User login
A Facility-Wide Plan to Increase Access to Medication for Opioid Use Disorder in Primary Care and General Mental Health Settings
In the United States, opioid use disorder (OUD) is a major public health challenge. In 2018 drug overdose deaths were 4 times higher than they were in 1999.1 This increase highlights a critical need to expand treatment access. Medication for opioid use disorder (MOUD), including methadone, naltrexone, and buprenorphine, improves outcomes for patients retained in care.2 Compared with the general population, veterans, particularly those with co-occurring posttraumatic stress disorder (PTSD) or depression, are more likely to receive higher dosages of opioid medications and experience opioid-related adverse outcomes (eg, overdose, OUD).3,4 As a risk reduction strategy, patients receiving potentially dangerous full-dose agonist opioid medication who are unable to taper to safer dosages may be eligible to transition to buprenorphine.5
Buprenorphine and naltrexone can be prescribed in office-based settings or in addiction, primary care, mental health, and pain clinics. Office-based opioid treatment with buprenorphine (OBOT-B) expands access to patients who are not reached by addiction treatment programs.6,7 This is particularly true in rural settings, where addiction care services are typically scarce.8 OBOT-B prevents relapse and maintains opioid-free days and may increase patient engagement by reducing stigma and providing treatment within an existing clinical care team.9 For many patients, OBOT-B results in good retention with just medical monitoring and minimal or no ancillary addiction counseling.10,11
Successful implementation of OBOT-B has occurred through a variety of care models in selected community health care settings.8,12,13 Historically in the Veterans Health Administration (VHA), MOUD has been prescribed in substance use disorder clinics by mental health practitioners. Currently, more than 44% of veterans with OUD are on MOUD.14
The VHA has invested significant resources to improve access to MOUD. In 2018, the Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative launched, with the aim to improve access within primary care, mental health, and pain clinics.15 SCOUTT emphasizes stepped-care treatment, with patients engaging in the step of care most appropriate to their needs. Step 0 is self-directed care/self-management, including mutual support groups; step-1 environments include office-based primary care, mental health, and pain clinics; and step-2 environments are specialty care settings. Through a series of remote webinars, an in-person national 2-day conference, and external facilitation, SCOUTT engaged 18 teams representing each Veterans Integrated Service Network (VISN) across the country to assist in implementing MOUD within 2 step-1 clinics. These teams have developed several models of providing step-1 care, including an interdisciplinary team-based primary care delivery model as well as a pharmacist care manager model.16, 17
US Department of Veterans Affairs (VA) Connecticut Health Care System (VACHS), which delivers care to approximately 58,000 veterans, was chosen to be a phase 1 SCOUTT site. Though all patients in VACHS have access to specialty care step-2 clinics, including methadone and buprenorphine programs, there remained many patients not yet on MOUD who could benefit from it. Baseline data (fiscal year [FY] 2018 4th quarter), obtained through electronic health record (EHR) database dashboards indicated that 710 (56%) patients with an OUD diagnosis were not receiving MOUD. International Classification of Disease, 10th Revision codes are the foundation for VA population management dashboards, and based their data on codes for opioid abuse and opioid dependence. These tools are limited by the accuracy of coding in EHRs. Additionally, 366 patients receiving long-term opioid prescriptions were identified as moderate, high, or very high risk for overdose or death based on an algorithm that considered prescribed medications, sociodemographics, and comorbid conditions, as characterized in the VA EHR (Stratification Tool for Opioid Risk Mitigation [STORM] report).18
This article describes the VACHSquality-improvement effort to extend OBOT-B into step-1 primary care and general mental health clinics. Our objectives are to (1) outline the process for initiating SCOUTT within VACHS; (2) examine barriers to implementation and the SCOUTT team response; (3) review VACHS patient and prescriber data at baseline and 1 year after implementation; and (4) explore future implementation strategies.
SCOUTT Team
A VACHS interdisciplinary team was formed and attended the national SCOUTT kickoff conference in 2018.15 Similar to other SCOUTT teams, the team consisted of VISN leadership (in primary care, mental health, and addiction care), pharmacists, and a team of health care practitioners (HCPs) from step-2 clinics (including 2 addiction psychiatrists, and an advanced practice registered nurse, a registered nurse specializing in addiction care), and a team of HCPs from prospective step-1 clinics (including a clinical psychologist and 2 primary care physicians). An external facilitator was provided from outside the VISN who met remotely with the team to assist in facilitation. Our team met monthly, with the goal to identify local barriers and facilitators to OBOT-B and implement interventions to enhance prescribing in step-1 primary care and general mental health clinics.
Implementation Steps
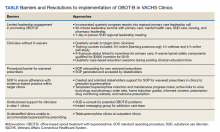
The team identified multiple barriers to dissemination of OBOT-B in target clinics (Table). The 3 main barriers were limited leadership engagement in promoting OBOT-B in target clinics, inadequate number of HCPs with active X-waivered prescribing status in the targeted clinics, and the need for standardized processes and tools to facilitate prescribing and follow-up.
To address leadership engagement, the SCOUTT team held quarterly presentations of SCOUTT goals and progress on target clinic leadership calls (usually 15 minutes) and arranged a 90-minute multidisciplinary leadership summit with key leadership representation from primary care, general mental health, specialty addiction care, nursing, and pharmacy. To enhance X-waivered prescribers in target clinics, the SCOUTT team sent quarterly emails with brief education points on MOUD and links to waiver trainings. At the time of implementation, in order to prescribe buprenorphine and meet qualifications to treat OUD, prescribers were required to complete specialized training as necessitated by the Drug Addiction Treatment Act of 2000. X-waivered status can now be obtained without requiring training
The SCOUTT team advocated for X-waivered status to be incentivized by performance pay for primary care practitioners and held quarterly case-based education sessions during preexisting allotted time. The onboarding process for new waivered prescribers to navigate from waiver training to active prescribing within the EHR was standardized via development of a standard operating procedure (SOP).
The SCOUTT team also assisted in the development of standardized processes and tools for prescribing in target clinics, including implementation of a standard operating procedure regarding prescribing (both initiation of buprenorphine, and maintenance) in target clinics. This procedure specifies that target clinic HCPs prescribe for patients requiring less intensive management, and who are appropriate for office-based treatment based on specific criteria (eAppendix
Templated progress notes were created for buprenorphine initiation and buprenorphine maintenance with links to recommended laboratory tests and urine toxicology test ordering, home induction guides, prescription drug monitoring database, naloxone prescribing, and pharmacy order sets. Communication with specialty HCPs was facilitated by development of e-consultation within the EHR and instant messaging options within the local intranet. In the SCOUTT team model, the prescriber independently completed assessment/follow-up without nursing or clinical pharmacy support.
Analysis
We examined changes in MOUD receipt and prescriber characteristics at baseline (FY 2018 4th quarter) and 1 year after implementation (FY 2019 4th quarter). Patient data were extracted from the VHA Corporate Data Warehouse (CDW), which contains data from all VHA EHRs. The VA STORM, is a CDW tool that automatically flags patients prescribed opioids who are at risk for overdose and suicide. Prescriber data were obtained from the Buprenorphine/X-Waivered Provider Report, a VA Academic Detailing Service database that provides details on HCP type, X-waivered status, and prescribing by location. χ2 analyses were conducted on before and after measures when total values were available.
Results
There was a 4% increase in patients with an OUD diagnosis receiving MOUD, from 552 (44%) to 582 (48%) (P = .04), over this time. The number of waivered prescribers increased from 67 to 131, the number of prescribers of buprenorphine in a 6-month span increased from 35 to 52, and the percentage of HCPs capable of prescribing within the EHR increased from 75% to 89% (P =.01).
Initially, addiction HCPs prescribed to about 68% of patients on buprenorphine, with target clinic HCPs prescribing to 24% (with the remaining coming from other specialty HCPs). On follow-up, addiction professionals prescribed to 63%, with target clinic clincians prescribing to 32%.
Interpretation
SCOUTT team interventions succeeded in increasing the number of patients receiving MOUD, a substantial increase in waivered HCPs, an increase in the number of waivered HCPs prescribing MOUD, and an increase in the proportion of patients receiving MOUD in step-1 target clinics. It is important to note that within the quality-improvement framework and goals of our SCOUTT team that the data were not collected as part of a research study but to assess impact of our interventions. Within this framework, it is not possible to directly attribute the increase in eligible patients receiving MOUD solely to SCOUTT team interventions, as other factors may have contributed, including improved awareness of HCPs.
Summary and Future Directions
Since implementation of SCOUTT in August 2018, VACHS has identified several barriers to buprenorphine prescribing in step-1 clinics and implemented strategies to overcome them. Describing our approach will hopefully inform other large health care systems (VA or non-VA) on changes required in order to scale up implementation of OBOT-B. The VACHS SCOUTT team was successful at enhancing a ready workforce in step-1 clinics, though noted a delay in changing prescribing practice and culture.
We recommend utilizing academic detailing to work with clinics and individual HCPs to identify and overcome barriers to prescribing. Also, we recommend implementation of a nursing or clinical pharmacy collaborative care model in target step-1 clinics (rather than the HCP-driven model). A collaborative care model reflects the patient aligned care team (PACT) principle of team-based efficient care, and PACT nurses or clinical pharmacists should be able to provide the minimal quarterly follow-up of clinically stable patients on MOUD within the step-1 clinics. Templated notes for assessment, initiation, and follow-up of patients on MOUD are now available from the SCOUTT national program and should be broadly implemented to facilitate adoption of the collaborative model in target clinics. In order to accomplish a full collaborative model, the VHA would need to enhance appropriate staffing to support this model, broaden access to telehealth, and expand incentives to teams/clinicians who prescribe in these settings.
Acknowledgments/Funding
This material is based upon work supported by the US Department of Veterans Affairs (VA), Office of Mental Health and Suicide Prevention, Veterans Health Administration; the VA Health Services Research and Development (HSR&D) Quality Enhancement Research Initiative (QUERI) Partnered Evaluation Initiative (PEC) grants #19-001. Supporting organizations had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
1. Centers for Disease Control and Prevention. Understanding the epidemic. Updated March 17, 2021. Accessed September 17, 2021. https://www.cdc.gov/drugoverdose/epidemic/index.html
2. Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393(10182):1760-1772. doi:10.1016/S0140-6736(18)33078-2
3. Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan [published correction appears in JAMA. 2012 Jun 20;307(23):2489]. JAMA. 2012;307(9):940-947. doi:10.1001/jama.2012.234
4. Bohnert AS, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605-612. doi:10.1097/AJP.0000000000000011
5. US Department of Health and Human Services, Working Group on Patient-Centered Reduction or Discontinuation of Long-term Opioid Analgesics. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of Long-term opioid analgesics. Published October 2019. Accessed September 17, 2021. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf
6. Sullivan LE, Chawarski M, O’Connor PG, Schottenfeld RS, Fiellin DA. The practice of office-based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment?. Drug Alcohol Depend. 2005;79(1):113-116. doi:10.1016/j.drugalcdep.2004.12.008
7. LaBelle CT, Han SC, Bergeron A, Samet JH. Office-based opioid treatment with buprenorphine (OBOT-B): statewide implementation of the Massachusetts collaborative care model in community health centers. J Subst Abuse Treat. 2016;60:6-13. doi:10.1016/j.jsat.2015.06.010
8. Rubin R. Rural veterans less likely to get medication for opioid use disorder. JAMA. 2020;323(4):300. doi:10.1001/jama.2019.21856
9. Kahan M, Srivastava A, Ordean A, Cirone S. Buprenorphine: new treatment of opioid addiction in primary care. Can Fam Physician. 2011;57(3):281-289.
10. Fiellin DA, Moore BA, Sullivan LE, et al. Long-term treatment with buprenorphine/naloxone in primary care: results at 2-5 years. Am J Addict. 2008;17(2):116-120. doi:10.1080/10550490701860971
11. Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006;355(4):365-374. doi:10.1056/NEJMoa055255
12. Haddad MS, Zelenev A, Altice FL. Integrating buprenorphine maintenance therapy into federally qualified health centers: real-world substance abuse treatment outcomes. Drug Alcohol Depend. 2013;131(1-2):127-135. doi:10.1016/j.drugalcdep.2012.12.008
13. Alford DP, LaBelle CT, Richardson JM, et al. Treating homeless opioid dependent patients with buprenorphine in an office-based setting. J Gen Intern Med. 2007;22(2):171-176. doi:10.1007/s11606-006-0023-1
14. Wyse JJ, Gordon AJ, Dobscha SK, et al. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: Historical perspective, lessons learned, and next steps. Subst Abus. 2018;39(2):139-144. doi:10.1080/08897077.2018.1452327
15. Gordon AJ, Drexler K, Hawkins EJ, et al. Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative: Expanding access to medication treatment for opioid use disorder within Veterans Health Administration facilities. Subst Abus. 2020;41(3):275-282. doi:10.1080/08897077.2020.1787299
16. Codell N, Kelley AT, Jones AL, et al. Aims, development, and early results of an interdisciplinary primary care initiative to address patient vulnerabilities. Am J Drug Alcohol Abuse. 2021;47(2):160-169. doi:10.1080/00952990.2020.1832507
17. DeRonne BM, Wong KR, Schultz E, Jones E, Krebs EE. Implementation of a pharmacist care manager model to expand availability of medications for opioid use disorder. Am J Health Syst Pharm. 2021;78(4):354-359. doi:10.1093/ajhp/zxaa405
18. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
19. US Department of Defense, US Department of Veterans Affairs, Opioid Therapy for Chronic Pain Work Group. VA/DoD clinical practice guideline for opioid therapy for chronic pain. Published February 2017. Accessed August 20, 2021. https://www.va.gov/HOMELESS/nchav/resources/docs/mental-health/substance-abuse/VA_DoD-CLINICAL-PRACTICE-GUIDELINE-FOR-OPIOID-THERAPY-FOR-CHRONIC-PAIN-508.pdf
In the United States, opioid use disorder (OUD) is a major public health challenge. In 2018 drug overdose deaths were 4 times higher than they were in 1999.1 This increase highlights a critical need to expand treatment access. Medication for opioid use disorder (MOUD), including methadone, naltrexone, and buprenorphine, improves outcomes for patients retained in care.2 Compared with the general population, veterans, particularly those with co-occurring posttraumatic stress disorder (PTSD) or depression, are more likely to receive higher dosages of opioid medications and experience opioid-related adverse outcomes (eg, overdose, OUD).3,4 As a risk reduction strategy, patients receiving potentially dangerous full-dose agonist opioid medication who are unable to taper to safer dosages may be eligible to transition to buprenorphine.5
Buprenorphine and naltrexone can be prescribed in office-based settings or in addiction, primary care, mental health, and pain clinics. Office-based opioid treatment with buprenorphine (OBOT-B) expands access to patients who are not reached by addiction treatment programs.6,7 This is particularly true in rural settings, where addiction care services are typically scarce.8 OBOT-B prevents relapse and maintains opioid-free days and may increase patient engagement by reducing stigma and providing treatment within an existing clinical care team.9 For many patients, OBOT-B results in good retention with just medical monitoring and minimal or no ancillary addiction counseling.10,11
Successful implementation of OBOT-B has occurred through a variety of care models in selected community health care settings.8,12,13 Historically in the Veterans Health Administration (VHA), MOUD has been prescribed in substance use disorder clinics by mental health practitioners. Currently, more than 44% of veterans with OUD are on MOUD.14
The VHA has invested significant resources to improve access to MOUD. In 2018, the Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative launched, with the aim to improve access within primary care, mental health, and pain clinics.15 SCOUTT emphasizes stepped-care treatment, with patients engaging in the step of care most appropriate to their needs. Step 0 is self-directed care/self-management, including mutual support groups; step-1 environments include office-based primary care, mental health, and pain clinics; and step-2 environments are specialty care settings. Through a series of remote webinars, an in-person national 2-day conference, and external facilitation, SCOUTT engaged 18 teams representing each Veterans Integrated Service Network (VISN) across the country to assist in implementing MOUD within 2 step-1 clinics. These teams have developed several models of providing step-1 care, including an interdisciplinary team-based primary care delivery model as well as a pharmacist care manager model.16, 17
US Department of Veterans Affairs (VA) Connecticut Health Care System (VACHS), which delivers care to approximately 58,000 veterans, was chosen to be a phase 1 SCOUTT site. Though all patients in VACHS have access to specialty care step-2 clinics, including methadone and buprenorphine programs, there remained many patients not yet on MOUD who could benefit from it. Baseline data (fiscal year [FY] 2018 4th quarter), obtained through electronic health record (EHR) database dashboards indicated that 710 (56%) patients with an OUD diagnosis were not receiving MOUD. International Classification of Disease, 10th Revision codes are the foundation for VA population management dashboards, and based their data on codes for opioid abuse and opioid dependence. These tools are limited by the accuracy of coding in EHRs. Additionally, 366 patients receiving long-term opioid prescriptions were identified as moderate, high, or very high risk for overdose or death based on an algorithm that considered prescribed medications, sociodemographics, and comorbid conditions, as characterized in the VA EHR (Stratification Tool for Opioid Risk Mitigation [STORM] report).18
This article describes the VACHSquality-improvement effort to extend OBOT-B into step-1 primary care and general mental health clinics. Our objectives are to (1) outline the process for initiating SCOUTT within VACHS; (2) examine barriers to implementation and the SCOUTT team response; (3) review VACHS patient and prescriber data at baseline and 1 year after implementation; and (4) explore future implementation strategies.
SCOUTT Team
A VACHS interdisciplinary team was formed and attended the national SCOUTT kickoff conference in 2018.15 Similar to other SCOUTT teams, the team consisted of VISN leadership (in primary care, mental health, and addiction care), pharmacists, and a team of health care practitioners (HCPs) from step-2 clinics (including 2 addiction psychiatrists, and an advanced practice registered nurse, a registered nurse specializing in addiction care), and a team of HCPs from prospective step-1 clinics (including a clinical psychologist and 2 primary care physicians). An external facilitator was provided from outside the VISN who met remotely with the team to assist in facilitation. Our team met monthly, with the goal to identify local barriers and facilitators to OBOT-B and implement interventions to enhance prescribing in step-1 primary care and general mental health clinics.
Implementation Steps
The team identified multiple barriers to dissemination of OBOT-B in target clinics (Table). The 3 main barriers were limited leadership engagement in promoting OBOT-B in target clinics, inadequate number of HCPs with active X-waivered prescribing status in the targeted clinics, and the need for standardized processes and tools to facilitate prescribing and follow-up.
To address leadership engagement, the SCOUTT team held quarterly presentations of SCOUTT goals and progress on target clinic leadership calls (usually 15 minutes) and arranged a 90-minute multidisciplinary leadership summit with key leadership representation from primary care, general mental health, specialty addiction care, nursing, and pharmacy. To enhance X-waivered prescribers in target clinics, the SCOUTT team sent quarterly emails with brief education points on MOUD and links to waiver trainings. At the time of implementation, in order to prescribe buprenorphine and meet qualifications to treat OUD, prescribers were required to complete specialized training as necessitated by the Drug Addiction Treatment Act of 2000. X-waivered status can now be obtained without requiring training
The SCOUTT team advocated for X-waivered status to be incentivized by performance pay for primary care practitioners and held quarterly case-based education sessions during preexisting allotted time. The onboarding process for new waivered prescribers to navigate from waiver training to active prescribing within the EHR was standardized via development of a standard operating procedure (SOP).
The SCOUTT team also assisted in the development of standardized processes and tools for prescribing in target clinics, including implementation of a standard operating procedure regarding prescribing (both initiation of buprenorphine, and maintenance) in target clinics. This procedure specifies that target clinic HCPs prescribe for patients requiring less intensive management, and who are appropriate for office-based treatment based on specific criteria (eAppendix
Templated progress notes were created for buprenorphine initiation and buprenorphine maintenance with links to recommended laboratory tests and urine toxicology test ordering, home induction guides, prescription drug monitoring database, naloxone prescribing, and pharmacy order sets. Communication with specialty HCPs was facilitated by development of e-consultation within the EHR and instant messaging options within the local intranet. In the SCOUTT team model, the prescriber independently completed assessment/follow-up without nursing or clinical pharmacy support.
Analysis
We examined changes in MOUD receipt and prescriber characteristics at baseline (FY 2018 4th quarter) and 1 year after implementation (FY 2019 4th quarter). Patient data were extracted from the VHA Corporate Data Warehouse (CDW), which contains data from all VHA EHRs. The VA STORM, is a CDW tool that automatically flags patients prescribed opioids who are at risk for overdose and suicide. Prescriber data were obtained from the Buprenorphine/X-Waivered Provider Report, a VA Academic Detailing Service database that provides details on HCP type, X-waivered status, and prescribing by location. χ2 analyses were conducted on before and after measures when total values were available.
Results
There was a 4% increase in patients with an OUD diagnosis receiving MOUD, from 552 (44%) to 582 (48%) (P = .04), over this time. The number of waivered prescribers increased from 67 to 131, the number of prescribers of buprenorphine in a 6-month span increased from 35 to 52, and the percentage of HCPs capable of prescribing within the EHR increased from 75% to 89% (P =.01).
Initially, addiction HCPs prescribed to about 68% of patients on buprenorphine, with target clinic HCPs prescribing to 24% (with the remaining coming from other specialty HCPs). On follow-up, addiction professionals prescribed to 63%, with target clinic clincians prescribing to 32%.
Interpretation
SCOUTT team interventions succeeded in increasing the number of patients receiving MOUD, a substantial increase in waivered HCPs, an increase in the number of waivered HCPs prescribing MOUD, and an increase in the proportion of patients receiving MOUD in step-1 target clinics. It is important to note that within the quality-improvement framework and goals of our SCOUTT team that the data were not collected as part of a research study but to assess impact of our interventions. Within this framework, it is not possible to directly attribute the increase in eligible patients receiving MOUD solely to SCOUTT team interventions, as other factors may have contributed, including improved awareness of HCPs.
Summary and Future Directions
Since implementation of SCOUTT in August 2018, VACHS has identified several barriers to buprenorphine prescribing in step-1 clinics and implemented strategies to overcome them. Describing our approach will hopefully inform other large health care systems (VA or non-VA) on changes required in order to scale up implementation of OBOT-B. The VACHS SCOUTT team was successful at enhancing a ready workforce in step-1 clinics, though noted a delay in changing prescribing practice and culture.
We recommend utilizing academic detailing to work with clinics and individual HCPs to identify and overcome barriers to prescribing. Also, we recommend implementation of a nursing or clinical pharmacy collaborative care model in target step-1 clinics (rather than the HCP-driven model). A collaborative care model reflects the patient aligned care team (PACT) principle of team-based efficient care, and PACT nurses or clinical pharmacists should be able to provide the minimal quarterly follow-up of clinically stable patients on MOUD within the step-1 clinics. Templated notes for assessment, initiation, and follow-up of patients on MOUD are now available from the SCOUTT national program and should be broadly implemented to facilitate adoption of the collaborative model in target clinics. In order to accomplish a full collaborative model, the VHA would need to enhance appropriate staffing to support this model, broaden access to telehealth, and expand incentives to teams/clinicians who prescribe in these settings.
Acknowledgments/Funding
This material is based upon work supported by the US Department of Veterans Affairs (VA), Office of Mental Health and Suicide Prevention, Veterans Health Administration; the VA Health Services Research and Development (HSR&D) Quality Enhancement Research Initiative (QUERI) Partnered Evaluation Initiative (PEC) grants #19-001. Supporting organizations had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
In the United States, opioid use disorder (OUD) is a major public health challenge. In 2018 drug overdose deaths were 4 times higher than they were in 1999.1 This increase highlights a critical need to expand treatment access. Medication for opioid use disorder (MOUD), including methadone, naltrexone, and buprenorphine, improves outcomes for patients retained in care.2 Compared with the general population, veterans, particularly those with co-occurring posttraumatic stress disorder (PTSD) or depression, are more likely to receive higher dosages of opioid medications and experience opioid-related adverse outcomes (eg, overdose, OUD).3,4 As a risk reduction strategy, patients receiving potentially dangerous full-dose agonist opioid medication who are unable to taper to safer dosages may be eligible to transition to buprenorphine.5
Buprenorphine and naltrexone can be prescribed in office-based settings or in addiction, primary care, mental health, and pain clinics. Office-based opioid treatment with buprenorphine (OBOT-B) expands access to patients who are not reached by addiction treatment programs.6,7 This is particularly true in rural settings, where addiction care services are typically scarce.8 OBOT-B prevents relapse and maintains opioid-free days and may increase patient engagement by reducing stigma and providing treatment within an existing clinical care team.9 For many patients, OBOT-B results in good retention with just medical monitoring and minimal or no ancillary addiction counseling.10,11
Successful implementation of OBOT-B has occurred through a variety of care models in selected community health care settings.8,12,13 Historically in the Veterans Health Administration (VHA), MOUD has been prescribed in substance use disorder clinics by mental health practitioners. Currently, more than 44% of veterans with OUD are on MOUD.14
The VHA has invested significant resources to improve access to MOUD. In 2018, the Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative launched, with the aim to improve access within primary care, mental health, and pain clinics.15 SCOUTT emphasizes stepped-care treatment, with patients engaging in the step of care most appropriate to their needs. Step 0 is self-directed care/self-management, including mutual support groups; step-1 environments include office-based primary care, mental health, and pain clinics; and step-2 environments are specialty care settings. Through a series of remote webinars, an in-person national 2-day conference, and external facilitation, SCOUTT engaged 18 teams representing each Veterans Integrated Service Network (VISN) across the country to assist in implementing MOUD within 2 step-1 clinics. These teams have developed several models of providing step-1 care, including an interdisciplinary team-based primary care delivery model as well as a pharmacist care manager model.16, 17
US Department of Veterans Affairs (VA) Connecticut Health Care System (VACHS), which delivers care to approximately 58,000 veterans, was chosen to be a phase 1 SCOUTT site. Though all patients in VACHS have access to specialty care step-2 clinics, including methadone and buprenorphine programs, there remained many patients not yet on MOUD who could benefit from it. Baseline data (fiscal year [FY] 2018 4th quarter), obtained through electronic health record (EHR) database dashboards indicated that 710 (56%) patients with an OUD diagnosis were not receiving MOUD. International Classification of Disease, 10th Revision codes are the foundation for VA population management dashboards, and based their data on codes for opioid abuse and opioid dependence. These tools are limited by the accuracy of coding in EHRs. Additionally, 366 patients receiving long-term opioid prescriptions were identified as moderate, high, or very high risk for overdose or death based on an algorithm that considered prescribed medications, sociodemographics, and comorbid conditions, as characterized in the VA EHR (Stratification Tool for Opioid Risk Mitigation [STORM] report).18
This article describes the VACHSquality-improvement effort to extend OBOT-B into step-1 primary care and general mental health clinics. Our objectives are to (1) outline the process for initiating SCOUTT within VACHS; (2) examine barriers to implementation and the SCOUTT team response; (3) review VACHS patient and prescriber data at baseline and 1 year after implementation; and (4) explore future implementation strategies.
SCOUTT Team
A VACHS interdisciplinary team was formed and attended the national SCOUTT kickoff conference in 2018.15 Similar to other SCOUTT teams, the team consisted of VISN leadership (in primary care, mental health, and addiction care), pharmacists, and a team of health care practitioners (HCPs) from step-2 clinics (including 2 addiction psychiatrists, and an advanced practice registered nurse, a registered nurse specializing in addiction care), and a team of HCPs from prospective step-1 clinics (including a clinical psychologist and 2 primary care physicians). An external facilitator was provided from outside the VISN who met remotely with the team to assist in facilitation. Our team met monthly, with the goal to identify local barriers and facilitators to OBOT-B and implement interventions to enhance prescribing in step-1 primary care and general mental health clinics.
Implementation Steps
The team identified multiple barriers to dissemination of OBOT-B in target clinics (Table). The 3 main barriers were limited leadership engagement in promoting OBOT-B in target clinics, inadequate number of HCPs with active X-waivered prescribing status in the targeted clinics, and the need for standardized processes and tools to facilitate prescribing and follow-up.
To address leadership engagement, the SCOUTT team held quarterly presentations of SCOUTT goals and progress on target clinic leadership calls (usually 15 minutes) and arranged a 90-minute multidisciplinary leadership summit with key leadership representation from primary care, general mental health, specialty addiction care, nursing, and pharmacy. To enhance X-waivered prescribers in target clinics, the SCOUTT team sent quarterly emails with brief education points on MOUD and links to waiver trainings. At the time of implementation, in order to prescribe buprenorphine and meet qualifications to treat OUD, prescribers were required to complete specialized training as necessitated by the Drug Addiction Treatment Act of 2000. X-waivered status can now be obtained without requiring training
The SCOUTT team advocated for X-waivered status to be incentivized by performance pay for primary care practitioners and held quarterly case-based education sessions during preexisting allotted time. The onboarding process for new waivered prescribers to navigate from waiver training to active prescribing within the EHR was standardized via development of a standard operating procedure (SOP).
The SCOUTT team also assisted in the development of standardized processes and tools for prescribing in target clinics, including implementation of a standard operating procedure regarding prescribing (both initiation of buprenorphine, and maintenance) in target clinics. This procedure specifies that target clinic HCPs prescribe for patients requiring less intensive management, and who are appropriate for office-based treatment based on specific criteria (eAppendix
Templated progress notes were created for buprenorphine initiation and buprenorphine maintenance with links to recommended laboratory tests and urine toxicology test ordering, home induction guides, prescription drug monitoring database, naloxone prescribing, and pharmacy order sets. Communication with specialty HCPs was facilitated by development of e-consultation within the EHR and instant messaging options within the local intranet. In the SCOUTT team model, the prescriber independently completed assessment/follow-up without nursing or clinical pharmacy support.
Analysis
We examined changes in MOUD receipt and prescriber characteristics at baseline (FY 2018 4th quarter) and 1 year after implementation (FY 2019 4th quarter). Patient data were extracted from the VHA Corporate Data Warehouse (CDW), which contains data from all VHA EHRs. The VA STORM, is a CDW tool that automatically flags patients prescribed opioids who are at risk for overdose and suicide. Prescriber data were obtained from the Buprenorphine/X-Waivered Provider Report, a VA Academic Detailing Service database that provides details on HCP type, X-waivered status, and prescribing by location. χ2 analyses were conducted on before and after measures when total values were available.
Results
There was a 4% increase in patients with an OUD diagnosis receiving MOUD, from 552 (44%) to 582 (48%) (P = .04), over this time. The number of waivered prescribers increased from 67 to 131, the number of prescribers of buprenorphine in a 6-month span increased from 35 to 52, and the percentage of HCPs capable of prescribing within the EHR increased from 75% to 89% (P =.01).
Initially, addiction HCPs prescribed to about 68% of patients on buprenorphine, with target clinic HCPs prescribing to 24% (with the remaining coming from other specialty HCPs). On follow-up, addiction professionals prescribed to 63%, with target clinic clincians prescribing to 32%.
Interpretation
SCOUTT team interventions succeeded in increasing the number of patients receiving MOUD, a substantial increase in waivered HCPs, an increase in the number of waivered HCPs prescribing MOUD, and an increase in the proportion of patients receiving MOUD in step-1 target clinics. It is important to note that within the quality-improvement framework and goals of our SCOUTT team that the data were not collected as part of a research study but to assess impact of our interventions. Within this framework, it is not possible to directly attribute the increase in eligible patients receiving MOUD solely to SCOUTT team interventions, as other factors may have contributed, including improved awareness of HCPs.
Summary and Future Directions
Since implementation of SCOUTT in August 2018, VACHS has identified several barriers to buprenorphine prescribing in step-1 clinics and implemented strategies to overcome them. Describing our approach will hopefully inform other large health care systems (VA or non-VA) on changes required in order to scale up implementation of OBOT-B. The VACHS SCOUTT team was successful at enhancing a ready workforce in step-1 clinics, though noted a delay in changing prescribing practice and culture.
We recommend utilizing academic detailing to work with clinics and individual HCPs to identify and overcome barriers to prescribing. Also, we recommend implementation of a nursing or clinical pharmacy collaborative care model in target step-1 clinics (rather than the HCP-driven model). A collaborative care model reflects the patient aligned care team (PACT) principle of team-based efficient care, and PACT nurses or clinical pharmacists should be able to provide the minimal quarterly follow-up of clinically stable patients on MOUD within the step-1 clinics. Templated notes for assessment, initiation, and follow-up of patients on MOUD are now available from the SCOUTT national program and should be broadly implemented to facilitate adoption of the collaborative model in target clinics. In order to accomplish a full collaborative model, the VHA would need to enhance appropriate staffing to support this model, broaden access to telehealth, and expand incentives to teams/clinicians who prescribe in these settings.
Acknowledgments/Funding
This material is based upon work supported by the US Department of Veterans Affairs (VA), Office of Mental Health and Suicide Prevention, Veterans Health Administration; the VA Health Services Research and Development (HSR&D) Quality Enhancement Research Initiative (QUERI) Partnered Evaluation Initiative (PEC) grants #19-001. Supporting organizations had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
1. Centers for Disease Control and Prevention. Understanding the epidemic. Updated March 17, 2021. Accessed September 17, 2021. https://www.cdc.gov/drugoverdose/epidemic/index.html
2. Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393(10182):1760-1772. doi:10.1016/S0140-6736(18)33078-2
3. Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan [published correction appears in JAMA. 2012 Jun 20;307(23):2489]. JAMA. 2012;307(9):940-947. doi:10.1001/jama.2012.234
4. Bohnert AS, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605-612. doi:10.1097/AJP.0000000000000011
5. US Department of Health and Human Services, Working Group on Patient-Centered Reduction or Discontinuation of Long-term Opioid Analgesics. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of Long-term opioid analgesics. Published October 2019. Accessed September 17, 2021. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf
6. Sullivan LE, Chawarski M, O’Connor PG, Schottenfeld RS, Fiellin DA. The practice of office-based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment?. Drug Alcohol Depend. 2005;79(1):113-116. doi:10.1016/j.drugalcdep.2004.12.008
7. LaBelle CT, Han SC, Bergeron A, Samet JH. Office-based opioid treatment with buprenorphine (OBOT-B): statewide implementation of the Massachusetts collaborative care model in community health centers. J Subst Abuse Treat. 2016;60:6-13. doi:10.1016/j.jsat.2015.06.010
8. Rubin R. Rural veterans less likely to get medication for opioid use disorder. JAMA. 2020;323(4):300. doi:10.1001/jama.2019.21856
9. Kahan M, Srivastava A, Ordean A, Cirone S. Buprenorphine: new treatment of opioid addiction in primary care. Can Fam Physician. 2011;57(3):281-289.
10. Fiellin DA, Moore BA, Sullivan LE, et al. Long-term treatment with buprenorphine/naloxone in primary care: results at 2-5 years. Am J Addict. 2008;17(2):116-120. doi:10.1080/10550490701860971
11. Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006;355(4):365-374. doi:10.1056/NEJMoa055255
12. Haddad MS, Zelenev A, Altice FL. Integrating buprenorphine maintenance therapy into federally qualified health centers: real-world substance abuse treatment outcomes. Drug Alcohol Depend. 2013;131(1-2):127-135. doi:10.1016/j.drugalcdep.2012.12.008
13. Alford DP, LaBelle CT, Richardson JM, et al. Treating homeless opioid dependent patients with buprenorphine in an office-based setting. J Gen Intern Med. 2007;22(2):171-176. doi:10.1007/s11606-006-0023-1
14. Wyse JJ, Gordon AJ, Dobscha SK, et al. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: Historical perspective, lessons learned, and next steps. Subst Abus. 2018;39(2):139-144. doi:10.1080/08897077.2018.1452327
15. Gordon AJ, Drexler K, Hawkins EJ, et al. Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative: Expanding access to medication treatment for opioid use disorder within Veterans Health Administration facilities. Subst Abus. 2020;41(3):275-282. doi:10.1080/08897077.2020.1787299
16. Codell N, Kelley AT, Jones AL, et al. Aims, development, and early results of an interdisciplinary primary care initiative to address patient vulnerabilities. Am J Drug Alcohol Abuse. 2021;47(2):160-169. doi:10.1080/00952990.2020.1832507
17. DeRonne BM, Wong KR, Schultz E, Jones E, Krebs EE. Implementation of a pharmacist care manager model to expand availability of medications for opioid use disorder. Am J Health Syst Pharm. 2021;78(4):354-359. doi:10.1093/ajhp/zxaa405
18. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
19. US Department of Defense, US Department of Veterans Affairs, Opioid Therapy for Chronic Pain Work Group. VA/DoD clinical practice guideline for opioid therapy for chronic pain. Published February 2017. Accessed August 20, 2021. https://www.va.gov/HOMELESS/nchav/resources/docs/mental-health/substance-abuse/VA_DoD-CLINICAL-PRACTICE-GUIDELINE-FOR-OPIOID-THERAPY-FOR-CHRONIC-PAIN-508.pdf
1. Centers for Disease Control and Prevention. Understanding the epidemic. Updated March 17, 2021. Accessed September 17, 2021. https://www.cdc.gov/drugoverdose/epidemic/index.html
2. Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393(10182):1760-1772. doi:10.1016/S0140-6736(18)33078-2
3. Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan [published correction appears in JAMA. 2012 Jun 20;307(23):2489]. JAMA. 2012;307(9):940-947. doi:10.1001/jama.2012.234
4. Bohnert AS, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605-612. doi:10.1097/AJP.0000000000000011
5. US Department of Health and Human Services, Working Group on Patient-Centered Reduction or Discontinuation of Long-term Opioid Analgesics. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of Long-term opioid analgesics. Published October 2019. Accessed September 17, 2021. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf
6. Sullivan LE, Chawarski M, O’Connor PG, Schottenfeld RS, Fiellin DA. The practice of office-based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment?. Drug Alcohol Depend. 2005;79(1):113-116. doi:10.1016/j.drugalcdep.2004.12.008
7. LaBelle CT, Han SC, Bergeron A, Samet JH. Office-based opioid treatment with buprenorphine (OBOT-B): statewide implementation of the Massachusetts collaborative care model in community health centers. J Subst Abuse Treat. 2016;60:6-13. doi:10.1016/j.jsat.2015.06.010
8. Rubin R. Rural veterans less likely to get medication for opioid use disorder. JAMA. 2020;323(4):300. doi:10.1001/jama.2019.21856
9. Kahan M, Srivastava A, Ordean A, Cirone S. Buprenorphine: new treatment of opioid addiction in primary care. Can Fam Physician. 2011;57(3):281-289.
10. Fiellin DA, Moore BA, Sullivan LE, et al. Long-term treatment with buprenorphine/naloxone in primary care: results at 2-5 years. Am J Addict. 2008;17(2):116-120. doi:10.1080/10550490701860971
11. Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006;355(4):365-374. doi:10.1056/NEJMoa055255
12. Haddad MS, Zelenev A, Altice FL. Integrating buprenorphine maintenance therapy into federally qualified health centers: real-world substance abuse treatment outcomes. Drug Alcohol Depend. 2013;131(1-2):127-135. doi:10.1016/j.drugalcdep.2012.12.008
13. Alford DP, LaBelle CT, Richardson JM, et al. Treating homeless opioid dependent patients with buprenorphine in an office-based setting. J Gen Intern Med. 2007;22(2):171-176. doi:10.1007/s11606-006-0023-1
14. Wyse JJ, Gordon AJ, Dobscha SK, et al. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: Historical perspective, lessons learned, and next steps. Subst Abus. 2018;39(2):139-144. doi:10.1080/08897077.2018.1452327
15. Gordon AJ, Drexler K, Hawkins EJ, et al. Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative: Expanding access to medication treatment for opioid use disorder within Veterans Health Administration facilities. Subst Abus. 2020;41(3):275-282. doi:10.1080/08897077.2020.1787299
16. Codell N, Kelley AT, Jones AL, et al. Aims, development, and early results of an interdisciplinary primary care initiative to address patient vulnerabilities. Am J Drug Alcohol Abuse. 2021;47(2):160-169. doi:10.1080/00952990.2020.1832507
17. DeRonne BM, Wong KR, Schultz E, Jones E, Krebs EE. Implementation of a pharmacist care manager model to expand availability of medications for opioid use disorder. Am J Health Syst Pharm. 2021;78(4):354-359. doi:10.1093/ajhp/zxaa405
18. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
19. US Department of Defense, US Department of Veterans Affairs, Opioid Therapy for Chronic Pain Work Group. VA/DoD clinical practice guideline for opioid therapy for chronic pain. Published February 2017. Accessed August 20, 2021. https://www.va.gov/HOMELESS/nchav/resources/docs/mental-health/substance-abuse/VA_DoD-CLINICAL-PRACTICE-GUIDELINE-FOR-OPIOID-THERAPY-FOR-CHRONIC-PAIN-508.pdf
Access to Pain Care From Compensation Clinics: A Relational Coordination Perspective
Chronic pain is common in veterans, and early engagement in pain treatment is recommended to forestall consequences of untreated pain, including depression, disability, and substance use disorders. The Veterans Health Administration (VHA) employs a stepped care model of pain treatment, with the majority of pain care based in primary care (step 1), and an array of specialty/multimodal treatment options made available at each step in the model for patients with more complex problems, or those who do not respond to more conservative interventions.1
Recognizing the need for comprehensive pain care, the US Congress passed the Comprehensive Addiction and Recovery Act, 21 USC §1521 (2016), which included provisions for VHA facilities to offer multimodal pain treatment and to report the availability of pain care options at each step in the stepped care model.2, With the passage of the Veterans Access, Choice, and Accountability Act of 2014, 38 USC §101 (2014) and now the MISSION Act of 2018, 38 USC §703 (2018) veterans whose VHA facilities are too distant, who require care unavailable at that facility, or who have to wait too long to receive care are eligible for treatment at either VHA or non-VHA facilities.3 These laws allocate the same pool of funds to both VHA and community care and thus create an incentive to engage veterans in care within the VHA network so the funds are not spent out of network.4
An opportunity to connect veterans with VHA care arises at specialized VHA Compensation and Pension (C&P) clinics during examinations that determine whether a veteran’s health conditions were caused or exacerbated by their military service. Veterans file claims with the US Department of Veterans Affairs (VA) Veterans Benefits Administration (VBA), which sends the patient to either a VHA facility or private practitioners for these examinations. Although the number of examinations conducted each year is not available, there were 274,528 veterans newly awarded compensation in fiscal year 2018, and a substantial number of the total of 4,743,108 veterans with C&P awards had reevaluation examinations for at least 1 of their conditions during that year.5 Based largely on the compensation examination results, military service records, and medical records, veterans are granted a service-connected rating for conditions deemed related to military service. A service-connection rating between 0% and 100% is assigned by the VBA, with higher ratings indicating more impairment and, consequently, more financial compensation. Service-connection ratings also are used to decide which veterans are in the highest priority groups for receipt of VHA health care services and are exempt from copayments.
Although traditionally thought of as a forensic evaluation with no clinical purpose, the C&P examination process affords many opportunities to explain VHA care to veterans in distress who file claims.6 A randomized clinical trials (RCT) involving veterans with mental health claims and a second RCT including veterans with musculoskeletal claims each found that veterans use more VHA services if offered outreach at the time of the C&P examination.7,8 In addition to clinical benefits, outreach around the time of C&P examinations also might mitigate the well documented adversarial aspects of the service-connection claims process.6,9,10 Currently, such outreach is not part of routine VHA procedures. Ironically, it is the VBA and not VHA that contacts veterans who are awarded service-connection with information about their eligibility for VHA care based on their award.
Connecting veterans to pain treatment can involve clarifying eligibility for VHA care for veterans in whom eligibility is unknown, involving primary care providers (PCPs) who are the fulcrum of VHA pain care referrals, and motivating veterans to seek specific pain treatment modalities. Connecting veterans to treatment at the time of their compensation examinations also likely involves bidirectional cooperation between the specialized C&P clinics where veterans are examined and the clinics that provide treatment.
Relational coordination is a theoretical framework that can describe the horizontal relationships between different teams within the same medical facility. Relational coordination theorizes that communication between workgroups is related synergistically to the quality of relationships between workgroups. Relational coordination is better between workgroups that share goals and often have high levels of relational coordination, which is thought to be especially important when activities are ambiguous, require cooperation, and are conducted under time pressure.11 High relational coordination also has been associated with high staff job satisfaction, high satisfaction with delivered services, and adherence to treatment guidelines.12-14 An observational cohort study suggested that relational coordination can be improved by targeted interventions that bring workgroups together and facilitate intercommunication.15
To better understand referral and engagement for pain treatment at compensation examinations, VA staff from primary care, mental health, pain management, and C&P teams at the 8 VHA medical centers in New England were invited to complete a validated relational coordination survey.11,16 A subset of invited staff participated in a semistructured interview about pain treatment referral practices within their medical centers.
Assessments were conducted as part of a mixed methods formative evaluation involving quantitative and qualitative methods for a clinical trial at the 8 VHA medical centers in New England. The trial is testing an intervention in which veterans presenting for service-connection examinations for musculoskeletal conditions receive brief counseling to engage them in nonopioid pain treatments. The VHA Central Institutional Review Board approved this formative evaluation and the clinical trial has begun (ClinicalTrials.gov NCT04062214).
Potential interviewees were involved in referrals to and provision of nonpharmacologic pain treatment and were identified by site investigators in the randomized trial. Identified interviewees were clinical and administrative staff belonging to VHA Primary Care, Pain Management, and Compensation and Pension clinics. A total of 83 staff were identified.
Semistructured Interviews
A subset of the 83 staff were invited to participate in a semistructured interview because their position impacted coordination of pain care at their facilities or they worked in C&P. Staff at a site were interviewed until no new themes emerged from additional interviews, and each of the 8 sites was represented. Interviews were conducted between June and August 2018. Standardized scripts describing the study and inviting participation in a semistructured interview were e-mailed to VA staff. At the time of the interview the study purpose was restated and consent for audiotaping was obtained. The interviews followed a guide designed to assess a relational coordination framework among various workgroups. The data in this manuscript were elicited by specific prompts concerning: (1) How veterans learn about pain care when they come through C&P; and (2) How staff in C&P communicate with treatment providers about veterans who have chronic pain. Each interview lasted about 30 minutes.
Relational Coordination Survey
All identified staff were invited to participate in a relational coordination survey. The survey was administered through VA REDCap. Survey invitations were e-mailed from REDCap to VA staff and included a description of the study and assurances of the confidentiality of data collected. Surveys took < 10 minutes to complete. To begin, respondents identified their primary workgroup (C&P, primary care, pain management, or administrative leadership or staff), secondary workgroup (if they were in > 1), and site. Respondents provided no other identifying information and were assured their responses would be confidential.
The survey consisted of 7 questions regarding beliefs about the quality of communication and interactions among workgroup members in obtaining a shared goal.11 The shared goal in the survey used in this study was providing pain care services for veterans with musculoskeletal conditions. Using a 5-point Likert scale, the 7 questions concerned frequency, timeliness, and accuracy of communication; response to problems providing pain services; sharing goals; and knowledge and respect for respondent’s job function. Higher scores indicated better relational coordination among members of a workgroup. Using the survey’s 7 items, composite mean relational coordination scores were calculated for each of the 4 primary workgroups. To account for the possibility that a member rated their own workgroups, 2 scores were created for each workgroup; one included members of the workgroup and another excluded them.
Data Analysis
The audio-recorded semistructured interviews were transcribed and entered into Atlas.ti qualitative data analysis software. To identify cross-cutting themes, a semistructured telephone interview guide was developed by the qualitative study team that emphasized interrelationships between different clinical teams. The transcripts were then analyzed using the grounded theory approach, a systematic methodology to reduce themes from collected qualitative data. Two research staff read each transcript twice; first to familiarize themselves with the text and then, using open coding, to identify important concepts that emerged from the language and assign codes to segments of text. To ensure accuracy, researchers included suitable contextual information in the coding. Using the constant comparative method, research staff then met to examine the themes that emerged in the interviews, discuss and coalesce coding discrepancies, and compare perspectives.17
The composite score (mean of the 7 items and 95% CI) of the survey responses was analyzed to identify significant differences in coordination across the 4 workgroups. Analysis of variance (ANOVA) was used to examine each relational coordination score by respondents’ workgroup. Post hoc analyses examined relational coordination survey differences among the 4 respondent groups.
Results
Thirty-nine survey respondents participated in the semistructured interviews. C&P examiners expressed varying degrees of comfort with their role in extending access to pain care for veterans. Some of the examiners strongly believed that their role was purely forensic, and going beyond this forensic role to refer or recommend treatment to veterans would be a violation of their role to conduct a forensic examination. “We don’t have an ongoing therapeutic relationship with any of the patients,” a C&P examiner explained: “We see them once; they’re out the door. It’s forensic. We’re investigating the person as a claimant, we’re investigating it and using our tools to go and review information from 30, 40 years ago.”
Other examiners had a less strict approach for working with veterans in C&P, even though examiners are asked not to provide advice or therapy. One C&P examiner noted that because he “can’t watch people in pain,” during the examination this doctor recommends that patients go to the office that determines whether they are eligible for benefits and choose a PCP. Another C&P examiner concurred with this approach. “I certainly spend a little time with the veteran talking to them about their personal life, who they are, what they do, what they’ve done, what they’re going to do to kind of break the ice between us,” the second examiner explained. “At the end, I will make some suggestions to them. I’m comfortable doing that. I don’t know that everybody is.”
Many of the VHA providers we interviewed had little knowledge of the C&P process or whether C&P examiners had any role or responsibilities in referring veterans for pain care. Most VHA providers could not name any C&P examiners at their facility and were generally unfamiliar with the content of C&P examinations. One provider bluntly said, “I’ve never communicated with anyone in comp and pen [C&P].”
Another PCP also expressed concerns with referrals, suggesting that C&P and primary care “are totally separate and should remain separate,” the PCP explained. “My concern with getting referral from comp and pen is that is it then they’re seeking all sorts of treatment that they wouldn’t necessarily need or ask for otherwise.”
Conversely a different PCP had a positive outlook on how C&P examiners might help ease the transition into the VHA for veterans with pain, especially for newly discharged veterans. “Having comp and pen address these issues is really going to be helpful. I think it could be significant that the topic is introduced early on.”
Relational Coordination Survey
Relational coordination surveys were sent to 83 participants of whom 66 responded. Respondents were from
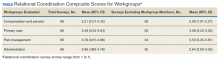
The relational coordination composite scores were lowest for C&P. This finding remained whether C&P staff surveys were included or removed from the C&P responses. As demonstrated by the 95% CI, when team members’ surveys were included, C&P scores (95% CI, 2.01-2.42) were significantly lower than the primary care (95% CI, 3.34-3.64) and pain management (95% CI, 3.61-3.96) groups. All the relational coordination composite scores were slightly lower when staff who described their own workgroup were removed (ie, respondents rated their own workgroups as having higher relational coordination than others did). Using the composite scores excluding same workgroup members, the composite scores of the C&P remained significantly lower than all 3 other workgroups (Table). Means values for each individual item in the C&P group were significantly less than all other group means for each item except for the question on responses to problems providing pain services (data not shown). On this item only, the mean C&P rating was > 3 (3.19), but this was still lower than the means of the primary care and pain management workgroups.
Further analyses were undertaken to understand the importance of stakeholders’ ratings of their own workgroup compared with ratings by others of that workgroup. A 1-way ANOVA of workgroup was conducted and displayed significant workgroup differences between member and nonmember relational coordination ratings on 3 of the 4 workgroup’s scores C&P (F = 5.75, 3, 62 df; P < .01) primary care (F = 4.30, 3, 62 df; P < .008) and pain management (F = 8.22, 3, 62 df; P < .001). Post hoc contrasts between the different workgroups doing the rating revealed: (1) significant differences in the assessment of the C&P workgroup between the C&P workgroup and both the primary care (P < .01) and pain management groups (P < .001) with C&P rating their own workgroup significantly higher; (2) a significant difference in the scoring of the primary care workgroup with the primary care group rating themselves significantly higher than the C&P group; and (3) significant differences in the scoring of the pain management workgroup with both pain management and primary care groups rating the pain management group significantly higher than the C&P group. The results were not substantially changed by removing the 18 respondents who identified themselves as being part of > 1 workgroup .
Discussion
Mixed methods revealed disparate viewpoints about the role of C&P in referring veterans to pain care services. Overall, C&P teams coordinated less with other workgroups than the other groups coordinated with each other, and the C&P clinics took only limited steps to engage veterans in VHA treatment. The relational coordination results appeared to be valid. The mean scores were near the middle of the relational coordination rating scale, with standard deviations indicating a range of responses. The lower relational coordination scores of the C&P group remained after removing stakeholders who were rating their own workgroup. Further support for the validity of the relational coordination survey results is that they were consistent with the reports of C&P clinic isolation in the semistructured interviews.
The interview data suggest that one reason the C&P teams had low relational coordination scores is that VA staff interpret the emphasis on evaluative rather than therapeutic examinations to preclude other attempts to engage veterans into VHA treatment, even though such treatment engagement is permitted within existing guidelines. VBA referrals for examinations say nothing, either way, about engaging veterans in VHA care. The relational coordination results suggest that an intervention that might increase treatment referrals from the C&P clinics would be to explain the (existing) policy allowing for outreach around the time of compensation examinations to VHA staff so this goal is clearly agreed-upon. Another approach to facilitating treatment engagement at the C&P examination is to use other interventions that have been associated with better relational coordination such as intergroup meetings, horizontal integration more generally, and an atmosphere is which people from different backgrounds feel empowered to speak frankly to each other.15,18,19 An important linkage to forge is between C&P teams and the administrative workgroups responsible for verifying a veteran’s eligibility for VHA care and enrolling eligible veterans in VHA treatment. Having C&P clinicians who are familiar with the eligibility and treatment engagement processes would facilitate providing that information to veterans, without compromising the evaluative format of the compensation examination.
An interesting ancillary finding is that relational coordination ratings by members of 3 of the 4 workgroups were higher than ratings by other staff of that workgroup. A possible explanation for this finding is that workgroup members are more aware of the relational coordination efforts made by their own workgroup than those by other workgroups, and therefore rate their own workgroup higher. This also might be part of a broader self-aggrandizement heuristic that has been described in multiple domains.20 Staff may apply this heuristic in reporting that their staff engage in more relational coordination, reflecting the social desirability of being cooperative.
There are simple facility-level interventions that would facilitate veterans access to care such as conducting C&P examinations for potentially treatment-eligible veterans at VHA facilities (vs conducted outside VHA) and having access to materials that explain the treatment options to veterans when they check in for their compensation examinations. The approach to C&P-based treatment engagement that was successfully employed in 2 clinical trials involved having counselors not connected with the C&P clinic contact veterans around the time of their compensation examination to explain VA treatment options and motivate veterans to pursue treatment.8,9 This independent counselor approach is being evaluated in a larger study.
Limitations
These data are from a small number of VA staff evaluating veterans in a single region of the US. They do not show causation, and it is possible that relational coordination is not necessary for referrals from C&P clinics. Relational coordination might not be necessary when referral processes can be simply routinized with little need for communication.11 However, other analyses in these clinics have found that pain treatment referrals in fact are not routinized, with substantial variability within and across institutions. Another possibility is that features that have been associated with less relational coordination, such as male gender and medical specialist guild, were disproportionately present in C&P clinics compared to the other clinics.21
Conclusions
There have been public calls to improve the evaluation of service-connection claims such that this process includes approaches to engage veterans in treatment.22 Referring veterans to treatment when they come for C&P examinations will likely involve improving relational coordination between the C&P service and other parts of VHA. Nationwide, sites that integrate C&P more fully may have valuable lessons to impart about the benefits of such integration. An important step towards better relational coordination will be clarifying that engaging veterans in VHA care around the time of their C&P examinations is a facility-wide goal.
Acknowledgments
The authors thank Brian Linde and Efia James for their perspectives on C&P procedures. This work was supported by the Veterans Integrated Service Network 1 Mental Illness Research Education and Clinical Center (MIRECC) and National Institute of Health, National Center for Complementary and Integrative Health Project # 5UG3AT009758-02. (MIR, SM mPIs).
1. US Department Veterans Affairs, Veterans Health Administration. VHA Directive 2009-053: pain management. https://www.va.gov/painmanagement/docs/vha09paindirective.pdf. Published October 28, 2019. Accessed June 18, 2020.
2. Rosenberger PH, Phillip EJ, Lee A, Kerns RD. The VHA’s national pain management strategy: implementing the stepped care model. Fed Pract. 2011;28(8):39-42.
3. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: A Qualitative Examination of Rapid Policy Implementation in the Department of Veterans Affairs. Med Care. 2017;55 Suppl 7 Suppl 1:S71-S75. doi:10.1097/MLR.0000000000000667
4. Rieselbach RE, Epperly T, Nycz G, Shin P. Community health centers could provide better outsourced primary care for veterans. J Gen Intern Med. 2019;34(1):150-153. doi:10.1007/s11606-018-4691-4
5. US Department of Veterans Affairs, Veterans Benefit Administration. VBA annual benefits report fiscal year 2018. https://www.benefits.va.gov/REPORTS/abr/docs/2018-abr.pdf. Updated March 29, 2019. Accessed June 17, 2020.
6. Rosen MI. Compensation examinations for PTSD-an opportunity for treatment? J Rehabil Res Dev. 2010;47(5):xv-xxii. doi:10.1682/jrrd.2010.04.0075
7. Rosen MI, Ablondi K, Black AC, et al. Work outcomes after benefits counseling among veterans applying for service connection for a psychiatric condition. Psychiatr Serv. 2014;65(12):1426-1432. doi:10.1176/appi.ps.201300478
8. Rosen MI, Becker WC, Black AC, Martino S, Edens EL, Kerns RD. Brief counseling for veterans with musculoskeletal disorder, risky substance use, and service connection claims. Pain Med. 2019;20(3):528-542. doi:10.1093/pm/pny071
9. Meshberg-Cohen S, DeViva JC, Rosen MI. Counseling veterans applying for service connection status for mental health conditions. Psychiatr Serv. 2017;68(4):396-399. doi:10.1176/appi.ps.201500533
10. Sayer NA, Spoont M, Nelson DB. Post-traumatic stress disorder claims from the viewpoint of veterans service officers. Mil Med. 2005;170(10):867-870. doi:10.7205/milmed.170.10.867
11. Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manage Sci. 2002;48(11):1408-1426. doi: 10.1287/mnsc.48.11.1408.268
12. Havens DS, Gittell JH, Vasey J. Impact of relational coordination on nurse job satisfaction, work engagement and burnout: achieving the quadruple aim. J Nurs Adm. 2018;48(3):132-140. doi:10.1097/NNA.0000000000000587
13. Gittell JH, Logan C, Cronenwett J, et al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Manage Rev. 2020;45(1):12-20. doi:10.1097/HMR.0000000000000192
14. Cramm JM, Nieboer AP. Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Health Care Manage Rev. 2012;37(4):301-309. doi:10.1097/HMR.0b013e3182355ea4
15. Abu-Rish Blakeney E, Lavallee DC, Baik D, Pambianco S, O’Brien KD, Zierler BK. Purposeful interprofessional team intervention improves relational coordination among advanced heart failure care teams. J Interprof Care. 2019;33(5):481-489. doi:10.1080/13561820.2018.1560248
16. Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16-e30. doi:10.1097/MLR.0b013e31827feef6
17. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL. Transaction Publishers; 2009.
18. Gittell JH. How interdependent parties build relational coordination to achieve their desired outcomes. Negot J. 2015;31(4):387-391. doi: 10.1111/nejo.12114
19. Solberg MT, Hansen TW, Bjørk IT. The need for predictability in coordination of ventilator treatment of newborn infants--a qualitative study. Intensive Crit Care Nurs. 2015;31(4):205-212. doi:10.1016/j.iccn.2014.12.003
20. Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull. 1988;103(2):193-210.
21. Hartgerink JM, Cramm JM, Bakker TJ, van Eijsden AM, Mackenbach JP, Nieboer AP. The importance of multidisciplinary teamwork and team climate for relational coordination among teams delivering care to older patients. J Adv Nurs. 2014;70(4):791-799. doi:10.1111/jan.12233
22. Bilmes L. soldiers returning from iraq and afghanistan: the long-term costs of providing veterans medical care and disability benefits RWP07-001. https://research.hks.harvard.edu/publications/getFile.aspx?Id=237. Published January 2007. Accessed June 18, 2020.
Chronic pain is common in veterans, and early engagement in pain treatment is recommended to forestall consequences of untreated pain, including depression, disability, and substance use disorders. The Veterans Health Administration (VHA) employs a stepped care model of pain treatment, with the majority of pain care based in primary care (step 1), and an array of specialty/multimodal treatment options made available at each step in the model for patients with more complex problems, or those who do not respond to more conservative interventions.1
Recognizing the need for comprehensive pain care, the US Congress passed the Comprehensive Addiction and Recovery Act, 21 USC §1521 (2016), which included provisions for VHA facilities to offer multimodal pain treatment and to report the availability of pain care options at each step in the stepped care model.2, With the passage of the Veterans Access, Choice, and Accountability Act of 2014, 38 USC §101 (2014) and now the MISSION Act of 2018, 38 USC §703 (2018) veterans whose VHA facilities are too distant, who require care unavailable at that facility, or who have to wait too long to receive care are eligible for treatment at either VHA or non-VHA facilities.3 These laws allocate the same pool of funds to both VHA and community care and thus create an incentive to engage veterans in care within the VHA network so the funds are not spent out of network.4
An opportunity to connect veterans with VHA care arises at specialized VHA Compensation and Pension (C&P) clinics during examinations that determine whether a veteran’s health conditions were caused or exacerbated by their military service. Veterans file claims with the US Department of Veterans Affairs (VA) Veterans Benefits Administration (VBA), which sends the patient to either a VHA facility or private practitioners for these examinations. Although the number of examinations conducted each year is not available, there were 274,528 veterans newly awarded compensation in fiscal year 2018, and a substantial number of the total of 4,743,108 veterans with C&P awards had reevaluation examinations for at least 1 of their conditions during that year.5 Based largely on the compensation examination results, military service records, and medical records, veterans are granted a service-connected rating for conditions deemed related to military service. A service-connection rating between 0% and 100% is assigned by the VBA, with higher ratings indicating more impairment and, consequently, more financial compensation. Service-connection ratings also are used to decide which veterans are in the highest priority groups for receipt of VHA health care services and are exempt from copayments.
Although traditionally thought of as a forensic evaluation with no clinical purpose, the C&P examination process affords many opportunities to explain VHA care to veterans in distress who file claims.6 A randomized clinical trials (RCT) involving veterans with mental health claims and a second RCT including veterans with musculoskeletal claims each found that veterans use more VHA services if offered outreach at the time of the C&P examination.7,8 In addition to clinical benefits, outreach around the time of C&P examinations also might mitigate the well documented adversarial aspects of the service-connection claims process.6,9,10 Currently, such outreach is not part of routine VHA procedures. Ironically, it is the VBA and not VHA that contacts veterans who are awarded service-connection with information about their eligibility for VHA care based on their award.
Connecting veterans to pain treatment can involve clarifying eligibility for VHA care for veterans in whom eligibility is unknown, involving primary care providers (PCPs) who are the fulcrum of VHA pain care referrals, and motivating veterans to seek specific pain treatment modalities. Connecting veterans to treatment at the time of their compensation examinations also likely involves bidirectional cooperation between the specialized C&P clinics where veterans are examined and the clinics that provide treatment.
Relational coordination is a theoretical framework that can describe the horizontal relationships between different teams within the same medical facility. Relational coordination theorizes that communication between workgroups is related synergistically to the quality of relationships between workgroups. Relational coordination is better between workgroups that share goals and often have high levels of relational coordination, which is thought to be especially important when activities are ambiguous, require cooperation, and are conducted under time pressure.11 High relational coordination also has been associated with high staff job satisfaction, high satisfaction with delivered services, and adherence to treatment guidelines.12-14 An observational cohort study suggested that relational coordination can be improved by targeted interventions that bring workgroups together and facilitate intercommunication.15
To better understand referral and engagement for pain treatment at compensation examinations, VA staff from primary care, mental health, pain management, and C&P teams at the 8 VHA medical centers in New England were invited to complete a validated relational coordination survey.11,16 A subset of invited staff participated in a semistructured interview about pain treatment referral practices within their medical centers.
Assessments were conducted as part of a mixed methods formative evaluation involving quantitative and qualitative methods for a clinical trial at the 8 VHA medical centers in New England. The trial is testing an intervention in which veterans presenting for service-connection examinations for musculoskeletal conditions receive brief counseling to engage them in nonopioid pain treatments. The VHA Central Institutional Review Board approved this formative evaluation and the clinical trial has begun (ClinicalTrials.gov NCT04062214).
Potential interviewees were involved in referrals to and provision of nonpharmacologic pain treatment and were identified by site investigators in the randomized trial. Identified interviewees were clinical and administrative staff belonging to VHA Primary Care, Pain Management, and Compensation and Pension clinics. A total of 83 staff were identified.
Semistructured Interviews
A subset of the 83 staff were invited to participate in a semistructured interview because their position impacted coordination of pain care at their facilities or they worked in C&P. Staff at a site were interviewed until no new themes emerged from additional interviews, and each of the 8 sites was represented. Interviews were conducted between June and August 2018. Standardized scripts describing the study and inviting participation in a semistructured interview were e-mailed to VA staff. At the time of the interview the study purpose was restated and consent for audiotaping was obtained. The interviews followed a guide designed to assess a relational coordination framework among various workgroups. The data in this manuscript were elicited by specific prompts concerning: (1) How veterans learn about pain care when they come through C&P; and (2) How staff in C&P communicate with treatment providers about veterans who have chronic pain. Each interview lasted about 30 minutes.
Relational Coordination Survey
All identified staff were invited to participate in a relational coordination survey. The survey was administered through VA REDCap. Survey invitations were e-mailed from REDCap to VA staff and included a description of the study and assurances of the confidentiality of data collected. Surveys took < 10 minutes to complete. To begin, respondents identified their primary workgroup (C&P, primary care, pain management, or administrative leadership or staff), secondary workgroup (if they were in > 1), and site. Respondents provided no other identifying information and were assured their responses would be confidential.
The survey consisted of 7 questions regarding beliefs about the quality of communication and interactions among workgroup members in obtaining a shared goal.11 The shared goal in the survey used in this study was providing pain care services for veterans with musculoskeletal conditions. Using a 5-point Likert scale, the 7 questions concerned frequency, timeliness, and accuracy of communication; response to problems providing pain services; sharing goals; and knowledge and respect for respondent’s job function. Higher scores indicated better relational coordination among members of a workgroup. Using the survey’s 7 items, composite mean relational coordination scores were calculated for each of the 4 primary workgroups. To account for the possibility that a member rated their own workgroups, 2 scores were created for each workgroup; one included members of the workgroup and another excluded them.
Data Analysis
The audio-recorded semistructured interviews were transcribed and entered into Atlas.ti qualitative data analysis software. To identify cross-cutting themes, a semistructured telephone interview guide was developed by the qualitative study team that emphasized interrelationships between different clinical teams. The transcripts were then analyzed using the grounded theory approach, a systematic methodology to reduce themes from collected qualitative data. Two research staff read each transcript twice; first to familiarize themselves with the text and then, using open coding, to identify important concepts that emerged from the language and assign codes to segments of text. To ensure accuracy, researchers included suitable contextual information in the coding. Using the constant comparative method, research staff then met to examine the themes that emerged in the interviews, discuss and coalesce coding discrepancies, and compare perspectives.17
The composite score (mean of the 7 items and 95% CI) of the survey responses was analyzed to identify significant differences in coordination across the 4 workgroups. Analysis of variance (ANOVA) was used to examine each relational coordination score by respondents’ workgroup. Post hoc analyses examined relational coordination survey differences among the 4 respondent groups.
Results
Thirty-nine survey respondents participated in the semistructured interviews. C&P examiners expressed varying degrees of comfort with their role in extending access to pain care for veterans. Some of the examiners strongly believed that their role was purely forensic, and going beyond this forensic role to refer or recommend treatment to veterans would be a violation of their role to conduct a forensic examination. “We don’t have an ongoing therapeutic relationship with any of the patients,” a C&P examiner explained: “We see them once; they’re out the door. It’s forensic. We’re investigating the person as a claimant, we’re investigating it and using our tools to go and review information from 30, 40 years ago.”
Other examiners had a less strict approach for working with veterans in C&P, even though examiners are asked not to provide advice or therapy. One C&P examiner noted that because he “can’t watch people in pain,” during the examination this doctor recommends that patients go to the office that determines whether they are eligible for benefits and choose a PCP. Another C&P examiner concurred with this approach. “I certainly spend a little time with the veteran talking to them about their personal life, who they are, what they do, what they’ve done, what they’re going to do to kind of break the ice between us,” the second examiner explained. “At the end, I will make some suggestions to them. I’m comfortable doing that. I don’t know that everybody is.”
Many of the VHA providers we interviewed had little knowledge of the C&P process or whether C&P examiners had any role or responsibilities in referring veterans for pain care. Most VHA providers could not name any C&P examiners at their facility and were generally unfamiliar with the content of C&P examinations. One provider bluntly said, “I’ve never communicated with anyone in comp and pen [C&P].”
Another PCP also expressed concerns with referrals, suggesting that C&P and primary care “are totally separate and should remain separate,” the PCP explained. “My concern with getting referral from comp and pen is that is it then they’re seeking all sorts of treatment that they wouldn’t necessarily need or ask for otherwise.”
Conversely a different PCP had a positive outlook on how C&P examiners might help ease the transition into the VHA for veterans with pain, especially for newly discharged veterans. “Having comp and pen address these issues is really going to be helpful. I think it could be significant that the topic is introduced early on.”
Relational Coordination Survey
Relational coordination surveys were sent to 83 participants of whom 66 responded. Respondents were from
The relational coordination composite scores were lowest for C&P. This finding remained whether C&P staff surveys were included or removed from the C&P responses. As demonstrated by the 95% CI, when team members’ surveys were included, C&P scores (95% CI, 2.01-2.42) were significantly lower than the primary care (95% CI, 3.34-3.64) and pain management (95% CI, 3.61-3.96) groups. All the relational coordination composite scores were slightly lower when staff who described their own workgroup were removed (ie, respondents rated their own workgroups as having higher relational coordination than others did). Using the composite scores excluding same workgroup members, the composite scores of the C&P remained significantly lower than all 3 other workgroups (Table). Means values for each individual item in the C&P group were significantly less than all other group means for each item except for the question on responses to problems providing pain services (data not shown). On this item only, the mean C&P rating was > 3 (3.19), but this was still lower than the means of the primary care and pain management workgroups.
Further analyses were undertaken to understand the importance of stakeholders’ ratings of their own workgroup compared with ratings by others of that workgroup. A 1-way ANOVA of workgroup was conducted and displayed significant workgroup differences between member and nonmember relational coordination ratings on 3 of the 4 workgroup’s scores C&P (F = 5.75, 3, 62 df; P < .01) primary care (F = 4.30, 3, 62 df; P < .008) and pain management (F = 8.22, 3, 62 df; P < .001). Post hoc contrasts between the different workgroups doing the rating revealed: (1) significant differences in the assessment of the C&P workgroup between the C&P workgroup and both the primary care (P < .01) and pain management groups (P < .001) with C&P rating their own workgroup significantly higher; (2) a significant difference in the scoring of the primary care workgroup with the primary care group rating themselves significantly higher than the C&P group; and (3) significant differences in the scoring of the pain management workgroup with both pain management and primary care groups rating the pain management group significantly higher than the C&P group. The results were not substantially changed by removing the 18 respondents who identified themselves as being part of > 1 workgroup .
Discussion
Mixed methods revealed disparate viewpoints about the role of C&P in referring veterans to pain care services. Overall, C&P teams coordinated less with other workgroups than the other groups coordinated with each other, and the C&P clinics took only limited steps to engage veterans in VHA treatment. The relational coordination results appeared to be valid. The mean scores were near the middle of the relational coordination rating scale, with standard deviations indicating a range of responses. The lower relational coordination scores of the C&P group remained after removing stakeholders who were rating their own workgroup. Further support for the validity of the relational coordination survey results is that they were consistent with the reports of C&P clinic isolation in the semistructured interviews.
The interview data suggest that one reason the C&P teams had low relational coordination scores is that VA staff interpret the emphasis on evaluative rather than therapeutic examinations to preclude other attempts to engage veterans into VHA treatment, even though such treatment engagement is permitted within existing guidelines. VBA referrals for examinations say nothing, either way, about engaging veterans in VHA care. The relational coordination results suggest that an intervention that might increase treatment referrals from the C&P clinics would be to explain the (existing) policy allowing for outreach around the time of compensation examinations to VHA staff so this goal is clearly agreed-upon. Another approach to facilitating treatment engagement at the C&P examination is to use other interventions that have been associated with better relational coordination such as intergroup meetings, horizontal integration more generally, and an atmosphere is which people from different backgrounds feel empowered to speak frankly to each other.15,18,19 An important linkage to forge is between C&P teams and the administrative workgroups responsible for verifying a veteran’s eligibility for VHA care and enrolling eligible veterans in VHA treatment. Having C&P clinicians who are familiar with the eligibility and treatment engagement processes would facilitate providing that information to veterans, without compromising the evaluative format of the compensation examination.
An interesting ancillary finding is that relational coordination ratings by members of 3 of the 4 workgroups were higher than ratings by other staff of that workgroup. A possible explanation for this finding is that workgroup members are more aware of the relational coordination efforts made by their own workgroup than those by other workgroups, and therefore rate their own workgroup higher. This also might be part of a broader self-aggrandizement heuristic that has been described in multiple domains.20 Staff may apply this heuristic in reporting that their staff engage in more relational coordination, reflecting the social desirability of being cooperative.
There are simple facility-level interventions that would facilitate veterans access to care such as conducting C&P examinations for potentially treatment-eligible veterans at VHA facilities (vs conducted outside VHA) and having access to materials that explain the treatment options to veterans when they check in for their compensation examinations. The approach to C&P-based treatment engagement that was successfully employed in 2 clinical trials involved having counselors not connected with the C&P clinic contact veterans around the time of their compensation examination to explain VA treatment options and motivate veterans to pursue treatment.8,9 This independent counselor approach is being evaluated in a larger study.
Limitations
These data are from a small number of VA staff evaluating veterans in a single region of the US. They do not show causation, and it is possible that relational coordination is not necessary for referrals from C&P clinics. Relational coordination might not be necessary when referral processes can be simply routinized with little need for communication.11 However, other analyses in these clinics have found that pain treatment referrals in fact are not routinized, with substantial variability within and across institutions. Another possibility is that features that have been associated with less relational coordination, such as male gender and medical specialist guild, were disproportionately present in C&P clinics compared to the other clinics.21
Conclusions
There have been public calls to improve the evaluation of service-connection claims such that this process includes approaches to engage veterans in treatment.22 Referring veterans to treatment when they come for C&P examinations will likely involve improving relational coordination between the C&P service and other parts of VHA. Nationwide, sites that integrate C&P more fully may have valuable lessons to impart about the benefits of such integration. An important step towards better relational coordination will be clarifying that engaging veterans in VHA care around the time of their C&P examinations is a facility-wide goal.
Acknowledgments
The authors thank Brian Linde and Efia James for their perspectives on C&P procedures. This work was supported by the Veterans Integrated Service Network 1 Mental Illness Research Education and Clinical Center (MIRECC) and National Institute of Health, National Center for Complementary and Integrative Health Project # 5UG3AT009758-02. (MIR, SM mPIs).
Chronic pain is common in veterans, and early engagement in pain treatment is recommended to forestall consequences of untreated pain, including depression, disability, and substance use disorders. The Veterans Health Administration (VHA) employs a stepped care model of pain treatment, with the majority of pain care based in primary care (step 1), and an array of specialty/multimodal treatment options made available at each step in the model for patients with more complex problems, or those who do not respond to more conservative interventions.1
Recognizing the need for comprehensive pain care, the US Congress passed the Comprehensive Addiction and Recovery Act, 21 USC §1521 (2016), which included provisions for VHA facilities to offer multimodal pain treatment and to report the availability of pain care options at each step in the stepped care model.2, With the passage of the Veterans Access, Choice, and Accountability Act of 2014, 38 USC §101 (2014) and now the MISSION Act of 2018, 38 USC §703 (2018) veterans whose VHA facilities are too distant, who require care unavailable at that facility, or who have to wait too long to receive care are eligible for treatment at either VHA or non-VHA facilities.3 These laws allocate the same pool of funds to both VHA and community care and thus create an incentive to engage veterans in care within the VHA network so the funds are not spent out of network.4
An opportunity to connect veterans with VHA care arises at specialized VHA Compensation and Pension (C&P) clinics during examinations that determine whether a veteran’s health conditions were caused or exacerbated by their military service. Veterans file claims with the US Department of Veterans Affairs (VA) Veterans Benefits Administration (VBA), which sends the patient to either a VHA facility or private practitioners for these examinations. Although the number of examinations conducted each year is not available, there were 274,528 veterans newly awarded compensation in fiscal year 2018, and a substantial number of the total of 4,743,108 veterans with C&P awards had reevaluation examinations for at least 1 of their conditions during that year.5 Based largely on the compensation examination results, military service records, and medical records, veterans are granted a service-connected rating for conditions deemed related to military service. A service-connection rating between 0% and 100% is assigned by the VBA, with higher ratings indicating more impairment and, consequently, more financial compensation. Service-connection ratings also are used to decide which veterans are in the highest priority groups for receipt of VHA health care services and are exempt from copayments.
Although traditionally thought of as a forensic evaluation with no clinical purpose, the C&P examination process affords many opportunities to explain VHA care to veterans in distress who file claims.6 A randomized clinical trials (RCT) involving veterans with mental health claims and a second RCT including veterans with musculoskeletal claims each found that veterans use more VHA services if offered outreach at the time of the C&P examination.7,8 In addition to clinical benefits, outreach around the time of C&P examinations also might mitigate the well documented adversarial aspects of the service-connection claims process.6,9,10 Currently, such outreach is not part of routine VHA procedures. Ironically, it is the VBA and not VHA that contacts veterans who are awarded service-connection with information about their eligibility for VHA care based on their award.
Connecting veterans to pain treatment can involve clarifying eligibility for VHA care for veterans in whom eligibility is unknown, involving primary care providers (PCPs) who are the fulcrum of VHA pain care referrals, and motivating veterans to seek specific pain treatment modalities. Connecting veterans to treatment at the time of their compensation examinations also likely involves bidirectional cooperation between the specialized C&P clinics where veterans are examined and the clinics that provide treatment.
Relational coordination is a theoretical framework that can describe the horizontal relationships between different teams within the same medical facility. Relational coordination theorizes that communication between workgroups is related synergistically to the quality of relationships between workgroups. Relational coordination is better between workgroups that share goals and often have high levels of relational coordination, which is thought to be especially important when activities are ambiguous, require cooperation, and are conducted under time pressure.11 High relational coordination also has been associated with high staff job satisfaction, high satisfaction with delivered services, and adherence to treatment guidelines.12-14 An observational cohort study suggested that relational coordination can be improved by targeted interventions that bring workgroups together and facilitate intercommunication.15
To better understand referral and engagement for pain treatment at compensation examinations, VA staff from primary care, mental health, pain management, and C&P teams at the 8 VHA medical centers in New England were invited to complete a validated relational coordination survey.11,16 A subset of invited staff participated in a semistructured interview about pain treatment referral practices within their medical centers.
Assessments were conducted as part of a mixed methods formative evaluation involving quantitative and qualitative methods for a clinical trial at the 8 VHA medical centers in New England. The trial is testing an intervention in which veterans presenting for service-connection examinations for musculoskeletal conditions receive brief counseling to engage them in nonopioid pain treatments. The VHA Central Institutional Review Board approved this formative evaluation and the clinical trial has begun (ClinicalTrials.gov NCT04062214).
Potential interviewees were involved in referrals to and provision of nonpharmacologic pain treatment and were identified by site investigators in the randomized trial. Identified interviewees were clinical and administrative staff belonging to VHA Primary Care, Pain Management, and Compensation and Pension clinics. A total of 83 staff were identified.
Semistructured Interviews
A subset of the 83 staff were invited to participate in a semistructured interview because their position impacted coordination of pain care at their facilities or they worked in C&P. Staff at a site were interviewed until no new themes emerged from additional interviews, and each of the 8 sites was represented. Interviews were conducted between June and August 2018. Standardized scripts describing the study and inviting participation in a semistructured interview were e-mailed to VA staff. At the time of the interview the study purpose was restated and consent for audiotaping was obtained. The interviews followed a guide designed to assess a relational coordination framework among various workgroups. The data in this manuscript were elicited by specific prompts concerning: (1) How veterans learn about pain care when they come through C&P; and (2) How staff in C&P communicate with treatment providers about veterans who have chronic pain. Each interview lasted about 30 minutes.
Relational Coordination Survey
All identified staff were invited to participate in a relational coordination survey. The survey was administered through VA REDCap. Survey invitations were e-mailed from REDCap to VA staff and included a description of the study and assurances of the confidentiality of data collected. Surveys took < 10 minutes to complete. To begin, respondents identified their primary workgroup (C&P, primary care, pain management, or administrative leadership or staff), secondary workgroup (if they were in > 1), and site. Respondents provided no other identifying information and were assured their responses would be confidential.
The survey consisted of 7 questions regarding beliefs about the quality of communication and interactions among workgroup members in obtaining a shared goal.11 The shared goal in the survey used in this study was providing pain care services for veterans with musculoskeletal conditions. Using a 5-point Likert scale, the 7 questions concerned frequency, timeliness, and accuracy of communication; response to problems providing pain services; sharing goals; and knowledge and respect for respondent’s job function. Higher scores indicated better relational coordination among members of a workgroup. Using the survey’s 7 items, composite mean relational coordination scores were calculated for each of the 4 primary workgroups. To account for the possibility that a member rated their own workgroups, 2 scores were created for each workgroup; one included members of the workgroup and another excluded them.
Data Analysis
The audio-recorded semistructured interviews were transcribed and entered into Atlas.ti qualitative data analysis software. To identify cross-cutting themes, a semistructured telephone interview guide was developed by the qualitative study team that emphasized interrelationships between different clinical teams. The transcripts were then analyzed using the grounded theory approach, a systematic methodology to reduce themes from collected qualitative data. Two research staff read each transcript twice; first to familiarize themselves with the text and then, using open coding, to identify important concepts that emerged from the language and assign codes to segments of text. To ensure accuracy, researchers included suitable contextual information in the coding. Using the constant comparative method, research staff then met to examine the themes that emerged in the interviews, discuss and coalesce coding discrepancies, and compare perspectives.17
The composite score (mean of the 7 items and 95% CI) of the survey responses was analyzed to identify significant differences in coordination across the 4 workgroups. Analysis of variance (ANOVA) was used to examine each relational coordination score by respondents’ workgroup. Post hoc analyses examined relational coordination survey differences among the 4 respondent groups.
Results
Thirty-nine survey respondents participated in the semistructured interviews. C&P examiners expressed varying degrees of comfort with their role in extending access to pain care for veterans. Some of the examiners strongly believed that their role was purely forensic, and going beyond this forensic role to refer or recommend treatment to veterans would be a violation of their role to conduct a forensic examination. “We don’t have an ongoing therapeutic relationship with any of the patients,” a C&P examiner explained: “We see them once; they’re out the door. It’s forensic. We’re investigating the person as a claimant, we’re investigating it and using our tools to go and review information from 30, 40 years ago.”
Other examiners had a less strict approach for working with veterans in C&P, even though examiners are asked not to provide advice or therapy. One C&P examiner noted that because he “can’t watch people in pain,” during the examination this doctor recommends that patients go to the office that determines whether they are eligible for benefits and choose a PCP. Another C&P examiner concurred with this approach. “I certainly spend a little time with the veteran talking to them about their personal life, who they are, what they do, what they’ve done, what they’re going to do to kind of break the ice between us,” the second examiner explained. “At the end, I will make some suggestions to them. I’m comfortable doing that. I don’t know that everybody is.”
Many of the VHA providers we interviewed had little knowledge of the C&P process or whether C&P examiners had any role or responsibilities in referring veterans for pain care. Most VHA providers could not name any C&P examiners at their facility and were generally unfamiliar with the content of C&P examinations. One provider bluntly said, “I’ve never communicated with anyone in comp and pen [C&P].”
Another PCP also expressed concerns with referrals, suggesting that C&P and primary care “are totally separate and should remain separate,” the PCP explained. “My concern with getting referral from comp and pen is that is it then they’re seeking all sorts of treatment that they wouldn’t necessarily need or ask for otherwise.”
Conversely a different PCP had a positive outlook on how C&P examiners might help ease the transition into the VHA for veterans with pain, especially for newly discharged veterans. “Having comp and pen address these issues is really going to be helpful. I think it could be significant that the topic is introduced early on.”
Relational Coordination Survey
Relational coordination surveys were sent to 83 participants of whom 66 responded. Respondents were from
The relational coordination composite scores were lowest for C&P. This finding remained whether C&P staff surveys were included or removed from the C&P responses. As demonstrated by the 95% CI, when team members’ surveys were included, C&P scores (95% CI, 2.01-2.42) were significantly lower than the primary care (95% CI, 3.34-3.64) and pain management (95% CI, 3.61-3.96) groups. All the relational coordination composite scores were slightly lower when staff who described their own workgroup were removed (ie, respondents rated their own workgroups as having higher relational coordination than others did). Using the composite scores excluding same workgroup members, the composite scores of the C&P remained significantly lower than all 3 other workgroups (Table). Means values for each individual item in the C&P group were significantly less than all other group means for each item except for the question on responses to problems providing pain services (data not shown). On this item only, the mean C&P rating was > 3 (3.19), but this was still lower than the means of the primary care and pain management workgroups.
Further analyses were undertaken to understand the importance of stakeholders’ ratings of their own workgroup compared with ratings by others of that workgroup. A 1-way ANOVA of workgroup was conducted and displayed significant workgroup differences between member and nonmember relational coordination ratings on 3 of the 4 workgroup’s scores C&P (F = 5.75, 3, 62 df; P < .01) primary care (F = 4.30, 3, 62 df; P < .008) and pain management (F = 8.22, 3, 62 df; P < .001). Post hoc contrasts between the different workgroups doing the rating revealed: (1) significant differences in the assessment of the C&P workgroup between the C&P workgroup and both the primary care (P < .01) and pain management groups (P < .001) with C&P rating their own workgroup significantly higher; (2) a significant difference in the scoring of the primary care workgroup with the primary care group rating themselves significantly higher than the C&P group; and (3) significant differences in the scoring of the pain management workgroup with both pain management and primary care groups rating the pain management group significantly higher than the C&P group. The results were not substantially changed by removing the 18 respondents who identified themselves as being part of > 1 workgroup .
Discussion
Mixed methods revealed disparate viewpoints about the role of C&P in referring veterans to pain care services. Overall, C&P teams coordinated less with other workgroups than the other groups coordinated with each other, and the C&P clinics took only limited steps to engage veterans in VHA treatment. The relational coordination results appeared to be valid. The mean scores were near the middle of the relational coordination rating scale, with standard deviations indicating a range of responses. The lower relational coordination scores of the C&P group remained after removing stakeholders who were rating their own workgroup. Further support for the validity of the relational coordination survey results is that they were consistent with the reports of C&P clinic isolation in the semistructured interviews.
The interview data suggest that one reason the C&P teams had low relational coordination scores is that VA staff interpret the emphasis on evaluative rather than therapeutic examinations to preclude other attempts to engage veterans into VHA treatment, even though such treatment engagement is permitted within existing guidelines. VBA referrals for examinations say nothing, either way, about engaging veterans in VHA care. The relational coordination results suggest that an intervention that might increase treatment referrals from the C&P clinics would be to explain the (existing) policy allowing for outreach around the time of compensation examinations to VHA staff so this goal is clearly agreed-upon. Another approach to facilitating treatment engagement at the C&P examination is to use other interventions that have been associated with better relational coordination such as intergroup meetings, horizontal integration more generally, and an atmosphere is which people from different backgrounds feel empowered to speak frankly to each other.15,18,19 An important linkage to forge is between C&P teams and the administrative workgroups responsible for verifying a veteran’s eligibility for VHA care and enrolling eligible veterans in VHA treatment. Having C&P clinicians who are familiar with the eligibility and treatment engagement processes would facilitate providing that information to veterans, without compromising the evaluative format of the compensation examination.
An interesting ancillary finding is that relational coordination ratings by members of 3 of the 4 workgroups were higher than ratings by other staff of that workgroup. A possible explanation for this finding is that workgroup members are more aware of the relational coordination efforts made by their own workgroup than those by other workgroups, and therefore rate their own workgroup higher. This also might be part of a broader self-aggrandizement heuristic that has been described in multiple domains.20 Staff may apply this heuristic in reporting that their staff engage in more relational coordination, reflecting the social desirability of being cooperative.
There are simple facility-level interventions that would facilitate veterans access to care such as conducting C&P examinations for potentially treatment-eligible veterans at VHA facilities (vs conducted outside VHA) and having access to materials that explain the treatment options to veterans when they check in for their compensation examinations. The approach to C&P-based treatment engagement that was successfully employed in 2 clinical trials involved having counselors not connected with the C&P clinic contact veterans around the time of their compensation examination to explain VA treatment options and motivate veterans to pursue treatment.8,9 This independent counselor approach is being evaluated in a larger study.
Limitations
These data are from a small number of VA staff evaluating veterans in a single region of the US. They do not show causation, and it is possible that relational coordination is not necessary for referrals from C&P clinics. Relational coordination might not be necessary when referral processes can be simply routinized with little need for communication.11 However, other analyses in these clinics have found that pain treatment referrals in fact are not routinized, with substantial variability within and across institutions. Another possibility is that features that have been associated with less relational coordination, such as male gender and medical specialist guild, were disproportionately present in C&P clinics compared to the other clinics.21
Conclusions
There have been public calls to improve the evaluation of service-connection claims such that this process includes approaches to engage veterans in treatment.22 Referring veterans to treatment when they come for C&P examinations will likely involve improving relational coordination between the C&P service and other parts of VHA. Nationwide, sites that integrate C&P more fully may have valuable lessons to impart about the benefits of such integration. An important step towards better relational coordination will be clarifying that engaging veterans in VHA care around the time of their C&P examinations is a facility-wide goal.
Acknowledgments
The authors thank Brian Linde and Efia James for their perspectives on C&P procedures. This work was supported by the Veterans Integrated Service Network 1 Mental Illness Research Education and Clinical Center (MIRECC) and National Institute of Health, National Center for Complementary and Integrative Health Project # 5UG3AT009758-02. (MIR, SM mPIs).
1. US Department Veterans Affairs, Veterans Health Administration. VHA Directive 2009-053: pain management. https://www.va.gov/painmanagement/docs/vha09paindirective.pdf. Published October 28, 2019. Accessed June 18, 2020.
2. Rosenberger PH, Phillip EJ, Lee A, Kerns RD. The VHA’s national pain management strategy: implementing the stepped care model. Fed Pract. 2011;28(8):39-42.
3. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: A Qualitative Examination of Rapid Policy Implementation in the Department of Veterans Affairs. Med Care. 2017;55 Suppl 7 Suppl 1:S71-S75. doi:10.1097/MLR.0000000000000667
4. Rieselbach RE, Epperly T, Nycz G, Shin P. Community health centers could provide better outsourced primary care for veterans. J Gen Intern Med. 2019;34(1):150-153. doi:10.1007/s11606-018-4691-4
5. US Department of Veterans Affairs, Veterans Benefit Administration. VBA annual benefits report fiscal year 2018. https://www.benefits.va.gov/REPORTS/abr/docs/2018-abr.pdf. Updated March 29, 2019. Accessed June 17, 2020.
6. Rosen MI. Compensation examinations for PTSD-an opportunity for treatment? J Rehabil Res Dev. 2010;47(5):xv-xxii. doi:10.1682/jrrd.2010.04.0075
7. Rosen MI, Ablondi K, Black AC, et al. Work outcomes after benefits counseling among veterans applying for service connection for a psychiatric condition. Psychiatr Serv. 2014;65(12):1426-1432. doi:10.1176/appi.ps.201300478
8. Rosen MI, Becker WC, Black AC, Martino S, Edens EL, Kerns RD. Brief counseling for veterans with musculoskeletal disorder, risky substance use, and service connection claims. Pain Med. 2019;20(3):528-542. doi:10.1093/pm/pny071
9. Meshberg-Cohen S, DeViva JC, Rosen MI. Counseling veterans applying for service connection status for mental health conditions. Psychiatr Serv. 2017;68(4):396-399. doi:10.1176/appi.ps.201500533
10. Sayer NA, Spoont M, Nelson DB. Post-traumatic stress disorder claims from the viewpoint of veterans service officers. Mil Med. 2005;170(10):867-870. doi:10.7205/milmed.170.10.867
11. Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manage Sci. 2002;48(11):1408-1426. doi: 10.1287/mnsc.48.11.1408.268
12. Havens DS, Gittell JH, Vasey J. Impact of relational coordination on nurse job satisfaction, work engagement and burnout: achieving the quadruple aim. J Nurs Adm. 2018;48(3):132-140. doi:10.1097/NNA.0000000000000587
13. Gittell JH, Logan C, Cronenwett J, et al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Manage Rev. 2020;45(1):12-20. doi:10.1097/HMR.0000000000000192
14. Cramm JM, Nieboer AP. Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Health Care Manage Rev. 2012;37(4):301-309. doi:10.1097/HMR.0b013e3182355ea4
15. Abu-Rish Blakeney E, Lavallee DC, Baik D, Pambianco S, O’Brien KD, Zierler BK. Purposeful interprofessional team intervention improves relational coordination among advanced heart failure care teams. J Interprof Care. 2019;33(5):481-489. doi:10.1080/13561820.2018.1560248
16. Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16-e30. doi:10.1097/MLR.0b013e31827feef6
17. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL. Transaction Publishers; 2009.
18. Gittell JH. How interdependent parties build relational coordination to achieve their desired outcomes. Negot J. 2015;31(4):387-391. doi: 10.1111/nejo.12114
19. Solberg MT, Hansen TW, Bjørk IT. The need for predictability in coordination of ventilator treatment of newborn infants--a qualitative study. Intensive Crit Care Nurs. 2015;31(4):205-212. doi:10.1016/j.iccn.2014.12.003
20. Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull. 1988;103(2):193-210.
21. Hartgerink JM, Cramm JM, Bakker TJ, van Eijsden AM, Mackenbach JP, Nieboer AP. The importance of multidisciplinary teamwork and team climate for relational coordination among teams delivering care to older patients. J Adv Nurs. 2014;70(4):791-799. doi:10.1111/jan.12233
22. Bilmes L. soldiers returning from iraq and afghanistan: the long-term costs of providing veterans medical care and disability benefits RWP07-001. https://research.hks.harvard.edu/publications/getFile.aspx?Id=237. Published January 2007. Accessed June 18, 2020.
1. US Department Veterans Affairs, Veterans Health Administration. VHA Directive 2009-053: pain management. https://www.va.gov/painmanagement/docs/vha09paindirective.pdf. Published October 28, 2019. Accessed June 18, 2020.
2. Rosenberger PH, Phillip EJ, Lee A, Kerns RD. The VHA’s national pain management strategy: implementing the stepped care model. Fed Pract. 2011;28(8):39-42.
3. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: A Qualitative Examination of Rapid Policy Implementation in the Department of Veterans Affairs. Med Care. 2017;55 Suppl 7 Suppl 1:S71-S75. doi:10.1097/MLR.0000000000000667
4. Rieselbach RE, Epperly T, Nycz G, Shin P. Community health centers could provide better outsourced primary care for veterans. J Gen Intern Med. 2019;34(1):150-153. doi:10.1007/s11606-018-4691-4
5. US Department of Veterans Affairs, Veterans Benefit Administration. VBA annual benefits report fiscal year 2018. https://www.benefits.va.gov/REPORTS/abr/docs/2018-abr.pdf. Updated March 29, 2019. Accessed June 17, 2020.
6. Rosen MI. Compensation examinations for PTSD-an opportunity for treatment? J Rehabil Res Dev. 2010;47(5):xv-xxii. doi:10.1682/jrrd.2010.04.0075
7. Rosen MI, Ablondi K, Black AC, et al. Work outcomes after benefits counseling among veterans applying for service connection for a psychiatric condition. Psychiatr Serv. 2014;65(12):1426-1432. doi:10.1176/appi.ps.201300478
8. Rosen MI, Becker WC, Black AC, Martino S, Edens EL, Kerns RD. Brief counseling for veterans with musculoskeletal disorder, risky substance use, and service connection claims. Pain Med. 2019;20(3):528-542. doi:10.1093/pm/pny071
9. Meshberg-Cohen S, DeViva JC, Rosen MI. Counseling veterans applying for service connection status for mental health conditions. Psychiatr Serv. 2017;68(4):396-399. doi:10.1176/appi.ps.201500533
10. Sayer NA, Spoont M, Nelson DB. Post-traumatic stress disorder claims from the viewpoint of veterans service officers. Mil Med. 2005;170(10):867-870. doi:10.7205/milmed.170.10.867
11. Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manage Sci. 2002;48(11):1408-1426. doi: 10.1287/mnsc.48.11.1408.268
12. Havens DS, Gittell JH, Vasey J. Impact of relational coordination on nurse job satisfaction, work engagement and burnout: achieving the quadruple aim. J Nurs Adm. 2018;48(3):132-140. doi:10.1097/NNA.0000000000000587
13. Gittell JH, Logan C, Cronenwett J, et al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Manage Rev. 2020;45(1):12-20. doi:10.1097/HMR.0000000000000192
14. Cramm JM, Nieboer AP. Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Health Care Manage Rev. 2012;37(4):301-309. doi:10.1097/HMR.0b013e3182355ea4
15. Abu-Rish Blakeney E, Lavallee DC, Baik D, Pambianco S, O’Brien KD, Zierler BK. Purposeful interprofessional team intervention improves relational coordination among advanced heart failure care teams. J Interprof Care. 2019;33(5):481-489. doi:10.1080/13561820.2018.1560248
16. Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16-e30. doi:10.1097/MLR.0b013e31827feef6
17. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL. Transaction Publishers; 2009.
18. Gittell JH. How interdependent parties build relational coordination to achieve their desired outcomes. Negot J. 2015;31(4):387-391. doi: 10.1111/nejo.12114
19. Solberg MT, Hansen TW, Bjørk IT. The need for predictability in coordination of ventilator treatment of newborn infants--a qualitative study. Intensive Crit Care Nurs. 2015;31(4):205-212. doi:10.1016/j.iccn.2014.12.003
20. Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull. 1988;103(2):193-210.
21. Hartgerink JM, Cramm JM, Bakker TJ, van Eijsden AM, Mackenbach JP, Nieboer AP. The importance of multidisciplinary teamwork and team climate for relational coordination among teams delivering care to older patients. J Adv Nurs. 2014;70(4):791-799. doi:10.1111/jan.12233
22. Bilmes L. soldiers returning from iraq and afghanistan: the long-term costs of providing veterans medical care and disability benefits RWP07-001. https://research.hks.harvard.edu/publications/getFile.aspx?Id=237. Published January 2007. Accessed June 18, 2020.