User login
Study identifies important predictors for PC/PGL
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
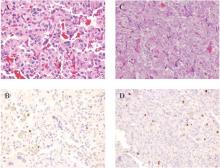
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: SDHB mutation and tumor size may be better predictors of outcomes in patients with pheochromocytoma and abdominal paraganglioma than are other previously identified predictors.
Major finding: The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation.
Data source: Retrospective analysis of 84 patients with PC/PGL evaluated by the Surgical Endocrine Oncology branch at George Washington University Hospital from 1998-2015.
Disclosures: The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors reported having no financial disclosures.
Resection of recurrence shows survival benefit for adrenocortical carcinoma
BALTIMORE – Patients who have recurrent adrenocortical carcinoma appear to have one option to increase their survival: surgery that includes complete tumor resection – but it may a viable path only if the recurrence occurred a year or more after the initial resection and diagnosis, according to an retrospective study of patients at five French university hospitals. “Adrenocortical carcinoma (ACC) is a rare, malignant tumor that has a poor prognosis, and recurrence of the tumor is considerable with 75% recurrence at 5 years,” Dr. Claire Blanchard of the Digestive and Endocrine Surgery Clinic at the Central University Hospital, Nantes, France, reported at the annual meeting of the American Association of Endocrine Surgeons. “Complete resection of recurrence is the only curative treatment.”
The researchers conducted a retrospective study of patients with at least one recurrence, diagnosed between 1980 and 2014, after initial resection of ACC, comparing outcomes in 29 patients who underwent surgery with 30 who had non-operative treatment, mainly chemotherapy and radiation.
Patients who had an operation for recurrence more often had local recurrence, 75% vs. 10% in the nonoperative group, and more frequently had a unique site of recurrence, 97% vs. 45%, than the nonoperative patients, Dr. Blanchard said.
These other demographic and tumor characteristics were similar between the operative and nonoperative groups, respectively: age, 49 years and 53 years; gender, 63% and 79% female; Weiss score, 6 and 7; Ki-67 protein index, 23% and 24%; tumor size, 99.2 mm and 115.5 mm; ENSAT stage, 65% and 45% stages I and II; and R0 resection status of the primary tumor at initial surgery, 83% and 71%.
The univariate analysis showed that appearance of the first recurrence more than 12 months after the initial diagnosis increased a patient’s chance of survival after treatment for recurrence, Dr. Blanchard said.
“Recurrences occurred at median delay of 12 months after the initial surgery,” Dr. Blanchard said. “In the 59 patients, 24 had local recurrences and 35 had distant metastases.”
Overall median survival after the first recurrence was 91 months for patients who had surgery vs. 15 months for those who did not. Overall median survival after initial resection of the primary tumor was 133 months, with a range of 14 to 252 months, in operated patients vs. 32 months, ranging from 21 to 43 months, in those who had no surgery, Dr. Blanchard said.
Of the 29 surgery patients in the surgery group, 22 had local-regional resections, 6 of whom had adjunctive radiation of the tumor bed.
“The type of resection in recurrent ACC depends on the location of the recurrence,” senior coauthor Dr. Eric Mirallié said. “In the case of local recurrence, we resected the adrenalectomy bed and all the adjacent invaded organs.”
In this series, 6 patients had resection of the tumor bed and 16 had adjacent organ resections; 8 patients (28%) had two or more operations for recurrences. These operations involved eight splenectomies, seven resections for abdominal nodules, six nephrectomies, three distal pancreatectomies, three segmental colectomies, and two minor hepatectomies. All operations were by laparotomy.
“In cases of distant recurrence, complete metastasectomy was performed,” Dr. Mirallié said. The series reported two right hepatectomies, one liver tumorectomy, one lung tumorectomy, and one brain tumorectomy.
“Nonoperative management is reserved for nonresectable patients with recurrent adrenocortical carcinoma,” Dr. Mirallié said. “Oral chemotherapy like mitotane was always given when possible. In cases of nonresectable local recurrence, radiotherapy can be used.”
During the discussion, Dr. Bradford K. Mitchell of Michigan State University, East Lansing, said that the benefit of improved survival in surgical patients in the study may have been a function of selection bias as patients who were not operated on may have had more advanced disease.
Dr. Blanchard and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have recurrent adrenocortical carcinoma appear to have one option to increase their survival: surgery that includes complete tumor resection – but it may a viable path only if the recurrence occurred a year or more after the initial resection and diagnosis, according to an retrospective study of patients at five French university hospitals. “Adrenocortical carcinoma (ACC) is a rare, malignant tumor that has a poor prognosis, and recurrence of the tumor is considerable with 75% recurrence at 5 years,” Dr. Claire Blanchard of the Digestive and Endocrine Surgery Clinic at the Central University Hospital, Nantes, France, reported at the annual meeting of the American Association of Endocrine Surgeons. “Complete resection of recurrence is the only curative treatment.”
The researchers conducted a retrospective study of patients with at least one recurrence, diagnosed between 1980 and 2014, after initial resection of ACC, comparing outcomes in 29 patients who underwent surgery with 30 who had non-operative treatment, mainly chemotherapy and radiation.
Patients who had an operation for recurrence more often had local recurrence, 75% vs. 10% in the nonoperative group, and more frequently had a unique site of recurrence, 97% vs. 45%, than the nonoperative patients, Dr. Blanchard said.
These other demographic and tumor characteristics were similar between the operative and nonoperative groups, respectively: age, 49 years and 53 years; gender, 63% and 79% female; Weiss score, 6 and 7; Ki-67 protein index, 23% and 24%; tumor size, 99.2 mm and 115.5 mm; ENSAT stage, 65% and 45% stages I and II; and R0 resection status of the primary tumor at initial surgery, 83% and 71%.
The univariate analysis showed that appearance of the first recurrence more than 12 months after the initial diagnosis increased a patient’s chance of survival after treatment for recurrence, Dr. Blanchard said.
“Recurrences occurred at median delay of 12 months after the initial surgery,” Dr. Blanchard said. “In the 59 patients, 24 had local recurrences and 35 had distant metastases.”
Overall median survival after the first recurrence was 91 months for patients who had surgery vs. 15 months for those who did not. Overall median survival after initial resection of the primary tumor was 133 months, with a range of 14 to 252 months, in operated patients vs. 32 months, ranging from 21 to 43 months, in those who had no surgery, Dr. Blanchard said.
Of the 29 surgery patients in the surgery group, 22 had local-regional resections, 6 of whom had adjunctive radiation of the tumor bed.
“The type of resection in recurrent ACC depends on the location of the recurrence,” senior coauthor Dr. Eric Mirallié said. “In the case of local recurrence, we resected the adrenalectomy bed and all the adjacent invaded organs.”
In this series, 6 patients had resection of the tumor bed and 16 had adjacent organ resections; 8 patients (28%) had two or more operations for recurrences. These operations involved eight splenectomies, seven resections for abdominal nodules, six nephrectomies, three distal pancreatectomies, three segmental colectomies, and two minor hepatectomies. All operations were by laparotomy.
“In cases of distant recurrence, complete metastasectomy was performed,” Dr. Mirallié said. The series reported two right hepatectomies, one liver tumorectomy, one lung tumorectomy, and one brain tumorectomy.
“Nonoperative management is reserved for nonresectable patients with recurrent adrenocortical carcinoma,” Dr. Mirallié said. “Oral chemotherapy like mitotane was always given when possible. In cases of nonresectable local recurrence, radiotherapy can be used.”
During the discussion, Dr. Bradford K. Mitchell of Michigan State University, East Lansing, said that the benefit of improved survival in surgical patients in the study may have been a function of selection bias as patients who were not operated on may have had more advanced disease.
Dr. Blanchard and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have recurrent adrenocortical carcinoma appear to have one option to increase their survival: surgery that includes complete tumor resection – but it may a viable path only if the recurrence occurred a year or more after the initial resection and diagnosis, according to an retrospective study of patients at five French university hospitals. “Adrenocortical carcinoma (ACC) is a rare, malignant tumor that has a poor prognosis, and recurrence of the tumor is considerable with 75% recurrence at 5 years,” Dr. Claire Blanchard of the Digestive and Endocrine Surgery Clinic at the Central University Hospital, Nantes, France, reported at the annual meeting of the American Association of Endocrine Surgeons. “Complete resection of recurrence is the only curative treatment.”
The researchers conducted a retrospective study of patients with at least one recurrence, diagnosed between 1980 and 2014, after initial resection of ACC, comparing outcomes in 29 patients who underwent surgery with 30 who had non-operative treatment, mainly chemotherapy and radiation.
Patients who had an operation for recurrence more often had local recurrence, 75% vs. 10% in the nonoperative group, and more frequently had a unique site of recurrence, 97% vs. 45%, than the nonoperative patients, Dr. Blanchard said.
These other demographic and tumor characteristics were similar between the operative and nonoperative groups, respectively: age, 49 years and 53 years; gender, 63% and 79% female; Weiss score, 6 and 7; Ki-67 protein index, 23% and 24%; tumor size, 99.2 mm and 115.5 mm; ENSAT stage, 65% and 45% stages I and II; and R0 resection status of the primary tumor at initial surgery, 83% and 71%.
The univariate analysis showed that appearance of the first recurrence more than 12 months after the initial diagnosis increased a patient’s chance of survival after treatment for recurrence, Dr. Blanchard said.
“Recurrences occurred at median delay of 12 months after the initial surgery,” Dr. Blanchard said. “In the 59 patients, 24 had local recurrences and 35 had distant metastases.”
Overall median survival after the first recurrence was 91 months for patients who had surgery vs. 15 months for those who did not. Overall median survival after initial resection of the primary tumor was 133 months, with a range of 14 to 252 months, in operated patients vs. 32 months, ranging from 21 to 43 months, in those who had no surgery, Dr. Blanchard said.
Of the 29 surgery patients in the surgery group, 22 had local-regional resections, 6 of whom had adjunctive radiation of the tumor bed.
“The type of resection in recurrent ACC depends on the location of the recurrence,” senior coauthor Dr. Eric Mirallié said. “In the case of local recurrence, we resected the adrenalectomy bed and all the adjacent invaded organs.”
In this series, 6 patients had resection of the tumor bed and 16 had adjacent organ resections; 8 patients (28%) had two or more operations for recurrences. These operations involved eight splenectomies, seven resections for abdominal nodules, six nephrectomies, three distal pancreatectomies, three segmental colectomies, and two minor hepatectomies. All operations were by laparotomy.
“In cases of distant recurrence, complete metastasectomy was performed,” Dr. Mirallié said. The series reported two right hepatectomies, one liver tumorectomy, one lung tumorectomy, and one brain tumorectomy.
“Nonoperative management is reserved for nonresectable patients with recurrent adrenocortical carcinoma,” Dr. Mirallié said. “Oral chemotherapy like mitotane was always given when possible. In cases of nonresectable local recurrence, radiotherapy can be used.”
During the discussion, Dr. Bradford K. Mitchell of Michigan State University, East Lansing, said that the benefit of improved survival in surgical patients in the study may have been a function of selection bias as patients who were not operated on may have had more advanced disease.
Dr. Blanchard and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: Surgery carries a significant survival benefit in patients with recurrent adrenocortical carcinoma (ACC).
Major finding: Overall median survival after the first recurrence was 91 months in patients who had surgery vs. 32 months in those who did not.
Data source: Retrospective case-control study of 59 patients at five French teaching hospitals who had treatment for recurrent ACC from 1980-2014.
Disclosures: Dr. Blanchard and her coauthors reported having no financial disclosures.
Accuracy of gene test for thyroid nodules questioned
BALTIMORE – Biopsy results from a commercially available genetic test for ruling out malignancy of thyroid nodules may not provide reliable answers to clinicians and patients.
When fine-needle aspiration biopsy of thyroid nodules comes back inconclusive, clinicians have increasingly utilized the Afirma gene expression classifier (GEC) to rule out malignancy, but a retrospective analysis of almost 200 patients with indeterminate biopsy results along with a pooled analysis of 11 previous studies has raised questions about the negative predictive value of the test.
“The Afirma GEC test has substantial variability in performance,” said Dr. Zaid Al-Qurayshi of Tulane University, New Orleans, who reported the results at the annual meeting of the American Association of Endocrine Surgeons. “This variability cannot be explained based on differences in prevalence alone, but may also be the result of intrinsic test properties.”
The Afirma GEC measures the expression of 167 genes to more precisely determine the cancer risk of an indeterminate biopsied thyroid nodule and avoid unnecessary surgery. The test costs approximately $4,800 per nodule.
The researchers undertook the study in light of an American Thyroid Association (ATA) statement last year that concluded that test results are predicated on the clinician knowing the prevalence of malignancy within each indeterminate cytologic category at his/her own institution. Without this information, the performance of the diagnostic tests may vary substantially (Thyroid. 2015;25:760-8).
The single-center, retrospective cohort analysis included 192 patients with 210 indeterminate biopsy results, 145 of whom had surgery with 154 thyroid nodules. With a malignancy prevalence of 45%, the expected negative predictive value (NPV) of the test was estimated to be 85%, Dr. Al-Qurayshi said. However, the actual observed NPV was 69%. “If the prevalence was assumed to be 25%, the expected NPV was estimated to be 94%, while the observed NPV would have been 85%,” Dr. Al-Qurayshi said.
The researchers calculated the expected NPV by adopting the sensitivity and specificity rates of the test as reported in previous studies, while they calculated the observed NPV based on the actual negative rate among the Tulane cohort, Dr. Al-Qurayshi said.
Dr. Al-Qurayshi and colleagues then compared their results with pooled data from 11 other studies of the Afirma GEC. The pooled data analysis included 1,303 patients and yielded a malignancy prevalence of 31.1%, with a range of 29%-35%, and a pooled NPV of 92%, with a range of 87%-96%, Dr. Al-Qurayshi said.
“A lot of previously published studies took the sensitivity and specificity that were previously reported for granted, and now we are showing this sensitivity is all over the place,” Dr. Al-Qurayshi said. “Now, we don’t know which is the true one, and we need a larger clinical trial first to determine the true properties. Then we can ask how the prevalence in one’s institution is affecting the performance of the test.”
In an interview, Dr. Emad Kandil, senior study coauthor, also of Tulane, said the 69% NPV of the Tulane cohort puts the diagnostic scenario “back to ground zero, which is similar to what we had prior to the use of the new commercially available genetic tests.” He added, “A larger, randomized trial of the Afirma GEC test should answer those questions.”
The seminal study for the Afirma GEC, authored by Dr. Erik Alexander of Brigham and Women’s Hospital, Boston, in 2012, reported a 92% NPV with the test (N Engl J Med. 2012;367:705-15).
“The first thought was that they had different results because their population was different,” Dr. Al-Qurayshi said. “The ATA statement noted that it is the clinician’s responsibility to determine if this test is appropriate for their population or not, but the performance of the test doesn’t just depend on the population property, but it also depends on the intrinsic testing properties.”
Dr. Kandil disclosed that he has been a primary investigator in the ENHANCE multicenter study of the Afirma GEC. The other coauthors had no financial disclosures.
BALTIMORE – Biopsy results from a commercially available genetic test for ruling out malignancy of thyroid nodules may not provide reliable answers to clinicians and patients.
When fine-needle aspiration biopsy of thyroid nodules comes back inconclusive, clinicians have increasingly utilized the Afirma gene expression classifier (GEC) to rule out malignancy, but a retrospective analysis of almost 200 patients with indeterminate biopsy results along with a pooled analysis of 11 previous studies has raised questions about the negative predictive value of the test.
“The Afirma GEC test has substantial variability in performance,” said Dr. Zaid Al-Qurayshi of Tulane University, New Orleans, who reported the results at the annual meeting of the American Association of Endocrine Surgeons. “This variability cannot be explained based on differences in prevalence alone, but may also be the result of intrinsic test properties.”
The Afirma GEC measures the expression of 167 genes to more precisely determine the cancer risk of an indeterminate biopsied thyroid nodule and avoid unnecessary surgery. The test costs approximately $4,800 per nodule.
The researchers undertook the study in light of an American Thyroid Association (ATA) statement last year that concluded that test results are predicated on the clinician knowing the prevalence of malignancy within each indeterminate cytologic category at his/her own institution. Without this information, the performance of the diagnostic tests may vary substantially (Thyroid. 2015;25:760-8).
The single-center, retrospective cohort analysis included 192 patients with 210 indeterminate biopsy results, 145 of whom had surgery with 154 thyroid nodules. With a malignancy prevalence of 45%, the expected negative predictive value (NPV) of the test was estimated to be 85%, Dr. Al-Qurayshi said. However, the actual observed NPV was 69%. “If the prevalence was assumed to be 25%, the expected NPV was estimated to be 94%, while the observed NPV would have been 85%,” Dr. Al-Qurayshi said.
The researchers calculated the expected NPV by adopting the sensitivity and specificity rates of the test as reported in previous studies, while they calculated the observed NPV based on the actual negative rate among the Tulane cohort, Dr. Al-Qurayshi said.
Dr. Al-Qurayshi and colleagues then compared their results with pooled data from 11 other studies of the Afirma GEC. The pooled data analysis included 1,303 patients and yielded a malignancy prevalence of 31.1%, with a range of 29%-35%, and a pooled NPV of 92%, with a range of 87%-96%, Dr. Al-Qurayshi said.
“A lot of previously published studies took the sensitivity and specificity that were previously reported for granted, and now we are showing this sensitivity is all over the place,” Dr. Al-Qurayshi said. “Now, we don’t know which is the true one, and we need a larger clinical trial first to determine the true properties. Then we can ask how the prevalence in one’s institution is affecting the performance of the test.”
In an interview, Dr. Emad Kandil, senior study coauthor, also of Tulane, said the 69% NPV of the Tulane cohort puts the diagnostic scenario “back to ground zero, which is similar to what we had prior to the use of the new commercially available genetic tests.” He added, “A larger, randomized trial of the Afirma GEC test should answer those questions.”
The seminal study for the Afirma GEC, authored by Dr. Erik Alexander of Brigham and Women’s Hospital, Boston, in 2012, reported a 92% NPV with the test (N Engl J Med. 2012;367:705-15).
“The first thought was that they had different results because their population was different,” Dr. Al-Qurayshi said. “The ATA statement noted that it is the clinician’s responsibility to determine if this test is appropriate for their population or not, but the performance of the test doesn’t just depend on the population property, but it also depends on the intrinsic testing properties.”
Dr. Kandil disclosed that he has been a primary investigator in the ENHANCE multicenter study of the Afirma GEC. The other coauthors had no financial disclosures.
BALTIMORE – Biopsy results from a commercially available genetic test for ruling out malignancy of thyroid nodules may not provide reliable answers to clinicians and patients.
When fine-needle aspiration biopsy of thyroid nodules comes back inconclusive, clinicians have increasingly utilized the Afirma gene expression classifier (GEC) to rule out malignancy, but a retrospective analysis of almost 200 patients with indeterminate biopsy results along with a pooled analysis of 11 previous studies has raised questions about the negative predictive value of the test.
“The Afirma GEC test has substantial variability in performance,” said Dr. Zaid Al-Qurayshi of Tulane University, New Orleans, who reported the results at the annual meeting of the American Association of Endocrine Surgeons. “This variability cannot be explained based on differences in prevalence alone, but may also be the result of intrinsic test properties.”
The Afirma GEC measures the expression of 167 genes to more precisely determine the cancer risk of an indeterminate biopsied thyroid nodule and avoid unnecessary surgery. The test costs approximately $4,800 per nodule.
The researchers undertook the study in light of an American Thyroid Association (ATA) statement last year that concluded that test results are predicated on the clinician knowing the prevalence of malignancy within each indeterminate cytologic category at his/her own institution. Without this information, the performance of the diagnostic tests may vary substantially (Thyroid. 2015;25:760-8).
The single-center, retrospective cohort analysis included 192 patients with 210 indeterminate biopsy results, 145 of whom had surgery with 154 thyroid nodules. With a malignancy prevalence of 45%, the expected negative predictive value (NPV) of the test was estimated to be 85%, Dr. Al-Qurayshi said. However, the actual observed NPV was 69%. “If the prevalence was assumed to be 25%, the expected NPV was estimated to be 94%, while the observed NPV would have been 85%,” Dr. Al-Qurayshi said.
The researchers calculated the expected NPV by adopting the sensitivity and specificity rates of the test as reported in previous studies, while they calculated the observed NPV based on the actual negative rate among the Tulane cohort, Dr. Al-Qurayshi said.
Dr. Al-Qurayshi and colleagues then compared their results with pooled data from 11 other studies of the Afirma GEC. The pooled data analysis included 1,303 patients and yielded a malignancy prevalence of 31.1%, with a range of 29%-35%, and a pooled NPV of 92%, with a range of 87%-96%, Dr. Al-Qurayshi said.
“A lot of previously published studies took the sensitivity and specificity that were previously reported for granted, and now we are showing this sensitivity is all over the place,” Dr. Al-Qurayshi said. “Now, we don’t know which is the true one, and we need a larger clinical trial first to determine the true properties. Then we can ask how the prevalence in one’s institution is affecting the performance of the test.”
In an interview, Dr. Emad Kandil, senior study coauthor, also of Tulane, said the 69% NPV of the Tulane cohort puts the diagnostic scenario “back to ground zero, which is similar to what we had prior to the use of the new commercially available genetic tests.” He added, “A larger, randomized trial of the Afirma GEC test should answer those questions.”
The seminal study for the Afirma GEC, authored by Dr. Erik Alexander of Brigham and Women’s Hospital, Boston, in 2012, reported a 92% NPV with the test (N Engl J Med. 2012;367:705-15).
“The first thought was that they had different results because their population was different,” Dr. Al-Qurayshi said. “The ATA statement noted that it is the clinician’s responsibility to determine if this test is appropriate for their population or not, but the performance of the test doesn’t just depend on the population property, but it also depends on the intrinsic testing properties.”
Dr. Kandil disclosed that he has been a primary investigator in the ENHANCE multicenter study of the Afirma GEC. The other coauthors had no financial disclosures.
At AAES 2016
Key clinical point: Biopsy results from a commercially available genetic test for ruling out malignancy of thyroid nodules may not provide reliable answers to clinicians and patients.
Major finding: With a malignancy prevalence of 45%, the expected negative predictive value of the test was estimated to be 85%, but the actual observed NPV was 69%.
Data source: A single-center, retrospective cohort analysis involving 145 patients with 154 thyroid nodules.
Disclosures: Coauthor Dr. Emad Kandil disclosed that he has been a primary investigator in the ENHANCE multicenter study of the Afirma GEC. The other coauthors reported having no financial disclosures.
Parathyroidectomy before kidney transplant may reduce complications
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: Parathyroidectomy reduces graft failure in individuals with uremic hyperparathyroidism (UHPT) who undergo kidney transplant.
Major finding: Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 of complications a year after transplant; patients who had parathyroidectomy before transplant had a reduced 0.547 odds ratio risk of graft failure.
Data source: Review of 913 patients who had kidney transplant from 2005 to 2014 at a single institution.
Disclosures: Dr. Callender and her coauthors reported having no financial disclosures.
Surgery for PHPT Improves Sleep Quality
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
AT AAES 2016
Surgery for PHPT improves sleep quality
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
BALTIMORE – Research into how primary hyperparathyroidism and parathyroidectomy affect sleep quality has been limited, but investigators at the Medical College of Wisconsin, Milwaukee, reported that primary hyperparathyroidism does indeed disrupt sleep patterns and that curative surgery can improve sleep quality in a third of patients.
“Today, most patients with primary hyperparathyroidism have what is considered asymptomatic disease,” Justin La reported at the annual meeting of the American Association of Endocrine Surgeons. “However, recent studies demonstrate that many of these asymptomatic patients commonly exhibit neuropsychological problems, including sleep disturbances.” Mr. La is a fourth-year medical student at the Medical College of Wisconsin.
This prospective study, led by Dr. Tina Yen, recruited patients between June 2013 and September 2015 and compared 110 patients who had parathyroidectomy for primary hyperparathyroidism (PHPT) with 45 controls who had thyroidectomy for benign euthyroid disease between June 2013 and September 2015.
“Multiple studies, including recent meta-analyses, have demonstrated lower quality of life in patients with primary hyperparathyroidism and have suggested that patients, regardless of symptoms or degree of hypercalcemia, report varying degrees of improvement after parathyroidectomy,” Mr. La said. “In contrast there is a relative paucity of literature on the effects of primary hyperparathyroidism on sleep quality and changes after parathyroidectomy.”
He noted studies from both the University of Texas M.D. Anderson Cancer Center, Houston, and the University of Wisconsin–Madison had demonstrated a 44%-63% incidence of sleep disturbance preoperatively and improvement postoperatively in patients with PHPT who had parathyroidectomy (Endocr Pract. 2007 Jul-Aug;13:338-44; World J Surg. 2014 Mar;38:542-8; Surgery. 2009 Dec;146:1116-22).
“However, these studies were limited by small sample sizes and lack of a control group,” La said.
The latest study had subjects complete questionnaires inquiring about quality of life and sleep patterns at three different intervals: before surgery; and 1 and 6 months after surgery. The study used the Medical Outcomes Study SF-36 to assess quality of life and the Pittsburgh Sleep Quality Index (PSQI) to evaluate sleep quality. The PSQI rates sleep quality on a scale of 0 to 21; a score of 5 or higher indicates poor sleep quality.
“Compared to the preoperative scores, sleep scores after parathyroidectomy were lower, signifying better sleep quality among the 105 patients who completed 1-month postoperative surveys and the 94 patients who completed the 6-month surveys,” La said.
Before surgery, PHPT patients had worse sleep quality than their thyroid counterparts with PSQI scores of 8.1 vs. 5.3, respectively. After surgery, sleep quality scores between the two groups were similar, with mean PSQI scores of 6.3 vs. 5.3 at 1 month after surgery for the parathyroid and thyroid groups, respectively, and 5.8 vs. 4.6 for the two groups at 6 months.
Also, the proportion of patients in both groups who had poor sleep quality after surgery showed no statistical difference. At 1 month after surgery, 50% of patients in the parathyroid group and 40% in the thyroid group continued to have poor sleep quality, La said. However, when comparing preoperative with postoperative sleep scores, 37% in the parathyroid group had a noticeable improvement in their sleep scores, while only 10% of the thyroid group demonstrated improvement.
The researchers also evaluated physical and mental function in the two groups. “Preoperative overall health status was significantly worse in the parathyroid group,” La said. At 1 and 6 months after parathyroidectomy, only two physical components, physical functioning and bodily pain, remained worse in the PHPT patients. Compared with preoperative scores, PHPT patients showed statistically significant improvement in all four mental components at both postoperative periods. “In contrast, the thyroid group demonstrated no significant changes in the preoperative to postoperative scores in all eight components,” La said.
“Our study adds to the body of literature suggesting that asymptomatic patients with primary hyperparathyroidism are unlikely to be truly asymptomatic,” La said. “All patients with primary hyperparathyroidism should be referred for surgical consultation, particularly those with neurocognitive symptoms.”
He also said that patients should be counseled that improvement in sleep quality and quality of life, if they are to occur, typically are seen within 1 month after surgery.
Mr. La, Dr. Yen, and the study coauthors had no relationships to disclose.
AT AAES 2016
Key clinical point: A large proportion of “asymptomatic” patients with primary hyperparathyroidism (PHPT) actually have sleep disturbances.
Major finding: Sleep scores a month after parathyroidectomy were found to improve in 50% of patients with PHPT.
Data source: Single institution, prospective study of 155 patients comparing sleep patterns in patients with PHPT and thyroid controls.
Disclosures: Mr. La and his coauthors reported having no financial disclosures.
Surgery has edge over surveillance for micropapillary thyroid cancer
BALTIMORE – Hemithyroidectomy for low-risk micropapillary thyroid cancer can have advantages over active surveillance, according to findings from a study that examined outcomes by cost and quality of life data.
Endocrinologists and surgeons need to have in-depth conversations with their patients to determine their level of anxiety about cancer, surgery, and about their quality of life, to determine the best course of treatment, researchers at the University of California, San Francisco (UCSF) reported at the annual meeting of the American Association of Endocrine Surgeons.
“Our study found that hemithyroidectomy is cost effective in the majority of scenarios,” presenter Shriya Venkatesh said. “However, patient perception of micropapillary thyroid cancer as well as [the patient’s] life expectancy can play a major role in deciding which therapeutic option to choose.”
The study involved a cost-effectiveness analysis of the surgery vs. active surveillance, “which is especially relevant in our current times,” Ms. Venkatesh said in an interview. “What we wanted to do is give physicians information for when they approach their patients, not only in assessing the tumor from the medical aspect but also when looking at it from quality-of-life and cost-benefit perspectives.”
Both courses of management were modeled over a 20-year period with Medicare data and literature review to calculate costs and health utilities. The UCSF researchers used Markov statistical models for both approaches in which the reference case was a 40-year-old, otherwise healthy patient with a recent diagnosis of micropapillary thyroid cancer without high-risk factors. Either hemithyroidectomy or surveillance would be reasonable treatment options.
“We found that hemithyroidectomy was about $8,000 more costly than active surveillance, but it also afforded an increase in about 1.09 quality-adjusted life years,” Ms. Venkatesh said. Hemithyroidectomy is most cost effective for patients with a life expectancy of 3 years or more and who perceive that living with low-grade thyroid cancer would have even a modest detriment on their quality of life, she said.
“Unfortunately there is no current published quality-of-life assessment of active surveillance for thyroid cancer,” Ms. Venkatesh said. “We believe that estimating active surveillance to the equivalent of surgery underestimates the anxiety some patients may feel upon receiving their diagnosis.”
The paucity of literature on active surveillance for thyroid cancer prompted the UCSF researchers to turn to the prostate cancer literature, which has more data on active surveillance, to try to determine the disutility of active surveillance for micropapillary thyroid cancer. “Our extrapolation from the literature yields a mean disutility of 0.11,” she said.
However, the utility estimates the researchers came up with were variable, Ms. Venkatesh said. “This really pushes physicians to have that conversation with their patients, not only about the physical aspects of how they’re doing but also the mental aspects,” she said.
But quality of life is difficult to quantify, senior author Dr. Insoo Suh said in an interview. “What we found is that no matter how one measures quality of life, the qualitative degree of quality of life decrease that people associate with ‘living with cancer’ need not be that significant in order for surgery to be a potentially cost-effective treatment for them,” said Dr. Suh, an endocrine surgeon at UCSF and an ACS Fellow.
During the discussion, Dr. Peter Angelos of the University of Chicago and an ACS Fellow, said, “I’m curious how this information should impact the individual decision-making and informed consent for a specific patient, because I’m not sure that an individual patient would care if active surveillance is more cost effective or not.”
“When speaking to your patients, obviously discussing the rates of progression of the disease is important and then [so is] talking to them about different therapeutic options,” Ms. Venkatesh said. “The physician should also make an assessment about the patient’s quality of life to see if there are likely to be any changes due to the diagnosis.”
The limitations of the study include the extrapolation of data from the prostate cancer literature to define a utility scale and also the reference case used in the Markov model. Other utility measures showed variability as well.
Ms. Venkatesh, Dr. Suh and their coauthors had no financial relationships to disclose.
BALTIMORE – Hemithyroidectomy for low-risk micropapillary thyroid cancer can have advantages over active surveillance, according to findings from a study that examined outcomes by cost and quality of life data.
Endocrinologists and surgeons need to have in-depth conversations with their patients to determine their level of anxiety about cancer, surgery, and about their quality of life, to determine the best course of treatment, researchers at the University of California, San Francisco (UCSF) reported at the annual meeting of the American Association of Endocrine Surgeons.
“Our study found that hemithyroidectomy is cost effective in the majority of scenarios,” presenter Shriya Venkatesh said. “However, patient perception of micropapillary thyroid cancer as well as [the patient’s] life expectancy can play a major role in deciding which therapeutic option to choose.”
The study involved a cost-effectiveness analysis of the surgery vs. active surveillance, “which is especially relevant in our current times,” Ms. Venkatesh said in an interview. “What we wanted to do is give physicians information for when they approach their patients, not only in assessing the tumor from the medical aspect but also when looking at it from quality-of-life and cost-benefit perspectives.”
Both courses of management were modeled over a 20-year period with Medicare data and literature review to calculate costs and health utilities. The UCSF researchers used Markov statistical models for both approaches in which the reference case was a 40-year-old, otherwise healthy patient with a recent diagnosis of micropapillary thyroid cancer without high-risk factors. Either hemithyroidectomy or surveillance would be reasonable treatment options.
“We found that hemithyroidectomy was about $8,000 more costly than active surveillance, but it also afforded an increase in about 1.09 quality-adjusted life years,” Ms. Venkatesh said. Hemithyroidectomy is most cost effective for patients with a life expectancy of 3 years or more and who perceive that living with low-grade thyroid cancer would have even a modest detriment on their quality of life, she said.
“Unfortunately there is no current published quality-of-life assessment of active surveillance for thyroid cancer,” Ms. Venkatesh said. “We believe that estimating active surveillance to the equivalent of surgery underestimates the anxiety some patients may feel upon receiving their diagnosis.”
The paucity of literature on active surveillance for thyroid cancer prompted the UCSF researchers to turn to the prostate cancer literature, which has more data on active surveillance, to try to determine the disutility of active surveillance for micropapillary thyroid cancer. “Our extrapolation from the literature yields a mean disutility of 0.11,” she said.
However, the utility estimates the researchers came up with were variable, Ms. Venkatesh said. “This really pushes physicians to have that conversation with their patients, not only about the physical aspects of how they’re doing but also the mental aspects,” she said.
But quality of life is difficult to quantify, senior author Dr. Insoo Suh said in an interview. “What we found is that no matter how one measures quality of life, the qualitative degree of quality of life decrease that people associate with ‘living with cancer’ need not be that significant in order for surgery to be a potentially cost-effective treatment for them,” said Dr. Suh, an endocrine surgeon at UCSF and an ACS Fellow.
During the discussion, Dr. Peter Angelos of the University of Chicago and an ACS Fellow, said, “I’m curious how this information should impact the individual decision-making and informed consent for a specific patient, because I’m not sure that an individual patient would care if active surveillance is more cost effective or not.”
“When speaking to your patients, obviously discussing the rates of progression of the disease is important and then [so is] talking to them about different therapeutic options,” Ms. Venkatesh said. “The physician should also make an assessment about the patient’s quality of life to see if there are likely to be any changes due to the diagnosis.”
The limitations of the study include the extrapolation of data from the prostate cancer literature to define a utility scale and also the reference case used in the Markov model. Other utility measures showed variability as well.
Ms. Venkatesh, Dr. Suh and their coauthors had no financial relationships to disclose.
BALTIMORE – Hemithyroidectomy for low-risk micropapillary thyroid cancer can have advantages over active surveillance, according to findings from a study that examined outcomes by cost and quality of life data.
Endocrinologists and surgeons need to have in-depth conversations with their patients to determine their level of anxiety about cancer, surgery, and about their quality of life, to determine the best course of treatment, researchers at the University of California, San Francisco (UCSF) reported at the annual meeting of the American Association of Endocrine Surgeons.
“Our study found that hemithyroidectomy is cost effective in the majority of scenarios,” presenter Shriya Venkatesh said. “However, patient perception of micropapillary thyroid cancer as well as [the patient’s] life expectancy can play a major role in deciding which therapeutic option to choose.”
The study involved a cost-effectiveness analysis of the surgery vs. active surveillance, “which is especially relevant in our current times,” Ms. Venkatesh said in an interview. “What we wanted to do is give physicians information for when they approach their patients, not only in assessing the tumor from the medical aspect but also when looking at it from quality-of-life and cost-benefit perspectives.”
Both courses of management were modeled over a 20-year period with Medicare data and literature review to calculate costs and health utilities. The UCSF researchers used Markov statistical models for both approaches in which the reference case was a 40-year-old, otherwise healthy patient with a recent diagnosis of micropapillary thyroid cancer without high-risk factors. Either hemithyroidectomy or surveillance would be reasonable treatment options.
“We found that hemithyroidectomy was about $8,000 more costly than active surveillance, but it also afforded an increase in about 1.09 quality-adjusted life years,” Ms. Venkatesh said. Hemithyroidectomy is most cost effective for patients with a life expectancy of 3 years or more and who perceive that living with low-grade thyroid cancer would have even a modest detriment on their quality of life, she said.
“Unfortunately there is no current published quality-of-life assessment of active surveillance for thyroid cancer,” Ms. Venkatesh said. “We believe that estimating active surveillance to the equivalent of surgery underestimates the anxiety some patients may feel upon receiving their diagnosis.”
The paucity of literature on active surveillance for thyroid cancer prompted the UCSF researchers to turn to the prostate cancer literature, which has more data on active surveillance, to try to determine the disutility of active surveillance for micropapillary thyroid cancer. “Our extrapolation from the literature yields a mean disutility of 0.11,” she said.
However, the utility estimates the researchers came up with were variable, Ms. Venkatesh said. “This really pushes physicians to have that conversation with their patients, not only about the physical aspects of how they’re doing but also the mental aspects,” she said.
But quality of life is difficult to quantify, senior author Dr. Insoo Suh said in an interview. “What we found is that no matter how one measures quality of life, the qualitative degree of quality of life decrease that people associate with ‘living with cancer’ need not be that significant in order for surgery to be a potentially cost-effective treatment for them,” said Dr. Suh, an endocrine surgeon at UCSF and an ACS Fellow.
During the discussion, Dr. Peter Angelos of the University of Chicago and an ACS Fellow, said, “I’m curious how this information should impact the individual decision-making and informed consent for a specific patient, because I’m not sure that an individual patient would care if active surveillance is more cost effective or not.”
“When speaking to your patients, obviously discussing the rates of progression of the disease is important and then [so is] talking to them about different therapeutic options,” Ms. Venkatesh said. “The physician should also make an assessment about the patient’s quality of life to see if there are likely to be any changes due to the diagnosis.”
The limitations of the study include the extrapolation of data from the prostate cancer literature to define a utility scale and also the reference case used in the Markov model. Other utility measures showed variability as well.
Ms. Venkatesh, Dr. Suh and their coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: Patient psychological factors are key determinants in choosing a course of management for low-risk micropapillary thyroid cancer.
Major finding: Hemithyroidectomy typically costs about $8,000 more than active surveillance but also accounts for improved quality of life in these patients.
Data source: Markov models for both courses of management over a 20-year period with Medicare data and literature review to calculate costs and health utilities.
Disclosures: Ms. Venkatesh and her coauthors reported having no financial disclosures.
Post-parathyroidectomy follow-up may need to be open-ended
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
BALTIMORE – Patients who have had parathyroidectomy for primary hyperparathyroidism can have disease recurrence 10 years or longer after surgery, raising the possibility that postop follow-up should never end, according to a study presented at the annual meeting of the American Association of Endocrine Surgeons.
Dr. Irene Lou of the University of Wisconsin–Madison reported on results of a retrospective study of 196 patients who had a presumably “curative” parathyroidectomy at the institution between November 2000 and June 2005. The mean age of the study population was 61 years.
“The long-term recurrences of primary hyperparathyroidism after curative parathyroidectomy is likely higher than previously reported, with over a third of recurrences occurring 10 years after their operation,” Dr. Lou said.
The study also identified independent predictors of recurrence, among them younger age, a drop in intraoperative parathyroid hormone less than 70%, and double adenoma, Dr. Lou said. All patients after parathyroidectomy should have at minimum an annual serum calcium test, especially younger patients with longer life expectancies, she said. This recommendation, however, may be altered for older patients or those with additional comorbidities.
The study defined recurrence as serum calcium of 10.2 mg/dL or greater 6 months or longer after the initial operation. The overall 10-year recurrence rate was 14.8% and the median time to recurrence was 6.3 years. “We found that 41.4% of patients who recurred did so by 5 years and 65.5% by 10 years,” Dr. Lou said.
The University of Wisconsin and University of Alabama at Birmingham investigators undertook the study because the recent data on recurrence was limited, with the longest study topping out at 7 years, Dr. Lou said. “We previously looked at this problem in other perspectives and we found that a lot of curves separated at around 8 years,” she said.
With regard to the type of operation the patients had, whether unilateral minimally invasive parathyroidectomy or bilateral open surgery, the study found no significant differences in recurrence rates, Dr. Lou said. “This is an excellent study,” Dr. Samuel K. Snyder of Temple, Tex., said during the discussion. “You’re telling us we need to follow patients much longer than perhaps we did previously, but we all see patients who have normal calcium and still have a residual elevated parathyroid hormone level.” He asked if the study considered parathyroid hormone levels at 6 months or more after surgery or vitamin D levels, but Dr. Lou said this information was not available, therefore could not be evaluated.
Dr. Lou and her coauthors had no financial relationships to disclose.
FROM AAES 2016
Key clinical point: Long-term recurrence rates for hyperparathyroidism (HPT) after “curative” parathyroidectomy are likely higher than previously reported.
Major finding: Approximately one-third of patients were found to have recurrences 10 or more years after the initial operation.
Data source: Single-institution cohort of 196 patients who had initial parathyroidectomy for HPT between November 2000 and June 2005.
Disclosures: Dr. Lou and her study coauthors reported having no financial disclosures.
Negative sestamibi scan for primary hyperparathyroidism can mean no referral or surgery
BALTIMORE – In the treatment of primary hyperparathyroidism, clinical guidelines recommend using sestamibi scan for localizing adenoma, but increasingly endocrinologists are using sestamibi results to determine whether or not to refer a patient for parathyroidectomy surgery, while surgeons are using the scans as a factor in deciding whether to perform the operation.
That was the conclusion of a paper Dr. Susana Wu presented at the American Association of Endocrine Surgeons annual meeting. Dr. Wu reported on behalf of her colleagues at Kaiser Permanente Los Angeles Medical Center and at Scripps Clinic in San Diego.
“This study suggests that negative sestamibi scan (SS) results influence management of patients with primary hyperparathyroidism,” Dr. Wu said. “Endocrinologists were less likely to refer to surgeons and surgeons were less likely to offer parathyroidectomy to a patient with a negative sestamibi scan.”
The study involved a retrospective chart review of all 539 patients with primary hyperparathyroidism in the Kaiser Permanente Southern California database from December 2011 to December 2013, 452 of whom were seen by 63 endocrinologists at 14 centers. Among these patients, 260 had SS – 120 negative and 140 positive. The study identified statistically significant variations in how both endocrinologists and surgeons managed patients depending on SS results. The researchers used Kaiser Permanente’s electronic referral system to track referrals.
“The most significant negative predictor for endocrinologists referring to surgeons was a negative sestamibi scan, with an odds ratio of 0.36,” Dr. Wu said.
Endocrinologists referred 86% of patients with positive SS to surgeons, but only 68% of those with negative SS. Surgeons exhibited a similar practice pattern. “Surgeons were less likely to recommend parathyroidectomy for patients with a negative sestamibi scan, with an odds ratio of 0.20,” Dr. Wu said. Surgeons operated on 87% of patients with a negative SS scan but 96% with a positive SS.
In an interview, study coauthor Dr. Philip Haigh explained that parathyroidectomy when the SS is negative is a more difficult operation for the surgeon, and that might make some physicians hesitate before going forward with surgery. “It has been previously shown by other studies that it is a more difficult operation when the sestamibi scan is negative because you have to look at four glands instead of removing just one, but if the surgeon is experienced, it should achieve a high success rate,” Dr. Haigh said. He said that parathyroidectomy in sestamibi-negative hyperparathyroidism had a cure rate as high as 98% in the study presented.
He offered two thoughts on how clinicians should use the study results. “To the endocrinologist, if you’re going to order a sestamibi scan, don’t change your referral practice depending on the result,” Dr. Haigh said. “To the surgeon, if you’re not comfortable operating on a patient with a negative sestamibi scan, then find someone who is.”
The study had a few limitations, Dr. Wu said. Along with its retrospective nature, the study also did not account for potential disparity in radiological vs. surgeon interpretation of the scans.
During the discussion, Dr. Samuel Snyder, of Baylor Scott & White Health, Temple, Tex., said he concurred with the results Dr. Wu reported. “It really worries me about what is happening to patients who have negative scans,” he said. “What I’ve seen in patients referred for surgery is a lot of variation in how the sestamibi scan is done.” He asked if the study accounted for the different types of sestamibi scans and how they were performed, but Dr. Wu said it did not.
Dr. Christopher McHenry of MetroHealth Medical Center, Cleveland, also concurred. “I think this is a phenomenon that occurs more often than we think or we’re aware of,” he said. “I continue to be amazed with how clinicians equate a negative sestamibi scan with not having primary hyperparathyroidism. I think it needs to reemphasized that the sestamibi scan is not diagnostic; it’s for localization.”
He asked Dr. Wu, “How do we change behavior to deal with this problem?”
Dr. Wu said her institution is developing a safety-net program that would aim to increase the identification and chart coding of patients with primary hyperparathyroidism, automate essential labs to be ordered in patients with high calcium, and automate referral to endocrinologists. The study and its findings will be disseminated to endocrinologists in the region.
The study authors had no disclosures.
BALTIMORE – In the treatment of primary hyperparathyroidism, clinical guidelines recommend using sestamibi scan for localizing adenoma, but increasingly endocrinologists are using sestamibi results to determine whether or not to refer a patient for parathyroidectomy surgery, while surgeons are using the scans as a factor in deciding whether to perform the operation.
That was the conclusion of a paper Dr. Susana Wu presented at the American Association of Endocrine Surgeons annual meeting. Dr. Wu reported on behalf of her colleagues at Kaiser Permanente Los Angeles Medical Center and at Scripps Clinic in San Diego.
“This study suggests that negative sestamibi scan (SS) results influence management of patients with primary hyperparathyroidism,” Dr. Wu said. “Endocrinologists were less likely to refer to surgeons and surgeons were less likely to offer parathyroidectomy to a patient with a negative sestamibi scan.”
The study involved a retrospective chart review of all 539 patients with primary hyperparathyroidism in the Kaiser Permanente Southern California database from December 2011 to December 2013, 452 of whom were seen by 63 endocrinologists at 14 centers. Among these patients, 260 had SS – 120 negative and 140 positive. The study identified statistically significant variations in how both endocrinologists and surgeons managed patients depending on SS results. The researchers used Kaiser Permanente’s electronic referral system to track referrals.
“The most significant negative predictor for endocrinologists referring to surgeons was a negative sestamibi scan, with an odds ratio of 0.36,” Dr. Wu said.
Endocrinologists referred 86% of patients with positive SS to surgeons, but only 68% of those with negative SS. Surgeons exhibited a similar practice pattern. “Surgeons were less likely to recommend parathyroidectomy for patients with a negative sestamibi scan, with an odds ratio of 0.20,” Dr. Wu said. Surgeons operated on 87% of patients with a negative SS scan but 96% with a positive SS.
In an interview, study coauthor Dr. Philip Haigh explained that parathyroidectomy when the SS is negative is a more difficult operation for the surgeon, and that might make some physicians hesitate before going forward with surgery. “It has been previously shown by other studies that it is a more difficult operation when the sestamibi scan is negative because you have to look at four glands instead of removing just one, but if the surgeon is experienced, it should achieve a high success rate,” Dr. Haigh said. He said that parathyroidectomy in sestamibi-negative hyperparathyroidism had a cure rate as high as 98% in the study presented.
He offered two thoughts on how clinicians should use the study results. “To the endocrinologist, if you’re going to order a sestamibi scan, don’t change your referral practice depending on the result,” Dr. Haigh said. “To the surgeon, if you’re not comfortable operating on a patient with a negative sestamibi scan, then find someone who is.”
The study had a few limitations, Dr. Wu said. Along with its retrospective nature, the study also did not account for potential disparity in radiological vs. surgeon interpretation of the scans.
During the discussion, Dr. Samuel Snyder, of Baylor Scott & White Health, Temple, Tex., said he concurred with the results Dr. Wu reported. “It really worries me about what is happening to patients who have negative scans,” he said. “What I’ve seen in patients referred for surgery is a lot of variation in how the sestamibi scan is done.” He asked if the study accounted for the different types of sestamibi scans and how they were performed, but Dr. Wu said it did not.
Dr. Christopher McHenry of MetroHealth Medical Center, Cleveland, also concurred. “I think this is a phenomenon that occurs more often than we think or we’re aware of,” he said. “I continue to be amazed with how clinicians equate a negative sestamibi scan with not having primary hyperparathyroidism. I think it needs to reemphasized that the sestamibi scan is not diagnostic; it’s for localization.”
He asked Dr. Wu, “How do we change behavior to deal with this problem?”
Dr. Wu said her institution is developing a safety-net program that would aim to increase the identification and chart coding of patients with primary hyperparathyroidism, automate essential labs to be ordered in patients with high calcium, and automate referral to endocrinologists. The study and its findings will be disseminated to endocrinologists in the region.
The study authors had no disclosures.
BALTIMORE – In the treatment of primary hyperparathyroidism, clinical guidelines recommend using sestamibi scan for localizing adenoma, but increasingly endocrinologists are using sestamibi results to determine whether or not to refer a patient for parathyroidectomy surgery, while surgeons are using the scans as a factor in deciding whether to perform the operation.
That was the conclusion of a paper Dr. Susana Wu presented at the American Association of Endocrine Surgeons annual meeting. Dr. Wu reported on behalf of her colleagues at Kaiser Permanente Los Angeles Medical Center and at Scripps Clinic in San Diego.
“This study suggests that negative sestamibi scan (SS) results influence management of patients with primary hyperparathyroidism,” Dr. Wu said. “Endocrinologists were less likely to refer to surgeons and surgeons were less likely to offer parathyroidectomy to a patient with a negative sestamibi scan.”
The study involved a retrospective chart review of all 539 patients with primary hyperparathyroidism in the Kaiser Permanente Southern California database from December 2011 to December 2013, 452 of whom were seen by 63 endocrinologists at 14 centers. Among these patients, 260 had SS – 120 negative and 140 positive. The study identified statistically significant variations in how both endocrinologists and surgeons managed patients depending on SS results. The researchers used Kaiser Permanente’s electronic referral system to track referrals.
“The most significant negative predictor for endocrinologists referring to surgeons was a negative sestamibi scan, with an odds ratio of 0.36,” Dr. Wu said.
Endocrinologists referred 86% of patients with positive SS to surgeons, but only 68% of those with negative SS. Surgeons exhibited a similar practice pattern. “Surgeons were less likely to recommend parathyroidectomy for patients with a negative sestamibi scan, with an odds ratio of 0.20,” Dr. Wu said. Surgeons operated on 87% of patients with a negative SS scan but 96% with a positive SS.
In an interview, study coauthor Dr. Philip Haigh explained that parathyroidectomy when the SS is negative is a more difficult operation for the surgeon, and that might make some physicians hesitate before going forward with surgery. “It has been previously shown by other studies that it is a more difficult operation when the sestamibi scan is negative because you have to look at four glands instead of removing just one, but if the surgeon is experienced, it should achieve a high success rate,” Dr. Haigh said. He said that parathyroidectomy in sestamibi-negative hyperparathyroidism had a cure rate as high as 98% in the study presented.
He offered two thoughts on how clinicians should use the study results. “To the endocrinologist, if you’re going to order a sestamibi scan, don’t change your referral practice depending on the result,” Dr. Haigh said. “To the surgeon, if you’re not comfortable operating on a patient with a negative sestamibi scan, then find someone who is.”
The study had a few limitations, Dr. Wu said. Along with its retrospective nature, the study also did not account for potential disparity in radiological vs. surgeon interpretation of the scans.
During the discussion, Dr. Samuel Snyder, of Baylor Scott & White Health, Temple, Tex., said he concurred with the results Dr. Wu reported. “It really worries me about what is happening to patients who have negative scans,” he said. “What I’ve seen in patients referred for surgery is a lot of variation in how the sestamibi scan is done.” He asked if the study accounted for the different types of sestamibi scans and how they were performed, but Dr. Wu said it did not.
Dr. Christopher McHenry of MetroHealth Medical Center, Cleveland, also concurred. “I think this is a phenomenon that occurs more often than we think or we’re aware of,” he said. “I continue to be amazed with how clinicians equate a negative sestamibi scan with not having primary hyperparathyroidism. I think it needs to reemphasized that the sestamibi scan is not diagnostic; it’s for localization.”
He asked Dr. Wu, “How do we change behavior to deal with this problem?”
Dr. Wu said her institution is developing a safety-net program that would aim to increase the identification and chart coding of patients with primary hyperparathyroidism, automate essential labs to be ordered in patients with high calcium, and automate referral to endocrinologists. The study and its findings will be disseminated to endocrinologists in the region.
The study authors had no disclosures.
AT AAES 2016
Key clinical point: Endocrinologists and surgeons are less likely to order surgery when patients with primary hyperparathyroidism have negative sestamibi scan (SS) results.
Major finding: Endocrinologists referred 86% of patients with positive SS to surgeons, but only 68% of those with negative SS.
Data source: A retrospective chart review of all 539 patients with primary hyperparathyroidism in the Kaiser Permanente Southern California database over a 2-year period.
Disclosures: Dr. Wu and her coauthors reported having no financial disclosures.