User login
Reducing Inappropriate Laboratory Testing in the Hospital Setting: How Low Can We Go?
From the University of Toronto (Dr. Basuita, Corey L. Kamen, and Dr. Soong) and Sinai Health System (Corey L. Kamen, Cheryl Ethier, and Dr. Soong), Toronto, Ontario, Canada. Co-first authors are Manpreet Basuita, MD, and Corey L. Kamen, BSc.
Abstract
- Objective: Routine laboratory testing is common among medical inpatients; however, when ordered inappropriately testing can represent low-value care. We examined the impact of an evidence-based intervention bundle on utilization.
- Participants/setting: This prospective cohort study took place at a tertiary academic medical center and included 6424 patients admitted to the general internal medicine service between April 2016 and March 2018.
- Intervention: An intervention bundle, whose first components were implemented in July 2016, included computer order entry restrictions on repetitive laboratory testing, education, and audit-feedback.
- Measures: Data were extracted from the hospital electronic health record. The primary outcome was the number of routine blood tests (complete blood count, creatinine, and electrolytes) ordered per inpatient day.
- Analysis: Descriptive statistics were calculated for demographic variables. We used statistical process control charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome.
- Results: The mean number of combined routine laboratory tests ordered per inpatient day decreased from 1.19 (SD, 0.21) tests to 1.11 (SD, 0.05), a relative reduction of 6.7% (P < 0.0001). Mean cost per case related to laboratory tests decreased from $17.24 in the pre-intervention period to $16.17 in the post-intervention period (relative reduction of 6.2%). This resulted in savings of $26,851 in the intervention year.
- Conclusion: A laboratory intervention bundle was associated with small reductions in testing and costs. A routine test performed less than once per inpatient day may not be clinically appropriate or possible.
Keywords: utilization; clinical costs; quality improvement; QI intervention; internal medicine; inpatient.
Routine laboratory blood testing is a commonly used diagnostic tool that physicians rely on to provide patient care. Although routine blood testing represents less than 5% of most hospital budgets, routine use and over-reliance on testing among physicians makes it a target of cost-reduction efforts.1-3 A variety of interventions have been proposed to reduce inappropriate laboratory tests, with varying results.1,4-6 Successful interventions include providing physicians with fee data associated with ordered laboratory tests, unbundling panels of tests, and multicomponent interventions.6 We conducted a multifaceted quality improvement study to promote and develop interventions to adopt appropriate blood test ordering practices.
Methods
Setting
This prospective cohort study took place at Mount Sinai Hospital, a 443-bed academic hospital affiliated with the University of Toronto, where more than 2400 learners rotate through annually. The study was approved by the Mount Sinai Hospital Research Ethics Board.
Participants
We included all inpatient admissions to the general internal medicine service between April 2016 and March 2018. Exclusion criteria included a length of stay (LOS) longer than 365 days and admission to a critical care unit. Patients with more than 1 admission were counted as separate hospital inpatient visits.
Intervention
Based on internal data, we targeted the top 3 most frequently ordered routine blood tests: complete blood count (CBC), creatinine, and electrolytes. Trainee interviews revealed that habit, bundled order sets, and fear of “missing something” contributed to inappropriate routine blood test ordering. Based on these root causes, we used the Model for Improvement to iteratively develop a multimodal intervention that began in July 2016.7,8 This included a change to the computerized provider order entry (CPOE) to nudge clinicians to a restrictive ordering strategy by substituting the “Daily x3” frequency of blood test ordering with a “Daily x1” option on a pick list of order options. Clinicians could still order daily routine blood tests for any specified duration, but would have to do so by manually changing the default setting within the CPOE.
From July 2017 to March 2018, the research team educated residents on appropriate laboratory test ordering and provided audit and feedback data to the clinicians. Diagnostic uncertainty was addressed in teaching sessions. Attending physicians were surveyed on appropriate indications for daily laboratory testing for each of CBC, electrolytes, and creatinine. Appropriate indications (Figure 1) were displayed in visible clinical areas and incorporated into teaching sessions.9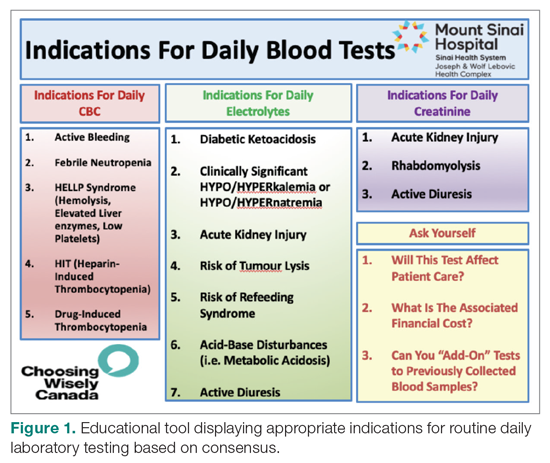
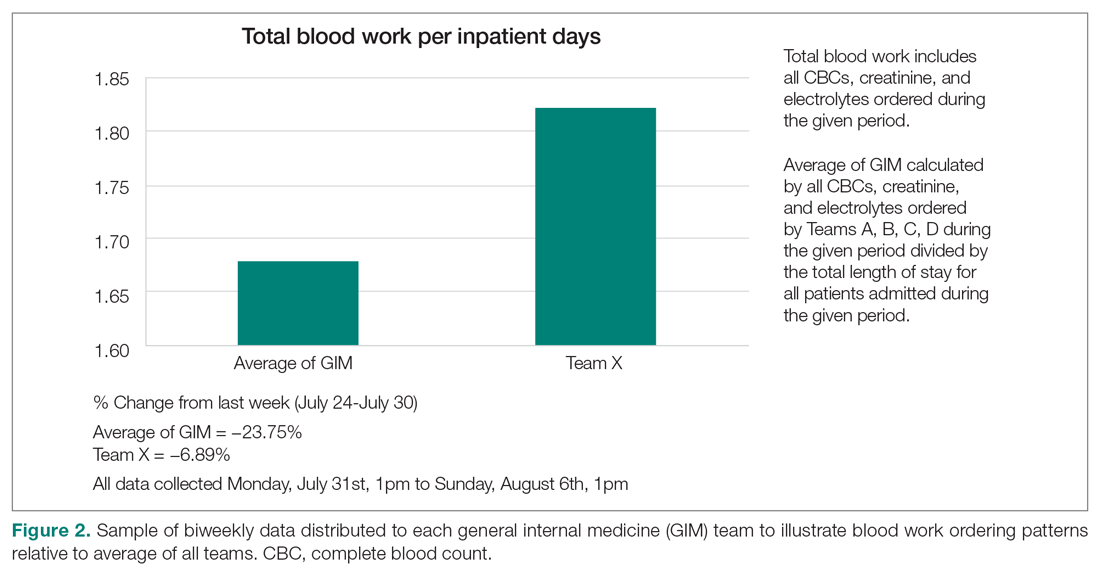
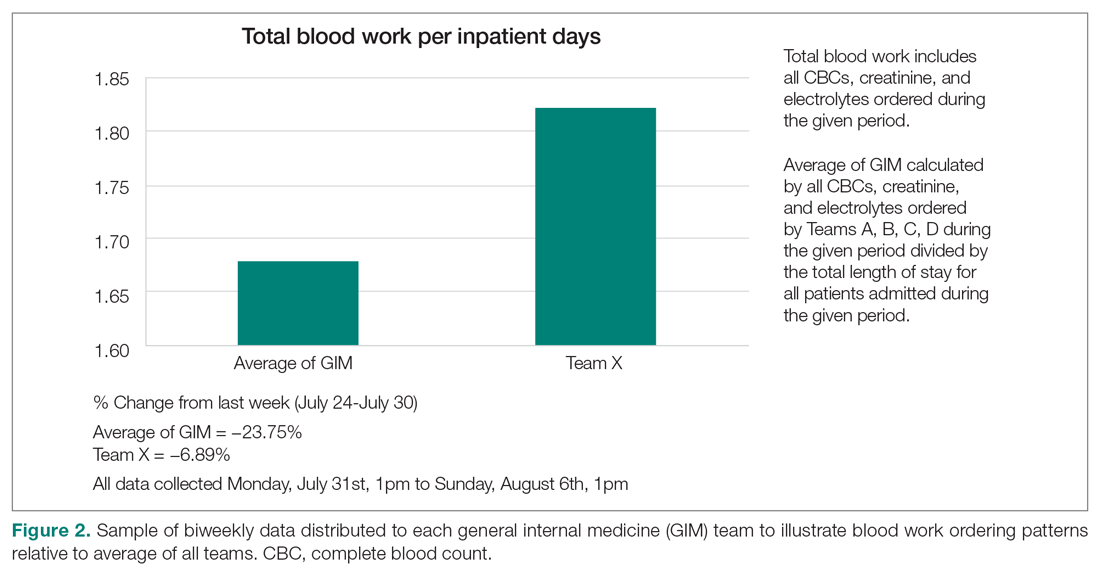
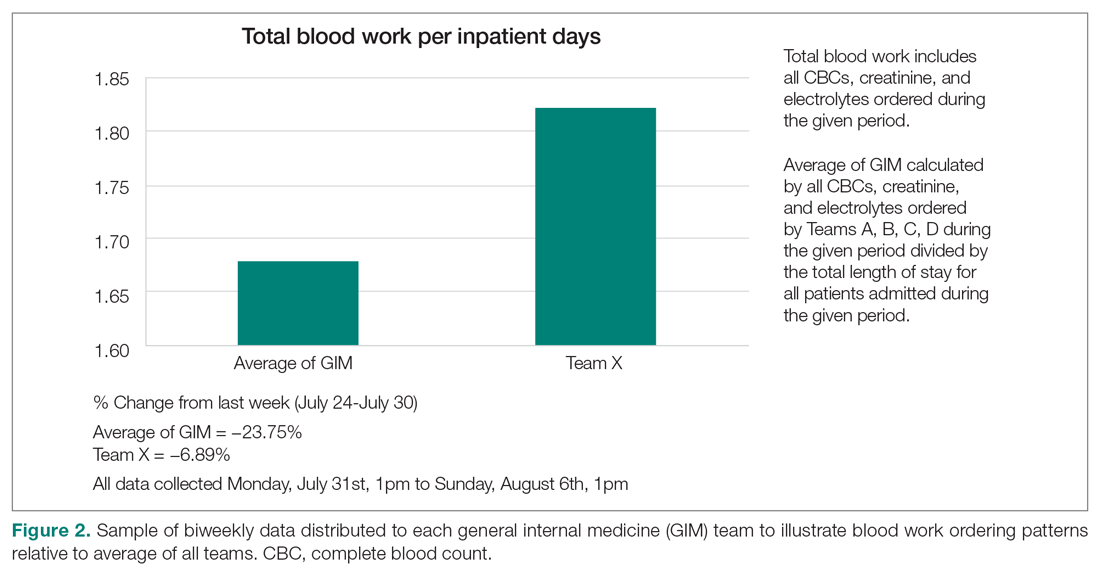
Clinician teams received real-time performance data on their routine blood test ordering patterns compared with an institutional benchmark. Bar graphs of blood work ordering rates (sum of CBCs, creatinine, and electrolytes ordered for all patients on a given team divided by the total LOS for all patients) were distributed to each internal medicine team via email every 2 weeks (Figure 2).1,10-12
Data Collection and Analysis
Data were extracted from the hospital electronic health record (EHR). The primary outcome was the number of routine blood tests (CBC, creatinine, and electrolytes) ordered per inpatient day. Descriptive statistics were calculated for demographic variables. We used statistical process control (SPC) charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome. SPC charts display process changes over time. Data are plotted in chronological order, with the central line representing the outcome mean, an upper line representing the upper control limit, and a lower line representing the lower control limit. The upper and lower limits were set at 3δ, which correspond to 3 standard deviations above and below the mean. Six successive points above or beyond the mean suggests “special cause variation,” indicating that observed results are unlikely due to secular trends. SPC charts are commonly used quality tools for process improvement as well as research.13-16 These charts were created using QI Macros SPC software for Excel V. 2012.07 (KnowWare International, Denver, CO).
The direct cost of each laboratory test was acquired from the hospital laboratory department. The cost of each laboratory test (CBC = $7.54/test, electrolytes = $2.04/test, creatinine = $1.28/test, in Canadian dollars) was subsequently added together and multiplied by the pre- and post-intervention difference of total blood tests saved per inpatient day and then multiplied by 365 to arrive at an estimated cost savings per year.
Results
Over the study period, there were 6424 unique patient admissions on the general internal medicine service, with a median LOS of 3.5 days (Table). 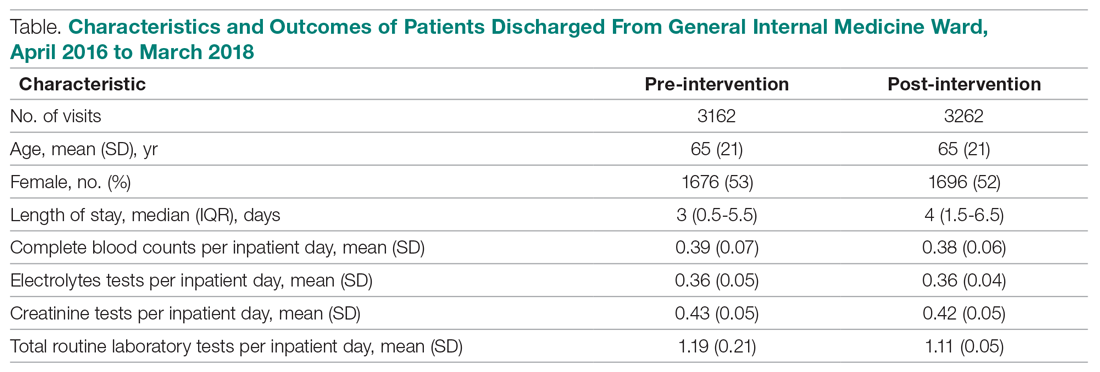
The majority of inpatient visits had at least 1 test of CBC (80%; mean, 3.6 tests/visit), creatinine (79.3%; mean, 3.5 tests/visit), or electrolytes (81.6%; mean, 3.9 tests/visit) completed. In total, 56,767 laboratory tests were ordered.
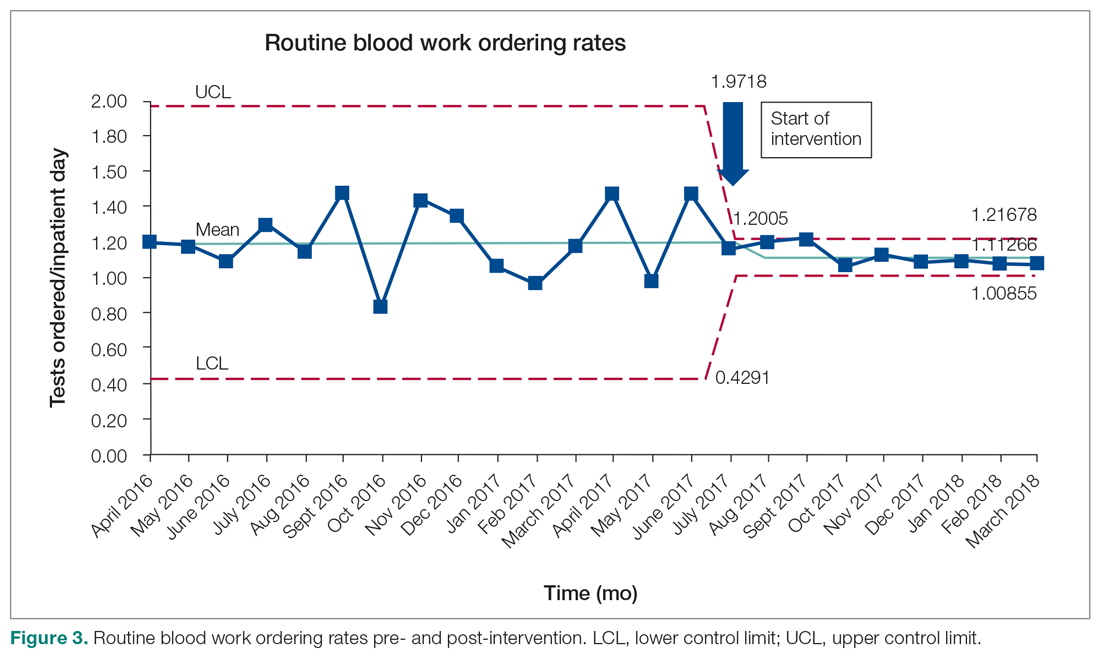
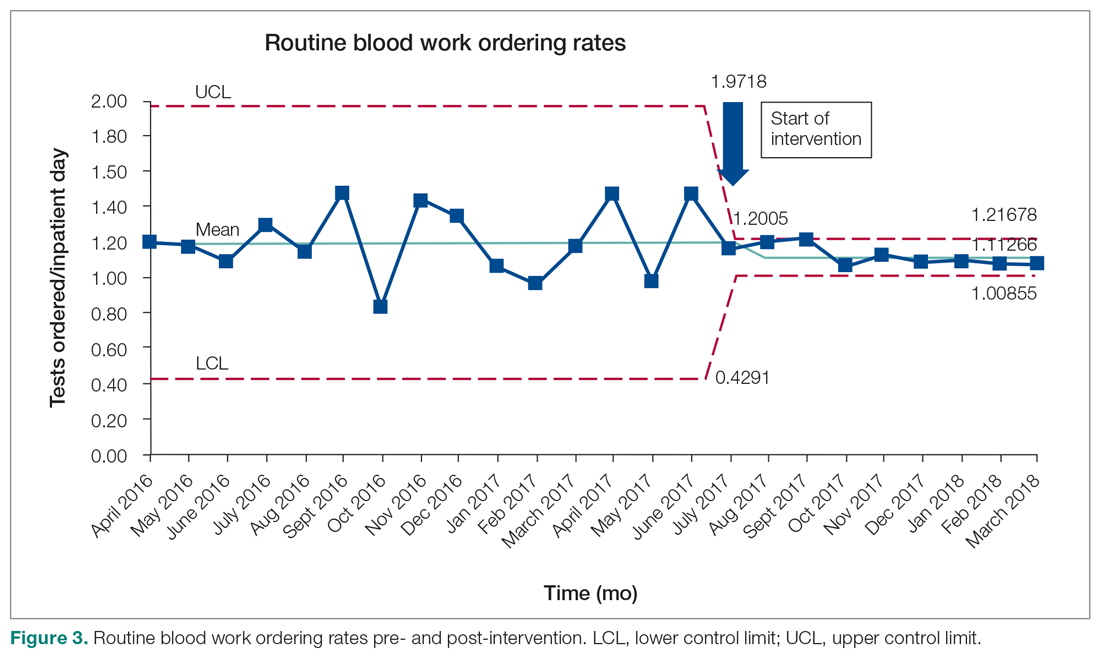
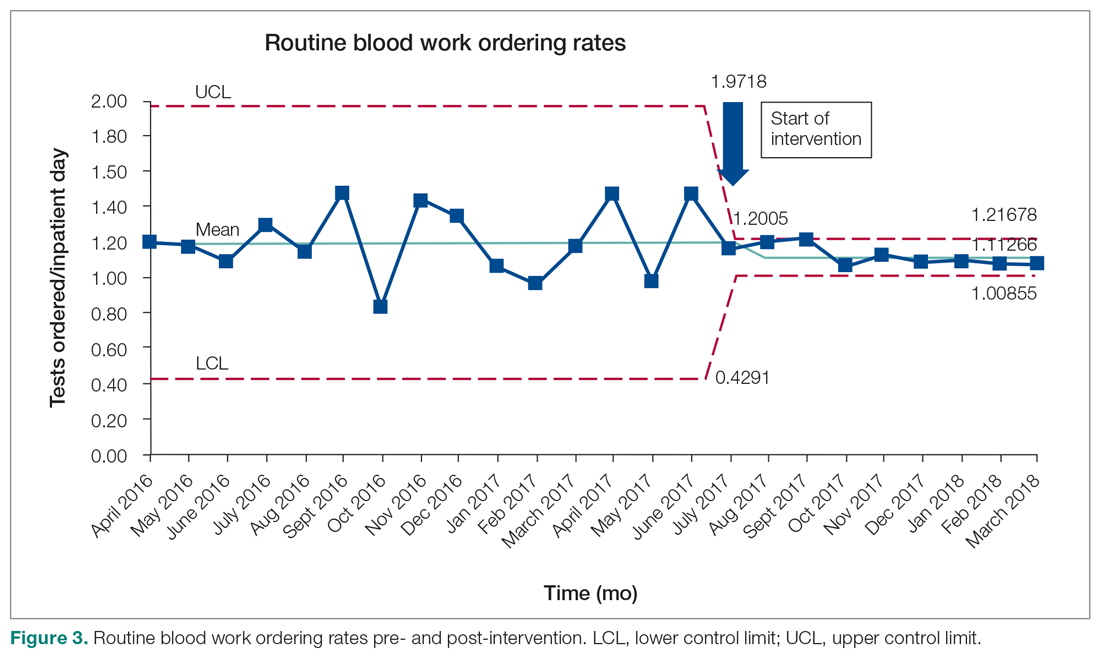
Following the intervention, there was a reduction in both rates of routine blood test orders and their associated costs, with a shift below the mean. The mean number of tests ordered (combined CBC, creatinine, and electrolytes) per inpatient day decreased from 1.19 (SD, 0.21) in the pre-intervention period to 1.11 (SD, 0.05) in the post-intervention period (P < 0.0001), representing a 6.7% relative reduction (Figure 3). We observed a 6.2% relative reduction in costs per inpatient day, translating to a total savings of $26,851 over 1 year for the intervention period.
Discussion
Our study suggests that a multimodal intervention, including CPOE restrictions, resident education with posters, and audit and feedback strategies, can reduce lab test ordering on general internal medicine wards. This finding is similar to those of previous studies using a similar intervention, although different laboratory tests were targeted.1,2,5,6,10,17
Our study found lower test result reductions than those reported by a previous study, which reported a relative reduction of 17% to 30%,18 and by another investigation that was conducted recently in a similar setting.17 In the latter study, reductions in laboratory testing were mostly found in nonroutine tests, and no significant improvements were noted in CBC, electrolytes, and creatine, the 3 tests we studied over the same duration.17 This may represent a ceiling effect to reducing laboratory testing, and efforts to reduce CBC, electrolytes, and creatinine testing beyond 0.3 to 0.4 tests per inpatient day (or combined 1.16 tests per inpatient day) may not be clinically appropriate or possible. This information can guide institutions to include other areas of overuse based on rates of utilization in order to maximize the benefits from a resource intensive intervention.
There are a number of limitations that merit discussion. First, observational studies do not demonstrate causation; however, to our knowledge, there were no other co-interventions that were being conducted during the study duration. One important note is that our project’s intervention began in July, at which point there are new internal medicine residents beginning their training. As the concept of resource allocation becomes more important, medical schools are spending more time educating students about Choosing Wisely, and, therefore, newer cohorts of residents may be more cognizant of appropriate blood testing. Second, this is a single-center study, limiting generalizability; however, we note that many other centers have reported similar findings. Another limitation is that we do not know whether there were any adverse clinical events associated with blood work ordering that was too restrictive, although informal tracking of STAT laboratory testing remained stable throughout the study period. It is important to ensure that blood work is ordered in moderation and tailored to patients using one’s clinical judgment.
Future Directions
We observed modest reductions in the quantity and costs associated with a quality improvement intervention aimed at reducing routine blood testing. A baseline rate of laboratory testing of less than 1 test per inpatient day may require including other target tests to drive down absolute utilization.
Corresponding author: Christine Soong, MD, MSc, 433-600 University Avenue, Toronto, Ontario, Canada M5G 1X5; Christine.soong@utoronto.ca.
Financial disclosures: None.
1. Eaton KP, Levy K, Soong C, et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;178:431.
2. May TA, Clancy M, Critchfield J, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006;126:200-206.
3. Thavendiranathan P, Bagai A, Ebidia A, et al. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20:520-524.
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173:903-908.
5. Attali, M, Barel Y, Somin M, et al. A cost-effective method for reducing the volume of laboratory tests in a university-associated teaching hospital. Mt Sinai J Med. 2006;73:787-794.
6. Faisal A, Andres K, Rind JAK, et al. Reducing the number of unnecessary routine laboratory tests through education of internal medicine residents. Postgrad Med J. 2018;94:716-719.
7. How to Improve. Institute for Healthcare Improvement. 2009. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed June 5, 2019.
8. Langley GL, Moen R, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco: Jossey-Bass Publishers; 2009.
9. Hicks L. Blood Draws Toolkit. Choosing Wisely Canada. 2017. https://choosingwiselycanada.org/wpcontent/uploads/2017/10/CWC_BloodDraws_Toolkit.pdf. Accessed March 5, 2019.
10. Sadowski BW, Lane AB, Wood SM, et al. High-value, cost-conscious care: iterative systems-based interventions to reduce unnecessary laboratory testing. Am J Med. 2017;130:1112e1-1112e7.
11. Minerowicz C, Abel N, Hunter K, et al. Impact of weekly feedback on test ordering patterns. Am J Manag Care. 2015;21:763-768.
12. Calderon-Margalit R, Mor-Yosef S, et al. An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care. 2005;17:243-248.
13. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-64.
14. American Society for Quality. Control chart. ASM website. https://asq.org/quality-resources/control-chart. Accessed November 5, 2020.
15. American Society for Quality. The 7 Basic Quality Tools For Process Improvement. ASM website. https://asq.org/quality-resources/seven-basic-quality-tools. Accessed November 5, 2020.
16. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-464.
17. Ambasta A, Ma IWY, Woo S, et al. Impact of an education and multilevel social comparison-based intervention bundle on use of routine blood tests in hospitalised patients at an academic tertiary care hospital: a controlled pre-intervention post-intervention study. BMJ Qual Saf. 2020;29:1-2.
18. Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061-1072.
From the University of Toronto (Dr. Basuita, Corey L. Kamen, and Dr. Soong) and Sinai Health System (Corey L. Kamen, Cheryl Ethier, and Dr. Soong), Toronto, Ontario, Canada. Co-first authors are Manpreet Basuita, MD, and Corey L. Kamen, BSc.
Abstract
- Objective: Routine laboratory testing is common among medical inpatients; however, when ordered inappropriately testing can represent low-value care. We examined the impact of an evidence-based intervention bundle on utilization.
- Participants/setting: This prospective cohort study took place at a tertiary academic medical center and included 6424 patients admitted to the general internal medicine service between April 2016 and March 2018.
- Intervention: An intervention bundle, whose first components were implemented in July 2016, included computer order entry restrictions on repetitive laboratory testing, education, and audit-feedback.
- Measures: Data were extracted from the hospital electronic health record. The primary outcome was the number of routine blood tests (complete blood count, creatinine, and electrolytes) ordered per inpatient day.
- Analysis: Descriptive statistics were calculated for demographic variables. We used statistical process control charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome.
- Results: The mean number of combined routine laboratory tests ordered per inpatient day decreased from 1.19 (SD, 0.21) tests to 1.11 (SD, 0.05), a relative reduction of 6.7% (P < 0.0001). Mean cost per case related to laboratory tests decreased from $17.24 in the pre-intervention period to $16.17 in the post-intervention period (relative reduction of 6.2%). This resulted in savings of $26,851 in the intervention year.
- Conclusion: A laboratory intervention bundle was associated with small reductions in testing and costs. A routine test performed less than once per inpatient day may not be clinically appropriate or possible.
Keywords: utilization; clinical costs; quality improvement; QI intervention; internal medicine; inpatient.
Routine laboratory blood testing is a commonly used diagnostic tool that physicians rely on to provide patient care. Although routine blood testing represents less than 5% of most hospital budgets, routine use and over-reliance on testing among physicians makes it a target of cost-reduction efforts.1-3 A variety of interventions have been proposed to reduce inappropriate laboratory tests, with varying results.1,4-6 Successful interventions include providing physicians with fee data associated with ordered laboratory tests, unbundling panels of tests, and multicomponent interventions.6 We conducted a multifaceted quality improvement study to promote and develop interventions to adopt appropriate blood test ordering practices.
Methods
Setting
This prospective cohort study took place at Mount Sinai Hospital, a 443-bed academic hospital affiliated with the University of Toronto, where more than 2400 learners rotate through annually. The study was approved by the Mount Sinai Hospital Research Ethics Board.
Participants
We included all inpatient admissions to the general internal medicine service between April 2016 and March 2018. Exclusion criteria included a length of stay (LOS) longer than 365 days and admission to a critical care unit. Patients with more than 1 admission were counted as separate hospital inpatient visits.
Intervention
Based on internal data, we targeted the top 3 most frequently ordered routine blood tests: complete blood count (CBC), creatinine, and electrolytes. Trainee interviews revealed that habit, bundled order sets, and fear of “missing something” contributed to inappropriate routine blood test ordering. Based on these root causes, we used the Model for Improvement to iteratively develop a multimodal intervention that began in July 2016.7,8 This included a change to the computerized provider order entry (CPOE) to nudge clinicians to a restrictive ordering strategy by substituting the “Daily x3” frequency of blood test ordering with a “Daily x1” option on a pick list of order options. Clinicians could still order daily routine blood tests for any specified duration, but would have to do so by manually changing the default setting within the CPOE.
From July 2017 to March 2018, the research team educated residents on appropriate laboratory test ordering and provided audit and feedback data to the clinicians. Diagnostic uncertainty was addressed in teaching sessions. Attending physicians were surveyed on appropriate indications for daily laboratory testing for each of CBC, electrolytes, and creatinine. Appropriate indications (Figure 1) were displayed in visible clinical areas and incorporated into teaching sessions.9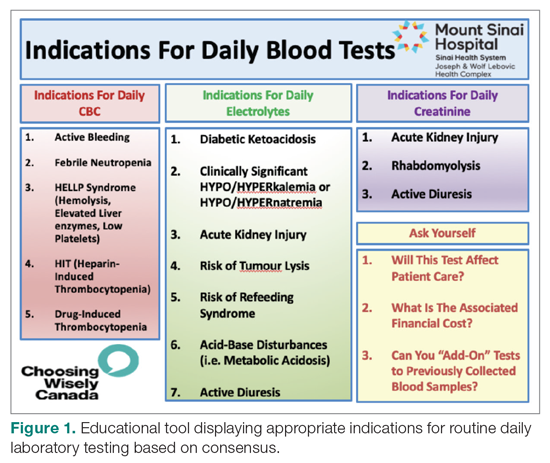
Clinician teams received real-time performance data on their routine blood test ordering patterns compared with an institutional benchmark. Bar graphs of blood work ordering rates (sum of CBCs, creatinine, and electrolytes ordered for all patients on a given team divided by the total LOS for all patients) were distributed to each internal medicine team via email every 2 weeks (Figure 2).1,10-12
Data Collection and Analysis
Data were extracted from the hospital electronic health record (EHR). The primary outcome was the number of routine blood tests (CBC, creatinine, and electrolytes) ordered per inpatient day. Descriptive statistics were calculated for demographic variables. We used statistical process control (SPC) charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome. SPC charts display process changes over time. Data are plotted in chronological order, with the central line representing the outcome mean, an upper line representing the upper control limit, and a lower line representing the lower control limit. The upper and lower limits were set at 3δ, which correspond to 3 standard deviations above and below the mean. Six successive points above or beyond the mean suggests “special cause variation,” indicating that observed results are unlikely due to secular trends. SPC charts are commonly used quality tools for process improvement as well as research.13-16 These charts were created using QI Macros SPC software for Excel V. 2012.07 (KnowWare International, Denver, CO).
The direct cost of each laboratory test was acquired from the hospital laboratory department. The cost of each laboratory test (CBC = $7.54/test, electrolytes = $2.04/test, creatinine = $1.28/test, in Canadian dollars) was subsequently added together and multiplied by the pre- and post-intervention difference of total blood tests saved per inpatient day and then multiplied by 365 to arrive at an estimated cost savings per year.
Results
Over the study period, there were 6424 unique patient admissions on the general internal medicine service, with a median LOS of 3.5 days (Table). 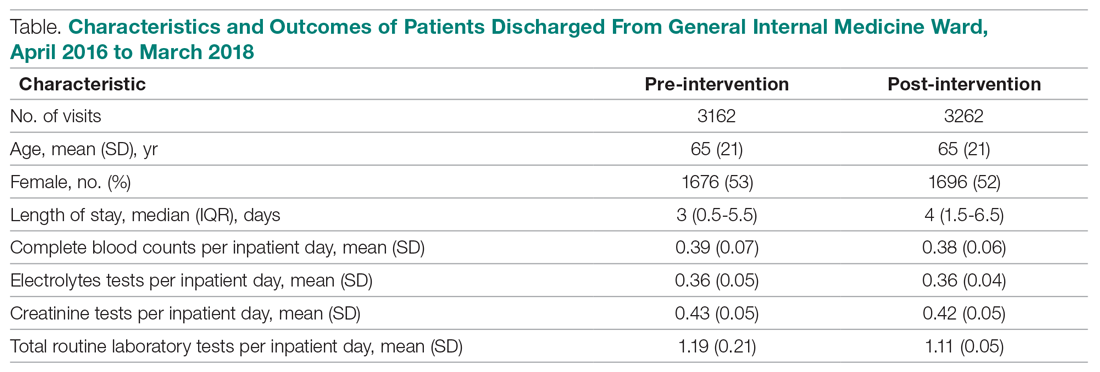
The majority of inpatient visits had at least 1 test of CBC (80%; mean, 3.6 tests/visit), creatinine (79.3%; mean, 3.5 tests/visit), or electrolytes (81.6%; mean, 3.9 tests/visit) completed. In total, 56,767 laboratory tests were ordered.
Following the intervention, there was a reduction in both rates of routine blood test orders and their associated costs, with a shift below the mean. The mean number of tests ordered (combined CBC, creatinine, and electrolytes) per inpatient day decreased from 1.19 (SD, 0.21) in the pre-intervention period to 1.11 (SD, 0.05) in the post-intervention period (P < 0.0001), representing a 6.7% relative reduction (Figure 3). We observed a 6.2% relative reduction in costs per inpatient day, translating to a total savings of $26,851 over 1 year for the intervention period.
Discussion
Our study suggests that a multimodal intervention, including CPOE restrictions, resident education with posters, and audit and feedback strategies, can reduce lab test ordering on general internal medicine wards. This finding is similar to those of previous studies using a similar intervention, although different laboratory tests were targeted.1,2,5,6,10,17
Our study found lower test result reductions than those reported by a previous study, which reported a relative reduction of 17% to 30%,18 and by another investigation that was conducted recently in a similar setting.17 In the latter study, reductions in laboratory testing were mostly found in nonroutine tests, and no significant improvements were noted in CBC, electrolytes, and creatine, the 3 tests we studied over the same duration.17 This may represent a ceiling effect to reducing laboratory testing, and efforts to reduce CBC, electrolytes, and creatinine testing beyond 0.3 to 0.4 tests per inpatient day (or combined 1.16 tests per inpatient day) may not be clinically appropriate or possible. This information can guide institutions to include other areas of overuse based on rates of utilization in order to maximize the benefits from a resource intensive intervention.
There are a number of limitations that merit discussion. First, observational studies do not demonstrate causation; however, to our knowledge, there were no other co-interventions that were being conducted during the study duration. One important note is that our project’s intervention began in July, at which point there are new internal medicine residents beginning their training. As the concept of resource allocation becomes more important, medical schools are spending more time educating students about Choosing Wisely, and, therefore, newer cohorts of residents may be more cognizant of appropriate blood testing. Second, this is a single-center study, limiting generalizability; however, we note that many other centers have reported similar findings. Another limitation is that we do not know whether there were any adverse clinical events associated with blood work ordering that was too restrictive, although informal tracking of STAT laboratory testing remained stable throughout the study period. It is important to ensure that blood work is ordered in moderation and tailored to patients using one’s clinical judgment.
Future Directions
We observed modest reductions in the quantity and costs associated with a quality improvement intervention aimed at reducing routine blood testing. A baseline rate of laboratory testing of less than 1 test per inpatient day may require including other target tests to drive down absolute utilization.
Corresponding author: Christine Soong, MD, MSc, 433-600 University Avenue, Toronto, Ontario, Canada M5G 1X5; Christine.soong@utoronto.ca.
Financial disclosures: None.
From the University of Toronto (Dr. Basuita, Corey L. Kamen, and Dr. Soong) and Sinai Health System (Corey L. Kamen, Cheryl Ethier, and Dr. Soong), Toronto, Ontario, Canada. Co-first authors are Manpreet Basuita, MD, and Corey L. Kamen, BSc.
Abstract
- Objective: Routine laboratory testing is common among medical inpatients; however, when ordered inappropriately testing can represent low-value care. We examined the impact of an evidence-based intervention bundle on utilization.
- Participants/setting: This prospective cohort study took place at a tertiary academic medical center and included 6424 patients admitted to the general internal medicine service between April 2016 and March 2018.
- Intervention: An intervention bundle, whose first components were implemented in July 2016, included computer order entry restrictions on repetitive laboratory testing, education, and audit-feedback.
- Measures: Data were extracted from the hospital electronic health record. The primary outcome was the number of routine blood tests (complete blood count, creatinine, and electrolytes) ordered per inpatient day.
- Analysis: Descriptive statistics were calculated for demographic variables. We used statistical process control charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome.
- Results: The mean number of combined routine laboratory tests ordered per inpatient day decreased from 1.19 (SD, 0.21) tests to 1.11 (SD, 0.05), a relative reduction of 6.7% (P < 0.0001). Mean cost per case related to laboratory tests decreased from $17.24 in the pre-intervention period to $16.17 in the post-intervention period (relative reduction of 6.2%). This resulted in savings of $26,851 in the intervention year.
- Conclusion: A laboratory intervention bundle was associated with small reductions in testing and costs. A routine test performed less than once per inpatient day may not be clinically appropriate or possible.
Keywords: utilization; clinical costs; quality improvement; QI intervention; internal medicine; inpatient.
Routine laboratory blood testing is a commonly used diagnostic tool that physicians rely on to provide patient care. Although routine blood testing represents less than 5% of most hospital budgets, routine use and over-reliance on testing among physicians makes it a target of cost-reduction efforts.1-3 A variety of interventions have been proposed to reduce inappropriate laboratory tests, with varying results.1,4-6 Successful interventions include providing physicians with fee data associated with ordered laboratory tests, unbundling panels of tests, and multicomponent interventions.6 We conducted a multifaceted quality improvement study to promote and develop interventions to adopt appropriate blood test ordering practices.
Methods
Setting
This prospective cohort study took place at Mount Sinai Hospital, a 443-bed academic hospital affiliated with the University of Toronto, where more than 2400 learners rotate through annually. The study was approved by the Mount Sinai Hospital Research Ethics Board.
Participants
We included all inpatient admissions to the general internal medicine service between April 2016 and March 2018. Exclusion criteria included a length of stay (LOS) longer than 365 days and admission to a critical care unit. Patients with more than 1 admission were counted as separate hospital inpatient visits.
Intervention
Based on internal data, we targeted the top 3 most frequently ordered routine blood tests: complete blood count (CBC), creatinine, and electrolytes. Trainee interviews revealed that habit, bundled order sets, and fear of “missing something” contributed to inappropriate routine blood test ordering. Based on these root causes, we used the Model for Improvement to iteratively develop a multimodal intervention that began in July 2016.7,8 This included a change to the computerized provider order entry (CPOE) to nudge clinicians to a restrictive ordering strategy by substituting the “Daily x3” frequency of blood test ordering with a “Daily x1” option on a pick list of order options. Clinicians could still order daily routine blood tests for any specified duration, but would have to do so by manually changing the default setting within the CPOE.
From July 2017 to March 2018, the research team educated residents on appropriate laboratory test ordering and provided audit and feedback data to the clinicians. Diagnostic uncertainty was addressed in teaching sessions. Attending physicians were surveyed on appropriate indications for daily laboratory testing for each of CBC, electrolytes, and creatinine. Appropriate indications (Figure 1) were displayed in visible clinical areas and incorporated into teaching sessions.9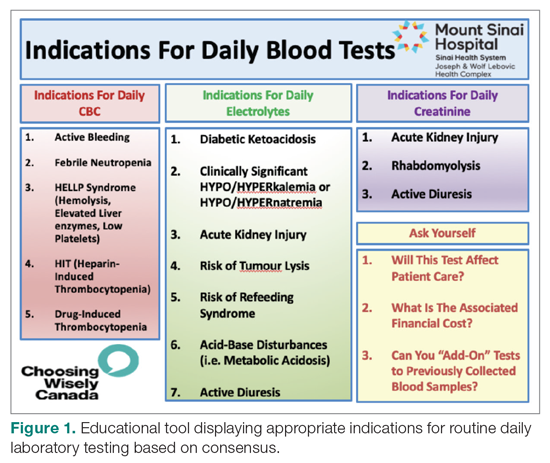
Clinician teams received real-time performance data on their routine blood test ordering patterns compared with an institutional benchmark. Bar graphs of blood work ordering rates (sum of CBCs, creatinine, and electrolytes ordered for all patients on a given team divided by the total LOS for all patients) were distributed to each internal medicine team via email every 2 weeks (Figure 2).1,10-12
Data Collection and Analysis
Data were extracted from the hospital electronic health record (EHR). The primary outcome was the number of routine blood tests (CBC, creatinine, and electrolytes) ordered per inpatient day. Descriptive statistics were calculated for demographic variables. We used statistical process control (SPC) charts to compare the baseline period (April 2016-June 2017) and the intervention period (July 2017-March 2018) for the primary outcome. SPC charts display process changes over time. Data are plotted in chronological order, with the central line representing the outcome mean, an upper line representing the upper control limit, and a lower line representing the lower control limit. The upper and lower limits were set at 3δ, which correspond to 3 standard deviations above and below the mean. Six successive points above or beyond the mean suggests “special cause variation,” indicating that observed results are unlikely due to secular trends. SPC charts are commonly used quality tools for process improvement as well as research.13-16 These charts were created using QI Macros SPC software for Excel V. 2012.07 (KnowWare International, Denver, CO).
The direct cost of each laboratory test was acquired from the hospital laboratory department. The cost of each laboratory test (CBC = $7.54/test, electrolytes = $2.04/test, creatinine = $1.28/test, in Canadian dollars) was subsequently added together and multiplied by the pre- and post-intervention difference of total blood tests saved per inpatient day and then multiplied by 365 to arrive at an estimated cost savings per year.
Results
Over the study period, there were 6424 unique patient admissions on the general internal medicine service, with a median LOS of 3.5 days (Table). 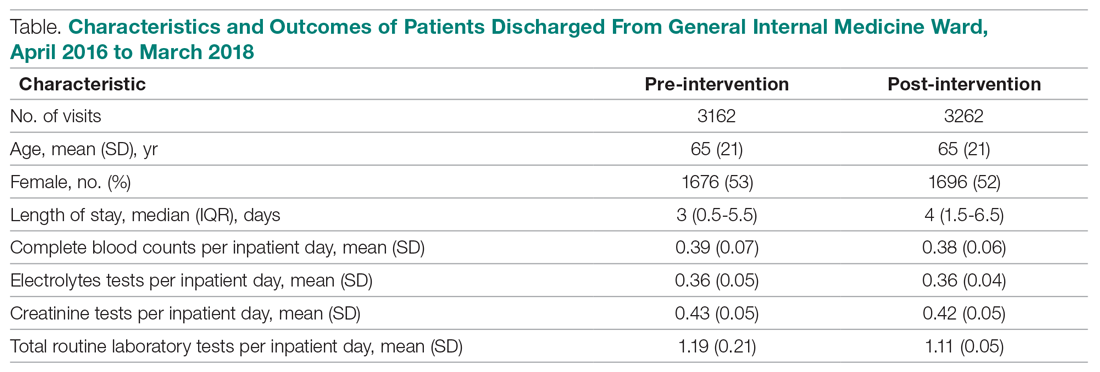
The majority of inpatient visits had at least 1 test of CBC (80%; mean, 3.6 tests/visit), creatinine (79.3%; mean, 3.5 tests/visit), or electrolytes (81.6%; mean, 3.9 tests/visit) completed. In total, 56,767 laboratory tests were ordered.
Following the intervention, there was a reduction in both rates of routine blood test orders and their associated costs, with a shift below the mean. The mean number of tests ordered (combined CBC, creatinine, and electrolytes) per inpatient day decreased from 1.19 (SD, 0.21) in the pre-intervention period to 1.11 (SD, 0.05) in the post-intervention period (P < 0.0001), representing a 6.7% relative reduction (Figure 3). We observed a 6.2% relative reduction in costs per inpatient day, translating to a total savings of $26,851 over 1 year for the intervention period.
Discussion
Our study suggests that a multimodal intervention, including CPOE restrictions, resident education with posters, and audit and feedback strategies, can reduce lab test ordering on general internal medicine wards. This finding is similar to those of previous studies using a similar intervention, although different laboratory tests were targeted.1,2,5,6,10,17
Our study found lower test result reductions than those reported by a previous study, which reported a relative reduction of 17% to 30%,18 and by another investigation that was conducted recently in a similar setting.17 In the latter study, reductions in laboratory testing were mostly found in nonroutine tests, and no significant improvements were noted in CBC, electrolytes, and creatine, the 3 tests we studied over the same duration.17 This may represent a ceiling effect to reducing laboratory testing, and efforts to reduce CBC, electrolytes, and creatinine testing beyond 0.3 to 0.4 tests per inpatient day (or combined 1.16 tests per inpatient day) may not be clinically appropriate or possible. This information can guide institutions to include other areas of overuse based on rates of utilization in order to maximize the benefits from a resource intensive intervention.
There are a number of limitations that merit discussion. First, observational studies do not demonstrate causation; however, to our knowledge, there were no other co-interventions that were being conducted during the study duration. One important note is that our project’s intervention began in July, at which point there are new internal medicine residents beginning their training. As the concept of resource allocation becomes more important, medical schools are spending more time educating students about Choosing Wisely, and, therefore, newer cohorts of residents may be more cognizant of appropriate blood testing. Second, this is a single-center study, limiting generalizability; however, we note that many other centers have reported similar findings. Another limitation is that we do not know whether there were any adverse clinical events associated with blood work ordering that was too restrictive, although informal tracking of STAT laboratory testing remained stable throughout the study period. It is important to ensure that blood work is ordered in moderation and tailored to patients using one’s clinical judgment.
Future Directions
We observed modest reductions in the quantity and costs associated with a quality improvement intervention aimed at reducing routine blood testing. A baseline rate of laboratory testing of less than 1 test per inpatient day may require including other target tests to drive down absolute utilization.
Corresponding author: Christine Soong, MD, MSc, 433-600 University Avenue, Toronto, Ontario, Canada M5G 1X5; Christine.soong@utoronto.ca.
Financial disclosures: None.
1. Eaton KP, Levy K, Soong C, et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;178:431.
2. May TA, Clancy M, Critchfield J, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006;126:200-206.
3. Thavendiranathan P, Bagai A, Ebidia A, et al. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20:520-524.
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173:903-908.
5. Attali, M, Barel Y, Somin M, et al. A cost-effective method for reducing the volume of laboratory tests in a university-associated teaching hospital. Mt Sinai J Med. 2006;73:787-794.
6. Faisal A, Andres K, Rind JAK, et al. Reducing the number of unnecessary routine laboratory tests through education of internal medicine residents. Postgrad Med J. 2018;94:716-719.
7. How to Improve. Institute for Healthcare Improvement. 2009. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed June 5, 2019.
8. Langley GL, Moen R, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco: Jossey-Bass Publishers; 2009.
9. Hicks L. Blood Draws Toolkit. Choosing Wisely Canada. 2017. https://choosingwiselycanada.org/wpcontent/uploads/2017/10/CWC_BloodDraws_Toolkit.pdf. Accessed March 5, 2019.
10. Sadowski BW, Lane AB, Wood SM, et al. High-value, cost-conscious care: iterative systems-based interventions to reduce unnecessary laboratory testing. Am J Med. 2017;130:1112e1-1112e7.
11. Minerowicz C, Abel N, Hunter K, et al. Impact of weekly feedback on test ordering patterns. Am J Manag Care. 2015;21:763-768.
12. Calderon-Margalit R, Mor-Yosef S, et al. An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care. 2005;17:243-248.
13. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-64.
14. American Society for Quality. Control chart. ASM website. https://asq.org/quality-resources/control-chart. Accessed November 5, 2020.
15. American Society for Quality. The 7 Basic Quality Tools For Process Improvement. ASM website. https://asq.org/quality-resources/seven-basic-quality-tools. Accessed November 5, 2020.
16. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-464.
17. Ambasta A, Ma IWY, Woo S, et al. Impact of an education and multilevel social comparison-based intervention bundle on use of routine blood tests in hospitalised patients at an academic tertiary care hospital: a controlled pre-intervention post-intervention study. BMJ Qual Saf. 2020;29:1-2.
18. Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061-1072.
1. Eaton KP, Levy K, Soong C, et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;178:431.
2. May TA, Clancy M, Critchfield J, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006;126:200-206.
3. Thavendiranathan P, Bagai A, Ebidia A, et al. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20:520-524.
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173:903-908.
5. Attali, M, Barel Y, Somin M, et al. A cost-effective method for reducing the volume of laboratory tests in a university-associated teaching hospital. Mt Sinai J Med. 2006;73:787-794.
6. Faisal A, Andres K, Rind JAK, et al. Reducing the number of unnecessary routine laboratory tests through education of internal medicine residents. Postgrad Med J. 2018;94:716-719.
7. How to Improve. Institute for Healthcare Improvement. 2009. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed June 5, 2019.
8. Langley GL, Moen R, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco: Jossey-Bass Publishers; 2009.
9. Hicks L. Blood Draws Toolkit. Choosing Wisely Canada. 2017. https://choosingwiselycanada.org/wpcontent/uploads/2017/10/CWC_BloodDraws_Toolkit.pdf. Accessed March 5, 2019.
10. Sadowski BW, Lane AB, Wood SM, et al. High-value, cost-conscious care: iterative systems-based interventions to reduce unnecessary laboratory testing. Am J Med. 2017;130:1112e1-1112e7.
11. Minerowicz C, Abel N, Hunter K, et al. Impact of weekly feedback on test ordering patterns. Am J Manag Care. 2015;21:763-768.
12. Calderon-Margalit R, Mor-Yosef S, et al. An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care. 2005;17:243-248.
13. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-64.
14. American Society for Quality. Control chart. ASM website. https://asq.org/quality-resources/control-chart. Accessed November 5, 2020.
15. American Society for Quality. The 7 Basic Quality Tools For Process Improvement. ASM website. https://asq.org/quality-resources/seven-basic-quality-tools. Accessed November 5, 2020.
16. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-464.
17. Ambasta A, Ma IWY, Woo S, et al. Impact of an education and multilevel social comparison-based intervention bundle on use of routine blood tests in hospitalised patients at an academic tertiary care hospital: a controlled pre-intervention post-intervention study. BMJ Qual Saf. 2020;29:1-2.
18. Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061-1072.
Cardiac Biomarkers—Are We Testing Wisely?
Cardiac biomarker testing, along with a thorough patient history, physical exam, and an electrocardiogram, is required for the diagnosis of patients with suspected acute coronary syndrome (ACS). For nearly 3 decades, 2 cardiac biomarkers, troponin (I or T) and creatine kinase-MB fraction (CK-MB), have been ordered together to evaluate ACS patients out of concern that utilizing a single biomarker might be less diagnostically accurate than using 2 biomarkers. However, subsequent studies have shown that troponin is far more sensitive and specific for myocardial injury than CK-MB.1,2 Troponin testing offers important prognostic information irrespective of whether the CK-MB is normal or abnormal.3,4 In 2015, the American Society of Clinical Pathology released a Choosing Wisely® recommendation against ordering CK-MB (or myoglobin) for the diagnosis of acute myocardial infarction (AMI).5 This reflects an emerging consensus that CK-MB testing represents low-value care while troponin testing alone is the appropriate diagnostic strategy for ACS patients.
Remarkably, we know very little about patterns of cardiac biomarker utilization in clinical practice. In this issue of the Journal of Hospital Medicine, Prochaska et al.6 provide a valuable snapshot of troponin and CK-MB utilization at 91 U.S. academic medical centers (AMCs) for 18 months prior to and following the release of the 2015 Choosing Wisely® recommendation. From a retrospective review of 106,954 inpatient discharges with a principal diagnosis of AMI, they report a 29.2% rate of troponin-only testing in 2013 with a gradual increase over 3 years to 53.5% in 2016. Interestingly, the study’s baseline troponin-only utilization rate is consistent with a 2013 College of American Pathologists survey, which estimated that 23% of U.S. clinical laboratories no longer process CK-MB (and therefore run troponins alone).7
Did the 2015 Choosing Wisely® recommendation have an impact on providers choosing cardiac biomarkers wisely? The authors answer this question in a novel way by stratifying hospitals into performance tertiles for each study quarter and then further classifying them into groups that were consistently high, middle, and low performers throughout the study period. Using an interrupted time series design, they identify 26 hospitals who improved their troponin-only testing performance tertile during the study period and examine their average quarterly rate of change. As illustrated in Figure 3, they report a sharp increase in the rate of change of troponin-only testing shortly after the release of the 2015 Choosing Wisely® recommendation. The authors reasonably conclude that the Choosing Wisely® campaign “appeared to facilitate accelerated adoption of troponin-only testing” among these hospitals.
However, we should interpret these results with caution. The authors highlight several limitations, including the absence of causality common in observational studies and insufficient time to follow-up to capture the full (or transient) impact of the intervention. There are factors external to the Choosing Wisely® campaign that may have influenced cardiac biomarker testing patterns observed. Examples include variation in hospital leadership, financial drivers, and local culture that promote high-value care. We also note that (1) there are several published interventions to improve troponin-only ordering that predate the Choosing Wisely® campaign8,9; (2) a prominent cardiology guideline endorsed the use of troponin as a preferred cardiac biomarker in 201210; and (3) a widely cited opinion by prominent researchers called for the elimination of CK-MB from clinical practice in 2008.11 These publications suggest there was already an awareness of and efforts underway to improve cardiac enzyme testing contributing to the results described by Prochaska et al.
Limitations notwithstanding, we commend Prochaska et al. for conducting the first-known description of patient-level trend rates of troponin and CK-MB testing. Finally, it is worth noting that where there is accomplishment, there is also opportunity. At the end of the study period, nearly 50% of institutions had yet to adopt a troponin-only strategy. While there has been an overall trend towards improvement, this number remains high. We may conjecture as to possible explanations: Providers may be unconvinced that a single troponin is sufficient in the diagnosis of ACS (ie, lack of knowledge or debate over the interpretation of available science), stakeholders may be slow to de-adopt practices using appropriate systems levers (eg, laboratories delisting CK-MB processing), and incentives may be lacking to motivate AMCs. The results of this study should be used as a burning platform to those who wish to “test wisely” in cardiac biomarker use.
Disclosure
The authors report no conflicts of interest or financial disclosures.
1. Katus HA, Remppis A, Neumann FJ, et al. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991;83:902-912. PubMed
2. Adams JE III, Bodor GS, Dávila-Román VG, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993;88:101-106. PubMed
3. Newby LK, Roe MT, Chen AY, et al. Frequency and clinical implications of discordant creatine kinase-MB and troponin measurements in acute coronary syndromes. J Am Coll Cardiol. 2006;47:312-318. PubMed
4. Goodman SG, Steg PG, Eagle KA, et al. The diagnostic and prognostic impact of the redefinition of acute myocardial infarction: lessons from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2006;151:654-660. PubMed
5. American Society of Clinical Pathology - Choosing Wisely recommendations; http://www.choosingwisely.org/clinicianlists/#parentSociety=American_Society_for_Clinical_Pathology. Released February 2015. Accessed June 12, 2017.
6. Prochaska MT, Hohmann SF, Modes M, Arora VM. Trends in Troponin-Only Testing for AMI in Academic Teaching Hospitals and the Impact of Choosing Wisely®. J Hosp
7. Singh G, Baweja PS. CK-MB: Journey to Obsolescence. Am J Clin Pathol. 2014;141(3):415-419. PubMed
8. Larochelle MR, Knight AM, Pantle H, Riedel S, Trost JC. Reducing excess biomarker use at an academic medical center. J Gen Intern Med. 2014;29(11):1468-1474. PubMed
9. Baron JM, Lewandrowski KB, Kamis IK, Singh B, Belkziz SM, Dighe AS. A novel strategy for evaluating the effects of an electronic test ordering alert message: optimizing cardiac marker use. J Pathol Inform. 2012;3:3. PubMed
10. Thygesen K, Alpert JS, Jaffe AS, et al. Third Universal Definition of Myocardial Infarction. Circulation. 2012;126:2020-2035. PubMed
11. Saenger AK, Jaffe AS. Requiem for a Heavyweight: The Demise of CK-MB. Circulation. 2008;118(21):2200-2206. PubMed
Cardiac biomarker testing, along with a thorough patient history, physical exam, and an electrocardiogram, is required for the diagnosis of patients with suspected acute coronary syndrome (ACS). For nearly 3 decades, 2 cardiac biomarkers, troponin (I or T) and creatine kinase-MB fraction (CK-MB), have been ordered together to evaluate ACS patients out of concern that utilizing a single biomarker might be less diagnostically accurate than using 2 biomarkers. However, subsequent studies have shown that troponin is far more sensitive and specific for myocardial injury than CK-MB.1,2 Troponin testing offers important prognostic information irrespective of whether the CK-MB is normal or abnormal.3,4 In 2015, the American Society of Clinical Pathology released a Choosing Wisely® recommendation against ordering CK-MB (or myoglobin) for the diagnosis of acute myocardial infarction (AMI).5 This reflects an emerging consensus that CK-MB testing represents low-value care while troponin testing alone is the appropriate diagnostic strategy for ACS patients.
Remarkably, we know very little about patterns of cardiac biomarker utilization in clinical practice. In this issue of the Journal of Hospital Medicine, Prochaska et al.6 provide a valuable snapshot of troponin and CK-MB utilization at 91 U.S. academic medical centers (AMCs) for 18 months prior to and following the release of the 2015 Choosing Wisely® recommendation. From a retrospective review of 106,954 inpatient discharges with a principal diagnosis of AMI, they report a 29.2% rate of troponin-only testing in 2013 with a gradual increase over 3 years to 53.5% in 2016. Interestingly, the study’s baseline troponin-only utilization rate is consistent with a 2013 College of American Pathologists survey, which estimated that 23% of U.S. clinical laboratories no longer process CK-MB (and therefore run troponins alone).7
Did the 2015 Choosing Wisely® recommendation have an impact on providers choosing cardiac biomarkers wisely? The authors answer this question in a novel way by stratifying hospitals into performance tertiles for each study quarter and then further classifying them into groups that were consistently high, middle, and low performers throughout the study period. Using an interrupted time series design, they identify 26 hospitals who improved their troponin-only testing performance tertile during the study period and examine their average quarterly rate of change. As illustrated in Figure 3, they report a sharp increase in the rate of change of troponin-only testing shortly after the release of the 2015 Choosing Wisely® recommendation. The authors reasonably conclude that the Choosing Wisely® campaign “appeared to facilitate accelerated adoption of troponin-only testing” among these hospitals.
However, we should interpret these results with caution. The authors highlight several limitations, including the absence of causality common in observational studies and insufficient time to follow-up to capture the full (or transient) impact of the intervention. There are factors external to the Choosing Wisely® campaign that may have influenced cardiac biomarker testing patterns observed. Examples include variation in hospital leadership, financial drivers, and local culture that promote high-value care. We also note that (1) there are several published interventions to improve troponin-only ordering that predate the Choosing Wisely® campaign8,9; (2) a prominent cardiology guideline endorsed the use of troponin as a preferred cardiac biomarker in 201210; and (3) a widely cited opinion by prominent researchers called for the elimination of CK-MB from clinical practice in 2008.11 These publications suggest there was already an awareness of and efforts underway to improve cardiac enzyme testing contributing to the results described by Prochaska et al.
Limitations notwithstanding, we commend Prochaska et al. for conducting the first-known description of patient-level trend rates of troponin and CK-MB testing. Finally, it is worth noting that where there is accomplishment, there is also opportunity. At the end of the study period, nearly 50% of institutions had yet to adopt a troponin-only strategy. While there has been an overall trend towards improvement, this number remains high. We may conjecture as to possible explanations: Providers may be unconvinced that a single troponin is sufficient in the diagnosis of ACS (ie, lack of knowledge or debate over the interpretation of available science), stakeholders may be slow to de-adopt practices using appropriate systems levers (eg, laboratories delisting CK-MB processing), and incentives may be lacking to motivate AMCs. The results of this study should be used as a burning platform to those who wish to “test wisely” in cardiac biomarker use.
Disclosure
The authors report no conflicts of interest or financial disclosures.
Cardiac biomarker testing, along with a thorough patient history, physical exam, and an electrocardiogram, is required for the diagnosis of patients with suspected acute coronary syndrome (ACS). For nearly 3 decades, 2 cardiac biomarkers, troponin (I or T) and creatine kinase-MB fraction (CK-MB), have been ordered together to evaluate ACS patients out of concern that utilizing a single biomarker might be less diagnostically accurate than using 2 biomarkers. However, subsequent studies have shown that troponin is far more sensitive and specific for myocardial injury than CK-MB.1,2 Troponin testing offers important prognostic information irrespective of whether the CK-MB is normal or abnormal.3,4 In 2015, the American Society of Clinical Pathology released a Choosing Wisely® recommendation against ordering CK-MB (or myoglobin) for the diagnosis of acute myocardial infarction (AMI).5 This reflects an emerging consensus that CK-MB testing represents low-value care while troponin testing alone is the appropriate diagnostic strategy for ACS patients.
Remarkably, we know very little about patterns of cardiac biomarker utilization in clinical practice. In this issue of the Journal of Hospital Medicine, Prochaska et al.6 provide a valuable snapshot of troponin and CK-MB utilization at 91 U.S. academic medical centers (AMCs) for 18 months prior to and following the release of the 2015 Choosing Wisely® recommendation. From a retrospective review of 106,954 inpatient discharges with a principal diagnosis of AMI, they report a 29.2% rate of troponin-only testing in 2013 with a gradual increase over 3 years to 53.5% in 2016. Interestingly, the study’s baseline troponin-only utilization rate is consistent with a 2013 College of American Pathologists survey, which estimated that 23% of U.S. clinical laboratories no longer process CK-MB (and therefore run troponins alone).7
Did the 2015 Choosing Wisely® recommendation have an impact on providers choosing cardiac biomarkers wisely? The authors answer this question in a novel way by stratifying hospitals into performance tertiles for each study quarter and then further classifying them into groups that were consistently high, middle, and low performers throughout the study period. Using an interrupted time series design, they identify 26 hospitals who improved their troponin-only testing performance tertile during the study period and examine their average quarterly rate of change. As illustrated in Figure 3, they report a sharp increase in the rate of change of troponin-only testing shortly after the release of the 2015 Choosing Wisely® recommendation. The authors reasonably conclude that the Choosing Wisely® campaign “appeared to facilitate accelerated adoption of troponin-only testing” among these hospitals.
However, we should interpret these results with caution. The authors highlight several limitations, including the absence of causality common in observational studies and insufficient time to follow-up to capture the full (or transient) impact of the intervention. There are factors external to the Choosing Wisely® campaign that may have influenced cardiac biomarker testing patterns observed. Examples include variation in hospital leadership, financial drivers, and local culture that promote high-value care. We also note that (1) there are several published interventions to improve troponin-only ordering that predate the Choosing Wisely® campaign8,9; (2) a prominent cardiology guideline endorsed the use of troponin as a preferred cardiac biomarker in 201210; and (3) a widely cited opinion by prominent researchers called for the elimination of CK-MB from clinical practice in 2008.11 These publications suggest there was already an awareness of and efforts underway to improve cardiac enzyme testing contributing to the results described by Prochaska et al.
Limitations notwithstanding, we commend Prochaska et al. for conducting the first-known description of patient-level trend rates of troponin and CK-MB testing. Finally, it is worth noting that where there is accomplishment, there is also opportunity. At the end of the study period, nearly 50% of institutions had yet to adopt a troponin-only strategy. While there has been an overall trend towards improvement, this number remains high. We may conjecture as to possible explanations: Providers may be unconvinced that a single troponin is sufficient in the diagnosis of ACS (ie, lack of knowledge or debate over the interpretation of available science), stakeholders may be slow to de-adopt practices using appropriate systems levers (eg, laboratories delisting CK-MB processing), and incentives may be lacking to motivate AMCs. The results of this study should be used as a burning platform to those who wish to “test wisely” in cardiac biomarker use.
Disclosure
The authors report no conflicts of interest or financial disclosures.
1. Katus HA, Remppis A, Neumann FJ, et al. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991;83:902-912. PubMed
2. Adams JE III, Bodor GS, Dávila-Román VG, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993;88:101-106. PubMed
3. Newby LK, Roe MT, Chen AY, et al. Frequency and clinical implications of discordant creatine kinase-MB and troponin measurements in acute coronary syndromes. J Am Coll Cardiol. 2006;47:312-318. PubMed
4. Goodman SG, Steg PG, Eagle KA, et al. The diagnostic and prognostic impact of the redefinition of acute myocardial infarction: lessons from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2006;151:654-660. PubMed
5. American Society of Clinical Pathology - Choosing Wisely recommendations; http://www.choosingwisely.org/clinicianlists/#parentSociety=American_Society_for_Clinical_Pathology. Released February 2015. Accessed June 12, 2017.
6. Prochaska MT, Hohmann SF, Modes M, Arora VM. Trends in Troponin-Only Testing for AMI in Academic Teaching Hospitals and the Impact of Choosing Wisely®. J Hosp
7. Singh G, Baweja PS. CK-MB: Journey to Obsolescence. Am J Clin Pathol. 2014;141(3):415-419. PubMed
8. Larochelle MR, Knight AM, Pantle H, Riedel S, Trost JC. Reducing excess biomarker use at an academic medical center. J Gen Intern Med. 2014;29(11):1468-1474. PubMed
9. Baron JM, Lewandrowski KB, Kamis IK, Singh B, Belkziz SM, Dighe AS. A novel strategy for evaluating the effects of an electronic test ordering alert message: optimizing cardiac marker use. J Pathol Inform. 2012;3:3. PubMed
10. Thygesen K, Alpert JS, Jaffe AS, et al. Third Universal Definition of Myocardial Infarction. Circulation. 2012;126:2020-2035. PubMed
11. Saenger AK, Jaffe AS. Requiem for a Heavyweight: The Demise of CK-MB. Circulation. 2008;118(21):2200-2206. PubMed
1. Katus HA, Remppis A, Neumann FJ, et al. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991;83:902-912. PubMed
2. Adams JE III, Bodor GS, Dávila-Román VG, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993;88:101-106. PubMed
3. Newby LK, Roe MT, Chen AY, et al. Frequency and clinical implications of discordant creatine kinase-MB and troponin measurements in acute coronary syndromes. J Am Coll Cardiol. 2006;47:312-318. PubMed
4. Goodman SG, Steg PG, Eagle KA, et al. The diagnostic and prognostic impact of the redefinition of acute myocardial infarction: lessons from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2006;151:654-660. PubMed
5. American Society of Clinical Pathology - Choosing Wisely recommendations; http://www.choosingwisely.org/clinicianlists/#parentSociety=American_Society_for_Clinical_Pathology. Released February 2015. Accessed June 12, 2017.
6. Prochaska MT, Hohmann SF, Modes M, Arora VM. Trends in Troponin-Only Testing for AMI in Academic Teaching Hospitals and the Impact of Choosing Wisely®. J Hosp
7. Singh G, Baweja PS. CK-MB: Journey to Obsolescence. Am J Clin Pathol. 2014;141(3):415-419. PubMed
8. Larochelle MR, Knight AM, Pantle H, Riedel S, Trost JC. Reducing excess biomarker use at an academic medical center. J Gen Intern Med. 2014;29(11):1468-1474. PubMed
9. Baron JM, Lewandrowski KB, Kamis IK, Singh B, Belkziz SM, Dighe AS. A novel strategy for evaluating the effects of an electronic test ordering alert message: optimizing cardiac marker use. J Pathol Inform. 2012;3:3. PubMed
10. Thygesen K, Alpert JS, Jaffe AS, et al. Third Universal Definition of Myocardial Infarction. Circulation. 2012;126:2020-2035. PubMed
11. Saenger AK, Jaffe AS. Requiem for a Heavyweight: The Demise of CK-MB. Circulation. 2008;118(21):2200-2206. PubMed
© 2017 Society of Hospital Medicine
High prevalence of inappropriate benzodiazepine and sedative hypnotic prescriptions among hospitalized older adults
Older adults commonly experience insomnia and agitation during hospitalization. Unfortunately, the use of benzodiazepines and sedative hypnotics (BSH) to treat these conditions can be ineffective and expose patients to significant adverse effects.1,2 Choosing Wisely® is a campaign that promotes dialogue to reduce unnecessary medical tests, procedures, or treatments. This international campaign has highlighted BSHs as potentially harmful and has recommended against their use as first-line treatment of insomnia and agitation.3-5 Examples of harm with benzodiazepine use include cognitive impairment, impaired postural stability, and an increased incidence of falls and hip fractures in both community and acute care settings.6-8 In addition, prescriptions initiated in hospital appear to be associated with a higher risk of falls and unplanned readmission.9,10 The newer nonbenzodiazepine sedative hypnotics, commonly referred to as “z-drugs”, were initially marketed as a safer alternative in older adults due to their more favorable pharmacokinetics. Evidence has emerged that they carry similar risks.6,11,12 A study comparing benzodiazepines and zolpidem found relatively greater risk of fractures requiring hospitalization with the use of zolpidem compared to lorazepam.13
The use of benzodiazepines in the acute care setting has been evaluated in a number of studies and ranges from 20% to 45%.14-16 Few studies focus on the initiation of these medications in BSH-naïve hospitalized patients; however, reports range from 18% to 29%.17,18 Factors found to be associated with potentially inappropriate prescriptions (PIP) include Hispanic ethnicity, residing in an assisted care setting, and a greater number of BSH prescriptions prior to admission.16,19 Additionally, Cumbler et al.15 found that the presence of dementia was associated with fewer prescriptions for sleep aids in hospital. To our knowledge, there are no published studies that have investigated prescriber factors associated with the use of BSH.
The purpose of our study was to determine the frequency of PIPs of BSH in our academic hospital. Additionally, we aimed to identify patient and prescriber factors that were associated with increased likelihood of prescriptions to help guide future quality improvement initiatives.
METHODS
Study Design and Setting
This was a retrospective observational study conducted at Mount Sinai Hospital (MSH) in Toronto over a 4-month period from January 2013 to April 2013. The hospital is a 442-bed acute care academic health science center affiliated with the University of Toronto. The MSH electronic health record contains demographic data, medications and allergies, nursing documentation, and medical histories from prior encounters. It also includes computerized physician order entry (CPOE) and a detailed medication administration record. This system is integrated with an electronic pharmacy database used to monitor and dispense medications for each patient.
Patient and Medication Selection
We included inpatients over the age of 65 who were prescribed a BSH during the study period from the following services: general internal medicine, cardiology, general surgery, orthopedic surgery, and otolaryngology. To identify new exposure to BSHs, we excluded patients who were regularly prescribed a BSH prior to admission to hospital. The medications of interest included all benzodiazepines and the nonbenzodiazepine sedative hypnotic, zopiclone. Zopiclone is the most commonly used nonbenzodiazepine sedative hypnotic in Canada and the only 1 available on our hospital formulary. These were selected based on the strength of evidence to recommend against their use as first-line agents in older adults and in consultation with our geriatric medicine consultation team pharmacist.20
Data Collection
The hospital administrative database provided patient demographic information, admission service, admitting diagnosis, length of stay, and the total number of patients discharged from the study units over the study period. We then searched the pharmacy electronic database for all benzodiazepines and zopiclone prescribed during the study period for patients who met the inclusion criteria. Manual review of paper and electronic health records for this cohort of patients was conducted to extract additional variables. We used a standardized form to record data elements. Dr. Pek collected all data elements. Dr. Remfry reviewed a random sample of patient records (10%) to ensure accuracy. The agreement between reviewers was 100%.
In compliance with hospital accreditation standards, a clinical pharmacist documents a best possible medication history (BPMH) on every inpatient on admission. We used the BPMH to identify and exclude patients who were prescribed a BSH prior to hospitalization. Because all medications were ordered through the CPOE system, as-needed medication prescriptions required the selection of a specified indication. Available options included ‘agitation/anxiety’ and necessitated combining these 2 indications into 1 category. Indications were primarily extracted through electronic order entry reviews. Paper charts were reviewed when further clarification was needed.
We identified ordering physicians’ training level and familiarity with the service from administrative records obtained from medical education offices, hospital records, and relevant call schedules. Fellows were defined as trainees with a minimum of 6 years of postgraduate training.
Our primary outcome of interest was the proportion of eligible patients age 65 and older who received a PIP for a BSH. Patient variables of interest included age, sex, comorbid conditions, and a pre-admission diagnosis of dementia. Comorbid conditions and age were used to calculate the Carlson Comorbidity Index for each patient.21 Prescription variables included the medication prescribed, time of first prescription (“overnight hours” refer to prescriptions ordered after 7:00
Appropriateness Criteria
Criteria for potentially inappropriate use were modified from the American and Canadian Geriatrics Societies’ Choosing Wisely recommendations,4,5 and included insomnia and agitation. These recommendations are in line with other evidence based guidelines for safe prescribing in older adults.20 For the purposes of our study, prescriptions for “agitation/anxiety”, “agitation”, or “insomnia/sleep” were considered potentially inappropriate. Appropriate indications included alcohol withdrawal, end-of-life symptom control, preprocedural sedation, and seizure.5 Patients who were already using a BSH prior to admission for any indication, including a psychiatric diagnosis, were excluded.
Statistical Analyses
We determined the proportion of patients with at least one PIP, as well as the proportion of all prescribing events that were potentially inappropriate. We used the Chi-square statistic and 2-sample t tests to compare the unadjusted associations between patient-level characteristics and receipt of at least 1 inappropriate prescription and prescribing event-level factors with inappropriate prescriptions. Given that first-year residents are more likely to be working overnight when most PIPs are prescribed, we performed a simple logistic regression of potentially inappropriate prescribing by level of training stratified by time of prescription. A multivariable random-intercept logistic regression model was used to assess the adjusted association between patient- and prescribing event-level characteristics with inappropriate prescribing, adjusting for clustering of prescribing events within patients. Characteristics of interest were identified a priori and those with significant bivariate associations with potentially inappropriate were selected for inclusion in the model. Additionally, we included time of prescription in our model to control for potential confounding. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, North Carolina). The MSH Research Ethics Board approved the study.
RESULTS
Description of Patients Prescribed a Benzodiazepine Sedative Hypnotic
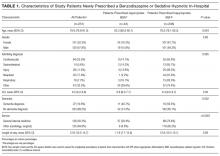
There were 1540 patients over the age of 65 discharged during the 4-month study period. We excluded the 232 patients who had been prescribed a BSH prior to admission. Of the remaining eligible 1308 BSH-naïve patients, 251 (19.2%) were prescribed a new BSH in hospital and were included in the study. Of this cohort of 251 patients, 193 (76.9%) patients were prescribed a single BSH during their admission while 58 (23.1%) received 2 or more. Of all eligible patients, 208 (15.9%) were prescribed at least 1 PIP. Approximately half of the cohort was admitted to the general internal medicine service, and the most common reason for admission was cardiovascular disease (Table 1).
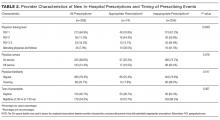
Description of Prescriptions of Benzodiazepine Sedative Hypnotic
We reviewed 328 prescriptions for BSH during the study period. The majority of these, 254 (77.4%) were potentially inappropriate (Table 2). The most common PIPs were zopiclone (167; 65.7%) and lorazepam (82; 32.3%). The PIPs were most frequently ordered on an as-needed basis (219; 86%), followed by one-time orders (30; 12%), and standing orders (5; 2%). The majority of PIPs (222; 87.4%) was prescribed for insomnia with a minority (32; 12.6%) prescribed for agitation and/or anxiety.
Most PIP were prescribed during overnight hours (159; 62.6%) and when an in-house pharmacist was unavailable (211; 83.1%). These variables were highly correlated with prescription of sleep aid, which was defined in our criteria as potentially inappropriate. Copies of discharge prescriptions were available for 189 patients. Of these 189 patients, 19 (10.1%) were sent home with a prescription for a new sedative.
Association Between Patient/Provider Variables and Prescriptions
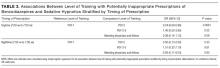
Patient factors associated with fewer PIPs in our bivariate analyses included older age and dementia (Table 1). A greater proportion of nighttime prescriptions were PIPs; however, this finding was not statistically significant (P = 0.067). The majority of all prescriptions was prescribed by residents in their first year of training (64.9%; Table 2), and there was a significant difference in rates of PIP across level of training (P = 0.0007). When stratified by time of prescription, there was no significant difference by level of training for nighttime prescriptions. Among daytime prescriptions, second-year residents and staff (attending physicians and fellows) were less likely to prescribe a PIP than first-year residents (odds ratio [OR], 0.24; 95% confidence interval [CI], 0.09-0.66 and OR, 0.39; 95% CI, 0.14-1.13, respectively; Table 3); however, the association between staff and first-years only approached statistical significance (P = 0.08). Interestingly, 20.4% of all PIPs were ordered routinely as part of an admission or postoperative order set.
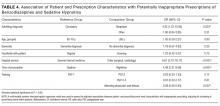
In our regression model, admission to a specialty or surgical service, compared to the general internal medicine service, was associated with a significantly higher likelihood of a PIP (OR, 6.61; 95% CI, 2.70-16.17; Table 4). Additionally, compared to cardiovascular admission diagnoses, neoplastic admitting diagnoses were associated with a higher likelihood of a PIP (OR, 4.43; 95% CI, 1.23-15.95). Time of prescription was a significant predictor in our multivariable regression model with nighttime prescriptions having increased odds of a PIP (OR, 4.48; 95% CI, 2.21-9.06,). When comparing prescribers at the extremes of training, attending physicians and fellows were much less likely to prescribe a PIP compared to first-year residents (OR, 0.23; 95% CI, 0.08-0.69; Table 4). However, there were no other significant differences across training levels after adjusting for patient and prescribing event characteristics.
DISCUSSION
We found that the majority of newly prescribed BSH in hospital was for the potentially inappropriate indications of insomnia and agitation/anxiety. Medications for insomnia were primarily initiated during overnight hours. Training level of prescribers and admitting service were found to be associated with appropriateness of prescriptions.
Our study showed that 15.9% of hospitalized older adults were newly prescribed a PIP during their admission. Of all new in hospital prescriptions, 77% were deemed potentially inappropriate. These numbers are similar to those reported by other centers; however, wide ranges exist.16,19 This is likely the result of differences in appropriate use and inclusion criteria. Gillis et al.17 focused their investigation on sleep aids and showed that 26% of all admitted patients and 18% of BSH naïve patients received a prescription for insomnia. While this is similar to our findings, more than half of these patients were under the age of 65, and additional medications, such as trazodone, antihistamines, and antipsychotics were included.17 Other studies did not exclude patients who used a BSH regularly prior to admission. For example, 21% of veterans admitted to an acute care facility received a prescription for potentially inappropriate indications, but this included continuation of prior home medications.19 In contrast, we chose to focus on older adults in whom BSH pose a greater risk of harm. Exclusion of patients who regularly used a BSH prior to admission allowed us to better understand the circumstances surrounding the initiation of these medications in hospital. Furthermore, abrupt cessation of benzodiazepines can cause withdrawal and worsen confusion.22
We found that 10% of patients newly prescribed a BSH in hospital were discharged with a prescription for a BSH. The accuracy of this is limited by the lack of availability of electronic discharge prescriptions on our surgical wards; however, it is likely an underrepresentation of the true effect given the high rates of PIPs on these wards. Our study highlights the concerning practice of continuing newly prescribed BSH following discharge from hospital.
Sleep disruption and poor quality sleep in hospital is a common issue that leads to significant use of BSH.15 Nonpharmacologic interventions in older adults can be effective in improving sleep quality and reducing the need for BSH; however, they can be time-consuming to implement.23 With the exception of preventative strategies used on our Acute Care for Elders unit, formal nonpharmacologic interventions for sleep are not practiced in our hospital. We found that the majority of PIPs were prescribed as sleep aids in the overnight hours. This suggests that disruptions in sleep are leading patients and nursing staff to request pharmacologic treatments and highlights an area with significant room for improvement. Work is underway to implement and evaluate safe sleep protocols for older adults.
To our knowledge, we are the first to report an association between training level and PIP of BSH in older adults. The highest rates of PIPs were found among the first-year residents and, after controlling for patient and prescribing event characteristics, such as time of prescription, first-year residents were significantly more likely to prescribe a PIP. First-year residents are more likely to respond first to issues on the wards. There may be pressure on first-year trainees to prescribe sleep aids, as many patients and nurses may seek pharmacologic solutions for symptom management. Knowledge gaps may also be a contributing factor early in their training. A survey of physicians found that residents were more likely than attending physicians to list lack of formal education as a barrier to appropriate prescribing.24
Similarities are seen in a study of antibiotic appropriateness, where residents demonstrated gaps in knowledge of treatment of asymptomatic bacteriuria that seemed to vary by specialty.25 Interestingly, we found that patients admitted to general internal medicine were prescribed fewer PIPs. This service includes our Acute Care for Elders unit, which is staffed by trained geriatric nurses and other allied health professionals. Residents who rotated on internal medicine are also likely to have received informal teaching about medication safety in older adults. Educational interventions highlighting adverse effects of BSH and promoting nonpharmacologic solutions should be targeted at first-year residents. However, an interprofessional team approach to sleep disturbance in hospital, in combination with decision support for appropriate BSH use will achieve greater impact than education alone.
Several limitations of this study merit discussion. First, findings from a single academic center may lack generalizability. However, the demographics of our patient population and our rates of BSH use were similar to those reported in previous studies. Second, our study may be subject to observer bias, as the data collectors were not blinded. To minimize this, a strict template and clear appropriateness criteria were developed. Additionally, a second reviewer independently conducted data validation with 100% agreement among reviewers. Third, we studied prescribing patterns rather than medication administration and lacked data on filling of new BSH prescriptions in the postdischarge period. However, our primary goal is to determine risk of exposure to a BSH to minimize it. Fourth, although BSH are discouraged as “first choice for insomnia, anxiety or delirium,”4 they may be appropriate in limited situations where all nonpharmacologic strategies have failed and patient or staff safety is at risk. In our chart reviews, we were unable to determine whether all nonpharmacologic strategies were exhausted prior to prescription initiation. However, more than 20% of all PIP were routinely prescribed as part of an admission or postoperative order set, suggesting a reflexive rather than reflective approach to sedative use. Furthermore, the indications of anxiety and agitation were combined as they appear in the CPOE as a combination indication, thus leaving us unable to determine the true proportion for each indication. However, more than 87% of all PIPs were for insomnia, reflecting a clear opportunity to improve sleep management in hospital. Last, the lack of a power calculation may have resulted in the study being underpowered and thus affected the ability to detect a significant effect of covariates that have real differences on the likelihood of sedative prescriptions. For example, the low number of prescribing events by second-year residents and staff may have resulted in a type II error when comparing PIP rates with first-year residents.
We found that the majority of newly prescribed BSH among older adults in hospital were potentially inappropriate. They were most frequently prescribed by first-year residents overnight in response to insomnia. Our findings demonstrate BSH overuse remains prevalent and is associated with poor sleep in hospital. Future work will focus on implementing and evaluating safe sleep protocols and educational interventions aimed at first-year residents.
Acknowledgments
Elisabeth Pek had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Ciara Pendrith conducted and is responsible for the statistical analysis.
Disclosure
The authors report no financial conflicts of interest.
1. Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331(7526):1169. PubMed
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165. PubMed
3. Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely--the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589-592. PubMed
4. Ten Things Physicians and Patients Should Question. American Geriatrics Society 2013. Revised April 23, 2015. http://www.choosingwisely.org/societies/american-geriatrics-society/. Accessed April 30, 2016.
5. Five Things Physicians and Patients Should Question. Canadian Geriatrics Society. Released April 2, 2014. http://www.choosingwiselycanada.org/recommendations/geriatrics/. Accessed April 30, 2016.
6. de Groot MH, van Campen JP, Moek MA, Tulner LR, Beijnen JH, Lamoth CJ. The effects of fall-risk-increasing drugs on postural control: a literature review. Drugs Aging. 2013;30(11):901-920. PubMed
7. Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952-1960. PubMed
8. Pariente A, Dartigues JF, Benichou J, Letenneur L, Moore N, Fourrier-Réglat A. Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging. 2008;25(1):61-70. PubMed
9. Frels C, Williams P, Narayanan S, Gariballa SE. Iatrogenic causes of falls in hospitalised elderly patients: a case-control study. Postgrad Med J. 2002;78(922):487-489. PubMed
10. Pavon JM, Zhao Y, McConnell E, Hastings SN. Identifying risk of readmission in hospitalized elderly adults through inpatient medication exposure. J Am Geriatr Soc. 2014;62(6):1116-1121. PubMed
11. Kang DY, Park S, Rhee CW, et al. Zolpidem use and risk of fracture in elderly insomnia patients. J Prev Med Public Health. 2012;45(4):219-226. PubMed
12. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
13. Finkle WD, Der JS, Greenland S, et al. Risk of fractures requiring hospitalization after an initial prescription for zolpidem, alprazolam, lorazepam, or diazepam in older adults. J Am Geriatr Soc. 2011;59(10):1883-1890. PubMed
14. Elliott RA, Woodward MC, Oborne CA. Improving benzodiazepine prescribing for elderly hospital inpatients using audit and multidisciplinary feedback. Intern Med J. 2001;31(9):529-535. PubMed
15. Cumbler E, Guerrasio J, Kim J, Glasheen J. Use of medications for insomnia in the hospitalized geriatric population. J Am Geriatr Soc. 2008;56(3):579-581. PubMed
16. Somers A, Robays H, Audenaert K, Van Maele G, Bogaert M, Petrovic M. The use of hypnosedative drugs in a university hospital: has anything changed in 10 years? Eur J Clin Pharmacol. 2011;67(7):723-729. PubMed
17. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
18. Frighetto L, Marra C, Bandali S, Wilbur K, Naumann T, Jewesson P. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17. PubMed
19. Garrido MM, Prigerson HG, Penrod JD, Jones SC, Boockvar KS. Benzodiazepine and sedative-hypnotic use among older seriously Ill veterans: choosing wisely? Clin Ther. 2014;36(11):1547-1554. PubMed
20. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults: The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. J Am Geriatr Soc. 2012;60(4):616-631. PubMed
21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. PubMed
22. Foy A, Drinkwater V, March S, Mearrick P. Confusion after admission to hospital in elderly patients using benzodiazepines. Br Med J (Clin Res Ed). 1986;293(6554):1072. PubMed
23. McDowell JA, Mion LC, Lydon TJ, Inouye SK. A nonpharmacologic sleep protocol for hospitalized older patients. J Am Geriatr Soc. 1998;46(6):700-705. PubMed
24. Ramaswamy R, Maio V, Diamond JJ, et al. Potentially inappropriate prescribing in elderly: assessing doctor knowledge, confidence and barriers. J Eval Clin Pract. 2011;17(6):1153-1159. PubMed
25. Lee MJ, Kim M, Kim NH, et al. Why is asymptomatic bacteriuria overtreated?: A tertiary care institutional survey of resident physicians. BMC Infect Dis. 2015;15:289. PubMed
Older adults commonly experience insomnia and agitation during hospitalization. Unfortunately, the use of benzodiazepines and sedative hypnotics (BSH) to treat these conditions can be ineffective and expose patients to significant adverse effects.1,2 Choosing Wisely® is a campaign that promotes dialogue to reduce unnecessary medical tests, procedures, or treatments. This international campaign has highlighted BSHs as potentially harmful and has recommended against their use as first-line treatment of insomnia and agitation.3-5 Examples of harm with benzodiazepine use include cognitive impairment, impaired postural stability, and an increased incidence of falls and hip fractures in both community and acute care settings.6-8 In addition, prescriptions initiated in hospital appear to be associated with a higher risk of falls and unplanned readmission.9,10 The newer nonbenzodiazepine sedative hypnotics, commonly referred to as “z-drugs”, were initially marketed as a safer alternative in older adults due to their more favorable pharmacokinetics. Evidence has emerged that they carry similar risks.6,11,12 A study comparing benzodiazepines and zolpidem found relatively greater risk of fractures requiring hospitalization with the use of zolpidem compared to lorazepam.13
The use of benzodiazepines in the acute care setting has been evaluated in a number of studies and ranges from 20% to 45%.14-16 Few studies focus on the initiation of these medications in BSH-naïve hospitalized patients; however, reports range from 18% to 29%.17,18 Factors found to be associated with potentially inappropriate prescriptions (PIP) include Hispanic ethnicity, residing in an assisted care setting, and a greater number of BSH prescriptions prior to admission.16,19 Additionally, Cumbler et al.15 found that the presence of dementia was associated with fewer prescriptions for sleep aids in hospital. To our knowledge, there are no published studies that have investigated prescriber factors associated with the use of BSH.
The purpose of our study was to determine the frequency of PIPs of BSH in our academic hospital. Additionally, we aimed to identify patient and prescriber factors that were associated with increased likelihood of prescriptions to help guide future quality improvement initiatives.
METHODS
Study Design and Setting
This was a retrospective observational study conducted at Mount Sinai Hospital (MSH) in Toronto over a 4-month period from January 2013 to April 2013. The hospital is a 442-bed acute care academic health science center affiliated with the University of Toronto. The MSH electronic health record contains demographic data, medications and allergies, nursing documentation, and medical histories from prior encounters. It also includes computerized physician order entry (CPOE) and a detailed medication administration record. This system is integrated with an electronic pharmacy database used to monitor and dispense medications for each patient.
Patient and Medication Selection
We included inpatients over the age of 65 who were prescribed a BSH during the study period from the following services: general internal medicine, cardiology, general surgery, orthopedic surgery, and otolaryngology. To identify new exposure to BSHs, we excluded patients who were regularly prescribed a BSH prior to admission to hospital. The medications of interest included all benzodiazepines and the nonbenzodiazepine sedative hypnotic, zopiclone. Zopiclone is the most commonly used nonbenzodiazepine sedative hypnotic in Canada and the only 1 available on our hospital formulary. These were selected based on the strength of evidence to recommend against their use as first-line agents in older adults and in consultation with our geriatric medicine consultation team pharmacist.20
Data Collection
The hospital administrative database provided patient demographic information, admission service, admitting diagnosis, length of stay, and the total number of patients discharged from the study units over the study period. We then searched the pharmacy electronic database for all benzodiazepines and zopiclone prescribed during the study period for patients who met the inclusion criteria. Manual review of paper and electronic health records for this cohort of patients was conducted to extract additional variables. We used a standardized form to record data elements. Dr. Pek collected all data elements. Dr. Remfry reviewed a random sample of patient records (10%) to ensure accuracy. The agreement between reviewers was 100%.
In compliance with hospital accreditation standards, a clinical pharmacist documents a best possible medication history (BPMH) on every inpatient on admission. We used the BPMH to identify and exclude patients who were prescribed a BSH prior to hospitalization. Because all medications were ordered through the CPOE system, as-needed medication prescriptions required the selection of a specified indication. Available options included ‘agitation/anxiety’ and necessitated combining these 2 indications into 1 category. Indications were primarily extracted through electronic order entry reviews. Paper charts were reviewed when further clarification was needed.
We identified ordering physicians’ training level and familiarity with the service from administrative records obtained from medical education offices, hospital records, and relevant call schedules. Fellows were defined as trainees with a minimum of 6 years of postgraduate training.
Our primary outcome of interest was the proportion of eligible patients age 65 and older who received a PIP for a BSH. Patient variables of interest included age, sex, comorbid conditions, and a pre-admission diagnosis of dementia. Comorbid conditions and age were used to calculate the Carlson Comorbidity Index for each patient.21 Prescription variables included the medication prescribed, time of first prescription (“overnight hours” refer to prescriptions ordered after 7:00
Appropriateness Criteria
Criteria for potentially inappropriate use were modified from the American and Canadian Geriatrics Societies’ Choosing Wisely recommendations,4,5 and included insomnia and agitation. These recommendations are in line with other evidence based guidelines for safe prescribing in older adults.20 For the purposes of our study, prescriptions for “agitation/anxiety”, “agitation”, or “insomnia/sleep” were considered potentially inappropriate. Appropriate indications included alcohol withdrawal, end-of-life symptom control, preprocedural sedation, and seizure.5 Patients who were already using a BSH prior to admission for any indication, including a psychiatric diagnosis, were excluded.
Statistical Analyses
We determined the proportion of patients with at least one PIP, as well as the proportion of all prescribing events that were potentially inappropriate. We used the Chi-square statistic and 2-sample t tests to compare the unadjusted associations between patient-level characteristics and receipt of at least 1 inappropriate prescription and prescribing event-level factors with inappropriate prescriptions. Given that first-year residents are more likely to be working overnight when most PIPs are prescribed, we performed a simple logistic regression of potentially inappropriate prescribing by level of training stratified by time of prescription. A multivariable random-intercept logistic regression model was used to assess the adjusted association between patient- and prescribing event-level characteristics with inappropriate prescribing, adjusting for clustering of prescribing events within patients. Characteristics of interest were identified a priori and those with significant bivariate associations with potentially inappropriate were selected for inclusion in the model. Additionally, we included time of prescription in our model to control for potential confounding. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, North Carolina). The MSH Research Ethics Board approved the study.
RESULTS
Description of Patients Prescribed a Benzodiazepine Sedative Hypnotic
There were 1540 patients over the age of 65 discharged during the 4-month study period. We excluded the 232 patients who had been prescribed a BSH prior to admission. Of the remaining eligible 1308 BSH-naïve patients, 251 (19.2%) were prescribed a new BSH in hospital and were included in the study. Of this cohort of 251 patients, 193 (76.9%) patients were prescribed a single BSH during their admission while 58 (23.1%) received 2 or more. Of all eligible patients, 208 (15.9%) were prescribed at least 1 PIP. Approximately half of the cohort was admitted to the general internal medicine service, and the most common reason for admission was cardiovascular disease (Table 1).
Description of Prescriptions of Benzodiazepine Sedative Hypnotic
We reviewed 328 prescriptions for BSH during the study period. The majority of these, 254 (77.4%) were potentially inappropriate (Table 2). The most common PIPs were zopiclone (167; 65.7%) and lorazepam (82; 32.3%). The PIPs were most frequently ordered on an as-needed basis (219; 86%), followed by one-time orders (30; 12%), and standing orders (5; 2%). The majority of PIPs (222; 87.4%) was prescribed for insomnia with a minority (32; 12.6%) prescribed for agitation and/or anxiety.
Most PIP were prescribed during overnight hours (159; 62.6%) and when an in-house pharmacist was unavailable (211; 83.1%). These variables were highly correlated with prescription of sleep aid, which was defined in our criteria as potentially inappropriate. Copies of discharge prescriptions were available for 189 patients. Of these 189 patients, 19 (10.1%) were sent home with a prescription for a new sedative.
Association Between Patient/Provider Variables and Prescriptions
Patient factors associated with fewer PIPs in our bivariate analyses included older age and dementia (Table 1). A greater proportion of nighttime prescriptions were PIPs; however, this finding was not statistically significant (P = 0.067). The majority of all prescriptions was prescribed by residents in their first year of training (64.9%; Table 2), and there was a significant difference in rates of PIP across level of training (P = 0.0007). When stratified by time of prescription, there was no significant difference by level of training for nighttime prescriptions. Among daytime prescriptions, second-year residents and staff (attending physicians and fellows) were less likely to prescribe a PIP than first-year residents (odds ratio [OR], 0.24; 95% confidence interval [CI], 0.09-0.66 and OR, 0.39; 95% CI, 0.14-1.13, respectively; Table 3); however, the association between staff and first-years only approached statistical significance (P = 0.08). Interestingly, 20.4% of all PIPs were ordered routinely as part of an admission or postoperative order set.
In our regression model, admission to a specialty or surgical service, compared to the general internal medicine service, was associated with a significantly higher likelihood of a PIP (OR, 6.61; 95% CI, 2.70-16.17; Table 4). Additionally, compared to cardiovascular admission diagnoses, neoplastic admitting diagnoses were associated with a higher likelihood of a PIP (OR, 4.43; 95% CI, 1.23-15.95). Time of prescription was a significant predictor in our multivariable regression model with nighttime prescriptions having increased odds of a PIP (OR, 4.48; 95% CI, 2.21-9.06,). When comparing prescribers at the extremes of training, attending physicians and fellows were much less likely to prescribe a PIP compared to first-year residents (OR, 0.23; 95% CI, 0.08-0.69; Table 4). However, there were no other significant differences across training levels after adjusting for patient and prescribing event characteristics.
DISCUSSION
We found that the majority of newly prescribed BSH in hospital was for the potentially inappropriate indications of insomnia and agitation/anxiety. Medications for insomnia were primarily initiated during overnight hours. Training level of prescribers and admitting service were found to be associated with appropriateness of prescriptions.
Our study showed that 15.9% of hospitalized older adults were newly prescribed a PIP during their admission. Of all new in hospital prescriptions, 77% were deemed potentially inappropriate. These numbers are similar to those reported by other centers; however, wide ranges exist.16,19 This is likely the result of differences in appropriate use and inclusion criteria. Gillis et al.17 focused their investigation on sleep aids and showed that 26% of all admitted patients and 18% of BSH naïve patients received a prescription for insomnia. While this is similar to our findings, more than half of these patients were under the age of 65, and additional medications, such as trazodone, antihistamines, and antipsychotics were included.17 Other studies did not exclude patients who used a BSH regularly prior to admission. For example, 21% of veterans admitted to an acute care facility received a prescription for potentially inappropriate indications, but this included continuation of prior home medications.19 In contrast, we chose to focus on older adults in whom BSH pose a greater risk of harm. Exclusion of patients who regularly used a BSH prior to admission allowed us to better understand the circumstances surrounding the initiation of these medications in hospital. Furthermore, abrupt cessation of benzodiazepines can cause withdrawal and worsen confusion.22
We found that 10% of patients newly prescribed a BSH in hospital were discharged with a prescription for a BSH. The accuracy of this is limited by the lack of availability of electronic discharge prescriptions on our surgical wards; however, it is likely an underrepresentation of the true effect given the high rates of PIPs on these wards. Our study highlights the concerning practice of continuing newly prescribed BSH following discharge from hospital.
Sleep disruption and poor quality sleep in hospital is a common issue that leads to significant use of BSH.15 Nonpharmacologic interventions in older adults can be effective in improving sleep quality and reducing the need for BSH; however, they can be time-consuming to implement.23 With the exception of preventative strategies used on our Acute Care for Elders unit, formal nonpharmacologic interventions for sleep are not practiced in our hospital. We found that the majority of PIPs were prescribed as sleep aids in the overnight hours. This suggests that disruptions in sleep are leading patients and nursing staff to request pharmacologic treatments and highlights an area with significant room for improvement. Work is underway to implement and evaluate safe sleep protocols for older adults.
To our knowledge, we are the first to report an association between training level and PIP of BSH in older adults. The highest rates of PIPs were found among the first-year residents and, after controlling for patient and prescribing event characteristics, such as time of prescription, first-year residents were significantly more likely to prescribe a PIP. First-year residents are more likely to respond first to issues on the wards. There may be pressure on first-year trainees to prescribe sleep aids, as many patients and nurses may seek pharmacologic solutions for symptom management. Knowledge gaps may also be a contributing factor early in their training. A survey of physicians found that residents were more likely than attending physicians to list lack of formal education as a barrier to appropriate prescribing.24
Similarities are seen in a study of antibiotic appropriateness, where residents demonstrated gaps in knowledge of treatment of asymptomatic bacteriuria that seemed to vary by specialty.25 Interestingly, we found that patients admitted to general internal medicine were prescribed fewer PIPs. This service includes our Acute Care for Elders unit, which is staffed by trained geriatric nurses and other allied health professionals. Residents who rotated on internal medicine are also likely to have received informal teaching about medication safety in older adults. Educational interventions highlighting adverse effects of BSH and promoting nonpharmacologic solutions should be targeted at first-year residents. However, an interprofessional team approach to sleep disturbance in hospital, in combination with decision support for appropriate BSH use will achieve greater impact than education alone.
Several limitations of this study merit discussion. First, findings from a single academic center may lack generalizability. However, the demographics of our patient population and our rates of BSH use were similar to those reported in previous studies. Second, our study may be subject to observer bias, as the data collectors were not blinded. To minimize this, a strict template and clear appropriateness criteria were developed. Additionally, a second reviewer independently conducted data validation with 100% agreement among reviewers. Third, we studied prescribing patterns rather than medication administration and lacked data on filling of new BSH prescriptions in the postdischarge period. However, our primary goal is to determine risk of exposure to a BSH to minimize it. Fourth, although BSH are discouraged as “first choice for insomnia, anxiety or delirium,”4 they may be appropriate in limited situations where all nonpharmacologic strategies have failed and patient or staff safety is at risk. In our chart reviews, we were unable to determine whether all nonpharmacologic strategies were exhausted prior to prescription initiation. However, more than 20% of all PIP were routinely prescribed as part of an admission or postoperative order set, suggesting a reflexive rather than reflective approach to sedative use. Furthermore, the indications of anxiety and agitation were combined as they appear in the CPOE as a combination indication, thus leaving us unable to determine the true proportion for each indication. However, more than 87% of all PIPs were for insomnia, reflecting a clear opportunity to improve sleep management in hospital. Last, the lack of a power calculation may have resulted in the study being underpowered and thus affected the ability to detect a significant effect of covariates that have real differences on the likelihood of sedative prescriptions. For example, the low number of prescribing events by second-year residents and staff may have resulted in a type II error when comparing PIP rates with first-year residents.
We found that the majority of newly prescribed BSH among older adults in hospital were potentially inappropriate. They were most frequently prescribed by first-year residents overnight in response to insomnia. Our findings demonstrate BSH overuse remains prevalent and is associated with poor sleep in hospital. Future work will focus on implementing and evaluating safe sleep protocols and educational interventions aimed at first-year residents.
Acknowledgments
Elisabeth Pek had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Ciara Pendrith conducted and is responsible for the statistical analysis.
Disclosure
The authors report no financial conflicts of interest.
Older adults commonly experience insomnia and agitation during hospitalization. Unfortunately, the use of benzodiazepines and sedative hypnotics (BSH) to treat these conditions can be ineffective and expose patients to significant adverse effects.1,2 Choosing Wisely® is a campaign that promotes dialogue to reduce unnecessary medical tests, procedures, or treatments. This international campaign has highlighted BSHs as potentially harmful and has recommended against their use as first-line treatment of insomnia and agitation.3-5 Examples of harm with benzodiazepine use include cognitive impairment, impaired postural stability, and an increased incidence of falls and hip fractures in both community and acute care settings.6-8 In addition, prescriptions initiated in hospital appear to be associated with a higher risk of falls and unplanned readmission.9,10 The newer nonbenzodiazepine sedative hypnotics, commonly referred to as “z-drugs”, were initially marketed as a safer alternative in older adults due to their more favorable pharmacokinetics. Evidence has emerged that they carry similar risks.6,11,12 A study comparing benzodiazepines and zolpidem found relatively greater risk of fractures requiring hospitalization with the use of zolpidem compared to lorazepam.13
The use of benzodiazepines in the acute care setting has been evaluated in a number of studies and ranges from 20% to 45%.14-16 Few studies focus on the initiation of these medications in BSH-naïve hospitalized patients; however, reports range from 18% to 29%.17,18 Factors found to be associated with potentially inappropriate prescriptions (PIP) include Hispanic ethnicity, residing in an assisted care setting, and a greater number of BSH prescriptions prior to admission.16,19 Additionally, Cumbler et al.15 found that the presence of dementia was associated with fewer prescriptions for sleep aids in hospital. To our knowledge, there are no published studies that have investigated prescriber factors associated with the use of BSH.
The purpose of our study was to determine the frequency of PIPs of BSH in our academic hospital. Additionally, we aimed to identify patient and prescriber factors that were associated with increased likelihood of prescriptions to help guide future quality improvement initiatives.
METHODS
Study Design and Setting
This was a retrospective observational study conducted at Mount Sinai Hospital (MSH) in Toronto over a 4-month period from January 2013 to April 2013. The hospital is a 442-bed acute care academic health science center affiliated with the University of Toronto. The MSH electronic health record contains demographic data, medications and allergies, nursing documentation, and medical histories from prior encounters. It also includes computerized physician order entry (CPOE) and a detailed medication administration record. This system is integrated with an electronic pharmacy database used to monitor and dispense medications for each patient.
Patient and Medication Selection
We included inpatients over the age of 65 who were prescribed a BSH during the study period from the following services: general internal medicine, cardiology, general surgery, orthopedic surgery, and otolaryngology. To identify new exposure to BSHs, we excluded patients who were regularly prescribed a BSH prior to admission to hospital. The medications of interest included all benzodiazepines and the nonbenzodiazepine sedative hypnotic, zopiclone. Zopiclone is the most commonly used nonbenzodiazepine sedative hypnotic in Canada and the only 1 available on our hospital formulary. These were selected based on the strength of evidence to recommend against their use as first-line agents in older adults and in consultation with our geriatric medicine consultation team pharmacist.20
Data Collection
The hospital administrative database provided patient demographic information, admission service, admitting diagnosis, length of stay, and the total number of patients discharged from the study units over the study period. We then searched the pharmacy electronic database for all benzodiazepines and zopiclone prescribed during the study period for patients who met the inclusion criteria. Manual review of paper and electronic health records for this cohort of patients was conducted to extract additional variables. We used a standardized form to record data elements. Dr. Pek collected all data elements. Dr. Remfry reviewed a random sample of patient records (10%) to ensure accuracy. The agreement between reviewers was 100%.
In compliance with hospital accreditation standards, a clinical pharmacist documents a best possible medication history (BPMH) on every inpatient on admission. We used the BPMH to identify and exclude patients who were prescribed a BSH prior to hospitalization. Because all medications were ordered through the CPOE system, as-needed medication prescriptions required the selection of a specified indication. Available options included ‘agitation/anxiety’ and necessitated combining these 2 indications into 1 category. Indications were primarily extracted through electronic order entry reviews. Paper charts were reviewed when further clarification was needed.
We identified ordering physicians’ training level and familiarity with the service from administrative records obtained from medical education offices, hospital records, and relevant call schedules. Fellows were defined as trainees with a minimum of 6 years of postgraduate training.
Our primary outcome of interest was the proportion of eligible patients age 65 and older who received a PIP for a BSH. Patient variables of interest included age, sex, comorbid conditions, and a pre-admission diagnosis of dementia. Comorbid conditions and age were used to calculate the Carlson Comorbidity Index for each patient.21 Prescription variables included the medication prescribed, time of first prescription (“overnight hours” refer to prescriptions ordered after 7:00
Appropriateness Criteria
Criteria for potentially inappropriate use were modified from the American and Canadian Geriatrics Societies’ Choosing Wisely recommendations,4,5 and included insomnia and agitation. These recommendations are in line with other evidence based guidelines for safe prescribing in older adults.20 For the purposes of our study, prescriptions for “agitation/anxiety”, “agitation”, or “insomnia/sleep” were considered potentially inappropriate. Appropriate indications included alcohol withdrawal, end-of-life symptom control, preprocedural sedation, and seizure.5 Patients who were already using a BSH prior to admission for any indication, including a psychiatric diagnosis, were excluded.
Statistical Analyses
We determined the proportion of patients with at least one PIP, as well as the proportion of all prescribing events that were potentially inappropriate. We used the Chi-square statistic and 2-sample t tests to compare the unadjusted associations between patient-level characteristics and receipt of at least 1 inappropriate prescription and prescribing event-level factors with inappropriate prescriptions. Given that first-year residents are more likely to be working overnight when most PIPs are prescribed, we performed a simple logistic regression of potentially inappropriate prescribing by level of training stratified by time of prescription. A multivariable random-intercept logistic regression model was used to assess the adjusted association between patient- and prescribing event-level characteristics with inappropriate prescribing, adjusting for clustering of prescribing events within patients. Characteristics of interest were identified a priori and those with significant bivariate associations with potentially inappropriate were selected for inclusion in the model. Additionally, we included time of prescription in our model to control for potential confounding. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc, Cary, North Carolina). The MSH Research Ethics Board approved the study.
RESULTS
Description of Patients Prescribed a Benzodiazepine Sedative Hypnotic
There were 1540 patients over the age of 65 discharged during the 4-month study period. We excluded the 232 patients who had been prescribed a BSH prior to admission. Of the remaining eligible 1308 BSH-naïve patients, 251 (19.2%) were prescribed a new BSH in hospital and were included in the study. Of this cohort of 251 patients, 193 (76.9%) patients were prescribed a single BSH during their admission while 58 (23.1%) received 2 or more. Of all eligible patients, 208 (15.9%) were prescribed at least 1 PIP. Approximately half of the cohort was admitted to the general internal medicine service, and the most common reason for admission was cardiovascular disease (Table 1).
Description of Prescriptions of Benzodiazepine Sedative Hypnotic
We reviewed 328 prescriptions for BSH during the study period. The majority of these, 254 (77.4%) were potentially inappropriate (Table 2). The most common PIPs were zopiclone (167; 65.7%) and lorazepam (82; 32.3%). The PIPs were most frequently ordered on an as-needed basis (219; 86%), followed by one-time orders (30; 12%), and standing orders (5; 2%). The majority of PIPs (222; 87.4%) was prescribed for insomnia with a minority (32; 12.6%) prescribed for agitation and/or anxiety.
Most PIP were prescribed during overnight hours (159; 62.6%) and when an in-house pharmacist was unavailable (211; 83.1%). These variables were highly correlated with prescription of sleep aid, which was defined in our criteria as potentially inappropriate. Copies of discharge prescriptions were available for 189 patients. Of these 189 patients, 19 (10.1%) were sent home with a prescription for a new sedative.
Association Between Patient/Provider Variables and Prescriptions
Patient factors associated with fewer PIPs in our bivariate analyses included older age and dementia (Table 1). A greater proportion of nighttime prescriptions were PIPs; however, this finding was not statistically significant (P = 0.067). The majority of all prescriptions was prescribed by residents in their first year of training (64.9%; Table 2), and there was a significant difference in rates of PIP across level of training (P = 0.0007). When stratified by time of prescription, there was no significant difference by level of training for nighttime prescriptions. Among daytime prescriptions, second-year residents and staff (attending physicians and fellows) were less likely to prescribe a PIP than first-year residents (odds ratio [OR], 0.24; 95% confidence interval [CI], 0.09-0.66 and OR, 0.39; 95% CI, 0.14-1.13, respectively; Table 3); however, the association between staff and first-years only approached statistical significance (P = 0.08). Interestingly, 20.4% of all PIPs were ordered routinely as part of an admission or postoperative order set.
In our regression model, admission to a specialty or surgical service, compared to the general internal medicine service, was associated with a significantly higher likelihood of a PIP (OR, 6.61; 95% CI, 2.70-16.17; Table 4). Additionally, compared to cardiovascular admission diagnoses, neoplastic admitting diagnoses were associated with a higher likelihood of a PIP (OR, 4.43; 95% CI, 1.23-15.95). Time of prescription was a significant predictor in our multivariable regression model with nighttime prescriptions having increased odds of a PIP (OR, 4.48; 95% CI, 2.21-9.06,). When comparing prescribers at the extremes of training, attending physicians and fellows were much less likely to prescribe a PIP compared to first-year residents (OR, 0.23; 95% CI, 0.08-0.69; Table 4). However, there were no other significant differences across training levels after adjusting for patient and prescribing event characteristics.
DISCUSSION
We found that the majority of newly prescribed BSH in hospital was for the potentially inappropriate indications of insomnia and agitation/anxiety. Medications for insomnia were primarily initiated during overnight hours. Training level of prescribers and admitting service were found to be associated with appropriateness of prescriptions.
Our study showed that 15.9% of hospitalized older adults were newly prescribed a PIP during their admission. Of all new in hospital prescriptions, 77% were deemed potentially inappropriate. These numbers are similar to those reported by other centers; however, wide ranges exist.16,19 This is likely the result of differences in appropriate use and inclusion criteria. Gillis et al.17 focused their investigation on sleep aids and showed that 26% of all admitted patients and 18% of BSH naïve patients received a prescription for insomnia. While this is similar to our findings, more than half of these patients were under the age of 65, and additional medications, such as trazodone, antihistamines, and antipsychotics were included.17 Other studies did not exclude patients who used a BSH regularly prior to admission. For example, 21% of veterans admitted to an acute care facility received a prescription for potentially inappropriate indications, but this included continuation of prior home medications.19 In contrast, we chose to focus on older adults in whom BSH pose a greater risk of harm. Exclusion of patients who regularly used a BSH prior to admission allowed us to better understand the circumstances surrounding the initiation of these medications in hospital. Furthermore, abrupt cessation of benzodiazepines can cause withdrawal and worsen confusion.22
We found that 10% of patients newly prescribed a BSH in hospital were discharged with a prescription for a BSH. The accuracy of this is limited by the lack of availability of electronic discharge prescriptions on our surgical wards; however, it is likely an underrepresentation of the true effect given the high rates of PIPs on these wards. Our study highlights the concerning practice of continuing newly prescribed BSH following discharge from hospital.
Sleep disruption and poor quality sleep in hospital is a common issue that leads to significant use of BSH.15 Nonpharmacologic interventions in older adults can be effective in improving sleep quality and reducing the need for BSH; however, they can be time-consuming to implement.23 With the exception of preventative strategies used on our Acute Care for Elders unit, formal nonpharmacologic interventions for sleep are not practiced in our hospital. We found that the majority of PIPs were prescribed as sleep aids in the overnight hours. This suggests that disruptions in sleep are leading patients and nursing staff to request pharmacologic treatments and highlights an area with significant room for improvement. Work is underway to implement and evaluate safe sleep protocols for older adults.
To our knowledge, we are the first to report an association between training level and PIP of BSH in older adults. The highest rates of PIPs were found among the first-year residents and, after controlling for patient and prescribing event characteristics, such as time of prescription, first-year residents were significantly more likely to prescribe a PIP. First-year residents are more likely to respond first to issues on the wards. There may be pressure on first-year trainees to prescribe sleep aids, as many patients and nurses may seek pharmacologic solutions for symptom management. Knowledge gaps may also be a contributing factor early in their training. A survey of physicians found that residents were more likely than attending physicians to list lack of formal education as a barrier to appropriate prescribing.24
Similarities are seen in a study of antibiotic appropriateness, where residents demonstrated gaps in knowledge of treatment of asymptomatic bacteriuria that seemed to vary by specialty.25 Interestingly, we found that patients admitted to general internal medicine were prescribed fewer PIPs. This service includes our Acute Care for Elders unit, which is staffed by trained geriatric nurses and other allied health professionals. Residents who rotated on internal medicine are also likely to have received informal teaching about medication safety in older adults. Educational interventions highlighting adverse effects of BSH and promoting nonpharmacologic solutions should be targeted at first-year residents. However, an interprofessional team approach to sleep disturbance in hospital, in combination with decision support for appropriate BSH use will achieve greater impact than education alone.
Several limitations of this study merit discussion. First, findings from a single academic center may lack generalizability. However, the demographics of our patient population and our rates of BSH use were similar to those reported in previous studies. Second, our study may be subject to observer bias, as the data collectors were not blinded. To minimize this, a strict template and clear appropriateness criteria were developed. Additionally, a second reviewer independently conducted data validation with 100% agreement among reviewers. Third, we studied prescribing patterns rather than medication administration and lacked data on filling of new BSH prescriptions in the postdischarge period. However, our primary goal is to determine risk of exposure to a BSH to minimize it. Fourth, although BSH are discouraged as “first choice for insomnia, anxiety or delirium,”4 they may be appropriate in limited situations where all nonpharmacologic strategies have failed and patient or staff safety is at risk. In our chart reviews, we were unable to determine whether all nonpharmacologic strategies were exhausted prior to prescription initiation. However, more than 20% of all PIP were routinely prescribed as part of an admission or postoperative order set, suggesting a reflexive rather than reflective approach to sedative use. Furthermore, the indications of anxiety and agitation were combined as they appear in the CPOE as a combination indication, thus leaving us unable to determine the true proportion for each indication. However, more than 87% of all PIPs were for insomnia, reflecting a clear opportunity to improve sleep management in hospital. Last, the lack of a power calculation may have resulted in the study being underpowered and thus affected the ability to detect a significant effect of covariates that have real differences on the likelihood of sedative prescriptions. For example, the low number of prescribing events by second-year residents and staff may have resulted in a type II error when comparing PIP rates with first-year residents.
We found that the majority of newly prescribed BSH among older adults in hospital were potentially inappropriate. They were most frequently prescribed by first-year residents overnight in response to insomnia. Our findings demonstrate BSH overuse remains prevalent and is associated with poor sleep in hospital. Future work will focus on implementing and evaluating safe sleep protocols and educational interventions aimed at first-year residents.
Acknowledgments
Elisabeth Pek had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Ciara Pendrith conducted and is responsible for the statistical analysis.
Disclosure
The authors report no financial conflicts of interest.
1. Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331(7526):1169. PubMed
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165. PubMed
3. Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely--the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589-592. PubMed
4. Ten Things Physicians and Patients Should Question. American Geriatrics Society 2013. Revised April 23, 2015. http://www.choosingwisely.org/societies/american-geriatrics-society/. Accessed April 30, 2016.
5. Five Things Physicians and Patients Should Question. Canadian Geriatrics Society. Released April 2, 2014. http://www.choosingwiselycanada.org/recommendations/geriatrics/. Accessed April 30, 2016.
6. de Groot MH, van Campen JP, Moek MA, Tulner LR, Beijnen JH, Lamoth CJ. The effects of fall-risk-increasing drugs on postural control: a literature review. Drugs Aging. 2013;30(11):901-920. PubMed
7. Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952-1960. PubMed
8. Pariente A, Dartigues JF, Benichou J, Letenneur L, Moore N, Fourrier-Réglat A. Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging. 2008;25(1):61-70. PubMed
9. Frels C, Williams P, Narayanan S, Gariballa SE. Iatrogenic causes of falls in hospitalised elderly patients: a case-control study. Postgrad Med J. 2002;78(922):487-489. PubMed
10. Pavon JM, Zhao Y, McConnell E, Hastings SN. Identifying risk of readmission in hospitalized elderly adults through inpatient medication exposure. J Am Geriatr Soc. 2014;62(6):1116-1121. PubMed
11. Kang DY, Park S, Rhee CW, et al. Zolpidem use and risk of fracture in elderly insomnia patients. J Prev Med Public Health. 2012;45(4):219-226. PubMed
12. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
13. Finkle WD, Der JS, Greenland S, et al. Risk of fractures requiring hospitalization after an initial prescription for zolpidem, alprazolam, lorazepam, or diazepam in older adults. J Am Geriatr Soc. 2011;59(10):1883-1890. PubMed
14. Elliott RA, Woodward MC, Oborne CA. Improving benzodiazepine prescribing for elderly hospital inpatients using audit and multidisciplinary feedback. Intern Med J. 2001;31(9):529-535. PubMed
15. Cumbler E, Guerrasio J, Kim J, Glasheen J. Use of medications for insomnia in the hospitalized geriatric population. J Am Geriatr Soc. 2008;56(3):579-581. PubMed
16. Somers A, Robays H, Audenaert K, Van Maele G, Bogaert M, Petrovic M. The use of hypnosedative drugs in a university hospital: has anything changed in 10 years? Eur J Clin Pharmacol. 2011;67(7):723-729. PubMed
17. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
18. Frighetto L, Marra C, Bandali S, Wilbur K, Naumann T, Jewesson P. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17. PubMed
19. Garrido MM, Prigerson HG, Penrod JD, Jones SC, Boockvar KS. Benzodiazepine and sedative-hypnotic use among older seriously Ill veterans: choosing wisely? Clin Ther. 2014;36(11):1547-1554. PubMed
20. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults: The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. J Am Geriatr Soc. 2012;60(4):616-631. PubMed
21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. PubMed
22. Foy A, Drinkwater V, March S, Mearrick P. Confusion after admission to hospital in elderly patients using benzodiazepines. Br Med J (Clin Res Ed). 1986;293(6554):1072. PubMed
23. McDowell JA, Mion LC, Lydon TJ, Inouye SK. A nonpharmacologic sleep protocol for hospitalized older patients. J Am Geriatr Soc. 1998;46(6):700-705. PubMed
24. Ramaswamy R, Maio V, Diamond JJ, et al. Potentially inappropriate prescribing in elderly: assessing doctor knowledge, confidence and barriers. J Eval Clin Pract. 2011;17(6):1153-1159. PubMed
25. Lee MJ, Kim M, Kim NH, et al. Why is asymptomatic bacteriuria overtreated?: A tertiary care institutional survey of resident physicians. BMC Infect Dis. 2015;15:289. PubMed
1. Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331(7526):1169. PubMed
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165. PubMed
3. Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely--the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589-592. PubMed
4. Ten Things Physicians and Patients Should Question. American Geriatrics Society 2013. Revised April 23, 2015. http://www.choosingwisely.org/societies/american-geriatrics-society/. Accessed April 30, 2016.
5. Five Things Physicians and Patients Should Question. Canadian Geriatrics Society. Released April 2, 2014. http://www.choosingwiselycanada.org/recommendations/geriatrics/. Accessed April 30, 2016.
6. de Groot MH, van Campen JP, Moek MA, Tulner LR, Beijnen JH, Lamoth CJ. The effects of fall-risk-increasing drugs on postural control: a literature review. Drugs Aging. 2013;30(11):901-920. PubMed
7. Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952-1960. PubMed
8. Pariente A, Dartigues JF, Benichou J, Letenneur L, Moore N, Fourrier-Réglat A. Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging. 2008;25(1):61-70. PubMed
9. Frels C, Williams P, Narayanan S, Gariballa SE. Iatrogenic causes of falls in hospitalised elderly patients: a case-control study. Postgrad Med J. 2002;78(922):487-489. PubMed
10. Pavon JM, Zhao Y, McConnell E, Hastings SN. Identifying risk of readmission in hospitalized elderly adults through inpatient medication exposure. J Am Geriatr Soc. 2014;62(6):1116-1121. PubMed
11. Kang DY, Park S, Rhee CW, et al. Zolpidem use and risk of fracture in elderly insomnia patients. J Prev Med Public Health. 2012;45(4):219-226. PubMed
12. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
13. Finkle WD, Der JS, Greenland S, et al. Risk of fractures requiring hospitalization after an initial prescription for zolpidem, alprazolam, lorazepam, or diazepam in older adults. J Am Geriatr Soc. 2011;59(10):1883-1890. PubMed
14. Elliott RA, Woodward MC, Oborne CA. Improving benzodiazepine prescribing for elderly hospital inpatients using audit and multidisciplinary feedback. Intern Med J. 2001;31(9):529-535. PubMed
15. Cumbler E, Guerrasio J, Kim J, Glasheen J. Use of medications for insomnia in the hospitalized geriatric population. J Am Geriatr Soc. 2008;56(3):579-581. PubMed
16. Somers A, Robays H, Audenaert K, Van Maele G, Bogaert M, Petrovic M. The use of hypnosedative drugs in a university hospital: has anything changed in 10 years? Eur J Clin Pharmacol. 2011;67(7):723-729. PubMed
17. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
18. Frighetto L, Marra C, Bandali S, Wilbur K, Naumann T, Jewesson P. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17. PubMed
19. Garrido MM, Prigerson HG, Penrod JD, Jones SC, Boockvar KS. Benzodiazepine and sedative-hypnotic use among older seriously Ill veterans: choosing wisely? Clin Ther. 2014;36(11):1547-1554. PubMed
20. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults: The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. J Am Geriatr Soc. 2012;60(4):616-631. PubMed
21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. PubMed
22. Foy A, Drinkwater V, March S, Mearrick P. Confusion after admission to hospital in elderly patients using benzodiazepines. Br Med J (Clin Res Ed). 1986;293(6554):1072. PubMed
23. McDowell JA, Mion LC, Lydon TJ, Inouye SK. A nonpharmacologic sleep protocol for hospitalized older patients. J Am Geriatr Soc. 1998;46(6):700-705. PubMed
24. Ramaswamy R, Maio V, Diamond JJ, et al. Potentially inappropriate prescribing in elderly: assessing doctor knowledge, confidence and barriers. J Eval Clin Pract. 2011;17(6):1153-1159. PubMed
25. Lee MJ, Kim M, Kim NH, et al. Why is asymptomatic bacteriuria overtreated?: A tertiary care institutional survey of resident physicians. BMC Infect Dis. 2015;15:289. PubMed
© 2017 Society of Hospital Medicine
Catheter Use Among Teaching Hospitals
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
© 2016 Society of Hospital Medicine