User login
Consider PET/CT when infectious source is a puzzler
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
REPORTING FROM RSNA 2019
Pelvic insufficiency fractures are common after chemoradiotherapy for cervical cancer
CHICAGO – Radiation therapy for cervical cancer resulted in pelvic insufficiency fractures more frequently than previously thought, and many fractures were slow to heal, according to research presented at the annual meeting of the Radiological Society of North America.
“Pelvic insufficiency fractures had a prevalence of 38% on MRI follow-up” after chemoradiotherapy for locally advanced cervical cancer, said Alina Dragan, MD. This figure is more than double the previously reported prevalence of about 14%.
Dr. Dragan, a radiology resident at London North West Healthcare, National Health Service Trust, and coinvestigators also tracked the natural history of these fractures over time, to fill a knowledge gap about whether, and at what rate, these pelvic insufficiency fractures healed.
In the single-center retrospective study, the investigators found that just 14% of sacral fractures healed during the period of observation. For acetabular and pubic fractures, roughly one in three fractures had healed by the last MRI scan. About a third of all fractures remained stable across scans, while just over 10% of fractures were either fluctuant or worsened.
The study included 115 women with locally advanced cervical cancer who were treated with radical or adjuvant concurrent chemoradiotherapy over a 5-year period, and had MRI scans performed in-house; the follow-up protocol had patients receiving scans at 3, 12, and 24 months post treatment. From an initial pool of 197 patients, those who had previously had pelvic radiation or were receiving palliative treatment, as well as those with incomplete imaging follow-up and those with metal implants or prostheses that could affect radiation therapy delivery or imaging quality were excluded.
The chemoradiotherapy protocol involved five doses of weekly cisplatin at 400 mg/m2 of body surface area, as well as high–dose rate cervix brachytherapy. In practice, all but six participants received these treatments. Patients also received external beam radiotherapy with or without a simultaneous integrated boost to target affected lymph nodes, as clinically indicated.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema.
Patients were aged a median of 54 years, and 64 (56%) were postmenopausal. Most patients (n = 84; 73%) had never used tobacco. Participants’ median body mass index was 26 kg/m2.
Most patients (n = 73; 64%) were International Federation of Gynecology and Obstetrics stage 2b, and almost half (n = 55; 48%) had pelvic nodal involvement.
Patients were followed for a median of 12 months, with patients receiving a median of two MRIs curing that period. In all, 105 fractures were identified in 44 patients. A median of two fractures were identified among the group of patients who had pelvic insufficiency fractures.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema. In this schema, 41% of identified fractures were considered mild, while 32% were moderate and 12% were severe.
Although just over two-thirds of fractures (70%) were identified within 6 months of beginning surveillance, a quarter were not identified until 9-13 months post therapy, and 5% were found after more than 13 months.
Sacral fractures accounted for 72% of those identified, in keeping with previous findings, said Dr. Dragan. Acetabular and pubic fractures made up 16% and 10% of fractures, respectively. One fracture was seen at the ilium and one at the ischium.
Dr. Dragan and colleagues turned to multivariable analysis to look for risk factors for pelvic insufficiency fractures in this cohort of cervical cancer patients. Younger patients had a hazard ratio of 0.30 for fracture, compared with those over the age of 50 years (P less than .01). Similarly, being menopausal carried a hazard ratio of 2.25 for fracture. Higher radiation doses to the sacrum also boosted fracture risk (HR, 2.00; P = .03). Neither sacral volume and slope nor the receipt of simultaneous integrated boost were associated with increased fracture risk.
Dr. Dragan reported that she had no relevant conflicts of interest. She reported no outside sources of funding.
SOURCE: Dragan A et al. RSNA 2019, Presentation SSE25-03.
CHICAGO – Radiation therapy for cervical cancer resulted in pelvic insufficiency fractures more frequently than previously thought, and many fractures were slow to heal, according to research presented at the annual meeting of the Radiological Society of North America.
“Pelvic insufficiency fractures had a prevalence of 38% on MRI follow-up” after chemoradiotherapy for locally advanced cervical cancer, said Alina Dragan, MD. This figure is more than double the previously reported prevalence of about 14%.
Dr. Dragan, a radiology resident at London North West Healthcare, National Health Service Trust, and coinvestigators also tracked the natural history of these fractures over time, to fill a knowledge gap about whether, and at what rate, these pelvic insufficiency fractures healed.
In the single-center retrospective study, the investigators found that just 14% of sacral fractures healed during the period of observation. For acetabular and pubic fractures, roughly one in three fractures had healed by the last MRI scan. About a third of all fractures remained stable across scans, while just over 10% of fractures were either fluctuant or worsened.
The study included 115 women with locally advanced cervical cancer who were treated with radical or adjuvant concurrent chemoradiotherapy over a 5-year period, and had MRI scans performed in-house; the follow-up protocol had patients receiving scans at 3, 12, and 24 months post treatment. From an initial pool of 197 patients, those who had previously had pelvic radiation or were receiving palliative treatment, as well as those with incomplete imaging follow-up and those with metal implants or prostheses that could affect radiation therapy delivery or imaging quality were excluded.
The chemoradiotherapy protocol involved five doses of weekly cisplatin at 400 mg/m2 of body surface area, as well as high–dose rate cervix brachytherapy. In practice, all but six participants received these treatments. Patients also received external beam radiotherapy with or without a simultaneous integrated boost to target affected lymph nodes, as clinically indicated.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema.
Patients were aged a median of 54 years, and 64 (56%) were postmenopausal. Most patients (n = 84; 73%) had never used tobacco. Participants’ median body mass index was 26 kg/m2.
Most patients (n = 73; 64%) were International Federation of Gynecology and Obstetrics stage 2b, and almost half (n = 55; 48%) had pelvic nodal involvement.
Patients were followed for a median of 12 months, with patients receiving a median of two MRIs curing that period. In all, 105 fractures were identified in 44 patients. A median of two fractures were identified among the group of patients who had pelvic insufficiency fractures.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema. In this schema, 41% of identified fractures were considered mild, while 32% were moderate and 12% were severe.
Although just over two-thirds of fractures (70%) were identified within 6 months of beginning surveillance, a quarter were not identified until 9-13 months post therapy, and 5% were found after more than 13 months.
Sacral fractures accounted for 72% of those identified, in keeping with previous findings, said Dr. Dragan. Acetabular and pubic fractures made up 16% and 10% of fractures, respectively. One fracture was seen at the ilium and one at the ischium.
Dr. Dragan and colleagues turned to multivariable analysis to look for risk factors for pelvic insufficiency fractures in this cohort of cervical cancer patients. Younger patients had a hazard ratio of 0.30 for fracture, compared with those over the age of 50 years (P less than .01). Similarly, being menopausal carried a hazard ratio of 2.25 for fracture. Higher radiation doses to the sacrum also boosted fracture risk (HR, 2.00; P = .03). Neither sacral volume and slope nor the receipt of simultaneous integrated boost were associated with increased fracture risk.
Dr. Dragan reported that she had no relevant conflicts of interest. She reported no outside sources of funding.
SOURCE: Dragan A et al. RSNA 2019, Presentation SSE25-03.
CHICAGO – Radiation therapy for cervical cancer resulted in pelvic insufficiency fractures more frequently than previously thought, and many fractures were slow to heal, according to research presented at the annual meeting of the Radiological Society of North America.
“Pelvic insufficiency fractures had a prevalence of 38% on MRI follow-up” after chemoradiotherapy for locally advanced cervical cancer, said Alina Dragan, MD. This figure is more than double the previously reported prevalence of about 14%.
Dr. Dragan, a radiology resident at London North West Healthcare, National Health Service Trust, and coinvestigators also tracked the natural history of these fractures over time, to fill a knowledge gap about whether, and at what rate, these pelvic insufficiency fractures healed.
In the single-center retrospective study, the investigators found that just 14% of sacral fractures healed during the period of observation. For acetabular and pubic fractures, roughly one in three fractures had healed by the last MRI scan. About a third of all fractures remained stable across scans, while just over 10% of fractures were either fluctuant or worsened.
The study included 115 women with locally advanced cervical cancer who were treated with radical or adjuvant concurrent chemoradiotherapy over a 5-year period, and had MRI scans performed in-house; the follow-up protocol had patients receiving scans at 3, 12, and 24 months post treatment. From an initial pool of 197 patients, those who had previously had pelvic radiation or were receiving palliative treatment, as well as those with incomplete imaging follow-up and those with metal implants or prostheses that could affect radiation therapy delivery or imaging quality were excluded.
The chemoradiotherapy protocol involved five doses of weekly cisplatin at 400 mg/m2 of body surface area, as well as high–dose rate cervix brachytherapy. In practice, all but six participants received these treatments. Patients also received external beam radiotherapy with or without a simultaneous integrated boost to target affected lymph nodes, as clinically indicated.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema.
Patients were aged a median of 54 years, and 64 (56%) were postmenopausal. Most patients (n = 84; 73%) had never used tobacco. Participants’ median body mass index was 26 kg/m2.
Most patients (n = 73; 64%) were International Federation of Gynecology and Obstetrics stage 2b, and almost half (n = 55; 48%) had pelvic nodal involvement.
Patients were followed for a median of 12 months, with patients receiving a median of two MRIs curing that period. In all, 105 fractures were identified in 44 patients. A median of two fractures were identified among the group of patients who had pelvic insufficiency fractures.
The fractures were graded as mild, moderate, or severe by the interpreting radiologist according to the course of the fracture line and corresponding bone edema. In this schema, 41% of identified fractures were considered mild, while 32% were moderate and 12% were severe.
Although just over two-thirds of fractures (70%) were identified within 6 months of beginning surveillance, a quarter were not identified until 9-13 months post therapy, and 5% were found after more than 13 months.
Sacral fractures accounted for 72% of those identified, in keeping with previous findings, said Dr. Dragan. Acetabular and pubic fractures made up 16% and 10% of fractures, respectively. One fracture was seen at the ilium and one at the ischium.
Dr. Dragan and colleagues turned to multivariable analysis to look for risk factors for pelvic insufficiency fractures in this cohort of cervical cancer patients. Younger patients had a hazard ratio of 0.30 for fracture, compared with those over the age of 50 years (P less than .01). Similarly, being menopausal carried a hazard ratio of 2.25 for fracture. Higher radiation doses to the sacrum also boosted fracture risk (HR, 2.00; P = .03). Neither sacral volume and slope nor the receipt of simultaneous integrated boost were associated with increased fracture risk.
Dr. Dragan reported that she had no relevant conflicts of interest. She reported no outside sources of funding.
SOURCE: Dragan A et al. RSNA 2019, Presentation SSE25-03.
REPORTING FROM RSNA 2019
Patients need physicians who see – and feel – beyond the EMR
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
EXPERT ANALYSIS FROM RSNA 2019
Reward, decision-making brain regions altered in teens with obesity
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
REPORTING FROM RSNA 2019
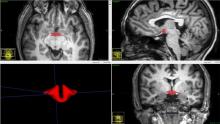
Oral contraceptive use associated with smaller hypothalamic and pituitary volumes
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
REPORTING FROM RSNA 2019
Gunshot wound victims are at high risk for readmission
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
REPORTING FROM RSNA 2019