User login
How not to miss the ‘invisible gorilla’: Visual intelligence in dermatology
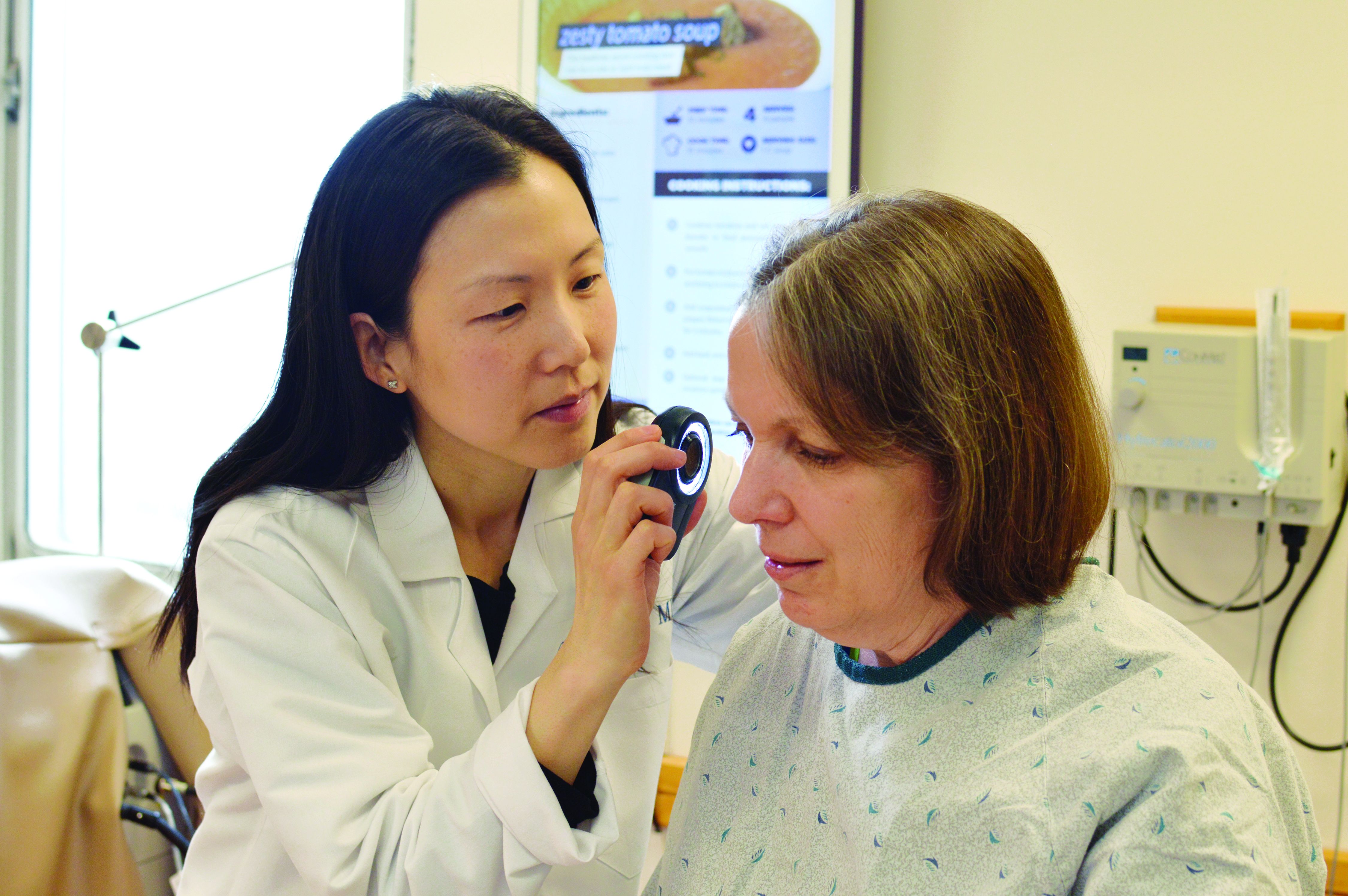
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
CHICAGO – Medicine, perhaps uniquely among the highly skilled professions, requires the practitioner to use his or her senses on a daily basis. Dermatologists and dermatopathologists rely on visual skills – pattern recognition, gestalt or “gut” first impressions, and step-by-step deliberations – to care for their patients.
But, like all human cognitive processes, visual assessments are error prone. The same brains that can parse a field of blue and pink dots to discern melanoma on a slide are also capable of glaring errors of omission: All too often, the brain follows a cognitive path for the wrong reasons.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., became interested in the meta-cognition of her trade; that is, she sought to learn how to think about the thinking that’s needed to be a dermatologist or a dermatopathologist.
In a wide-ranging discussion at the summer meeting of the American Academy of Dermatology, Dr. Ko took attendees through The path led through lessons learned from cognitive science to the fine arts, to lessons learned from other visually oriented medical disciplines.
“Deliberate practice in dermatology is augmented by knowledge of specific cognitive principles that affect visual perception,” Dr. Ko said at the meeting. “This session will open your eyes to the world of visual intelligence that underlies expert dermatologic diagnosis.”
To begin with, what constitutes deliberate practice of dermatology or dermatopathology? Practically speaking, seeing many patients (or reading many slides) builds the base for true expertise, she noted. Physicians continue to hone their learning through independent reading, journal clubs, and meeting attendance, and seek opportunities for deliberate review of what’s still unknown, as in grand rounds – where, ideally, feedback is instantaneous.
Deliberate practice, though, should also include honing visual skills. “We find only the world we look for,” said Dr. Ko, quoting Henry David Thoreau. To sharpen the pattern recognition and keen observation that underpin dermatology and dermatopathology, she said, “We can train the brain.”
Radiology, another medical discipline that requires sustained visual attention, has a significant body of literature addressing common visually-related cognitive errors, she pointed out. In radiology, it’s been shown that deliberate observation of visual art can improve accuracy of reading films.
She observed that dermatologists and dermatopathologists need to think in color, so they may need to develop slightly different visual skills from radiologists who largely see a gray-scale world while they’re working.
Cognitive psychology also offers lessons. One seminal paper, “The invisible gorilla strikes again: Sustained inattentional blindness in expert observers,” issues a stern admonition: “[A] high level of expertise does not immunize individuals against inherent limitations of human attention imperception” (Psychol Sci. 2013 Sep;24[9]:1848-53). Inattentional blindness, Dr. Ko explained, occurs when “what we are focused on filters the world around us aggressively.” First author Trafton Drew, PhD, and his colleagues added: “Researchers should seek better understanding of these limits, so that medical and other man-made search tasks could be designed in ways that reduce the consequences of these limitations.”
How to overcome these limitations? “Concentrate on the camouflaged,” said Dr. Ko, taking a page – literally – from “Visual Intelligence: Sharpen Your Perception, Change Your Life” (Houghton Mifflin Harcourt, 2016), a book by Amy Herman, JD. Ms. Herman devised the mnemonic “COBRA” to identify several steps that can prevent cognitive error from visual observation:
- Concentrating on the camouflaged, for dermatologists, might mean just looking again and focusing on the less-obvious. But, Dr. Ko said, it might mean turning your attention elsewhere for a while, and then looking back at the area in question. Or the patient or slide – or even the examiner – might need repositioning, for a fresh perspective.
- Taking One thing at a time. For dermatologists and dermatopathologists, this means sorting out the who, what, when, and where of the problem at hand. “ ‘Who’ is always the patient,” said Dr. Ko. “But part of ‘who’ is also us; if we’re tired, it can affect things.” There are many ‘whats’ to consider about the presenting problem or the tissue sample: What is the configuration? The architecture? What is the morphology? What’s the color, or cell type? Are there secondary changes? Does the tissue fit into the general category of a benign, or a malignant, lesion? The examination should include a methodical search for clues as to the duration of the problem – Is it acute or chronic? Finally, the ‘where’ – distribution on the body, or of a specimen on a slide, should also be noted.
- Take a Break. This means resting the eye and the mind by turning attention elsewhere, or shifting to light conversation with the patient, or just stepping away from the microscope for a time.
- Realign your expectations. What might you have missed? Is the patient telling you something in the history? Is it possible this is an uncommon presentation of a common condition, rather than a “zebra”?
- Ask someone else to look with you. Sometimes there’s no substitute for another set of eyes, and another brain working on the problem.
A congruent perspective comes from Daniel Kahneman, PhD, a Nobel Prize–winning economist. In 2011, he published a work addressing meta-cognition, called “Thinking Fast and Slow.”
From Dr. Kahneman’s work, Dr. Ko says dermatologists can learn to recognize two complementary ways of thinking. The “fast” system engages multiple cognitive processes to create a gestalt, “gut” impression. “Slow” thinking, in Dr. Kahneman’s construct, is deliberative, methodical, and traditionally thought of as “logical.” However, it would be a mistake to think of these two systems as existing in opposition, or even as completely separate from each other. “It’s sort of just a linguistic tool for us to have something to call it,” she said.
A “fast” analysis will involve some key elements of visual assessment, said Dr. Ko. Figure-ground separation is a basic element of visual assessment and is vital for the work of the dermatopathologist. “Choosing the wrong ‘figure’ may lead to cognitive error,” she explained, citing work on visual perception among dermatopathologists that found that figure-ground separation errors account for a significant number of diagnostic errors.
Other contributors to “fast” thinking include one’s own experience, seeing just a part of the image, judging which elements are close to each other and similar, and noting color contrasts and gradations.
The “slow” assessment is where deliberate practice comes in, said Dr. Ko. Here, the physician goes further, “to check for pertinent positive and negative evidence” for the initial diagnosis. “Play devil’s advocate, and ask yourself why it couldn’t be something else,” she said.
Eve Lowenstein, MD, PhD, is a dermatologist who publishes about heuristics in dermatology. She and Dr. Ko have collaborated to create a forthcoming two-part continuing medical education article in the Journal of the American Academy of Dermatology (JAAD) about cognitive biases and errors in dermatology.
Dr. Lowenstein’s perspective, recently elucidated in two British Journal of Dermatology articles, acknowledges that while “ubiquitous cognitive and visual heuristics can enhance diagnostic speed, they also create pitfalls and thinking traps that introduce significant variation in the diagnostic process,” she and her coauthor Richard Sidlow, MD, of Staten Island (N.Y.) University Hospital, wrote in the abstract accompanying the first article (Br J Dermatol. 2018 Dec;179[6]:1263-9). The second article was published in the same issue (Br J Dermatol. 2018 Dec;179[6]:1270-6).
Heuristics are cognitive shortcuts used to speed decision-making that build on what’s already known, as in the “fast” thinking of Dr. Kahneman’s paradigm. Though heuristics are used in all sorts of professions with high cognitive loads, there’s a risk when physicians get too comfortable with the shortcuts. Speaking frankly in an interview, Dr. Lowenstein said, “intellectual presumptiveness or overconfidence, which is a natural human tendency, can result in oversights and missing information critical to making a correct diagnosis, and premature closure on the wrong diagnosis.”
Diagnostic error, Dr. Lowenstein pointed out, can also result from an “attitudinal overconfidence,” which can come from complacency – being satisfied with the status quo or a lack of intellectual curiosity – or arrogance, she said.
“Complacency is the opposite of what is needed in medicine: an attitude where one cannot know enough. The pursuit of knowledge goes on, ever vigilantly. The world changes; practitioners must keep up and cannot fall back on their knowledge,” she said.
This kind of attitudinal and cognitive humility, she said, is essential to practicing quality care in dermatology. Having practical strategies to improve diagnosis, especially in difficult cases, can make a big difference. For Dr. Lowenstein, one of these tactics is to keep an error diary. “It has been said that ‘the only way to safeguard against error is to embrace it,’ ” she said, quoting Kathryn Schulz in “Being Wrong.” “Unfortunately, we learn some of our most profound lessons from our errors.”
By recording and tracking her own errors, not only is she able to see her own cognitive blind spots through meta-cognition – thinking about how we think – but she’s also able to share these lessons in her teaching. “Some of my best teaching tools for residents are from everything I have screwed up,” said Dr. Lowenstein, director of medical dermatology at the State University of New York Downstate Medical Center and Kings County Hospital, Brooklyn, N.Y.
Another useful tip is simply “to put what you see into words,” when the presentation is confusing or the diagnosis doesn’t quite fit, she added.
“Transforming signs and findings into semantics triggers a differential diagnosis, which is especially useful when we are diagnostically stumped. Studies have found that successful diagnosticians use twice as many semantic qualifiers as the physicians who were diagnostically incorrect.” This is especially significant in visual fields like dermatology, where a single word can paint a picture and rapidly focus a diagnostic search. “We often undervalue this function and relegate it to students starting out in the field,” Dr. Lowenstein said.
Cognitive shortcuts such as diagnostic heuristics all have blind spots, and diagnostic errors tend to fall in these blind spots, she added. “We tend to ignore them. In driving, we adapt to the use of rear and side view mirrors in order to drive safely. Similarly, in diagnostics, alternative views on the data can be very helpful. For example, when faced with difficult cases, take a time out to reanalyze the information without framing or context. Use systematic approaches, such as running down a papulosquamous differential diagnosis. Ask yourself: What can’t be explained in the picture? What doesn’t fit? Think in terms of probabilities – a rare presentation of a common disease is more likely than a rare disease,” she said.
Finally, asking for advice or second opinions from peers, whether by face-to-face discussion or via an online chat site, within the department or appealing to broader groups such as hospitalist dermatologist chat groups, can be helpful with difficult cases. Another strategy is simply to email an expert. Dr. Lowenstein said she’s had great success reaching out to authors of relevant papers by email. Most of her peers, she said, are interested in unusual cases and happy to help.
Dr. Ko has authored or coauthored books on the topics of visual recognition in dermatology and dermatopathology. They are “Dermatology: Visual Recognition and Case Reviews,” and “Dermatopathology: Diagnosis by First Impression.” Dr. Lowenstein reported that she has no conflicts of interest.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Consider different etiologies in patients with vaginal pruritus
CHICAGO – Diagnosing the cause of vaginal itching, which can have a significant negative impact on a woman’s quality of life, can be particularly difficult for multiple reasons, according to Rachel Kornik, MD, of the departments of dermatology and obstetrics and gynecology at the University of Wisconsin, Madison.
“The anatomy is really challenging in this area, and there’s a broad differential. Often there’s more than one thing happening,” Dr. Kornik said during a session on diagnosing and managing genital pruritus in women at the American Academy of Dermatology summer meeting. Like hair loss, vaginal pruritus is also very emotionally distressing.
“Patients are very anxious when they have all this itching,” she said. “It has an impact on personal relationships. Some patients find it difficult to talk about because it’s a taboo subject, so we have to make them comfortable.”
Dr. Kornik showed a chart of the inflammatory, neoplastic, infections, infestations, environmental, neuropathic, and hormonal. But she focused her presentation primarily on the most common causes: contact dermatitis, lichen sclerosus, and lichen simplex chronicus.
Contact dermatitis
The most common factors that contribute to contact dermatitis are friction, hygiene practices, unique body exposures (such as body fluids and menstrual and personal care products), and occlusion/maceration, which facilitates penetration of external agents. Estrogen deficiency may also play a role.
Taking a thorough history from the patient is key to finding out possible causes. Dr. Kornik provided a list of common irritants to consider.
- Hygiene-related irritants, such as frequent washing and the use of soaps, wash cloths, loofahs, wipes, bath oil, bubbles, and water.
- Laundry products, such as fabric softeners or dryer sheets.
- Menstrual products, such as panty liners, pads, and scents or additives for retaining moisture.
- Over-the-counter itch products, such as those containing benzocaine.
- Medications, such as alcohol-based creams and gels, trichloroacetic acid, fluorouracil (Efudex), imiquimod, and topical antifungals.
- Heat-related irritants, such as use of hair dryers and heating pads.
- Body fluids, including urine, feces, menstrual blood, sweat, semen, and excessive discharge.
It’s also important to consider whether there is an allergic cause. “Contact dermatitis and allergic dermatitis can look very similar both clinically and histologically, and patients can even have them both at the same time,” Dr. Kornik said. “So really, patch testing is essential sometimes to identify a true allergic contact dermatitis.”
She cited a study that identified the top five most common allergens as fragrance mixes, balsam of Peru, benzocaine, terconazole, and quaternium-15 (a formaldehyde-releasing preservative) (Dermatitis. 2013 Mar-Apr;24(2):64-72).
“If somebody’s coming into your office and they have vulvar itching for any reason, the No. 1 thing is making sure that they eliminate and not use any products with fragrances,” Dr. Kornik said. “It’s also important to note that over time, industries’ use of preservatives does change, the concentrations change, and so we may see more emerging allergens or different ones over time.”
The causative allergens are rarely consumed orally, but they may be ectopic, such as shampoo or nail polish.
“What I’ve learned over the years in treating patients with vulvar itching is that they don’t always think to tell you about everything they are applying,” Dr. Kornik said. “You have to ask specific questions. Are you using any wipes or using any lubricants? What is the type and brand of menstrual pad you’re using?”
Patients might also think they can eliminate the cause of irritation by changing products, but “there are cross reactants in many preservatives and fragrances in many products, so they might not eliminate exposure, and intermittent exposures can lead to chronic dermatitis,” she pointed out.
One example is wipes: Some women may use them only periodically, such as after a yoga class, and not think of this as a possibility or realize that wipes could perpetuate chronic dermatitis.
Research has also found that it’s very common for patients with allergic contact dermatitis to have a concomitant vulvar diagnosis. In one study, more than half of patients had another condition, the most common of which was lichen sclerosus. Others included simplex chronicus, atopic dermatitis, condyloma acuminatum, psoriasis, and Paget disease.
Therefore, if patients are not responding as expected, it’s important to consider that the condition is multifactorial “and consider allergic contact dermatitis in addition to whatever other underlying dermatosis they have,” Dr. Kornik said.
Lichen sclerosus
Prevalence of the scarring disorder lichen sclerosus ranges from 1.7% to 3% in the research literature and pathogenesis is likely multifactorial.
“It’s a very frustrating condition for patients and for physicians because we don’t know exactly what causes it, but it definitely has a predilection for the vulva area, and it affects women of all ages,” she said. “I also think it’s more common than we think.”
Loss of normal anatomical structures are a key feature, so physicians need to know their anatomy well to look for what’s not there. Lichen sclerosus involves modified mucous membranes and the perianal area, and it may spread to the crural folds and upper thighs. Symptoms can include periclitoral edema, white patches, pale skin, textural changes (such as wrinkling, waxiness, or hyperkeratosis), fissures, melanosis, and sometimes ulcerations or erosions from scratching.
There is no standardized treatment for lichen sclerosus. Research suggests using a high potency topical steroid treatment daily until skin texture normalizes, which can take anywhere from 6 weeks to 5 months, depending on severity, Dr. Kornik said. Few data are available for management if topical steroids do not work, she added.*
If dealing with recalcitrant disease, she recommends first checking the patients’ compliance and then considering alternative diagnoses or secondary conditions. Do patch testing, rule out contact dermatitis, and rebiopsy if needed. Other options are to add tacrolimus ointment, offer intralesional triamcinolone, consider a systemic agent (acitretin, methotrexate, or possibly hydroxychloroquine), or try laser or photodynamic therapy. She emphasizes the importance of demonstrating to the patient where to apply ointment, since they may not be applying to the right areas.*
Lichen simplex chronicus
Lichen simplex chronicus is a clinical description of the result of chronic rubbing and scratching. It might be triggered by something that has now resolved or be linked to other itching conditions, but clinicians need to consider the possibility of neuropathic itch as well.
Features of lichen simplex chronicus can include bilateral or unilateral involvement of the labia majora, erythematous plaques with lichenification, hyper- or hypopigmentation, or angulated excoriations and hypertrophy of labia caused by thickened skin, though the signs may be subtle, she said.
Treatment requires management of the skin problem itself – the underlying cause of the itch – as well as the behavioral component. Topical steroids are first line, plus an antihistamine at night as needed to stop the scratching. If those are insufficient, the next treatments to consider are intralesional triamcinolone (Kenalog), tacrolimus ointment, topical or oral doxepin, mirtazapine, or even selective serotonin reuptake inhibitors.
Women using topical steroids should also be aware of the possible side effects, including atrophy, infections, and allergic contact dermatitis if the steroid itself or the cream it’s in is an allergen. If stinging or burning occurs, switch to a steroid without propylene glycol, she added.
If no changes occur in the skin, clinicians may have to consider the existence of neuropathic pruritus diagnosis, an injury or dysfunction along the afferent itch pathway. Burning is more common with this neuropathy, but itching can occur too.
Other issues include symptoms that worsen with sitting and pain that worsens throughout the day. Causes can include childbirth, surgery, pelvic trauma, infection, and chemoradiation, and diagnosis requires imaging to rule out other possible causes. Treatment involves pelvic floor physical therapy, pudendal nerve block, or gabapentin.
Dr. Kornik wrapped up with a reminder that vulvar itch is often multifactorial, so clinicians need to chip away at the potential causes – sometimes with cultures, scrapes, and biopsies as needed.
She reported no financial disclosures.
Correction, 10/26/18: Dr. Kornik's treatment recommendations for lichen sclerosus were misstated.
CHICAGO – Diagnosing the cause of vaginal itching, which can have a significant negative impact on a woman’s quality of life, can be particularly difficult for multiple reasons, according to Rachel Kornik, MD, of the departments of dermatology and obstetrics and gynecology at the University of Wisconsin, Madison.
“The anatomy is really challenging in this area, and there’s a broad differential. Often there’s more than one thing happening,” Dr. Kornik said during a session on diagnosing and managing genital pruritus in women at the American Academy of Dermatology summer meeting. Like hair loss, vaginal pruritus is also very emotionally distressing.
“Patients are very anxious when they have all this itching,” she said. “It has an impact on personal relationships. Some patients find it difficult to talk about because it’s a taboo subject, so we have to make them comfortable.”
Dr. Kornik showed a chart of the inflammatory, neoplastic, infections, infestations, environmental, neuropathic, and hormonal. But she focused her presentation primarily on the most common causes: contact dermatitis, lichen sclerosus, and lichen simplex chronicus.
Contact dermatitis
The most common factors that contribute to contact dermatitis are friction, hygiene practices, unique body exposures (such as body fluids and menstrual and personal care products), and occlusion/maceration, which facilitates penetration of external agents. Estrogen deficiency may also play a role.
Taking a thorough history from the patient is key to finding out possible causes. Dr. Kornik provided a list of common irritants to consider.
- Hygiene-related irritants, such as frequent washing and the use of soaps, wash cloths, loofahs, wipes, bath oil, bubbles, and water.
- Laundry products, such as fabric softeners or dryer sheets.
- Menstrual products, such as panty liners, pads, and scents or additives for retaining moisture.
- Over-the-counter itch products, such as those containing benzocaine.
- Medications, such as alcohol-based creams and gels, trichloroacetic acid, fluorouracil (Efudex), imiquimod, and topical antifungals.
- Heat-related irritants, such as use of hair dryers and heating pads.
- Body fluids, including urine, feces, menstrual blood, sweat, semen, and excessive discharge.
It’s also important to consider whether there is an allergic cause. “Contact dermatitis and allergic dermatitis can look very similar both clinically and histologically, and patients can even have them both at the same time,” Dr. Kornik said. “So really, patch testing is essential sometimes to identify a true allergic contact dermatitis.”
She cited a study that identified the top five most common allergens as fragrance mixes, balsam of Peru, benzocaine, terconazole, and quaternium-15 (a formaldehyde-releasing preservative) (Dermatitis. 2013 Mar-Apr;24(2):64-72).
“If somebody’s coming into your office and they have vulvar itching for any reason, the No. 1 thing is making sure that they eliminate and not use any products with fragrances,” Dr. Kornik said. “It’s also important to note that over time, industries’ use of preservatives does change, the concentrations change, and so we may see more emerging allergens or different ones over time.”
The causative allergens are rarely consumed orally, but they may be ectopic, such as shampoo or nail polish.
“What I’ve learned over the years in treating patients with vulvar itching is that they don’t always think to tell you about everything they are applying,” Dr. Kornik said. “You have to ask specific questions. Are you using any wipes or using any lubricants? What is the type and brand of menstrual pad you’re using?”
Patients might also think they can eliminate the cause of irritation by changing products, but “there are cross reactants in many preservatives and fragrances in many products, so they might not eliminate exposure, and intermittent exposures can lead to chronic dermatitis,” she pointed out.
One example is wipes: Some women may use them only periodically, such as after a yoga class, and not think of this as a possibility or realize that wipes could perpetuate chronic dermatitis.
Research has also found that it’s very common for patients with allergic contact dermatitis to have a concomitant vulvar diagnosis. In one study, more than half of patients had another condition, the most common of which was lichen sclerosus. Others included simplex chronicus, atopic dermatitis, condyloma acuminatum, psoriasis, and Paget disease.
Therefore, if patients are not responding as expected, it’s important to consider that the condition is multifactorial “and consider allergic contact dermatitis in addition to whatever other underlying dermatosis they have,” Dr. Kornik said.
Lichen sclerosus
Prevalence of the scarring disorder lichen sclerosus ranges from 1.7% to 3% in the research literature and pathogenesis is likely multifactorial.
“It’s a very frustrating condition for patients and for physicians because we don’t know exactly what causes it, but it definitely has a predilection for the vulva area, and it affects women of all ages,” she said. “I also think it’s more common than we think.”
Loss of normal anatomical structures are a key feature, so physicians need to know their anatomy well to look for what’s not there. Lichen sclerosus involves modified mucous membranes and the perianal area, and it may spread to the crural folds and upper thighs. Symptoms can include periclitoral edema, white patches, pale skin, textural changes (such as wrinkling, waxiness, or hyperkeratosis), fissures, melanosis, and sometimes ulcerations or erosions from scratching.
There is no standardized treatment for lichen sclerosus. Research suggests using a high potency topical steroid treatment daily until skin texture normalizes, which can take anywhere from 6 weeks to 5 months, depending on severity, Dr. Kornik said. Few data are available for management if topical steroids do not work, she added.*
If dealing with recalcitrant disease, she recommends first checking the patients’ compliance and then considering alternative diagnoses or secondary conditions. Do patch testing, rule out contact dermatitis, and rebiopsy if needed. Other options are to add tacrolimus ointment, offer intralesional triamcinolone, consider a systemic agent (acitretin, methotrexate, or possibly hydroxychloroquine), or try laser or photodynamic therapy. She emphasizes the importance of demonstrating to the patient where to apply ointment, since they may not be applying to the right areas.*
Lichen simplex chronicus
Lichen simplex chronicus is a clinical description of the result of chronic rubbing and scratching. It might be triggered by something that has now resolved or be linked to other itching conditions, but clinicians need to consider the possibility of neuropathic itch as well.
Features of lichen simplex chronicus can include bilateral or unilateral involvement of the labia majora, erythematous plaques with lichenification, hyper- or hypopigmentation, or angulated excoriations and hypertrophy of labia caused by thickened skin, though the signs may be subtle, she said.
Treatment requires management of the skin problem itself – the underlying cause of the itch – as well as the behavioral component. Topical steroids are first line, plus an antihistamine at night as needed to stop the scratching. If those are insufficient, the next treatments to consider are intralesional triamcinolone (Kenalog), tacrolimus ointment, topical or oral doxepin, mirtazapine, or even selective serotonin reuptake inhibitors.
Women using topical steroids should also be aware of the possible side effects, including atrophy, infections, and allergic contact dermatitis if the steroid itself or the cream it’s in is an allergen. If stinging or burning occurs, switch to a steroid without propylene glycol, she added.
If no changes occur in the skin, clinicians may have to consider the existence of neuropathic pruritus diagnosis, an injury or dysfunction along the afferent itch pathway. Burning is more common with this neuropathy, but itching can occur too.
Other issues include symptoms that worsen with sitting and pain that worsens throughout the day. Causes can include childbirth, surgery, pelvic trauma, infection, and chemoradiation, and diagnosis requires imaging to rule out other possible causes. Treatment involves pelvic floor physical therapy, pudendal nerve block, or gabapentin.
Dr. Kornik wrapped up with a reminder that vulvar itch is often multifactorial, so clinicians need to chip away at the potential causes – sometimes with cultures, scrapes, and biopsies as needed.
She reported no financial disclosures.
Correction, 10/26/18: Dr. Kornik's treatment recommendations for lichen sclerosus were misstated.
CHICAGO – Diagnosing the cause of vaginal itching, which can have a significant negative impact on a woman’s quality of life, can be particularly difficult for multiple reasons, according to Rachel Kornik, MD, of the departments of dermatology and obstetrics and gynecology at the University of Wisconsin, Madison.
“The anatomy is really challenging in this area, and there’s a broad differential. Often there’s more than one thing happening,” Dr. Kornik said during a session on diagnosing and managing genital pruritus in women at the American Academy of Dermatology summer meeting. Like hair loss, vaginal pruritus is also very emotionally distressing.
“Patients are very anxious when they have all this itching,” she said. “It has an impact on personal relationships. Some patients find it difficult to talk about because it’s a taboo subject, so we have to make them comfortable.”
Dr. Kornik showed a chart of the inflammatory, neoplastic, infections, infestations, environmental, neuropathic, and hormonal. But she focused her presentation primarily on the most common causes: contact dermatitis, lichen sclerosus, and lichen simplex chronicus.
Contact dermatitis
The most common factors that contribute to contact dermatitis are friction, hygiene practices, unique body exposures (such as body fluids and menstrual and personal care products), and occlusion/maceration, which facilitates penetration of external agents. Estrogen deficiency may also play a role.
Taking a thorough history from the patient is key to finding out possible causes. Dr. Kornik provided a list of common irritants to consider.
- Hygiene-related irritants, such as frequent washing and the use of soaps, wash cloths, loofahs, wipes, bath oil, bubbles, and water.
- Laundry products, such as fabric softeners or dryer sheets.
- Menstrual products, such as panty liners, pads, and scents or additives for retaining moisture.
- Over-the-counter itch products, such as those containing benzocaine.
- Medications, such as alcohol-based creams and gels, trichloroacetic acid, fluorouracil (Efudex), imiquimod, and topical antifungals.
- Heat-related irritants, such as use of hair dryers and heating pads.
- Body fluids, including urine, feces, menstrual blood, sweat, semen, and excessive discharge.
It’s also important to consider whether there is an allergic cause. “Contact dermatitis and allergic dermatitis can look very similar both clinically and histologically, and patients can even have them both at the same time,” Dr. Kornik said. “So really, patch testing is essential sometimes to identify a true allergic contact dermatitis.”
She cited a study that identified the top five most common allergens as fragrance mixes, balsam of Peru, benzocaine, terconazole, and quaternium-15 (a formaldehyde-releasing preservative) (Dermatitis. 2013 Mar-Apr;24(2):64-72).
“If somebody’s coming into your office and they have vulvar itching for any reason, the No. 1 thing is making sure that they eliminate and not use any products with fragrances,” Dr. Kornik said. “It’s also important to note that over time, industries’ use of preservatives does change, the concentrations change, and so we may see more emerging allergens or different ones over time.”
The causative allergens are rarely consumed orally, but they may be ectopic, such as shampoo or nail polish.
“What I’ve learned over the years in treating patients with vulvar itching is that they don’t always think to tell you about everything they are applying,” Dr. Kornik said. “You have to ask specific questions. Are you using any wipes or using any lubricants? What is the type and brand of menstrual pad you’re using?”
Patients might also think they can eliminate the cause of irritation by changing products, but “there are cross reactants in many preservatives and fragrances in many products, so they might not eliminate exposure, and intermittent exposures can lead to chronic dermatitis,” she pointed out.
One example is wipes: Some women may use them only periodically, such as after a yoga class, and not think of this as a possibility or realize that wipes could perpetuate chronic dermatitis.
Research has also found that it’s very common for patients with allergic contact dermatitis to have a concomitant vulvar diagnosis. In one study, more than half of patients had another condition, the most common of which was lichen sclerosus. Others included simplex chronicus, atopic dermatitis, condyloma acuminatum, psoriasis, and Paget disease.
Therefore, if patients are not responding as expected, it’s important to consider that the condition is multifactorial “and consider allergic contact dermatitis in addition to whatever other underlying dermatosis they have,” Dr. Kornik said.
Lichen sclerosus
Prevalence of the scarring disorder lichen sclerosus ranges from 1.7% to 3% in the research literature and pathogenesis is likely multifactorial.
“It’s a very frustrating condition for patients and for physicians because we don’t know exactly what causes it, but it definitely has a predilection for the vulva area, and it affects women of all ages,” she said. “I also think it’s more common than we think.”
Loss of normal anatomical structures are a key feature, so physicians need to know their anatomy well to look for what’s not there. Lichen sclerosus involves modified mucous membranes and the perianal area, and it may spread to the crural folds and upper thighs. Symptoms can include periclitoral edema, white patches, pale skin, textural changes (such as wrinkling, waxiness, or hyperkeratosis), fissures, melanosis, and sometimes ulcerations or erosions from scratching.
There is no standardized treatment for lichen sclerosus. Research suggests using a high potency topical steroid treatment daily until skin texture normalizes, which can take anywhere from 6 weeks to 5 months, depending on severity, Dr. Kornik said. Few data are available for management if topical steroids do not work, she added.*
If dealing with recalcitrant disease, she recommends first checking the patients’ compliance and then considering alternative diagnoses or secondary conditions. Do patch testing, rule out contact dermatitis, and rebiopsy if needed. Other options are to add tacrolimus ointment, offer intralesional triamcinolone, consider a systemic agent (acitretin, methotrexate, or possibly hydroxychloroquine), or try laser or photodynamic therapy. She emphasizes the importance of demonstrating to the patient where to apply ointment, since they may not be applying to the right areas.*
Lichen simplex chronicus
Lichen simplex chronicus is a clinical description of the result of chronic rubbing and scratching. It might be triggered by something that has now resolved or be linked to other itching conditions, but clinicians need to consider the possibility of neuropathic itch as well.
Features of lichen simplex chronicus can include bilateral or unilateral involvement of the labia majora, erythematous plaques with lichenification, hyper- or hypopigmentation, or angulated excoriations and hypertrophy of labia caused by thickened skin, though the signs may be subtle, she said.
Treatment requires management of the skin problem itself – the underlying cause of the itch – as well as the behavioral component. Topical steroids are first line, plus an antihistamine at night as needed to stop the scratching. If those are insufficient, the next treatments to consider are intralesional triamcinolone (Kenalog), tacrolimus ointment, topical or oral doxepin, mirtazapine, or even selective serotonin reuptake inhibitors.
Women using topical steroids should also be aware of the possible side effects, including atrophy, infections, and allergic contact dermatitis if the steroid itself or the cream it’s in is an allergen. If stinging or burning occurs, switch to a steroid without propylene glycol, she added.
If no changes occur in the skin, clinicians may have to consider the existence of neuropathic pruritus diagnosis, an injury or dysfunction along the afferent itch pathway. Burning is more common with this neuropathy, but itching can occur too.
Other issues include symptoms that worsen with sitting and pain that worsens throughout the day. Causes can include childbirth, surgery, pelvic trauma, infection, and chemoradiation, and diagnosis requires imaging to rule out other possible causes. Treatment involves pelvic floor physical therapy, pudendal nerve block, or gabapentin.
Dr. Kornik wrapped up with a reminder that vulvar itch is often multifactorial, so clinicians need to chip away at the potential causes – sometimes with cultures, scrapes, and biopsies as needed.
She reported no financial disclosures.
Correction, 10/26/18: Dr. Kornik's treatment recommendations for lichen sclerosus were misstated.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Most dermatologic drugs safe for breastfeeding mothers
CHICAGO – A common reason why a women stops breastfeeding is the use of medication her doctor has claimed is unsafe during lactation. But most drugs have little or no effect on an infant’s well-being or milk supply, explained Jenny Eileen Murase, MD, of Palo Alto (Calif.) Foundation Medical Group.
“The bottom line I want you to take away from this [session] is that ,” Dr. Murase told attendees at the American Academy of Dermatology summer meeting. “I really want everyone in this room to understand that most of the time, you should not be recommending that a woman is pumping and dumping her milk or stopping breastfeeding because she’s on an agent.”
Dr. Murase, also affiliated with the University of California, San Francisco, provided an overview of drug safety during lactation for major categories of medications that dermatologists prescribe. She recommended that physicians get a copy of Medications and Mother’s Milk by Thomas Hale, PhD, which she considers the best reference for looking up specific drugs. It categorizes drugs as L1 (safest) to L5 (contraindicated), and L2 as “safer,” L3 as “moderately safe,” and L4 as “possibly hazardous.”
Steroids
Contrary to what many believe, prednisone is not contraindicated in breastfeeding, Dr. Murase said. Instead of advising patients to “pump and dump their milk,” she said, “the only recommendation you need to make is that they wait 4 hours after taking the medicine to breastfeed.” For example, a mother can take prednisone before bed and then wake 4 hours later to nurse. Higher doses, such as more than 40 mg daily over long periods, may have the potential to affect growth and development, but more typical doses don’t pose the same risk.
Topical steroids (except for those that are class 1) also are safe to apply directly to the nipple in breastfeeding women, she noted.
Biologics and immunosuppressants
One of the few medications that are contraindicated are topical pimecrolimus and tacrolimus if applied directly to the nipple, since “oral consumption in the infant could be significant,” Dr. Murase said.
Biologics, on the other hand, are not a concern during lactation. “They have low oral bioavailability because of their large molecular size,” and are broken down in the stomach “in a proteolytic environment,” Dr. Murase explained. The CRADLE study, for example, examined the concentration of certolizumab (Cimzia) in mothers’ mature breast milk and found the highest concentration to be just 0.077 mcg/mL, resulting in an average daily infant dose of less than 0.01 mg/kg per day.
Antihistamines and cosmetic topicals
The major antihistamines – brompheniramine, chlorpheniramine, diphenhydramine, hydroxyzine, cetirizine, fexofenadine and loratadine – are likewise safe as L1-L3 drugs. It is preferable to prescribe nonsedating antihistamines, opting for loratadine as the first-line choice. But dermatologists should be reassured that no data support concerns about milk supply reduction from antihistamines, Dr. Murase said.
It’s best to avoid cosmetic topical products, but hydroquinone (L3), topical minoxidil (L2), and botulinum toxin A (L3) do not pose significant risk to the infant. Neither do the anesthetics lidocaine (L2) and epinephrine (L1) for breastfeeding women who need surgery.
Antibiotics
The vast majority of antibiotics are safe for women to use while breastfeeding, but a few notable exceptions exist, including erythromycin.
“People associate erythromycin as safe in lactation because it’s safe in pregnancy, but that’s not the case,” Dr. Murase pointed out. Erythromycin has been linked to pyloric stenosis in newborns and therefore should be avoided in the early months of breastfeeding. In older infants, however, erythromycin becomes an L1 medication.”
Tetracyclines fall into a borderline category. “Tetracyclines would be fine for a complicated infection,” but should not be used for more than 3 weeks, at which point they are regarded as L4, Dr. Murase said. “So long-term use of the tetracyclines should be avoided.”
Aside from these, topical antibiotics are considered safe. Women taking other oral antibiotics should be monitored for gastrointestinal symptoms or allergic responses.
Antifungals
As for antifungals, topicals are safe, and nystatin and clotrimazole are the best first-line options (both L1). Oral antifungals are similarly fine, with griseofulvin, fluconazole, ketoconazole, itraconazole, and terbinafine all classified as L2 and amphotericin B as L3.
If antifungals or antibiotics are being prescribed for a breast fungal infection or for mastitis, Dr. Murase underscored the importance of not stopping breastfeeding.
“The most important thing is that they continue to actually breastfeed on the affected breast that has the staph infection,” she said. She then reiterated that physicians should “reassure new mothers that the majority of oral and topical medications are safe.”
Dr. Murase disclosed serving on the advisory boards of Dermira, UCB, and Genzyme/Sanofi, and she has consulted for Ferndale and UpToDate.
CHICAGO – A common reason why a women stops breastfeeding is the use of medication her doctor has claimed is unsafe during lactation. But most drugs have little or no effect on an infant’s well-being or milk supply, explained Jenny Eileen Murase, MD, of Palo Alto (Calif.) Foundation Medical Group.
“The bottom line I want you to take away from this [session] is that ,” Dr. Murase told attendees at the American Academy of Dermatology summer meeting. “I really want everyone in this room to understand that most of the time, you should not be recommending that a woman is pumping and dumping her milk or stopping breastfeeding because she’s on an agent.”
Dr. Murase, also affiliated with the University of California, San Francisco, provided an overview of drug safety during lactation for major categories of medications that dermatologists prescribe. She recommended that physicians get a copy of Medications and Mother’s Milk by Thomas Hale, PhD, which she considers the best reference for looking up specific drugs. It categorizes drugs as L1 (safest) to L5 (contraindicated), and L2 as “safer,” L3 as “moderately safe,” and L4 as “possibly hazardous.”
Steroids
Contrary to what many believe, prednisone is not contraindicated in breastfeeding, Dr. Murase said. Instead of advising patients to “pump and dump their milk,” she said, “the only recommendation you need to make is that they wait 4 hours after taking the medicine to breastfeed.” For example, a mother can take prednisone before bed and then wake 4 hours later to nurse. Higher doses, such as more than 40 mg daily over long periods, may have the potential to affect growth and development, but more typical doses don’t pose the same risk.
Topical steroids (except for those that are class 1) also are safe to apply directly to the nipple in breastfeeding women, she noted.
Biologics and immunosuppressants
One of the few medications that are contraindicated are topical pimecrolimus and tacrolimus if applied directly to the nipple, since “oral consumption in the infant could be significant,” Dr. Murase said.
Biologics, on the other hand, are not a concern during lactation. “They have low oral bioavailability because of their large molecular size,” and are broken down in the stomach “in a proteolytic environment,” Dr. Murase explained. The CRADLE study, for example, examined the concentration of certolizumab (Cimzia) in mothers’ mature breast milk and found the highest concentration to be just 0.077 mcg/mL, resulting in an average daily infant dose of less than 0.01 mg/kg per day.
Antihistamines and cosmetic topicals
The major antihistamines – brompheniramine, chlorpheniramine, diphenhydramine, hydroxyzine, cetirizine, fexofenadine and loratadine – are likewise safe as L1-L3 drugs. It is preferable to prescribe nonsedating antihistamines, opting for loratadine as the first-line choice. But dermatologists should be reassured that no data support concerns about milk supply reduction from antihistamines, Dr. Murase said.
It’s best to avoid cosmetic topical products, but hydroquinone (L3), topical minoxidil (L2), and botulinum toxin A (L3) do not pose significant risk to the infant. Neither do the anesthetics lidocaine (L2) and epinephrine (L1) for breastfeeding women who need surgery.
Antibiotics
The vast majority of antibiotics are safe for women to use while breastfeeding, but a few notable exceptions exist, including erythromycin.
“People associate erythromycin as safe in lactation because it’s safe in pregnancy, but that’s not the case,” Dr. Murase pointed out. Erythromycin has been linked to pyloric stenosis in newborns and therefore should be avoided in the early months of breastfeeding. In older infants, however, erythromycin becomes an L1 medication.”
Tetracyclines fall into a borderline category. “Tetracyclines would be fine for a complicated infection,” but should not be used for more than 3 weeks, at which point they are regarded as L4, Dr. Murase said. “So long-term use of the tetracyclines should be avoided.”
Aside from these, topical antibiotics are considered safe. Women taking other oral antibiotics should be monitored for gastrointestinal symptoms or allergic responses.
Antifungals
As for antifungals, topicals are safe, and nystatin and clotrimazole are the best first-line options (both L1). Oral antifungals are similarly fine, with griseofulvin, fluconazole, ketoconazole, itraconazole, and terbinafine all classified as L2 and amphotericin B as L3.
If antifungals or antibiotics are being prescribed for a breast fungal infection or for mastitis, Dr. Murase underscored the importance of not stopping breastfeeding.
“The most important thing is that they continue to actually breastfeed on the affected breast that has the staph infection,” she said. She then reiterated that physicians should “reassure new mothers that the majority of oral and topical medications are safe.”
Dr. Murase disclosed serving on the advisory boards of Dermira, UCB, and Genzyme/Sanofi, and she has consulted for Ferndale and UpToDate.
CHICAGO – A common reason why a women stops breastfeeding is the use of medication her doctor has claimed is unsafe during lactation. But most drugs have little or no effect on an infant’s well-being or milk supply, explained Jenny Eileen Murase, MD, of Palo Alto (Calif.) Foundation Medical Group.
“The bottom line I want you to take away from this [session] is that ,” Dr. Murase told attendees at the American Academy of Dermatology summer meeting. “I really want everyone in this room to understand that most of the time, you should not be recommending that a woman is pumping and dumping her milk or stopping breastfeeding because she’s on an agent.”
Dr. Murase, also affiliated with the University of California, San Francisco, provided an overview of drug safety during lactation for major categories of medications that dermatologists prescribe. She recommended that physicians get a copy of Medications and Mother’s Milk by Thomas Hale, PhD, which she considers the best reference for looking up specific drugs. It categorizes drugs as L1 (safest) to L5 (contraindicated), and L2 as “safer,” L3 as “moderately safe,” and L4 as “possibly hazardous.”
Steroids
Contrary to what many believe, prednisone is not contraindicated in breastfeeding, Dr. Murase said. Instead of advising patients to “pump and dump their milk,” she said, “the only recommendation you need to make is that they wait 4 hours after taking the medicine to breastfeed.” For example, a mother can take prednisone before bed and then wake 4 hours later to nurse. Higher doses, such as more than 40 mg daily over long periods, may have the potential to affect growth and development, but more typical doses don’t pose the same risk.
Topical steroids (except for those that are class 1) also are safe to apply directly to the nipple in breastfeeding women, she noted.
Biologics and immunosuppressants
One of the few medications that are contraindicated are topical pimecrolimus and tacrolimus if applied directly to the nipple, since “oral consumption in the infant could be significant,” Dr. Murase said.
Biologics, on the other hand, are not a concern during lactation. “They have low oral bioavailability because of their large molecular size,” and are broken down in the stomach “in a proteolytic environment,” Dr. Murase explained. The CRADLE study, for example, examined the concentration of certolizumab (Cimzia) in mothers’ mature breast milk and found the highest concentration to be just 0.077 mcg/mL, resulting in an average daily infant dose of less than 0.01 mg/kg per day.
Antihistamines and cosmetic topicals
The major antihistamines – brompheniramine, chlorpheniramine, diphenhydramine, hydroxyzine, cetirizine, fexofenadine and loratadine – are likewise safe as L1-L3 drugs. It is preferable to prescribe nonsedating antihistamines, opting for loratadine as the first-line choice. But dermatologists should be reassured that no data support concerns about milk supply reduction from antihistamines, Dr. Murase said.
It’s best to avoid cosmetic topical products, but hydroquinone (L3), topical minoxidil (L2), and botulinum toxin A (L3) do not pose significant risk to the infant. Neither do the anesthetics lidocaine (L2) and epinephrine (L1) for breastfeeding women who need surgery.
Antibiotics
The vast majority of antibiotics are safe for women to use while breastfeeding, but a few notable exceptions exist, including erythromycin.
“People associate erythromycin as safe in lactation because it’s safe in pregnancy, but that’s not the case,” Dr. Murase pointed out. Erythromycin has been linked to pyloric stenosis in newborns and therefore should be avoided in the early months of breastfeeding. In older infants, however, erythromycin becomes an L1 medication.”
Tetracyclines fall into a borderline category. “Tetracyclines would be fine for a complicated infection,” but should not be used for more than 3 weeks, at which point they are regarded as L4, Dr. Murase said. “So long-term use of the tetracyclines should be avoided.”
Aside from these, topical antibiotics are considered safe. Women taking other oral antibiotics should be monitored for gastrointestinal symptoms or allergic responses.
Antifungals
As for antifungals, topicals are safe, and nystatin and clotrimazole are the best first-line options (both L1). Oral antifungals are similarly fine, with griseofulvin, fluconazole, ketoconazole, itraconazole, and terbinafine all classified as L2 and amphotericin B as L3.
If antifungals or antibiotics are being prescribed for a breast fungal infection or for mastitis, Dr. Murase underscored the importance of not stopping breastfeeding.
“The most important thing is that they continue to actually breastfeed on the affected breast that has the staph infection,” she said. She then reiterated that physicians should “reassure new mothers that the majority of oral and topical medications are safe.”
Dr. Murase disclosed serving on the advisory boards of Dermira, UCB, and Genzyme/Sanofi, and she has consulted for Ferndale and UpToDate.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Anti-TNF agents preferred for severe psoriasis in pregnancy
CHICAGO – according to Kenneth B. Gordon, MD, professor and chair of dermatology at Medical College of Wisconsin in Milwaukee.
“We always had this concept that psoriasis gets better during pregnancy, that you might have 20% or 30% of patients who might have a little bit of a flare or maintain, but most keep on getting better,” Dr. Gordon told attendees at the American Academy of Dermatology summer meeting.
But the majority doesn’t mean everyone. He shared the case of one pregnant woman who came to him with severe psoriasis, covering the whole of her inner thigh, to underscore that severe cases do happen in pregnancy.
“These are real situations, and when you talk about maternal health, this woman is uncomfortable, she can’t sleep, and she’s having huge stressors that are not only going to impact her and her pregnancy but also that impact her child,” Dr. Gordon said.
Dr. Gordon clarified that he is not referring to patients with limited psoriasis or those who respond to topicals or phototherapy. But because methotrexate or acitretin are “hands-off during pregnancy,” he said, the only systemic therapy available for serious cases besides biologics is cyclosporine, which has its own risks. “We know that [cyclosporine] is associated with preterm labor and preterm birth and significant low birth weight, so even in the best scenario, when we have someone with persistent severe psoriasis in pregnancy, our best agent has a lot of downsides.”
Too few data exist on anti–interleukin (IL)-17 or anti-IL-23 therapies to draw conclusions about their use, he said, and but gastroenterology and rheumatology have a fair amount of evidence on anti–tumor necrosis factor (TNF) therapies during pregnancy because it’s usually too risky to stop treating conditions such as Crohn’s with these drugs. Still, Dr. Gordon cautioned, much of the data on biologics in pregnancy are conflicting.
The question of what medications to use, and in whom, centers on balancing risks to the fetus from the medication versus risks from the condition.
“There are impacts on the fetus of having severe psoriasis, and it varies with severity of disease,” Dr. Gordon said. For example, data suggest an increased likelihood of low birth weight in children born to mothers with severe psoriasis, and that risk may extend to preterm birth as well, although “we don’t know exactly the magnitude of that effect.”
Meanwhile, the consensus from the literature throughout dermatology, rheumatology, and gastroenterology is that anti-TNF agents do not cause birth defects or affect risk of preterm birth or low birth weight.
“The bigger question is what’s the impact on the immune system of the child,” Dr. Gordon said. Data from a small Scandinavian study suggested no increased risk of allergies, infections, or similar immunologic outcomes, but evidence remains limited.
Research has shown that infants’ exposure to anti-TNF medications persists for 3-6 months after delivery, and the American Academy of Pediatrics recommends delaying immunization in children exposed to anti-TNF agents in pregnancy. But actual evidence on immunization outcomes shows no reduced immunogenicity in such children.
“Clearly there is persistence of drug in the child, but in fact you have normal responses to immunization,” Dr. Gordon said. “The pediatricians’ argument is not based on data of what actually happens in immunization; it’s based on the fact that the drug is there.”
So what’s the bottom line?
The National Psoriasis Foundation recommends moisturizers and topical corticosteroids as first-line therapy in pregnant women with psoriasis, followed by phototherapy for second-line treatment.
But some patients will need systemic therapy during pregnancy, although it’s “best not to introduce more medications than needed in pregnancy,” Dr. Gordon said. For women with a significant flare-up or very persistent volatile disease, NPF first recommends cyclosporine, but Dr. Gordon disagrees and would go with anti-TNF agents before cyclosporine.
Data show that certolizumab is not actively transported across the placenta therefore reducing fetal exposure, so Dr. Gordon would specifically use certolizumab first, all other things being equal.
“But if the patient has been on another anti-TNF that’s been working, I don’t really have an issue with staying with it,” he added.
Existing evidence so far shows no impact in terms of genetic abnormalities, birth weight, premature birth, or even infant immunizations from anti-TNF agents. But beyond those, “there is simply not enough information on pregnancy with other forms of biologic therapy to draw conclusions.” Dr. Gordon said.
Dr. Gordon disclosed that he has received grant support and/or honoraria from Abbvie, Amgen, Almirall, and Boehringer Ingelheim.
CHICAGO – according to Kenneth B. Gordon, MD, professor and chair of dermatology at Medical College of Wisconsin in Milwaukee.
“We always had this concept that psoriasis gets better during pregnancy, that you might have 20% or 30% of patients who might have a little bit of a flare or maintain, but most keep on getting better,” Dr. Gordon told attendees at the American Academy of Dermatology summer meeting.
But the majority doesn’t mean everyone. He shared the case of one pregnant woman who came to him with severe psoriasis, covering the whole of her inner thigh, to underscore that severe cases do happen in pregnancy.
“These are real situations, and when you talk about maternal health, this woman is uncomfortable, she can’t sleep, and she’s having huge stressors that are not only going to impact her and her pregnancy but also that impact her child,” Dr. Gordon said.
Dr. Gordon clarified that he is not referring to patients with limited psoriasis or those who respond to topicals or phototherapy. But because methotrexate or acitretin are “hands-off during pregnancy,” he said, the only systemic therapy available for serious cases besides biologics is cyclosporine, which has its own risks. “We know that [cyclosporine] is associated with preterm labor and preterm birth and significant low birth weight, so even in the best scenario, when we have someone with persistent severe psoriasis in pregnancy, our best agent has a lot of downsides.”
Too few data exist on anti–interleukin (IL)-17 or anti-IL-23 therapies to draw conclusions about their use, he said, and but gastroenterology and rheumatology have a fair amount of evidence on anti–tumor necrosis factor (TNF) therapies during pregnancy because it’s usually too risky to stop treating conditions such as Crohn’s with these drugs. Still, Dr. Gordon cautioned, much of the data on biologics in pregnancy are conflicting.
The question of what medications to use, and in whom, centers on balancing risks to the fetus from the medication versus risks from the condition.
“There are impacts on the fetus of having severe psoriasis, and it varies with severity of disease,” Dr. Gordon said. For example, data suggest an increased likelihood of low birth weight in children born to mothers with severe psoriasis, and that risk may extend to preterm birth as well, although “we don’t know exactly the magnitude of that effect.”
Meanwhile, the consensus from the literature throughout dermatology, rheumatology, and gastroenterology is that anti-TNF agents do not cause birth defects or affect risk of preterm birth or low birth weight.
“The bigger question is what’s the impact on the immune system of the child,” Dr. Gordon said. Data from a small Scandinavian study suggested no increased risk of allergies, infections, or similar immunologic outcomes, but evidence remains limited.
Research has shown that infants’ exposure to anti-TNF medications persists for 3-6 months after delivery, and the American Academy of Pediatrics recommends delaying immunization in children exposed to anti-TNF agents in pregnancy. But actual evidence on immunization outcomes shows no reduced immunogenicity in such children.
“Clearly there is persistence of drug in the child, but in fact you have normal responses to immunization,” Dr. Gordon said. “The pediatricians’ argument is not based on data of what actually happens in immunization; it’s based on the fact that the drug is there.”
So what’s the bottom line?
The National Psoriasis Foundation recommends moisturizers and topical corticosteroids as first-line therapy in pregnant women with psoriasis, followed by phototherapy for second-line treatment.
But some patients will need systemic therapy during pregnancy, although it’s “best not to introduce more medications than needed in pregnancy,” Dr. Gordon said. For women with a significant flare-up or very persistent volatile disease, NPF first recommends cyclosporine, but Dr. Gordon disagrees and would go with anti-TNF agents before cyclosporine.
Data show that certolizumab is not actively transported across the placenta therefore reducing fetal exposure, so Dr. Gordon would specifically use certolizumab first, all other things being equal.
“But if the patient has been on another anti-TNF that’s been working, I don’t really have an issue with staying with it,” he added.
Existing evidence so far shows no impact in terms of genetic abnormalities, birth weight, premature birth, or even infant immunizations from anti-TNF agents. But beyond those, “there is simply not enough information on pregnancy with other forms of biologic therapy to draw conclusions.” Dr. Gordon said.
Dr. Gordon disclosed that he has received grant support and/or honoraria from Abbvie, Amgen, Almirall, and Boehringer Ingelheim.
CHICAGO – according to Kenneth B. Gordon, MD, professor and chair of dermatology at Medical College of Wisconsin in Milwaukee.
“We always had this concept that psoriasis gets better during pregnancy, that you might have 20% or 30% of patients who might have a little bit of a flare or maintain, but most keep on getting better,” Dr. Gordon told attendees at the American Academy of Dermatology summer meeting.
But the majority doesn’t mean everyone. He shared the case of one pregnant woman who came to him with severe psoriasis, covering the whole of her inner thigh, to underscore that severe cases do happen in pregnancy.
“These are real situations, and when you talk about maternal health, this woman is uncomfortable, she can’t sleep, and she’s having huge stressors that are not only going to impact her and her pregnancy but also that impact her child,” Dr. Gordon said.
Dr. Gordon clarified that he is not referring to patients with limited psoriasis or those who respond to topicals or phototherapy. But because methotrexate or acitretin are “hands-off during pregnancy,” he said, the only systemic therapy available for serious cases besides biologics is cyclosporine, which has its own risks. “We know that [cyclosporine] is associated with preterm labor and preterm birth and significant low birth weight, so even in the best scenario, when we have someone with persistent severe psoriasis in pregnancy, our best agent has a lot of downsides.”
Too few data exist on anti–interleukin (IL)-17 or anti-IL-23 therapies to draw conclusions about their use, he said, and but gastroenterology and rheumatology have a fair amount of evidence on anti–tumor necrosis factor (TNF) therapies during pregnancy because it’s usually too risky to stop treating conditions such as Crohn’s with these drugs. Still, Dr. Gordon cautioned, much of the data on biologics in pregnancy are conflicting.
The question of what medications to use, and in whom, centers on balancing risks to the fetus from the medication versus risks from the condition.
“There are impacts on the fetus of having severe psoriasis, and it varies with severity of disease,” Dr. Gordon said. For example, data suggest an increased likelihood of low birth weight in children born to mothers with severe psoriasis, and that risk may extend to preterm birth as well, although “we don’t know exactly the magnitude of that effect.”
Meanwhile, the consensus from the literature throughout dermatology, rheumatology, and gastroenterology is that anti-TNF agents do not cause birth defects or affect risk of preterm birth or low birth weight.
“The bigger question is what’s the impact on the immune system of the child,” Dr. Gordon said. Data from a small Scandinavian study suggested no increased risk of allergies, infections, or similar immunologic outcomes, but evidence remains limited.
Research has shown that infants’ exposure to anti-TNF medications persists for 3-6 months after delivery, and the American Academy of Pediatrics recommends delaying immunization in children exposed to anti-TNF agents in pregnancy. But actual evidence on immunization outcomes shows no reduced immunogenicity in such children.
“Clearly there is persistence of drug in the child, but in fact you have normal responses to immunization,” Dr. Gordon said. “The pediatricians’ argument is not based on data of what actually happens in immunization; it’s based on the fact that the drug is there.”
So what’s the bottom line?
The National Psoriasis Foundation recommends moisturizers and topical corticosteroids as first-line therapy in pregnant women with psoriasis, followed by phototherapy for second-line treatment.
But some patients will need systemic therapy during pregnancy, although it’s “best not to introduce more medications than needed in pregnancy,” Dr. Gordon said. For women with a significant flare-up or very persistent volatile disease, NPF first recommends cyclosporine, but Dr. Gordon disagrees and would go with anti-TNF agents before cyclosporine.
Data show that certolizumab is not actively transported across the placenta therefore reducing fetal exposure, so Dr. Gordon would specifically use certolizumab first, all other things being equal.
“But if the patient has been on another anti-TNF that’s been working, I don’t really have an issue with staying with it,” he added.
Existing evidence so far shows no impact in terms of genetic abnormalities, birth weight, premature birth, or even infant immunizations from anti-TNF agents. But beyond those, “there is simply not enough information on pregnancy with other forms of biologic therapy to draw conclusions.” Dr. Gordon said.
Dr. Gordon disclosed that he has received grant support and/or honoraria from Abbvie, Amgen, Almirall, and Boehringer Ingelheim.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Nonpharmaceutical therapies offer alternatives for atopic dermatitis
CHICAGO – When topical and oral medications alone don’t meet the needs of patients with atopic dermatitis, nonpharmaceutical options may benefit patients as adjunctive therapies, according to Peter A. Lio, MD, of Northwestern University, Chicago.
Cryotherapy and silk or silver fabrics have seen some good results, according to Dr. Lio, who cited his paper on nonpharmacologic therapies for atopic dermatitis. “There is another world of nonpharmacologic treatments that is perhaps nearly as extensive, though less well known, and likely underutilized by some clinicians.”
Dr. Lio described the treatment options for atopic dermatitis as the four points of a tetrahedron: anti-inflammatories, antibiotics, antipruritics, and moisturization.
Moisturization
“More moisturizer means less eczema,” Dr. Lio said. If patients find the moisturizer too cold, they can float the jar in a hot bath before applying it. On the flip side, patients who feel hotter or itchier when applying moisturizer may prefer keeping it in the refrigerator.
Evidence also supports balneotherapy and spa therapy, Dr. Lio said, though limited data exist to guide clinicians on the frequency or duration of baths or how soon to apply moisturizer after a bath. Research indicates benefit from bath and spa therapy lasting up to 3-6 months for mild to moderate eczema.
However, it’s hard to distinguish between the possible benefits of the spa therapy itself versus possible confounding benefits from what often accompanies spa therapy, such as climatotherapy (warm weather), heliotherapy (sunshine), and relaxation from being in a vacation setting.
It’s also unclear whether the minerals in the water matter. Balneotherapy studies have shown benefits from mineral-rich water, but research has shown no benefit from using a water softener to remove minerals from hard water. Furthermore, balneotherapy and spa therapy are expensive, time-consuming, and temporary.
Using wet wraps overnight is an easy and cheap alternative treatment. Dr. Lio recommended soaking onesies, pajamas, gloves, or socks (depending on the location of affected skin) in warm water and then wringing them out until slightly damp. The person puts on the damp clothes and dry pajamas, gloves, or socks over them, and ensures the room is warm enough before going to sleep.
Antibacterial agents
Some research has found an association between environmental Staphylococcus aureus and severe atopic dermatitis, suggesting a role for antibacterial agents, Dr. Lio said. Though the mechanism is unclear, a dilute bleach bath may help.
In a small, randomized, controlled trial of 31 children with moderate to severe eczema, all received oral antibiotics and were then randomized to receive either intranasal mupirocin and a dilute bleach bath twice weekly for 4 weeks or intranasal vaseline and a placebo bath. Those in the mupirocin/bleach bath group showed significant greater improvement, compared with the placebo group.
Yet other research has shown regular baths are superior to dilute bleach baths. It seems more likely that dilute bleach baths act more as an anti-inflammatory than an antibacterial agent, Dr. Lio said at the American Academy of Dermatology summer meeting.
Probiotics “is an area that’s teeming with potential, but right now we don’t really write a prescription for probiotics,” Dr. Lio told attendees. He shared a systematic review supporting probiotics’ use in pregnant mothers and newborns for preventing atopic dermatitis.
“I’m convinced there actually is significant evidence that, if you give expecting moms probiotics and then give it to the baby as soon as they come out, you can prevent or at least reduce the severity of the atopic dermatitis in a measurable portion of patients,” Dr. Lio said. However, he acknowledged other research suggesting probiotics simply delay onset of atopic dermatitis.
“The bacteria in our gut are quite different than [the bacteria] on our skin,” Dr. Lio said. Topical probiotics are under study, and “could be a nonpharmacologic adjunctive therapy.”
Silver and silver-coated clothing are anecdotally successful in select patients. One small study compared silk with topical steroids and implied good results, but most studies with silk remain small and underpowered. If patients want to try textile therapy, they can purchase small silk sleep sacs similar to a sleeping bag.
Silver-impregnated products display true antibacterial effects and do seem to improve atopic dermatitis and pruritus scores, he added, but there are downsides. “These products are pricey, and there’s an environmental issue when you wash these silver clothes and the silver hangs out in the water supply.”
Anti-inflammatories
Cryotherapy is a potential anti-inflammatory, nonpharmaceutical treatment worth exploring, Dr. Lio said. It’s not exactly clear how or why cryotherapy works, but there are several possibilities: Very cold air may increase the body’s antioxidative capacity or reduce the conduction velocity of peripheral nerves, or the cold may simply relieve itch through local or systemic anti-inflammatory effects. At the same time, treatment-related adverse effects from whole-body cryotherapy are a risk – particularly frostbite, Dr. Lio said.
Vitamin D “is a bit of a controversial topic,” Dr. Lio said. The research has gone up and down supporting its potential benefits, so Dr. Lio errs on the side of recommending it.
“It’s one of those things I just give to everybody,” he said, adding that the risk-benefit ratio makes vitamin D worth trying as adverse events are unlikely.
Antipruritics
Dr. Lio discussed the fourth point of the tetrahedron: anti-itching agents. Much has been tried – antihistamines, various topical agents (camphor, menthol, pramoxine), antidepressants, gabapentin, antipsychotics – but little has panned out from these medications.
One study found significantly less refractory uremic pruritus at 1 and 3 months after receiving acupressure.
Hypnosis and biofeedback appear worthwhile as well, perhaps via stress relief. Stress and sleep deprivation can worsen atopic dermatitis and slow healing of the skin barrier. Some research has found subjective and objective benefits from hypnosis.
Dr. Lio endorsed a “write it down” approach when managing atopic dermatitis patients. An Eczema Action Plan, clearly written and provided to the patient, can reduce anxiety levels and increase understanding of the treatment regimens and their risks and benefits.
Dr. Lio has received honoraria for speaking and/or consulting from Pierre-Fabre, L’Oreal, Regeneron, Sanofi Genzyme, Pfizer, Theraplex, Johnson & Johnson, AbbVie, Eli Lilly, Exeltis, Franklin BioScience, Galderma, Kiniksa Pharmaceuticals, Menlo Therapeutics, and Mission Pharmacal. He has also received research grants from Pierre-Fabre and AOBiome.
CHICAGO – When topical and oral medications alone don’t meet the needs of patients with atopic dermatitis, nonpharmaceutical options may benefit patients as adjunctive therapies, according to Peter A. Lio, MD, of Northwestern University, Chicago.
Cryotherapy and silk or silver fabrics have seen some good results, according to Dr. Lio, who cited his paper on nonpharmacologic therapies for atopic dermatitis. “There is another world of nonpharmacologic treatments that is perhaps nearly as extensive, though less well known, and likely underutilized by some clinicians.”
Dr. Lio described the treatment options for atopic dermatitis as the four points of a tetrahedron: anti-inflammatories, antibiotics, antipruritics, and moisturization.
Moisturization
“More moisturizer means less eczema,” Dr. Lio said. If patients find the moisturizer too cold, they can float the jar in a hot bath before applying it. On the flip side, patients who feel hotter or itchier when applying moisturizer may prefer keeping it in the refrigerator.
Evidence also supports balneotherapy and spa therapy, Dr. Lio said, though limited data exist to guide clinicians on the frequency or duration of baths or how soon to apply moisturizer after a bath. Research indicates benefit from bath and spa therapy lasting up to 3-6 months for mild to moderate eczema.
However, it’s hard to distinguish between the possible benefits of the spa therapy itself versus possible confounding benefits from what often accompanies spa therapy, such as climatotherapy (warm weather), heliotherapy (sunshine), and relaxation from being in a vacation setting.
It’s also unclear whether the minerals in the water matter. Balneotherapy studies have shown benefits from mineral-rich water, but research has shown no benefit from using a water softener to remove minerals from hard water. Furthermore, balneotherapy and spa therapy are expensive, time-consuming, and temporary.
Using wet wraps overnight is an easy and cheap alternative treatment. Dr. Lio recommended soaking onesies, pajamas, gloves, or socks (depending on the location of affected skin) in warm water and then wringing them out until slightly damp. The person puts on the damp clothes and dry pajamas, gloves, or socks over them, and ensures the room is warm enough before going to sleep.
Antibacterial agents
Some research has found an association between environmental Staphylococcus aureus and severe atopic dermatitis, suggesting a role for antibacterial agents, Dr. Lio said. Though the mechanism is unclear, a dilute bleach bath may help.
In a small, randomized, controlled trial of 31 children with moderate to severe eczema, all received oral antibiotics and were then randomized to receive either intranasal mupirocin and a dilute bleach bath twice weekly for 4 weeks or intranasal vaseline and a placebo bath. Those in the mupirocin/bleach bath group showed significant greater improvement, compared with the placebo group.
Yet other research has shown regular baths are superior to dilute bleach baths. It seems more likely that dilute bleach baths act more as an anti-inflammatory than an antibacterial agent, Dr. Lio said at the American Academy of Dermatology summer meeting.
Probiotics “is an area that’s teeming with potential, but right now we don’t really write a prescription for probiotics,” Dr. Lio told attendees. He shared a systematic review supporting probiotics’ use in pregnant mothers and newborns for preventing atopic dermatitis.
“I’m convinced there actually is significant evidence that, if you give expecting moms probiotics and then give it to the baby as soon as they come out, you can prevent or at least reduce the severity of the atopic dermatitis in a measurable portion of patients,” Dr. Lio said. However, he acknowledged other research suggesting probiotics simply delay onset of atopic dermatitis.
“The bacteria in our gut are quite different than [the bacteria] on our skin,” Dr. Lio said. Topical probiotics are under study, and “could be a nonpharmacologic adjunctive therapy.”
Silver and silver-coated clothing are anecdotally successful in select patients. One small study compared silk with topical steroids and implied good results, but most studies with silk remain small and underpowered. If patients want to try textile therapy, they can purchase small silk sleep sacs similar to a sleeping bag.
Silver-impregnated products display true antibacterial effects and do seem to improve atopic dermatitis and pruritus scores, he added, but there are downsides. “These products are pricey, and there’s an environmental issue when you wash these silver clothes and the silver hangs out in the water supply.”
Anti-inflammatories
Cryotherapy is a potential anti-inflammatory, nonpharmaceutical treatment worth exploring, Dr. Lio said. It’s not exactly clear how or why cryotherapy works, but there are several possibilities: Very cold air may increase the body’s antioxidative capacity or reduce the conduction velocity of peripheral nerves, or the cold may simply relieve itch through local or systemic anti-inflammatory effects. At the same time, treatment-related adverse effects from whole-body cryotherapy are a risk – particularly frostbite, Dr. Lio said.
Vitamin D “is a bit of a controversial topic,” Dr. Lio said. The research has gone up and down supporting its potential benefits, so Dr. Lio errs on the side of recommending it.
“It’s one of those things I just give to everybody,” he said, adding that the risk-benefit ratio makes vitamin D worth trying as adverse events are unlikely.
Antipruritics
Dr. Lio discussed the fourth point of the tetrahedron: anti-itching agents. Much has been tried – antihistamines, various topical agents (camphor, menthol, pramoxine), antidepressants, gabapentin, antipsychotics – but little has panned out from these medications.
One study found significantly less refractory uremic pruritus at 1 and 3 months after receiving acupressure.
Hypnosis and biofeedback appear worthwhile as well, perhaps via stress relief. Stress and sleep deprivation can worsen atopic dermatitis and slow healing of the skin barrier. Some research has found subjective and objective benefits from hypnosis.
Dr. Lio endorsed a “write it down” approach when managing atopic dermatitis patients. An Eczema Action Plan, clearly written and provided to the patient, can reduce anxiety levels and increase understanding of the treatment regimens and their risks and benefits.
Dr. Lio has received honoraria for speaking and/or consulting from Pierre-Fabre, L’Oreal, Regeneron, Sanofi Genzyme, Pfizer, Theraplex, Johnson & Johnson, AbbVie, Eli Lilly, Exeltis, Franklin BioScience, Galderma, Kiniksa Pharmaceuticals, Menlo Therapeutics, and Mission Pharmacal. He has also received research grants from Pierre-Fabre and AOBiome.
CHICAGO – When topical and oral medications alone don’t meet the needs of patients with atopic dermatitis, nonpharmaceutical options may benefit patients as adjunctive therapies, according to Peter A. Lio, MD, of Northwestern University, Chicago.
Cryotherapy and silk or silver fabrics have seen some good results, according to Dr. Lio, who cited his paper on nonpharmacologic therapies for atopic dermatitis. “There is another world of nonpharmacologic treatments that is perhaps nearly as extensive, though less well known, and likely underutilized by some clinicians.”
Dr. Lio described the treatment options for atopic dermatitis as the four points of a tetrahedron: anti-inflammatories, antibiotics, antipruritics, and moisturization.
Moisturization
“More moisturizer means less eczema,” Dr. Lio said. If patients find the moisturizer too cold, they can float the jar in a hot bath before applying it. On the flip side, patients who feel hotter or itchier when applying moisturizer may prefer keeping it in the refrigerator.
Evidence also supports balneotherapy and spa therapy, Dr. Lio said, though limited data exist to guide clinicians on the frequency or duration of baths or how soon to apply moisturizer after a bath. Research indicates benefit from bath and spa therapy lasting up to 3-6 months for mild to moderate eczema.
However, it’s hard to distinguish between the possible benefits of the spa therapy itself versus possible confounding benefits from what often accompanies spa therapy, such as climatotherapy (warm weather), heliotherapy (sunshine), and relaxation from being in a vacation setting.
It’s also unclear whether the minerals in the water matter. Balneotherapy studies have shown benefits from mineral-rich water, but research has shown no benefit from using a water softener to remove minerals from hard water. Furthermore, balneotherapy and spa therapy are expensive, time-consuming, and temporary.
Using wet wraps overnight is an easy and cheap alternative treatment. Dr. Lio recommended soaking onesies, pajamas, gloves, or socks (depending on the location of affected skin) in warm water and then wringing them out until slightly damp. The person puts on the damp clothes and dry pajamas, gloves, or socks over them, and ensures the room is warm enough before going to sleep.
Antibacterial agents
Some research has found an association between environmental Staphylococcus aureus and severe atopic dermatitis, suggesting a role for antibacterial agents, Dr. Lio said. Though the mechanism is unclear, a dilute bleach bath may help.
In a small, randomized, controlled trial of 31 children with moderate to severe eczema, all received oral antibiotics and were then randomized to receive either intranasal mupirocin and a dilute bleach bath twice weekly for 4 weeks or intranasal vaseline and a placebo bath. Those in the mupirocin/bleach bath group showed significant greater improvement, compared with the placebo group.
Yet other research has shown regular baths are superior to dilute bleach baths. It seems more likely that dilute bleach baths act more as an anti-inflammatory than an antibacterial agent, Dr. Lio said at the American Academy of Dermatology summer meeting.
Probiotics “is an area that’s teeming with potential, but right now we don’t really write a prescription for probiotics,” Dr. Lio told attendees. He shared a systematic review supporting probiotics’ use in pregnant mothers and newborns for preventing atopic dermatitis.
“I’m convinced there actually is significant evidence that, if you give expecting moms probiotics and then give it to the baby as soon as they come out, you can prevent or at least reduce the severity of the atopic dermatitis in a measurable portion of patients,” Dr. Lio said. However, he acknowledged other research suggesting probiotics simply delay onset of atopic dermatitis.
“The bacteria in our gut are quite different than [the bacteria] on our skin,” Dr. Lio said. Topical probiotics are under study, and “could be a nonpharmacologic adjunctive therapy.”
Silver and silver-coated clothing are anecdotally successful in select patients. One small study compared silk with topical steroids and implied good results, but most studies with silk remain small and underpowered. If patients want to try textile therapy, they can purchase small silk sleep sacs similar to a sleeping bag.
Silver-impregnated products display true antibacterial effects and do seem to improve atopic dermatitis and pruritus scores, he added, but there are downsides. “These products are pricey, and there’s an environmental issue when you wash these silver clothes and the silver hangs out in the water supply.”
Anti-inflammatories
Cryotherapy is a potential anti-inflammatory, nonpharmaceutical treatment worth exploring, Dr. Lio said. It’s not exactly clear how or why cryotherapy works, but there are several possibilities: Very cold air may increase the body’s antioxidative capacity or reduce the conduction velocity of peripheral nerves, or the cold may simply relieve itch through local or systemic anti-inflammatory effects. At the same time, treatment-related adverse effects from whole-body cryotherapy are a risk – particularly frostbite, Dr. Lio said.
Vitamin D “is a bit of a controversial topic,” Dr. Lio said. The research has gone up and down supporting its potential benefits, so Dr. Lio errs on the side of recommending it.
“It’s one of those things I just give to everybody,” he said, adding that the risk-benefit ratio makes vitamin D worth trying as adverse events are unlikely.
Antipruritics
Dr. Lio discussed the fourth point of the tetrahedron: anti-itching agents. Much has been tried – antihistamines, various topical agents (camphor, menthol, pramoxine), antidepressants, gabapentin, antipsychotics – but little has panned out from these medications.
One study found significantly less refractory uremic pruritus at 1 and 3 months after receiving acupressure.
Hypnosis and biofeedback appear worthwhile as well, perhaps via stress relief. Stress and sleep deprivation can worsen atopic dermatitis and slow healing of the skin barrier. Some research has found subjective and objective benefits from hypnosis.
Dr. Lio endorsed a “write it down” approach when managing atopic dermatitis patients. An Eczema Action Plan, clearly written and provided to the patient, can reduce anxiety levels and increase understanding of the treatment regimens and their risks and benefits.
Dr. Lio has received honoraria for speaking and/or consulting from Pierre-Fabre, L’Oreal, Regeneron, Sanofi Genzyme, Pfizer, Theraplex, Johnson & Johnson, AbbVie, Eli Lilly, Exeltis, Franklin BioScience, Galderma, Kiniksa Pharmaceuticals, Menlo Therapeutics, and Mission Pharmacal. He has also received research grants from Pierre-Fabre and AOBiome.
EXPERT ANALYSIS FROM SUMMER AAD 2018
So it’s pediatric onychomycosis. Now what?
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
koakes@mdedge.com
EXPERT ANALYSIS FROM SUMMER AAD 2018
Longitudinal melanonychia: the good, the bad, and the confusing
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
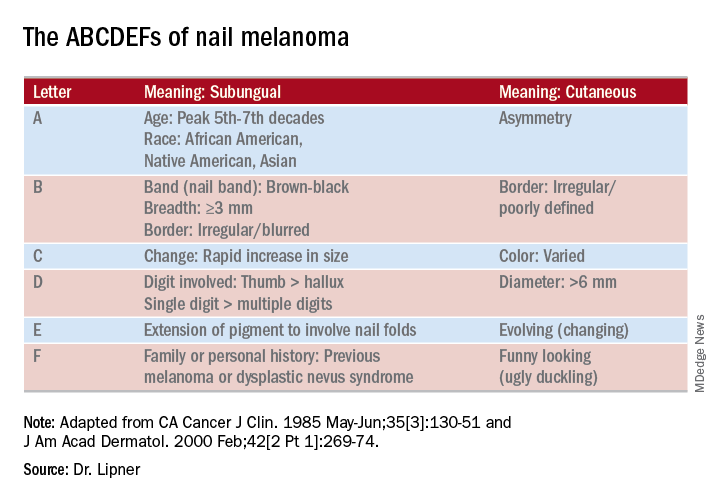
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
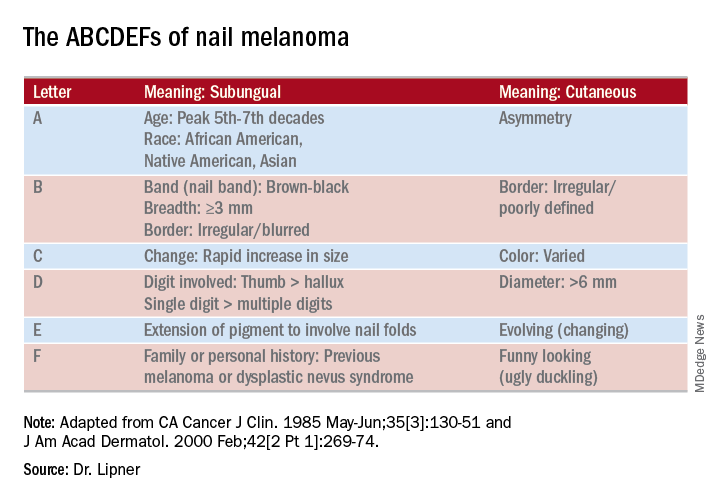
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
CHICAGO – A discolored nail can give even seasoned dermatologists pause: Is the cause exogenous? Fungal or bacterial, perhaps? Could it be a subungual melanoma? Should it be followed, clipped, or biopsied? of the American Academy of Dermatology summer meeting.
The session came after a recent nationwide survey performed by Dr. Lipner and her collaborators who asked dermatologists at different practice stages how confident they were in the diagnosis and management of melanonychia. “On the whole, they were not very confident at all,” said Dr. Lipner, director of the nail division at Cornell University, New York.
Of 142 dermatology residents, as well as 58 junior and 199 senior attending dermatologists, just 18.2% performed nail exams at each visit, and most (58%) only looked at nails during the total body skin exam. Over half (62%) of resident physicians reported feeling not confident about melanonychia diagnosis and management, while that figure dropped to 8.6% for senior attending physicians. Still, most senior physicians (64.3%) were just “fairly confident” in their melanonychia skills (J Am Acad Dermatol. 2017 May;76[5]:994-6).
Tools of the trade
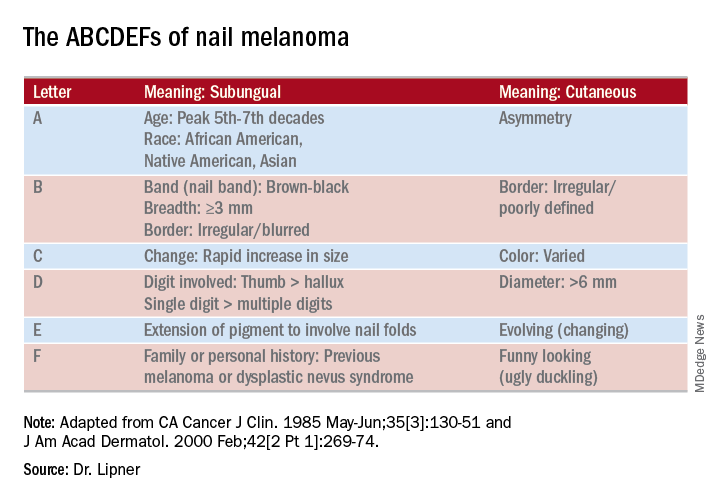
Dermoscopy can be an invaluable tool for determining the cause of longitudinal melanonychia (LM). “Contact dermoscopy is helpful, so I always have ultrasound gel available,” Dr. Lipner said. “The gel makes the nail more of a flat surface,” which makes accurate viewing easier. Other useful tools include a double-action nail clipper, which, she said, is a worthwhile investment.
Because patients who are concerned about one of their nails will often come to their appointment with nail polish still on the other nails, Dr. Lipner always has polish remover pads available in the office. It’s important to be able to see all nails, she said, but she and her collaborators, including first author Pierre Halteh, MD, who was then a medical student at Cornell, discovered from their survey that “few physicians (32/402; 8%) asked their patients to remove nail polish at every visit.”
Nonmelanocytic causes of LM
Longitudinal melanonychias can have a nonmelanocytic etiology, which can range from subungual hematomas to pseudomonas and fungal infections to exogenous pigment.
Overall, subungual hematomas are the most common cause of melanonychia, although longitudinal hematomas are not commonly seen. The more remote the causative trauma, the darker the subungual discoloration, Dr. Lipner said. “Dermoscopy is very helpful” for subungual hematomas, which will usually show a homogeneous pattern, although “you can also see peripheral fadings, streaks, and periungual hemorrhages,” she added.
It is important to monitor these patients “because melanomas can bleed,” she said. In-office photography, or even pictures taken by patients, can be used to track the hematoma to resolution.
When thinking about exogenous sources of pigment, in addition to clues from the history, a tip-off can be that the proximal nail fold is also discolored, Dr. Lipner pointed out. A wide variety of common and less-common culprits may crop up, including from tar, tobacco, henna and other hair dyes, potassium permanganate, and even newspaper print, she said. With an exogenous source, careful clinical and dermoscopic examination may show that the pigment does not extend all the way proximally to the lunula, although it may follow the outline of the proximal nail fold.
When fungus is the cause of LM, the band is often wider proximally and tapers distally, Dr. Lipner noted. While Trichophyton rubrum var. nigricans is a known culprit, nondermatophytes, such as Neoscytalidium dimidiatum, can also cause an LM that often runs along the proximal and lateral nail folds. “To make the diagnosis, sending a clipping to the dermatopathologist is helpful,” she said. Hyphae can often be seen on staining and culture, she said. Polymerase chain reaction “is also possible and very helpful for these nondermatophytes.”
Bacterial colonization of the nail bed can be a cause of LM. Pathogens can include Pseudomonas aeruginosa, which will often show the characteristic greenish tint. Klebsiella and Proteus species may result in more of a grayish-black discoloration. A history of wet work, such as farming and other agricultural and dairy occupations, as well as housekeeping work, increases the risk for bacterial colonization.
Commonly, a bacterial etiology will result in discoloration beginning at the lateral nail fold or at the juncture of the proximal and lateral nail folds. Dermoscopy will show irregular fading of the discoloration toward the medial aspect of the nail, and gram staining of affected clippings will show gram-negative rods.
Melanocytic causes of longitudinal melanonychia
The melanotic macule, sometimes called melanocytic activation, is the most common subtype of melanin-derived LM in adults, Dr. Lipner said. This benign condition results from increased melanin synthesis without an increase in the number of melanocytes, which will be evident on histopathologic examination of the nail bed. Any of a variety of triggers can provoke the increased pigment, which can range from endocrine disruptions to inflammatory conditions, such as psoriasis, to trauma (including nail biting or habit tics).
Pregnancy, normal ethnic variation, and chemotherapy administration are all also associated with melanotic macules. In any case, dermoscopy will show an LM characterized by a grayish background that contains darker grayish lines.
Melanocyte hyperplasia can also cause melanonychia, in which case the trick is sorting out which cases are benign and which are malignant, Dr. Lipner noted. And getting the diagnosis right in a timely fashion matters: “Ideally, we want to catch these melanomas in in situ stages where we can preserve the digit,” she said. “It’s been shown that there is no survival benefit for amputation versus en bloc excision for nail melanomas in situ.”
Nail matrix nevi are the most common cause of LM in children, Dr. Lipner said. Here, dermoscopy shows a brown background with brown lines, with regular color, thickness, and spacing.
On examination of a nail with a melanoma, “typically, we see features suggestive of melanoma but really no pathognomonic features,” she commented. Some signs that should prompt concern and a more thorough investigation, she said, include a dark brown or black band of LM; lack of homogeneity, such as the presence of lines of different colors; blurring of the borders of the pigmentation; and a triangular or wavering outline. Changes in the nail, such as fissuring or splitting, also are worrying, as is any associated discoloration of the periungual skin.
Dermoscopy may confirm the irregularity of the pigmentation pattern and show irregularly colored and spaced lines of varying thicknesses within the pigmented band. An LM caused by melanoma may also be marked by loss of parallelism within the pigmented band.
She pointed out that these concerning characteristics have been encapsulated in a mnemonic, first created in 2000, that’s meant to mirror the ABCDs of nonnail melanoma detection (J Am Acad Dermatol. Feb 2000;42[2 Pt 1]:269-74). Her survey found that overall, just one in four (24.8%) of respondents knew of the mnemonic for subungual melanomas.
Dr. Lipner reported that she has received research support from MOE Medical Devices and has served as a consultant to BAKO Therapeutics.
SOURCE: Lipner S. Summer AAD 2018, Presentation F004.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Psoriasis pipeline is full of biologics
CHICAGO – Most psoriasis therapies in the pipeline are biologics, including several interleukin (IL)-23 inhibitors and a promising dual inhibitor of IL-17A and IL-17F, so dermatologists are likely to gain a few more options for treating psoriasis patients who have not responded well to or tolerated existing therapies.
“The IL-23 blockers are ideal for patients who want a few injections,” Mark Lebwohl, MD, professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and chair of the department of dermatology of the Mount Sinai Health System, said after the American Academy of Dermatology summer meeting. He discussed clinical trial results for risankizumab, mirikizumab, certolizumab pegol (which was recently approved for psoriasis), bimekizumab, as well as tildrakizumab, which has been approved by the Food and Drug Administration, but has not yet been released.
Tildrakizumab: The FDA approved tildrakizumab (Ilumya), a selective IL-23p19 inhibitor, for treatment of moderate to severe plaque psoriasis in March 2018 based on data from the reSURFACE 1 and reSURFACE 2 trials. After initial doses at weeks 0 and 4, patients received a 100-mg subcutaneous injection dose every 12 weeks. Results of reSURFACE 1 showed that 14% of trial participants achieved a Psoriasis Area and Severity Index (PASI) score of 100 with tildrakizumab at week 12, compared with 1% of those receiving a placebo. Similarly, 35% achieved a PASI 90 and 64% achieved a PASI 75 with the drug, compared with 3% and 6%, respectively, in the placebo group. Findings for reSURFACE 2 were similar; in a pooled analysis, a quarter of the 371 patients reached PASI 100 by week 28, 36% reached PASI 90-PASI 99, 24% reached PASI 75-PASI 89, and 10% reached PASI 50-PASI 74. Efficacy remained high 2 years after treatment, although body weight affected the efficacy. “The authors concluded that PASI and PGA [Physician Global Assessment] responses were numerically greater in patients with lower versus higher body weight,” Dr. Lebwohl said at the meeting.
Tildrakizumab also has an “overall clean safety profile,” he said. Among all patients treated in the trials, the rate of severe infections, malignancies and major adverse cardiac events did not significantly differ from placebo.*
Risankizumab: Also an IL-23 inhibitor, risankizumab, under FDA review for treatment of moderate to severe plaque psoriasis, outperformed both ustekinumab and adalimumab in pivotal phase 3 trials reported in October 2017. In the two ultlMMa trials, 75% of 598 total patients achieved a PASI 90 score after 16 weeks of treatment, compared with 2%-5% of placebo participants and 42%-48% of those on ustekinumab. In ultlMMa-1, just over a third of patients treated with achieved PASI 100, and just over half did in ultlMMa-2, compared with 12% and 24% of those on ustekinumab, respectively.
At 1 year, the proportion of those with PASI 90 rose to 82% in ultlMMa-1 and 81% in ultlMMa-2, with over half the participants achieving PASI 100 in both studies. The risankizumab trial findings were “among highest efficacy results reported to date, with impressive durability of response on and off drug,” Dr. Lebwohl said. “Preliminary safety is encouraging,” but “long-term data are required.”
Mirikizumab: Although not as far along in clinical trials, mirikizumab is another IL-23 inhibitor with “interesting and impressive preliminary results,” Dr. Lebwohl said. In a phase 2 trial of 205 participants whose baseline demographics indicated more severe psoriasis, 67% achieved PASI 90 at week 16 with a 300-mg dose (administered every 8 weeks). Doses of 100 mg and 30 mg resulted in 59% and 29% of participants achieving PASI 90 at week 16.
“The most common treatment emergent adverse events included upper respiratory tract infection [including viral], injection site pain, hypertension and diarrhea,” Dr. Lebwohl said. Patients are now being recruited for two phase 3 studies of mirikizumab (OASIS-1 and OASIS-2).
Certolizumab pegol: Certolizumab pegol is a tumor necrosis factor blocker approved in 2013 for treatment of psoriatic arthritis, and for moderate to severe plaque psoriasis in May 2018. In a pooled data analysis of three phase 3 trials (CIMPASI-1, CIMPASI-2, and CIMPACT), 52.3% of participants taking 400 mg subcutaneously every 2 weeks and 44.5% of those taking 200 mg every 2 weeks achieved PASI 90 at week 16, compared with 1.6% of those on placebo. In addition, a trial evaluating maternal transfer of certolizumab to the fetus via placenta found minimal drug concentration levels in the umbilical cord and infant’s plasma. “Certolizumab is ideal for women of childbearing potential,” Dr. Lebwohl said after the meeting.
Bimekizumab: This is a dual inhibitor of IL-17A and IL-17F being studied for treatment of mild psoriasis but “is very promising for psoriatic arthritis, as well as psoriasis,” Dr. Lebwohl said. In the phase 2b BE ABLE 1 trial, up to 79% of patients receiving bimekizumab achieved PASI 90 at week 12, and up to 46% of psoriatic arthritis patients had at least a 50% improvement in joint symptoms, compared with 7% of those on placebo.
Dr. Lebwohl is a consultant for Allergan, Boehringer-Ingelheim, Leo and Promius Pharma, and is an employee of Mount Sinai, which receives research funds from Abbvie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen/Johnson & Johnson, Kadmon, Medimmune/AstraZeneca, Novartis, Pfizer, and ViDac Pharma.
*Correction, 8/6/18: An earlier version of this article misstated the adverse event data for tildrakizumab.
CHICAGO – Most psoriasis therapies in the pipeline are biologics, including several interleukin (IL)-23 inhibitors and a promising dual inhibitor of IL-17A and IL-17F, so dermatologists are likely to gain a few more options for treating psoriasis patients who have not responded well to or tolerated existing therapies.
“The IL-23 blockers are ideal for patients who want a few injections,” Mark Lebwohl, MD, professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and chair of the department of dermatology of the Mount Sinai Health System, said after the American Academy of Dermatology summer meeting. He discussed clinical trial results for risankizumab, mirikizumab, certolizumab pegol (which was recently approved for psoriasis), bimekizumab, as well as tildrakizumab, which has been approved by the Food and Drug Administration, but has not yet been released.
Tildrakizumab: The FDA approved tildrakizumab (Ilumya), a selective IL-23p19 inhibitor, for treatment of moderate to severe plaque psoriasis in March 2018 based on data from the reSURFACE 1 and reSURFACE 2 trials. After initial doses at weeks 0 and 4, patients received a 100-mg subcutaneous injection dose every 12 weeks. Results of reSURFACE 1 showed that 14% of trial participants achieved a Psoriasis Area and Severity Index (PASI) score of 100 with tildrakizumab at week 12, compared with 1% of those receiving a placebo. Similarly, 35% achieved a PASI 90 and 64% achieved a PASI 75 with the drug, compared with 3% and 6%, respectively, in the placebo group. Findings for reSURFACE 2 were similar; in a pooled analysis, a quarter of the 371 patients reached PASI 100 by week 28, 36% reached PASI 90-PASI 99, 24% reached PASI 75-PASI 89, and 10% reached PASI 50-PASI 74. Efficacy remained high 2 years after treatment, although body weight affected the efficacy. “The authors concluded that PASI and PGA [Physician Global Assessment] responses were numerically greater in patients with lower versus higher body weight,” Dr. Lebwohl said at the meeting.
Tildrakizumab also has an “overall clean safety profile,” he said. Among all patients treated in the trials, the rate of severe infections, malignancies and major adverse cardiac events did not significantly differ from placebo.*
Risankizumab: Also an IL-23 inhibitor, risankizumab, under FDA review for treatment of moderate to severe plaque psoriasis, outperformed both ustekinumab and adalimumab in pivotal phase 3 trials reported in October 2017. In the two ultlMMa trials, 75% of 598 total patients achieved a PASI 90 score after 16 weeks of treatment, compared with 2%-5% of placebo participants and 42%-48% of those on ustekinumab. In ultlMMa-1, just over a third of patients treated with achieved PASI 100, and just over half did in ultlMMa-2, compared with 12% and 24% of those on ustekinumab, respectively.
At 1 year, the proportion of those with PASI 90 rose to 82% in ultlMMa-1 and 81% in ultlMMa-2, with over half the participants achieving PASI 100 in both studies. The risankizumab trial findings were “among highest efficacy results reported to date, with impressive durability of response on and off drug,” Dr. Lebwohl said. “Preliminary safety is encouraging,” but “long-term data are required.”
Mirikizumab: Although not as far along in clinical trials, mirikizumab is another IL-23 inhibitor with “interesting and impressive preliminary results,” Dr. Lebwohl said. In a phase 2 trial of 205 participants whose baseline demographics indicated more severe psoriasis, 67% achieved PASI 90 at week 16 with a 300-mg dose (administered every 8 weeks). Doses of 100 mg and 30 mg resulted in 59% and 29% of participants achieving PASI 90 at week 16.
“The most common treatment emergent adverse events included upper respiratory tract infection [including viral], injection site pain, hypertension and diarrhea,” Dr. Lebwohl said. Patients are now being recruited for two phase 3 studies of mirikizumab (OASIS-1 and OASIS-2).
Certolizumab pegol: Certolizumab pegol is a tumor necrosis factor blocker approved in 2013 for treatment of psoriatic arthritis, and for moderate to severe plaque psoriasis in May 2018. In a pooled data analysis of three phase 3 trials (CIMPASI-1, CIMPASI-2, and CIMPACT), 52.3% of participants taking 400 mg subcutaneously every 2 weeks and 44.5% of those taking 200 mg every 2 weeks achieved PASI 90 at week 16, compared with 1.6% of those on placebo. In addition, a trial evaluating maternal transfer of certolizumab to the fetus via placenta found minimal drug concentration levels in the umbilical cord and infant’s plasma. “Certolizumab is ideal for women of childbearing potential,” Dr. Lebwohl said after the meeting.
Bimekizumab: This is a dual inhibitor of IL-17A and IL-17F being studied for treatment of mild psoriasis but “is very promising for psoriatic arthritis, as well as psoriasis,” Dr. Lebwohl said. In the phase 2b BE ABLE 1 trial, up to 79% of patients receiving bimekizumab achieved PASI 90 at week 12, and up to 46% of psoriatic arthritis patients had at least a 50% improvement in joint symptoms, compared with 7% of those on placebo.
Dr. Lebwohl is a consultant for Allergan, Boehringer-Ingelheim, Leo and Promius Pharma, and is an employee of Mount Sinai, which receives research funds from Abbvie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen/Johnson & Johnson, Kadmon, Medimmune/AstraZeneca, Novartis, Pfizer, and ViDac Pharma.
*Correction, 8/6/18: An earlier version of this article misstated the adverse event data for tildrakizumab.
CHICAGO – Most psoriasis therapies in the pipeline are biologics, including several interleukin (IL)-23 inhibitors and a promising dual inhibitor of IL-17A and IL-17F, so dermatologists are likely to gain a few more options for treating psoriasis patients who have not responded well to or tolerated existing therapies.
“The IL-23 blockers are ideal for patients who want a few injections,” Mark Lebwohl, MD, professor of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and chair of the department of dermatology of the Mount Sinai Health System, said after the American Academy of Dermatology summer meeting. He discussed clinical trial results for risankizumab, mirikizumab, certolizumab pegol (which was recently approved for psoriasis), bimekizumab, as well as tildrakizumab, which has been approved by the Food and Drug Administration, but has not yet been released.
Tildrakizumab: The FDA approved tildrakizumab (Ilumya), a selective IL-23p19 inhibitor, for treatment of moderate to severe plaque psoriasis in March 2018 based on data from the reSURFACE 1 and reSURFACE 2 trials. After initial doses at weeks 0 and 4, patients received a 100-mg subcutaneous injection dose every 12 weeks. Results of reSURFACE 1 showed that 14% of trial participants achieved a Psoriasis Area and Severity Index (PASI) score of 100 with tildrakizumab at week 12, compared with 1% of those receiving a placebo. Similarly, 35% achieved a PASI 90 and 64% achieved a PASI 75 with the drug, compared with 3% and 6%, respectively, in the placebo group. Findings for reSURFACE 2 were similar; in a pooled analysis, a quarter of the 371 patients reached PASI 100 by week 28, 36% reached PASI 90-PASI 99, 24% reached PASI 75-PASI 89, and 10% reached PASI 50-PASI 74. Efficacy remained high 2 years after treatment, although body weight affected the efficacy. “The authors concluded that PASI and PGA [Physician Global Assessment] responses were numerically greater in patients with lower versus higher body weight,” Dr. Lebwohl said at the meeting.
Tildrakizumab also has an “overall clean safety profile,” he said. Among all patients treated in the trials, the rate of severe infections, malignancies and major adverse cardiac events did not significantly differ from placebo.*
Risankizumab: Also an IL-23 inhibitor, risankizumab, under FDA review for treatment of moderate to severe plaque psoriasis, outperformed both ustekinumab and adalimumab in pivotal phase 3 trials reported in October 2017. In the two ultlMMa trials, 75% of 598 total patients achieved a PASI 90 score after 16 weeks of treatment, compared with 2%-5% of placebo participants and 42%-48% of those on ustekinumab. In ultlMMa-1, just over a third of patients treated with achieved PASI 100, and just over half did in ultlMMa-2, compared with 12% and 24% of those on ustekinumab, respectively.
At 1 year, the proportion of those with PASI 90 rose to 82% in ultlMMa-1 and 81% in ultlMMa-2, with over half the participants achieving PASI 100 in both studies. The risankizumab trial findings were “among highest efficacy results reported to date, with impressive durability of response on and off drug,” Dr. Lebwohl said. “Preliminary safety is encouraging,” but “long-term data are required.”
Mirikizumab: Although not as far along in clinical trials, mirikizumab is another IL-23 inhibitor with “interesting and impressive preliminary results,” Dr. Lebwohl said. In a phase 2 trial of 205 participants whose baseline demographics indicated more severe psoriasis, 67% achieved PASI 90 at week 16 with a 300-mg dose (administered every 8 weeks). Doses of 100 mg and 30 mg resulted in 59% and 29% of participants achieving PASI 90 at week 16.
“The most common treatment emergent adverse events included upper respiratory tract infection [including viral], injection site pain, hypertension and diarrhea,” Dr. Lebwohl said. Patients are now being recruited for two phase 3 studies of mirikizumab (OASIS-1 and OASIS-2).
Certolizumab pegol: Certolizumab pegol is a tumor necrosis factor blocker approved in 2013 for treatment of psoriatic arthritis, and for moderate to severe plaque psoriasis in May 2018. In a pooled data analysis of three phase 3 trials (CIMPASI-1, CIMPASI-2, and CIMPACT), 52.3% of participants taking 400 mg subcutaneously every 2 weeks and 44.5% of those taking 200 mg every 2 weeks achieved PASI 90 at week 16, compared with 1.6% of those on placebo. In addition, a trial evaluating maternal transfer of certolizumab to the fetus via placenta found minimal drug concentration levels in the umbilical cord and infant’s plasma. “Certolizumab is ideal for women of childbearing potential,” Dr. Lebwohl said after the meeting.
Bimekizumab: This is a dual inhibitor of IL-17A and IL-17F being studied for treatment of mild psoriasis but “is very promising for psoriatic arthritis, as well as psoriasis,” Dr. Lebwohl said. In the phase 2b BE ABLE 1 trial, up to 79% of patients receiving bimekizumab achieved PASI 90 at week 12, and up to 46% of psoriatic arthritis patients had at least a 50% improvement in joint symptoms, compared with 7% of those on placebo.
Dr. Lebwohl is a consultant for Allergan, Boehringer-Ingelheim, Leo and Promius Pharma, and is an employee of Mount Sinai, which receives research funds from Abbvie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen/Johnson & Johnson, Kadmon, Medimmune/AstraZeneca, Novartis, Pfizer, and ViDac Pharma.
*Correction, 8/6/18: An earlier version of this article misstated the adverse event data for tildrakizumab.
EXPERT ANALYSIS FROM SUMMER AAD 2018
Taking the sting out of nail surgery: Postoperative pain pearls
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
CHICAGO – In a busy clinic it can be hard to find the time to stop, talk, and listen. But doing so will “pay dividends in time spent later – and in reduced complications” of nail surgery, according to Molly A. Hinshaw, MD.
Dr. Hinshaw, director of the nail clinic at the University of Wisconsin–Madison, shared her
“One pearl is the importance of patient education before we start,” Dr. Hinshaw said. Preoperatively, she takes time to talk through the entire surgery and expected postoperative course. Critically, she reassures patients that pain will be controlled; she also reviews in detail what the pharmacologic and nonpharmacologic pain control strategies will be.
In addition, it’s important to address patients’ natural anxiety about what the surgical site will look and feel like and how healing will progress, particularly in those first few days after surgery. “I offer a first dressing change in my practice, either at 24 or 48 hours. This can be very anxiolytic for the patient,” she said.
At the preoperative stage, Dr. Hinshaw also tells patients that, from a healing and pain management standpoint, to make sure they plan “to have a restful 48 hours after surgery.” Her patient instructions for the immediate postoperative period include keeping the limb elevated and avoiding unnecessary activity with the affected limb while the digit, whether a finger or toe, is still anesthetized. To stay on top of the pain, the appropriate oral pain medication should be started once sensation starts to return to the digit. She recommends patients also take a dose of their pain medication at bedtime, as this will help them get a restful night of sleep.
“One thing that I’ve learned over the years is that throbbing and a little bit of swelling after surgery is not uncommon,” said Dr. Hinshaw, who uses elastic self-adherent wrap for the top layer of wound dressings after nail surgery. She tells her patients, “if you’re feeling throbbing, you’re welcome to unwrap it and rewrap it more loosely.” Just giving the patient the ability to find a comfortable level of pressure on the affected digit is often enough to alleviate the throbbing, as opposed to treating that throbbing with pain medication.
Dr. Hinshaw said she’s learned to tailor her postoperative analgesia to the surgery and to the patient. With all patients, she is sure to make medication and dosing choices that take comorbidities and potential drug-drug interactions into account. She does not ask patients to stop anticoagulation before nail procedures.
For phenolization procedures and punch biopsies, she’ll advise patients to use acetaminophen or NSAIDs. Some procedures are going to have a more painful recovery course, said Dr. Hinshaw, so she’ll use an opioid such as hydrocodone with acetaminophen for shave excisions and fusiform longitudinal excisions.
The physician and patient can also plan ahead for a brief course of more potent opioids for some procedures. “Certainly for lateral longitudinal excisions, they will need narcotic pain management for at least 48 hours after surgery,” she noted. “It’s a painful surgery.”
Other procedures that will need more postoperative analgesia include flaps and nail unit grafts, she said. In general, NSAIDs are useful to add after the first 24 hours. In addition, “I always call my patients the day after surgery to see how they’re doing. This helps identify any issues and questions early and is comforting to the patient,” she added.
Dr. Hinshaw disclosed that she has an ownership stake in and sits on the board of directors of Accure Medical.
EXPERT ANALYSIS FROM SUMMER AAD 2018
How to watch – and when to biopsy – atypical nevi
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
CHICAGO – Among the many difficult decisions dermatologists have to make, some of the more challenging involve caring for patients with atypical melanocytic lesions. A session at the summer meeting of the American Academy of Dermatology provided some guidance for surveillance of these patients.
Caroline C. Kim, MD, directs the pigmented lesion clinic at Beth Israel Deaconess Medical Center, Boston, and shared the evidence base for her management schema, along with some clinical pearls. No dermatologist ever wants to miss a melanoma, she acknowledged. “We want to avoid those scenarios but not make people feel like Swiss cheese” from multiple biopsies, she said during her presentation.
One key concept that can help physicians find the balance, she said, is that although the presence of atypical or dysplastic nevi increases the risk for melanoma in a given patient, the actual transformation rate of dysplastic nevi to melanomas is not known. In fact, she said, between 50% and 75% of melanomas may arise de novo.
From a dermatopathologic perspective, nevi exist along a continuum of mild to moderate to severe dysplasia, and some lesions are melanomas. But mildly dysplastic nevi are not fated to continue a transformation to increasingly severely dysplastic ones, or to melanomas.
Bringing these ideas to the patient discussion means that one should avoid ever calling a dysplastic nevus “precancerous,” said Dr. Kim; not only is this inaccurate, but it is unnecessarily anxiety provoking, she said.
Within this framework, . Each patient will have a pattern, or several patterns, that typify their nevi. Though the markings may be “atypical,” they’ll have some consistency; if the nevus has several neighbors that look just like it, it’s much less likely to be melanoma. “If they are matching partners, it’s more likely that it’s your typical nevus pattern,” said Dr. Kim, also an assistant professor of dermatology at Harvard Medical School, Boston.
By contrast, some lesions stand out from the patient’s other atypical nevi. They may be larger, darker, more elevated, but sometimes, “Even from the doorway, they just stand out,” Dr. Kim said. And these dual concepts of signature patterns and ugly ducklings are useful to talk over with patients, she said. “It’s so easy for patients to grab on to – they totally get it.”
“Use dermoscopy” when you get to the detailed skin exam, she said. “Data have shown that as clinicians, we are pretty good at picking up melanomas ... But with dermoscopy, our detection rate goes up to 70%-95%,” Dr. Kim said. The caveat is that dermoscopy without proper training is a dangerous tool: Several studies have shown that melanoma detection rates drop compared to the naked eye when dermoscopy is performed by untrained users, she said. “Training matters.”
A further tool to help train the eye and mind to recognize benign and malignant patterns when performing dermoscopy of atypical nevi is a now-classic paper that maps these patterns out, she said (Dermatol Surg. 2007;33[11]:1388-91).
“Beware of de novo and changing lesions,” Dr. Kim said. “A picture truly is worth a thousand words” for tracking these, she said.
Total body digital photography, if it’s available, is the best way to track subtle changes, and to spot new lesions as they crop up, said Dr. Kim. In head-to-head studies with dermoscopy and visual exam alone, digital photography can reduce the number of lesions excised, detect early melanoma, and reduce patient anxiety. One study found a 3.8-fold reduction in the mean rate of nevus biopsies when total body digital photography was used, she said (J Am Acad Dermatol. 2016 Mar. doi: 10.1016/j.jaad.2016.02.1152).
A patient care pearl Dr. Kim shared is that she’ll ask patients for their smartphones and take a photograph of the patients’ backs with those phones. This lets them have a handy reference image for monitoring their own skin in the intervals between visits. But make sure, she said, that patients know that “all change is not bad change – you can get new nevi through your 50s.
“Consider sharing care with a local pigmented lesion clinic” if digital photography is not available at your site, said Dr. Kim. She does this for several of her patients, alternating visits with the primary dermatologist.
When should you perform a biopsy?
“You don’t need to biopsy an atypical nevus to call it atypical. You biopsy lesions if you’re suspicious for calling it melanoma,” Dr. Kim said. Removal also can be considered if, for example, a patient lives alone and the nevi of concern are on her back so home monitoring is a challenge, she said.
Once you’ve decided to biopsy, a narrow excisional biopsy with saucerization and 1- to 3-mm margins is preferred when there’s a high suspicion for melanoma, said Dr. Kim, citing a study that found that 2-mm margins using this method yielded an 87% rate of clear pathologic specimen margins in dysplastic nevi (J Am Acad Dermatol. 2017 Dec;77[6]:1096-9). There is some leeway in the guidelines, but “the preferred technique is a narrow excisional biopsy when you are worried,” she said.
There may be times when a partial or incisional biopsy is a rational choice, as when lesions are very large, located on the face or acral areas, or when suspicion for melanoma is low. “If you do partial biopsies, you really have to be aware of the limitations” of the technique since it may miss the nidus of melanoma within an otherwise bland lesion, Dr. Kim pointed out.
And don’t forget to plan your closure with future follow-up in mind: Dr. Kim related that she’d seen a patient for melanoma who’d had the large excisional biopsy performed elsewhere; the patient’s site was closed with an advancement flap, which made sentinel node biopsy impossible.
When the results come back, then what?
Studies have found that atypical nevi are characterized differently at different sites and that management strategies vary geographically, Dr. Kim said. “There’s a need for large-scale data to further investigate the role of observation versus re-excision of dysplastic nevi,” and a multicenter study is underway to do just that, she said, under the auspices of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group (ECOG/SWOG).
That same subcommittee has issued a consensus statement for dealing with histologically positive excisional biopsy margins. For mildly dysplastic lesions without clinically observable residual pigment, observation is preferred. Severely dysplastic lesions with unpigmented margins should be re-excised, says the statement (JAMA Dermatol. 2015;151[2]:212-18).
For the intermediate lesions, the group recommended that a reasonable option is to observe a moderately dysplastic nevus site that’s been excisionally biopsied with a finding of positive margins, while acknowledging that more data are needed.
All biopsy sites should be followed for regrowth, though recurrence of pigment alone doesn’t necessarily mean another excision is in the patient’s future, Dr. Kim said.
She reported no conflicts of interest.
SOURCE: Kim C. Summer AAD 2018, Presentation F014.
EXPERT ANALYSIS FROM SUMMER AAD 2018