CHEST-2, and were either maintained on their optimum riociguat dose, up to 2.5 mg three times daily, or switched to riociguat titrated up to 2.5 mg three times daily. Only 8% of patients required additional PAH drugs at 1 year.
Patients maintained on riociguat gained only 15 m on the 6-minute walk test at 1 year, but added 66 m overall from baseline, said Dr. Simonneau, head of pneumology and intensive care medicine at Hôpital Kremlin Bicêtre, University of Paris-Sud, Le Kremlin-Bicêtre, France.
Patients switching from placebo to riociguat gained 37 m in the walk test at 1 year, but only 45 m from baseline.
WHO functional class improved in about 15% of patients in the riociguat maintenance arm and about 30% of those switched from placebo, he reported.
Freedom from clinical worsening at years 1 and 2 were 88% and 80%, with estimated overall survival rates of 97% and 94%.
During a discussion of the results, Dr. Simonneau observed that the 2-year overall survival rate for CTEPH patients is approximately 92% for patients treated surgically, but only about 70% for those receiving traditional medical therapy.
Adverse events
One fatal pulmonary hemorrhage occurred during CHEST-2, but it was not considered related to the study drug, said Dr. Simonneau, who noted that riociguat's label includes a warning about the risk of pulmonary bleeding events.
Two fatal pulmonary hemorrhages occurred in PATENT-2, and one was related to riociguat, Dr. Lewis Rubin reported during the same session. A third serious pulmonary hemorrhage occurred that was considered related to riociguat, but it resolved.
Hemoptysis was another serious adverse event (SAE) of "interest and concern" in both pulmonary arterial hypertension and CTEPH patients, said Dr. Rubin of the University of California, San Diego. Two patients (1%) had serious hemoptysis in PATENT-1, with seven additional events occurring in the extension phase (2%). All but one case resolved, five were moderate, and no cases were considered related to the study drug, although this could not be entirely excluded.
"The outcome of pulmonary bleeding-related SAEs was, in general, resolved in most cases, and there does not appear to be an association between dose of riociguat used and the occurrence of hemoptysis," said Dr. Rubin. However, "we need some further clarification on the mechanism responsible," he added.
Six serious hemoptysis events occurred in the two CHEST studies (three each), and one patient required bronchial artery embolization. All patients were receiving anticoagulants and none of these events was considered related to the study drug, Dr. Simonneau said.
Overall, 100 (42%) patients in CHEST-2 had a serious AE, and 12 were considered related to riociguat. SAEs were reported in 204 patients (52%) in PATENT-2, with 7% considered study drug related. Syncope was the most common adverse event (2%).
PATENT study
PATENT-1 randomized 443 patients with PAH to placebo or riociguat titrated to 1.5 mg or 2.5 mg three times daily. In all, 98% of patients (434) entered PATENT-2 and received riociguat titrated up to 2.5 mg three times daily. Notably, 54% of patients were on additional PAH medications at 1 year (97% of those pretreated with riociguat and 11% of controls).
Six-minute walk distances increased from a mean of 400 m at the close of PATENT-1 to 417 m in patients initially given the maximum dose of riociguat, for a gain of 17 m; from 406 to 417 m in those initially capped at riociguat 1.5 mg; and from 390 to 426 m in the former placebo group, Dr. Rubin said.
WHO functional class improved by approximately 10% in all three arms.
Freedom from clinical worsening at 1 and 2 years was 88% and 77%, with overall survival estimated at 97% and 93%, he said.
CHEST-2 and PATENT-2 are supported by Bayer Healthcare, maker of riociguat. Dr. Simonneau and Dr. Lewis reported financial relationships with several drug companies including Bayer.
CHICAGO – Patients with chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension maintained benefits with riociguat at 1 year in two long-term extension studies.
Riociguat (Adempas) is the first drug approved for chronic thromboembolic pulmonary hypertension (CTEPH) and the first to show sustained benefits in 6-minute walk distance and functional class in this setting, Dr. Gérald Simonneau said in a late-breaking session at the annual meeting of the American College of Chest Physicians.
The oral soluble guanylate cyclase stimulator was approved in the United States in October 2013 to treat CTEPH and pulmonary arterial hypertension (PAH) based on the phase III CHEST-1 and PATENT-1 studies.
CHEST-1 randomized 261 patients with inoperable CTEPH or persistent pulmonary hypertension after endarterectomy to placebo or riociguat up to 2.5 mg three times daily for 16 weeks.
In all, 237 patients entered CHEST-2, and were either maintained on their optimum riociguat dose, up to 2.5 mg three times daily, or switched to riociguat titrated up to 2.5 mg three times daily. Only 8% of patients required additional PAH drugs at 1 year.
Patients maintained on riociguat gained only 15 m on the 6-minute walk test at 1 year, but added 66 m overall from baseline, said Dr. Simonneau, head of pneumology and intensive care medicine at Hôpital Kremlin Bicêtre, University of Paris-Sud, Le Kremlin-Bicêtre, France.
Patients switching from placebo to riociguat gained 37 m in the walk test at 1 year, but only 45 m from baseline.
WHO functional class improved in about 15% of patients in the riociguat maintenance arm and about 30% of those switched from placebo, he reported.
Freedom from clinical worsening at years 1 and 2 were 88% and 80%, with estimated overall survival rates of 97% and 94%.
During a discussion of the results, Dr. Simonneau observed that the 2-year overall survival rate for CTEPH patients is approximately 92% for patients treated surgically, but only about 70% for those receiving traditional medical therapy.
Adverse events
One fatal pulmonary hemorrhage occurred during CHEST-2, but it was not considered related to the study drug, said Dr. Simonneau, who noted that riociguat's label includes a warning about the risk of pulmonary bleeding events.
Two fatal pulmonary hemorrhages occurred in PATENT-2, and one was related to riociguat, Dr. Lewis Rubin reported during the same session. A third serious pulmonary hemorrhage occurred that was considered related to riociguat, but it resolved.
Hemoptysis was another serious adverse event (SAE) of "interest and concern" in both pulmonary arterial hypertension and CTEPH patients, said Dr. Rubin of the University of California, San Diego. Two patients (1%) had serious hemoptysis in PATENT-1, with seven additional events occurring in the extension phase (2%). All but one case resolved, five were moderate, and no cases were considered related to the study drug, although this could not be entirely excluded.
"The outcome of pulmonary bleeding-related SAEs was, in general, resolved in most cases, and there does not appear to be an association between dose of riociguat used and the occurrence of hemoptysis," said Dr. Rubin. However, "we need some further clarification on the mechanism responsible," he added.
Six serious hemoptysis events occurred in the two CHEST studies (three each), and one patient required bronchial artery embolization. All patients were receiving anticoagulants and none of these events was considered related to the study drug, Dr. Simonneau said.
Overall, 100 (42%) patients in CHEST-2 had a serious AE, and 12 were considered related to riociguat. SAEs were reported in 204 patients (52%) in PATENT-2, with 7% considered study drug related. Syncope was the most common adverse event (2%).
PATENT study
PATENT-1 randomized 443 patients with PAH to placebo or riociguat titrated to 1.5 mg or 2.5 mg three times daily. In all, 98% of patients (434) entered PATENT-2 and received riociguat titrated up to 2.5 mg three times daily. Notably, 54% of patients were on additional PAH medications at 1 year (97% of those pretreated with riociguat and 11% of controls).
Six-minute walk distances increased from a mean of 400 m at the close of PATENT-1 to 417 m in patients initially given the maximum dose of riociguat, for a gain of 17 m; from 406 to 417 m in those initially capped at riociguat 1.5 mg; and from 390 to 426 m in the former placebo group, Dr. Rubin said.
WHO functional class improved by approximately 10% in all three arms.
Freedom from clinical worsening at 1 and 2 years was 88% and 77%, with overall survival estimated at 97% and 93%, he said.
CHEST-2 and PATENT-2 are supported by Bayer Healthcare, maker of riociguat. Dr. Simonneau and Dr. Lewis reported financial relationships with several drug companies including Bayer.
AT CHEST 2013
Major finding: Patients on continuous riociguat gained an average of 15 m on the 6-minute timed walk test after 1 year in CHEST-2 and 17 m in PATENT-2.
Data source: Prospective extension studies in 237 patients with chronic thromboembolic pulmonary hypertension and 434 patients with pulmonary arterial hypertension.
Disclosures: CHEST-2 and PATENT-2 are supported by Bayer Healthcare, maker of riociguat. Dr. Simonneau and Dr. Lewis reported financial relationships with several drug companies, including Bayer.
LABA/LAMA combo beneficial in moderate, severe COPD
CHICAGO – A fixed-dose combination of aclidinium bromide and formoterol fumarate improved lung function better than either drug alone without increasing toxicity in patients with moderate to severe chronic obstructive pulmonary disease in the phase III AUGMENT trial.
Aclidinium bromide (Tudorza Pressair) 400 mcg twice daily is a long-acting muscarinic antagonist (LAMA) approved in 2012 for the long-term maintenance treatment of COPD-associated bronchospasm. Formoterol fumarate (Foradil Aerolizer), a long-acting beta2-agonist (LABA), is also used in COPD to control symptoms and prevent wheezing.
Several fixed-dose LABA/LAMA combinations are in development, but none have been approved in COPD.
Combining two agents with different mechanisms of action is often recommended for improved bronchodilation, patient compliance, and cost-effectiveness in patients with COPD, Dr. Anthony D’Urzo said during a late-breaking abstract session at the annual meeting of the American College of Chest Physicians.
AUGMENT investigators (Chest 2013;144[4 MeetingAbstracts]:1025A) evenly randomized 1,692 patients with moderate to severe COPD to one of five twice-daily, metered-dose inhaler treatments: aclidinium 400 mcg plus formoterol 6 mcg or 12 mcg, aclidinium 400 mcg monotherapy, formoterol 12 mcg monotherapy, or placebo. Mean prebronchodilator forced expiratory volume in 1 second (FEV1) was 1.36 mL, and the mean age of the patients was 64 years. About half of the patients were current smokers, an intentional choice to reflect daily clinical practice, he said.
At week 24, the low- and high-dose formoterol combinations significantly increased FEV1 1 hour after morning dosing by 87 mL and 108 mL, respectively, compared with aclidinium alone (both P < .0001), said Dr. D’Urzo, director of the Primary Care Lung Clinic, University of Toronto.
Specifically, peak FEV1 increased by 176 mL with aclidinium alone, 201 mL with formoterol alone, 263 mL with the low-dose combination, and 284 mL with the high-dose combination, and decreased by 37 mL with placebo.
The low- and high-dose formoterol combinations also increased the coprimary endpoint of morning predose (trough) FEV1 at week 24 by 45 mL and 26 mL, respectively, compared with formoterol alone, but the increase was significant only for the higher-dose combination (P = .010), he said.
Specifically, trough FEV1 increased by 102 mL with aclidinium alone, 85 mL with formoterol alone, 111 mL with the low-dose combination, and 130 mL with the high-dose combination, and decreased by 35 mL with placebo.
Session comoderator Dr. Andrew Berman, division director of pulmonary and critical care medicine at Rutgers New Jersey Medical School in Newark, said targeting two different receptors clearly increases the degree of bronchodilation, but he questioned what the combined mechanism of action is and whether there’s perhaps a negative effect when combining two drugs since most clinicians would agree there’s only so much the airways can dilate.
Dr. D’Urzo said the combined mechanism is uncertain, but that there is evidence which suggests that beta2-agonists may augment the bronchial smooth muscle relaxation that is directly induced by muscarinic antagonists via a mechanism that decreases the release of acetylcholine via a modulation of cholinergic neurotransmission.
Adverse events leading to treatment discontinuation were similar across treatment arms, as were serious adverse events reported in 5.7% of patients on the high-dose combination, 5.4% on the low-dose combination, 5% on aclidinium alone, 4.5% on formoterol alone, and 3.6% on placebo. Three deaths occurred in the aclidinium monotherapy arm and one each in the high-dose formoterol combination and formoterol monotherapy arms, but none were thought related to treatment, he said.
Positive results have been reported from a second clinical trial, but codevelopers Forest Laboratories and Almirall announced in August that the New Drug Application submission planned for late 2013 was being delayed in order to resolve concerns raised by the Food and Drug Administration related to "chemistry, manufacturing, and control specifications associated with the combination formula." Forest is preparing a "robust package to address the FDA’s concerns" and is hoping to meet with its officials in early 2014, Forest R&D president Marco Taglietti said during an October earnings conference call.
Dr. D’Urzo reported having financial ties with several drug firms, including study sponsor Forest Research Institute; two coauthors are Forest employees.
CHICAGO – A fixed-dose combination of aclidinium bromide and formoterol fumarate improved lung function better than either drug alone without increasing toxicity in patients with moderate to severe chronic obstructive pulmonary disease in the phase III AUGMENT trial.
Aclidinium bromide (Tudorza Pressair) 400 mcg twice daily is a long-acting muscarinic antagonist (LAMA) approved in 2012 for the long-term maintenance treatment of COPD-associated bronchospasm. Formoterol fumarate (Foradil Aerolizer), a long-acting beta2-agonist (LABA), is also used in COPD to control symptoms and prevent wheezing.
Several fixed-dose LABA/LAMA combinations are in development, but none have been approved in COPD.
Combining two agents with different mechanisms of action is often recommended for improved bronchodilation, patient compliance, and cost-effectiveness in patients with COPD, Dr. Anthony D’Urzo said during a late-breaking abstract session at the annual meeting of the American College of Chest Physicians.
AUGMENT investigators (Chest 2013;144[4 MeetingAbstracts]:1025A) evenly randomized 1,692 patients with moderate to severe COPD to one of five twice-daily, metered-dose inhaler treatments: aclidinium 400 mcg plus formoterol 6 mcg or 12 mcg, aclidinium 400 mcg monotherapy, formoterol 12 mcg monotherapy, or placebo. Mean prebronchodilator forced expiratory volume in 1 second (FEV1) was 1.36 mL, and the mean age of the patients was 64 years. About half of the patients were current smokers, an intentional choice to reflect daily clinical practice, he said.
At week 24, the low- and high-dose formoterol combinations significantly increased FEV1 1 hour after morning dosing by 87 mL and 108 mL, respectively, compared with aclidinium alone (both P < .0001), said Dr. D’Urzo, director of the Primary Care Lung Clinic, University of Toronto.
Specifically, peak FEV1 increased by 176 mL with aclidinium alone, 201 mL with formoterol alone, 263 mL with the low-dose combination, and 284 mL with the high-dose combination, and decreased by 37 mL with placebo.
The low- and high-dose formoterol combinations also increased the coprimary endpoint of morning predose (trough) FEV1 at week 24 by 45 mL and 26 mL, respectively, compared with formoterol alone, but the increase was significant only for the higher-dose combination (P = .010), he said.
Specifically, trough FEV1 increased by 102 mL with aclidinium alone, 85 mL with formoterol alone, 111 mL with the low-dose combination, and 130 mL with the high-dose combination, and decreased by 35 mL with placebo.
Session comoderator Dr. Andrew Berman, division director of pulmonary and critical care medicine at Rutgers New Jersey Medical School in Newark, said targeting two different receptors clearly increases the degree of bronchodilation, but he questioned what the combined mechanism of action is and whether there’s perhaps a negative effect when combining two drugs since most clinicians would agree there’s only so much the airways can dilate.
Dr. D’Urzo said the combined mechanism is uncertain, but that there is evidence which suggests that beta2-agonists may augment the bronchial smooth muscle relaxation that is directly induced by muscarinic antagonists via a mechanism that decreases the release of acetylcholine via a modulation of cholinergic neurotransmission.
Adverse events leading to treatment discontinuation were similar across treatment arms, as were serious adverse events reported in 5.7% of patients on the high-dose combination, 5.4% on the low-dose combination, 5% on aclidinium alone, 4.5% on formoterol alone, and 3.6% on placebo. Three deaths occurred in the aclidinium monotherapy arm and one each in the high-dose formoterol combination and formoterol monotherapy arms, but none were thought related to treatment, he said.
Positive results have been reported from a second clinical trial, but codevelopers Forest Laboratories and Almirall announced in August that the New Drug Application submission planned for late 2013 was being delayed in order to resolve concerns raised by the Food and Drug Administration related to "chemistry, manufacturing, and control specifications associated with the combination formula." Forest is preparing a "robust package to address the FDA’s concerns" and is hoping to meet with its officials in early 2014, Forest R&D president Marco Taglietti said during an October earnings conference call.
Dr. D’Urzo reported having financial ties with several drug firms, including study sponsor Forest Research Institute; two coauthors are Forest employees.
CHICAGO – A fixed-dose combination of aclidinium bromide and formoterol fumarate improved lung function better than either drug alone without increasing toxicity in patients with moderate to severe chronic obstructive pulmonary disease in the phase III AUGMENT trial.
Aclidinium bromide (Tudorza Pressair) 400 mcg twice daily is a long-acting muscarinic antagonist (LAMA) approved in 2012 for the long-term maintenance treatment of COPD-associated bronchospasm. Formoterol fumarate (Foradil Aerolizer), a long-acting beta2-agonist (LABA), is also used in COPD to control symptoms and prevent wheezing.
Several fixed-dose LABA/LAMA combinations are in development, but none have been approved in COPD.
Combining two agents with different mechanisms of action is often recommended for improved bronchodilation, patient compliance, and cost-effectiveness in patients with COPD, Dr. Anthony D’Urzo said during a late-breaking abstract session at the annual meeting of the American College of Chest Physicians.
AUGMENT investigators (Chest 2013;144[4 MeetingAbstracts]:1025A) evenly randomized 1,692 patients with moderate to severe COPD to one of five twice-daily, metered-dose inhaler treatments: aclidinium 400 mcg plus formoterol 6 mcg or 12 mcg, aclidinium 400 mcg monotherapy, formoterol 12 mcg monotherapy, or placebo. Mean prebronchodilator forced expiratory volume in 1 second (FEV1) was 1.36 mL, and the mean age of the patients was 64 years. About half of the patients were current smokers, an intentional choice to reflect daily clinical practice, he said.
At week 24, the low- and high-dose formoterol combinations significantly increased FEV1 1 hour after morning dosing by 87 mL and 108 mL, respectively, compared with aclidinium alone (both P < .0001), said Dr. D’Urzo, director of the Primary Care Lung Clinic, University of Toronto.
Specifically, peak FEV1 increased by 176 mL with aclidinium alone, 201 mL with formoterol alone, 263 mL with the low-dose combination, and 284 mL with the high-dose combination, and decreased by 37 mL with placebo.
The low- and high-dose formoterol combinations also increased the coprimary endpoint of morning predose (trough) FEV1 at week 24 by 45 mL and 26 mL, respectively, compared with formoterol alone, but the increase was significant only for the higher-dose combination (P = .010), he said.
Specifically, trough FEV1 increased by 102 mL with aclidinium alone, 85 mL with formoterol alone, 111 mL with the low-dose combination, and 130 mL with the high-dose combination, and decreased by 35 mL with placebo.
Session comoderator Dr. Andrew Berman, division director of pulmonary and critical care medicine at Rutgers New Jersey Medical School in Newark, said targeting two different receptors clearly increases the degree of bronchodilation, but he questioned what the combined mechanism of action is and whether there’s perhaps a negative effect when combining two drugs since most clinicians would agree there’s only so much the airways can dilate.
Dr. D’Urzo said the combined mechanism is uncertain, but that there is evidence which suggests that beta2-agonists may augment the bronchial smooth muscle relaxation that is directly induced by muscarinic antagonists via a mechanism that decreases the release of acetylcholine via a modulation of cholinergic neurotransmission.
Adverse events leading to treatment discontinuation were similar across treatment arms, as were serious adverse events reported in 5.7% of patients on the high-dose combination, 5.4% on the low-dose combination, 5% on aclidinium alone, 4.5% on formoterol alone, and 3.6% on placebo. Three deaths occurred in the aclidinium monotherapy arm and one each in the high-dose formoterol combination and formoterol monotherapy arms, but none were thought related to treatment, he said.
Positive results have been reported from a second clinical trial, but codevelopers Forest Laboratories and Almirall announced in August that the New Drug Application submission planned for late 2013 was being delayed in order to resolve concerns raised by the Food and Drug Administration related to "chemistry, manufacturing, and control specifications associated with the combination formula." Forest is preparing a "robust package to address the FDA’s concerns" and is hoping to meet with its officials in early 2014, Forest R&D president Marco Taglietti said during an October earnings conference call.
Dr. D’Urzo reported having financial ties with several drug firms, including study sponsor Forest Research Institute; two coauthors are Forest employees.
AT CHEST 2013
Major finding: Low- and high-dose formoterol combinations increased week-24 peak FEV1 by 87 mL and 108 mL, respectively, over aclidinium alone (P < .0001).
Data source: A prospective study of 1,692 patients with moderate to severe COPD.
Disclosures: Dr. D’Urzo reported having financial ties with several drug firms, including study sponsor Forest Research Institute; two coauthors are Forest employees.
Ready or not? Most ICUs not as prepared for disaster as they think
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
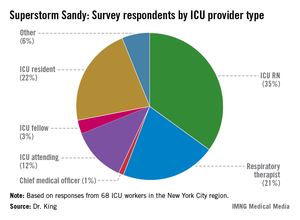
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Although 78% of ICU staff had never performed a vertical ICU evacuation drill, only 23% admitted to feeling "inadequately trained" during Superstorm Sandy evacuations.
Data source: Survey of 68 ICU workers in the New York City region, all of whom worked through Superstorm Sandy.
Disclosures: Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ready or not? Most ICUs not as prepared for disaster as they think
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
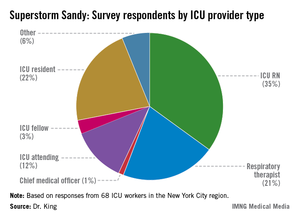
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
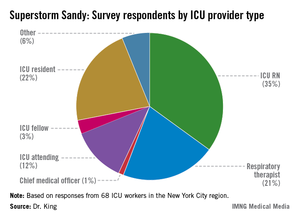
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
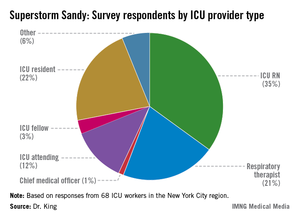
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Although 78% of ICU staff had never performed a vertical ICU evacuation drill, only 23% admitted to feeling "inadequately trained" during Superstorm Sandy evacuations.
Data source: Survey of 68 ICU workers in the New York City region, all of whom worked through Superstorm Sandy.
Disclosures: Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Electrocautery incision of lymph nodes improved biopsy yield
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Major finding: EBUS-guided lymph node biopsies made after electrocautery incision improved biopsy yields from 39% to 71% in 38 lymph nodes.
Data source: Prospective observational cohort study of 20 patients at a single tertiary academic medical center.
Disclosures: Dr. Bramley had no relevant disclosures.
Roflumilast holds up in real world, postapproval studies
CHICAGO – Patients with chronic obstructive pulmonary disease treated with roflumilast had fewer all-cause hospital readmissions and monthly COPD exacerbations than nonusers in two real world database analyses.
Among 1,400 patients, all-cause, 30-day hospital readmissions were 6.9% for those using once-daily oral roflumilast (Daliresp) and 11.1% for nonusers (P = .021).
COPD-related hospital readmissions were also lower with roflumilast, but these findings did not reach statistical significance (6.3% vs. 9.2%; P = .086), Dr. Alpesh N. Amin reported at the annual meeting of the American College of Chest Physicians.
He noted that Medicare recently fined 230 hospitals $227 million for high readmission rates.
"Heart failure, MI, and pneumonia are first on the list, but COPD is right behind that in terms of the penalty issues," said Dr. Amin, chair of the department of medicine and executive director of the hospitalist program at the University of California, Irvine.
Roflumilast, a selective phosphodiesterase-4 inhibitor, was approved in May 2011 to reduce the frequency of COPD exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations.
Dr. Amin's retrospective study used data from MarketScan, a large U.S. commercial health insurance claims database, and Medicare supplemental data to evaluate hospitalizations among 15,755 patients discharged for COPD between July 1, 2011, and Dec. 31, 2011. Patients had to have used roflumilast within 14 days after hospitalization or be discharged for COPD without roflumilast use during the entire study period.
After propensity score matching and logistic regression to control for confounding by indication and baseline characteristics, a matched cohort of 350 roflumilast and 1,050 nonroflumilast patients remained.
Conditional logistic regressions showed that roflumilast use is associated with a significantly lower likelihood of all-cause 30-day hospital readmission (odds ratio, 0.59), and a trend toward decreased COPD 30-day readmission (OR, 0.66; P = .089), Dr. Amin said.
All patients in the study were covered by large employer-sponsored private health insurance programs, so generalization of the results to the Medicare and Medicaid populations cannot be assumed, he noted. During the same session, a second database analysis showed that despite being sicker at baseline, adults treated with roflumilast along with other COPD medications had significantly fewer monthly exacerbations than those receiving at least three other COPD maintenance medications.
During the 12-month baseline period, roflumilast patients used significantly more COPD drugs than nonroflumilast patients (mean 3.2 vs. 2.6), were on those drugs significantly longer (mean, 187 days vs. 166 days), and had significantly more baseline ER visits (mean, 0.5 vs. 0.3), and hospitalizations (79% vs. 72%).
The benefit was mainly driven by a reduction in moderate exacerbations, said Dr. Andrew Shorr, a critical care pulmonologist at Washington (D.C.) Hospital Center.
In unadjusted models, rates of combined monthly moderate and severe exacerbations fell 11.1% in the roflumilast group and rose 15.9% among controls, a significant difference.
When looked at separately, the difference was statistically significant for moderate exacerbations (–11.8% vs. +20.7%; P = .001), but not for severe exacerbations requiring hospitalization (–8.8% vs. –5.3%), he said.
After the investigators adjusted for baseline characteristics in a difference-in-difference model, the reduction remained significant for monthly severe/moderate (–0.0160) and moderate exacerbations (–0.0149), but not for severe exacerbations (–0.0012; P = .63).
"We estimated that the magnitude of the effect, after adjusting for baseline imbalances and natural time trends, was about a 23% absolute reduction in monthly exacerbations for the roflumilast group over controls," Dr. Shorr said.
The analysis was based on medical and pharmacy claims in the IMS LifeLink PharMetrics Plus database from May 2010 to December 2012. Data were for 710 COPD patients receiving roflumilast plus other COPD medications and 13,501 patients receiving at least two COPD maintenance medications and prescribed a third maintenance drug during the study index period of May 2011 and September 2012. Patients with asthma or who were corticosteroid dependent were excluded.
Forest Research Institute sponsored the studies. Dr. Amin and Dr. Shorr reported research support and other remuneration from Forest. Some coauthors in each study are Forest employees.
CHICAGO – Patients with chronic obstructive pulmonary disease treated with roflumilast had fewer all-cause hospital readmissions and monthly COPD exacerbations than nonusers in two real world database analyses.
Among 1,400 patients, all-cause, 30-day hospital readmissions were 6.9% for those using once-daily oral roflumilast (Daliresp) and 11.1% for nonusers (P = .021).
COPD-related hospital readmissions were also lower with roflumilast, but these findings did not reach statistical significance (6.3% vs. 9.2%; P = .086), Dr. Alpesh N. Amin reported at the annual meeting of the American College of Chest Physicians.
He noted that Medicare recently fined 230 hospitals $227 million for high readmission rates.
"Heart failure, MI, and pneumonia are first on the list, but COPD is right behind that in terms of the penalty issues," said Dr. Amin, chair of the department of medicine and executive director of the hospitalist program at the University of California, Irvine.
Roflumilast, a selective phosphodiesterase-4 inhibitor, was approved in May 2011 to reduce the frequency of COPD exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations.
Dr. Amin's retrospective study used data from MarketScan, a large U.S. commercial health insurance claims database, and Medicare supplemental data to evaluate hospitalizations among 15,755 patients discharged for COPD between July 1, 2011, and Dec. 31, 2011. Patients had to have used roflumilast within 14 days after hospitalization or be discharged for COPD without roflumilast use during the entire study period.
After propensity score matching and logistic regression to control for confounding by indication and baseline characteristics, a matched cohort of 350 roflumilast and 1,050 nonroflumilast patients remained.
Conditional logistic regressions showed that roflumilast use is associated with a significantly lower likelihood of all-cause 30-day hospital readmission (odds ratio, 0.59), and a trend toward decreased COPD 30-day readmission (OR, 0.66; P = .089), Dr. Amin said.
All patients in the study were covered by large employer-sponsored private health insurance programs, so generalization of the results to the Medicare and Medicaid populations cannot be assumed, he noted. During the same session, a second database analysis showed that despite being sicker at baseline, adults treated with roflumilast along with other COPD medications had significantly fewer monthly exacerbations than those receiving at least three other COPD maintenance medications.
During the 12-month baseline period, roflumilast patients used significantly more COPD drugs than nonroflumilast patients (mean 3.2 vs. 2.6), were on those drugs significantly longer (mean, 187 days vs. 166 days), and had significantly more baseline ER visits (mean, 0.5 vs. 0.3), and hospitalizations (79% vs. 72%).
The benefit was mainly driven by a reduction in moderate exacerbations, said Dr. Andrew Shorr, a critical care pulmonologist at Washington (D.C.) Hospital Center.
In unadjusted models, rates of combined monthly moderate and severe exacerbations fell 11.1% in the roflumilast group and rose 15.9% among controls, a significant difference.
When looked at separately, the difference was statistically significant for moderate exacerbations (–11.8% vs. +20.7%; P = .001), but not for severe exacerbations requiring hospitalization (–8.8% vs. –5.3%), he said.
After the investigators adjusted for baseline characteristics in a difference-in-difference model, the reduction remained significant for monthly severe/moderate (–0.0160) and moderate exacerbations (–0.0149), but not for severe exacerbations (–0.0012; P = .63).
"We estimated that the magnitude of the effect, after adjusting for baseline imbalances and natural time trends, was about a 23% absolute reduction in monthly exacerbations for the roflumilast group over controls," Dr. Shorr said.
The analysis was based on medical and pharmacy claims in the IMS LifeLink PharMetrics Plus database from May 2010 to December 2012. Data were for 710 COPD patients receiving roflumilast plus other COPD medications and 13,501 patients receiving at least two COPD maintenance medications and prescribed a third maintenance drug during the study index period of May 2011 and September 2012. Patients with asthma or who were corticosteroid dependent were excluded.
Forest Research Institute sponsored the studies. Dr. Amin and Dr. Shorr reported research support and other remuneration from Forest. Some coauthors in each study are Forest employees.
CHICAGO – Patients with chronic obstructive pulmonary disease treated with roflumilast had fewer all-cause hospital readmissions and monthly COPD exacerbations than nonusers in two real world database analyses.
Among 1,400 patients, all-cause, 30-day hospital readmissions were 6.9% for those using once-daily oral roflumilast (Daliresp) and 11.1% for nonusers (P = .021).
COPD-related hospital readmissions were also lower with roflumilast, but these findings did not reach statistical significance (6.3% vs. 9.2%; P = .086), Dr. Alpesh N. Amin reported at the annual meeting of the American College of Chest Physicians.
He noted that Medicare recently fined 230 hospitals $227 million for high readmission rates.
"Heart failure, MI, and pneumonia are first on the list, but COPD is right behind that in terms of the penalty issues," said Dr. Amin, chair of the department of medicine and executive director of the hospitalist program at the University of California, Irvine.
Roflumilast, a selective phosphodiesterase-4 inhibitor, was approved in May 2011 to reduce the frequency of COPD exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations.
Dr. Amin's retrospective study used data from MarketScan, a large U.S. commercial health insurance claims database, and Medicare supplemental data to evaluate hospitalizations among 15,755 patients discharged for COPD between July 1, 2011, and Dec. 31, 2011. Patients had to have used roflumilast within 14 days after hospitalization or be discharged for COPD without roflumilast use during the entire study period.
After propensity score matching and logistic regression to control for confounding by indication and baseline characteristics, a matched cohort of 350 roflumilast and 1,050 nonroflumilast patients remained.
Conditional logistic regressions showed that roflumilast use is associated with a significantly lower likelihood of all-cause 30-day hospital readmission (odds ratio, 0.59), and a trend toward decreased COPD 30-day readmission (OR, 0.66; P = .089), Dr. Amin said.
All patients in the study were covered by large employer-sponsored private health insurance programs, so generalization of the results to the Medicare and Medicaid populations cannot be assumed, he noted. During the same session, a second database analysis showed that despite being sicker at baseline, adults treated with roflumilast along with other COPD medications had significantly fewer monthly exacerbations than those receiving at least three other COPD maintenance medications.
During the 12-month baseline period, roflumilast patients used significantly more COPD drugs than nonroflumilast patients (mean 3.2 vs. 2.6), were on those drugs significantly longer (mean, 187 days vs. 166 days), and had significantly more baseline ER visits (mean, 0.5 vs. 0.3), and hospitalizations (79% vs. 72%).
The benefit was mainly driven by a reduction in moderate exacerbations, said Dr. Andrew Shorr, a critical care pulmonologist at Washington (D.C.) Hospital Center.
In unadjusted models, rates of combined monthly moderate and severe exacerbations fell 11.1% in the roflumilast group and rose 15.9% among controls, a significant difference.
When looked at separately, the difference was statistically significant for moderate exacerbations (–11.8% vs. +20.7%; P = .001), but not for severe exacerbations requiring hospitalization (–8.8% vs. –5.3%), he said.
After the investigators adjusted for baseline characteristics in a difference-in-difference model, the reduction remained significant for monthly severe/moderate (–0.0160) and moderate exacerbations (–0.0149), but not for severe exacerbations (–0.0012; P = .63).
"We estimated that the magnitude of the effect, after adjusting for baseline imbalances and natural time trends, was about a 23% absolute reduction in monthly exacerbations for the roflumilast group over controls," Dr. Shorr said.
The analysis was based on medical and pharmacy claims in the IMS LifeLink PharMetrics Plus database from May 2010 to December 2012. Data were for 710 COPD patients receiving roflumilast plus other COPD medications and 13,501 patients receiving at least two COPD maintenance medications and prescribed a third maintenance drug during the study index period of May 2011 and September 2012. Patients with asthma or who were corticosteroid dependent were excluded.
Forest Research Institute sponsored the studies. Dr. Amin and Dr. Shorr reported research support and other remuneration from Forest. Some coauthors in each study are Forest employees.
AT CHEST 2013
Major finding: 30-day hospital readmissions were 6.9% for those using once-daily oral roflumilast vs. 11.1% for nonusers.
Data source: Two database analyses of COPD patients.
Disclosures: Forest Research Institute sponsored the studies. Dr. Amin and Dr. Shorr reported research support and other remuneration from Forest. Some coauthors in each study are Forest employees.
Embracing change is the only option in ACA era
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Private physicians may be unprepared for how drastically the ACA will change their practice.
Data source: Expert analysis from CHEST 2013
Disclosures: Dr. Kahn, Dr. Levine, Dr. Pak, and Dr. Diamond had no relevant disclosures.
Under ACA, practices risk tripping over antitrust regulations
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.
 |
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.
 |
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.
 |
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.
EXPERT ANALYSIS FROM CHEST 2013