User login
23rd World Congress of Dermatology
WCD: Look for TNF inhibitor–induced psoriasis in kids
VANCOUVER – Tumor necrosis factor inhibitor–induced psoriasiform dermatitis can occur in pediatric patients after any length of treatment, with documented cases emerging after the very first dose and as late as 63 months into anti-TNF therapy, Dr. Amy S. Paller said at the World Congress of Dermatology.
Histopathologically, this medication-induced condition is psoriasis. But it tends to follow a distinctive pattern, favoring the scalp, dorsal hands and feet, nails, and periorificial skin. Palmoplantar pustulosis is not uncommon. The lesions are often secondarily infected with Staphylococcus aureus, according to Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University in Chicago.
The phenomenon was first described in adults. But in the past several years, as the use of tumor necrosis factor (TNF) antagonists has gained increasing traction for treatment of pediatric inflammatory bowel disease and rheumatologic diseases, the dermatologic disorder has become better characterized in youths. In a retrospective study at McMaster Children’s Hospital in Hamilton, Ont., 17 of 172 (10%) infliximab-treated patients with Crohn’s disease developed new-onset psoriasis and another (0.6%) experienced worsening of preexisting psoriasis after anywhere from 1 to 25 infusions. Most patients responded well to topical steroids; however, three discontinued the biologic because of this complication (J Pediatr Gastroenterol Nutr. 2013 May;56[5]:512-8).
It’s now clear that the emergence of TNF inhibitor–induced psoriasis does not adversely affect the response of a patient’s inflammatory bowel disease or juvenile arthritis to the biologic. Also, the risk of recurrent psoriatic eruption is not reduced by concurrent methotrexate.
Researchers find TNF inhibitor–induced psoriasis to be an intriguing puzzle because of its paradoxical nature. After all, the TNF inhibitors are a highly effective treatment for moderate to severe plaque psoriasis. The leading theory as to the underlying basis for TNF inhibitor–induced psoriasis is that it may have a genetic basis, Dr. Paller noted.
The McMaster group found that their pediatric Crohn’s disease patients who developed psoriasis in conjunction with infliximab (Remicade) therapy were more likely than disease-matched controls to be homozygous for one of several specific polymorphisms in the interleukin-23R gene. And investigators at the University of Helsinki have reported that children with inflammatory bowel disease who developed psoriasiform dermatitis while on infliximab only rarely possessed the HLA-Cw*0602 genotype, which is commonly associated with psoriasis (Inflamm Bowel Dis. 2014 Aug;20[8]:1309-15).
The possibility of streptococcal or staphylococcal infection serving as a trigger for TNF inhibitor–induced psoriasis is also being explored, according to Dr. Paller.
She has received research funding from LEO Pharma and Amgen and serves as a consultant to AbbVie.
VANCOUVER – Tumor necrosis factor inhibitor–induced psoriasiform dermatitis can occur in pediatric patients after any length of treatment, with documented cases emerging after the very first dose and as late as 63 months into anti-TNF therapy, Dr. Amy S. Paller said at the World Congress of Dermatology.
Histopathologically, this medication-induced condition is psoriasis. But it tends to follow a distinctive pattern, favoring the scalp, dorsal hands and feet, nails, and periorificial skin. Palmoplantar pustulosis is not uncommon. The lesions are often secondarily infected with Staphylococcus aureus, according to Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University in Chicago.
The phenomenon was first described in adults. But in the past several years, as the use of tumor necrosis factor (TNF) antagonists has gained increasing traction for treatment of pediatric inflammatory bowel disease and rheumatologic diseases, the dermatologic disorder has become better characterized in youths. In a retrospective study at McMaster Children’s Hospital in Hamilton, Ont., 17 of 172 (10%) infliximab-treated patients with Crohn’s disease developed new-onset psoriasis and another (0.6%) experienced worsening of preexisting psoriasis after anywhere from 1 to 25 infusions. Most patients responded well to topical steroids; however, three discontinued the biologic because of this complication (J Pediatr Gastroenterol Nutr. 2013 May;56[5]:512-8).
It’s now clear that the emergence of TNF inhibitor–induced psoriasis does not adversely affect the response of a patient’s inflammatory bowel disease or juvenile arthritis to the biologic. Also, the risk of recurrent psoriatic eruption is not reduced by concurrent methotrexate.
Researchers find TNF inhibitor–induced psoriasis to be an intriguing puzzle because of its paradoxical nature. After all, the TNF inhibitors are a highly effective treatment for moderate to severe plaque psoriasis. The leading theory as to the underlying basis for TNF inhibitor–induced psoriasis is that it may have a genetic basis, Dr. Paller noted.
The McMaster group found that their pediatric Crohn’s disease patients who developed psoriasis in conjunction with infliximab (Remicade) therapy were more likely than disease-matched controls to be homozygous for one of several specific polymorphisms in the interleukin-23R gene. And investigators at the University of Helsinki have reported that children with inflammatory bowel disease who developed psoriasiform dermatitis while on infliximab only rarely possessed the HLA-Cw*0602 genotype, which is commonly associated with psoriasis (Inflamm Bowel Dis. 2014 Aug;20[8]:1309-15).
The possibility of streptococcal or staphylococcal infection serving as a trigger for TNF inhibitor–induced psoriasis is also being explored, according to Dr. Paller.
She has received research funding from LEO Pharma and Amgen and serves as a consultant to AbbVie.
VANCOUVER – Tumor necrosis factor inhibitor–induced psoriasiform dermatitis can occur in pediatric patients after any length of treatment, with documented cases emerging after the very first dose and as late as 63 months into anti-TNF therapy, Dr. Amy S. Paller said at the World Congress of Dermatology.
Histopathologically, this medication-induced condition is psoriasis. But it tends to follow a distinctive pattern, favoring the scalp, dorsal hands and feet, nails, and periorificial skin. Palmoplantar pustulosis is not uncommon. The lesions are often secondarily infected with Staphylococcus aureus, according to Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University in Chicago.
The phenomenon was first described in adults. But in the past several years, as the use of tumor necrosis factor (TNF) antagonists has gained increasing traction for treatment of pediatric inflammatory bowel disease and rheumatologic diseases, the dermatologic disorder has become better characterized in youths. In a retrospective study at McMaster Children’s Hospital in Hamilton, Ont., 17 of 172 (10%) infliximab-treated patients with Crohn’s disease developed new-onset psoriasis and another (0.6%) experienced worsening of preexisting psoriasis after anywhere from 1 to 25 infusions. Most patients responded well to topical steroids; however, three discontinued the biologic because of this complication (J Pediatr Gastroenterol Nutr. 2013 May;56[5]:512-8).
It’s now clear that the emergence of TNF inhibitor–induced psoriasis does not adversely affect the response of a patient’s inflammatory bowel disease or juvenile arthritis to the biologic. Also, the risk of recurrent psoriatic eruption is not reduced by concurrent methotrexate.
Researchers find TNF inhibitor–induced psoriasis to be an intriguing puzzle because of its paradoxical nature. After all, the TNF inhibitors are a highly effective treatment for moderate to severe plaque psoriasis. The leading theory as to the underlying basis for TNF inhibitor–induced psoriasis is that it may have a genetic basis, Dr. Paller noted.
The McMaster group found that their pediatric Crohn’s disease patients who developed psoriasis in conjunction with infliximab (Remicade) therapy were more likely than disease-matched controls to be homozygous for one of several specific polymorphisms in the interleukin-23R gene. And investigators at the University of Helsinki have reported that children with inflammatory bowel disease who developed psoriasiform dermatitis while on infliximab only rarely possessed the HLA-Cw*0602 genotype, which is commonly associated with psoriasis (Inflamm Bowel Dis. 2014 Aug;20[8]:1309-15).
The possibility of streptococcal or staphylococcal infection serving as a trigger for TNF inhibitor–induced psoriasis is also being explored, according to Dr. Paller.
She has received research funding from LEO Pharma and Amgen and serves as a consultant to AbbVie.
EXPERT ANALYSIS FROM WCD 2015
Nail psoriasis therapies lack supporting evidence
VANCOUVER – Evidence-based therapy for nail psoriasis is in a sorry state because of a lack of consensus on a reliable nail psoriasis scoring system for use in clinical trials, according to a coauthor of the Cochrane systematic review of interventions for nail psoriasis.
“The last 12 randomized clinical trials used 21 ways of scoring the results of treatment, so comparing the studies means comparing apples to oranges. Which is the most effective treatment? What should we advise our patients? We don’t know. Comparison is impossible,” Dr. Marcel C. Pasch said at the World Congress of Dermatology.
The Cochrane report (Cochrane Database Syst Rev. 2013 Jan 31;1:CD007633) deemed the evidence for topical therapies as “inconclusive and weak,” even though topicals are the treatment mainstay for this localized expression of psoriasis. Indeed, Dr. Pasch and his coauthors found that no topical therapy has been shown effective in improving nail psoriasis. The Cochrane group concluded that just five therapies rise to the standard of being evidence based in terms of efficacy: the tumor necrosis factor (TNF) inhibitors infliximab (Remicade) and golimumab (Simponi), superficial radiation therapy, Grenz rays, and electron beam therapy. All five are strikingly impractical for use in clinical practice.
“The findings are quite disappointing because nobody sends a patient with psoriasis to the radiotherapist, and while giving an anti-TNF biologic only for the nails will be effective, at least in my country it won’t be reimbursed,” wrote Dr. Pasch, a dermatologist at Radboud University Nijmegen (the Netherlands) Medical Centre.
The presence and severity of nail psoriasis is unrelated to the severity of cutaneous psoriasis. Moreover, nail psoriasis without cutaneous involvement occurs in 5%-10% of psoriasis patients.
Since publication of the Cochrane systematic review, 12 new randomized controlled trials of treatments for nail psoriasis have appeared. Six focused on biologics: the anti-TNF agents certolizumab (Cimzia), etanercept (Enbrel), and adalimumab (Humira); the anti–interleukin-12/23 agent ustekinumab (Stelara); and the interleukin-17A inhibitor secukiumab (Cosentyx). Dr. Pasch said in his opinion all five biologics were supported by convincing studies and now can be added to the short list of evidence-based nail psoriasis therapies.
Of the six recent studies of topical therapies, two provided persuasive evidence of efficacy, in his view: tacrolimus ointment and indigo naturalis extract in oil (Lindioil), a variant of a traditional Chinese medicine therapy, which at this time isn’t commercially available.
In contrast, studies of clobetasol nail lacquer, pulsed dye laser therapy, a nail lacquer based upon chitin from crab shells, and a study of calcitriol ointment versus betamethasone dipropionate ointment failed to be convincing either because of methodologic problems or lack of efficacy, he continued.
These 12 recent randomized clinical trials utilized 21 different nail psoriasis scoring systems.
“Which scoring system is best? The answer is, we don’t know,” Dr. Pasch said.
He and his coinvestigators compared eight different scoring systems in a prospective study and concluded that the Nijmegen–Nail Psoriasis Activity Index Tool (N-NAIL), which Dr. Pasch helped develop, best reflected the clinical severity of nail psoriasis (J Am Acad Dermatol. 2014 Jun;70[6]:1061-6).
However, he added that at present there is no validated scoring system for nail psoriasis. And creation of a single validated scoring system that researchers can agree on as the standard is a prerequisite for making major advances in the treatment of nail psoriasis, in Dr. Pasch’s view.
He is so convinced of this that he has created an organization whose goal is to achieve consensus on one reliable, validated nail psoriasis scoring system for use in clinical trials. At the World Congress of Dermatology, he invited stakeholders – including academic and community dermatologists, patient organizations, and the pharmaceutical industry – to join (www.nailinitiative.org).
Session chair Dr. Peter van de Kerkhof, chairman of dermatology at Radboud University, said he sees the NAPSI (Nail Psoriasis Severity Index) being used in lots of clinical trials in psoriasis. What’s wrong with building a consensus around NAPSI? he asked.
“The problem is not the NAPSI score,” Dr. Pasch replied. “The problem is that in each trial a modified NAPSI score is used, but they are all modified in different ways. We have the single-hand NAPSI, the eight-finger NAPSI, the 10-finger NAPSI, the target NAPSI. The NAPSI doesn’t exist anymore.”
He reported receiving research grants from Pfizer and Janssen-Cilag.
VANCOUVER – Evidence-based therapy for nail psoriasis is in a sorry state because of a lack of consensus on a reliable nail psoriasis scoring system for use in clinical trials, according to a coauthor of the Cochrane systematic review of interventions for nail psoriasis.
“The last 12 randomized clinical trials used 21 ways of scoring the results of treatment, so comparing the studies means comparing apples to oranges. Which is the most effective treatment? What should we advise our patients? We don’t know. Comparison is impossible,” Dr. Marcel C. Pasch said at the World Congress of Dermatology.
The Cochrane report (Cochrane Database Syst Rev. 2013 Jan 31;1:CD007633) deemed the evidence for topical therapies as “inconclusive and weak,” even though topicals are the treatment mainstay for this localized expression of psoriasis. Indeed, Dr. Pasch and his coauthors found that no topical therapy has been shown effective in improving nail psoriasis. The Cochrane group concluded that just five therapies rise to the standard of being evidence based in terms of efficacy: the tumor necrosis factor (TNF) inhibitors infliximab (Remicade) and golimumab (Simponi), superficial radiation therapy, Grenz rays, and electron beam therapy. All five are strikingly impractical for use in clinical practice.
“The findings are quite disappointing because nobody sends a patient with psoriasis to the radiotherapist, and while giving an anti-TNF biologic only for the nails will be effective, at least in my country it won’t be reimbursed,” wrote Dr. Pasch, a dermatologist at Radboud University Nijmegen (the Netherlands) Medical Centre.
The presence and severity of nail psoriasis is unrelated to the severity of cutaneous psoriasis. Moreover, nail psoriasis without cutaneous involvement occurs in 5%-10% of psoriasis patients.
Since publication of the Cochrane systematic review, 12 new randomized controlled trials of treatments for nail psoriasis have appeared. Six focused on biologics: the anti-TNF agents certolizumab (Cimzia), etanercept (Enbrel), and adalimumab (Humira); the anti–interleukin-12/23 agent ustekinumab (Stelara); and the interleukin-17A inhibitor secukiumab (Cosentyx). Dr. Pasch said in his opinion all five biologics were supported by convincing studies and now can be added to the short list of evidence-based nail psoriasis therapies.
Of the six recent studies of topical therapies, two provided persuasive evidence of efficacy, in his view: tacrolimus ointment and indigo naturalis extract in oil (Lindioil), a variant of a traditional Chinese medicine therapy, which at this time isn’t commercially available.
In contrast, studies of clobetasol nail lacquer, pulsed dye laser therapy, a nail lacquer based upon chitin from crab shells, and a study of calcitriol ointment versus betamethasone dipropionate ointment failed to be convincing either because of methodologic problems or lack of efficacy, he continued.
These 12 recent randomized clinical trials utilized 21 different nail psoriasis scoring systems.
“Which scoring system is best? The answer is, we don’t know,” Dr. Pasch said.
He and his coinvestigators compared eight different scoring systems in a prospective study and concluded that the Nijmegen–Nail Psoriasis Activity Index Tool (N-NAIL), which Dr. Pasch helped develop, best reflected the clinical severity of nail psoriasis (J Am Acad Dermatol. 2014 Jun;70[6]:1061-6).
However, he added that at present there is no validated scoring system for nail psoriasis. And creation of a single validated scoring system that researchers can agree on as the standard is a prerequisite for making major advances in the treatment of nail psoriasis, in Dr. Pasch’s view.
He is so convinced of this that he has created an organization whose goal is to achieve consensus on one reliable, validated nail psoriasis scoring system for use in clinical trials. At the World Congress of Dermatology, he invited stakeholders – including academic and community dermatologists, patient organizations, and the pharmaceutical industry – to join (www.nailinitiative.org).
Session chair Dr. Peter van de Kerkhof, chairman of dermatology at Radboud University, said he sees the NAPSI (Nail Psoriasis Severity Index) being used in lots of clinical trials in psoriasis. What’s wrong with building a consensus around NAPSI? he asked.
“The problem is not the NAPSI score,” Dr. Pasch replied. “The problem is that in each trial a modified NAPSI score is used, but they are all modified in different ways. We have the single-hand NAPSI, the eight-finger NAPSI, the 10-finger NAPSI, the target NAPSI. The NAPSI doesn’t exist anymore.”
He reported receiving research grants from Pfizer and Janssen-Cilag.
VANCOUVER – Evidence-based therapy for nail psoriasis is in a sorry state because of a lack of consensus on a reliable nail psoriasis scoring system for use in clinical trials, according to a coauthor of the Cochrane systematic review of interventions for nail psoriasis.
“The last 12 randomized clinical trials used 21 ways of scoring the results of treatment, so comparing the studies means comparing apples to oranges. Which is the most effective treatment? What should we advise our patients? We don’t know. Comparison is impossible,” Dr. Marcel C. Pasch said at the World Congress of Dermatology.
The Cochrane report (Cochrane Database Syst Rev. 2013 Jan 31;1:CD007633) deemed the evidence for topical therapies as “inconclusive and weak,” even though topicals are the treatment mainstay for this localized expression of psoriasis. Indeed, Dr. Pasch and his coauthors found that no topical therapy has been shown effective in improving nail psoriasis. The Cochrane group concluded that just five therapies rise to the standard of being evidence based in terms of efficacy: the tumor necrosis factor (TNF) inhibitors infliximab (Remicade) and golimumab (Simponi), superficial radiation therapy, Grenz rays, and electron beam therapy. All five are strikingly impractical for use in clinical practice.
“The findings are quite disappointing because nobody sends a patient with psoriasis to the radiotherapist, and while giving an anti-TNF biologic only for the nails will be effective, at least in my country it won’t be reimbursed,” wrote Dr. Pasch, a dermatologist at Radboud University Nijmegen (the Netherlands) Medical Centre.
The presence and severity of nail psoriasis is unrelated to the severity of cutaneous psoriasis. Moreover, nail psoriasis without cutaneous involvement occurs in 5%-10% of psoriasis patients.
Since publication of the Cochrane systematic review, 12 new randomized controlled trials of treatments for nail psoriasis have appeared. Six focused on biologics: the anti-TNF agents certolizumab (Cimzia), etanercept (Enbrel), and adalimumab (Humira); the anti–interleukin-12/23 agent ustekinumab (Stelara); and the interleukin-17A inhibitor secukiumab (Cosentyx). Dr. Pasch said in his opinion all five biologics were supported by convincing studies and now can be added to the short list of evidence-based nail psoriasis therapies.
Of the six recent studies of topical therapies, two provided persuasive evidence of efficacy, in his view: tacrolimus ointment and indigo naturalis extract in oil (Lindioil), a variant of a traditional Chinese medicine therapy, which at this time isn’t commercially available.
In contrast, studies of clobetasol nail lacquer, pulsed dye laser therapy, a nail lacquer based upon chitin from crab shells, and a study of calcitriol ointment versus betamethasone dipropionate ointment failed to be convincing either because of methodologic problems or lack of efficacy, he continued.
These 12 recent randomized clinical trials utilized 21 different nail psoriasis scoring systems.
“Which scoring system is best? The answer is, we don’t know,” Dr. Pasch said.
He and his coinvestigators compared eight different scoring systems in a prospective study and concluded that the Nijmegen–Nail Psoriasis Activity Index Tool (N-NAIL), which Dr. Pasch helped develop, best reflected the clinical severity of nail psoriasis (J Am Acad Dermatol. 2014 Jun;70[6]:1061-6).
However, he added that at present there is no validated scoring system for nail psoriasis. And creation of a single validated scoring system that researchers can agree on as the standard is a prerequisite for making major advances in the treatment of nail psoriasis, in Dr. Pasch’s view.
He is so convinced of this that he has created an organization whose goal is to achieve consensus on one reliable, validated nail psoriasis scoring system for use in clinical trials. At the World Congress of Dermatology, he invited stakeholders – including academic and community dermatologists, patient organizations, and the pharmaceutical industry – to join (www.nailinitiative.org).
Session chair Dr. Peter van de Kerkhof, chairman of dermatology at Radboud University, said he sees the NAPSI (Nail Psoriasis Severity Index) being used in lots of clinical trials in psoriasis. What’s wrong with building a consensus around NAPSI? he asked.
“The problem is not the NAPSI score,” Dr. Pasch replied. “The problem is that in each trial a modified NAPSI score is used, but they are all modified in different ways. We have the single-hand NAPSI, the eight-finger NAPSI, the 10-finger NAPSI, the target NAPSI. The NAPSI doesn’t exist anymore.”
He reported receiving research grants from Pfizer and Janssen-Cilag.
EXPERT ANALYSIS FROM WCD 2015
In Diabetic Foot Ulcers, Use 50% Rule to Gauge Need for Advanced Therapies
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
In diabetic foot ulcers, use 50% rule to gauge need for advanced therapies
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – When diabetic foot ulcer healing has stalled despite 4 weeks of optimal standard therapy, it’s time to seriously consider resorting to advanced therapies, according to Dr. Afsaneh Alavi of the University of Toronto.
Advanced therapy options include negative pressure wound therapy, hyperbaric oxygen, artificial skin substitutes, growth factors, collagen-based dressings, and electromagnetic therapy.
“You hear a lot about advanced therapy for diabetic foot ulcers. It’s expensive. But it can be cost-effective if used properly. It’s our duty to see who is the best person to receive this therapy,” she said at the World Congress of Dermatology.
A useful rule of thumb, the dermatologist added, is that if a healable ulcer isn’t 50% smaller at week 4 despite optimal care, it’s time to consider moving on to advanced therapies. As was shown in a well-conducted, 203-patient, randomized, prospective controlled clinical trial, a wound that hasn’t met that threshold is unlikely to be healed at 12 weeks (Diabetes Care. 2003 Jun;26(6):1879-82).
Two caveats: advanced therapy is appropriate only for healable diabetic foot ulcers, meaning those in patients with adequate peripheral circulation as defined by measurements of transcutaneous oxygen pressure, toe pressure brachial index, and Doppler studies.
“Eighty percent of diabetic patients have noncompressible arteries and therefore the ankle brachial index is not an accurate test to evaluate their circulation,” according to Dr. Avali.
The other caveat regarding advanced therapy is that appropriate candidates should have a wound edge that’s sharp, not migrating, she continued.
The 4-week cutoff for seeing substantial progress in wound healing with standard therapy before turning to advanced therapies is based in part upon an influential study of 2,517 patients with diabetic neuropathic foot ulcers who received one of three advanced biological therapies. On average, patients started advanced biological therapy within 28 days following their first visit to a specialized wound clinic. Prolonged time to initiation of advanced treatment was associated with significantly longer time to healing (Arch Dermatol. 2010 Aug;146(8):857-62).
While thinking about local wound care in a patient with a diabetic foot ulcer, Dr. Avali said it’s also important to take a step back and make sure hypertension and other conventional cardiovascular risk factors are well controlled and also to take a close look at the HbA1c. In a study of 183 patients with diabetic wounds treated at a specialized academic wound center, for every 1.0% increase in HbA1c above the mean level of 8.0%, the wound-area healing rate was reduced by 0.028 cm2 per day. The implication is that HbA1c may be a key biomarker that’s useful in predicting wound-healing rate in patients with diabetic ulcers (J. Invest Dermatol. 2011 Oct;131(10):2121-7).
She reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
Offloading is key to diabetic foot ulcer management
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
VANCOUVER – Offloading of plantar pressures is the key component of successful management of plantar diabetic foot ulcers, Dr. Afsaneh Alavi asserted at the World Congress of Dermatology.
“Debridement to remove the callous is the most important part of local wound care, but debridement without offloading afterwards will rebuild callous,” explained Dr. Alavi, a University of Toronto dermatologist.
Many options exist in terms of offloading devices. The total contact cast is recognized as the gold standard. It reduces pressures by 90%. Yet a national survey of more than 900 foot clinics found that less than 2% of centers utilized total contact casts for the majority of their patients with plantar diabetic foot ulcers. Only 15% of centers utilized another highly effective option, the removable cast walker, in the majority of patients (Diabetes Care. 2008 Nov; 31(11): 2118–2119). Cost is believed to be a major issue. Other options include custom orthotic inserts and forefoot and heel relief shoes.
The diabetic foot ulcer recurrence rate is extremely high: up to 83% within the first year.
“Counsel patients to use therapeutic shoes and insoles, engage in self-inspection, and get professional foot care. Shoes should be worn at all times, even in the house. Patients typically spend 30%-40% of their time at home,” Dr. Alavi continued.
The pathophysiology of diabetic foot ulcers is a vicious circle of immunopathy, neuropathy, and angiopathy. Callous formation secondary to sensory and motor neuropathy leads to subcutaneous bleeding, ulcer formation, and deeper infection, sometimes with life- or limb-threatening osteomyelitis.
“Detection of this chain of events at the stage of callous formation would make a huge difference,” according to the dermatologist. She pointed out that “Most of our health care system is focused more on management than prevention. We spend more on amputations due to diabetic foot ulcers than for prevention.”
Although many methods of callous removal are available, including autolytic therapy with hydrogels, whirlpools, and wet-to-dry dressings, Dr. Alavi said the best method is sharp surgical debridement. She highlighted a retrospective 12-week study of topical wound treatments in 310 diabetic foot ulcers and 366 chronic venous leg ulcers which found that venous leg ulcers showed a 34% greater median wound surface area reduction following office visits with surgical debridement compared with no surgical debridement. Serial surgical debridement in patients with diabetic foot ulcers was also associated with a 2.35-fold increased likelihood of wound closure (Wound Repair Regen. 2009 May-June;17(3):306-11).
She noted that it has been estimated that by 2030, at least 10% of the world’s adult population -- some 550 million people -- will have diabetes. And a diabetic individual’s lifetime risk of developing diabetic foot ulcers is up to 25%. The 5-year mortality rate following amputation related to a diabetic foot ulcer is nearly 50%, about the same as following diagnosis of colon cancer.
Dr. Alavi reported serving as a consultant to Acelity and Smith & Nephew.
EXPERT ANALYSIS FROM WCD 2015
Fungal foot infections risk secondary infection in diabetic patients
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
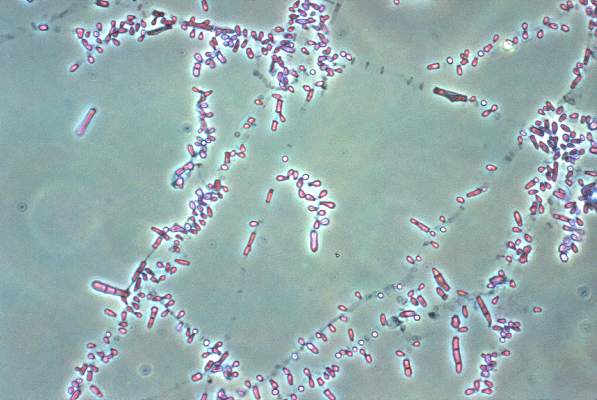
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
SVELT uses small amounts of fat for breast augmentation
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
EXPERT ANALYSIS FROM WCD 2015
Nail surgery: Top anesthesia tips
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
Beware of Skin Complications of Newer Antidiabetic Agents
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM WCD 2015
Beware of skin complications of newer antidiabetic agents
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM WCD 2015