User login
Gender Disparities for Academic Hospitalists
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
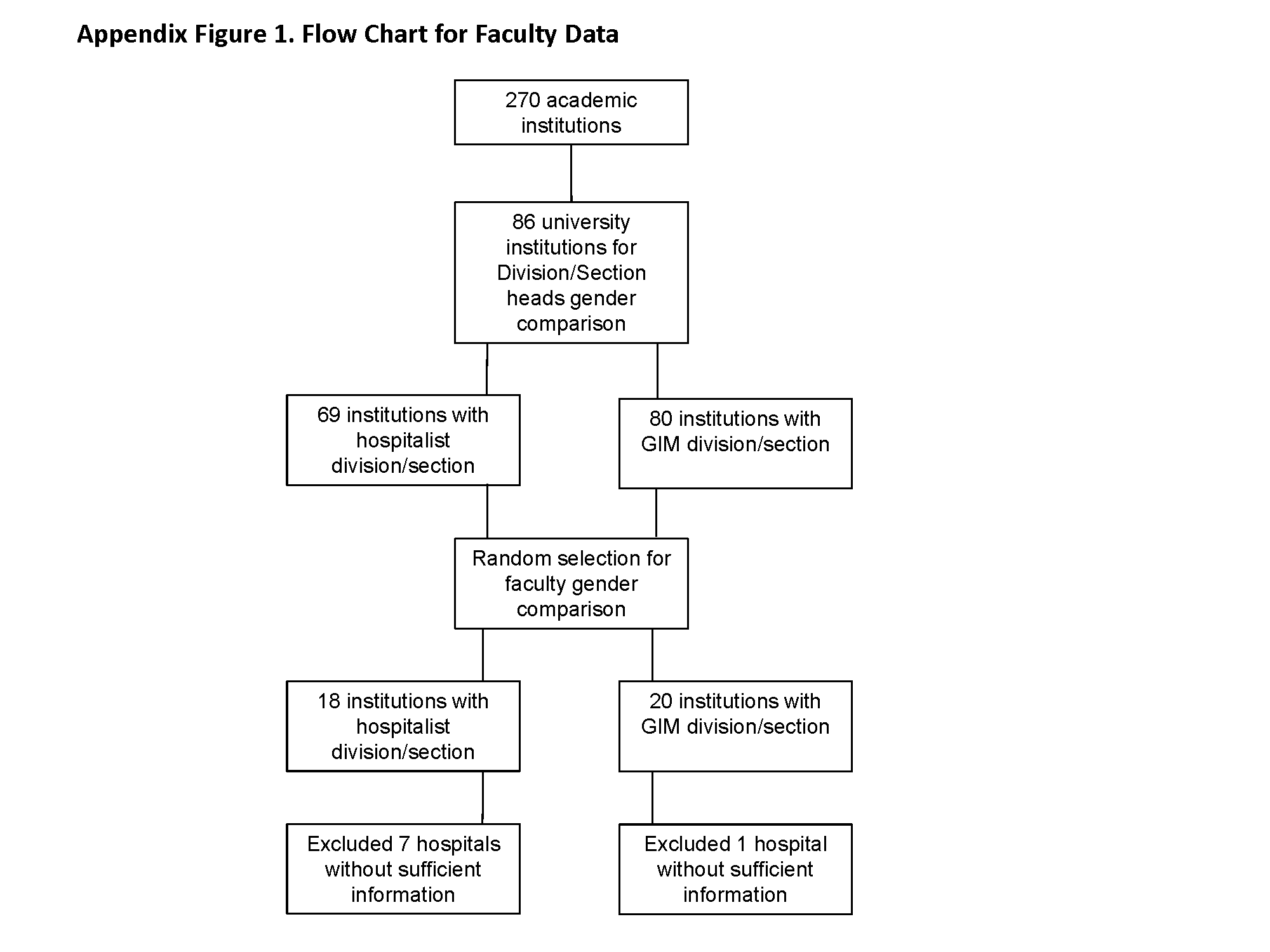
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
Gender disparities still exist for women in academic medicine.[1, 2, 3, 4, 5, 6, 7, 8, 9] The most recent data from the Association of American Medical Colleges (AAMC) show that although gender disparities are decreasing, women are still under‐represented in the assistant, associate, and full‐professor ranks as well as in leadership positions.[1]
Some studies indicate that gender differences are less evident when examining younger cohorts.[1, 10, 11, 12, 13] Hospital medicine emerged around 1996, when the term hospitalist was first coined.[14] The gender distribution of academic hospitalists is likely nearly equal,[15, 16] and they are generally younger physicians.[15, 17, 18, 19, 20] Accordingly, we questioned whether gender disparities existed in academic hospital medicine (HM) and, if so, whether these disparities were greater than those that might exist in academic general internal medicine (GIM).
METHODS
This study consisted of both prospective and retrospective observation of data collected for academic adult hospitalists and general internists who practice in the United States. It was approved by the Colorado Multiple Institutional Review Board.
Gender distribution was assessed with respect to: (1) academic HM and GIM faculty, (2) leadership (ie, division or section heads), and (3) scholarly work (ie, speaking opportunities and publications). Data were collected between October 1, 2012 and August 31, 2014.
Gender Distribution of Faculty and Division/Section Heads
All US internal medicine residency programs were identified from the list of members or affiliates of the AAMC that were fully accredited by the Liaison Committee on Medical Education[21] using the Graduate Medical Education Directory.[22] We then determined the primary training hospital(s) affiliated with each program and selected those that were considered to be university hospitals and eliminated those that did not have divisions or sections of HM or GIM. We determined the gender of the respective division/section heads on the basis of the faculty member's first name (and often from accompanying photos) as well as from information obtained via Internet searches and, if necessary, contacted the individual institutions via email or phone call(s). We also determined the number and gender of all of the HM and GIM faculty members in a random sample of 25% of these hospitals from information on their respective websites.
Gender Distribution for Scholarly Productivity
We determined the gender and specialty of all speakers at the Society of Hospital Medicine and the Society of General Internal Medicine national conferences from 2006 to 2012. A list of speakers at each conference was obtained from conference pamphlets or agendas that were available via Internet searches or obtained directly from the organization. We also determined whether each presenter was a featured speaker (defined as one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), or if they spoke in a group format (also as indicated in the conference pamphlets). Because of the low number of featured and plenary speakers, these data were combined. Faculty labeled as additional faculty when presenting in a group format were excluded as were speakers at precourses, those presenting abstracts, and those participating in interest group sessions.
For authorship, a PubMed search was used to identify all articles published in the Journal of Hospital Medicine (JHM) and the Journal of General Internal Medicine (JGIM) from January 1, 2006 through December 31, 2012, and the gender and specialty of all the first and last authors were determined as described above. Specialty was determined from the division, section or department affiliation indicated for each author and by Internet searches. In some instances, it was necessary to contact the authors or their departments directly to verify their specialty. When articles had only 1 author, the author was considered a first author.
Duplicate records (eg, same author, same journal) and articles without an author were excluded, as were authors who did not have an MD, DO, or MBBS degree and those who were not affiliated with an institution in the United States. All manuscripts, with the exception of errata, were analyzed together as well as in 3 subgroups: original research, editorials, and others.
A second investigator corroborated data regarding gender and specialty for all speakers and authors to strengthen data integrity. On the rare occasion when discrepancies were found, a third investigator adjudicated the results.
Definitions
Physicians were defined as being hospitalists if they were listed as a member of a division or section of HM on their publications or if Internet searches indicated that they were a hospitalist or primarily worked on inpatient medical services. Physicians were considered to be general internists if they were listed as such on their publications and their specialty could be verified in Web‐based searches. If physicians appeared to have changing roles over time, we attempted to assign their specialty based upon their role at the time the article was published or the presentation was delivered. If necessary, phone calls and/or emails were also done to determine the physician's specialty.
Analysis
REDCap, a secure, Web‐based application for building and managing online surveys and databases, was used to collect and manage all study data.[23] All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc., Cary, NC). A [2] test was used to compare proportions of male versus female physicians, and data from hospitalists versus general internists. Because we performed multiple comparisons when analyzing presentations and publications, a Bonferroni adjustment was made such that a P<0.0125 for presentations and P<0.006 (within specialty) or P<0.0125 (between specialty) for the publication analyses were considered significant. P<0.05 was considered significant for all other comparisons.
RESULTS
Gender Distribution of Faculty
Eighteen HM and 20 GIM programs from university hospitals were randomly selected for review (see Supporting Figure 1 in the online version of this article). Seven of the HM programs and 1 of the GIM programs did not have a website, did not differentiate hospitalists from other faculty, or did not list their faculty on the website and were excluded from the analysis. In the remaining 11 HM programs and 19 GIM programs, women made up 277/568 (49%) and 555/1099 (51%) of the faculty, respectively (P=0.50).
Gender Distribution of Division/Section Heads
Eighty‐six of the programs were classified as university hospitals (see Supporting Figure 1 in the online version of this article), and in these, women led 11/69 (16%) of the HM divisions or sections and 28/80 (35%) of the GIM divisions (P=0.008).
Gender Distribution for Scholarly Productivity
Speaking Opportunities
A total of 1227 presentations were given at the 2 conferences from 2006 to 2012, with 1343 of the speakers meeting inclusion criteria (see Supporting Figure 2 in the online version of this article). Hospitalists accounted for 557 of the speakers, of which 146 (26%) were women. General internists accounted for 580 of the speakers, of which 291 (50%) were women (P<0.0001) (Table 1).
| Male, N (%) | Female, N (%) | |
|---|---|---|
| ||
| Hospitalists | ||
| All presentations | 411 (74) | 146 (26)* |
| Featured or plenary presentations | 49 (91) | 5 (9)* |
| General internists | ||
| All presentations | 289 (50) | 291 (50) |
| Featured or plenary presentations | 27 (55) | 22 (45) |
Of the 117 featured or plenary speakers, 54 were hospitalists and 5 (9%) of these were women. Of the 49 who were general internists, 22 (45%) were women (P<0.0001).
Authorship
The PubMed search identified a total of 3285 articles published in the JHM and the JGIM from 2006 to 2012, and 2172 first authors and 1869 last authors met inclusion criteria (see Supporting Figure 3 in the online version of this article). Hospitalists were listed as first or last authors on 464 and 305 articles, respectively, and of these, women were first authors on 153 (33%) and last authors on 63 (21%). General internists were listed as first or last authors on 895 and 769 articles, respectively, with women as first authors on 423 (47%) and last authors on 265 (34%). Compared with general internists, fewer women hospitalists were listed as either first or last authors (both P<0.0001) (Table 2).
| First Author | Last Author | |||
|---|---|---|---|---|
| Male, N (%) | Female, N (%) | Male, N (%) | Female, N (%) | |
| ||||
| Hospitalists | ||||
| All publications | 311 (67) | 153 (33)* | 242 (79) | 63 (21)* |
| Original investigations/brief reports | 124 (61) | 79 (39)* | 96 (76) | 30 (24)* |
| Editorials | 34 (77) | 10 (23)* | 18 (86) | 3 (14)* |
| Other | 153 (71) | 64 (29)* | 128 (81) | 30 (19)* |
| General internists | ||||
| All publications | 472 (53) | 423 (47) | 504 (66) | 265 (34)* |
| Original investigations/brief reports | 218 (46) | 261 (54) | 310 (65) | 170 (35)* |
| Editorial | 98 (68) | 46 (32)* | 43 (73) | 16 (27)* |
| Other | 156 (57) | 116 (43) | 151 (66) | 79 (34)* |
Fewer women hospitalists were listed as first or last authors on all article types. For original research articles written by general internists, there was a trend for more women to be listed as first authors than men (261/479, 54%), but this difference was not statistically significant.
DISCUSSION
The important findings of this study are that, despite an equal gender distribution of academic HM and GIM faculty, fewer women were HM division/section chiefs, fewer women were speakers at the 2 selected national meetings, and fewer women were first or last authors of publications in 2 selected journals in comparison with general internists.
Previous studies have found that women lag behind their male counterparts with respect to academic productivity, leadership, and promotion.[1, 5, 7] Some studies suggest, however, that gender differences are reduced when younger cohorts are examined.[1, 10, 11, 12, 13] Surveys indicate that that the mean age of hospitalists is younger than most other specialties.[15, 19, 20, 24] The mean age of academic GIM physicians is unknown, but surveys of GIM (not differentiating academic from nonacademic) suggest that it is an older cohort than that of HM.[24] Despite hospitalists being a younger cohort, we found gender disparities in all areas investigated.
Our findings with respect to gender disparities in HM division or section leadership are consistent with the annual AAMC Women in US Academic Medicine and Science Benchmarking Report that found only 22% of all permanent division or section heads were women.[1]
Gender disparities with respect to authorship of medical publications have been previously noted,[3, 6, 15, 25] but to our knowledge, this is the first study to investigate the gender of authors who were hospitalists. Although we found a higher proportion of women hospitalists who were first or last authors than was observed by Jagsi and colleagues,[3] women hospitalists were still under‐represented with respect to this measure of academic productivity. Erren et al. reviewed 6 major journals from 2010 and 2011, and found that first authorship of original research by women ranged from 23.7% to 46.7%, and for last authorship from 18.3% to 28.8%.[25] Interestingly, we found no significant gender difference for first authors who were general internists, and there was a trend toward more women general internists being first authors than men for original research, reviews, and brief reports (data not shown).
Our study did not attempt to answer the question of why gender disparities persist, but many previous studies have explored this issue.[4, 8, 12, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42] Issues raised by others include the quantity of academic work (ie, publications and grants obtained), differences in hours worked and allocation of time, lack of mentorship, family responsibilities, discrimination, differences in career motivation, and levels of institutional support, to name a few.
The under‐representation of women hospitalists in leadership, authorship, and speaking opportunities may be consistent with gender‐related differences in research productivity. Fewer publications could lead to fewer national presentations, which could lead to fewer leadership opportunities. Our findings with respect to general internists are not consistent with this idea, however, as whereas women were under‐represented in GIM leadership positions, we found no disparities with respect to the gender of first authors or speakers at national meetings for general internists. The finding that hospitalists had gender disparities with respect to first authors and national speakers but general internists did not, argues against several hypotheses (ie, that women lack mentorship, have less career motivation, fewer career building opportunities).
One notable hypothesis, and perhaps one that is often discussed in the literature, is that women shoulder the majority of family responsibilities, and this may result in women having less time for their careers. Jolly and colleagues studied physician‐researchers and noted that women were more likely than men to have spouses or domestic partners who were fully employed, spent 8.5 more hours per week on domestic activities, and were more likely to take time off during disruptions of usual child care.[33] Carr and colleagues found that women with children (compared to men with children) had fewer publications, slower self‐perceived career progress, and lower career satisfaction, but having children had little effect on faculty aspirations and goals.[2] Kaplan et al., however, found that family responsibilities do not appear to account for sex differences in academic advancement.[4] Interestingly, in a study comparing physicians from Generation X to those of the Baby Boomer age, Generation X women reported working more than their male Generation X counterparts, and both had more of a focus on worklife balance than the older generation.[12]
The nature the of 2 specialties' work environment and job requirements could have also resulted in some of the differences seen. Primary care clinical work is typically conducted Monday through Friday, and hospitalist work frequently includes some weekend, evening, night, and holiday coverage. Although these are known differences, both specialties have also been noted to offer many advantages to women and men alike, including collaborative working environments and flexible work hours.[16]
Finally, finding disparity in leadership positions in both specialties supports the possibility that those responsible for hiring could have implicit gender biases. Under‐representation in entry‐level positions is also not a likely explanation for the differences we observed, because nearly an equal number of men and women graduate from medical school, pursue residency training in internal medicine, and become either academic hospitalists or general internists at university settings.[1, 15, 24] This hypothesis could, however, explain why disparities exist with respect to senior authorship and leadership positions, as typically, these individuals have been in practice longer and the current trends of improved gender equality have not always been the case.
Our study has a number of limitations. First, we only examined publications in 2 journals and presentations at 2 national conferences, although the journals and conferences selected are considered to be the major ones in the 2 specialties. Second, using Internet searches may have resulted in inaccurate gender and specialty assignment, but previous studies have used similar methodology.[3, 43] Additionally, we also attempted to contact individuals for direct confirmation when the information we obtained was not clear and had a second investigator independently verify the gender and specialty data. Third, we utilized division/department websites when available to determine the gender of HM divisions/sections. If not recently updated, these websites may not have reflected the most current leader of the unit, but this concern would seemingly pertain to both hospitalists and general internists. Fourth, we opted to only study faculty and division/section heads at university hospitals, as typically these institutions had GIM and hospitalist groups and also typically had websites. Because we only studied faculty and leadership at university hospitals, our data are not generalizable to all hospitalist and GIM groups. Finally, we excluded pediatric hospitalists, and thus, this study is representative of adult hospitalists only. Including pediatric hospitalists was out of the scope of this project.
Our study also had a number of strengths. To our knowledge, this is the first study to provide an estimate of the gender distribution in academic HM, of hospitalists as speakers at national meetings, as first and last authors, and of HM division or section heads, and is the first to compare these results with those observed for general internists. In addition, we examined 7 years of data from 2 of the major journals and national conferences for these specialties.
In summary, despite HM being a newer field with a younger cohort of physicians, we found that gender disparities exist for women with respect to authorship, national speaking opportunities, and division or section leadership. Identifying why these gender differences exist presents an important next step.
Disclosures: Nothing to report. Marisha Burden, MD and Maria G. Frank, MD are coprincipal authors.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
- Association of American Medical Colleges. Women in U.S. academic medicine and science: Statistics and benchmarking report. 2012. Available at: https://members.aamc.org/eweb/upload/Women%20in%20U%20S%20%20Academic%20Medicine%20Statistics%20and%20Benchmarking%20Report%202011-20123.pdf. Accessed September 1, 2014.
- , , , et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538.
- , , , et al. The “gender gap” in authorship of academic medical literature—a 35‐year perspective. N Engl J Med. 2006;355:281–287.
- , , , , , . Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–1289.
- . Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405.
- , , , , . Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–47.
- , , , . Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025.
- , , , . Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–212.
- , , . Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–114.
- , , , . The status of women at one academic medical center. Breaking through the glass ceiling. JAMA. 1990;264:1813–1817.
- , . Status of women in academic anesthesiology. Anesthesiology. 1986;64:496–500.
- , , . The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006;6:55.
- Pew Research Center. On pay gap, millenial women near parity—for now. December 2013. Available at: http://www.pewsocialtrends.org/files/2013/12/gender-and-work_final.pdf. Published December 11, 2013. Accessed February 5, 2015.
- , . The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27:23–27.
- . The gender factor. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/the‐gender‐factor. Published March 1, 2006. Accessed September 1, 2014.
- Association of American Medical Colleges. Analysis in brief: Supplemental information for estimating the number and characteristics of hospitalist physicians in the United States and their possible workforce implications. Available at: https://www.aamc.org/download/300686/data/aibvol12_no3-supplemental.pdf. Published August 2012. Accessed September 1, 2014.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6:5–9.
- State of Hospital Medicine: 2011 Report Based on 2010 Data. Medical Group Management Association and Society of Hospital Medicine. www.mgma.com, www.hospitalmedicine.org.
- Today's Hospitalist Survey. Compensation and Career Survey Results. 2013. Available at: http://www.todayshospitalist.com/index.php?b=salary_survey_results. Accessed January 11, 2015.
- Association of American Medical Colleges. Women in U.S. Academic Medicine: Statistics and Benchmarking Report. 2009–2010. Available at: https://www.aamc.org/download/182674/data/gwims_stats_2009‐2010.pdf. Accessed September 1, 2014.
- American Medical Association. Graduate Medical Education Directory 2012–2013. Chicago, IL: American Medical Association; 2012:182–203.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Association of American Medical Colleges. 2012 Physician Specialty Data Book. Center for Workforce Studies. Available at: https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Published November 2012. Accessed September 1, 2014.
- , , , . Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174:633–635.
- , , , et al. Relationships of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–186.
- , , , et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896.
- , , , . Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160:2625–2629.
- , , , , . A "ton of feathers": gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt). 2003;12:1009–1018.
- , , . Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135:972–977.
- , , , . Career satisfaction of US women physicians: results from the Women Physicians' Health Study. Society of General Internal Medicine Career Satisfaction Study Group. Arch Intern Med. 1999;159:1417–1426.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–315.
- , , , , , . Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344–353.
- , , , , . Stories from early‐career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–758.
- , , , . The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193–201.
- , , , , . Experiencing the culture of academic medicine: gender matters, a national study. J Gen Intern Med. 2013;28:201–207.
- . Gender pay gaps in hospital medicine. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/gender‐pay‐gaps‐in‐hospital‐medicine. Published February 29, 2012. Accessed September 1, 2014.
- , , . Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103–1115.
- . Inequality quantified: mind the gender gap. Nature. 2013;495:22–24.
- , , , et al. Gender differences in academic advancement: patterns, causes, and potential solutions in one US College of Medicine. Acad Med. 2003;78:500–508.
- , . Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med. 2001;76:453–465.
- . Gender factors in reviewer recommendations for manuscript publication. J Appl Behav Anal. 1990;23:539–543.
- , , , . Scientific impact of women in academic surgery. J Surg Res. 2008;148:13–16.
© 2015 Society of Hospital Medicine
Curbside vs Formal Consultation
A curbside consultation is an informal process whereby a consultant is asked to provide information or advice about a patient's care without doing a formal assessment of the patient.14 Curbside consultations are common in the practice of medicine2, 3, 5 and are frequently requested by physicians caring for hospitalized patients. Several surveys have documented the quantity of curbside consultations requested of various subspecialties, the types of questions asked, the time it takes to respond, and physicians' perceptions about the quality of the information exchanged.111 While curbside consultations have a number of advantages, physicians' perceptions are that the information conveyed may be inaccurate or incomplete and that the advice offered may be erroneous.13, 5, 10, 12, 13
Cartmill and White14 performed a random audit of 10% of the telephone referrals they received for neurosurgical consultation over a 1‐year period and noted discrepancies between the Glascow Coma Scores reported during the telephone referrals and those noted in the medical records, but the frequency of these discrepancies was not reported. To our knowledge, no studies have compared the quality of the information provided in curbside consultations with that obtained in formal consultations that included direct face‐to‐face patient evaluations and primary data collection, and whether the advice provided in curbside and formal consultations on the same patient differed.
We performed a prospective cohort study to compare the information received by hospitalists during curbside consultations on hospitalized patients, with that obtained from formal consultations done the same day on the same patients, by different hospitalists who were unaware of any details regarding the curbside consultation. We also compared the advice provided by the 2 hospitalists following their curbside and formal consultations. Our hypotheses were that the information received during curbside consultations was frequently inaccurate or incomplete, that the recommendations made after the formal consultation would frequently differ from those made in the curbside consultation, and that these differences would have important implications on patient care.
METHODS
This was a quality improvement study conducted at Denver Health, a 500‐bed university‐affiliated urban safety net hospital from January 10, 2011 to January 9, 2012. The study design was a prospective cohort that included all curbside consultations on hospitalized patients received between 7 AM and 3 PM, on intermittently selected weekdays, by the Internal Medicine Consultation Service that was staffed by 18 hospitalists. Data were collected intermittently based upon hospitalist availability and was done to limit potential alterations in the consulting practices of the providers requesting consultations.
Consultations were defined as being curbside when the consulting provider asked for advice, suggestions, or opinions about a patient's care but did not ask the hospitalist to see the patient.15, 15 Consultations pertaining to administrative issues (eg, whether a patient should be admitted to an intensive care bed as opposed to an acute care floor bed) or on patients who were already being followed by a hospitalist were excluded.
The hospitalist receiving the curbside consultation was allowed to ask questions as they normally would, but could not verify the accuracy of the information received (eg, could not review any portion of the patient's medical record, such as notes or lab data). A standardized data collection sheet was used to record the service and level of training of the requesting provider, the medical issue(s) of concern, all clinical data offered by the provider, the number of questions asked by the hospitalist of the provider, and whether, on the basis of the information provided, the hospitalist felt that the question(s) being asked was (were) of sufficient complexity that a formal consultation should occur. The hospitalist then offered advice based upon the information given during the curbside consultation.
After completing the curbside consultation, the hospitalist requested verbal permission from the requesting provider to perform a formal consultation. If the request was approved, the hospitalist performing the curbside consultation contacted a different hospitalist who performed the formal consultation within the next few hours. The only information given to the second hospitalist was the patient's identifiers and the clinical question(s) being asked. The formal consultation included a complete face‐to‐face history and physical examination, a review of the patient's medical record, documentation of the provider's findings, and recommendations for care.
Upon completion of the formal consultation, the hospitalists who performed the curbside and the formal consultations met to review the advice each gave to the requesting provider and the information on which this advice was based. The 2 hospitalists jointly determined the following: (a) whether the information received during the curbside consultation was correct and complete, (b) whether the advice provided in the formal consultation differed from that provided in the curbside consultation, (c) whether the advice provided in the formal consultation dealt with issues other than one(s) leading to the curbside consultation, (d) whether differences in the recommendations given in the curbside versus the formal consultation changed patient management in a meaningful way, and (e) whether the curbside consultation alone was felt to be sufficient.
Information obtained by the hospitalist performing the formal consultation that was different from, or not included in, the information recorded during the curbside consultation was considered to be incorrect or incomplete, respectively. A change in management was defined as an alteration in the direction or type of care that the patient would have received as a result of the advice being given. A pulmonary and critical care physician, with >35 years of experience in inpatient medicine, reviewed the information provided in the curbside and formal consultations, and independently assessed whether the curbside consultation alone would have been sufficient and whether the formal consultation changed management.
Curbside consultations were neither solicited nor discouraged during the course of the study. The provider requesting the curbside consultation was not informed or debriefed about the study in an attempt to avoid affecting future consultation practices from that provider or service.
Associations were sought between the frequency of inaccurate or incomplete data and the requesting service and provider, the consultative category and medical issue, the number of questions asked by the hospitalist during the curbside consultation, and whether the hospitalist doing the curbside consultation thought that formal consultation was needed. A chi‐square test was used to analyze all associations. A P value of <0.05 was considered significant. All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc, Cary, NC) software. The study was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Fifty curbside consultations were requested on a total of 215 study days. The requesting service declined formal consultation in 3 instances, leaving 47 curbside consultations that had a formal consultation. Curbside consultations came from a variety of services and providers, and addressed a variety of issues and concerns (Table 1).
| Curbside Consultations, N (%) | |
|---|---|
| 47 (100) | |
| |
| Requesting service | |
| Psychiatry | 21 (45) |
| Emergency Department | 9 (19) |
| Obstetrics/Gynecology | 5 (11) |
| Neurology | 4 (8) |
| Other (Orthopedics, Anesthesia, General Surgery, Neurosurgery, and Interventional Radiology) | 8 (17) |
| Requesting provider | |
| Resident | 25 (53) |
| Intern | 8 (17) |
| Attending | 9 (19) |
| Other | 5 (11) |
| Consultative issue* | |
| Diagnosis | 10 (21) |
| Treatment | 29 (62) |
| Evaluation | 20 (43) |
| Discharge | 13 (28) |
| Lab interpretation | 4 (9) |
| Medical concern* | |
| Cardiac | 27 (57) |
| Endocrine | 17 (36) |
| Infectious disease | 9 (19) |
| Pulmonary | 8 (17) |
| Gastroenterology | 6 (13) |
| Fluid and electrolyte | 6 (13) |
| Others | 23 (49) |
The hospitalists asked 0 to 2 questions during 8/47 (17%) of the curbside consultations, 3 to 5 questions during 26/47 (55%) consultations, and more than 5 questions during 13/47 (28%). Based on the information received during the curbside consultations, the hospitalists thought that the curbside consultations were insufficient for 18/47 (38%) of patients. In all instances, the opinions of the 2 hospitalists concurred with respect to this conclusion, and the independent reviewer agreed with this assessment in 17 of these 18 (94%).
The advice rendered in the formal consultations differed from that provided in 26/47 (55%) of the curbside consultations, and the formal consultation was thought to have changed management for 28/47 (60%) of patients (Table 2). The independent reviewer thought that the advice provided in the formal consultations changed management in 29/47 (62%) of the cases, and in 24/28 cases (86%) where the hospitalist felt that the formal consult changed management.
| Curbside Consultations, N (%) | |||
|---|---|---|---|
| Total | Accurate and Complete | Inaccurate or Incomplete | |
| 47 (100) | 23 (49) | 24 (51) | |
| |||
| Advice in formal consultation differed from advice in curbside consultation | 26 (55) | 7 (30) | 19 (79)* |
| Formal consultation changed management | 28 (60) | 6 (26) | 22 (92) |
| Minor change | 18 (64) | 6 (100) | 12 (55) |
| Major change | 10 (36) | 0 (0) | 10 (45) |
| Curbside consultation insufficient | 18 (38) | 2 (9) | 16 (67) |
Information was felt to be inaccurate or incomplete in 24/47 (51%) of the curbside consultations (13/47 inaccurate, 16/47 incomplete, 5/47 both inaccurate and incomplete), and when inaccurate or incomplete information was obtained, the advice given in the formal consultations more commonly differed from that provided in the curbside consultation (19/24, 79% vs 7/23, 30%; P < 0.001), and was more commonly felt to change management (22/24, 92% vs 6/23, 26%; P < 0.0001) (Table 2). No association was found between whether the curbside consultation contained complete or accurate information and the consulting service from which the curbside originated, the consulting provider, the consultative aspect(s) or medical issue(s) addressed, the number of questions asked by the hospitalist during the curbside consultation, nor whether the hospitalists felt that a formal consultation was needed.
DISCUSSION
The important findings of this study are that (a) the recommendations made by hospitalists in curbside versus formal consultations on the same patient frequently differ, (b) these differences frequently result in changes in clinical management, (c) the information presented in curbside consultations by providers is frequently inaccurate or incomplete, regardless of the providers specialty or seniority, (d) when inaccurate or incomplete information is received, the recommendations made in curbside and formal consultations differ more frequently, and (e) we found no way to predict whether the information provided in a curbside consultation was likely to be inaccurate or incomplete.
Our hospitalists thought that 38% of the curbside consultations they received should have had formal consultations. Manian and McKinsey7 reported that as many as 53% of questions asked of infectious disease consultants were thought to be too complex to be addressed in an informal consultation. Others, however, report that only 11%33% of curbside consultations were thought to require formal consultation.1, 9, 10, 16 Our hospitalists asked 3 or more questions of the consulting providers in more than 80% of the curbside consultations, suggesting that the curbside consultations we received might have had a higher complexity than those seen by others.
Our finding that information provided in curbside consultation was frequently inaccurate or incomplete is consistent with a number of previous studies reporting physicians' perceptions of the accuracy of curbside consultations.2, 3 Hospital medicine is not likely to be the only discipline affected by inaccurate curbside consultation practices, as surveys of specialists in infectious disease, gynecology, and neurosurgery report that practitioners in these disciplines have similar concerns.1, 10, 14 In a survey returned by 34 physicians, Myers1 found that 50% thought the information exchanged during curbside consultations was inaccurate, leading him to conclude that inaccuracies presented during curbside consultations required further study.
We found no way of predicting whether curbside consultations were likely to include inaccurate or incomplete information. This observation is consistent with the results of Bergus et al16 who found that the frequency of curbside consultations being converted to formal consultations was independent of the training status of the consulting physician, and with the data of Myers1 who found no way of predicting the likelihood that a curbside consultation should be converted to a formal consultation.
We found that formal consultations resulted in management changes more often than differences in recommendations (ie, 60% vs 55%, respectively). This small difference occurred because, on occasion, the formal consultations found issues to address other than the one(s) for which the curbside consultation was requested. In the majority of these instances, the management changes were minor and the curbside consultation was still felt to be sufficient.
In some instances, the advice given after the curbside and the formal consultations differed to only a minor extent (eg, varying recommendations for oral diabetes management). In other instances, however, the advice differed substantially (eg, change in antibiotic management in a septic patient with a multidrug resistant organism, when the original curbside question was for when to order a follow‐up chest roentgenogram for hypoxia; see Supporting Information, Appendix, in the online version of this article). In 26 patients (55%), formal consultation resulted in different medications being started or stopped, additional tests being performed, or different decisions being made about admission versus discharge.
Our study has a number of strengths. First, while a number of reports document that physicians' perceptions are that curbside consultations frequently contain errors,2, 3, 5, 12 to our knowledge this is the first study that prospectively compared the information collected and advice given in curbside versus formal consultation. Second, while this study was conducted as a quality improvement project, thereby requiring us to conclude that the results are not generalizable, the data presented were collected by 18 different hospitalists, reducing the potential of bias from an individual provider's knowledge base or practice. Third, there was excellent agreement between the independent reviewer and the 2 hospitalists who performed the curbside and formal consultations regarding whether a curbside consultation would have been sufficient, and whether the formal consultation changed patient management. Fourth, the study was conducted over a 1‐year period, which should have reduced potential bias arising from the increasing experience of residents requesting consultations as their training progressed.
Our study has several limitations. First, the number of curbside consultations we received during the study period (50 over 215 days) was lower than anticipated, and lower than the rates of consultation reported by others.1, 7, 9 This likely relates to the fact that, prior to beginning the study, Denver Health hospitalists already provided mandatory consultations for several surgical services (thereby reducing the number of curbside consultations received from these services), because curbside consultations received during evenings, nights, and weekends were not included in the study for reasons of convenience, and because we excluded all administrative curbside consultations. Our hospitalist service also provides consultative services 24 hours a day, thereby reducing the number of consultations received during daytime hours. Second, the frequency with which curbside consultations included inaccurate or incomplete information might be higher than what occurs in other hospitals, as Denver Health is an urban, university‐affiliated public hospital and the patients encountered may be more complex and trainees may be less adept at recognizing the information that would facilitate accurate curbside consultations (although we found no difference in the frequency with which inaccurate or incomplete information was provided as a function of the seniority of the requesting physician). Third, the disparity between curbside and formal consultations that we observed could have been biased by the Hawthorne effect. We attempted to address this by not providing the hospitalists who did the formal consultation with any information collected by the hospitalist involved with the curbside consultation, and by comparing the conclusions reached by the hospitalists performing the curbside and formal consultations with those of a third party reviewer. Fourth, while we found no association between the frequency of curbside consultations in which information was inaccurate or incomplete and the consulting service, there could be a selection bias of the consulting service requesting the curbside consultations as a result of the mandatory consultations already provided by our hospitalists. Finally, our study was not designed or adequately powered to determine why curbside consultations frequently have inaccurate or incomplete information.
In summary, we found that the information provided to hospitalists during a curbside consultation was often inaccurate and incomplete, and that these problems with information exchange adversely affected the accuracy of the resulting recommendations. While there are a number of advantages to curbside consultations,1, 3, 7, 10, 12, 13 our findings indicate that the risk associated with this practice is substantial.
Acknowledgements
Disclosure: Nothing to report.
- .Curbside consultation in infectious diseases: a prospective study.J Infect Dis.1984;150:797–802.
- ,,.Physicians' experiences and beliefs regarding informal consultation.JAMA.1998;280:900–904.
- ,,.Curbside consultation practices and attitudes among primary care physicians and medical subspecialists.JAMA.1998;280:905–909.
- ,,,,,.The complexity, relative value, and financial worth of curbside consultations in an academic infectious diseases unit.Clin Infect Dis.2010;51:651–655.
- ,.Curbside consultations. A closer look at a common practice.JAMA.1996;275:145–147.
- ,,,.Informal advice‐ and information‐seeking between physicians.J Med Educ.1981;56;174–180.
- ,.A prospective study of 2,092 “curbside” questions asked of two infectious disease consultants in private practice in the midwest.Clin Infect Dis.1996;22:303–307.
- ,,,,.Curbside consultation in endocrine practice: a prospective observational study.Endocrinologist.1996;6:328–331.
- ,,.Informal consultations provided to general internists by the gastroenterology department of an HMO.J Gen Intern Med.1998;13:435–438.
- .“Curbside” consultations in gynecologic oncology: a closer look at a common practice.Gynecol Oncol.1999;74:456–459.
- ,,, et al.Informal consultations in infectious diseases and clinical microbiology practice.Clin Microbiol Infect.2003;9:724–726.
- .Curbside consultations and the viaduct effect.JAMA.1998;280:929–930.
- .What do we really need to know about consultation and referral?J Gen Intern Med.1998;13:497–498.
- ,.Telephone advice for neurosurgical referrals. Who assumes duty of care?Br J Neurosurg.2001;15:453–455.
- ,.Malpractice liability for informal consultations.Fam Med.2003;35:476–481.
- ,,,.Does the structure of clinical questions affect the outcome of curbside consultations with specialty colleagues?Arch Fam Med.2000;9:541–547.
A curbside consultation is an informal process whereby a consultant is asked to provide information or advice about a patient's care without doing a formal assessment of the patient.14 Curbside consultations are common in the practice of medicine2, 3, 5 and are frequently requested by physicians caring for hospitalized patients. Several surveys have documented the quantity of curbside consultations requested of various subspecialties, the types of questions asked, the time it takes to respond, and physicians' perceptions about the quality of the information exchanged.111 While curbside consultations have a number of advantages, physicians' perceptions are that the information conveyed may be inaccurate or incomplete and that the advice offered may be erroneous.13, 5, 10, 12, 13
Cartmill and White14 performed a random audit of 10% of the telephone referrals they received for neurosurgical consultation over a 1‐year period and noted discrepancies between the Glascow Coma Scores reported during the telephone referrals and those noted in the medical records, but the frequency of these discrepancies was not reported. To our knowledge, no studies have compared the quality of the information provided in curbside consultations with that obtained in formal consultations that included direct face‐to‐face patient evaluations and primary data collection, and whether the advice provided in curbside and formal consultations on the same patient differed.
We performed a prospective cohort study to compare the information received by hospitalists during curbside consultations on hospitalized patients, with that obtained from formal consultations done the same day on the same patients, by different hospitalists who were unaware of any details regarding the curbside consultation. We also compared the advice provided by the 2 hospitalists following their curbside and formal consultations. Our hypotheses were that the information received during curbside consultations was frequently inaccurate or incomplete, that the recommendations made after the formal consultation would frequently differ from those made in the curbside consultation, and that these differences would have important implications on patient care.
METHODS
This was a quality improvement study conducted at Denver Health, a 500‐bed university‐affiliated urban safety net hospital from January 10, 2011 to January 9, 2012. The study design was a prospective cohort that included all curbside consultations on hospitalized patients received between 7 AM and 3 PM, on intermittently selected weekdays, by the Internal Medicine Consultation Service that was staffed by 18 hospitalists. Data were collected intermittently based upon hospitalist availability and was done to limit potential alterations in the consulting practices of the providers requesting consultations.
Consultations were defined as being curbside when the consulting provider asked for advice, suggestions, or opinions about a patient's care but did not ask the hospitalist to see the patient.15, 15 Consultations pertaining to administrative issues (eg, whether a patient should be admitted to an intensive care bed as opposed to an acute care floor bed) or on patients who were already being followed by a hospitalist were excluded.
The hospitalist receiving the curbside consultation was allowed to ask questions as they normally would, but could not verify the accuracy of the information received (eg, could not review any portion of the patient's medical record, such as notes or lab data). A standardized data collection sheet was used to record the service and level of training of the requesting provider, the medical issue(s) of concern, all clinical data offered by the provider, the number of questions asked by the hospitalist of the provider, and whether, on the basis of the information provided, the hospitalist felt that the question(s) being asked was (were) of sufficient complexity that a formal consultation should occur. The hospitalist then offered advice based upon the information given during the curbside consultation.
After completing the curbside consultation, the hospitalist requested verbal permission from the requesting provider to perform a formal consultation. If the request was approved, the hospitalist performing the curbside consultation contacted a different hospitalist who performed the formal consultation within the next few hours. The only information given to the second hospitalist was the patient's identifiers and the clinical question(s) being asked. The formal consultation included a complete face‐to‐face history and physical examination, a review of the patient's medical record, documentation of the provider's findings, and recommendations for care.
Upon completion of the formal consultation, the hospitalists who performed the curbside and the formal consultations met to review the advice each gave to the requesting provider and the information on which this advice was based. The 2 hospitalists jointly determined the following: (a) whether the information received during the curbside consultation was correct and complete, (b) whether the advice provided in the formal consultation differed from that provided in the curbside consultation, (c) whether the advice provided in the formal consultation dealt with issues other than one(s) leading to the curbside consultation, (d) whether differences in the recommendations given in the curbside versus the formal consultation changed patient management in a meaningful way, and (e) whether the curbside consultation alone was felt to be sufficient.
Information obtained by the hospitalist performing the formal consultation that was different from, or not included in, the information recorded during the curbside consultation was considered to be incorrect or incomplete, respectively. A change in management was defined as an alteration in the direction or type of care that the patient would have received as a result of the advice being given. A pulmonary and critical care physician, with >35 years of experience in inpatient medicine, reviewed the information provided in the curbside and formal consultations, and independently assessed whether the curbside consultation alone would have been sufficient and whether the formal consultation changed management.
Curbside consultations were neither solicited nor discouraged during the course of the study. The provider requesting the curbside consultation was not informed or debriefed about the study in an attempt to avoid affecting future consultation practices from that provider or service.
Associations were sought between the frequency of inaccurate or incomplete data and the requesting service and provider, the consultative category and medical issue, the number of questions asked by the hospitalist during the curbside consultation, and whether the hospitalist doing the curbside consultation thought that formal consultation was needed. A chi‐square test was used to analyze all associations. A P value of <0.05 was considered significant. All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc, Cary, NC) software. The study was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Fifty curbside consultations were requested on a total of 215 study days. The requesting service declined formal consultation in 3 instances, leaving 47 curbside consultations that had a formal consultation. Curbside consultations came from a variety of services and providers, and addressed a variety of issues and concerns (Table 1).
| Curbside Consultations, N (%) | |
|---|---|
| 47 (100) | |
| |
| Requesting service | |
| Psychiatry | 21 (45) |
| Emergency Department | 9 (19) |
| Obstetrics/Gynecology | 5 (11) |
| Neurology | 4 (8) |
| Other (Orthopedics, Anesthesia, General Surgery, Neurosurgery, and Interventional Radiology) | 8 (17) |
| Requesting provider | |
| Resident | 25 (53) |
| Intern | 8 (17) |
| Attending | 9 (19) |
| Other | 5 (11) |
| Consultative issue* | |
| Diagnosis | 10 (21) |
| Treatment | 29 (62) |
| Evaluation | 20 (43) |
| Discharge | 13 (28) |
| Lab interpretation | 4 (9) |
| Medical concern* | |
| Cardiac | 27 (57) |
| Endocrine | 17 (36) |
| Infectious disease | 9 (19) |
| Pulmonary | 8 (17) |
| Gastroenterology | 6 (13) |
| Fluid and electrolyte | 6 (13) |
| Others | 23 (49) |
The hospitalists asked 0 to 2 questions during 8/47 (17%) of the curbside consultations, 3 to 5 questions during 26/47 (55%) consultations, and more than 5 questions during 13/47 (28%). Based on the information received during the curbside consultations, the hospitalists thought that the curbside consultations were insufficient for 18/47 (38%) of patients. In all instances, the opinions of the 2 hospitalists concurred with respect to this conclusion, and the independent reviewer agreed with this assessment in 17 of these 18 (94%).
The advice rendered in the formal consultations differed from that provided in 26/47 (55%) of the curbside consultations, and the formal consultation was thought to have changed management for 28/47 (60%) of patients (Table 2). The independent reviewer thought that the advice provided in the formal consultations changed management in 29/47 (62%) of the cases, and in 24/28 cases (86%) where the hospitalist felt that the formal consult changed management.
| Curbside Consultations, N (%) | |||
|---|---|---|---|
| Total | Accurate and Complete | Inaccurate or Incomplete | |
| 47 (100) | 23 (49) | 24 (51) | |
| |||
| Advice in formal consultation differed from advice in curbside consultation | 26 (55) | 7 (30) | 19 (79)* |
| Formal consultation changed management | 28 (60) | 6 (26) | 22 (92) |
| Minor change | 18 (64) | 6 (100) | 12 (55) |
| Major change | 10 (36) | 0 (0) | 10 (45) |
| Curbside consultation insufficient | 18 (38) | 2 (9) | 16 (67) |
Information was felt to be inaccurate or incomplete in 24/47 (51%) of the curbside consultations (13/47 inaccurate, 16/47 incomplete, 5/47 both inaccurate and incomplete), and when inaccurate or incomplete information was obtained, the advice given in the formal consultations more commonly differed from that provided in the curbside consultation (19/24, 79% vs 7/23, 30%; P < 0.001), and was more commonly felt to change management (22/24, 92% vs 6/23, 26%; P < 0.0001) (Table 2). No association was found between whether the curbside consultation contained complete or accurate information and the consulting service from which the curbside originated, the consulting provider, the consultative aspect(s) or medical issue(s) addressed, the number of questions asked by the hospitalist during the curbside consultation, nor whether the hospitalists felt that a formal consultation was needed.
DISCUSSION
The important findings of this study are that (a) the recommendations made by hospitalists in curbside versus formal consultations on the same patient frequently differ, (b) these differences frequently result in changes in clinical management, (c) the information presented in curbside consultations by providers is frequently inaccurate or incomplete, regardless of the providers specialty or seniority, (d) when inaccurate or incomplete information is received, the recommendations made in curbside and formal consultations differ more frequently, and (e) we found no way to predict whether the information provided in a curbside consultation was likely to be inaccurate or incomplete.
Our hospitalists thought that 38% of the curbside consultations they received should have had formal consultations. Manian and McKinsey7 reported that as many as 53% of questions asked of infectious disease consultants were thought to be too complex to be addressed in an informal consultation. Others, however, report that only 11%33% of curbside consultations were thought to require formal consultation.1, 9, 10, 16 Our hospitalists asked 3 or more questions of the consulting providers in more than 80% of the curbside consultations, suggesting that the curbside consultations we received might have had a higher complexity than those seen by others.
Our finding that information provided in curbside consultation was frequently inaccurate or incomplete is consistent with a number of previous studies reporting physicians' perceptions of the accuracy of curbside consultations.2, 3 Hospital medicine is not likely to be the only discipline affected by inaccurate curbside consultation practices, as surveys of specialists in infectious disease, gynecology, and neurosurgery report that practitioners in these disciplines have similar concerns.1, 10, 14 In a survey returned by 34 physicians, Myers1 found that 50% thought the information exchanged during curbside consultations was inaccurate, leading him to conclude that inaccuracies presented during curbside consultations required further study.
We found no way of predicting whether curbside consultations were likely to include inaccurate or incomplete information. This observation is consistent with the results of Bergus et al16 who found that the frequency of curbside consultations being converted to formal consultations was independent of the training status of the consulting physician, and with the data of Myers1 who found no way of predicting the likelihood that a curbside consultation should be converted to a formal consultation.
We found that formal consultations resulted in management changes more often than differences in recommendations (ie, 60% vs 55%, respectively). This small difference occurred because, on occasion, the formal consultations found issues to address other than the one(s) for which the curbside consultation was requested. In the majority of these instances, the management changes were minor and the curbside consultation was still felt to be sufficient.
In some instances, the advice given after the curbside and the formal consultations differed to only a minor extent (eg, varying recommendations for oral diabetes management). In other instances, however, the advice differed substantially (eg, change in antibiotic management in a septic patient with a multidrug resistant organism, when the original curbside question was for when to order a follow‐up chest roentgenogram for hypoxia; see Supporting Information, Appendix, in the online version of this article). In 26 patients (55%), formal consultation resulted in different medications being started or stopped, additional tests being performed, or different decisions being made about admission versus discharge.
Our study has a number of strengths. First, while a number of reports document that physicians' perceptions are that curbside consultations frequently contain errors,2, 3, 5, 12 to our knowledge this is the first study that prospectively compared the information collected and advice given in curbside versus formal consultation. Second, while this study was conducted as a quality improvement project, thereby requiring us to conclude that the results are not generalizable, the data presented were collected by 18 different hospitalists, reducing the potential of bias from an individual provider's knowledge base or practice. Third, there was excellent agreement between the independent reviewer and the 2 hospitalists who performed the curbside and formal consultations regarding whether a curbside consultation would have been sufficient, and whether the formal consultation changed patient management. Fourth, the study was conducted over a 1‐year period, which should have reduced potential bias arising from the increasing experience of residents requesting consultations as their training progressed.
Our study has several limitations. First, the number of curbside consultations we received during the study period (50 over 215 days) was lower than anticipated, and lower than the rates of consultation reported by others.1, 7, 9 This likely relates to the fact that, prior to beginning the study, Denver Health hospitalists already provided mandatory consultations for several surgical services (thereby reducing the number of curbside consultations received from these services), because curbside consultations received during evenings, nights, and weekends were not included in the study for reasons of convenience, and because we excluded all administrative curbside consultations. Our hospitalist service also provides consultative services 24 hours a day, thereby reducing the number of consultations received during daytime hours. Second, the frequency with which curbside consultations included inaccurate or incomplete information might be higher than what occurs in other hospitals, as Denver Health is an urban, university‐affiliated public hospital and the patients encountered may be more complex and trainees may be less adept at recognizing the information that would facilitate accurate curbside consultations (although we found no difference in the frequency with which inaccurate or incomplete information was provided as a function of the seniority of the requesting physician). Third, the disparity between curbside and formal consultations that we observed could have been biased by the Hawthorne effect. We attempted to address this by not providing the hospitalists who did the formal consultation with any information collected by the hospitalist involved with the curbside consultation, and by comparing the conclusions reached by the hospitalists performing the curbside and formal consultations with those of a third party reviewer. Fourth, while we found no association between the frequency of curbside consultations in which information was inaccurate or incomplete and the consulting service, there could be a selection bias of the consulting service requesting the curbside consultations as a result of the mandatory consultations already provided by our hospitalists. Finally, our study was not designed or adequately powered to determine why curbside consultations frequently have inaccurate or incomplete information.
In summary, we found that the information provided to hospitalists during a curbside consultation was often inaccurate and incomplete, and that these problems with information exchange adversely affected the accuracy of the resulting recommendations. While there are a number of advantages to curbside consultations,1, 3, 7, 10, 12, 13 our findings indicate that the risk associated with this practice is substantial.
Acknowledgements
Disclosure: Nothing to report.
A curbside consultation is an informal process whereby a consultant is asked to provide information or advice about a patient's care without doing a formal assessment of the patient.14 Curbside consultations are common in the practice of medicine2, 3, 5 and are frequently requested by physicians caring for hospitalized patients. Several surveys have documented the quantity of curbside consultations requested of various subspecialties, the types of questions asked, the time it takes to respond, and physicians' perceptions about the quality of the information exchanged.111 While curbside consultations have a number of advantages, physicians' perceptions are that the information conveyed may be inaccurate or incomplete and that the advice offered may be erroneous.13, 5, 10, 12, 13
Cartmill and White14 performed a random audit of 10% of the telephone referrals they received for neurosurgical consultation over a 1‐year period and noted discrepancies between the Glascow Coma Scores reported during the telephone referrals and those noted in the medical records, but the frequency of these discrepancies was not reported. To our knowledge, no studies have compared the quality of the information provided in curbside consultations with that obtained in formal consultations that included direct face‐to‐face patient evaluations and primary data collection, and whether the advice provided in curbside and formal consultations on the same patient differed.
We performed a prospective cohort study to compare the information received by hospitalists during curbside consultations on hospitalized patients, with that obtained from formal consultations done the same day on the same patients, by different hospitalists who were unaware of any details regarding the curbside consultation. We also compared the advice provided by the 2 hospitalists following their curbside and formal consultations. Our hypotheses were that the information received during curbside consultations was frequently inaccurate or incomplete, that the recommendations made after the formal consultation would frequently differ from those made in the curbside consultation, and that these differences would have important implications on patient care.
METHODS
This was a quality improvement study conducted at Denver Health, a 500‐bed university‐affiliated urban safety net hospital from January 10, 2011 to January 9, 2012. The study design was a prospective cohort that included all curbside consultations on hospitalized patients received between 7 AM and 3 PM, on intermittently selected weekdays, by the Internal Medicine Consultation Service that was staffed by 18 hospitalists. Data were collected intermittently based upon hospitalist availability and was done to limit potential alterations in the consulting practices of the providers requesting consultations.
Consultations were defined as being curbside when the consulting provider asked for advice, suggestions, or opinions about a patient's care but did not ask the hospitalist to see the patient.15, 15 Consultations pertaining to administrative issues (eg, whether a patient should be admitted to an intensive care bed as opposed to an acute care floor bed) or on patients who were already being followed by a hospitalist were excluded.
The hospitalist receiving the curbside consultation was allowed to ask questions as they normally would, but could not verify the accuracy of the information received (eg, could not review any portion of the patient's medical record, such as notes or lab data). A standardized data collection sheet was used to record the service and level of training of the requesting provider, the medical issue(s) of concern, all clinical data offered by the provider, the number of questions asked by the hospitalist of the provider, and whether, on the basis of the information provided, the hospitalist felt that the question(s) being asked was (were) of sufficient complexity that a formal consultation should occur. The hospitalist then offered advice based upon the information given during the curbside consultation.
After completing the curbside consultation, the hospitalist requested verbal permission from the requesting provider to perform a formal consultation. If the request was approved, the hospitalist performing the curbside consultation contacted a different hospitalist who performed the formal consultation within the next few hours. The only information given to the second hospitalist was the patient's identifiers and the clinical question(s) being asked. The formal consultation included a complete face‐to‐face history and physical examination, a review of the patient's medical record, documentation of the provider's findings, and recommendations for care.
Upon completion of the formal consultation, the hospitalists who performed the curbside and the formal consultations met to review the advice each gave to the requesting provider and the information on which this advice was based. The 2 hospitalists jointly determined the following: (a) whether the information received during the curbside consultation was correct and complete, (b) whether the advice provided in the formal consultation differed from that provided in the curbside consultation, (c) whether the advice provided in the formal consultation dealt with issues other than one(s) leading to the curbside consultation, (d) whether differences in the recommendations given in the curbside versus the formal consultation changed patient management in a meaningful way, and (e) whether the curbside consultation alone was felt to be sufficient.
Information obtained by the hospitalist performing the formal consultation that was different from, or not included in, the information recorded during the curbside consultation was considered to be incorrect or incomplete, respectively. A change in management was defined as an alteration in the direction or type of care that the patient would have received as a result of the advice being given. A pulmonary and critical care physician, with >35 years of experience in inpatient medicine, reviewed the information provided in the curbside and formal consultations, and independently assessed whether the curbside consultation alone would have been sufficient and whether the formal consultation changed management.
Curbside consultations were neither solicited nor discouraged during the course of the study. The provider requesting the curbside consultation was not informed or debriefed about the study in an attempt to avoid affecting future consultation practices from that provider or service.
Associations were sought between the frequency of inaccurate or incomplete data and the requesting service and provider, the consultative category and medical issue, the number of questions asked by the hospitalist during the curbside consultation, and whether the hospitalist doing the curbside consultation thought that formal consultation was needed. A chi‐square test was used to analyze all associations. A P value of <0.05 was considered significant. All analyses were performed using SAS Enterprise Guide 4.3 (SAS Institute, Inc, Cary, NC) software. The study was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Fifty curbside consultations were requested on a total of 215 study days. The requesting service declined formal consultation in 3 instances, leaving 47 curbside consultations that had a formal consultation. Curbside consultations came from a variety of services and providers, and addressed a variety of issues and concerns (Table 1).
| Curbside Consultations, N (%) | |
|---|---|
| 47 (100) | |
| |
| Requesting service | |
| Psychiatry | 21 (45) |
| Emergency Department | 9 (19) |
| Obstetrics/Gynecology | 5 (11) |
| Neurology | 4 (8) |
| Other (Orthopedics, Anesthesia, General Surgery, Neurosurgery, and Interventional Radiology) | 8 (17) |
| Requesting provider | |
| Resident | 25 (53) |
| Intern | 8 (17) |
| Attending | 9 (19) |
| Other | 5 (11) |
| Consultative issue* | |
| Diagnosis | 10 (21) |
| Treatment | 29 (62) |
| Evaluation | 20 (43) |
| Discharge | 13 (28) |
| Lab interpretation | 4 (9) |
| Medical concern* | |
| Cardiac | 27 (57) |
| Endocrine | 17 (36) |
| Infectious disease | 9 (19) |
| Pulmonary | 8 (17) |
| Gastroenterology | 6 (13) |
| Fluid and electrolyte | 6 (13) |
| Others | 23 (49) |
The hospitalists asked 0 to 2 questions during 8/47 (17%) of the curbside consultations, 3 to 5 questions during 26/47 (55%) consultations, and more than 5 questions during 13/47 (28%). Based on the information received during the curbside consultations, the hospitalists thought that the curbside consultations were insufficient for 18/47 (38%) of patients. In all instances, the opinions of the 2 hospitalists concurred with respect to this conclusion, and the independent reviewer agreed with this assessment in 17 of these 18 (94%).
The advice rendered in the formal consultations differed from that provided in 26/47 (55%) of the curbside consultations, and the formal consultation was thought to have changed management for 28/47 (60%) of patients (Table 2). The independent reviewer thought that the advice provided in the formal consultations changed management in 29/47 (62%) of the cases, and in 24/28 cases (86%) where the hospitalist felt that the formal consult changed management.
| Curbside Consultations, N (%) | |||
|---|---|---|---|
| Total | Accurate and Complete | Inaccurate or Incomplete | |
| 47 (100) | 23 (49) | 24 (51) | |
| |||
| Advice in formal consultation differed from advice in curbside consultation | 26 (55) | 7 (30) | 19 (79)* |
| Formal consultation changed management | 28 (60) | 6 (26) | 22 (92) |
| Minor change | 18 (64) | 6 (100) | 12 (55) |
| Major change | 10 (36) | 0 (0) | 10 (45) |
| Curbside consultation insufficient | 18 (38) | 2 (9) | 16 (67) |
Information was felt to be inaccurate or incomplete in 24/47 (51%) of the curbside consultations (13/47 inaccurate, 16/47 incomplete, 5/47 both inaccurate and incomplete), and when inaccurate or incomplete information was obtained, the advice given in the formal consultations more commonly differed from that provided in the curbside consultation (19/24, 79% vs 7/23, 30%; P < 0.001), and was more commonly felt to change management (22/24, 92% vs 6/23, 26%; P < 0.0001) (Table 2). No association was found between whether the curbside consultation contained complete or accurate information and the consulting service from which the curbside originated, the consulting provider, the consultative aspect(s) or medical issue(s) addressed, the number of questions asked by the hospitalist during the curbside consultation, nor whether the hospitalists felt that a formal consultation was needed.
DISCUSSION
The important findings of this study are that (a) the recommendations made by hospitalists in curbside versus formal consultations on the same patient frequently differ, (b) these differences frequently result in changes in clinical management, (c) the information presented in curbside consultations by providers is frequently inaccurate or incomplete, regardless of the providers specialty or seniority, (d) when inaccurate or incomplete information is received, the recommendations made in curbside and formal consultations differ more frequently, and (e) we found no way to predict whether the information provided in a curbside consultation was likely to be inaccurate or incomplete.
Our hospitalists thought that 38% of the curbside consultations they received should have had formal consultations. Manian and McKinsey7 reported that as many as 53% of questions asked of infectious disease consultants were thought to be too complex to be addressed in an informal consultation. Others, however, report that only 11%33% of curbside consultations were thought to require formal consultation.1, 9, 10, 16 Our hospitalists asked 3 or more questions of the consulting providers in more than 80% of the curbside consultations, suggesting that the curbside consultations we received might have had a higher complexity than those seen by others.
Our finding that information provided in curbside consultation was frequently inaccurate or incomplete is consistent with a number of previous studies reporting physicians' perceptions of the accuracy of curbside consultations.2, 3 Hospital medicine is not likely to be the only discipline affected by inaccurate curbside consultation practices, as surveys of specialists in infectious disease, gynecology, and neurosurgery report that practitioners in these disciplines have similar concerns.1, 10, 14 In a survey returned by 34 physicians, Myers1 found that 50% thought the information exchanged during curbside consultations was inaccurate, leading him to conclude that inaccuracies presented during curbside consultations required further study.
We found no way of predicting whether curbside consultations were likely to include inaccurate or incomplete information. This observation is consistent with the results of Bergus et al16 who found that the frequency of curbside consultations being converted to formal consultations was independent of the training status of the consulting physician, and with the data of Myers1 who found no way of predicting the likelihood that a curbside consultation should be converted to a formal consultation.
We found that formal consultations resulted in management changes more often than differences in recommendations (ie, 60% vs 55%, respectively). This small difference occurred because, on occasion, the formal consultations found issues to address other than the one(s) for which the curbside consultation was requested. In the majority of these instances, the management changes were minor and the curbside consultation was still felt to be sufficient.
In some instances, the advice given after the curbside and the formal consultations differed to only a minor extent (eg, varying recommendations for oral diabetes management). In other instances, however, the advice differed substantially (eg, change in antibiotic management in a septic patient with a multidrug resistant organism, when the original curbside question was for when to order a follow‐up chest roentgenogram for hypoxia; see Supporting Information, Appendix, in the online version of this article). In 26 patients (55%), formal consultation resulted in different medications being started or stopped, additional tests being performed, or different decisions being made about admission versus discharge.
Our study has a number of strengths. First, while a number of reports document that physicians' perceptions are that curbside consultations frequently contain errors,2, 3, 5, 12 to our knowledge this is the first study that prospectively compared the information collected and advice given in curbside versus formal consultation. Second, while this study was conducted as a quality improvement project, thereby requiring us to conclude that the results are not generalizable, the data presented were collected by 18 different hospitalists, reducing the potential of bias from an individual provider's knowledge base or practice. Third, there was excellent agreement between the independent reviewer and the 2 hospitalists who performed the curbside and formal consultations regarding whether a curbside consultation would have been sufficient, and whether the formal consultation changed patient management. Fourth, the study was conducted over a 1‐year period, which should have reduced potential bias arising from the increasing experience of residents requesting consultations as their training progressed.
Our study has several limitations. First, the number of curbside consultations we received during the study period (50 over 215 days) was lower than anticipated, and lower than the rates of consultation reported by others.1, 7, 9 This likely relates to the fact that, prior to beginning the study, Denver Health hospitalists already provided mandatory consultations for several surgical services (thereby reducing the number of curbside consultations received from these services), because curbside consultations received during evenings, nights, and weekends were not included in the study for reasons of convenience, and because we excluded all administrative curbside consultations. Our hospitalist service also provides consultative services 24 hours a day, thereby reducing the number of consultations received during daytime hours. Second, the frequency with which curbside consultations included inaccurate or incomplete information might be higher than what occurs in other hospitals, as Denver Health is an urban, university‐affiliated public hospital and the patients encountered may be more complex and trainees may be less adept at recognizing the information that would facilitate accurate curbside consultations (although we found no difference in the frequency with which inaccurate or incomplete information was provided as a function of the seniority of the requesting physician). Third, the disparity between curbside and formal consultations that we observed could have been biased by the Hawthorne effect. We attempted to address this by not providing the hospitalists who did the formal consultation with any information collected by the hospitalist involved with the curbside consultation, and by comparing the conclusions reached by the hospitalists performing the curbside and formal consultations with those of a third party reviewer. Fourth, while we found no association between the frequency of curbside consultations in which information was inaccurate or incomplete and the consulting service, there could be a selection bias of the consulting service requesting the curbside consultations as a result of the mandatory consultations already provided by our hospitalists. Finally, our study was not designed or adequately powered to determine why curbside consultations frequently have inaccurate or incomplete information.
In summary, we found that the information provided to hospitalists during a curbside consultation was often inaccurate and incomplete, and that these problems with information exchange adversely affected the accuracy of the resulting recommendations. While there are a number of advantages to curbside consultations,1, 3, 7, 10, 12, 13 our findings indicate that the risk associated with this practice is substantial.
Acknowledgements
Disclosure: Nothing to report.
- .Curbside consultation in infectious diseases: a prospective study.J Infect Dis.1984;150:797–802.
- ,,.Physicians' experiences and beliefs regarding informal consultation.JAMA.1998;280:900–904.
- ,,.Curbside consultation practices and attitudes among primary care physicians and medical subspecialists.JAMA.1998;280:905–909.
- ,,,,,.The complexity, relative value, and financial worth of curbside consultations in an academic infectious diseases unit.Clin Infect Dis.2010;51:651–655.
- ,.Curbside consultations. A closer look at a common practice.JAMA.1996;275:145–147.
- ,,,.Informal advice‐ and information‐seeking between physicians.J Med Educ.1981;56;174–180.
- ,.A prospective study of 2,092 “curbside” questions asked of two infectious disease consultants in private practice in the midwest.Clin Infect Dis.1996;22:303–307.
- ,,,,.Curbside consultation in endocrine practice: a prospective observational study.Endocrinologist.1996;6:328–331.
- ,,.Informal consultations provided to general internists by the gastroenterology department of an HMO.J Gen Intern Med.1998;13:435–438.
- .“Curbside” consultations in gynecologic oncology: a closer look at a common practice.Gynecol Oncol.1999;74:456–459.
- ,,, et al.Informal consultations in infectious diseases and clinical microbiology practice.Clin Microbiol Infect.2003;9:724–726.
- .Curbside consultations and the viaduct effect.JAMA.1998;280:929–930.
- .What do we really need to know about consultation and referral?J Gen Intern Med.1998;13:497–498.
- ,.Telephone advice for neurosurgical referrals. Who assumes duty of care?Br J Neurosurg.2001;15:453–455.
- ,.Malpractice liability for informal consultations.Fam Med.2003;35:476–481.
- ,,,.Does the structure of clinical questions affect the outcome of curbside consultations with specialty colleagues?Arch Fam Med.2000;9:541–547.
- .Curbside consultation in infectious diseases: a prospective study.J Infect Dis.1984;150:797–802.
- ,,.Physicians' experiences and beliefs regarding informal consultation.JAMA.1998;280:900–904.
- ,,.Curbside consultation practices and attitudes among primary care physicians and medical subspecialists.JAMA.1998;280:905–909.
- ,,,,,.The complexity, relative value, and financial worth of curbside consultations in an academic infectious diseases unit.Clin Infect Dis.2010;51:651–655.
- ,.Curbside consultations. A closer look at a common practice.JAMA.1996;275:145–147.
- ,,,.Informal advice‐ and information‐seeking between physicians.J Med Educ.1981;56;174–180.
- ,.A prospective study of 2,092 “curbside” questions asked of two infectious disease consultants in private practice in the midwest.Clin Infect Dis.1996;22:303–307.
- ,,,,.Curbside consultation in endocrine practice: a prospective observational study.Endocrinologist.1996;6:328–331.
- ,,.Informal consultations provided to general internists by the gastroenterology department of an HMO.J Gen Intern Med.1998;13:435–438.
- .“Curbside” consultations in gynecologic oncology: a closer look at a common practice.Gynecol Oncol.1999;74:456–459.
- ,,, et al.Informal consultations in infectious diseases and clinical microbiology practice.Clin Microbiol Infect.2003;9:724–726.
- .Curbside consultations and the viaduct effect.JAMA.1998;280:929–930.
- .What do we really need to know about consultation and referral?J Gen Intern Med.1998;13:497–498.
- ,.Telephone advice for neurosurgical referrals. Who assumes duty of care?Br J Neurosurg.2001;15:453–455.
- ,.Malpractice liability for informal consultations.Fam Med.2003;35:476–481.
- ,,,.Does the structure of clinical questions affect the outcome of curbside consultations with specialty colleagues?Arch Fam Med.2000;9:541–547.
Copyright © 2012 Society of Hospital Medicine
Hospitalist‐Led Medicine ED Team
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
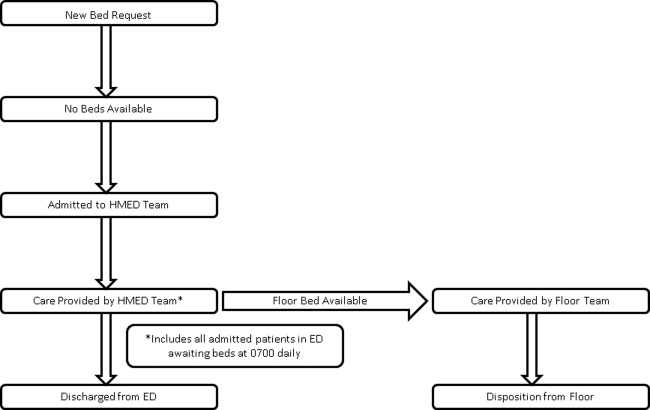
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
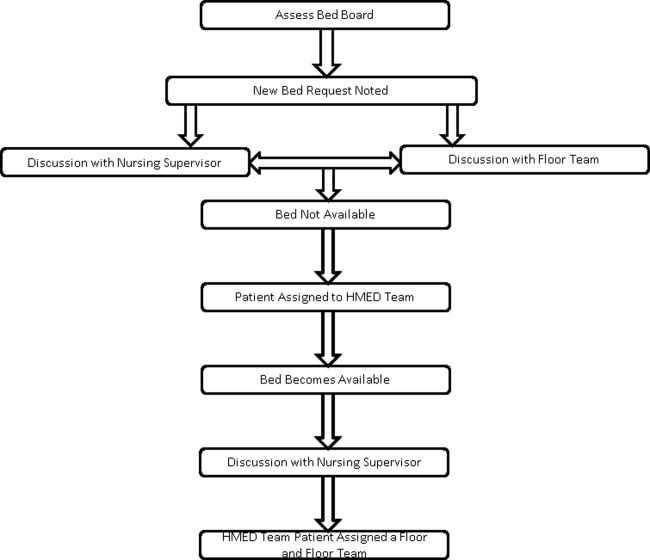
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
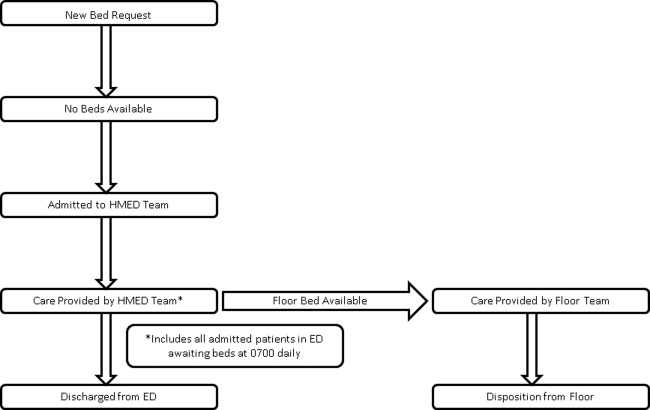
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
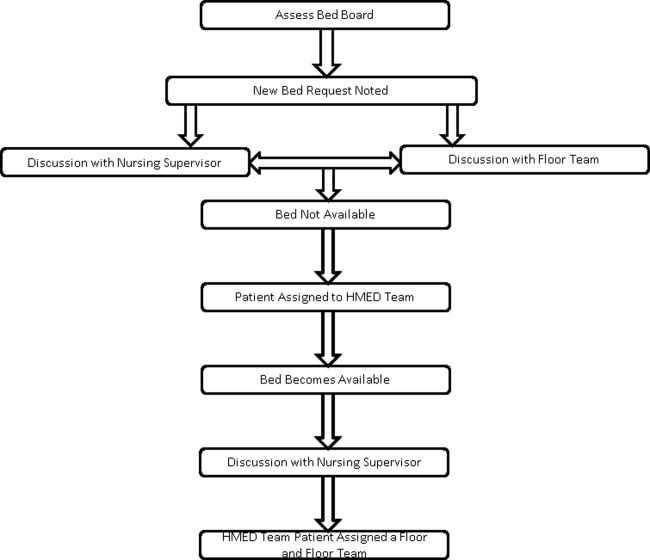
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
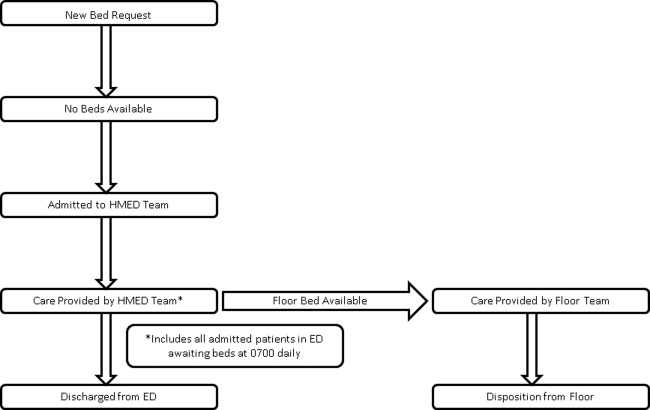
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
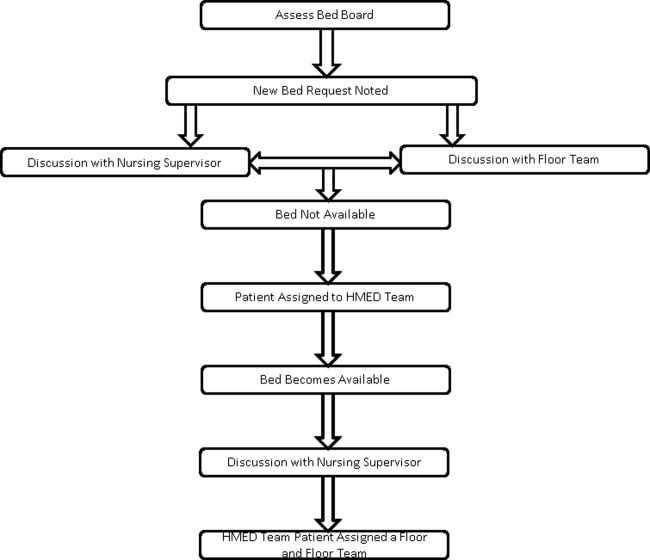
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Copyright © 2012 Society of Hospital Medicine
Evolving Practice of Hospital Medicine
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P < 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P < 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P < 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P < 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P < 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P < 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.