User login
Antimalarial Response in CLE Takes Time
BOSTON – The use of adjunctive therapy and a lot of patience may go a long way to improving the response of cutaneous lupus erythematosus to antimalarial agents, according to Dr. Jennie T. Clarke.
Antimalarials are the go-to treatment for cutaneous lupus erythematosus (CLE), yet roughly a third of patients do not respond, said Dr. Clarke, who spoke at the American Academy of Dermatology’s Summer Academy Meeting.
Findings from some recent studies shed light on how to improve that dismal response rate. In one of these trials involving 128 patients with CLE, researchers found that slightly more than half of patients who initiated treatment with hydroxychloroquine monotherapy were responders (55%) (Arch. Dermatol. 2011;147:1261-7). When quinacrine was added to the treatment regimen of the nonresponders, two-thirds experienced a lessening of their disease. Improvement continued beyond 2 months in 43%.
"With antimalarials remember that patience is important. [These agents] have a slow onset. You have to give the drugs for 2-3 months before assessing for efficacy. Patients need to know this because otherwise they’re going to become frustrated and noncompliant," said Dr. Clarke of the department of dermatology at Pennsylvania State University, Hershey.
The other important lesson from the study is about combination antimalarial therapy. Quinacrine can be added to either hydroxychloroquine or chloroquine to achieve improvement in patients who don’t respond to a single antimalarial agent.
However, roughly a third of patients don’t respond to a combination of antimalarials. Some research in the last 18 months has tried to identify which patients fail antimalarial treatment and why, in order to improve subsequent treatment. Three possible reasons have been identified: dosing and compliance, disease severity, and smoking status.
Bioavailability and clearance of hydroxychloroquine seems to vary by individual, she said. In addition, noncompliance is estimated to be about 10%. In a study of 300 CLE patients, French researchers found that the median blood concentration of hydroxychloroquine correlated with response (Arch. Dermatol. 2012;148:479-84). Specifically, the median blood hydroxychloroquine concentration was significantly higher in patients with complete remission compared with those with either partial remission or treatment failure. Findings from the multivariate analysis showed that complete remission was associated with higher blood hydroxychloroquine concentrations and the absence of discoid lesions.
Concentration and response were correlated with actual rather than ideal body weight dosing. Smoking was not found to be related to concentration, and the subset of 170 patients with discoid lupus erythematosus (DLE) was less responsive to hydroxychloroquine.
Thirty patients (10%) had very low blood hydroxychloroquine concentrations (less than 200 ng/mL) and may be considered nonadherent to the treatment regimen, Dr. Clarke noted. However, additional study is needed to determine the optimal blood concentration of hydroxychloroquine and the impact of toxicity with actual weight-based dosing rather than ideal body weight dosing.
In another study, researchers assessed the clinical and pharmacogenic influences of disease severity on response to blood concentration of hydroxychloroquine (J. Invest. Dermatol. 2011;131:1981-6). They assessed 200 patients with DLE. Slightly more than a third (35%) of patients had not responded to hydroxychloroquine at 6 months. Poor response was associated with disease severity and concomitant systemic lupus erythematosus (SLE). However, response was not associated with the presence of cytochrome P450 genotype or smoking.
It has been long held medical dogma that smoking lessens patients’ response to antimalarial drugs. The impact of smoking in patients with CLE was assessed directly in another paper (Arch. Dermatol. 2012;148:317-22). The researchers included 218 patients with CLE or SLE with skin disease. They found that current smokers had more severe disease and poorer disease-related quality of life. Smokers were also more likely to receive combination antimalarial therapy. Current smokers responded better to antimalarials than past or never smokers. However, smokers responded worse than nonsmokers if antimalarials and immunomodulator/suppressives were required.
"This tells us that antimalarials can be effective for smokers, particularly in those with more mild disease. But we need to remember that smokers who don’t respond are likely going to have poorer outcomes than nonsmokers who don’t respond to antimalarials."
Dr. Clarke reported having no relevant financial conflicts.
BOSTON – The use of adjunctive therapy and a lot of patience may go a long way to improving the response of cutaneous lupus erythematosus to antimalarial agents, according to Dr. Jennie T. Clarke.
Antimalarials are the go-to treatment for cutaneous lupus erythematosus (CLE), yet roughly a third of patients do not respond, said Dr. Clarke, who spoke at the American Academy of Dermatology’s Summer Academy Meeting.
Findings from some recent studies shed light on how to improve that dismal response rate. In one of these trials involving 128 patients with CLE, researchers found that slightly more than half of patients who initiated treatment with hydroxychloroquine monotherapy were responders (55%) (Arch. Dermatol. 2011;147:1261-7). When quinacrine was added to the treatment regimen of the nonresponders, two-thirds experienced a lessening of their disease. Improvement continued beyond 2 months in 43%.
"With antimalarials remember that patience is important. [These agents] have a slow onset. You have to give the drugs for 2-3 months before assessing for efficacy. Patients need to know this because otherwise they’re going to become frustrated and noncompliant," said Dr. Clarke of the department of dermatology at Pennsylvania State University, Hershey.
The other important lesson from the study is about combination antimalarial therapy. Quinacrine can be added to either hydroxychloroquine or chloroquine to achieve improvement in patients who don’t respond to a single antimalarial agent.
However, roughly a third of patients don’t respond to a combination of antimalarials. Some research in the last 18 months has tried to identify which patients fail antimalarial treatment and why, in order to improve subsequent treatment. Three possible reasons have been identified: dosing and compliance, disease severity, and smoking status.
Bioavailability and clearance of hydroxychloroquine seems to vary by individual, she said. In addition, noncompliance is estimated to be about 10%. In a study of 300 CLE patients, French researchers found that the median blood concentration of hydroxychloroquine correlated with response (Arch. Dermatol. 2012;148:479-84). Specifically, the median blood hydroxychloroquine concentration was significantly higher in patients with complete remission compared with those with either partial remission or treatment failure. Findings from the multivariate analysis showed that complete remission was associated with higher blood hydroxychloroquine concentrations and the absence of discoid lesions.
Concentration and response were correlated with actual rather than ideal body weight dosing. Smoking was not found to be related to concentration, and the subset of 170 patients with discoid lupus erythematosus (DLE) was less responsive to hydroxychloroquine.
Thirty patients (10%) had very low blood hydroxychloroquine concentrations (less than 200 ng/mL) and may be considered nonadherent to the treatment regimen, Dr. Clarke noted. However, additional study is needed to determine the optimal blood concentration of hydroxychloroquine and the impact of toxicity with actual weight-based dosing rather than ideal body weight dosing.
In another study, researchers assessed the clinical and pharmacogenic influences of disease severity on response to blood concentration of hydroxychloroquine (J. Invest. Dermatol. 2011;131:1981-6). They assessed 200 patients with DLE. Slightly more than a third (35%) of patients had not responded to hydroxychloroquine at 6 months. Poor response was associated with disease severity and concomitant systemic lupus erythematosus (SLE). However, response was not associated with the presence of cytochrome P450 genotype or smoking.
It has been long held medical dogma that smoking lessens patients’ response to antimalarial drugs. The impact of smoking in patients with CLE was assessed directly in another paper (Arch. Dermatol. 2012;148:317-22). The researchers included 218 patients with CLE or SLE with skin disease. They found that current smokers had more severe disease and poorer disease-related quality of life. Smokers were also more likely to receive combination antimalarial therapy. Current smokers responded better to antimalarials than past or never smokers. However, smokers responded worse than nonsmokers if antimalarials and immunomodulator/suppressives were required.
"This tells us that antimalarials can be effective for smokers, particularly in those with more mild disease. But we need to remember that smokers who don’t respond are likely going to have poorer outcomes than nonsmokers who don’t respond to antimalarials."
Dr. Clarke reported having no relevant financial conflicts.
BOSTON – The use of adjunctive therapy and a lot of patience may go a long way to improving the response of cutaneous lupus erythematosus to antimalarial agents, according to Dr. Jennie T. Clarke.
Antimalarials are the go-to treatment for cutaneous lupus erythematosus (CLE), yet roughly a third of patients do not respond, said Dr. Clarke, who spoke at the American Academy of Dermatology’s Summer Academy Meeting.
Findings from some recent studies shed light on how to improve that dismal response rate. In one of these trials involving 128 patients with CLE, researchers found that slightly more than half of patients who initiated treatment with hydroxychloroquine monotherapy were responders (55%) (Arch. Dermatol. 2011;147:1261-7). When quinacrine was added to the treatment regimen of the nonresponders, two-thirds experienced a lessening of their disease. Improvement continued beyond 2 months in 43%.
"With antimalarials remember that patience is important. [These agents] have a slow onset. You have to give the drugs for 2-3 months before assessing for efficacy. Patients need to know this because otherwise they’re going to become frustrated and noncompliant," said Dr. Clarke of the department of dermatology at Pennsylvania State University, Hershey.
The other important lesson from the study is about combination antimalarial therapy. Quinacrine can be added to either hydroxychloroquine or chloroquine to achieve improvement in patients who don’t respond to a single antimalarial agent.
However, roughly a third of patients don’t respond to a combination of antimalarials. Some research in the last 18 months has tried to identify which patients fail antimalarial treatment and why, in order to improve subsequent treatment. Three possible reasons have been identified: dosing and compliance, disease severity, and smoking status.
Bioavailability and clearance of hydroxychloroquine seems to vary by individual, she said. In addition, noncompliance is estimated to be about 10%. In a study of 300 CLE patients, French researchers found that the median blood concentration of hydroxychloroquine correlated with response (Arch. Dermatol. 2012;148:479-84). Specifically, the median blood hydroxychloroquine concentration was significantly higher in patients with complete remission compared with those with either partial remission or treatment failure. Findings from the multivariate analysis showed that complete remission was associated with higher blood hydroxychloroquine concentrations and the absence of discoid lesions.
Concentration and response were correlated with actual rather than ideal body weight dosing. Smoking was not found to be related to concentration, and the subset of 170 patients with discoid lupus erythematosus (DLE) was less responsive to hydroxychloroquine.
Thirty patients (10%) had very low blood hydroxychloroquine concentrations (less than 200 ng/mL) and may be considered nonadherent to the treatment regimen, Dr. Clarke noted. However, additional study is needed to determine the optimal blood concentration of hydroxychloroquine and the impact of toxicity with actual weight-based dosing rather than ideal body weight dosing.
In another study, researchers assessed the clinical and pharmacogenic influences of disease severity on response to blood concentration of hydroxychloroquine (J. Invest. Dermatol. 2011;131:1981-6). They assessed 200 patients with DLE. Slightly more than a third (35%) of patients had not responded to hydroxychloroquine at 6 months. Poor response was associated with disease severity and concomitant systemic lupus erythematosus (SLE). However, response was not associated with the presence of cytochrome P450 genotype or smoking.
It has been long held medical dogma that smoking lessens patients’ response to antimalarial drugs. The impact of smoking in patients with CLE was assessed directly in another paper (Arch. Dermatol. 2012;148:317-22). The researchers included 218 patients with CLE or SLE with skin disease. They found that current smokers had more severe disease and poorer disease-related quality of life. Smokers were also more likely to receive combination antimalarial therapy. Current smokers responded better to antimalarials than past or never smokers. However, smokers responded worse than nonsmokers if antimalarials and immunomodulator/suppressives were required.
"This tells us that antimalarials can be effective for smokers, particularly in those with more mild disease. But we need to remember that smokers who don’t respond are likely going to have poorer outcomes than nonsmokers who don’t respond to antimalarials."
Dr. Clarke reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Psoriasis Severity Linked to Tonsil Size
BOSTON – Patients with psoriasis are almost nine times more likely to have enlarged tonsils, compared with patients without psoriasis, according to the results of a small study.
"Our findings suggest that hypertrophic tonsils may be associated with a pathogenic role in psoriasis," Dr. Marianna Shvartsbeyn and her coinvestigators reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. But it is still too soon to know the clinical implications.
In all, 32 patients with psoriasis and 14 patients with noninflammatory skin conditions (common warts, melanoma, and nonmelanoma skin diseases) were recruited. Patients who previously underwent tonsillectomy were excluded.
Tonsils were examined by one investigator, using a 5-point standardized tonsillar hypertrophy grading scale (adopted from Am. Fam. Physician 2004;69:1147-55).
Tonsils that were entirely within the tonsillar fossa received a grade of 0. Tonsils occupying less than 25% of the lateral dimension of the oropharynx, as measured between the anterior tonsillar pillars, received a grade of 1; tonsils occupying less than 50% of the lateral dimension of the oropharynx were a 2; tonsils occupying less than 75% of the lateral dimension of the oropharynx were a 3; and tonsils occupying 75 % or more of the lateral dimension of the oropharynx received a grade of 4.
Chart reviews were conducted to collect information on patient age, sex, race, social history (tobacco, alcohol, and drug use), diagnosis of skin condition, and the duration/severity of disease, noted Dr. Shvartsbeyn and her colleague of the departments of pathology and dermatology at the New York University.
Patients with psoriasis were found to have had an odds ratio of 8.77 for having enlarged tonsils (grade 2 or greater), compared with healthy controls. Tonsillar size also was significantly larger in patients with psoriasis (mean tonsil grade, 1.78), than in control patients (mean tonsil grade, 0.86); the severity of psoriasis was positively associated with tonsil size, Dr. Shvartsbeyn and her colleagues reported.
Limited clinical data have suggested that there is an association between hypertrophic tonsils and inflammatory skin disease. Small studies have shown that among patients with psoriasis, the cutaneous lesions disappeared or improved after tonsillectomy. It is suspected that there may be a genetic predisposition that makes certain patient populations more susceptible, the researchers noted.
Histopathologic studies also point to the possible link between the robust immune response that takes place in the tonsils and the changes in the skin of patients with pustulosis palmaris et plantaris (PPP).
Histologic evaluation of tonsils obtained from patients with PPP has revealed enlargement of the secondary T nodules and atrophy of the lymph follicles, with a decrease in the number of the germinal center cells and fibrosis – changes typically seen in older tonsils. This finding provides indirect evidence of the intensely advanced stage of the immune response within the tonsils.
"Our hypothesis is that in chronic tonsillar hypertrophy, bacterial species that reside in the tonsils are released into the circulation and cause stimulation of T cells. As a result of this constant chronic stimulation, an autoreactive clone may be formed. The auto-clone may produce an antibody attacking the skin and drive inflammatory response. In some individuals, this exaggerated immune response may manifest as psoriasis," the investigators wrote.
And although there is empirical evidence "that tonsillectomy improved skin lesions in patients with psoriasis and pustulosis palmaris et plantaris in small retrospective studies, further studies are needed. ... The observed association needs validation and interventional study is needed to prove causation/contribution," Dr. Shvartsbeyn noted in an interview.
The study was supported by grants from the National Cancer Institute, the National Institute for Allergy and Infectious Diseases, and the National Institute of Dental and Craniofacial Research. The investigators did not report having any conflicts of interest.
BOSTON – Patients with psoriasis are almost nine times more likely to have enlarged tonsils, compared with patients without psoriasis, according to the results of a small study.
"Our findings suggest that hypertrophic tonsils may be associated with a pathogenic role in psoriasis," Dr. Marianna Shvartsbeyn and her coinvestigators reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. But it is still too soon to know the clinical implications.
In all, 32 patients with psoriasis and 14 patients with noninflammatory skin conditions (common warts, melanoma, and nonmelanoma skin diseases) were recruited. Patients who previously underwent tonsillectomy were excluded.
Tonsils were examined by one investigator, using a 5-point standardized tonsillar hypertrophy grading scale (adopted from Am. Fam. Physician 2004;69:1147-55).
Tonsils that were entirely within the tonsillar fossa received a grade of 0. Tonsils occupying less than 25% of the lateral dimension of the oropharynx, as measured between the anterior tonsillar pillars, received a grade of 1; tonsils occupying less than 50% of the lateral dimension of the oropharynx were a 2; tonsils occupying less than 75% of the lateral dimension of the oropharynx were a 3; and tonsils occupying 75 % or more of the lateral dimension of the oropharynx received a grade of 4.
Chart reviews were conducted to collect information on patient age, sex, race, social history (tobacco, alcohol, and drug use), diagnosis of skin condition, and the duration/severity of disease, noted Dr. Shvartsbeyn and her colleague of the departments of pathology and dermatology at the New York University.
Patients with psoriasis were found to have had an odds ratio of 8.77 for having enlarged tonsils (grade 2 or greater), compared with healthy controls. Tonsillar size also was significantly larger in patients with psoriasis (mean tonsil grade, 1.78), than in control patients (mean tonsil grade, 0.86); the severity of psoriasis was positively associated with tonsil size, Dr. Shvartsbeyn and her colleagues reported.
Limited clinical data have suggested that there is an association between hypertrophic tonsils and inflammatory skin disease. Small studies have shown that among patients with psoriasis, the cutaneous lesions disappeared or improved after tonsillectomy. It is suspected that there may be a genetic predisposition that makes certain patient populations more susceptible, the researchers noted.
Histopathologic studies also point to the possible link between the robust immune response that takes place in the tonsils and the changes in the skin of patients with pustulosis palmaris et plantaris (PPP).
Histologic evaluation of tonsils obtained from patients with PPP has revealed enlargement of the secondary T nodules and atrophy of the lymph follicles, with a decrease in the number of the germinal center cells and fibrosis – changes typically seen in older tonsils. This finding provides indirect evidence of the intensely advanced stage of the immune response within the tonsils.
"Our hypothesis is that in chronic tonsillar hypertrophy, bacterial species that reside in the tonsils are released into the circulation and cause stimulation of T cells. As a result of this constant chronic stimulation, an autoreactive clone may be formed. The auto-clone may produce an antibody attacking the skin and drive inflammatory response. In some individuals, this exaggerated immune response may manifest as psoriasis," the investigators wrote.
And although there is empirical evidence "that tonsillectomy improved skin lesions in patients with psoriasis and pustulosis palmaris et plantaris in small retrospective studies, further studies are needed. ... The observed association needs validation and interventional study is needed to prove causation/contribution," Dr. Shvartsbeyn noted in an interview.
The study was supported by grants from the National Cancer Institute, the National Institute for Allergy and Infectious Diseases, and the National Institute of Dental and Craniofacial Research. The investigators did not report having any conflicts of interest.
BOSTON – Patients with psoriasis are almost nine times more likely to have enlarged tonsils, compared with patients without psoriasis, according to the results of a small study.
"Our findings suggest that hypertrophic tonsils may be associated with a pathogenic role in psoriasis," Dr. Marianna Shvartsbeyn and her coinvestigators reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. But it is still too soon to know the clinical implications.
In all, 32 patients with psoriasis and 14 patients with noninflammatory skin conditions (common warts, melanoma, and nonmelanoma skin diseases) were recruited. Patients who previously underwent tonsillectomy were excluded.
Tonsils were examined by one investigator, using a 5-point standardized tonsillar hypertrophy grading scale (adopted from Am. Fam. Physician 2004;69:1147-55).
Tonsils that were entirely within the tonsillar fossa received a grade of 0. Tonsils occupying less than 25% of the lateral dimension of the oropharynx, as measured between the anterior tonsillar pillars, received a grade of 1; tonsils occupying less than 50% of the lateral dimension of the oropharynx were a 2; tonsils occupying less than 75% of the lateral dimension of the oropharynx were a 3; and tonsils occupying 75 % or more of the lateral dimension of the oropharynx received a grade of 4.
Chart reviews were conducted to collect information on patient age, sex, race, social history (tobacco, alcohol, and drug use), diagnosis of skin condition, and the duration/severity of disease, noted Dr. Shvartsbeyn and her colleague of the departments of pathology and dermatology at the New York University.
Patients with psoriasis were found to have had an odds ratio of 8.77 for having enlarged tonsils (grade 2 or greater), compared with healthy controls. Tonsillar size also was significantly larger in patients with psoriasis (mean tonsil grade, 1.78), than in control patients (mean tonsil grade, 0.86); the severity of psoriasis was positively associated with tonsil size, Dr. Shvartsbeyn and her colleagues reported.
Limited clinical data have suggested that there is an association between hypertrophic tonsils and inflammatory skin disease. Small studies have shown that among patients with psoriasis, the cutaneous lesions disappeared or improved after tonsillectomy. It is suspected that there may be a genetic predisposition that makes certain patient populations more susceptible, the researchers noted.
Histopathologic studies also point to the possible link between the robust immune response that takes place in the tonsils and the changes in the skin of patients with pustulosis palmaris et plantaris (PPP).
Histologic evaluation of tonsils obtained from patients with PPP has revealed enlargement of the secondary T nodules and atrophy of the lymph follicles, with a decrease in the number of the germinal center cells and fibrosis – changes typically seen in older tonsils. This finding provides indirect evidence of the intensely advanced stage of the immune response within the tonsils.
"Our hypothesis is that in chronic tonsillar hypertrophy, bacterial species that reside in the tonsils are released into the circulation and cause stimulation of T cells. As a result of this constant chronic stimulation, an autoreactive clone may be formed. The auto-clone may produce an antibody attacking the skin and drive inflammatory response. In some individuals, this exaggerated immune response may manifest as psoriasis," the investigators wrote.
And although there is empirical evidence "that tonsillectomy improved skin lesions in patients with psoriasis and pustulosis palmaris et plantaris in small retrospective studies, further studies are needed. ... The observed association needs validation and interventional study is needed to prove causation/contribution," Dr. Shvartsbeyn noted in an interview.
The study was supported by grants from the National Cancer Institute, the National Institute for Allergy and Infectious Diseases, and the National Institute of Dental and Craniofacial Research. The investigators did not report having any conflicts of interest.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: Patients with psoriasis had an odds ratio of 8.77 for having enlarged tonsils (grade 2 or greater), compared with healthy controls.
Data Source: The findings come from a prospective study of 32 patients with psoriasis and 14 patients with noninflammatory skin conditions, who served as controls.
Disclosures: The study was supported by grants from the National Cancer Institute, the National Institute for Allergy and Infectious Diseases, and the National Institute of Dental and Craniofacial Research. The investigators did not report having any conflicts of interest.
Psoriasis Patients Still Going Unscreened for Heart Disease
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: Approximately 41% of psoriasis patients were screened for at least one of four risk factors for cardiovascular disease during outpatient visits, compared with 66.3% of patients without the chronic inflammatory disease.
Data Source: Analysis of data from the National Ambulatory Medical Care Survey on outpatient psoriasis visits from 2005-2009.
Disclosures: The Center for Dermatology Research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
Lipid Abnormalities Common in Granuloma Annulare
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: The prevalence of dyslipidemia among granuloma annulare patients was 79.3%, compared with 51.9% among matched controls.
Data Source: This was a two-center study of 140 adult patients with idiopathic granuloma annulare and 420 matched controls.
Disclosures: The investigators disclosed no financial conflicts of interest.
Acne Prescriptions for Topical Combination Therapy Rising
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: From 2007 to 2009, dermatologists and primary care physicians prescribed topical fixed combination treatment for 20% and 33.8% of their acne vulgaris patients, respectively.
Data Source: Analysis of data from the National Ambulatory Medical Care Survey on prescribing trends for the treatment of acne vulgaris for 1989-2009.
Disclosures: The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
Derm Research Unsettles Ped's Treatment of Acne
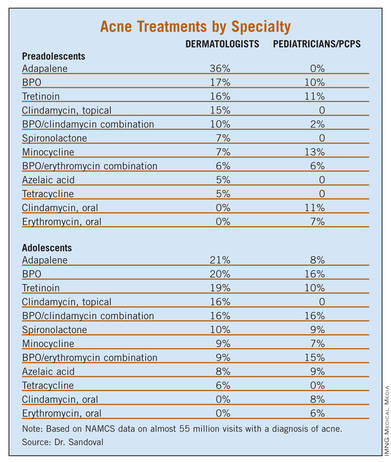
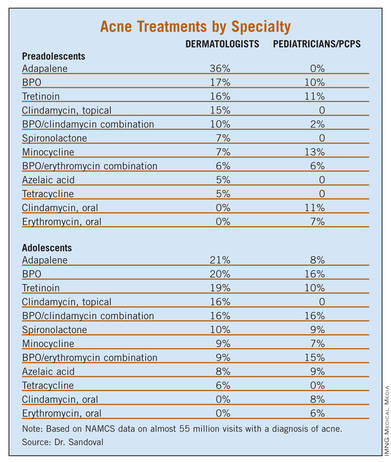
BOSTON – Pediatricians treat preadolescent acne nearly as often as dermatologists but appear to be less comfortable with the use of topical retinoids, according to the results of a study of almost 55 million pediatric acne visits.
"This study identifies a significant knowledge gap among pediatricians, in terms of treatment of acne based on age of the patient. This is especially important in the preadolescent age group, since pediatricians treat acne in this population nearly as much as dermatologists," Dr. Laura F. Sandoval wrote in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting.
Treatment by physicians in different specialties differed markedly. The younger the child, the more likely a pediatrician treated the acne; most (75.6%) neonatal or infantile acne was managed by a pediatrician. However, the older the child, the more likely a dermatologist treated the acne; slightly more than two-thirds (67.1%) of adolescent acne was managed by a dermatologist. Dermatologists and pediatricians almost equally managed preadolescent acne – 38.4% and 34.2%, respectively.
NAMCS (National Ambulatory Medical Care Survey) data were collected for outpatient visits of children receiving a diagnosis of acne vulgaris during 1993-2009. Patient visits were stratified by age groups: younger than 1 year (neonatal or infantile acne), 1-6 years (mid-childhood acne), 7-11 years (preadolescent acne), and 12-18 years (adolescent acne). Medications prescribed for each age group were compared across physician specialties.
There were almost 55 million estimated visits for patients aged 18 years and younger with a diagnosis of acne. Adolescent acne accounted for most of these visits (91.4%), followed by preadolescent visits (4.8%), mid-childhood visits (0.9%) and neonatal or infantile acne visits (3.0%).
Treatment of preadolescent and adolescent acne differed substantially between dermatologists and pediatricians/primary care physicians (PCPs), with prescribing differences being most pronounced in the preadolescent population. Topical retinoids were prescribed mainly by dermatologists in this age group, while oral antibiotics were preferred by pediatricians/PCPs.
"Comedonal acne is the most common type of acne in preadolescents and thus warrants the use of topical retinoids. Most PCPs have minimal dermatologic education and may be unaware of the benefits of retinoids," wrote Dr. Sandoval of the Center for Dermatology Research at Wake Forest University in Winston-Salem, N.C., and her coauthors.
The most common treatment for preadolescent acne across all specialties was adapalene (14.4%), followed by benzoyl peroxide [BPO] (12.8%), tretinoin (12.5%), minocycline (10.4%), and a combination of BPO/erythromycin (8.1%). The most common treatment for adolescent acne was tretinoin (19.5%), followed by isotretinoin (18.1%), minocycline (16.9%), BPO (16.1%) and adapalene (14.1%).
Isotretinoin was the only medication commonly prescribed in adolescents but not in preadolescents, by both dermatologists and pediatricians/PCPs.
This could be because severe acne is typically rare in young children, according to Dr. Sandoval and her colleagues. And, severity is not recorded by the NAMCS, making it difficult to determine whether preadolescent children had severe enough acne to warrant the use of isotretinoin.
However, when topicals, BPO, and antibiotics fail, isotretinoin should be considered, the researchers noted. Also, isotretinoin should be considered in preadolescents when scarring is a concern.
While dermatologists prescribed isotretinoin and topical retinoids more frequently for adolescent acne than did pediatricians/PCPs, "Hesitancy to prescribe isotretinoin by PCPs may be due to strict requirements of federal monitoring programs, the need for monitoring blood work, and/or safety concerns," the authors noted.
Although tetracycline is the only Food and Drug Administration–approved drug for use in children aged 8 years and older, the data showed it was prescribed to an estimated 120,000 patients younger than 8 years, including children as young as 3 years. This practice was seen among both dermatologists and pediatricians. In all cases, it was used in conjunction with tretinoin, BPO, and/or topical clindamycin.
Minocycline is only FDA approved for use in patients 12 years and older. However, it was prescribed more often in younger patients than are doxycycline and tetracycline by both dermatologists and pediatricians/PCPs.
"All specialties recognize that off-label prescribing is necessary given the very limited range of treatment that is currently FDA-approved for preadolescent patients," the researchers wrote. "PCPs may have outdated concerns in regards to the efficacy and tolerability of retinoids, which is not supported by newer retinoid formulations."
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. Principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
BOSTON – Pediatricians treat preadolescent acne nearly as often as dermatologists but appear to be less comfortable with the use of topical retinoids, according to the results of a study of almost 55 million pediatric acne visits.
"This study identifies a significant knowledge gap among pediatricians, in terms of treatment of acne based on age of the patient. This is especially important in the preadolescent age group, since pediatricians treat acne in this population nearly as much as dermatologists," Dr. Laura F. Sandoval wrote in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting.
Treatment by physicians in different specialties differed markedly. The younger the child, the more likely a pediatrician treated the acne; most (75.6%) neonatal or infantile acne was managed by a pediatrician. However, the older the child, the more likely a dermatologist treated the acne; slightly more than two-thirds (67.1%) of adolescent acne was managed by a dermatologist. Dermatologists and pediatricians almost equally managed preadolescent acne – 38.4% and 34.2%, respectively.
NAMCS (National Ambulatory Medical Care Survey) data were collected for outpatient visits of children receiving a diagnosis of acne vulgaris during 1993-2009. Patient visits were stratified by age groups: younger than 1 year (neonatal or infantile acne), 1-6 years (mid-childhood acne), 7-11 years (preadolescent acne), and 12-18 years (adolescent acne). Medications prescribed for each age group were compared across physician specialties.
There were almost 55 million estimated visits for patients aged 18 years and younger with a diagnosis of acne. Adolescent acne accounted for most of these visits (91.4%), followed by preadolescent visits (4.8%), mid-childhood visits (0.9%) and neonatal or infantile acne visits (3.0%).
Treatment of preadolescent and adolescent acne differed substantially between dermatologists and pediatricians/primary care physicians (PCPs), with prescribing differences being most pronounced in the preadolescent population. Topical retinoids were prescribed mainly by dermatologists in this age group, while oral antibiotics were preferred by pediatricians/PCPs.
"Comedonal acne is the most common type of acne in preadolescents and thus warrants the use of topical retinoids. Most PCPs have minimal dermatologic education and may be unaware of the benefits of retinoids," wrote Dr. Sandoval of the Center for Dermatology Research at Wake Forest University in Winston-Salem, N.C., and her coauthors.
The most common treatment for preadolescent acne across all specialties was adapalene (14.4%), followed by benzoyl peroxide [BPO] (12.8%), tretinoin (12.5%), minocycline (10.4%), and a combination of BPO/erythromycin (8.1%). The most common treatment for adolescent acne was tretinoin (19.5%), followed by isotretinoin (18.1%), minocycline (16.9%), BPO (16.1%) and adapalene (14.1%).
Isotretinoin was the only medication commonly prescribed in adolescents but not in preadolescents, by both dermatologists and pediatricians/PCPs.
This could be because severe acne is typically rare in young children, according to Dr. Sandoval and her colleagues. And, severity is not recorded by the NAMCS, making it difficult to determine whether preadolescent children had severe enough acne to warrant the use of isotretinoin.
However, when topicals, BPO, and antibiotics fail, isotretinoin should be considered, the researchers noted. Also, isotretinoin should be considered in preadolescents when scarring is a concern.
While dermatologists prescribed isotretinoin and topical retinoids more frequently for adolescent acne than did pediatricians/PCPs, "Hesitancy to prescribe isotretinoin by PCPs may be due to strict requirements of federal monitoring programs, the need for monitoring blood work, and/or safety concerns," the authors noted.
Although tetracycline is the only Food and Drug Administration–approved drug for use in children aged 8 years and older, the data showed it was prescribed to an estimated 120,000 patients younger than 8 years, including children as young as 3 years. This practice was seen among both dermatologists and pediatricians. In all cases, it was used in conjunction with tretinoin, BPO, and/or topical clindamycin.
Minocycline is only FDA approved for use in patients 12 years and older. However, it was prescribed more often in younger patients than are doxycycline and tetracycline by both dermatologists and pediatricians/PCPs.
"All specialties recognize that off-label prescribing is necessary given the very limited range of treatment that is currently FDA-approved for preadolescent patients," the researchers wrote. "PCPs may have outdated concerns in regards to the efficacy and tolerability of retinoids, which is not supported by newer retinoid formulations."
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. Principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
BOSTON – Pediatricians treat preadolescent acne nearly as often as dermatologists but appear to be less comfortable with the use of topical retinoids, according to the results of a study of almost 55 million pediatric acne visits.
"This study identifies a significant knowledge gap among pediatricians, in terms of treatment of acne based on age of the patient. This is especially important in the preadolescent age group, since pediatricians treat acne in this population nearly as much as dermatologists," Dr. Laura F. Sandoval wrote in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting.
Treatment by physicians in different specialties differed markedly. The younger the child, the more likely a pediatrician treated the acne; most (75.6%) neonatal or infantile acne was managed by a pediatrician. However, the older the child, the more likely a dermatologist treated the acne; slightly more than two-thirds (67.1%) of adolescent acne was managed by a dermatologist. Dermatologists and pediatricians almost equally managed preadolescent acne – 38.4% and 34.2%, respectively.
NAMCS (National Ambulatory Medical Care Survey) data were collected for outpatient visits of children receiving a diagnosis of acne vulgaris during 1993-2009. Patient visits were stratified by age groups: younger than 1 year (neonatal or infantile acne), 1-6 years (mid-childhood acne), 7-11 years (preadolescent acne), and 12-18 years (adolescent acne). Medications prescribed for each age group were compared across physician specialties.
There were almost 55 million estimated visits for patients aged 18 years and younger with a diagnosis of acne. Adolescent acne accounted for most of these visits (91.4%), followed by preadolescent visits (4.8%), mid-childhood visits (0.9%) and neonatal or infantile acne visits (3.0%).
Treatment of preadolescent and adolescent acne differed substantially between dermatologists and pediatricians/primary care physicians (PCPs), with prescribing differences being most pronounced in the preadolescent population. Topical retinoids were prescribed mainly by dermatologists in this age group, while oral antibiotics were preferred by pediatricians/PCPs.
"Comedonal acne is the most common type of acne in preadolescents and thus warrants the use of topical retinoids. Most PCPs have minimal dermatologic education and may be unaware of the benefits of retinoids," wrote Dr. Sandoval of the Center for Dermatology Research at Wake Forest University in Winston-Salem, N.C., and her coauthors.
The most common treatment for preadolescent acne across all specialties was adapalene (14.4%), followed by benzoyl peroxide [BPO] (12.8%), tretinoin (12.5%), minocycline (10.4%), and a combination of BPO/erythromycin (8.1%). The most common treatment for adolescent acne was tretinoin (19.5%), followed by isotretinoin (18.1%), minocycline (16.9%), BPO (16.1%) and adapalene (14.1%).
Isotretinoin was the only medication commonly prescribed in adolescents but not in preadolescents, by both dermatologists and pediatricians/PCPs.
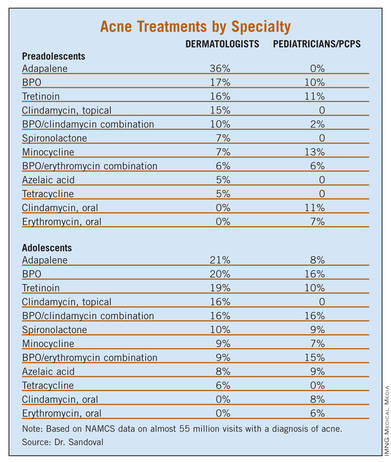
This could be because severe acne is typically rare in young children, according to Dr. Sandoval and her colleagues. And, severity is not recorded by the NAMCS, making it difficult to determine whether preadolescent children had severe enough acne to warrant the use of isotretinoin.
However, when topicals, BPO, and antibiotics fail, isotretinoin should be considered, the researchers noted. Also, isotretinoin should be considered in preadolescents when scarring is a concern.
While dermatologists prescribed isotretinoin and topical retinoids more frequently for adolescent acne than did pediatricians/PCPs, "Hesitancy to prescribe isotretinoin by PCPs may be due to strict requirements of federal monitoring programs, the need for monitoring blood work, and/or safety concerns," the authors noted.
Although tetracycline is the only Food and Drug Administration–approved drug for use in children aged 8 years and older, the data showed it was prescribed to an estimated 120,000 patients younger than 8 years, including children as young as 3 years. This practice was seen among both dermatologists and pediatricians. In all cases, it was used in conjunction with tretinoin, BPO, and/or topical clindamycin.
Minocycline is only FDA approved for use in patients 12 years and older. However, it was prescribed more often in younger patients than are doxycycline and tetracycline by both dermatologists and pediatricians/PCPs.
"All specialties recognize that off-label prescribing is necessary given the very limited range of treatment that is currently FDA-approved for preadolescent patients," the researchers wrote. "PCPs may have outdated concerns in regards to the efficacy and tolerability of retinoids, which is not supported by newer retinoid formulations."
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. Principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: Most (75.6%) neonatal and infantile acne was managed by a pediatrician, while most (67.1%) adolescent acne was managed by a dermatologist.
Data Source: NAMCS data was collected for outpatient visits by children receiving a diagnosis of acne vulgaris from 1993 to 2009.
Disclosures: The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. Principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
Infantile Hemangioma Growth Peaks in Second Month of Life
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Acanthosis Nigricans Severity Helps Predict Diabetes Risk
BOSTON – Patients with a high grade of acanthosis nigricans should be screened for insulin resistance, according to Dr. Sandhya Venkatswami.
His cross-sectional study found that 47 of 150 acanthosis nigricans patients (31%) were insulin resistant, with an acanthosis nigricans grade of 3 or 4 being more predictive of the condition.
"We suggest that all patients with severe AN [acanthosis nigricans] grades should be evaluated for IR [insulin resistance] and thereby prevent further complications," wrote Dr. Venkatswami, who presented his findings during a poster session at the American Academy of Dermatology’s Summer Academy Meeting.
While previous studies have found acanthosis nigricans to be a marker for prediabetes, Dr. Venkatswami’s study found that taking severity into account helps to further identify patients who may be at risk.
He and his fellow investigators enrolled 150 consecutive patients with acanthosis nigricans of the neck (25 males), aged 18-64 years. The patients were graded according to acanthosis nigricans severity on a scale of I-IV.
Grade I was defined as acanthosis nigricans that was only visible on close inspection (21 patients); grade II was defined as acanthosis nigricans confined to the base of the skull (58 patients); grade III was defined as acanthosis nigricans that extended laterally to the posterior border of the sternocleidomastoid but was not visible when the patient was facing forward (48 patients); and grade IV was defined as acanthosis nigricans that was visible when the patient was facing forward, as the acanthosis nigricans encircled the neck (23 patients), said Dr. Venkatswami of the department of dermatology, Sri Ramachandra University, Chennai, India.
One patient with grade I acanthosis nigricans was found to be insulin resistant; 10 patients with grade II acanthosis nigricans were found to be insulin resistance; 20 patients with grade III acanthosis nigricans were insulin resistant; and 16 patients with grade IV showed a resistance to insulin.
Secondary study findings showed that patients with higher grades of texture of acanthosis nigricans were also more likely to be insulin resistant. That is, those with visible and extremely coarse "hills and valleys."
"AN lesions are asymptomatic and usually ignored by the patients unless they are of cosmetic concern. However, this is of clinical importance in diagnosing prediabetes," he noted in his poster.
Further studies will look to see if behavior modifications will help lower the risk for diabetes in patients with the condition.
Dr. Venkatswami did not disclose having any conflicts of interest.
BOSTON – Patients with a high grade of acanthosis nigricans should be screened for insulin resistance, according to Dr. Sandhya Venkatswami.
His cross-sectional study found that 47 of 150 acanthosis nigricans patients (31%) were insulin resistant, with an acanthosis nigricans grade of 3 or 4 being more predictive of the condition.
"We suggest that all patients with severe AN [acanthosis nigricans] grades should be evaluated for IR [insulin resistance] and thereby prevent further complications," wrote Dr. Venkatswami, who presented his findings during a poster session at the American Academy of Dermatology’s Summer Academy Meeting.
While previous studies have found acanthosis nigricans to be a marker for prediabetes, Dr. Venkatswami’s study found that taking severity into account helps to further identify patients who may be at risk.
He and his fellow investigators enrolled 150 consecutive patients with acanthosis nigricans of the neck (25 males), aged 18-64 years. The patients were graded according to acanthosis nigricans severity on a scale of I-IV.
Grade I was defined as acanthosis nigricans that was only visible on close inspection (21 patients); grade II was defined as acanthosis nigricans confined to the base of the skull (58 patients); grade III was defined as acanthosis nigricans that extended laterally to the posterior border of the sternocleidomastoid but was not visible when the patient was facing forward (48 patients); and grade IV was defined as acanthosis nigricans that was visible when the patient was facing forward, as the acanthosis nigricans encircled the neck (23 patients), said Dr. Venkatswami of the department of dermatology, Sri Ramachandra University, Chennai, India.
One patient with grade I acanthosis nigricans was found to be insulin resistant; 10 patients with grade II acanthosis nigricans were found to be insulin resistance; 20 patients with grade III acanthosis nigricans were insulin resistant; and 16 patients with grade IV showed a resistance to insulin.
Secondary study findings showed that patients with higher grades of texture of acanthosis nigricans were also more likely to be insulin resistant. That is, those with visible and extremely coarse "hills and valleys."
"AN lesions are asymptomatic and usually ignored by the patients unless they are of cosmetic concern. However, this is of clinical importance in diagnosing prediabetes," he noted in his poster.
Further studies will look to see if behavior modifications will help lower the risk for diabetes in patients with the condition.
Dr. Venkatswami did not disclose having any conflicts of interest.
BOSTON – Patients with a high grade of acanthosis nigricans should be screened for insulin resistance, according to Dr. Sandhya Venkatswami.
His cross-sectional study found that 47 of 150 acanthosis nigricans patients (31%) were insulin resistant, with an acanthosis nigricans grade of 3 or 4 being more predictive of the condition.
"We suggest that all patients with severe AN [acanthosis nigricans] grades should be evaluated for IR [insulin resistance] and thereby prevent further complications," wrote Dr. Venkatswami, who presented his findings during a poster session at the American Academy of Dermatology’s Summer Academy Meeting.
While previous studies have found acanthosis nigricans to be a marker for prediabetes, Dr. Venkatswami’s study found that taking severity into account helps to further identify patients who may be at risk.
He and his fellow investigators enrolled 150 consecutive patients with acanthosis nigricans of the neck (25 males), aged 18-64 years. The patients were graded according to acanthosis nigricans severity on a scale of I-IV.
Grade I was defined as acanthosis nigricans that was only visible on close inspection (21 patients); grade II was defined as acanthosis nigricans confined to the base of the skull (58 patients); grade III was defined as acanthosis nigricans that extended laterally to the posterior border of the sternocleidomastoid but was not visible when the patient was facing forward (48 patients); and grade IV was defined as acanthosis nigricans that was visible when the patient was facing forward, as the acanthosis nigricans encircled the neck (23 patients), said Dr. Venkatswami of the department of dermatology, Sri Ramachandra University, Chennai, India.
One patient with grade I acanthosis nigricans was found to be insulin resistant; 10 patients with grade II acanthosis nigricans were found to be insulin resistance; 20 patients with grade III acanthosis nigricans were insulin resistant; and 16 patients with grade IV showed a resistance to insulin.
Secondary study findings showed that patients with higher grades of texture of acanthosis nigricans were also more likely to be insulin resistant. That is, those with visible and extremely coarse "hills and valleys."
"AN lesions are asymptomatic and usually ignored by the patients unless they are of cosmetic concern. However, this is of clinical importance in diagnosing prediabetes," he noted in his poster.
Further studies will look to see if behavior modifications will help lower the risk for diabetes in patients with the condition.
Dr. Venkatswami did not disclose having any conflicts of interest.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: Of 150 patients with acanthosis nigricans, 47 (31%) were insulin resistant.
Data Source: A cross-sectional study of 150 consecutive patients with acanthosis nigricans of the neck who presented to a dermatology practice.
Disclosures: Dr. Venkatswami did not disclose having any conflicts of interest.
Blog: Check Infants to ID Family Infestations
Think you’ve got a parasite infestation going on in your patient’s home but can’t identify the culprit?
"If you’re trying to make a diagnosis and you’re having difficulty finding the organism ... bring in the infants. They don’t scratch well," Dr. Bernard Cohen said at the American Academy of Dermatology’s Summer Academy meeting in Boston. In the case of scabies in infants (Sarcoptes scabiei var. hominis), "you’ll see tons of burrows, and your scrapings should be positive close to 100% of the time."
How should you treat infants with scabies? Permethrin 5% cream is approved for infants 2 months and older, said Dr. Cohen, who is director of pediatric dermatology at the Johns Hopkins Children’s Center in Baltimore.
–Kerri Wachter (@knwachter on Twitter)
Think you’ve got a parasite infestation going on in your patient’s home but can’t identify the culprit?
"If you’re trying to make a diagnosis and you’re having difficulty finding the organism ... bring in the infants. They don’t scratch well," Dr. Bernard Cohen said at the American Academy of Dermatology’s Summer Academy meeting in Boston. In the case of scabies in infants (Sarcoptes scabiei var. hominis), "you’ll see tons of burrows, and your scrapings should be positive close to 100% of the time."
How should you treat infants with scabies? Permethrin 5% cream is approved for infants 2 months and older, said Dr. Cohen, who is director of pediatric dermatology at the Johns Hopkins Children’s Center in Baltimore.
–Kerri Wachter (@knwachter on Twitter)
Think you’ve got a parasite infestation going on in your patient’s home but can’t identify the culprit?
"If you’re trying to make a diagnosis and you’re having difficulty finding the organism ... bring in the infants. They don’t scratch well," Dr. Bernard Cohen said at the American Academy of Dermatology’s Summer Academy meeting in Boston. In the case of scabies in infants (Sarcoptes scabiei var. hominis), "you’ll see tons of burrows, and your scrapings should be positive close to 100% of the time."
How should you treat infants with scabies? Permethrin 5% cream is approved for infants 2 months and older, said Dr. Cohen, who is director of pediatric dermatology at the Johns Hopkins Children’s Center in Baltimore.
–Kerri Wachter (@knwachter on Twitter)
Blog: AAD President Shaves Head for SkinPAC
American Academy of Dermatology President, Dr. Daniel M. Siegel, had his head publicly shaved at the Summer Academy Meeting in Boston to celebrate $1 million in contributions to SkinPAC, the AAD's political action committee. The highest donors took turns shaving Dr. Siegel's locks.
American Academy of Dermatology President, Dr. Daniel M. Siegel, had his head publicly shaved at the Summer Academy Meeting in Boston to celebrate $1 million in contributions to SkinPAC, the AAD's political action committee. The highest donors took turns shaving Dr. Siegel's locks.
American Academy of Dermatology President, Dr. Daniel M. Siegel, had his head publicly shaved at the Summer Academy Meeting in Boston to celebrate $1 million in contributions to SkinPAC, the AAD's political action committee. The highest donors took turns shaving Dr. Siegel's locks.