User login
American Association for the Study of Liver Disease (AASLD): The Liver Meeting
New regimen for hepatitis C genotype 2 beats previous standard of care
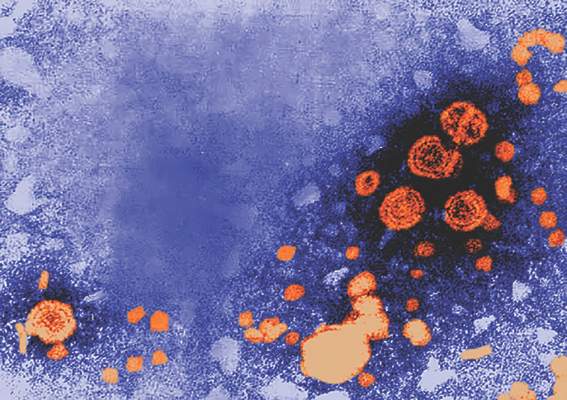
SAN FRANCISCO – A simple, fixed-dose, one-pill combination of sofosbuvir and velpatasvir (SOF/VEL) was found superior to the current standard of sofosbuvir and ribavirin (SOF/R) for treatment of genotype 2 (GT2) hepatitis C virus (HCV) in a phase 3 multicenter, open-label trial presented at the annual meeting of the American Association for the Study of Liver Diseases.
There were no virologic failures on SOF/VEL, which produced a higher 12-week sustained virologic response (SVR12) rate than SOF/R (99% vs. 94%; P = .018) while avoiding ribavirin-related adverse events such as fatigue, reported Dr. Mark S. Sulkowski, medical director of the Viral Hepatitis Center at Johns Hopkins University, Baltimore.
“This combination is currently under regulatory review. If approved, SOF/VEL for 12 weeks will provide a single-tablet, once-daily, highly-effective, ribavirin-free regimen for treatment of patients with genotype 2 infection,” Dr. Sulkowski said.
In this study, which was published on the day of presentation (N Engl J Med. 2015 Nov 17. doi: 10.1056/NEJMoa1512612), 266 patients were randomized to SOF/VEL (400 mg SOF and 100 mg VEL) or to 400 mg SOF plus ribavirin. The primary endpoint was HCV RNA less than 15 IU/mL 12 weeks after the completion of treatment. About 14% of patients had cirrhosis at the time of enrollment and another 14% were treatment experienced, including those with previous exposure to SOF.
Both regimens achieved a SVR12 of 100% in patients who were treatment experienced. In those with cirrhosis, SVR12 rates were 100% for SOF/VEL but only 93% for SOF/R achieved SVR12. Indeed, there were no virologic failures at all in the SOF/VEL arm. The only patient not achieving SVR12 on SOF/VEL left the study after a single dose of therapy.
About 60% of patients had a resistance-associated variant to nonstructural protein 5A, which is the target of VEL, but as there were no virologic failures on SOF/VEL, the presence of resistance-associated variants did not compromise efficacy.
Serious adverse events were uncommon in both arms. Grade 3 or higher laboratory abnormalities (9% vs. 12%) were higher on SOF/R, a difference attributed to the greater reductions in hemoglobin associated with ribavirin. Several nuisance side effects for patients, particularly fatigue (15% vs. 36%) and headache (18% vs. 22%) were also less common on SOF/VEL.
“In general, the adverse event profile did lead to improved quality of life profile [for SOF/VEL] across the 12-week treatment period,” Dr. Sulkowski said.
Due to the adverse events associated with ribavirin, SOF/VEL would have already been attractive as a therapy if it had achieved comparable efficacy to SOF/R, but the near 100% rate of efficacy suggests that this will be a new standard of care when this fixed-dose combination becomes available. In a separate summary of highlights at the meeting, Dr. Norah Terrault, director of viral hepatitis research at the University of California, San Francisco, singled out the study, calling these response rates across different subgroups of GT2 patients “excellent.”
“This now gives us a ribavirin-free option for genotype 2 patients,” Dr. Terrault said.
Dr. Sulkowski reported financial relationships with AbbVie, Bristol-Myers Squibb, Janssen, Merck, and Gilead, which was the sponsor of this study.
SAN FRANCISCO – A simple, fixed-dose, one-pill combination of sofosbuvir and velpatasvir (SOF/VEL) was found superior to the current standard of sofosbuvir and ribavirin (SOF/R) for treatment of genotype 2 (GT2) hepatitis C virus (HCV) in a phase 3 multicenter, open-label trial presented at the annual meeting of the American Association for the Study of Liver Diseases.
There were no virologic failures on SOF/VEL, which produced a higher 12-week sustained virologic response (SVR12) rate than SOF/R (99% vs. 94%; P = .018) while avoiding ribavirin-related adverse events such as fatigue, reported Dr. Mark S. Sulkowski, medical director of the Viral Hepatitis Center at Johns Hopkins University, Baltimore.
“This combination is currently under regulatory review. If approved, SOF/VEL for 12 weeks will provide a single-tablet, once-daily, highly-effective, ribavirin-free regimen for treatment of patients with genotype 2 infection,” Dr. Sulkowski said.
In this study, which was published on the day of presentation (N Engl J Med. 2015 Nov 17. doi: 10.1056/NEJMoa1512612), 266 patients were randomized to SOF/VEL (400 mg SOF and 100 mg VEL) or to 400 mg SOF plus ribavirin. The primary endpoint was HCV RNA less than 15 IU/mL 12 weeks after the completion of treatment. About 14% of patients had cirrhosis at the time of enrollment and another 14% were treatment experienced, including those with previous exposure to SOF.
Both regimens achieved a SVR12 of 100% in patients who were treatment experienced. In those with cirrhosis, SVR12 rates were 100% for SOF/VEL but only 93% for SOF/R achieved SVR12. Indeed, there were no virologic failures at all in the SOF/VEL arm. The only patient not achieving SVR12 on SOF/VEL left the study after a single dose of therapy.
About 60% of patients had a resistance-associated variant to nonstructural protein 5A, which is the target of VEL, but as there were no virologic failures on SOF/VEL, the presence of resistance-associated variants did not compromise efficacy.
Serious adverse events were uncommon in both arms. Grade 3 or higher laboratory abnormalities (9% vs. 12%) were higher on SOF/R, a difference attributed to the greater reductions in hemoglobin associated with ribavirin. Several nuisance side effects for patients, particularly fatigue (15% vs. 36%) and headache (18% vs. 22%) were also less common on SOF/VEL.
“In general, the adverse event profile did lead to improved quality of life profile [for SOF/VEL] across the 12-week treatment period,” Dr. Sulkowski said.
Due to the adverse events associated with ribavirin, SOF/VEL would have already been attractive as a therapy if it had achieved comparable efficacy to SOF/R, but the near 100% rate of efficacy suggests that this will be a new standard of care when this fixed-dose combination becomes available. In a separate summary of highlights at the meeting, Dr. Norah Terrault, director of viral hepatitis research at the University of California, San Francisco, singled out the study, calling these response rates across different subgroups of GT2 patients “excellent.”
“This now gives us a ribavirin-free option for genotype 2 patients,” Dr. Terrault said.
Dr. Sulkowski reported financial relationships with AbbVie, Bristol-Myers Squibb, Janssen, Merck, and Gilead, which was the sponsor of this study.
SAN FRANCISCO – A simple, fixed-dose, one-pill combination of sofosbuvir and velpatasvir (SOF/VEL) was found superior to the current standard of sofosbuvir and ribavirin (SOF/R) for treatment of genotype 2 (GT2) hepatitis C virus (HCV) in a phase 3 multicenter, open-label trial presented at the annual meeting of the American Association for the Study of Liver Diseases.
There were no virologic failures on SOF/VEL, which produced a higher 12-week sustained virologic response (SVR12) rate than SOF/R (99% vs. 94%; P = .018) while avoiding ribavirin-related adverse events such as fatigue, reported Dr. Mark S. Sulkowski, medical director of the Viral Hepatitis Center at Johns Hopkins University, Baltimore.
“This combination is currently under regulatory review. If approved, SOF/VEL for 12 weeks will provide a single-tablet, once-daily, highly-effective, ribavirin-free regimen for treatment of patients with genotype 2 infection,” Dr. Sulkowski said.
In this study, which was published on the day of presentation (N Engl J Med. 2015 Nov 17. doi: 10.1056/NEJMoa1512612), 266 patients were randomized to SOF/VEL (400 mg SOF and 100 mg VEL) or to 400 mg SOF plus ribavirin. The primary endpoint was HCV RNA less than 15 IU/mL 12 weeks after the completion of treatment. About 14% of patients had cirrhosis at the time of enrollment and another 14% were treatment experienced, including those with previous exposure to SOF.
Both regimens achieved a SVR12 of 100% in patients who were treatment experienced. In those with cirrhosis, SVR12 rates were 100% for SOF/VEL but only 93% for SOF/R achieved SVR12. Indeed, there were no virologic failures at all in the SOF/VEL arm. The only patient not achieving SVR12 on SOF/VEL left the study after a single dose of therapy.
About 60% of patients had a resistance-associated variant to nonstructural protein 5A, which is the target of VEL, but as there were no virologic failures on SOF/VEL, the presence of resistance-associated variants did not compromise efficacy.
Serious adverse events were uncommon in both arms. Grade 3 or higher laboratory abnormalities (9% vs. 12%) were higher on SOF/R, a difference attributed to the greater reductions in hemoglobin associated with ribavirin. Several nuisance side effects for patients, particularly fatigue (15% vs. 36%) and headache (18% vs. 22%) were also less common on SOF/VEL.
“In general, the adverse event profile did lead to improved quality of life profile [for SOF/VEL] across the 12-week treatment period,” Dr. Sulkowski said.
Due to the adverse events associated with ribavirin, SOF/VEL would have already been attractive as a therapy if it had achieved comparable efficacy to SOF/R, but the near 100% rate of efficacy suggests that this will be a new standard of care when this fixed-dose combination becomes available. In a separate summary of highlights at the meeting, Dr. Norah Terrault, director of viral hepatitis research at the University of California, San Francisco, singled out the study, calling these response rates across different subgroups of GT2 patients “excellent.”
“This now gives us a ribavirin-free option for genotype 2 patients,” Dr. Terrault said.
Dr. Sulkowski reported financial relationships with AbbVie, Bristol-Myers Squibb, Janssen, Merck, and Gilead, which was the sponsor of this study.
AT THE LIVER MEETING 2015
Key clinical point: A two-drug regimen without ribavirin was found superior to the current standard for genotype 2 (GT2) hepatitis C virus (HCV) infection.
Major finding: The sustained virologic response (SVR) on sofosbuvir/velpatasvir was 99% vs. 94% (P = .018) for the current standard of sofosbuvir/ribavirin.
Data source: Phase III multicenter, open-label, randomized trial.
Disclosures: Dr. Sulkowski reported financial relationships with AbbVie, Bristol-Myers Squibb, Janssen, Merck, and Gilead, which was the sponsor of this study.
Roux-en-Y improves NASH in obese patients
SAN FRANCISCO – Bariatric surgery is an effective treatment for nonalcoholic steatohepatitis (NASH) in obese patients, a Markov model suggests.
Patients with all classes of obesity, including, mild, moderate, and severe, with all stages of fibrosis, experienced gains in life years following laparoscopic Roux-en-Y gastric bypass, compared with standard management and intensive lifestyle changes, based on the model, Dr. Kathleen Corey reported at the annual meeting of the American Association for the Study of Liver Diseases.
Surgery also increased quality-adjusted life years (QALY) in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis, said Dr Corey of Massachusetts General Hospital, Boston.
The number of F3 patients needed to treat to prevent one liver-related death was favorable across all body mass indexes for those with stage F3 fibrosis. The number needed to treat to prevent one case of cirrhosis in these patients was six to seven, and to prevent one liver-related death was eight to 11, she said.
A cost-effectiveness analysis, with a willingness-to-pay threshold of less than $100,000, also showed that surgery was cost effective for all fibrosis stages for those with severe and moderate obesity.
“The [incremental cost-effectiveness ratio] for BMI of 35-39.9 [kg/m2] was $34,000, for those with a BMI of 40 or greater it was $26,000, and we found that with overweight patients with F3 fibrosis, the ratio was also favorable at $59,000,” she said.
More than 78 million American adults suffer from obesity, and the prevalence of obesity is rising nationwide, she said, adding that obesity results in annual medical costs exceeding $147 billion. Treatment options for obesity are limited, and weight regain after weight loss is frequent, Dr. Corey noted.
“However, bariatric surgery has been shown to be a very effective treatment for obesity. Surgery has been shown to significantly reduce mortality in patients, and reduces progression of many comorbidities, including diabetes,” she said.
Guidelines suggest that bariatric surgery is appropriate for patients with a body mass index of 40 or greater and for those with a BMI of 35 or greater if obesity-related comorbidities such as diabetes or obstructive sleep apnea are present, and data suggest that surgery is also of benefit in those with BMI below 35 with diabetes.
The question remains, though, whether nonalcoholic fatty liver disease (NAFLD) – the most common cause of liver disease in the United States – is an indication in itself for bariatric surgery.
NAFLD is strongly associated with obesity, and its progressive form – NASH – can lead to cirrhosis, hepatocellular carcinoma, and the need for liver transplantation.
“However, there are no FDA-approved therapies for NASH and no randomized controlled trials have been conducted to evaluate the role of bariatric surgery in NASH ... and appropriate BMI cutoffs in those with NASH have not been established,” Dr. Corey said.
Several nonrandomized prospective trials have, however, evaluated bariatric surgery in NASH patients with BMIs of 35 or greater with comorbidities, and in patients with BMIs of 40 or greater, and these have shown that NASH resolution can occur in up to 85% of patients at 1-5 years with fibrosis reduction seen in nearly a third, she said, adding that the risk-benefit ratio for surgery is unknown, as is the value of surgery in NASH patients with BMIs less than 35.
The current study looked at three treatment strategies, including standard management with lifestyle counseling; intensive lifestyle intervention based on a diabetes prevention program with lifestyle, nutrition, and exercise counseling; and bariatric Roux-en-Y gastric bypass in a hypothetical simulated cohort of 45-year-olds with NASH, F0-F3 fibrosis, and varying BMI values.
The findings, though limited by a lack of data on the impact of surgery on patients with a BMI of less than 35, and by evaluation of only one type of surgery, showed that bariatric surgery increased incremental life years at all weight and fibrosis stages vs. standard management and intensive lifestyle intervention, and that surgery increased QALY in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis.
“We found that surgery was cost effective for F3 fibrosis in those with moderate and severe obesity and those with overweight. Randomized trials, though, are needed to assess the management of weight loss surgery for NASH before this can be recommended, certainly in patients with a BMI of less than 35,” she concluded.
Dr. Corey reported serving on an advisory committee or review panel for Gilead, and serving in a speaking or teaching role for Synageva.
SAN FRANCISCO – Bariatric surgery is an effective treatment for nonalcoholic steatohepatitis (NASH) in obese patients, a Markov model suggests.
Patients with all classes of obesity, including, mild, moderate, and severe, with all stages of fibrosis, experienced gains in life years following laparoscopic Roux-en-Y gastric bypass, compared with standard management and intensive lifestyle changes, based on the model, Dr. Kathleen Corey reported at the annual meeting of the American Association for the Study of Liver Diseases.
Surgery also increased quality-adjusted life years (QALY) in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis, said Dr Corey of Massachusetts General Hospital, Boston.
The number of F3 patients needed to treat to prevent one liver-related death was favorable across all body mass indexes for those with stage F3 fibrosis. The number needed to treat to prevent one case of cirrhosis in these patients was six to seven, and to prevent one liver-related death was eight to 11, she said.
A cost-effectiveness analysis, with a willingness-to-pay threshold of less than $100,000, also showed that surgery was cost effective for all fibrosis stages for those with severe and moderate obesity.
“The [incremental cost-effectiveness ratio] for BMI of 35-39.9 [kg/m2] was $34,000, for those with a BMI of 40 or greater it was $26,000, and we found that with overweight patients with F3 fibrosis, the ratio was also favorable at $59,000,” she said.
More than 78 million American adults suffer from obesity, and the prevalence of obesity is rising nationwide, she said, adding that obesity results in annual medical costs exceeding $147 billion. Treatment options for obesity are limited, and weight regain after weight loss is frequent, Dr. Corey noted.
“However, bariatric surgery has been shown to be a very effective treatment for obesity. Surgery has been shown to significantly reduce mortality in patients, and reduces progression of many comorbidities, including diabetes,” she said.
Guidelines suggest that bariatric surgery is appropriate for patients with a body mass index of 40 or greater and for those with a BMI of 35 or greater if obesity-related comorbidities such as diabetes or obstructive sleep apnea are present, and data suggest that surgery is also of benefit in those with BMI below 35 with diabetes.
The question remains, though, whether nonalcoholic fatty liver disease (NAFLD) – the most common cause of liver disease in the United States – is an indication in itself for bariatric surgery.
NAFLD is strongly associated with obesity, and its progressive form – NASH – can lead to cirrhosis, hepatocellular carcinoma, and the need for liver transplantation.
“However, there are no FDA-approved therapies for NASH and no randomized controlled trials have been conducted to evaluate the role of bariatric surgery in NASH ... and appropriate BMI cutoffs in those with NASH have not been established,” Dr. Corey said.
Several nonrandomized prospective trials have, however, evaluated bariatric surgery in NASH patients with BMIs of 35 or greater with comorbidities, and in patients with BMIs of 40 or greater, and these have shown that NASH resolution can occur in up to 85% of patients at 1-5 years with fibrosis reduction seen in nearly a third, she said, adding that the risk-benefit ratio for surgery is unknown, as is the value of surgery in NASH patients with BMIs less than 35.
The current study looked at three treatment strategies, including standard management with lifestyle counseling; intensive lifestyle intervention based on a diabetes prevention program with lifestyle, nutrition, and exercise counseling; and bariatric Roux-en-Y gastric bypass in a hypothetical simulated cohort of 45-year-olds with NASH, F0-F3 fibrosis, and varying BMI values.
The findings, though limited by a lack of data on the impact of surgery on patients with a BMI of less than 35, and by evaluation of only one type of surgery, showed that bariatric surgery increased incremental life years at all weight and fibrosis stages vs. standard management and intensive lifestyle intervention, and that surgery increased QALY in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis.
“We found that surgery was cost effective for F3 fibrosis in those with moderate and severe obesity and those with overweight. Randomized trials, though, are needed to assess the management of weight loss surgery for NASH before this can be recommended, certainly in patients with a BMI of less than 35,” she concluded.
Dr. Corey reported serving on an advisory committee or review panel for Gilead, and serving in a speaking or teaching role for Synageva.
SAN FRANCISCO – Bariatric surgery is an effective treatment for nonalcoholic steatohepatitis (NASH) in obese patients, a Markov model suggests.
Patients with all classes of obesity, including, mild, moderate, and severe, with all stages of fibrosis, experienced gains in life years following laparoscopic Roux-en-Y gastric bypass, compared with standard management and intensive lifestyle changes, based on the model, Dr. Kathleen Corey reported at the annual meeting of the American Association for the Study of Liver Diseases.
Surgery also increased quality-adjusted life years (QALY) in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis, said Dr Corey of Massachusetts General Hospital, Boston.
The number of F3 patients needed to treat to prevent one liver-related death was favorable across all body mass indexes for those with stage F3 fibrosis. The number needed to treat to prevent one case of cirrhosis in these patients was six to seven, and to prevent one liver-related death was eight to 11, she said.
A cost-effectiveness analysis, with a willingness-to-pay threshold of less than $100,000, also showed that surgery was cost effective for all fibrosis stages for those with severe and moderate obesity.
“The [incremental cost-effectiveness ratio] for BMI of 35-39.9 [kg/m2] was $34,000, for those with a BMI of 40 or greater it was $26,000, and we found that with overweight patients with F3 fibrosis, the ratio was also favorable at $59,000,” she said.
More than 78 million American adults suffer from obesity, and the prevalence of obesity is rising nationwide, she said, adding that obesity results in annual medical costs exceeding $147 billion. Treatment options for obesity are limited, and weight regain after weight loss is frequent, Dr. Corey noted.
“However, bariatric surgery has been shown to be a very effective treatment for obesity. Surgery has been shown to significantly reduce mortality in patients, and reduces progression of many comorbidities, including diabetes,” she said.
Guidelines suggest that bariatric surgery is appropriate for patients with a body mass index of 40 or greater and for those with a BMI of 35 or greater if obesity-related comorbidities such as diabetes or obstructive sleep apnea are present, and data suggest that surgery is also of benefit in those with BMI below 35 with diabetes.
The question remains, though, whether nonalcoholic fatty liver disease (NAFLD) – the most common cause of liver disease in the United States – is an indication in itself for bariatric surgery.
NAFLD is strongly associated with obesity, and its progressive form – NASH – can lead to cirrhosis, hepatocellular carcinoma, and the need for liver transplantation.
“However, there are no FDA-approved therapies for NASH and no randomized controlled trials have been conducted to evaluate the role of bariatric surgery in NASH ... and appropriate BMI cutoffs in those with NASH have not been established,” Dr. Corey said.
Several nonrandomized prospective trials have, however, evaluated bariatric surgery in NASH patients with BMIs of 35 or greater with comorbidities, and in patients with BMIs of 40 or greater, and these have shown that NASH resolution can occur in up to 85% of patients at 1-5 years with fibrosis reduction seen in nearly a third, she said, adding that the risk-benefit ratio for surgery is unknown, as is the value of surgery in NASH patients with BMIs less than 35.
The current study looked at three treatment strategies, including standard management with lifestyle counseling; intensive lifestyle intervention based on a diabetes prevention program with lifestyle, nutrition, and exercise counseling; and bariatric Roux-en-Y gastric bypass in a hypothetical simulated cohort of 45-year-olds with NASH, F0-F3 fibrosis, and varying BMI values.
The findings, though limited by a lack of data on the impact of surgery on patients with a BMI of less than 35, and by evaluation of only one type of surgery, showed that bariatric surgery increased incremental life years at all weight and fibrosis stages vs. standard management and intensive lifestyle intervention, and that surgery increased QALY in those with moderate and severe obesity with all fibrosis stages, those with mild obesity and F2-F3 fibrosis, and in overweight patients with F3 fibrosis.
“We found that surgery was cost effective for F3 fibrosis in those with moderate and severe obesity and those with overweight. Randomized trials, though, are needed to assess the management of weight loss surgery for NASH before this can be recommended, certainly in patients with a BMI of less than 35,” she concluded.
Dr. Corey reported serving on an advisory committee or review panel for Gilead, and serving in a speaking or teaching role for Synageva.
AT THE LIVER MEETING 2015
Key clinical point: Bariatric surgery is an effective treatment for nonalcoholic steatohepatitis (NASH) in obese patients, a Markov model suggests.
Major finding: The number needed to treat to prevent 1 case of cirrhosis was 6-7; to prevent 1 liver-related death, it was 8-11.
Data source: A Markov modeling study involving a hypothetical simulated cohort of patients.
Disclosures: Dr. Corey reported serving on an advisory committee or review panel for Gilead, and serving in a speaking or teaching role for Synageva.
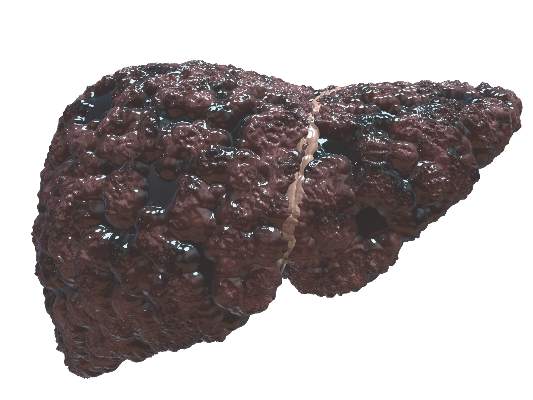
Proportion of HCV patients in U.S. with cirrhosis climbing
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
AT THE LIVER MEETING 2015
Key clinical point: Despite a national decline in the prevalence of hepatitis C virus infection, the prevalence of cirrhosis among HCV-infected patients is climbing.
Major finding: The estimated prevalence of cirrhosis in HCV-infected patients has climbed from 6.6% in the early 1990s to more than 17% in the present era.
Data source: A retrospective cohort study performed with a large database.
Disclosures: Dr. Udompap reported no relevant financial relationships.
ARC-520 shows promise in chronic hepatitis B
SAN FRANCISCO – ARC-520, the first RNA interference–based drug to reach patients, produced deep and durable knockdown of viral antigens and DNA in chronic hepatitis B patients in a phase II study.
Of 58 patients with chronic hepatitis B (CHB) who were included in the study, 38 were hepatitis B e antigen negative (HBeAg-neg), and 20 were hepatitis B e antigen positive (HBeAg-pos). At enrollment, 32 of the 38 HBeAG-neg, and 14 of the 20 HBeAG-pos patients were treated with entecavir (mean duration, 5 years) and remained on that treatment throughout the study, and the remaining 6 patients in each group initiated entecavir treatment during the study, Dr. Man-Fung Yuen of the University of Hong Kong, China reported at the annual meeting of the American Association for the Study of Liver Diseases.
All subjects received either an intravenous dose of ARC (Arrowhead Research Corporation)-520 (48 patients) or placebo (10 patients). The dose was 1-4 mg/kg, divided and given 2 weeks apart in the HBeAg-neg patients, and was 4 mg/kg in the HBeAg-pos patients.
Knockdown of viral parameters was measured over 85 days.
Viral DNA measures showed levels below the threshold for quantification in all patients on entecavir at study entry. Those who were entecavir naive at entry had reduced viral DNA up to 4.3 log (mean, 2.2 log) after treatment with ARC and entecavir, he noted.
ARC reduced viral antigens with quantitative HBeAg (qHBeAg) with best knockdown of 1.7 log after a single 4 mg/kg dose. In treatment-naive patients, the best observed quantitative hepatitis B surface antigen (qHBsAg) knockdown was 1.9 log (99%) in HBeAg-pos patients, and 0.7 log in HBeAg-neg patients (mean max, 1.2 log and 1.1 log, respectively).
A dose-response was seen for quantitative hepatitis B core-related antigen (qHBcrAg) in HBeAg-neg patients, with best knockdown of 0.18 log at a dose of 1 mg/kg (mean max, 0.15 log), and best knockdown of 1.1 log at 4 mg/kg (mean max, 0.9 log). HbeAg-pos showed best knockdown of 1.1 log (mean max, 0.92 log).
The qHBsAg dose response was less deep in patients treated chronically with entecavir (best observed reduction of 0.3 log at 1 mg/kg (mean max, 0.2 log) vs. 0.5 log at 4 mg/kg (mean max, 0.4 log) in HBeAg-neg, and 0.7 log in HBeAg-pos patients (mean max, 0.3).
Divided doses at 4 mg/kg did not increase antigen knockdown, Dr. Yuen noted.
The duration of qHBsAG knockdown was typically 8 weeks, and two distinct knockdown patterns were noted, including an immediate, direct ARC antiviral effect in about 70% of patients, and a delayed response of several weeks after treatment in about 30% of patients, he said.
Chronic hepatitis B has become an important target for drug development, and ARC-520, which targets covalently close circular DNA (ccc-DNA)-derived messenger RNA, is of particular interest. The findings of the current study, which suggest more ccc-DNA–driven antigen production in HBeAg-pos disease, are consistent with those from studies in chimpanzees, as well as with previously reported chronic entecavir reductions in patients for ccc-DNA, Dr. Yuen said.
Studies are currently underway to evaluate the ability of chronic ARC therapy to produce HBsAG seroclearance, he noted.
Dr. Yuen reported advisory committee or review panel participation with GlaxoSmithKline, Bristol-Myers Squibb, and Pfizer, and grant or research support from Roche, Bristol-Myers Squibb, Pfizer, and Gilead Science.
SAN FRANCISCO – ARC-520, the first RNA interference–based drug to reach patients, produced deep and durable knockdown of viral antigens and DNA in chronic hepatitis B patients in a phase II study.
Of 58 patients with chronic hepatitis B (CHB) who were included in the study, 38 were hepatitis B e antigen negative (HBeAg-neg), and 20 were hepatitis B e antigen positive (HBeAg-pos). At enrollment, 32 of the 38 HBeAG-neg, and 14 of the 20 HBeAG-pos patients were treated with entecavir (mean duration, 5 years) and remained on that treatment throughout the study, and the remaining 6 patients in each group initiated entecavir treatment during the study, Dr. Man-Fung Yuen of the University of Hong Kong, China reported at the annual meeting of the American Association for the Study of Liver Diseases.
All subjects received either an intravenous dose of ARC (Arrowhead Research Corporation)-520 (48 patients) or placebo (10 patients). The dose was 1-4 mg/kg, divided and given 2 weeks apart in the HBeAg-neg patients, and was 4 mg/kg in the HBeAg-pos patients.
Knockdown of viral parameters was measured over 85 days.
Viral DNA measures showed levels below the threshold for quantification in all patients on entecavir at study entry. Those who were entecavir naive at entry had reduced viral DNA up to 4.3 log (mean, 2.2 log) after treatment with ARC and entecavir, he noted.
ARC reduced viral antigens with quantitative HBeAg (qHBeAg) with best knockdown of 1.7 log after a single 4 mg/kg dose. In treatment-naive patients, the best observed quantitative hepatitis B surface antigen (qHBsAg) knockdown was 1.9 log (99%) in HBeAg-pos patients, and 0.7 log in HBeAg-neg patients (mean max, 1.2 log and 1.1 log, respectively).
A dose-response was seen for quantitative hepatitis B core-related antigen (qHBcrAg) in HBeAg-neg patients, with best knockdown of 0.18 log at a dose of 1 mg/kg (mean max, 0.15 log), and best knockdown of 1.1 log at 4 mg/kg (mean max, 0.9 log). HbeAg-pos showed best knockdown of 1.1 log (mean max, 0.92 log).
The qHBsAg dose response was less deep in patients treated chronically with entecavir (best observed reduction of 0.3 log at 1 mg/kg (mean max, 0.2 log) vs. 0.5 log at 4 mg/kg (mean max, 0.4 log) in HBeAg-neg, and 0.7 log in HBeAg-pos patients (mean max, 0.3).
Divided doses at 4 mg/kg did not increase antigen knockdown, Dr. Yuen noted.
The duration of qHBsAG knockdown was typically 8 weeks, and two distinct knockdown patterns were noted, including an immediate, direct ARC antiviral effect in about 70% of patients, and a delayed response of several weeks after treatment in about 30% of patients, he said.
Chronic hepatitis B has become an important target for drug development, and ARC-520, which targets covalently close circular DNA (ccc-DNA)-derived messenger RNA, is of particular interest. The findings of the current study, which suggest more ccc-DNA–driven antigen production in HBeAg-pos disease, are consistent with those from studies in chimpanzees, as well as with previously reported chronic entecavir reductions in patients for ccc-DNA, Dr. Yuen said.
Studies are currently underway to evaluate the ability of chronic ARC therapy to produce HBsAG seroclearance, he noted.
Dr. Yuen reported advisory committee or review panel participation with GlaxoSmithKline, Bristol-Myers Squibb, and Pfizer, and grant or research support from Roche, Bristol-Myers Squibb, Pfizer, and Gilead Science.
SAN FRANCISCO – ARC-520, the first RNA interference–based drug to reach patients, produced deep and durable knockdown of viral antigens and DNA in chronic hepatitis B patients in a phase II study.
Of 58 patients with chronic hepatitis B (CHB) who were included in the study, 38 were hepatitis B e antigen negative (HBeAg-neg), and 20 were hepatitis B e antigen positive (HBeAg-pos). At enrollment, 32 of the 38 HBeAG-neg, and 14 of the 20 HBeAG-pos patients were treated with entecavir (mean duration, 5 years) and remained on that treatment throughout the study, and the remaining 6 patients in each group initiated entecavir treatment during the study, Dr. Man-Fung Yuen of the University of Hong Kong, China reported at the annual meeting of the American Association for the Study of Liver Diseases.
All subjects received either an intravenous dose of ARC (Arrowhead Research Corporation)-520 (48 patients) or placebo (10 patients). The dose was 1-4 mg/kg, divided and given 2 weeks apart in the HBeAg-neg patients, and was 4 mg/kg in the HBeAg-pos patients.
Knockdown of viral parameters was measured over 85 days.
Viral DNA measures showed levels below the threshold for quantification in all patients on entecavir at study entry. Those who were entecavir naive at entry had reduced viral DNA up to 4.3 log (mean, 2.2 log) after treatment with ARC and entecavir, he noted.
ARC reduced viral antigens with quantitative HBeAg (qHBeAg) with best knockdown of 1.7 log after a single 4 mg/kg dose. In treatment-naive patients, the best observed quantitative hepatitis B surface antigen (qHBsAg) knockdown was 1.9 log (99%) in HBeAg-pos patients, and 0.7 log in HBeAg-neg patients (mean max, 1.2 log and 1.1 log, respectively).
A dose-response was seen for quantitative hepatitis B core-related antigen (qHBcrAg) in HBeAg-neg patients, with best knockdown of 0.18 log at a dose of 1 mg/kg (mean max, 0.15 log), and best knockdown of 1.1 log at 4 mg/kg (mean max, 0.9 log). HbeAg-pos showed best knockdown of 1.1 log (mean max, 0.92 log).
The qHBsAg dose response was less deep in patients treated chronically with entecavir (best observed reduction of 0.3 log at 1 mg/kg (mean max, 0.2 log) vs. 0.5 log at 4 mg/kg (mean max, 0.4 log) in HBeAg-neg, and 0.7 log in HBeAg-pos patients (mean max, 0.3).
Divided doses at 4 mg/kg did not increase antigen knockdown, Dr. Yuen noted.
The duration of qHBsAG knockdown was typically 8 weeks, and two distinct knockdown patterns were noted, including an immediate, direct ARC antiviral effect in about 70% of patients, and a delayed response of several weeks after treatment in about 30% of patients, he said.
Chronic hepatitis B has become an important target for drug development, and ARC-520, which targets covalently close circular DNA (ccc-DNA)-derived messenger RNA, is of particular interest. The findings of the current study, which suggest more ccc-DNA–driven antigen production in HBeAg-pos disease, are consistent with those from studies in chimpanzees, as well as with previously reported chronic entecavir reductions in patients for ccc-DNA, Dr. Yuen said.
Studies are currently underway to evaluate the ability of chronic ARC therapy to produce HBsAG seroclearance, he noted.
Dr. Yuen reported advisory committee or review panel participation with GlaxoSmithKline, Bristol-Myers Squibb, and Pfizer, and grant or research support from Roche, Bristol-Myers Squibb, Pfizer, and Gilead Science.
AT THE LIVER MEETING 2015
Key clinical point: ARC-520, the first RNA interference–based drug to reach patients, produced deep and durable knockdown of viral antigens and DNA in chronic hepatitis B patients in a phase II study.
Major finding: In treatment-naive patients, the best observed quantitative hepatitis B surface antigen (qHBsAg) knockdown was 1.9 log (99%) in HBeAg-pos patients, and 0.7 log in HBeAg-neg patients (mean max, 1.2 log and 1.1 log, respectively).
Data source: A phase II study of 58 CHB patients.
Disclosures: Dr. Yuen reported advisory committee or review panel participation with GlaxoSmithKline, Bristol-Myers Squibb, and Pfizer, and grant or research support from Roche, Bristol-Myers Squibb, Pfizer, and Gilead Science.
VIDEO: U.S. hepatitis C treatment capacity falls short of need
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2015
AASLD: HCV cure associated with reduction in all-cause mortality
SAN FRANCISCO – Sustained virologic response (SVR) in patients with hepatitis C virus (HCV) infection is associated with large reductions in all-cause mortality and appears to eliminate liver-related mortality in those patients who achieve SVR before developing cirrhosis, according to a real-world study presented at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
“This study strongly supports treatment and cure of HCV to reduce deaths in this patient population,” reported Dr. Lisa M. Nyberg, a specialist in hepatology at Kaiser Permanente, San Diego.
In this study, 24,968 patients diagnosed with HCV in the Kaiser Permanente health care system from January 2002 until the end of 2013 were evaluated retrospectively. The overall mortality over the course of follow-up was 18.5%, but the proportion of patients who died was higher in the group with cirrhosis (33.2%) versus those without cirrhosis (7.8%).
Of the 5,203 treated for HCV, 45.1% achieved SVR. The mortality rates were 18.9% in the absence of SVR versus 5.4% in those who achieved SVR. SVR was associated with reductions in all-cause mortality in those with cirrhosis (8.11% vs. 23.3%; P less than .0001) as well as those without cirrhosis (2.1% vs. 5.3%; P less than .0001).
When liver-related mortality was evaluated, SVR was again associated with large reductions in those with cirrhosis (24.7% vs. 41.9%; P less than .0001) as well as in those without cirrhosis (0% vs. 12%; P = .0178). Indeed, this latter finding indicates that SVR essentially eliminates risk of liver-related death in the absence of cirrhosis.
“The data suggest that treatment of HCV should be initiated at all stages of disease with the intention to cure HCV when possible before progression to cirrhosis,” said Dr. Nyberg, indicating that these findings are relevant to the debate about when to consider curative therapies.
However, Dr. Nyberg suggested that the significant reductions in death by any cause even in patients without cirrhosis suggest that HCV should be considered a systemic illness. She suggested that it is important to recognize that the benefit of eradication extends beyond complications in the liver.
The vast majority of SVRs were achieved in this study with interferon-based regimens, which typically have limited efficacy in many HCV subpopulations, such as those defined by viral genotype. During the discussion that followed presentation of these data, this was a criticism directed at the overall conclusion that SVR can be isolated as a factor in improved outcomes.
“Patients [who achieve SVR on interferon-based therapies] may be very different people to start with,” cautioned Dr. Hans L. Tillmann, professor of medicine, East Carolina University, Greenville, N.C. He pointed out that factors that influence the likelihood of achieving SVR on an interferon-based therapy might be associated with risk factors for mortality over time. With direct-acting antivirals, which have the potential to provide SVR in the vast majority of patients, “you may not be able to reproduce these outcomes.”
While acknowledging the relevance of this criticism, Dr. Nyberg reported that further study is ongoing, including efforts to consider severity of liver disease to evaluate the effect of SVR on the natural history of long-term liver complications following HCV infection.
SAN FRANCISCO – Sustained virologic response (SVR) in patients with hepatitis C virus (HCV) infection is associated with large reductions in all-cause mortality and appears to eliminate liver-related mortality in those patients who achieve SVR before developing cirrhosis, according to a real-world study presented at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
“This study strongly supports treatment and cure of HCV to reduce deaths in this patient population,” reported Dr. Lisa M. Nyberg, a specialist in hepatology at Kaiser Permanente, San Diego.
In this study, 24,968 patients diagnosed with HCV in the Kaiser Permanente health care system from January 2002 until the end of 2013 were evaluated retrospectively. The overall mortality over the course of follow-up was 18.5%, but the proportion of patients who died was higher in the group with cirrhosis (33.2%) versus those without cirrhosis (7.8%).
Of the 5,203 treated for HCV, 45.1% achieved SVR. The mortality rates were 18.9% in the absence of SVR versus 5.4% in those who achieved SVR. SVR was associated with reductions in all-cause mortality in those with cirrhosis (8.11% vs. 23.3%; P less than .0001) as well as those without cirrhosis (2.1% vs. 5.3%; P less than .0001).
When liver-related mortality was evaluated, SVR was again associated with large reductions in those with cirrhosis (24.7% vs. 41.9%; P less than .0001) as well as in those without cirrhosis (0% vs. 12%; P = .0178). Indeed, this latter finding indicates that SVR essentially eliminates risk of liver-related death in the absence of cirrhosis.
“The data suggest that treatment of HCV should be initiated at all stages of disease with the intention to cure HCV when possible before progression to cirrhosis,” said Dr. Nyberg, indicating that these findings are relevant to the debate about when to consider curative therapies.
However, Dr. Nyberg suggested that the significant reductions in death by any cause even in patients without cirrhosis suggest that HCV should be considered a systemic illness. She suggested that it is important to recognize that the benefit of eradication extends beyond complications in the liver.
The vast majority of SVRs were achieved in this study with interferon-based regimens, which typically have limited efficacy in many HCV subpopulations, such as those defined by viral genotype. During the discussion that followed presentation of these data, this was a criticism directed at the overall conclusion that SVR can be isolated as a factor in improved outcomes.
“Patients [who achieve SVR on interferon-based therapies] may be very different people to start with,” cautioned Dr. Hans L. Tillmann, professor of medicine, East Carolina University, Greenville, N.C. He pointed out that factors that influence the likelihood of achieving SVR on an interferon-based therapy might be associated with risk factors for mortality over time. With direct-acting antivirals, which have the potential to provide SVR in the vast majority of patients, “you may not be able to reproduce these outcomes.”
While acknowledging the relevance of this criticism, Dr. Nyberg reported that further study is ongoing, including efforts to consider severity of liver disease to evaluate the effect of SVR on the natural history of long-term liver complications following HCV infection.
SAN FRANCISCO – Sustained virologic response (SVR) in patients with hepatitis C virus (HCV) infection is associated with large reductions in all-cause mortality and appears to eliminate liver-related mortality in those patients who achieve SVR before developing cirrhosis, according to a real-world study presented at the annual meeting of the American Association for the Study of Liver Disease (AASLD).
“This study strongly supports treatment and cure of HCV to reduce deaths in this patient population,” reported Dr. Lisa M. Nyberg, a specialist in hepatology at Kaiser Permanente, San Diego.
In this study, 24,968 patients diagnosed with HCV in the Kaiser Permanente health care system from January 2002 until the end of 2013 were evaluated retrospectively. The overall mortality over the course of follow-up was 18.5%, but the proportion of patients who died was higher in the group with cirrhosis (33.2%) versus those without cirrhosis (7.8%).
Of the 5,203 treated for HCV, 45.1% achieved SVR. The mortality rates were 18.9% in the absence of SVR versus 5.4% in those who achieved SVR. SVR was associated with reductions in all-cause mortality in those with cirrhosis (8.11% vs. 23.3%; P less than .0001) as well as those without cirrhosis (2.1% vs. 5.3%; P less than .0001).
When liver-related mortality was evaluated, SVR was again associated with large reductions in those with cirrhosis (24.7% vs. 41.9%; P less than .0001) as well as in those without cirrhosis (0% vs. 12%; P = .0178). Indeed, this latter finding indicates that SVR essentially eliminates risk of liver-related death in the absence of cirrhosis.
“The data suggest that treatment of HCV should be initiated at all stages of disease with the intention to cure HCV when possible before progression to cirrhosis,” said Dr. Nyberg, indicating that these findings are relevant to the debate about when to consider curative therapies.
However, Dr. Nyberg suggested that the significant reductions in death by any cause even in patients without cirrhosis suggest that HCV should be considered a systemic illness. She suggested that it is important to recognize that the benefit of eradication extends beyond complications in the liver.
The vast majority of SVRs were achieved in this study with interferon-based regimens, which typically have limited efficacy in many HCV subpopulations, such as those defined by viral genotype. During the discussion that followed presentation of these data, this was a criticism directed at the overall conclusion that SVR can be isolated as a factor in improved outcomes.
“Patients [who achieve SVR on interferon-based therapies] may be very different people to start with,” cautioned Dr. Hans L. Tillmann, professor of medicine, East Carolina University, Greenville, N.C. He pointed out that factors that influence the likelihood of achieving SVR on an interferon-based therapy might be associated with risk factors for mortality over time. With direct-acting antivirals, which have the potential to provide SVR in the vast majority of patients, “you may not be able to reproduce these outcomes.”
While acknowledging the relevance of this criticism, Dr. Nyberg reported that further study is ongoing, including efforts to consider severity of liver disease to evaluate the effect of SVR on the natural history of long-term liver complications following HCV infection.
AT THE LIVER MEETING 2015
Key clinical point: Achieving an SVR is associated with a large reduction in liver-related and all-cause mortality over long-term follow-up.
Major finding: In follow-up, all-cause mortality was more than threefold lower (5.4% vs. 18.9%) in those who achieved SVR relative to those who did not.
Data source: Retrospective cohort study performed with large database.
Disclosures: Dr. Nyberg has reported financial relationships with AbbVie, Merck, and Gilead, which was the sponsor of this study.
Elevated liver cancer risk after HCV cure may justify surveillance
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
AT THE LIVER MEETING 2015
Key clinical point: Elevated rates of hepatocellular carcinoma (HCC) remain elevated in patients with hepatitis C virus infection who achieved a sustained virologic response.
Major finding: In a VA database, the overall risk of HCC after SVR was 0.3% per year but was higher among the elderly, those with diabetes, and those with cirrhosis.
Data source: Retrospective cohort study performed with a large database.
Disclosures: Dr. El-Serag has a financial relationship with Gilead.
Investigational hepatitis B therapy shows activity in proof-of-concept study
SAN FRANCISCO – NVR 3-778, an experimental hepatitis B virus (HBV) core inhibitor, showed substantial activity and was well tolerated in an initial phase Ib study presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Diseases.
Through its core-related mechanisms, which may prevent viral assembly and replication, NVR 3-778, particularly when used in combination with other antivirals, may represent a step “toward a goal of increased durable response rates in HBV patients,” reported Dr. Man-Fung Yuen of Queen Mary Hospital, University of Hong Kong.
In this phase Ib study, safety and efficacy of NVR 3-778 were evaluated in 36 HBV-infected patients who were randomized to one of four dosing cohorts. An additional eight patients received a matching placebo. Enrollment requirements included serum HBV DNA greater than 20,000 IU/mL and age between 19 and 65 years. ALT levels could be normal or less than seven times the upper limit of normal. The majority of subjects were male.
The four doses of NVR 3-778 evaluated were 100 mg once daily (10 patients), 200 mg once daily (10 patients), 400 mg once daily (8 patients), and 600 mg twice daily (8 patients). Viral load reductions and safety were monitored.
All doses were well tolerated with no treatment-related discontinuations or serious adverse events observed. A single patient, who was on the lowest dose, developed a serious rash. No other patients developed significant rashes.
There appeared to be a dose response with no significant reductions in HBV DNA observed on the lowest dose and modest reductions with the 200-mg and 400-mg once-daily doses. On the 600-mg twice-daily dose, HBV DNA levels fell 1.72 log10 IU mL (range, 1.06-3.71 log10 IU/mL) from baseline.
Based on the dose response and the tolerability of the 600-mg twice-daily dose, studies are now planned to evaluate higher doses. Greater viral control may also be achieved if this agent is combined with other agents, such as peg-interferon or a nucleoside. According to Dr. Yuen, there are already plans to evaluate both types of combinations.
As a core inhibitor, NVR 3-778 “can potentially inhibit viral assembly, HBV genome replication, covalently closed circular DNA [the permanent viral DNA structure in the nuclei of infected cells], and hepatic reinfection cycles,” Dr. Yuen said. This is not achieved routinely with current therapies, which Dr. Yuen said can suppress HBV replication but must be maintained to sustain control.
The further development of NVR 3-778 and other core inhibitors is being directed “toward a goal of increased durable response rates in HBV patients,” Dr. Yuen reported.
SAN FRANCISCO – NVR 3-778, an experimental hepatitis B virus (HBV) core inhibitor, showed substantial activity and was well tolerated in an initial phase Ib study presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Diseases.
Through its core-related mechanisms, which may prevent viral assembly and replication, NVR 3-778, particularly when used in combination with other antivirals, may represent a step “toward a goal of increased durable response rates in HBV patients,” reported Dr. Man-Fung Yuen of Queen Mary Hospital, University of Hong Kong.
In this phase Ib study, safety and efficacy of NVR 3-778 were evaluated in 36 HBV-infected patients who were randomized to one of four dosing cohorts. An additional eight patients received a matching placebo. Enrollment requirements included serum HBV DNA greater than 20,000 IU/mL and age between 19 and 65 years. ALT levels could be normal or less than seven times the upper limit of normal. The majority of subjects were male.
The four doses of NVR 3-778 evaluated were 100 mg once daily (10 patients), 200 mg once daily (10 patients), 400 mg once daily (8 patients), and 600 mg twice daily (8 patients). Viral load reductions and safety were monitored.
All doses were well tolerated with no treatment-related discontinuations or serious adverse events observed. A single patient, who was on the lowest dose, developed a serious rash. No other patients developed significant rashes.
There appeared to be a dose response with no significant reductions in HBV DNA observed on the lowest dose and modest reductions with the 200-mg and 400-mg once-daily doses. On the 600-mg twice-daily dose, HBV DNA levels fell 1.72 log10 IU mL (range, 1.06-3.71 log10 IU/mL) from baseline.
Based on the dose response and the tolerability of the 600-mg twice-daily dose, studies are now planned to evaluate higher doses. Greater viral control may also be achieved if this agent is combined with other agents, such as peg-interferon or a nucleoside. According to Dr. Yuen, there are already plans to evaluate both types of combinations.
As a core inhibitor, NVR 3-778 “can potentially inhibit viral assembly, HBV genome replication, covalently closed circular DNA [the permanent viral DNA structure in the nuclei of infected cells], and hepatic reinfection cycles,” Dr. Yuen said. This is not achieved routinely with current therapies, which Dr. Yuen said can suppress HBV replication but must be maintained to sustain control.
The further development of NVR 3-778 and other core inhibitors is being directed “toward a goal of increased durable response rates in HBV patients,” Dr. Yuen reported.
SAN FRANCISCO – NVR 3-778, an experimental hepatitis B virus (HBV) core inhibitor, showed substantial activity and was well tolerated in an initial phase Ib study presented as a late-breaker at the annual meeting of the American Association for the Study of Liver Diseases.
Through its core-related mechanisms, which may prevent viral assembly and replication, NVR 3-778, particularly when used in combination with other antivirals, may represent a step “toward a goal of increased durable response rates in HBV patients,” reported Dr. Man-Fung Yuen of Queen Mary Hospital, University of Hong Kong.
In this phase Ib study, safety and efficacy of NVR 3-778 were evaluated in 36 HBV-infected patients who were randomized to one of four dosing cohorts. An additional eight patients received a matching placebo. Enrollment requirements included serum HBV DNA greater than 20,000 IU/mL and age between 19 and 65 years. ALT levels could be normal or less than seven times the upper limit of normal. The majority of subjects were male.
The four doses of NVR 3-778 evaluated were 100 mg once daily (10 patients), 200 mg once daily (10 patients), 400 mg once daily (8 patients), and 600 mg twice daily (8 patients). Viral load reductions and safety were monitored.
All doses were well tolerated with no treatment-related discontinuations or serious adverse events observed. A single patient, who was on the lowest dose, developed a serious rash. No other patients developed significant rashes.
There appeared to be a dose response with no significant reductions in HBV DNA observed on the lowest dose and modest reductions with the 200-mg and 400-mg once-daily doses. On the 600-mg twice-daily dose, HBV DNA levels fell 1.72 log10 IU mL (range, 1.06-3.71 log10 IU/mL) from baseline.
Based on the dose response and the tolerability of the 600-mg twice-daily dose, studies are now planned to evaluate higher doses. Greater viral control may also be achieved if this agent is combined with other agents, such as peg-interferon or a nucleoside. According to Dr. Yuen, there are already plans to evaluate both types of combinations.
As a core inhibitor, NVR 3-778 “can potentially inhibit viral assembly, HBV genome replication, covalently closed circular DNA [the permanent viral DNA structure in the nuclei of infected cells], and hepatic reinfection cycles,” Dr. Yuen said. This is not achieved routinely with current therapies, which Dr. Yuen said can suppress HBV replication but must be maintained to sustain control.
The further development of NVR 3-778 and other core inhibitors is being directed “toward a goal of increased durable response rates in HBV patients,” Dr. Yuen reported.
AT THE LIVER MEETING 2015
Key clinical point:The experimental agent NVR 3-778 produced significant reductions in hepatitis B viral load in an initial dose-ranging study.
Major finding: At the highest tested dose (600 mg twice daily), the mean 28-day reduction in hepatitis B virus DNA levels reached 1.72 log10 IU/mL (range, 1.06-3.71 log10 IU/mL).
Data source: Multicenter open-label phase Ib study.
Disclosures: Dr. Chan reported financial relationships with Abbvie, Bristol-Myers Squibb, Echosens, Gilead, Novartis, and Roche
Transplant waiting-list registrations dropped after direct acting–antiviral approval
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
AT THE LIVER MEETING 2015
Key clinical point: New waiting-list registrations for liver transplantation in patients with hepatitis C virus declined significantly after introduction of second-generation direct-acting antiviral agents.
Major finding: HCV-specific waiting-list registrations declined by 23% in the 15 months after vs. before FDA approval of simeprevir and sofosbuvir (34.8% vs. 26.8%).
Data source: A review of United Network for Organ Sharing data.
Disclosures: Dr. Perumpail reported having no disclosures.
VIDEO: 12-week HCV retreatment effective if short course fails
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2015