User login
Building Tailored Resource Guides to Address Social Risks and Advance Health Equity in the Veterans Health Administration
Social risk factors and social needs have significant, often cumulative, impacts on health outcomes and are closely tied to health inequities. Defined as the individual-level adverse social conditions associated with poor health, social risk factors broadly include experiences such as food insecurity and housing instability; whereas the term social needs incorporates a person’s perceptions of and priorities related to their health-related needs.1 One recent study examining data from the Veterans Health Administration (VHA) found a 27% higher odds of mortality with each additional identified social risk, underscoring the critical link between social risks and veteran health outcomes.2
Assessing Circumstances and Offering Resources for Needs (ACORN), a collaborative quality improvement initiative conducted in partnership with the VHA Office of Health Equity and VHA National Social Work Program, Care Management and Social Work Services, is a social risk screening and referral program that aims to systematically identify and address unmet social needs among veterans to improve health and advance health equity.3,4 ACORN consists of 2 components: (1) a veteran-tailored screener to identify social risks within 9 domains; and (2) provision of relevant VA and community resources and referrals to address identified needs.3,5 Veterans who screen positive for ≥ 1 need receive referrals to a social worker or other relevant services, such as nutrition and food services or mental health, support navigating resources, and/or geographically tailored resource guides. This article describes the development and use of resource guides as a cross-cutting intervention component to address unmet social needs in diverse clinical settings and shares lessons learned from implementation in VHA outpatient clinics.
BACKGROUND
Unequal distribution of resources combined with historical discriminatory policies and practices, often linked to institutionalized racism, create inequities that lead to health disparities and hinder advancements in population health.6,7 Although health care systems alone cannot eliminate all health inequities, they can implement programs to identify social risks and address individual-level needs as 1 component of the multilevel approach needed to achieve health equity.8
As a national health care system serving > 9 million veterans, the VHA is well positioned to address social needs as an essential part of health. The VHA routinely screens for certain social risks, including housing instability, food insecurity, and intimate partner violence, and has a robust system of supports to address these and other needs among veterans, such as supportive housing services, vocational rehabilitation, assistance for justice-involved veterans, technology access support, and peer-support services.9-11 However, the VHA lacks a systematic approach to broader screening for social risks.
To address this gap, ACORN was developed in 2018 by an advisory board of subject matter experts, including clinical leaders, clinical psychologists, social workers, and health services researchers with content expertise in social risks and social needs.3 This interprofessional team sought to develop a veteran-tailored screener and resource referral initiative that could be scaled efficiently across VHA clinical settings.
Although health care organizations are increasingly implementing screening and interventions for social risks within clinical care, best practices and evidence-based tools to support clinical staff in these efforts are limited.12 Resource guides—curated lists of supportive services and organizations—may serve as a scalable “low-touch” intervention to help clinical staff address needs either alone or with more intensive interventions, such as social worker case management or patient navigation services.13
RESOURCE GUIDES—A Cross-Cutting Tool
The VHA has a uniquely robust network of nearly 18,000 social workers with clinical expertise in identifying, comprehensively assessing, and addressing social risks and needs among veterans. Interprofessional patient aligned care teams (PACTs)—a patient-centered medical home initiative that includes embedding social workers into primary care teams—facilitate the VHA’s capacity to address both medical and social needs.14 Social workers in PACTs and other care settings provide in-depth assessment and case management services to veterans who have a range of complex social needs. However, despite these comprehensive social services, in the setting of universal screening with a tool such as ACORN, it may not be feasible or practical to refer all patients who screen positive to a social worker for immediate follow-up, particularly in settings with capacity or resource limitations. For example, rates of screening positive on ACORN for ≥ 1 social risk have ranged from 48% of veterans in primary care sites and 80% in social work sites to nearly 100% in a PACT clinic for veterans experiencing homelessness.15
Additionally, a key challenge in the design of social needs interventions is determining how to optimize intervention intensity based on individual patient needs, acuity, and preferences. A substantial proportion of individuals who screen positive for social risks decline offered assistance, such as referrals.16 Resource guides are a cross-cutting tool that can be offered to veterans across a variety of settings, including primary care, specialty clinics, or emergency departments, as either a standalone intervention or one provided in combination with other resources or services. For patients who may not be interested in or feel comfortable accepting assistance at the time of screening or for those who prefer to research and navigate resources on their own, tailored resource guides can serve as a lower touch intervention to ensure interprofessional clinical staff across a range of settings and specialties have accessible, reliable, and up-to-date information to give to patients at the point of clinical care.17
Resource guides also can be used with higher touch clinical social work interventions, such as crisis management, supportive counseling, and case management. For example, social workers can use resource guides to provide education on VHA or community resources during clinical encounters with veterans and/or provide the guides to veterans to reference for future needs. Resource guides can further be used as a tool to support community resource navigation provided by nonclinical staff, such as peer specialists or community health workers.
How to BUILD RESOURCE GUIDES
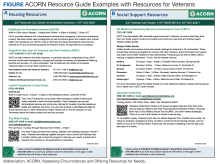
Our team created resource guides (Figure) to provide veterans with concise, geographically tailored lists of VHA and other federal, state, and community services for the social risk domains included on the ACORN screener. To inform and develop a framework for building and maintaining ACORN guides, we first reviewed existing models that use this approach, including Boston Medical Center's WE CARE (Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education) and Thrive programs. We provide an overview of our process, which can be applied to clinical settings both within and outside the VHA.18,19
Partnerships
Active collaboration with frontline clinical social workers and local social work leadership is a critical part of identifying and prioritizing quality resources. Equipped with the knowledge of the local resource landscape, social workers can provide recommendations pertaining to national or federal, state, and local programs that have a history of being responsive to patients’ expressed needs.20 VHA social workers have robust knowledge of the veteran-specific resources available at VHA medical centers and nationally, and their clinical training equips them with the expertise to provide guidance about which resources to prioritize for inclusion in the guides.20
After receiving initial guidance from clinical social workers, our team began outreach to compile detailed program information, gauge program serviceability, and build relationships with both VHA and community-based services. Aligning with programs that share a similar mission in addressing social needs has proved crucial when developing the resource guides. Beyond ensuring the accuracy of program information, regular contact provides an opportunity to address capacity and workflow concerns that may arise from increased referrals. Additionally, open lines of communication with various supportive services facilitate connections with additional organizations and resources within the area.
The value of these relationships was evident at the onset of the COVID-19 pandemic, when the ACORN resource guides in use by our clinical site partners required frequent modifications to reflect rapid changes in services (eg, closures, transition to fully virtual programs, social distancing and masking requirements). Having established connections with community organizations was essential to navigating the evolving landscape of available programs and supports.
Curating Quality Resources
ACORN currently screens for social risks in 9 domains: food, housing, utilities, transportation, education, employment, legal, social isolation/loneliness, and digital needs. Each resource guide pertains to a specific social risk domain and associated question(s) in the screener, allowing staff to quickly identify which guides a veteran may benefit from based on their screening responses. The guides are meant to be short and comprehensive but not exhaustive lists of programs and services. We limit the length of the guides to one single-sided page to provide high-yield, geographically tailored resources in an easy-to-use format. The guides should reflect the geographic area served by the VHA medical center or the community-based outpatient clinic (CBOC) where a veteran receives clinical care, but they also may include national- and state-level resources that provide services and programs to veterans.
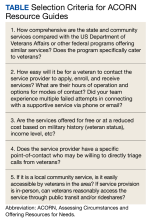
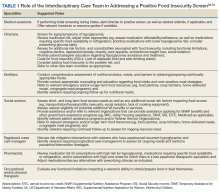
Although there is local variation in the availability and accessibility of services across social risk domains, some domains have an abundance of resources and organizations at federal or national, state, and/or community levels. To narrow the list of resources to the highest yield programs, we developed a series of questions that serve as selection criteria to inform resource inclusion (Table).
Because the resource guides are intended to be broadly applicable to a large number of veterans, we prioritize generalizable resources over those with narrow eligibility criteria and/or services. When more intensive support is needed, social workers and other VHA clinical and nonclinical staff can supplement the resources on the guides with additional, more tailored resources that are based on individual factors, such as physical residence, income, transportation access, or household composition (eg, veteran families with children or older adults).
Formatting Resource Guides
Along with relevant information, such as the program name, location, and a specific point of contact, brief program descriptions provide information about services offered, eligibility criteria, application requirements, alternate contacts and locations, and website links. At the bottom of each guide, a section is included with the name and direct contact information for a social worker (often the individual assigned to the clinic where the veteran completed the ACORN screener) or another VHA staff member who can be reached for further assistance. These staff members are familiar with the content included on the guides and provide veterans with additional information or higher touch support as necessary. This contact information is useful for veterans who initially decline assistance or referrals but later want to follow up with staff for support or questions.
Visual consistency is a key feature of the ACORN resource guides, and layout and design elements are used to maximize space and enhance usability. Corresponding font colors for all program titles, contact information, and website links assist in visually separating and drawing attention to pertinent contact information. QR codes linked to program websites also are incorporated for veterans to easily access resource information from their smartphone or other electronic device.
Maintaining Resource Guides
To ensure continued accuracy, resource guides are updated about every 6 months to reflect changes in closures, transitions to virtual/in-person services, changes in location, new points of contact, and modifications to services or eligibility requirements. Notations also are made if any changes to services or eligibility are temporary or permanent. Recording these temporary adjustments was critical early in the COVID-19 pandemic as service offerings, eligibility requirements, and application processes changed often.
Updating the guides also facilitates continuous relationship building and connections with VHA and community-based services. Resource guides are living documents: they maintain lines of communication with designated contacts, allow for opportunities to improve the presentation of evolving program information in the guides, and offer the chance to learn about additional programs in the area that may meet veterans' needs.
Creating a Manual for ACORN Resource Guide Development
To facilitate dissemination of ACORN across VHA clinical settings and locations, our team developed a Resource Guide Manual to aid ACORN clinical sites in developing resource guides.21 The manual provides step-by-step guidance from recommendations for identifying resources to formatting and layout considerations. Supplemental materials include a checklist to ensure each program description includes the necessary information for veterans to successfully access the resource, as well as page templates and style suggestions to maximize usability. These templates standardize formatting across the social risk domain guides and include options for electronic and paper distribution.
RESOURCE GUIDE LIMITATIONS
The labor involved in building and maintaining multiple guides is considerable and requires a time investment both upfront and long term, which may not be feasible for clinical sites with limited staff. However, many VHA social workers maintain lists of resource and referral services for veterans as part of their routine clinical case management. These lists can serve as a valuable and timesaving starting point in curating high-yield resources for formal resource guides. To further reduce the time needed to develop guides, sites can use ACORN resource guide templates rather than designing and formatting guides from scratch. In addition to informing veterans of relevant services and programs, resource guides also can be provided to new staff, such as social workers or peer specialists, during onboarding to help familiarize them with available services to address veterans’ unmet needs.
Resources included on the guides also are geographically tailored, based on the physical location of the VHA medical center or CBOC. Some community-based services listed may not be as relevant, accessible, available, or convenient to veterans who live far from the clinic, which is relevant for nearly 25% of veterans who live in rural communities.22 This is a circumstance in which the expertise of VHA social workers should be used to recommend more appropriately tailored resources to a veteran. Use of free, publicly available electronic resource databases (eg, 211 Helpline Center) also can provide social workers and patients with an overview of all available resources within their community. There are paid referral platform services that health systems can contract with as well.23 However, the potential drawbacks to these alternative platforms include high startup costs or costly user-license fees for medical centers or clinics, inconsistent updates to resource information, and lack of compatibility with some electronic health record systems.23
Resource guides are not intended to take the place of a clinical social worker or other health professional but rather to serve in a supplemental capacity to clinical services. Certain circumstances necessitate a more comprehensive clinical assessment and/or a warm handoff to a social worker, including assistance with urgent food or housing needs, and ACORN workflows are created with urgent needs pathways in mind. Determining how to optimize intervention intensity based on individual patients’ expressed needs, preferences, and acuity remains a challenge for health care organizations conducting social risk screening.12 While distribution of geographically tailored resource guides can be a useful low touch intervention for some veterans, others will require more intensive case management to address or meet their needs. Some veterans also may fall in the middle of this spectrum, where a resource guide is not enough but intensive case management services facilitated by social workers are not needed or wanted by the patient. Integration of peer specialists, patient navigators, or community health workers who can work with veterans to support them in identifying, connecting with, and receiving support from relevant programs may help fill this gap. Given their knowledge and lived experience, these professionals also can promote patient-centered care as part of the health care team.
CONCLUSIONS
Whether used as a low-touch, standalone intervention or in combination with higher touch services (eg, case management or resource navigation), resource guides are a valuable tool for health care organizations working to address social needs as a component of efforts to advance health equity, reduce health disparities, and promote population health. We provide a pragmatic framework for developing and maintaining resource guides used in the ACORN initiative. However, additional work is needed to optimize the design, content, and format of resource guides for both usability and effectiveness as a social risk intervention across health care settings.
Acknowledgments
We express our gratitude for the Veterans Health Administration (VHA) Office of Health Equity and the VHA National Social Work Program, Care Management and Social Work Services for their support of the Assessing Circumstances and Offering Resources for Needs (ACORN) initiative. We also express our appreciation for those who supported the initial screener development as part of the ACORN Advisory Board, including Stacey Curran, BA; Charles Drebing, PhD; J. Stewart Evans, MD, MSc; Edward Federman, PhD; Maneesha Gulati, LICSW, ACSW; Nancy Kressin, PhD; Kenneth Link, LICSW; Monica Sharma, MD; and Jacqueline Spencer, MD, MPH. We also express our appreciation for those who supported the initial ACORN resource guide development, including Chuck Drebing, PhD, Ed Federman, PhD, and Ken Link, LICSW, and for the clinical care team members, especially the social workers and nurses, at our ACORN partner sites as well as the community-based partners who have helped us develop comprehensive resource guides for veterans. This work was supported by funding from the VHA Office of Health Equity and by resources and use of facilities at the VA Bedford Healthcare System, VA New England Healthcare System, and VA Providence Healthcare System. Alicia J. Cohen was additionally supported by a VA HSR&D Career Development Award (CDA 20-037).
1. Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407-419. doi:10.1111/1468-0009.12390
2. Blosnich JM, Montgomery AE, Taylor LD, Dichter ME. Adverse social factors and all-cause mortality among male and female patients receiving care in the Veterans Health Administration. Prev Med. 2020;141:106272. doi:10.1016/j.ypmed.2020.106272
3. Russell LE, Cohen AJ, Chrzas S, et al. Implementing a social needs screening and referral program among veterans: Assessing Circumstances & Offering Resources for Needs (ACORN). J Gen Intern Med. 2023;38(13):2906-2913. doi:10.1007/s11606-023-08181-9
4. Cohen AJ, Russell LE, Elwy AR, et al. Adaptation of a social risk screening and referral initiative across clinical populations, settings, and contexts in the Department of Veterans Affairs Health System. Front Health Serv. 2023;2. doi:10.3389/frhs.2022.958969
5. Cohen AJ, Kennedy MA, Mitchell KM, Russell LE. The Assessing Circumstances & Offering Resources for Needs (ACORN) initiative. Updated September 2022. Accessed December 4, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Screening_Tool.pdf
6. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212-1215. doi:10.2105/ajph.90.8.1212
7. American Public Health Association. Creating the healthiest nation: advancing health equity. Accessed November 28, 2023. https://www.apha.org/-/media/files/pdf/factsheets/advancing_health_equity.ashx?la=en&hash=9144021FDA33B4E7E02447CB28CA3F9D4BE5EF18
8. Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Aff. Published January 16, 2019. doi:10.1377/hblog20190115.234942
9. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-211. doi:10.2105/AJPH.2013.301398
10. Cohen AJ, Rudolph JL, Thomas KS, et al. Food insecurity among veterans: resources to screen and intervene. Fed Pract. 2020;37(1):16-23.
11. Iverson KM, Adjognon O, Grillo AR, et al. Intimate partner violence screening programs in the Veterans Health Administration: informing scale-up of successful practices. J Gen Intern Med. 2019;34(11):2435-2442. doi:10.1007/s11606-019-05240-y
12. National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. Accessed November 28, 2023. https://nap.nationalacademies.org/catalog/25467/integrating-social-care-into-the-delivery-of-health-care-moving
13. Gottlieb LM, Adler NE, Wing H, et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e200701. doi:10.1001/jamanetworkopen.2020.0701
14. Cornell PY, Halladay CW, Ader J, et al. Embedding social workers in Veterans Health Administration primary care teams reduces emergency department visits. Health Aff (Millwood). 2020;39(4):603-612. doi:10.1377/hlthaff.2019.01589
15. Cohen AJ, Bruton M, Hooshyar D. US Department of Veterans Affairs, Office of Health Services Research and Development. The WHO’s greatest ICD-10 hits for fiscal year 2022: social determinants of health. Published March 9, 2022. Updated November 6, 2023. Accessed December 4, 2023. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=4125

16. De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170-175. doi:10.3122/jabfm.2020.02.190309
17. Cohen AJ, Isaacson N, Torby M, Smith A, Zhang G, Patel MR. Motivators, barriers, and preferences to engagement with offered social care assistance among people with diabetes: a mixed methods study. Am J Prev Med. 2022;63(3, suppl 2):S152-S163. doi:10.1016/j.amepre.2022.02.022
18. Buitron de la Vega P, Losi S, Sprague Martinez L, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(suppl 6, suppl 2):S133-S139. doi:10.1097/MLR.0000000000001029
19. Boston Medical Center. The WE CARE Model. Accessed November 28, 2023. https://www.bmc.org/pediatrics-primary-care/we-care/we-care-model
20. US Department of Veterans Affairs, Office of Rural Health. VA social work. Updated July 11, 2023. Accessed December 4, 2023. https://www.socialwork.va.gov
21. Mitchell KM, Russell LE, Cohen AJ, Kennedy MA. Building ACORN resource guides for veterans. Accessed November 28, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Resource_Guide_Manual.pdf
22. US Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health. Rural Veterans. Accessed November 28, 2023. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
23. Cartier Y, Fichtenberg C, Gottlieb L. Community resource referral platforms: a guide for health care organizations. Published 2019. Accessed December 4, 2023. https://sirenetwork.ucsf.edu/tools-resources/resources/community-resource-referral-platforms-guide-health-care-organizations
Social risk factors and social needs have significant, often cumulative, impacts on health outcomes and are closely tied to health inequities. Defined as the individual-level adverse social conditions associated with poor health, social risk factors broadly include experiences such as food insecurity and housing instability; whereas the term social needs incorporates a person’s perceptions of and priorities related to their health-related needs.1 One recent study examining data from the Veterans Health Administration (VHA) found a 27% higher odds of mortality with each additional identified social risk, underscoring the critical link between social risks and veteran health outcomes.2
Assessing Circumstances and Offering Resources for Needs (ACORN), a collaborative quality improvement initiative conducted in partnership with the VHA Office of Health Equity and VHA National Social Work Program, Care Management and Social Work Services, is a social risk screening and referral program that aims to systematically identify and address unmet social needs among veterans to improve health and advance health equity.3,4 ACORN consists of 2 components: (1) a veteran-tailored screener to identify social risks within 9 domains; and (2) provision of relevant VA and community resources and referrals to address identified needs.3,5 Veterans who screen positive for ≥ 1 need receive referrals to a social worker or other relevant services, such as nutrition and food services or mental health, support navigating resources, and/or geographically tailored resource guides. This article describes the development and use of resource guides as a cross-cutting intervention component to address unmet social needs in diverse clinical settings and shares lessons learned from implementation in VHA outpatient clinics.
BACKGROUND
Unequal distribution of resources combined with historical discriminatory policies and practices, often linked to institutionalized racism, create inequities that lead to health disparities and hinder advancements in population health.6,7 Although health care systems alone cannot eliminate all health inequities, they can implement programs to identify social risks and address individual-level needs as 1 component of the multilevel approach needed to achieve health equity.8
As a national health care system serving > 9 million veterans, the VHA is well positioned to address social needs as an essential part of health. The VHA routinely screens for certain social risks, including housing instability, food insecurity, and intimate partner violence, and has a robust system of supports to address these and other needs among veterans, such as supportive housing services, vocational rehabilitation, assistance for justice-involved veterans, technology access support, and peer-support services.9-11 However, the VHA lacks a systematic approach to broader screening for social risks.
To address this gap, ACORN was developed in 2018 by an advisory board of subject matter experts, including clinical leaders, clinical psychologists, social workers, and health services researchers with content expertise in social risks and social needs.3 This interprofessional team sought to develop a veteran-tailored screener and resource referral initiative that could be scaled efficiently across VHA clinical settings.
Although health care organizations are increasingly implementing screening and interventions for social risks within clinical care, best practices and evidence-based tools to support clinical staff in these efforts are limited.12 Resource guides—curated lists of supportive services and organizations—may serve as a scalable “low-touch” intervention to help clinical staff address needs either alone or with more intensive interventions, such as social worker case management or patient navigation services.13
RESOURCE GUIDES—A Cross-Cutting Tool
The VHA has a uniquely robust network of nearly 18,000 social workers with clinical expertise in identifying, comprehensively assessing, and addressing social risks and needs among veterans. Interprofessional patient aligned care teams (PACTs)—a patient-centered medical home initiative that includes embedding social workers into primary care teams—facilitate the VHA’s capacity to address both medical and social needs.14 Social workers in PACTs and other care settings provide in-depth assessment and case management services to veterans who have a range of complex social needs. However, despite these comprehensive social services, in the setting of universal screening with a tool such as ACORN, it may not be feasible or practical to refer all patients who screen positive to a social worker for immediate follow-up, particularly in settings with capacity or resource limitations. For example, rates of screening positive on ACORN for ≥ 1 social risk have ranged from 48% of veterans in primary care sites and 80% in social work sites to nearly 100% in a PACT clinic for veterans experiencing homelessness.15
Additionally, a key challenge in the design of social needs interventions is determining how to optimize intervention intensity based on individual patient needs, acuity, and preferences. A substantial proportion of individuals who screen positive for social risks decline offered assistance, such as referrals.16 Resource guides are a cross-cutting tool that can be offered to veterans across a variety of settings, including primary care, specialty clinics, or emergency departments, as either a standalone intervention or one provided in combination with other resources or services. For patients who may not be interested in or feel comfortable accepting assistance at the time of screening or for those who prefer to research and navigate resources on their own, tailored resource guides can serve as a lower touch intervention to ensure interprofessional clinical staff across a range of settings and specialties have accessible, reliable, and up-to-date information to give to patients at the point of clinical care.17
Resource guides also can be used with higher touch clinical social work interventions, such as crisis management, supportive counseling, and case management. For example, social workers can use resource guides to provide education on VHA or community resources during clinical encounters with veterans and/or provide the guides to veterans to reference for future needs. Resource guides can further be used as a tool to support community resource navigation provided by nonclinical staff, such as peer specialists or community health workers.
How to BUILD RESOURCE GUIDES
Our team created resource guides (Figure) to provide veterans with concise, geographically tailored lists of VHA and other federal, state, and community services for the social risk domains included on the ACORN screener. To inform and develop a framework for building and maintaining ACORN guides, we first reviewed existing models that use this approach, including Boston Medical Center's WE CARE (Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education) and Thrive programs. We provide an overview of our process, which can be applied to clinical settings both within and outside the VHA.18,19
Partnerships
Active collaboration with frontline clinical social workers and local social work leadership is a critical part of identifying and prioritizing quality resources. Equipped with the knowledge of the local resource landscape, social workers can provide recommendations pertaining to national or federal, state, and local programs that have a history of being responsive to patients’ expressed needs.20 VHA social workers have robust knowledge of the veteran-specific resources available at VHA medical centers and nationally, and their clinical training equips them with the expertise to provide guidance about which resources to prioritize for inclusion in the guides.20
After receiving initial guidance from clinical social workers, our team began outreach to compile detailed program information, gauge program serviceability, and build relationships with both VHA and community-based services. Aligning with programs that share a similar mission in addressing social needs has proved crucial when developing the resource guides. Beyond ensuring the accuracy of program information, regular contact provides an opportunity to address capacity and workflow concerns that may arise from increased referrals. Additionally, open lines of communication with various supportive services facilitate connections with additional organizations and resources within the area.
The value of these relationships was evident at the onset of the COVID-19 pandemic, when the ACORN resource guides in use by our clinical site partners required frequent modifications to reflect rapid changes in services (eg, closures, transition to fully virtual programs, social distancing and masking requirements). Having established connections with community organizations was essential to navigating the evolving landscape of available programs and supports.
Curating Quality Resources
ACORN currently screens for social risks in 9 domains: food, housing, utilities, transportation, education, employment, legal, social isolation/loneliness, and digital needs. Each resource guide pertains to a specific social risk domain and associated question(s) in the screener, allowing staff to quickly identify which guides a veteran may benefit from based on their screening responses. The guides are meant to be short and comprehensive but not exhaustive lists of programs and services. We limit the length of the guides to one single-sided page to provide high-yield, geographically tailored resources in an easy-to-use format. The guides should reflect the geographic area served by the VHA medical center or the community-based outpatient clinic (CBOC) where a veteran receives clinical care, but they also may include national- and state-level resources that provide services and programs to veterans.
Although there is local variation in the availability and accessibility of services across social risk domains, some domains have an abundance of resources and organizations at federal or national, state, and/or community levels. To narrow the list of resources to the highest yield programs, we developed a series of questions that serve as selection criteria to inform resource inclusion (Table).
Because the resource guides are intended to be broadly applicable to a large number of veterans, we prioritize generalizable resources over those with narrow eligibility criteria and/or services. When more intensive support is needed, social workers and other VHA clinical and nonclinical staff can supplement the resources on the guides with additional, more tailored resources that are based on individual factors, such as physical residence, income, transportation access, or household composition (eg, veteran families with children or older adults).
Formatting Resource Guides
Along with relevant information, such as the program name, location, and a specific point of contact, brief program descriptions provide information about services offered, eligibility criteria, application requirements, alternate contacts and locations, and website links. At the bottom of each guide, a section is included with the name and direct contact information for a social worker (often the individual assigned to the clinic where the veteran completed the ACORN screener) or another VHA staff member who can be reached for further assistance. These staff members are familiar with the content included on the guides and provide veterans with additional information or higher touch support as necessary. This contact information is useful for veterans who initially decline assistance or referrals but later want to follow up with staff for support or questions.
Visual consistency is a key feature of the ACORN resource guides, and layout and design elements are used to maximize space and enhance usability. Corresponding font colors for all program titles, contact information, and website links assist in visually separating and drawing attention to pertinent contact information. QR codes linked to program websites also are incorporated for veterans to easily access resource information from their smartphone or other electronic device.
Maintaining Resource Guides
To ensure continued accuracy, resource guides are updated about every 6 months to reflect changes in closures, transitions to virtual/in-person services, changes in location, new points of contact, and modifications to services or eligibility requirements. Notations also are made if any changes to services or eligibility are temporary or permanent. Recording these temporary adjustments was critical early in the COVID-19 pandemic as service offerings, eligibility requirements, and application processes changed often.
Updating the guides also facilitates continuous relationship building and connections with VHA and community-based services. Resource guides are living documents: they maintain lines of communication with designated contacts, allow for opportunities to improve the presentation of evolving program information in the guides, and offer the chance to learn about additional programs in the area that may meet veterans' needs.
Creating a Manual for ACORN Resource Guide Development
To facilitate dissemination of ACORN across VHA clinical settings and locations, our team developed a Resource Guide Manual to aid ACORN clinical sites in developing resource guides.21 The manual provides step-by-step guidance from recommendations for identifying resources to formatting and layout considerations. Supplemental materials include a checklist to ensure each program description includes the necessary information for veterans to successfully access the resource, as well as page templates and style suggestions to maximize usability. These templates standardize formatting across the social risk domain guides and include options for electronic and paper distribution.
RESOURCE GUIDE LIMITATIONS
The labor involved in building and maintaining multiple guides is considerable and requires a time investment both upfront and long term, which may not be feasible for clinical sites with limited staff. However, many VHA social workers maintain lists of resource and referral services for veterans as part of their routine clinical case management. These lists can serve as a valuable and timesaving starting point in curating high-yield resources for formal resource guides. To further reduce the time needed to develop guides, sites can use ACORN resource guide templates rather than designing and formatting guides from scratch. In addition to informing veterans of relevant services and programs, resource guides also can be provided to new staff, such as social workers or peer specialists, during onboarding to help familiarize them with available services to address veterans’ unmet needs.
Resources included on the guides also are geographically tailored, based on the physical location of the VHA medical center or CBOC. Some community-based services listed may not be as relevant, accessible, available, or convenient to veterans who live far from the clinic, which is relevant for nearly 25% of veterans who live in rural communities.22 This is a circumstance in which the expertise of VHA social workers should be used to recommend more appropriately tailored resources to a veteran. Use of free, publicly available electronic resource databases (eg, 211 Helpline Center) also can provide social workers and patients with an overview of all available resources within their community. There are paid referral platform services that health systems can contract with as well.23 However, the potential drawbacks to these alternative platforms include high startup costs or costly user-license fees for medical centers or clinics, inconsistent updates to resource information, and lack of compatibility with some electronic health record systems.23
Resource guides are not intended to take the place of a clinical social worker or other health professional but rather to serve in a supplemental capacity to clinical services. Certain circumstances necessitate a more comprehensive clinical assessment and/or a warm handoff to a social worker, including assistance with urgent food or housing needs, and ACORN workflows are created with urgent needs pathways in mind. Determining how to optimize intervention intensity based on individual patients’ expressed needs, preferences, and acuity remains a challenge for health care organizations conducting social risk screening.12 While distribution of geographically tailored resource guides can be a useful low touch intervention for some veterans, others will require more intensive case management to address or meet their needs. Some veterans also may fall in the middle of this spectrum, where a resource guide is not enough but intensive case management services facilitated by social workers are not needed or wanted by the patient. Integration of peer specialists, patient navigators, or community health workers who can work with veterans to support them in identifying, connecting with, and receiving support from relevant programs may help fill this gap. Given their knowledge and lived experience, these professionals also can promote patient-centered care as part of the health care team.
CONCLUSIONS
Whether used as a low-touch, standalone intervention or in combination with higher touch services (eg, case management or resource navigation), resource guides are a valuable tool for health care organizations working to address social needs as a component of efforts to advance health equity, reduce health disparities, and promote population health. We provide a pragmatic framework for developing and maintaining resource guides used in the ACORN initiative. However, additional work is needed to optimize the design, content, and format of resource guides for both usability and effectiveness as a social risk intervention across health care settings.
Acknowledgments
We express our gratitude for the Veterans Health Administration (VHA) Office of Health Equity and the VHA National Social Work Program, Care Management and Social Work Services for their support of the Assessing Circumstances and Offering Resources for Needs (ACORN) initiative. We also express our appreciation for those who supported the initial screener development as part of the ACORN Advisory Board, including Stacey Curran, BA; Charles Drebing, PhD; J. Stewart Evans, MD, MSc; Edward Federman, PhD; Maneesha Gulati, LICSW, ACSW; Nancy Kressin, PhD; Kenneth Link, LICSW; Monica Sharma, MD; and Jacqueline Spencer, MD, MPH. We also express our appreciation for those who supported the initial ACORN resource guide development, including Chuck Drebing, PhD, Ed Federman, PhD, and Ken Link, LICSW, and for the clinical care team members, especially the social workers and nurses, at our ACORN partner sites as well as the community-based partners who have helped us develop comprehensive resource guides for veterans. This work was supported by funding from the VHA Office of Health Equity and by resources and use of facilities at the VA Bedford Healthcare System, VA New England Healthcare System, and VA Providence Healthcare System. Alicia J. Cohen was additionally supported by a VA HSR&D Career Development Award (CDA 20-037).
Social risk factors and social needs have significant, often cumulative, impacts on health outcomes and are closely tied to health inequities. Defined as the individual-level adverse social conditions associated with poor health, social risk factors broadly include experiences such as food insecurity and housing instability; whereas the term social needs incorporates a person’s perceptions of and priorities related to their health-related needs.1 One recent study examining data from the Veterans Health Administration (VHA) found a 27% higher odds of mortality with each additional identified social risk, underscoring the critical link between social risks and veteran health outcomes.2
Assessing Circumstances and Offering Resources for Needs (ACORN), a collaborative quality improvement initiative conducted in partnership with the VHA Office of Health Equity and VHA National Social Work Program, Care Management and Social Work Services, is a social risk screening and referral program that aims to systematically identify and address unmet social needs among veterans to improve health and advance health equity.3,4 ACORN consists of 2 components: (1) a veteran-tailored screener to identify social risks within 9 domains; and (2) provision of relevant VA and community resources and referrals to address identified needs.3,5 Veterans who screen positive for ≥ 1 need receive referrals to a social worker or other relevant services, such as nutrition and food services or mental health, support navigating resources, and/or geographically tailored resource guides. This article describes the development and use of resource guides as a cross-cutting intervention component to address unmet social needs in diverse clinical settings and shares lessons learned from implementation in VHA outpatient clinics.
BACKGROUND
Unequal distribution of resources combined with historical discriminatory policies and practices, often linked to institutionalized racism, create inequities that lead to health disparities and hinder advancements in population health.6,7 Although health care systems alone cannot eliminate all health inequities, they can implement programs to identify social risks and address individual-level needs as 1 component of the multilevel approach needed to achieve health equity.8
As a national health care system serving > 9 million veterans, the VHA is well positioned to address social needs as an essential part of health. The VHA routinely screens for certain social risks, including housing instability, food insecurity, and intimate partner violence, and has a robust system of supports to address these and other needs among veterans, such as supportive housing services, vocational rehabilitation, assistance for justice-involved veterans, technology access support, and peer-support services.9-11 However, the VHA lacks a systematic approach to broader screening for social risks.
To address this gap, ACORN was developed in 2018 by an advisory board of subject matter experts, including clinical leaders, clinical psychologists, social workers, and health services researchers with content expertise in social risks and social needs.3 This interprofessional team sought to develop a veteran-tailored screener and resource referral initiative that could be scaled efficiently across VHA clinical settings.
Although health care organizations are increasingly implementing screening and interventions for social risks within clinical care, best practices and evidence-based tools to support clinical staff in these efforts are limited.12 Resource guides—curated lists of supportive services and organizations—may serve as a scalable “low-touch” intervention to help clinical staff address needs either alone or with more intensive interventions, such as social worker case management or patient navigation services.13
RESOURCE GUIDES—A Cross-Cutting Tool
The VHA has a uniquely robust network of nearly 18,000 social workers with clinical expertise in identifying, comprehensively assessing, and addressing social risks and needs among veterans. Interprofessional patient aligned care teams (PACTs)—a patient-centered medical home initiative that includes embedding social workers into primary care teams—facilitate the VHA’s capacity to address both medical and social needs.14 Social workers in PACTs and other care settings provide in-depth assessment and case management services to veterans who have a range of complex social needs. However, despite these comprehensive social services, in the setting of universal screening with a tool such as ACORN, it may not be feasible or practical to refer all patients who screen positive to a social worker for immediate follow-up, particularly in settings with capacity or resource limitations. For example, rates of screening positive on ACORN for ≥ 1 social risk have ranged from 48% of veterans in primary care sites and 80% in social work sites to nearly 100% in a PACT clinic for veterans experiencing homelessness.15
Additionally, a key challenge in the design of social needs interventions is determining how to optimize intervention intensity based on individual patient needs, acuity, and preferences. A substantial proportion of individuals who screen positive for social risks decline offered assistance, such as referrals.16 Resource guides are a cross-cutting tool that can be offered to veterans across a variety of settings, including primary care, specialty clinics, or emergency departments, as either a standalone intervention or one provided in combination with other resources or services. For patients who may not be interested in or feel comfortable accepting assistance at the time of screening or for those who prefer to research and navigate resources on their own, tailored resource guides can serve as a lower touch intervention to ensure interprofessional clinical staff across a range of settings and specialties have accessible, reliable, and up-to-date information to give to patients at the point of clinical care.17
Resource guides also can be used with higher touch clinical social work interventions, such as crisis management, supportive counseling, and case management. For example, social workers can use resource guides to provide education on VHA or community resources during clinical encounters with veterans and/or provide the guides to veterans to reference for future needs. Resource guides can further be used as a tool to support community resource navigation provided by nonclinical staff, such as peer specialists or community health workers.
How to BUILD RESOURCE GUIDES
Our team created resource guides (Figure) to provide veterans with concise, geographically tailored lists of VHA and other federal, state, and community services for the social risk domains included on the ACORN screener. To inform and develop a framework for building and maintaining ACORN guides, we first reviewed existing models that use this approach, including Boston Medical Center's WE CARE (Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education) and Thrive programs. We provide an overview of our process, which can be applied to clinical settings both within and outside the VHA.18,19
Partnerships
Active collaboration with frontline clinical social workers and local social work leadership is a critical part of identifying and prioritizing quality resources. Equipped with the knowledge of the local resource landscape, social workers can provide recommendations pertaining to national or federal, state, and local programs that have a history of being responsive to patients’ expressed needs.20 VHA social workers have robust knowledge of the veteran-specific resources available at VHA medical centers and nationally, and their clinical training equips them with the expertise to provide guidance about which resources to prioritize for inclusion in the guides.20
After receiving initial guidance from clinical social workers, our team began outreach to compile detailed program information, gauge program serviceability, and build relationships with both VHA and community-based services. Aligning with programs that share a similar mission in addressing social needs has proved crucial when developing the resource guides. Beyond ensuring the accuracy of program information, regular contact provides an opportunity to address capacity and workflow concerns that may arise from increased referrals. Additionally, open lines of communication with various supportive services facilitate connections with additional organizations and resources within the area.
The value of these relationships was evident at the onset of the COVID-19 pandemic, when the ACORN resource guides in use by our clinical site partners required frequent modifications to reflect rapid changes in services (eg, closures, transition to fully virtual programs, social distancing and masking requirements). Having established connections with community organizations was essential to navigating the evolving landscape of available programs and supports.
Curating Quality Resources
ACORN currently screens for social risks in 9 domains: food, housing, utilities, transportation, education, employment, legal, social isolation/loneliness, and digital needs. Each resource guide pertains to a specific social risk domain and associated question(s) in the screener, allowing staff to quickly identify which guides a veteran may benefit from based on their screening responses. The guides are meant to be short and comprehensive but not exhaustive lists of programs and services. We limit the length of the guides to one single-sided page to provide high-yield, geographically tailored resources in an easy-to-use format. The guides should reflect the geographic area served by the VHA medical center or the community-based outpatient clinic (CBOC) where a veteran receives clinical care, but they also may include national- and state-level resources that provide services and programs to veterans.
Although there is local variation in the availability and accessibility of services across social risk domains, some domains have an abundance of resources and organizations at federal or national, state, and/or community levels. To narrow the list of resources to the highest yield programs, we developed a series of questions that serve as selection criteria to inform resource inclusion (Table).
Because the resource guides are intended to be broadly applicable to a large number of veterans, we prioritize generalizable resources over those with narrow eligibility criteria and/or services. When more intensive support is needed, social workers and other VHA clinical and nonclinical staff can supplement the resources on the guides with additional, more tailored resources that are based on individual factors, such as physical residence, income, transportation access, or household composition (eg, veteran families with children or older adults).
Formatting Resource Guides
Along with relevant information, such as the program name, location, and a specific point of contact, brief program descriptions provide information about services offered, eligibility criteria, application requirements, alternate contacts and locations, and website links. At the bottom of each guide, a section is included with the name and direct contact information for a social worker (often the individual assigned to the clinic where the veteran completed the ACORN screener) or another VHA staff member who can be reached for further assistance. These staff members are familiar with the content included on the guides and provide veterans with additional information or higher touch support as necessary. This contact information is useful for veterans who initially decline assistance or referrals but later want to follow up with staff for support or questions.
Visual consistency is a key feature of the ACORN resource guides, and layout and design elements are used to maximize space and enhance usability. Corresponding font colors for all program titles, contact information, and website links assist in visually separating and drawing attention to pertinent contact information. QR codes linked to program websites also are incorporated for veterans to easily access resource information from their smartphone or other electronic device.
Maintaining Resource Guides
To ensure continued accuracy, resource guides are updated about every 6 months to reflect changes in closures, transitions to virtual/in-person services, changes in location, new points of contact, and modifications to services or eligibility requirements. Notations also are made if any changes to services or eligibility are temporary or permanent. Recording these temporary adjustments was critical early in the COVID-19 pandemic as service offerings, eligibility requirements, and application processes changed often.
Updating the guides also facilitates continuous relationship building and connections with VHA and community-based services. Resource guides are living documents: they maintain lines of communication with designated contacts, allow for opportunities to improve the presentation of evolving program information in the guides, and offer the chance to learn about additional programs in the area that may meet veterans' needs.
Creating a Manual for ACORN Resource Guide Development
To facilitate dissemination of ACORN across VHA clinical settings and locations, our team developed a Resource Guide Manual to aid ACORN clinical sites in developing resource guides.21 The manual provides step-by-step guidance from recommendations for identifying resources to formatting and layout considerations. Supplemental materials include a checklist to ensure each program description includes the necessary information for veterans to successfully access the resource, as well as page templates and style suggestions to maximize usability. These templates standardize formatting across the social risk domain guides and include options for electronic and paper distribution.
RESOURCE GUIDE LIMITATIONS
The labor involved in building and maintaining multiple guides is considerable and requires a time investment both upfront and long term, which may not be feasible for clinical sites with limited staff. However, many VHA social workers maintain lists of resource and referral services for veterans as part of their routine clinical case management. These lists can serve as a valuable and timesaving starting point in curating high-yield resources for formal resource guides. To further reduce the time needed to develop guides, sites can use ACORN resource guide templates rather than designing and formatting guides from scratch. In addition to informing veterans of relevant services and programs, resource guides also can be provided to new staff, such as social workers or peer specialists, during onboarding to help familiarize them with available services to address veterans’ unmet needs.
Resources included on the guides also are geographically tailored, based on the physical location of the VHA medical center or CBOC. Some community-based services listed may not be as relevant, accessible, available, or convenient to veterans who live far from the clinic, which is relevant for nearly 25% of veterans who live in rural communities.22 This is a circumstance in which the expertise of VHA social workers should be used to recommend more appropriately tailored resources to a veteran. Use of free, publicly available electronic resource databases (eg, 211 Helpline Center) also can provide social workers and patients with an overview of all available resources within their community. There are paid referral platform services that health systems can contract with as well.23 However, the potential drawbacks to these alternative platforms include high startup costs or costly user-license fees for medical centers or clinics, inconsistent updates to resource information, and lack of compatibility with some electronic health record systems.23
Resource guides are not intended to take the place of a clinical social worker or other health professional but rather to serve in a supplemental capacity to clinical services. Certain circumstances necessitate a more comprehensive clinical assessment and/or a warm handoff to a social worker, including assistance with urgent food or housing needs, and ACORN workflows are created with urgent needs pathways in mind. Determining how to optimize intervention intensity based on individual patients’ expressed needs, preferences, and acuity remains a challenge for health care organizations conducting social risk screening.12 While distribution of geographically tailored resource guides can be a useful low touch intervention for some veterans, others will require more intensive case management to address or meet their needs. Some veterans also may fall in the middle of this spectrum, where a resource guide is not enough but intensive case management services facilitated by social workers are not needed or wanted by the patient. Integration of peer specialists, patient navigators, or community health workers who can work with veterans to support them in identifying, connecting with, and receiving support from relevant programs may help fill this gap. Given their knowledge and lived experience, these professionals also can promote patient-centered care as part of the health care team.
CONCLUSIONS
Whether used as a low-touch, standalone intervention or in combination with higher touch services (eg, case management or resource navigation), resource guides are a valuable tool for health care organizations working to address social needs as a component of efforts to advance health equity, reduce health disparities, and promote population health. We provide a pragmatic framework for developing and maintaining resource guides used in the ACORN initiative. However, additional work is needed to optimize the design, content, and format of resource guides for both usability and effectiveness as a social risk intervention across health care settings.
Acknowledgments
We express our gratitude for the Veterans Health Administration (VHA) Office of Health Equity and the VHA National Social Work Program, Care Management and Social Work Services for their support of the Assessing Circumstances and Offering Resources for Needs (ACORN) initiative. We also express our appreciation for those who supported the initial screener development as part of the ACORN Advisory Board, including Stacey Curran, BA; Charles Drebing, PhD; J. Stewart Evans, MD, MSc; Edward Federman, PhD; Maneesha Gulati, LICSW, ACSW; Nancy Kressin, PhD; Kenneth Link, LICSW; Monica Sharma, MD; and Jacqueline Spencer, MD, MPH. We also express our appreciation for those who supported the initial ACORN resource guide development, including Chuck Drebing, PhD, Ed Federman, PhD, and Ken Link, LICSW, and for the clinical care team members, especially the social workers and nurses, at our ACORN partner sites as well as the community-based partners who have helped us develop comprehensive resource guides for veterans. This work was supported by funding from the VHA Office of Health Equity and by resources and use of facilities at the VA Bedford Healthcare System, VA New England Healthcare System, and VA Providence Healthcare System. Alicia J. Cohen was additionally supported by a VA HSR&D Career Development Award (CDA 20-037).
1. Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407-419. doi:10.1111/1468-0009.12390
2. Blosnich JM, Montgomery AE, Taylor LD, Dichter ME. Adverse social factors and all-cause mortality among male and female patients receiving care in the Veterans Health Administration. Prev Med. 2020;141:106272. doi:10.1016/j.ypmed.2020.106272
3. Russell LE, Cohen AJ, Chrzas S, et al. Implementing a social needs screening and referral program among veterans: Assessing Circumstances & Offering Resources for Needs (ACORN). J Gen Intern Med. 2023;38(13):2906-2913. doi:10.1007/s11606-023-08181-9
4. Cohen AJ, Russell LE, Elwy AR, et al. Adaptation of a social risk screening and referral initiative across clinical populations, settings, and contexts in the Department of Veterans Affairs Health System. Front Health Serv. 2023;2. doi:10.3389/frhs.2022.958969
5. Cohen AJ, Kennedy MA, Mitchell KM, Russell LE. The Assessing Circumstances & Offering Resources for Needs (ACORN) initiative. Updated September 2022. Accessed December 4, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Screening_Tool.pdf
6. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212-1215. doi:10.2105/ajph.90.8.1212
7. American Public Health Association. Creating the healthiest nation: advancing health equity. Accessed November 28, 2023. https://www.apha.org/-/media/files/pdf/factsheets/advancing_health_equity.ashx?la=en&hash=9144021FDA33B4E7E02447CB28CA3F9D4BE5EF18
8. Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Aff. Published January 16, 2019. doi:10.1377/hblog20190115.234942
9. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-211. doi:10.2105/AJPH.2013.301398
10. Cohen AJ, Rudolph JL, Thomas KS, et al. Food insecurity among veterans: resources to screen and intervene. Fed Pract. 2020;37(1):16-23.
11. Iverson KM, Adjognon O, Grillo AR, et al. Intimate partner violence screening programs in the Veterans Health Administration: informing scale-up of successful practices. J Gen Intern Med. 2019;34(11):2435-2442. doi:10.1007/s11606-019-05240-y
12. National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. Accessed November 28, 2023. https://nap.nationalacademies.org/catalog/25467/integrating-social-care-into-the-delivery-of-health-care-moving
13. Gottlieb LM, Adler NE, Wing H, et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e200701. doi:10.1001/jamanetworkopen.2020.0701
14. Cornell PY, Halladay CW, Ader J, et al. Embedding social workers in Veterans Health Administration primary care teams reduces emergency department visits. Health Aff (Millwood). 2020;39(4):603-612. doi:10.1377/hlthaff.2019.01589
15. Cohen AJ, Bruton M, Hooshyar D. US Department of Veterans Affairs, Office of Health Services Research and Development. The WHO’s greatest ICD-10 hits for fiscal year 2022: social determinants of health. Published March 9, 2022. Updated November 6, 2023. Accessed December 4, 2023. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=4125

16. De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170-175. doi:10.3122/jabfm.2020.02.190309
17. Cohen AJ, Isaacson N, Torby M, Smith A, Zhang G, Patel MR. Motivators, barriers, and preferences to engagement with offered social care assistance among people with diabetes: a mixed methods study. Am J Prev Med. 2022;63(3, suppl 2):S152-S163. doi:10.1016/j.amepre.2022.02.022
18. Buitron de la Vega P, Losi S, Sprague Martinez L, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(suppl 6, suppl 2):S133-S139. doi:10.1097/MLR.0000000000001029
19. Boston Medical Center. The WE CARE Model. Accessed November 28, 2023. https://www.bmc.org/pediatrics-primary-care/we-care/we-care-model
20. US Department of Veterans Affairs, Office of Rural Health. VA social work. Updated July 11, 2023. Accessed December 4, 2023. https://www.socialwork.va.gov
21. Mitchell KM, Russell LE, Cohen AJ, Kennedy MA. Building ACORN resource guides for veterans. Accessed November 28, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Resource_Guide_Manual.pdf
22. US Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health. Rural Veterans. Accessed November 28, 2023. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
23. Cartier Y, Fichtenberg C, Gottlieb L. Community resource referral platforms: a guide for health care organizations. Published 2019. Accessed December 4, 2023. https://sirenetwork.ucsf.edu/tools-resources/resources/community-resource-referral-platforms-guide-health-care-organizations
1. Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407-419. doi:10.1111/1468-0009.12390
2. Blosnich JM, Montgomery AE, Taylor LD, Dichter ME. Adverse social factors and all-cause mortality among male and female patients receiving care in the Veterans Health Administration. Prev Med. 2020;141:106272. doi:10.1016/j.ypmed.2020.106272
3. Russell LE, Cohen AJ, Chrzas S, et al. Implementing a social needs screening and referral program among veterans: Assessing Circumstances & Offering Resources for Needs (ACORN). J Gen Intern Med. 2023;38(13):2906-2913. doi:10.1007/s11606-023-08181-9
4. Cohen AJ, Russell LE, Elwy AR, et al. Adaptation of a social risk screening and referral initiative across clinical populations, settings, and contexts in the Department of Veterans Affairs Health System. Front Health Serv. 2023;2. doi:10.3389/frhs.2022.958969
5. Cohen AJ, Kennedy MA, Mitchell KM, Russell LE. The Assessing Circumstances & Offering Resources for Needs (ACORN) initiative. Updated September 2022. Accessed December 4, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Screening_Tool.pdf
6. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212-1215. doi:10.2105/ajph.90.8.1212
7. American Public Health Association. Creating the healthiest nation: advancing health equity. Accessed November 28, 2023. https://www.apha.org/-/media/files/pdf/factsheets/advancing_health_equity.ashx?la=en&hash=9144021FDA33B4E7E02447CB28CA3F9D4BE5EF18
8. Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Aff. Published January 16, 2019. doi:10.1377/hblog20190115.234942
9. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-211. doi:10.2105/AJPH.2013.301398
10. Cohen AJ, Rudolph JL, Thomas KS, et al. Food insecurity among veterans: resources to screen and intervene. Fed Pract. 2020;37(1):16-23.
11. Iverson KM, Adjognon O, Grillo AR, et al. Intimate partner violence screening programs in the Veterans Health Administration: informing scale-up of successful practices. J Gen Intern Med. 2019;34(11):2435-2442. doi:10.1007/s11606-019-05240-y
12. National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. Accessed November 28, 2023. https://nap.nationalacademies.org/catalog/25467/integrating-social-care-into-the-delivery-of-health-care-moving
13. Gottlieb LM, Adler NE, Wing H, et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e200701. doi:10.1001/jamanetworkopen.2020.0701
14. Cornell PY, Halladay CW, Ader J, et al. Embedding social workers in Veterans Health Administration primary care teams reduces emergency department visits. Health Aff (Millwood). 2020;39(4):603-612. doi:10.1377/hlthaff.2019.01589
15. Cohen AJ, Bruton M, Hooshyar D. US Department of Veterans Affairs, Office of Health Services Research and Development. The WHO’s greatest ICD-10 hits for fiscal year 2022: social determinants of health. Published March 9, 2022. Updated November 6, 2023. Accessed December 4, 2023. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=4125

16. De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170-175. doi:10.3122/jabfm.2020.02.190309
17. Cohen AJ, Isaacson N, Torby M, Smith A, Zhang G, Patel MR. Motivators, barriers, and preferences to engagement with offered social care assistance among people with diabetes: a mixed methods study. Am J Prev Med. 2022;63(3, suppl 2):S152-S163. doi:10.1016/j.amepre.2022.02.022
18. Buitron de la Vega P, Losi S, Sprague Martinez L, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(suppl 6, suppl 2):S133-S139. doi:10.1097/MLR.0000000000001029
19. Boston Medical Center. The WE CARE Model. Accessed November 28, 2023. https://www.bmc.org/pediatrics-primary-care/we-care/we-care-model
20. US Department of Veterans Affairs, Office of Rural Health. VA social work. Updated July 11, 2023. Accessed December 4, 2023. https://www.socialwork.va.gov
21. Mitchell KM, Russell LE, Cohen AJ, Kennedy MA. Building ACORN resource guides for veterans. Accessed November 28, 2023. https://www.va.gov/HEALTHEQUITY/docs/ACORN_Resource_Guide_Manual.pdf
22. US Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health. Rural Veterans. Accessed November 28, 2023. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
23. Cartier Y, Fichtenberg C, Gottlieb L. Community resource referral platforms: a guide for health care organizations. Published 2019. Accessed December 4, 2023. https://sirenetwork.ucsf.edu/tools-resources/resources/community-resource-referral-platforms-guide-health-care-organizations
Food Insecurity Among Veterans: Resources to Screen and Intervene
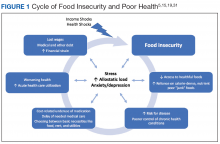
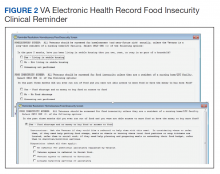
Nearly 1 in 8 households—and 1 in 6 households with children—experienced food insecurity in 2017, defined as limited or uncertain availability of nutritionally adequate and safe foods.1 Food insecurity is often even more pronounced among households with individuals with acute or chronic medical conditions.2-6 Moreover, food insecurity is independently associated with a range of adverse health outcomes, including poorer control of diabetes mellitus, hypertension, depression and other major psychiatric disorders, HIV, and chronic lung and kidney disease, as well as poorer overall health status.7-14 Food insecurity also has been associated with increased health care costs and acute care utilization as well as increased probability of delayed or missed care.15-19
The relationship between food insecurity and poor health outcomes is a complex and often cyclic phenomenon (Figure 1). Poor nutritional status is fueled by limited access to healthful foods as well as increased reliance on calorie-dense and nutrient-poor “junk” foods, which are less expensive and often more readily available in low-income neighborhoods.5,20-24 These compensatory dietary patterns place individuals at higher risk for developing cardiometabolic conditions and for poor control of these conditions.5,8,9,12,25,26 Additionally, the physiological and psychological stressors of food insecurity may precipitate depression and anxiety or worsen existing mental health conditions, resulting in feelings of overwhelm and decreased self-management capacity.5,8,27-31 Food insecurity has further been associated with poor sleep, declines in cognitive function, and increased falls, particularly among the frail and elderly.32-34
Individuals experiencing food insecurity often report having to make trade-offs between food and other necessities, such as paying rent or utilities. Additional strategies to stretch limited resources include cost-related underuse of medication and delays in needed medical care.4,17,31,35 In a nationally representative survey among adults with at least 1 chronic medical condition, 1 in 3 reported having to choose between food and medicine; 11% were unable to afford either.3 Furthermore, the inability to reliably adhere to medication regimens that need to be taken with food can result in potentially life-threatening hypoglycemia (as can lack of food regardless of medication use).5,26,36 In addition to the more obvious risks of glucose-lowering medications, such as insulin and long-acting sulfonylureas in patients experiencing food insecurity, many drugs commonly used among nondiabetic adults such as ACE-inhibitors, β blockers, quinolones, and salicylates can also precipitate hypoglycemia, and food insecurity has been associated with experiences of hypoglycemia even among individuals without diabetes mellitus.32,37 In one study the risk for hospital admissions for hypoglycemia among low-income populations increased by 27% at the end of the month when food budgets were more likely to be exhausted.38 Worsening health status and increased emergency department visits and hospitalizations may then result in lost wages and mounting medical bills, contributing to further financial strain and worsening food insecurity.
Prevalence and Importance of Food Insecurity Among US Veterans
Nearly 1.5 million veterans in the US are living below the federal poverty level (FPL).39 An additional 2.4 million veterans are living paycheck to paycheck at < 200% of the FPL.40 Veterans living in poverty are at even higher risk than nonveterans for food insecurity, homelessness, and other material hardship.41
Estimates of food insecurity among veterans vary widely, ranging from 6% to 24%—nearly twice that of the general US population.8,42-45 Higher rates of food insecurity have been reported among certain high-risk subgroups, including veterans who served in Iraq and Afghanistan (27%), female veterans (28%), homeless and formerly homeless veterans (49%), and veterans with serious mental illness (35%).6,32,43,46 Additional risk factors for food insecurity specific to veteran populations include younger age, having recently left active-duty military service, and lower final military paygrade.42,45-47 As in the general population, veteran food insecurity is associated with a range of adverse health outcomes, including poorer overall health status as well as increased probability of delayed or missed care.6,8,32,42-44,46
Even among veterans enrolled in federal food assistance programs, many still struggle to afford nutritionally adequate foods. As one example, in a study of mostly male homeless and formerly homeless veterans, O’Toole and colleagues found that nearly half of those reporting food insecurity were already receiving federal food assistance benefits, and 22% relied on emergency food resources.32 Of households served by Feeding America food pantries and meal programs, 20% have a member who has served in the US military.48
Federal Programs To Address Food Insecurity
There are several important federal food assistance programs designed to help alleviate food insecurity. The Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp program) is the largest federal food assistance program and provides low-income Americans with cash benefits to purchase food. SNAP has been shown to substantially reduce food insecurity.7,49 The program also is associated with significant decreases in cost-related medication nonadherence as well as reductions in health care costs and both acute care and nursing home utilization.16,50-54 Although nearly 1.4 million veterans live in SNAP-enrolled households, 59% of eligible veterans are not enrolled.43,55 Closing this SNAP eligibility-enrollment gap, has been a focus of recent efforts to improve long-term food security among veterans. There also are several federal food assistance programs for households with children, including the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and school meals programs. Among federal nutrition programs for seniors, the Older American’s Act contains designated funding to support nutrition services for older adults, including congregate meal programs in community settings like senior centers, places of worship, and housing communities, and home-delivered meals through programs like Meals on Wheels.56
VHA Response to Food Insecurity
The Veterans Health Administration (VHA) is the country’s largest integrated, federally funded health care system.57 In November 2015, congressional briefings on veteran food insecurity organized by the national non-profit organization MAZON: A Jewish Response to Hunger and hosted with bipartisan support were provided to the US House and Senate. As a result of these briefings, VHA chartered the national Ensuring Veteran Food Security Workgroup with a mandate to partner with governmental and nonprofit agencies to “focus on the issue of food insecurity, the identification of veterans at risk, the needed training of VHA staff and the coordination of resources and initiatives to support the veterans for whom we care.” Building off a pilot in US Department of Veterans Affairs (VA) Homeless Patient Aligned Care Teams (H-PACTs),32 VHA subsequently integrated a single-item food insecurity screening tool into the VA electronic health record (EHR) clinical reminder system (Figure 2). The clinical reminder, which was rolled out across VA medical centers nationally in October 2017, provides an alert to screen all noninstitutionalized veterans for food insecurity. To date, nearly 5 million veterans have been screened. When a veteran endorses food insecurity based on the initial screening question, a prompt appears to offer the veteran a referral to a social worker and/or dietitian. Positive screening results also should be communicated to the patient’s primary care provider. Depending on site-specific clinical flow, the reminders are typically completed in the outpatient setting either by nurses or medical assistants during intake or by providers as part of the clinical visit. However, any member of the health care team can complete the clinical reminder at any time. As of September 2019, approximately 74,000 veterans have been identified as food insecure.58
Addressing Food Insecurity
VHA has been a recognized leader in addressing homelessness and other social determinants of health through its integrated care and PACT delivery models.59-61 The food insecurity clinical reminder was designed to facilitate a tailored, interdisciplinary approach to identify and address food insecurity. Interdisciplinary care team members—including medical assistants, clinicians, social workers, registered dietitians, nurse care managers, occupational or physical therapists, and pharmacists—are uniquely positioned to identify veterans impacted by food insecurity, assess for associated clinical and/or social risk factors, and offer appropriate medical and nutrition interventions and resource referrals.
This interdisciplinary team-based model is essential given the range of potential drivers underlying veteran experiences of food insecurity and subsequent health outcomes. It is critically important for clinicians to review the medication list with veterans screening positive for food insecurity to assess for risk of hypoglycemia and/or cost-related nonadherence, make any necessary adjustments to therapeutic regimens, and assess for additional risk factors associated with food insecurity. Examples of tailored nutrition counseling that clinical dietitians may provide include meal preparation strategies for veterans who only have access to a microwave or hotplate, or recommendations for how veterans on medically restricted diets can best navigate food selection at soup kitchens or food pantries. Resource referrals provided by social workers or other care team members may include both emergency food resources to address immediate shortages (eg, food pantries, soup kitchens, or vouchers for free lunch) as well as resources focused on improving longer term food security (eg, federal food assistance programs or home delivered meal programs). Importantly, although providing a list of food resources may be helpful for some patients, such lists are often insufficient.62,63 Many patients require active assistance with program enrollment either onsite the day of their clinic visit or through connection with a partnering community-based organization that can, in turn, identify appropriate resources and facilitate program enrollment.63,64 Planned follow-up is also crucial to determine whether referrals are successful and to assess for ongoing need. Proposed roles for interdisciplinary care team members in addressing a positive food insecurity screen are outlined in Table 1.
VHA-Community Partnerships
In addition to services offered within VA, public and private sector partnerships can greatly enhance the range of resources available to food insecure veterans. Several VA facilities have developed formal community partnerships, such as the Veterans Pantry Pilot (VPP) program, a national partnership between Feeding America food banks and VA medical centers to establish onsite or mobile food pantries. There are currently 17 active Feeding America VPP sites, with a number of additional sites under development. Several of the VPP sites also include other “wraparound services,” such as SNAP application assistance.65,66
State Veterans Affairs offices67 and Veterans Service Organizations (VSOs)68 also can serve as valuable partners for connecting veterans with needed resources. VSOs offer a range of services, including assistancewith benefit claims, employment and housing assistance, emergency food assistance, and transportation to medical appointments. Some VSOs also have established local affiliations with Meals on Wheels focused on veteran outreach and providing hot meals for low-income, homebound, and disabled veterans.
Additional Resources
Although resources vary by regional setting, several key governmental and community-based food assistance programs are summarized in Table 2. Local community partners and online/phone-based directories, such as United Way’s 2-1-1 can help identify additional local resources. For older adults and individuals with disabilities, local Aging and Disability Resources Centers can provide information and assistance connecting to needed resources.69 Finally, there are a number of online resources available for clinicians interested in learning more about the impact of food insecurity on health and tools to use in the clinical setting (Table 3).
Conclusion
The VA has recognized food insecurity as a critical concern for the well-being of our nation’s veterans. Use of the EHR clinical reminder represents a crucial first step toward increasing provider awareness about veteran food insecurity and improving clinical efforts to address food insecurity once identified. Through the reminder, health care teams can connect veterans to needed resources and create both the individual and population-level data necessary to inform VHA and community efforts to address veteran food insecurity. Clinical reminder data are currently being used for local quality improvement efforts and have established the need nationally for formalized partnerships between VHA Social Work Services and Nutrition and Food Services to connect veterans with food and provide them with strategies to best use available food resources.
Moving forward, the Ensuring Veteran Food Security Workgroup continues to work with agencies and organizations across the country to improve food insecure veterans’ access to needed services. In addition to existing VA partnerships with Feeding America for the VPP, memorandums of understanding are currently underway to formalize partnerships with both the Food Research and Action Center (FRAC) and MAZON. Additional research is needed both to formally validate the current food insecurity clinical reminder screening question and to identify best practices and potential models for how to most effectively use VHA-community partnerships to address the unique needs of the veteran population.
Ensuring the food security of our nation’s veterans is essential to VA’s commitment to providing integrated, veteran-centered, whole person care. Toward that goal, VA health care teams are urged to use the clinical reminder and help connect food insecure veterans with relevant resources both within and outside of the VA health care system.
1. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017. http://www.ers.usda.gov/publications/pub-details/?pubid=90022. Published September 2018. Accessed December 9, 2019.
2. Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265.
3. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303-310.e3.
4. Lyles CR, Seligman HK, Parker MM, et al. Financial strain and medication adherence among diabetes patients in an integrated health care delivery system: The Diabetes Study of Northern California (DISTANCE). Health Serv Res. 2016;51(2):610-624.
5. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9.
6. Narain K, Bean-Mayberry B, Washington DL, Canelo IA, Darling JE, Yano EM. Access to care and health outcomes among women veterans using veterans administration health care: association with food insufficiency. Womens Health Issues. 2018;28(3):267-272.
7. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830-1839.
8. Wang EA, McGinnis KA, Goulet J, et al; Veterans Aging Cohort Study Project Team. Food insecurity and health: data from the Veterans Aging Cohort Study. Public Health Rep. 2015;130(3):261-268.
9. Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. PloS One. 2017;12(6):e0179172.
10. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310.
11. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093-3099.
12. Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238.
13. Banerjee T, Crews DC, Wesson DE, et al; CDC CKD Surveillance Team. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38-47.
14. Bruening M, Dinour LM, Chavez JBR. Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr. 2017;20(17):3200-3208.
15. Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food insecurity and health care expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600-1620.
16. Berkowitz SA, Seligman HK, Basu S. Impact of food insecurity and SNAP participation on healthcare utilization and expenditures. http://www.ukcpr.org/research/discussion-papers. Published 2017. Accessed December 9, 2019.
17. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71-77.
18. Garcia SP, Haddix A, Barnett K. Incremental health care costs associated with food insecurity and chronic conditions among older adults. Chronic Dis. 2018;15:180058.
19. Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
20. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74-81.
21. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643-660.
22. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107-1117.
23. Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181-1188.
24. Lucan SC, Maroko AR, Seitchik JL, Yoon DH, Sperry LE, Schechter CB. Unexpected neighborhood sources of food and drink: implications for research and community health. Am J Prev Med. 2018;55(2):e29-e38.
25. Castillo DC, Ramsey NL, Yu SS, Ricks M, Courville AB, Sumner AE. Inconsistent access to food and cardiometabolic disease: the effect of food insecurity. Curr Cardiovasc Risk Rep. 2012;6(3):245-250.
26. Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233.
27. Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171-186.
28. Mangurian C, Sreshta N, Seligman H. Food insecurity among adults with severe mental illness. Psychiatr Serv. 2013;64(9):931-932.
29. Melchior M, Caspi A, Howard LM, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124(4):e564-e572.
30. Brostow DP, Gunzburger E, Abbate LM, Brenner LA, Thomas KS. Mental illness, not obesity status, is associated with food insecurity among the elderly in the health and retirement study. J Nutr Gerontol Geriatr. 2019;38(2):149-172.
31. Higashi RT, Craddock Lee SJ, Pezzia C, Quirk L, Leonard T, Pruitt SL. Family and social context contributes to the interplay of economic insecurity, food insecurity, and health. Ann Anthropol Pract. 2017;41(2):67-77.
32. O’Toole TP, Roberts CB, Johnson EE. Screening for food insecurity in six Veterans Administration clinics for the homeless, June-December 2015. Prev Chronic Dis. 2017;14:160375.
33. Feil DG, Pogach LM. Cognitive impairment is a major risk factor for serious hypoglycaemia; public health intervention is warranted. Evid Based Med. 2014;19(2):77.
34. Frith E, Loprinzi PD. Food insecurity and cognitive function in older adults: Brief report. Clin Nutr. 2018;37(5):1765-1768.
35. Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health. 2015;105(10):e48-e59.
36. Tseng C-L, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2014;174(2):259-268.
37. Vue MH, Setter SM. Drug-induced glucose alterations part 1: drug-induced hypoglycemia. Diabetes Spectr. 2011;24(3):171-177.
38. Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Aff (Millwood). 2014;33(1):116-123.
39. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Veteran poverty trends. https://www.va.gov/vetdata/docs/specialreports/veteran_poverty_trends.pdf. Published May 2015. Accessed December 9, 2019.
40. Robbins KG, Ravi A. Veterans living paycheck to paycheck are under threat during budget debates. https://www.americanprogress.org/issues/poverty/news/2017/09/19/439023/veterans-living-paycheck-paycheck-threat-budget-debates. Published September 19, 2017. Accessed December 9, 2019.
41. Wilmoth JM, London AS, Heflin CM. Economic well-being among older-adult households: variation by veteran and disability status. J Gerontol Soc Work. 2015;58(4):399-419.
42. Brostow DP, Gunzburger E, Thomas KS. Food insecurity among veterans: findings from the health and retirement study. J Nutr Health Aging. 2017;21(10):1358-1364.
43. Pooler J, Mian P, Srinivasan M, Miller Z. Veterans and food insecurity. https://www.impaqint.com/sites/default/files/issue-briefs/VeteransFoodInsecurity_IssueBrief_V1.3.pdf. Published November 2018. Accessed December 9, 2019.
44. Schure MB, Katon JG, Wong E, Liu C-F. Food and housing insecurity and health status among U.S. adults with and without prior military service. SSM Popul Health. 2016;29(2):244-248.
45. Miller DP, Larson MJ, Byrne T, DeVoe E. Food insecurity in veteran households: findings from nationally representative data. Public Health Nutr. 2016;19(10):1731-1740.
46. Widome R, Jensen A, Bangerter A, Fu SS. Food insecurity among veterans of the US wars in Iraq and Afghanistan. Public Health Nutr. 2015;18(5):844-849.
47. London AS, Heflin CM. Supplemental Nutrition Assistance Program (SNAP) use among active-duty military personnel, veterans, and reservists. Popul Res Policy Rev. 2015;34(6):805-826.
48. Weinfield NS, Mills G, Borger C, et al. Hunger in America 2014. Natl rep prepared for Feeding America. https://www.feedingamerica.org/research/hunger-in-america. Published 2014. Accessed December 9, 2019.
49. Mabli J, Ohls J, Dragoset L, Castner L, Santos B. Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security. Washington, DC: US Department of Agriculture, Food and Nutrition Service; 2013.
50. Srinivasan M, Pooler JA. Cost-related medication nonadherence for older adults participating in SNAP, 2013–2015. Am J Public Health. 2017;108(2):224-230.
51. Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Progam benefits and emergency room visits for hypoglycaemia. Public Health Nutr. 2017;20(7):1314-1321.
52. Samuel LJ, Szanton SL, Cahill R, et al. Does the Supplemental Nutrition Assistance Program affect hospital utilization among older adults? The case of Maryland. Popul Health Manag. 2018;21(2):88-95.
53. Szanton SL, Samuel LJ, Cahill R, et al. Food assistance is associated with decreased nursing home admissions for Maryland’s dually eligible older adults. BMC Geriatr. 2017;17(1):162.
54. Carlson S, Keith-Jennings B. SNAP is linked with improved nutritional outcomes and lower health care costs. https://www.cbpp.org/research/food-assistance/snap-is-linked-with-improved-nutritional-outcomes-and-lower-health-care. Published January 17, 2018. Accessed December 10, 2019.
55. Keith-Jennings B, Cai L. SNAP helps almost 1.4 million low-income veterans, including thousands in every state. https://www.cbpp.org/research/food-assistance/snap-helps-almost-14-million-low-income-veterans-including-thousands-in. Updated November 8, 2018. Accessed December 10, 2019.
56. US Department of Health and Human Services. Older Americans Act nutrition programs. https://acl.gov/sites/default/files/news%202017-03/OAA-Nutrition_Programs_Fact_Sheet.pdf. Accessed December 10, 2019.
57. US Department of Veterans Affairs. About VHA. https://www.va.gov/health/aboutvha.asp. Accessed December 10, 2019.
58. US Department of Veterans Affairs. VA Corporate Data Warehouse.
59. Yano EM, Bair MJ, Carrasquillo O, Krein SL, Rubenstein LV. Patient aligned care teams (PACT): VA’s journey to implement patient-centered medical homes. J Gen Intern Med. 2014;29(suppl 2):S547-s549.
60. O’Toole TP, Pape L. Innovative efforts to address homelessness among veterans. N C Med J. 2015;76(5):311-314.
61. O’Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: the Veterans Health Administration’s “Homeless Patient Aligned Care Team” Program. Prev Chronic Dis. 2016;13:150567.
62. Marpadga S, Fernandez A, Leung J, Tang A, Seligman H, Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23.
63. Stenmark SH, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman H. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente Colorado. Perm J. 2018;22.
64. Martel ML, Klein LR, Hager KA, Cutts DB. Emergency department experience with novel electronic medical record order for referral to food resources. West J Emerg Med. 2018;19(2):232-237.
65. Going C, Cohen AJ, Bares M, Christensen M. Interdisciplinary approaches to addressing the food insecure veteran. Veterans Health Administration Employee Education System webinar; October 30, 2018.
66. Feeding America Announces New Partnership With U.S. Department Of Veterans Affairs. https://www.prnewswire.com/news-releases/feeding-america-announces-new-partnership-with-us-department-of-veterans-affairs-300481891.html. Published June 29, 2017. Accessed December 10, 2019.
67. US Department of Veterans Affairs. State Veterans Affairs offices. https://www.va.gov/statedva.htm. Updated March 20, 2019. Accessed December 10, 2019.
68. US Department of Veterans Affairs. Directory of veterans service organizations. https://www.va.gov/vso. Updated December 24, 2013. Accessed December 10, 2019.
69. ACL Administration for Community Living. Aging and disability resource centers. https://acl.gov/programs/aging-and-disability-networks/aging-and-disability-resource-centers. Updated December 13, 2017. Accessed December 10, 2019.
70. Nutrition and Obesity Policy Research and Evaluation Network (NOPREN). Clinical screening algorithms. https://nopren.org/resource/download-food-insecurity-screening-and-referral-algorithms-for-adults-patients-living-with-diabetes-and-pediatric-patients. Accessed December 10, 2019.
Nearly 1 in 8 households—and 1 in 6 households with children—experienced food insecurity in 2017, defined as limited or uncertain availability of nutritionally adequate and safe foods.1 Food insecurity is often even more pronounced among households with individuals with acute or chronic medical conditions.2-6 Moreover, food insecurity is independently associated with a range of adverse health outcomes, including poorer control of diabetes mellitus, hypertension, depression and other major psychiatric disorders, HIV, and chronic lung and kidney disease, as well as poorer overall health status.7-14 Food insecurity also has been associated with increased health care costs and acute care utilization as well as increased probability of delayed or missed care.15-19
The relationship between food insecurity and poor health outcomes is a complex and often cyclic phenomenon (Figure 1). Poor nutritional status is fueled by limited access to healthful foods as well as increased reliance on calorie-dense and nutrient-poor “junk” foods, which are less expensive and often more readily available in low-income neighborhoods.5,20-24 These compensatory dietary patterns place individuals at higher risk for developing cardiometabolic conditions and for poor control of these conditions.5,8,9,12,25,26 Additionally, the physiological and psychological stressors of food insecurity may precipitate depression and anxiety or worsen existing mental health conditions, resulting in feelings of overwhelm and decreased self-management capacity.5,8,27-31 Food insecurity has further been associated with poor sleep, declines in cognitive function, and increased falls, particularly among the frail and elderly.32-34
Individuals experiencing food insecurity often report having to make trade-offs between food and other necessities, such as paying rent or utilities. Additional strategies to stretch limited resources include cost-related underuse of medication and delays in needed medical care.4,17,31,35 In a nationally representative survey among adults with at least 1 chronic medical condition, 1 in 3 reported having to choose between food and medicine; 11% were unable to afford either.3 Furthermore, the inability to reliably adhere to medication regimens that need to be taken with food can result in potentially life-threatening hypoglycemia (as can lack of food regardless of medication use).5,26,36 In addition to the more obvious risks of glucose-lowering medications, such as insulin and long-acting sulfonylureas in patients experiencing food insecurity, many drugs commonly used among nondiabetic adults such as ACE-inhibitors, β blockers, quinolones, and salicylates can also precipitate hypoglycemia, and food insecurity has been associated with experiences of hypoglycemia even among individuals without diabetes mellitus.32,37 In one study the risk for hospital admissions for hypoglycemia among low-income populations increased by 27% at the end of the month when food budgets were more likely to be exhausted.38 Worsening health status and increased emergency department visits and hospitalizations may then result in lost wages and mounting medical bills, contributing to further financial strain and worsening food insecurity.
Prevalence and Importance of Food Insecurity Among US Veterans
Nearly 1.5 million veterans in the US are living below the federal poverty level (FPL).39 An additional 2.4 million veterans are living paycheck to paycheck at < 200% of the FPL.40 Veterans living in poverty are at even higher risk than nonveterans for food insecurity, homelessness, and other material hardship.41
Estimates of food insecurity among veterans vary widely, ranging from 6% to 24%—nearly twice that of the general US population.8,42-45 Higher rates of food insecurity have been reported among certain high-risk subgroups, including veterans who served in Iraq and Afghanistan (27%), female veterans (28%), homeless and formerly homeless veterans (49%), and veterans with serious mental illness (35%).6,32,43,46 Additional risk factors for food insecurity specific to veteran populations include younger age, having recently left active-duty military service, and lower final military paygrade.42,45-47 As in the general population, veteran food insecurity is associated with a range of adverse health outcomes, including poorer overall health status as well as increased probability of delayed or missed care.6,8,32,42-44,46
Even among veterans enrolled in federal food assistance programs, many still struggle to afford nutritionally adequate foods. As one example, in a study of mostly male homeless and formerly homeless veterans, O’Toole and colleagues found that nearly half of those reporting food insecurity were already receiving federal food assistance benefits, and 22% relied on emergency food resources.32 Of households served by Feeding America food pantries and meal programs, 20% have a member who has served in the US military.48
Federal Programs To Address Food Insecurity
There are several important federal food assistance programs designed to help alleviate food insecurity. The Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp program) is the largest federal food assistance program and provides low-income Americans with cash benefits to purchase food. SNAP has been shown to substantially reduce food insecurity.7,49 The program also is associated with significant decreases in cost-related medication nonadherence as well as reductions in health care costs and both acute care and nursing home utilization.16,50-54 Although nearly 1.4 million veterans live in SNAP-enrolled households, 59% of eligible veterans are not enrolled.43,55 Closing this SNAP eligibility-enrollment gap, has been a focus of recent efforts to improve long-term food security among veterans. There also are several federal food assistance programs for households with children, including the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and school meals programs. Among federal nutrition programs for seniors, the Older American’s Act contains designated funding to support nutrition services for older adults, including congregate meal programs in community settings like senior centers, places of worship, and housing communities, and home-delivered meals through programs like Meals on Wheels.56
VHA Response to Food Insecurity
The Veterans Health Administration (VHA) is the country’s largest integrated, federally funded health care system.57 In November 2015, congressional briefings on veteran food insecurity organized by the national non-profit organization MAZON: A Jewish Response to Hunger and hosted with bipartisan support were provided to the US House and Senate. As a result of these briefings, VHA chartered the national Ensuring Veteran Food Security Workgroup with a mandate to partner with governmental and nonprofit agencies to “focus on the issue of food insecurity, the identification of veterans at risk, the needed training of VHA staff and the coordination of resources and initiatives to support the veterans for whom we care.” Building off a pilot in US Department of Veterans Affairs (VA) Homeless Patient Aligned Care Teams (H-PACTs),32 VHA subsequently integrated a single-item food insecurity screening tool into the VA electronic health record (EHR) clinical reminder system (Figure 2). The clinical reminder, which was rolled out across VA medical centers nationally in October 2017, provides an alert to screen all noninstitutionalized veterans for food insecurity. To date, nearly 5 million veterans have been screened. When a veteran endorses food insecurity based on the initial screening question, a prompt appears to offer the veteran a referral to a social worker and/or dietitian. Positive screening results also should be communicated to the patient’s primary care provider. Depending on site-specific clinical flow, the reminders are typically completed in the outpatient setting either by nurses or medical assistants during intake or by providers as part of the clinical visit. However, any member of the health care team can complete the clinical reminder at any time. As of September 2019, approximately 74,000 veterans have been identified as food insecure.58
Addressing Food Insecurity
VHA has been a recognized leader in addressing homelessness and other social determinants of health through its integrated care and PACT delivery models.59-61 The food insecurity clinical reminder was designed to facilitate a tailored, interdisciplinary approach to identify and address food insecurity. Interdisciplinary care team members—including medical assistants, clinicians, social workers, registered dietitians, nurse care managers, occupational or physical therapists, and pharmacists—are uniquely positioned to identify veterans impacted by food insecurity, assess for associated clinical and/or social risk factors, and offer appropriate medical and nutrition interventions and resource referrals.
This interdisciplinary team-based model is essential given the range of potential drivers underlying veteran experiences of food insecurity and subsequent health outcomes. It is critically important for clinicians to review the medication list with veterans screening positive for food insecurity to assess for risk of hypoglycemia and/or cost-related nonadherence, make any necessary adjustments to therapeutic regimens, and assess for additional risk factors associated with food insecurity. Examples of tailored nutrition counseling that clinical dietitians may provide include meal preparation strategies for veterans who only have access to a microwave or hotplate, or recommendations for how veterans on medically restricted diets can best navigate food selection at soup kitchens or food pantries. Resource referrals provided by social workers or other care team members may include both emergency food resources to address immediate shortages (eg, food pantries, soup kitchens, or vouchers for free lunch) as well as resources focused on improving longer term food security (eg, federal food assistance programs or home delivered meal programs). Importantly, although providing a list of food resources may be helpful for some patients, such lists are often insufficient.62,63 Many patients require active assistance with program enrollment either onsite the day of their clinic visit or through connection with a partnering community-based organization that can, in turn, identify appropriate resources and facilitate program enrollment.63,64 Planned follow-up is also crucial to determine whether referrals are successful and to assess for ongoing need. Proposed roles for interdisciplinary care team members in addressing a positive food insecurity screen are outlined in Table 1.
VHA-Community Partnerships
In addition to services offered within VA, public and private sector partnerships can greatly enhance the range of resources available to food insecure veterans. Several VA facilities have developed formal community partnerships, such as the Veterans Pantry Pilot (VPP) program, a national partnership between Feeding America food banks and VA medical centers to establish onsite or mobile food pantries. There are currently 17 active Feeding America VPP sites, with a number of additional sites under development. Several of the VPP sites also include other “wraparound services,” such as SNAP application assistance.65,66
State Veterans Affairs offices67 and Veterans Service Organizations (VSOs)68 also can serve as valuable partners for connecting veterans with needed resources. VSOs offer a range of services, including assistancewith benefit claims, employment and housing assistance, emergency food assistance, and transportation to medical appointments. Some VSOs also have established local affiliations with Meals on Wheels focused on veteran outreach and providing hot meals for low-income, homebound, and disabled veterans.
Additional Resources
Although resources vary by regional setting, several key governmental and community-based food assistance programs are summarized in Table 2. Local community partners and online/phone-based directories, such as United Way’s 2-1-1 can help identify additional local resources. For older adults and individuals with disabilities, local Aging and Disability Resources Centers can provide information and assistance connecting to needed resources.69 Finally, there are a number of online resources available for clinicians interested in learning more about the impact of food insecurity on health and tools to use in the clinical setting (Table 3).
Conclusion
The VA has recognized food insecurity as a critical concern for the well-being of our nation’s veterans. Use of the EHR clinical reminder represents a crucial first step toward increasing provider awareness about veteran food insecurity and improving clinical efforts to address food insecurity once identified. Through the reminder, health care teams can connect veterans to needed resources and create both the individual and population-level data necessary to inform VHA and community efforts to address veteran food insecurity. Clinical reminder data are currently being used for local quality improvement efforts and have established the need nationally for formalized partnerships between VHA Social Work Services and Nutrition and Food Services to connect veterans with food and provide them with strategies to best use available food resources.
Moving forward, the Ensuring Veteran Food Security Workgroup continues to work with agencies and organizations across the country to improve food insecure veterans’ access to needed services. In addition to existing VA partnerships with Feeding America for the VPP, memorandums of understanding are currently underway to formalize partnerships with both the Food Research and Action Center (FRAC) and MAZON. Additional research is needed both to formally validate the current food insecurity clinical reminder screening question and to identify best practices and potential models for how to most effectively use VHA-community partnerships to address the unique needs of the veteran population.
Ensuring the food security of our nation’s veterans is essential to VA’s commitment to providing integrated, veteran-centered, whole person care. Toward that goal, VA health care teams are urged to use the clinical reminder and help connect food insecure veterans with relevant resources both within and outside of the VA health care system.
Nearly 1 in 8 households—and 1 in 6 households with children—experienced food insecurity in 2017, defined as limited or uncertain availability of nutritionally adequate and safe foods.1 Food insecurity is often even more pronounced among households with individuals with acute or chronic medical conditions.2-6 Moreover, food insecurity is independently associated with a range of adverse health outcomes, including poorer control of diabetes mellitus, hypertension, depression and other major psychiatric disorders, HIV, and chronic lung and kidney disease, as well as poorer overall health status.7-14 Food insecurity also has been associated with increased health care costs and acute care utilization as well as increased probability of delayed or missed care.15-19
The relationship between food insecurity and poor health outcomes is a complex and often cyclic phenomenon (Figure 1). Poor nutritional status is fueled by limited access to healthful foods as well as increased reliance on calorie-dense and nutrient-poor “junk” foods, which are less expensive and often more readily available in low-income neighborhoods.5,20-24 These compensatory dietary patterns place individuals at higher risk for developing cardiometabolic conditions and for poor control of these conditions.5,8,9,12,25,26 Additionally, the physiological and psychological stressors of food insecurity may precipitate depression and anxiety or worsen existing mental health conditions, resulting in feelings of overwhelm and decreased self-management capacity.5,8,27-31 Food insecurity has further been associated with poor sleep, declines in cognitive function, and increased falls, particularly among the frail and elderly.32-34
Individuals experiencing food insecurity often report having to make trade-offs between food and other necessities, such as paying rent or utilities. Additional strategies to stretch limited resources include cost-related underuse of medication and delays in needed medical care.4,17,31,35 In a nationally representative survey among adults with at least 1 chronic medical condition, 1 in 3 reported having to choose between food and medicine; 11% were unable to afford either.3 Furthermore, the inability to reliably adhere to medication regimens that need to be taken with food can result in potentially life-threatening hypoglycemia (as can lack of food regardless of medication use).5,26,36 In addition to the more obvious risks of glucose-lowering medications, such as insulin and long-acting sulfonylureas in patients experiencing food insecurity, many drugs commonly used among nondiabetic adults such as ACE-inhibitors, β blockers, quinolones, and salicylates can also precipitate hypoglycemia, and food insecurity has been associated with experiences of hypoglycemia even among individuals without diabetes mellitus.32,37 In one study the risk for hospital admissions for hypoglycemia among low-income populations increased by 27% at the end of the month when food budgets were more likely to be exhausted.38 Worsening health status and increased emergency department visits and hospitalizations may then result in lost wages and mounting medical bills, contributing to further financial strain and worsening food insecurity.
Prevalence and Importance of Food Insecurity Among US Veterans
Nearly 1.5 million veterans in the US are living below the federal poverty level (FPL).39 An additional 2.4 million veterans are living paycheck to paycheck at < 200% of the FPL.40 Veterans living in poverty are at even higher risk than nonveterans for food insecurity, homelessness, and other material hardship.41
Estimates of food insecurity among veterans vary widely, ranging from 6% to 24%—nearly twice that of the general US population.8,42-45 Higher rates of food insecurity have been reported among certain high-risk subgroups, including veterans who served in Iraq and Afghanistan (27%), female veterans (28%), homeless and formerly homeless veterans (49%), and veterans with serious mental illness (35%).6,32,43,46 Additional risk factors for food insecurity specific to veteran populations include younger age, having recently left active-duty military service, and lower final military paygrade.42,45-47 As in the general population, veteran food insecurity is associated with a range of adverse health outcomes, including poorer overall health status as well as increased probability of delayed or missed care.6,8,32,42-44,46
Even among veterans enrolled in federal food assistance programs, many still struggle to afford nutritionally adequate foods. As one example, in a study of mostly male homeless and formerly homeless veterans, O’Toole and colleagues found that nearly half of those reporting food insecurity were already receiving federal food assistance benefits, and 22% relied on emergency food resources.32 Of households served by Feeding America food pantries and meal programs, 20% have a member who has served in the US military.48
Federal Programs To Address Food Insecurity
There are several important federal food assistance programs designed to help alleviate food insecurity. The Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp program) is the largest federal food assistance program and provides low-income Americans with cash benefits to purchase food. SNAP has been shown to substantially reduce food insecurity.7,49 The program also is associated with significant decreases in cost-related medication nonadherence as well as reductions in health care costs and both acute care and nursing home utilization.16,50-54 Although nearly 1.4 million veterans live in SNAP-enrolled households, 59% of eligible veterans are not enrolled.43,55 Closing this SNAP eligibility-enrollment gap, has been a focus of recent efforts to improve long-term food security among veterans. There also are several federal food assistance programs for households with children, including the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and school meals programs. Among federal nutrition programs for seniors, the Older American’s Act contains designated funding to support nutrition services for older adults, including congregate meal programs in community settings like senior centers, places of worship, and housing communities, and home-delivered meals through programs like Meals on Wheels.56
VHA Response to Food Insecurity
The Veterans Health Administration (VHA) is the country’s largest integrated, federally funded health care system.57 In November 2015, congressional briefings on veteran food insecurity organized by the national non-profit organization MAZON: A Jewish Response to Hunger and hosted with bipartisan support were provided to the US House and Senate. As a result of these briefings, VHA chartered the national Ensuring Veteran Food Security Workgroup with a mandate to partner with governmental and nonprofit agencies to “focus on the issue of food insecurity, the identification of veterans at risk, the needed training of VHA staff and the coordination of resources and initiatives to support the veterans for whom we care.” Building off a pilot in US Department of Veterans Affairs (VA) Homeless Patient Aligned Care Teams (H-PACTs),32 VHA subsequently integrated a single-item food insecurity screening tool into the VA electronic health record (EHR) clinical reminder system (Figure 2). The clinical reminder, which was rolled out across VA medical centers nationally in October 2017, provides an alert to screen all noninstitutionalized veterans for food insecurity. To date, nearly 5 million veterans have been screened. When a veteran endorses food insecurity based on the initial screening question, a prompt appears to offer the veteran a referral to a social worker and/or dietitian. Positive screening results also should be communicated to the patient’s primary care provider. Depending on site-specific clinical flow, the reminders are typically completed in the outpatient setting either by nurses or medical assistants during intake or by providers as part of the clinical visit. However, any member of the health care team can complete the clinical reminder at any time. As of September 2019, approximately 74,000 veterans have been identified as food insecure.58
Addressing Food Insecurity
VHA has been a recognized leader in addressing homelessness and other social determinants of health through its integrated care and PACT delivery models.59-61 The food insecurity clinical reminder was designed to facilitate a tailored, interdisciplinary approach to identify and address food insecurity. Interdisciplinary care team members—including medical assistants, clinicians, social workers, registered dietitians, nurse care managers, occupational or physical therapists, and pharmacists—are uniquely positioned to identify veterans impacted by food insecurity, assess for associated clinical and/or social risk factors, and offer appropriate medical and nutrition interventions and resource referrals.
This interdisciplinary team-based model is essential given the range of potential drivers underlying veteran experiences of food insecurity and subsequent health outcomes. It is critically important for clinicians to review the medication list with veterans screening positive for food insecurity to assess for risk of hypoglycemia and/or cost-related nonadherence, make any necessary adjustments to therapeutic regimens, and assess for additional risk factors associated with food insecurity. Examples of tailored nutrition counseling that clinical dietitians may provide include meal preparation strategies for veterans who only have access to a microwave or hotplate, or recommendations for how veterans on medically restricted diets can best navigate food selection at soup kitchens or food pantries. Resource referrals provided by social workers or other care team members may include both emergency food resources to address immediate shortages (eg, food pantries, soup kitchens, or vouchers for free lunch) as well as resources focused on improving longer term food security (eg, federal food assistance programs or home delivered meal programs). Importantly, although providing a list of food resources may be helpful for some patients, such lists are often insufficient.62,63 Many patients require active assistance with program enrollment either onsite the day of their clinic visit or through connection with a partnering community-based organization that can, in turn, identify appropriate resources and facilitate program enrollment.63,64 Planned follow-up is also crucial to determine whether referrals are successful and to assess for ongoing need. Proposed roles for interdisciplinary care team members in addressing a positive food insecurity screen are outlined in Table 1.
VHA-Community Partnerships
In addition to services offered within VA, public and private sector partnerships can greatly enhance the range of resources available to food insecure veterans. Several VA facilities have developed formal community partnerships, such as the Veterans Pantry Pilot (VPP) program, a national partnership between Feeding America food banks and VA medical centers to establish onsite or mobile food pantries. There are currently 17 active Feeding America VPP sites, with a number of additional sites under development. Several of the VPP sites also include other “wraparound services,” such as SNAP application assistance.65,66
State Veterans Affairs offices67 and Veterans Service Organizations (VSOs)68 also can serve as valuable partners for connecting veterans with needed resources. VSOs offer a range of services, including assistancewith benefit claims, employment and housing assistance, emergency food assistance, and transportation to medical appointments. Some VSOs also have established local affiliations with Meals on Wheels focused on veteran outreach and providing hot meals for low-income, homebound, and disabled veterans.
Additional Resources
Although resources vary by regional setting, several key governmental and community-based food assistance programs are summarized in Table 2. Local community partners and online/phone-based directories, such as United Way’s 2-1-1 can help identify additional local resources. For older adults and individuals with disabilities, local Aging and Disability Resources Centers can provide information and assistance connecting to needed resources.69 Finally, there are a number of online resources available for clinicians interested in learning more about the impact of food insecurity on health and tools to use in the clinical setting (Table 3).
Conclusion
The VA has recognized food insecurity as a critical concern for the well-being of our nation’s veterans. Use of the EHR clinical reminder represents a crucial first step toward increasing provider awareness about veteran food insecurity and improving clinical efforts to address food insecurity once identified. Through the reminder, health care teams can connect veterans to needed resources and create both the individual and population-level data necessary to inform VHA and community efforts to address veteran food insecurity. Clinical reminder data are currently being used for local quality improvement efforts and have established the need nationally for formalized partnerships between VHA Social Work Services and Nutrition and Food Services to connect veterans with food and provide them with strategies to best use available food resources.
Moving forward, the Ensuring Veteran Food Security Workgroup continues to work with agencies and organizations across the country to improve food insecure veterans’ access to needed services. In addition to existing VA partnerships with Feeding America for the VPP, memorandums of understanding are currently underway to formalize partnerships with both the Food Research and Action Center (FRAC) and MAZON. Additional research is needed both to formally validate the current food insecurity clinical reminder screening question and to identify best practices and potential models for how to most effectively use VHA-community partnerships to address the unique needs of the veteran population.
Ensuring the food security of our nation’s veterans is essential to VA’s commitment to providing integrated, veteran-centered, whole person care. Toward that goal, VA health care teams are urged to use the clinical reminder and help connect food insecure veterans with relevant resources both within and outside of the VA health care system.
1. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017. http://www.ers.usda.gov/publications/pub-details/?pubid=90022. Published September 2018. Accessed December 9, 2019.
2. Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265.
3. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303-310.e3.
4. Lyles CR, Seligman HK, Parker MM, et al. Financial strain and medication adherence among diabetes patients in an integrated health care delivery system: The Diabetes Study of Northern California (DISTANCE). Health Serv Res. 2016;51(2):610-624.
5. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9.
6. Narain K, Bean-Mayberry B, Washington DL, Canelo IA, Darling JE, Yano EM. Access to care and health outcomes among women veterans using veterans administration health care: association with food insufficiency. Womens Health Issues. 2018;28(3):267-272.
7. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830-1839.
8. Wang EA, McGinnis KA, Goulet J, et al; Veterans Aging Cohort Study Project Team. Food insecurity and health: data from the Veterans Aging Cohort Study. Public Health Rep. 2015;130(3):261-268.
9. Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. PloS One. 2017;12(6):e0179172.
10. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310.
11. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093-3099.
12. Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238.
13. Banerjee T, Crews DC, Wesson DE, et al; CDC CKD Surveillance Team. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38-47.
14. Bruening M, Dinour LM, Chavez JBR. Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr. 2017;20(17):3200-3208.
15. Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food insecurity and health care expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600-1620.
16. Berkowitz SA, Seligman HK, Basu S. Impact of food insecurity and SNAP participation on healthcare utilization and expenditures. http://www.ukcpr.org/research/discussion-papers. Published 2017. Accessed December 9, 2019.
17. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71-77.
18. Garcia SP, Haddix A, Barnett K. Incremental health care costs associated with food insecurity and chronic conditions among older adults. Chronic Dis. 2018;15:180058.
19. Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
20. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74-81.
21. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643-660.
22. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107-1117.
23. Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181-1188.
24. Lucan SC, Maroko AR, Seitchik JL, Yoon DH, Sperry LE, Schechter CB. Unexpected neighborhood sources of food and drink: implications for research and community health. Am J Prev Med. 2018;55(2):e29-e38.
25. Castillo DC, Ramsey NL, Yu SS, Ricks M, Courville AB, Sumner AE. Inconsistent access to food and cardiometabolic disease: the effect of food insecurity. Curr Cardiovasc Risk Rep. 2012;6(3):245-250.
26. Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233.
27. Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171-186.
28. Mangurian C, Sreshta N, Seligman H. Food insecurity among adults with severe mental illness. Psychiatr Serv. 2013;64(9):931-932.
29. Melchior M, Caspi A, Howard LM, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124(4):e564-e572.
30. Brostow DP, Gunzburger E, Abbate LM, Brenner LA, Thomas KS. Mental illness, not obesity status, is associated with food insecurity among the elderly in the health and retirement study. J Nutr Gerontol Geriatr. 2019;38(2):149-172.
31. Higashi RT, Craddock Lee SJ, Pezzia C, Quirk L, Leonard T, Pruitt SL. Family and social context contributes to the interplay of economic insecurity, food insecurity, and health. Ann Anthropol Pract. 2017;41(2):67-77.
32. O’Toole TP, Roberts CB, Johnson EE. Screening for food insecurity in six Veterans Administration clinics for the homeless, June-December 2015. Prev Chronic Dis. 2017;14:160375.
33. Feil DG, Pogach LM. Cognitive impairment is a major risk factor for serious hypoglycaemia; public health intervention is warranted. Evid Based Med. 2014;19(2):77.
34. Frith E, Loprinzi PD. Food insecurity and cognitive function in older adults: Brief report. Clin Nutr. 2018;37(5):1765-1768.
35. Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health. 2015;105(10):e48-e59.
36. Tseng C-L, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2014;174(2):259-268.
37. Vue MH, Setter SM. Drug-induced glucose alterations part 1: drug-induced hypoglycemia. Diabetes Spectr. 2011;24(3):171-177.
38. Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Aff (Millwood). 2014;33(1):116-123.
39. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Veteran poverty trends. https://www.va.gov/vetdata/docs/specialreports/veteran_poverty_trends.pdf. Published May 2015. Accessed December 9, 2019.
40. Robbins KG, Ravi A. Veterans living paycheck to paycheck are under threat during budget debates. https://www.americanprogress.org/issues/poverty/news/2017/09/19/439023/veterans-living-paycheck-paycheck-threat-budget-debates. Published September 19, 2017. Accessed December 9, 2019.
41. Wilmoth JM, London AS, Heflin CM. Economic well-being among older-adult households: variation by veteran and disability status. J Gerontol Soc Work. 2015;58(4):399-419.
42. Brostow DP, Gunzburger E, Thomas KS. Food insecurity among veterans: findings from the health and retirement study. J Nutr Health Aging. 2017;21(10):1358-1364.
43. Pooler J, Mian P, Srinivasan M, Miller Z. Veterans and food insecurity. https://www.impaqint.com/sites/default/files/issue-briefs/VeteransFoodInsecurity_IssueBrief_V1.3.pdf. Published November 2018. Accessed December 9, 2019.
44. Schure MB, Katon JG, Wong E, Liu C-F. Food and housing insecurity and health status among U.S. adults with and without prior military service. SSM Popul Health. 2016;29(2):244-248.
45. Miller DP, Larson MJ, Byrne T, DeVoe E. Food insecurity in veteran households: findings from nationally representative data. Public Health Nutr. 2016;19(10):1731-1740.
46. Widome R, Jensen A, Bangerter A, Fu SS. Food insecurity among veterans of the US wars in Iraq and Afghanistan. Public Health Nutr. 2015;18(5):844-849.
47. London AS, Heflin CM. Supplemental Nutrition Assistance Program (SNAP) use among active-duty military personnel, veterans, and reservists. Popul Res Policy Rev. 2015;34(6):805-826.
48. Weinfield NS, Mills G, Borger C, et al. Hunger in America 2014. Natl rep prepared for Feeding America. https://www.feedingamerica.org/research/hunger-in-america. Published 2014. Accessed December 9, 2019.
49. Mabli J, Ohls J, Dragoset L, Castner L, Santos B. Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security. Washington, DC: US Department of Agriculture, Food and Nutrition Service; 2013.
50. Srinivasan M, Pooler JA. Cost-related medication nonadherence for older adults participating in SNAP, 2013–2015. Am J Public Health. 2017;108(2):224-230.
51. Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Progam benefits and emergency room visits for hypoglycaemia. Public Health Nutr. 2017;20(7):1314-1321.
52. Samuel LJ, Szanton SL, Cahill R, et al. Does the Supplemental Nutrition Assistance Program affect hospital utilization among older adults? The case of Maryland. Popul Health Manag. 2018;21(2):88-95.
53. Szanton SL, Samuel LJ, Cahill R, et al. Food assistance is associated with decreased nursing home admissions for Maryland’s dually eligible older adults. BMC Geriatr. 2017;17(1):162.
54. Carlson S, Keith-Jennings B. SNAP is linked with improved nutritional outcomes and lower health care costs. https://www.cbpp.org/research/food-assistance/snap-is-linked-with-improved-nutritional-outcomes-and-lower-health-care. Published January 17, 2018. Accessed December 10, 2019.
55. Keith-Jennings B, Cai L. SNAP helps almost 1.4 million low-income veterans, including thousands in every state. https://www.cbpp.org/research/food-assistance/snap-helps-almost-14-million-low-income-veterans-including-thousands-in. Updated November 8, 2018. Accessed December 10, 2019.
56. US Department of Health and Human Services. Older Americans Act nutrition programs. https://acl.gov/sites/default/files/news%202017-03/OAA-Nutrition_Programs_Fact_Sheet.pdf. Accessed December 10, 2019.
57. US Department of Veterans Affairs. About VHA. https://www.va.gov/health/aboutvha.asp. Accessed December 10, 2019.
58. US Department of Veterans Affairs. VA Corporate Data Warehouse.
59. Yano EM, Bair MJ, Carrasquillo O, Krein SL, Rubenstein LV. Patient aligned care teams (PACT): VA’s journey to implement patient-centered medical homes. J Gen Intern Med. 2014;29(suppl 2):S547-s549.
60. O’Toole TP, Pape L. Innovative efforts to address homelessness among veterans. N C Med J. 2015;76(5):311-314.
61. O’Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: the Veterans Health Administration’s “Homeless Patient Aligned Care Team” Program. Prev Chronic Dis. 2016;13:150567.
62. Marpadga S, Fernandez A, Leung J, Tang A, Seligman H, Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23.
63. Stenmark SH, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman H. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente Colorado. Perm J. 2018;22.
64. Martel ML, Klein LR, Hager KA, Cutts DB. Emergency department experience with novel electronic medical record order for referral to food resources. West J Emerg Med. 2018;19(2):232-237.
65. Going C, Cohen AJ, Bares M, Christensen M. Interdisciplinary approaches to addressing the food insecure veteran. Veterans Health Administration Employee Education System webinar; October 30, 2018.
66. Feeding America Announces New Partnership With U.S. Department Of Veterans Affairs. https://www.prnewswire.com/news-releases/feeding-america-announces-new-partnership-with-us-department-of-veterans-affairs-300481891.html. Published June 29, 2017. Accessed December 10, 2019.
67. US Department of Veterans Affairs. State Veterans Affairs offices. https://www.va.gov/statedva.htm. Updated March 20, 2019. Accessed December 10, 2019.
68. US Department of Veterans Affairs. Directory of veterans service organizations. https://www.va.gov/vso. Updated December 24, 2013. Accessed December 10, 2019.
69. ACL Administration for Community Living. Aging and disability resource centers. https://acl.gov/programs/aging-and-disability-networks/aging-and-disability-resource-centers. Updated December 13, 2017. Accessed December 10, 2019.
70. Nutrition and Obesity Policy Research and Evaluation Network (NOPREN). Clinical screening algorithms. https://nopren.org/resource/download-food-insecurity-screening-and-referral-algorithms-for-adults-patients-living-with-diabetes-and-pediatric-patients. Accessed December 10, 2019.
1. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017. http://www.ers.usda.gov/publications/pub-details/?pubid=90022. Published September 2018. Accessed December 9, 2019.
2. Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265.
3. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303-310.e3.
4. Lyles CR, Seligman HK, Parker MM, et al. Financial strain and medication adherence among diabetes patients in an integrated health care delivery system: The Diabetes Study of Northern California (DISTANCE). Health Serv Res. 2016;51(2):610-624.
5. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9.
6. Narain K, Bean-Mayberry B, Washington DL, Canelo IA, Darling JE, Yano EM. Access to care and health outcomes among women veterans using veterans administration health care: association with food insufficiency. Womens Health Issues. 2018;28(3):267-272.
7. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830-1839.
8. Wang EA, McGinnis KA, Goulet J, et al; Veterans Aging Cohort Study Project Team. Food insecurity and health: data from the Veterans Aging Cohort Study. Public Health Rep. 2015;130(3):261-268.
9. Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. PloS One. 2017;12(6):e0179172.
10. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310.
11. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093-3099.
12. Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238.
13. Banerjee T, Crews DC, Wesson DE, et al; CDC CKD Surveillance Team. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38-47.
14. Bruening M, Dinour LM, Chavez JBR. Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr. 2017;20(17):3200-3208.
15. Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food insecurity and health care expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600-1620.
16. Berkowitz SA, Seligman HK, Basu S. Impact of food insecurity and SNAP participation on healthcare utilization and expenditures. http://www.ukcpr.org/research/discussion-papers. Published 2017. Accessed December 9, 2019.
17. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71-77.
18. Garcia SP, Haddix A, Barnett K. Incremental health care costs associated with food insecurity and chronic conditions among older adults. Chronic Dis. 2018;15:180058.
19. Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
20. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74-81.
21. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643-660.
22. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107-1117.
23. Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181-1188.
24. Lucan SC, Maroko AR, Seitchik JL, Yoon DH, Sperry LE, Schechter CB. Unexpected neighborhood sources of food and drink: implications for research and community health. Am J Prev Med. 2018;55(2):e29-e38.
25. Castillo DC, Ramsey NL, Yu SS, Ricks M, Courville AB, Sumner AE. Inconsistent access to food and cardiometabolic disease: the effect of food insecurity. Curr Cardiovasc Risk Rep. 2012;6(3):245-250.
26. Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233.
27. Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171-186.
28. Mangurian C, Sreshta N, Seligman H. Food insecurity among adults with severe mental illness. Psychiatr Serv. 2013;64(9):931-932.
29. Melchior M, Caspi A, Howard LM, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124(4):e564-e572.
30. Brostow DP, Gunzburger E, Abbate LM, Brenner LA, Thomas KS. Mental illness, not obesity status, is associated with food insecurity among the elderly in the health and retirement study. J Nutr Gerontol Geriatr. 2019;38(2):149-172.
31. Higashi RT, Craddock Lee SJ, Pezzia C, Quirk L, Leonard T, Pruitt SL. Family and social context contributes to the interplay of economic insecurity, food insecurity, and health. Ann Anthropol Pract. 2017;41(2):67-77.
32. O’Toole TP, Roberts CB, Johnson EE. Screening for food insecurity in six Veterans Administration clinics for the homeless, June-December 2015. Prev Chronic Dis. 2017;14:160375.
33. Feil DG, Pogach LM. Cognitive impairment is a major risk factor for serious hypoglycaemia; public health intervention is warranted. Evid Based Med. 2014;19(2):77.
34. Frith E, Loprinzi PD. Food insecurity and cognitive function in older adults: Brief report. Clin Nutr. 2018;37(5):1765-1768.
35. Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health. 2015;105(10):e48-e59.
36. Tseng C-L, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2014;174(2):259-268.
37. Vue MH, Setter SM. Drug-induced glucose alterations part 1: drug-induced hypoglycemia. Diabetes Spectr. 2011;24(3):171-177.
38. Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Aff (Millwood). 2014;33(1):116-123.
39. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Veteran poverty trends. https://www.va.gov/vetdata/docs/specialreports/veteran_poverty_trends.pdf. Published May 2015. Accessed December 9, 2019.
40. Robbins KG, Ravi A. Veterans living paycheck to paycheck are under threat during budget debates. https://www.americanprogress.org/issues/poverty/news/2017/09/19/439023/veterans-living-paycheck-paycheck-threat-budget-debates. Published September 19, 2017. Accessed December 9, 2019.
41. Wilmoth JM, London AS, Heflin CM. Economic well-being among older-adult households: variation by veteran and disability status. J Gerontol Soc Work. 2015;58(4):399-419.
42. Brostow DP, Gunzburger E, Thomas KS. Food insecurity among veterans: findings from the health and retirement study. J Nutr Health Aging. 2017;21(10):1358-1364.
43. Pooler J, Mian P, Srinivasan M, Miller Z. Veterans and food insecurity. https://www.impaqint.com/sites/default/files/issue-briefs/VeteransFoodInsecurity_IssueBrief_V1.3.pdf. Published November 2018. Accessed December 9, 2019.
44. Schure MB, Katon JG, Wong E, Liu C-F. Food and housing insecurity and health status among U.S. adults with and without prior military service. SSM Popul Health. 2016;29(2):244-248.
45. Miller DP, Larson MJ, Byrne T, DeVoe E. Food insecurity in veteran households: findings from nationally representative data. Public Health Nutr. 2016;19(10):1731-1740.
46. Widome R, Jensen A, Bangerter A, Fu SS. Food insecurity among veterans of the US wars in Iraq and Afghanistan. Public Health Nutr. 2015;18(5):844-849.
47. London AS, Heflin CM. Supplemental Nutrition Assistance Program (SNAP) use among active-duty military personnel, veterans, and reservists. Popul Res Policy Rev. 2015;34(6):805-826.
48. Weinfield NS, Mills G, Borger C, et al. Hunger in America 2014. Natl rep prepared for Feeding America. https://www.feedingamerica.org/research/hunger-in-america. Published 2014. Accessed December 9, 2019.
49. Mabli J, Ohls J, Dragoset L, Castner L, Santos B. Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security. Washington, DC: US Department of Agriculture, Food and Nutrition Service; 2013.
50. Srinivasan M, Pooler JA. Cost-related medication nonadherence for older adults participating in SNAP, 2013–2015. Am J Public Health. 2017;108(2):224-230.
51. Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Progam benefits and emergency room visits for hypoglycaemia. Public Health Nutr. 2017;20(7):1314-1321.
52. Samuel LJ, Szanton SL, Cahill R, et al. Does the Supplemental Nutrition Assistance Program affect hospital utilization among older adults? The case of Maryland. Popul Health Manag. 2018;21(2):88-95.
53. Szanton SL, Samuel LJ, Cahill R, et al. Food assistance is associated with decreased nursing home admissions for Maryland’s dually eligible older adults. BMC Geriatr. 2017;17(1):162.
54. Carlson S, Keith-Jennings B. SNAP is linked with improved nutritional outcomes and lower health care costs. https://www.cbpp.org/research/food-assistance/snap-is-linked-with-improved-nutritional-outcomes-and-lower-health-care. Published January 17, 2018. Accessed December 10, 2019.
55. Keith-Jennings B, Cai L. SNAP helps almost 1.4 million low-income veterans, including thousands in every state. https://www.cbpp.org/research/food-assistance/snap-helps-almost-14-million-low-income-veterans-including-thousands-in. Updated November 8, 2018. Accessed December 10, 2019.
56. US Department of Health and Human Services. Older Americans Act nutrition programs. https://acl.gov/sites/default/files/news%202017-03/OAA-Nutrition_Programs_Fact_Sheet.pdf. Accessed December 10, 2019.
57. US Department of Veterans Affairs. About VHA. https://www.va.gov/health/aboutvha.asp. Accessed December 10, 2019.
58. US Department of Veterans Affairs. VA Corporate Data Warehouse.
59. Yano EM, Bair MJ, Carrasquillo O, Krein SL, Rubenstein LV. Patient aligned care teams (PACT): VA’s journey to implement patient-centered medical homes. J Gen Intern Med. 2014;29(suppl 2):S547-s549.
60. O’Toole TP, Pape L. Innovative efforts to address homelessness among veterans. N C Med J. 2015;76(5):311-314.
61. O’Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: the Veterans Health Administration’s “Homeless Patient Aligned Care Team” Program. Prev Chronic Dis. 2016;13:150567.
62. Marpadga S, Fernandez A, Leung J, Tang A, Seligman H, Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23.
63. Stenmark SH, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman H. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente Colorado. Perm J. 2018;22.
64. Martel ML, Klein LR, Hager KA, Cutts DB. Emergency department experience with novel electronic medical record order for referral to food resources. West J Emerg Med. 2018;19(2):232-237.
65. Going C, Cohen AJ, Bares M, Christensen M. Interdisciplinary approaches to addressing the food insecure veteran. Veterans Health Administration Employee Education System webinar; October 30, 2018.
66. Feeding America Announces New Partnership With U.S. Department Of Veterans Affairs. https://www.prnewswire.com/news-releases/feeding-america-announces-new-partnership-with-us-department-of-veterans-affairs-300481891.html. Published June 29, 2017. Accessed December 10, 2019.
67. US Department of Veterans Affairs. State Veterans Affairs offices. https://www.va.gov/statedva.htm. Updated March 20, 2019. Accessed December 10, 2019.
68. US Department of Veterans Affairs. Directory of veterans service organizations. https://www.va.gov/vso. Updated December 24, 2013. Accessed December 10, 2019.
69. ACL Administration for Community Living. Aging and disability resource centers. https://acl.gov/programs/aging-and-disability-networks/aging-and-disability-resource-centers. Updated December 13, 2017. Accessed December 10, 2019.
70. Nutrition and Obesity Policy Research and Evaluation Network (NOPREN). Clinical screening algorithms. https://nopren.org/resource/download-food-insecurity-screening-and-referral-algorithms-for-adults-patients-living-with-diabetes-and-pediatric-patients. Accessed December 10, 2019.