User login
Traditional Chinese medicine improves outcomes in HFrEF
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
FROM ESC CONGRESS 2023
Wegovy scores HFpEF benefits in people with obesity
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMSTERDAM – Adults with heart failure with preserved ejection fraction (HFpEF) but without diabetes showed significant improvements in their heart failure-related symptoms and physical limitations, exercise function, and weight loss when treated with a weight-reducing dose of semaglutide for 52 weeks, compared with placebo, in the randomized STEP-HFpEF trial.
The results, which also showed the treatment’s safety in these patients, “indicate that treatment with semaglutide is a valuable therapeutic approach in the management of patients with HFpEF and obesity,” Mikhail Kosiborod, MD, said at the annual congress of the European Society of Cardiology.
The findings establish semaglutide, a glucagonlike peptide–1 (GLP-1) receptor agonist, as a second class of medication with proven efficacy and safety for people with HFpEF, joining two agents also proven beneficial for people with HFpEF, dapagliflozin (Farxiga) and empagliflozin (Jardiance), both from the class of sodium-glucose cotransporter 2 (SGLT2) inhibitors.
When administered at the approved dose for weight loss of 2.4 mg, injected subcutaneously weekly for 52 weeks, semaglutide (Wegovy) produced an average 7.8-point incremental improvement in patients’ scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated measure of symptoms and functional limitations, compared with controls who received placebo injections, as well as an average incremental weight loss from baseline, compared with placebo, of 10.7%. Both were significant effects, compared with placebo, and clinically meaningful benefits for the study’s two primary endpoints.
Simultaneously with Kosiborod’s report the results also appeared in a report posted online in the New England Journal of Medicine.
A ‘paradigm shift’ for medical weight loss in cardiology
The findings from this study with 529 randomized patients immediately propelled the weight loss formulation of semaglutide into the ranks of agents used to treat and prevent cardiovascular disease events. This evolution in the indications for semaglutide will be driven not only by the STEP-HFpEF results but also by findings from the SELECT trial, which tested the same semaglutide weight-loss dose in people with obesity, established cardiovascular disease, and had positive top-line results for prevention of major cardiovascular adverse events, according to a press release from Novo Nordisk on Aug. 8.
The STEP-HFpEF and SELECT results will trigger “a paradigm shift” for cardiologists, who will now need to consider prescribing a weight-loss medication to many of their patients, agents that until now were not part of the usual pharmacologic toolbox for cardiologists, said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. This shift will require education to bring the clinical cardiology community on board, he added in an interview.
Given that semaglutide administered at this dose already has a Food and Drug Administration–approved indication for weight loss in people with obesity or overweight plus at least one comorbidity, clinicians could immediately start using the treatment in people with obesity and HFpEF, said Dr. Kosiborod and other cardiologists.
Weekly semaglutide injections “could be considered a treatment option right now” for people with obesity and HFpEF, Dr. Kosiborod said during a press briefing.
Other experts agreed, especially because the STEP-HFpEF results confirmed that weight loss treatment with semaglutide was safe in this population.
‘A terrific win for patients’
The new findings are “a terrific win and game changer for patients with HFpEF,” commented Gregg C. Fonarow, MD, professor and cochief of cardiology at the University of California, Los Angeles, who was not involved with the study.
“The magnitude of improvement in the patient-reported health status scores are large and impressive. These data support clinical use of this agent for individuals with HFpEF with a body mass index of 30 kg/m2, patients who already fall within existing indications,” Dr. Fonarow said in an interview.
“Given the improvements in clinical outcomes in the STEP-HFpEF and SELECT trials, cardiologists should be prescribing these medications to eligible patients without conditions,” he added. “The perception of [semaglutide] needs to shift and be viewed as a component of the comprehensive medical therapies provided to individuals with established cardiovascular disease or HFpEF who also have elevated body mass index to improve their clinical outcomes.”
Historically, cardiologists have had a concern that weight loss was potentially harmful in people with heart failure and that obesity was protective, a phenomenon known as the “obesity paradox,” but the STEP-HFpEF data help disprove that notion, commented Nancy K. Sweitzer, MD, PhD, a heart failure specialist and vice chair of clinical research in the department of medicine at Washington University in St. Louis, who also was not involved in the study.
No signal of an obesity paradox
“There’s been a concern in the heart failure community to use weight-loss strategies in people with heart failure because of this, but this evidence provides a lot of confidence that it’s safe to use this weight loss treatment. The results show that patients feel better and lose weight with no signal of harm,” Dr. Sweitzer said in an interview.
The “encouraging findings” for semaglutide in patients with HFpEF “potentially add a much needed extra option for these patients and provide another upstream treatment for patients with signs of this condition plus a high body mass index,” commented Yigal M. Pinto, MD, PhD, in an editorial that accompanied the published report.
“How these findings translate to hard end points remains to be established and will be important in determining the role of GLP-1 agonism,” wrote Dr. Pinto, a professor and heart failure specialist at Amsterdam University Medical Center.
But Dr. Kosiborod said that the improvement seen in the KCCQ score was itself an important benefit for patients. “Heart failure is defined clinically based on symptoms,” he noted, and results in prior studies documented that patients value improvements in symptoms and physical limitations even more than they value “hard endpoints” such as survival.
The new findings, which indicate that two different and expensive classes of medications are now standard of care for many people with HFpEF and obesity – the SGLT2 inhibitors and the GLP-1 receptor agonist semaglutide – also raise concerns over patient access and affordability, as many U.S. insurers have a history of requiring prior authorization, high copays, or coverage denials for these two medical classes.
But Dr. Sweitzer and Dr. Kosiborod both said that the insurance-coverage climate seems, in just the past couple of years or so, to have dramatically improved, although it’s still not ideal.
Prior authorization hoops have decreased
“We still have prior-authorization hoops to jump through, but I expect these will continue to decrease over time as evidence for clinical benefits [from weight loss] continues to accumulate,” said Dr. Sweitzer.
And “the SELECT data mean that cardiologists will need to become comfortable prescribing GLP-1 receptor agonists,” she added.
“It’s not okay for insurers to say we are not going to cover weight loss medications because it’s a cosmetic indication,” said Dr. Kosiborod. “Obesity appears to be very important in the pathogenesis and progression of heart failure, and if patients derive substantial benefit, they should have access to this treatment.”
The improvements in KCCQ score, as well as in several secondary and exploratory endpoints including a significant reduction in C-reactive protein (an indication of a potent anti-inflammatory effect), an average 20 m increase in 6-minute walk distance, a significant average drop in N-terminal pro-brain natriuretic peptide, and a drop in heart failure hospitalizations or urgent heart failure visits (although the trial was not powered to show differences in clinical events), “were the largest benefits in these outcomes we’ve seen,” compared with any other medical intervention in people with HFpEF, he noted.
“About 80% of U.S. patients with HFpEF have obesity or overweight,” Dr. Kosiborod noted. Using semaglutide on these patients “is an issue of access and insurance coverage. My hope is that these and other data will favorably change this.”
A related trial with a similar design, STEP-HFpEF DM, is still in progress and testing the same semaglutide treatment in adults with HFpEF, obesity, and type 2 diabetes, noted Dr. Kosiborod, who is also lead investigator for that study. He said those results will likely become available before the end of 2023.
The study was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to and has received honoraria from Novo Nordisk. He has also been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Fonarow has been a consultant to Abbott, Amgen, AstraZeneca, CHF Solutions, Cytokinetics, Edwards, Janssen, Medtronic, Merck, Novartis, and Regeneron. Dr. Sweitzer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT THE ESC CONGRESS 2023
How should muscle mass be measured in heart failure?
, research suggests.
In a single-center, retrospective study that included more than 800 patients, high MUAC (hazard ratio for combined events, 0.590) and high AMC (HR for combined events, 0.529) were associated with significantly better prognoses than low MUAC and low AMC.
The findings were “surprising,” Kentaro Kamiya, PT, PhD, and Shota Uchida, PT, PhD, of Kitasato University School of Allied Health Sciences in Kanagawa, Japan, said in an interview.
“These findings challenge the current recommendations found in sarcopenia guidelines,” they noted. The European Working Group on Sarcopenia in Older People and the Asian Working Group for Sarcopenia recommend SMI, as measured by bioelectrical impedance analysis (BIA), and CC as methods for screening skeletal muscle mass.
The study was published online in the Canadian Journal of Cardiology.
Arm measures prognostic
Sarcopenia, which is marked by a loss of skeletal muscle mass and strength, is associated with risks of adverse outcomes. Patients with heart failure have a high rate of sarcopenia, but assessing skeletal muscle mass in these patients is difficult because of the fluid retention they often have.
The investigators examined the association between skeletal muscle mass metrics, measured using bioelectrical impedance analysis, and anthropometric measures and prognosis in patients with heart failure.
SMI was calculated using the BIA by dividing appendicular skeletal muscle mass by height squared. MUAC and CC were measured to the nearest 1 mm using a plastic tape measure. AMC was calculated as follows: MUAC (cm) − (0.314 x triceps skinfold [TSF]). The TSF was measured to the nearest 2 mm with a skinfold caliper. The measuring spot for TSF was the same measuring spot for MUAC. MUAC, CC, and TSF were measured by trained physiotherapists or nurses.
The investigators identified 1,930 consecutive patients with heart failure who underwent cardiac rehabilitation during their hospitalization. They excluded from their analysis 1,013 patients who did not undergo a skeletal mass metrics evaluation and 48 who could not be followed up.
The analysis included 869 patients (median age, 73 years; 62% men). Patients were separated into three groups on the basis of the sex-specific tertiles of skeletal muscle mass. The study endpoint was all-cause death or readmission due to heart failure, and the median follow-up period was 1.24 years.
After the investigators adjusted the data for age, sex, New York Heart Association functional class III or IV, left ventricular ejection fraction (LVEF), ischemic etiology, prior heart failure, diabetes, chronic obstructive pulmonary disease, log-transformed B-type natriuretic peptide (BNP), and estimated glomerular filtration rate (eGFR), the high MUAC and high AMC groups were associated with significantly better prognoses than their respective low groups. By contrast, high SMI and high CC were not associated with better prognoses.
Subgroup analyses showed no interactions between MUAC and age, sex, LVEF, BNP, eGFR, prior heart failure, beta-blocker use, and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker use. However, diuretic agents significantly interacted with AMC (P = .03).
“These results support the use of MUAC and AMC to determine the risk stratification of sarcopenia and a poor prognosis in patients with heart failure and suggest that they may be useful in developing treatment strategies in patients with heart failure,” wrote the authors.
“When caring for patients with heart failure, it seems that the often overlooked and simple measure of arm circumference might carry significant prognostic value,” said Dr. Kamiya and Dr. Uchida. “So, as you cuff the arm for routine blood pressure measurement, it might be worthwhile to also pay attention to arm girth.”
Although the findings provide valuable insights, they should be approached with caution, Dr. Kamiya and Dr. Uchida added. “Before considering them practice-changing, further research is needed to validate these results in diverse patient cohorts.”
Prospective study needed
Commenting on the study for this news organization, Jonathan H. Whiteson, MD, vice chair of clinical operations and medical director of cardiac and pulmonary rehabilitation at NYU Langone Health’s Rusk Rehabilitation in New York, expressed concerns about the study methodology.
Methodologic weaknesses include the retrospective, observational nature of the study and the fact that incomplete data collection led to the exclusion of more than half of the potential participants, he said. In addition, “anthropometric measurements are prone to inter-rater error. It is not clear if the same or different researchers conducted these measurements.
“Furthermore, hospitalized patients may not be clinically stable when discharged,” said Dr. Whiteson. “It is recommended that biometrics for muscle mass and fluid retention be done when patients are at an optimized clinical state: that is, stabilized outpatients.”
For now, Dr. Whiteson concluded, the findings should be considered “interesting and suggestive of further study.” What’s needed is “a prospective study including all patients admitted with heart failure, but measurements done when the patient is stabilized as an outpatient.”
The study was partially supported by the Japan Society for the Promotion of Science KAKENHI. Dr. Kamiya, Dr. Uchida, and Dr. Whiteson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
, research suggests.
In a single-center, retrospective study that included more than 800 patients, high MUAC (hazard ratio for combined events, 0.590) and high AMC (HR for combined events, 0.529) were associated with significantly better prognoses than low MUAC and low AMC.
The findings were “surprising,” Kentaro Kamiya, PT, PhD, and Shota Uchida, PT, PhD, of Kitasato University School of Allied Health Sciences in Kanagawa, Japan, said in an interview.
“These findings challenge the current recommendations found in sarcopenia guidelines,” they noted. The European Working Group on Sarcopenia in Older People and the Asian Working Group for Sarcopenia recommend SMI, as measured by bioelectrical impedance analysis (BIA), and CC as methods for screening skeletal muscle mass.
The study was published online in the Canadian Journal of Cardiology.
Arm measures prognostic
Sarcopenia, which is marked by a loss of skeletal muscle mass and strength, is associated with risks of adverse outcomes. Patients with heart failure have a high rate of sarcopenia, but assessing skeletal muscle mass in these patients is difficult because of the fluid retention they often have.
The investigators examined the association between skeletal muscle mass metrics, measured using bioelectrical impedance analysis, and anthropometric measures and prognosis in patients with heart failure.
SMI was calculated using the BIA by dividing appendicular skeletal muscle mass by height squared. MUAC and CC were measured to the nearest 1 mm using a plastic tape measure. AMC was calculated as follows: MUAC (cm) − (0.314 x triceps skinfold [TSF]). The TSF was measured to the nearest 2 mm with a skinfold caliper. The measuring spot for TSF was the same measuring spot for MUAC. MUAC, CC, and TSF were measured by trained physiotherapists or nurses.
The investigators identified 1,930 consecutive patients with heart failure who underwent cardiac rehabilitation during their hospitalization. They excluded from their analysis 1,013 patients who did not undergo a skeletal mass metrics evaluation and 48 who could not be followed up.
The analysis included 869 patients (median age, 73 years; 62% men). Patients were separated into three groups on the basis of the sex-specific tertiles of skeletal muscle mass. The study endpoint was all-cause death or readmission due to heart failure, and the median follow-up period was 1.24 years.
After the investigators adjusted the data for age, sex, New York Heart Association functional class III or IV, left ventricular ejection fraction (LVEF), ischemic etiology, prior heart failure, diabetes, chronic obstructive pulmonary disease, log-transformed B-type natriuretic peptide (BNP), and estimated glomerular filtration rate (eGFR), the high MUAC and high AMC groups were associated with significantly better prognoses than their respective low groups. By contrast, high SMI and high CC were not associated with better prognoses.
Subgroup analyses showed no interactions between MUAC and age, sex, LVEF, BNP, eGFR, prior heart failure, beta-blocker use, and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker use. However, diuretic agents significantly interacted with AMC (P = .03).
“These results support the use of MUAC and AMC to determine the risk stratification of sarcopenia and a poor prognosis in patients with heart failure and suggest that they may be useful in developing treatment strategies in patients with heart failure,” wrote the authors.
“When caring for patients with heart failure, it seems that the often overlooked and simple measure of arm circumference might carry significant prognostic value,” said Dr. Kamiya and Dr. Uchida. “So, as you cuff the arm for routine blood pressure measurement, it might be worthwhile to also pay attention to arm girth.”
Although the findings provide valuable insights, they should be approached with caution, Dr. Kamiya and Dr. Uchida added. “Before considering them practice-changing, further research is needed to validate these results in diverse patient cohorts.”
Prospective study needed
Commenting on the study for this news organization, Jonathan H. Whiteson, MD, vice chair of clinical operations and medical director of cardiac and pulmonary rehabilitation at NYU Langone Health’s Rusk Rehabilitation in New York, expressed concerns about the study methodology.
Methodologic weaknesses include the retrospective, observational nature of the study and the fact that incomplete data collection led to the exclusion of more than half of the potential participants, he said. In addition, “anthropometric measurements are prone to inter-rater error. It is not clear if the same or different researchers conducted these measurements.
“Furthermore, hospitalized patients may not be clinically stable when discharged,” said Dr. Whiteson. “It is recommended that biometrics for muscle mass and fluid retention be done when patients are at an optimized clinical state: that is, stabilized outpatients.”
For now, Dr. Whiteson concluded, the findings should be considered “interesting and suggestive of further study.” What’s needed is “a prospective study including all patients admitted with heart failure, but measurements done when the patient is stabilized as an outpatient.”
The study was partially supported by the Japan Society for the Promotion of Science KAKENHI. Dr. Kamiya, Dr. Uchida, and Dr. Whiteson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
, research suggests.
In a single-center, retrospective study that included more than 800 patients, high MUAC (hazard ratio for combined events, 0.590) and high AMC (HR for combined events, 0.529) were associated with significantly better prognoses than low MUAC and low AMC.
The findings were “surprising,” Kentaro Kamiya, PT, PhD, and Shota Uchida, PT, PhD, of Kitasato University School of Allied Health Sciences in Kanagawa, Japan, said in an interview.
“These findings challenge the current recommendations found in sarcopenia guidelines,” they noted. The European Working Group on Sarcopenia in Older People and the Asian Working Group for Sarcopenia recommend SMI, as measured by bioelectrical impedance analysis (BIA), and CC as methods for screening skeletal muscle mass.
The study was published online in the Canadian Journal of Cardiology.
Arm measures prognostic
Sarcopenia, which is marked by a loss of skeletal muscle mass and strength, is associated with risks of adverse outcomes. Patients with heart failure have a high rate of sarcopenia, but assessing skeletal muscle mass in these patients is difficult because of the fluid retention they often have.
The investigators examined the association between skeletal muscle mass metrics, measured using bioelectrical impedance analysis, and anthropometric measures and prognosis in patients with heart failure.
SMI was calculated using the BIA by dividing appendicular skeletal muscle mass by height squared. MUAC and CC were measured to the nearest 1 mm using a plastic tape measure. AMC was calculated as follows: MUAC (cm) − (0.314 x triceps skinfold [TSF]). The TSF was measured to the nearest 2 mm with a skinfold caliper. The measuring spot for TSF was the same measuring spot for MUAC. MUAC, CC, and TSF were measured by trained physiotherapists or nurses.
The investigators identified 1,930 consecutive patients with heart failure who underwent cardiac rehabilitation during their hospitalization. They excluded from their analysis 1,013 patients who did not undergo a skeletal mass metrics evaluation and 48 who could not be followed up.
The analysis included 869 patients (median age, 73 years; 62% men). Patients were separated into three groups on the basis of the sex-specific tertiles of skeletal muscle mass. The study endpoint was all-cause death or readmission due to heart failure, and the median follow-up period was 1.24 years.
After the investigators adjusted the data for age, sex, New York Heart Association functional class III or IV, left ventricular ejection fraction (LVEF), ischemic etiology, prior heart failure, diabetes, chronic obstructive pulmonary disease, log-transformed B-type natriuretic peptide (BNP), and estimated glomerular filtration rate (eGFR), the high MUAC and high AMC groups were associated with significantly better prognoses than their respective low groups. By contrast, high SMI and high CC were not associated with better prognoses.
Subgroup analyses showed no interactions between MUAC and age, sex, LVEF, BNP, eGFR, prior heart failure, beta-blocker use, and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker use. However, diuretic agents significantly interacted with AMC (P = .03).
“These results support the use of MUAC and AMC to determine the risk stratification of sarcopenia and a poor prognosis in patients with heart failure and suggest that they may be useful in developing treatment strategies in patients with heart failure,” wrote the authors.
“When caring for patients with heart failure, it seems that the often overlooked and simple measure of arm circumference might carry significant prognostic value,” said Dr. Kamiya and Dr. Uchida. “So, as you cuff the arm for routine blood pressure measurement, it might be worthwhile to also pay attention to arm girth.”
Although the findings provide valuable insights, they should be approached with caution, Dr. Kamiya and Dr. Uchida added. “Before considering them practice-changing, further research is needed to validate these results in diverse patient cohorts.”
Prospective study needed
Commenting on the study for this news organization, Jonathan H. Whiteson, MD, vice chair of clinical operations and medical director of cardiac and pulmonary rehabilitation at NYU Langone Health’s Rusk Rehabilitation in New York, expressed concerns about the study methodology.
Methodologic weaknesses include the retrospective, observational nature of the study and the fact that incomplete data collection led to the exclusion of more than half of the potential participants, he said. In addition, “anthropometric measurements are prone to inter-rater error. It is not clear if the same or different researchers conducted these measurements.
“Furthermore, hospitalized patients may not be clinically stable when discharged,” said Dr. Whiteson. “It is recommended that biometrics for muscle mass and fluid retention be done when patients are at an optimized clinical state: that is, stabilized outpatients.”
For now, Dr. Whiteson concluded, the findings should be considered “interesting and suggestive of further study.” What’s needed is “a prospective study including all patients admitted with heart failure, but measurements done when the patient is stabilized as an outpatient.”
The study was partially supported by the Japan Society for the Promotion of Science KAKENHI. Dr. Kamiya, Dr. Uchida, and Dr. Whiteson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN JOURNAL OF CARDIOLOGY
Another FDA class I recall of Cardiosave Hybrid/Rescue IABPs
due to electrical failures in the power management board or solenoid board (power source path).
“Using an affected pump may cause serious adverse health events, including unstable blood pressure, injury (e.g., inadequate blood supply or a vital organ injury), and death,” the Food and Drug Administration said in the recall notice.
The FDA has identified this as a class I recall, the most serious type of recall due to the risk for serious injury or death. To date, Datascope/Maquet/Getinge received 26 complaints, but no reports of injuries or death.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
The recall includes a total of 4,586 Cardiosave Hybrid or Rescue IABP units distributed from March 2, 2012, to May 19, 2023. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
On June 5, Datascope/Maquet/Getinge sent an “important medical device advisory” to all affected customers. The letter advises customers to be sure there is an alternative IABP available to continue therapy and provide alternative hemodynamic support if there is no other means to continue counterpulsation therapy.
Customers with questions about this recall should contact their company representative or call technical support at 1-888-943-8872, Monday through Friday, between 8:00 a.m. and 6:00 p.m. ET.
Last March, Datascope/Getinge recalled 2,300 Cardiosave Hybrid or Rescue IABPs because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The Cardiosave IABPs have also been previously flagged by the FDA for subpar battery performance and fluid leaks.
Any adverse events or suspected adverse events related to the recalled Cardiosave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article appeared on Medscape.com.
due to electrical failures in the power management board or solenoid board (power source path).
“Using an affected pump may cause serious adverse health events, including unstable blood pressure, injury (e.g., inadequate blood supply or a vital organ injury), and death,” the Food and Drug Administration said in the recall notice.
The FDA has identified this as a class I recall, the most serious type of recall due to the risk for serious injury or death. To date, Datascope/Maquet/Getinge received 26 complaints, but no reports of injuries or death.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
The recall includes a total of 4,586 Cardiosave Hybrid or Rescue IABP units distributed from March 2, 2012, to May 19, 2023. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
On June 5, Datascope/Maquet/Getinge sent an “important medical device advisory” to all affected customers. The letter advises customers to be sure there is an alternative IABP available to continue therapy and provide alternative hemodynamic support if there is no other means to continue counterpulsation therapy.
Customers with questions about this recall should contact their company representative or call technical support at 1-888-943-8872, Monday through Friday, between 8:00 a.m. and 6:00 p.m. ET.
Last March, Datascope/Getinge recalled 2,300 Cardiosave Hybrid or Rescue IABPs because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The Cardiosave IABPs have also been previously flagged by the FDA for subpar battery performance and fluid leaks.
Any adverse events or suspected adverse events related to the recalled Cardiosave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article appeared on Medscape.com.
due to electrical failures in the power management board or solenoid board (power source path).
“Using an affected pump may cause serious adverse health events, including unstable blood pressure, injury (e.g., inadequate blood supply or a vital organ injury), and death,” the Food and Drug Administration said in the recall notice.
The FDA has identified this as a class I recall, the most serious type of recall due to the risk for serious injury or death. To date, Datascope/Maquet/Getinge received 26 complaints, but no reports of injuries or death.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
The recall includes a total of 4,586 Cardiosave Hybrid or Rescue IABP units distributed from March 2, 2012, to May 19, 2023. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
On June 5, Datascope/Maquet/Getinge sent an “important medical device advisory” to all affected customers. The letter advises customers to be sure there is an alternative IABP available to continue therapy and provide alternative hemodynamic support if there is no other means to continue counterpulsation therapy.
Customers with questions about this recall should contact their company representative or call technical support at 1-888-943-8872, Monday through Friday, between 8:00 a.m. and 6:00 p.m. ET.
Last March, Datascope/Getinge recalled 2,300 Cardiosave Hybrid or Rescue IABPs because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The Cardiosave IABPs have also been previously flagged by the FDA for subpar battery performance and fluid leaks.
Any adverse events or suspected adverse events related to the recalled Cardiosave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article appeared on Medscape.com.
Higher step counts tied to fewer symptoms in HF
Daily step counts between 1,000 and 5,000 were significantly associated with symptoms and physical limitations, as reflected in Kansas City Cardiomyopathy Questionnaire (KCCQ) total symptom (TS) and physical limitation (PL) scores.
Participants whose step counts increased by 2,000 steps per day demonstrated a 5.2-point increase in their KCCQ-TS scores and a 5.33-point increase in their KCCQ-PL scores, with higher scores reflecting improvement.
However, declines in step counts were not associated with significant declines in KCCQ-PL scores.
The findings are not yet ready to be implemented into practice, first author Jessica R. Golbus, MD, of the University of Michigan, Ann Arbor, said in an interview. However, she said, they “suggest that clinicians should interpret improvements in step counts as indicative of improving health status, though they should not necessarily be as concerned with reductions in step count.
“I would certainly, however, still encourage clinicians to discuss decrementing physical activity levels with their patients, though an intervention may not necessarily be warranted,” she added.
The study was published online in JACC: Heart Failure.
Nonlinear relationship
The investigators analyzed data from the Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure (CHIEF-HF) trial, a randomized, controlled trial that enrolled participants with heart failure who had a smartphone.
Participants were given a Fitbit Versa 2 and completed serial KCCQs via the smartphone app.
The researchers assessed the relationship between daily step count and KCCQ-TS and KCCQ-PL scores at baseline, as well as changes in the scores between 2 and 12 weeks.
The study included 425 patients. The mean age was 63.5 years, 44.5% were women, and 83.3% were White; 40.9% had reduced ejection fraction, 59.1% had preserved ejection fraction, and 27.5% had type 2 diabetes.
At 2 weeks, the mean KCCQ-TS score was 62.7, and the mean KCCQ-PL score was 55.7.
KCCQ-TS scores increased by 2.5 points on average, and KCCQ-PL scores by 4 points through 12 weeks.
When categorized by 25-point ranges, the step count increased with increasing scores for both KCCQ-TS and KCCQ-PL. Those with KCCQ-TS scores of 0-24 averaged 2,437.6 steps daily, and those with scores of 75-100 averaged 4,870.9 steps daily.
Similarly, participants with KCCQ-PL scores of 0-24 averaged 2301.5 steps daily, and those with scores of 75-100 averaged 5,351.9. The relationship remained significant after adjustment.
There were nonlinear relationships between activity and KCCQ scores: Daily step counts below 5,000 steps were associated with KCCQ scores, but there was little association with counts above 5,000 steps.
Compared with participants who walked 2,000 steps per day, those who walked 1,000 had KCCQ-TS scores that were 3.11 points lower; participants who walked 3,000 had KCCQ-TS scores that were 2.89 points higher.
Similarly, participants who walked 1,000 steps per day had KCCQ-PL scores that were 5.36 points lower than those who walked 2,000 steps, and those who walked 3,000 steps had KCCQ-PL scores that were 4.97 points higher.
After adjustment, change in daily step counts was significantly associated with a change in KCCQ-PL scores from baseline through 12 weeks; for example, participants whose step counts increased by 2,000 steps per day experienced a 5.33 increase in their KCCQ-PL scores relative to participants whose step counts did not change.
‘New kid on the block’
Frederick Ho, PhD, a lecturer in public health at the University of Glasgow (Scotland), who is a volunteer spokesperson for the American Heart Association, called the study “promising.”
“The study follow-up is relatively short, so it is not known whether the association is valid longer term,” he said in an interview. “It is also possible that patients with more severe symptoms became physically less active, and at the same time had worse outcomes.
“A study with longer follow-up among patients from a broader background would provide confidence on the generalizability of the findings,” said Dr. Ho, who led a recent study that showed accelerometer-measured physical activity was associated with a lower risk of heart failure. “It’d also be interesting to validate the findings using different types of wearable devices.”
Previous studies have shown that wrist-worn wearables might overestimate light-intensity activities, compared with hip-worn devices, he noted. “I’d imagine that the findings would be slightly different due to different types of devices, but the overall premise should remain.”
In a related editorial, Mitchell Psotka, MD, PhD, writes that Dr. Golbus and colleagues “have thankfully moved our understanding of actigraphy forward, although it is still the new kid on the block and will require substantial further testing and validation before widespread reliable clinical and research use.”
Terminology and reporting features need to be standardized, and preferred methods of implementation need to be established, including how to wear the devices, he suggests.
Further research is needed to validate that “accelerometers and their digitally processed movement ‘counts’ actually measure activity and that this measured activity has clinical relevance.”
The study did not receive commercial funding. Dr. Golbus, Dr. Ho, and Dr. Psotka report no relevant relationships.
A version of this article first appeared on Medscape.com.
Daily step counts between 1,000 and 5,000 were significantly associated with symptoms and physical limitations, as reflected in Kansas City Cardiomyopathy Questionnaire (KCCQ) total symptom (TS) and physical limitation (PL) scores.
Participants whose step counts increased by 2,000 steps per day demonstrated a 5.2-point increase in their KCCQ-TS scores and a 5.33-point increase in their KCCQ-PL scores, with higher scores reflecting improvement.
However, declines in step counts were not associated with significant declines in KCCQ-PL scores.
The findings are not yet ready to be implemented into practice, first author Jessica R. Golbus, MD, of the University of Michigan, Ann Arbor, said in an interview. However, she said, they “suggest that clinicians should interpret improvements in step counts as indicative of improving health status, though they should not necessarily be as concerned with reductions in step count.
“I would certainly, however, still encourage clinicians to discuss decrementing physical activity levels with their patients, though an intervention may not necessarily be warranted,” she added.
The study was published online in JACC: Heart Failure.
Nonlinear relationship
The investigators analyzed data from the Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure (CHIEF-HF) trial, a randomized, controlled trial that enrolled participants with heart failure who had a smartphone.
Participants were given a Fitbit Versa 2 and completed serial KCCQs via the smartphone app.
The researchers assessed the relationship between daily step count and KCCQ-TS and KCCQ-PL scores at baseline, as well as changes in the scores between 2 and 12 weeks.
The study included 425 patients. The mean age was 63.5 years, 44.5% were women, and 83.3% were White; 40.9% had reduced ejection fraction, 59.1% had preserved ejection fraction, and 27.5% had type 2 diabetes.
At 2 weeks, the mean KCCQ-TS score was 62.7, and the mean KCCQ-PL score was 55.7.
KCCQ-TS scores increased by 2.5 points on average, and KCCQ-PL scores by 4 points through 12 weeks.
When categorized by 25-point ranges, the step count increased with increasing scores for both KCCQ-TS and KCCQ-PL. Those with KCCQ-TS scores of 0-24 averaged 2,437.6 steps daily, and those with scores of 75-100 averaged 4,870.9 steps daily.
Similarly, participants with KCCQ-PL scores of 0-24 averaged 2301.5 steps daily, and those with scores of 75-100 averaged 5,351.9. The relationship remained significant after adjustment.
There were nonlinear relationships between activity and KCCQ scores: Daily step counts below 5,000 steps were associated with KCCQ scores, but there was little association with counts above 5,000 steps.
Compared with participants who walked 2,000 steps per day, those who walked 1,000 had KCCQ-TS scores that were 3.11 points lower; participants who walked 3,000 had KCCQ-TS scores that were 2.89 points higher.
Similarly, participants who walked 1,000 steps per day had KCCQ-PL scores that were 5.36 points lower than those who walked 2,000 steps, and those who walked 3,000 steps had KCCQ-PL scores that were 4.97 points higher.
After adjustment, change in daily step counts was significantly associated with a change in KCCQ-PL scores from baseline through 12 weeks; for example, participants whose step counts increased by 2,000 steps per day experienced a 5.33 increase in their KCCQ-PL scores relative to participants whose step counts did not change.
‘New kid on the block’
Frederick Ho, PhD, a lecturer in public health at the University of Glasgow (Scotland), who is a volunteer spokesperson for the American Heart Association, called the study “promising.”
“The study follow-up is relatively short, so it is not known whether the association is valid longer term,” he said in an interview. “It is also possible that patients with more severe symptoms became physically less active, and at the same time had worse outcomes.
“A study with longer follow-up among patients from a broader background would provide confidence on the generalizability of the findings,” said Dr. Ho, who led a recent study that showed accelerometer-measured physical activity was associated with a lower risk of heart failure. “It’d also be interesting to validate the findings using different types of wearable devices.”
Previous studies have shown that wrist-worn wearables might overestimate light-intensity activities, compared with hip-worn devices, he noted. “I’d imagine that the findings would be slightly different due to different types of devices, but the overall premise should remain.”
In a related editorial, Mitchell Psotka, MD, PhD, writes that Dr. Golbus and colleagues “have thankfully moved our understanding of actigraphy forward, although it is still the new kid on the block and will require substantial further testing and validation before widespread reliable clinical and research use.”
Terminology and reporting features need to be standardized, and preferred methods of implementation need to be established, including how to wear the devices, he suggests.
Further research is needed to validate that “accelerometers and their digitally processed movement ‘counts’ actually measure activity and that this measured activity has clinical relevance.”
The study did not receive commercial funding. Dr. Golbus, Dr. Ho, and Dr. Psotka report no relevant relationships.
A version of this article first appeared on Medscape.com.
Daily step counts between 1,000 and 5,000 were significantly associated with symptoms and physical limitations, as reflected in Kansas City Cardiomyopathy Questionnaire (KCCQ) total symptom (TS) and physical limitation (PL) scores.
Participants whose step counts increased by 2,000 steps per day demonstrated a 5.2-point increase in their KCCQ-TS scores and a 5.33-point increase in their KCCQ-PL scores, with higher scores reflecting improvement.
However, declines in step counts were not associated with significant declines in KCCQ-PL scores.
The findings are not yet ready to be implemented into practice, first author Jessica R. Golbus, MD, of the University of Michigan, Ann Arbor, said in an interview. However, she said, they “suggest that clinicians should interpret improvements in step counts as indicative of improving health status, though they should not necessarily be as concerned with reductions in step count.
“I would certainly, however, still encourage clinicians to discuss decrementing physical activity levels with their patients, though an intervention may not necessarily be warranted,” she added.
The study was published online in JACC: Heart Failure.
Nonlinear relationship
The investigators analyzed data from the Canagliflozin: Impact on Health Status, Quality of Life and Functional Status in Heart Failure (CHIEF-HF) trial, a randomized, controlled trial that enrolled participants with heart failure who had a smartphone.
Participants were given a Fitbit Versa 2 and completed serial KCCQs via the smartphone app.
The researchers assessed the relationship between daily step count and KCCQ-TS and KCCQ-PL scores at baseline, as well as changes in the scores between 2 and 12 weeks.
The study included 425 patients. The mean age was 63.5 years, 44.5% were women, and 83.3% were White; 40.9% had reduced ejection fraction, 59.1% had preserved ejection fraction, and 27.5% had type 2 diabetes.
At 2 weeks, the mean KCCQ-TS score was 62.7, and the mean KCCQ-PL score was 55.7.
KCCQ-TS scores increased by 2.5 points on average, and KCCQ-PL scores by 4 points through 12 weeks.
When categorized by 25-point ranges, the step count increased with increasing scores for both KCCQ-TS and KCCQ-PL. Those with KCCQ-TS scores of 0-24 averaged 2,437.6 steps daily, and those with scores of 75-100 averaged 4,870.9 steps daily.
Similarly, participants with KCCQ-PL scores of 0-24 averaged 2301.5 steps daily, and those with scores of 75-100 averaged 5,351.9. The relationship remained significant after adjustment.
There were nonlinear relationships between activity and KCCQ scores: Daily step counts below 5,000 steps were associated with KCCQ scores, but there was little association with counts above 5,000 steps.
Compared with participants who walked 2,000 steps per day, those who walked 1,000 had KCCQ-TS scores that were 3.11 points lower; participants who walked 3,000 had KCCQ-TS scores that were 2.89 points higher.
Similarly, participants who walked 1,000 steps per day had KCCQ-PL scores that were 5.36 points lower than those who walked 2,000 steps, and those who walked 3,000 steps had KCCQ-PL scores that were 4.97 points higher.
After adjustment, change in daily step counts was significantly associated with a change in KCCQ-PL scores from baseline through 12 weeks; for example, participants whose step counts increased by 2,000 steps per day experienced a 5.33 increase in their KCCQ-PL scores relative to participants whose step counts did not change.
‘New kid on the block’
Frederick Ho, PhD, a lecturer in public health at the University of Glasgow (Scotland), who is a volunteer spokesperson for the American Heart Association, called the study “promising.”
“The study follow-up is relatively short, so it is not known whether the association is valid longer term,” he said in an interview. “It is also possible that patients with more severe symptoms became physically less active, and at the same time had worse outcomes.
“A study with longer follow-up among patients from a broader background would provide confidence on the generalizability of the findings,” said Dr. Ho, who led a recent study that showed accelerometer-measured physical activity was associated with a lower risk of heart failure. “It’d also be interesting to validate the findings using different types of wearable devices.”
Previous studies have shown that wrist-worn wearables might overestimate light-intensity activities, compared with hip-worn devices, he noted. “I’d imagine that the findings would be slightly different due to different types of devices, but the overall premise should remain.”
In a related editorial, Mitchell Psotka, MD, PhD, writes that Dr. Golbus and colleagues “have thankfully moved our understanding of actigraphy forward, although it is still the new kid on the block and will require substantial further testing and validation before widespread reliable clinical and research use.”
Terminology and reporting features need to be standardized, and preferred methods of implementation need to be established, including how to wear the devices, he suggests.
Further research is needed to validate that “accelerometers and their digitally processed movement ‘counts’ actually measure activity and that this measured activity has clinical relevance.”
The study did not receive commercial funding. Dr. Golbus, Dr. Ho, and Dr. Psotka report no relevant relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE
Early or delayed AFib ablation after heart failure hospitalization?
TOPLINE:
Among patients with atrial fibrillation (AFib) hospitalized for worsening heart failure (HF), catheter (cath) ablation within 90 days of admission, compared with other times, is associated with reduced risk for all-cause mortality and HF-related mortality.
METHODOLOGY:
Cath ablation has become technically safer for patients with both AFib and HF, but the best timing for the ablation procedure after HF hospitalization has been unclear.
The study included 2,786 patients with HF who underwent cath ablation for AFib at 128 centers in the nationwide Japanese Registry of Acute Decompensated Heart Failure, were hospitalized with worsening HF, and survived at least 90 days after discharge.
The population included 103 individuals who underwent cath ablation within 90 days after admission; the remaining 2,683 participants served as the control group.
The researchers also looked at all-cause mortality 90 days after admission for HF in analysis of 83 early-ablation cases vs. 83 propensity-matched controls.
TAKEAWAY:
The early–cath ablation group was younger, predominantly male, had less history of prior HF hospitalizations, and greater incidence of paroxysmal AF, compared with the control group.
All-cause mortality was significantly lower in the early–cath ablation group than in the control group (hazard ratio, 0.38; 95% confidence interval, 0.24-0.60; P < .001) over a median of 4.1 years.
Risk reductions were similarly significant for secondary endpoints, including cardiovascular (CV) mortality and HF mortality.
In the matched cohort analysis (83 in both groups) all-cause mortality was significantly reduced for those in the early–cath ablation group, compared with the matched controls (HR, 0.47; 95% CI, 0.25-0.88; P = .014), with similarly significant risk reductions for CV mortality and HF mortality.
IN PRACTICE:
the report states. Early catheter ablation, as early as during the hospitalization for HF, “might be a way to stabilize HF and solve the problems associated with long hospitalization periods and polypharmacy.”
SOURCE:
The study was conducted by Kazuo Sakamoto, MD, PhD, Kyushu University, Fukuoka, Japan, and colleagues. It was published online July 19, 2023 in JACC: Clinical Electrophysiology.
LIMITATIONS:
The early-ablation cohort was much smaller than the control group, and the analysis could not adjust for any variation in institutional characteristics, such as location and available equipment. Other unmeasured potential confounders include duration of AFib and patient lifestyle characteristics and success or failure of ablation.
DISCLOSURES:
The study was funded by Johnson & Johnson, the Japan Agency for Medical Research and Development, and Ministry of Health and Labor. Dr. Sakamoto reports no relevant conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
Among patients with atrial fibrillation (AFib) hospitalized for worsening heart failure (HF), catheter (cath) ablation within 90 days of admission, compared with other times, is associated with reduced risk for all-cause mortality and HF-related mortality.
METHODOLOGY:
Cath ablation has become technically safer for patients with both AFib and HF, but the best timing for the ablation procedure after HF hospitalization has been unclear.
The study included 2,786 patients with HF who underwent cath ablation for AFib at 128 centers in the nationwide Japanese Registry of Acute Decompensated Heart Failure, were hospitalized with worsening HF, and survived at least 90 days after discharge.
The population included 103 individuals who underwent cath ablation within 90 days after admission; the remaining 2,683 participants served as the control group.
The researchers also looked at all-cause mortality 90 days after admission for HF in analysis of 83 early-ablation cases vs. 83 propensity-matched controls.
TAKEAWAY:
The early–cath ablation group was younger, predominantly male, had less history of prior HF hospitalizations, and greater incidence of paroxysmal AF, compared with the control group.
All-cause mortality was significantly lower in the early–cath ablation group than in the control group (hazard ratio, 0.38; 95% confidence interval, 0.24-0.60; P < .001) over a median of 4.1 years.
Risk reductions were similarly significant for secondary endpoints, including cardiovascular (CV) mortality and HF mortality.
In the matched cohort analysis (83 in both groups) all-cause mortality was significantly reduced for those in the early–cath ablation group, compared with the matched controls (HR, 0.47; 95% CI, 0.25-0.88; P = .014), with similarly significant risk reductions for CV mortality and HF mortality.
IN PRACTICE:
the report states. Early catheter ablation, as early as during the hospitalization for HF, “might be a way to stabilize HF and solve the problems associated with long hospitalization periods and polypharmacy.”
SOURCE:
The study was conducted by Kazuo Sakamoto, MD, PhD, Kyushu University, Fukuoka, Japan, and colleagues. It was published online July 19, 2023 in JACC: Clinical Electrophysiology.
LIMITATIONS:
The early-ablation cohort was much smaller than the control group, and the analysis could not adjust for any variation in institutional characteristics, such as location and available equipment. Other unmeasured potential confounders include duration of AFib and patient lifestyle characteristics and success or failure of ablation.
DISCLOSURES:
The study was funded by Johnson & Johnson, the Japan Agency for Medical Research and Development, and Ministry of Health and Labor. Dr. Sakamoto reports no relevant conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
Among patients with atrial fibrillation (AFib) hospitalized for worsening heart failure (HF), catheter (cath) ablation within 90 days of admission, compared with other times, is associated with reduced risk for all-cause mortality and HF-related mortality.
METHODOLOGY:
Cath ablation has become technically safer for patients with both AFib and HF, but the best timing for the ablation procedure after HF hospitalization has been unclear.
The study included 2,786 patients with HF who underwent cath ablation for AFib at 128 centers in the nationwide Japanese Registry of Acute Decompensated Heart Failure, were hospitalized with worsening HF, and survived at least 90 days after discharge.
The population included 103 individuals who underwent cath ablation within 90 days after admission; the remaining 2,683 participants served as the control group.
The researchers also looked at all-cause mortality 90 days after admission for HF in analysis of 83 early-ablation cases vs. 83 propensity-matched controls.
TAKEAWAY:
The early–cath ablation group was younger, predominantly male, had less history of prior HF hospitalizations, and greater incidence of paroxysmal AF, compared with the control group.
All-cause mortality was significantly lower in the early–cath ablation group than in the control group (hazard ratio, 0.38; 95% confidence interval, 0.24-0.60; P < .001) over a median of 4.1 years.
Risk reductions were similarly significant for secondary endpoints, including cardiovascular (CV) mortality and HF mortality.
In the matched cohort analysis (83 in both groups) all-cause mortality was significantly reduced for those in the early–cath ablation group, compared with the matched controls (HR, 0.47; 95% CI, 0.25-0.88; P = .014), with similarly significant risk reductions for CV mortality and HF mortality.
IN PRACTICE:
the report states. Early catheter ablation, as early as during the hospitalization for HF, “might be a way to stabilize HF and solve the problems associated with long hospitalization periods and polypharmacy.”
SOURCE:
The study was conducted by Kazuo Sakamoto, MD, PhD, Kyushu University, Fukuoka, Japan, and colleagues. It was published online July 19, 2023 in JACC: Clinical Electrophysiology.
LIMITATIONS:
The early-ablation cohort was much smaller than the control group, and the analysis could not adjust for any variation in institutional characteristics, such as location and available equipment. Other unmeasured potential confounders include duration of AFib and patient lifestyle characteristics and success or failure of ablation.
DISCLOSURES:
The study was funded by Johnson & Johnson, the Japan Agency for Medical Research and Development, and Ministry of Health and Labor. Dr. Sakamoto reports no relevant conflicts.
A version of this article first appeared on Medscape.com.
FROM JACC: CLINICAL ELECTROPHYSIOLOGY
Global burden of brain disorders surpasses cardiovascular disease and cancer
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– at huge cost to health care systems and society, an analysis of data from the most recent Global Burden of Disease (GBD) study shows.
“The burden of brain conditions will increase as populations continue to grow and age,” said study presenter Shayla Smith, MPH, an epidemiologist at the Institute for Health Metrics and Evaluation, the University of Washington, Seattle, in a press release.
“By 2050, more than 50 million people will be aged 65-79,” she explained, adding that the COVID-19 pandemic “has also influenced the prevalence of mental disorders globally, as people were forced to isolate and social networks broke down.”
Other factors related to brain disorders, she noted, include education level, obesity, and smoking.
“There’s still research to be done on what is the most effective way to maintain brain health, but some literature suggests a healthy brain can be achieved through a healthy lifestyle of managing conditions such as high blood pressure and diabetes, limiting alcohol consumption and smoking, prioritizing sleep, eating healthy, and staying physically and mentally active,” said Ms. Smith.
The findings were presented at the annual meeting of the Congress of the European Academy of Neurology.
An ‘ambitious exercise’
Coinvestigator Xaviera Steele, also from the IHME, told press conference attendees that the institute was established at the University of Washington in 2007 with the aim of “standardizing the measurement of health outcomes around the world and for all health conditions.”
A central part of that is the GBD study, “which is a very ambitious exercise in descriptive epidemiology in an effort to systematically quantify health loss” due to disease, injury, and risk factors over time, stratified by country, region, age, and sex. In addition, researchers are mapping and projecting trends over the next century and are estimating disease expenditure by country, by type of expense, and by condition “to derive a health care access and quality score for each health system in the world,” Ms. Steele said.
They are also estimating exposure to risk factors, how those risk factors contribute to health burden, and associated health outcomes by race and ethnicity to reflect the “disparities that we know are very prevalent in countries such as the United States.” From that work, Ms. Steele said that brain health and related conditions “do emerge as one of the more pressing challenges of the 21st century.”
Increase in dementia, mental health conditions
The data, which were gathered from 200,000 sources by the IHME, indicate that the number of individuals aged 65 years or older will increase by 350% by 2100. Ms. Steele underlined that “policy action will be needed to help families, who will struggle to provide high-quality care for their loved ones with dementia at a reasonable cost.”
The IHME calculates that in Europe health care spending on Alzheimer’s disease will increase by 226% between 2015 and 2040.
Turning to other conditions, Ms. Steele showed that since 1990, the number of individuals living with anxiety in the European region has increased by 14%, while the number living with depressive disorders has gone up by 13%.
Worldwide, the figures are even starker. Depression is estimated to affect 300 million people across the globe, which represents a 71% increase since 1990. The number of strokes increased by 95% over the same period.
Nevertheless, the “impact of brain conditions such as stroke has decreased since the 1990s due to improved treatments available,” Ms. Smith noted in the press release.
To estimate the toll caused by brain conditions, including neurologic disorders, mental disorders, cerebrovascular disease, brain cancer, brain injuries, and select infectious conditions, the researchers calculated disability-adjusted life years (DALYs).
This, Ms. Smith explained in her presentation, “captures the morbidity and mortality associated with brain conditions” and is adjusted for patient location, age, and sex.
The investigators found that, globally, brain conditions accounted for more than 15% of all health loss in 2021, at 406 DALYs – more than the 206 million DALYs that were associated with cancer, and the 402 million that were linked to cardiovascular disease.
This health loss is associated with a $1.22 trillion loss in income for people living with health disorders worldwide and accounts for $1.14 trillion in direct health care costs.
The burden of mental disorders, neurologic conditions, and stroke is expected to increase dramatically between now and 2050, said Ms. Smith, who noted that health loss linked to brain conditions is higher in younger patients. This will create “new challenges for health systems, employers, patients, and families,” she said in the press release.
“Our goal is to see an improved prevention and treatment landscape for other brain conditions and reverse the growing health loss that we are currently forecasting.”
Worrying increase in stroke
Jurgita Valaikiene, MD, PhD, center of neurology, clinic of neurology and neurosurgery, Vilnius (Lithuania) University Faculty of Medicine, who chaired the session, was taken aback by the findings, particularly by the worldwide increase in stroke cases.
“I work in stroke,” she said, and “we spend a lot of time on the diagnosis of stroke” and its prevention. “We try to be faster, to catch asymptomatic stenosis in the neck or head, and to apply the best medical treatment to avoid a stroke. But despite that, the numbers are increasing. I understand the population is getting older ... but still it’s a huge number.”
Dr. Valaikiene pointed out that stroke is not necessarily a condition of aging, insofar as increasing age “is not related directly to stenosis in the neck. “For example, we can have healthier vessels in older age and unhealthy vessels, with high-grade stenosis, in someone aged 30 or 40 years.”
“There are a lot of risk factors, such as smoking, physical activity, and so on. It depends on the individual,” she added.
The study was funded by the Institute for Health Metrics and Evaluation at the University of Washington. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PCPs key to heart failure care after discharge
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
New definition for iron deficiency in CV disease proposed
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.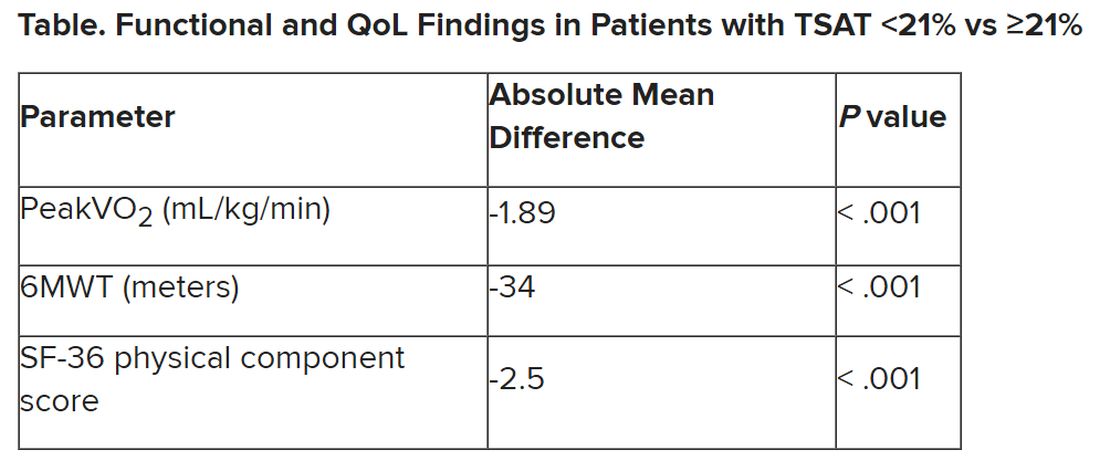
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.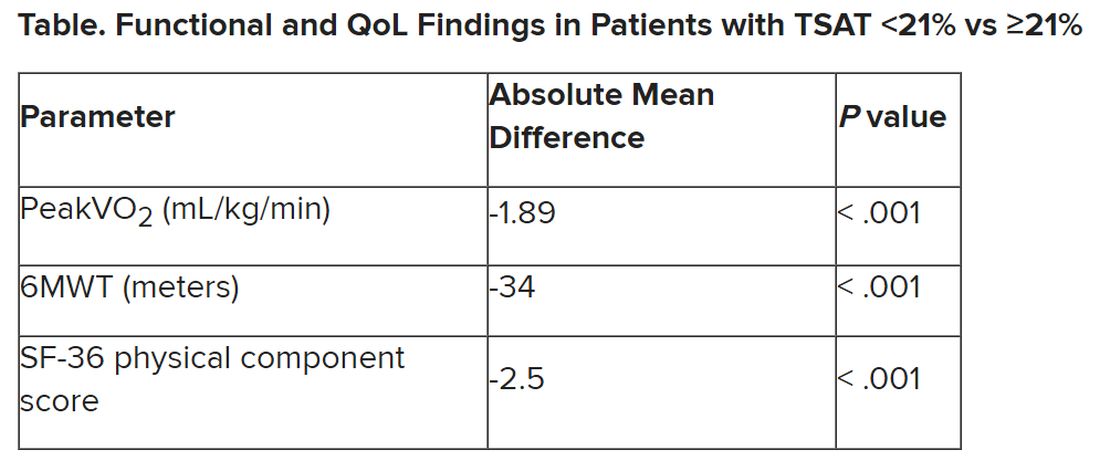
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.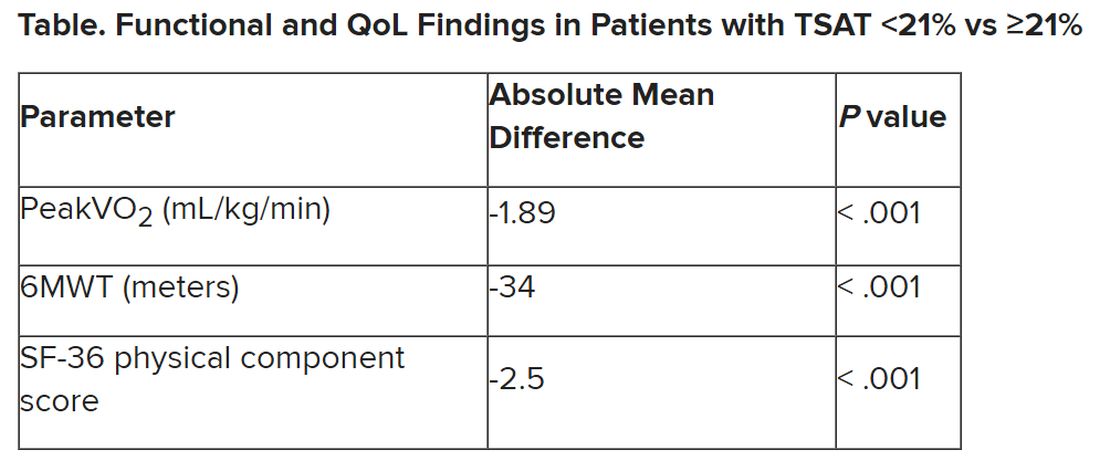
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL
Starting indicated heart failure meds in-hospital: Progress, opportunities
Most patients aren’t receiving all the medications they should based on guidelines, nor are they getting them at the most effective time in their disease course, suggests a registry study of patients in the United States hospitalized with heart failure with reduced ejection fraction (HFrEF).
On average, one such medication was initiated per patient for every 6 days in the hospital.
Shortfalls in predischarge GDMT initiation disproportionately landed on women, patients at rural centers, and those with renal failure or other comorbidities. But they didn’t seem related to patient race or ethnicity in the study reported in JACC: Heart Failure.
The analysis covers the 3 years preceding the May 2020 first-time approval of a sodium-glucose cotransporter 2 (SGLT2) inhibitor for nondiabetic patients with HFrEF, and therefore doesn’t cover such drugs for that indication. The SGLT2 inhibitors would later join beta-blockers, renin-angiotensin system (RAS) inhibitors, and mineralocorticoid receptor antagonists (MRAs) in the quartet of core GDMT medications broadly indicated for HFrEF.
In-hospital initiation of GDMT for HFrEF is considered a predictor of being on those medications after discharge and is itself guideline recommended. There’s clear evidence that treatment with the four core medications boosts survival and cuts rehospitalization risk, and that “getting those on board as soon as possible will eventually benefit many patients,” Paul L. Hess, MD, MHS, said in an interview.
Dr. Hess, University of Colorado Anschutz Medical Campus, Aurora, is senior author on the report from the Get With The Guidelines–Heart Failure (GWTG-HF) quality improvement program of the American Heart Association.
Broad uptake of new medical therapies into practice may sometimes take 15 or more years from first publication, Dr. Hess said, so, “I find it encouraging in the study that over a shorter time period, 2017-2020, there was improvement.”
Indeed, the odds of in-hospital initiation of an indicated med during that period on average climbed a significant 8% every 3 months, the report states.
The finding suggests that “heart failure hospitalization is, in and of itself, an important intervention for getting folks on the appropriate medications,” Dr. Hess said. It also means “we’re getting better at it,” at least at the study’s 160 GWTG-HF participating hospitals nationwide.
Those centers, the report acknowledges, varied in size, geography, and teaching status but were not necessarily representative of all U.S. hospitals. In another potential limitation, the study couldn’t account for patients who weren’t prescribed all indicated medications for clinically valid reasons. It excluded patients with “clear contraindications,” Dr. Hess said. But there could have been “legitimate reasons” some indicated medications weren’t always prescribed, including patient frailty, hemodynamic intolerance, renal dysfunction, or polypharmacy concerns.
“Positive takeaways” from the analysis, notes an accompanying editorial, include improved prescription rates for key GDMT categories across more than 3 years of data, and evidence that in-hospital initiation “was feasible and, at least for some medications, reliably undertaken.”
Of note, new GDMT prescriptions from admission to discharge went from 70% to almost 98% for beta-blockers, from 59% to about 91% for RAS inhibitors, from about 26% to 56% for MRAs, and from 15.5% to 27.4% for hydralazine/nitrates, wrote Karen E. Joynt Maddox, MD, MPH, and Daniel K. Fox, MD, PhD, both of Washington University in St. Louis.
“Key areas for improvement,” they noted, include prescriptions for women, who were 12% less likely than men to have appropriate GDMT initiated during hospitalization (P < .001); and practice at rural hospitals, which were 40% less likely than urban centers to have patients on full GDMT by discharge (P = .017).
Although only 2.6% of the GWTG-HF centers were in rural locations, “rural hospitals make up approximately one-third of general acute care hospitals in this country,” the editorial states. They therefore “represent a key source of health disparity” in the United States in need of further study.
The analysis of 50,170 patients hospitalized with HFrEF compared the number of GDMT medications for which they were eligible, on at-hospital admission, and by discharge.
The drug categories included “evidence based beta blockers,” that is, bisoprolol, carvedilol, or sustained-release metoprolol; RAS inhibitors, specifically ACE inhibitors, angiotensin receptor blockers, or sacubitril/valsartan (Entresto); MRAs; SGLT2 inhibitors in patients with diabetes; diuretics for congestion; oral anticoagulants for atrial fibrillation; and hydralazine/nitrates in African Americans.
About 15% of the patients at hospital admission were on all indicated HFrEF medications for which they were eligible. The proportion more than doubled to 32.8% by discharge.
Factors significantly associated with reduced odds for in-hospital GDMT initiation include older age (odds ratio, 0.94 per 5-year increment), being female versus male (OR, 0.88), rural location (OR, 0.60), Medicaid versus Medicare or private insurance (OR, 0.93), stroke history (OR, 0.91), peripheral artery disease (OR, 0.93), chronic obstructive pulmonary disease or asthma (OR, 0.86), and renal insufficiency (OR, 0.77).
The findings suggest that there has been at least some progress in getting hospitalized patients “on the right meds” by discharge, Dr. Hess observed. To help address shortfalls in some patient groups, “there is interest in engaging pharmacists in helping us encourage providers on the front lines to initiate and titrate medications.”
The GWTG-HF program is sponsored, in part, by Novartis, Boehringer Ingelheim, Novo Nordisk, AstraZeneca, Bayer, Tylenol, and Alnylam Pharmaceuticals. Dr. Hess disclosed no relevant financial relationships. Dr. Maddox disclosed serving on the Health Policy Advisory Council for Centene. Dr. Fox reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most patients aren’t receiving all the medications they should based on guidelines, nor are they getting them at the most effective time in their disease course, suggests a registry study of patients in the United States hospitalized with heart failure with reduced ejection fraction (HFrEF).
On average, one such medication was initiated per patient for every 6 days in the hospital.
Shortfalls in predischarge GDMT initiation disproportionately landed on women, patients at rural centers, and those with renal failure or other comorbidities. But they didn’t seem related to patient race or ethnicity in the study reported in JACC: Heart Failure.
The analysis covers the 3 years preceding the May 2020 first-time approval of a sodium-glucose cotransporter 2 (SGLT2) inhibitor for nondiabetic patients with HFrEF, and therefore doesn’t cover such drugs for that indication. The SGLT2 inhibitors would later join beta-blockers, renin-angiotensin system (RAS) inhibitors, and mineralocorticoid receptor antagonists (MRAs) in the quartet of core GDMT medications broadly indicated for HFrEF.
In-hospital initiation of GDMT for HFrEF is considered a predictor of being on those medications after discharge and is itself guideline recommended. There’s clear evidence that treatment with the four core medications boosts survival and cuts rehospitalization risk, and that “getting those on board as soon as possible will eventually benefit many patients,” Paul L. Hess, MD, MHS, said in an interview.
Dr. Hess, University of Colorado Anschutz Medical Campus, Aurora, is senior author on the report from the Get With The Guidelines–Heart Failure (GWTG-HF) quality improvement program of the American Heart Association.
Broad uptake of new medical therapies into practice may sometimes take 15 or more years from first publication, Dr. Hess said, so, “I find it encouraging in the study that over a shorter time period, 2017-2020, there was improvement.”
Indeed, the odds of in-hospital initiation of an indicated med during that period on average climbed a significant 8% every 3 months, the report states.
The finding suggests that “heart failure hospitalization is, in and of itself, an important intervention for getting folks on the appropriate medications,” Dr. Hess said. It also means “we’re getting better at it,” at least at the study’s 160 GWTG-HF participating hospitals nationwide.
Those centers, the report acknowledges, varied in size, geography, and teaching status but were not necessarily representative of all U.S. hospitals. In another potential limitation, the study couldn’t account for patients who weren’t prescribed all indicated medications for clinically valid reasons. It excluded patients with “clear contraindications,” Dr. Hess said. But there could have been “legitimate reasons” some indicated medications weren’t always prescribed, including patient frailty, hemodynamic intolerance, renal dysfunction, or polypharmacy concerns.
“Positive takeaways” from the analysis, notes an accompanying editorial, include improved prescription rates for key GDMT categories across more than 3 years of data, and evidence that in-hospital initiation “was feasible and, at least for some medications, reliably undertaken.”
Of note, new GDMT prescriptions from admission to discharge went from 70% to almost 98% for beta-blockers, from 59% to about 91% for RAS inhibitors, from about 26% to 56% for MRAs, and from 15.5% to 27.4% for hydralazine/nitrates, wrote Karen E. Joynt Maddox, MD, MPH, and Daniel K. Fox, MD, PhD, both of Washington University in St. Louis.
“Key areas for improvement,” they noted, include prescriptions for women, who were 12% less likely than men to have appropriate GDMT initiated during hospitalization (P < .001); and practice at rural hospitals, which were 40% less likely than urban centers to have patients on full GDMT by discharge (P = .017).
Although only 2.6% of the GWTG-HF centers were in rural locations, “rural hospitals make up approximately one-third of general acute care hospitals in this country,” the editorial states. They therefore “represent a key source of health disparity” in the United States in need of further study.
The analysis of 50,170 patients hospitalized with HFrEF compared the number of GDMT medications for which they were eligible, on at-hospital admission, and by discharge.
The drug categories included “evidence based beta blockers,” that is, bisoprolol, carvedilol, or sustained-release metoprolol; RAS inhibitors, specifically ACE inhibitors, angiotensin receptor blockers, or sacubitril/valsartan (Entresto); MRAs; SGLT2 inhibitors in patients with diabetes; diuretics for congestion; oral anticoagulants for atrial fibrillation; and hydralazine/nitrates in African Americans.
About 15% of the patients at hospital admission were on all indicated HFrEF medications for which they were eligible. The proportion more than doubled to 32.8% by discharge.
Factors significantly associated with reduced odds for in-hospital GDMT initiation include older age (odds ratio, 0.94 per 5-year increment), being female versus male (OR, 0.88), rural location (OR, 0.60), Medicaid versus Medicare or private insurance (OR, 0.93), stroke history (OR, 0.91), peripheral artery disease (OR, 0.93), chronic obstructive pulmonary disease or asthma (OR, 0.86), and renal insufficiency (OR, 0.77).
The findings suggest that there has been at least some progress in getting hospitalized patients “on the right meds” by discharge, Dr. Hess observed. To help address shortfalls in some patient groups, “there is interest in engaging pharmacists in helping us encourage providers on the front lines to initiate and titrate medications.”
The GWTG-HF program is sponsored, in part, by Novartis, Boehringer Ingelheim, Novo Nordisk, AstraZeneca, Bayer, Tylenol, and Alnylam Pharmaceuticals. Dr. Hess disclosed no relevant financial relationships. Dr. Maddox disclosed serving on the Health Policy Advisory Council for Centene. Dr. Fox reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most patients aren’t receiving all the medications they should based on guidelines, nor are they getting them at the most effective time in their disease course, suggests a registry study of patients in the United States hospitalized with heart failure with reduced ejection fraction (HFrEF).
On average, one such medication was initiated per patient for every 6 days in the hospital.
Shortfalls in predischarge GDMT initiation disproportionately landed on women, patients at rural centers, and those with renal failure or other comorbidities. But they didn’t seem related to patient race or ethnicity in the study reported in JACC: Heart Failure.
The analysis covers the 3 years preceding the May 2020 first-time approval of a sodium-glucose cotransporter 2 (SGLT2) inhibitor for nondiabetic patients with HFrEF, and therefore doesn’t cover such drugs for that indication. The SGLT2 inhibitors would later join beta-blockers, renin-angiotensin system (RAS) inhibitors, and mineralocorticoid receptor antagonists (MRAs) in the quartet of core GDMT medications broadly indicated for HFrEF.
In-hospital initiation of GDMT for HFrEF is considered a predictor of being on those medications after discharge and is itself guideline recommended. There’s clear evidence that treatment with the four core medications boosts survival and cuts rehospitalization risk, and that “getting those on board as soon as possible will eventually benefit many patients,” Paul L. Hess, MD, MHS, said in an interview.
Dr. Hess, University of Colorado Anschutz Medical Campus, Aurora, is senior author on the report from the Get With The Guidelines–Heart Failure (GWTG-HF) quality improvement program of the American Heart Association.
Broad uptake of new medical therapies into practice may sometimes take 15 or more years from first publication, Dr. Hess said, so, “I find it encouraging in the study that over a shorter time period, 2017-2020, there was improvement.”
Indeed, the odds of in-hospital initiation of an indicated med during that period on average climbed a significant 8% every 3 months, the report states.
The finding suggests that “heart failure hospitalization is, in and of itself, an important intervention for getting folks on the appropriate medications,” Dr. Hess said. It also means “we’re getting better at it,” at least at the study’s 160 GWTG-HF participating hospitals nationwide.
Those centers, the report acknowledges, varied in size, geography, and teaching status but were not necessarily representative of all U.S. hospitals. In another potential limitation, the study couldn’t account for patients who weren’t prescribed all indicated medications for clinically valid reasons. It excluded patients with “clear contraindications,” Dr. Hess said. But there could have been “legitimate reasons” some indicated medications weren’t always prescribed, including patient frailty, hemodynamic intolerance, renal dysfunction, or polypharmacy concerns.
“Positive takeaways” from the analysis, notes an accompanying editorial, include improved prescription rates for key GDMT categories across more than 3 years of data, and evidence that in-hospital initiation “was feasible and, at least for some medications, reliably undertaken.”
Of note, new GDMT prescriptions from admission to discharge went from 70% to almost 98% for beta-blockers, from 59% to about 91% for RAS inhibitors, from about 26% to 56% for MRAs, and from 15.5% to 27.4% for hydralazine/nitrates, wrote Karen E. Joynt Maddox, MD, MPH, and Daniel K. Fox, MD, PhD, both of Washington University in St. Louis.
“Key areas for improvement,” they noted, include prescriptions for women, who were 12% less likely than men to have appropriate GDMT initiated during hospitalization (P < .001); and practice at rural hospitals, which were 40% less likely than urban centers to have patients on full GDMT by discharge (P = .017).
Although only 2.6% of the GWTG-HF centers were in rural locations, “rural hospitals make up approximately one-third of general acute care hospitals in this country,” the editorial states. They therefore “represent a key source of health disparity” in the United States in need of further study.
The analysis of 50,170 patients hospitalized with HFrEF compared the number of GDMT medications for which they were eligible, on at-hospital admission, and by discharge.
The drug categories included “evidence based beta blockers,” that is, bisoprolol, carvedilol, or sustained-release metoprolol; RAS inhibitors, specifically ACE inhibitors, angiotensin receptor blockers, or sacubitril/valsartan (Entresto); MRAs; SGLT2 inhibitors in patients with diabetes; diuretics for congestion; oral anticoagulants for atrial fibrillation; and hydralazine/nitrates in African Americans.
About 15% of the patients at hospital admission were on all indicated HFrEF medications for which they were eligible. The proportion more than doubled to 32.8% by discharge.
Factors significantly associated with reduced odds for in-hospital GDMT initiation include older age (odds ratio, 0.94 per 5-year increment), being female versus male (OR, 0.88), rural location (OR, 0.60), Medicaid versus Medicare or private insurance (OR, 0.93), stroke history (OR, 0.91), peripheral artery disease (OR, 0.93), chronic obstructive pulmonary disease or asthma (OR, 0.86), and renal insufficiency (OR, 0.77).
The findings suggest that there has been at least some progress in getting hospitalized patients “on the right meds” by discharge, Dr. Hess observed. To help address shortfalls in some patient groups, “there is interest in engaging pharmacists in helping us encourage providers on the front lines to initiate and titrate medications.”
The GWTG-HF program is sponsored, in part, by Novartis, Boehringer Ingelheim, Novo Nordisk, AstraZeneca, Bayer, Tylenol, and Alnylam Pharmaceuticals. Dr. Hess disclosed no relevant financial relationships. Dr. Maddox disclosed serving on the Health Policy Advisory Council for Centene. Dr. Fox reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE




