User login
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
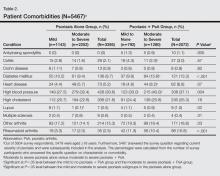
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
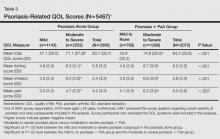
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
Approximately 3% of the US adult population, or roughly 5 million Americans, have been diagnosed with psoriasis.1 Psoriasis has a high disease burden, with one review of 817 quality-of-life (QOL) studies concluding that the degree to which psoriasis negatively affects patients’ QOL is comparable with major diseases such as diabetes mellitus or cancer.2
Psoriatic arthritis (PsA) is a chronic, often progressive, inflammatory arthropathy that can lead to permanent joint damage and severe disability.3,4 Psoriatic arthritis is a common comorbidity among patients with psoriasis, affecting 6% to 10% of psoriasis patients overall5 and 20% to 40% of psoriasis patients with more extensive skin involvement.5-7
The comorbidity profile and overall disease impact are not well understood in psoriasis patients with and without comorbid PsA. The primary objective of this study was to compare disease characteristics, comorbidities, and psoriasis-related QOL in patients with moderate to severe psoriasis with and without comorbid PsA.
Methods
Study Design and Participants
Since 2003 the National Psoriasis Foundation (NPF) has conducted semiannual survey panels to collect patient-reported data on topics including disease characteristics, treatment utilization, and psoriasis-related QOL impact. Responses from approximately 5604 individuals have been collected and analyzed from a total of 13 survey panels conducted from 2003-2009 and 2011. No data were available for 2010. In each survey panel, responses from approximately 400 randomly selected respondents were collected, with approximately 300 respondents having moderate to severe psoriasis and 200 respondents being NPF members. Respondents were surveyed via telephone and the Internet.
This study examined 2 main patient groups: (1) adults (>18 years of age) with psoriasis alone and (2) those with comorbid PsA. The 2 study groups were subdivided according to percentage of body surface area (BSA) affected; specifically, patients with psoriasis alone were classified as having mild psoriasis (<3% BSA) or moderate to severe psoriasis (>3% BSA) and patients with PsA were classified as having mild to no psoriasis (<3% BSA) or moderate to severe psoriasis (≥3% BSA).8
Assessments
Comparisons of patient demographics, disease characteristics, comorbidities, psoriasis-related QOL, and symptom impact were made for patients with moderate to severe psoriasis and PsA versus those with moderate to severe psoriasis alone. The overall impact of psoriasis on patients’ physical and emotional QOL was assessed via a 12-item survey with each item rated on an 11-point scale (0=not at all; 5=somewhat; 10=very much). Total QOL scores ranged from 0 to 120. Higher scores indicated greater (ie, worse) impact of psoriasis on the patient’s QOL. To evaluate symptom impact (ie, to what degree a patient felt affected by individual symptoms), ratings from 3 symptoms—itching, irritation, and pain—that were included in the overall QOL assessment also were analyzed individually. Results also were compared for patients with mild psoriasis alone versus those with moderate to severe psoriasis alone as well as for patients with PsA and mild to no psoriasis versus those with PsA and moderate to severe psoriasis.
Statistical Analysis
Adult survey respondents who answered survey questions relevant to the analysis were included. For patient demographics and comorbidities, t tests were used for continuous variables and Χ2 tests were used for categorical variables. For overall psoriasis-related QOL and symptom impact scores, differences among the study groups were compared using analyses of covariance, which adjusted for age, gender, and race. All analyses were conducted using SAS version 9.2.
Results
Patient Demographics
Of 5467 total respondents, 3532 reported moderate to severe psoriasis of which 1280 (36.2%) had comorbid PsA (Table 1). Compared to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA were older, less commonly male, less likely to be employed, had a longer duration of psoriasis, were more likely to be white, and were more likely to have health insurance coverage. Among the psoriasis alone group, those patients reporting moderate to severe psoriasis were younger, less likely to have health insurance coverage, and were less likely to be treated by a dermatologist only than those with mild psoriasis. Among the group with PsA, patients with moderate to severe psoriasis were more likely to be treated by a dermatologist only versus those with mild or no psoriasis (Table 1).
Patient Comorbidities
Patients with moderate to severe psoriasis and comorbid PsA reported significantly higher rates of diabetes mellitus, lupus, rheumatoid arthritis, other arthritis, ankylosing spondylitis, and high blood pressure than patients with moderate to severe psoriasis alone (P<.05)(Table 2). In the group with psoriasis alone, patients with moderate to severe psoriasis had significantly lower rates of lupus compared to those with mild psoriasis (P<.05). In the group with PsA, patients with moderate to severe psoriasis were significantly more likely to report diagnoses of colitis, diabetes mellitus, heart disease, and high blood pressure compared to those with mild to no psoriasis (P<.05).
Psoriasis-Related QOL
The psoriasis-related QOL analyses are shown in Table 3. Patients with moderate to severe psoriasis and comorbid PsA reported a greater impact on overall QOL compared to their counterparts with moderate to severe psoriasis alone. Similarly, patients with moderate to severe psoriasis and comorbid PsA reported a greater impact of itching, physical irritation/soreness, and pain symptoms.
Disease severity was associated with psoriasis-related QOL. Compared to patients with mild psoriasis alone, those with moderate to severe psoriasis alone had significantly higher (ie, worse) scores in the categories of itching, irritation, pain, and overall QOL (P<.05). In the PsA group, patients with moderate to severe psoriasis also reported significantly worse itching, irritation, pain, and overall QOL compared to their counterparts with mild to no psoriasis (P<.05).
Comment
The results of this study showed that patient demographics, comorbidities, and psoriasis-related QOL in psoriasis patients varied significantly depending on presence or absence of comorbid PsA as well as disease severity. Patients with more severe cutaneous psoriasis with and without PsA were associated with worse QOL scores and higher rates of self-reported heart disease and hypertension. Among patients with moderate to severe psoriasis, those with comorbid PsA were associated with greater rates of self-reported diabetes mellitus and high blood pressure and worse QOL scores including worse itching, irritation, and pain than those with moderate to severe psoriasis alone.
The present study is one of the first to compare psoriasis-related QOL in patients with and without PsA. A prior study demonstrated patients with PsA had worse physical impairment, fatigue severity, and health status relative to patients with psoriasis alone but no differences in dermatology-specific QOL measures.9 Our analysis revealed that patients with moderate to severe psoriasis and comorbid PsA experienced a greater impact on overall QOL as well as symptoms of itching, irritation, and pain relative to patients with moderate to severe psoriasis alone. Among both treatment groups, reports of overall QOL and itching, irritation, and pain became worse as the disease severity increased. These findings are consistent with prior studies that have shown greater impairment of QOL among patients with severe psoriasis compared to mild psoriasis.10-12
Relative to patients with moderate to severe psoriasis alone, those with moderate to severe psoriasis and comorbid PsA reported a greater prevalence of comorbid diagnoses overall, with notably higher rates of type 2 diabetes mellitus, hypertension, and rheumatoid arthritis. These findings are consistent with an earlier report by Husted et al.13
Limitations
The results of this study should be interpreted in light of several important limitations associated with survey data (ie, patient-reported data, no details on length of therapy or comorbid disease, multiple surveys taken over time, respondents aged >18 years only).
Conclusion
This study provides evidence that patients with moderate to severe psoriasis and comorbid PsA have a higher psoriasis-related disease burden compared to those with moderate to severe psoriasis alone, which suggests that physicians may wish to consider this comorbidity when designing patient treatment plans. Our findings also confirm that disease severity is associated with comorbid conditions and psoriasis-related QOL impact in psoriasis patients. These findings highlight the importance of screening for PsA in patients with psoriasis and effective treatment of skin disease in patients with PsA.
Acknowledgment
The authors thank Maureen Lage, PhD, Healthmetrics, Bonita Springs, Florida, for her work in drafting the manuscript.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
2. Raho G, Koleva DM, Garattini L, et al. The burden of moderate to severe psoriasis: an overview. Pharmacoeconomics. 2012;30:1005-1013.
3. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis. 2005;64(suppl 2):14-17.
4. Ogdie A, Langan S, Love T, et al. Prevalence and treatment patterns of psoriatic arthritis in the UK. Rheumatology (Oxford). 2013;52:568-575.
5. Ogdie A, Gelfand JM. Identification of risk factors for psoriatic arthritis: scientific opportunity meets clinical need. Arch Dermatol. 2010;146:785-788.
6. Gelfand JM, Gladman DD, Mease PJ, et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.
7. Richardson SK, Gelfand JM. Update on the natural history and systemic treatment of psoriasis. Adv Dermatol. 2008;24:171-196.
8. Armstrong AW, Robertson AD, Wu J, et al. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003-2011. JAMA Dermatol. 2013;149:1180-1185.
9. Rosen CF, Mussani F, Chandran V, et al. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571-576.
10. Armstrong AW, Schupp C, Wu J, et al. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS ONE. 2012;7:e52935.
11. Colombo G, Altomare G, Peris K, et al. Moderate and severe plaque psoriasis: cost-of-illness study in Italy. Ther Clin Risk Manag. 2008;4:559-568.
12. Gelfand JM, Feldman SR, Stern RS, et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J Am Acad Dermatol. 2004;51:704-708.
13. Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729-1735.
Practice Points
- Patients with psoriatic arthritis (PsA) often have severe cutaneous psoriasis. These patients may be at higher risk for comorbid conditions and impaired quality of life (QOL) compared to patients with psoriasis alone.
- The severity of cutaneous psoriasis, both in patients with psoriasis alone and those with comorbid PsA, is remarkable and is associated with worse QOL scores.