User login
Does Scheduling a Postdischarge Visit with a Primary Care Physician Increase Rates of Follow-up and Decrease Readmissions?
Under the Hospital Readmission Reduction Program (HRRP), hospitals with higher than expected readmissions for select conditions receive a financial penalty. In 2017, hospitals were penalized a total of $528 million.1,2 In an effort to deter readmissions, hospitals have focused on the transition from inpatient to outpatient care with particular emphasis on timely follow-up with a primary care physician (PCP).3-7 Medicare has also introduced transitional care codes, which reimburse physicians for follow-up care after a hospitalization.
METHODS
Postdischarge Appointment Service
In the fall of 2009, Beth Israel Deaconess introduced a postdischarge appointment intervention to facilitate follow-up with PCPs and specialty physicians after discharge from the hospital. Within the provider order entry system, attending and resident physicians enter a discharge appointment request for specified providers within and outside of the medical center and a specified time period. For example, a physician may enter a request to schedule a PCP appointment within 2-3, 4-8, 9-15, 16-30, or >30 days of discharge.
Study Population
We conducted a retrospective, cohort study at Beth Israel Deaconess Medical Center, a tertiary care hospital, using data derived from electronic health records for all hospitalizations
Outcomes
The primary outcomes of this study were kept PCP follow-up visits within seven days and readmission within 30 days of discharge. We focused on PCP visits within seven days, as this has been the measure used in prior research,5,7 but conducted a sensitivity analysis of PCP follow-up within 14 days. No-shows for the scheduled follow-up PCP appointments were not included. We focused on readmissions within 30 days of discharge, given this is the measure used in the HRRP,16 but conducted a sensitivity analysis of 14 days. Secondary outcomes included ED revisit within the 30 days. Given the data available, we only observed physician visits and hospitalizations that occurred within the Beth Israel Deaconess system.
Analyses
We conducted two analyses to assess whether the implementation of the postdischarge appointment service was associated with an increase in PCP follow-up and a decrease in the readmission rate.
In the first analysis, we focused only on hospitalizations from the medical and cardiology services during the postintervention period between January 2011 and September 2015 (n = 17,582). We compared the PCP follow-up rate and the readmission rate among hospitalizations where the postdischarge appointment service was used versus those where it was not used. We used a multivariable logistic regression, and the covariates included in the model were age, gender, hospital length of stay, and diagnosis-related group (DRG) cost weight. The DRG cost weight captures the average resources used to treat Medicare patients’ hospitalizations within a given DRG category and was used as a surrogate marker for the complexity of hospitalization.17 Instead of presenting odds ratios, we used predictive margins to generate adjusted percentage point estimates of the differences in our outcomes associated with the use of the postdischarge appointment service.18
This instrumental variable exploits the fact that the postdischarge appointment service was only available on weekdays and that physicians are asked to only submit the order for follow-up appointments on the day of discharge. We focused on the day of the week of admission (versus discharge) because of concerns that patients with more complicated hospital courses might be kept in the hospital over the weekend (eg, to facilitate testing available only on weekdays or to consult with regular physicians only available on weekdays). This would create a relationship between the day of discharge and the outcomes (follow-up visits, readmissions). The day of admission is less likely to be impacted by this bias. Given concerns that admissions on different days of the week might be different, our instrument is the day of the week interacted with the time period. Therefore, to create bias, there must be a systematic change in the nature of admissions on a given day of the week during this time period. We provide more details on this analysis, testing of the instrument, and results in the Appendix.
Analyses were conducted in Stata, version 14.2 (StataCorp LP, College Station, Texas). Statistical testing was two-sided, with a significance level of 0.05, and the project was judged exempt by the Committee on Clinical Investigations for Beth Israel Deaconess Medical Center.
RESULTS
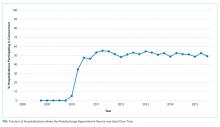
Overall, there were 17,582 hospitalizations on the medicine and cardiology services following implementation of the postdischarge appointment service. The use of the postdischarge appointment service rose rapidly after it was introduced (Figure) and then plateaued at roughly 50%.
Multivariable Logistic Regression
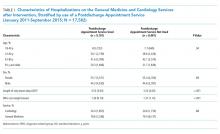
In this analysis, we focused on the 17,582 hospitalizations from January 2011 to September 2015 on the general medicine and cardiology services that occurred after the postdischarge appointment service was introduced. Among these hospitalizations, the postdischarge appointment service was used in 51.8% of discharges.
In an unadjusted analysis, patients discharged using the tool had higher rates of seven-day PCP follow-up (60.2% vs 29.2%, P < .001) and lower 30-day readmission rates (14.7% vs 16.7%; P < .001) than those who were not (Table 2). There was no significant difference in 30-day ED revisit between hospitalizations with and without use of the postdischarge appointment service (22.3% vs 23.1%; P = .23).
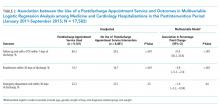
This was echoed in our multivariable analysis where, controlling for other patient factors, use of the postdischarge appointment service was associated with an increased rate of follow-up with a PCP in seven days (+31.9 percentage points; 95% CI: 30.2, 33.6; P < .01) and a decreased likelihood of readmission within 30 days (−3.8 percentage points; 95% CI: −5.2, −2.4; P < .01) (Table 2).
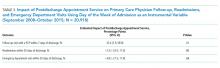
Instrumental Variable Analysis
In our instrumental variable analysis, we used all hospitalizations both before and after the introduction of the intervention. In this analysis, we estimate that use of the postdischarge appointment service increases the probability of visiting a PCP within seven days by 33.4 percentage points (95% CI: 7.9%, 58.9%; P = .01) (Table 3). The use of the postdischarge appointment was associated with a 2.5 percentage point (95% CI: −22.0%, 17.1%; P = .80) reduction in readmissions and a 4.8 percentage point (95% CI; −27.5%, 17.9%; P = .68) reduction in an ED visit within 30 days (Table 3). Neither of these differences were statistically significant with wide confidence intervals.
In sensitivity analyses, we obtained similar results when we considered PCP visits and readmissions within 14 days.
DISCUSSION
The hospital introduced the postdischarge appointment service to facilitate postdischarge appointments and to deter readmissions. In our analyses the use of the postdischarge appointment service was associated with a substantial 30 percentage point increase in the likelihood of a PCP follow-up visit within seven days after hospital discharge. There was a roughly 2% reduction in 30-day readmissions, but this difference was not consistently statistically significant across our analyses. Together, our evaluation implies that this type of intervention may make it much easier for patients to attend a PCP appointment, but scheduling an appointment alone may have a modest impact on deterring a readmission.
Our findings are inconsistent with prior studies that described a strong association between early PCP follow-up and readmissions. However, our results were consistent with research where follow-up visits were not clearly protective against readmissions.20 One potential explanation of the discrepant findings is that there are unmeasured socioeconomic differences between patients who have a PCP follow-up appointment and those who do not.
Regardless of the impact on readmissions, it is important to acknowledge that early PCP follow-up offers many potential benefits. Continuing to evaluate and treat new diagnoses, adjusting and reconciling medications, reconnecting with outpatient providers, capturing new incidental findings, and ensuring stability through regular follow-up are just a few of the potential benefits. We believe the dramatic increase observed in PCP follow-up reflects the administrative complexity required for a patient to call their PCP’s office and to schedule a follow-up appointment soon after they are discharged from the hospital.
Our study has many limitations. The study was limited to a single academic center, and the intervention was limited to patients cared for by the general medicine and cardiology services.
In summary, we found that the introduction of a postdischarge appointment service resulted in substantially increased rates of early PCP follow-up but less clear benefits in preventing readmissions.
1. Boccutti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program; March 10, 2017. https://www.kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program. Accessed July 22, 2019
2. Centers for Medicare and Medicaid Services. FY 2017 IPPS Final Rule: Hospital Readmissions Reduction Program Su pplemental Data File. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Archived-Supplemental-Data-Files.html. Accessed June 22, 2019
3. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. https://doi.org/10.1001/archinternmed.2010.345.
4. Rennke S, Nguyen OK, Shoeb MH, et al. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):433-440. https://doi.org/10.7326/0003-4819-158-5-201303051-00011.
5. Misky GJ, Wald HL, Coleman EA. Post hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. https://doi.org/10.1002/jhm.666.
6. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417-428. https://doi.org/10.7326/0003-4819-157-6-201209180-00006.
7. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. https://doi.org/10.1001/jama.2010.533.
8. Muus KJ, Knudson A, Klug MG, et al. Effect of post discharge follow-up care on re-admissions among US veterans with congestive heart failure: a rural-urban comparison. Rural Remote Health. 2010;10(2):1447.
9. Brooke BS, Stone DH, Cronenwett JL, et al. Early primary care provider follow-up and readmission after high-risk surgery. JAMA Surg. 2014;149(8):821-828. https://doi.org/10.1001/jamasurg.2014.157.
10. Leschke J, Panepinto JA, Nimmer M, et al. Outpatient follow-up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406-409. https://doi.org/10.1002/pbc.23140.
11. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. https://doi.org/10.1007/s11606-014-3106-4.
12. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. https://doi.org/10.1177/1062860611409197.
13. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. https://doi.org/10.7326/0003-4819-155-8-201110180-00008.
14. Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. Am J Med. 2013;126(11):989–994.e1. https://doi.org/10.1016/j.amjmed.2013.06.027.
15. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. https://doi.org/10.1001/archinte.166.17.1822.
16. Thomas JW. Should episode-based economic profiles be risk adjusted to account for differences in patients’ health risks? Health Serv Res. 2006;41(2):581-598. https://doi.org/10.1111/j.1475-6773.2005.00499.x.
17. Mendez CM, Harrington DW, Christenson P, Spellberg B. Impact of hospital variables on case mix index as a marker of disease severity. Popul Health Manag. 2014;17(1):28-34. https://doi.org/10.1089/pop.2013.0002.
18. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962-970. https://doi.org/10.1093/ije/dyu029.
19. Angrist JD, Krueger AB. Instrumental variables and the search for identification: From supply and demand to natural experiments. J Econ Perspect. 2001;15(4):69-85. https://doi.org/10.1257/jep.15.4.69.
20. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. https://doi.org/10.1001/jama.2014.16153.
21. Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603-618. https://doi.org/10.1001/jama.2009.126.
22. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. https://doi.org/10.7326/0003-4819-150-3-200902030-00007.
23. Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675-684. https://doi.org/10.1111/j.1532-5415.2004.52202.x.
24. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. https://doi.org/10.1001/jamainternmed.2014.1608.
25. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841. https://doi.org/10.1001/jama.297.8.831.
26. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x.
27. Hoyer EH, Brotman DJ, Apfel A, et al. Improving outcomes after hospitalization: A prospective observational multicenter evaluation of care coordination strategies for reducing 30-day readmissions to Maryland Hospitals. J Gen Intern Med. 2018;33(5):621-627. https://doi.org/10.1007/s11606-017-4218-4.
Under the Hospital Readmission Reduction Program (HRRP), hospitals with higher than expected readmissions for select conditions receive a financial penalty. In 2017, hospitals were penalized a total of $528 million.1,2 In an effort to deter readmissions, hospitals have focused on the transition from inpatient to outpatient care with particular emphasis on timely follow-up with a primary care physician (PCP).3-7 Medicare has also introduced transitional care codes, which reimburse physicians for follow-up care after a hospitalization.
METHODS
Postdischarge Appointment Service
In the fall of 2009, Beth Israel Deaconess introduced a postdischarge appointment intervention to facilitate follow-up with PCPs and specialty physicians after discharge from the hospital. Within the provider order entry system, attending and resident physicians enter a discharge appointment request for specified providers within and outside of the medical center and a specified time period. For example, a physician may enter a request to schedule a PCP appointment within 2-3, 4-8, 9-15, 16-30, or >30 days of discharge.
Study Population
We conducted a retrospective, cohort study at Beth Israel Deaconess Medical Center, a tertiary care hospital, using data derived from electronic health records for all hospitalizations
Outcomes
The primary outcomes of this study were kept PCP follow-up visits within seven days and readmission within 30 days of discharge. We focused on PCP visits within seven days, as this has been the measure used in prior research,5,7 but conducted a sensitivity analysis of PCP follow-up within 14 days. No-shows for the scheduled follow-up PCP appointments were not included. We focused on readmissions within 30 days of discharge, given this is the measure used in the HRRP,16 but conducted a sensitivity analysis of 14 days. Secondary outcomes included ED revisit within the 30 days. Given the data available, we only observed physician visits and hospitalizations that occurred within the Beth Israel Deaconess system.
Analyses
We conducted two analyses to assess whether the implementation of the postdischarge appointment service was associated with an increase in PCP follow-up and a decrease in the readmission rate.
In the first analysis, we focused only on hospitalizations from the medical and cardiology services during the postintervention period between January 2011 and September 2015 (n = 17,582). We compared the PCP follow-up rate and the readmission rate among hospitalizations where the postdischarge appointment service was used versus those where it was not used. We used a multivariable logistic regression, and the covariates included in the model were age, gender, hospital length of stay, and diagnosis-related group (DRG) cost weight. The DRG cost weight captures the average resources used to treat Medicare patients’ hospitalizations within a given DRG category and was used as a surrogate marker for the complexity of hospitalization.17 Instead of presenting odds ratios, we used predictive margins to generate adjusted percentage point estimates of the differences in our outcomes associated with the use of the postdischarge appointment service.18
This instrumental variable exploits the fact that the postdischarge appointment service was only available on weekdays and that physicians are asked to only submit the order for follow-up appointments on the day of discharge. We focused on the day of the week of admission (versus discharge) because of concerns that patients with more complicated hospital courses might be kept in the hospital over the weekend (eg, to facilitate testing available only on weekdays or to consult with regular physicians only available on weekdays). This would create a relationship between the day of discharge and the outcomes (follow-up visits, readmissions). The day of admission is less likely to be impacted by this bias. Given concerns that admissions on different days of the week might be different, our instrument is the day of the week interacted with the time period. Therefore, to create bias, there must be a systematic change in the nature of admissions on a given day of the week during this time period. We provide more details on this analysis, testing of the instrument, and results in the Appendix.
Analyses were conducted in Stata, version 14.2 (StataCorp LP, College Station, Texas). Statistical testing was two-sided, with a significance level of 0.05, and the project was judged exempt by the Committee on Clinical Investigations for Beth Israel Deaconess Medical Center.
RESULTS
Overall, there were 17,582 hospitalizations on the medicine and cardiology services following implementation of the postdischarge appointment service. The use of the postdischarge appointment service rose rapidly after it was introduced (Figure) and then plateaued at roughly 50%.
Multivariable Logistic Regression
In this analysis, we focused on the 17,582 hospitalizations from January 2011 to September 2015 on the general medicine and cardiology services that occurred after the postdischarge appointment service was introduced. Among these hospitalizations, the postdischarge appointment service was used in 51.8% of discharges.
In an unadjusted analysis, patients discharged using the tool had higher rates of seven-day PCP follow-up (60.2% vs 29.2%, P < .001) and lower 30-day readmission rates (14.7% vs 16.7%; P < .001) than those who were not (Table 2). There was no significant difference in 30-day ED revisit between hospitalizations with and without use of the postdischarge appointment service (22.3% vs 23.1%; P = .23).
This was echoed in our multivariable analysis where, controlling for other patient factors, use of the postdischarge appointment service was associated with an increased rate of follow-up with a PCP in seven days (+31.9 percentage points; 95% CI: 30.2, 33.6; P < .01) and a decreased likelihood of readmission within 30 days (−3.8 percentage points; 95% CI: −5.2, −2.4; P < .01) (Table 2).
Instrumental Variable Analysis
In our instrumental variable analysis, we used all hospitalizations both before and after the introduction of the intervention. In this analysis, we estimate that use of the postdischarge appointment service increases the probability of visiting a PCP within seven days by 33.4 percentage points (95% CI: 7.9%, 58.9%; P = .01) (Table 3). The use of the postdischarge appointment was associated with a 2.5 percentage point (95% CI: −22.0%, 17.1%; P = .80) reduction in readmissions and a 4.8 percentage point (95% CI; −27.5%, 17.9%; P = .68) reduction in an ED visit within 30 days (Table 3). Neither of these differences were statistically significant with wide confidence intervals.
In sensitivity analyses, we obtained similar results when we considered PCP visits and readmissions within 14 days.
DISCUSSION
The hospital introduced the postdischarge appointment service to facilitate postdischarge appointments and to deter readmissions. In our analyses the use of the postdischarge appointment service was associated with a substantial 30 percentage point increase in the likelihood of a PCP follow-up visit within seven days after hospital discharge. There was a roughly 2% reduction in 30-day readmissions, but this difference was not consistently statistically significant across our analyses. Together, our evaluation implies that this type of intervention may make it much easier for patients to attend a PCP appointment, but scheduling an appointment alone may have a modest impact on deterring a readmission.
Our findings are inconsistent with prior studies that described a strong association between early PCP follow-up and readmissions. However, our results were consistent with research where follow-up visits were not clearly protective against readmissions.20 One potential explanation of the discrepant findings is that there are unmeasured socioeconomic differences between patients who have a PCP follow-up appointment and those who do not.
Regardless of the impact on readmissions, it is important to acknowledge that early PCP follow-up offers many potential benefits. Continuing to evaluate and treat new diagnoses, adjusting and reconciling medications, reconnecting with outpatient providers, capturing new incidental findings, and ensuring stability through regular follow-up are just a few of the potential benefits. We believe the dramatic increase observed in PCP follow-up reflects the administrative complexity required for a patient to call their PCP’s office and to schedule a follow-up appointment soon after they are discharged from the hospital.
Our study has many limitations. The study was limited to a single academic center, and the intervention was limited to patients cared for by the general medicine and cardiology services.
In summary, we found that the introduction of a postdischarge appointment service resulted in substantially increased rates of early PCP follow-up but less clear benefits in preventing readmissions.
Under the Hospital Readmission Reduction Program (HRRP), hospitals with higher than expected readmissions for select conditions receive a financial penalty. In 2017, hospitals were penalized a total of $528 million.1,2 In an effort to deter readmissions, hospitals have focused on the transition from inpatient to outpatient care with particular emphasis on timely follow-up with a primary care physician (PCP).3-7 Medicare has also introduced transitional care codes, which reimburse physicians for follow-up care after a hospitalization.
METHODS
Postdischarge Appointment Service
In the fall of 2009, Beth Israel Deaconess introduced a postdischarge appointment intervention to facilitate follow-up with PCPs and specialty physicians after discharge from the hospital. Within the provider order entry system, attending and resident physicians enter a discharge appointment request for specified providers within and outside of the medical center and a specified time period. For example, a physician may enter a request to schedule a PCP appointment within 2-3, 4-8, 9-15, 16-30, or >30 days of discharge.
Study Population
We conducted a retrospective, cohort study at Beth Israel Deaconess Medical Center, a tertiary care hospital, using data derived from electronic health records for all hospitalizations
Outcomes
The primary outcomes of this study were kept PCP follow-up visits within seven days and readmission within 30 days of discharge. We focused on PCP visits within seven days, as this has been the measure used in prior research,5,7 but conducted a sensitivity analysis of PCP follow-up within 14 days. No-shows for the scheduled follow-up PCP appointments were not included. We focused on readmissions within 30 days of discharge, given this is the measure used in the HRRP,16 but conducted a sensitivity analysis of 14 days. Secondary outcomes included ED revisit within the 30 days. Given the data available, we only observed physician visits and hospitalizations that occurred within the Beth Israel Deaconess system.
Analyses
We conducted two analyses to assess whether the implementation of the postdischarge appointment service was associated with an increase in PCP follow-up and a decrease in the readmission rate.
In the first analysis, we focused only on hospitalizations from the medical and cardiology services during the postintervention period between January 2011 and September 2015 (n = 17,582). We compared the PCP follow-up rate and the readmission rate among hospitalizations where the postdischarge appointment service was used versus those where it was not used. We used a multivariable logistic regression, and the covariates included in the model were age, gender, hospital length of stay, and diagnosis-related group (DRG) cost weight. The DRG cost weight captures the average resources used to treat Medicare patients’ hospitalizations within a given DRG category and was used as a surrogate marker for the complexity of hospitalization.17 Instead of presenting odds ratios, we used predictive margins to generate adjusted percentage point estimates of the differences in our outcomes associated with the use of the postdischarge appointment service.18
This instrumental variable exploits the fact that the postdischarge appointment service was only available on weekdays and that physicians are asked to only submit the order for follow-up appointments on the day of discharge. We focused on the day of the week of admission (versus discharge) because of concerns that patients with more complicated hospital courses might be kept in the hospital over the weekend (eg, to facilitate testing available only on weekdays or to consult with regular physicians only available on weekdays). This would create a relationship between the day of discharge and the outcomes (follow-up visits, readmissions). The day of admission is less likely to be impacted by this bias. Given concerns that admissions on different days of the week might be different, our instrument is the day of the week interacted with the time period. Therefore, to create bias, there must be a systematic change in the nature of admissions on a given day of the week during this time period. We provide more details on this analysis, testing of the instrument, and results in the Appendix.
Analyses were conducted in Stata, version 14.2 (StataCorp LP, College Station, Texas). Statistical testing was two-sided, with a significance level of 0.05, and the project was judged exempt by the Committee on Clinical Investigations for Beth Israel Deaconess Medical Center.
RESULTS
Overall, there were 17,582 hospitalizations on the medicine and cardiology services following implementation of the postdischarge appointment service. The use of the postdischarge appointment service rose rapidly after it was introduced (Figure) and then plateaued at roughly 50%.
Multivariable Logistic Regression
In this analysis, we focused on the 17,582 hospitalizations from January 2011 to September 2015 on the general medicine and cardiology services that occurred after the postdischarge appointment service was introduced. Among these hospitalizations, the postdischarge appointment service was used in 51.8% of discharges.
In an unadjusted analysis, patients discharged using the tool had higher rates of seven-day PCP follow-up (60.2% vs 29.2%, P < .001) and lower 30-day readmission rates (14.7% vs 16.7%; P < .001) than those who were not (Table 2). There was no significant difference in 30-day ED revisit between hospitalizations with and without use of the postdischarge appointment service (22.3% vs 23.1%; P = .23).
This was echoed in our multivariable analysis where, controlling for other patient factors, use of the postdischarge appointment service was associated with an increased rate of follow-up with a PCP in seven days (+31.9 percentage points; 95% CI: 30.2, 33.6; P < .01) and a decreased likelihood of readmission within 30 days (−3.8 percentage points; 95% CI: −5.2, −2.4; P < .01) (Table 2).
Instrumental Variable Analysis
In our instrumental variable analysis, we used all hospitalizations both before and after the introduction of the intervention. In this analysis, we estimate that use of the postdischarge appointment service increases the probability of visiting a PCP within seven days by 33.4 percentage points (95% CI: 7.9%, 58.9%; P = .01) (Table 3). The use of the postdischarge appointment was associated with a 2.5 percentage point (95% CI: −22.0%, 17.1%; P = .80) reduction in readmissions and a 4.8 percentage point (95% CI; −27.5%, 17.9%; P = .68) reduction in an ED visit within 30 days (Table 3). Neither of these differences were statistically significant with wide confidence intervals.
In sensitivity analyses, we obtained similar results when we considered PCP visits and readmissions within 14 days.
DISCUSSION
The hospital introduced the postdischarge appointment service to facilitate postdischarge appointments and to deter readmissions. In our analyses the use of the postdischarge appointment service was associated with a substantial 30 percentage point increase in the likelihood of a PCP follow-up visit within seven days after hospital discharge. There was a roughly 2% reduction in 30-day readmissions, but this difference was not consistently statistically significant across our analyses. Together, our evaluation implies that this type of intervention may make it much easier for patients to attend a PCP appointment, but scheduling an appointment alone may have a modest impact on deterring a readmission.
Our findings are inconsistent with prior studies that described a strong association between early PCP follow-up and readmissions. However, our results were consistent with research where follow-up visits were not clearly protective against readmissions.20 One potential explanation of the discrepant findings is that there are unmeasured socioeconomic differences between patients who have a PCP follow-up appointment and those who do not.
Regardless of the impact on readmissions, it is important to acknowledge that early PCP follow-up offers many potential benefits. Continuing to evaluate and treat new diagnoses, adjusting and reconciling medications, reconnecting with outpatient providers, capturing new incidental findings, and ensuring stability through regular follow-up are just a few of the potential benefits. We believe the dramatic increase observed in PCP follow-up reflects the administrative complexity required for a patient to call their PCP’s office and to schedule a follow-up appointment soon after they are discharged from the hospital.
Our study has many limitations. The study was limited to a single academic center, and the intervention was limited to patients cared for by the general medicine and cardiology services.
In summary, we found that the introduction of a postdischarge appointment service resulted in substantially increased rates of early PCP follow-up but less clear benefits in preventing readmissions.
1. Boccutti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program; March 10, 2017. https://www.kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program. Accessed July 22, 2019
2. Centers for Medicare and Medicaid Services. FY 2017 IPPS Final Rule: Hospital Readmissions Reduction Program Su pplemental Data File. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Archived-Supplemental-Data-Files.html. Accessed June 22, 2019
3. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. https://doi.org/10.1001/archinternmed.2010.345.
4. Rennke S, Nguyen OK, Shoeb MH, et al. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):433-440. https://doi.org/10.7326/0003-4819-158-5-201303051-00011.
5. Misky GJ, Wald HL, Coleman EA. Post hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. https://doi.org/10.1002/jhm.666.
6. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417-428. https://doi.org/10.7326/0003-4819-157-6-201209180-00006.
7. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. https://doi.org/10.1001/jama.2010.533.
8. Muus KJ, Knudson A, Klug MG, et al. Effect of post discharge follow-up care on re-admissions among US veterans with congestive heart failure: a rural-urban comparison. Rural Remote Health. 2010;10(2):1447.
9. Brooke BS, Stone DH, Cronenwett JL, et al. Early primary care provider follow-up and readmission after high-risk surgery. JAMA Surg. 2014;149(8):821-828. https://doi.org/10.1001/jamasurg.2014.157.
10. Leschke J, Panepinto JA, Nimmer M, et al. Outpatient follow-up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406-409. https://doi.org/10.1002/pbc.23140.
11. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. https://doi.org/10.1007/s11606-014-3106-4.
12. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. https://doi.org/10.1177/1062860611409197.
13. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. https://doi.org/10.7326/0003-4819-155-8-201110180-00008.
14. Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. Am J Med. 2013;126(11):989–994.e1. https://doi.org/10.1016/j.amjmed.2013.06.027.
15. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. https://doi.org/10.1001/archinte.166.17.1822.
16. Thomas JW. Should episode-based economic profiles be risk adjusted to account for differences in patients’ health risks? Health Serv Res. 2006;41(2):581-598. https://doi.org/10.1111/j.1475-6773.2005.00499.x.
17. Mendez CM, Harrington DW, Christenson P, Spellberg B. Impact of hospital variables on case mix index as a marker of disease severity. Popul Health Manag. 2014;17(1):28-34. https://doi.org/10.1089/pop.2013.0002.
18. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962-970. https://doi.org/10.1093/ije/dyu029.
19. Angrist JD, Krueger AB. Instrumental variables and the search for identification: From supply and demand to natural experiments. J Econ Perspect. 2001;15(4):69-85. https://doi.org/10.1257/jep.15.4.69.
20. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. https://doi.org/10.1001/jama.2014.16153.
21. Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603-618. https://doi.org/10.1001/jama.2009.126.
22. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. https://doi.org/10.7326/0003-4819-150-3-200902030-00007.
23. Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675-684. https://doi.org/10.1111/j.1532-5415.2004.52202.x.
24. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. https://doi.org/10.1001/jamainternmed.2014.1608.
25. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841. https://doi.org/10.1001/jama.297.8.831.
26. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x.
27. Hoyer EH, Brotman DJ, Apfel A, et al. Improving outcomes after hospitalization: A prospective observational multicenter evaluation of care coordination strategies for reducing 30-day readmissions to Maryland Hospitals. J Gen Intern Med. 2018;33(5):621-627. https://doi.org/10.1007/s11606-017-4218-4.
1. Boccutti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program; March 10, 2017. https://www.kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program. Accessed July 22, 2019
2. Centers for Medicare and Medicaid Services. FY 2017 IPPS Final Rule: Hospital Readmissions Reduction Program Su pplemental Data File. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Archived-Supplemental-Data-Files.html. Accessed June 22, 2019
3. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. https://doi.org/10.1001/archinternmed.2010.345.
4. Rennke S, Nguyen OK, Shoeb MH, et al. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):433-440. https://doi.org/10.7326/0003-4819-158-5-201303051-00011.
5. Misky GJ, Wald HL, Coleman EA. Post hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397. https://doi.org/10.1002/jhm.666.
6. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417-428. https://doi.org/10.7326/0003-4819-157-6-201209180-00006.
7. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. https://doi.org/10.1001/jama.2010.533.
8. Muus KJ, Knudson A, Klug MG, et al. Effect of post discharge follow-up care on re-admissions among US veterans with congestive heart failure: a rural-urban comparison. Rural Remote Health. 2010;10(2):1447.
9. Brooke BS, Stone DH, Cronenwett JL, et al. Early primary care provider follow-up and readmission after high-risk surgery. JAMA Surg. 2014;149(8):821-828. https://doi.org/10.1001/jamasurg.2014.157.
10. Leschke J, Panepinto JA, Nimmer M, et al. Outpatient follow-up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406-409. https://doi.org/10.1002/pbc.23140.
11. Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565-571. https://doi.org/10.1007/s11606-014-3106-4.
12. Kashiwagi DT, Burton MC, Kirkland LL, Cha S, Varkey P. Do timely outpatient follow-up visits decrease hospital readmission rates? Am J Med Qual. 2012;27(1):11-15. https://doi.org/10.1177/1062860611409197.
13. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. https://doi.org/10.7326/0003-4819-155-8-201110180-00008.
14. Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. Am J Med. 2013;126(11):989–994.e1. https://doi.org/10.1016/j.amjmed.2013.06.027.
15. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. https://doi.org/10.1001/archinte.166.17.1822.
16. Thomas JW. Should episode-based economic profiles be risk adjusted to account for differences in patients’ health risks? Health Serv Res. 2006;41(2):581-598. https://doi.org/10.1111/j.1475-6773.2005.00499.x.
17. Mendez CM, Harrington DW, Christenson P, Spellberg B. Impact of hospital variables on case mix index as a marker of disease severity. Popul Health Manag. 2014;17(1):28-34. https://doi.org/10.1089/pop.2013.0002.
18. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962-970. https://doi.org/10.1093/ije/dyu029.
19. Angrist JD, Krueger AB. Instrumental variables and the search for identification: From supply and demand to natural experiments. J Econ Perspect. 2001;15(4):69-85. https://doi.org/10.1257/jep.15.4.69.
20. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. https://doi.org/10.1001/jama.2014.16153.
21. Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603-618. https://doi.org/10.1001/jama.2009.126.
22. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. https://doi.org/10.7326/0003-4819-150-3-200902030-00007.
23. Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675-684. https://doi.org/10.1111/j.1532-5415.2004.52202.x.
24. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. https://doi.org/10.1001/jamainternmed.2014.1608.
25. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831-841. https://doi.org/10.1001/jama.297.8.831.
26. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x.
27. Hoyer EH, Brotman DJ, Apfel A, et al. Improving outcomes after hospitalization: A prospective observational multicenter evaluation of care coordination strategies for reducing 30-day readmissions to Maryland Hospitals. J Gen Intern Med. 2018;33(5):621-627. https://doi.org/10.1007/s11606-017-4218-4.
© 2019 Society of Hospital Medicine
Postdischarge clinics and hospitalists: A review of the evidence and existing models
Readmission prevention is paramount for hospitals and, by extension, hospitalist programs. Hospitalists see early and reliable outpatient follow-up as a safe landing for their most complicated patient cases. The option of a postdischarge clinic arises from the challenge to arrange adequate postdischarge care for patients who lack easy access because of insurance or provider availability. Guaranteeing postdischarge access by opening a dedicated, hospitalist-led postdischarge clinic appears to be an easy solution, but it is a solution that requires significant investment (including investment in physician and staff training and administrative support) and careful navigation of existing primary care relationships. In addition, a clinic staffed only with physicians may not be well equipped to address the complex social factors in healthcare utilization and readmission. Better understanding of the evidence supporting post discharge physician visits, several models of clinics, and the key operational questions are essential to address before crossing the inpatient-outpatient divide.
POSTDISCHARGE PHYSICIAN VISITS AND READMISSIONS
A postdischarge outpatient provider visit is often seen as a key factor in reducing readmissions. In 2013, Medicare added strength to this association by establishing transitional care management codes, which provide enhanced reimbursement to providers for a visit within 7 or 14 days of discharge, with focused attention on transitional issues.1 However, whether a postdischarge visit reduces readmissions remains unclear. Given evidence that higher primary care density is associated with lower healthcare utilization,2 CMS’s financial investment in incentivizing post discharge physician visits may be a good bet. On the other hand, simply having a primary care physician (PCP) may be a risk factor for readmission. This association suggests that postdischarge vigilance leads to identification of medical problems that lead to rehospitalization.3 This uncertainty is not resolved in systematic reviews of readmission reduction initiatives, which were not focused solely on the impact of a physician visit.4,5
The earliest study of postdischarge visits in a general medical population found an association between intensive outpatient follow-up by new providers in a Veterans Affairs population and an increase in hospital readmissions.6 This model is similar to some hospitalist models for postdischarge clinics, as the visit was with a noncontinuity provider. The largest recent study, of patients hospitalized with acute myocardial infarction, community-acquired pneumonia, or congestive heart failure (CHF) between 2009 and 2012, found increased frequency of postdischarge follow-up but no concomitant reduction in readmissions.7 Although small observational studies8 have found a postdischarge primary care visit may reduce the risk for readmission in general medical patients, the bulk of the recent data is negative.
In high-risk patients, however, there may be a clear benefit to postdischarge follow-up. In a North Carolina Medicaid population, a physician visit after discharge was associated with fewer readmissions among high-risk patients, but not among lower risk patients, whose readmission rates were low to start.9 The results of that study support the idea that risk stratification may identify patients who can benefit from more intensive outpatient follow-up. In general medical populations, existing studies may suffer from an absence of adequate risk assessment.
The evidence in specific disease states may show a clearer association between a postdischarge physician visit and reduced risk for readmission. One quarter of patients with CHF are rehospitalized within 30 days of discharge.10 In this disease with frequent exacerbations, a clinic visit to monitor volume status, weight, and medication adherence might reduce the frequency of readmissions or prolong the interval between rehospitalizations. A large observational study observed that earlier post discharge follow up by a cardiologist or a PCP was associated with lower risk of readmission, but only in the quintile with the closest follow-up. In addition, fewer than 40% of patients in this group had a visit within 7 days.11 In another heart failure population, follow-up with either a PCP or cardiologist within 7 days of discharge was again associated with lower risk for readmission.12 Thus, data suggest a protective effect of postdischarge visits in CHF patients, in contrast to a general medical population. Patients with end-stage renal disease may also fit in this group protected by a postdischarge physician visit, as 1 additional visit within the month after discharge was estimated to reduce rehospitalizations and produce significant cost savings.13
With other specific discharge diagnoses, results are varied. Two small observational studies in chronic obstructive pulmonary disease had conflicting results—one found a modest reduction in readmission and emergency department (ED) visits for patients seen by a PCP or pulmonologist within 30 days of discharge,14 and the other found no effect on readmissions but an associated reduction in mortality.15 More data are needed to clarify further the interaction of postdischarge visits with mortality, but the association between postdischarge physician visits and readmission reduction is controversial for patients with chronic obstructive pulmonary disease.
Finally, the evidence for dedicated postdischarge clinics is even more limited. A study of a hospitalist-led postdischarge clinic in a Veterans Affairs hospital found reduced length of stay and earlier postdischarge follow-up in a postdischarge clinic, but no effect on readmissions.16 Other studies have found earlier postdischarge follow-up with dedicated discharge clinics but have not evaluated readmission rates specifically.17In summary, the effect of postdischarge visits on risk for readmission is an area of active research, but remains unclear. The data reviewed suggest a benefit for the highest risk patients, specifically those with severe chronic illness, or those deemed high-risk with a readmission tool.9 At present, because physicians cannot accurately predict which patients will be readmitted,18 discharging physicians often take a broad approach and schedule outpatient visits for all patients. As readmission tools are further refined, the group of patients who will benefit from postdischarge care will be easier to identify, and a benefit to postdischarge visits may be seen
It is also important to note that this review emphasizes the physician visit and its potential impact on readmissions. Socioeconomic causes are increasingly being recognized as driving readmissions and other utilization.19 Whether an isolated physician visit is sufficient to prevent readmissions for patients with nonmedical drivers of healthcare utilization is unclear. For those patients, a discharge visit likely is a necessary component of a readmission reduction strategy for high-risk patients, but may be insufficient for patients who require not just an isolated visit but rather a more integrated and comprehensive care program.8,20,21
POSTDISCHARGE CLINIC MODELS
Despite the unclear relationship between postdischarge physician care and readmissions, dedicated postdischarge clinics, some staffed by hospitalists, have been adopted over the past 10 years. The three primary types of clinics arise in safety net environments, in academic medical centers, and as comprehensive high-risk patient solutions. Reviewing several types of clinics further clarifies the nature of this structural innovation.
Safety Net Hospital Models
Safety net hospitals and their hospitalists struggle with securing adequate postdischarge access for their population, which has inadequate insurance and poor access to primary care. Patient characteristics also play a role in the complex postdischarge care for this population, given its high rate of ED use (owing to perceived convenience and capabilities) for ambulatory-sensitive conditions.22 In addition, immigrants, particularly those with low English-language proficiency, underuse and have poor access to primary care.23,24 Postdischarge clinics in this environment focus first on providing a reliable postdischarge plan and then on linking to primary care. Examples of two clinics are at Harborview Medical Center in Seattle, Washington25 and Texas Health in Fort Worth.
Harborview is a 400-bed hospital affiliated with the University of Washington. More than 50% of its patients are considered indigent. The clinic was established in 2007 to provide a postdischarge option for uninsured patients, and a link to primary care in federally qualified health centers. The clinic was staffed 5 days a week with one or two hospitalists or advanced practice nurses. Visit duration was 20 minutes, 270 visits occurred per month, and the no-show rate was 30%. A small subgroup of the hospitalist group staffed the clinic. Particular clinical foci included CHF patients, patients with wound-care needs, and homeless, immigrant, and recently incarcerated patients. A key goal was connecting to longitudinal primary care, and the clinic successfully connected more than 70% of patients to primary care in community health centers. This clinic ultimately transitioned from a hospitalist practice to a primary care practice with a primary focus on post-ED follow-up for unaffiliated patients.26
In 2010, Texas Health faced a similar challenge with unaffiliated patients, and established a nurse practitioner–based clinic with hospitalist oversight to provide care primarily for patients without insurance or without an existing primary care relationship.
Academic Medical Center Models
Another clinical model is designed for patients who receive primary care at practices affiliated with academic medical centers. Although many of these patients have insurance and a PCP, there is often no availability with their continuity provider, because of the resident’s inpatient schedule or the faculty member’s conflicting priorities.27,28 Academic medical centers, including the University of California at San Francisco, the University of New Mexico, and the Beth Israel Deaconess Medical Center, have established discharge clinics within their faculty primary care practices. A model of this type of clinic was set up at Beth Israel Deaconess in 2010. Staffed by four hospitalists and using 40-minute appointments, this clinic was physically based in the primary care practice. As such, it took advantage of the existing clinic’s administrative and clinical functions, including triage, billing, and scheduling. A visit was scheduled in that clinic by the discharging physician team if a primary care appointment was not available with the patient’s continuity provider. Visits were standardized and focused on outstanding issues at discharge, medication reconciliation, and symptom trajectory. The hospitalists used the clinic’s clinical resources, including nurses, social workers, and pharmacists, but had no other dedicated staff. That there were only four hospitalists meant they were able to gain sufficient exposure to the outpatient setting, provide consistent high-quality care, and gain credibility with the PCPs. As the patients who were seen had PCPs of their own, during the visit significant attention was focused first on the postdischarge concerns, and then on promptly returning the patients to routine primary care. Significant patient outreach was used to address the clinic’s no-show rate, which was almost 50% in the early months. Within a year, the rate was down, closer to 20%. This clinic closed in 2015 after the primary care practice, in which it was based, transitioned to a patient-centered medical home. Since that time, this type of initiative has spread further, with neurohospitalist discharge clinics established, and postdischarge neurology follow-up becoming faster and more reliable.29
Academic medical centers and safety net hospitals substitute for routine primary care to address the basic challenge of primary care access, often without significant enhancements or additional resources, such as dedicated care management and pharmacy, social work, and nursing support. Commonalities of these clinics include dedicated physician staff, appointments generally longer than average outpatient appointments, and visit content concentrated on the key issues at transition (medication reconciliation, outstanding tests, symptom trajectory). As possible, clinics adopted a multidisciplinary approach, with social workers, community health workers, and nurses, to respond to the breadth of patients’ postdischarge needs, which often extend beyond pure medical need. The most frequent barriers encountered included the knowledge gap for hospitalist providers in the outpatient setting (a gap mitigated by using dedicated providers) and the patients’ high no-show rate (not surprising given that the providers are generally new to them). Few clinics have attempted to create continuity across inpatient and outpatient providers, though continuity might reduce no-shows as well as eliminate at least 1 transition.
Comprehensive High-Risk Patient Solutions
At the other end of the clinic spectrum are more integrated postdischarge approaches, which also evolved from the hospitalist model with hospitalist staffing. However, these approaches were introduced in response to the clinical needs of the highest risk patients (who are most vulnerable to frequent provider transitions), not to a systemic inability to provide routine postdischarge care.30
The most long-standing model for this type of clinic is represented by CareMore Health System, a subsidiary of Anthem.30-32 The extensivist, an expanded-scope hospitalist, acts as primary care coordinator, coordinating a multidisciplinary team for a panel of about 100 patients, representing the sickest 5% of the Medicare Advantage–insured population. Unlike the traditional hospitalist, the extensivist follows patients across all care sites, including hospital, rehabilitation sites, and outpatient clinic. For the most part, this relationship is not designed to evolve into a longitudinal relationship, but rather is an intervention only for the several-months period of acute need. Internal data have shown effects on hospital readmissions as well as length of stay.30
Another integrated clinic was established in 2013, at the University of Chicago. This was an effort to redesign care for patients at highest risk for hospitalization.33 Similar to the CareMore process, a high-risk population is identified by prior hospitalization and expected high Medicare costs. A comprehensive care physician cares for these patients across care settings. The clinic takes a team-based approach to patient care, with team members selected on the basis of patient need. Physicians have panels limited to only 200 patients, and generally spend part of the day in clinic, and part in seeing their hospitalized patients. Although reminiscent of a traditional primary care setting, this clinic is designed specifically for a high-risk, frequently hospitalized population, and therefore requires physicians with both a skill set akin to that of hospitalists, and an approach of palliative care and holistic patient care. Outcomes from this trial clinic are expected in 2017 or 2018.
LOGISTICAL CONSIDERATIONS FOR DISCHARGE CLINICS
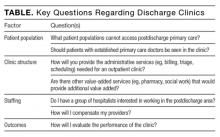
Considering some key operational questions (Table) can help guide hospitals, hospitalists, and healthcare systems as they venture into the postdischarge clinic space. Return on investment and sustainability are two key questions for postdischarge clinics.
Return on investment varies by payment structure. In capitated environments with a strong emphasis on readmissions and total medical expenditure, a successful postdischarge clinic would recoup the investment through readmission reduction. However, maintaining adequate patient volume against high no-show rates may strain the group financially. In addition, although a hospitalist group may reap few measurable benefits from this clinical exposure, the unique view of the outpatient world afforded to hospitalists working in this environment could enrich the group as a whole by providing a more well-rounded vantage point.
Another key question surrounds sustainability. The clinic at the Beth Israel Deaconess Medical Center in Boston temporarily closed due to high inpatient volume and corresponding need for those hospitalists in the inpatient setting, early in its inception. It subsequently closed due to evolution in the clinic where it was based, rendering it unnecessary. Clinics that are contingent on other clinics will be vulnerable to external forces. Finally, staffing these clinics may be a stretch for a hospitalist group, as a partly different skill set is required for patient care in the outpatient setting. Hospitalists interested in care transitions are well suited for this role. In addition, hospitalists interested in more clinical variety, or in more schedule variety than that provided in a traditional hospitalist schedule, often enjoy the work. A vast majority of hospitalists think PCPs are responsible for postdischarge problems, and would not be interested in working in the postdischarge world.34 A poor fit for providers may lead to clinic failure.
As evident from this review, gaps in understanding the benefits of postdischarge care have persisted for 10 years. Discharge clinics have been scantly described in the literature. The primary unanswered question remains the effect on readmissions, but this has been the sole research focus to date. Other key research areas are the impact on other patient-centered clinical and system outcomes (eg, patient satisfaction, particularly for patients seeing new providers), postdischarge mortality, the effect on other adverse events, and total medical expenditure.
The healthcare system is evolving in the context of a focus on readmissions, primary care access challenges, and high-risk patients’ specific needs. These forces are spurring innovation in the realm of postdischarge physician clinics, as even the basic need for an appointment may not be met by the existing outpatient primary care system. In this context, multiple new outpatient care structures have arisen, many staffed by hospitalists. Some, such as clinics based in safety net hospitals and academic medical centers, address the simple requirement that patients who lack easy access, because of insurance status or provider availability, can see a doctor after discharge. This type of clinic may be an essential step in alleviating a strained system but may not represent a sustainable long-term solution. More comprehensive solutions for improving patient care and clinical outcomes may be offered by integrated systems, such as CareMore, which also emerged from the hospitalist model. A lasting question is whether these clinics, both the narrowly focused and the comprehensive, will have longevity in the evolving healthcare market. Inevitably, though, hospitalist directors will continue to raise such questions, and should stand to benefit from the experiences of others described in this review.
Disclosure
Nothing to report.
1. US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Transitional Care Management Services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. Fact sheet ICN 908628.. Accessed June 29, 2016.
2. Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, Wright SM. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142-148. PubMed
3. Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219. PubMed
4. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. PubMed
5. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. PubMed
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441-1447. PubMed
7. DeLia D, Tong J, Gaboda D, Casalino LP. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007-2010. Medicare Medicaid Res Rev. 2014;4(2). PubMed
8. Dedhia P, Kravet S, Bulger J, et al. A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc. 2009;57(9):1540-1546. PubMed
9. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
10. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. PubMed
11. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. PubMed
12. Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372. PubMed
13. Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol. 2014;25(9):2079-2087. PubMed
14. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. PubMed
15. Fidahussein SS, Croghan IT, Cha SS, Klocke DL. Posthospital follow-up visits and 30-day readmission rates in chronic obstructive pulmonary disease. Risk Manag Healthc Policy. 2014;7:105-112. PubMed
16. Burke RE, Whitfield E, Prochazka AV. Effect of a hospitalist-run postdischarge clinic on outcomes. J Hosp Med. 2014;9(1):7-12. PubMed
17. Doctoroff L, Nijhawan A, McNally D, Vanka A, Yu R, Mukamal KJ. The characteristics and impact of a hospitalist-staffed post-discharge clinic. Am J Med. 2013;126(11):1016.e9-e15. PubMed
18. Allaudeen N, Schnipper JL, Orav EJ, Wachter RM, Vidyarthi AR. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26(7):771-776. PubMed
19. Barnett ML, Hsu J, McWilliams J. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803-1812. PubMed
20. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. PubMed
21. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. PubMed
22. Capp R, Camp-Binford M, Sobolewski S, Bulmer S, Kelley L. Do adult Medicaid enrollees prefer going to their primary care provider’s clinic rather than emergency department (ED) for low acuity conditions? Med Care. 2015;53(6):530-533. PubMed
23. Vargas Bustamante A, Fang H, Garza J, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146-155. PubMed
24. Chi JT, Handcock MS. Identifying sources of health care underutilization among California’s immigrants. J Racial Ethn Health Disparities. 2014;1(3):207-218. PubMed
25. Martinez S. Bridging the Gap: Discharge Clinics Providing Safe Transitions for High Risk Patients. Workshop presented at: Northwest Patient Safety Conference; May 15, 2012; Seattle, WA. http://www.wapatientsafety.org/downloads/Martinez.pdf. Published 2011. Accessed April 26, 2017.
26. Elliott K, W Klein J, Basu A, Sabbatini AK. Transitional care clinics for follow-up and primary care linkage for patients discharged from the ED. Am J Emerg Med. 2016;34(7):1230-1235. PubMed
27. Baxley EG, Weir S. Advanced access in academic settings: definitional challenges. Ann Fam Med. 2009;7(1):90-91. PubMed
28. Doctoroff L, McNally D, Vanka A, Nall R, Mukamal KJ. Inpatient–outpatient transitions for patients with resident primary care physicians: access and readmission. Am J Med. 2014;127(9):886.e15-e20. PubMed
29. Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2016;6(2):64-69. PubMed
30. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24. PubMed
31. Milstein A, Gilbertson E. American medical home runs. Health Aff (Millwood). 2009;28(5):1317-1326. PubMed
32. Reuben DB. Physicians in supporting roles in chronic disease care: the CareMore model. J Am Geriatr Soc. 2011;59(1):158-160. PubMed
33. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777. PubMed
34. Burke RE, Ryan P. Postdischarge clinics: hospitalist attitudes and experiences. J Hosp Med. 2013;8(10):578-581. PubMed
Readmission prevention is paramount for hospitals and, by extension, hospitalist programs. Hospitalists see early and reliable outpatient follow-up as a safe landing for their most complicated patient cases. The option of a postdischarge clinic arises from the challenge to arrange adequate postdischarge care for patients who lack easy access because of insurance or provider availability. Guaranteeing postdischarge access by opening a dedicated, hospitalist-led postdischarge clinic appears to be an easy solution, but it is a solution that requires significant investment (including investment in physician and staff training and administrative support) and careful navigation of existing primary care relationships. In addition, a clinic staffed only with physicians may not be well equipped to address the complex social factors in healthcare utilization and readmission. Better understanding of the evidence supporting post discharge physician visits, several models of clinics, and the key operational questions are essential to address before crossing the inpatient-outpatient divide.
POSTDISCHARGE PHYSICIAN VISITS AND READMISSIONS
A postdischarge outpatient provider visit is often seen as a key factor in reducing readmissions. In 2013, Medicare added strength to this association by establishing transitional care management codes, which provide enhanced reimbursement to providers for a visit within 7 or 14 days of discharge, with focused attention on transitional issues.1 However, whether a postdischarge visit reduces readmissions remains unclear. Given evidence that higher primary care density is associated with lower healthcare utilization,2 CMS’s financial investment in incentivizing post discharge physician visits may be a good bet. On the other hand, simply having a primary care physician (PCP) may be a risk factor for readmission. This association suggests that postdischarge vigilance leads to identification of medical problems that lead to rehospitalization.3 This uncertainty is not resolved in systematic reviews of readmission reduction initiatives, which were not focused solely on the impact of a physician visit.4,5
The earliest study of postdischarge visits in a general medical population found an association between intensive outpatient follow-up by new providers in a Veterans Affairs population and an increase in hospital readmissions.6 This model is similar to some hospitalist models for postdischarge clinics, as the visit was with a noncontinuity provider. The largest recent study, of patients hospitalized with acute myocardial infarction, community-acquired pneumonia, or congestive heart failure (CHF) between 2009 and 2012, found increased frequency of postdischarge follow-up but no concomitant reduction in readmissions.7 Although small observational studies8 have found a postdischarge primary care visit may reduce the risk for readmission in general medical patients, the bulk of the recent data is negative.
In high-risk patients, however, there may be a clear benefit to postdischarge follow-up. In a North Carolina Medicaid population, a physician visit after discharge was associated with fewer readmissions among high-risk patients, but not among lower risk patients, whose readmission rates were low to start.9 The results of that study support the idea that risk stratification may identify patients who can benefit from more intensive outpatient follow-up. In general medical populations, existing studies may suffer from an absence of adequate risk assessment.
The evidence in specific disease states may show a clearer association between a postdischarge physician visit and reduced risk for readmission. One quarter of patients with CHF are rehospitalized within 30 days of discharge.10 In this disease with frequent exacerbations, a clinic visit to monitor volume status, weight, and medication adherence might reduce the frequency of readmissions or prolong the interval between rehospitalizations. A large observational study observed that earlier post discharge follow up by a cardiologist or a PCP was associated with lower risk of readmission, but only in the quintile with the closest follow-up. In addition, fewer than 40% of patients in this group had a visit within 7 days.11 In another heart failure population, follow-up with either a PCP or cardiologist within 7 days of discharge was again associated with lower risk for readmission.12 Thus, data suggest a protective effect of postdischarge visits in CHF patients, in contrast to a general medical population. Patients with end-stage renal disease may also fit in this group protected by a postdischarge physician visit, as 1 additional visit within the month after discharge was estimated to reduce rehospitalizations and produce significant cost savings.13
With other specific discharge diagnoses, results are varied. Two small observational studies in chronic obstructive pulmonary disease had conflicting results—one found a modest reduction in readmission and emergency department (ED) visits for patients seen by a PCP or pulmonologist within 30 days of discharge,14 and the other found no effect on readmissions but an associated reduction in mortality.15 More data are needed to clarify further the interaction of postdischarge visits with mortality, but the association between postdischarge physician visits and readmission reduction is controversial for patients with chronic obstructive pulmonary disease.
Finally, the evidence for dedicated postdischarge clinics is even more limited. A study of a hospitalist-led postdischarge clinic in a Veterans Affairs hospital found reduced length of stay and earlier postdischarge follow-up in a postdischarge clinic, but no effect on readmissions.16 Other studies have found earlier postdischarge follow-up with dedicated discharge clinics but have not evaluated readmission rates specifically.17In summary, the effect of postdischarge visits on risk for readmission is an area of active research, but remains unclear. The data reviewed suggest a benefit for the highest risk patients, specifically those with severe chronic illness, or those deemed high-risk with a readmission tool.9 At present, because physicians cannot accurately predict which patients will be readmitted,18 discharging physicians often take a broad approach and schedule outpatient visits for all patients. As readmission tools are further refined, the group of patients who will benefit from postdischarge care will be easier to identify, and a benefit to postdischarge visits may be seen
It is also important to note that this review emphasizes the physician visit and its potential impact on readmissions. Socioeconomic causes are increasingly being recognized as driving readmissions and other utilization.19 Whether an isolated physician visit is sufficient to prevent readmissions for patients with nonmedical drivers of healthcare utilization is unclear. For those patients, a discharge visit likely is a necessary component of a readmission reduction strategy for high-risk patients, but may be insufficient for patients who require not just an isolated visit but rather a more integrated and comprehensive care program.8,20,21
POSTDISCHARGE CLINIC MODELS
Despite the unclear relationship between postdischarge physician care and readmissions, dedicated postdischarge clinics, some staffed by hospitalists, have been adopted over the past 10 years. The three primary types of clinics arise in safety net environments, in academic medical centers, and as comprehensive high-risk patient solutions. Reviewing several types of clinics further clarifies the nature of this structural innovation.
Safety Net Hospital Models
Safety net hospitals and their hospitalists struggle with securing adequate postdischarge access for their population, which has inadequate insurance and poor access to primary care. Patient characteristics also play a role in the complex postdischarge care for this population, given its high rate of ED use (owing to perceived convenience and capabilities) for ambulatory-sensitive conditions.22 In addition, immigrants, particularly those with low English-language proficiency, underuse and have poor access to primary care.23,24 Postdischarge clinics in this environment focus first on providing a reliable postdischarge plan and then on linking to primary care. Examples of two clinics are at Harborview Medical Center in Seattle, Washington25 and Texas Health in Fort Worth.
Harborview is a 400-bed hospital affiliated with the University of Washington. More than 50% of its patients are considered indigent. The clinic was established in 2007 to provide a postdischarge option for uninsured patients, and a link to primary care in federally qualified health centers. The clinic was staffed 5 days a week with one or two hospitalists or advanced practice nurses. Visit duration was 20 minutes, 270 visits occurred per month, and the no-show rate was 30%. A small subgroup of the hospitalist group staffed the clinic. Particular clinical foci included CHF patients, patients with wound-care needs, and homeless, immigrant, and recently incarcerated patients. A key goal was connecting to longitudinal primary care, and the clinic successfully connected more than 70% of patients to primary care in community health centers. This clinic ultimately transitioned from a hospitalist practice to a primary care practice with a primary focus on post-ED follow-up for unaffiliated patients.26
In 2010, Texas Health faced a similar challenge with unaffiliated patients, and established a nurse practitioner–based clinic with hospitalist oversight to provide care primarily for patients without insurance or without an existing primary care relationship.
Academic Medical Center Models
Another clinical model is designed for patients who receive primary care at practices affiliated with academic medical centers. Although many of these patients have insurance and a PCP, there is often no availability with their continuity provider, because of the resident’s inpatient schedule or the faculty member’s conflicting priorities.27,28 Academic medical centers, including the University of California at San Francisco, the University of New Mexico, and the Beth Israel Deaconess Medical Center, have established discharge clinics within their faculty primary care practices. A model of this type of clinic was set up at Beth Israel Deaconess in 2010. Staffed by four hospitalists and using 40-minute appointments, this clinic was physically based in the primary care practice. As such, it took advantage of the existing clinic’s administrative and clinical functions, including triage, billing, and scheduling. A visit was scheduled in that clinic by the discharging physician team if a primary care appointment was not available with the patient’s continuity provider. Visits were standardized and focused on outstanding issues at discharge, medication reconciliation, and symptom trajectory. The hospitalists used the clinic’s clinical resources, including nurses, social workers, and pharmacists, but had no other dedicated staff. That there were only four hospitalists meant they were able to gain sufficient exposure to the outpatient setting, provide consistent high-quality care, and gain credibility with the PCPs. As the patients who were seen had PCPs of their own, during the visit significant attention was focused first on the postdischarge concerns, and then on promptly returning the patients to routine primary care. Significant patient outreach was used to address the clinic’s no-show rate, which was almost 50% in the early months. Within a year, the rate was down, closer to 20%. This clinic closed in 2015 after the primary care practice, in which it was based, transitioned to a patient-centered medical home. Since that time, this type of initiative has spread further, with neurohospitalist discharge clinics established, and postdischarge neurology follow-up becoming faster and more reliable.29
Academic medical centers and safety net hospitals substitute for routine primary care to address the basic challenge of primary care access, often without significant enhancements or additional resources, such as dedicated care management and pharmacy, social work, and nursing support. Commonalities of these clinics include dedicated physician staff, appointments generally longer than average outpatient appointments, and visit content concentrated on the key issues at transition (medication reconciliation, outstanding tests, symptom trajectory). As possible, clinics adopted a multidisciplinary approach, with social workers, community health workers, and nurses, to respond to the breadth of patients’ postdischarge needs, which often extend beyond pure medical need. The most frequent barriers encountered included the knowledge gap for hospitalist providers in the outpatient setting (a gap mitigated by using dedicated providers) and the patients’ high no-show rate (not surprising given that the providers are generally new to them). Few clinics have attempted to create continuity across inpatient and outpatient providers, though continuity might reduce no-shows as well as eliminate at least 1 transition.
Comprehensive High-Risk Patient Solutions
At the other end of the clinic spectrum are more integrated postdischarge approaches, which also evolved from the hospitalist model with hospitalist staffing. However, these approaches were introduced in response to the clinical needs of the highest risk patients (who are most vulnerable to frequent provider transitions), not to a systemic inability to provide routine postdischarge care.30
The most long-standing model for this type of clinic is represented by CareMore Health System, a subsidiary of Anthem.30-32 The extensivist, an expanded-scope hospitalist, acts as primary care coordinator, coordinating a multidisciplinary team for a panel of about 100 patients, representing the sickest 5% of the Medicare Advantage–insured population. Unlike the traditional hospitalist, the extensivist follows patients across all care sites, including hospital, rehabilitation sites, and outpatient clinic. For the most part, this relationship is not designed to evolve into a longitudinal relationship, but rather is an intervention only for the several-months period of acute need. Internal data have shown effects on hospital readmissions as well as length of stay.30
Another integrated clinic was established in 2013, at the University of Chicago. This was an effort to redesign care for patients at highest risk for hospitalization.33 Similar to the CareMore process, a high-risk population is identified by prior hospitalization and expected high Medicare costs. A comprehensive care physician cares for these patients across care settings. The clinic takes a team-based approach to patient care, with team members selected on the basis of patient need. Physicians have panels limited to only 200 patients, and generally spend part of the day in clinic, and part in seeing their hospitalized patients. Although reminiscent of a traditional primary care setting, this clinic is designed specifically for a high-risk, frequently hospitalized population, and therefore requires physicians with both a skill set akin to that of hospitalists, and an approach of palliative care and holistic patient care. Outcomes from this trial clinic are expected in 2017 or 2018.
LOGISTICAL CONSIDERATIONS FOR DISCHARGE CLINICS
Considering some key operational questions (Table) can help guide hospitals, hospitalists, and healthcare systems as they venture into the postdischarge clinic space. Return on investment and sustainability are two key questions for postdischarge clinics.
Return on investment varies by payment structure. In capitated environments with a strong emphasis on readmissions and total medical expenditure, a successful postdischarge clinic would recoup the investment through readmission reduction. However, maintaining adequate patient volume against high no-show rates may strain the group financially. In addition, although a hospitalist group may reap few measurable benefits from this clinical exposure, the unique view of the outpatient world afforded to hospitalists working in this environment could enrich the group as a whole by providing a more well-rounded vantage point.
Another key question surrounds sustainability. The clinic at the Beth Israel Deaconess Medical Center in Boston temporarily closed due to high inpatient volume and corresponding need for those hospitalists in the inpatient setting, early in its inception. It subsequently closed due to evolution in the clinic where it was based, rendering it unnecessary. Clinics that are contingent on other clinics will be vulnerable to external forces. Finally, staffing these clinics may be a stretch for a hospitalist group, as a partly different skill set is required for patient care in the outpatient setting. Hospitalists interested in care transitions are well suited for this role. In addition, hospitalists interested in more clinical variety, or in more schedule variety than that provided in a traditional hospitalist schedule, often enjoy the work. A vast majority of hospitalists think PCPs are responsible for postdischarge problems, and would not be interested in working in the postdischarge world.34 A poor fit for providers may lead to clinic failure.
As evident from this review, gaps in understanding the benefits of postdischarge care have persisted for 10 years. Discharge clinics have been scantly described in the literature. The primary unanswered question remains the effect on readmissions, but this has been the sole research focus to date. Other key research areas are the impact on other patient-centered clinical and system outcomes (eg, patient satisfaction, particularly for patients seeing new providers), postdischarge mortality, the effect on other adverse events, and total medical expenditure.
The healthcare system is evolving in the context of a focus on readmissions, primary care access challenges, and high-risk patients’ specific needs. These forces are spurring innovation in the realm of postdischarge physician clinics, as even the basic need for an appointment may not be met by the existing outpatient primary care system. In this context, multiple new outpatient care structures have arisen, many staffed by hospitalists. Some, such as clinics based in safety net hospitals and academic medical centers, address the simple requirement that patients who lack easy access, because of insurance status or provider availability, can see a doctor after discharge. This type of clinic may be an essential step in alleviating a strained system but may not represent a sustainable long-term solution. More comprehensive solutions for improving patient care and clinical outcomes may be offered by integrated systems, such as CareMore, which also emerged from the hospitalist model. A lasting question is whether these clinics, both the narrowly focused and the comprehensive, will have longevity in the evolving healthcare market. Inevitably, though, hospitalist directors will continue to raise such questions, and should stand to benefit from the experiences of others described in this review.
Disclosure
Nothing to report.
Readmission prevention is paramount for hospitals and, by extension, hospitalist programs. Hospitalists see early and reliable outpatient follow-up as a safe landing for their most complicated patient cases. The option of a postdischarge clinic arises from the challenge to arrange adequate postdischarge care for patients who lack easy access because of insurance or provider availability. Guaranteeing postdischarge access by opening a dedicated, hospitalist-led postdischarge clinic appears to be an easy solution, but it is a solution that requires significant investment (including investment in physician and staff training and administrative support) and careful navigation of existing primary care relationships. In addition, a clinic staffed only with physicians may not be well equipped to address the complex social factors in healthcare utilization and readmission. Better understanding of the evidence supporting post discharge physician visits, several models of clinics, and the key operational questions are essential to address before crossing the inpatient-outpatient divide.
POSTDISCHARGE PHYSICIAN VISITS AND READMISSIONS
A postdischarge outpatient provider visit is often seen as a key factor in reducing readmissions. In 2013, Medicare added strength to this association by establishing transitional care management codes, which provide enhanced reimbursement to providers for a visit within 7 or 14 days of discharge, with focused attention on transitional issues.1 However, whether a postdischarge visit reduces readmissions remains unclear. Given evidence that higher primary care density is associated with lower healthcare utilization,2 CMS’s financial investment in incentivizing post discharge physician visits may be a good bet. On the other hand, simply having a primary care physician (PCP) may be a risk factor for readmission. This association suggests that postdischarge vigilance leads to identification of medical problems that lead to rehospitalization.3 This uncertainty is not resolved in systematic reviews of readmission reduction initiatives, which were not focused solely on the impact of a physician visit.4,5
The earliest study of postdischarge visits in a general medical population found an association between intensive outpatient follow-up by new providers in a Veterans Affairs population and an increase in hospital readmissions.6 This model is similar to some hospitalist models for postdischarge clinics, as the visit was with a noncontinuity provider. The largest recent study, of patients hospitalized with acute myocardial infarction, community-acquired pneumonia, or congestive heart failure (CHF) between 2009 and 2012, found increased frequency of postdischarge follow-up but no concomitant reduction in readmissions.7 Although small observational studies8 have found a postdischarge primary care visit may reduce the risk for readmission in general medical patients, the bulk of the recent data is negative.
In high-risk patients, however, there may be a clear benefit to postdischarge follow-up. In a North Carolina Medicaid population, a physician visit after discharge was associated with fewer readmissions among high-risk patients, but not among lower risk patients, whose readmission rates were low to start.9 The results of that study support the idea that risk stratification may identify patients who can benefit from more intensive outpatient follow-up. In general medical populations, existing studies may suffer from an absence of adequate risk assessment.
The evidence in specific disease states may show a clearer association between a postdischarge physician visit and reduced risk for readmission. One quarter of patients with CHF are rehospitalized within 30 days of discharge.10 In this disease with frequent exacerbations, a clinic visit to monitor volume status, weight, and medication adherence might reduce the frequency of readmissions or prolong the interval between rehospitalizations. A large observational study observed that earlier post discharge follow up by a cardiologist or a PCP was associated with lower risk of readmission, but only in the quintile with the closest follow-up. In addition, fewer than 40% of patients in this group had a visit within 7 days.11 In another heart failure population, follow-up with either a PCP or cardiologist within 7 days of discharge was again associated with lower risk for readmission.12 Thus, data suggest a protective effect of postdischarge visits in CHF patients, in contrast to a general medical population. Patients with end-stage renal disease may also fit in this group protected by a postdischarge physician visit, as 1 additional visit within the month after discharge was estimated to reduce rehospitalizations and produce significant cost savings.13
With other specific discharge diagnoses, results are varied. Two small observational studies in chronic obstructive pulmonary disease had conflicting results—one found a modest reduction in readmission and emergency department (ED) visits for patients seen by a PCP or pulmonologist within 30 days of discharge,14 and the other found no effect on readmissions but an associated reduction in mortality.15 More data are needed to clarify further the interaction of postdischarge visits with mortality, but the association between postdischarge physician visits and readmission reduction is controversial for patients with chronic obstructive pulmonary disease.
Finally, the evidence for dedicated postdischarge clinics is even more limited. A study of a hospitalist-led postdischarge clinic in a Veterans Affairs hospital found reduced length of stay and earlier postdischarge follow-up in a postdischarge clinic, but no effect on readmissions.16 Other studies have found earlier postdischarge follow-up with dedicated discharge clinics but have not evaluated readmission rates specifically.17In summary, the effect of postdischarge visits on risk for readmission is an area of active research, but remains unclear. The data reviewed suggest a benefit for the highest risk patients, specifically those with severe chronic illness, or those deemed high-risk with a readmission tool.9 At present, because physicians cannot accurately predict which patients will be readmitted,18 discharging physicians often take a broad approach and schedule outpatient visits for all patients. As readmission tools are further refined, the group of patients who will benefit from postdischarge care will be easier to identify, and a benefit to postdischarge visits may be seen
It is also important to note that this review emphasizes the physician visit and its potential impact on readmissions. Socioeconomic causes are increasingly being recognized as driving readmissions and other utilization.19 Whether an isolated physician visit is sufficient to prevent readmissions for patients with nonmedical drivers of healthcare utilization is unclear. For those patients, a discharge visit likely is a necessary component of a readmission reduction strategy for high-risk patients, but may be insufficient for patients who require not just an isolated visit but rather a more integrated and comprehensive care program.8,20,21
POSTDISCHARGE CLINIC MODELS
Despite the unclear relationship between postdischarge physician care and readmissions, dedicated postdischarge clinics, some staffed by hospitalists, have been adopted over the past 10 years. The three primary types of clinics arise in safety net environments, in academic medical centers, and as comprehensive high-risk patient solutions. Reviewing several types of clinics further clarifies the nature of this structural innovation.
Safety Net Hospital Models
Safety net hospitals and their hospitalists struggle with securing adequate postdischarge access for their population, which has inadequate insurance and poor access to primary care. Patient characteristics also play a role in the complex postdischarge care for this population, given its high rate of ED use (owing to perceived convenience and capabilities) for ambulatory-sensitive conditions.22 In addition, immigrants, particularly those with low English-language proficiency, underuse and have poor access to primary care.23,24 Postdischarge clinics in this environment focus first on providing a reliable postdischarge plan and then on linking to primary care. Examples of two clinics are at Harborview Medical Center in Seattle, Washington25 and Texas Health in Fort Worth.
Harborview is a 400-bed hospital affiliated with the University of Washington. More than 50% of its patients are considered indigent. The clinic was established in 2007 to provide a postdischarge option for uninsured patients, and a link to primary care in federally qualified health centers. The clinic was staffed 5 days a week with one or two hospitalists or advanced practice nurses. Visit duration was 20 minutes, 270 visits occurred per month, and the no-show rate was 30%. A small subgroup of the hospitalist group staffed the clinic. Particular clinical foci included CHF patients, patients with wound-care needs, and homeless, immigrant, and recently incarcerated patients. A key goal was connecting to longitudinal primary care, and the clinic successfully connected more than 70% of patients to primary care in community health centers. This clinic ultimately transitioned from a hospitalist practice to a primary care practice with a primary focus on post-ED follow-up for unaffiliated patients.26
In 2010, Texas Health faced a similar challenge with unaffiliated patients, and established a nurse practitioner–based clinic with hospitalist oversight to provide care primarily for patients without insurance or without an existing primary care relationship.
Academic Medical Center Models
Another clinical model is designed for patients who receive primary care at practices affiliated with academic medical centers. Although many of these patients have insurance and a PCP, there is often no availability with their continuity provider, because of the resident’s inpatient schedule or the faculty member’s conflicting priorities.27,28 Academic medical centers, including the University of California at San Francisco, the University of New Mexico, and the Beth Israel Deaconess Medical Center, have established discharge clinics within their faculty primary care practices. A model of this type of clinic was set up at Beth Israel Deaconess in 2010. Staffed by four hospitalists and using 40-minute appointments, this clinic was physically based in the primary care practice. As such, it took advantage of the existing clinic’s administrative and clinical functions, including triage, billing, and scheduling. A visit was scheduled in that clinic by the discharging physician team if a primary care appointment was not available with the patient’s continuity provider. Visits were standardized and focused on outstanding issues at discharge, medication reconciliation, and symptom trajectory. The hospitalists used the clinic’s clinical resources, including nurses, social workers, and pharmacists, but had no other dedicated staff. That there were only four hospitalists meant they were able to gain sufficient exposure to the outpatient setting, provide consistent high-quality care, and gain credibility with the PCPs. As the patients who were seen had PCPs of their own, during the visit significant attention was focused first on the postdischarge concerns, and then on promptly returning the patients to routine primary care. Significant patient outreach was used to address the clinic’s no-show rate, which was almost 50% in the early months. Within a year, the rate was down, closer to 20%. This clinic closed in 2015 after the primary care practice, in which it was based, transitioned to a patient-centered medical home. Since that time, this type of initiative has spread further, with neurohospitalist discharge clinics established, and postdischarge neurology follow-up becoming faster and more reliable.29
Academic medical centers and safety net hospitals substitute for routine primary care to address the basic challenge of primary care access, often without significant enhancements or additional resources, such as dedicated care management and pharmacy, social work, and nursing support. Commonalities of these clinics include dedicated physician staff, appointments generally longer than average outpatient appointments, and visit content concentrated on the key issues at transition (medication reconciliation, outstanding tests, symptom trajectory). As possible, clinics adopted a multidisciplinary approach, with social workers, community health workers, and nurses, to respond to the breadth of patients’ postdischarge needs, which often extend beyond pure medical need. The most frequent barriers encountered included the knowledge gap for hospitalist providers in the outpatient setting (a gap mitigated by using dedicated providers) and the patients’ high no-show rate (not surprising given that the providers are generally new to them). Few clinics have attempted to create continuity across inpatient and outpatient providers, though continuity might reduce no-shows as well as eliminate at least 1 transition.
Comprehensive High-Risk Patient Solutions
At the other end of the clinic spectrum are more integrated postdischarge approaches, which also evolved from the hospitalist model with hospitalist staffing. However, these approaches were introduced in response to the clinical needs of the highest risk patients (who are most vulnerable to frequent provider transitions), not to a systemic inability to provide routine postdischarge care.30
The most long-standing model for this type of clinic is represented by CareMore Health System, a subsidiary of Anthem.30-32 The extensivist, an expanded-scope hospitalist, acts as primary care coordinator, coordinating a multidisciplinary team for a panel of about 100 patients, representing the sickest 5% of the Medicare Advantage–insured population. Unlike the traditional hospitalist, the extensivist follows patients across all care sites, including hospital, rehabilitation sites, and outpatient clinic. For the most part, this relationship is not designed to evolve into a longitudinal relationship, but rather is an intervention only for the several-months period of acute need. Internal data have shown effects on hospital readmissions as well as length of stay.30
Another integrated clinic was established in 2013, at the University of Chicago. This was an effort to redesign care for patients at highest risk for hospitalization.33 Similar to the CareMore process, a high-risk population is identified by prior hospitalization and expected high Medicare costs. A comprehensive care physician cares for these patients across care settings. The clinic takes a team-based approach to patient care, with team members selected on the basis of patient need. Physicians have panels limited to only 200 patients, and generally spend part of the day in clinic, and part in seeing their hospitalized patients. Although reminiscent of a traditional primary care setting, this clinic is designed specifically for a high-risk, frequently hospitalized population, and therefore requires physicians with both a skill set akin to that of hospitalists, and an approach of palliative care and holistic patient care. Outcomes from this trial clinic are expected in 2017 or 2018.
LOGISTICAL CONSIDERATIONS FOR DISCHARGE CLINICS
Considering some key operational questions (Table) can help guide hospitals, hospitalists, and healthcare systems as they venture into the postdischarge clinic space. Return on investment and sustainability are two key questions for postdischarge clinics.
Return on investment varies by payment structure. In capitated environments with a strong emphasis on readmissions and total medical expenditure, a successful postdischarge clinic would recoup the investment through readmission reduction. However, maintaining adequate patient volume against high no-show rates may strain the group financially. In addition, although a hospitalist group may reap few measurable benefits from this clinical exposure, the unique view of the outpatient world afforded to hospitalists working in this environment could enrich the group as a whole by providing a more well-rounded vantage point.
Another key question surrounds sustainability. The clinic at the Beth Israel Deaconess Medical Center in Boston temporarily closed due to high inpatient volume and corresponding need for those hospitalists in the inpatient setting, early in its inception. It subsequently closed due to evolution in the clinic where it was based, rendering it unnecessary. Clinics that are contingent on other clinics will be vulnerable to external forces. Finally, staffing these clinics may be a stretch for a hospitalist group, as a partly different skill set is required for patient care in the outpatient setting. Hospitalists interested in care transitions are well suited for this role. In addition, hospitalists interested in more clinical variety, or in more schedule variety than that provided in a traditional hospitalist schedule, often enjoy the work. A vast majority of hospitalists think PCPs are responsible for postdischarge problems, and would not be interested in working in the postdischarge world.34 A poor fit for providers may lead to clinic failure.
As evident from this review, gaps in understanding the benefits of postdischarge care have persisted for 10 years. Discharge clinics have been scantly described in the literature. The primary unanswered question remains the effect on readmissions, but this has been the sole research focus to date. Other key research areas are the impact on other patient-centered clinical and system outcomes (eg, patient satisfaction, particularly for patients seeing new providers), postdischarge mortality, the effect on other adverse events, and total medical expenditure.
The healthcare system is evolving in the context of a focus on readmissions, primary care access challenges, and high-risk patients’ specific needs. These forces are spurring innovation in the realm of postdischarge physician clinics, as even the basic need for an appointment may not be met by the existing outpatient primary care system. In this context, multiple new outpatient care structures have arisen, many staffed by hospitalists. Some, such as clinics based in safety net hospitals and academic medical centers, address the simple requirement that patients who lack easy access, because of insurance status or provider availability, can see a doctor after discharge. This type of clinic may be an essential step in alleviating a strained system but may not represent a sustainable long-term solution. More comprehensive solutions for improving patient care and clinical outcomes may be offered by integrated systems, such as CareMore, which also emerged from the hospitalist model. A lasting question is whether these clinics, both the narrowly focused and the comprehensive, will have longevity in the evolving healthcare market. Inevitably, though, hospitalist directors will continue to raise such questions, and should stand to benefit from the experiences of others described in this review.
Disclosure
Nothing to report.
1. US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Transitional Care Management Services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. Fact sheet ICN 908628.. Accessed June 29, 2016.
2. Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, Wright SM. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142-148. PubMed
3. Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219. PubMed
4. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. PubMed
5. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. PubMed
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441-1447. PubMed
7. DeLia D, Tong J, Gaboda D, Casalino LP. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007-2010. Medicare Medicaid Res Rev. 2014;4(2). PubMed
8. Dedhia P, Kravet S, Bulger J, et al. A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc. 2009;57(9):1540-1546. PubMed
9. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
10. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. PubMed
11. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. PubMed
12. Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372. PubMed
13. Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol. 2014;25(9):2079-2087. PubMed
14. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. PubMed
15. Fidahussein SS, Croghan IT, Cha SS, Klocke DL. Posthospital follow-up visits and 30-day readmission rates in chronic obstructive pulmonary disease. Risk Manag Healthc Policy. 2014;7:105-112. PubMed
16. Burke RE, Whitfield E, Prochazka AV. Effect of a hospitalist-run postdischarge clinic on outcomes. J Hosp Med. 2014;9(1):7-12. PubMed
17. Doctoroff L, Nijhawan A, McNally D, Vanka A, Yu R, Mukamal KJ. The characteristics and impact of a hospitalist-staffed post-discharge clinic. Am J Med. 2013;126(11):1016.e9-e15. PubMed
18. Allaudeen N, Schnipper JL, Orav EJ, Wachter RM, Vidyarthi AR. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26(7):771-776. PubMed
19. Barnett ML, Hsu J, McWilliams J. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803-1812. PubMed
20. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. PubMed
21. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. PubMed
22. Capp R, Camp-Binford M, Sobolewski S, Bulmer S, Kelley L. Do adult Medicaid enrollees prefer going to their primary care provider’s clinic rather than emergency department (ED) for low acuity conditions? Med Care. 2015;53(6):530-533. PubMed
23. Vargas Bustamante A, Fang H, Garza J, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146-155. PubMed
24. Chi JT, Handcock MS. Identifying sources of health care underutilization among California’s immigrants. J Racial Ethn Health Disparities. 2014;1(3):207-218. PubMed
25. Martinez S. Bridging the Gap: Discharge Clinics Providing Safe Transitions for High Risk Patients. Workshop presented at: Northwest Patient Safety Conference; May 15, 2012; Seattle, WA. http://www.wapatientsafety.org/downloads/Martinez.pdf. Published 2011. Accessed April 26, 2017.
26. Elliott K, W Klein J, Basu A, Sabbatini AK. Transitional care clinics for follow-up and primary care linkage for patients discharged from the ED. Am J Emerg Med. 2016;34(7):1230-1235. PubMed
27. Baxley EG, Weir S. Advanced access in academic settings: definitional challenges. Ann Fam Med. 2009;7(1):90-91. PubMed
28. Doctoroff L, McNally D, Vanka A, Nall R, Mukamal KJ. Inpatient–outpatient transitions for patients with resident primary care physicians: access and readmission. Am J Med. 2014;127(9):886.e15-e20. PubMed
29. Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2016;6(2):64-69. PubMed
30. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24. PubMed
31. Milstein A, Gilbertson E. American medical home runs. Health Aff (Millwood). 2009;28(5):1317-1326. PubMed
32. Reuben DB. Physicians in supporting roles in chronic disease care: the CareMore model. J Am Geriatr Soc. 2011;59(1):158-160. PubMed
33. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777. PubMed
34. Burke RE, Ryan P. Postdischarge clinics: hospitalist attitudes and experiences. J Hosp Med. 2013;8(10):578-581. PubMed
1. US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Transitional Care Management Services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. Fact sheet ICN 908628.. Accessed June 29, 2016.
2. Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, Wright SM. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142-148. PubMed
3. Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219. PubMed
4. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. PubMed
5. Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107. PubMed
6. Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441-1447. PubMed
7. DeLia D, Tong J, Gaboda D, Casalino LP. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007-2010. Medicare Medicaid Res Rev. 2014;4(2). PubMed
8. Dedhia P, Kravet S, Bulger J, et al. A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc. 2009;57(9):1540-1546. PubMed
9. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. PubMed
10. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. PubMed
11. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. PubMed
12. Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372. PubMed
13. Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol. 2014;25(9):2079-2087. PubMed
14. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664-1670. PubMed
15. Fidahussein SS, Croghan IT, Cha SS, Klocke DL. Posthospital follow-up visits and 30-day readmission rates in chronic obstructive pulmonary disease. Risk Manag Healthc Policy. 2014;7:105-112. PubMed
16. Burke RE, Whitfield E, Prochazka AV. Effect of a hospitalist-run postdischarge clinic on outcomes. J Hosp Med. 2014;9(1):7-12. PubMed
17. Doctoroff L, Nijhawan A, McNally D, Vanka A, Yu R, Mukamal KJ. The characteristics and impact of a hospitalist-staffed post-discharge clinic. Am J Med. 2013;126(11):1016.e9-e15. PubMed
18. Allaudeen N, Schnipper JL, Orav EJ, Wachter RM, Vidyarthi AR. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011;26(7):771-776. PubMed
19. Barnett ML, Hsu J, McWilliams J. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803-1812. PubMed
20. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187. PubMed
21. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. PubMed
22. Capp R, Camp-Binford M, Sobolewski S, Bulmer S, Kelley L. Do adult Medicaid enrollees prefer going to their primary care provider’s clinic rather than emergency department (ED) for low acuity conditions? Med Care. 2015;53(6):530-533. PubMed
23. Vargas Bustamante A, Fang H, Garza J, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146-155. PubMed
24. Chi JT, Handcock MS. Identifying sources of health care underutilization among California’s immigrants. J Racial Ethn Health Disparities. 2014;1(3):207-218. PubMed
25. Martinez S. Bridging the Gap: Discharge Clinics Providing Safe Transitions for High Risk Patients. Workshop presented at: Northwest Patient Safety Conference; May 15, 2012; Seattle, WA. http://www.wapatientsafety.org/downloads/Martinez.pdf. Published 2011. Accessed April 26, 2017.
26. Elliott K, W Klein J, Basu A, Sabbatini AK. Transitional care clinics for follow-up and primary care linkage for patients discharged from the ED. Am J Emerg Med. 2016;34(7):1230-1235. PubMed
27. Baxley EG, Weir S. Advanced access in academic settings: definitional challenges. Ann Fam Med. 2009;7(1):90-91. PubMed
28. Doctoroff L, McNally D, Vanka A, Nall R, Mukamal KJ. Inpatient–outpatient transitions for patients with resident primary care physicians: access and readmission. Am J Med. 2014;127(9):886.e15-e20. PubMed
29. Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2016;6(2):64-69. PubMed
30. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24. PubMed
31. Milstein A, Gilbertson E. American medical home runs. Health Aff (Millwood). 2009;28(5):1317-1326. PubMed
32. Reuben DB. Physicians in supporting roles in chronic disease care: the CareMore model. J Am Geriatr Soc. 2011;59(1):158-160. PubMed
33. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777. PubMed
34. Burke RE, Ryan P. Postdischarge clinics: hospitalist attitudes and experiences. J Hosp Med. 2013;8(10):578-581. PubMed
© 2017 Society of Hospital Medicine
In the Literature: The latest research you need to know
In This Edition
Literature At A Glance
A guide to this month’s studies
- High-dose vs. low-dose clopidogrel after cardiac stenting
- Rates of overdiagnosis of PE with CTPA
- Outcomes of hospitalists with PAs or residents
- White coats and MRSA
- Correlation of vital signs and pain
- Rate of asymptomatic perioperative MI
- Relationship of opioid prescription patterns and overdose
- Interdisciplinary rounds and rates of adverse events
High-Dose Clopidogrel Is Not Superior to Standard-Dose Clopidogrel in Patients with High On-Treatment Platelet Activity after Percutaneous Corona
Clinical question: In patients with high on-treatment platelet activity, does the use of high-dose clopidogrel after percutaneous coronary intervention (PCI) decrease the risk of cardiovascular events?
Background: In patients receiving clopidogrel, high platelet reactivity after PCI is associated with an increase in cardiovascular events. At present, treatments targeted at this population are not well-defined.
Study design: Randomized, double-blind, active-control trial.
Setting: Eighty-three centers in North America.
Synopsis: Researchers randomized 2,214 patients with drug-eluting stents to receive either high-dose clopidogrel (600 mg initial dose, 150 mg daily thereafter) or standard-dose clopidogrel (no additional loading dose, 75 mg daily). At six months, the primary endpoint of death from cardiovascular causes, nonfatal myocardial infarction, or stent thrombosis was no different in the two groups (2.3% in the high-dose group versus 2.3% in the standard-dose group; hazard ratio 1.01).
Bottom line: High-dose clopidogrel adds no benefit over standard-dose clopidogrel in patients with high platelet reactivity who have undergone PCI with drug-eluting stent placement.
Citation: Price MJ, Berger PB, Teirstein PS, et al. Standard- vs. high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA. 2011;305(11):1097-1105.
Computed Tomographic Pulmonary Angiography (CTPA) Is Associated with Overdiagnosis and Overtreatment of Pulmonary Embolism (PE)
Clinical question: Is the use of CTPA associated with increased incidence of PE and increased complications from anticoagulation treatment?
Background: CTPA is a sensitive, noninvasive test for diagnosing PE that could have a drawback: identifying potentially clinically unimportant (small) pulmonary emboli that subsequently are treated. Overtreatment might be associated with patient harm due to increased complications of anticoagulation therapy.
Study design: Time-trend analysis of PE between the pre-CTPA period (1993 to 1998) and the post-CTPA period (1998 to 2006).
Setting: Nongovernmental U.S. hospitals.
Synopsis: The Nationwide Inpatient Sample and Multiple Cause-of-Death databases were used to determine national estimates of hospitalization for PE, along with morbidity and mortality from PE.
The age-adjusted analysis revealed a statistically significant increase in the incidence of PE diagnosis after introduction of CTPA (to 112 per 100,000 from 62 per 100,000), with minimal change in overall PE mortality. This was accompanied by a substantial reduction in PE case-fatality rate, the rate of hospital deaths among patients with a diagnosis of pulmonary embolism.
Availability of CTPA was associated with a significant increase in anticoagulation complication rates (to 5.3 per 100,000 from 3.1 per 100,000), including statistically significant increases in gastrointestinal hemorrhage and secondary thrombocytopenia, and a trend toward higher rates of intracranial hemorrhage.
Bottom line: Introduction of CTPA was associated with changes suggestive of overdiagnosis (increased incidence, relatively unchanged mortality) and overtreatment (increased complication rates) of PE, but it remains unknown which small PEs are clinically significant.
Citation: Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med. 2011;171(9):831-837.
Hospitalist-Physician Assistant Teams Associated with Longer Length of Stay, No Change in Mortality, Readmission Rates
Clinical question: Do length of stay (LOS), hospital mortality, or readmission rate change if hospitalists and physician assistants, or the traditional resident-hospitalist teams, provide the patient care?
Background: Resident work-hour limitations require new models of care for hospitalized patients. Many academic medical centers have hired physician assistants to work with hospitalists to provide care. Little is known about how these models affect such outcomes as LOS, inpatient mortality rates, and readmission rates.
Study design: Retrospective cohort.
Setting: A 430-bed urban academic medical center in Milwaukee.
Synopsis: Administrative data were gathered on 9,681 patients admitted to the general medical service. Of those enrolled, 2,171 were cared for by a hospitalist-physician assistant (H-PA) team, while resident-hospitalist teams cared for 7,510 patients. Patient assignment was dependent on time of admission but not on patient complexity. Patients admitted overnight after the resident team capped were assigned to the H-PA team the next morning, resulting in increased transitions of care for the H-PA team.
Adjusted analyses revealed a 6.45% increase in LOS for the H-PA team compared with the resident team. Charges, inpatient mortality, and readmission rates at seven, 14, and 30 days were unchanged. Subgroup analyses revealed smaller differences in LOS for H-PA teams and resident-hospitalist teams with the same hospitalist (LOS 5.44% higher, P=0.081).
Conclusions from this study are limited due to lack of randomization of assignment, the retrospective design, and the use of administrative data at one institution.
Bottom line: Hospitalist-PA teams might result in a slightly increased LOS compared with the traditional resident teams; however, inpatient mortality and readmission rates are similar.
Citation: Singh S, Fletcher KE, Schapira MM, et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist-physician assistant model vs a traditional resident-based model. J Hosp Med. 2011;6:122-130.
Washing White Coats Does Not Lower MRSA Bacterial Contamination
Clinical question: Are clean, short-sleeved uniforms less likely to carry MRSA than regularly laundered long-sleeved white coats?
Background: Studies have shown that bacteria frequently colonize in physician garments. However, evidence that short-sleeved garments or newly laundered garments are less likely to be contaminated has been lacking. Despite the paucity of evidence, the British Department of Health barred the use of traditional white coats and long-sleeved garments in 2007.
Study design: Prospective, randomized, controlled trial.
Setting: Urban U.S. hospital.
Synopsis: Study authors randomized 100 internal-medicine residents and hospitalists to their own long-sleeved white coats or freshly laundered short-sleeved uniforms from August 2008 to November 2009. Swabs were taken from the sleeves of the white coats or uniform, the breast pocket, and the volar wrist surface of the dominant hand. Swabs were cultured for MRSA and for general colony count.
Results showed no significant difference in colony counts or MRSA colonization in any of the sites tested between the newly laundered uniforms and the white coats. Additionally, there was no effect in relation to the frequency of laundering the white coats. Notably, within three hours of donning freshly laundered uniforms, bacterial counts approached 50% of the total bacterial counts seen at eight hours.
Bottom line: Laundering of uniforms does not affect MRSA colonization rate or general bacterial burden on physician uniforms or skin surfaces, though the effect on nosocomial infection has not been established.
Citation: Burden M, Cervantes L, Weed D, Keniston A, Price CS, Albert RK. Newly cleaned physician uniforms and infrequently washed white coats have similar rates of bacterial contamination after an 8-hour workday: a randomized controlled trial. J Hosp Med. 2011;6:177-182.
Self-Reported Pain Severity Does Not Correlate with Heart Rate or Blood Pressure Measurements in Pre-Hospital Setting
Clinical question: Do measured vital signs, including heart rate, blood pressure, and respiratory rate, correlate with the degree of self-reported pain?
Background: Because pain often can be associated with alterations in autonomic tone, it has been hypothesized that alterations in vital signs will occur in patients who report pain.
Study design: Retrospective cohort study.
Setting: Pre-hospital in Melbourne, Australia.
Synopsis: The authors reviewed all ambulance patient care records for patients age >14 years with a Glasgow Coma Score (GCS) >12 transported to a hospital during a seven-day period in 2005. Patients were selected for analysis if their patient care record included an initial assessment of pain severity, as measured by a numeric rating scale (NRS), in which patients rate their pain from 0 to 10.
More than half of the 3,357 patients transported by paramedics during the period were included in this analysis (n=1286). There was no correlation between heart rate or systolic blood pressure with the degree of self-reported pain. Although an increased respiratory rate was statistically correlated with a higher rating of pain, this relationship was not clinically significant, as each one-point increase in the pain rating scale was associated with a 0.16-breaths-per-minute increase in the respiratory rate.
Limitations included the large number of records excluded from analysis because pain was not evaluated, as well as numerous unmeasured confounders, including active disease processes such as sepsis, that were not accounted for.
Bottom line: Severity of pain did not correlate with heart rate or systolic blood pressure in the pre-hospital setting.
Citation: Lord B, Woollard M. The reliability of vital signs in estimating pain severity among adult patients treated by paramedics. Emerg Med J. 2011;28:147-150.
Asymptomatic Perioperative Myocardial Infarction Is Common in Patients Undergoing Noncardiac Surgery
Clinical question: In patients undergoing noncardiac surgery, what is the incidence and clinical characteristics of perioperative myocardial infarction (MI)?
Background: Though millions of patients experience perioperative MI after noncardiac surgery, little is known about the characteristics and outcomes of these patients.
Study design: Cohort study.
Setting: One hundred ninety centers in 23 countries.
Synopsis: Using data from the 8,351 patients in the POISE (PeriOperative ISchemic Evaluation) trial, this study showed that perioperative MI occurred in 5% of patients; 65% were asymptomatic. Patients who experienced postoperative MI were older and had more cardiovascular risk factors when compared to those who did not. The 30-day mortality was higher in patients with a perioperative MI (11.6%) compared with those who did not (2.2%); the presence or absence of ischemic symptoms was not associated with mortality rate.
Of the 8.3% of patients who experienced an elevation in cardiac biomarkers but who did not meet the definition of MI, there was an increased risk of nonfatal cardiac arrest and nonacute coronary revascularization. Those in the highest quartile also had increased 30-day mortality.
Bottom line: Given the high proportion of asymptomatic MIs and isolated elevations in cardiac biomarkers and the association between these events and increased risk of death, hospitalists should consider routine monitoring of troponin in at-risk patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154(8):523-528.
Patients Prescribed Higher Opioid Doses Are at Increased Risk of Opioid Overdose Death
Clinical question: What is the association between opioid prescribing patterns and fatal opioid overdose?
Background: In the past 10 years, the rate of fatal overdose from opioid prescription for pain has more than doubled. Little is known about how the indications (substance abuse disorders, cancer-related pain, chronic pain, acute pain), maximal daily dose, and scheduling (standing, as-needed, or both) of opioid prescriptions relate to this increased risk.
Study design: Case-cohort study.
Setting: Veterans Health Administration (VHA) patients.
Synopsis: The VHA’s National Patient Care Database was used to randomly select a cohort of 154,684 nonhospice/nonpalliative-care patients who were prescribed opioids from 2004 to 2008. They were compared with 750 patients who were treated with prescription opioids who died from opioid overdose during this time.
Fatal opioid overdose was a rare event (0.04%), but risk increased with higher prescribed maximum daily morphine dose-equivalence, especially when greater than or equal to 50 mg/day in all subgroups (substance abuse, acute and chronic pain, and cancer). Fatal overdoses were higher in middle-aged white men with acute or chronic pain, substance abuse disorders, and other psychiatric illness. Patients with cancer were at increased risk of fatal overdose if they were prescribed as-needed opioids alone.
Treatment with both as-needed and standing opioids did not statistically affect risk of overdose death in any subgroup.
Bottom line: Although rare, risk of fatal opioid overdose in patients prescribed opiate medication increases with higher maximum prescribed daily dose.
Citation: Bohnert AS, Valenstein M, Bair M, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011; 305:1315-1321.
Structured Interdisciplinary Rounds on Medical Teaching Unit Significantly Decrease Adverse Events
Clinical question: Do structured interdisciplinary rounds have an impact on the rate of adverse events?
Background: Many preventable adverse events occurring during hospitalization can be attributed to communication failures. Structured interdisciplinary rounds provide a format as well as a forum for team members to discuss patient care. Prior studies demonstrated improvements in collaboration; whether this translates to better patient care is not known.
Study design: Retrospective cohort using historic and concurrent control.
Setting: Tertiary-care teaching hospital in Chicago.
Synopsis: Structured interdisciplinary rounds, led by a nurse manager and medical director, and including nurses, residents, pharmacists, social workers, and case managers, were implemented on a medical teaching unit. New patients were discussed using a structured communication tool; existing patients were discussed in an unstructured format. Medical records were abstracted for 370 patients hospitalized after implementation of the intervention, equally divided between intervention and control units. One hundred eighty-five patients hospitalized on the intervention unit prior to the implementation of rounds served as a historic control.
Patients in the intervention unit had significantly lower rates of total adverse events (3.9 per 100 patient days in the intervention, compared with 7.2 and 7.7 per 100 patient days for the concurrent and historic control units, respectively), and preventable adverse events (0.9 per 100 patient days, compared with 2.8 and 2.1 per 100 patient days for the concurrent and historic controls, respectively).
Limitations of the study include lack of blinding of the medical record, slightly different patient populations in intervention and control groups, and the one-hospital setting, which could limit generalizability.
Bottom line: Structured interdisciplinary rounds might serve to improve communication between nurses, pharmacists, and physicians, resulting in decreases in adverse events.
Citation: O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
In This Edition
Literature At A Glance
A guide to this month’s studies
- High-dose vs. low-dose clopidogrel after cardiac stenting
- Rates of overdiagnosis of PE with CTPA
- Outcomes of hospitalists with PAs or residents
- White coats and MRSA
- Correlation of vital signs and pain
- Rate of asymptomatic perioperative MI
- Relationship of opioid prescription patterns and overdose
- Interdisciplinary rounds and rates of adverse events
High-Dose Clopidogrel Is Not Superior to Standard-Dose Clopidogrel in Patients with High On-Treatment Platelet Activity after Percutaneous Corona
Clinical question: In patients with high on-treatment platelet activity, does the use of high-dose clopidogrel after percutaneous coronary intervention (PCI) decrease the risk of cardiovascular events?
Background: In patients receiving clopidogrel, high platelet reactivity after PCI is associated with an increase in cardiovascular events. At present, treatments targeted at this population are not well-defined.
Study design: Randomized, double-blind, active-control trial.
Setting: Eighty-three centers in North America.
Synopsis: Researchers randomized 2,214 patients with drug-eluting stents to receive either high-dose clopidogrel (600 mg initial dose, 150 mg daily thereafter) or standard-dose clopidogrel (no additional loading dose, 75 mg daily). At six months, the primary endpoint of death from cardiovascular causes, nonfatal myocardial infarction, or stent thrombosis was no different in the two groups (2.3% in the high-dose group versus 2.3% in the standard-dose group; hazard ratio 1.01).
Bottom line: High-dose clopidogrel adds no benefit over standard-dose clopidogrel in patients with high platelet reactivity who have undergone PCI with drug-eluting stent placement.
Citation: Price MJ, Berger PB, Teirstein PS, et al. Standard- vs. high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA. 2011;305(11):1097-1105.
Computed Tomographic Pulmonary Angiography (CTPA) Is Associated with Overdiagnosis and Overtreatment of Pulmonary Embolism (PE)
Clinical question: Is the use of CTPA associated with increased incidence of PE and increased complications from anticoagulation treatment?
Background: CTPA is a sensitive, noninvasive test for diagnosing PE that could have a drawback: identifying potentially clinically unimportant (small) pulmonary emboli that subsequently are treated. Overtreatment might be associated with patient harm due to increased complications of anticoagulation therapy.
Study design: Time-trend analysis of PE between the pre-CTPA period (1993 to 1998) and the post-CTPA period (1998 to 2006).
Setting: Nongovernmental U.S. hospitals.
Synopsis: The Nationwide Inpatient Sample and Multiple Cause-of-Death databases were used to determine national estimates of hospitalization for PE, along with morbidity and mortality from PE.
The age-adjusted analysis revealed a statistically significant increase in the incidence of PE diagnosis after introduction of CTPA (to 112 per 100,000 from 62 per 100,000), with minimal change in overall PE mortality. This was accompanied by a substantial reduction in PE case-fatality rate, the rate of hospital deaths among patients with a diagnosis of pulmonary embolism.
Availability of CTPA was associated with a significant increase in anticoagulation complication rates (to 5.3 per 100,000 from 3.1 per 100,000), including statistically significant increases in gastrointestinal hemorrhage and secondary thrombocytopenia, and a trend toward higher rates of intracranial hemorrhage.
Bottom line: Introduction of CTPA was associated with changes suggestive of overdiagnosis (increased incidence, relatively unchanged mortality) and overtreatment (increased complication rates) of PE, but it remains unknown which small PEs are clinically significant.
Citation: Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med. 2011;171(9):831-837.
Hospitalist-Physician Assistant Teams Associated with Longer Length of Stay, No Change in Mortality, Readmission Rates
Clinical question: Do length of stay (LOS), hospital mortality, or readmission rate change if hospitalists and physician assistants, or the traditional resident-hospitalist teams, provide the patient care?
Background: Resident work-hour limitations require new models of care for hospitalized patients. Many academic medical centers have hired physician assistants to work with hospitalists to provide care. Little is known about how these models affect such outcomes as LOS, inpatient mortality rates, and readmission rates.
Study design: Retrospective cohort.
Setting: A 430-bed urban academic medical center in Milwaukee.
Synopsis: Administrative data were gathered on 9,681 patients admitted to the general medical service. Of those enrolled, 2,171 were cared for by a hospitalist-physician assistant (H-PA) team, while resident-hospitalist teams cared for 7,510 patients. Patient assignment was dependent on time of admission but not on patient complexity. Patients admitted overnight after the resident team capped were assigned to the H-PA team the next morning, resulting in increased transitions of care for the H-PA team.
Adjusted analyses revealed a 6.45% increase in LOS for the H-PA team compared with the resident team. Charges, inpatient mortality, and readmission rates at seven, 14, and 30 days were unchanged. Subgroup analyses revealed smaller differences in LOS for H-PA teams and resident-hospitalist teams with the same hospitalist (LOS 5.44% higher, P=0.081).
Conclusions from this study are limited due to lack of randomization of assignment, the retrospective design, and the use of administrative data at one institution.
Bottom line: Hospitalist-PA teams might result in a slightly increased LOS compared with the traditional resident teams; however, inpatient mortality and readmission rates are similar.
Citation: Singh S, Fletcher KE, Schapira MM, et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist-physician assistant model vs a traditional resident-based model. J Hosp Med. 2011;6:122-130.
Washing White Coats Does Not Lower MRSA Bacterial Contamination
Clinical question: Are clean, short-sleeved uniforms less likely to carry MRSA than regularly laundered long-sleeved white coats?
Background: Studies have shown that bacteria frequently colonize in physician garments. However, evidence that short-sleeved garments or newly laundered garments are less likely to be contaminated has been lacking. Despite the paucity of evidence, the British Department of Health barred the use of traditional white coats and long-sleeved garments in 2007.
Study design: Prospective, randomized, controlled trial.
Setting: Urban U.S. hospital.
Synopsis: Study authors randomized 100 internal-medicine residents and hospitalists to their own long-sleeved white coats or freshly laundered short-sleeved uniforms from August 2008 to November 2009. Swabs were taken from the sleeves of the white coats or uniform, the breast pocket, and the volar wrist surface of the dominant hand. Swabs were cultured for MRSA and for general colony count.
Results showed no significant difference in colony counts or MRSA colonization in any of the sites tested between the newly laundered uniforms and the white coats. Additionally, there was no effect in relation to the frequency of laundering the white coats. Notably, within three hours of donning freshly laundered uniforms, bacterial counts approached 50% of the total bacterial counts seen at eight hours.
Bottom line: Laundering of uniforms does not affect MRSA colonization rate or general bacterial burden on physician uniforms or skin surfaces, though the effect on nosocomial infection has not been established.
Citation: Burden M, Cervantes L, Weed D, Keniston A, Price CS, Albert RK. Newly cleaned physician uniforms and infrequently washed white coats have similar rates of bacterial contamination after an 8-hour workday: a randomized controlled trial. J Hosp Med. 2011;6:177-182.
Self-Reported Pain Severity Does Not Correlate with Heart Rate or Blood Pressure Measurements in Pre-Hospital Setting
Clinical question: Do measured vital signs, including heart rate, blood pressure, and respiratory rate, correlate with the degree of self-reported pain?
Background: Because pain often can be associated with alterations in autonomic tone, it has been hypothesized that alterations in vital signs will occur in patients who report pain.
Study design: Retrospective cohort study.
Setting: Pre-hospital in Melbourne, Australia.
Synopsis: The authors reviewed all ambulance patient care records for patients age >14 years with a Glasgow Coma Score (GCS) >12 transported to a hospital during a seven-day period in 2005. Patients were selected for analysis if their patient care record included an initial assessment of pain severity, as measured by a numeric rating scale (NRS), in which patients rate their pain from 0 to 10.
More than half of the 3,357 patients transported by paramedics during the period were included in this analysis (n=1286). There was no correlation between heart rate or systolic blood pressure with the degree of self-reported pain. Although an increased respiratory rate was statistically correlated with a higher rating of pain, this relationship was not clinically significant, as each one-point increase in the pain rating scale was associated with a 0.16-breaths-per-minute increase in the respiratory rate.
Limitations included the large number of records excluded from analysis because pain was not evaluated, as well as numerous unmeasured confounders, including active disease processes such as sepsis, that were not accounted for.
Bottom line: Severity of pain did not correlate with heart rate or systolic blood pressure in the pre-hospital setting.
Citation: Lord B, Woollard M. The reliability of vital signs in estimating pain severity among adult patients treated by paramedics. Emerg Med J. 2011;28:147-150.
Asymptomatic Perioperative Myocardial Infarction Is Common in Patients Undergoing Noncardiac Surgery
Clinical question: In patients undergoing noncardiac surgery, what is the incidence and clinical characteristics of perioperative myocardial infarction (MI)?
Background: Though millions of patients experience perioperative MI after noncardiac surgery, little is known about the characteristics and outcomes of these patients.
Study design: Cohort study.
Setting: One hundred ninety centers in 23 countries.
Synopsis: Using data from the 8,351 patients in the POISE (PeriOperative ISchemic Evaluation) trial, this study showed that perioperative MI occurred in 5% of patients; 65% were asymptomatic. Patients who experienced postoperative MI were older and had more cardiovascular risk factors when compared to those who did not. The 30-day mortality was higher in patients with a perioperative MI (11.6%) compared with those who did not (2.2%); the presence or absence of ischemic symptoms was not associated with mortality rate.
Of the 8.3% of patients who experienced an elevation in cardiac biomarkers but who did not meet the definition of MI, there was an increased risk of nonfatal cardiac arrest and nonacute coronary revascularization. Those in the highest quartile also had increased 30-day mortality.
Bottom line: Given the high proportion of asymptomatic MIs and isolated elevations in cardiac biomarkers and the association between these events and increased risk of death, hospitalists should consider routine monitoring of troponin in at-risk patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154(8):523-528.
Patients Prescribed Higher Opioid Doses Are at Increased Risk of Opioid Overdose Death
Clinical question: What is the association between opioid prescribing patterns and fatal opioid overdose?
Background: In the past 10 years, the rate of fatal overdose from opioid prescription for pain has more than doubled. Little is known about how the indications (substance abuse disorders, cancer-related pain, chronic pain, acute pain), maximal daily dose, and scheduling (standing, as-needed, or both) of opioid prescriptions relate to this increased risk.
Study design: Case-cohort study.
Setting: Veterans Health Administration (VHA) patients.
Synopsis: The VHA’s National Patient Care Database was used to randomly select a cohort of 154,684 nonhospice/nonpalliative-care patients who were prescribed opioids from 2004 to 2008. They were compared with 750 patients who were treated with prescription opioids who died from opioid overdose during this time.
Fatal opioid overdose was a rare event (0.04%), but risk increased with higher prescribed maximum daily morphine dose-equivalence, especially when greater than or equal to 50 mg/day in all subgroups (substance abuse, acute and chronic pain, and cancer). Fatal overdoses were higher in middle-aged white men with acute or chronic pain, substance abuse disorders, and other psychiatric illness. Patients with cancer were at increased risk of fatal overdose if they were prescribed as-needed opioids alone.
Treatment with both as-needed and standing opioids did not statistically affect risk of overdose death in any subgroup.
Bottom line: Although rare, risk of fatal opioid overdose in patients prescribed opiate medication increases with higher maximum prescribed daily dose.
Citation: Bohnert AS, Valenstein M, Bair M, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011; 305:1315-1321.
Structured Interdisciplinary Rounds on Medical Teaching Unit Significantly Decrease Adverse Events
Clinical question: Do structured interdisciplinary rounds have an impact on the rate of adverse events?
Background: Many preventable adverse events occurring during hospitalization can be attributed to communication failures. Structured interdisciplinary rounds provide a format as well as a forum for team members to discuss patient care. Prior studies demonstrated improvements in collaboration; whether this translates to better patient care is not known.
Study design: Retrospective cohort using historic and concurrent control.
Setting: Tertiary-care teaching hospital in Chicago.
Synopsis: Structured interdisciplinary rounds, led by a nurse manager and medical director, and including nurses, residents, pharmacists, social workers, and case managers, were implemented on a medical teaching unit. New patients were discussed using a structured communication tool; existing patients were discussed in an unstructured format. Medical records were abstracted for 370 patients hospitalized after implementation of the intervention, equally divided between intervention and control units. One hundred eighty-five patients hospitalized on the intervention unit prior to the implementation of rounds served as a historic control.
Patients in the intervention unit had significantly lower rates of total adverse events (3.9 per 100 patient days in the intervention, compared with 7.2 and 7.7 per 100 patient days for the concurrent and historic control units, respectively), and preventable adverse events (0.9 per 100 patient days, compared with 2.8 and 2.1 per 100 patient days for the concurrent and historic controls, respectively).
Limitations of the study include lack of blinding of the medical record, slightly different patient populations in intervention and control groups, and the one-hospital setting, which could limit generalizability.
Bottom line: Structured interdisciplinary rounds might serve to improve communication between nurses, pharmacists, and physicians, resulting in decreases in adverse events.
Citation: O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
In This Edition
Literature At A Glance
A guide to this month’s studies
- High-dose vs. low-dose clopidogrel after cardiac stenting
- Rates of overdiagnosis of PE with CTPA
- Outcomes of hospitalists with PAs or residents
- White coats and MRSA
- Correlation of vital signs and pain
- Rate of asymptomatic perioperative MI
- Relationship of opioid prescription patterns and overdose
- Interdisciplinary rounds and rates of adverse events
High-Dose Clopidogrel Is Not Superior to Standard-Dose Clopidogrel in Patients with High On-Treatment Platelet Activity after Percutaneous Corona
Clinical question: In patients with high on-treatment platelet activity, does the use of high-dose clopidogrel after percutaneous coronary intervention (PCI) decrease the risk of cardiovascular events?
Background: In patients receiving clopidogrel, high platelet reactivity after PCI is associated with an increase in cardiovascular events. At present, treatments targeted at this population are not well-defined.
Study design: Randomized, double-blind, active-control trial.
Setting: Eighty-three centers in North America.
Synopsis: Researchers randomized 2,214 patients with drug-eluting stents to receive either high-dose clopidogrel (600 mg initial dose, 150 mg daily thereafter) or standard-dose clopidogrel (no additional loading dose, 75 mg daily). At six months, the primary endpoint of death from cardiovascular causes, nonfatal myocardial infarction, or stent thrombosis was no different in the two groups (2.3% in the high-dose group versus 2.3% in the standard-dose group; hazard ratio 1.01).
Bottom line: High-dose clopidogrel adds no benefit over standard-dose clopidogrel in patients with high platelet reactivity who have undergone PCI with drug-eluting stent placement.
Citation: Price MJ, Berger PB, Teirstein PS, et al. Standard- vs. high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA. 2011;305(11):1097-1105.
Computed Tomographic Pulmonary Angiography (CTPA) Is Associated with Overdiagnosis and Overtreatment of Pulmonary Embolism (PE)
Clinical question: Is the use of CTPA associated with increased incidence of PE and increased complications from anticoagulation treatment?
Background: CTPA is a sensitive, noninvasive test for diagnosing PE that could have a drawback: identifying potentially clinically unimportant (small) pulmonary emboli that subsequently are treated. Overtreatment might be associated with patient harm due to increased complications of anticoagulation therapy.
Study design: Time-trend analysis of PE between the pre-CTPA period (1993 to 1998) and the post-CTPA period (1998 to 2006).
Setting: Nongovernmental U.S. hospitals.
Synopsis: The Nationwide Inpatient Sample and Multiple Cause-of-Death databases were used to determine national estimates of hospitalization for PE, along with morbidity and mortality from PE.
The age-adjusted analysis revealed a statistically significant increase in the incidence of PE diagnosis after introduction of CTPA (to 112 per 100,000 from 62 per 100,000), with minimal change in overall PE mortality. This was accompanied by a substantial reduction in PE case-fatality rate, the rate of hospital deaths among patients with a diagnosis of pulmonary embolism.
Availability of CTPA was associated with a significant increase in anticoagulation complication rates (to 5.3 per 100,000 from 3.1 per 100,000), including statistically significant increases in gastrointestinal hemorrhage and secondary thrombocytopenia, and a trend toward higher rates of intracranial hemorrhage.
Bottom line: Introduction of CTPA was associated with changes suggestive of overdiagnosis (increased incidence, relatively unchanged mortality) and overtreatment (increased complication rates) of PE, but it remains unknown which small PEs are clinically significant.
Citation: Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med. 2011;171(9):831-837.
Hospitalist-Physician Assistant Teams Associated with Longer Length of Stay, No Change in Mortality, Readmission Rates
Clinical question: Do length of stay (LOS), hospital mortality, or readmission rate change if hospitalists and physician assistants, or the traditional resident-hospitalist teams, provide the patient care?
Background: Resident work-hour limitations require new models of care for hospitalized patients. Many academic medical centers have hired physician assistants to work with hospitalists to provide care. Little is known about how these models affect such outcomes as LOS, inpatient mortality rates, and readmission rates.
Study design: Retrospective cohort.
Setting: A 430-bed urban academic medical center in Milwaukee.
Synopsis: Administrative data were gathered on 9,681 patients admitted to the general medical service. Of those enrolled, 2,171 were cared for by a hospitalist-physician assistant (H-PA) team, while resident-hospitalist teams cared for 7,510 patients. Patient assignment was dependent on time of admission but not on patient complexity. Patients admitted overnight after the resident team capped were assigned to the H-PA team the next morning, resulting in increased transitions of care for the H-PA team.
Adjusted analyses revealed a 6.45% increase in LOS for the H-PA team compared with the resident team. Charges, inpatient mortality, and readmission rates at seven, 14, and 30 days were unchanged. Subgroup analyses revealed smaller differences in LOS for H-PA teams and resident-hospitalist teams with the same hospitalist (LOS 5.44% higher, P=0.081).
Conclusions from this study are limited due to lack of randomization of assignment, the retrospective design, and the use of administrative data at one institution.
Bottom line: Hospitalist-PA teams might result in a slightly increased LOS compared with the traditional resident teams; however, inpatient mortality and readmission rates are similar.
Citation: Singh S, Fletcher KE, Schapira MM, et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist-physician assistant model vs a traditional resident-based model. J Hosp Med. 2011;6:122-130.
Washing White Coats Does Not Lower MRSA Bacterial Contamination
Clinical question: Are clean, short-sleeved uniforms less likely to carry MRSA than regularly laundered long-sleeved white coats?
Background: Studies have shown that bacteria frequently colonize in physician garments. However, evidence that short-sleeved garments or newly laundered garments are less likely to be contaminated has been lacking. Despite the paucity of evidence, the British Department of Health barred the use of traditional white coats and long-sleeved garments in 2007.
Study design: Prospective, randomized, controlled trial.
Setting: Urban U.S. hospital.
Synopsis: Study authors randomized 100 internal-medicine residents and hospitalists to their own long-sleeved white coats or freshly laundered short-sleeved uniforms from August 2008 to November 2009. Swabs were taken from the sleeves of the white coats or uniform, the breast pocket, and the volar wrist surface of the dominant hand. Swabs were cultured for MRSA and for general colony count.
Results showed no significant difference in colony counts or MRSA colonization in any of the sites tested between the newly laundered uniforms and the white coats. Additionally, there was no effect in relation to the frequency of laundering the white coats. Notably, within three hours of donning freshly laundered uniforms, bacterial counts approached 50% of the total bacterial counts seen at eight hours.
Bottom line: Laundering of uniforms does not affect MRSA colonization rate or general bacterial burden on physician uniforms or skin surfaces, though the effect on nosocomial infection has not been established.
Citation: Burden M, Cervantes L, Weed D, Keniston A, Price CS, Albert RK. Newly cleaned physician uniforms and infrequently washed white coats have similar rates of bacterial contamination after an 8-hour workday: a randomized controlled trial. J Hosp Med. 2011;6:177-182.
Self-Reported Pain Severity Does Not Correlate with Heart Rate or Blood Pressure Measurements in Pre-Hospital Setting
Clinical question: Do measured vital signs, including heart rate, blood pressure, and respiratory rate, correlate with the degree of self-reported pain?
Background: Because pain often can be associated with alterations in autonomic tone, it has been hypothesized that alterations in vital signs will occur in patients who report pain.
Study design: Retrospective cohort study.
Setting: Pre-hospital in Melbourne, Australia.
Synopsis: The authors reviewed all ambulance patient care records for patients age >14 years with a Glasgow Coma Score (GCS) >12 transported to a hospital during a seven-day period in 2005. Patients were selected for analysis if their patient care record included an initial assessment of pain severity, as measured by a numeric rating scale (NRS), in which patients rate their pain from 0 to 10.
More than half of the 3,357 patients transported by paramedics during the period were included in this analysis (n=1286). There was no correlation between heart rate or systolic blood pressure with the degree of self-reported pain. Although an increased respiratory rate was statistically correlated with a higher rating of pain, this relationship was not clinically significant, as each one-point increase in the pain rating scale was associated with a 0.16-breaths-per-minute increase in the respiratory rate.
Limitations included the large number of records excluded from analysis because pain was not evaluated, as well as numerous unmeasured confounders, including active disease processes such as sepsis, that were not accounted for.
Bottom line: Severity of pain did not correlate with heart rate or systolic blood pressure in the pre-hospital setting.
Citation: Lord B, Woollard M. The reliability of vital signs in estimating pain severity among adult patients treated by paramedics. Emerg Med J. 2011;28:147-150.
Asymptomatic Perioperative Myocardial Infarction Is Common in Patients Undergoing Noncardiac Surgery
Clinical question: In patients undergoing noncardiac surgery, what is the incidence and clinical characteristics of perioperative myocardial infarction (MI)?
Background: Though millions of patients experience perioperative MI after noncardiac surgery, little is known about the characteristics and outcomes of these patients.
Study design: Cohort study.
Setting: One hundred ninety centers in 23 countries.
Synopsis: Using data from the 8,351 patients in the POISE (PeriOperative ISchemic Evaluation) trial, this study showed that perioperative MI occurred in 5% of patients; 65% were asymptomatic. Patients who experienced postoperative MI were older and had more cardiovascular risk factors when compared to those who did not. The 30-day mortality was higher in patients with a perioperative MI (11.6%) compared with those who did not (2.2%); the presence or absence of ischemic symptoms was not associated with mortality rate.
Of the 8.3% of patients who experienced an elevation in cardiac biomarkers but who did not meet the definition of MI, there was an increased risk of nonfatal cardiac arrest and nonacute coronary revascularization. Those in the highest quartile also had increased 30-day mortality.
Bottom line: Given the high proportion of asymptomatic MIs and isolated elevations in cardiac biomarkers and the association between these events and increased risk of death, hospitalists should consider routine monitoring of troponin in at-risk patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154(8):523-528.
Patients Prescribed Higher Opioid Doses Are at Increased Risk of Opioid Overdose Death
Clinical question: What is the association between opioid prescribing patterns and fatal opioid overdose?
Background: In the past 10 years, the rate of fatal overdose from opioid prescription for pain has more than doubled. Little is known about how the indications (substance abuse disorders, cancer-related pain, chronic pain, acute pain), maximal daily dose, and scheduling (standing, as-needed, or both) of opioid prescriptions relate to this increased risk.
Study design: Case-cohort study.
Setting: Veterans Health Administration (VHA) patients.
Synopsis: The VHA’s National Patient Care Database was used to randomly select a cohort of 154,684 nonhospice/nonpalliative-care patients who were prescribed opioids from 2004 to 2008. They were compared with 750 patients who were treated with prescription opioids who died from opioid overdose during this time.
Fatal opioid overdose was a rare event (0.04%), but risk increased with higher prescribed maximum daily morphine dose-equivalence, especially when greater than or equal to 50 mg/day in all subgroups (substance abuse, acute and chronic pain, and cancer). Fatal overdoses were higher in middle-aged white men with acute or chronic pain, substance abuse disorders, and other psychiatric illness. Patients with cancer were at increased risk of fatal overdose if they were prescribed as-needed opioids alone.
Treatment with both as-needed and standing opioids did not statistically affect risk of overdose death in any subgroup.
Bottom line: Although rare, risk of fatal opioid overdose in patients prescribed opiate medication increases with higher maximum prescribed daily dose.
Citation: Bohnert AS, Valenstein M, Bair M, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011; 305:1315-1321.
Structured Interdisciplinary Rounds on Medical Teaching Unit Significantly Decrease Adverse Events
Clinical question: Do structured interdisciplinary rounds have an impact on the rate of adverse events?
Background: Many preventable adverse events occurring during hospitalization can be attributed to communication failures. Structured interdisciplinary rounds provide a format as well as a forum for team members to discuss patient care. Prior studies demonstrated improvements in collaboration; whether this translates to better patient care is not known.
Study design: Retrospective cohort using historic and concurrent control.
Setting: Tertiary-care teaching hospital in Chicago.
Synopsis: Structured interdisciplinary rounds, led by a nurse manager and medical director, and including nurses, residents, pharmacists, social workers, and case managers, were implemented on a medical teaching unit. New patients were discussed using a structured communication tool; existing patients were discussed in an unstructured format. Medical records were abstracted for 370 patients hospitalized after implementation of the intervention, equally divided between intervention and control units. One hundred eighty-five patients hospitalized on the intervention unit prior to the implementation of rounds served as a historic control.
Patients in the intervention unit had significantly lower rates of total adverse events (3.9 per 100 patient days in the intervention, compared with 7.2 and 7.7 per 100 patient days for the concurrent and historic control units, respectively), and preventable adverse events (0.9 per 100 patient days, compared with 2.8 and 2.1 per 100 patient days for the concurrent and historic controls, respectively).
Limitations of the study include lack of blinding of the medical record, slightly different patient populations in intervention and control groups, and the one-hospital setting, which could limit generalizability.
Bottom line: Structured interdisciplinary rounds might serve to improve communication between nurses, pharmacists, and physicians, resulting in decreases in adverse events.
Citation: O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
In the Literature: Research You Need to Know
Clinical question: Is dalteparin better than unfractionated heparin at preventing venous thromboembolism (VTE) in ICU patients?
Background: VTE is an important health problem for critically ill patients, but prevention is possible, with both unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) superior to placebo in previous studies. Studies comparing UFH and LMWH in ICU patients have been inconclusive thus far.
Study design: Randomized controlled trial.
Setting: Sixty-seven ICUs in six countries from 2006 to 2010.
Synopsis: Researchers randomized 3,746 patients who met the enrollment criteria to either the LMWH dalteparin 5,000 units daily or UFH 5,000 IU twice daily. The drug was held if major bleeding occurred or the patient developed thrombocytopenia concerning heparin-induced thrombocytopenia (HIT). Patients were followed until discharge or death. VTE was evaluated by ultrasound two days after ICU admission and then twice weekly.
There was no difference in incidence of VTE in patients receiving dalteparin versus UFH [5.1% vs. 5.8%, HR 0.92 (CI 0.68-1.23), P=0.57]. Fewer pulmonary emboli occurred in the dalteparin group (1.3% vs. 2.3%, HR 0.51, P=0.01). There was no difference in major bleeding or HIT between groups.
Bottom line: Dalteparin and UFH were equally effective at preventing proximal VTE in ICU patients, but dalteparin prevented more pulmonary emboli.
Citation: The PROTECT investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2010;364(14):1305-1314.
For more physician reviews of HM-related research, visit our website.
Clinical question: Is dalteparin better than unfractionated heparin at preventing venous thromboembolism (VTE) in ICU patients?
Background: VTE is an important health problem for critically ill patients, but prevention is possible, with both unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) superior to placebo in previous studies. Studies comparing UFH and LMWH in ICU patients have been inconclusive thus far.
Study design: Randomized controlled trial.
Setting: Sixty-seven ICUs in six countries from 2006 to 2010.
Synopsis: Researchers randomized 3,746 patients who met the enrollment criteria to either the LMWH dalteparin 5,000 units daily or UFH 5,000 IU twice daily. The drug was held if major bleeding occurred or the patient developed thrombocytopenia concerning heparin-induced thrombocytopenia (HIT). Patients were followed until discharge or death. VTE was evaluated by ultrasound two days after ICU admission and then twice weekly.
There was no difference in incidence of VTE in patients receiving dalteparin versus UFH [5.1% vs. 5.8%, HR 0.92 (CI 0.68-1.23), P=0.57]. Fewer pulmonary emboli occurred in the dalteparin group (1.3% vs. 2.3%, HR 0.51, P=0.01). There was no difference in major bleeding or HIT between groups.
Bottom line: Dalteparin and UFH were equally effective at preventing proximal VTE in ICU patients, but dalteparin prevented more pulmonary emboli.
Citation: The PROTECT investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2010;364(14):1305-1314.
For more physician reviews of HM-related research, visit our website.
Clinical question: Is dalteparin better than unfractionated heparin at preventing venous thromboembolism (VTE) in ICU patients?
Background: VTE is an important health problem for critically ill patients, but prevention is possible, with both unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) superior to placebo in previous studies. Studies comparing UFH and LMWH in ICU patients have been inconclusive thus far.
Study design: Randomized controlled trial.
Setting: Sixty-seven ICUs in six countries from 2006 to 2010.
Synopsis: Researchers randomized 3,746 patients who met the enrollment criteria to either the LMWH dalteparin 5,000 units daily or UFH 5,000 IU twice daily. The drug was held if major bleeding occurred or the patient developed thrombocytopenia concerning heparin-induced thrombocytopenia (HIT). Patients were followed until discharge or death. VTE was evaluated by ultrasound two days after ICU admission and then twice weekly.
There was no difference in incidence of VTE in patients receiving dalteparin versus UFH [5.1% vs. 5.8%, HR 0.92 (CI 0.68-1.23), P=0.57]. Fewer pulmonary emboli occurred in the dalteparin group (1.3% vs. 2.3%, HR 0.51, P=0.01). There was no difference in major bleeding or HIT between groups.
Bottom line: Dalteparin and UFH were equally effective at preventing proximal VTE in ICU patients, but dalteparin prevented more pulmonary emboli.
Citation: The PROTECT investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2010;364(14):1305-1314.
For more physician reviews of HM-related research, visit our website.
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
In the Literature
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH