User login
Fewer GI docs, more alcohol-associated liver disease deaths
People are more likely to die of alcohol-associated liver disease (ALD) when there are fewer gastroenterologists in their state, researchers say.
The finding raises questions about steps that policymakers could take to increase the number of gastroenterologists and spread them more evenly around the United States.
“We found that there’s a fivefold difference in density of gastroenterologists through different states,” said Brian P. Lee, MD, MAS, an assistant professor of clinical medicine at the University of Southern California, Los Angeles.
Dr. Lee and colleagues published their findings in Clinical Gastroenterology and Hepatology.
ALD is becoming more common, and it is killing more people. Research among veterans has linked visits to gastroenterologists to a lower risk for death from liver disease.
To see whether that correlation applies more broadly, Dr. Lee and colleagues compared multiple datasets. One from the U.S. Health Resources & Service Administration provided the number of gastroenterologists per 100,000 population. The other from the U.S. Centers for Disease Control and Prevention provided ALD-related deaths per 1,000,000 adults for each state and the District of Columbia.
The researchers adjusted for many variables that could affect the relationship between the availability of gastroenterologists and deaths related to ALD, including the age distribution of the population in each state, the gender balance, race and ethnicity, binge drinking, household income, obesity, and the proportion of rural residents.
They found that for every additional gastroenterologist, there is almost one fewer ALD-related death each year per 100,000 population (9.0 [95% confidence interval, 1.3-16.7] fewer ALD-related deaths per 1,000,000 population for each additional gastroenterologist per 100,000 population).
The strength of the association appeared to plateau when there were at least 7.5 gastroenterologists per 100,000 people.
From these findings, the researchers calculated that as many as 40% of deaths from ALD nationwide could be prevented by providing more gastroenterologists in the places where they are lacking.
The mean number of gastroenterologists per 100,000 people in the United States was 4.6, and the annual ALD-related death rate was 85.6 per 1,000,000 people.
The Atlantic states had the greatest concentration of gastroenterologists and the lowest ALD-related mortality, whereas the Mountain states had the lowest concentration of gastroenterologists and the highest ALD-related mortality.
The lowest mortality related to ALD was in New Jersey, Maryland, and Hawaii, with 52 per 1,000,000 people, and the highest was in Wyoming, with 289.
Study shines spotlight on general GI care
Access to liver transplants did not make a statistically significant difference in mortality from ALD.
“It makes you realize that transplant will only be accessible for really just a small fraction of the population who needs it,” Dr. Lee told this news organization.
General gastroenterologic care appears to make a bigger difference in saving patients’ lives. “Are they getting endoscopy for bleeding from varices?” Dr. Lee asked. “Are they getting appropriate antibiotics prescribed to prevent bacterial infection of ascites?”
The concentration of primary care physicians did not reduce mortality from ALD, and neither did the concentration of substance use, behavioral disorder, and mental health counselors.
Previous research has shown that substance abuse therapy is effective. But many people do not want to undertake it, or they face barriers of transportation, language, or insurance, said Dr. Lee.
“I have many patients whose insurance will provide them access to medical visits to me but will not to substance-use rehab, for example,” he said.
To see whether the effect was more generally due to the concentration of medical specialists, the researchers examined the state-level density of ophthalmologists and dermatologists. They found no significant difference in ALD-related mortality.
The finding builds on reports by the American Gastroenterological Association and the American Association for the Study of Liver Diseases that the number of gastroenterologists has not kept up with the U.S. population nor the burden of digestive diseases, and that predicts a critical shortage in the future.
Overcoming barriers to care for liver disease
The overall supply of gastroenterologists could be increased by reducing the educational requirements and increasing the funding for fellowships, said Dr. Lee.
“We have to have a better understanding as to the barriers to gastroenterology practice in certain areas, then interventions to address those barriers and also incentives to attract gastroenterologists to those areas,” Dr. Lee said.
The study underscores the importance of access to gastroenterological care, said George Cholankeril, MD, assistant professor of medicine at Baylor College of Medicine, Houston, who was not involved in the study. That urgency has only grown as ALD has spiraled up with the COVID-19 pandemic, he said.
“Anyone in clinical practice right now will be able to say that there’s been a clear rising tide of patients with alcohol-related liver disease,” he told this news organization. “There’s an urgent need to address this and provide the necessary resources.”
Prevention remains essential, Dr. Cholankeril said.
Gastroenterologists and primary care physicians can help stem the tide of ALD by screening their patients for the disease through a tool like AUDIT (Alcohol Use Disorders Identification Test), he said. They can then refer patients to substance abuse treatment centers or to psychologists and psychiatrists.
Dr. Lee and Dr. Cholankeril report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People are more likely to die of alcohol-associated liver disease (ALD) when there are fewer gastroenterologists in their state, researchers say.
The finding raises questions about steps that policymakers could take to increase the number of gastroenterologists and spread them more evenly around the United States.
“We found that there’s a fivefold difference in density of gastroenterologists through different states,” said Brian P. Lee, MD, MAS, an assistant professor of clinical medicine at the University of Southern California, Los Angeles.
Dr. Lee and colleagues published their findings in Clinical Gastroenterology and Hepatology.
ALD is becoming more common, and it is killing more people. Research among veterans has linked visits to gastroenterologists to a lower risk for death from liver disease.
To see whether that correlation applies more broadly, Dr. Lee and colleagues compared multiple datasets. One from the U.S. Health Resources & Service Administration provided the number of gastroenterologists per 100,000 population. The other from the U.S. Centers for Disease Control and Prevention provided ALD-related deaths per 1,000,000 adults for each state and the District of Columbia.
The researchers adjusted for many variables that could affect the relationship between the availability of gastroenterologists and deaths related to ALD, including the age distribution of the population in each state, the gender balance, race and ethnicity, binge drinking, household income, obesity, and the proportion of rural residents.
They found that for every additional gastroenterologist, there is almost one fewer ALD-related death each year per 100,000 population (9.0 [95% confidence interval, 1.3-16.7] fewer ALD-related deaths per 1,000,000 population for each additional gastroenterologist per 100,000 population).
The strength of the association appeared to plateau when there were at least 7.5 gastroenterologists per 100,000 people.
From these findings, the researchers calculated that as many as 40% of deaths from ALD nationwide could be prevented by providing more gastroenterologists in the places where they are lacking.
The mean number of gastroenterologists per 100,000 people in the United States was 4.6, and the annual ALD-related death rate was 85.6 per 1,000,000 people.
The Atlantic states had the greatest concentration of gastroenterologists and the lowest ALD-related mortality, whereas the Mountain states had the lowest concentration of gastroenterologists and the highest ALD-related mortality.
The lowest mortality related to ALD was in New Jersey, Maryland, and Hawaii, with 52 per 1,000,000 people, and the highest was in Wyoming, with 289.
Study shines spotlight on general GI care
Access to liver transplants did not make a statistically significant difference in mortality from ALD.
“It makes you realize that transplant will only be accessible for really just a small fraction of the population who needs it,” Dr. Lee told this news organization.
General gastroenterologic care appears to make a bigger difference in saving patients’ lives. “Are they getting endoscopy for bleeding from varices?” Dr. Lee asked. “Are they getting appropriate antibiotics prescribed to prevent bacterial infection of ascites?”
The concentration of primary care physicians did not reduce mortality from ALD, and neither did the concentration of substance use, behavioral disorder, and mental health counselors.
Previous research has shown that substance abuse therapy is effective. But many people do not want to undertake it, or they face barriers of transportation, language, or insurance, said Dr. Lee.
“I have many patients whose insurance will provide them access to medical visits to me but will not to substance-use rehab, for example,” he said.
To see whether the effect was more generally due to the concentration of medical specialists, the researchers examined the state-level density of ophthalmologists and dermatologists. They found no significant difference in ALD-related mortality.
The finding builds on reports by the American Gastroenterological Association and the American Association for the Study of Liver Diseases that the number of gastroenterologists has not kept up with the U.S. population nor the burden of digestive diseases, and that predicts a critical shortage in the future.
Overcoming barriers to care for liver disease
The overall supply of gastroenterologists could be increased by reducing the educational requirements and increasing the funding for fellowships, said Dr. Lee.
“We have to have a better understanding as to the barriers to gastroenterology practice in certain areas, then interventions to address those barriers and also incentives to attract gastroenterologists to those areas,” Dr. Lee said.
The study underscores the importance of access to gastroenterological care, said George Cholankeril, MD, assistant professor of medicine at Baylor College of Medicine, Houston, who was not involved in the study. That urgency has only grown as ALD has spiraled up with the COVID-19 pandemic, he said.
“Anyone in clinical practice right now will be able to say that there’s been a clear rising tide of patients with alcohol-related liver disease,” he told this news organization. “There’s an urgent need to address this and provide the necessary resources.”
Prevention remains essential, Dr. Cholankeril said.
Gastroenterologists and primary care physicians can help stem the tide of ALD by screening their patients for the disease through a tool like AUDIT (Alcohol Use Disorders Identification Test), he said. They can then refer patients to substance abuse treatment centers or to psychologists and psychiatrists.
Dr. Lee and Dr. Cholankeril report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People are more likely to die of alcohol-associated liver disease (ALD) when there are fewer gastroenterologists in their state, researchers say.
The finding raises questions about steps that policymakers could take to increase the number of gastroenterologists and spread them more evenly around the United States.
“We found that there’s a fivefold difference in density of gastroenterologists through different states,” said Brian P. Lee, MD, MAS, an assistant professor of clinical medicine at the University of Southern California, Los Angeles.
Dr. Lee and colleagues published their findings in Clinical Gastroenterology and Hepatology.
ALD is becoming more common, and it is killing more people. Research among veterans has linked visits to gastroenterologists to a lower risk for death from liver disease.
To see whether that correlation applies more broadly, Dr. Lee and colleagues compared multiple datasets. One from the U.S. Health Resources & Service Administration provided the number of gastroenterologists per 100,000 population. The other from the U.S. Centers for Disease Control and Prevention provided ALD-related deaths per 1,000,000 adults for each state and the District of Columbia.
The researchers adjusted for many variables that could affect the relationship between the availability of gastroenterologists and deaths related to ALD, including the age distribution of the population in each state, the gender balance, race and ethnicity, binge drinking, household income, obesity, and the proportion of rural residents.
They found that for every additional gastroenterologist, there is almost one fewer ALD-related death each year per 100,000 population (9.0 [95% confidence interval, 1.3-16.7] fewer ALD-related deaths per 1,000,000 population for each additional gastroenterologist per 100,000 population).
The strength of the association appeared to plateau when there were at least 7.5 gastroenterologists per 100,000 people.
From these findings, the researchers calculated that as many as 40% of deaths from ALD nationwide could be prevented by providing more gastroenterologists in the places where they are lacking.
The mean number of gastroenterologists per 100,000 people in the United States was 4.6, and the annual ALD-related death rate was 85.6 per 1,000,000 people.
The Atlantic states had the greatest concentration of gastroenterologists and the lowest ALD-related mortality, whereas the Mountain states had the lowest concentration of gastroenterologists and the highest ALD-related mortality.
The lowest mortality related to ALD was in New Jersey, Maryland, and Hawaii, with 52 per 1,000,000 people, and the highest was in Wyoming, with 289.
Study shines spotlight on general GI care
Access to liver transplants did not make a statistically significant difference in mortality from ALD.
“It makes you realize that transplant will only be accessible for really just a small fraction of the population who needs it,” Dr. Lee told this news organization.
General gastroenterologic care appears to make a bigger difference in saving patients’ lives. “Are they getting endoscopy for bleeding from varices?” Dr. Lee asked. “Are they getting appropriate antibiotics prescribed to prevent bacterial infection of ascites?”
The concentration of primary care physicians did not reduce mortality from ALD, and neither did the concentration of substance use, behavioral disorder, and mental health counselors.
Previous research has shown that substance abuse therapy is effective. But many people do not want to undertake it, or they face barriers of transportation, language, or insurance, said Dr. Lee.
“I have many patients whose insurance will provide them access to medical visits to me but will not to substance-use rehab, for example,” he said.
To see whether the effect was more generally due to the concentration of medical specialists, the researchers examined the state-level density of ophthalmologists and dermatologists. They found no significant difference in ALD-related mortality.
The finding builds on reports by the American Gastroenterological Association and the American Association for the Study of Liver Diseases that the number of gastroenterologists has not kept up with the U.S. population nor the burden of digestive diseases, and that predicts a critical shortage in the future.
Overcoming barriers to care for liver disease
The overall supply of gastroenterologists could be increased by reducing the educational requirements and increasing the funding for fellowships, said Dr. Lee.
“We have to have a better understanding as to the barriers to gastroenterology practice in certain areas, then interventions to address those barriers and also incentives to attract gastroenterologists to those areas,” Dr. Lee said.
The study underscores the importance of access to gastroenterological care, said George Cholankeril, MD, assistant professor of medicine at Baylor College of Medicine, Houston, who was not involved in the study. That urgency has only grown as ALD has spiraled up with the COVID-19 pandemic, he said.
“Anyone in clinical practice right now will be able to say that there’s been a clear rising tide of patients with alcohol-related liver disease,” he told this news organization. “There’s an urgent need to address this and provide the necessary resources.”
Prevention remains essential, Dr. Cholankeril said.
Gastroenterologists and primary care physicians can help stem the tide of ALD by screening their patients for the disease through a tool like AUDIT (Alcohol Use Disorders Identification Test), he said. They can then refer patients to substance abuse treatment centers or to psychologists and psychiatrists.
Dr. Lee and Dr. Cholankeril report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Gene variants found to protect against liver disease
Rare gene variants are associated with a reduced risk for multiple types of liver disease, including cirrhosis, researchers say.
People with certain variants in the gene CIDEB are one-third less likely to develop any sort of liver disease, according to Aris Baras, MD, a senior vice president at Regeneron, and colleagues.
“The unprecedented protective effect that these CIDEB genetic variants have against liver disease provides us with one of our most exciting targets and potential therapeutic approaches for a notoriously hard-to-treat disease where there are currently no approved treatments,” said Dr. Baras in a press release.
Dr. Baras and colleagues published the finding in The New England Journal of Medicine.
The finding follows on a similar discovery about a common variant in the gene HSD17B13. Treatments targeting this gene are being tested in clinical trials.
To search for more such genes, the researchers analyzed human exomes – the part of the genome that codes for proteins – to look for associations between gene variants and liver function.
The researchers used exome sequencing on 542,904 people from the UK Biobank, the Geisinger Health System MyCode cohort, and other datasets.
They found that coding variants in APOB, ABCB4, SLC30A10, and TM6SF2 were associated with increased aminotransferase levels and an increased risk for liver disease.
But variants in CIDEB were associated with decreased levels of alanine aminotransferase, a biomarker of hepatocellular injury. And they were associated with a decreased risk for liver disease of any cause (odds ratio per allele, 0.67; 95% confidence interval, 0.57-0.79).
The CIDEB variants were present in only 0.7% of the persons in the study.
Zeroing in on various kinds of liver disease, the researchers found that the CIDEB variants were associated with a reduced risk for alcoholic liver disease, nonalcoholic liver disease, any liver cirrhosis, alcoholic liver cirrhosis, nonalcoholic liver cirrhosis, and viral hepatitis.
In 3,599 patients who had undergone bariatric surgery, variants in CIDEB were associated with a reduced nonalcoholic fatty liver disease activity score of –0.98 beta per allele in score units, where scores range from 0-8, with a higher score indicating more severe disease.
In patients for whom MRI data were available, those with rare coding variants in CIDEB had lower proportions of liver fat. However, percentage of liver fat did not fully explain the reduced risk for liver disease.
Pursuing another line of investigation, the researchers found that they could prevent the buildup of large lipid droplets in oleic acid-treated human hepatoma cell lines by silencing the CIDEB gene using small interfering RNA.
The association was particularly strong among people with higher body mass indices and type 2 diabetes.
The associations with the rare protective CIDEB variants were consistent across ancestries, but people of non-European ancestry, who might be disproportionately affected by liver disease, were underrepresented in the database, the researchers note.
The study was supported by Regeneron Pharmaceuticals, which also employed several of the researchers.
A version of this article first appeared on Medscape.com.
Rare gene variants are associated with a reduced risk for multiple types of liver disease, including cirrhosis, researchers say.
People with certain variants in the gene CIDEB are one-third less likely to develop any sort of liver disease, according to Aris Baras, MD, a senior vice president at Regeneron, and colleagues.
“The unprecedented protective effect that these CIDEB genetic variants have against liver disease provides us with one of our most exciting targets and potential therapeutic approaches for a notoriously hard-to-treat disease where there are currently no approved treatments,” said Dr. Baras in a press release.
Dr. Baras and colleagues published the finding in The New England Journal of Medicine.
The finding follows on a similar discovery about a common variant in the gene HSD17B13. Treatments targeting this gene are being tested in clinical trials.
To search for more such genes, the researchers analyzed human exomes – the part of the genome that codes for proteins – to look for associations between gene variants and liver function.
The researchers used exome sequencing on 542,904 people from the UK Biobank, the Geisinger Health System MyCode cohort, and other datasets.
They found that coding variants in APOB, ABCB4, SLC30A10, and TM6SF2 were associated with increased aminotransferase levels and an increased risk for liver disease.
But variants in CIDEB were associated with decreased levels of alanine aminotransferase, a biomarker of hepatocellular injury. And they were associated with a decreased risk for liver disease of any cause (odds ratio per allele, 0.67; 95% confidence interval, 0.57-0.79).
The CIDEB variants were present in only 0.7% of the persons in the study.
Zeroing in on various kinds of liver disease, the researchers found that the CIDEB variants were associated with a reduced risk for alcoholic liver disease, nonalcoholic liver disease, any liver cirrhosis, alcoholic liver cirrhosis, nonalcoholic liver cirrhosis, and viral hepatitis.
In 3,599 patients who had undergone bariatric surgery, variants in CIDEB were associated with a reduced nonalcoholic fatty liver disease activity score of –0.98 beta per allele in score units, where scores range from 0-8, with a higher score indicating more severe disease.
In patients for whom MRI data were available, those with rare coding variants in CIDEB had lower proportions of liver fat. However, percentage of liver fat did not fully explain the reduced risk for liver disease.
Pursuing another line of investigation, the researchers found that they could prevent the buildup of large lipid droplets in oleic acid-treated human hepatoma cell lines by silencing the CIDEB gene using small interfering RNA.
The association was particularly strong among people with higher body mass indices and type 2 diabetes.
The associations with the rare protective CIDEB variants were consistent across ancestries, but people of non-European ancestry, who might be disproportionately affected by liver disease, were underrepresented in the database, the researchers note.
The study was supported by Regeneron Pharmaceuticals, which also employed several of the researchers.
A version of this article first appeared on Medscape.com.
Rare gene variants are associated with a reduced risk for multiple types of liver disease, including cirrhosis, researchers say.
People with certain variants in the gene CIDEB are one-third less likely to develop any sort of liver disease, according to Aris Baras, MD, a senior vice president at Regeneron, and colleagues.
“The unprecedented protective effect that these CIDEB genetic variants have against liver disease provides us with one of our most exciting targets and potential therapeutic approaches for a notoriously hard-to-treat disease where there are currently no approved treatments,” said Dr. Baras in a press release.
Dr. Baras and colleagues published the finding in The New England Journal of Medicine.
The finding follows on a similar discovery about a common variant in the gene HSD17B13. Treatments targeting this gene are being tested in clinical trials.
To search for more such genes, the researchers analyzed human exomes – the part of the genome that codes for proteins – to look for associations between gene variants and liver function.
The researchers used exome sequencing on 542,904 people from the UK Biobank, the Geisinger Health System MyCode cohort, and other datasets.
They found that coding variants in APOB, ABCB4, SLC30A10, and TM6SF2 were associated with increased aminotransferase levels and an increased risk for liver disease.
But variants in CIDEB were associated with decreased levels of alanine aminotransferase, a biomarker of hepatocellular injury. And they were associated with a decreased risk for liver disease of any cause (odds ratio per allele, 0.67; 95% confidence interval, 0.57-0.79).
The CIDEB variants were present in only 0.7% of the persons in the study.
Zeroing in on various kinds of liver disease, the researchers found that the CIDEB variants were associated with a reduced risk for alcoholic liver disease, nonalcoholic liver disease, any liver cirrhosis, alcoholic liver cirrhosis, nonalcoholic liver cirrhosis, and viral hepatitis.
In 3,599 patients who had undergone bariatric surgery, variants in CIDEB were associated with a reduced nonalcoholic fatty liver disease activity score of –0.98 beta per allele in score units, where scores range from 0-8, with a higher score indicating more severe disease.
In patients for whom MRI data were available, those with rare coding variants in CIDEB had lower proportions of liver fat. However, percentage of liver fat did not fully explain the reduced risk for liver disease.
Pursuing another line of investigation, the researchers found that they could prevent the buildup of large lipid droplets in oleic acid-treated human hepatoma cell lines by silencing the CIDEB gene using small interfering RNA.
The association was particularly strong among people with higher body mass indices and type 2 diabetes.
The associations with the rare protective CIDEB variants were consistent across ancestries, but people of non-European ancestry, who might be disproportionately affected by liver disease, were underrepresented in the database, the researchers note.
The study was supported by Regeneron Pharmaceuticals, which also employed several of the researchers.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
COVID-19 may trigger irritable bowel syndrome
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Low urate limits for gout questioned in study
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
FROM ARTHRITIS & RHEUMATOLOGY
Artificial intelligence colonoscopy system shows promise
A new artificial intelligence (AI) system can help expert endoscopists improve their colonoscopies, a new study indicates.
Endoscopists using the computer program SKOUT (Iterative Scopes) achieved a 27% better detection rate of adenomas per colonoscopy, compared with endoscopists working without computer assistance, said lead author Aasma Shaukat, MD, MPH, director of outcomes research in the division of gastroenterology and hepatology at New York University.
The study showed that AI colonoscopy systems can work in a routine population of U.S. patients, Dr. Shaukat said in an interview.
“As gastroenterologists, we are very excited,” she said.
The study was published online in Gastroenterology and was presented at the annual Digestive Disease® Week.
Previous research has shown that experienced endoscopists miss many polyps. To improve their detection rate, multiple companies have used machine learning to develop algorithms to identify suspicious areas.
“Once the computer sees the polyp, it puts a bounding box around it,” said Dr. Shaukat. “It draws the attention of the endoscopist to it. It assists the endoscopist but doesn’t replace the endoscopist.”
The Food and Drug Administration has approved two such systems: EndoScreener (Wision AI) and GI Genius (Cosmo Pharmaceuticals).
The SKOUT algorithm was trained on 3,616 full-length colonoscopy procedure videos from multiple centers. In bench testing, it achieved a 93.5% polyp-level true positive rate and a 2.3% false positive rate.
Randomized trial pits AI against standard procedure
To see how well the system works in the clinic, Dr. Shaukat and colleagues recruited 22 U.S. board-certified gastroenterologists from five academic and community centers. The gastroenterologists all had a minimum adenoma detection rate of 25%, defined as the number of colonoscopies in which at least one adenoma is found, divided by the number of colonoscopies performed. All the gastroenterologists had performed a minimum of 1,000 colonoscopy procedures.
The researchers randomly assigned 682 patients to undergo colonoscopy with the SKOUT and 677 to undergo colonoscopy using the standard procedure. The patients were aged 40 years or older and were scheduled for either screening or surveillance.
The endoscopists who received computer assistance detected 1.05 adenomas per colonoscopy versus 0.83 for those who did not have computer assistance, a statistically significant difference.
The proportion of resections with clinically significant histology was 71.7% with standard colonoscopies versus 67.4% with computer-assisted colonoscopies. This fell within the 14% margin that the researchers had set to show noninferiority for the computer system.
“The important thing is not just detecting all polyps but the polyps we care about, which are adenomas, and doing so without increasing the false positive rate,” said Dr. Shaukat.
The adenoma detection rate was 43.9% for the standard procedure and 47.8% for the computer-assisted procedure. This difference was not statistically significant, but Dr. Shaukat argued that the adenoma detection rate is not the best measure of success, because endoscopists sometimes stop looking for polyps once they find one.
The overall sessile serrated lesion detection rate for the standard colonoscopies was 16.0% versus 12.6% for the computer-assisted colonoscopies, which also was not statistically significant.
Next steps
This study is important because it was a large, multicenter trial in the United States, said Omer Ahmad, BSc, MBBS, MRCP, a gastroenterologist and clinical researcher at University College London, who was not involved in the study. Most of the trials of AI have been in China or Europe. “It was very important just to see this replicated in the U.S. population.”
The average procedure time was 15.41 minutes for the standard colonoscopies versus 15.82 minutes for the computer-assisted colonoscopies, which was not statistically different.
“It is important to note that the studies so far suggest that false positives do not have a significant impact on workflow,” said Dr. Ahmad.
The next crucial step in evaluating AI colonoscopy will be to track the effects over the long term, said Dr. Shaukat.
“As these technologies get approved and we see them in practice, we need to see that it’s leading to some outcome, like reduced colon cancer,” she said.
That also may be necessary before payers in the United States are willing to pay the additional cost for this technology, she added.
In the meantime, Dr. Ahmad said computer assistance is improving his own colonoscopies.
“I have found the systems have spotted some polyps that I may have otherwise missed,” he said. “There is a false positive rate, but for me, it doesn’t distract from my workflow.”
He believes the systems will be particularly helpful in improving the performance of less-skilled endoscopists.
He is also looking forward to systems that can help complete the reports needed at the end of each colonoscopy. “Most of us dislike having to write a laborious report and having to code everything at the end of the procedure,” he said.
The study was funded by Iterative Scopes. Dr. Shaukat reported having received research funding to her institution for the current study from Iterative Scopes and consulting fees from Freenome and Medtronic. Dr. Ahmad reports receiving speaker fees from the Canadian Association of Gastroenterology/Medtronic.
A version of this article first appeared on Medscape.com.
A new artificial intelligence (AI) system can help expert endoscopists improve their colonoscopies, a new study indicates.
Endoscopists using the computer program SKOUT (Iterative Scopes) achieved a 27% better detection rate of adenomas per colonoscopy, compared with endoscopists working without computer assistance, said lead author Aasma Shaukat, MD, MPH, director of outcomes research in the division of gastroenterology and hepatology at New York University.
The study showed that AI colonoscopy systems can work in a routine population of U.S. patients, Dr. Shaukat said in an interview.
“As gastroenterologists, we are very excited,” she said.
The study was published online in Gastroenterology and was presented at the annual Digestive Disease® Week.
Previous research has shown that experienced endoscopists miss many polyps. To improve their detection rate, multiple companies have used machine learning to develop algorithms to identify suspicious areas.
“Once the computer sees the polyp, it puts a bounding box around it,” said Dr. Shaukat. “It draws the attention of the endoscopist to it. It assists the endoscopist but doesn’t replace the endoscopist.”
The Food and Drug Administration has approved two such systems: EndoScreener (Wision AI) and GI Genius (Cosmo Pharmaceuticals).
The SKOUT algorithm was trained on 3,616 full-length colonoscopy procedure videos from multiple centers. In bench testing, it achieved a 93.5% polyp-level true positive rate and a 2.3% false positive rate.
Randomized trial pits AI against standard procedure
To see how well the system works in the clinic, Dr. Shaukat and colleagues recruited 22 U.S. board-certified gastroenterologists from five academic and community centers. The gastroenterologists all had a minimum adenoma detection rate of 25%, defined as the number of colonoscopies in which at least one adenoma is found, divided by the number of colonoscopies performed. All the gastroenterologists had performed a minimum of 1,000 colonoscopy procedures.
The researchers randomly assigned 682 patients to undergo colonoscopy with the SKOUT and 677 to undergo colonoscopy using the standard procedure. The patients were aged 40 years or older and were scheduled for either screening or surveillance.
The endoscopists who received computer assistance detected 1.05 adenomas per colonoscopy versus 0.83 for those who did not have computer assistance, a statistically significant difference.
The proportion of resections with clinically significant histology was 71.7% with standard colonoscopies versus 67.4% with computer-assisted colonoscopies. This fell within the 14% margin that the researchers had set to show noninferiority for the computer system.
“The important thing is not just detecting all polyps but the polyps we care about, which are adenomas, and doing so without increasing the false positive rate,” said Dr. Shaukat.
The adenoma detection rate was 43.9% for the standard procedure and 47.8% for the computer-assisted procedure. This difference was not statistically significant, but Dr. Shaukat argued that the adenoma detection rate is not the best measure of success, because endoscopists sometimes stop looking for polyps once they find one.
The overall sessile serrated lesion detection rate for the standard colonoscopies was 16.0% versus 12.6% for the computer-assisted colonoscopies, which also was not statistically significant.
Next steps
This study is important because it was a large, multicenter trial in the United States, said Omer Ahmad, BSc, MBBS, MRCP, a gastroenterologist and clinical researcher at University College London, who was not involved in the study. Most of the trials of AI have been in China or Europe. “It was very important just to see this replicated in the U.S. population.”
The average procedure time was 15.41 minutes for the standard colonoscopies versus 15.82 minutes for the computer-assisted colonoscopies, which was not statistically different.
“It is important to note that the studies so far suggest that false positives do not have a significant impact on workflow,” said Dr. Ahmad.
The next crucial step in evaluating AI colonoscopy will be to track the effects over the long term, said Dr. Shaukat.
“As these technologies get approved and we see them in practice, we need to see that it’s leading to some outcome, like reduced colon cancer,” she said.
That also may be necessary before payers in the United States are willing to pay the additional cost for this technology, she added.
In the meantime, Dr. Ahmad said computer assistance is improving his own colonoscopies.
“I have found the systems have spotted some polyps that I may have otherwise missed,” he said. “There is a false positive rate, but for me, it doesn’t distract from my workflow.”
He believes the systems will be particularly helpful in improving the performance of less-skilled endoscopists.
He is also looking forward to systems that can help complete the reports needed at the end of each colonoscopy. “Most of us dislike having to write a laborious report and having to code everything at the end of the procedure,” he said.
The study was funded by Iterative Scopes. Dr. Shaukat reported having received research funding to her institution for the current study from Iterative Scopes and consulting fees from Freenome and Medtronic. Dr. Ahmad reports receiving speaker fees from the Canadian Association of Gastroenterology/Medtronic.
A version of this article first appeared on Medscape.com.
A new artificial intelligence (AI) system can help expert endoscopists improve their colonoscopies, a new study indicates.
Endoscopists using the computer program SKOUT (Iterative Scopes) achieved a 27% better detection rate of adenomas per colonoscopy, compared with endoscopists working without computer assistance, said lead author Aasma Shaukat, MD, MPH, director of outcomes research in the division of gastroenterology and hepatology at New York University.
The study showed that AI colonoscopy systems can work in a routine population of U.S. patients, Dr. Shaukat said in an interview.
“As gastroenterologists, we are very excited,” she said.
The study was published online in Gastroenterology and was presented at the annual Digestive Disease® Week.
Previous research has shown that experienced endoscopists miss many polyps. To improve their detection rate, multiple companies have used machine learning to develop algorithms to identify suspicious areas.
“Once the computer sees the polyp, it puts a bounding box around it,” said Dr. Shaukat. “It draws the attention of the endoscopist to it. It assists the endoscopist but doesn’t replace the endoscopist.”
The Food and Drug Administration has approved two such systems: EndoScreener (Wision AI) and GI Genius (Cosmo Pharmaceuticals).
The SKOUT algorithm was trained on 3,616 full-length colonoscopy procedure videos from multiple centers. In bench testing, it achieved a 93.5% polyp-level true positive rate and a 2.3% false positive rate.
Randomized trial pits AI against standard procedure
To see how well the system works in the clinic, Dr. Shaukat and colleagues recruited 22 U.S. board-certified gastroenterologists from five academic and community centers. The gastroenterologists all had a minimum adenoma detection rate of 25%, defined as the number of colonoscopies in which at least one adenoma is found, divided by the number of colonoscopies performed. All the gastroenterologists had performed a minimum of 1,000 colonoscopy procedures.
The researchers randomly assigned 682 patients to undergo colonoscopy with the SKOUT and 677 to undergo colonoscopy using the standard procedure. The patients were aged 40 years or older and were scheduled for either screening or surveillance.
The endoscopists who received computer assistance detected 1.05 adenomas per colonoscopy versus 0.83 for those who did not have computer assistance, a statistically significant difference.
The proportion of resections with clinically significant histology was 71.7% with standard colonoscopies versus 67.4% with computer-assisted colonoscopies. This fell within the 14% margin that the researchers had set to show noninferiority for the computer system.
“The important thing is not just detecting all polyps but the polyps we care about, which are adenomas, and doing so without increasing the false positive rate,” said Dr. Shaukat.
The adenoma detection rate was 43.9% for the standard procedure and 47.8% for the computer-assisted procedure. This difference was not statistically significant, but Dr. Shaukat argued that the adenoma detection rate is not the best measure of success, because endoscopists sometimes stop looking for polyps once they find one.
The overall sessile serrated lesion detection rate for the standard colonoscopies was 16.0% versus 12.6% for the computer-assisted colonoscopies, which also was not statistically significant.
Next steps
This study is important because it was a large, multicenter trial in the United States, said Omer Ahmad, BSc, MBBS, MRCP, a gastroenterologist and clinical researcher at University College London, who was not involved in the study. Most of the trials of AI have been in China or Europe. “It was very important just to see this replicated in the U.S. population.”
The average procedure time was 15.41 minutes for the standard colonoscopies versus 15.82 minutes for the computer-assisted colonoscopies, which was not statistically different.
“It is important to note that the studies so far suggest that false positives do not have a significant impact on workflow,” said Dr. Ahmad.
The next crucial step in evaluating AI colonoscopy will be to track the effects over the long term, said Dr. Shaukat.
“As these technologies get approved and we see them in practice, we need to see that it’s leading to some outcome, like reduced colon cancer,” she said.
That also may be necessary before payers in the United States are willing to pay the additional cost for this technology, she added.
In the meantime, Dr. Ahmad said computer assistance is improving his own colonoscopies.
“I have found the systems have spotted some polyps that I may have otherwise missed,” he said. “There is a false positive rate, but for me, it doesn’t distract from my workflow.”
He believes the systems will be particularly helpful in improving the performance of less-skilled endoscopists.
He is also looking forward to systems that can help complete the reports needed at the end of each colonoscopy. “Most of us dislike having to write a laborious report and having to code everything at the end of the procedure,” he said.
The study was funded by Iterative Scopes. Dr. Shaukat reported having received research funding to her institution for the current study from Iterative Scopes and consulting fees from Freenome and Medtronic. Dr. Ahmad reports receiving speaker fees from the Canadian Association of Gastroenterology/Medtronic.
A version of this article first appeared on Medscape.com.
Psychological intervention looks promising in Crohn’s disease
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.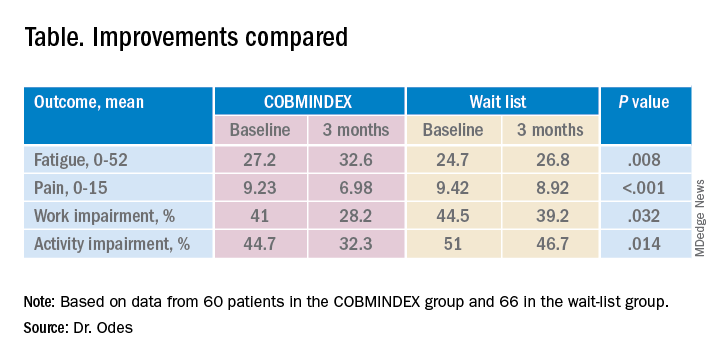
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.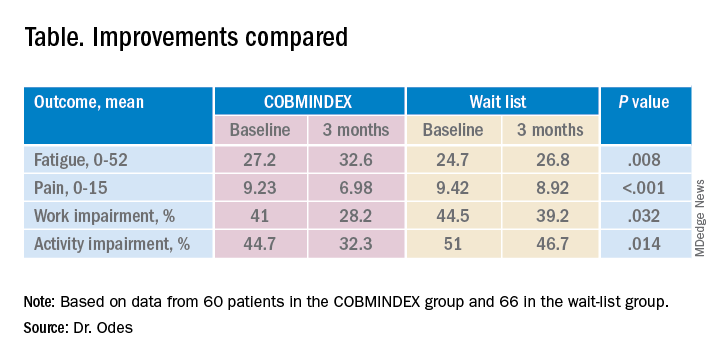
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.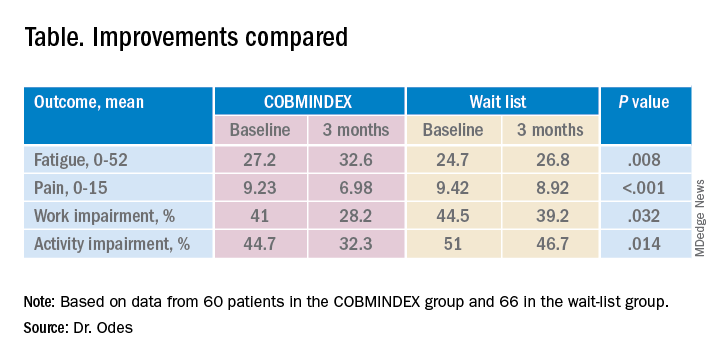
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
AT DDW 2022
Index cholecystectomy reduces readmissions after acute cholangitis
SAN DIEGO – Patients with acute cholangitis are twice as likely to be readmitted within 30 days if they don’t get a cholecystectomy in the same hospital admission for which they get biliary decompression, researchers say.
The readmissions result mostly from sepsis and recurrence of the acute cholangitis, said Ahmad Khan, MD, MS, a gastroenterology fellow at Case Western Reserve University in Cleveland, at Digestive Diseases Week® (DDW) 2022. “These added readmissions can cause a significant burden in terms of costs and extra days of hospitalization in these patients.”
Acute cholangitis in patients without bile duct stents is most often caused by biliary calculi, benign biliary stricture, or malignancy. A gastrointestinal emergency, it requires treatment with biliary decompression followed by cholecystectomy, but the cholecystectomy is considered an elective procedure.
Surgeons may delay it if the patient is very sick, or simply for scheduling reasons, Dr. Khan said. “There are some areas where the surgeons may be too busy,” he said. Or if the patient first presents at the end of the week, some surgeons will send the patient home so they don’t have to operate on the weekend, he said.
To understand the consequences of these decisions, Dr. Khan and his colleagues analyzed data from 2016 to 2018 from the National Readmission Database of the U.S. Agency for Healthcare Research and Quality.
They found that 11% of patients who went home before returning for a cholecystectomy had to be readmitted versus only 5.5% of those who got a cholecystectomy during the same (index) admission as their biliary decompression.
Patients who got cholecystectomies during their index admissions were slightly younger and healthier: Their mean age was 67.29 years and 20.59% had three or more comorbidities at index admission versus 70.77 years of age and 39.80% with three or more comorbidities at index admission for those who got their cholecystectomies later.
The researchers did not find any significant differences in the hospitals’ characteristics, such as being urban or academic, between the two groups.
Mortality was higher for those who received their cholecystectomy after returning home, but they spent less time in the hospital at lower total cost. The differences in outcomes between the index admission and readmission were all statistically significant (P < .01).
This observational study could not determine cause and effect, but it justifies a prospective trial that could more definitely determine which approach results in better outcomes, Dr. Khan said.
That patients are less likely to need readmission if they return home without a gall bladder after treatment for acute cholangitis “makes sense,” said session comoderator Richard Sterling, MD, MSc, chief of hepatology at Virginia Commonwealth University in Richmond.
“Should you do it immediately or can you wait a day or 2? They didn’t really address when during that admission, so we still don’t know the optimal sequence of events.”
If a patient has so many comorbidities that the surgeon and anesthesiologist don’t think the patient could survive a cholecystectomy, then the surgeon might do a cholecystostomy instead, he said.
Dr. Khan said he hopes to delve deeper into the data to determine what factors might have influenced the surgeons’ decisions to delay the cholecystectomy. “I want to see, of the patients who did not get same-admission cholecystectomies, how many had diabetes, how many had coronary artery disease, how many were on blood thinners, and things like that.”
Neither Dr. Khan nor Dr. Sterling reported any relevant financial interests.
SAN DIEGO – Patients with acute cholangitis are twice as likely to be readmitted within 30 days if they don’t get a cholecystectomy in the same hospital admission for which they get biliary decompression, researchers say.
The readmissions result mostly from sepsis and recurrence of the acute cholangitis, said Ahmad Khan, MD, MS, a gastroenterology fellow at Case Western Reserve University in Cleveland, at Digestive Diseases Week® (DDW) 2022. “These added readmissions can cause a significant burden in terms of costs and extra days of hospitalization in these patients.”
Acute cholangitis in patients without bile duct stents is most often caused by biliary calculi, benign biliary stricture, or malignancy. A gastrointestinal emergency, it requires treatment with biliary decompression followed by cholecystectomy, but the cholecystectomy is considered an elective procedure.
Surgeons may delay it if the patient is very sick, or simply for scheduling reasons, Dr. Khan said. “There are some areas where the surgeons may be too busy,” he said. Or if the patient first presents at the end of the week, some surgeons will send the patient home so they don’t have to operate on the weekend, he said.
To understand the consequences of these decisions, Dr. Khan and his colleagues analyzed data from 2016 to 2018 from the National Readmission Database of the U.S. Agency for Healthcare Research and Quality.
They found that 11% of patients who went home before returning for a cholecystectomy had to be readmitted versus only 5.5% of those who got a cholecystectomy during the same (index) admission as their biliary decompression.
Patients who got cholecystectomies during their index admissions were slightly younger and healthier: Their mean age was 67.29 years and 20.59% had three or more comorbidities at index admission versus 70.77 years of age and 39.80% with three or more comorbidities at index admission for those who got their cholecystectomies later.
The researchers did not find any significant differences in the hospitals’ characteristics, such as being urban or academic, between the two groups.
Mortality was higher for those who received their cholecystectomy after returning home, but they spent less time in the hospital at lower total cost. The differences in outcomes between the index admission and readmission were all statistically significant (P < .01).
This observational study could not determine cause and effect, but it justifies a prospective trial that could more definitely determine which approach results in better outcomes, Dr. Khan said.
That patients are less likely to need readmission if they return home without a gall bladder after treatment for acute cholangitis “makes sense,” said session comoderator Richard Sterling, MD, MSc, chief of hepatology at Virginia Commonwealth University in Richmond.
“Should you do it immediately or can you wait a day or 2? They didn’t really address when during that admission, so we still don’t know the optimal sequence of events.”
If a patient has so many comorbidities that the surgeon and anesthesiologist don’t think the patient could survive a cholecystectomy, then the surgeon might do a cholecystostomy instead, he said.
Dr. Khan said he hopes to delve deeper into the data to determine what factors might have influenced the surgeons’ decisions to delay the cholecystectomy. “I want to see, of the patients who did not get same-admission cholecystectomies, how many had diabetes, how many had coronary artery disease, how many were on blood thinners, and things like that.”
Neither Dr. Khan nor Dr. Sterling reported any relevant financial interests.
SAN DIEGO – Patients with acute cholangitis are twice as likely to be readmitted within 30 days if they don’t get a cholecystectomy in the same hospital admission for which they get biliary decompression, researchers say.
The readmissions result mostly from sepsis and recurrence of the acute cholangitis, said Ahmad Khan, MD, MS, a gastroenterology fellow at Case Western Reserve University in Cleveland, at Digestive Diseases Week® (DDW) 2022. “These added readmissions can cause a significant burden in terms of costs and extra days of hospitalization in these patients.”
Acute cholangitis in patients without bile duct stents is most often caused by biliary calculi, benign biliary stricture, or malignancy. A gastrointestinal emergency, it requires treatment with biliary decompression followed by cholecystectomy, but the cholecystectomy is considered an elective procedure.
Surgeons may delay it if the patient is very sick, or simply for scheduling reasons, Dr. Khan said. “There are some areas where the surgeons may be too busy,” he said. Or if the patient first presents at the end of the week, some surgeons will send the patient home so they don’t have to operate on the weekend, he said.
To understand the consequences of these decisions, Dr. Khan and his colleagues analyzed data from 2016 to 2018 from the National Readmission Database of the U.S. Agency for Healthcare Research and Quality.
They found that 11% of patients who went home before returning for a cholecystectomy had to be readmitted versus only 5.5% of those who got a cholecystectomy during the same (index) admission as their biliary decompression.
Patients who got cholecystectomies during their index admissions were slightly younger and healthier: Their mean age was 67.29 years and 20.59% had three or more comorbidities at index admission versus 70.77 years of age and 39.80% with three or more comorbidities at index admission for those who got their cholecystectomies later.
The researchers did not find any significant differences in the hospitals’ characteristics, such as being urban or academic, between the two groups.
Mortality was higher for those who received their cholecystectomy after returning home, but they spent less time in the hospital at lower total cost. The differences in outcomes between the index admission and readmission were all statistically significant (P < .01).
This observational study could not determine cause and effect, but it justifies a prospective trial that could more definitely determine which approach results in better outcomes, Dr. Khan said.
That patients are less likely to need readmission if they return home without a gall bladder after treatment for acute cholangitis “makes sense,” said session comoderator Richard Sterling, MD, MSc, chief of hepatology at Virginia Commonwealth University in Richmond.
“Should you do it immediately or can you wait a day or 2? They didn’t really address when during that admission, so we still don’t know the optimal sequence of events.”
If a patient has so many comorbidities that the surgeon and anesthesiologist don’t think the patient could survive a cholecystectomy, then the surgeon might do a cholecystostomy instead, he said.
Dr. Khan said he hopes to delve deeper into the data to determine what factors might have influenced the surgeons’ decisions to delay the cholecystectomy. “I want to see, of the patients who did not get same-admission cholecystectomies, how many had diabetes, how many had coronary artery disease, how many were on blood thinners, and things like that.”
Neither Dr. Khan nor Dr. Sterling reported any relevant financial interests.
AT DDW 2022
H. pylori antibiotics briefly disrupt gut microbiome
SAN DIEGO – Treatments to eradicate Helicobacter pylori (H. pylori) infections do increase the antibiotic resistance of the gut microbiota, but for only a few months, researchers reported at Digestive Disease Week® (DDW).
The finding applies similarly to levofloxacin quadruple therapy and bismuth quadruple therapy, both of which are equally efficacious as second-line treatments, said Jyh-Ming Liou, MD, PhD, clinical professor of internal medicine at National Taiwan University in Taipei.
This provides some reassurance that increased use of antibiotics to treat these infections won’t cause long-term disruptions to the patients’ microbiomes, said Dr. Liou.
“Maybe if we have indications for antibiotic treatment, then we don’t worry about the emergence of resistance in our bodies,” he said. “But the accumulation of antibodies in the environment may induce bacteria to mutate, so maybe we still need cautious use of antibiotics.”
H. pylori infections are becoming harder to treat as more strains develop resistance to antibiotics, leading physicians to use regimens with multiple agents. This in turn has raised concerns that gut microbiota could be disrupted, with pathogens potentially developing their own resistance.
To explore these risks, Dr. Liou and colleagues recruited adults whose H. pylori infections were not successfully eradicated.
They randomly assigned 280 patients each to one of two second-line therapies, levofloxacin quadruple or bismuth quadruple. At baseline, the researchers could not find any statistically significant differences in the two groups’ demographics, cigarette and alcohol use, or ulcers, as well as antibiotic resistance in patients’ microbiome between the groups.
Levofloxacin quadruple therapy consisted of esomeprazole 40 mg and amoxicillin 1 g for the first 7 days, followed by esomeprazole 40 mg, metronidazole 500 mg, and levofloxacin 250 mg for another 7 days (all twice daily).
Bismuth quadruple therapy consisted of esomeprazole 40 mg twice daily, bismuth tripotassium dicitrate 300 mg four times a day, tetracycline 500 mg four times a day, and metronidazole 500 mg three times a day, for 10 days.
The researchers collected stool samples at baseline, week 2, week 8, and 1 year after eradication therapy and analyzed them for microbiota diversity and antibiotic susceptibility.
The H. pylori eradication rates were almost the same in the two second-line therapies: 87.9% for levofloxacin quadruple and 87.5% for bismuth quadruple. When they were used as third-line (rescue) therapies, the success rates were also statistically the same, and the cumulative second-line and third-line eradication rate was 95.6% for levofloxacin quadruple and 96.6% for bismuth quadruple.
The two treatments did differ in adverse events with 48.4% for levofloxacin quadruple and 77.3% for bismuth quadruple, which was statistically significant (P < .0001).
After a year, H. pylori reinfected 2.5% of the levofloxacin group and 3% of the bismuth quadruple group.
The researchers used metagenomic sequencing to examine the bacteria in the patients’ microbiome for antibiotic resistance. Using 16S rRNA sequencing, they found that the proportion of genera and species with significant changes in abundance at 2 weeks after treatment compared with baseline was 52.4% for levofloxacin quadruple therapy versus 45.1% for bismuth quadruple therapy.
However, 8 weeks after treatment, the proportion with significant changes had dropped to 5.8% for the levofloxacin group and 21.5% for the bismuth group. And at the end of a year, they had further dropped to 0.9% for the levofloxacin group and 8.4% for the bismuth group.
“It was generally reassuring that, even after giving these combinations of different antibiotics, eventually it doesn’t seem to affect the resistance pattern in bacteria lower down in the gut,” said session moderator Steven Moss, MD, professor of medicine at Brown University in Providence, R.I.
Still, continuing to pile on more and more antibiotics to treat H. pylori infections won’t work forever because H. pylori strains are themselves developing resistance so rapidly, he said. “We’re certainly going to have worse eradications in the future unless we can come up with new tricks.”
A hopeful development are new techniques to test H. pylori for resistance to specific antibiotics before initiating treatment, said Dr. Moss.
Dr. Moss consults with companies developing H. pylori therapies and diagnostics. Dr. Liou reported no relevant financial interests.
SAN DIEGO – Treatments to eradicate Helicobacter pylori (H. pylori) infections do increase the antibiotic resistance of the gut microbiota, but for only a few months, researchers reported at Digestive Disease Week® (DDW).
The finding applies similarly to levofloxacin quadruple therapy and bismuth quadruple therapy, both of which are equally efficacious as second-line treatments, said Jyh-Ming Liou, MD, PhD, clinical professor of internal medicine at National Taiwan University in Taipei.
This provides some reassurance that increased use of antibiotics to treat these infections won’t cause long-term disruptions to the patients’ microbiomes, said Dr. Liou.
“Maybe if we have indications for antibiotic treatment, then we don’t worry about the emergence of resistance in our bodies,” he said. “But the accumulation of antibodies in the environment may induce bacteria to mutate, so maybe we still need cautious use of antibiotics.”
H. pylori infections are becoming harder to treat as more strains develop resistance to antibiotics, leading physicians to use regimens with multiple agents. This in turn has raised concerns that gut microbiota could be disrupted, with pathogens potentially developing their own resistance.
To explore these risks, Dr. Liou and colleagues recruited adults whose H. pylori infections were not successfully eradicated.
They randomly assigned 280 patients each to one of two second-line therapies, levofloxacin quadruple or bismuth quadruple. At baseline, the researchers could not find any statistically significant differences in the two groups’ demographics, cigarette and alcohol use, or ulcers, as well as antibiotic resistance in patients’ microbiome between the groups.
Levofloxacin quadruple therapy consisted of esomeprazole 40 mg and amoxicillin 1 g for the first 7 days, followed by esomeprazole 40 mg, metronidazole 500 mg, and levofloxacin 250 mg for another 7 days (all twice daily).
Bismuth quadruple therapy consisted of esomeprazole 40 mg twice daily, bismuth tripotassium dicitrate 300 mg four times a day, tetracycline 500 mg four times a day, and metronidazole 500 mg three times a day, for 10 days.
The researchers collected stool samples at baseline, week 2, week 8, and 1 year after eradication therapy and analyzed them for microbiota diversity and antibiotic susceptibility.
The H. pylori eradication rates were almost the same in the two second-line therapies: 87.9% for levofloxacin quadruple and 87.5% for bismuth quadruple. When they were used as third-line (rescue) therapies, the success rates were also statistically the same, and the cumulative second-line and third-line eradication rate was 95.6% for levofloxacin quadruple and 96.6% for bismuth quadruple.
The two treatments did differ in adverse events with 48.4% for levofloxacin quadruple and 77.3% for bismuth quadruple, which was statistically significant (P < .0001).
After a year, H. pylori reinfected 2.5% of the levofloxacin group and 3% of the bismuth quadruple group.
The researchers used metagenomic sequencing to examine the bacteria in the patients’ microbiome for antibiotic resistance. Using 16S rRNA sequencing, they found that the proportion of genera and species with significant changes in abundance at 2 weeks after treatment compared with baseline was 52.4% for levofloxacin quadruple therapy versus 45.1% for bismuth quadruple therapy.
However, 8 weeks after treatment, the proportion with significant changes had dropped to 5.8% for the levofloxacin group and 21.5% for the bismuth group. And at the end of a year, they had further dropped to 0.9% for the levofloxacin group and 8.4% for the bismuth group.
“It was generally reassuring that, even after giving these combinations of different antibiotics, eventually it doesn’t seem to affect the resistance pattern in bacteria lower down in the gut,” said session moderator Steven Moss, MD, professor of medicine at Brown University in Providence, R.I.
Still, continuing to pile on more and more antibiotics to treat H. pylori infections won’t work forever because H. pylori strains are themselves developing resistance so rapidly, he said. “We’re certainly going to have worse eradications in the future unless we can come up with new tricks.”
A hopeful development are new techniques to test H. pylori for resistance to specific antibiotics before initiating treatment, said Dr. Moss.
Dr. Moss consults with companies developing H. pylori therapies and diagnostics. Dr. Liou reported no relevant financial interests.
SAN DIEGO – Treatments to eradicate Helicobacter pylori (H. pylori) infections do increase the antibiotic resistance of the gut microbiota, but for only a few months, researchers reported at Digestive Disease Week® (DDW).
The finding applies similarly to levofloxacin quadruple therapy and bismuth quadruple therapy, both of which are equally efficacious as second-line treatments, said Jyh-Ming Liou, MD, PhD, clinical professor of internal medicine at National Taiwan University in Taipei.
This provides some reassurance that increased use of antibiotics to treat these infections won’t cause long-term disruptions to the patients’ microbiomes, said Dr. Liou.
“Maybe if we have indications for antibiotic treatment, then we don’t worry about the emergence of resistance in our bodies,” he said. “But the accumulation of antibodies in the environment may induce bacteria to mutate, so maybe we still need cautious use of antibiotics.”
H. pylori infections are becoming harder to treat as more strains develop resistance to antibiotics, leading physicians to use regimens with multiple agents. This in turn has raised concerns that gut microbiota could be disrupted, with pathogens potentially developing their own resistance.
To explore these risks, Dr. Liou and colleagues recruited adults whose H. pylori infections were not successfully eradicated.
They randomly assigned 280 patients each to one of two second-line therapies, levofloxacin quadruple or bismuth quadruple. At baseline, the researchers could not find any statistically significant differences in the two groups’ demographics, cigarette and alcohol use, or ulcers, as well as antibiotic resistance in patients’ microbiome between the groups.
Levofloxacin quadruple therapy consisted of esomeprazole 40 mg and amoxicillin 1 g for the first 7 days, followed by esomeprazole 40 mg, metronidazole 500 mg, and levofloxacin 250 mg for another 7 days (all twice daily).
Bismuth quadruple therapy consisted of esomeprazole 40 mg twice daily, bismuth tripotassium dicitrate 300 mg four times a day, tetracycline 500 mg four times a day, and metronidazole 500 mg three times a day, for 10 days.
The researchers collected stool samples at baseline, week 2, week 8, and 1 year after eradication therapy and analyzed them for microbiota diversity and antibiotic susceptibility.
The H. pylori eradication rates were almost the same in the two second-line therapies: 87.9% for levofloxacin quadruple and 87.5% for bismuth quadruple. When they were used as third-line (rescue) therapies, the success rates were also statistically the same, and the cumulative second-line and third-line eradication rate was 95.6% for levofloxacin quadruple and 96.6% for bismuth quadruple.
The two treatments did differ in adverse events with 48.4% for levofloxacin quadruple and 77.3% for bismuth quadruple, which was statistically significant (P < .0001).
After a year, H. pylori reinfected 2.5% of the levofloxacin group and 3% of the bismuth quadruple group.
The researchers used metagenomic sequencing to examine the bacteria in the patients’ microbiome for antibiotic resistance. Using 16S rRNA sequencing, they found that the proportion of genera and species with significant changes in abundance at 2 weeks after treatment compared with baseline was 52.4% for levofloxacin quadruple therapy versus 45.1% for bismuth quadruple therapy.
However, 8 weeks after treatment, the proportion with significant changes had dropped to 5.8% for the levofloxacin group and 21.5% for the bismuth group. And at the end of a year, they had further dropped to 0.9% for the levofloxacin group and 8.4% for the bismuth group.
“It was generally reassuring that, even after giving these combinations of different antibiotics, eventually it doesn’t seem to affect the resistance pattern in bacteria lower down in the gut,” said session moderator Steven Moss, MD, professor of medicine at Brown University in Providence, R.I.
Still, continuing to pile on more and more antibiotics to treat H. pylori infections won’t work forever because H. pylori strains are themselves developing resistance so rapidly, he said. “We’re certainly going to have worse eradications in the future unless we can come up with new tricks.”
A hopeful development are new techniques to test H. pylori for resistance to specific antibiotics before initiating treatment, said Dr. Moss.
Dr. Moss consults with companies developing H. pylori therapies and diagnostics. Dr. Liou reported no relevant financial interests.
AT DDW 2022
Videos may not increase vaccinations in IBD
SAN DIEGO – Video and text messaging may not increase the proportion of people with inflammatory bowel disease (IBD) who get influenza vaccinations.
Although patients who received the messages expressed greater intention to get the vaccinations in a trial of the two methods, they didn’t follow through and get the shots, said Keren Appel, MD, a pediatric gastroenterologist at Children’s Hospital of Orange County in Orange, Calif.
“We found there was no difference in the uptake of the influenza vaccine between the two groups,” she said in an interview. Dr. Appel, who participated in the research while at Cedars-Sinai Medical Center in Los Angeles, presented the finding at the annual Digestive Diseases Week® (DDW) 2022.
People with IBD run an increased risk of complications such as infection, bone fractures, and cancer, said Dr. Appel. Previous research has suggested many people with IBD lack understanding or awareness or are skeptical of immunizations.
A previous trial with text-based email reminders did not result in more immunizations, according to Dr. Appel, so she and her colleagues decided to try promoting health prevention with videos. With feedback from patients, they created a series of animations encouraging patients to get influenza, pneumococcal, and zoster vaccinations and screening for bone health and skin cancer.
They randomly assigned 511 to receive videos and 545 patients to receive texts as a control group. After 6 months, 345 patients remained in the text group and 322 remained in the video group. The two groups had similar demographics, health status, and preventive health behaviors. They were mostly educated White women whose IBD was in remission.
The percentage of those who got flu vaccines increased from 59% (for the 2018-2019 season) to 63% (for the 2019-2020 flu season) in the group that watched the videos. However this change did not quite reach statistical significance (P = .07). The change in the text group, from 55% to 57%, was also not significant (P = .23).
The subjects did express more intention to get flu vaccines. The percentage with this intention increased from 59 to 75 in the video group, and from 55 to 72 in the text group. Both changes were statistically significant (P < .001).
Intentions to receive pneumonia and shingles vaccines, and bone and skin cancer screening, were not statistically different between the groups.
The researchers looked at age, immunosuppression, gender, and education to see if these factors could predict who was most likely to get the flu vaccine, but the only significant predictor was having received a previous flu shot.
Dr. Appel speculated that the videos might have been more effective in a more racially diverse, less educated population, or one where fewer people had previously received vaccinations.
“While we didn’t see a difference in this study, I think it opens up a lot of other questions that we can explore and answer,” she said. “It’s possible that patients may not have a one size fits all on their response. Some may respond better to video. Some may respond to text. Some may need more frequent reminders. Some might need to hear it from their doctor directly.”
Session comoderator Alyse Bedell, PhD, an assistant professor of psychiatry and behavioral neuroscience at the University of Chicago, agreed that a different patient population might have responded differently. “A population that may have lower access to educational resources, or has less educational attainment, or may have fewer people in their communities that are already receiving vaccines – those I think are going to be the populations where we’re going to be more likely to see the effects of an intervention like this,” she said in an interview.
Neither Dr. Appel nor Dr. Bedell reported any relevant financial interests. The study was funded by Pfizer.
SAN DIEGO – Video and text messaging may not increase the proportion of people with inflammatory bowel disease (IBD) who get influenza vaccinations.
Although patients who received the messages expressed greater intention to get the vaccinations in a trial of the two methods, they didn’t follow through and get the shots, said Keren Appel, MD, a pediatric gastroenterologist at Children’s Hospital of Orange County in Orange, Calif.
“We found there was no difference in the uptake of the influenza vaccine between the two groups,” she said in an interview. Dr. Appel, who participated in the research while at Cedars-Sinai Medical Center in Los Angeles, presented the finding at the annual Digestive Diseases Week® (DDW) 2022.
People with IBD run an increased risk of complications such as infection, bone fractures, and cancer, said Dr. Appel. Previous research has suggested many people with IBD lack understanding or awareness or are skeptical of immunizations.
A previous trial with text-based email reminders did not result in more immunizations, according to Dr. Appel, so she and her colleagues decided to try promoting health prevention with videos. With feedback from patients, they created a series of animations encouraging patients to get influenza, pneumococcal, and zoster vaccinations and screening for bone health and skin cancer.
They randomly assigned 511 to receive videos and 545 patients to receive texts as a control group. After 6 months, 345 patients remained in the text group and 322 remained in the video group. The two groups had similar demographics, health status, and preventive health behaviors. They were mostly educated White women whose IBD was in remission.
The percentage of those who got flu vaccines increased from 59% (for the 2018-2019 season) to 63% (for the 2019-2020 flu season) in the group that watched the videos. However this change did not quite reach statistical significance (P = .07). The change in the text group, from 55% to 57%, was also not significant (P = .23).
The subjects did express more intention to get flu vaccines. The percentage with this intention increased from 59 to 75 in the video group, and from 55 to 72 in the text group. Both changes were statistically significant (P < .001).
Intentions to receive pneumonia and shingles vaccines, and bone and skin cancer screening, were not statistically different between the groups.
The researchers looked at age, immunosuppression, gender, and education to see if these factors could predict who was most likely to get the flu vaccine, but the only significant predictor was having received a previous flu shot.
Dr. Appel speculated that the videos might have been more effective in a more racially diverse, less educated population, or one where fewer people had previously received vaccinations.
“While we didn’t see a difference in this study, I think it opens up a lot of other questions that we can explore and answer,” she said. “It’s possible that patients may not have a one size fits all on their response. Some may respond better to video. Some may respond to text. Some may need more frequent reminders. Some might need to hear it from their doctor directly.”
Session comoderator Alyse Bedell, PhD, an assistant professor of psychiatry and behavioral neuroscience at the University of Chicago, agreed that a different patient population might have responded differently. “A population that may have lower access to educational resources, or has less educational attainment, or may have fewer people in their communities that are already receiving vaccines – those I think are going to be the populations where we’re going to be more likely to see the effects of an intervention like this,” she said in an interview.
Neither Dr. Appel nor Dr. Bedell reported any relevant financial interests. The study was funded by Pfizer.
SAN DIEGO – Video and text messaging may not increase the proportion of people with inflammatory bowel disease (IBD) who get influenza vaccinations.
Although patients who received the messages expressed greater intention to get the vaccinations in a trial of the two methods, they didn’t follow through and get the shots, said Keren Appel, MD, a pediatric gastroenterologist at Children’s Hospital of Orange County in Orange, Calif.
“We found there was no difference in the uptake of the influenza vaccine between the two groups,” she said in an interview. Dr. Appel, who participated in the research while at Cedars-Sinai Medical Center in Los Angeles, presented the finding at the annual Digestive Diseases Week® (DDW) 2022.
People with IBD run an increased risk of complications such as infection, bone fractures, and cancer, said Dr. Appel. Previous research has suggested many people with IBD lack understanding or awareness or are skeptical of immunizations.
A previous trial with text-based email reminders did not result in more immunizations, according to Dr. Appel, so she and her colleagues decided to try promoting health prevention with videos. With feedback from patients, they created a series of animations encouraging patients to get influenza, pneumococcal, and zoster vaccinations and screening for bone health and skin cancer.
They randomly assigned 511 to receive videos and 545 patients to receive texts as a control group. After 6 months, 345 patients remained in the text group and 322 remained in the video group. The two groups had similar demographics, health status, and preventive health behaviors. They were mostly educated White women whose IBD was in remission.
The percentage of those who got flu vaccines increased from 59% (for the 2018-2019 season) to 63% (for the 2019-2020 flu season) in the group that watched the videos. However this change did not quite reach statistical significance (P = .07). The change in the text group, from 55% to 57%, was also not significant (P = .23).
The subjects did express more intention to get flu vaccines. The percentage with this intention increased from 59 to 75 in the video group, and from 55 to 72 in the text group. Both changes were statistically significant (P < .001).
Intentions to receive pneumonia and shingles vaccines, and bone and skin cancer screening, were not statistically different between the groups.
The researchers looked at age, immunosuppression, gender, and education to see if these factors could predict who was most likely to get the flu vaccine, but the only significant predictor was having received a previous flu shot.
Dr. Appel speculated that the videos might have been more effective in a more racially diverse, less educated population, or one where fewer people had previously received vaccinations.
“While we didn’t see a difference in this study, I think it opens up a lot of other questions that we can explore and answer,” she said. “It’s possible that patients may not have a one size fits all on their response. Some may respond better to video. Some may respond to text. Some may need more frequent reminders. Some might need to hear it from their doctor directly.”
Session comoderator Alyse Bedell, PhD, an assistant professor of psychiatry and behavioral neuroscience at the University of Chicago, agreed that a different patient population might have responded differently. “A population that may have lower access to educational resources, or has less educational attainment, or may have fewer people in their communities that are already receiving vaccines – those I think are going to be the populations where we’re going to be more likely to see the effects of an intervention like this,” she said in an interview.
Neither Dr. Appel nor Dr. Bedell reported any relevant financial interests. The study was funded by Pfizer.
AT DDW 2022
Adsorbent offers promise for irritable bowel syndrome diarrhea
SAN DIEGO – An intestinal adsorbent, polymethylsiloxane polyhydrate (PMSPH), may relieve the diarrhea associated with irritable bowel syndrome (IBS), researchers say.
The adsorbent reduced abdominal pain, improved stool consistency, and won praise from patients, said Yan Yiannakou, MBChB, a consultant in gastroenterology at County Durham and Darlington (England) National Health Service Foundation Trust.
“It’s great to have something new for patients to try,” he told MDEdge. “And it’s great that this treatment is so safe, and easy to use.”
Dr. Yiannakou presented the finding at the annual Digestive Diseases Week® (DDW).
Many people with irritable bowel syndrome find the currently available treatments and diets difficult to use or ineffective.
First developed 30 years ago in Eastern Europe, PMSPH is marketed over the counter in 30 European countries under the name Enterosgel as a treatment for diarrhea, said Dr. Yiannakou. It received conformité européenne (CE) mark in 2011.
Since PMSPH is not adsorbed by the body, it has been approved as a medical device rather than as a drug, said Dr. Yiannakou. Although its manufacturer is not yet marketing it in the United States, websites there are offering it as a dietary supplement for "toxin binding" and "cleansing the gut."*
Since the etiology of IBS is poorly understood, it is also not clear exactly how PMSPH improves IBS symptoms, Dr. Yiannakou said. “I think this is binding a whole range of molecules which are either irritant or induce diarrhea through secretion.” Fat, bile salts, immune chemicals, and bacterial breakdown products are possibilities, he said.
PMSPH’s approval in Europe rests largely on trials for other forms of diarrhea; it did not undergo a high-quality randomized, placebo-controlled trial for IBS, Dr. Yiannakou said.
To fill that gap, he and his colleagues recruited 440 people with IBS, aged 16-75 years, from 28 sites in England. They randomly assigned 219 to receive PMSPH and 221 to receive a placebo for 8 weeks. Following this blinded phase, both groups received PMSPH for another 8 weeks (a phase requested by the patients who helped design the trial). The investigators then followed up with a phone call 8 weeks later to those who responded to the treatment.
The subjects recorded their symptoms in an e-diary and completed questionnaires. Because of COVID-19 constraints imposed after the trial began, the researchers collected some of the data through virtual visits and online questionnaires.
On a U.S. Food and Drug Administration–recommended composite score for abdominal pain and stool consistency, 37.4% of the patients receiving PMSPH were defined as responders versus 24.3% of the patients receiving the placebo, a statistically significant difference.
However, that score does not accurately reflect the main concerns of people with IBS diarrhea, said Dr. Yiannakou. More important is how often they have diarrhea, and by that measure the difference between the placebo and treatment groups was larger.
There were also statistically significant differences in favor of the PMSPH group in separate scores for abdominal pain, stool frequency, bloating, and urgency.
Surveyed between week 5 and week 8, 69% of patients taking PMSPH reported that they were getting adequate relief, compared with 30% of those taking the placebo. Among the responders surveyed 8 weeks after the open-label phase ended, 74% said they were still benefiting from the treatment. And 81% said they were still using PMSPH, even though they had to buy it for themselves.
Only a handful of patients experienced any adverse events, and there were no significant differences in the number of these events between those taking the placebo and those taking PMSPH.
“I think we’re going to be eager to learn which patients that have irritable bowel syndrome would benefit from this particular treatment,” said session comoderator Eric Shah, MD, MBA, director of gastrointestinal motility at Dartmouth University in Hanover, N.H., who was not involved in the study. He also wanted to know how PMSPH compares to similar binding agents on the market.
Session comoderator Nikrad Shahnavaz, MD, an associate professor of medicine in the division of digestive diseases, department of medicine, at Emory University, Atlanta, said his patients complain two binding agents now prescribed for IBS in the United States, cholestyramine and colestipol, cause nausea and vomiting. That could be an advantage for PMSPH, he said. “It’s good to add to your tools.”
Dr. Yiannakou, Dr. Shahnavaz, and Dr. Shah reported no relevant financial interests.
*An earlier version of this article misstated PMSPH's mechanism of action. It is not adsorbed by the body. Additionally, the marketing status of PMSPH was misstated; it is not currently on the U.S. market.
SAN DIEGO – An intestinal adsorbent, polymethylsiloxane polyhydrate (PMSPH), may relieve the diarrhea associated with irritable bowel syndrome (IBS), researchers say.
The adsorbent reduced abdominal pain, improved stool consistency, and won praise from patients, said Yan Yiannakou, MBChB, a consultant in gastroenterology at County Durham and Darlington (England) National Health Service Foundation Trust.
“It’s great to have something new for patients to try,” he told MDEdge. “And it’s great that this treatment is so safe, and easy to use.”
Dr. Yiannakou presented the finding at the annual Digestive Diseases Week® (DDW).
Many people with irritable bowel syndrome find the currently available treatments and diets difficult to use or ineffective.
First developed 30 years ago in Eastern Europe, PMSPH is marketed over the counter in 30 European countries under the name Enterosgel as a treatment for diarrhea, said Dr. Yiannakou. It received conformité européenne (CE) mark in 2011.
Since PMSPH is not adsorbed by the body, it has been approved as a medical device rather than as a drug, said Dr. Yiannakou. Although its manufacturer is not yet marketing it in the United States, websites there are offering it as a dietary supplement for "toxin binding" and "cleansing the gut."*
Since the etiology of IBS is poorly understood, it is also not clear exactly how PMSPH improves IBS symptoms, Dr. Yiannakou said. “I think this is binding a whole range of molecules which are either irritant or induce diarrhea through secretion.” Fat, bile salts, immune chemicals, and bacterial breakdown products are possibilities, he said.
PMSPH’s approval in Europe rests largely on trials for other forms of diarrhea; it did not undergo a high-quality randomized, placebo-controlled trial for IBS, Dr. Yiannakou said.
To fill that gap, he and his colleagues recruited 440 people with IBS, aged 16-75 years, from 28 sites in England. They randomly assigned 219 to receive PMSPH and 221 to receive a placebo for 8 weeks. Following this blinded phase, both groups received PMSPH for another 8 weeks (a phase requested by the patients who helped design the trial). The investigators then followed up with a phone call 8 weeks later to those who responded to the treatment.
The subjects recorded their symptoms in an e-diary and completed questionnaires. Because of COVID-19 constraints imposed after the trial began, the researchers collected some of the data through virtual visits and online questionnaires.
On a U.S. Food and Drug Administration–recommended composite score for abdominal pain and stool consistency, 37.4% of the patients receiving PMSPH were defined as responders versus 24.3% of the patients receiving the placebo, a statistically significant difference.
However, that score does not accurately reflect the main concerns of people with IBS diarrhea, said Dr. Yiannakou. More important is how often they have diarrhea, and by that measure the difference between the placebo and treatment groups was larger.
There were also statistically significant differences in favor of the PMSPH group in separate scores for abdominal pain, stool frequency, bloating, and urgency.
Surveyed between week 5 and week 8, 69% of patients taking PMSPH reported that they were getting adequate relief, compared with 30% of those taking the placebo. Among the responders surveyed 8 weeks after the open-label phase ended, 74% said they were still benefiting from the treatment. And 81% said they were still using PMSPH, even though they had to buy it for themselves.
Only a handful of patients experienced any adverse events, and there were no significant differences in the number of these events between those taking the placebo and those taking PMSPH.
“I think we’re going to be eager to learn which patients that have irritable bowel syndrome would benefit from this particular treatment,” said session comoderator Eric Shah, MD, MBA, director of gastrointestinal motility at Dartmouth University in Hanover, N.H., who was not involved in the study. He also wanted to know how PMSPH compares to similar binding agents on the market.
Session comoderator Nikrad Shahnavaz, MD, an associate professor of medicine in the division of digestive diseases, department of medicine, at Emory University, Atlanta, said his patients complain two binding agents now prescribed for IBS in the United States, cholestyramine and colestipol, cause nausea and vomiting. That could be an advantage for PMSPH, he said. “It’s good to add to your tools.”
Dr. Yiannakou, Dr. Shahnavaz, and Dr. Shah reported no relevant financial interests.
*An earlier version of this article misstated PMSPH's mechanism of action. It is not adsorbed by the body. Additionally, the marketing status of PMSPH was misstated; it is not currently on the U.S. market.
SAN DIEGO – An intestinal adsorbent, polymethylsiloxane polyhydrate (PMSPH), may relieve the diarrhea associated with irritable bowel syndrome (IBS), researchers say.
The adsorbent reduced abdominal pain, improved stool consistency, and won praise from patients, said Yan Yiannakou, MBChB, a consultant in gastroenterology at County Durham and Darlington (England) National Health Service Foundation Trust.
“It’s great to have something new for patients to try,” he told MDEdge. “And it’s great that this treatment is so safe, and easy to use.”
Dr. Yiannakou presented the finding at the annual Digestive Diseases Week® (DDW).
Many people with irritable bowel syndrome find the currently available treatments and diets difficult to use or ineffective.
First developed 30 years ago in Eastern Europe, PMSPH is marketed over the counter in 30 European countries under the name Enterosgel as a treatment for diarrhea, said Dr. Yiannakou. It received conformité européenne (CE) mark in 2011.
Since PMSPH is not adsorbed by the body, it has been approved as a medical device rather than as a drug, said Dr. Yiannakou. Although its manufacturer is not yet marketing it in the United States, websites there are offering it as a dietary supplement for "toxin binding" and "cleansing the gut."*
Since the etiology of IBS is poorly understood, it is also not clear exactly how PMSPH improves IBS symptoms, Dr. Yiannakou said. “I think this is binding a whole range of molecules which are either irritant or induce diarrhea through secretion.” Fat, bile salts, immune chemicals, and bacterial breakdown products are possibilities, he said.
PMSPH’s approval in Europe rests largely on trials for other forms of diarrhea; it did not undergo a high-quality randomized, placebo-controlled trial for IBS, Dr. Yiannakou said.
To fill that gap, he and his colleagues recruited 440 people with IBS, aged 16-75 years, from 28 sites in England. They randomly assigned 219 to receive PMSPH and 221 to receive a placebo for 8 weeks. Following this blinded phase, both groups received PMSPH for another 8 weeks (a phase requested by the patients who helped design the trial). The investigators then followed up with a phone call 8 weeks later to those who responded to the treatment.
The subjects recorded their symptoms in an e-diary and completed questionnaires. Because of COVID-19 constraints imposed after the trial began, the researchers collected some of the data through virtual visits and online questionnaires.
On a U.S. Food and Drug Administration–recommended composite score for abdominal pain and stool consistency, 37.4% of the patients receiving PMSPH were defined as responders versus 24.3% of the patients receiving the placebo, a statistically significant difference.
However, that score does not accurately reflect the main concerns of people with IBS diarrhea, said Dr. Yiannakou. More important is how often they have diarrhea, and by that measure the difference between the placebo and treatment groups was larger.
There were also statistically significant differences in favor of the PMSPH group in separate scores for abdominal pain, stool frequency, bloating, and urgency.
Surveyed between week 5 and week 8, 69% of patients taking PMSPH reported that they were getting adequate relief, compared with 30% of those taking the placebo. Among the responders surveyed 8 weeks after the open-label phase ended, 74% said they were still benefiting from the treatment. And 81% said they were still using PMSPH, even though they had to buy it for themselves.
Only a handful of patients experienced any adverse events, and there were no significant differences in the number of these events between those taking the placebo and those taking PMSPH.
“I think we’re going to be eager to learn which patients that have irritable bowel syndrome would benefit from this particular treatment,” said session comoderator Eric Shah, MD, MBA, director of gastrointestinal motility at Dartmouth University in Hanover, N.H., who was not involved in the study. He also wanted to know how PMSPH compares to similar binding agents on the market.
Session comoderator Nikrad Shahnavaz, MD, an associate professor of medicine in the division of digestive diseases, department of medicine, at Emory University, Atlanta, said his patients complain two binding agents now prescribed for IBS in the United States, cholestyramine and colestipol, cause nausea and vomiting. That could be an advantage for PMSPH, he said. “It’s good to add to your tools.”
Dr. Yiannakou, Dr. Shahnavaz, and Dr. Shah reported no relevant financial interests.
*An earlier version of this article misstated PMSPH's mechanism of action. It is not adsorbed by the body. Additionally, the marketing status of PMSPH was misstated; it is not currently on the U.S. market.
AT DDW 2022