User login
Hospitalist‐Led Antimicrobial Stewardship
Inappropriate antimicrobial use in hospitalized patients is a well‐recognized driver for the development of drug‐resistant organisms and antimicrobial‐related complications such as Clostridium difficile infection (CDI).[1, 2] Infection with C difficile affects nearly 500,000 people annually resulting in higher healthcare expenditures, longer lengths of hospital stay, and nearly 15,000 deaths.[3] Data from the Centers for Disease Control and Prevention (CDC) suggest that a 30% reduction in the use of broad‐spectrum antimicrobials, or a 5% reduction in the proportion of hospitalized patients receiving antimicrobials, could equate to a 26% reduction in CDI.[4] It is estimated that up to 50% of antimicrobial use in the hospital setting may be inappropriate.[5]
Since the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America published guidelines for developing formal, hospital‐based antimicrobial stewardship programs in 2007, stewardship practices have been adapted by frontline providers to fit day‐to‐day inpatient care.[5] A recent review by Hamilton et al. described several studies in which stewardship practices were imbedded into daily workflows by way of checklists, education reminders, and periodic review of antimicrobial usage, as well as a multicenter pilot of point‐of‐care stewardship interventions successfully implemented by various providers including nursing, pharmacists, and hospitalists.[6]
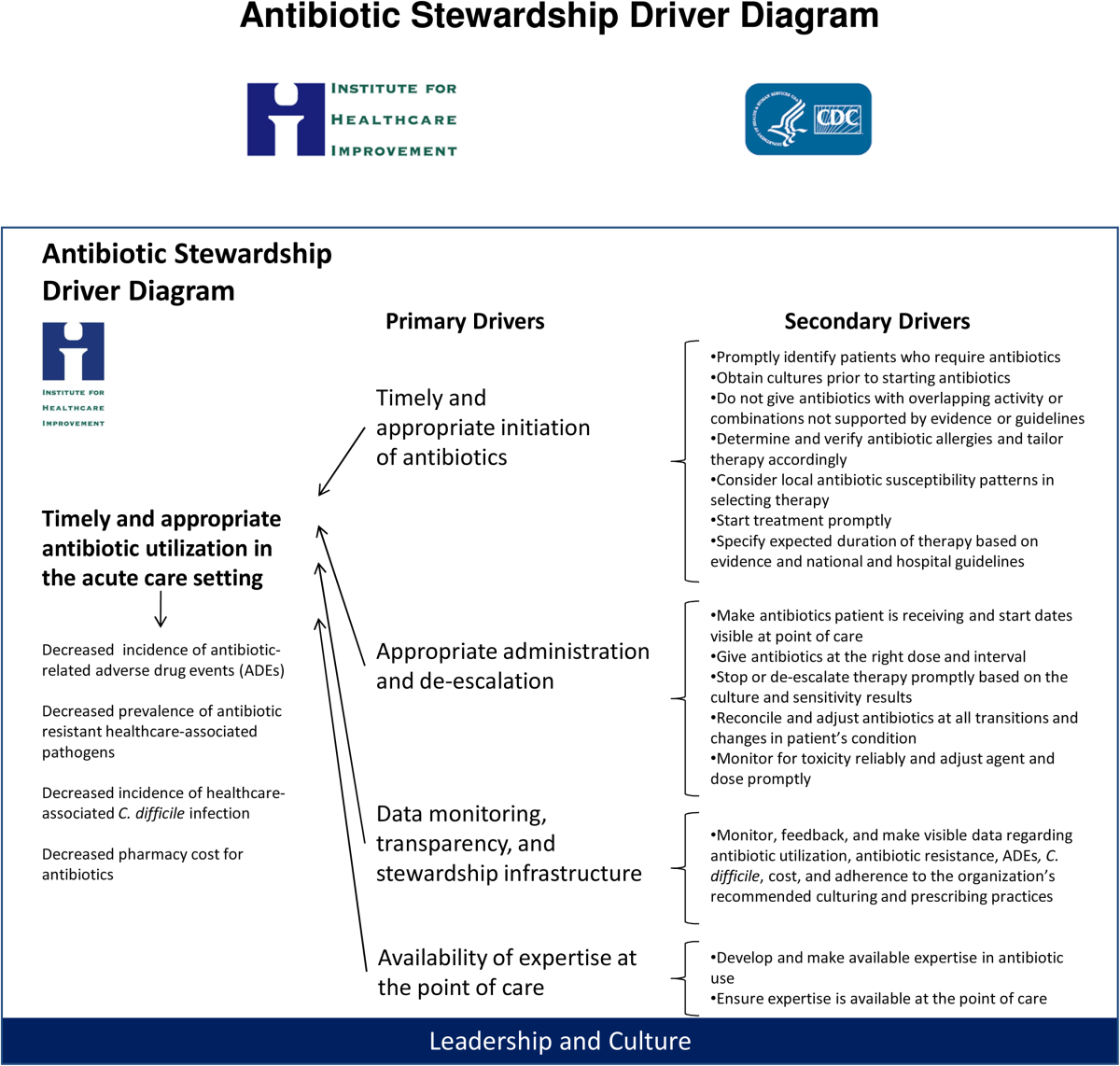
In response to the CDC's 2010 Get Smart for Healthcare campaign, which focused on stemming antimicrobial resistance and improving antimicrobial use, the Institute for Healthcare Improvement (IHI), in partnership with the CDC, brought together experts in the field to identify practical and feasible target practices for hospital‐based stewardship and created a Driver Diagram to guide implementation efforts (Figure 1). Rohde et al. described the initial pilot testing of these practices, the decision to more actively engage frontline providers, and the 3 key strategies identified as high‐yield improvement targets: enhancing the visibility of antimicrobial use at the point of care, creating easily accessible antimicrobial guidelines for common infections, and the implementation of a 72‐hour timeout after initiation of antimicrobials.[7]

In this article, we describe how, in partnership with the IHI and the CDC, the hospital medicine programs at 5 diverse hospitals iteratively tested these 3 strategies with a goal of identifying the barriers and facilitators to effective hospitalist‐led antimicrobial stewardship.
METHODS
Representatives from 5 hospital medicine programs, IHI, and the CDC attended a kick‐off meeting at the CDC in November 2012 to discuss the 3 proposed strategies, examples of prior testing, and ideas for implementation. Each hospitalist provided a high‐level summary of the current state of stewardship efforts at their respective institutions, identified possible future states related to the improvement strategies, and anticipated problems in achieving them. The 3 key strategies are described below.
Improved Documentation/Visibility at Points of Care
Making antimicrobial indication, day of therapy, and anticipated duration transparent in the medical record was the targeted improvement strategy to avoid unnecessary antimicrobial days that can result from provider uncertainty, particularly during patient handoffs. Daily hospitalist documentation was identified as a vehicle through which these aspects of antimicrobial use could be effectively communicated and propagated from provider to provider.
Stewardship educational sessions and/or awareness campaigns were hospitalist led, and were accompanied by follow‐up reminders in the forms of emails, texts, flyers, or conferences. Infectious disease physicians were not directly involved in education but were available for consultation if needed.
Improved Guideline Clarity and Accessibility
Enhancing the availability of guidelines for frequently encountered infections and clarifying key guideline recommendations such as treatment duration were identified as the improvement strategies to help make treatment regimens more appropriate and consistent across providers.
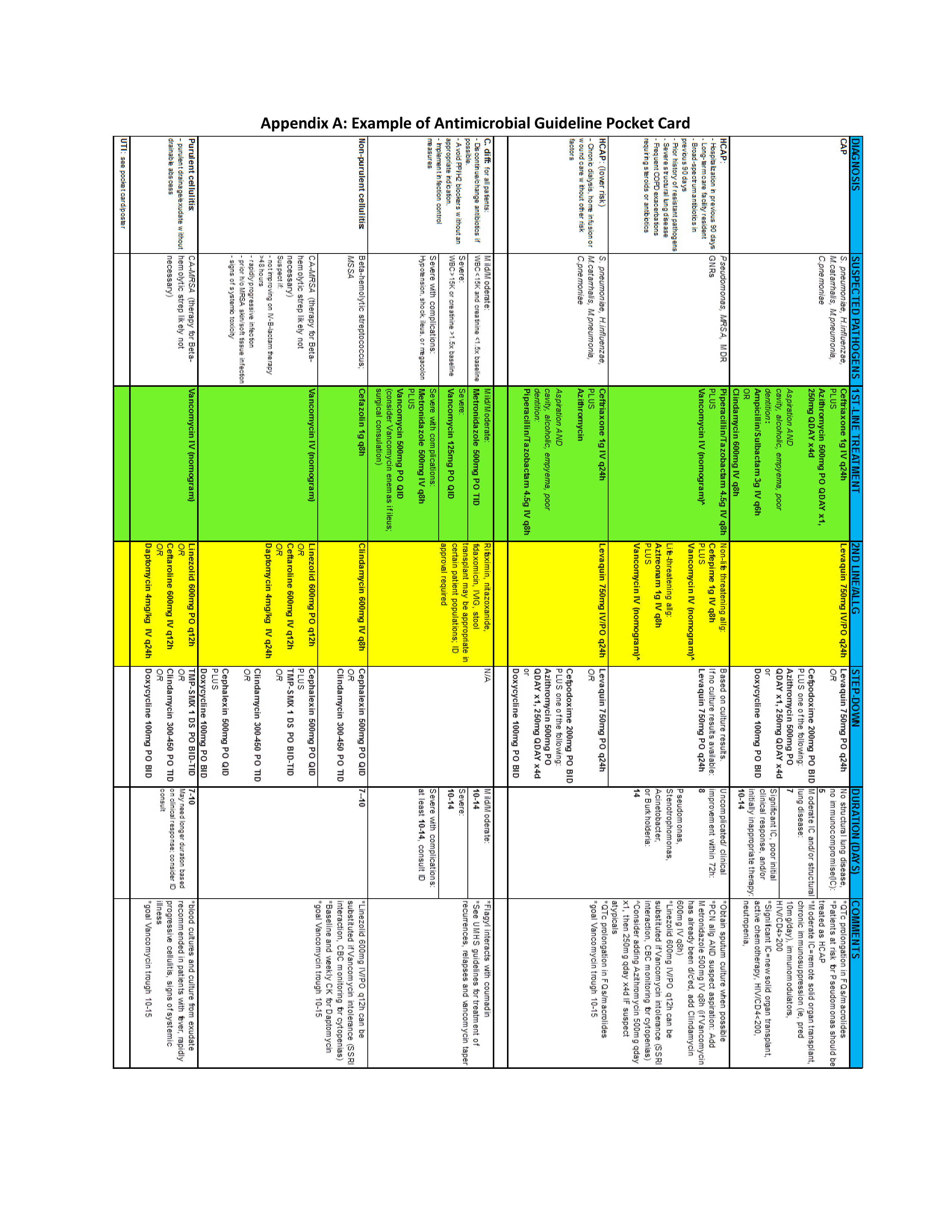
Interventions included designing simplified pocket cards for commonly encountered infections, (see Supporting Information, Appendix A, in the online version of this article), collaborating with infectious disease physicians on guideline development, and dissemination through email, smartphone, and wall flyers, and creation of a continuous medical education module focused on stewardship practices.
72‐Hour Antimicrobial Timeout
The 72‐hour antimicrobial timeout required that hospitalists routinely reassess antimicrobial use 72 hours following antimicrobial initiation, a time when most pertinent culture data had returned. Hospitalists partnered with clinical pharmacists at all sites, and addressed the following questions during each timeout: (1) Does the patient have a condition that requires continued use of antimicrobials? (2) Can the current antimicrobial regimen be tailored based on culture data? (3) What is the anticipated treatment duration? A variety of modifications occurred during timeouts, including broadening or narrowing the antimicrobial regimen based on culture data, switching to an oral antimicrobial, adjusting dose or frequency based on patient‐specific factors, as well as discontinuation of antimicrobials. Following the initial timeout, further adjustments were made as the clinical situation dictated; intermittent partnered timeouts continued during a patient's hospitalization on an individualized basis. Hospitalists were encouraged to independently review new diagnostic information daily and make changes as needed outside the dedicated time‐out sessions. All decisions to adjust antimicrobial regimens were provider driven; no hospitals employed automated antimicrobial discontinuation without provider input.
Implementation and Evaluation
Each site was tasked with conducting small tests of change aimed at implementing at least 1, and ideally all 3 strategies. Small, reasonably achievable interventions were preferred to large hospital‐wide initiatives so that key barriers and facilitators to the change could be quickly identified and addressed.
Methods of data collection varied across institutions and included anonymous physician survey, face‐to‐face physician interviews, and medical record review. Evaluations of hospital‐specific interventions utilized convenience samples to obtain real time, actionable data. Postintervention data were distributed through biweekly calls and compiled at the conclusion of the project. Barriers and facilitators of hospitalist‐centered antimicrobial stewardship collected over the course of the project were reviewed and used to identify common themes.
RESULTS
Participating hospitals included 1 community nonteaching hospital, 2 community teaching hospitals, and 2 academic medical centers. All hospitals used computerized order entry and had prior quality improvement experience; 4 out of 5 hospitals used electronic medical records. Postintervention data on antimicrobial documentation and timeouts were compiled, shared, and successes identified. For example, 2 hospitals saw an increase in complete antimicrobial documentation from 4% and 8% to 51% and 65%, respectively, of medical records reviewed over a 3‐month period. Additionally, cumulative timeout data across all hospitals showed that out of 726 antimicrobial timeouts evaluated, optimization or discontinuation occurred 218 times or 30% of the time.
Each site's key implementation barriers and facilitators were collected. Examples were compiled and common themes emerged (Table 1).
| ||
| Barriers: What impediments did we experience during our stewardship project? | Schedule and practice variability | Physician variability in structure of antimicrobial documentation |
| Prescribing etiquette: it's difficult to change course of treatment plan started by a colleague | ||
| Competing schedule demands of hospitalist and pharmacist | ||
| Skepticism of antimicrobial stewardship importance | Perception of incorporating stewardship practices into daily work as time consuming | |
| Improvement project fatigue from competing quality improvement initiatives | ||
| Unclear leadership buy‐in | ||
| Focusing too broadly | Choosing large initial interventions, which take significant time/effort to complete and quantify | |
| Setting unrealistic expectations (eg, expecting perfect adherence to documentation, guidelines, or timeout) | ||
| Facilitators: What countermeasures did we target to overcome barriers? | Engage the hospitalists | Establish a core part of the hospitalist group as stewardship champions |
| Speak 1‐on‐1 to colleagues about specific goals and ways to achieve them | ||
| Establish buy‐in from leadership | ||
| Encourage participation from a multidisciplinary team (eg, bedside nursing, clinical pharmacists) | ||
| Collect real time data and feedback | Utilize a data collection tool if possible/engage hospital coders to identify appropriate diagnoses | |
| Define your question and identify baseline data prior to intervention | ||
| Give rapid cycle feedback to colleagues that can impact antimicrobial prescribing in real time | ||
| Recognize and reward high performers | ||
| Limit scope | Start with small, quickly implementable interventions | |
| Identify interventions that are easy to integrate into hospitalist workflow | ||
DISCUSSION
We successfully brought together hospitalists from diverse institutions to undertake small tests of change aimed at 3 key antimicrobial use improvement strategies. Following our interventions, significant improvement in antimicrobial documentation occurred at 2 institutions focusing on this improvement strategy, and 72‐hour timeouts performed across all hospitals tailored antimicrobial use in 30% of the sessions. Through frequent collaborative discussions and information sharing, we were able to identify common barriers and facilitators to hospitalist‐centered stewardship efforts.
Each participating hospital medicine program noticed a gradual shift in thinking among their colleagues, from initial skepticism about embedding stewardship within their daily workflow, to general acceptance that it was a worthwhile and meaningful endeavor. We posited that this transition in belief and behavior evolved for several reasons. First, each group was educated about their own, personal prescribing practices from the outset rather than presenting abstract data. This allowed for ownership of the problem and buy‐in to improve it. Second, participants were able to experience the benefits at an individual level while the interventions were ongoing (eg, having other providers reciprocate structured documentation during patient handoffs, making antimicrobial plans clearer), reinforcing the achievability of stewardship practices within each group. Additionally, we focused on making small, manageable interventions that did not seem disruptive to hospitalists' daily workflow. For example, 1 group instituted antimicrobial timeouts during preexisting multidisciplinary rounds with clinical pharmacists. Last, project champions had both leadership and frontline roles within their groups and set the example for stewardship practices, which conveyed that this was a priority at the leadership level. These findings are in line with those of Charani et al., who evaluated behavior change strategies that influence antimicrobial prescribing in acute care. The authors found that behavioral determinants and social norms strongly influence prescribing practices in acute care, and that antimicrobial stewardship improvement projects should account for these influences.[8]
We also identified several barriers to antimicrobial stewardship implementation (Table 1) and proposed measures to address these barriers in future improvement efforts. For example, hospital medicine programs without a preexisting clinical pharmacy partnership asked hospitalist leadership for more direct clinical pharmacy involvement, recognizing the importance of a physician‐pharmacy alliance for stewardship efforts. To more effectively embed antimicrobial stewardship into daily routine, several hospitalists suggested standardized order sets for commonly encountered infections, as well as routine feedback on prescribing practices. Furthermore, although our simplified antimicrobial guideline pocket card enhanced access to this information, several colleagues suggested a smart phone application that would make access even easier and less cumbersome. Last, given the concern about the sustainability of antimicrobial stewardship initiatives, we recommended periodic reminders, random medical record review, and re‐education if necessary on our 3 strategies and their purpose.
Our study is not without limitations. Each participating hospitalist group enacted hospital‐specific interventions based on individual hospitalist program needs and goals, and although there was collective discussion, no group was tasked to undertake another group's initiative, thereby limiting generalizability. We did, however, identify common facilitators that could be adapted to a wide variety of hospitalist programs. We also note that our 3 main strategies were included in a recent review of quality indicators for measuring the success of antimicrobial stewardship programs; thus, although details of individual practice may vary, in principle these concepts can help identify areas for improvement within each unique stewardship program.[9] Importantly, we were unable to evaluate the impact of the 3 key improvement strategies on important clinical outcomes such as overall antimicrobial use, complications including CDI, and cost. However, others have found that improvement strategies similar to our 3 key processes are associated with meaningful improvements in clinical outcomes as well as reductions in healthcare costs.[10, 11] Last, long‐ term impact and sustainability were not evaluated. By choosing interventions that were viewed by frontline providers as valuable and attainable, however, we feel that each group will likely continue current practices beyond the initial evaluation timeframe.
Although these 5 hospitalist groups were able to successfully implement several aspects of the 3 key improvement strategies, we recognize that this is only the first step. Further effort is needed to quantify the impact of these improvement efforts on objective patient outcomes such as readmissions, length of stay, and antimicrobial‐related complications, which will better inform our local and national leaders on the inherent clinical and financial gains associated with hospitalist‐led stewardship work. Finally, creative ways to better integrate stewardship activities into existing provider workflows (eg, decision support and automation) will further accelerate improvement efforts.
In summary, hospitalists at 5 diverse institutions successfully implemented key antimicrobial improvement strategies and identified important implementation facilitators and barriers. Future efforts at hospitalist‐led stewardship should focus on strategies to scale‐up interventions and evaluate their impact on clinical outcomes and cost.
Acknowledgements
The authors thank Latoya Kuhn, MPH, for her assistance with statistical analyses. We also thank the clinical pharmacists at each institution for their partnership in stewardship efforts: Patrick Arnold, PharmD, and Matthew Tupps, PharmD, MHA, from University of Michigan Hospital and Health System; and Roland Tam, PharmD, from Emory Johns Creek Hospital.
Disclosures: Dr. Flanders reports consulting fees or honoraria from the Institute for Healthcare Improvement, has provided consultancy to the Society of Hospital Medicine, has served as a reviewer for expert testimony, received honoraria as a visiting lecturer to various hospitals, and has received royalties from publisher John Wiley & Sons. He has also received grant funding from Blue Cross Blue Shield of Michigan and the Agency for Healthcare Research and Quality. Dr. Ko reports consultancy for the American Hospital Association and the Society of Hospital Medicine involving work with catheter‐associated urinary tract infections. Ms. Jacobsen reports grant funding from the Institute for Healthcare Improvement. Dr. Rosenberg reports consultancy for Bristol‐Myers Squibb, Forest Pharmaceuticals, and Pfizer. The funding source for this collaborative was through the Institute for Healthcare Improvement and Centers for Disease Control and Prevention. Funding was provided by the Department of Health and Human Services, the Centers for Disease Control and Prevention, the National Center for Emerging Zoonotic and Infectious Diseases, and the Division of Healthcare Quality Promotion/Office of the Director. Avaris Concepts served as the prime contractor and the Institute for Healthcare Improvement as the subcontractor for the initiative. The findings and conclusions in this report represent the views of the authors and might not reflect the views of the Centers for Disease Control and Prevention. The authors report no conflicts of interest.
- , , . Clinical and economic burden of antimicrobial resistance. Expert Rev Anti Infect Ther. 2008;6(5):751–763.
- , , , et al. Hospital and societal costs of antimicrobial‐resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis. 2009;49(8):1175–1184.
- , , , et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834.
- , , , et al.; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , , et al.; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177.
- , , , et al.; Centers for Disease Control and Prevention Epicenters Program. Point‐of‐prescription interventions to improve antimicrobial stewardship. Clin Infect Dis. 2015;60(8):1252–1258.
- , , . Role of the hospitalist in antimicrobial stewardship: a review of work completed and description of a multisite collaborative. Clin Ther. 2013;35(6):751–757.
- , , , et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53(7):651–662.
- , , , , . Quality indicators to measure appropriate antibiotic use in hospitalized adults. Clin Infect Dis. 2015;60(2):281–291.
- , . Application of antimicrobial stewardship to optimise management of community acquired pneumonia. Int J Clin Pract. 2011;65(7):775–783.
- , , , et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013;4:CD003543.
Inappropriate antimicrobial use in hospitalized patients is a well‐recognized driver for the development of drug‐resistant organisms and antimicrobial‐related complications such as Clostridium difficile infection (CDI).[1, 2] Infection with C difficile affects nearly 500,000 people annually resulting in higher healthcare expenditures, longer lengths of hospital stay, and nearly 15,000 deaths.[3] Data from the Centers for Disease Control and Prevention (CDC) suggest that a 30% reduction in the use of broad‐spectrum antimicrobials, or a 5% reduction in the proportion of hospitalized patients receiving antimicrobials, could equate to a 26% reduction in CDI.[4] It is estimated that up to 50% of antimicrobial use in the hospital setting may be inappropriate.[5]
Since the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America published guidelines for developing formal, hospital‐based antimicrobial stewardship programs in 2007, stewardship practices have been adapted by frontline providers to fit day‐to‐day inpatient care.[5] A recent review by Hamilton et al. described several studies in which stewardship practices were imbedded into daily workflows by way of checklists, education reminders, and periodic review of antimicrobial usage, as well as a multicenter pilot of point‐of‐care stewardship interventions successfully implemented by various providers including nursing, pharmacists, and hospitalists.[6]
In response to the CDC's 2010 Get Smart for Healthcare campaign, which focused on stemming antimicrobial resistance and improving antimicrobial use, the Institute for Healthcare Improvement (IHI), in partnership with the CDC, brought together experts in the field to identify practical and feasible target practices for hospital‐based stewardship and created a Driver Diagram to guide implementation efforts (Figure 1). Rohde et al. described the initial pilot testing of these practices, the decision to more actively engage frontline providers, and the 3 key strategies identified as high‐yield improvement targets: enhancing the visibility of antimicrobial use at the point of care, creating easily accessible antimicrobial guidelines for common infections, and the implementation of a 72‐hour timeout after initiation of antimicrobials.[7]

In this article, we describe how, in partnership with the IHI and the CDC, the hospital medicine programs at 5 diverse hospitals iteratively tested these 3 strategies with a goal of identifying the barriers and facilitators to effective hospitalist‐led antimicrobial stewardship.
METHODS
Representatives from 5 hospital medicine programs, IHI, and the CDC attended a kick‐off meeting at the CDC in November 2012 to discuss the 3 proposed strategies, examples of prior testing, and ideas for implementation. Each hospitalist provided a high‐level summary of the current state of stewardship efforts at their respective institutions, identified possible future states related to the improvement strategies, and anticipated problems in achieving them. The 3 key strategies are described below.
Improved Documentation/Visibility at Points of Care
Making antimicrobial indication, day of therapy, and anticipated duration transparent in the medical record was the targeted improvement strategy to avoid unnecessary antimicrobial days that can result from provider uncertainty, particularly during patient handoffs. Daily hospitalist documentation was identified as a vehicle through which these aspects of antimicrobial use could be effectively communicated and propagated from provider to provider.
Stewardship educational sessions and/or awareness campaigns were hospitalist led, and were accompanied by follow‐up reminders in the forms of emails, texts, flyers, or conferences. Infectious disease physicians were not directly involved in education but were available for consultation if needed.
Improved Guideline Clarity and Accessibility
Enhancing the availability of guidelines for frequently encountered infections and clarifying key guideline recommendations such as treatment duration were identified as the improvement strategies to help make treatment regimens more appropriate and consistent across providers.
Interventions included designing simplified pocket cards for commonly encountered infections, (see Supporting Information, Appendix A, in the online version of this article), collaborating with infectious disease physicians on guideline development, and dissemination through email, smartphone, and wall flyers, and creation of a continuous medical education module focused on stewardship practices.
72‐Hour Antimicrobial Timeout
The 72‐hour antimicrobial timeout required that hospitalists routinely reassess antimicrobial use 72 hours following antimicrobial initiation, a time when most pertinent culture data had returned. Hospitalists partnered with clinical pharmacists at all sites, and addressed the following questions during each timeout: (1) Does the patient have a condition that requires continued use of antimicrobials? (2) Can the current antimicrobial regimen be tailored based on culture data? (3) What is the anticipated treatment duration? A variety of modifications occurred during timeouts, including broadening or narrowing the antimicrobial regimen based on culture data, switching to an oral antimicrobial, adjusting dose or frequency based on patient‐specific factors, as well as discontinuation of antimicrobials. Following the initial timeout, further adjustments were made as the clinical situation dictated; intermittent partnered timeouts continued during a patient's hospitalization on an individualized basis. Hospitalists were encouraged to independently review new diagnostic information daily and make changes as needed outside the dedicated time‐out sessions. All decisions to adjust antimicrobial regimens were provider driven; no hospitals employed automated antimicrobial discontinuation without provider input.
Implementation and Evaluation
Each site was tasked with conducting small tests of change aimed at implementing at least 1, and ideally all 3 strategies. Small, reasonably achievable interventions were preferred to large hospital‐wide initiatives so that key barriers and facilitators to the change could be quickly identified and addressed.
Methods of data collection varied across institutions and included anonymous physician survey, face‐to‐face physician interviews, and medical record review. Evaluations of hospital‐specific interventions utilized convenience samples to obtain real time, actionable data. Postintervention data were distributed through biweekly calls and compiled at the conclusion of the project. Barriers and facilitators of hospitalist‐centered antimicrobial stewardship collected over the course of the project were reviewed and used to identify common themes.
RESULTS
Participating hospitals included 1 community nonteaching hospital, 2 community teaching hospitals, and 2 academic medical centers. All hospitals used computerized order entry and had prior quality improvement experience; 4 out of 5 hospitals used electronic medical records. Postintervention data on antimicrobial documentation and timeouts were compiled, shared, and successes identified. For example, 2 hospitals saw an increase in complete antimicrobial documentation from 4% and 8% to 51% and 65%, respectively, of medical records reviewed over a 3‐month period. Additionally, cumulative timeout data across all hospitals showed that out of 726 antimicrobial timeouts evaluated, optimization or discontinuation occurred 218 times or 30% of the time.
Each site's key implementation barriers and facilitators were collected. Examples were compiled and common themes emerged (Table 1).
| ||
| Barriers: What impediments did we experience during our stewardship project? | Schedule and practice variability | Physician variability in structure of antimicrobial documentation |
| Prescribing etiquette: it's difficult to change course of treatment plan started by a colleague | ||
| Competing schedule demands of hospitalist and pharmacist | ||
| Skepticism of antimicrobial stewardship importance | Perception of incorporating stewardship practices into daily work as time consuming | |
| Improvement project fatigue from competing quality improvement initiatives | ||
| Unclear leadership buy‐in | ||
| Focusing too broadly | Choosing large initial interventions, which take significant time/effort to complete and quantify | |
| Setting unrealistic expectations (eg, expecting perfect adherence to documentation, guidelines, or timeout) | ||
| Facilitators: What countermeasures did we target to overcome barriers? | Engage the hospitalists | Establish a core part of the hospitalist group as stewardship champions |
| Speak 1‐on‐1 to colleagues about specific goals and ways to achieve them | ||
| Establish buy‐in from leadership | ||
| Encourage participation from a multidisciplinary team (eg, bedside nursing, clinical pharmacists) | ||
| Collect real time data and feedback | Utilize a data collection tool if possible/engage hospital coders to identify appropriate diagnoses | |
| Define your question and identify baseline data prior to intervention | ||
| Give rapid cycle feedback to colleagues that can impact antimicrobial prescribing in real time | ||
| Recognize and reward high performers | ||
| Limit scope | Start with small, quickly implementable interventions | |
| Identify interventions that are easy to integrate into hospitalist workflow | ||
DISCUSSION
We successfully brought together hospitalists from diverse institutions to undertake small tests of change aimed at 3 key antimicrobial use improvement strategies. Following our interventions, significant improvement in antimicrobial documentation occurred at 2 institutions focusing on this improvement strategy, and 72‐hour timeouts performed across all hospitals tailored antimicrobial use in 30% of the sessions. Through frequent collaborative discussions and information sharing, we were able to identify common barriers and facilitators to hospitalist‐centered stewardship efforts.
Each participating hospital medicine program noticed a gradual shift in thinking among their colleagues, from initial skepticism about embedding stewardship within their daily workflow, to general acceptance that it was a worthwhile and meaningful endeavor. We posited that this transition in belief and behavior evolved for several reasons. First, each group was educated about their own, personal prescribing practices from the outset rather than presenting abstract data. This allowed for ownership of the problem and buy‐in to improve it. Second, participants were able to experience the benefits at an individual level while the interventions were ongoing (eg, having other providers reciprocate structured documentation during patient handoffs, making antimicrobial plans clearer), reinforcing the achievability of stewardship practices within each group. Additionally, we focused on making small, manageable interventions that did not seem disruptive to hospitalists' daily workflow. For example, 1 group instituted antimicrobial timeouts during preexisting multidisciplinary rounds with clinical pharmacists. Last, project champions had both leadership and frontline roles within their groups and set the example for stewardship practices, which conveyed that this was a priority at the leadership level. These findings are in line with those of Charani et al., who evaluated behavior change strategies that influence antimicrobial prescribing in acute care. The authors found that behavioral determinants and social norms strongly influence prescribing practices in acute care, and that antimicrobial stewardship improvement projects should account for these influences.[8]
We also identified several barriers to antimicrobial stewardship implementation (Table 1) and proposed measures to address these barriers in future improvement efforts. For example, hospital medicine programs without a preexisting clinical pharmacy partnership asked hospitalist leadership for more direct clinical pharmacy involvement, recognizing the importance of a physician‐pharmacy alliance for stewardship efforts. To more effectively embed antimicrobial stewardship into daily routine, several hospitalists suggested standardized order sets for commonly encountered infections, as well as routine feedback on prescribing practices. Furthermore, although our simplified antimicrobial guideline pocket card enhanced access to this information, several colleagues suggested a smart phone application that would make access even easier and less cumbersome. Last, given the concern about the sustainability of antimicrobial stewardship initiatives, we recommended periodic reminders, random medical record review, and re‐education if necessary on our 3 strategies and their purpose.
Our study is not without limitations. Each participating hospitalist group enacted hospital‐specific interventions based on individual hospitalist program needs and goals, and although there was collective discussion, no group was tasked to undertake another group's initiative, thereby limiting generalizability. We did, however, identify common facilitators that could be adapted to a wide variety of hospitalist programs. We also note that our 3 main strategies were included in a recent review of quality indicators for measuring the success of antimicrobial stewardship programs; thus, although details of individual practice may vary, in principle these concepts can help identify areas for improvement within each unique stewardship program.[9] Importantly, we were unable to evaluate the impact of the 3 key improvement strategies on important clinical outcomes such as overall antimicrobial use, complications including CDI, and cost. However, others have found that improvement strategies similar to our 3 key processes are associated with meaningful improvements in clinical outcomes as well as reductions in healthcare costs.[10, 11] Last, long‐ term impact and sustainability were not evaluated. By choosing interventions that were viewed by frontline providers as valuable and attainable, however, we feel that each group will likely continue current practices beyond the initial evaluation timeframe.
Although these 5 hospitalist groups were able to successfully implement several aspects of the 3 key improvement strategies, we recognize that this is only the first step. Further effort is needed to quantify the impact of these improvement efforts on objective patient outcomes such as readmissions, length of stay, and antimicrobial‐related complications, which will better inform our local and national leaders on the inherent clinical and financial gains associated with hospitalist‐led stewardship work. Finally, creative ways to better integrate stewardship activities into existing provider workflows (eg, decision support and automation) will further accelerate improvement efforts.
In summary, hospitalists at 5 diverse institutions successfully implemented key antimicrobial improvement strategies and identified important implementation facilitators and barriers. Future efforts at hospitalist‐led stewardship should focus on strategies to scale‐up interventions and evaluate their impact on clinical outcomes and cost.
Acknowledgements
The authors thank Latoya Kuhn, MPH, for her assistance with statistical analyses. We also thank the clinical pharmacists at each institution for their partnership in stewardship efforts: Patrick Arnold, PharmD, and Matthew Tupps, PharmD, MHA, from University of Michigan Hospital and Health System; and Roland Tam, PharmD, from Emory Johns Creek Hospital.
Disclosures: Dr. Flanders reports consulting fees or honoraria from the Institute for Healthcare Improvement, has provided consultancy to the Society of Hospital Medicine, has served as a reviewer for expert testimony, received honoraria as a visiting lecturer to various hospitals, and has received royalties from publisher John Wiley & Sons. He has also received grant funding from Blue Cross Blue Shield of Michigan and the Agency for Healthcare Research and Quality. Dr. Ko reports consultancy for the American Hospital Association and the Society of Hospital Medicine involving work with catheter‐associated urinary tract infections. Ms. Jacobsen reports grant funding from the Institute for Healthcare Improvement. Dr. Rosenberg reports consultancy for Bristol‐Myers Squibb, Forest Pharmaceuticals, and Pfizer. The funding source for this collaborative was through the Institute for Healthcare Improvement and Centers for Disease Control and Prevention. Funding was provided by the Department of Health and Human Services, the Centers for Disease Control and Prevention, the National Center for Emerging Zoonotic and Infectious Diseases, and the Division of Healthcare Quality Promotion/Office of the Director. Avaris Concepts served as the prime contractor and the Institute for Healthcare Improvement as the subcontractor for the initiative. The findings and conclusions in this report represent the views of the authors and might not reflect the views of the Centers for Disease Control and Prevention. The authors report no conflicts of interest.
Inappropriate antimicrobial use in hospitalized patients is a well‐recognized driver for the development of drug‐resistant organisms and antimicrobial‐related complications such as Clostridium difficile infection (CDI).[1, 2] Infection with C difficile affects nearly 500,000 people annually resulting in higher healthcare expenditures, longer lengths of hospital stay, and nearly 15,000 deaths.[3] Data from the Centers for Disease Control and Prevention (CDC) suggest that a 30% reduction in the use of broad‐spectrum antimicrobials, or a 5% reduction in the proportion of hospitalized patients receiving antimicrobials, could equate to a 26% reduction in CDI.[4] It is estimated that up to 50% of antimicrobial use in the hospital setting may be inappropriate.[5]
Since the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America published guidelines for developing formal, hospital‐based antimicrobial stewardship programs in 2007, stewardship practices have been adapted by frontline providers to fit day‐to‐day inpatient care.[5] A recent review by Hamilton et al. described several studies in which stewardship practices were imbedded into daily workflows by way of checklists, education reminders, and periodic review of antimicrobial usage, as well as a multicenter pilot of point‐of‐care stewardship interventions successfully implemented by various providers including nursing, pharmacists, and hospitalists.[6]
In response to the CDC's 2010 Get Smart for Healthcare campaign, which focused on stemming antimicrobial resistance and improving antimicrobial use, the Institute for Healthcare Improvement (IHI), in partnership with the CDC, brought together experts in the field to identify practical and feasible target practices for hospital‐based stewardship and created a Driver Diagram to guide implementation efforts (Figure 1). Rohde et al. described the initial pilot testing of these practices, the decision to more actively engage frontline providers, and the 3 key strategies identified as high‐yield improvement targets: enhancing the visibility of antimicrobial use at the point of care, creating easily accessible antimicrobial guidelines for common infections, and the implementation of a 72‐hour timeout after initiation of antimicrobials.[7]

In this article, we describe how, in partnership with the IHI and the CDC, the hospital medicine programs at 5 diverse hospitals iteratively tested these 3 strategies with a goal of identifying the barriers and facilitators to effective hospitalist‐led antimicrobial stewardship.
METHODS
Representatives from 5 hospital medicine programs, IHI, and the CDC attended a kick‐off meeting at the CDC in November 2012 to discuss the 3 proposed strategies, examples of prior testing, and ideas for implementation. Each hospitalist provided a high‐level summary of the current state of stewardship efforts at their respective institutions, identified possible future states related to the improvement strategies, and anticipated problems in achieving them. The 3 key strategies are described below.
Improved Documentation/Visibility at Points of Care
Making antimicrobial indication, day of therapy, and anticipated duration transparent in the medical record was the targeted improvement strategy to avoid unnecessary antimicrobial days that can result from provider uncertainty, particularly during patient handoffs. Daily hospitalist documentation was identified as a vehicle through which these aspects of antimicrobial use could be effectively communicated and propagated from provider to provider.
Stewardship educational sessions and/or awareness campaigns were hospitalist led, and were accompanied by follow‐up reminders in the forms of emails, texts, flyers, or conferences. Infectious disease physicians were not directly involved in education but were available for consultation if needed.
Improved Guideline Clarity and Accessibility
Enhancing the availability of guidelines for frequently encountered infections and clarifying key guideline recommendations such as treatment duration were identified as the improvement strategies to help make treatment regimens more appropriate and consistent across providers.
Interventions included designing simplified pocket cards for commonly encountered infections, (see Supporting Information, Appendix A, in the online version of this article), collaborating with infectious disease physicians on guideline development, and dissemination through email, smartphone, and wall flyers, and creation of a continuous medical education module focused on stewardship practices.
72‐Hour Antimicrobial Timeout
The 72‐hour antimicrobial timeout required that hospitalists routinely reassess antimicrobial use 72 hours following antimicrobial initiation, a time when most pertinent culture data had returned. Hospitalists partnered with clinical pharmacists at all sites, and addressed the following questions during each timeout: (1) Does the patient have a condition that requires continued use of antimicrobials? (2) Can the current antimicrobial regimen be tailored based on culture data? (3) What is the anticipated treatment duration? A variety of modifications occurred during timeouts, including broadening or narrowing the antimicrobial regimen based on culture data, switching to an oral antimicrobial, adjusting dose or frequency based on patient‐specific factors, as well as discontinuation of antimicrobials. Following the initial timeout, further adjustments were made as the clinical situation dictated; intermittent partnered timeouts continued during a patient's hospitalization on an individualized basis. Hospitalists were encouraged to independently review new diagnostic information daily and make changes as needed outside the dedicated time‐out sessions. All decisions to adjust antimicrobial regimens were provider driven; no hospitals employed automated antimicrobial discontinuation without provider input.
Implementation and Evaluation
Each site was tasked with conducting small tests of change aimed at implementing at least 1, and ideally all 3 strategies. Small, reasonably achievable interventions were preferred to large hospital‐wide initiatives so that key barriers and facilitators to the change could be quickly identified and addressed.
Methods of data collection varied across institutions and included anonymous physician survey, face‐to‐face physician interviews, and medical record review. Evaluations of hospital‐specific interventions utilized convenience samples to obtain real time, actionable data. Postintervention data were distributed through biweekly calls and compiled at the conclusion of the project. Barriers and facilitators of hospitalist‐centered antimicrobial stewardship collected over the course of the project were reviewed and used to identify common themes.
RESULTS
Participating hospitals included 1 community nonteaching hospital, 2 community teaching hospitals, and 2 academic medical centers. All hospitals used computerized order entry and had prior quality improvement experience; 4 out of 5 hospitals used electronic medical records. Postintervention data on antimicrobial documentation and timeouts were compiled, shared, and successes identified. For example, 2 hospitals saw an increase in complete antimicrobial documentation from 4% and 8% to 51% and 65%, respectively, of medical records reviewed over a 3‐month period. Additionally, cumulative timeout data across all hospitals showed that out of 726 antimicrobial timeouts evaluated, optimization or discontinuation occurred 218 times or 30% of the time.
Each site's key implementation barriers and facilitators were collected. Examples were compiled and common themes emerged (Table 1).
| ||
| Barriers: What impediments did we experience during our stewardship project? | Schedule and practice variability | Physician variability in structure of antimicrobial documentation |
| Prescribing etiquette: it's difficult to change course of treatment plan started by a colleague | ||
| Competing schedule demands of hospitalist and pharmacist | ||
| Skepticism of antimicrobial stewardship importance | Perception of incorporating stewardship practices into daily work as time consuming | |
| Improvement project fatigue from competing quality improvement initiatives | ||
| Unclear leadership buy‐in | ||
| Focusing too broadly | Choosing large initial interventions, which take significant time/effort to complete and quantify | |
| Setting unrealistic expectations (eg, expecting perfect adherence to documentation, guidelines, or timeout) | ||
| Facilitators: What countermeasures did we target to overcome barriers? | Engage the hospitalists | Establish a core part of the hospitalist group as stewardship champions |
| Speak 1‐on‐1 to colleagues about specific goals and ways to achieve them | ||
| Establish buy‐in from leadership | ||
| Encourage participation from a multidisciplinary team (eg, bedside nursing, clinical pharmacists) | ||
| Collect real time data and feedback | Utilize a data collection tool if possible/engage hospital coders to identify appropriate diagnoses | |
| Define your question and identify baseline data prior to intervention | ||
| Give rapid cycle feedback to colleagues that can impact antimicrobial prescribing in real time | ||
| Recognize and reward high performers | ||
| Limit scope | Start with small, quickly implementable interventions | |
| Identify interventions that are easy to integrate into hospitalist workflow | ||
DISCUSSION
We successfully brought together hospitalists from diverse institutions to undertake small tests of change aimed at 3 key antimicrobial use improvement strategies. Following our interventions, significant improvement in antimicrobial documentation occurred at 2 institutions focusing on this improvement strategy, and 72‐hour timeouts performed across all hospitals tailored antimicrobial use in 30% of the sessions. Through frequent collaborative discussions and information sharing, we were able to identify common barriers and facilitators to hospitalist‐centered stewardship efforts.
Each participating hospital medicine program noticed a gradual shift in thinking among their colleagues, from initial skepticism about embedding stewardship within their daily workflow, to general acceptance that it was a worthwhile and meaningful endeavor. We posited that this transition in belief and behavior evolved for several reasons. First, each group was educated about their own, personal prescribing practices from the outset rather than presenting abstract data. This allowed for ownership of the problem and buy‐in to improve it. Second, participants were able to experience the benefits at an individual level while the interventions were ongoing (eg, having other providers reciprocate structured documentation during patient handoffs, making antimicrobial plans clearer), reinforcing the achievability of stewardship practices within each group. Additionally, we focused on making small, manageable interventions that did not seem disruptive to hospitalists' daily workflow. For example, 1 group instituted antimicrobial timeouts during preexisting multidisciplinary rounds with clinical pharmacists. Last, project champions had both leadership and frontline roles within their groups and set the example for stewardship practices, which conveyed that this was a priority at the leadership level. These findings are in line with those of Charani et al., who evaluated behavior change strategies that influence antimicrobial prescribing in acute care. The authors found that behavioral determinants and social norms strongly influence prescribing practices in acute care, and that antimicrobial stewardship improvement projects should account for these influences.[8]
We also identified several barriers to antimicrobial stewardship implementation (Table 1) and proposed measures to address these barriers in future improvement efforts. For example, hospital medicine programs without a preexisting clinical pharmacy partnership asked hospitalist leadership for more direct clinical pharmacy involvement, recognizing the importance of a physician‐pharmacy alliance for stewardship efforts. To more effectively embed antimicrobial stewardship into daily routine, several hospitalists suggested standardized order sets for commonly encountered infections, as well as routine feedback on prescribing practices. Furthermore, although our simplified antimicrobial guideline pocket card enhanced access to this information, several colleagues suggested a smart phone application that would make access even easier and less cumbersome. Last, given the concern about the sustainability of antimicrobial stewardship initiatives, we recommended periodic reminders, random medical record review, and re‐education if necessary on our 3 strategies and their purpose.
Our study is not without limitations. Each participating hospitalist group enacted hospital‐specific interventions based on individual hospitalist program needs and goals, and although there was collective discussion, no group was tasked to undertake another group's initiative, thereby limiting generalizability. We did, however, identify common facilitators that could be adapted to a wide variety of hospitalist programs. We also note that our 3 main strategies were included in a recent review of quality indicators for measuring the success of antimicrobial stewardship programs; thus, although details of individual practice may vary, in principle these concepts can help identify areas for improvement within each unique stewardship program.[9] Importantly, we were unable to evaluate the impact of the 3 key improvement strategies on important clinical outcomes such as overall antimicrobial use, complications including CDI, and cost. However, others have found that improvement strategies similar to our 3 key processes are associated with meaningful improvements in clinical outcomes as well as reductions in healthcare costs.[10, 11] Last, long‐ term impact and sustainability were not evaluated. By choosing interventions that were viewed by frontline providers as valuable and attainable, however, we feel that each group will likely continue current practices beyond the initial evaluation timeframe.
Although these 5 hospitalist groups were able to successfully implement several aspects of the 3 key improvement strategies, we recognize that this is only the first step. Further effort is needed to quantify the impact of these improvement efforts on objective patient outcomes such as readmissions, length of stay, and antimicrobial‐related complications, which will better inform our local and national leaders on the inherent clinical and financial gains associated with hospitalist‐led stewardship work. Finally, creative ways to better integrate stewardship activities into existing provider workflows (eg, decision support and automation) will further accelerate improvement efforts.
In summary, hospitalists at 5 diverse institutions successfully implemented key antimicrobial improvement strategies and identified important implementation facilitators and barriers. Future efforts at hospitalist‐led stewardship should focus on strategies to scale‐up interventions and evaluate their impact on clinical outcomes and cost.
Acknowledgements
The authors thank Latoya Kuhn, MPH, for her assistance with statistical analyses. We also thank the clinical pharmacists at each institution for their partnership in stewardship efforts: Patrick Arnold, PharmD, and Matthew Tupps, PharmD, MHA, from University of Michigan Hospital and Health System; and Roland Tam, PharmD, from Emory Johns Creek Hospital.
Disclosures: Dr. Flanders reports consulting fees or honoraria from the Institute for Healthcare Improvement, has provided consultancy to the Society of Hospital Medicine, has served as a reviewer for expert testimony, received honoraria as a visiting lecturer to various hospitals, and has received royalties from publisher John Wiley & Sons. He has also received grant funding from Blue Cross Blue Shield of Michigan and the Agency for Healthcare Research and Quality. Dr. Ko reports consultancy for the American Hospital Association and the Society of Hospital Medicine involving work with catheter‐associated urinary tract infections. Ms. Jacobsen reports grant funding from the Institute for Healthcare Improvement. Dr. Rosenberg reports consultancy for Bristol‐Myers Squibb, Forest Pharmaceuticals, and Pfizer. The funding source for this collaborative was through the Institute for Healthcare Improvement and Centers for Disease Control and Prevention. Funding was provided by the Department of Health and Human Services, the Centers for Disease Control and Prevention, the National Center for Emerging Zoonotic and Infectious Diseases, and the Division of Healthcare Quality Promotion/Office of the Director. Avaris Concepts served as the prime contractor and the Institute for Healthcare Improvement as the subcontractor for the initiative. The findings and conclusions in this report represent the views of the authors and might not reflect the views of the Centers for Disease Control and Prevention. The authors report no conflicts of interest.
- , , . Clinical and economic burden of antimicrobial resistance. Expert Rev Anti Infect Ther. 2008;6(5):751–763.
- , , , et al. Hospital and societal costs of antimicrobial‐resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis. 2009;49(8):1175–1184.
- , , , et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834.
- , , , et al.; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , , et al.; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177.
- , , , et al.; Centers for Disease Control and Prevention Epicenters Program. Point‐of‐prescription interventions to improve antimicrobial stewardship. Clin Infect Dis. 2015;60(8):1252–1258.
- , , . Role of the hospitalist in antimicrobial stewardship: a review of work completed and description of a multisite collaborative. Clin Ther. 2013;35(6):751–757.
- , , , et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53(7):651–662.
- , , , , . Quality indicators to measure appropriate antibiotic use in hospitalized adults. Clin Infect Dis. 2015;60(2):281–291.
- , . Application of antimicrobial stewardship to optimise management of community acquired pneumonia. Int J Clin Pract. 2011;65(7):775–783.
- , , , et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013;4:CD003543.
- , , . Clinical and economic burden of antimicrobial resistance. Expert Rev Anti Infect Ther. 2008;6(5):751–763.
- , , , et al. Hospital and societal costs of antimicrobial‐resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis. 2009;49(8):1175–1184.
- , , , et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834.
- , , , et al.; Centers for Disease Control and Prevention (CDC). Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , , et al.; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177.
- , , , et al.; Centers for Disease Control and Prevention Epicenters Program. Point‐of‐prescription interventions to improve antimicrobial stewardship. Clin Infect Dis. 2015;60(8):1252–1258.
- , , . Role of the hospitalist in antimicrobial stewardship: a review of work completed and description of a multisite collaborative. Clin Ther. 2013;35(6):751–757.
- , , , et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53(7):651–662.
- , , , , . Quality indicators to measure appropriate antibiotic use in hospitalized adults. Clin Infect Dis. 2015;60(2):281–291.
- , . Application of antimicrobial stewardship to optimise management of community acquired pneumonia. Int J Clin Pract. 2011;65(7):775–783.
- , , , et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013;4:CD003543.
Epidemiology of Organ System Dysfunction
The International Consensus Conference (ICC) for sepsis defines severe sepsis as an infection leading to acute organ dysfunction.[1, 2] Severe sepsis afflicts over 1 million patients each year in Medicare alone, and is substantially more common among older Americans than acute myocardial infarction.[3, 4, 5] Recently, the Agency for Healthcare Research and Quality identified severe sepsis as the single most expensive cause of hospitalization in the United States.[6] The incidence of severe sepsis continues to rise.[4, 5]
Severe sepsis is often mischaracterized as a diagnosis cared for primarily in the intensive care unit (ICU). Yet, studies indicate that only 32% to 50% of patients with severe sepsis require ICU care, leaving the majority on the general care wards.[7, 8] These studies also reveal mortality rates of 26% to 30% among patients with severe sepsis who are not admitted to an ICU compared to 11% to 33% in the ICU.[7, 8]
Although a number of epidemiologic and interventional studies have focused on severe sepsis in the ICU,[3, 9, 10] much less is known about patients cared for on the general medicine wards. Without this information, clinicians cannot make informed choices about important management decisions such as targeted diagnostic testing, empirical antimicrobials, and other therapies. To this end, we sought to further characterize the infectious etiologies and resultant organ system dysfunctions in the subset of patients with severe sepsis admitted to non‐ICU medical services at a tertiary academic medical center.
METHODS
Population/Setting
All hospitalizations of adult patients (18 years old) who were initially admitted to non‐ICU medical services at the University of Michigan Hospital during 2009 through 2010 were included. The University of Michigan Hospital has 610 general medical‐surgical beds, including telemetry beds, with closed ICUs comprised of 179 beds staffed by intensivists. Patients transferred from other hospitals and those admitted to non‐medical services were excluded.
Data Abstraction and Definitions
All International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis codes for hospitalizations were screened using a previously published and validated algorithm for severe sepsis.[11] Following this screening, 3 randomly selected round‐numbered batches of hospitalizations were sampled with subsequent application of the exclusion criteria. Medical records including physicians' notes, consultants' notes, nurses' notes, physical therapy notes, discharge coordinators' notes, emergency room flow sheets, as well as ward flow sheets were reviewed in detail by 3 practicing hospitalists using a structured instrument closely aligned with the ICC definition of severe sepsis.[2] We also sampled a smaller number of patients whose ICD‐9‐CM diagnoses screened negative for severe sepsis. Sample size was selected as part of a project with multiple objectives, and reflected a pragmatic balance between the anticipated precision of the results and the resources available to conduct chart review.[11] All discrepancies were reconciled among the 3 reviewers.
Reviewers first assessed whether infection was present, then evaluated for evidence of each organ system dysfunction, and finally determined the extent to which those organ dysfunctions were a response to the infection. Infection was defined either as a patient with a microbiologic culture growing a pathologic organism in a normally sterile site or documentation of a suspected infection with other confirmatory evidence (radiological, physical exam finding) with resultant systemic inflammatory response and administration of antimicrobials. Community‐acquired and healthcare‐associated infections were not differentiated. Microbiologic data, confirmatory tests, and site of infection were abstracted in detail.
Organ dysfunction was defined as per the 2001 ICC criteria,[2] and was assessed for neurological, pulmonary, cardiovascular, renal, gastrointestinal, hematological, and hepatic system involvement in all patients. A summary of these clinical definitions is included in Table 1. Data on important comorbidities were also abstracted. Immunosuppression was defined as having any of the following: solid organ transplant, bone marrow/stem cell transplant, human immunodeficiency virus/acquired immunodeficiency syndrome, neutropenia (absolute neutrophil count <1000), hematologic malignancy, solid organ malignancy with chemotherapy within the past 12 months, or pharmacologic immunosuppression (prednisone >20 mg daily for >4 weeks, calcineurin inhibitor, methotrexate, tumor necrosis factor inhibitors, azathioprine, sulfasalazine, hydroxychloroquine). Last, each chart was evaluated for the presence of explicit documentation with the presence of the words or phrases: sepsis, septic shock, or severe sepsis, indicating that the clinical service recognized and fully documented that a patient had severe sepsis.
| Organ System | Parameters to Indicate Dysfunction |
|---|---|
| |
| Cardiovascular | Systolic BP <90, elevated lactate, MAP <70, requiring pressors >2 hours, decrease in systolic BP of >40 |
| Renal | Creatinine increase >0.5 mg/dL, oliguria |
| Neurological | Acute mental status changes |
| Pulmonary | Intubation, BiPAP, supplemental oxygen >6 LPM or 40% face mask, PaO2/FiO2 <300 |
| Hematologic | INR >1.5 or PTT >60 not on anticoagulation, platelets <100 or 50% of baseline |
| Ileus | Decreased bowel motility requiring a change in diet |
| Hepatic | Bilirubin >4 mg/dL and >1.5 baseline |
Data Analysis
Methods for assessment of reviewer concordance have been previously described and were summarized using the kappa statistic.[11] Initial data extraction was performed in SAS 9.1 (SAS Institute, Cary, NC) and all analyses were conducted in Stata 12 (StataCorp LP, College Station, TX). Binomial 95% confidence intervals (CIs) are presented. This project was approved by the University of Michigan Institutional Review Board.
RESULTS
Of 23,288 hospitalizations examined from 2009 through 2010, the ICD‐9based automated screen for severe sepsis was positive for 3,146 (14 %). A random sample of 111 medical records, of which 92 had screened positive for severe sepsis and 19 had screened negative, was reviewed in detail. After review by the hospitalists, 64 of these 111 hospitalizations were judged to have severe sepsis, 61 of the 92 screened positive cases (66%), and 3 of the 19 screened negative cases (16%). The 3 reviewers had a kappa of 0.70, indicating good agreement.
Characteristics of the 64 patients with severe sepsis are shown in Table 2. The mean age was 63 years old (standard deviation [SD]=17.7), and 41% were male. The mean length of stay was 13.7 days (SD=20.8). Thirty‐nine percent (95% CI, 27%‐52%) of patients (25/64) were immunosuppressed. Of patients initially admitted to the general medical ward, 25% (16/64; 95% CI, 15%‐37%) ultimately required ICU care during their admission. The overall in‐hospital mortality rate was 13% (8/64; 95% CI, 6%‐23%). Immunosuppressed patients had a mortality rate of 20% and nonimmunosuppressed patients had a mortality rate of 8%. Only 47% (30/64; 95% CI, 34%‐60%) of the medical records had explicit clinician documentation of severe sepsis.
| Age, mean (SD), y | 63 (18) |
|---|---|
| |
| Male sex, no. (%) | 26 (41) |
| Preexisting conditions, no. (%) | |
| History of diabetes | 20 (31) |
| End stage renal disease on chronic dialysis | 2 (3) |
| Chronic obstructive pulmonary disease on oxygen | 3 (5) |
| History of cancer | 15 (23) |
| Liver cirrhosis | 5 (8) |
| Immunosuppression | 25 (39) |
| Median length of stay (days) | 7.5 |
| Mean length of stay (SD) | 13.7 (20.8) |
The most common site of infection was found to be the genitourinary system, occurring in 41% (26/64; 95% CI, 29%‐54%) of patients (Table 3). Pulmonary and intra‐abdominal sites were also common, accounting for 14% (95% CI, 6.6%‐25%) and 13% (95% CI, 5.6%‐23%) of sites, respectively. An infecting organism was identified by culture in 66% (42/64; 95% CI, 53%‐77%) of case patients with specific pathogens listed in Table 4. Among patients with positive culture results, the majority grew Gram‐negative organisms (57%; 95% CI, 41%‐72%). Non‐Clostridium difficile Gram‐positive organisms were also prominent and identified in 48% (95% CI, 32%‐64%) of positive cultures. Candida was less common (12%, 95% CI, 4.0%‐26%). Fourteen cases (22%, 95% CI, 10%‐30%) had 2 or more concomitant infectious pathogens.
| Site | No. (%) |
|---|---|
| |
| Genitourinary | 26 (41) |
| Pulmonary | 9 (14) |
| Intra‐abdominal (not intraluminal) | 8 (13) |
| Bloodstream/cardiac | 5 (8) |
| Skin and soft tissue | 4 (6) |
| GI lumen | 4 (6) |
| Joint | 2 (3) |
| Multiple sites | 4 (6) |
| Unknown | 2 (2) |
| Absolute Frequency, Total Positive Culture Results, N=64, No. (%)*?>a | Patients With Cultures Growing at Least One of the Pathogens, N=42, No. (%)*?>a | |
|---|---|---|
| ||
| Gram‐negative pathogens | 30 (47) | 24 (57) |
| Escherichia coli | 12 (19) | 12 (29) |
| Escherichia coli (multidrug resistant) | 2 (3) | 2 (5) |
| Klebsiella | 6 (9) | 5 (12) |
| Pseudomonas aeruginosa | 6 (9) | 4 (10) |
| Pseudomonas aeruginosa (multidrug resistant) | 2 (3) | 2 (5) |
| Otherb | 6 (9) | 6 (14) |
| Gram‐positive pathogens | 29 (45) | 25 (59) |
| Enterococcus | 14 (22) | 13 (31) |
| Vancomycin‐resistant Enterococcus species | 5 (8) | 4 (10) |
| Staphylococcus aureus | 7 (11) | 7 (17) |
| Methicillin‐resistant Staphylococcus aureus | 3 (5) | 3 (7) |
| Streptococcus pneumoniae | 2 (3) | 2 (5) |
| Coagulase‐negative staphylococci | 1 (2) | 1 (2) |
| Clostridium difficile | 5 (8) | 5 (12) |
| Fungi | ||
| Candida species | 5 (8) | 5 (12) |
| Mycobacterium avium | 1 (2) | 1 (2) |
| Two organisms | 9 (21) | |
| Three or more organisms | 5 (12) | |
All 64 patients had at least 1 organ dysfunction, as required by the ICC definition of severe sepsis. Organ dysfunction in 2 or more organ systems occurred in 77% (95% CI, 64%‐86%) of the cases (49/64). The incidence for each organ system dysfunction is presented in Table 5, as well as its relationship to both mortality and ICU admission. The most common organ system dysfunctions were found to be cardiovascular (hypotension) and renal dysfunction occurring in 66% and 64% of the cases, respectively. In this non‐ICU population, pulmonary dysfunction occurred in 30% of cases, but was frequently associated with transfer to the ICU, as 63% of the patients with pulmonary failure required ICU care. Patients with more organ systems affected were more likely to be transferred to the ICU and to die.
| No. (%) | ICU Transfer, No. (%) | Mortality, No. (%) | |
|---|---|---|---|
| |||
| Number of failed organs, N = 64 | |||
| 1 | 15 (23%) | 0 (0%) | 0 (0%) |
| 2 | 25 (39%) | 2 (8%) | 0 (0%) |
| 3 | 7 (11%) | 2 (29%) | 1 (14%) |
| 4 | 10 (16%) | 6 (60%) | 3 (30%) |
| >4 | 7 (11%) | 6 (86%) | 4 (57%) |
| Types of organ system dysfunction, all patients, N = 64*?>a | |||
| Cardiovascular | 42 (66%) | 16 (38%)b | 8 (19%)c |
| Renal | 41 (64%) | 10 (24%)b | 5 (12%)c |
| Central nervous system | 35 (54%) | 14 (40%)b | 7 (18%)c |
| Pulmonary | 19 (30%) | 12 (63%)b | 8 (42%)c |
| Hematologic | 15 (23%) | 6 (40%)b | 6 (40%)c |
| GI (ileus) | 8 (13%) | 5 (63%)b | 1 (13%)c |
| Hepatic | 5 (8%) | 4 (80%)b | 2 (40%)c |
DISCUSSION
Severe sepsis was common among patients admitted to the general medical ward in this tertiary care center. Our patient cohort differed in important ways from previously described typical cases of severe sepsis among ICU populations. Severe sepsis on the general medical wards was more commonly associated with Gram‐negative pathogens in the setting of genitourinary tract infections. This is in contrast to Gram‐positive organisms and respiratory tract infections, which are more common in the ICU.[3, 10] Renal and cardiac dysfunction were commonly observed organ failures, whereas in the ICU, severe sepsis has been reported to more likely involve respiratory failure. These results suggest that hospitalists seeking to provide evidence‐based care to prevent postsepsis morbidity and mortality for their non‐ICU patients need to heighten their index of suspicion when caring for an infected patient and appreciate that many severe sepsis patients may not fit neatly into traditional sepsis treatment algorithms.
Studies characterizing severe sepsis in the ICU setting indicate a predominance of pulmonary infections and respiratory failure with occurrence rates of 74% to 95% and 54% to 61%, respectively.[3, 12, 13] Given that either shock or pulmonary dysfunction is often required for admission to many ICUs, it is perhaps not surprising that these rates are dramatically different on the general medicine ward, with a relative scarcity of pulmonary infections (14%) and respiratory dysfunction (30%). Instead, genitourinary infections were noted in 41% (95% CI, 29%‐54%) of the cases, in contrast to the rates of genitourinary infections in ICU patients with severe sepsis, which have rates of 5.4% to 9.1%.[3, 10] Likely as a result of this, a Gram‐negative predominance is noted in the associated microbiology. Furthermore, our study indicates that C difficile and vancomycin‐resistant Enterococcus (VRE) species appear to represent an emerging cause of severe sepsis on the general medicine wards, as they have not been noted to be causative micro‐organisms in previous studies of sepsis. This is concordant with other studies showing increases in incidence and severity of disease for C difficile as well as VRE.[14, 15]
Previous epidemiologic studies of severe sepsis originating outside the ICU are lacking, but some work has been done. One study on the epidemiology of sepsis both with and without organ dysfunction aggregated all hospitalized patients and included those both admitted to the general medicine wards and directly to the ICU.[7] Similar to our study, this study also found a predominance of Gram‐negative causative organisms, as well as comparable in‐hospital mortality rates (12.8% vs 13%). Additionally, genitourinary infections were noted in 20% of the patients, notably higher than rates reported to have been found in patients with severe sepsis in the ICU, but not the magnitude found in our study, perhaps as a result of the combined ICU‐ward population studied. A similar high prevalence of genitourinary infections was also noted in a recent administrative data‐based study of emergency medical services‐transported patients with severe sepsis, half of whom required intensive care during their hospitalization.[16]
Our study is unique in that it focuses on severe sepsis in patients, commonly cared for by hospitalists, who were admitted to the general medical ward, and uses patient level data to elucidate more characteristics of the defining organ dysfunction. Furthermore, our results suggest that severe sepsis was poorly documented in this setting, indicating a potential impact on billing, coding, case mix index, and hospital mortality statistics that rely on very specific wording, as well as a possible need for increased awareness among hospitalists. Without this awareness, an opportunity may be missed for improved patient care via specific sepsis‐targeted measures,[13, 17, 18] including more aggressive resuscitative measures[19] or intensive physical and occupational therapy interventions aimed at impacting the cognitive and functional debilities[20] that result from severe sepsis. Highlighting this growing need to better assist clinicians assess the severity of septic patients and recognize these complex cases on the general medicine wards, 1 recent study evaluated the fitness of several clinical disease‐severity scoring systems for patients with sepsis in general internal medicine departments.[21] Perhaps with the help of tools such as these, which are being piloted in some hospitals, the care of this growing population can be enhanced.
Our study has a number of limitations that should be kept in mind. First, this is a single center study performed at an academic tertiary care center with a relatively high incidence of immunosuppression, which may influence the spectrum of infecting organisms. Our center also has a relatively large, closed‐model ICU, which often operates at near capacity, potentially affecting the severity of our non‐ICU population. Second, although we screened a large number of patients, as necessitated by our intensive and detailed review of clinical information, our sample size with hospitalist‐validated severe sepsis is relatively small. With this small sample size, less prevalent infections, patient characteristics, and organ dysfunctions may by chance have been under or over‐represented, and one could expect some variance in the occurrence rates of organ system dysfunction and infection rates by sampling error alone. Further larger scale studies are warranted to confirm these data and their generalizability. Third, the data necessary to calculate sequential organ failure assessment or multiple organ dysfunction score were not collected. This may limit the ability to directly compare the organ dysfunction noted in this study with others. Additionally, given the ICC definitions of organ dysfunction, some of the organ dysfunction noted, particularly for neurological dysfunction, was reliant on subjective clinical findings documented in the record. Finally, we relied on the lack of specific terminology to indicate a lack of documentation of sepsis, which does not necessarily indicate a lack of recognition or undertreatment of this condition. However, these limitations are offset by the strengths of this study, including the patient‐level medical record validation of severe sepsis by trained hospitalist physicians, high kappa statistic, and strict application of guideline‐based definitions.
This work has important implications for both clinicians and for future research on severe sepsis. The results suggest that severe sepsis may be quite common outside the ICU, and that patients presenting with this condition who are admitted to general medical wards are not routinely characterized by the profound hypoxemia and refractory shock of iconic cases. Certainly, further study looking at larger numbers of cases is needed to better understand the specifics and nuances of this important topic as well as to further evaluate clinicians' ability to recognize and treat such patients in this setting. Furthermore, future research on the treatment of severe sepsis, including both antimicrobials and disease‐modifying agents (eg, anti‐inflammatories) must continue to include and even focus on this large population of non‐ICU patients with severe sepsis, as the risk/benefit ratios of such potential treatments may vary with severity of illness.
In conclusion, severe sepsis was commonly found in patients admitted on the general medicine wards. The epidemiology of the infections and resultant organ dysfunction appears to differ from that found in the ICU. More studies are needed to provide a deeper understanding of this disease process, as this will enable clinicians to better recognize and treat patients thus afflicted, no matter the setting.
Acknowledgments
The authors thank Laetitia Shapiro, AM, for her programming assistance.
Disclosures: This work was supported in part by the US National Institutes of HealthK08, HL091249 (TJI) and the University of Michigan SpecialistHospitalist Allied Research Program (SHARP). This work was also supported in part by VA Ann Arbor Healthcare System, Geriatric Research Education and Clinical Center (GRECC).
- , , , et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655.
- , , , et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–1256.
- , , , , , . Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310.
- , , , . Population burden of long‐term survivorship after severe sepsis in older americans. J Am Geriatr Soc. 2012;60(6):1070–1077.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , . Septicemia in U.S. hospitals, 2009: statistical brief #122. October 2011. In: Healthcare Cost and Utilization Project Statistical Briefs. Rockville, MD: Agency for Health Care Policy and Research; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK65391. Accessed June 2, 2012.
- , , , et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med. 2007;35(5):1284–1289.
- , , , , . Epidemiology of sepsis in Victoria, Australia. Crit Care Med. 2005;33(1):71–80.
- , , , et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis‐related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012;307(22):2390–2399.
- , , , , . Incidence and impact of organ dysfunctions associated with sepsis. Chest. 2005;127(3):942–951.
- , , , et al. Identifying patients with severe sepsis using administrative claims: patient‐level validation of the Angus Implementation of the International Consensus Conference definition of severe sepsis [published online ahead of print September 18, 2012]. Medical Care. doi: 10.1097/MLR.0b013e318268ac86.
- , , , . Current epidemiology of septic shock: the CUB‐Rea Network. Am J Respir Crit Care Med. 2003;168(2):165–172.
- . Management of sepsis. N Engl J Med. 2006;355(16):1699–1713.
- , , . Current status of Clostridium difficile infection ipidemiology. Clin Infect Dis. 2012;55(suppl 2):S65–S70.
- , . Vancomycin‐resistant enterococci. Semin Respir Infect. 2000;15(4):314–326.
- , , , , , . Severe sepsis in prehospital emergency care: analysis of incidence, care, and outcome. Am J Respir Crit Care Med. 2012;186(12):1264–1271.
- , . Novel Therapies for Septic Shock Over the Past 4 Decades. JAMA. 2011;306(2):194–199.
- , , , et al. Impact of the Surviving Sepsis Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study. Crit Care Med. 2010;38(4):1036–1043.
- , . Diagnosis and treatment of severe sepsis. Crit Care. 2007;11(suppl 5):S2.
- , , , . Long‐term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794.
- , , , , . Assessment of disease‐severity scoring systems for patients with sepsis in general internal medicine departments. Crit Care. 2011;15:R95.
The International Consensus Conference (ICC) for sepsis defines severe sepsis as an infection leading to acute organ dysfunction.[1, 2] Severe sepsis afflicts over 1 million patients each year in Medicare alone, and is substantially more common among older Americans than acute myocardial infarction.[3, 4, 5] Recently, the Agency for Healthcare Research and Quality identified severe sepsis as the single most expensive cause of hospitalization in the United States.[6] The incidence of severe sepsis continues to rise.[4, 5]
Severe sepsis is often mischaracterized as a diagnosis cared for primarily in the intensive care unit (ICU). Yet, studies indicate that only 32% to 50% of patients with severe sepsis require ICU care, leaving the majority on the general care wards.[7, 8] These studies also reveal mortality rates of 26% to 30% among patients with severe sepsis who are not admitted to an ICU compared to 11% to 33% in the ICU.[7, 8]
Although a number of epidemiologic and interventional studies have focused on severe sepsis in the ICU,[3, 9, 10] much less is known about patients cared for on the general medicine wards. Without this information, clinicians cannot make informed choices about important management decisions such as targeted diagnostic testing, empirical antimicrobials, and other therapies. To this end, we sought to further characterize the infectious etiologies and resultant organ system dysfunctions in the subset of patients with severe sepsis admitted to non‐ICU medical services at a tertiary academic medical center.
METHODS
Population/Setting
All hospitalizations of adult patients (18 years old) who were initially admitted to non‐ICU medical services at the University of Michigan Hospital during 2009 through 2010 were included. The University of Michigan Hospital has 610 general medical‐surgical beds, including telemetry beds, with closed ICUs comprised of 179 beds staffed by intensivists. Patients transferred from other hospitals and those admitted to non‐medical services were excluded.
Data Abstraction and Definitions
All International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis codes for hospitalizations were screened using a previously published and validated algorithm for severe sepsis.[11] Following this screening, 3 randomly selected round‐numbered batches of hospitalizations were sampled with subsequent application of the exclusion criteria. Medical records including physicians' notes, consultants' notes, nurses' notes, physical therapy notes, discharge coordinators' notes, emergency room flow sheets, as well as ward flow sheets were reviewed in detail by 3 practicing hospitalists using a structured instrument closely aligned with the ICC definition of severe sepsis.[2] We also sampled a smaller number of patients whose ICD‐9‐CM diagnoses screened negative for severe sepsis. Sample size was selected as part of a project with multiple objectives, and reflected a pragmatic balance between the anticipated precision of the results and the resources available to conduct chart review.[11] All discrepancies were reconciled among the 3 reviewers.
Reviewers first assessed whether infection was present, then evaluated for evidence of each organ system dysfunction, and finally determined the extent to which those organ dysfunctions were a response to the infection. Infection was defined either as a patient with a microbiologic culture growing a pathologic organism in a normally sterile site or documentation of a suspected infection with other confirmatory evidence (radiological, physical exam finding) with resultant systemic inflammatory response and administration of antimicrobials. Community‐acquired and healthcare‐associated infections were not differentiated. Microbiologic data, confirmatory tests, and site of infection were abstracted in detail.
Organ dysfunction was defined as per the 2001 ICC criteria,[2] and was assessed for neurological, pulmonary, cardiovascular, renal, gastrointestinal, hematological, and hepatic system involvement in all patients. A summary of these clinical definitions is included in Table 1. Data on important comorbidities were also abstracted. Immunosuppression was defined as having any of the following: solid organ transplant, bone marrow/stem cell transplant, human immunodeficiency virus/acquired immunodeficiency syndrome, neutropenia (absolute neutrophil count <1000), hematologic malignancy, solid organ malignancy with chemotherapy within the past 12 months, or pharmacologic immunosuppression (prednisone >20 mg daily for >4 weeks, calcineurin inhibitor, methotrexate, tumor necrosis factor inhibitors, azathioprine, sulfasalazine, hydroxychloroquine). Last, each chart was evaluated for the presence of explicit documentation with the presence of the words or phrases: sepsis, septic shock, or severe sepsis, indicating that the clinical service recognized and fully documented that a patient had severe sepsis.
| Organ System | Parameters to Indicate Dysfunction |
|---|---|
| |
| Cardiovascular | Systolic BP <90, elevated lactate, MAP <70, requiring pressors >2 hours, decrease in systolic BP of >40 |
| Renal | Creatinine increase >0.5 mg/dL, oliguria |
| Neurological | Acute mental status changes |
| Pulmonary | Intubation, BiPAP, supplemental oxygen >6 LPM or 40% face mask, PaO2/FiO2 <300 |
| Hematologic | INR >1.5 or PTT >60 not on anticoagulation, platelets <100 or 50% of baseline |
| Ileus | Decreased bowel motility requiring a change in diet |
| Hepatic | Bilirubin >4 mg/dL and >1.5 baseline |
Data Analysis
Methods for assessment of reviewer concordance have been previously described and were summarized using the kappa statistic.[11] Initial data extraction was performed in SAS 9.1 (SAS Institute, Cary, NC) and all analyses were conducted in Stata 12 (StataCorp LP, College Station, TX). Binomial 95% confidence intervals (CIs) are presented. This project was approved by the University of Michigan Institutional Review Board.
RESULTS
Of 23,288 hospitalizations examined from 2009 through 2010, the ICD‐9based automated screen for severe sepsis was positive for 3,146 (14 %). A random sample of 111 medical records, of which 92 had screened positive for severe sepsis and 19 had screened negative, was reviewed in detail. After review by the hospitalists, 64 of these 111 hospitalizations were judged to have severe sepsis, 61 of the 92 screened positive cases (66%), and 3 of the 19 screened negative cases (16%). The 3 reviewers had a kappa of 0.70, indicating good agreement.
Characteristics of the 64 patients with severe sepsis are shown in Table 2. The mean age was 63 years old (standard deviation [SD]=17.7), and 41% were male. The mean length of stay was 13.7 days (SD=20.8). Thirty‐nine percent (95% CI, 27%‐52%) of patients (25/64) were immunosuppressed. Of patients initially admitted to the general medical ward, 25% (16/64; 95% CI, 15%‐37%) ultimately required ICU care during their admission. The overall in‐hospital mortality rate was 13% (8/64; 95% CI, 6%‐23%). Immunosuppressed patients had a mortality rate of 20% and nonimmunosuppressed patients had a mortality rate of 8%. Only 47% (30/64; 95% CI, 34%‐60%) of the medical records had explicit clinician documentation of severe sepsis.
| Age, mean (SD), y | 63 (18) |
|---|---|
| |
| Male sex, no. (%) | 26 (41) |
| Preexisting conditions, no. (%) | |
| History of diabetes | 20 (31) |
| End stage renal disease on chronic dialysis | 2 (3) |
| Chronic obstructive pulmonary disease on oxygen | 3 (5) |
| History of cancer | 15 (23) |
| Liver cirrhosis | 5 (8) |
| Immunosuppression | 25 (39) |
| Median length of stay (days) | 7.5 |
| Mean length of stay (SD) | 13.7 (20.8) |
The most common site of infection was found to be the genitourinary system, occurring in 41% (26/64; 95% CI, 29%‐54%) of patients (Table 3). Pulmonary and intra‐abdominal sites were also common, accounting for 14% (95% CI, 6.6%‐25%) and 13% (95% CI, 5.6%‐23%) of sites, respectively. An infecting organism was identified by culture in 66% (42/64; 95% CI, 53%‐77%) of case patients with specific pathogens listed in Table 4. Among patients with positive culture results, the majority grew Gram‐negative organisms (57%; 95% CI, 41%‐72%). Non‐Clostridium difficile Gram‐positive organisms were also prominent and identified in 48% (95% CI, 32%‐64%) of positive cultures. Candida was less common (12%, 95% CI, 4.0%‐26%). Fourteen cases (22%, 95% CI, 10%‐30%) had 2 or more concomitant infectious pathogens.
| Site | No. (%) |
|---|---|
| |
| Genitourinary | 26 (41) |
| Pulmonary | 9 (14) |
| Intra‐abdominal (not intraluminal) | 8 (13) |
| Bloodstream/cardiac | 5 (8) |
| Skin and soft tissue | 4 (6) |
| GI lumen | 4 (6) |
| Joint | 2 (3) |
| Multiple sites | 4 (6) |
| Unknown | 2 (2) |
| Absolute Frequency, Total Positive Culture Results, N=64, No. (%)*?>a | Patients With Cultures Growing at Least One of the Pathogens, N=42, No. (%)*?>a | |
|---|---|---|
| ||
| Gram‐negative pathogens | 30 (47) | 24 (57) |
| Escherichia coli | 12 (19) | 12 (29) |
| Escherichia coli (multidrug resistant) | 2 (3) | 2 (5) |
| Klebsiella | 6 (9) | 5 (12) |
| Pseudomonas aeruginosa | 6 (9) | 4 (10) |
| Pseudomonas aeruginosa (multidrug resistant) | 2 (3) | 2 (5) |
| Otherb | 6 (9) | 6 (14) |
| Gram‐positive pathogens | 29 (45) | 25 (59) |
| Enterococcus | 14 (22) | 13 (31) |
| Vancomycin‐resistant Enterococcus species | 5 (8) | 4 (10) |
| Staphylococcus aureus | 7 (11) | 7 (17) |
| Methicillin‐resistant Staphylococcus aureus | 3 (5) | 3 (7) |
| Streptococcus pneumoniae | 2 (3) | 2 (5) |
| Coagulase‐negative staphylococci | 1 (2) | 1 (2) |
| Clostridium difficile | 5 (8) | 5 (12) |
| Fungi | ||
| Candida species | 5 (8) | 5 (12) |
| Mycobacterium avium | 1 (2) | 1 (2) |
| Two organisms | 9 (21) | |
| Three or more organisms | 5 (12) | |
All 64 patients had at least 1 organ dysfunction, as required by the ICC definition of severe sepsis. Organ dysfunction in 2 or more organ systems occurred in 77% (95% CI, 64%‐86%) of the cases (49/64). The incidence for each organ system dysfunction is presented in Table 5, as well as its relationship to both mortality and ICU admission. The most common organ system dysfunctions were found to be cardiovascular (hypotension) and renal dysfunction occurring in 66% and 64% of the cases, respectively. In this non‐ICU population, pulmonary dysfunction occurred in 30% of cases, but was frequently associated with transfer to the ICU, as 63% of the patients with pulmonary failure required ICU care. Patients with more organ systems affected were more likely to be transferred to the ICU and to die.
| No. (%) | ICU Transfer, No. (%) | Mortality, No. (%) | |
|---|---|---|---|
| |||
| Number of failed organs, N = 64 | |||
| 1 | 15 (23%) | 0 (0%) | 0 (0%) |
| 2 | 25 (39%) | 2 (8%) | 0 (0%) |
| 3 | 7 (11%) | 2 (29%) | 1 (14%) |
| 4 | 10 (16%) | 6 (60%) | 3 (30%) |
| >4 | 7 (11%) | 6 (86%) | 4 (57%) |
| Types of organ system dysfunction, all patients, N = 64*?>a | |||
| Cardiovascular | 42 (66%) | 16 (38%)b | 8 (19%)c |
| Renal | 41 (64%) | 10 (24%)b | 5 (12%)c |
| Central nervous system | 35 (54%) | 14 (40%)b | 7 (18%)c |
| Pulmonary | 19 (30%) | 12 (63%)b | 8 (42%)c |
| Hematologic | 15 (23%) | 6 (40%)b | 6 (40%)c |
| GI (ileus) | 8 (13%) | 5 (63%)b | 1 (13%)c |
| Hepatic | 5 (8%) | 4 (80%)b | 2 (40%)c |
DISCUSSION
Severe sepsis was common among patients admitted to the general medical ward in this tertiary care center. Our patient cohort differed in important ways from previously described typical cases of severe sepsis among ICU populations. Severe sepsis on the general medical wards was more commonly associated with Gram‐negative pathogens in the setting of genitourinary tract infections. This is in contrast to Gram‐positive organisms and respiratory tract infections, which are more common in the ICU.[3, 10] Renal and cardiac dysfunction were commonly observed organ failures, whereas in the ICU, severe sepsis has been reported to more likely involve respiratory failure. These results suggest that hospitalists seeking to provide evidence‐based care to prevent postsepsis morbidity and mortality for their non‐ICU patients need to heighten their index of suspicion when caring for an infected patient and appreciate that many severe sepsis patients may not fit neatly into traditional sepsis treatment algorithms.
Studies characterizing severe sepsis in the ICU setting indicate a predominance of pulmonary infections and respiratory failure with occurrence rates of 74% to 95% and 54% to 61%, respectively.[3, 12, 13] Given that either shock or pulmonary dysfunction is often required for admission to many ICUs, it is perhaps not surprising that these rates are dramatically different on the general medicine ward, with a relative scarcity of pulmonary infections (14%) and respiratory dysfunction (30%). Instead, genitourinary infections were noted in 41% (95% CI, 29%‐54%) of the cases, in contrast to the rates of genitourinary infections in ICU patients with severe sepsis, which have rates of 5.4% to 9.1%.[3, 10] Likely as a result of this, a Gram‐negative predominance is noted in the associated microbiology. Furthermore, our study indicates that C difficile and vancomycin‐resistant Enterococcus (VRE) species appear to represent an emerging cause of severe sepsis on the general medicine wards, as they have not been noted to be causative micro‐organisms in previous studies of sepsis. This is concordant with other studies showing increases in incidence and severity of disease for C difficile as well as VRE.[14, 15]
Previous epidemiologic studies of severe sepsis originating outside the ICU are lacking, but some work has been done. One study on the epidemiology of sepsis both with and without organ dysfunction aggregated all hospitalized patients and included those both admitted to the general medicine wards and directly to the ICU.[7] Similar to our study, this study also found a predominance of Gram‐negative causative organisms, as well as comparable in‐hospital mortality rates (12.8% vs 13%). Additionally, genitourinary infections were noted in 20% of the patients, notably higher than rates reported to have been found in patients with severe sepsis in the ICU, but not the magnitude found in our study, perhaps as a result of the combined ICU‐ward population studied. A similar high prevalence of genitourinary infections was also noted in a recent administrative data‐based study of emergency medical services‐transported patients with severe sepsis, half of whom required intensive care during their hospitalization.[16]
Our study is unique in that it focuses on severe sepsis in patients, commonly cared for by hospitalists, who were admitted to the general medical ward, and uses patient level data to elucidate more characteristics of the defining organ dysfunction. Furthermore, our results suggest that severe sepsis was poorly documented in this setting, indicating a potential impact on billing, coding, case mix index, and hospital mortality statistics that rely on very specific wording, as well as a possible need for increased awareness among hospitalists. Without this awareness, an opportunity may be missed for improved patient care via specific sepsis‐targeted measures,[13, 17, 18] including more aggressive resuscitative measures[19] or intensive physical and occupational therapy interventions aimed at impacting the cognitive and functional debilities[20] that result from severe sepsis. Highlighting this growing need to better assist clinicians assess the severity of septic patients and recognize these complex cases on the general medicine wards, 1 recent study evaluated the fitness of several clinical disease‐severity scoring systems for patients with sepsis in general internal medicine departments.[21] Perhaps with the help of tools such as these, which are being piloted in some hospitals, the care of this growing population can be enhanced.
Our study has a number of limitations that should be kept in mind. First, this is a single center study performed at an academic tertiary care center with a relatively high incidence of immunosuppression, which may influence the spectrum of infecting organisms. Our center also has a relatively large, closed‐model ICU, which often operates at near capacity, potentially affecting the severity of our non‐ICU population. Second, although we screened a large number of patients, as necessitated by our intensive and detailed review of clinical information, our sample size with hospitalist‐validated severe sepsis is relatively small. With this small sample size, less prevalent infections, patient characteristics, and organ dysfunctions may by chance have been under or over‐represented, and one could expect some variance in the occurrence rates of organ system dysfunction and infection rates by sampling error alone. Further larger scale studies are warranted to confirm these data and their generalizability. Third, the data necessary to calculate sequential organ failure assessment or multiple organ dysfunction score were not collected. This may limit the ability to directly compare the organ dysfunction noted in this study with others. Additionally, given the ICC definitions of organ dysfunction, some of the organ dysfunction noted, particularly for neurological dysfunction, was reliant on subjective clinical findings documented in the record. Finally, we relied on the lack of specific terminology to indicate a lack of documentation of sepsis, which does not necessarily indicate a lack of recognition or undertreatment of this condition. However, these limitations are offset by the strengths of this study, including the patient‐level medical record validation of severe sepsis by trained hospitalist physicians, high kappa statistic, and strict application of guideline‐based definitions.
This work has important implications for both clinicians and for future research on severe sepsis. The results suggest that severe sepsis may be quite common outside the ICU, and that patients presenting with this condition who are admitted to general medical wards are not routinely characterized by the profound hypoxemia and refractory shock of iconic cases. Certainly, further study looking at larger numbers of cases is needed to better understand the specifics and nuances of this important topic as well as to further evaluate clinicians' ability to recognize and treat such patients in this setting. Furthermore, future research on the treatment of severe sepsis, including both antimicrobials and disease‐modifying agents (eg, anti‐inflammatories) must continue to include and even focus on this large population of non‐ICU patients with severe sepsis, as the risk/benefit ratios of such potential treatments may vary with severity of illness.
In conclusion, severe sepsis was commonly found in patients admitted on the general medicine wards. The epidemiology of the infections and resultant organ dysfunction appears to differ from that found in the ICU. More studies are needed to provide a deeper understanding of this disease process, as this will enable clinicians to better recognize and treat patients thus afflicted, no matter the setting.
Acknowledgments
The authors thank Laetitia Shapiro, AM, for her programming assistance.
Disclosures: This work was supported in part by the US National Institutes of HealthK08, HL091249 (TJI) and the University of Michigan SpecialistHospitalist Allied Research Program (SHARP). This work was also supported in part by VA Ann Arbor Healthcare System, Geriatric Research Education and Clinical Center (GRECC).
The International Consensus Conference (ICC) for sepsis defines severe sepsis as an infection leading to acute organ dysfunction.[1, 2] Severe sepsis afflicts over 1 million patients each year in Medicare alone, and is substantially more common among older Americans than acute myocardial infarction.[3, 4, 5] Recently, the Agency for Healthcare Research and Quality identified severe sepsis as the single most expensive cause of hospitalization in the United States.[6] The incidence of severe sepsis continues to rise.[4, 5]
Severe sepsis is often mischaracterized as a diagnosis cared for primarily in the intensive care unit (ICU). Yet, studies indicate that only 32% to 50% of patients with severe sepsis require ICU care, leaving the majority on the general care wards.[7, 8] These studies also reveal mortality rates of 26% to 30% among patients with severe sepsis who are not admitted to an ICU compared to 11% to 33% in the ICU.[7, 8]
Although a number of epidemiologic and interventional studies have focused on severe sepsis in the ICU,[3, 9, 10] much less is known about patients cared for on the general medicine wards. Without this information, clinicians cannot make informed choices about important management decisions such as targeted diagnostic testing, empirical antimicrobials, and other therapies. To this end, we sought to further characterize the infectious etiologies and resultant organ system dysfunctions in the subset of patients with severe sepsis admitted to non‐ICU medical services at a tertiary academic medical center.
METHODS
Population/Setting
All hospitalizations of adult patients (18 years old) who were initially admitted to non‐ICU medical services at the University of Michigan Hospital during 2009 through 2010 were included. The University of Michigan Hospital has 610 general medical‐surgical beds, including telemetry beds, with closed ICUs comprised of 179 beds staffed by intensivists. Patients transferred from other hospitals and those admitted to non‐medical services were excluded.
Data Abstraction and Definitions
All International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis codes for hospitalizations were screened using a previously published and validated algorithm for severe sepsis.[11] Following this screening, 3 randomly selected round‐numbered batches of hospitalizations were sampled with subsequent application of the exclusion criteria. Medical records including physicians' notes, consultants' notes, nurses' notes, physical therapy notes, discharge coordinators' notes, emergency room flow sheets, as well as ward flow sheets were reviewed in detail by 3 practicing hospitalists using a structured instrument closely aligned with the ICC definition of severe sepsis.[2] We also sampled a smaller number of patients whose ICD‐9‐CM diagnoses screened negative for severe sepsis. Sample size was selected as part of a project with multiple objectives, and reflected a pragmatic balance between the anticipated precision of the results and the resources available to conduct chart review.[11] All discrepancies were reconciled among the 3 reviewers.
Reviewers first assessed whether infection was present, then evaluated for evidence of each organ system dysfunction, and finally determined the extent to which those organ dysfunctions were a response to the infection. Infection was defined either as a patient with a microbiologic culture growing a pathologic organism in a normally sterile site or documentation of a suspected infection with other confirmatory evidence (radiological, physical exam finding) with resultant systemic inflammatory response and administration of antimicrobials. Community‐acquired and healthcare‐associated infections were not differentiated. Microbiologic data, confirmatory tests, and site of infection were abstracted in detail.
Organ dysfunction was defined as per the 2001 ICC criteria,[2] and was assessed for neurological, pulmonary, cardiovascular, renal, gastrointestinal, hematological, and hepatic system involvement in all patients. A summary of these clinical definitions is included in Table 1. Data on important comorbidities were also abstracted. Immunosuppression was defined as having any of the following: solid organ transplant, bone marrow/stem cell transplant, human immunodeficiency virus/acquired immunodeficiency syndrome, neutropenia (absolute neutrophil count <1000), hematologic malignancy, solid organ malignancy with chemotherapy within the past 12 months, or pharmacologic immunosuppression (prednisone >20 mg daily for >4 weeks, calcineurin inhibitor, methotrexate, tumor necrosis factor inhibitors, azathioprine, sulfasalazine, hydroxychloroquine). Last, each chart was evaluated for the presence of explicit documentation with the presence of the words or phrases: sepsis, septic shock, or severe sepsis, indicating that the clinical service recognized and fully documented that a patient had severe sepsis.
| Organ System | Parameters to Indicate Dysfunction |
|---|---|
| |
| Cardiovascular | Systolic BP <90, elevated lactate, MAP <70, requiring pressors >2 hours, decrease in systolic BP of >40 |
| Renal | Creatinine increase >0.5 mg/dL, oliguria |
| Neurological | Acute mental status changes |
| Pulmonary | Intubation, BiPAP, supplemental oxygen >6 LPM or 40% face mask, PaO2/FiO2 <300 |
| Hematologic | INR >1.5 or PTT >60 not on anticoagulation, platelets <100 or 50% of baseline |
| Ileus | Decreased bowel motility requiring a change in diet |
| Hepatic | Bilirubin >4 mg/dL and >1.5 baseline |
Data Analysis
Methods for assessment of reviewer concordance have been previously described and were summarized using the kappa statistic.[11] Initial data extraction was performed in SAS 9.1 (SAS Institute, Cary, NC) and all analyses were conducted in Stata 12 (StataCorp LP, College Station, TX). Binomial 95% confidence intervals (CIs) are presented. This project was approved by the University of Michigan Institutional Review Board.
RESULTS
Of 23,288 hospitalizations examined from 2009 through 2010, the ICD‐9based automated screen for severe sepsis was positive for 3,146 (14 %). A random sample of 111 medical records, of which 92 had screened positive for severe sepsis and 19 had screened negative, was reviewed in detail. After review by the hospitalists, 64 of these 111 hospitalizations were judged to have severe sepsis, 61 of the 92 screened positive cases (66%), and 3 of the 19 screened negative cases (16%). The 3 reviewers had a kappa of 0.70, indicating good agreement.
Characteristics of the 64 patients with severe sepsis are shown in Table 2. The mean age was 63 years old (standard deviation [SD]=17.7), and 41% were male. The mean length of stay was 13.7 days (SD=20.8). Thirty‐nine percent (95% CI, 27%‐52%) of patients (25/64) were immunosuppressed. Of patients initially admitted to the general medical ward, 25% (16/64; 95% CI, 15%‐37%) ultimately required ICU care during their admission. The overall in‐hospital mortality rate was 13% (8/64; 95% CI, 6%‐23%). Immunosuppressed patients had a mortality rate of 20% and nonimmunosuppressed patients had a mortality rate of 8%. Only 47% (30/64; 95% CI, 34%‐60%) of the medical records had explicit clinician documentation of severe sepsis.
| Age, mean (SD), y | 63 (18) |
|---|---|
| |
| Male sex, no. (%) | 26 (41) |
| Preexisting conditions, no. (%) | |
| History of diabetes | 20 (31) |
| End stage renal disease on chronic dialysis | 2 (3) |
| Chronic obstructive pulmonary disease on oxygen | 3 (5) |
| History of cancer | 15 (23) |
| Liver cirrhosis | 5 (8) |
| Immunosuppression | 25 (39) |
| Median length of stay (days) | 7.5 |
| Mean length of stay (SD) | 13.7 (20.8) |
The most common site of infection was found to be the genitourinary system, occurring in 41% (26/64; 95% CI, 29%‐54%) of patients (Table 3). Pulmonary and intra‐abdominal sites were also common, accounting for 14% (95% CI, 6.6%‐25%) and 13% (95% CI, 5.6%‐23%) of sites, respectively. An infecting organism was identified by culture in 66% (42/64; 95% CI, 53%‐77%) of case patients with specific pathogens listed in Table 4. Among patients with positive culture results, the majority grew Gram‐negative organisms (57%; 95% CI, 41%‐72%). Non‐Clostridium difficile Gram‐positive organisms were also prominent and identified in 48% (95% CI, 32%‐64%) of positive cultures. Candida was less common (12%, 95% CI, 4.0%‐26%). Fourteen cases (22%, 95% CI, 10%‐30%) had 2 or more concomitant infectious pathogens.
| Site | No. (%) |
|---|---|
| |
| Genitourinary | 26 (41) |
| Pulmonary | 9 (14) |
| Intra‐abdominal (not intraluminal) | 8 (13) |
| Bloodstream/cardiac | 5 (8) |
| Skin and soft tissue | 4 (6) |
| GI lumen | 4 (6) |
| Joint | 2 (3) |
| Multiple sites | 4 (6) |
| Unknown | 2 (2) |
| Absolute Frequency, Total Positive Culture Results, N=64, No. (%)*?>a | Patients With Cultures Growing at Least One of the Pathogens, N=42, No. (%)*?>a | |
|---|---|---|
| ||
| Gram‐negative pathogens | 30 (47) | 24 (57) |
| Escherichia coli | 12 (19) | 12 (29) |
| Escherichia coli (multidrug resistant) | 2 (3) | 2 (5) |
| Klebsiella | 6 (9) | 5 (12) |
| Pseudomonas aeruginosa | 6 (9) | 4 (10) |
| Pseudomonas aeruginosa (multidrug resistant) | 2 (3) | 2 (5) |
| Otherb | 6 (9) | 6 (14) |
| Gram‐positive pathogens | 29 (45) | 25 (59) |
| Enterococcus | 14 (22) | 13 (31) |
| Vancomycin‐resistant Enterococcus species | 5 (8) | 4 (10) |
| Staphylococcus aureus | 7 (11) | 7 (17) |
| Methicillin‐resistant Staphylococcus aureus | 3 (5) | 3 (7) |
| Streptococcus pneumoniae | 2 (3) | 2 (5) |
| Coagulase‐negative staphylococci | 1 (2) | 1 (2) |
| Clostridium difficile | 5 (8) | 5 (12) |
| Fungi | ||
| Candida species | 5 (8) | 5 (12) |
| Mycobacterium avium | 1 (2) | 1 (2) |
| Two organisms | 9 (21) | |
| Three or more organisms | 5 (12) | |
All 64 patients had at least 1 organ dysfunction, as required by the ICC definition of severe sepsis. Organ dysfunction in 2 or more organ systems occurred in 77% (95% CI, 64%‐86%) of the cases (49/64). The incidence for each organ system dysfunction is presented in Table 5, as well as its relationship to both mortality and ICU admission. The most common organ system dysfunctions were found to be cardiovascular (hypotension) and renal dysfunction occurring in 66% and 64% of the cases, respectively. In this non‐ICU population, pulmonary dysfunction occurred in 30% of cases, but was frequently associated with transfer to the ICU, as 63% of the patients with pulmonary failure required ICU care. Patients with more organ systems affected were more likely to be transferred to the ICU and to die.
| No. (%) | ICU Transfer, No. (%) | Mortality, No. (%) | |
|---|---|---|---|
| |||
| Number of failed organs, N = 64 | |||
| 1 | 15 (23%) | 0 (0%) | 0 (0%) |
| 2 | 25 (39%) | 2 (8%) | 0 (0%) |
| 3 | 7 (11%) | 2 (29%) | 1 (14%) |
| 4 | 10 (16%) | 6 (60%) | 3 (30%) |
| >4 | 7 (11%) | 6 (86%) | 4 (57%) |
| Types of organ system dysfunction, all patients, N = 64*?>a | |||
| Cardiovascular | 42 (66%) | 16 (38%)b | 8 (19%)c |
| Renal | 41 (64%) | 10 (24%)b | 5 (12%)c |
| Central nervous system | 35 (54%) | 14 (40%)b | 7 (18%)c |
| Pulmonary | 19 (30%) | 12 (63%)b | 8 (42%)c |
| Hematologic | 15 (23%) | 6 (40%)b | 6 (40%)c |
| GI (ileus) | 8 (13%) | 5 (63%)b | 1 (13%)c |
| Hepatic | 5 (8%) | 4 (80%)b | 2 (40%)c |
DISCUSSION
Severe sepsis was common among patients admitted to the general medical ward in this tertiary care center. Our patient cohort differed in important ways from previously described typical cases of severe sepsis among ICU populations. Severe sepsis on the general medical wards was more commonly associated with Gram‐negative pathogens in the setting of genitourinary tract infections. This is in contrast to Gram‐positive organisms and respiratory tract infections, which are more common in the ICU.[3, 10] Renal and cardiac dysfunction were commonly observed organ failures, whereas in the ICU, severe sepsis has been reported to more likely involve respiratory failure. These results suggest that hospitalists seeking to provide evidence‐based care to prevent postsepsis morbidity and mortality for their non‐ICU patients need to heighten their index of suspicion when caring for an infected patient and appreciate that many severe sepsis patients may not fit neatly into traditional sepsis treatment algorithms.
Studies characterizing severe sepsis in the ICU setting indicate a predominance of pulmonary infections and respiratory failure with occurrence rates of 74% to 95% and 54% to 61%, respectively.[3, 12, 13] Given that either shock or pulmonary dysfunction is often required for admission to many ICUs, it is perhaps not surprising that these rates are dramatically different on the general medicine ward, with a relative scarcity of pulmonary infections (14%) and respiratory dysfunction (30%). Instead, genitourinary infections were noted in 41% (95% CI, 29%‐54%) of the cases, in contrast to the rates of genitourinary infections in ICU patients with severe sepsis, which have rates of 5.4% to 9.1%.[3, 10] Likely as a result of this, a Gram‐negative predominance is noted in the associated microbiology. Furthermore, our study indicates that C difficile and vancomycin‐resistant Enterococcus (VRE) species appear to represent an emerging cause of severe sepsis on the general medicine wards, as they have not been noted to be causative micro‐organisms in previous studies of sepsis. This is concordant with other studies showing increases in incidence and severity of disease for C difficile as well as VRE.[14, 15]
Previous epidemiologic studies of severe sepsis originating outside the ICU are lacking, but some work has been done. One study on the epidemiology of sepsis both with and without organ dysfunction aggregated all hospitalized patients and included those both admitted to the general medicine wards and directly to the ICU.[7] Similar to our study, this study also found a predominance of Gram‐negative causative organisms, as well as comparable in‐hospital mortality rates (12.8% vs 13%). Additionally, genitourinary infections were noted in 20% of the patients, notably higher than rates reported to have been found in patients with severe sepsis in the ICU, but not the magnitude found in our study, perhaps as a result of the combined ICU‐ward population studied. A similar high prevalence of genitourinary infections was also noted in a recent administrative data‐based study of emergency medical services‐transported patients with severe sepsis, half of whom required intensive care during their hospitalization.[16]
Our study is unique in that it focuses on severe sepsis in patients, commonly cared for by hospitalists, who were admitted to the general medical ward, and uses patient level data to elucidate more characteristics of the defining organ dysfunction. Furthermore, our results suggest that severe sepsis was poorly documented in this setting, indicating a potential impact on billing, coding, case mix index, and hospital mortality statistics that rely on very specific wording, as well as a possible need for increased awareness among hospitalists. Without this awareness, an opportunity may be missed for improved patient care via specific sepsis‐targeted measures,[13, 17, 18] including more aggressive resuscitative measures[19] or intensive physical and occupational therapy interventions aimed at impacting the cognitive and functional debilities[20] that result from severe sepsis. Highlighting this growing need to better assist clinicians assess the severity of septic patients and recognize these complex cases on the general medicine wards, 1 recent study evaluated the fitness of several clinical disease‐severity scoring systems for patients with sepsis in general internal medicine departments.[21] Perhaps with the help of tools such as these, which are being piloted in some hospitals, the care of this growing population can be enhanced.
Our study has a number of limitations that should be kept in mind. First, this is a single center study performed at an academic tertiary care center with a relatively high incidence of immunosuppression, which may influence the spectrum of infecting organisms. Our center also has a relatively large, closed‐model ICU, which often operates at near capacity, potentially affecting the severity of our non‐ICU population. Second, although we screened a large number of patients, as necessitated by our intensive and detailed review of clinical information, our sample size with hospitalist‐validated severe sepsis is relatively small. With this small sample size, less prevalent infections, patient characteristics, and organ dysfunctions may by chance have been under or over‐represented, and one could expect some variance in the occurrence rates of organ system dysfunction and infection rates by sampling error alone. Further larger scale studies are warranted to confirm these data and their generalizability. Third, the data necessary to calculate sequential organ failure assessment or multiple organ dysfunction score were not collected. This may limit the ability to directly compare the organ dysfunction noted in this study with others. Additionally, given the ICC definitions of organ dysfunction, some of the organ dysfunction noted, particularly for neurological dysfunction, was reliant on subjective clinical findings documented in the record. Finally, we relied on the lack of specific terminology to indicate a lack of documentation of sepsis, which does not necessarily indicate a lack of recognition or undertreatment of this condition. However, these limitations are offset by the strengths of this study, including the patient‐level medical record validation of severe sepsis by trained hospitalist physicians, high kappa statistic, and strict application of guideline‐based definitions.
This work has important implications for both clinicians and for future research on severe sepsis. The results suggest that severe sepsis may be quite common outside the ICU, and that patients presenting with this condition who are admitted to general medical wards are not routinely characterized by the profound hypoxemia and refractory shock of iconic cases. Certainly, further study looking at larger numbers of cases is needed to better understand the specifics and nuances of this important topic as well as to further evaluate clinicians' ability to recognize and treat such patients in this setting. Furthermore, future research on the treatment of severe sepsis, including both antimicrobials and disease‐modifying agents (eg, anti‐inflammatories) must continue to include and even focus on this large population of non‐ICU patients with severe sepsis, as the risk/benefit ratios of such potential treatments may vary with severity of illness.
In conclusion, severe sepsis was commonly found in patients admitted on the general medicine wards. The epidemiology of the infections and resultant organ dysfunction appears to differ from that found in the ICU. More studies are needed to provide a deeper understanding of this disease process, as this will enable clinicians to better recognize and treat patients thus afflicted, no matter the setting.
Acknowledgments
The authors thank Laetitia Shapiro, AM, for her programming assistance.
Disclosures: This work was supported in part by the US National Institutes of HealthK08, HL091249 (TJI) and the University of Michigan SpecialistHospitalist Allied Research Program (SHARP). This work was also supported in part by VA Ann Arbor Healthcare System, Geriatric Research Education and Clinical Center (GRECC).
- , , , et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655.
- , , , et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–1256.
- , , , , , . Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310.
- , , , . Population burden of long‐term survivorship after severe sepsis in older americans. J Am Geriatr Soc. 2012;60(6):1070–1077.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , . Septicemia in U.S. hospitals, 2009: statistical brief #122. October 2011. In: Healthcare Cost and Utilization Project Statistical Briefs. Rockville, MD: Agency for Health Care Policy and Research; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK65391. Accessed June 2, 2012.
- , , , et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med. 2007;35(5):1284–1289.
- , , , , . Epidemiology of sepsis in Victoria, Australia. Crit Care Med. 2005;33(1):71–80.
- , , , et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis‐related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012;307(22):2390–2399.
- , , , , . Incidence and impact of organ dysfunctions associated with sepsis. Chest. 2005;127(3):942–951.
- , , , et al. Identifying patients with severe sepsis using administrative claims: patient‐level validation of the Angus Implementation of the International Consensus Conference definition of severe sepsis [published online ahead of print September 18, 2012]. Medical Care. doi: 10.1097/MLR.0b013e318268ac86.
- , , , . Current epidemiology of septic shock: the CUB‐Rea Network. Am J Respir Crit Care Med. 2003;168(2):165–172.
- . Management of sepsis. N Engl J Med. 2006;355(16):1699–1713.
- , , . Current status of Clostridium difficile infection ipidemiology. Clin Infect Dis. 2012;55(suppl 2):S65–S70.
- , . Vancomycin‐resistant enterococci. Semin Respir Infect. 2000;15(4):314–326.
- , , , , , . Severe sepsis in prehospital emergency care: analysis of incidence, care, and outcome. Am J Respir Crit Care Med. 2012;186(12):1264–1271.
- , . Novel Therapies for Septic Shock Over the Past 4 Decades. JAMA. 2011;306(2):194–199.
- , , , et al. Impact of the Surviving Sepsis Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study. Crit Care Med. 2010;38(4):1036–1043.
- , . Diagnosis and treatment of severe sepsis. Crit Care. 2007;11(suppl 5):S2.
- , , , . Long‐term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794.
- , , , , . Assessment of disease‐severity scoring systems for patients with sepsis in general internal medicine departments. Crit Care. 2011;15:R95.
- , , , et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655.
- , , , et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–1256.
- , , , , , . Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310.
- , , , . Population burden of long‐term survivorship after severe sepsis in older americans. J Am Geriatr Soc. 2012;60(6):1070–1077.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , . Septicemia in U.S. hospitals, 2009: statistical brief #122. October 2011. In: Healthcare Cost and Utilization Project Statistical Briefs. Rockville, MD: Agency for Health Care Policy and Research; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK65391. Accessed June 2, 2012.
- , , , et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med. 2007;35(5):1284–1289.
- , , , , . Epidemiology of sepsis in Victoria, Australia. Crit Care Med. 2005;33(1):71–80.
- , , , et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis‐related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012;307(22):2390–2399.
- , , , , . Incidence and impact of organ dysfunctions associated with sepsis. Chest. 2005;127(3):942–951.
- , , , et al. Identifying patients with severe sepsis using administrative claims: patient‐level validation of the Angus Implementation of the International Consensus Conference definition of severe sepsis [published online ahead of print September 18, 2012]. Medical Care. doi: 10.1097/MLR.0b013e318268ac86.
- , , , . Current epidemiology of septic shock: the CUB‐Rea Network. Am J Respir Crit Care Med. 2003;168(2):165–172.
- . Management of sepsis. N Engl J Med. 2006;355(16):1699–1713.
- , , . Current status of Clostridium difficile infection ipidemiology. Clin Infect Dis. 2012;55(suppl 2):S65–S70.
- , . Vancomycin‐resistant enterococci. Semin Respir Infect. 2000;15(4):314–326.
- , , , , , . Severe sepsis in prehospital emergency care: analysis of incidence, care, and outcome. Am J Respir Crit Care Med. 2012;186(12):1264–1271.
- , . Novel Therapies for Septic Shock Over the Past 4 Decades. JAMA. 2011;306(2):194–199.
- , , , et al. Impact of the Surviving Sepsis Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study. Crit Care Med. 2010;38(4):1036–1043.
- , . Diagnosis and treatment of severe sepsis. Crit Care. 2007;11(suppl 5):S2.
- , , , . Long‐term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794.
- , , , , . Assessment of disease‐severity scoring systems for patients with sepsis in general internal medicine departments. Crit Care. 2011;15:R95.
Copyright © 2013 Society of Hospital Medicine
Prevention of Intravascular, Catheter-Related Infections
Background
have become a ubiquitous feature of modern-day patient care; current estimates suggest that as many as 2 million persons in the U.S. have an intravascular device that is used daily or intermittently.1 These devices fulfill a variety of clinical needs, including monitoring acutely ill patients and the administration of critical medications, in a variety of settings, including ICUs, medical and surgical units, and the outpatient setting.
This important therapeutic role comes with associated risks, including the possibility of bloodstream infection, which leads to an increase in morbidity, length of stay, and cost. Each year in the ICU alone, 80,000 catheter-related bloodstream infections (CRBSIs) occur. This figure increases to 250,000 to 500,000 infections per year when all hospitalized patients are considered.1,2
Infections related to intravascular catheters have been targeted by numerous quality-improvement (QI) initiatives, uncovering a number of clinical actions that can impact their rates. Studies have shown that these infections can be avoided and nearly eliminated entirely with close adherence to several evidence-based, infection-control measures.3 Furthermore, these results can be sustained across multiple ICUs over extended periods.4
The majority of data that describe the epidemiology of CRBSIs and the interventions needed to prevent these infections have been generated in the ICU. However, the pervasiveness of these devices in other care settings dictates the need for heightened awareness by the entire care team. As such, it is important for hospitalists to understand and be aware of guidelines outlining the standard of care not only in personal practice, but also in order to ensure that all members of the team are playing their part in preventing this serious complication.
Guideline Update
In May 2011, the Society of Critical Care Medicine (SCCM), in collaboration with 14 other professional organizations, published new guidelines for the prevention of intravascular catheter-related infections.5 These guidelines are a revision of guidelines published in 2002 and provide recommendations that apply to all intravascular catheters, as well as specific comments based on the type of device in use.6
Specific recommendations include:
- Responsible staff should be well-versed and assessed on the proper procedures for the care of all intravascular catheters with designated personnel responsible for central venous catheters (CVCs)
- and peripherally inserted central catheters (PICCs).
- Prior to CVC and arterial catheter insertion and during dressing changes, an antiseptic solution containing more than 0.5% chlorhexidine with alcohol should be used to prepare the skin.
- Nontunneled CVCs should be preferentially placed in a subclavian site rather than a jugular or a femoral site, except in hemodialysis or advanced kidney disease patients, for which this may cause subclavian stenosis, with the understanding that the risks of placing a CVC at a site be weighed against its benefits.
- Skilled personnel should use ultrasound guidance during CVC placement, and the minimal essential number of ports or lumens on the CVC should be present. Avoidance of routine placement of CVCs and prompt removal of any nonessential intravascular catheter is recommended.
- Maximal sterile barrier precautions should be taken during the placement of CVCs and PICCs or guidewire exchange, which includes a sterile full-body drape for the patient and use of cap, mask, sterile gown, and gloves for personnel. After the catheter has been placed, it should be secured with a sutureless securement device. In addition, patients with these intravascular catheters should bathe with 2% chlorhexidine daily.
- If rates of CLABSI remain high despite adherence to education/training, appropriate antisepsis, and maximal sterile barrier precautions, the use of antiseptic- or antibiotic-impregnated, short-term CVCs and chlorhexadine-impregnanted sponge dressings might help to further decrease rates.5
No single intervention alone appears to be sufficient to significantly reduce CRBSI rates. Therefore, the guideline recommends “bundling” several of these individual best practices into a streamlined approach—inclusive of feedback to healthcare personnel on infection rates and compliance—thereby promoting quality assurance and performance improvement. This bundling tactic makes best practices a priority and a reality, and offers the largest potential impact on the prevention of intravascular catheter-related infections.5
Analysis
Practical recommendations to assist clinicians in preventing CLABSI also were put forth in 2008 guidelines by the Society for Healthcare Epidemiology of America (SHEA) and Infectious Disease Society of America (IDSA).7 Compared to the SCCM guidelines, these guidelines are more focused on CVCs and do not directly address other available intravascular devices (PICCs, hemodialysis catheters, etc.). Beyond this, the SCCM guidelines also discuss the microbiology of infection, surveillance measures, and the specifics of the performance improvement measures involved in their implementation, which are not found in the SHEA and IDSA guidelines.
Numerous national initiatives and measures have been established based on these and other clinical practice guidelines. The Joint Commission recently produced the new monograph “Preventing Central Line-Associated Infections: A Global Challenge, A Global Perspective,” listing “Use proven guidelines to prevent infection of the blood from central lines” as one of its National Patient Safety Goals.8 The Institute for Healthcare Improvement (IHI) created its Central Line Bundle along with its “How-To Guide: Prevent CLABSI in 2011,” which has been implemented by many hospitals in the U.S. and United Kingdom. The IHI bundle has resulted in dozens of hospitals achieving more than a year of no CLABSIs in their ICU patients, and many have expanded the program to other areas of the hospital.9
Giving further impetus toward efforts to prevent these complications, the Centers for Medicare & Medicaid Services (CMS) determined that vascular-catheter-associated infections are hospital-acquired conditions that will no longer be reimbursed, as outlined in 2008 in the Acute Inpatient Prospective Payment System.10 Therefore, hospitals will not receive additional payment for these infections acquired during hospitalization (i.e. was not present on admission), and the case is paid as though the costly infection were not present, thus aligning improved patient care and outcomes with the financial bottom line for hospital reimbursement.
HM Takeaways
Given the significant economic and clinical burden of intravascular-device-related infections, hospital staffs should be aware of and adopt proven interventions to minimize this important complication. No one single intervention can meaningfully impact this infection rate, but a “bundled approach” appears to be the most influential.
Dr. Rohde is a hospitalist and assistant professor of internal medicine and Dr. Hartley is a hospitalist and clinical instructor of internal medicine at the University of Michigan Hospital and Health Systems in Ann Arbor.
Background
have become a ubiquitous feature of modern-day patient care; current estimates suggest that as many as 2 million persons in the U.S. have an intravascular device that is used daily or intermittently.1 These devices fulfill a variety of clinical needs, including monitoring acutely ill patients and the administration of critical medications, in a variety of settings, including ICUs, medical and surgical units, and the outpatient setting.
This important therapeutic role comes with associated risks, including the possibility of bloodstream infection, which leads to an increase in morbidity, length of stay, and cost. Each year in the ICU alone, 80,000 catheter-related bloodstream infections (CRBSIs) occur. This figure increases to 250,000 to 500,000 infections per year when all hospitalized patients are considered.1,2
Infections related to intravascular catheters have been targeted by numerous quality-improvement (QI) initiatives, uncovering a number of clinical actions that can impact their rates. Studies have shown that these infections can be avoided and nearly eliminated entirely with close adherence to several evidence-based, infection-control measures.3 Furthermore, these results can be sustained across multiple ICUs over extended periods.4
The majority of data that describe the epidemiology of CRBSIs and the interventions needed to prevent these infections have been generated in the ICU. However, the pervasiveness of these devices in other care settings dictates the need for heightened awareness by the entire care team. As such, it is important for hospitalists to understand and be aware of guidelines outlining the standard of care not only in personal practice, but also in order to ensure that all members of the team are playing their part in preventing this serious complication.
Guideline Update
In May 2011, the Society of Critical Care Medicine (SCCM), in collaboration with 14 other professional organizations, published new guidelines for the prevention of intravascular catheter-related infections.5 These guidelines are a revision of guidelines published in 2002 and provide recommendations that apply to all intravascular catheters, as well as specific comments based on the type of device in use.6
Specific recommendations include:
- Responsible staff should be well-versed and assessed on the proper procedures for the care of all intravascular catheters with designated personnel responsible for central venous catheters (CVCs)
- and peripherally inserted central catheters (PICCs).
- Prior to CVC and arterial catheter insertion and during dressing changes, an antiseptic solution containing more than 0.5% chlorhexidine with alcohol should be used to prepare the skin.
- Nontunneled CVCs should be preferentially placed in a subclavian site rather than a jugular or a femoral site, except in hemodialysis or advanced kidney disease patients, for which this may cause subclavian stenosis, with the understanding that the risks of placing a CVC at a site be weighed against its benefits.
- Skilled personnel should use ultrasound guidance during CVC placement, and the minimal essential number of ports or lumens on the CVC should be present. Avoidance of routine placement of CVCs and prompt removal of any nonessential intravascular catheter is recommended.
- Maximal sterile barrier precautions should be taken during the placement of CVCs and PICCs or guidewire exchange, which includes a sterile full-body drape for the patient and use of cap, mask, sterile gown, and gloves for personnel. After the catheter has been placed, it should be secured with a sutureless securement device. In addition, patients with these intravascular catheters should bathe with 2% chlorhexidine daily.
- If rates of CLABSI remain high despite adherence to education/training, appropriate antisepsis, and maximal sterile barrier precautions, the use of antiseptic- or antibiotic-impregnated, short-term CVCs and chlorhexadine-impregnanted sponge dressings might help to further decrease rates.5
No single intervention alone appears to be sufficient to significantly reduce CRBSI rates. Therefore, the guideline recommends “bundling” several of these individual best practices into a streamlined approach—inclusive of feedback to healthcare personnel on infection rates and compliance—thereby promoting quality assurance and performance improvement. This bundling tactic makes best practices a priority and a reality, and offers the largest potential impact on the prevention of intravascular catheter-related infections.5
Analysis
Practical recommendations to assist clinicians in preventing CLABSI also were put forth in 2008 guidelines by the Society for Healthcare Epidemiology of America (SHEA) and Infectious Disease Society of America (IDSA).7 Compared to the SCCM guidelines, these guidelines are more focused on CVCs and do not directly address other available intravascular devices (PICCs, hemodialysis catheters, etc.). Beyond this, the SCCM guidelines also discuss the microbiology of infection, surveillance measures, and the specifics of the performance improvement measures involved in their implementation, which are not found in the SHEA and IDSA guidelines.
Numerous national initiatives and measures have been established based on these and other clinical practice guidelines. The Joint Commission recently produced the new monograph “Preventing Central Line-Associated Infections: A Global Challenge, A Global Perspective,” listing “Use proven guidelines to prevent infection of the blood from central lines” as one of its National Patient Safety Goals.8 The Institute for Healthcare Improvement (IHI) created its Central Line Bundle along with its “How-To Guide: Prevent CLABSI in 2011,” which has been implemented by many hospitals in the U.S. and United Kingdom. The IHI bundle has resulted in dozens of hospitals achieving more than a year of no CLABSIs in their ICU patients, and many have expanded the program to other areas of the hospital.9
Giving further impetus toward efforts to prevent these complications, the Centers for Medicare & Medicaid Services (CMS) determined that vascular-catheter-associated infections are hospital-acquired conditions that will no longer be reimbursed, as outlined in 2008 in the Acute Inpatient Prospective Payment System.10 Therefore, hospitals will not receive additional payment for these infections acquired during hospitalization (i.e. was not present on admission), and the case is paid as though the costly infection were not present, thus aligning improved patient care and outcomes with the financial bottom line for hospital reimbursement.
HM Takeaways
Given the significant economic and clinical burden of intravascular-device-related infections, hospital staffs should be aware of and adopt proven interventions to minimize this important complication. No one single intervention can meaningfully impact this infection rate, but a “bundled approach” appears to be the most influential.
Dr. Rohde is a hospitalist and assistant professor of internal medicine and Dr. Hartley is a hospitalist and clinical instructor of internal medicine at the University of Michigan Hospital and Health Systems in Ann Arbor.
Background
have become a ubiquitous feature of modern-day patient care; current estimates suggest that as many as 2 million persons in the U.S. have an intravascular device that is used daily or intermittently.1 These devices fulfill a variety of clinical needs, including monitoring acutely ill patients and the administration of critical medications, in a variety of settings, including ICUs, medical and surgical units, and the outpatient setting.
This important therapeutic role comes with associated risks, including the possibility of bloodstream infection, which leads to an increase in morbidity, length of stay, and cost. Each year in the ICU alone, 80,000 catheter-related bloodstream infections (CRBSIs) occur. This figure increases to 250,000 to 500,000 infections per year when all hospitalized patients are considered.1,2
Infections related to intravascular catheters have been targeted by numerous quality-improvement (QI) initiatives, uncovering a number of clinical actions that can impact their rates. Studies have shown that these infections can be avoided and nearly eliminated entirely with close adherence to several evidence-based, infection-control measures.3 Furthermore, these results can be sustained across multiple ICUs over extended periods.4
The majority of data that describe the epidemiology of CRBSIs and the interventions needed to prevent these infections have been generated in the ICU. However, the pervasiveness of these devices in other care settings dictates the need for heightened awareness by the entire care team. As such, it is important for hospitalists to understand and be aware of guidelines outlining the standard of care not only in personal practice, but also in order to ensure that all members of the team are playing their part in preventing this serious complication.
Guideline Update
In May 2011, the Society of Critical Care Medicine (SCCM), in collaboration with 14 other professional organizations, published new guidelines for the prevention of intravascular catheter-related infections.5 These guidelines are a revision of guidelines published in 2002 and provide recommendations that apply to all intravascular catheters, as well as specific comments based on the type of device in use.6
Specific recommendations include:
- Responsible staff should be well-versed and assessed on the proper procedures for the care of all intravascular catheters with designated personnel responsible for central venous catheters (CVCs)
- and peripherally inserted central catheters (PICCs).
- Prior to CVC and arterial catheter insertion and during dressing changes, an antiseptic solution containing more than 0.5% chlorhexidine with alcohol should be used to prepare the skin.
- Nontunneled CVCs should be preferentially placed in a subclavian site rather than a jugular or a femoral site, except in hemodialysis or advanced kidney disease patients, for which this may cause subclavian stenosis, with the understanding that the risks of placing a CVC at a site be weighed against its benefits.
- Skilled personnel should use ultrasound guidance during CVC placement, and the minimal essential number of ports or lumens on the CVC should be present. Avoidance of routine placement of CVCs and prompt removal of any nonessential intravascular catheter is recommended.
- Maximal sterile barrier precautions should be taken during the placement of CVCs and PICCs or guidewire exchange, which includes a sterile full-body drape for the patient and use of cap, mask, sterile gown, and gloves for personnel. After the catheter has been placed, it should be secured with a sutureless securement device. In addition, patients with these intravascular catheters should bathe with 2% chlorhexidine daily.
- If rates of CLABSI remain high despite adherence to education/training, appropriate antisepsis, and maximal sterile barrier precautions, the use of antiseptic- or antibiotic-impregnated, short-term CVCs and chlorhexadine-impregnanted sponge dressings might help to further decrease rates.5
No single intervention alone appears to be sufficient to significantly reduce CRBSI rates. Therefore, the guideline recommends “bundling” several of these individual best practices into a streamlined approach—inclusive of feedback to healthcare personnel on infection rates and compliance—thereby promoting quality assurance and performance improvement. This bundling tactic makes best practices a priority and a reality, and offers the largest potential impact on the prevention of intravascular catheter-related infections.5
Analysis
Practical recommendations to assist clinicians in preventing CLABSI also were put forth in 2008 guidelines by the Society for Healthcare Epidemiology of America (SHEA) and Infectious Disease Society of America (IDSA).7 Compared to the SCCM guidelines, these guidelines are more focused on CVCs and do not directly address other available intravascular devices (PICCs, hemodialysis catheters, etc.). Beyond this, the SCCM guidelines also discuss the microbiology of infection, surveillance measures, and the specifics of the performance improvement measures involved in their implementation, which are not found in the SHEA and IDSA guidelines.
Numerous national initiatives and measures have been established based on these and other clinical practice guidelines. The Joint Commission recently produced the new monograph “Preventing Central Line-Associated Infections: A Global Challenge, A Global Perspective,” listing “Use proven guidelines to prevent infection of the blood from central lines” as one of its National Patient Safety Goals.8 The Institute for Healthcare Improvement (IHI) created its Central Line Bundle along with its “How-To Guide: Prevent CLABSI in 2011,” which has been implemented by many hospitals in the U.S. and United Kingdom. The IHI bundle has resulted in dozens of hospitals achieving more than a year of no CLABSIs in their ICU patients, and many have expanded the program to other areas of the hospital.9
Giving further impetus toward efforts to prevent these complications, the Centers for Medicare & Medicaid Services (CMS) determined that vascular-catheter-associated infections are hospital-acquired conditions that will no longer be reimbursed, as outlined in 2008 in the Acute Inpatient Prospective Payment System.10 Therefore, hospitals will not receive additional payment for these infections acquired during hospitalization (i.e. was not present on admission), and the case is paid as though the costly infection were not present, thus aligning improved patient care and outcomes with the financial bottom line for hospital reimbursement.
HM Takeaways
Given the significant economic and clinical burden of intravascular-device-related infections, hospital staffs should be aware of and adopt proven interventions to minimize this important complication. No one single intervention can meaningfully impact this infection rate, but a “bundled approach” appears to be the most influential.
Dr. Rohde is a hospitalist and assistant professor of internal medicine and Dr. Hartley is a hospitalist and clinical instructor of internal medicine at the University of Michigan Hospital and Health Systems in Ann Arbor.
What is the best initial treatment of an adult patient with healthcare-associated pneumonia?
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at jcarris@wiley.com.
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at jcarris@wiley.com.
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at jcarris@wiley.com.