User login
Statins don’t help, may harm in COPD, ARDS
SAN DIEGO – Two separate prospective, multicenter trials of statins stopped early when interim results showed they did not help – and potentially harmed – patients with moderate to severe chronic obstructive pulmonary disease or sepsis-associated acute respiratory distress syndrome.
The findings contradict previous observational data suggesting that the potential anti-inflammatory effects of statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors [HMG-CoA]) might benefit patients with these two diseases.
Statins did not significantly reduce rates of exacerbation of chronic obstructive pulmonary disease (COPD) or the time to first exacerbation in a study of 885 patients with moderate to severe COPD who were at high risk for exacerbations and who did not require statins for other indications. Patients in the STATCOPE study (Prospective Randomized Placebo-Controlled Trial of Simvastatin in the Prevention of COPD) received a daily oral dose of either 40 mg simvastatin or placebo for 12-36 months.
The simvastatin group had a mean of 1.36 exacerbations/person-year, compared with 1.39/person-year in the placebo group. The median number of days to the first exacerbation was 223 on simvastatin and 231 on placebo, differences that were not significant, Dr. Gerard J. Criner and his associates reported at an international conference of the American Thoracic Society.
The results were published online by the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1403086]).
Among the 885 patients for whom follow-up information was available, 1,982 acute COPD exacerbations occurred, 965 in 430 patients on simvastatin and 1,017 exacerbations in 447 patients on placebo, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia.
Overall, 34% of patients had three or more exacerbations of COPD, with similar numbers in each group – 141 in the simvastatin group and 155 in the placebo groups. The proportions of patients who received glucocorticoid therapy or antibiotics for exacerbations did not differ significantly between groups.
The simvastatin group had a significantly higher rate of nonfatal serious adverse events involving the GI tract (mainly nausea and bloating from simvastatin) in 30 patients (0.05 events/person-year), compared with events in 17 patients on placebo (0.02 events/person-year). Rates of other nonfatal adverse events were similar between groups, with pneumonia and other respiratory and cardiovascular events most common. Twenty-eight patients on simvastatin and 30 on placebo died.
Asked why he thinks the STATCOPE study’s negative results didn’t confirm previous positive findings from observational studies including thousands of patients, Dr. Criner speculated that excluding patients with indications for statins may have removed patients with cardiovascular risks who were included in other studies. "I think a lot of the problems we’re seeing for exacerbations in COPD might be related to cardiovascular events in patients who aren’t appropriately treated with statins, who should be," he said.
Rosuvastatin sags in SAILS trial
In the separate double-blind SAILS trial (Statins for Acutely Injured Lungs [ARDS] From Sepsis), enteral rosuvastatin did not decrease mortality, compared with placebo, in 745 patients with sepsis-associated acute respiratory distress syndrome (ARDS). Dr. Jonathon D. Truwit, FCCP, and his associates reported their findings, which were discussed at the ATS meeting, in the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1401520]).
Researchers found that 28.5% of patients on rosuvastatin and 25% on placebo died before hospital discharge or within 60 days if the patient was still in a health care facility, reported Dr. Truwit, professor of medicine at the Medical College of Wisconsin, Madison.
Patients in the rosuvastatin group received a loading dose of 40 mg followed by daily maintenance doses of 20 mg (or 10 mg for patients with a morning serum creatinine level of 2.8 mg/dL or more who were not receiving renal replacement therapy. Treatment continued until the third day of discharge from the ICU, hospital discharge, or death, whichever came first.
Both the rosuvastatin and placebo groups had a mean of 15 ventilator-free days.
Results also did not differ significantly between groups for the 339 patients who were in shock at the start of the study or for 109 patients who had used statins before the study and who underwent a 48-hour washout period before randomization.
Patients on rosuvastatin had a mean of 10.1 days free of renal failure and 10.8 days free of hepatic failure within the first 14 days, both significantly fewer compared with patients on placebo (11 and 11.8 days, respectively). "These differences in organ-failure-free days were small, and their significance may be spurious owing to the number of secondary endpoints analyzed. However, we cannot rule out a detrimental effect of rosuvastatin," the investigators wrote.
The results, combined with previous smaller randomized trials of other statins, suggest no benefits from starting or continuing statin therapy for sepsis-associated ARDS, Dr. Truwit said.
"The finding in observational studies that previous statin use provides a benefit may reflect better access to health care among patients who use statins than among those who do not, with a shorter time to the initiation of antibiotic therapy at the onset of symptoms of infection in statin users," according to the journal article.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes simvastatin. The SAILS trial was sponsored by the NHLBI and by AstraZeneca, which makes rosuvastatin. Dr. Truwit reported having no financial disclosures. Several of his coinvestigators reported financial ties to AstraZeneca and other companies.
On Twitter @sherryboschert
Dr. Eric Gartman, FCCP, comments: The results of these two studies represent two poignant examples of the importance of rigorous trial design and patience prior to changing clinical practice. As has been the case with many interventions in pulmonary and critical care medicine, the conclusions of observational studies were not replicated or contradicted when subjected to more structured study design. The data from these two studies should elicit a thoughtful pause in those who have been overheard stating, "We should just put statins in the water."
Dr. Eric Gartman, FCCP, comments: The results of these two studies represent two poignant examples of the importance of rigorous trial design and patience prior to changing clinical practice. As has been the case with many interventions in pulmonary and critical care medicine, the conclusions of observational studies were not replicated or contradicted when subjected to more structured study design. The data from these two studies should elicit a thoughtful pause in those who have been overheard stating, "We should just put statins in the water."
Dr. Eric Gartman, FCCP, comments: The results of these two studies represent two poignant examples of the importance of rigorous trial design and patience prior to changing clinical practice. As has been the case with many interventions in pulmonary and critical care medicine, the conclusions of observational studies were not replicated or contradicted when subjected to more structured study design. The data from these two studies should elicit a thoughtful pause in those who have been overheard stating, "We should just put statins in the water."
SAN DIEGO – Two separate prospective, multicenter trials of statins stopped early when interim results showed they did not help – and potentially harmed – patients with moderate to severe chronic obstructive pulmonary disease or sepsis-associated acute respiratory distress syndrome.
The findings contradict previous observational data suggesting that the potential anti-inflammatory effects of statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors [HMG-CoA]) might benefit patients with these two diseases.
Statins did not significantly reduce rates of exacerbation of chronic obstructive pulmonary disease (COPD) or the time to first exacerbation in a study of 885 patients with moderate to severe COPD who were at high risk for exacerbations and who did not require statins for other indications. Patients in the STATCOPE study (Prospective Randomized Placebo-Controlled Trial of Simvastatin in the Prevention of COPD) received a daily oral dose of either 40 mg simvastatin or placebo for 12-36 months.
The simvastatin group had a mean of 1.36 exacerbations/person-year, compared with 1.39/person-year in the placebo group. The median number of days to the first exacerbation was 223 on simvastatin and 231 on placebo, differences that were not significant, Dr. Gerard J. Criner and his associates reported at an international conference of the American Thoracic Society.
The results were published online by the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1403086]).
Among the 885 patients for whom follow-up information was available, 1,982 acute COPD exacerbations occurred, 965 in 430 patients on simvastatin and 1,017 exacerbations in 447 patients on placebo, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia.
Overall, 34% of patients had three or more exacerbations of COPD, with similar numbers in each group – 141 in the simvastatin group and 155 in the placebo groups. The proportions of patients who received glucocorticoid therapy or antibiotics for exacerbations did not differ significantly between groups.
The simvastatin group had a significantly higher rate of nonfatal serious adverse events involving the GI tract (mainly nausea and bloating from simvastatin) in 30 patients (0.05 events/person-year), compared with events in 17 patients on placebo (0.02 events/person-year). Rates of other nonfatal adverse events were similar between groups, with pneumonia and other respiratory and cardiovascular events most common. Twenty-eight patients on simvastatin and 30 on placebo died.
Asked why he thinks the STATCOPE study’s negative results didn’t confirm previous positive findings from observational studies including thousands of patients, Dr. Criner speculated that excluding patients with indications for statins may have removed patients with cardiovascular risks who were included in other studies. "I think a lot of the problems we’re seeing for exacerbations in COPD might be related to cardiovascular events in patients who aren’t appropriately treated with statins, who should be," he said.
Rosuvastatin sags in SAILS trial
In the separate double-blind SAILS trial (Statins for Acutely Injured Lungs [ARDS] From Sepsis), enteral rosuvastatin did not decrease mortality, compared with placebo, in 745 patients with sepsis-associated acute respiratory distress syndrome (ARDS). Dr. Jonathon D. Truwit, FCCP, and his associates reported their findings, which were discussed at the ATS meeting, in the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1401520]).
Researchers found that 28.5% of patients on rosuvastatin and 25% on placebo died before hospital discharge or within 60 days if the patient was still in a health care facility, reported Dr. Truwit, professor of medicine at the Medical College of Wisconsin, Madison.
Patients in the rosuvastatin group received a loading dose of 40 mg followed by daily maintenance doses of 20 mg (or 10 mg for patients with a morning serum creatinine level of 2.8 mg/dL or more who were not receiving renal replacement therapy. Treatment continued until the third day of discharge from the ICU, hospital discharge, or death, whichever came first.
Both the rosuvastatin and placebo groups had a mean of 15 ventilator-free days.
Results also did not differ significantly between groups for the 339 patients who were in shock at the start of the study or for 109 patients who had used statins before the study and who underwent a 48-hour washout period before randomization.
Patients on rosuvastatin had a mean of 10.1 days free of renal failure and 10.8 days free of hepatic failure within the first 14 days, both significantly fewer compared with patients on placebo (11 and 11.8 days, respectively). "These differences in organ-failure-free days were small, and their significance may be spurious owing to the number of secondary endpoints analyzed. However, we cannot rule out a detrimental effect of rosuvastatin," the investigators wrote.
The results, combined with previous smaller randomized trials of other statins, suggest no benefits from starting or continuing statin therapy for sepsis-associated ARDS, Dr. Truwit said.
"The finding in observational studies that previous statin use provides a benefit may reflect better access to health care among patients who use statins than among those who do not, with a shorter time to the initiation of antibiotic therapy at the onset of symptoms of infection in statin users," according to the journal article.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes simvastatin. The SAILS trial was sponsored by the NHLBI and by AstraZeneca, which makes rosuvastatin. Dr. Truwit reported having no financial disclosures. Several of his coinvestigators reported financial ties to AstraZeneca and other companies.
On Twitter @sherryboschert
SAN DIEGO – Two separate prospective, multicenter trials of statins stopped early when interim results showed they did not help – and potentially harmed – patients with moderate to severe chronic obstructive pulmonary disease or sepsis-associated acute respiratory distress syndrome.
The findings contradict previous observational data suggesting that the potential anti-inflammatory effects of statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors [HMG-CoA]) might benefit patients with these two diseases.
Statins did not significantly reduce rates of exacerbation of chronic obstructive pulmonary disease (COPD) or the time to first exacerbation in a study of 885 patients with moderate to severe COPD who were at high risk for exacerbations and who did not require statins for other indications. Patients in the STATCOPE study (Prospective Randomized Placebo-Controlled Trial of Simvastatin in the Prevention of COPD) received a daily oral dose of either 40 mg simvastatin or placebo for 12-36 months.
The simvastatin group had a mean of 1.36 exacerbations/person-year, compared with 1.39/person-year in the placebo group. The median number of days to the first exacerbation was 223 on simvastatin and 231 on placebo, differences that were not significant, Dr. Gerard J. Criner and his associates reported at an international conference of the American Thoracic Society.
The results were published online by the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1403086]).
Among the 885 patients for whom follow-up information was available, 1,982 acute COPD exacerbations occurred, 965 in 430 patients on simvastatin and 1,017 exacerbations in 447 patients on placebo, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia.
Overall, 34% of patients had three or more exacerbations of COPD, with similar numbers in each group – 141 in the simvastatin group and 155 in the placebo groups. The proportions of patients who received glucocorticoid therapy or antibiotics for exacerbations did not differ significantly between groups.
The simvastatin group had a significantly higher rate of nonfatal serious adverse events involving the GI tract (mainly nausea and bloating from simvastatin) in 30 patients (0.05 events/person-year), compared with events in 17 patients on placebo (0.02 events/person-year). Rates of other nonfatal adverse events were similar between groups, with pneumonia and other respiratory and cardiovascular events most common. Twenty-eight patients on simvastatin and 30 on placebo died.
Asked why he thinks the STATCOPE study’s negative results didn’t confirm previous positive findings from observational studies including thousands of patients, Dr. Criner speculated that excluding patients with indications for statins may have removed patients with cardiovascular risks who were included in other studies. "I think a lot of the problems we’re seeing for exacerbations in COPD might be related to cardiovascular events in patients who aren’t appropriately treated with statins, who should be," he said.
Rosuvastatin sags in SAILS trial
In the separate double-blind SAILS trial (Statins for Acutely Injured Lungs [ARDS] From Sepsis), enteral rosuvastatin did not decrease mortality, compared with placebo, in 745 patients with sepsis-associated acute respiratory distress syndrome (ARDS). Dr. Jonathon D. Truwit, FCCP, and his associates reported their findings, which were discussed at the ATS meeting, in the New England Journal of Medicine (2014 May 18 [doi:10.1056/NEJMoa1401520]).
Researchers found that 28.5% of patients on rosuvastatin and 25% on placebo died before hospital discharge or within 60 days if the patient was still in a health care facility, reported Dr. Truwit, professor of medicine at the Medical College of Wisconsin, Madison.
Patients in the rosuvastatin group received a loading dose of 40 mg followed by daily maintenance doses of 20 mg (or 10 mg for patients with a morning serum creatinine level of 2.8 mg/dL or more who were not receiving renal replacement therapy. Treatment continued until the third day of discharge from the ICU, hospital discharge, or death, whichever came first.
Both the rosuvastatin and placebo groups had a mean of 15 ventilator-free days.
Results also did not differ significantly between groups for the 339 patients who were in shock at the start of the study or for 109 patients who had used statins before the study and who underwent a 48-hour washout period before randomization.
Patients on rosuvastatin had a mean of 10.1 days free of renal failure and 10.8 days free of hepatic failure within the first 14 days, both significantly fewer compared with patients on placebo (11 and 11.8 days, respectively). "These differences in organ-failure-free days were small, and their significance may be spurious owing to the number of secondary endpoints analyzed. However, we cannot rule out a detrimental effect of rosuvastatin," the investigators wrote.
The results, combined with previous smaller randomized trials of other statins, suggest no benefits from starting or continuing statin therapy for sepsis-associated ARDS, Dr. Truwit said.
"The finding in observational studies that previous statin use provides a benefit may reflect better access to health care among patients who use statins than among those who do not, with a shorter time to the initiation of antibiotic therapy at the onset of symptoms of infection in statin users," according to the journal article.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes simvastatin. The SAILS trial was sponsored by the NHLBI and by AstraZeneca, which makes rosuvastatin. Dr. Truwit reported having no financial disclosures. Several of his coinvestigators reported financial ties to AstraZeneca and other companies.
On Twitter @sherryboschert
Key clinical point: Statins did not help, and possibly harmed, patients with moderate to severe COPD or sepsis-associated ARDS who did not require statins for other indications.
Major finding: The mean rate of COPD exacerbations was 1.36 in the simvastatin group and 1.39 in the placebo group, not significantly different.
Data source: STATCOPE, a multicenter prospective randomized, placebo-controlled trial of daily oral simvastatin 40 mg or placebo in 885 patients with COPD at high risk for exacerbations.
Disclosures: The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded STATCOPE. Several coinvestigators reported financial associations with dozens of companies, including with Merck, which makes simvastatin.
Home-based OSA testing costs less than lab-based testing
SAN DIEGO – Home-based testing for obstructive sleep apnea averaged $564 less than laboratory-based testing and did not increase other costs or produce clinically inferior outcomes, based on data from a study of Veterans Affairs patients.
"If you do the home testing approach, that saves you money right off the bat, compared with laboratory testing," Dr. Charles W. Atwood, FCCP, associate professor of medicine at the University of Pittsburgh, said in an interview in advance of an international conference of the American Thoracic Society.
"Everything else for the patients is pretty comparable," he said. "That’s a good thing for people in favor of home testing. People don’t have deleterious outcomes because they were evaluated in the home setting, or because treatment was initiated in the home setting instead of a laboratory setting. People don’t generate more health care bills because they were evaluated in the home instead of in a lab."
In what he characterized as the most comprehensive study of its kind, Dr. Atwood, also director of the sleep disorders program for the VA Pittsburgh Health Care System and his associates enrolled 296 patients from two VA sites who were randomized to standard in-laboratory polysomnography testing (lab group) or unattended home testing (home group). Patients in the home group underwent overnight recording with an Embla type 3 portable monitor followed by at least three nights of using a Philips Respironics auto-titrating positive airway pressure apparatus.
The researchers obtained data from case report forms, staff logs, and VA records, and categorized the costs as sleep-related, pharmaceutical, lab, hospital, or "other."
The majority of participants (95%) were male. Of the 296 patients, 223 (110 in the lab group and 113 in the home group) were initiated on continuous positive airway pressure (CPAP).
After an average follow-up of 2.75 years, the researchers determined that home-based testing costs were $564 lower, compared with lab-based testing (an average per-patient cost of $4,057 vs. $4,621, respectively; P = .007). Differences in the other four categories of cost did not reach statistical significance, with P values ranging between .19 and .82. Results of the Functional Outcomes of Sleep Questionnaire revealed no statistical difference in clinical outcomes between the two groups.
 |
|
Dr. Paul A. Selecky, FCCP, comments: Most doctors who practice sleep medicine would agree with these results, always considering that certain patients would not perform a home study well, such as the frail elderly patients. What is interesting in this study is that patients with comorbidities were not excluded, and yet the outcome was no different.
 |
|
Dr. Paul A. Selecky, FCCP, comments: Most doctors who practice sleep medicine would agree with these results, always considering that certain patients would not perform a home study well, such as the frail elderly patients. What is interesting in this study is that patients with comorbidities were not excluded, and yet the outcome was no different.
 |
|
Dr. Paul A. Selecky, FCCP, comments: Most doctors who practice sleep medicine would agree with these results, always considering that certain patients would not perform a home study well, such as the frail elderly patients. What is interesting in this study is that patients with comorbidities were not excluded, and yet the outcome was no different.
SAN DIEGO – Home-based testing for obstructive sleep apnea averaged $564 less than laboratory-based testing and did not increase other costs or produce clinically inferior outcomes, based on data from a study of Veterans Affairs patients.
"If you do the home testing approach, that saves you money right off the bat, compared with laboratory testing," Dr. Charles W. Atwood, FCCP, associate professor of medicine at the University of Pittsburgh, said in an interview in advance of an international conference of the American Thoracic Society.
"Everything else for the patients is pretty comparable," he said. "That’s a good thing for people in favor of home testing. People don’t have deleterious outcomes because they were evaluated in the home setting, or because treatment was initiated in the home setting instead of a laboratory setting. People don’t generate more health care bills because they were evaluated in the home instead of in a lab."
In what he characterized as the most comprehensive study of its kind, Dr. Atwood, also director of the sleep disorders program for the VA Pittsburgh Health Care System and his associates enrolled 296 patients from two VA sites who were randomized to standard in-laboratory polysomnography testing (lab group) or unattended home testing (home group). Patients in the home group underwent overnight recording with an Embla type 3 portable monitor followed by at least three nights of using a Philips Respironics auto-titrating positive airway pressure apparatus.
The researchers obtained data from case report forms, staff logs, and VA records, and categorized the costs as sleep-related, pharmaceutical, lab, hospital, or "other."
The majority of participants (95%) were male. Of the 296 patients, 223 (110 in the lab group and 113 in the home group) were initiated on continuous positive airway pressure (CPAP).
After an average follow-up of 2.75 years, the researchers determined that home-based testing costs were $564 lower, compared with lab-based testing (an average per-patient cost of $4,057 vs. $4,621, respectively; P = .007). Differences in the other four categories of cost did not reach statistical significance, with P values ranging between .19 and .82. Results of the Functional Outcomes of Sleep Questionnaire revealed no statistical difference in clinical outcomes between the two groups.
SAN DIEGO – Home-based testing for obstructive sleep apnea averaged $564 less than laboratory-based testing and did not increase other costs or produce clinically inferior outcomes, based on data from a study of Veterans Affairs patients.
"If you do the home testing approach, that saves you money right off the bat, compared with laboratory testing," Dr. Charles W. Atwood, FCCP, associate professor of medicine at the University of Pittsburgh, said in an interview in advance of an international conference of the American Thoracic Society.
"Everything else for the patients is pretty comparable," he said. "That’s a good thing for people in favor of home testing. People don’t have deleterious outcomes because they were evaluated in the home setting, or because treatment was initiated in the home setting instead of a laboratory setting. People don’t generate more health care bills because they were evaluated in the home instead of in a lab."
In what he characterized as the most comprehensive study of its kind, Dr. Atwood, also director of the sleep disorders program for the VA Pittsburgh Health Care System and his associates enrolled 296 patients from two VA sites who were randomized to standard in-laboratory polysomnography testing (lab group) or unattended home testing (home group). Patients in the home group underwent overnight recording with an Embla type 3 portable monitor followed by at least three nights of using a Philips Respironics auto-titrating positive airway pressure apparatus.
The researchers obtained data from case report forms, staff logs, and VA records, and categorized the costs as sleep-related, pharmaceutical, lab, hospital, or "other."
The majority of participants (95%) were male. Of the 296 patients, 223 (110 in the lab group and 113 in the home group) were initiated on continuous positive airway pressure (CPAP).
After an average follow-up of 2.75 years, the researchers determined that home-based testing costs were $564 lower, compared with lab-based testing (an average per-patient cost of $4,057 vs. $4,621, respectively; P = .007). Differences in the other four categories of cost did not reach statistical significance, with P values ranging between .19 and .82. Results of the Functional Outcomes of Sleep Questionnaire revealed no statistical difference in clinical outcomes between the two groups.
Key clinical point: Patients did not have poor outcomes because they were evaluated in the home setting, or because treatment was initiated in the home setting instead of a laboratory setting.
Major finding: Home-based testing costs for obstructive sleep apnea were $564 lower, compared with lab-based testing costs, after a follow-up of 2.75 years.
Data source: 296 patients from two VA sites who were randomized to standard in-laboratory polysomnography testing or unattended home testing.
Disclosures: Embla provided the portable monitors used in the study, and Philips Respironics provided the auto-titrating CPAP apparatus. The study was funded by the VA’s Health Research and Development Service. Dr. Atwood had no relevant financial conflicts to disclose.
CPAP compliance similar among patients treated in primary care and sleep clinics
SAN DIEGO – Among patients diagnosed with obstructive sleep apnea, compliance with continuous positive airway pressure devices was similar whether they received treatment in a primary care clinic or in a sleep clinic, results from a Spanish study demonstrated.
However, after 6 months of follow-up, patients who received treatment in a sleep clinic had significantly better Epworth Sleepiness Scale (ESS) scores and ratings of satisfaction, compared with those who received treatment in a primary care clinic.
"OSA affects 4%-6% of the adult population, but only 10% of those with severe disease are treated," Dr. Ferran Barbé said at an international conference of the American Thoracic Society. "In all prevalent and chronic disease, all levels of assistance must be implicated."
In a controlled, noninferiority study, Dr. Barbé and his associates randomized 210 patients diagnosed with obstructive sleep apnea to receive management of continuous positive airway pressure (CPAP) compliance in one of two settings: 100 to one of eight primary care clinics in the region of Lleida, Spain, and 110 to the sleep unit at the University of Lleida. The main outcome was CPAP compliance at 6 months of follow-up. Secondary outcomes included change in the EuroQol scale score, patient satisfaction based on a 10-point visual analog scale, and the change in the ESS score.
The mean age of study participants was 56 years, and 80% were men. CPAP compliance was similar between patients in the sleep clinic group and those in the primary care group (a mean of 5.2 vs. 4.9 hr/day, respectively; P = .28), as was the change in EuroQol scale score (a mean change of 0.17; P = .49). However, patients in the sleep clinic group reported significantly higher rates of satisfaction, compared with their counterparts in the primary care group (a score of 9 vs. 7.5; P less than .001). They also demonstrated significantly greater changes in ESS score (–6.07 vs. –4.09; P = .04).
Overall treatment costs were less expensive in the primary care group, compared with the sleep clinic group.
Primary care physicians "need to reinforce actions that improve self-reported well-being in OSA patients," Dr. Barbé concluded.
The study was supported by the Instituto de Salud Carlos III, the Spanish Society of Pulmonology and Thoracic Surgery, Societat Catalana de Pneumologia, and ALLER (Respiratory Association of Lleida). Dr. Barbé said he had no relevant financial conflicts to disclose.
SAN DIEGO – Among patients diagnosed with obstructive sleep apnea, compliance with continuous positive airway pressure devices was similar whether they received treatment in a primary care clinic or in a sleep clinic, results from a Spanish study demonstrated.
However, after 6 months of follow-up, patients who received treatment in a sleep clinic had significantly better Epworth Sleepiness Scale (ESS) scores and ratings of satisfaction, compared with those who received treatment in a primary care clinic.
"OSA affects 4%-6% of the adult population, but only 10% of those with severe disease are treated," Dr. Ferran Barbé said at an international conference of the American Thoracic Society. "In all prevalent and chronic disease, all levels of assistance must be implicated."
In a controlled, noninferiority study, Dr. Barbé and his associates randomized 210 patients diagnosed with obstructive sleep apnea to receive management of continuous positive airway pressure (CPAP) compliance in one of two settings: 100 to one of eight primary care clinics in the region of Lleida, Spain, and 110 to the sleep unit at the University of Lleida. The main outcome was CPAP compliance at 6 months of follow-up. Secondary outcomes included change in the EuroQol scale score, patient satisfaction based on a 10-point visual analog scale, and the change in the ESS score.
The mean age of study participants was 56 years, and 80% were men. CPAP compliance was similar between patients in the sleep clinic group and those in the primary care group (a mean of 5.2 vs. 4.9 hr/day, respectively; P = .28), as was the change in EuroQol scale score (a mean change of 0.17; P = .49). However, patients in the sleep clinic group reported significantly higher rates of satisfaction, compared with their counterparts in the primary care group (a score of 9 vs. 7.5; P less than .001). They also demonstrated significantly greater changes in ESS score (–6.07 vs. –4.09; P = .04).
Overall treatment costs were less expensive in the primary care group, compared with the sleep clinic group.
Primary care physicians "need to reinforce actions that improve self-reported well-being in OSA patients," Dr. Barbé concluded.
The study was supported by the Instituto de Salud Carlos III, the Spanish Society of Pulmonology and Thoracic Surgery, Societat Catalana de Pneumologia, and ALLER (Respiratory Association of Lleida). Dr. Barbé said he had no relevant financial conflicts to disclose.
SAN DIEGO – Among patients diagnosed with obstructive sleep apnea, compliance with continuous positive airway pressure devices was similar whether they received treatment in a primary care clinic or in a sleep clinic, results from a Spanish study demonstrated.
However, after 6 months of follow-up, patients who received treatment in a sleep clinic had significantly better Epworth Sleepiness Scale (ESS) scores and ratings of satisfaction, compared with those who received treatment in a primary care clinic.
"OSA affects 4%-6% of the adult population, but only 10% of those with severe disease are treated," Dr. Ferran Barbé said at an international conference of the American Thoracic Society. "In all prevalent and chronic disease, all levels of assistance must be implicated."
In a controlled, noninferiority study, Dr. Barbé and his associates randomized 210 patients diagnosed with obstructive sleep apnea to receive management of continuous positive airway pressure (CPAP) compliance in one of two settings: 100 to one of eight primary care clinics in the region of Lleida, Spain, and 110 to the sleep unit at the University of Lleida. The main outcome was CPAP compliance at 6 months of follow-up. Secondary outcomes included change in the EuroQol scale score, patient satisfaction based on a 10-point visual analog scale, and the change in the ESS score.
The mean age of study participants was 56 years, and 80% were men. CPAP compliance was similar between patients in the sleep clinic group and those in the primary care group (a mean of 5.2 vs. 4.9 hr/day, respectively; P = .28), as was the change in EuroQol scale score (a mean change of 0.17; P = .49). However, patients in the sleep clinic group reported significantly higher rates of satisfaction, compared with their counterparts in the primary care group (a score of 9 vs. 7.5; P less than .001). They also demonstrated significantly greater changes in ESS score (–6.07 vs. –4.09; P = .04).
Overall treatment costs were less expensive in the primary care group, compared with the sleep clinic group.
Primary care physicians "need to reinforce actions that improve self-reported well-being in OSA patients," Dr. Barbé concluded.
The study was supported by the Instituto de Salud Carlos III, the Spanish Society of Pulmonology and Thoracic Surgery, Societat Catalana de Pneumologia, and ALLER (Respiratory Association of Lleida). Dr. Barbé said he had no relevant financial conflicts to disclose.
AT ATS 2014
Key clinical point: Among patients with obstructive sleep apnea, compliance with CPAP devices in a primary care clinic setting was similar to that in a sleep clinic setting.
Major finding: CPAP compliance was similar between patients in the sleep clinic group and those in the primary care group (a mean of 5.2 vs. 4.9 hr/day, respectively; P = .28), as was the change in EuroQol scale scores (a mean change of 0.17; P = .49).
Data source: A controlled, noninferiority study of 210 patients diagnosed with obstructive sleep apnea who were randomized to receive management of CPAP compliance in one of two settings: 100 to one of eight primary care clinics in the region of Lleida, Spain, and 110 to the sleep unit at the University of Lleida.
Disclosures: The study was supported by the Instituto de Salud Carlos III, the Spanish Society of Pulmonology and Thoracic Surgery, and the Societat Catalana de Pneumologia. Dr. Barbé said that he had no relevant financial conflicts to disclose.
Subsyndromal delirium common in critically ill patients
SAN DIEGO – Subsyndromal delirium was present in 86% of critically ill patients, results from a large observational study demonstrated. In addition, the duration of delirium was associated with increased odds of institutionalization, an association that was modified by the duration of delirium.
"In patients with less delirium, the effect of subsyndromal delirium on institutionalization was actually stronger," lead author Dr. Nathan E. Brummel said in an interview at an international conference of the American Thoracic Society, where the research was presented. "This identifies a cohort of people who previously were considered to have normal brain function, but it appears that this has long-term implications for their lives.
"Screening for delirium should occur not only in the ICU but on the wards as well. Patients who have delirium or delirium symptoms may benefit from measures used to prevent and treat this syndrome, such as the Hospital Elder Life Program, routine mobilization, and frequent reorientation through the use of nursing staff or even family members," he later added. This study data may help clinicians discuss long-term outcomes of critical illness with patients and their family members," he said.
For the study, Dr. Brummel, an instructor in medicine in the division of allergy, pulmonary and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates evaluated 821 medical or surgical ICU patients with respiratory failure and/or shock who were enrolled in the BRAIN-ICU observational cohort study (N. Engl. J. Med. 2013;369:1306-16).
They used the Confusion Assessment Method for the ICU (CAM-ICU) to screen for delirium symptoms twice daily in the ICU and daily thereafter. The researchers considered delirium to be present if the CAM-ICU was positive. If the CAM-ICU was negative, they considered subsyndromal delirium (SSD) to be present if any delirium features were present or if inattention was present with or without other features of delirium.
SSD "is said to be present when a patient exhibits some delirium symptoms but does not meet the full delirium diagnostic criteria," the researchers wrote in their poster. "In patients without critical illness, SSD is associated with institutionalization, mortality, and cognitive decline, but these associations remain unclear in the critically ill."
The researchers tracked discharge location, mortality after hospital discharge and assessed for cognitive impairment at 3 and 12 months follow-up and used multivariate regression to determine the relationship between days of SSD and outcomes.
The mean age of the 821 patients was 61 years and their mean APACHE II score was 25. In all, 702 patients (86%) had SSD that lasted an average of 3 days. The most common SSU pattern based on the CAM-ICU was fluctuation of mental status (which occurred in 50% of assessments) and fluctuation in mental status plus altered level of consciousness (which occurred in 22% of assessments).
Dr. Brummel and his associates also found that the duration of SSD was independently associated with increased odds of institutionalization (odds ratio, 1.90), but SSD did not predict mortality or long-term cognitive impairment at 3 or 12 months. "We don’t yet understand the mechanism behind why subsyndromal delirium and institutionalization are associated," Dr. Brummel said. "It probably relates to an association between SSD and factors that drive institutionalization, such as physical disability and cognitive impairment. Once patients survived the hospital stay, subsyndromal delirium wasn’t associated with an increased risk of mortality. It may be the fact that this less severe form of brain dysfunction in the ICU does not have the same effect as the full syndrome of delirium."
He acknowledged certain limitations of the study, including the fact that the CAM-ICU only measures four features of delirium and that no assessments of cognitive or physical function were conducted at hospital discharge.
The study was supported by the National Institutes of Health, the Vanderbilt Clinical and Translational Scholars Program, and the Veterans Affairs Tennessee Valley Healthcare System Geriatric Research Education and Clinical Centers. Dr. Brummel said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Subsyndromal delirium was present in 86% of critically ill patients, results from a large observational study demonstrated. In addition, the duration of delirium was associated with increased odds of institutionalization, an association that was modified by the duration of delirium.
"In patients with less delirium, the effect of subsyndromal delirium on institutionalization was actually stronger," lead author Dr. Nathan E. Brummel said in an interview at an international conference of the American Thoracic Society, where the research was presented. "This identifies a cohort of people who previously were considered to have normal brain function, but it appears that this has long-term implications for their lives.
"Screening for delirium should occur not only in the ICU but on the wards as well. Patients who have delirium or delirium symptoms may benefit from measures used to prevent and treat this syndrome, such as the Hospital Elder Life Program, routine mobilization, and frequent reorientation through the use of nursing staff or even family members," he later added. This study data may help clinicians discuss long-term outcomes of critical illness with patients and their family members," he said.
For the study, Dr. Brummel, an instructor in medicine in the division of allergy, pulmonary and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates evaluated 821 medical or surgical ICU patients with respiratory failure and/or shock who were enrolled in the BRAIN-ICU observational cohort study (N. Engl. J. Med. 2013;369:1306-16).
They used the Confusion Assessment Method for the ICU (CAM-ICU) to screen for delirium symptoms twice daily in the ICU and daily thereafter. The researchers considered delirium to be present if the CAM-ICU was positive. If the CAM-ICU was negative, they considered subsyndromal delirium (SSD) to be present if any delirium features were present or if inattention was present with or without other features of delirium.
SSD "is said to be present when a patient exhibits some delirium symptoms but does not meet the full delirium diagnostic criteria," the researchers wrote in their poster. "In patients without critical illness, SSD is associated with institutionalization, mortality, and cognitive decline, but these associations remain unclear in the critically ill."
The researchers tracked discharge location, mortality after hospital discharge and assessed for cognitive impairment at 3 and 12 months follow-up and used multivariate regression to determine the relationship between days of SSD and outcomes.
The mean age of the 821 patients was 61 years and their mean APACHE II score was 25. In all, 702 patients (86%) had SSD that lasted an average of 3 days. The most common SSU pattern based on the CAM-ICU was fluctuation of mental status (which occurred in 50% of assessments) and fluctuation in mental status plus altered level of consciousness (which occurred in 22% of assessments).
Dr. Brummel and his associates also found that the duration of SSD was independently associated with increased odds of institutionalization (odds ratio, 1.90), but SSD did not predict mortality or long-term cognitive impairment at 3 or 12 months. "We don’t yet understand the mechanism behind why subsyndromal delirium and institutionalization are associated," Dr. Brummel said. "It probably relates to an association between SSD and factors that drive institutionalization, such as physical disability and cognitive impairment. Once patients survived the hospital stay, subsyndromal delirium wasn’t associated with an increased risk of mortality. It may be the fact that this less severe form of brain dysfunction in the ICU does not have the same effect as the full syndrome of delirium."
He acknowledged certain limitations of the study, including the fact that the CAM-ICU only measures four features of delirium and that no assessments of cognitive or physical function were conducted at hospital discharge.
The study was supported by the National Institutes of Health, the Vanderbilt Clinical and Translational Scholars Program, and the Veterans Affairs Tennessee Valley Healthcare System Geriatric Research Education and Clinical Centers. Dr. Brummel said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Subsyndromal delirium was present in 86% of critically ill patients, results from a large observational study demonstrated. In addition, the duration of delirium was associated with increased odds of institutionalization, an association that was modified by the duration of delirium.
"In patients with less delirium, the effect of subsyndromal delirium on institutionalization was actually stronger," lead author Dr. Nathan E. Brummel said in an interview at an international conference of the American Thoracic Society, where the research was presented. "This identifies a cohort of people who previously were considered to have normal brain function, but it appears that this has long-term implications for their lives.
"Screening for delirium should occur not only in the ICU but on the wards as well. Patients who have delirium or delirium symptoms may benefit from measures used to prevent and treat this syndrome, such as the Hospital Elder Life Program, routine mobilization, and frequent reorientation through the use of nursing staff or even family members," he later added. This study data may help clinicians discuss long-term outcomes of critical illness with patients and their family members," he said.
For the study, Dr. Brummel, an instructor in medicine in the division of allergy, pulmonary and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates evaluated 821 medical or surgical ICU patients with respiratory failure and/or shock who were enrolled in the BRAIN-ICU observational cohort study (N. Engl. J. Med. 2013;369:1306-16).
They used the Confusion Assessment Method for the ICU (CAM-ICU) to screen for delirium symptoms twice daily in the ICU and daily thereafter. The researchers considered delirium to be present if the CAM-ICU was positive. If the CAM-ICU was negative, they considered subsyndromal delirium (SSD) to be present if any delirium features were present or if inattention was present with or without other features of delirium.
SSD "is said to be present when a patient exhibits some delirium symptoms but does not meet the full delirium diagnostic criteria," the researchers wrote in their poster. "In patients without critical illness, SSD is associated with institutionalization, mortality, and cognitive decline, but these associations remain unclear in the critically ill."
The researchers tracked discharge location, mortality after hospital discharge and assessed for cognitive impairment at 3 and 12 months follow-up and used multivariate regression to determine the relationship between days of SSD and outcomes.
The mean age of the 821 patients was 61 years and their mean APACHE II score was 25. In all, 702 patients (86%) had SSD that lasted an average of 3 days. The most common SSU pattern based on the CAM-ICU was fluctuation of mental status (which occurred in 50% of assessments) and fluctuation in mental status plus altered level of consciousness (which occurred in 22% of assessments).
Dr. Brummel and his associates also found that the duration of SSD was independently associated with increased odds of institutionalization (odds ratio, 1.90), but SSD did not predict mortality or long-term cognitive impairment at 3 or 12 months. "We don’t yet understand the mechanism behind why subsyndromal delirium and institutionalization are associated," Dr. Brummel said. "It probably relates to an association between SSD and factors that drive institutionalization, such as physical disability and cognitive impairment. Once patients survived the hospital stay, subsyndromal delirium wasn’t associated with an increased risk of mortality. It may be the fact that this less severe form of brain dysfunction in the ICU does not have the same effect as the full syndrome of delirium."
He acknowledged certain limitations of the study, including the fact that the CAM-ICU only measures four features of delirium and that no assessments of cognitive or physical function were conducted at hospital discharge.
The study was supported by the National Institutes of Health, the Vanderbilt Clinical and Translational Scholars Program, and the Veterans Affairs Tennessee Valley Healthcare System Geriatric Research Education and Clinical Centers. Dr. Brummel said that he had no relevant financial conflicts to disclose.
AT ATS 2014
Key clinical point: Patients who have even a few delirium symptoms may benefit from prevention and treatment measures.
Major finding: Among 821 critically ill patients, 702 (86%) had subsyndromal delirium that lasted an average of 3 days.
Data source: An evaluation of 821 medical or surgical ICU patients with respiratory failure and/or shock who were enrolled in the BRAIN-ICU observational cohort study.
Disclosures: The study was supported by the National Institutes of Health, the Vanderbilt Clinical and Translational Scholars Program, and the VA Tennessee Valley Healthcare System Geriatric Research Education and Clinical Centers. Dr. Brummel had no financial conflicts.
VIDEO: Statins in COPD may focus on subgroups
SAN DIEGO – Although statins failed to improve lung function or exacerbations of chronic obstructive pulmonary disease in several large studies presented at an international conference of the American Thoracic Society, a small caveat appeared in a trial by Dr. Anke Neukamm and her associates.
Rosuvastatin improved endothelial function in a subgroup of patients who had high levels of C-reactive protein before treatment, a prespecified analysis found.
Dr. Neukamm of Akershus University, Lørenskog, Norway, explained what her findings might mean for further research into the role of statins in patients with COPD, if any.
Her study was funded by the Norwegian Extra Foundation for Health and Rehabilitation and by AstraZeneca, which makes a brand-name formulation of rosuvastatin. Dr. Neukamm has been a speaker for AstraZeneca.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Although statins failed to improve lung function or exacerbations of chronic obstructive pulmonary disease in several large studies presented at an international conference of the American Thoracic Society, a small caveat appeared in a trial by Dr. Anke Neukamm and her associates.
Rosuvastatin improved endothelial function in a subgroup of patients who had high levels of C-reactive protein before treatment, a prespecified analysis found.
Dr. Neukamm of Akershus University, Lørenskog, Norway, explained what her findings might mean for further research into the role of statins in patients with COPD, if any.
Her study was funded by the Norwegian Extra Foundation for Health and Rehabilitation and by AstraZeneca, which makes a brand-name formulation of rosuvastatin. Dr. Neukamm has been a speaker for AstraZeneca.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Although statins failed to improve lung function or exacerbations of chronic obstructive pulmonary disease in several large studies presented at an international conference of the American Thoracic Society, a small caveat appeared in a trial by Dr. Anke Neukamm and her associates.
Rosuvastatin improved endothelial function in a subgroup of patients who had high levels of C-reactive protein before treatment, a prespecified analysis found.
Dr. Neukamm of Akershus University, Lørenskog, Norway, explained what her findings might mean for further research into the role of statins in patients with COPD, if any.
Her study was funded by the Norwegian Extra Foundation for Health and Rehabilitation and by AstraZeneca, which makes a brand-name formulation of rosuvastatin. Dr. Neukamm has been a speaker for AstraZeneca.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT ATS 2014
Monoclonal antibody attacks new asthma target
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial-cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, compared with placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ontario.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi:10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study are not the kind of patients who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma. "They use an awful lot of resources and costs in terms of hospital emergency room care. They are the folks who have an unmet need to treat their asthma," she said.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Dr. Gauvreau reported financial associations with Amgen and three other companies. Fourteen of her coinvestigators reported financial associations with Amgen and multiple other companies.
The magnitude of the effect of AMG 157 was sizable, similar to what could be achieved in allergen-induced asthma studies by blocking established asthma mediators such as the cysteinyl leukotrienes, Dr. Sven-Erik Dahlén wrote in an editorial accompanying Dr. Gauvreau’s article (N. Engl. J. Med.; 2014 May 20 [doi:10.1056/NEJMe1404737]).
The evidence of an effect from this highly selective anti-thymic stromal lymphopoietin [TSLP] antibody on both the early and late asthmatic responses might be because it directly inhibits interleukin-4 or interleukin-13 (two downstream cytokines induced by TSLP), this study and previous data suggest. There may be two ways to inhibit allergen-induced asthmatic responses, he suggested – direct antagonism of mast-cell mediators to block acute response, or long-term inhibition of regulatory networks. TSLP may be a "master switch" in the signaling between airway epithelium and other inflammatory cascades. Or, it may be part of action by several parallel pathways involving interleukins.
AMG 157 has "earned our respect" in this study, but it’s unclear whether this strategy will succeed in treating patients with asthma, Dr. Dahlén wrote. "We will first have to unravel the biologic mechanisms involved in this unexpected effect of AMG 157 and show why TSLP signaling" contributes to asthmatic responses.
Dr. Dahlén is a professor at the Center for Allergy Research, Institute of Environmental Medicine, Karolinska Institutet, Stockholm. He reported a financial association with AstraZeneca unrelated to this study.
The magnitude of the effect of AMG 157 was sizable, similar to what could be achieved in allergen-induced asthma studies by blocking established asthma mediators such as the cysteinyl leukotrienes, Dr. Sven-Erik Dahlén wrote in an editorial accompanying Dr. Gauvreau’s article (N. Engl. J. Med.; 2014 May 20 [doi:10.1056/NEJMe1404737]).
The evidence of an effect from this highly selective anti-thymic stromal lymphopoietin [TSLP] antibody on both the early and late asthmatic responses might be because it directly inhibits interleukin-4 or interleukin-13 (two downstream cytokines induced by TSLP), this study and previous data suggest. There may be two ways to inhibit allergen-induced asthmatic responses, he suggested – direct antagonism of mast-cell mediators to block acute response, or long-term inhibition of regulatory networks. TSLP may be a "master switch" in the signaling between airway epithelium and other inflammatory cascades. Or, it may be part of action by several parallel pathways involving interleukins.
AMG 157 has "earned our respect" in this study, but it’s unclear whether this strategy will succeed in treating patients with asthma, Dr. Dahlén wrote. "We will first have to unravel the biologic mechanisms involved in this unexpected effect of AMG 157 and show why TSLP signaling" contributes to asthmatic responses.
Dr. Dahlén is a professor at the Center for Allergy Research, Institute of Environmental Medicine, Karolinska Institutet, Stockholm. He reported a financial association with AstraZeneca unrelated to this study.
The magnitude of the effect of AMG 157 was sizable, similar to what could be achieved in allergen-induced asthma studies by blocking established asthma mediators such as the cysteinyl leukotrienes, Dr. Sven-Erik Dahlén wrote in an editorial accompanying Dr. Gauvreau’s article (N. Engl. J. Med.; 2014 May 20 [doi:10.1056/NEJMe1404737]).
The evidence of an effect from this highly selective anti-thymic stromal lymphopoietin [TSLP] antibody on both the early and late asthmatic responses might be because it directly inhibits interleukin-4 or interleukin-13 (two downstream cytokines induced by TSLP), this study and previous data suggest. There may be two ways to inhibit allergen-induced asthmatic responses, he suggested – direct antagonism of mast-cell mediators to block acute response, or long-term inhibition of regulatory networks. TSLP may be a "master switch" in the signaling between airway epithelium and other inflammatory cascades. Or, it may be part of action by several parallel pathways involving interleukins.
AMG 157 has "earned our respect" in this study, but it’s unclear whether this strategy will succeed in treating patients with asthma, Dr. Dahlén wrote. "We will first have to unravel the biologic mechanisms involved in this unexpected effect of AMG 157 and show why TSLP signaling" contributes to asthmatic responses.
Dr. Dahlén is a professor at the Center for Allergy Research, Institute of Environmental Medicine, Karolinska Institutet, Stockholm. He reported a financial association with AstraZeneca unrelated to this study.
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial-cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, compared with placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ontario.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi:10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study are not the kind of patients who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma. "They use an awful lot of resources and costs in terms of hospital emergency room care. They are the folks who have an unmet need to treat their asthma," she said.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Dr. Gauvreau reported financial associations with Amgen and three other companies. Fourteen of her coinvestigators reported financial associations with Amgen and multiple other companies.
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial-cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, compared with placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ontario.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi:10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study are not the kind of patients who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma. "They use an awful lot of resources and costs in terms of hospital emergency room care. They are the folks who have an unmet need to treat their asthma," she said.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Dr. Gauvreau reported financial associations with Amgen and three other companies. Fourteen of her coinvestigators reported financial associations with Amgen and multiple other companies.
AT ATS 2014
Key clinical point: A proof-of-concept study suggests that there may be a new asthma treatment pathway, to be tested next in a phase II clinical trial.
Major finding: The maximum percentage decrease in the FEV1 3-7 hours after allergy challenge was 46% smaller in the treatment group, compared with placebo on day 84 (P = .02)
Data source: A double-blind, placebo-controlled study of 31 patients with mild asthma treated with 3 months of intravenous AMG 157 or placebo assessed after allergen challenge.
Disclosures: Amgen, which is developing AMG 157, funded the study and analyzed the data. Dr. Gauvreau reported financial associations with Amgen and three other companies. Fourteen of her coinvestigators reported financial associations with Amgen and multiple other companies.
VIDEO: Statins flop in COPD, but hope remains
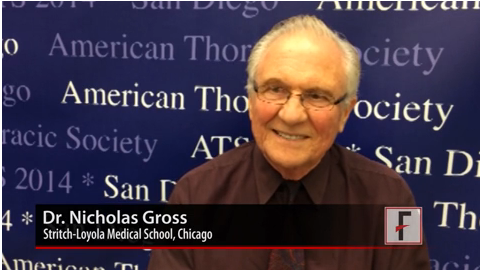
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT ATS 2014
VIDEO: Experimental inhaler targets small airways in asthma
SAN DIEGO – An experimental inhalation system could help patients with asthma who are dependent on chronic oral corticosteroid therapy to reduce their doses of these steroids and potentially their side effects.
A phase II/III study suggests the system helped preserve lung function as oral corticosteroids were reduced, by delivering small budesonide to the peripheral lungs to target small airway inflammation in a randomized, controlled study of 199 patients. The study was presented by an employee of the system’s developer.
What we don’t know yet is whether the new system is better than existing technology such as metered dose inhalers for delivering small-molecule medications for asthma, or can be used in conjunction with them, Dr. Sally E. Wenzel told us in an interview.
Dr. Wenzel, professor of medicine at the University of Pittsburgh, does target the small airways when treating some patients. She provided perspective on this strategy and what may lie ahead.
Dr. Wenzel disclosed financial associations with multiple companies involved in asthma medications.
On Twitter @sherryboschert
SAN DIEGO – An experimental inhalation system could help patients with asthma who are dependent on chronic oral corticosteroid therapy to reduce their doses of these steroids and potentially their side effects.
A phase II/III study suggests the system helped preserve lung function as oral corticosteroids were reduced, by delivering small budesonide to the peripheral lungs to target small airway inflammation in a randomized, controlled study of 199 patients. The study was presented by an employee of the system’s developer.
What we don’t know yet is whether the new system is better than existing technology such as metered dose inhalers for delivering small-molecule medications for asthma, or can be used in conjunction with them, Dr. Sally E. Wenzel told us in an interview.
Dr. Wenzel, professor of medicine at the University of Pittsburgh, does target the small airways when treating some patients. She provided perspective on this strategy and what may lie ahead.
Dr. Wenzel disclosed financial associations with multiple companies involved in asthma medications.
On Twitter @sherryboschert
SAN DIEGO – An experimental inhalation system could help patients with asthma who are dependent on chronic oral corticosteroid therapy to reduce their doses of these steroids and potentially their side effects.
A phase II/III study suggests the system helped preserve lung function as oral corticosteroids were reduced, by delivering small budesonide to the peripheral lungs to target small airway inflammation in a randomized, controlled study of 199 patients. The study was presented by an employee of the system’s developer.
What we don’t know yet is whether the new system is better than existing technology such as metered dose inhalers for delivering small-molecule medications for asthma, or can be used in conjunction with them, Dr. Sally E. Wenzel told us in an interview.
Dr. Wenzel, professor of medicine at the University of Pittsburgh, does target the small airways when treating some patients. She provided perspective on this strategy and what may lie ahead.
Dr. Wenzel disclosed financial associations with multiple companies involved in asthma medications.
On Twitter @sherryboschert
AT THE ATS INTERNATIONAL CONFERENCE
VIDEO: Lessons from statin failure in COPD
SAN DIEGO – The failure of statins in the STATCOPE trial to prevent exacerbations of chronic obstructive pulmonary disease isn’t the only important message of the trial, Dr. Gerard J. Criner said in an interview after he presented the findings at an international conference of the American Thoracic Society.
Previous observational studies of statins in COPD that suggested survival benefits from the drugs probably didn’t screen out patients with indications for statin therapy, as STATCOPE (Statins in COPD Exacerbations) did, for a more pristine assessment, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia. The real message may be that clinicians are missing patients who need statins but aren’t getting them, he suggested.
Dr. Criner also shared his take on other important statin trials presented at the meeting. Take a look.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes a brand name formulation of simvastatin.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – The failure of statins in the STATCOPE trial to prevent exacerbations of chronic obstructive pulmonary disease isn’t the only important message of the trial, Dr. Gerard J. Criner said in an interview after he presented the findings at an international conference of the American Thoracic Society.
Previous observational studies of statins in COPD that suggested survival benefits from the drugs probably didn’t screen out patients with indications for statin therapy, as STATCOPE (Statins in COPD Exacerbations) did, for a more pristine assessment, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia. The real message may be that clinicians are missing patients who need statins but aren’t getting them, he suggested.
Dr. Criner also shared his take on other important statin trials presented at the meeting. Take a look.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes a brand name formulation of simvastatin.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – The failure of statins in the STATCOPE trial to prevent exacerbations of chronic obstructive pulmonary disease isn’t the only important message of the trial, Dr. Gerard J. Criner said in an interview after he presented the findings at an international conference of the American Thoracic Society.
Previous observational studies of statins in COPD that suggested survival benefits from the drugs probably didn’t screen out patients with indications for statin therapy, as STATCOPE (Statins in COPD Exacerbations) did, for a more pristine assessment, said Dr. Criner, professor of medicine and director of the medical intensive care unit and the ventilator rehabilitation unit at Temple University, Philadelphia. The real message may be that clinicians are missing patients who need statins but aren’t getting them, he suggested.
Dr. Criner also shared his take on other important statin trials presented at the meeting. Take a look.
The National Heart, Lung, and Blood Institute and the Canadian Institutes of Health Research funded the STATCOPE trial. The investigators reported financial associations with dozens of companies, including five of Dr. Criner’s coinvestigators who had financial associations with Merck, which makes a brand name formulation of simvastatin.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ATS INTERNATIONAL CONFERENCE
Renal protective effect found for acetaminophen in ICU sepsis
SAN DIEGO – Three days of acetaminophen seemed to lower creatinine levels in severely septic patients, suggesting a renoprotective effect, according to results from a phase II study out of Vanderbilt University in Nashville, Tenn.
Investigators there randomized 18 septic ICU patients to acetaminophen 1 g every 6 hours for 3 days and 22 patients to placebo, both delivered by mouth or feeding tube. The patients had all been in the ICU for less than 24 hours, and had detectable levels of plasma cell-free hemoglobin (CFH).
The findings were presented at an international conference of the American Thoracic Society.
CFH has been associated with death in a number of conditions. The iron separates, radicalizes, and causes oxidative injury, especially to the kidneys. Acetaminophen chemically reduces the iron, and has been shown to counter the harm.
In an earlier observational study, the Vanderbilt team found that detectible CFH is common in ICU sepsis patients, as well as elevated plasma levels of F2-isoprostanes, an indicator of oxidative injury. They also observed that CFH was associated with death, and that exposure to acetaminophen seemed to reduce F2-isoprostanes levels and improve survival.
The findings prompted the phase II investigation. The team found that the acetaminophen group had lower levels of F2-isoprostanes on study day 2 (mean 24.9 pg/mL vs. 41.2 pg/mL; P = .022) and lower levels of serum creatinine on study day 3 (mean 1.0 mg/dL vs. 1.3 mg/dL, P = .039). These differences were significant and the renal benefit persisted throughout hospitalization.
Acetaminophen patients overall started with a lower mean baseline creatinine level (1.63 mg/dL vs. 2.06 mg/dL), so the investigators reran their analysis, excluding patients on renal replacement therapy. "The baseline imbalance went away, and the story remained the same: There was still a significant decrease in serum creatinine in the acetaminophen group," said lead investigator Dr. David Janz, a critical care fellow at Vanderbilt.
Despite a favorable trend, acetaminophen did not improve survival, a secondary outcome; one (5.6%) acetaminophen and four (18.2%) placebo patients died (P = .355).
Still, the results are strong enough to suggest that acetaminophen might one day prove to be "a potent intervention to improve sepsis outcomes. Even small creatinine changes are associated with increased length of stay and mortality," Dr. Janz said.
"Our trial contains some negative results" – most notably no significant effect on day 3 F2-isoprostanes levels – but "the consistent reduction in creatinine across a number of different analyses and the biologic plausibility underlying this signal prompt further investigation. We need larger studies that focus on length of stay and mortality," he said.
Acetaminophen patients were slightly younger (50 vs. 58 years), but besides that and the baseline creatinine difference, the groups were well matched. Both had mean Apache II scores in the low 20s. Nine acetaminophen patients (50%) and seven placebo patients (32%) were intubated.
Both groups received a median of 12 study doses. There was no statistical between-group difference in the number of patients whose AST/ALT topped 400 U/L, a stop-point hit by two acetaminophen patients and one placebo patient (P = .599). No one in the acetaminophen group developed a rash.
Patients who had liver disease or who had gotten acetaminophen within 48 hours were among those excluded from the study.
The work was funded by the National Institutes of Health and the American Heart Association. Dr. Janz had no disclosures.
SAN DIEGO – Three days of acetaminophen seemed to lower creatinine levels in severely septic patients, suggesting a renoprotective effect, according to results from a phase II study out of Vanderbilt University in Nashville, Tenn.
Investigators there randomized 18 septic ICU patients to acetaminophen 1 g every 6 hours for 3 days and 22 patients to placebo, both delivered by mouth or feeding tube. The patients had all been in the ICU for less than 24 hours, and had detectable levels of plasma cell-free hemoglobin (CFH).
The findings were presented at an international conference of the American Thoracic Society.
CFH has been associated with death in a number of conditions. The iron separates, radicalizes, and causes oxidative injury, especially to the kidneys. Acetaminophen chemically reduces the iron, and has been shown to counter the harm.
In an earlier observational study, the Vanderbilt team found that detectible CFH is common in ICU sepsis patients, as well as elevated plasma levels of F2-isoprostanes, an indicator of oxidative injury. They also observed that CFH was associated with death, and that exposure to acetaminophen seemed to reduce F2-isoprostanes levels and improve survival.
The findings prompted the phase II investigation. The team found that the acetaminophen group had lower levels of F2-isoprostanes on study day 2 (mean 24.9 pg/mL vs. 41.2 pg/mL; P = .022) and lower levels of serum creatinine on study day 3 (mean 1.0 mg/dL vs. 1.3 mg/dL, P = .039). These differences were significant and the renal benefit persisted throughout hospitalization.
Acetaminophen patients overall started with a lower mean baseline creatinine level (1.63 mg/dL vs. 2.06 mg/dL), so the investigators reran their analysis, excluding patients on renal replacement therapy. "The baseline imbalance went away, and the story remained the same: There was still a significant decrease in serum creatinine in the acetaminophen group," said lead investigator Dr. David Janz, a critical care fellow at Vanderbilt.
Despite a favorable trend, acetaminophen did not improve survival, a secondary outcome; one (5.6%) acetaminophen and four (18.2%) placebo patients died (P = .355).
Still, the results are strong enough to suggest that acetaminophen might one day prove to be "a potent intervention to improve sepsis outcomes. Even small creatinine changes are associated with increased length of stay and mortality," Dr. Janz said.
"Our trial contains some negative results" – most notably no significant effect on day 3 F2-isoprostanes levels – but "the consistent reduction in creatinine across a number of different analyses and the biologic plausibility underlying this signal prompt further investigation. We need larger studies that focus on length of stay and mortality," he said.
Acetaminophen patients were slightly younger (50 vs. 58 years), but besides that and the baseline creatinine difference, the groups were well matched. Both had mean Apache II scores in the low 20s. Nine acetaminophen patients (50%) and seven placebo patients (32%) were intubated.
Both groups received a median of 12 study doses. There was no statistical between-group difference in the number of patients whose AST/ALT topped 400 U/L, a stop-point hit by two acetaminophen patients and one placebo patient (P = .599). No one in the acetaminophen group developed a rash.
Patients who had liver disease or who had gotten acetaminophen within 48 hours were among those excluded from the study.
The work was funded by the National Institutes of Health and the American Heart Association. Dr. Janz had no disclosures.
SAN DIEGO – Three days of acetaminophen seemed to lower creatinine levels in severely septic patients, suggesting a renoprotective effect, according to results from a phase II study out of Vanderbilt University in Nashville, Tenn.
Investigators there randomized 18 septic ICU patients to acetaminophen 1 g every 6 hours for 3 days and 22 patients to placebo, both delivered by mouth or feeding tube. The patients had all been in the ICU for less than 24 hours, and had detectable levels of plasma cell-free hemoglobin (CFH).
The findings were presented at an international conference of the American Thoracic Society.
CFH has been associated with death in a number of conditions. The iron separates, radicalizes, and causes oxidative injury, especially to the kidneys. Acetaminophen chemically reduces the iron, and has been shown to counter the harm.
In an earlier observational study, the Vanderbilt team found that detectible CFH is common in ICU sepsis patients, as well as elevated plasma levels of F2-isoprostanes, an indicator of oxidative injury. They also observed that CFH was associated with death, and that exposure to acetaminophen seemed to reduce F2-isoprostanes levels and improve survival.
The findings prompted the phase II investigation. The team found that the acetaminophen group had lower levels of F2-isoprostanes on study day 2 (mean 24.9 pg/mL vs. 41.2 pg/mL; P = .022) and lower levels of serum creatinine on study day 3 (mean 1.0 mg/dL vs. 1.3 mg/dL, P = .039). These differences were significant and the renal benefit persisted throughout hospitalization.
Acetaminophen patients overall started with a lower mean baseline creatinine level (1.63 mg/dL vs. 2.06 mg/dL), so the investigators reran their analysis, excluding patients on renal replacement therapy. "The baseline imbalance went away, and the story remained the same: There was still a significant decrease in serum creatinine in the acetaminophen group," said lead investigator Dr. David Janz, a critical care fellow at Vanderbilt.
Despite a favorable trend, acetaminophen did not improve survival, a secondary outcome; one (5.6%) acetaminophen and four (18.2%) placebo patients died (P = .355).
Still, the results are strong enough to suggest that acetaminophen might one day prove to be "a potent intervention to improve sepsis outcomes. Even small creatinine changes are associated with increased length of stay and mortality," Dr. Janz said.
"Our trial contains some negative results" – most notably no significant effect on day 3 F2-isoprostanes levels – but "the consistent reduction in creatinine across a number of different analyses and the biologic plausibility underlying this signal prompt further investigation. We need larger studies that focus on length of stay and mortality," he said.
Acetaminophen patients were slightly younger (50 vs. 58 years), but besides that and the baseline creatinine difference, the groups were well matched. Both had mean Apache II scores in the low 20s. Nine acetaminophen patients (50%) and seven placebo patients (32%) were intubated.
Both groups received a median of 12 study doses. There was no statistical between-group difference in the number of patients whose AST/ALT topped 400 U/L, a stop-point hit by two acetaminophen patients and one placebo patient (P = .599). No one in the acetaminophen group developed a rash.
Patients who had liver disease or who had gotten acetaminophen within 48 hours were among those excluded from the study.
The work was funded by the National Institutes of Health and the American Heart Association. Dr. Janz had no disclosures.
AT ATS 2014
Key clinical point: Acetaminophen might protect septic patients’ kidneys.
Major finding: After 3 days, 18 septic ICU patients randomized to acetaminophen had a mean serum creatinine of 1.0 mg/dL; 22 randomized to placebo had a mean serum creatinine of 1.3 mg/dL (P = .039).
Data source: A phase II trial.
Disclosures: The work was funded by the National Institutes of Health and the American Heart Association. The lead investigator had no disclosures.