User login
Antibody linked to spontaneous reversal of ATTR-CM
Cardiac transthyretin amyloidosis (also called ATTR amyloidosis cardiomyopathy or ATTR-CM) is a progressive disease and a cause of heart failure resulting from accumulation of the protein transthyretin, which misfolds and forms amyloid deposits on the walls of the heart, causing both systolic and diastolic dysfunction.
The condition is progressive and normally fatal within a few years of diagnosis. Treatment options are limited and aimed at slowing progression; nothing has been shown to reverse the course of the disease.
However, an international team of researchers is now reporting the discovery of three patients with ATTR-CM–associated heart failure in whom the condition resolved spontaneously, with reversion to near normal cardiac structure and function. On further investigation, it was found that these three patients had developed circulating polyclonal IgG antibodies to human ATTR amyloid.
They are hopeful that a monoclonal form of these antibodies could be developed and may represent a novel treatment, or even a cure, for the condition.
The researchers report their findings in a letter to the New England Journal of Medicine.
“We are very optimistic about this discovery of these antibodies. They could become the first treatment to clear the amyloid that causes this horribly progressive and fatal condition,” senior author Julian Gillmore, MD, head of the University College London Centre for Amyloidosis, based at the Royal Free Hospital, said in an interview.
“Obviously, there is a lot of work to do before we can say this is the case, but it is very exciting,” he added.
Dr. Gillmore explained how the antibodies were discovered. “This disease has a universally progressive course, but we had one patient who on a repeat appointment said he felt better and on detailed cardiac MRI imaging, we found that the amyloid in his heart had reduced. That is totally unheard of,” he said.
“We then looked back at our cohort of 1,663 patients with ATTR-cardiomyopathy, and we discovered two others who had also improved both on imaging and clinically,” Dr. Gillmore said.
Each of these three patients reported a reduction in symptoms, although they had not received any new or potentially disease-modifying treatments. None of the patients had had recent vaccinations, notable infections, or any clinical suggestion of myocarditis.
Clinical recovery was corroborated by substantial improvement or normalization of findings on echocardiography, serum biomarker levels, and results of cardiopulmonary exercise tests and scintigraphy.
Serial cardiac MRI scans confirmed near-complete regression of myocardial extracellular volume, coupled with remodeling to near-normal cardiac structure and function without scarring.
The researchers wondered whether the changes in these patients may have been brought about by an antibody response. On further investigation, they found antibodies in the three patients that bound specifically to ATTR amyloid deposits in a transgenic mouse model of the condition, and to synthetic ATTR amyloid. No such antibodies were present in the other 350 patients in the cohort with a typical clinical course.
“The cause and clinical significance of the anti-ATTR amyloid antibodies are intriguing and presently unclear. However, the clinical recovery of these patients establishes the unanticipated potential for reversibility of ATTR-CM and raises expectations for its treatment,” the researchers conclude.
Dr. Gillmore said they didn’t know why these three patients had these antibodies, while all the other patients did not. “There must be something different about these patients. We don’t know what that is at present, but we are looking hard.”
The researchers are hoping that after this publication, other centers caring for patients with ATTR-cardiomyopathy will look in their cohorts and see if they can identify other cases where there has been improvement.
“It is very plausible that they do have such cases, but they will be rare, as we all think of this disease as universally progressive and fatal,” Dr. Gillmore noted.
“We haven’t absolutely proven that the antibodies have caused the clearance of amyloid in these patients, but we strongly suspect this to be the case,” Dr. Gillmore said. The researchers are planning to try to confirm this by isolating the antibodies and treating the transgenic mice.
Dr. Gillmore attributed the current discovery to the development of novel imaging cardiac MRI techniques. “This allowed us to monitor closely the amyloid burden in the heart. The observation that this had diminished in these three patients was the breakthrough that led us to look for antibodies.”
Another antibody product directed against ATTR cardiomyopathy is also in development by Neurimmune, a Swiss biopharmaceutical company. A phase 1 study of this agent was recently published, suggesting that it appeared to reduce the amount of amyloid protein deposited in the heart.
Dr. Gillmore said the antibody they have detected is different from the Neurimmune product.
The research was supported by a British Heart Foundation Intermediate Clinical Research Fellowship, a Medical Research Council Career Development Award, and a project grant from the British Heart Foundation. Dr. Gillmore reports being a consultant or expert advisory board member for Alnylam Pharmaceuticals, AstraZeneca, ATTRalus, Eidos Therapeutics, Intellia Therapeutics, Ionis Pharmaceuticals, and Pfizer.
A version of this article originally appeared on Medscape.com.
Cardiac transthyretin amyloidosis (also called ATTR amyloidosis cardiomyopathy or ATTR-CM) is a progressive disease and a cause of heart failure resulting from accumulation of the protein transthyretin, which misfolds and forms amyloid deposits on the walls of the heart, causing both systolic and diastolic dysfunction.
The condition is progressive and normally fatal within a few years of diagnosis. Treatment options are limited and aimed at slowing progression; nothing has been shown to reverse the course of the disease.
However, an international team of researchers is now reporting the discovery of three patients with ATTR-CM–associated heart failure in whom the condition resolved spontaneously, with reversion to near normal cardiac structure and function. On further investigation, it was found that these three patients had developed circulating polyclonal IgG antibodies to human ATTR amyloid.
They are hopeful that a monoclonal form of these antibodies could be developed and may represent a novel treatment, or even a cure, for the condition.
The researchers report their findings in a letter to the New England Journal of Medicine.
“We are very optimistic about this discovery of these antibodies. They could become the first treatment to clear the amyloid that causes this horribly progressive and fatal condition,” senior author Julian Gillmore, MD, head of the University College London Centre for Amyloidosis, based at the Royal Free Hospital, said in an interview.
“Obviously, there is a lot of work to do before we can say this is the case, but it is very exciting,” he added.
Dr. Gillmore explained how the antibodies were discovered. “This disease has a universally progressive course, but we had one patient who on a repeat appointment said he felt better and on detailed cardiac MRI imaging, we found that the amyloid in his heart had reduced. That is totally unheard of,” he said.
“We then looked back at our cohort of 1,663 patients with ATTR-cardiomyopathy, and we discovered two others who had also improved both on imaging and clinically,” Dr. Gillmore said.
Each of these three patients reported a reduction in symptoms, although they had not received any new or potentially disease-modifying treatments. None of the patients had had recent vaccinations, notable infections, or any clinical suggestion of myocarditis.
Clinical recovery was corroborated by substantial improvement or normalization of findings on echocardiography, serum biomarker levels, and results of cardiopulmonary exercise tests and scintigraphy.
Serial cardiac MRI scans confirmed near-complete regression of myocardial extracellular volume, coupled with remodeling to near-normal cardiac structure and function without scarring.
The researchers wondered whether the changes in these patients may have been brought about by an antibody response. On further investigation, they found antibodies in the three patients that bound specifically to ATTR amyloid deposits in a transgenic mouse model of the condition, and to synthetic ATTR amyloid. No such antibodies were present in the other 350 patients in the cohort with a typical clinical course.
“The cause and clinical significance of the anti-ATTR amyloid antibodies are intriguing and presently unclear. However, the clinical recovery of these patients establishes the unanticipated potential for reversibility of ATTR-CM and raises expectations for its treatment,” the researchers conclude.
Dr. Gillmore said they didn’t know why these three patients had these antibodies, while all the other patients did not. “There must be something different about these patients. We don’t know what that is at present, but we are looking hard.”
The researchers are hoping that after this publication, other centers caring for patients with ATTR-cardiomyopathy will look in their cohorts and see if they can identify other cases where there has been improvement.
“It is very plausible that they do have such cases, but they will be rare, as we all think of this disease as universally progressive and fatal,” Dr. Gillmore noted.
“We haven’t absolutely proven that the antibodies have caused the clearance of amyloid in these patients, but we strongly suspect this to be the case,” Dr. Gillmore said. The researchers are planning to try to confirm this by isolating the antibodies and treating the transgenic mice.
Dr. Gillmore attributed the current discovery to the development of novel imaging cardiac MRI techniques. “This allowed us to monitor closely the amyloid burden in the heart. The observation that this had diminished in these three patients was the breakthrough that led us to look for antibodies.”
Another antibody product directed against ATTR cardiomyopathy is also in development by Neurimmune, a Swiss biopharmaceutical company. A phase 1 study of this agent was recently published, suggesting that it appeared to reduce the amount of amyloid protein deposited in the heart.
Dr. Gillmore said the antibody they have detected is different from the Neurimmune product.
The research was supported by a British Heart Foundation Intermediate Clinical Research Fellowship, a Medical Research Council Career Development Award, and a project grant from the British Heart Foundation. Dr. Gillmore reports being a consultant or expert advisory board member for Alnylam Pharmaceuticals, AstraZeneca, ATTRalus, Eidos Therapeutics, Intellia Therapeutics, Ionis Pharmaceuticals, and Pfizer.
A version of this article originally appeared on Medscape.com.
Cardiac transthyretin amyloidosis (also called ATTR amyloidosis cardiomyopathy or ATTR-CM) is a progressive disease and a cause of heart failure resulting from accumulation of the protein transthyretin, which misfolds and forms amyloid deposits on the walls of the heart, causing both systolic and diastolic dysfunction.
The condition is progressive and normally fatal within a few years of diagnosis. Treatment options are limited and aimed at slowing progression; nothing has been shown to reverse the course of the disease.
However, an international team of researchers is now reporting the discovery of three patients with ATTR-CM–associated heart failure in whom the condition resolved spontaneously, with reversion to near normal cardiac structure and function. On further investigation, it was found that these three patients had developed circulating polyclonal IgG antibodies to human ATTR amyloid.
They are hopeful that a monoclonal form of these antibodies could be developed and may represent a novel treatment, or even a cure, for the condition.
The researchers report their findings in a letter to the New England Journal of Medicine.
“We are very optimistic about this discovery of these antibodies. They could become the first treatment to clear the amyloid that causes this horribly progressive and fatal condition,” senior author Julian Gillmore, MD, head of the University College London Centre for Amyloidosis, based at the Royal Free Hospital, said in an interview.
“Obviously, there is a lot of work to do before we can say this is the case, but it is very exciting,” he added.
Dr. Gillmore explained how the antibodies were discovered. “This disease has a universally progressive course, but we had one patient who on a repeat appointment said he felt better and on detailed cardiac MRI imaging, we found that the amyloid in his heart had reduced. That is totally unheard of,” he said.
“We then looked back at our cohort of 1,663 patients with ATTR-cardiomyopathy, and we discovered two others who had also improved both on imaging and clinically,” Dr. Gillmore said.
Each of these three patients reported a reduction in symptoms, although they had not received any new or potentially disease-modifying treatments. None of the patients had had recent vaccinations, notable infections, or any clinical suggestion of myocarditis.
Clinical recovery was corroborated by substantial improvement or normalization of findings on echocardiography, serum biomarker levels, and results of cardiopulmonary exercise tests and scintigraphy.
Serial cardiac MRI scans confirmed near-complete regression of myocardial extracellular volume, coupled with remodeling to near-normal cardiac structure and function without scarring.
The researchers wondered whether the changes in these patients may have been brought about by an antibody response. On further investigation, they found antibodies in the three patients that bound specifically to ATTR amyloid deposits in a transgenic mouse model of the condition, and to synthetic ATTR amyloid. No such antibodies were present in the other 350 patients in the cohort with a typical clinical course.
“The cause and clinical significance of the anti-ATTR amyloid antibodies are intriguing and presently unclear. However, the clinical recovery of these patients establishes the unanticipated potential for reversibility of ATTR-CM and raises expectations for its treatment,” the researchers conclude.
Dr. Gillmore said they didn’t know why these three patients had these antibodies, while all the other patients did not. “There must be something different about these patients. We don’t know what that is at present, but we are looking hard.”
The researchers are hoping that after this publication, other centers caring for patients with ATTR-cardiomyopathy will look in their cohorts and see if they can identify other cases where there has been improvement.
“It is very plausible that they do have such cases, but they will be rare, as we all think of this disease as universally progressive and fatal,” Dr. Gillmore noted.
“We haven’t absolutely proven that the antibodies have caused the clearance of amyloid in these patients, but we strongly suspect this to be the case,” Dr. Gillmore said. The researchers are planning to try to confirm this by isolating the antibodies and treating the transgenic mice.
Dr. Gillmore attributed the current discovery to the development of novel imaging cardiac MRI techniques. “This allowed us to monitor closely the amyloid burden in the heart. The observation that this had diminished in these three patients was the breakthrough that led us to look for antibodies.”
Another antibody product directed against ATTR cardiomyopathy is also in development by Neurimmune, a Swiss biopharmaceutical company. A phase 1 study of this agent was recently published, suggesting that it appeared to reduce the amount of amyloid protein deposited in the heart.
Dr. Gillmore said the antibody they have detected is different from the Neurimmune product.
The research was supported by a British Heart Foundation Intermediate Clinical Research Fellowship, a Medical Research Council Career Development Award, and a project grant from the British Heart Foundation. Dr. Gillmore reports being a consultant or expert advisory board member for Alnylam Pharmaceuticals, AstraZeneca, ATTRalus, Eidos Therapeutics, Intellia Therapeutics, Ionis Pharmaceuticals, and Pfizer.
A version of this article originally appeared on Medscape.com.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Big boost in sodium excretion with HF diuretic protocol
In patients with acute heart failure, a urine sodium-guided diuretic protocol, currently recommended in guidelines from the Heart Failure Association of the European Society of Cardiology (HFA-ESC), led to significant increases in natriuresis and diuresis over 2 days in the prospective ENACT-HF clinical trial.
The guideline protocol was based on a 2019 HFA position paper with expert consensus, but it had not been tested prospectively, Jeroen Dauw, MD, of AZ Sint-Lucas Ghent (Belgium), explained in a presentation at HFA-ESC 2023.
“We had 282 millimoles of sodium excretion after one day, which is an increase of 64%, compared with standard of care,” Dr. Dauw told meeting attendees. “We wanted to power for 15%, so we’re way above it, with a P value of lower than 0.001.”
The effect was consistent across predefined subgroups, he said. “In addition, there’s an even higher benefit in patients with a lower eGFR [estimated glomerular filtration rate] and a higher home dose of loop diuretics, which might signal more diuretic resistance and more benefit of the protocol.”
After 2 days, the investigators saw 52% higher natriuresis and 33% higher diuresis, compared with usual care.
In an interview, Dr. Dauw said, “The protocol is feasible, safe, and very effective. Cardiologists might consider how to implement a similar protocol in their center to improve the care of their acute heart failure patients.”
Twice the oral home dose
The investigators conducted a multicenter, open-label, nonrandomized pragmatic trial at 29 centers in 18 countries globally. “We aimed to recruit 500 to detect a 15% difference in natriuresis,” Dr. Dauw said in his presentation, “but because we were a really low-budget trial, we had to stop after 3 years of recruitment.”
Therefore, 401 patients participated, 254 in the SOC arm and 147 in the protocol arm, because of the sequential nature of the study; that is, patients in the SOC arm of the two-phase study were recruited first.
Patients’ mean age was 70 years, 38% were women, and they all had at least one sign of volume overload. They were on a maintenance daily diuretic dose of 40 mg of furosemide for a month or more, and the NT-proBNP was above 1,000.
In phase 1 of the study, all centers treated 10 consecutive patients according to the local standard of care, at the discretion of the physician. In phase 2, the centers again recruited and treated at least 10 consecutive patients, this time according to the standardized diuretic protocol.
In the protocol phase, patients were treated with twice the oral home dose as an IV bolus. “This meant if, for example, you have 40 mg of furosemide at home, then you receive 80 mg as a first bolus,” Dr. Dauw told attendees. A spot urine sample was taken after 2 hours, and the response was evaluated after 6 hours. A urine sodium above 50 millimoles per liter was considered a good response.
On the second day, patients were reevaluated in the morning using urine output as a measure of diuretic response. If it was above 3 L, then the same bolus was repeated again twice daily, with 6-12 hours between administrations.
As noted, after one day, natriuresis was 174 millimoles in the SOC arm versus 282 millimoles in the protocol group – an increase of 64%. The effect was consistent across subgroups, and those with a lower eGFR and a higher home dose of loop diuretics benefited more.
Furthermore, Dr. Dauw said, there was no interaction on the endpoints with SGLT2 inhibitor use at baseline.
After two days, natriuresis was 52% higher in the protocol group and diuresis was 33% higher.
However, there was no significant difference in weight loss and no difference in the congestion score.
“We did expect to see a difference in weight loss between the study groups, as higher natriuresis and diuresis would normally be associated with higher weight loss in the protocol group,” Dr. Dauw told this news organization. “However, looking back at the study design, weight was collected from the electronic health records and not rigorously collected by study nurses. Previous studies have shown discrepancies between fluid loss and weight loss, so this is an ‘explainable’ finding.”
Participants also had a relatively high congestion score at baseline, with edema above the knee and also some pleural effusion, he told meeting attendees. Therefore, it might take more time to see a change in congestion score in those patients.
The protocol also led to a shorter length of stay – one day less in the hospital – and was very safe on renal endpoints, Dr. Dauw concluded.
A session chair asked why only patients already on diuretics were included in the study, noting that in his clinic, about half of the admissions are de novo.
Dr. Dauw said that patients already taking diuretics chronically would benefit most from the protocol. “If patients are diuretic-naive, they probably will respond well to whatever you do; if you just give a higher dose, they will respond well,” he said. “We expected that the largest benefit would be in patients already taking diuretics because they have a higher chance of not responding well.”
“There also was a big difference in the starting dose,” he added. “In the SOC arm, the baseline dose was about 60 mg, whereas we gave 120 mg, and we could already see a high difference in the effect. So, in those patients, I think the gain is bigger if you follow the protocol.”
More data coming
Looking ahead, “we only showed efficacy in the first 2 days of treatment and a shorter length of stay, probably reflecting a faster decongestion, but we don’t know for sure,” Dr. Dauw told this news organization.
“It would be important to have a study where the protocol is followed until full decongestion is reached,” he said. “That way, we can directly prove that decongestion is better and/or faster with the protocol.”
“A good decongestive strategy is one that is fast, safe and effective in decreasing signs and symptoms that patients suffer from,” he added. “We believe our protocol can achieve that, but our study is only one piece of the puzzle.”
More data on natriuresis-guided decongestion is coming this year, he said, with the PUSH-AHF study from Groningen, the European DECONGEST study, and the U.S. ESCALATE study.
The study had no funding. Dr. Dauw declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In patients with acute heart failure, a urine sodium-guided diuretic protocol, currently recommended in guidelines from the Heart Failure Association of the European Society of Cardiology (HFA-ESC), led to significant increases in natriuresis and diuresis over 2 days in the prospective ENACT-HF clinical trial.
The guideline protocol was based on a 2019 HFA position paper with expert consensus, but it had not been tested prospectively, Jeroen Dauw, MD, of AZ Sint-Lucas Ghent (Belgium), explained in a presentation at HFA-ESC 2023.
“We had 282 millimoles of sodium excretion after one day, which is an increase of 64%, compared with standard of care,” Dr. Dauw told meeting attendees. “We wanted to power for 15%, so we’re way above it, with a P value of lower than 0.001.”
The effect was consistent across predefined subgroups, he said. “In addition, there’s an even higher benefit in patients with a lower eGFR [estimated glomerular filtration rate] and a higher home dose of loop diuretics, which might signal more diuretic resistance and more benefit of the protocol.”
After 2 days, the investigators saw 52% higher natriuresis and 33% higher diuresis, compared with usual care.
In an interview, Dr. Dauw said, “The protocol is feasible, safe, and very effective. Cardiologists might consider how to implement a similar protocol in their center to improve the care of their acute heart failure patients.”
Twice the oral home dose
The investigators conducted a multicenter, open-label, nonrandomized pragmatic trial at 29 centers in 18 countries globally. “We aimed to recruit 500 to detect a 15% difference in natriuresis,” Dr. Dauw said in his presentation, “but because we were a really low-budget trial, we had to stop after 3 years of recruitment.”
Therefore, 401 patients participated, 254 in the SOC arm and 147 in the protocol arm, because of the sequential nature of the study; that is, patients in the SOC arm of the two-phase study were recruited first.
Patients’ mean age was 70 years, 38% were women, and they all had at least one sign of volume overload. They were on a maintenance daily diuretic dose of 40 mg of furosemide for a month or more, and the NT-proBNP was above 1,000.
In phase 1 of the study, all centers treated 10 consecutive patients according to the local standard of care, at the discretion of the physician. In phase 2, the centers again recruited and treated at least 10 consecutive patients, this time according to the standardized diuretic protocol.
In the protocol phase, patients were treated with twice the oral home dose as an IV bolus. “This meant if, for example, you have 40 mg of furosemide at home, then you receive 80 mg as a first bolus,” Dr. Dauw told attendees. A spot urine sample was taken after 2 hours, and the response was evaluated after 6 hours. A urine sodium above 50 millimoles per liter was considered a good response.
On the second day, patients were reevaluated in the morning using urine output as a measure of diuretic response. If it was above 3 L, then the same bolus was repeated again twice daily, with 6-12 hours between administrations.
As noted, after one day, natriuresis was 174 millimoles in the SOC arm versus 282 millimoles in the protocol group – an increase of 64%. The effect was consistent across subgroups, and those with a lower eGFR and a higher home dose of loop diuretics benefited more.
Furthermore, Dr. Dauw said, there was no interaction on the endpoints with SGLT2 inhibitor use at baseline.
After two days, natriuresis was 52% higher in the protocol group and diuresis was 33% higher.
However, there was no significant difference in weight loss and no difference in the congestion score.
“We did expect to see a difference in weight loss between the study groups, as higher natriuresis and diuresis would normally be associated with higher weight loss in the protocol group,” Dr. Dauw told this news organization. “However, looking back at the study design, weight was collected from the electronic health records and not rigorously collected by study nurses. Previous studies have shown discrepancies between fluid loss and weight loss, so this is an ‘explainable’ finding.”
Participants also had a relatively high congestion score at baseline, with edema above the knee and also some pleural effusion, he told meeting attendees. Therefore, it might take more time to see a change in congestion score in those patients.
The protocol also led to a shorter length of stay – one day less in the hospital – and was very safe on renal endpoints, Dr. Dauw concluded.
A session chair asked why only patients already on diuretics were included in the study, noting that in his clinic, about half of the admissions are de novo.
Dr. Dauw said that patients already taking diuretics chronically would benefit most from the protocol. “If patients are diuretic-naive, they probably will respond well to whatever you do; if you just give a higher dose, they will respond well,” he said. “We expected that the largest benefit would be in patients already taking diuretics because they have a higher chance of not responding well.”
“There also was a big difference in the starting dose,” he added. “In the SOC arm, the baseline dose was about 60 mg, whereas we gave 120 mg, and we could already see a high difference in the effect. So, in those patients, I think the gain is bigger if you follow the protocol.”
More data coming
Looking ahead, “we only showed efficacy in the first 2 days of treatment and a shorter length of stay, probably reflecting a faster decongestion, but we don’t know for sure,” Dr. Dauw told this news organization.
“It would be important to have a study where the protocol is followed until full decongestion is reached,” he said. “That way, we can directly prove that decongestion is better and/or faster with the protocol.”
“A good decongestive strategy is one that is fast, safe and effective in decreasing signs and symptoms that patients suffer from,” he added. “We believe our protocol can achieve that, but our study is only one piece of the puzzle.”
More data on natriuresis-guided decongestion is coming this year, he said, with the PUSH-AHF study from Groningen, the European DECONGEST study, and the U.S. ESCALATE study.
The study had no funding. Dr. Dauw declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In patients with acute heart failure, a urine sodium-guided diuretic protocol, currently recommended in guidelines from the Heart Failure Association of the European Society of Cardiology (HFA-ESC), led to significant increases in natriuresis and diuresis over 2 days in the prospective ENACT-HF clinical trial.
The guideline protocol was based on a 2019 HFA position paper with expert consensus, but it had not been tested prospectively, Jeroen Dauw, MD, of AZ Sint-Lucas Ghent (Belgium), explained in a presentation at HFA-ESC 2023.
“We had 282 millimoles of sodium excretion after one day, which is an increase of 64%, compared with standard of care,” Dr. Dauw told meeting attendees. “We wanted to power for 15%, so we’re way above it, with a P value of lower than 0.001.”
The effect was consistent across predefined subgroups, he said. “In addition, there’s an even higher benefit in patients with a lower eGFR [estimated glomerular filtration rate] and a higher home dose of loop diuretics, which might signal more diuretic resistance and more benefit of the protocol.”
After 2 days, the investigators saw 52% higher natriuresis and 33% higher diuresis, compared with usual care.
In an interview, Dr. Dauw said, “The protocol is feasible, safe, and very effective. Cardiologists might consider how to implement a similar protocol in their center to improve the care of their acute heart failure patients.”
Twice the oral home dose
The investigators conducted a multicenter, open-label, nonrandomized pragmatic trial at 29 centers in 18 countries globally. “We aimed to recruit 500 to detect a 15% difference in natriuresis,” Dr. Dauw said in his presentation, “but because we were a really low-budget trial, we had to stop after 3 years of recruitment.”
Therefore, 401 patients participated, 254 in the SOC arm and 147 in the protocol arm, because of the sequential nature of the study; that is, patients in the SOC arm of the two-phase study were recruited first.
Patients’ mean age was 70 years, 38% were women, and they all had at least one sign of volume overload. They were on a maintenance daily diuretic dose of 40 mg of furosemide for a month or more, and the NT-proBNP was above 1,000.
In phase 1 of the study, all centers treated 10 consecutive patients according to the local standard of care, at the discretion of the physician. In phase 2, the centers again recruited and treated at least 10 consecutive patients, this time according to the standardized diuretic protocol.
In the protocol phase, patients were treated with twice the oral home dose as an IV bolus. “This meant if, for example, you have 40 mg of furosemide at home, then you receive 80 mg as a first bolus,” Dr. Dauw told attendees. A spot urine sample was taken after 2 hours, and the response was evaluated after 6 hours. A urine sodium above 50 millimoles per liter was considered a good response.
On the second day, patients were reevaluated in the morning using urine output as a measure of diuretic response. If it was above 3 L, then the same bolus was repeated again twice daily, with 6-12 hours between administrations.
As noted, after one day, natriuresis was 174 millimoles in the SOC arm versus 282 millimoles in the protocol group – an increase of 64%. The effect was consistent across subgroups, and those with a lower eGFR and a higher home dose of loop diuretics benefited more.
Furthermore, Dr. Dauw said, there was no interaction on the endpoints with SGLT2 inhibitor use at baseline.
After two days, natriuresis was 52% higher in the protocol group and diuresis was 33% higher.
However, there was no significant difference in weight loss and no difference in the congestion score.
“We did expect to see a difference in weight loss between the study groups, as higher natriuresis and diuresis would normally be associated with higher weight loss in the protocol group,” Dr. Dauw told this news organization. “However, looking back at the study design, weight was collected from the electronic health records and not rigorously collected by study nurses. Previous studies have shown discrepancies between fluid loss and weight loss, so this is an ‘explainable’ finding.”
Participants also had a relatively high congestion score at baseline, with edema above the knee and also some pleural effusion, he told meeting attendees. Therefore, it might take more time to see a change in congestion score in those patients.
The protocol also led to a shorter length of stay – one day less in the hospital – and was very safe on renal endpoints, Dr. Dauw concluded.
A session chair asked why only patients already on diuretics were included in the study, noting that in his clinic, about half of the admissions are de novo.
Dr. Dauw said that patients already taking diuretics chronically would benefit most from the protocol. “If patients are diuretic-naive, they probably will respond well to whatever you do; if you just give a higher dose, they will respond well,” he said. “We expected that the largest benefit would be in patients already taking diuretics because they have a higher chance of not responding well.”
“There also was a big difference in the starting dose,” he added. “In the SOC arm, the baseline dose was about 60 mg, whereas we gave 120 mg, and we could already see a high difference in the effect. So, in those patients, I think the gain is bigger if you follow the protocol.”
More data coming
Looking ahead, “we only showed efficacy in the first 2 days of treatment and a shorter length of stay, probably reflecting a faster decongestion, but we don’t know for sure,” Dr. Dauw told this news organization.
“It would be important to have a study where the protocol is followed until full decongestion is reached,” he said. “That way, we can directly prove that decongestion is better and/or faster with the protocol.”
“A good decongestive strategy is one that is fast, safe and effective in decreasing signs and symptoms that patients suffer from,” he added. “We believe our protocol can achieve that, but our study is only one piece of the puzzle.”
More data on natriuresis-guided decongestion is coming this year, he said, with the PUSH-AHF study from Groningen, the European DECONGEST study, and the U.S. ESCALATE study.
The study had no funding. Dr. Dauw declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM HFA-ESC 2023
First-line or BiV backup? Conduction system pacing for CRT in heart failure
Pacing as a device therapy for heart failure (HF) is headed for what is probably its next big advance.
After decades of biventricular (BiV) pacemaker success in resynchronizing the ventricles and improving clinical outcomes, relatively new conduction-system pacing (CSP) techniques that avoid the pitfalls of right-ventricular (RV) pacing using BiV lead systems have been supplanting traditional cardiac resynchronization therapy (CRT) in selected patients at some major centers. In fact, they are solidly ensconced in a new guideline document addressing indications for CSP and BiV pacing in HF.
But , an alternative when BiV pacing isn’t appropriate or can’t be engaged.
That’s mainly because the limited, mostly observational evidence supporting CSP in the document can’t measure up to the clinical experience and plethora of large, randomized trials behind BiV-CRT.
But that shortfall is headed for change. Several new comparative studies, including a small, randomized trial, have added significantly to evidence suggesting that CSP is at least as effective as traditional CRT for procedural, functional safety, and clinical outcomes.
The new studies “are inherently prone to bias, but their results are really good,” observed Juan C. Diaz, MD. They show improvements in left ventricular ejection fraction (LVEF) and symptoms with CSP that are “outstanding compared to what we have been doing for the last 20 years,” he said in an interview.
Dr. Diaz, Clínica Las Vegas, Medellin, Colombia, is an investigator with the observational SYNCHRONY, which is among the new CSP studies formally presented at the annual scientific sessions of the Heart Rhythm Society. He is also lead author on its same-day publication in JACC: Clinical Electrophysiology.
Dr. Diaz said that CSP, which sustains pacing via the native conduction system, makes more “physiologic sense” than BiV pacing and represents “a step forward” for HF device therapy.
SYNCHRONY compared LBB-area with BiV pacing as the initial strategy for achieving cardiac resynchronization in patients with ischemic or nonischemic cardiomyopathy.
CSP is “a long way” from replacing conventional CRT, he said. But the new studies at the HRS sessions should help extend His-bundle and LBB-area pacing to more patients, he added, given the significant long-term “drawbacks” of BiV pacing. These include inevitable RV pacing, multiple leads, and the risks associated with chronic transvenous leads.
Zachary Goldberger, MD, University of Wisconsin–Madison, went a bit further in support of CSP as invited discussant for the SYNCHRONY presentation.
Given that it improved LVEF, heart failure class, HF hospitalizations (HFH), and mortality in that study and others, Dr. Goldberger said, CSP could potentially “become the dominant mode of resynchronization going forward.”
Other experts at the meeting saw CSP’s potential more as one of several pacing techniques that could be brought to bear for patients with CRT indications.
“Conduction system pacing is going to be a huge complement to biventricular pacing,” to which about 30% of patients have a “less than optimal response,” said Pugazhendhi Vijayaraman, MD, chief of clinical electrophysiology, Geisinger Heart Institute, Danville, Pa.
“I don’t think it needs to replace biventricular pacing, because biventricular pacing is a well-established, incredibly powerful therapy,” he told this news organization. But CSP is likely to provide “a good alternative option” in patients with poor responses to BiV-CRT.
It may, however, render some current BiV-pacing alternatives “obsolete,” Dr. Vijayaraman observed. “At our center, at least for the last 5 years, no patient has needed epicardial surgical left ventricular lead placement” because CSP was a better backup option.
Dr. Vijayaraman presented two of the meeting’s CSP vs. BiV pacing comparisons. In one, the 100-patient randomized HOT-CRT trial, contractile function improved significantly on CSP, which could be either His-bundle or LBB-area pacing.
He also presented an observational study of LBB-area pacing at 15 centers in Asia, Europe, and North America and led the authors of its simultaneous publication in the Journal of the American College of Cardiology.
“I think left-bundle conduction system pacing is the future, for sure,” Jagmeet P. Singh, MD, DPhil, told this news organization. Still, it doesn’t always work and when it does, it “doesn’t work equally in all patients,” he said.
“Conduction system pacing certainly makes a lot of sense,” especially in patients with left-bundle-branch block (LBBB), and “maybe not as a primary approach but certainly as a secondary approach,” said Dr. Singh, Massachusetts General Hospital, Boston, who is not a coauthor on any of the three studies.
He acknowledged that CSP may work well as a first-line option in patients with LBBB at some experienced centers. For those without LBBB or who have an intraventricular conduction delay, who represent 45%-50% of current CRT cases, Dr. Singh observed, “there’s still more evidence” that BiV-CRT is a more appropriate initial approach.
Standard CRT may fail, however, even in some patients who otherwise meet guideline-based indications. “We don’t really understand all the mechanisms for nonresponse in conventional biventricular pacing,” observed Niraj Varma, MD, PhD, Cleveland Clinic, also not involved with any of the three studies.
In some groups, including “patients with larger ventricles,” for example, BiV-CRT doesn’t always narrow the electrocardiographic QRS complex or preexcite delayed left ventricular (LV) activation, hallmarks of successful CRT, he said in an interview.
“I think we need to understand why this occurs in both situations,” but in such cases, CSP alone or as an adjunct to direct LV pacing may be successful. “Sometimes we need both an LV lead and the conduction-system pacing lead.”
Narrower, more efficient use of CSP as a BiV-CRT alternative may also boost its chances for success, Dr. Varma added. “I think we need to refine patient selection.”
HOT-CRT: Randomized CSP vs. BiV pacing trial
Conducted at three centers in a single health system, the His-optimized cardiac resynchronization therapy study (HOT-CRT) randomly assigned 100 patients with primary or secondary CRT indications to either to CSP – by either His-bundle or LBB-area pacing – or to standard BiV-CRT as the first-line resynchronization method.
Treatment crossovers, allowed for either pacing modality in the event of implantation failure, occurred in two patients and nine patients initially assigned to CSP and BiV pacing, respectively (4% vs. 18%), Dr. Vijayaraman reported.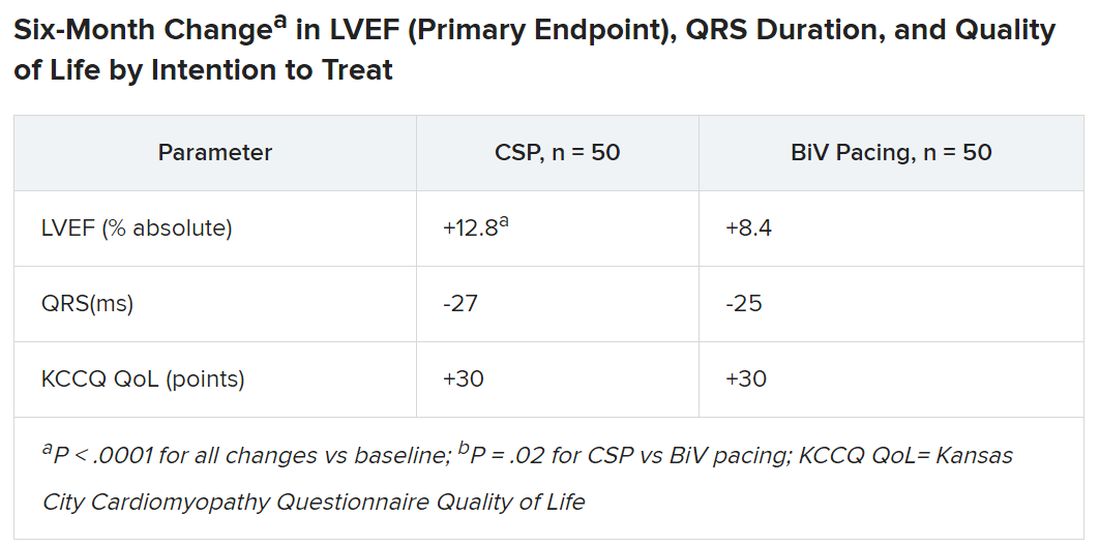
Historically in trials, BiV pacing has elevated LVEF by about 7%, he said. The mean 12-point increase observed with CSP “is huge, in that sense.” HOT-CRT enrolled a predominantly male and White population at centers highly experienced in both CSP and BiV pacing, limiting its broad relevance to practice, as pointed out by both Dr. Vijayaraman and his presentation’s invited discussant, Yong-Mei Cha, MD, Mayo Clinic, Rochester, Minn. Dr. Cha, who is director of cardiac device services at her center, also highlighted the greater rate of crossover from BiV pacing to CSP, 18% vs. 4% in the other direction. “This is a very encouraging result,” because the implant-failure rate for LBB-area pacing may drop once more operators become “familiar and skilled with conduction-system pacing.” Overall, the study supports CSP as “a very good alternative for heart failure patients when BiV pacing fails.”
International comparison of CSP and BiV pacing
In Dr. Vijayaraman’s other study, the observational comparison of LBB-area pacing and BiV-CRT, the CSP technique emerged as a “reasonable alternative to biventricular pacing, not only for improvement in LV function but also to reduce adverse clinical outcomes.”
Indeed, in the international study of 1,778 mostly male patients with primary or secondary CRT indications who received LBB-area or BiV pacing (797 and 981 patients, respectively), those on CSP saw a significant drop in risk for the primary endpoint, death or HFH.
Mean LVEF improved from 27% to 41% in the LBB-area pacing group and 27% to 37% with BiV pacing (P < .001 for both changes) over a follow-up averaging 33 months. The difference in improvement between CSP and BiV pacing was significant at P < .001.
In adjusted analysis, the risk for death or HFH was greater for BiV-pacing patients, a difference driven by HFH events.
- Death or HF: hazard ratio, 1.49 (95% confidence interval, 1.21-1.84; P < .001).
- Death: HR, 1.14 (95% CI, 0.88-1.48; P = .313).
- HFH: HR, 1.49 (95% CI, 1.16-1.92; P = .002)
The analysis has all the “inherent biases” of an observational study. The risk for patient-selection bias, however, was somewhat mitigated by consistent practice patterns at participating centers, Dr. Vijayaraman told this news organization.
For example, he said, operators at six of the institutions were most likely to use CSP as the first-line approach, and the same number of centers usually went with BiV pacing.
SYNCHRONY: First-line LBB-area pacing vs. BiV-CRT
Outcomes using the two approaches were similar in the prospective, international, observational study of 371 patients with ischemic or nonischemic cardiomyopathy and standard CRT indications. Allocation of 128 patients to LBB-area pacing and 243 to BiV-CRT was based on patient and operator preferences, reported Jorge Romero Jr, MD, Brigham and Women’s Hospital, Boston, at the HRS sessions.
Risk for the death-HFH primary endpoint dropped 38% for those initially treated with LBB-area pacing, compared with BiV pacing, primarily because of a lower HFH risk:
- Death or HFH: HR, 0.62 (95% CI, 0.41-0.93; P = .02).
- Death: HR, 0.57 (95% CI, 0.25-1.32; P = .19).
- HFH: HR, 0.61 (95% CI, 0.34-0.93; P = .02)
Patients in the CSP group were also more likely to improve by at least one NYHA (New York Heart Association) class (80.4% vs. 67.9%; P < .001), consistent with their greater absolute change in LVEF (8.0 vs. 3.9 points; P < .01).
The findings “suggest that LBBAP [left-bundle branch area pacing] is an excellent alternative to BiV pacing,” with a comparable safety profile, write Jayanthi N. Koneru, MBBS, and Kenneth A. Ellenbogen, MD, in an editorial accompanying the published SYNCHRONY report.
“The differences in improvement of LVEF are encouraging for both groups,” but were superior for LBB-area pacing, continue Dr. Koneru and Dr. Ellenbogen, both with Virginia Commonwealth University Medical Center, Richmond. “Whether these results would have regressed to the mean over a longer period of follow-up or diverge further with LBB-area pacing continuing to be superior is unknown.”
Years for an answer?
A large randomized comparison of CSP and BiV-CRT, called Left vs. Left, is currently in early stages, Sana M. Al-Khatib, MD, MHS, Duke University Medical Center, Durham, N.C., said in a media presentation on two of the presented studies. It has a planned enrollment of more than 2,100 patients on optimal meds with an LVEF of 50% or lower and either a QRS duration of at least 130 ms or an anticipated burden of RV pacing exceeding 40%.
The trial, she said, “will take years to give an answer, but it is actually designed to address the question of whether a composite endpoint of time to death or heart failure hospitalization can be improved with conduction system pacing vs. biventricular pacing.”
Dr. Al-Khatib is a coauthor on the new guideline covering both CSP and BiV-CRT in HF, as are Dr. Cha, Dr. Varma, Dr. Singh, Dr. Vijayaraman, and Dr. Goldberger; Dr. Ellenbogen is one of the reviewers.
Dr. Diaz discloses receiving honoraria or fees for speaking or teaching from Bayer Healthcare, Pfizer, AstraZeneca, Boston Scientific, and Medtronic. Dr. Vijayaraman discloses receiving honoraria or fees for speaking, teaching, or consulting for Abbott, Medtronic, Biotronik, and Boston Scientific; and receiving research grants from Medtronic. Dr. Varma discloses receiving honoraria or fees for speaking or consulting as an independent contractor for Medtronic, Boston Scientific, Biotronik, Impulse Dynamics USA, Cardiologs, Abbott, Pacemate, Implicity, and EP Solutions. Dr. Singh discloses receiving fees for consulting from EBR Systems, Merit Medical Systems, New Century Health, Biotronik, Abbott, Medtronic, MicroPort Scientific, Cardiologs, Sanofi, CVRx, Impulse Dynamics USA, Octagos, Implicity, Orchestra Biomed, Rhythm Management Group, and Biosense Webster; and receiving honoraria or fees for speaking and teaching from Medscape. Dr. Cha had no relevant financial relationships. Dr. Romero discloses receiving research grants from Biosense Webster; and speaking or receiving honoraria or fees for consulting, speaking, or teaching, or serving on a board for Sanofi, Boston Scientific, and AtriCure. Dr. Koneru discloses consulting for Medtronic and receiving honoraria from Abbott. Dr. Ellenbogen discloses consulting or lecturing for or receiving honoraria from Medtronic, Boston Scientific, and Abbott. Dr. Goldberger discloses receiving royalty income from and serving as an independent contractor for Elsevier. Dr. Al-Khatib discloses receiving research grants from Medtronic and Boston Scientific.
A version of this article first appeared on Medscape.com.
Pacing as a device therapy for heart failure (HF) is headed for what is probably its next big advance.
After decades of biventricular (BiV) pacemaker success in resynchronizing the ventricles and improving clinical outcomes, relatively new conduction-system pacing (CSP) techniques that avoid the pitfalls of right-ventricular (RV) pacing using BiV lead systems have been supplanting traditional cardiac resynchronization therapy (CRT) in selected patients at some major centers. In fact, they are solidly ensconced in a new guideline document addressing indications for CSP and BiV pacing in HF.
But , an alternative when BiV pacing isn’t appropriate or can’t be engaged.
That’s mainly because the limited, mostly observational evidence supporting CSP in the document can’t measure up to the clinical experience and plethora of large, randomized trials behind BiV-CRT.
But that shortfall is headed for change. Several new comparative studies, including a small, randomized trial, have added significantly to evidence suggesting that CSP is at least as effective as traditional CRT for procedural, functional safety, and clinical outcomes.
The new studies “are inherently prone to bias, but their results are really good,” observed Juan C. Diaz, MD. They show improvements in left ventricular ejection fraction (LVEF) and symptoms with CSP that are “outstanding compared to what we have been doing for the last 20 years,” he said in an interview.
Dr. Diaz, Clínica Las Vegas, Medellin, Colombia, is an investigator with the observational SYNCHRONY, which is among the new CSP studies formally presented at the annual scientific sessions of the Heart Rhythm Society. He is also lead author on its same-day publication in JACC: Clinical Electrophysiology.
Dr. Diaz said that CSP, which sustains pacing via the native conduction system, makes more “physiologic sense” than BiV pacing and represents “a step forward” for HF device therapy.
SYNCHRONY compared LBB-area with BiV pacing as the initial strategy for achieving cardiac resynchronization in patients with ischemic or nonischemic cardiomyopathy.
CSP is “a long way” from replacing conventional CRT, he said. But the new studies at the HRS sessions should help extend His-bundle and LBB-area pacing to more patients, he added, given the significant long-term “drawbacks” of BiV pacing. These include inevitable RV pacing, multiple leads, and the risks associated with chronic transvenous leads.
Zachary Goldberger, MD, University of Wisconsin–Madison, went a bit further in support of CSP as invited discussant for the SYNCHRONY presentation.
Given that it improved LVEF, heart failure class, HF hospitalizations (HFH), and mortality in that study and others, Dr. Goldberger said, CSP could potentially “become the dominant mode of resynchronization going forward.”
Other experts at the meeting saw CSP’s potential more as one of several pacing techniques that could be brought to bear for patients with CRT indications.
“Conduction system pacing is going to be a huge complement to biventricular pacing,” to which about 30% of patients have a “less than optimal response,” said Pugazhendhi Vijayaraman, MD, chief of clinical electrophysiology, Geisinger Heart Institute, Danville, Pa.
“I don’t think it needs to replace biventricular pacing, because biventricular pacing is a well-established, incredibly powerful therapy,” he told this news organization. But CSP is likely to provide “a good alternative option” in patients with poor responses to BiV-CRT.
It may, however, render some current BiV-pacing alternatives “obsolete,” Dr. Vijayaraman observed. “At our center, at least for the last 5 years, no patient has needed epicardial surgical left ventricular lead placement” because CSP was a better backup option.
Dr. Vijayaraman presented two of the meeting’s CSP vs. BiV pacing comparisons. In one, the 100-patient randomized HOT-CRT trial, contractile function improved significantly on CSP, which could be either His-bundle or LBB-area pacing.
He also presented an observational study of LBB-area pacing at 15 centers in Asia, Europe, and North America and led the authors of its simultaneous publication in the Journal of the American College of Cardiology.
“I think left-bundle conduction system pacing is the future, for sure,” Jagmeet P. Singh, MD, DPhil, told this news organization. Still, it doesn’t always work and when it does, it “doesn’t work equally in all patients,” he said.
“Conduction system pacing certainly makes a lot of sense,” especially in patients with left-bundle-branch block (LBBB), and “maybe not as a primary approach but certainly as a secondary approach,” said Dr. Singh, Massachusetts General Hospital, Boston, who is not a coauthor on any of the three studies.
He acknowledged that CSP may work well as a first-line option in patients with LBBB at some experienced centers. For those without LBBB or who have an intraventricular conduction delay, who represent 45%-50% of current CRT cases, Dr. Singh observed, “there’s still more evidence” that BiV-CRT is a more appropriate initial approach.
Standard CRT may fail, however, even in some patients who otherwise meet guideline-based indications. “We don’t really understand all the mechanisms for nonresponse in conventional biventricular pacing,” observed Niraj Varma, MD, PhD, Cleveland Clinic, also not involved with any of the three studies.
In some groups, including “patients with larger ventricles,” for example, BiV-CRT doesn’t always narrow the electrocardiographic QRS complex or preexcite delayed left ventricular (LV) activation, hallmarks of successful CRT, he said in an interview.
“I think we need to understand why this occurs in both situations,” but in such cases, CSP alone or as an adjunct to direct LV pacing may be successful. “Sometimes we need both an LV lead and the conduction-system pacing lead.”
Narrower, more efficient use of CSP as a BiV-CRT alternative may also boost its chances for success, Dr. Varma added. “I think we need to refine patient selection.”
HOT-CRT: Randomized CSP vs. BiV pacing trial
Conducted at three centers in a single health system, the His-optimized cardiac resynchronization therapy study (HOT-CRT) randomly assigned 100 patients with primary or secondary CRT indications to either to CSP – by either His-bundle or LBB-area pacing – or to standard BiV-CRT as the first-line resynchronization method.
Treatment crossovers, allowed for either pacing modality in the event of implantation failure, occurred in two patients and nine patients initially assigned to CSP and BiV pacing, respectively (4% vs. 18%), Dr. Vijayaraman reported.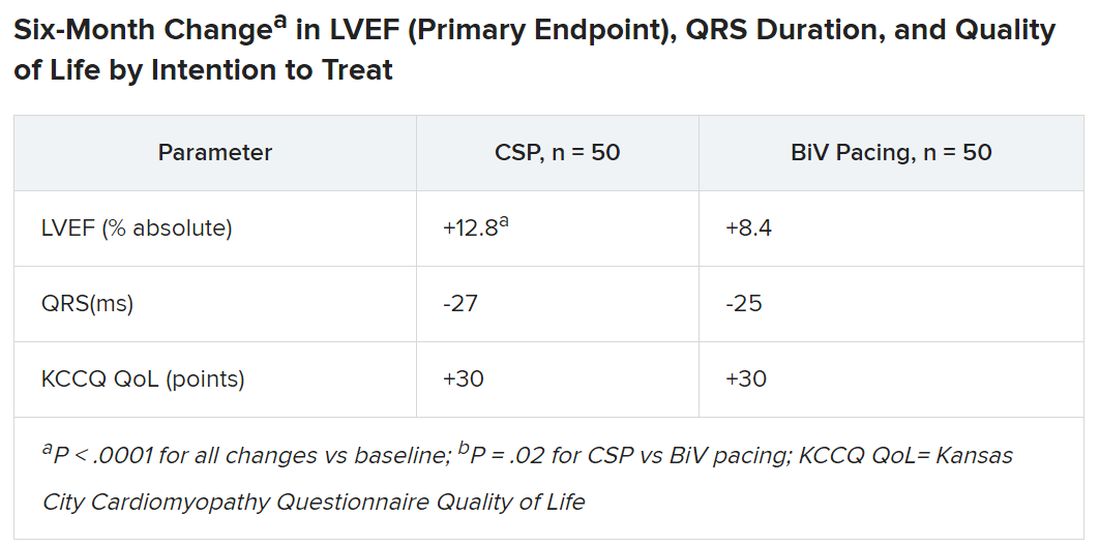
Historically in trials, BiV pacing has elevated LVEF by about 7%, he said. The mean 12-point increase observed with CSP “is huge, in that sense.” HOT-CRT enrolled a predominantly male and White population at centers highly experienced in both CSP and BiV pacing, limiting its broad relevance to practice, as pointed out by both Dr. Vijayaraman and his presentation’s invited discussant, Yong-Mei Cha, MD, Mayo Clinic, Rochester, Minn. Dr. Cha, who is director of cardiac device services at her center, also highlighted the greater rate of crossover from BiV pacing to CSP, 18% vs. 4% in the other direction. “This is a very encouraging result,” because the implant-failure rate for LBB-area pacing may drop once more operators become “familiar and skilled with conduction-system pacing.” Overall, the study supports CSP as “a very good alternative for heart failure patients when BiV pacing fails.”
International comparison of CSP and BiV pacing
In Dr. Vijayaraman’s other study, the observational comparison of LBB-area pacing and BiV-CRT, the CSP technique emerged as a “reasonable alternative to biventricular pacing, not only for improvement in LV function but also to reduce adverse clinical outcomes.”
Indeed, in the international study of 1,778 mostly male patients with primary or secondary CRT indications who received LBB-area or BiV pacing (797 and 981 patients, respectively), those on CSP saw a significant drop in risk for the primary endpoint, death or HFH.
Mean LVEF improved from 27% to 41% in the LBB-area pacing group and 27% to 37% with BiV pacing (P < .001 for both changes) over a follow-up averaging 33 months. The difference in improvement between CSP and BiV pacing was significant at P < .001.
In adjusted analysis, the risk for death or HFH was greater for BiV-pacing patients, a difference driven by HFH events.
- Death or HF: hazard ratio, 1.49 (95% confidence interval, 1.21-1.84; P < .001).
- Death: HR, 1.14 (95% CI, 0.88-1.48; P = .313).
- HFH: HR, 1.49 (95% CI, 1.16-1.92; P = .002)
The analysis has all the “inherent biases” of an observational study. The risk for patient-selection bias, however, was somewhat mitigated by consistent practice patterns at participating centers, Dr. Vijayaraman told this news organization.
For example, he said, operators at six of the institutions were most likely to use CSP as the first-line approach, and the same number of centers usually went with BiV pacing.
SYNCHRONY: First-line LBB-area pacing vs. BiV-CRT
Outcomes using the two approaches were similar in the prospective, international, observational study of 371 patients with ischemic or nonischemic cardiomyopathy and standard CRT indications. Allocation of 128 patients to LBB-area pacing and 243 to BiV-CRT was based on patient and operator preferences, reported Jorge Romero Jr, MD, Brigham and Women’s Hospital, Boston, at the HRS sessions.
Risk for the death-HFH primary endpoint dropped 38% for those initially treated with LBB-area pacing, compared with BiV pacing, primarily because of a lower HFH risk:
- Death or HFH: HR, 0.62 (95% CI, 0.41-0.93; P = .02).
- Death: HR, 0.57 (95% CI, 0.25-1.32; P = .19).
- HFH: HR, 0.61 (95% CI, 0.34-0.93; P = .02)
Patients in the CSP group were also more likely to improve by at least one NYHA (New York Heart Association) class (80.4% vs. 67.9%; P < .001), consistent with their greater absolute change in LVEF (8.0 vs. 3.9 points; P < .01).
The findings “suggest that LBBAP [left-bundle branch area pacing] is an excellent alternative to BiV pacing,” with a comparable safety profile, write Jayanthi N. Koneru, MBBS, and Kenneth A. Ellenbogen, MD, in an editorial accompanying the published SYNCHRONY report.
“The differences in improvement of LVEF are encouraging for both groups,” but were superior for LBB-area pacing, continue Dr. Koneru and Dr. Ellenbogen, both with Virginia Commonwealth University Medical Center, Richmond. “Whether these results would have regressed to the mean over a longer period of follow-up or diverge further with LBB-area pacing continuing to be superior is unknown.”
Years for an answer?
A large randomized comparison of CSP and BiV-CRT, called Left vs. Left, is currently in early stages, Sana M. Al-Khatib, MD, MHS, Duke University Medical Center, Durham, N.C., said in a media presentation on two of the presented studies. It has a planned enrollment of more than 2,100 patients on optimal meds with an LVEF of 50% or lower and either a QRS duration of at least 130 ms or an anticipated burden of RV pacing exceeding 40%.
The trial, she said, “will take years to give an answer, but it is actually designed to address the question of whether a composite endpoint of time to death or heart failure hospitalization can be improved with conduction system pacing vs. biventricular pacing.”
Dr. Al-Khatib is a coauthor on the new guideline covering both CSP and BiV-CRT in HF, as are Dr. Cha, Dr. Varma, Dr. Singh, Dr. Vijayaraman, and Dr. Goldberger; Dr. Ellenbogen is one of the reviewers.
Dr. Diaz discloses receiving honoraria or fees for speaking or teaching from Bayer Healthcare, Pfizer, AstraZeneca, Boston Scientific, and Medtronic. Dr. Vijayaraman discloses receiving honoraria or fees for speaking, teaching, or consulting for Abbott, Medtronic, Biotronik, and Boston Scientific; and receiving research grants from Medtronic. Dr. Varma discloses receiving honoraria or fees for speaking or consulting as an independent contractor for Medtronic, Boston Scientific, Biotronik, Impulse Dynamics USA, Cardiologs, Abbott, Pacemate, Implicity, and EP Solutions. Dr. Singh discloses receiving fees for consulting from EBR Systems, Merit Medical Systems, New Century Health, Biotronik, Abbott, Medtronic, MicroPort Scientific, Cardiologs, Sanofi, CVRx, Impulse Dynamics USA, Octagos, Implicity, Orchestra Biomed, Rhythm Management Group, and Biosense Webster; and receiving honoraria or fees for speaking and teaching from Medscape. Dr. Cha had no relevant financial relationships. Dr. Romero discloses receiving research grants from Biosense Webster; and speaking or receiving honoraria or fees for consulting, speaking, or teaching, or serving on a board for Sanofi, Boston Scientific, and AtriCure. Dr. Koneru discloses consulting for Medtronic and receiving honoraria from Abbott. Dr. Ellenbogen discloses consulting or lecturing for or receiving honoraria from Medtronic, Boston Scientific, and Abbott. Dr. Goldberger discloses receiving royalty income from and serving as an independent contractor for Elsevier. Dr. Al-Khatib discloses receiving research grants from Medtronic and Boston Scientific.
A version of this article first appeared on Medscape.com.
Pacing as a device therapy for heart failure (HF) is headed for what is probably its next big advance.
After decades of biventricular (BiV) pacemaker success in resynchronizing the ventricles and improving clinical outcomes, relatively new conduction-system pacing (CSP) techniques that avoid the pitfalls of right-ventricular (RV) pacing using BiV lead systems have been supplanting traditional cardiac resynchronization therapy (CRT) in selected patients at some major centers. In fact, they are solidly ensconced in a new guideline document addressing indications for CSP and BiV pacing in HF.
But , an alternative when BiV pacing isn’t appropriate or can’t be engaged.
That’s mainly because the limited, mostly observational evidence supporting CSP in the document can’t measure up to the clinical experience and plethora of large, randomized trials behind BiV-CRT.
But that shortfall is headed for change. Several new comparative studies, including a small, randomized trial, have added significantly to evidence suggesting that CSP is at least as effective as traditional CRT for procedural, functional safety, and clinical outcomes.
The new studies “are inherently prone to bias, but their results are really good,” observed Juan C. Diaz, MD. They show improvements in left ventricular ejection fraction (LVEF) and symptoms with CSP that are “outstanding compared to what we have been doing for the last 20 years,” he said in an interview.
Dr. Diaz, Clínica Las Vegas, Medellin, Colombia, is an investigator with the observational SYNCHRONY, which is among the new CSP studies formally presented at the annual scientific sessions of the Heart Rhythm Society. He is also lead author on its same-day publication in JACC: Clinical Electrophysiology.
Dr. Diaz said that CSP, which sustains pacing via the native conduction system, makes more “physiologic sense” than BiV pacing and represents “a step forward” for HF device therapy.
SYNCHRONY compared LBB-area with BiV pacing as the initial strategy for achieving cardiac resynchronization in patients with ischemic or nonischemic cardiomyopathy.
CSP is “a long way” from replacing conventional CRT, he said. But the new studies at the HRS sessions should help extend His-bundle and LBB-area pacing to more patients, he added, given the significant long-term “drawbacks” of BiV pacing. These include inevitable RV pacing, multiple leads, and the risks associated with chronic transvenous leads.
Zachary Goldberger, MD, University of Wisconsin–Madison, went a bit further in support of CSP as invited discussant for the SYNCHRONY presentation.
Given that it improved LVEF, heart failure class, HF hospitalizations (HFH), and mortality in that study and others, Dr. Goldberger said, CSP could potentially “become the dominant mode of resynchronization going forward.”
Other experts at the meeting saw CSP’s potential more as one of several pacing techniques that could be brought to bear for patients with CRT indications.
“Conduction system pacing is going to be a huge complement to biventricular pacing,” to which about 30% of patients have a “less than optimal response,” said Pugazhendhi Vijayaraman, MD, chief of clinical electrophysiology, Geisinger Heart Institute, Danville, Pa.
“I don’t think it needs to replace biventricular pacing, because biventricular pacing is a well-established, incredibly powerful therapy,” he told this news organization. But CSP is likely to provide “a good alternative option” in patients with poor responses to BiV-CRT.
It may, however, render some current BiV-pacing alternatives “obsolete,” Dr. Vijayaraman observed. “At our center, at least for the last 5 years, no patient has needed epicardial surgical left ventricular lead placement” because CSP was a better backup option.
Dr. Vijayaraman presented two of the meeting’s CSP vs. BiV pacing comparisons. In one, the 100-patient randomized HOT-CRT trial, contractile function improved significantly on CSP, which could be either His-bundle or LBB-area pacing.
He also presented an observational study of LBB-area pacing at 15 centers in Asia, Europe, and North America and led the authors of its simultaneous publication in the Journal of the American College of Cardiology.
“I think left-bundle conduction system pacing is the future, for sure,” Jagmeet P. Singh, MD, DPhil, told this news organization. Still, it doesn’t always work and when it does, it “doesn’t work equally in all patients,” he said.
“Conduction system pacing certainly makes a lot of sense,” especially in patients with left-bundle-branch block (LBBB), and “maybe not as a primary approach but certainly as a secondary approach,” said Dr. Singh, Massachusetts General Hospital, Boston, who is not a coauthor on any of the three studies.
He acknowledged that CSP may work well as a first-line option in patients with LBBB at some experienced centers. For those without LBBB or who have an intraventricular conduction delay, who represent 45%-50% of current CRT cases, Dr. Singh observed, “there’s still more evidence” that BiV-CRT is a more appropriate initial approach.
Standard CRT may fail, however, even in some patients who otherwise meet guideline-based indications. “We don’t really understand all the mechanisms for nonresponse in conventional biventricular pacing,” observed Niraj Varma, MD, PhD, Cleveland Clinic, also not involved with any of the three studies.
In some groups, including “patients with larger ventricles,” for example, BiV-CRT doesn’t always narrow the electrocardiographic QRS complex or preexcite delayed left ventricular (LV) activation, hallmarks of successful CRT, he said in an interview.
“I think we need to understand why this occurs in both situations,” but in such cases, CSP alone or as an adjunct to direct LV pacing may be successful. “Sometimes we need both an LV lead and the conduction-system pacing lead.”
Narrower, more efficient use of CSP as a BiV-CRT alternative may also boost its chances for success, Dr. Varma added. “I think we need to refine patient selection.”
HOT-CRT: Randomized CSP vs. BiV pacing trial
Conducted at three centers in a single health system, the His-optimized cardiac resynchronization therapy study (HOT-CRT) randomly assigned 100 patients with primary or secondary CRT indications to either to CSP – by either His-bundle or LBB-area pacing – or to standard BiV-CRT as the first-line resynchronization method.
Treatment crossovers, allowed for either pacing modality in the event of implantation failure, occurred in two patients and nine patients initially assigned to CSP and BiV pacing, respectively (4% vs. 18%), Dr. Vijayaraman reported.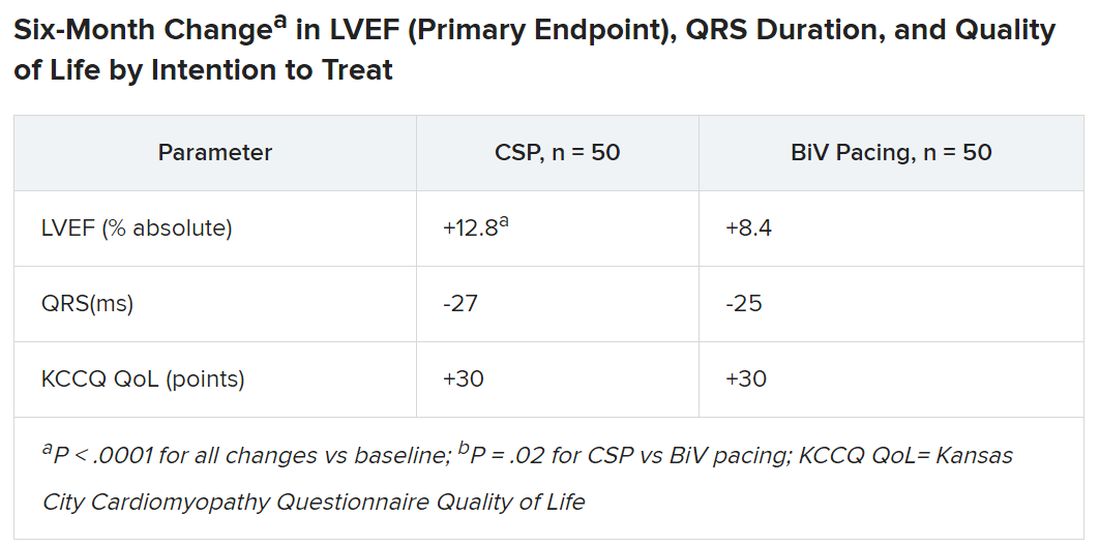
Historically in trials, BiV pacing has elevated LVEF by about 7%, he said. The mean 12-point increase observed with CSP “is huge, in that sense.” HOT-CRT enrolled a predominantly male and White population at centers highly experienced in both CSP and BiV pacing, limiting its broad relevance to practice, as pointed out by both Dr. Vijayaraman and his presentation’s invited discussant, Yong-Mei Cha, MD, Mayo Clinic, Rochester, Minn. Dr. Cha, who is director of cardiac device services at her center, also highlighted the greater rate of crossover from BiV pacing to CSP, 18% vs. 4% in the other direction. “This is a very encouraging result,” because the implant-failure rate for LBB-area pacing may drop once more operators become “familiar and skilled with conduction-system pacing.” Overall, the study supports CSP as “a very good alternative for heart failure patients when BiV pacing fails.”
International comparison of CSP and BiV pacing
In Dr. Vijayaraman’s other study, the observational comparison of LBB-area pacing and BiV-CRT, the CSP technique emerged as a “reasonable alternative to biventricular pacing, not only for improvement in LV function but also to reduce adverse clinical outcomes.”
Indeed, in the international study of 1,778 mostly male patients with primary or secondary CRT indications who received LBB-area or BiV pacing (797 and 981 patients, respectively), those on CSP saw a significant drop in risk for the primary endpoint, death or HFH.
Mean LVEF improved from 27% to 41% in the LBB-area pacing group and 27% to 37% with BiV pacing (P < .001 for both changes) over a follow-up averaging 33 months. The difference in improvement between CSP and BiV pacing was significant at P < .001.
In adjusted analysis, the risk for death or HFH was greater for BiV-pacing patients, a difference driven by HFH events.
- Death or HF: hazard ratio, 1.49 (95% confidence interval, 1.21-1.84; P < .001).
- Death: HR, 1.14 (95% CI, 0.88-1.48; P = .313).
- HFH: HR, 1.49 (95% CI, 1.16-1.92; P = .002)
The analysis has all the “inherent biases” of an observational study. The risk for patient-selection bias, however, was somewhat mitigated by consistent practice patterns at participating centers, Dr. Vijayaraman told this news organization.
For example, he said, operators at six of the institutions were most likely to use CSP as the first-line approach, and the same number of centers usually went with BiV pacing.
SYNCHRONY: First-line LBB-area pacing vs. BiV-CRT
Outcomes using the two approaches were similar in the prospective, international, observational study of 371 patients with ischemic or nonischemic cardiomyopathy and standard CRT indications. Allocation of 128 patients to LBB-area pacing and 243 to BiV-CRT was based on patient and operator preferences, reported Jorge Romero Jr, MD, Brigham and Women’s Hospital, Boston, at the HRS sessions.
Risk for the death-HFH primary endpoint dropped 38% for those initially treated with LBB-area pacing, compared with BiV pacing, primarily because of a lower HFH risk:
- Death or HFH: HR, 0.62 (95% CI, 0.41-0.93; P = .02).
- Death: HR, 0.57 (95% CI, 0.25-1.32; P = .19).
- HFH: HR, 0.61 (95% CI, 0.34-0.93; P = .02)
Patients in the CSP group were also more likely to improve by at least one NYHA (New York Heart Association) class (80.4% vs. 67.9%; P < .001), consistent with their greater absolute change in LVEF (8.0 vs. 3.9 points; P < .01).
The findings “suggest that LBBAP [left-bundle branch area pacing] is an excellent alternative to BiV pacing,” with a comparable safety profile, write Jayanthi N. Koneru, MBBS, and Kenneth A. Ellenbogen, MD, in an editorial accompanying the published SYNCHRONY report.
“The differences in improvement of LVEF are encouraging for both groups,” but were superior for LBB-area pacing, continue Dr. Koneru and Dr. Ellenbogen, both with Virginia Commonwealth University Medical Center, Richmond. “Whether these results would have regressed to the mean over a longer period of follow-up or diverge further with LBB-area pacing continuing to be superior is unknown.”
Years for an answer?
A large randomized comparison of CSP and BiV-CRT, called Left vs. Left, is currently in early stages, Sana M. Al-Khatib, MD, MHS, Duke University Medical Center, Durham, N.C., said in a media presentation on two of the presented studies. It has a planned enrollment of more than 2,100 patients on optimal meds with an LVEF of 50% or lower and either a QRS duration of at least 130 ms or an anticipated burden of RV pacing exceeding 40%.
The trial, she said, “will take years to give an answer, but it is actually designed to address the question of whether a composite endpoint of time to death or heart failure hospitalization can be improved with conduction system pacing vs. biventricular pacing.”
Dr. Al-Khatib is a coauthor on the new guideline covering both CSP and BiV-CRT in HF, as are Dr. Cha, Dr. Varma, Dr. Singh, Dr. Vijayaraman, and Dr. Goldberger; Dr. Ellenbogen is one of the reviewers.
Dr. Diaz discloses receiving honoraria or fees for speaking or teaching from Bayer Healthcare, Pfizer, AstraZeneca, Boston Scientific, and Medtronic. Dr. Vijayaraman discloses receiving honoraria or fees for speaking, teaching, or consulting for Abbott, Medtronic, Biotronik, and Boston Scientific; and receiving research grants from Medtronic. Dr. Varma discloses receiving honoraria or fees for speaking or consulting as an independent contractor for Medtronic, Boston Scientific, Biotronik, Impulse Dynamics USA, Cardiologs, Abbott, Pacemate, Implicity, and EP Solutions. Dr. Singh discloses receiving fees for consulting from EBR Systems, Merit Medical Systems, New Century Health, Biotronik, Abbott, Medtronic, MicroPort Scientific, Cardiologs, Sanofi, CVRx, Impulse Dynamics USA, Octagos, Implicity, Orchestra Biomed, Rhythm Management Group, and Biosense Webster; and receiving honoraria or fees for speaking and teaching from Medscape. Dr. Cha had no relevant financial relationships. Dr. Romero discloses receiving research grants from Biosense Webster; and speaking or receiving honoraria or fees for consulting, speaking, or teaching, or serving on a board for Sanofi, Boston Scientific, and AtriCure. Dr. Koneru discloses consulting for Medtronic and receiving honoraria from Abbott. Dr. Ellenbogen discloses consulting or lecturing for or receiving honoraria from Medtronic, Boston Scientific, and Abbott. Dr. Goldberger discloses receiving royalty income from and serving as an independent contractor for Elsevier. Dr. Al-Khatib discloses receiving research grants from Medtronic and Boston Scientific.
A version of this article first appeared on Medscape.com.
FROM HEART RHYTHM 2023
Dapagliflozin matches non–loop diuretic for congestion in AHF: DAPA-RESIST
suggests a new randomized trial. The drugs were given to the study’s loop diuretic–resistant patients on top of furosemide.
Changes in volume status and measures of pulmonary congestion and risk for serious adverse events were similar for those assigned to take dapagliflozin, an SGLT2 inhibitor, or metolazone, a quinazoline diuretic. Those on dapagliflozin zone ultimately received a larger cumulative furosemide dose in the 61-patient trial, called DAPA-RESIST.
“The next steps are to assess whether a strategy of using SGLT2 inhibitors up front in patients with HF reduces the incidence of diuretic resistance, and to test further combinations of diuretics such as thiazide or thiazide-like diuretics, compared with acetazolamide, when used in addition to an IV loop diuretic and SGLT2 inhibitors together,” Ross T. Campbell, MBChB, PhD, University of Glasgow and Queen Elizabeth University Hospital, also in Glasgow, said in an interview.
Dr. Campbell presented the findings at the annual meeting of the Heart Failure Association of the European Society of Cardiology and is senior author on its simultaneous publication in the European Heart Journal.
The multicenter trial randomly assigned 61 patients with AHF to receive dapagliflozin at a fixed dose of 10 mg once daily or metolazone 5 mg or 10 mg (starting dosage at physician discretion) once daily for 3 days of treatment on an open-label basis.
Patients had entered the trial on furosemide at a mean daily dosage of 260 mg in the dapagliflozin group and 229 mg for those assigned metolazone; dosages for the loop diuretic in the trial weren’t prespecified.
Their median age was 79 and 54% were women; 44% had HF with reduced ejection fraction. Their mean glomerular filtration rate was below 30 mL/min per 1.73 m2 in 26%, 90% had chronic kidney disease, 98% had peripheral edema, and 46% had diabetes.
The mean cumulative furosemide dose was significantly higher among the dapagliflozin group’s 31 patients, 976 mg versus 704 mg for the 30 on acetazolamide (P < .05), 96 hours after the start of randomized therapy. However, patients on dapagliflozin experienced a lesser increase in creatinine (P < .05) and in blood urea (P < .01), a greater change in serum sodium (P < .05), and a smaller reduction in serum potassium (P < .01).
Although the trial wasn’t powered for those outcomes, Dr. Campbell said, “less biochemical upset could be associated with better outcomes in terms of less medium- to long-term renal impairment, and in the short-term length of stay.”
The mean decrease in weight at 96 hours, the primary endpoint, reached 3 kg on dapagliflozin, compared with 3.6 kg with metolazone (P = .082), a difference that fell short of significance.
Loop diuretic efficiency, that is weight change in kg per 40 mg furosemide, “was smaller with dapagliflozin than with metolazone at each time point after randomization, although the difference was only significant at 24 hours,” the published report states.
Changes in pulmonary congestion (by lung ultrasound) and fluid volume were similar between the groups.
“This trial further adds to the evidence base and safety profile for using SGLT2 inhibitors in patients with acute heart failure,” and “gives further confidence to clinicians that this class can be started in ‘sicker’ patients with HF who also have diuretic resistance,” Dr. Campbell said.
Asked during his presentation’s question and answer whether dapagliflozin might have shown a greater effect had the dosage been higher, Dr. Campbell explained that the drug was investigational when the trial started. Adding a higher-dose dapagliflozin arm, he said, would have made for an excessively complex study. But “that’s a great research question for another trial.”
DAPA-RESIST was funded by AstraZeneca. Dr. Campbell disclosed receiving honoraria from AstraZeneca for speaking and from Bayer for serving on an advisory board.
A version of this article first appeared on Medscape.com.
suggests a new randomized trial. The drugs were given to the study’s loop diuretic–resistant patients on top of furosemide.
Changes in volume status and measures of pulmonary congestion and risk for serious adverse events were similar for those assigned to take dapagliflozin, an SGLT2 inhibitor, or metolazone, a quinazoline diuretic. Those on dapagliflozin zone ultimately received a larger cumulative furosemide dose in the 61-patient trial, called DAPA-RESIST.
“The next steps are to assess whether a strategy of using SGLT2 inhibitors up front in patients with HF reduces the incidence of diuretic resistance, and to test further combinations of diuretics such as thiazide or thiazide-like diuretics, compared with acetazolamide, when used in addition to an IV loop diuretic and SGLT2 inhibitors together,” Ross T. Campbell, MBChB, PhD, University of Glasgow and Queen Elizabeth University Hospital, also in Glasgow, said in an interview.
Dr. Campbell presented the findings at the annual meeting of the Heart Failure Association of the European Society of Cardiology and is senior author on its simultaneous publication in the European Heart Journal.
The multicenter trial randomly assigned 61 patients with AHF to receive dapagliflozin at a fixed dose of 10 mg once daily or metolazone 5 mg or 10 mg (starting dosage at physician discretion) once daily for 3 days of treatment on an open-label basis.
Patients had entered the trial on furosemide at a mean daily dosage of 260 mg in the dapagliflozin group and 229 mg for those assigned metolazone; dosages for the loop diuretic in the trial weren’t prespecified.
Their median age was 79 and 54% were women; 44% had HF with reduced ejection fraction. Their mean glomerular filtration rate was below 30 mL/min per 1.73 m2 in 26%, 90% had chronic kidney disease, 98% had peripheral edema, and 46% had diabetes.
The mean cumulative furosemide dose was significantly higher among the dapagliflozin group’s 31 patients, 976 mg versus 704 mg for the 30 on acetazolamide (P < .05), 96 hours after the start of randomized therapy. However, patients on dapagliflozin experienced a lesser increase in creatinine (P < .05) and in blood urea (P < .01), a greater change in serum sodium (P < .05), and a smaller reduction in serum potassium (P < .01).
Although the trial wasn’t powered for those outcomes, Dr. Campbell said, “less biochemical upset could be associated with better outcomes in terms of less medium- to long-term renal impairment, and in the short-term length of stay.”
The mean decrease in weight at 96 hours, the primary endpoint, reached 3 kg on dapagliflozin, compared with 3.6 kg with metolazone (P = .082), a difference that fell short of significance.
Loop diuretic efficiency, that is weight change in kg per 40 mg furosemide, “was smaller with dapagliflozin than with metolazone at each time point after randomization, although the difference was only significant at 24 hours,” the published report states.
Changes in pulmonary congestion (by lung ultrasound) and fluid volume were similar between the groups.
“This trial further adds to the evidence base and safety profile for using SGLT2 inhibitors in patients with acute heart failure,” and “gives further confidence to clinicians that this class can be started in ‘sicker’ patients with HF who also have diuretic resistance,” Dr. Campbell said.
Asked during his presentation’s question and answer whether dapagliflozin might have shown a greater effect had the dosage been higher, Dr. Campbell explained that the drug was investigational when the trial started. Adding a higher-dose dapagliflozin arm, he said, would have made for an excessively complex study. But “that’s a great research question for another trial.”
DAPA-RESIST was funded by AstraZeneca. Dr. Campbell disclosed receiving honoraria from AstraZeneca for speaking and from Bayer for serving on an advisory board.
A version of this article first appeared on Medscape.com.
suggests a new randomized trial. The drugs were given to the study’s loop diuretic–resistant patients on top of furosemide.
Changes in volume status and measures of pulmonary congestion and risk for serious adverse events were similar for those assigned to take dapagliflozin, an SGLT2 inhibitor, or metolazone, a quinazoline diuretic. Those on dapagliflozin zone ultimately received a larger cumulative furosemide dose in the 61-patient trial, called DAPA-RESIST.
“The next steps are to assess whether a strategy of using SGLT2 inhibitors up front in patients with HF reduces the incidence of diuretic resistance, and to test further combinations of diuretics such as thiazide or thiazide-like diuretics, compared with acetazolamide, when used in addition to an IV loop diuretic and SGLT2 inhibitors together,” Ross T. Campbell, MBChB, PhD, University of Glasgow and Queen Elizabeth University Hospital, also in Glasgow, said in an interview.
Dr. Campbell presented the findings at the annual meeting of the Heart Failure Association of the European Society of Cardiology and is senior author on its simultaneous publication in the European Heart Journal.
The multicenter trial randomly assigned 61 patients with AHF to receive dapagliflozin at a fixed dose of 10 mg once daily or metolazone 5 mg or 10 mg (starting dosage at physician discretion) once daily for 3 days of treatment on an open-label basis.
Patients had entered the trial on furosemide at a mean daily dosage of 260 mg in the dapagliflozin group and 229 mg for those assigned metolazone; dosages for the loop diuretic in the trial weren’t prespecified.
Their median age was 79 and 54% were women; 44% had HF with reduced ejection fraction. Their mean glomerular filtration rate was below 30 mL/min per 1.73 m2 in 26%, 90% had chronic kidney disease, 98% had peripheral edema, and 46% had diabetes.
The mean cumulative furosemide dose was significantly higher among the dapagliflozin group’s 31 patients, 976 mg versus 704 mg for the 30 on acetazolamide (P < .05), 96 hours after the start of randomized therapy. However, patients on dapagliflozin experienced a lesser increase in creatinine (P < .05) and in blood urea (P < .01), a greater change in serum sodium (P < .05), and a smaller reduction in serum potassium (P < .01).
Although the trial wasn’t powered for those outcomes, Dr. Campbell said, “less biochemical upset could be associated with better outcomes in terms of less medium- to long-term renal impairment, and in the short-term length of stay.”
The mean decrease in weight at 96 hours, the primary endpoint, reached 3 kg on dapagliflozin, compared with 3.6 kg with metolazone (P = .082), a difference that fell short of significance.
Loop diuretic efficiency, that is weight change in kg per 40 mg furosemide, “was smaller with dapagliflozin than with metolazone at each time point after randomization, although the difference was only significant at 24 hours,” the published report states.
Changes in pulmonary congestion (by lung ultrasound) and fluid volume were similar between the groups.
“This trial further adds to the evidence base and safety profile for using SGLT2 inhibitors in patients with acute heart failure,” and “gives further confidence to clinicians that this class can be started in ‘sicker’ patients with HF who also have diuretic resistance,” Dr. Campbell said.
Asked during his presentation’s question and answer whether dapagliflozin might have shown a greater effect had the dosage been higher, Dr. Campbell explained that the drug was investigational when the trial started. Adding a higher-dose dapagliflozin arm, he said, would have made for an excessively complex study. But “that’s a great research question for another trial.”
DAPA-RESIST was funded by AstraZeneca. Dr. Campbell disclosed receiving honoraria from AstraZeneca for speaking and from Bayer for serving on an advisory board.
A version of this article first appeared on Medscape.com.
FROM HFA-ESC 2023
Medicaid patients with heart failure get poor follow-up after hospital discharge
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
EHR nudges a bust for boosting guideline-directed meds in acute HF: PROMPT-AHF
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM ESC Heart Failure 2023
FDA OKs Injectafer for iron deficiency anemia in heart failure
“This new indication for Injectafer marks the first and only FDA approval of an intravenous iron replacement therapy for adult patients with heart failure,” Ravi Tayi, MD, MPH, chief medical officer at American Regent, said in a news release.
Ferric carboxymaltose injection is also indicated for the treatment of iron deficiency anemia in adults and children as young as 1 year of age who have either intolerance or an unsatisfactory response to oral iron, and in adult patients who have nondialysis dependent chronic kidney disease.
The new indication in HF was supported by data from the CONFIRM-HF randomized controlled trial that evaluated the efficacy and safety of ferric carboxymaltose injection in adults with chronic HF and iron deficiency.
In the study, results showed that treatment with ferric carboxymaltose injection significantly improved exercise capacity compared with placebo in iron-deficient patients with HF.
No new safety signals emerged. The most common treatment emergent adverse events were headache, nausea, hypertension, injection site reactions, hypophosphatemia, and dizziness.
According to the company, ferric carboxymaltose injection has been studied in more than 40 clinical trials that included over 8,800 patients worldwide and has been approved in 86 countries.
A version of this article first appeared on Medscape.com.
“This new indication for Injectafer marks the first and only FDA approval of an intravenous iron replacement therapy for adult patients with heart failure,” Ravi Tayi, MD, MPH, chief medical officer at American Regent, said in a news release.
Ferric carboxymaltose injection is also indicated for the treatment of iron deficiency anemia in adults and children as young as 1 year of age who have either intolerance or an unsatisfactory response to oral iron, and in adult patients who have nondialysis dependent chronic kidney disease.
The new indication in HF was supported by data from the CONFIRM-HF randomized controlled trial that evaluated the efficacy and safety of ferric carboxymaltose injection in adults with chronic HF and iron deficiency.
In the study, results showed that treatment with ferric carboxymaltose injection significantly improved exercise capacity compared with placebo in iron-deficient patients with HF.
No new safety signals emerged. The most common treatment emergent adverse events were headache, nausea, hypertension, injection site reactions, hypophosphatemia, and dizziness.
According to the company, ferric carboxymaltose injection has been studied in more than 40 clinical trials that included over 8,800 patients worldwide and has been approved in 86 countries.
A version of this article first appeared on Medscape.com.
“This new indication for Injectafer marks the first and only FDA approval of an intravenous iron replacement therapy for adult patients with heart failure,” Ravi Tayi, MD, MPH, chief medical officer at American Regent, said in a news release.
Ferric carboxymaltose injection is also indicated for the treatment of iron deficiency anemia in adults and children as young as 1 year of age who have either intolerance or an unsatisfactory response to oral iron, and in adult patients who have nondialysis dependent chronic kidney disease.
The new indication in HF was supported by data from the CONFIRM-HF randomized controlled trial that evaluated the efficacy and safety of ferric carboxymaltose injection in adults with chronic HF and iron deficiency.
In the study, results showed that treatment with ferric carboxymaltose injection significantly improved exercise capacity compared with placebo in iron-deficient patients with HF.
No new safety signals emerged. The most common treatment emergent adverse events were headache, nausea, hypertension, injection site reactions, hypophosphatemia, and dizziness.
According to the company, ferric carboxymaltose injection has been studied in more than 40 clinical trials that included over 8,800 patients worldwide and has been approved in 86 countries.
A version of this article first appeared on Medscape.com.
FDA approves new drug, sotagliflozin, for heart failure
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Circulatory support for RV failure caused by pulmonary embolism
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
FROM INTERVENTIONAL CARDIOLOGY CLINICS
ARNI bests ARB to reduce NT-proBNP in stabilized preserved-EF HF
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ESC HEART FAILURE 2023






