User login
Gender Disparities for Academic Hospitalists
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
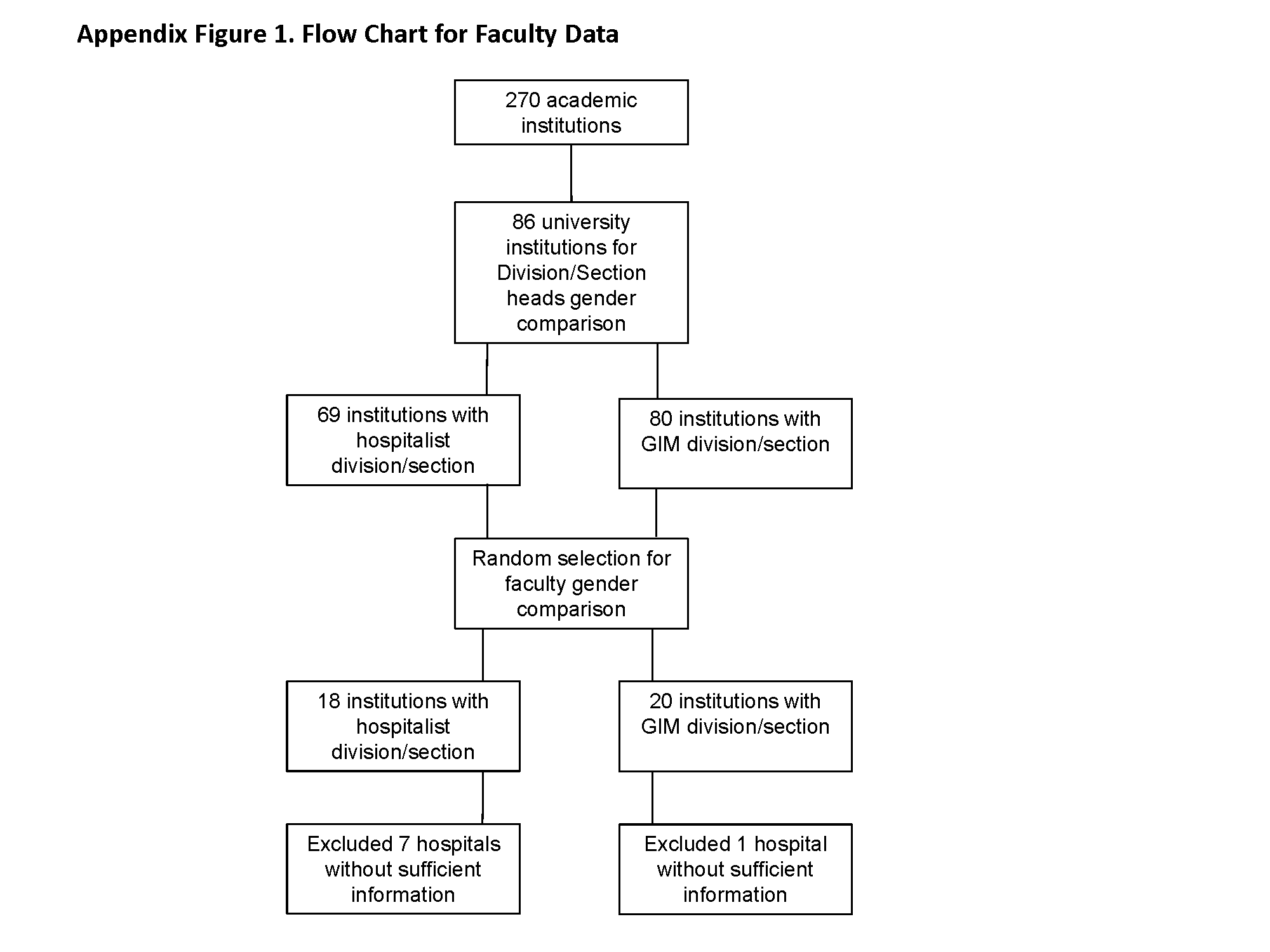
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
© 2015 Society of Hospital Medicine
Oral Proton Pump Inhibitors (PPIs) as Effective as IV PPIs in Peptic Ulcer Bleeding
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56–1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: Comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Visit our website for more information on the use of proton pump inhibitors.
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56–1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: Comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Visit our website for more information on the use of proton pump inhibitors.
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56–1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: Comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Visit our website for more information on the use of proton pump inhibitors.
Intravenous Haloperidol Does Not Prevent ICU Delirium
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Reviews of Research on Haloperidol and ICU Delirium, Proton Pump Inhibitors, Thrombolytics and Stroke
In This Edition
Literature At A Glance
A guide to this month’s studies
- Intravenous haloperidol does not prevent ICU delirium
- Predicting delirium risk in hospitalized adults
- Oral PPIs as effective as IV PPIs in peptic ulcer bleeding
- Probiotic benefit questioned in the elderly
- Colchicine and NSAID better than NSAID alone for acute pericarditis
- Improvement needed in patient understanding at hospital discharge
- Effectiveness of a multihospital effort to reduce rehospitalization
- Hospitals profit from preventing surgical site infections
- Prothrombin complex concentrate safer than fresh frozen plasma in rapidly reversing INR
- Hospital-acquired anemia associated with higher mortality, increased LOS
- Thrombolytics and stroke: the faster the better
Intravenous Haloperidol Does Not Prevent ICU Delirium
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Predicting Delirium Risk in Hospitalized Adults
Clinical question: Can a simple tool be developed and used for predicting delirium in hospitalized adults?
Background: Delirium is a common condition that results in higher mortality, longer length of stays, and higher probability of discharge to nursing home. Current delirium prediction tools are complicated, or restricted to surgical or critically ill patients.
Study design: Prospective cohort study, with separate derivation and validation cohorts.
Setting: Two academic hospitals and a VA hospital in San Francisco.
Synopsis: Investigators enrolled 374 hospitalized patients who were more than 50 years of age and not delirious at time of admission (209 patients in the derivation and 165 in the validation). The authors identified four predictors of delirium: Age >80; failure to spell “World” backwards; disOrientation to place; and higher nurse-rated iLlness severity (AWOL). The authors found that rates of delirium increased with increasing number of predictors (with zero predictors, 2% developed delirium; one predictor, 4%; two predictors, 14%; three predictors, 20%; four predictors, 64%).
These predictors are similar to other previously identified risk factors, as well as to prediction tools that are in use for surgical patients. However, this tool is quick and can be completed by nursing staff, so it may have a role to play in helping triage patients to units more specialized in preventing delirium.
Bottom line: The AWOL prediction tool is simple to use, broadly applicable, and adds another tool to the literature to determine delirium risk.
Citation: Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9);493-499.
Oral Proton Pump Inhibitors (PPIs) as Effective as IV PPIs in Peptic Ulcer Bleeding
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective, randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56-1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Probiotic Benefit Questioned in the Elderly
Clinical question: Do probiotics prevent antibiotic-associated diarrhea (AAD) in patients 65 and older?
Background: Individual studies using different protocols to assess the efficacy of probiotics in preventing AAD, including Clostridium difficile-associated diarrhea (CDAD), suggest a decreased incidence of AAD when taking probiotics. Meta-analysis of this data also suggests that probiotics are effective in prevention of AAD; however, these results are undermined by the high heterogeneity of the studies included.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: Multicenter trial in the United Kingdom.
Synopsis: Nearly 3,000 patients ages 65 years and older who had received one or more antibiotics within seven days were randomized to receive placebo or high-dose probiotics for 21 days. After recruitment, the patients were assessed for AAD up to eight weeks and CDAD up to 12 weeks. Results did not demonstrate a reduction of AAD or CDAD in patients taking probiotics. AAD occurred in 10.8% of patients taking the probiotic and 10.4% of patients taking placebo (95% confidence interval 0.83-1.32). CDAD occurred in 0.8% of patients taking the probiotic and 1.2% of patients taking placebo (95% confidence interval 0.34-1.47).
Based on the results of this double-blind, placebo-controlled trial, there is insufficient evidence to support initiation of probiotics for the prevention of AAD and CDAD in patients 65 years and older. Future studies utilizing standardized protocols against specific antibiotics, along with improved understanding of the underlying mechanisms of AAD prevention, are needed.
Bottom line: High-dose probiotics (lactobacillus acidophilus and bifidobacterium bifidum) do not prevent AAD in elderly patients.
Citation: Allen S, Wareham K, Wang D, et al. Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2013;382(9900):1249-1257.
Colchicine and NSAID Better than NSAID Alone for Acute Pericarditis
Clinical question: Is colchicine safe, effective, and able to prevent recurrence in acute pericarditis?
Background: Colchicine is effective for the treatment of recurrent pericarditis. More recent open-label trials have established its role in acute pericarditis when combined with conventional NSAID therapy. However, a definitive randomized control trial has not been performed to establish colchicine’s role in acute pericarditis.
Study design: Double-blinded, randomized, controlled trial.
Setting: Multicenter in Northern Italy.
Synopsis: Investigators randomized 240 patients to receive either colchicine or placebo in addition to standard therapy of either aspirin or ibuprofen. Incessant or recurrent pericarditis occurred in 16.7% of patients treated with colchicine versus 37.5% in patients receiving placebo (RR 0.56; 95% CI 0.30-0.72; P<0.001). The number needed to treat to prevent one episode of incessant or recurrent pericarditis was four. Colchicine therapy also reduced the frequency of symptom persistence at 72 hours, number of recurrences per patient, rate of hospitalization, and the rate of readmission within one week.
It should be noted that the study excluded the following groups: patients with an elevated troponin, elevated transaminases (>1.5 upper limit of normal), and serum creatinine >2.5.
Bottom line: In addition to conventional therapy, colchicine reduces incessant or recurrent pericarditis in patients with a first episode of acute pericarditis.
Citation: Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369(16):1522-1528.
Improvement Needed in Patient Understanding at Hospital Discharge
Clinical question: How well do older patients with heart failure, pneumonia, or acute coronary syndrome understand their diagnosis and post-discharge follow-up plans compared with medical record data?
Background: As hospitals across the country work on preventing 30-day readmissions, more attention has been given to assessing the quality of discharge processes; few evaluations have been conducted from a patient-centered perspective.
Study Design: Prospective, observational cohort study.
Setting: An urban, academic medical center.
Synopsis: This study evaluated the quality of the discharge process among 377 hospitalized patients >65 years old. Medical record data were compared with patient responses during a telephone interview within one week of discharge. By medical records, every patient received discharge instructions that in 97% of cases included discharge diagnosis, activity instructions, follow-up physician information, and warning signs. The authors determined that discharge diagnosis was not written in lay terms 26% of the time. By patient report, 90% expressed that they understood their discharge diagnosis, yet only around 60% fully understood their diagnosis as it was written in the medical record. Although about half of patients reported having a follow-up appointment upon discharge, only about a third of patients had a documented follow-up appointment in the medical record.
Bottom line: Multiple discrepancies were identified between medical record review and patients’ understanding of their discharge diagnosis and plans. Improvements in discharge processes (such as making follow-up appointments) and in patient education (such as increased use of layperson language) are needed.
Citation: Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center [published online ahead of print August 19, 2013]. JAMA Intern Med.
Effectiveness of a Multihospital Effort to Reduce Rehospitalization
Clinical question: Does Project BOOST reduce 30-day rehospitalization for hospitals participating in a quality improvement collaborative?
Background: With the advent of penalties for hospitals with excessive 30-day readmissions among Medicare beneficiaries, hospitals nationwide are attempting to reduce 30-day readmission rates. Few interventions aimed at reducing 30-day hospital readmissions have been effective, and successful interventions have limited generalizability.
Study design: Semi-controlled, pre-post study.
Setting: Volunteer sample of acute care pilot units within a nationally representative sample of 11 academic and non-academic hospitals.
Synopsis: The 11 hospitals enrolled in this quality improvement collaborative planned and implemented Project BOOST tools over 12 months with support from an external quality improvement mentor. Each hospital tailored the BOOST tools that they implemented based on a needs assessment. Reporting of clinical outcome data was voluntary; administrative sources at each hospital provided these data. Although 30 hospitals participated in this collaborative, only 11 hospitals reported data for this analysis.
Average 30-day rehospitalization rates among BOOST units fell from pre- to post-implementation (14.7% to 12.7%, P=0.010); 30-day rehospitalization rates among control units did not change during this same time period (14.1% to 14.0%, respectively, P=0.831).
Bottom line: Although the 11 hospitals in this collaborative found reduced 30-day readmissions in association with BOOST implementation, this finding may be biased due to voluntary reporting of data and improvements at one hospital driving the overall effect of the intervention. More rigorous evaluation of Project BOOST is needed.
Citation: Hansen LO, Greewald JL, Budnitz T, et al. Project BOOST: Effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421-427.
Hospitals Profit from Preventing Surgical Site Infections
Clinical question: Does quality improvement, in this case preventing surgical site infections (SSIs), necessarily lead to improvement in hospital profit?
Background: It’s clear that preventing SSIs benefits patients and saves money for health insurance providers, but it’s unclear what financial impact SSIs have on hospitals and how best to calculate it. This quantification is needed for cost-benefit analyses of interventions designed to prevent SSIs.
Study design: Retrospective study.
Setting: Four Johns Hopkins-affiliated, tertiary care hospitals.
Synopsis: This retrospective study included all patients admitted to or having certain surgical procedures at four Johns Hopkins-affiliated hospitals between Jan. 1, 2007, and Dec. 31, 2010. Patients were first stratified by complexity, and then those who had a SSI (618) were compared to those without SSIs (399,627 admissions and 25,849 surgeries) for differences in daily hospital charges, length of stay, 30-day readmission rates, and hospital profit.
Although daily charges were essentially the same between the groups, patients with SSIs had almost double the mean length of stay than patients without SSIs. SSI patients also had a drastically higher 30-day readmission rate.
The authors propose equations to determine the change in hospital profit due to a single SSI and calculated that preventing one SSI led to an increase in hospital profit between $4,147 and $22,239. These numbers haven’t included the cost of a SSI prevention program, and the limitations in applying these numbers to all hospitals include widely varying hospital costs and differing ability to fill empty beds.
Bottom line: In these four tertiary care hospitals, each SSI prevented could increase hospital profit by thousands of dollars, as well as significantly decrease length of stay and 30-day readmission rates.
Citation: Shepard J, Ward W, Milstone A, et al. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surg. 2013;148(10):907-914.
Prothrombin Complex Concentrate Is Safer than Fresh Frozen Plasma in Rapidly Reversing INR
Clinical question: Is prothrombin complex concentrate (PCC) safer and more effective than fresh frozen plasma (FFP) in reversing international normalized ratio (INR)?
Background: In Canada, PCC has become the standard of care over FFP for reversal of critical INR due to decreased time of administration, faster preparation, lack of allergic reactions, and small volume. Few studies compare these two products in their adverse effects, time to INR reversal, length of stay, and blood transfusion requirements.
Study design: Retrospective cohort study.
Setting: Two tertiary care EDs in Canada.
Synopsis: Health records of adult patients with an INR ≥1.8 who received FFP over a two-year period prior to PCC introduction (n=149) were compared to those who received PCC in the two years after PCC introduction (n=165). Total serious adverse events, which include mortality, myocardial infarction, and heart failure, were higher in the FFP group (19.5% versus 9.7%, P=0.0164). Heart failure exacerbations, time to reversal of INR, and units of blood transfused were increased in the FFP group. There was no difference in thromboembolic events or in length of stay.
Due to this study’s retrospective nature, there were issues with documentation of INR measurements, so true rapidity of INR reversal is unknown. In the United States, the FDA only recently approved PCC for use, so availability might be limited.
Bottom line: Prothrombin complex concentrate is an effective and fast alternative to FFP for reversal of critical INR levels.
Citation: Hickey M, Gatien M, Taljaard M, Aujnarain A, Giulivi A, Perry JJ. Outcomes of urgent warfarin reversal with frozen plasma versus prothombin complex concentrate in the emergency department. Circulation. 2013;128(4):360-364.
Hospital-Acquired Anemia Associated with Higher Mortality, Increased LOS
Clinical question: What is the prevalence of hospital-acquired anemia (HAA), and does it lead to increased mortality and resource utilization?
Background: HAA is a multifactorial care-based problem that occurs as a result of hemodilution, phlebotomy, blood loss from procedures, and impaired erythropoiesis. In the general hospital population, very little is known about HAA prevalence or whether HAA is associated with increased mortality, greater length of stay (LOS), or higher costs.
Study design: Retrospective cohort study.
Setting: Large academic health system in Ohio.
Synopsis: Using administrative data and electronic health record data, an analysis of 188,447 hospitalizations showed that HAA prevalence was 74%. Worsening HAA was correlated to an increase in mortality, so that the odds ratio of mortality with moderate anemia (Hgb between >9 and ≤11) was 1.51 (95% confidence interval 1.33-1.71, P<0.001) and severe anemia (Hgb ≤9) was 3.28 (95% confidence interval 2.90-3.72, P<0.001). Increased degree of HAA was correlated to increasing LOS (up to 1.88 extra days for patients with severe anemia) and higher hospital costs.
Because this is a retrospective observational study, no true causal relationship can be discerned from this study. However, the body of evidence linking iatrogenic causes of anemia to negative outcomes is compelling. Hospitalists should attempt to limit blood loss through judicious use of phlebotomy and procedures in their patients, so as to avoid anemia and subsequent unnecessary transfusions.
Bottom line: Hospital-acquired anemia is associated with higher mortality, LOS, and hospital costs in all hospitalized patients.
Citation: Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512.
Thrombolytics and Stroke: The Faster the Better
Clinical question: Does time from ischemic stroke onset to treatment with intravenous thrombolysis make a difference?
Background: Previous studies have shown that “time is brain.” Quicker treatment with intravenous thrombolysis improves outcomes. Multicenter comparison of very early treatment (i.e., <90 minutes) to a later onset to treatment has not been done.
Study design: Observational study.
Setting: Patient information from 1998 to 2012 from 10 European stroke centers.
Synopsis: A total of 6,856 patients were included, of which 19% received thrombolysis in <90 minutes. None of the patients received endovascular treatment for stroke. Modified Rankin score, a functional assessment, was used to determine outcome. A score of 0 or 1, an “excellent” outcome, was seen more often in patients with a moderate severity stroke (NIH stroke scale of 7-12) who received thrombolysis in <90 minutes, but not in other groups. Thrombolysis in <90 minutes was associated with fewer intracerebral hemorrhages (ICH), but symptomatic ICH was not statistically significantly different. Mortality at three months was not different in the two time groups.
Limitations to this study included an unknown presumed cause of stroke in more than a quarter of patients. Deviations from acute stroke protocols are not described. This study adds to the body of literature supporting the early use of intravenous thrombolysis in eligible acute stroke patients.
Bottom line: Expedient treatment with intravenous thrombolysis should occur in acute stroke patients.
Citation: Strbian D, Ringleb P, Michel P, et al. Ultra-early intravenous stroke thrombolysis: do all patients benefit similarly? Stroke. 2013;44(10):2913-2916.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Intravenous haloperidol does not prevent ICU delirium
- Predicting delirium risk in hospitalized adults
- Oral PPIs as effective as IV PPIs in peptic ulcer bleeding
- Probiotic benefit questioned in the elderly
- Colchicine and NSAID better than NSAID alone for acute pericarditis
- Improvement needed in patient understanding at hospital discharge
- Effectiveness of a multihospital effort to reduce rehospitalization
- Hospitals profit from preventing surgical site infections
- Prothrombin complex concentrate safer than fresh frozen plasma in rapidly reversing INR
- Hospital-acquired anemia associated with higher mortality, increased LOS
- Thrombolytics and stroke: the faster the better
Intravenous Haloperidol Does Not Prevent ICU Delirium
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Predicting Delirium Risk in Hospitalized Adults
Clinical question: Can a simple tool be developed and used for predicting delirium in hospitalized adults?
Background: Delirium is a common condition that results in higher mortality, longer length of stays, and higher probability of discharge to nursing home. Current delirium prediction tools are complicated, or restricted to surgical or critically ill patients.
Study design: Prospective cohort study, with separate derivation and validation cohorts.
Setting: Two academic hospitals and a VA hospital in San Francisco.
Synopsis: Investigators enrolled 374 hospitalized patients who were more than 50 years of age and not delirious at time of admission (209 patients in the derivation and 165 in the validation). The authors identified four predictors of delirium: Age >80; failure to spell “World” backwards; disOrientation to place; and higher nurse-rated iLlness severity (AWOL). The authors found that rates of delirium increased with increasing number of predictors (with zero predictors, 2% developed delirium; one predictor, 4%; two predictors, 14%; three predictors, 20%; four predictors, 64%).
These predictors are similar to other previously identified risk factors, as well as to prediction tools that are in use for surgical patients. However, this tool is quick and can be completed by nursing staff, so it may have a role to play in helping triage patients to units more specialized in preventing delirium.
Bottom line: The AWOL prediction tool is simple to use, broadly applicable, and adds another tool to the literature to determine delirium risk.
Citation: Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9);493-499.
Oral Proton Pump Inhibitors (PPIs) as Effective as IV PPIs in Peptic Ulcer Bleeding
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective, randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56-1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Probiotic Benefit Questioned in the Elderly
Clinical question: Do probiotics prevent antibiotic-associated diarrhea (AAD) in patients 65 and older?
Background: Individual studies using different protocols to assess the efficacy of probiotics in preventing AAD, including Clostridium difficile-associated diarrhea (CDAD), suggest a decreased incidence of AAD when taking probiotics. Meta-analysis of this data also suggests that probiotics are effective in prevention of AAD; however, these results are undermined by the high heterogeneity of the studies included.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: Multicenter trial in the United Kingdom.
Synopsis: Nearly 3,000 patients ages 65 years and older who had received one or more antibiotics within seven days were randomized to receive placebo or high-dose probiotics for 21 days. After recruitment, the patients were assessed for AAD up to eight weeks and CDAD up to 12 weeks. Results did not demonstrate a reduction of AAD or CDAD in patients taking probiotics. AAD occurred in 10.8% of patients taking the probiotic and 10.4% of patients taking placebo (95% confidence interval 0.83-1.32). CDAD occurred in 0.8% of patients taking the probiotic and 1.2% of patients taking placebo (95% confidence interval 0.34-1.47).
Based on the results of this double-blind, placebo-controlled trial, there is insufficient evidence to support initiation of probiotics for the prevention of AAD and CDAD in patients 65 years and older. Future studies utilizing standardized protocols against specific antibiotics, along with improved understanding of the underlying mechanisms of AAD prevention, are needed.
Bottom line: High-dose probiotics (lactobacillus acidophilus and bifidobacterium bifidum) do not prevent AAD in elderly patients.
Citation: Allen S, Wareham K, Wang D, et al. Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2013;382(9900):1249-1257.
Colchicine and NSAID Better than NSAID Alone for Acute Pericarditis
Clinical question: Is colchicine safe, effective, and able to prevent recurrence in acute pericarditis?
Background: Colchicine is effective for the treatment of recurrent pericarditis. More recent open-label trials have established its role in acute pericarditis when combined with conventional NSAID therapy. However, a definitive randomized control trial has not been performed to establish colchicine’s role in acute pericarditis.
Study design: Double-blinded, randomized, controlled trial.
Setting: Multicenter in Northern Italy.
Synopsis: Investigators randomized 240 patients to receive either colchicine or placebo in addition to standard therapy of either aspirin or ibuprofen. Incessant or recurrent pericarditis occurred in 16.7% of patients treated with colchicine versus 37.5% in patients receiving placebo (RR 0.56; 95% CI 0.30-0.72; P<0.001). The number needed to treat to prevent one episode of incessant or recurrent pericarditis was four. Colchicine therapy also reduced the frequency of symptom persistence at 72 hours, number of recurrences per patient, rate of hospitalization, and the rate of readmission within one week.
It should be noted that the study excluded the following groups: patients with an elevated troponin, elevated transaminases (>1.5 upper limit of normal), and serum creatinine >2.5.
Bottom line: In addition to conventional therapy, colchicine reduces incessant or recurrent pericarditis in patients with a first episode of acute pericarditis.
Citation: Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369(16):1522-1528.
Improvement Needed in Patient Understanding at Hospital Discharge
Clinical question: How well do older patients with heart failure, pneumonia, or acute coronary syndrome understand their diagnosis and post-discharge follow-up plans compared with medical record data?
Background: As hospitals across the country work on preventing 30-day readmissions, more attention has been given to assessing the quality of discharge processes; few evaluations have been conducted from a patient-centered perspective.
Study Design: Prospective, observational cohort study.
Setting: An urban, academic medical center.
Synopsis: This study evaluated the quality of the discharge process among 377 hospitalized patients >65 years old. Medical record data were compared with patient responses during a telephone interview within one week of discharge. By medical records, every patient received discharge instructions that in 97% of cases included discharge diagnosis, activity instructions, follow-up physician information, and warning signs. The authors determined that discharge diagnosis was not written in lay terms 26% of the time. By patient report, 90% expressed that they understood their discharge diagnosis, yet only around 60% fully understood their diagnosis as it was written in the medical record. Although about half of patients reported having a follow-up appointment upon discharge, only about a third of patients had a documented follow-up appointment in the medical record.
Bottom line: Multiple discrepancies were identified between medical record review and patients’ understanding of their discharge diagnosis and plans. Improvements in discharge processes (such as making follow-up appointments) and in patient education (such as increased use of layperson language) are needed.
Citation: Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center [published online ahead of print August 19, 2013]. JAMA Intern Med.
Effectiveness of a Multihospital Effort to Reduce Rehospitalization
Clinical question: Does Project BOOST reduce 30-day rehospitalization for hospitals participating in a quality improvement collaborative?
Background: With the advent of penalties for hospitals with excessive 30-day readmissions among Medicare beneficiaries, hospitals nationwide are attempting to reduce 30-day readmission rates. Few interventions aimed at reducing 30-day hospital readmissions have been effective, and successful interventions have limited generalizability.
Study design: Semi-controlled, pre-post study.
Setting: Volunteer sample of acute care pilot units within a nationally representative sample of 11 academic and non-academic hospitals.
Synopsis: The 11 hospitals enrolled in this quality improvement collaborative planned and implemented Project BOOST tools over 12 months with support from an external quality improvement mentor. Each hospital tailored the BOOST tools that they implemented based on a needs assessment. Reporting of clinical outcome data was voluntary; administrative sources at each hospital provided these data. Although 30 hospitals participated in this collaborative, only 11 hospitals reported data for this analysis.
Average 30-day rehospitalization rates among BOOST units fell from pre- to post-implementation (14.7% to 12.7%, P=0.010); 30-day rehospitalization rates among control units did not change during this same time period (14.1% to 14.0%, respectively, P=0.831).
Bottom line: Although the 11 hospitals in this collaborative found reduced 30-day readmissions in association with BOOST implementation, this finding may be biased due to voluntary reporting of data and improvements at one hospital driving the overall effect of the intervention. More rigorous evaluation of Project BOOST is needed.
Citation: Hansen LO, Greewald JL, Budnitz T, et al. Project BOOST: Effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421-427.
Hospitals Profit from Preventing Surgical Site Infections
Clinical question: Does quality improvement, in this case preventing surgical site infections (SSIs), necessarily lead to improvement in hospital profit?
Background: It’s clear that preventing SSIs benefits patients and saves money for health insurance providers, but it’s unclear what financial impact SSIs have on hospitals and how best to calculate it. This quantification is needed for cost-benefit analyses of interventions designed to prevent SSIs.
Study design: Retrospective study.
Setting: Four Johns Hopkins-affiliated, tertiary care hospitals.
Synopsis: This retrospective study included all patients admitted to or having certain surgical procedures at four Johns Hopkins-affiliated hospitals between Jan. 1, 2007, and Dec. 31, 2010. Patients were first stratified by complexity, and then those who had a SSI (618) were compared to those without SSIs (399,627 admissions and 25,849 surgeries) for differences in daily hospital charges, length of stay, 30-day readmission rates, and hospital profit.
Although daily charges were essentially the same between the groups, patients with SSIs had almost double the mean length of stay than patients without SSIs. SSI patients also had a drastically higher 30-day readmission rate.
The authors propose equations to determine the change in hospital profit due to a single SSI and calculated that preventing one SSI led to an increase in hospital profit between $4,147 and $22,239. These numbers haven’t included the cost of a SSI prevention program, and the limitations in applying these numbers to all hospitals include widely varying hospital costs and differing ability to fill empty beds.
Bottom line: In these four tertiary care hospitals, each SSI prevented could increase hospital profit by thousands of dollars, as well as significantly decrease length of stay and 30-day readmission rates.
Citation: Shepard J, Ward W, Milstone A, et al. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surg. 2013;148(10):907-914.
Prothrombin Complex Concentrate Is Safer than Fresh Frozen Plasma in Rapidly Reversing INR
Clinical question: Is prothrombin complex concentrate (PCC) safer and more effective than fresh frozen plasma (FFP) in reversing international normalized ratio (INR)?
Background: In Canada, PCC has become the standard of care over FFP for reversal of critical INR due to decreased time of administration, faster preparation, lack of allergic reactions, and small volume. Few studies compare these two products in their adverse effects, time to INR reversal, length of stay, and blood transfusion requirements.
Study design: Retrospective cohort study.
Setting: Two tertiary care EDs in Canada.
Synopsis: Health records of adult patients with an INR ≥1.8 who received FFP over a two-year period prior to PCC introduction (n=149) were compared to those who received PCC in the two years after PCC introduction (n=165). Total serious adverse events, which include mortality, myocardial infarction, and heart failure, were higher in the FFP group (19.5% versus 9.7%, P=0.0164). Heart failure exacerbations, time to reversal of INR, and units of blood transfused were increased in the FFP group. There was no difference in thromboembolic events or in length of stay.
Due to this study’s retrospective nature, there were issues with documentation of INR measurements, so true rapidity of INR reversal is unknown. In the United States, the FDA only recently approved PCC for use, so availability might be limited.
Bottom line: Prothrombin complex concentrate is an effective and fast alternative to FFP for reversal of critical INR levels.
Citation: Hickey M, Gatien M, Taljaard M, Aujnarain A, Giulivi A, Perry JJ. Outcomes of urgent warfarin reversal with frozen plasma versus prothombin complex concentrate in the emergency department. Circulation. 2013;128(4):360-364.
Hospital-Acquired Anemia Associated with Higher Mortality, Increased LOS
Clinical question: What is the prevalence of hospital-acquired anemia (HAA), and does it lead to increased mortality and resource utilization?
Background: HAA is a multifactorial care-based problem that occurs as a result of hemodilution, phlebotomy, blood loss from procedures, and impaired erythropoiesis. In the general hospital population, very little is known about HAA prevalence or whether HAA is associated with increased mortality, greater length of stay (LOS), or higher costs.
Study design: Retrospective cohort study.
Setting: Large academic health system in Ohio.
Synopsis: Using administrative data and electronic health record data, an analysis of 188,447 hospitalizations showed that HAA prevalence was 74%. Worsening HAA was correlated to an increase in mortality, so that the odds ratio of mortality with moderate anemia (Hgb between >9 and ≤11) was 1.51 (95% confidence interval 1.33-1.71, P<0.001) and severe anemia (Hgb ≤9) was 3.28 (95% confidence interval 2.90-3.72, P<0.001). Increased degree of HAA was correlated to increasing LOS (up to 1.88 extra days for patients with severe anemia) and higher hospital costs.
Because this is a retrospective observational study, no true causal relationship can be discerned from this study. However, the body of evidence linking iatrogenic causes of anemia to negative outcomes is compelling. Hospitalists should attempt to limit blood loss through judicious use of phlebotomy and procedures in their patients, so as to avoid anemia and subsequent unnecessary transfusions.
Bottom line: Hospital-acquired anemia is associated with higher mortality, LOS, and hospital costs in all hospitalized patients.
Citation: Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512.
Thrombolytics and Stroke: The Faster the Better
Clinical question: Does time from ischemic stroke onset to treatment with intravenous thrombolysis make a difference?
Background: Previous studies have shown that “time is brain.” Quicker treatment with intravenous thrombolysis improves outcomes. Multicenter comparison of very early treatment (i.e., <90 minutes) to a later onset to treatment has not been done.
Study design: Observational study.
Setting: Patient information from 1998 to 2012 from 10 European stroke centers.
Synopsis: A total of 6,856 patients were included, of which 19% received thrombolysis in <90 minutes. None of the patients received endovascular treatment for stroke. Modified Rankin score, a functional assessment, was used to determine outcome. A score of 0 or 1, an “excellent” outcome, was seen more often in patients with a moderate severity stroke (NIH stroke scale of 7-12) who received thrombolysis in <90 minutes, but not in other groups. Thrombolysis in <90 minutes was associated with fewer intracerebral hemorrhages (ICH), but symptomatic ICH was not statistically significantly different. Mortality at three months was not different in the two time groups.
Limitations to this study included an unknown presumed cause of stroke in more than a quarter of patients. Deviations from acute stroke protocols are not described. This study adds to the body of literature supporting the early use of intravenous thrombolysis in eligible acute stroke patients.
Bottom line: Expedient treatment with intravenous thrombolysis should occur in acute stroke patients.
Citation: Strbian D, Ringleb P, Michel P, et al. Ultra-early intravenous stroke thrombolysis: do all patients benefit similarly? Stroke. 2013;44(10):2913-2916.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Intravenous haloperidol does not prevent ICU delirium
- Predicting delirium risk in hospitalized adults
- Oral PPIs as effective as IV PPIs in peptic ulcer bleeding
- Probiotic benefit questioned in the elderly
- Colchicine and NSAID better than NSAID alone for acute pericarditis
- Improvement needed in patient understanding at hospital discharge
- Effectiveness of a multihospital effort to reduce rehospitalization
- Hospitals profit from preventing surgical site infections
- Prothrombin complex concentrate safer than fresh frozen plasma in rapidly reversing INR
- Hospital-acquired anemia associated with higher mortality, increased LOS
- Thrombolytics and stroke: the faster the better
Intravenous Haloperidol Does Not Prevent ICU Delirium
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Predicting Delirium Risk in Hospitalized Adults
Clinical question: Can a simple tool be developed and used for predicting delirium in hospitalized adults?
Background: Delirium is a common condition that results in higher mortality, longer length of stays, and higher probability of discharge to nursing home. Current delirium prediction tools are complicated, or restricted to surgical or critically ill patients.
Study design: Prospective cohort study, with separate derivation and validation cohorts.
Setting: Two academic hospitals and a VA hospital in San Francisco.
Synopsis: Investigators enrolled 374 hospitalized patients who were more than 50 years of age and not delirious at time of admission (209 patients in the derivation and 165 in the validation). The authors identified four predictors of delirium: Age >80; failure to spell “World” backwards; disOrientation to place; and higher nurse-rated iLlness severity (AWOL). The authors found that rates of delirium increased with increasing number of predictors (with zero predictors, 2% developed delirium; one predictor, 4%; two predictors, 14%; three predictors, 20%; four predictors, 64%).
These predictors are similar to other previously identified risk factors, as well as to prediction tools that are in use for surgical patients. However, this tool is quick and can be completed by nursing staff, so it may have a role to play in helping triage patients to units more specialized in preventing delirium.
Bottom line: The AWOL prediction tool is simple to use, broadly applicable, and adds another tool to the literature to determine delirium risk.
Citation: Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9);493-499.
Oral Proton Pump Inhibitors (PPIs) as Effective as IV PPIs in Peptic Ulcer Bleeding
Clinical question: In patients with peptic ulcer bleeding, are oral PPIs of equal benefit to intravenous PPIs?
Background: PPI therapy has been shown in several studies to reduce re-bleeding risk in patients when used adjunctively for peptic ulcer bleeding. In spite of this data, there is still uncertainty about the optimal dose and route of administration.
Study design: Meta-analysis of prospective, randomized control trials.
Setting: OVID database search in June 2012.
Synopsis: A literature search identified six prospective, randomized control trials. Overall, 615 patients were included across the six trials. No significant difference in risk of re-bleeding was discovered between the two groups (8.6% oral vs. 9.3% IV, RR: 0.92, 95% CI: 0.56-1.5). Length of hospital stay was statistically significantly lower for oral PPIs (-0.74 day, 95% CI: -1.10 to -0.39 day).
Because these findings are based on a meta-analysis of studies with notable flaws—including lack of blinding—it is difficult to draw any definitive conclusions from this data. Hospitalists should use care before changing their practice patterns, given the risk of bias and need for further study.
Bottom line: Oral PPIs may reduce hospital length of stay without an increased risk of re-bleeding; however, further study with a well-powered, double-blind, randomized control trial is necessary.
Citation: Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013;38(7):721-728.
Probiotic Benefit Questioned in the Elderly
Clinical question: Do probiotics prevent antibiotic-associated diarrhea (AAD) in patients 65 and older?
Background: Individual studies using different protocols to assess the efficacy of probiotics in preventing AAD, including Clostridium difficile-associated diarrhea (CDAD), suggest a decreased incidence of AAD when taking probiotics. Meta-analysis of this data also suggests that probiotics are effective in prevention of AAD; however, these results are undermined by the high heterogeneity of the studies included.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: Multicenter trial in the United Kingdom.
Synopsis: Nearly 3,000 patients ages 65 years and older who had received one or more antibiotics within seven days were randomized to receive placebo or high-dose probiotics for 21 days. After recruitment, the patients were assessed for AAD up to eight weeks and CDAD up to 12 weeks. Results did not demonstrate a reduction of AAD or CDAD in patients taking probiotics. AAD occurred in 10.8% of patients taking the probiotic and 10.4% of patients taking placebo (95% confidence interval 0.83-1.32). CDAD occurred in 0.8% of patients taking the probiotic and 1.2% of patients taking placebo (95% confidence interval 0.34-1.47).
Based on the results of this double-blind, placebo-controlled trial, there is insufficient evidence to support initiation of probiotics for the prevention of AAD and CDAD in patients 65 years and older. Future studies utilizing standardized protocols against specific antibiotics, along with improved understanding of the underlying mechanisms of AAD prevention, are needed.
Bottom line: High-dose probiotics (lactobacillus acidophilus and bifidobacterium bifidum) do not prevent AAD in elderly patients.
Citation: Allen S, Wareham K, Wang D, et al. Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2013;382(9900):1249-1257.
Colchicine and NSAID Better than NSAID Alone for Acute Pericarditis
Clinical question: Is colchicine safe, effective, and able to prevent recurrence in acute pericarditis?
Background: Colchicine is effective for the treatment of recurrent pericarditis. More recent open-label trials have established its role in acute pericarditis when combined with conventional NSAID therapy. However, a definitive randomized control trial has not been performed to establish colchicine’s role in acute pericarditis.
Study design: Double-blinded, randomized, controlled trial.
Setting: Multicenter in Northern Italy.
Synopsis: Investigators randomized 240 patients to receive either colchicine or placebo in addition to standard therapy of either aspirin or ibuprofen. Incessant or recurrent pericarditis occurred in 16.7% of patients treated with colchicine versus 37.5% in patients receiving placebo (RR 0.56; 95% CI 0.30-0.72; P<0.001). The number needed to treat to prevent one episode of incessant or recurrent pericarditis was four. Colchicine therapy also reduced the frequency of symptom persistence at 72 hours, number of recurrences per patient, rate of hospitalization, and the rate of readmission within one week.
It should be noted that the study excluded the following groups: patients with an elevated troponin, elevated transaminases (>1.5 upper limit of normal), and serum creatinine >2.5.
Bottom line: In addition to conventional therapy, colchicine reduces incessant or recurrent pericarditis in patients with a first episode of acute pericarditis.
Citation: Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369(16):1522-1528.
Improvement Needed in Patient Understanding at Hospital Discharge
Clinical question: How well do older patients with heart failure, pneumonia, or acute coronary syndrome understand their diagnosis and post-discharge follow-up plans compared with medical record data?
Background: As hospitals across the country work on preventing 30-day readmissions, more attention has been given to assessing the quality of discharge processes; few evaluations have been conducted from a patient-centered perspective.
Study Design: Prospective, observational cohort study.
Setting: An urban, academic medical center.
Synopsis: This study evaluated the quality of the discharge process among 377 hospitalized patients >65 years old. Medical record data were compared with patient responses during a telephone interview within one week of discharge. By medical records, every patient received discharge instructions that in 97% of cases included discharge diagnosis, activity instructions, follow-up physician information, and warning signs. The authors determined that discharge diagnosis was not written in lay terms 26% of the time. By patient report, 90% expressed that they understood their discharge diagnosis, yet only around 60% fully understood their diagnosis as it was written in the medical record. Although about half of patients reported having a follow-up appointment upon discharge, only about a third of patients had a documented follow-up appointment in the medical record.
Bottom line: Multiple discrepancies were identified between medical record review and patients’ understanding of their discharge diagnosis and plans. Improvements in discharge processes (such as making follow-up appointments) and in patient education (such as increased use of layperson language) are needed.
Citation: Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center [published online ahead of print August 19, 2013]. JAMA Intern Med.
Effectiveness of a Multihospital Effort to Reduce Rehospitalization
Clinical question: Does Project BOOST reduce 30-day rehospitalization for hospitals participating in a quality improvement collaborative?
Background: With the advent of penalties for hospitals with excessive 30-day readmissions among Medicare beneficiaries, hospitals nationwide are attempting to reduce 30-day readmission rates. Few interventions aimed at reducing 30-day hospital readmissions have been effective, and successful interventions have limited generalizability.
Study design: Semi-controlled, pre-post study.
Setting: Volunteer sample of acute care pilot units within a nationally representative sample of 11 academic and non-academic hospitals.
Synopsis: The 11 hospitals enrolled in this quality improvement collaborative planned and implemented Project BOOST tools over 12 months with support from an external quality improvement mentor. Each hospital tailored the BOOST tools that they implemented based on a needs assessment. Reporting of clinical outcome data was voluntary; administrative sources at each hospital provided these data. Although 30 hospitals participated in this collaborative, only 11 hospitals reported data for this analysis.
Average 30-day rehospitalization rates among BOOST units fell from pre- to post-implementation (14.7% to 12.7%, P=0.010); 30-day rehospitalization rates among control units did not change during this same time period (14.1% to 14.0%, respectively, P=0.831).
Bottom line: Although the 11 hospitals in this collaborative found reduced 30-day readmissions in association with BOOST implementation, this finding may be biased due to voluntary reporting of data and improvements at one hospital driving the overall effect of the intervention. More rigorous evaluation of Project BOOST is needed.
Citation: Hansen LO, Greewald JL, Budnitz T, et al. Project BOOST: Effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421-427.
Hospitals Profit from Preventing Surgical Site Infections
Clinical question: Does quality improvement, in this case preventing surgical site infections (SSIs), necessarily lead to improvement in hospital profit?
Background: It’s clear that preventing SSIs benefits patients and saves money for health insurance providers, but it’s unclear what financial impact SSIs have on hospitals and how best to calculate it. This quantification is needed for cost-benefit analyses of interventions designed to prevent SSIs.
Study design: Retrospective study.
Setting: Four Johns Hopkins-affiliated, tertiary care hospitals.
Synopsis: This retrospective study included all patients admitted to or having certain surgical procedures at four Johns Hopkins-affiliated hospitals between Jan. 1, 2007, and Dec. 31, 2010. Patients were first stratified by complexity, and then those who had a SSI (618) were compared to those without SSIs (399,627 admissions and 25,849 surgeries) for differences in daily hospital charges, length of stay, 30-day readmission rates, and hospital profit.
Although daily charges were essentially the same between the groups, patients with SSIs had almost double the mean length of stay than patients without SSIs. SSI patients also had a drastically higher 30-day readmission rate.
The authors propose equations to determine the change in hospital profit due to a single SSI and calculated that preventing one SSI led to an increase in hospital profit between $4,147 and $22,239. These numbers haven’t included the cost of a SSI prevention program, and the limitations in applying these numbers to all hospitals include widely varying hospital costs and differing ability to fill empty beds.
Bottom line: In these four tertiary care hospitals, each SSI prevented could increase hospital profit by thousands of dollars, as well as significantly decrease length of stay and 30-day readmission rates.
Citation: Shepard J, Ward W, Milstone A, et al. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surg. 2013;148(10):907-914.
Prothrombin Complex Concentrate Is Safer than Fresh Frozen Plasma in Rapidly Reversing INR
Clinical question: Is prothrombin complex concentrate (PCC) safer and more effective than fresh frozen plasma (FFP) in reversing international normalized ratio (INR)?
Background: In Canada, PCC has become the standard of care over FFP for reversal of critical INR due to decreased time of administration, faster preparation, lack of allergic reactions, and small volume. Few studies compare these two products in their adverse effects, time to INR reversal, length of stay, and blood transfusion requirements.
Study design: Retrospective cohort study.
Setting: Two tertiary care EDs in Canada.
Synopsis: Health records of adult patients with an INR ≥1.8 who received FFP over a two-year period prior to PCC introduction (n=149) were compared to those who received PCC in the two years after PCC introduction (n=165). Total serious adverse events, which include mortality, myocardial infarction, and heart failure, were higher in the FFP group (19.5% versus 9.7%, P=0.0164). Heart failure exacerbations, time to reversal of INR, and units of blood transfused were increased in the FFP group. There was no difference in thromboembolic events or in length of stay.
Due to this study’s retrospective nature, there were issues with documentation of INR measurements, so true rapidity of INR reversal is unknown. In the United States, the FDA only recently approved PCC for use, so availability might be limited.
Bottom line: Prothrombin complex concentrate is an effective and fast alternative to FFP for reversal of critical INR levels.
Citation: Hickey M, Gatien M, Taljaard M, Aujnarain A, Giulivi A, Perry JJ. Outcomes of urgent warfarin reversal with frozen plasma versus prothombin complex concentrate in the emergency department. Circulation. 2013;128(4):360-364.
Hospital-Acquired Anemia Associated with Higher Mortality, Increased LOS
Clinical question: What is the prevalence of hospital-acquired anemia (HAA), and does it lead to increased mortality and resource utilization?
Background: HAA is a multifactorial care-based problem that occurs as a result of hemodilution, phlebotomy, blood loss from procedures, and impaired erythropoiesis. In the general hospital population, very little is known about HAA prevalence or whether HAA is associated with increased mortality, greater length of stay (LOS), or higher costs.
Study design: Retrospective cohort study.
Setting: Large academic health system in Ohio.
Synopsis: Using administrative data and electronic health record data, an analysis of 188,447 hospitalizations showed that HAA prevalence was 74%. Worsening HAA was correlated to an increase in mortality, so that the odds ratio of mortality with moderate anemia (Hgb between >9 and ≤11) was 1.51 (95% confidence interval 1.33-1.71, P<0.001) and severe anemia (Hgb ≤9) was 3.28 (95% confidence interval 2.90-3.72, P<0.001). Increased degree of HAA was correlated to increasing LOS (up to 1.88 extra days for patients with severe anemia) and higher hospital costs.
Because this is a retrospective observational study, no true causal relationship can be discerned from this study. However, the body of evidence linking iatrogenic causes of anemia to negative outcomes is compelling. Hospitalists should attempt to limit blood loss through judicious use of phlebotomy and procedures in their patients, so as to avoid anemia and subsequent unnecessary transfusions.
Bottom line: Hospital-acquired anemia is associated with higher mortality, LOS, and hospital costs in all hospitalized patients.
Citation: Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512.
Thrombolytics and Stroke: The Faster the Better
Clinical question: Does time from ischemic stroke onset to treatment with intravenous thrombolysis make a difference?
Background: Previous studies have shown that “time is brain.” Quicker treatment with intravenous thrombolysis improves outcomes. Multicenter comparison of very early treatment (i.e., <90 minutes) to a later onset to treatment has not been done.
Study design: Observational study.
Setting: Patient information from 1998 to 2012 from 10 European stroke centers.
Synopsis: A total of 6,856 patients were included, of which 19% received thrombolysis in <90 minutes. None of the patients received endovascular treatment for stroke. Modified Rankin score, a functional assessment, was used to determine outcome. A score of 0 or 1, an “excellent” outcome, was seen more often in patients with a moderate severity stroke (NIH stroke scale of 7-12) who received thrombolysis in <90 minutes, but not in other groups. Thrombolysis in <90 minutes was associated with fewer intracerebral hemorrhages (ICH), but symptomatic ICH was not statistically significantly different. Mortality at three months was not different in the two time groups.
Limitations to this study included an unknown presumed cause of stroke in more than a quarter of patients. Deviations from acute stroke protocols are not described. This study adds to the body of literature supporting the early use of intravenous thrombolysis in eligible acute stroke patients.
Bottom line: Expedient treatment with intravenous thrombolysis should occur in acute stroke patients.
Citation: Strbian D, Ringleb P, Michel P, et al. Ultra-early intravenous stroke thrombolysis: do all patients benefit similarly? Stroke. 2013;44(10):2913-2916.