User login
Data-based Recommendations for CKD Screening
Q)
I’ve received mixed messages about whom to screen for chronic kidney disease (CKD). The US Preventive Services Task Force (USPSTF) recommends screening only patients at high risk, but kidney experts advise screening everyone. Who is right? What does the data show?
In 2012, the USPSTF stated that there was insufficient evidence to assess the benefit, or harm, of regularly screening asymptomatic adults for CKD.1 Other expert medical panels have come to this conclusion as well, and therefore only recommend screening highrisk patients.2
The National Kidney Foundation (NKF) encourages clinicians to assess all patients for risk factors of CKD. Diabetes and hypertension are strongly established risk factors for kidney disease; others include family history of kidney disease; cardiovascular disease; obesity; and older age.
If a patient is at risk for CKD, the NKF recommends testing serum creatinine levels to estimate glomerular filtration rate and testing urine for protein (microalbuminuria or macroalbuminuria). These tests are readily accessible in a primary care setting. It should be noted that one-time testing of serum creatinine and/or urine has not been studied for sensitivity or specificity in the diagnosis of CKD. Diagnosis should be based on decreased renal function or kidney damage occurring over a three-month span.3
In May 2016, Canadian researchers published results from the See Kidney Disease Targeted Screening Program for CKD, comparing CKD screening in the general population with a targeted, at-risk individual population.4 The study, which included more than 6,000 participants, revealed a higher rate of unrecognized CKD in the at-risk population than in the general population (21.9% and 14.7%, respectively).
These findings support the idea that screening at-risk patients identifies more cases of CKD than screening the general patient population does.4 Early diagnosis of CKD, through recognition of risk factors, provides an opportunity to decrease complications and manage conditions that contribute to the progression of renal disease.2,3 —RVR
Rebecca V. Rokosky, MSN, APRN, FNP
Renal Associates Clinical Advancement Center in San Antonio, Texas
1. Moyer VA. Screening for chronic kidney disease: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(8):567-570.
2. Vassalotti JA, Centor R, Turner BJ, et al. Practical approach to detection and management of chronic kidney disease for the primary care clinician. Am J Med. 2016;129(2):153-162.
3. Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837-846.
Q)
I’ve received mixed messages about whom to screen for chronic kidney disease (CKD). The US Preventive Services Task Force (USPSTF) recommends screening only patients at high risk, but kidney experts advise screening everyone. Who is right? What does the data show?
In 2012, the USPSTF stated that there was insufficient evidence to assess the benefit, or harm, of regularly screening asymptomatic adults for CKD.1 Other expert medical panels have come to this conclusion as well, and therefore only recommend screening highrisk patients.2
The National Kidney Foundation (NKF) encourages clinicians to assess all patients for risk factors of CKD. Diabetes and hypertension are strongly established risk factors for kidney disease; others include family history of kidney disease; cardiovascular disease; obesity; and older age.
If a patient is at risk for CKD, the NKF recommends testing serum creatinine levels to estimate glomerular filtration rate and testing urine for protein (microalbuminuria or macroalbuminuria). These tests are readily accessible in a primary care setting. It should be noted that one-time testing of serum creatinine and/or urine has not been studied for sensitivity or specificity in the diagnosis of CKD. Diagnosis should be based on decreased renal function or kidney damage occurring over a three-month span.3
In May 2016, Canadian researchers published results from the See Kidney Disease Targeted Screening Program for CKD, comparing CKD screening in the general population with a targeted, at-risk individual population.4 The study, which included more than 6,000 participants, revealed a higher rate of unrecognized CKD in the at-risk population than in the general population (21.9% and 14.7%, respectively).
These findings support the idea that screening at-risk patients identifies more cases of CKD than screening the general patient population does.4 Early diagnosis of CKD, through recognition of risk factors, provides an opportunity to decrease complications and manage conditions that contribute to the progression of renal disease.2,3 —RVR
Rebecca V. Rokosky, MSN, APRN, FNP
Renal Associates Clinical Advancement Center in San Antonio, Texas
Q)
I’ve received mixed messages about whom to screen for chronic kidney disease (CKD). The US Preventive Services Task Force (USPSTF) recommends screening only patients at high risk, but kidney experts advise screening everyone. Who is right? What does the data show?
In 2012, the USPSTF stated that there was insufficient evidence to assess the benefit, or harm, of regularly screening asymptomatic adults for CKD.1 Other expert medical panels have come to this conclusion as well, and therefore only recommend screening highrisk patients.2
The National Kidney Foundation (NKF) encourages clinicians to assess all patients for risk factors of CKD. Diabetes and hypertension are strongly established risk factors for kidney disease; others include family history of kidney disease; cardiovascular disease; obesity; and older age.
If a patient is at risk for CKD, the NKF recommends testing serum creatinine levels to estimate glomerular filtration rate and testing urine for protein (microalbuminuria or macroalbuminuria). These tests are readily accessible in a primary care setting. It should be noted that one-time testing of serum creatinine and/or urine has not been studied for sensitivity or specificity in the diagnosis of CKD. Diagnosis should be based on decreased renal function or kidney damage occurring over a three-month span.3
In May 2016, Canadian researchers published results from the See Kidney Disease Targeted Screening Program for CKD, comparing CKD screening in the general population with a targeted, at-risk individual population.4 The study, which included more than 6,000 participants, revealed a higher rate of unrecognized CKD in the at-risk population than in the general population (21.9% and 14.7%, respectively).
These findings support the idea that screening at-risk patients identifies more cases of CKD than screening the general patient population does.4 Early diagnosis of CKD, through recognition of risk factors, provides an opportunity to decrease complications and manage conditions that contribute to the progression of renal disease.2,3 —RVR
Rebecca V. Rokosky, MSN, APRN, FNP
Renal Associates Clinical Advancement Center in San Antonio, Texas
1. Moyer VA. Screening for chronic kidney disease: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(8):567-570.
2. Vassalotti JA, Centor R, Turner BJ, et al. Practical approach to detection and management of chronic kidney disease for the primary care clinician. Am J Med. 2016;129(2):153-162.
3. Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837-846.
1. Moyer VA. Screening for chronic kidney disease: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(8):567-570.
2. Vassalotti JA, Centor R, Turner BJ, et al. Practical approach to detection and management of chronic kidney disease for the primary care clinician. Am J Med. 2016;129(2):153-162.
3. Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837-846.
To Cut or Not to Cut? Evaluating Surgical Criteria for Benign & Nondiagnostic Thyroid Nodules
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
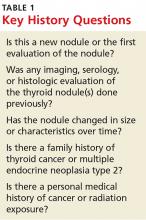
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.
The Most Expensive Drug in the World: To Continue or Discontinue, That Is the Question
A 59-year-old man with a 20-year history (1994) of HIV well controlled on highly active antiretroviral therapy (HAART) therapy (baseline viral load undetectable, CD4+ cell count 781), presented to a community hospital (May 7, 2014) with abdominal pain. The patient’s girlfriend reported unusual behavior for 1 week before admission, including decreased appetite, binge drinking, and nonadherence to HAART therapy.
There was no history of fever, illegal medication use, or diarrhea. In addition to HIV, his past history was remarkable for hepatitis B, hypertension, and left lower extremity amputation secondary to a motor vehicle accident. He had a remote history of cocaine, PCP (phencyclidine), LSD (lysergic acid diethylamide), marijuana, and alcohol misuse and a 50 pack-year smoking history. His family history was remarkable for a mother who died of pancreatic cancer.
During his hospitalization, he developed pronounced expressive aphasia and lethargy but was able to follow simple commands. A computed tomography (CT) scan of the head revealed a left lacunar infarction, and he was transferred to the VA Long Beach Healthcare System in California for further care of a possible stroke.
Shortly after arrival, he developed a fever of 100.9º F. His pulse was 100 bpm and regular, blood pressure was 164/92 mm Hg, and respiratory rate was 14 breaths per minute. A physical examination was remarkable for somnolence, disorientation, and aphasia. He was grimacing to light palpation in all 4 quadrants of the abdomen and had diffuse purpura on skin examination. Laboratory results showed worsening thrombocytopenia, acute kidney injury with proteinuria and hemoglobinuria, and hemolysis (schistocytes, low haptoglobin level, and elevated lactate dehydrogenase [LDH]).
The patient’s changes in baseline laboratory results were platelet count 206,000 mm3 to 64,000 mm3, serum creatinine level 0.98 mg/dL to 1.55 mg/dL. His hemogram showed normochromic normocytic anemia (hemoglobin [Hb] level 10.2 g/dL) with schistocytes. Serum samples were initially unreportable by the laboratory due to severe hemolysis, but his haptoglobin level was found to be low and, conversely, LDH remarkably high. Fifteen days after admission, his CD4+ cell count was 141. An abdominal CT scan showed right lower quadrant abdominal free fluid and thickening of the terminal ileum with surrounding stranding, suggestive of terminal ileitis, and he was started on piperacillin-tazobactam. A lumbar puncture was unremarkable, and HAART medications were resumed. The patient required intubation and a ventilator for acute respiratory failure.
Empiric treatment for presumed thrombotic thrombocytopenic purpura (TTP) with plasmapheresis and methylprednisolone was ineffective, and the patient required mechanical ventilation and hemodialysis.
In refractory cases of TTP-hemolytic uremic syndrome, rituximab, a monoclonal antibody directed at CD20 present on B lymphocytes, is added empirically as effective salvage therapy and was therefore tried in this case.1
However, the addition of rituximab failed to improve the patient’s condition, and he developed further seizure activity and evidence of new lacunar infarctions as seen on magnetic resonance imaging of the brain. His hospital course was complicated by recurrent hemoptysis and respiratory failure, requiring assisted ventilation and eventually tracheostomy.
A normal ADAMTS13 level (72%) and negative Shiga toxin test changed the diagnosis to atypical hemolytic uremic syndrome (aHUS). Mean complement C3 (74 mg/dL) and C4 (9 mg/dL) levels were low. Plasmapheresis was discontinued, and treatment with eculizumab (Soliris, Alexion Pharmaceuticals) was initiated. Meningococcal vaccine was administered post-eculizumab, aimed at reducing but not eliminating the risk of meningococcemia.2 Two weeks later, the patient’s platelet count normalized, renal function improved, hemolysis resolved, and the patient regained full mental status. Eight weeks after initiating eculizumab, he no longer required dialysis.
Discussion
Generalized thrombosis of smaller blood vessels (thrombotic microangiopathy [TMA]) occurs in 3 uncommon syndromes—TTP, HUS, and aHUS—all with similar clinical presentations but distinct pathologic etiologies and treatment. These syndromes share a clinical picture of thrombocytopenia, hemolytic anemia, and renal failure. Hemolysis in these conditions is manifested by schistocytes, elevated lactate dehydrogenase from damaged cells, decreased haptoglobin, anemia, and hemoglobinuria.
Thrombotic Thrombocytopenic Purpura
Thrombocytopenic purpura occurs in about 3 cases per 1,000,000 adults per year.3 It occurs when the metalloproteinase enzyme ADAMTS13 activity is impaired, interrupting its function to cleave large sticky von Willebrand factor (vWF) multimers, resulting in coagulation in microvasculature by increased platelet aggregation, hemolysis from shearing of red blood cells, and compromised circulation to the highly vascularized kidney and other vital organs.4 The hallmark of TTP is a severely decreased ADAMTS13 activity (< 5% of normal) secondary to coexisting conditions, such as cancer, pregnancy, HIV infection, adverse effects (AEs), or antibodies to ADAMTS13.5
The TTP pentad of thrombocytopenia, hemolytic anemia, neurologic symptoms, renal failure, and fever were present in our patient. The patient had a known HIV infection but no exposure to medications associated with TTP (such as acyclovir, quinine, oxymorphone, platelet aggregation inhibitors, or immunosuppressants). Prior to obtaining ADAMTS13 level, the patient was treated empirically for TTP with early and daily plasma exchange to remove the inhibitor of ADAMTS13 and replace it with fresh frozen plasma. Rituximab also was used to inhibit production of antibodies to ADAMTS13 from CD20 B lymphocytes. These empiric clinical measures were not effective in stopping his decline in renal and neurologic functions.
Hemolytic Uremic Syndrome
Like TTP, HUS is also a consequence of thrombotic microangiopathy. However, in contrast to TTP, which is more commonly seen in adults,3 HUS is usually seen in young children secondary to Shiga toxin-producing Escherichia coli (STEC).6 Hemolytic uremic syndrome, also referred to as STEC-HUS or typical HUS, is a rare disease affecting 10 to 20 people per million annually. About 10% of these patients are classified as having aHUS because STEC is not implicated in their disease. It is of interest that, unlike aHUS, STEC-HUS is usually a self-limited disease of children, the majority of whom recover without relapse, and evidence that eculizumab improves prognosis in STEC-HUS is not compelling.5
Atypical Hemolytic Uremic Syndrome
Atypical HUS is a complement-mediated disease. The usual function of complement proteins is to destroy foreign cells and activate immune cells. However, in aHUS this protective defense system goes awry resulting in a pathologic thrombotic milieu. Specifically, aHUS is a continuous complement mediated attack on vascular endothelial beds due to the failure of protein regulators to terminate the complement cascade. Unlike typical HUS, which is usually associated with a Shiga-toxin producing gastrointestinal infection, the trigger in aHUS is unknown and thought to be associated with a genetic predisposition.
Atypical HUS distinguishes itself from TTP and HUS in that it does not respond to plasma exchange, corticosteroids, rituximab, or other immunosupressants. This is due to the distinct underlying pathophysiology of aHUS in which the problem is the unbridled activation of the alternate arm of the complement system.
The complement system is part of the innate immune system, which acts with or without the adaptive immune system it “complements” by amplifying a cascade of responses to eliminate the trigger pathogen. There are 3 complement pathways—classical, lectin, and alternate. The alternate complement pathway, whose activation generates C5a complement (anaphylotoxin), was most pertinent to this case. This precipitates a number of downstream protein cleaving events that lead to the cell lysing membrane attack complex (MAC), which creates a pore in the cell membrane of pathogens seen as foreign. In aHUS, the patient’s own cells come under attack by their own complement, which is no longer inhibited due to mutations in regulatory proteins of the alternate pathway.
With the foot off the complement brake (the hallmark feature underlying aHUS), endothelial cells, leukocytes, and platelets become hyperactive and thrombogenic, thereby resulting in microangiopathy and ischemia of involved organs.7 These mutations may be sporadic or familial and occur in a genetically susceptible host.8 It should be emphasized that genetic testing in complement mediated HUS is a specialized and slow process (weeks); the initial clinical diagnosis is one of exclusion and does not rest on genetic testing. Furthermore, serum complement levels may be normal in cases of complement mediated aHUS.9-11
This patient had a life-threatening condition that required distinguishing it from 2 rare diseases with very similar presentations; failure to do so in a timely fashion could easily have resulted in his demise. TTP or HUS was the important question, and ADAMTS13 level was one of the determining diagnostic tests. The usual interventions for TTP and HUS (plasmapheresis/plasma exchange and, in some cases, rituximab) were ineffective in this patient with aHUS. The patient achieved full recovery of neurologic, renal, and hematologic impairments after treatment with eculizumab, the recombinant humanized monoclonal antibody that binds to the complement protein C5 brake and inhibits its enzymatic cleavage, thereby interfering with the production of the MAC and cell lysis.
Although the patient did not have an identifiable mutation in the panel of complement regulatory genes tested, the rather dramatic efficacy of the orphan drug eculizumab was in a sense confirmation of his complement related hemolytic uremia. Left undecided are the questions of how long to continue eculizumab, the potential risk of relapse with discontinuation, and the ethical dilemma of proper length of treatment with the most expensive medication in the world given its total cost and no clear discontinuation criteria.12-15 The cost of medications for rare and ultra-rare orphan drugs have approached unsustainable levels, posing ethical challenges to many developed countries.16
Eculizumab and Orphan Drugs
Several months before his assassination, President Kennedy awarded Frances Kathleen Oldham Kelsey, MD, PhD, the President’s Award for Distinguished Federal Civilian Service (August 7, 1962) for her insistence that more safety evidence for thalidomide be presented before she would approve its use in the U.S. As a result of the thalidomide tragedy, the Kefauver Harris amendment was passed unanimously by Congress and signed into law by President Kennedy on October 10, 1962. It required stringent evidence of safety and efficacy for FDA approval of a new medication, reporting of AEs to the FDA, truth in drug advertising, rules governing generic drugs, and informed consent from patients participating in clinical trials.
An unintended consequence was that the development of medications for uncommon diseases became fiscally unattractive to the pharmaceutical industry, ie, “orphaned.” The Orphan Drug Act was enacted by Congress in 1983 to encourage development of drugs to treat less common diseases (diseases/disorders affecting fewer than 200,000 people in the U.S.) through incentives such as exclusive use approval for 7 years, reduced taxes, grants, and favorable laws. Ironically, thalidomide was designated an orphan drug on October 14, 1998 for treatment of multiple myeloma. Since its enactment in 1983, more than 400 orphan drugs and biologic products have been marketed. There may be as many as 7,000 orphan diseases to target for drug therapy, and the 17 of the 20 most expensive drugs in the world in 2013 were for rare orphan diseases.16
Paroxysmal nocturnal hemoglobinuria (PNH) is one of those rare diseases. Mutations of hematopoietic stem cells produce red blood cell membranes deficient in the glycoprotein to which signaling proteins attach (glycosyl phosphatidylinositol) and serve to inhibit complement-induced lysis. This results in intravascular hemolysis (increased LDH and decreased haptoglobin) and increased thrombosis. The FDA approved the orphan drug eculizumab for the treatment of the orphan disease PNH on March 16, 2007.
Eculizumab is a humanized mouse monoclonal antibody that gained FDA orphan drug approval (and exclusivity rights until 2019) for the treatment of aHUS on September 23, 2011, based on 2 industry-sponsored small trials of 17 and 20 patients, and it remains the primary and only known effective treatment for this disease.17-19
Eculizumab has raised many interesting questions. Its mechanism of action wets the appetite of pharmacologists and unveils more basic science questions regarding other related mechanisms of disease, recognition of foreign vs self, genetic influences, virulence of organisms, and more. National and international dilemmas have arisen because of the extreme cost of eculizumab, its position as the only effective treatment for this rare and often fatal disease, and the manufacturer’s recommendation and promotion that it be continued indefinitely. How should the price of a drug, developed in large part by government-supported research and tax incentives, and without competition, be determined and justified?
Pharmaceutical Inflation
A marketplace for pharmaceuticals is simply not analogous to other industries. Advances in pharmacotherapy, some miraculous, have come at a substantial cost. The high cost of drugs became newsworthy with the AIDS pandemic and the approval of the lifesaving azidothymidine (AZT) in 1989 (Burroughs Wellcome–also the developer of pyrimethamine [Daraprim]) and its then record price. Cancer treatment that used to cost $10,000 per year now costs $10,000 per month while the oncology community extolls a 2- or 3-month progression free survival benefit. Patients must now deal with the shock of a cancer diagnosis followed by the shock of an exorbitant copayment.
Recent media attention focused derision on Martin Shkreli, chief executive officer of Turing Pharmaceuticals, for purchasing pyrimethamine and then raising the price of the 62-year-old treatment for protozoan infection toxoplasmosis from $13.50 to $750 per pill. The debacle may also serve to highlight the complexities and ethical issues involved when profit intersects with health care. Some drug costs have dramatically increased in the U.S. because of greed, a belief that a marketplace can control costs, and the lack of regulation. The usual suspects, such as cost of research, length of development, stimulus to innovation, and return on investment, are difficult to apply to old medications whose marketing rights were acquired by purchase of another company. Can marketplace economics be applied in health situations where there is no competition, legal protections afforded manufacturers, consumers unable to make an informed decision?
While pharmacy and therapeutics committees were debating treatment of hepatitis C with either of 2 drugs approved in 2011, boceprevir (Victrelis, Merck) or telapravir (Incivek, Vertex and Johnson & Johnson), Gilead Pharmaceuticals acquired Pharmasset Inc. and its hepatitis C drug sofosbuvir (Sovaldi) for a whopping $11.2 billion in 2012. It received FDA approval April 8, 2013, under Breakthrough Therapy Designation.
While economists argued over the wisdom of such a high-cost acquisition, Gilead generated $9 billion in sales during the first 3 quarters of 2014, surpassing adalimumab (Humira), which had been the highest earning drug in 2014. Hepatitis C could now be quickly treated with truly unprecedented efficacy and without the AEs of interferon. The oft-quoted cost $1,000 per pill or about $84,000 per treatment in the U.S. drew international attention. Prior options for hepatitis C treatment, which preceded sofosbuvir by a mere couple of years, fell into pharmaceutical extinction. Telapravir succumbed to competition and ceased to be manufactured on August 12, 2014. Shortly after approval of sofosbuvir, Gilead also gained approval of its combination product for hepatitis C ledipasvir 90 mg/sofosbuvir 400 mg (Harvoni) on October 10, 2014.
The Most Expensive Drug in the World
Although there are no shortages of contenders for the coveted most expensive title, eculizumab is the current champion. Drugs that offer a cure, such as antibiotics, usually involve a relatively short, onetime course. Lack of return on the cost of development of curative agents may have reduced industrial incentives to develop antibiotics. On the other hand, the extent of infectious diseases, such as malaria, Ebola, tuberculosis, HIV, hepatitis, and the proliferation of drug-resistant organisms, continues to fuel industrial interest for this lifesaving class of medications.
Cancer medications touting a brief interruption of the race to death have raised questions of affordability, equitable access, and quality vs quantity of life. The $11,000 per month endothelial growth factor inhibitor aflibercept (Zaltrap, Regeneron, and Sanofi) was approved by the FDA in November 2012 for colorectal cancer and was followed by a historic rejection by Memorial Sloan-Kettering Cancer Center, since its cost was nearly double that of a similar medication bevacizumab (Avastin) with similar meager benefit of a median progression free survival of 1.4 months.20 Moreover Medicare is mandated to cover the price the manufacturers charge plus a 6% cushion for any cancer drug that the FDA approves.21 Patients with private insurance, often elderly and on a fixed income, are burdened with a copayment requirement of 20% of the cost of the drug. The nonnegotiation clause of Medicare has not reduced cost of medications, particularly for cancer, which many of the elderly will likely face.
The VA, a single-payer system distinguished by bipartisan congressional support, can directly negotiate with pharmaceutical companies, resulting in lower drug prices than discounts guaranteed by federal law; but what if there is no competitor? Biosimilar drugs are currently being debated by those seeking to prolong their patent protection. Stem cell therapies that offer a cure for some rare diseases or hope for common diseases are certain to command astronomical prices. Gene therapy offers hope for cure of both rare and common afflictions but at astounding prices.
The medication alipogene tiparvovec (Glybera, UniQure) delivered by adenovirus, for example, has been approved for use in the rare disorder lipoprotein lipase deficiency and is anticipated to cost $1.6 million for a onetime curative treatment. The pharmaceutical industry has joined the gene therapy race. While this is indeed a record acquisition sum for alipogene tiparvovec, at least it offers a cure. Eculizumab, although unique and effective, offers indefinite administration at a cost exceeding $600,000 per year, every year, for life. In 2014, sales of eculizumab climbed 44% to $2.234 billion.
To Continue or Discontinue Treatment
The duration of treatment with eculizumab poses a challenging dilemma for patients, clinicians, and health care providers. Eculizumab is the only effective treatment for a life-threatening condition, and the manufacturer, Alexion, recommends lifelong therapy of its product that has no competitors. Our patient was treated with 47 fixed-dose infusions of eculizumab at 2-week intervals from May 31, 2014, to February 18, 2016, at a cost of $737,957.80. The commercial cost outside the VA would be about 1.8 times this amount ($1.3 million). This extraordinary cost is the basic ethical issue. Without competition there is little to negotiate.
Need the treatment be lifelong? The AEs of eculizumab are not trivial, and some clinicians felt evidence for indefinite use in this patient was not compelling. Our patient’s initial critical and unstable condition had completely resolved after 2 months of eculizumab. The initial unknown precipitating event triggering the patient’s aHUS probably had resolved. His genetic testing did not disclose any HUS-related mutation. The patient’s serum was sent to Cincinnati Children’s Hospital (CCH) Clinical Laboratory Service to determine his eculizumab level and complement inhibition. His complement inhibition, as measured by CH50 activity, was adequately suppressed at 6% on eculizumab (target of < 10%) in spite of a free serum eculizumab level (81 mg/mL) that was somewhat below the therapeutic range of > 100 mg/mL.
Arguments for lifelong eculizumab therapy are based in part on the theoretical development of anti-eculizumab antibodies that could render reinstitution of eculizumab ineffective.22 Monitoring patients for relapse of their aHUS involves following markers of disease activity (levels of creatinine, LDH, haptoglobin, platelet counts, and Hb in urine). A report of 10 adult patients with aHUS who were treated effectively with eculizumab supports a trial of discontinuation.23 Seven of the 10 patients did not relapse following discontinuation of eculizumab. Three of 10 patients experienced a relapse when monitored for a cumulative 95 months, but all 3 had immediate and complete recovery after resuming therapy. All 3 patients who experienced relapse carried a complement factor H mutation. Their relapses occurred within 6 weeks from the last dose and were detected simply by performing home urine dipstick monitoring for haptoglobin 3 times per week. The 3 patients who relapsed promptly responded to eculizumab reinstitution with return of their labs to baseline.
Monitoring of complement function in patients with aHUS can guide clinically appropriate dosing intervals without changing disease activity markers.24 The half-life of eculizumab is about 11 days, and dosing intervals may be safely extended beyond 2 weeks in select patients.25 The target minimum inhibitory serum eculizumab level necessary to inhibit complement-mediated hemolysis is 50 µg/mL and 35 mg/mL for aHUS and PNH, respectively. In a small pharmacokinetic pilot study, Gatault and colleagues noted that trough levels during eculizumab maintenance by enzyme-linked immunoabsorbent assay (ELISA) of 44 mg/mL to 59 mg/mL inhibited the complement cascade.26 We suggested that weight-based dosing aiming at a trough > 50 mg/mL (rather than fixed dosing at a fixed interval) would be a better maintenance strategy.
In select patients, a trial of gradual discontinuation by lengthening the dosing interval of eculizumab seems a reasonable and safe alternative to indefinite continuation of the drug. After a patient’s successful recovery, the initial and unknown trigger of aHUS may no longer play a role. Improvement in the patient’s medical condition may permit the restoration of the patient’s defenses to once again function normally. Eculizumab seemed to retain its efficacy in the small number of patients who relapsed. Those who relapsed had positive genetic markers.
Further arguments favoring trial discontinuation in patients without known genetic predisposition are that continuation is not without risk, particularly of meningococcal infection, necessity for infusion every 2 weeks for life, little is known regarding long-term risk of the drug, and a lot is known of its extreme cost. Suppression of C5 inhibitory effect can lead to increased susceptibility to infections, whereas increased C5 activity may lead to a continued autoimmune attack on native cells.
As proposed by others, we suggest that this decision be made on a case by case basis, tailoring treatment based on an individual’s genetics and medical history.27 Although the European Medicines Agency has approved lifelong therapy for aHUS, this may be appropriate only for patients who have aHUS complement mutations associated with poor outcomes.27 This approach may not be warranted, however, in a patient, such as the one presented with no genetic mutations, or in those with mutations of uncertain clinical consequence. In such cases, given that 90% of adults who have a relapse experience within the first year after an aHUS episode, a reasonable alternative may be a trial discontinuation.27,28 After 1 year of eculizumab therapy, a trial of discontinuation with urine dipstick monitoring for Hb (Hemastix) 3 times a week for relapse may avoid the unnecessary expense and risk for infection posed by lifelong therapy, and eculizumab may be effectively restarted in case of relapse.
We propose that in these cases it would be reasonable to perform a trial of discontinuation after 1 year of therapy with urine dipstick monitoring for relapse, as lifelong therapy may pose unnecessary expense and risk for infection. In fact, given the financial burden of prolonged therapy on society, we believe it is unethical to continue treatment in a patient with unknown risk for relapse without a trial of discontinuation, as evidence has shown good response to re-initiation of therapy in the event of relapse.28 Agencies that have negotiated or attempted to regulate the cost of eculizumab have been met with public media campaigns featuring afflicted children at risk of death without eculizumab. The public relations company behind these efforts received support from Alexion.29-31
Conclusion
Given the formidable cost and the international monopoly status of eculizumab for a life-threatening condition, prospective discontinuation trials supported by the manufacturer would seem warranted in select cases. Delineating which patients will have a chronic relapsing course and those who will not should be one of these clinical trials. For now, one can only wonder: What’s worse than having a rare disease like aHUS? Perhaps the cost of treatment for a potentially indefinite period of time—now that’s a “bitter pill.”32
1. Caramazza D, Quintini G, Abbene I, et al. Relapsing or refractory idiopathic thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: the role of rituximab. Transfusion. 2010;50(12):2753-2760.
2. Köse O, Zimmerhackl LB, Jungraithmayr T, Mache C, Nürnberger J. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin Thromb Hemost. 2010;36(6):669-672.
3. Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, George JN. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer. 2013;60(10):1676-1682.
4. Sadler JE. Von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood. 2008;112(1):11-18.
5. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19.
6. Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035-1050.
7. Liszewski MK, Atkinson JP. Exploring the complement system in human disease. The Rheumatologist website. http://www.the-rheumatologist.org/article/exploring-the-complement-system-in-human-disease. Published February 1, 2010. Accessed May 9, 2016.
8. Mayer CL, Leibowitz CS, Kurosawa S, Stearns-Kurosawa DJ. Shiga toxins and the pathophysiology of hemolytic uremic syndrome in humans and animals. Toxins (Basel). 2012;4(11):1261-1287.
9. Noris M, Mescia F, Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nat Rev Nephrol. 2012;8(11):622-633.
10. Geerdink LM, Westra D, van Wijk JA, et al. Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol. 2012;27(8):1283-1291.
11. Sellier-Leclerc AL, Frémeaux-Bacchi V, Dragon-Durey MA, et al; French Society of Pediatric Nephrology. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007;18(8):2392-2400.
12. Herper M. The worlds most expensive drugs. Forbes. February 22, 2010.
13. Nordrum A. Drug prices: world's most expensive medicine costs $440,000 a year, but is it worth the expense? International Business Times website. http://www.ibtimes.com/drug-prices-worlds-most-expensive-medicine-costs-440000-year-it-worth-expense-2302609. Updated February 13, 2016. Published June 24, 2015. Accessed June 15, 2016.
14. CBC News. The real cost of the world's most expensive drug [video]. CBC/Radio Canada website. http://www.cbc.ca/player/play/2670383596. Accessed June 15, 2016.
15. EvaluatePharma. Orphan Drug Report 2014. EvaluatePharma website. http://www.evaluategroup.com/orphandrug2014. Published 2014. Accessed June 15, 2016.
16. Isaacs D. Ethical dilemmas about orphan drugs for orphan diseases. J Paediatr Child Health. 2014;50(4):249-250.
17. Licht C, Muus P, Legendre CM, et al. Eculizumab (ECU) safety and efficacy in atypical hemolytic uremic syndrome (aHUS) patients with long disease duration and chronic kidney disease (CKD): 2-year results. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
18. Greenbaum L, Legendre CM, Babu S, et al. Eculizumab (ECU) in atypical hemolytic uremic syndrome (aHUS) patients with progressing thrombotic microangiopathy (TMA): 2-year data. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
19. Legendre CM, Licht C, Muus P, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Eng J Med. 2013;368(23):2169-2181.
20. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters. New York Times. October 14, 2012:Opinion Pages.
21. Medicare Prescription Drug, Improvement, and Modernization Act of 2003, Public Law 108-173;117 Stat 2066. U.S. Government Printing Office website. https://www.gpo.gov/fdsys/pkg/PLAW-108publ173/pdf/PLAW-108publ173.pdf. Approved December 8, 2003. Accessed June 6, 2016.
22. Jodele S, Fukuda T, Vinks A, et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2014;20(4):518-525.
23. Ardissino G, Testa S, Possenti I, et al. Discontinuation of eculizumab maintenance treatment for atypical hemolytic uremic syndrome: a report of 10 cases. Am J Kidney Dis. 2014;64(4):633-637.
24. Cugno M, Gualtierotti R, Possenti I, et al. Complement functional tests for monitoring eculizumab treatment in patients with atypical hemolytic uremic syndrome. J Thromb Haemost. 2014;12(9):1440-1448.
25. Waters AM, Licht C. aHUS caused by complement dysregulation: new therapies on the horizon. Pediatr Nephrol. 2011;26(1):41-57.
26. Gatault P, Brachet G, Ternant D, et al. Therapeutic drug monitoring of eculizumab: rational for an individualized dosing schedule. MAbs. 2015;7(6):1205-1211.
27. Zuber J, Fakhouri F, Roumenina LT, Loirat C, Frémeaux-Bacchi V; French Study Group for aHUS/C3G. Use of eculizumab for atypical haemolytic uraemic syndrome and C3 glomerulopathies. Nat Rev Nephrol. 2012;8(11):643-657.
28. Fakhouri F, Frémeaux-Bacchi V, Loirat C. Atypical hemolytic uremic syndrome: from the rediscovery of complement to targeted therapy. Eur J Intern Med. 2013;24(6):492-495.
29. Crowe K. Analysis: how pharmaceutical company Alexion set the price of the world's most expensive drug. CBC/Radio Canada website. http://www.cbc.ca/news/health/how-pharmaceutical-company-alexion-set-the-price-of-the-world-s-most-expensive-drug-1.3125251 Updated June 25, 2015. Accessed June 21, 2016.
30. Drug campaign for sick child was a PR stunt. FlandersToday website. http://www.flanderstoday.eu/business/drug-campaign-sick-child-was-pr-stunt. Published May 8, 2013. Accessed June 21, 2016.
31. Herald on Sunday editorial: miracle cure, morally derelect. New Zealand Herald website. http://www.nzherald.co.nz/opinion/news/article.cfm?c_id=466&objectid=10861630. Published January 27, 2013. Accessed June 21, 2016.
32. Brill S. Bitter pill: why medical bills are killing us. http://healthland.time.com/2013/02/20/bitter-pill-why-medical-bills-are-killing-us/print/[2/26/2013. Time website. Published February 20, 2013. Accessed June 6, 2016.
A 59-year-old man with a 20-year history (1994) of HIV well controlled on highly active antiretroviral therapy (HAART) therapy (baseline viral load undetectable, CD4+ cell count 781), presented to a community hospital (May 7, 2014) with abdominal pain. The patient’s girlfriend reported unusual behavior for 1 week before admission, including decreased appetite, binge drinking, and nonadherence to HAART therapy.
There was no history of fever, illegal medication use, or diarrhea. In addition to HIV, his past history was remarkable for hepatitis B, hypertension, and left lower extremity amputation secondary to a motor vehicle accident. He had a remote history of cocaine, PCP (phencyclidine), LSD (lysergic acid diethylamide), marijuana, and alcohol misuse and a 50 pack-year smoking history. His family history was remarkable for a mother who died of pancreatic cancer.
During his hospitalization, he developed pronounced expressive aphasia and lethargy but was able to follow simple commands. A computed tomography (CT) scan of the head revealed a left lacunar infarction, and he was transferred to the VA Long Beach Healthcare System in California for further care of a possible stroke.
Shortly after arrival, he developed a fever of 100.9º F. His pulse was 100 bpm and regular, blood pressure was 164/92 mm Hg, and respiratory rate was 14 breaths per minute. A physical examination was remarkable for somnolence, disorientation, and aphasia. He was grimacing to light palpation in all 4 quadrants of the abdomen and had diffuse purpura on skin examination. Laboratory results showed worsening thrombocytopenia, acute kidney injury with proteinuria and hemoglobinuria, and hemolysis (schistocytes, low haptoglobin level, and elevated lactate dehydrogenase [LDH]).
The patient’s changes in baseline laboratory results were platelet count 206,000 mm3 to 64,000 mm3, serum creatinine level 0.98 mg/dL to 1.55 mg/dL. His hemogram showed normochromic normocytic anemia (hemoglobin [Hb] level 10.2 g/dL) with schistocytes. Serum samples were initially unreportable by the laboratory due to severe hemolysis, but his haptoglobin level was found to be low and, conversely, LDH remarkably high. Fifteen days after admission, his CD4+ cell count was 141. An abdominal CT scan showed right lower quadrant abdominal free fluid and thickening of the terminal ileum with surrounding stranding, suggestive of terminal ileitis, and he was started on piperacillin-tazobactam. A lumbar puncture was unremarkable, and HAART medications were resumed. The patient required intubation and a ventilator for acute respiratory failure.
Empiric treatment for presumed thrombotic thrombocytopenic purpura (TTP) with plasmapheresis and methylprednisolone was ineffective, and the patient required mechanical ventilation and hemodialysis.
In refractory cases of TTP-hemolytic uremic syndrome, rituximab, a monoclonal antibody directed at CD20 present on B lymphocytes, is added empirically as effective salvage therapy and was therefore tried in this case.1
However, the addition of rituximab failed to improve the patient’s condition, and he developed further seizure activity and evidence of new lacunar infarctions as seen on magnetic resonance imaging of the brain. His hospital course was complicated by recurrent hemoptysis and respiratory failure, requiring assisted ventilation and eventually tracheostomy.
A normal ADAMTS13 level (72%) and negative Shiga toxin test changed the diagnosis to atypical hemolytic uremic syndrome (aHUS). Mean complement C3 (74 mg/dL) and C4 (9 mg/dL) levels were low. Plasmapheresis was discontinued, and treatment with eculizumab (Soliris, Alexion Pharmaceuticals) was initiated. Meningococcal vaccine was administered post-eculizumab, aimed at reducing but not eliminating the risk of meningococcemia.2 Two weeks later, the patient’s platelet count normalized, renal function improved, hemolysis resolved, and the patient regained full mental status. Eight weeks after initiating eculizumab, he no longer required dialysis.
Discussion
Generalized thrombosis of smaller blood vessels (thrombotic microangiopathy [TMA]) occurs in 3 uncommon syndromes—TTP, HUS, and aHUS—all with similar clinical presentations but distinct pathologic etiologies and treatment. These syndromes share a clinical picture of thrombocytopenia, hemolytic anemia, and renal failure. Hemolysis in these conditions is manifested by schistocytes, elevated lactate dehydrogenase from damaged cells, decreased haptoglobin, anemia, and hemoglobinuria.
Thrombotic Thrombocytopenic Purpura
Thrombocytopenic purpura occurs in about 3 cases per 1,000,000 adults per year.3 It occurs when the metalloproteinase enzyme ADAMTS13 activity is impaired, interrupting its function to cleave large sticky von Willebrand factor (vWF) multimers, resulting in coagulation in microvasculature by increased platelet aggregation, hemolysis from shearing of red blood cells, and compromised circulation to the highly vascularized kidney and other vital organs.4 The hallmark of TTP is a severely decreased ADAMTS13 activity (< 5% of normal) secondary to coexisting conditions, such as cancer, pregnancy, HIV infection, adverse effects (AEs), or antibodies to ADAMTS13.5
The TTP pentad of thrombocytopenia, hemolytic anemia, neurologic symptoms, renal failure, and fever were present in our patient. The patient had a known HIV infection but no exposure to medications associated with TTP (such as acyclovir, quinine, oxymorphone, platelet aggregation inhibitors, or immunosuppressants). Prior to obtaining ADAMTS13 level, the patient was treated empirically for TTP with early and daily plasma exchange to remove the inhibitor of ADAMTS13 and replace it with fresh frozen plasma. Rituximab also was used to inhibit production of antibodies to ADAMTS13 from CD20 B lymphocytes. These empiric clinical measures were not effective in stopping his decline in renal and neurologic functions.
Hemolytic Uremic Syndrome
Like TTP, HUS is also a consequence of thrombotic microangiopathy. However, in contrast to TTP, which is more commonly seen in adults,3 HUS is usually seen in young children secondary to Shiga toxin-producing Escherichia coli (STEC).6 Hemolytic uremic syndrome, also referred to as STEC-HUS or typical HUS, is a rare disease affecting 10 to 20 people per million annually. About 10% of these patients are classified as having aHUS because STEC is not implicated in their disease. It is of interest that, unlike aHUS, STEC-HUS is usually a self-limited disease of children, the majority of whom recover without relapse, and evidence that eculizumab improves prognosis in STEC-HUS is not compelling.5
Atypical Hemolytic Uremic Syndrome
Atypical HUS is a complement-mediated disease. The usual function of complement proteins is to destroy foreign cells and activate immune cells. However, in aHUS this protective defense system goes awry resulting in a pathologic thrombotic milieu. Specifically, aHUS is a continuous complement mediated attack on vascular endothelial beds due to the failure of protein regulators to terminate the complement cascade. Unlike typical HUS, which is usually associated with a Shiga-toxin producing gastrointestinal infection, the trigger in aHUS is unknown and thought to be associated with a genetic predisposition.
Atypical HUS distinguishes itself from TTP and HUS in that it does not respond to plasma exchange, corticosteroids, rituximab, or other immunosupressants. This is due to the distinct underlying pathophysiology of aHUS in which the problem is the unbridled activation of the alternate arm of the complement system.
The complement system is part of the innate immune system, which acts with or without the adaptive immune system it “complements” by amplifying a cascade of responses to eliminate the trigger pathogen. There are 3 complement pathways—classical, lectin, and alternate. The alternate complement pathway, whose activation generates C5a complement (anaphylotoxin), was most pertinent to this case. This precipitates a number of downstream protein cleaving events that lead to the cell lysing membrane attack complex (MAC), which creates a pore in the cell membrane of pathogens seen as foreign. In aHUS, the patient’s own cells come under attack by their own complement, which is no longer inhibited due to mutations in regulatory proteins of the alternate pathway.
With the foot off the complement brake (the hallmark feature underlying aHUS), endothelial cells, leukocytes, and platelets become hyperactive and thrombogenic, thereby resulting in microangiopathy and ischemia of involved organs.7 These mutations may be sporadic or familial and occur in a genetically susceptible host.8 It should be emphasized that genetic testing in complement mediated HUS is a specialized and slow process (weeks); the initial clinical diagnosis is one of exclusion and does not rest on genetic testing. Furthermore, serum complement levels may be normal in cases of complement mediated aHUS.9-11
This patient had a life-threatening condition that required distinguishing it from 2 rare diseases with very similar presentations; failure to do so in a timely fashion could easily have resulted in his demise. TTP or HUS was the important question, and ADAMTS13 level was one of the determining diagnostic tests. The usual interventions for TTP and HUS (plasmapheresis/plasma exchange and, in some cases, rituximab) were ineffective in this patient with aHUS. The patient achieved full recovery of neurologic, renal, and hematologic impairments after treatment with eculizumab, the recombinant humanized monoclonal antibody that binds to the complement protein C5 brake and inhibits its enzymatic cleavage, thereby interfering with the production of the MAC and cell lysis.
Although the patient did not have an identifiable mutation in the panel of complement regulatory genes tested, the rather dramatic efficacy of the orphan drug eculizumab was in a sense confirmation of his complement related hemolytic uremia. Left undecided are the questions of how long to continue eculizumab, the potential risk of relapse with discontinuation, and the ethical dilemma of proper length of treatment with the most expensive medication in the world given its total cost and no clear discontinuation criteria.12-15 The cost of medications for rare and ultra-rare orphan drugs have approached unsustainable levels, posing ethical challenges to many developed countries.16
Eculizumab and Orphan Drugs
Several months before his assassination, President Kennedy awarded Frances Kathleen Oldham Kelsey, MD, PhD, the President’s Award for Distinguished Federal Civilian Service (August 7, 1962) for her insistence that more safety evidence for thalidomide be presented before she would approve its use in the U.S. As a result of the thalidomide tragedy, the Kefauver Harris amendment was passed unanimously by Congress and signed into law by President Kennedy on October 10, 1962. It required stringent evidence of safety and efficacy for FDA approval of a new medication, reporting of AEs to the FDA, truth in drug advertising, rules governing generic drugs, and informed consent from patients participating in clinical trials.
An unintended consequence was that the development of medications for uncommon diseases became fiscally unattractive to the pharmaceutical industry, ie, “orphaned.” The Orphan Drug Act was enacted by Congress in 1983 to encourage development of drugs to treat less common diseases (diseases/disorders affecting fewer than 200,000 people in the U.S.) through incentives such as exclusive use approval for 7 years, reduced taxes, grants, and favorable laws. Ironically, thalidomide was designated an orphan drug on October 14, 1998 for treatment of multiple myeloma. Since its enactment in 1983, more than 400 orphan drugs and biologic products have been marketed. There may be as many as 7,000 orphan diseases to target for drug therapy, and the 17 of the 20 most expensive drugs in the world in 2013 were for rare orphan diseases.16
Paroxysmal nocturnal hemoglobinuria (PNH) is one of those rare diseases. Mutations of hematopoietic stem cells produce red blood cell membranes deficient in the glycoprotein to which signaling proteins attach (glycosyl phosphatidylinositol) and serve to inhibit complement-induced lysis. This results in intravascular hemolysis (increased LDH and decreased haptoglobin) and increased thrombosis. The FDA approved the orphan drug eculizumab for the treatment of the orphan disease PNH on March 16, 2007.
Eculizumab is a humanized mouse monoclonal antibody that gained FDA orphan drug approval (and exclusivity rights until 2019) for the treatment of aHUS on September 23, 2011, based on 2 industry-sponsored small trials of 17 and 20 patients, and it remains the primary and only known effective treatment for this disease.17-19
Eculizumab has raised many interesting questions. Its mechanism of action wets the appetite of pharmacologists and unveils more basic science questions regarding other related mechanisms of disease, recognition of foreign vs self, genetic influences, virulence of organisms, and more. National and international dilemmas have arisen because of the extreme cost of eculizumab, its position as the only effective treatment for this rare and often fatal disease, and the manufacturer’s recommendation and promotion that it be continued indefinitely. How should the price of a drug, developed in large part by government-supported research and tax incentives, and without competition, be determined and justified?
Pharmaceutical Inflation
A marketplace for pharmaceuticals is simply not analogous to other industries. Advances in pharmacotherapy, some miraculous, have come at a substantial cost. The high cost of drugs became newsworthy with the AIDS pandemic and the approval of the lifesaving azidothymidine (AZT) in 1989 (Burroughs Wellcome–also the developer of pyrimethamine [Daraprim]) and its then record price. Cancer treatment that used to cost $10,000 per year now costs $10,000 per month while the oncology community extolls a 2- or 3-month progression free survival benefit. Patients must now deal with the shock of a cancer diagnosis followed by the shock of an exorbitant copayment.
Recent media attention focused derision on Martin Shkreli, chief executive officer of Turing Pharmaceuticals, for purchasing pyrimethamine and then raising the price of the 62-year-old treatment for protozoan infection toxoplasmosis from $13.50 to $750 per pill. The debacle may also serve to highlight the complexities and ethical issues involved when profit intersects with health care. Some drug costs have dramatically increased in the U.S. because of greed, a belief that a marketplace can control costs, and the lack of regulation. The usual suspects, such as cost of research, length of development, stimulus to innovation, and return on investment, are difficult to apply to old medications whose marketing rights were acquired by purchase of another company. Can marketplace economics be applied in health situations where there is no competition, legal protections afforded manufacturers, consumers unable to make an informed decision?
While pharmacy and therapeutics committees were debating treatment of hepatitis C with either of 2 drugs approved in 2011, boceprevir (Victrelis, Merck) or telapravir (Incivek, Vertex and Johnson & Johnson), Gilead Pharmaceuticals acquired Pharmasset Inc. and its hepatitis C drug sofosbuvir (Sovaldi) for a whopping $11.2 billion in 2012. It received FDA approval April 8, 2013, under Breakthrough Therapy Designation.
While economists argued over the wisdom of such a high-cost acquisition, Gilead generated $9 billion in sales during the first 3 quarters of 2014, surpassing adalimumab (Humira), which had been the highest earning drug in 2014. Hepatitis C could now be quickly treated with truly unprecedented efficacy and without the AEs of interferon. The oft-quoted cost $1,000 per pill or about $84,000 per treatment in the U.S. drew international attention. Prior options for hepatitis C treatment, which preceded sofosbuvir by a mere couple of years, fell into pharmaceutical extinction. Telapravir succumbed to competition and ceased to be manufactured on August 12, 2014. Shortly after approval of sofosbuvir, Gilead also gained approval of its combination product for hepatitis C ledipasvir 90 mg/sofosbuvir 400 mg (Harvoni) on October 10, 2014.
The Most Expensive Drug in the World
Although there are no shortages of contenders for the coveted most expensive title, eculizumab is the current champion. Drugs that offer a cure, such as antibiotics, usually involve a relatively short, onetime course. Lack of return on the cost of development of curative agents may have reduced industrial incentives to develop antibiotics. On the other hand, the extent of infectious diseases, such as malaria, Ebola, tuberculosis, HIV, hepatitis, and the proliferation of drug-resistant organisms, continues to fuel industrial interest for this lifesaving class of medications.
Cancer medications touting a brief interruption of the race to death have raised questions of affordability, equitable access, and quality vs quantity of life. The $11,000 per month endothelial growth factor inhibitor aflibercept (Zaltrap, Regeneron, and Sanofi) was approved by the FDA in November 2012 for colorectal cancer and was followed by a historic rejection by Memorial Sloan-Kettering Cancer Center, since its cost was nearly double that of a similar medication bevacizumab (Avastin) with similar meager benefit of a median progression free survival of 1.4 months.20 Moreover Medicare is mandated to cover the price the manufacturers charge plus a 6% cushion for any cancer drug that the FDA approves.21 Patients with private insurance, often elderly and on a fixed income, are burdened with a copayment requirement of 20% of the cost of the drug. The nonnegotiation clause of Medicare has not reduced cost of medications, particularly for cancer, which many of the elderly will likely face.
The VA, a single-payer system distinguished by bipartisan congressional support, can directly negotiate with pharmaceutical companies, resulting in lower drug prices than discounts guaranteed by federal law; but what if there is no competitor? Biosimilar drugs are currently being debated by those seeking to prolong their patent protection. Stem cell therapies that offer a cure for some rare diseases or hope for common diseases are certain to command astronomical prices. Gene therapy offers hope for cure of both rare and common afflictions but at astounding prices.
The medication alipogene tiparvovec (Glybera, UniQure) delivered by adenovirus, for example, has been approved for use in the rare disorder lipoprotein lipase deficiency and is anticipated to cost $1.6 million for a onetime curative treatment. The pharmaceutical industry has joined the gene therapy race. While this is indeed a record acquisition sum for alipogene tiparvovec, at least it offers a cure. Eculizumab, although unique and effective, offers indefinite administration at a cost exceeding $600,000 per year, every year, for life. In 2014, sales of eculizumab climbed 44% to $2.234 billion.
To Continue or Discontinue Treatment
The duration of treatment with eculizumab poses a challenging dilemma for patients, clinicians, and health care providers. Eculizumab is the only effective treatment for a life-threatening condition, and the manufacturer, Alexion, recommends lifelong therapy of its product that has no competitors. Our patient was treated with 47 fixed-dose infusions of eculizumab at 2-week intervals from May 31, 2014, to February 18, 2016, at a cost of $737,957.80. The commercial cost outside the VA would be about 1.8 times this amount ($1.3 million). This extraordinary cost is the basic ethical issue. Without competition there is little to negotiate.
Need the treatment be lifelong? The AEs of eculizumab are not trivial, and some clinicians felt evidence for indefinite use in this patient was not compelling. Our patient’s initial critical and unstable condition had completely resolved after 2 months of eculizumab. The initial unknown precipitating event triggering the patient’s aHUS probably had resolved. His genetic testing did not disclose any HUS-related mutation. The patient’s serum was sent to Cincinnati Children’s Hospital (CCH) Clinical Laboratory Service to determine his eculizumab level and complement inhibition. His complement inhibition, as measured by CH50 activity, was adequately suppressed at 6% on eculizumab (target of < 10%) in spite of a free serum eculizumab level (81 mg/mL) that was somewhat below the therapeutic range of > 100 mg/mL.
Arguments for lifelong eculizumab therapy are based in part on the theoretical development of anti-eculizumab antibodies that could render reinstitution of eculizumab ineffective.22 Monitoring patients for relapse of their aHUS involves following markers of disease activity (levels of creatinine, LDH, haptoglobin, platelet counts, and Hb in urine). A report of 10 adult patients with aHUS who were treated effectively with eculizumab supports a trial of discontinuation.23 Seven of the 10 patients did not relapse following discontinuation of eculizumab. Three of 10 patients experienced a relapse when monitored for a cumulative 95 months, but all 3 had immediate and complete recovery after resuming therapy. All 3 patients who experienced relapse carried a complement factor H mutation. Their relapses occurred within 6 weeks from the last dose and were detected simply by performing home urine dipstick monitoring for haptoglobin 3 times per week. The 3 patients who relapsed promptly responded to eculizumab reinstitution with return of their labs to baseline.
Monitoring of complement function in patients with aHUS can guide clinically appropriate dosing intervals without changing disease activity markers.24 The half-life of eculizumab is about 11 days, and dosing intervals may be safely extended beyond 2 weeks in select patients.25 The target minimum inhibitory serum eculizumab level necessary to inhibit complement-mediated hemolysis is 50 µg/mL and 35 mg/mL for aHUS and PNH, respectively. In a small pharmacokinetic pilot study, Gatault and colleagues noted that trough levels during eculizumab maintenance by enzyme-linked immunoabsorbent assay (ELISA) of 44 mg/mL to 59 mg/mL inhibited the complement cascade.26 We suggested that weight-based dosing aiming at a trough > 50 mg/mL (rather than fixed dosing at a fixed interval) would be a better maintenance strategy.
In select patients, a trial of gradual discontinuation by lengthening the dosing interval of eculizumab seems a reasonable and safe alternative to indefinite continuation of the drug. After a patient’s successful recovery, the initial and unknown trigger of aHUS may no longer play a role. Improvement in the patient’s medical condition may permit the restoration of the patient’s defenses to once again function normally. Eculizumab seemed to retain its efficacy in the small number of patients who relapsed. Those who relapsed had positive genetic markers.
Further arguments favoring trial discontinuation in patients without known genetic predisposition are that continuation is not without risk, particularly of meningococcal infection, necessity for infusion every 2 weeks for life, little is known regarding long-term risk of the drug, and a lot is known of its extreme cost. Suppression of C5 inhibitory effect can lead to increased susceptibility to infections, whereas increased C5 activity may lead to a continued autoimmune attack on native cells.
As proposed by others, we suggest that this decision be made on a case by case basis, tailoring treatment based on an individual’s genetics and medical history.27 Although the European Medicines Agency has approved lifelong therapy for aHUS, this may be appropriate only for patients who have aHUS complement mutations associated with poor outcomes.27 This approach may not be warranted, however, in a patient, such as the one presented with no genetic mutations, or in those with mutations of uncertain clinical consequence. In such cases, given that 90% of adults who have a relapse experience within the first year after an aHUS episode, a reasonable alternative may be a trial discontinuation.27,28 After 1 year of eculizumab therapy, a trial of discontinuation with urine dipstick monitoring for Hb (Hemastix) 3 times a week for relapse may avoid the unnecessary expense and risk for infection posed by lifelong therapy, and eculizumab may be effectively restarted in case of relapse.
We propose that in these cases it would be reasonable to perform a trial of discontinuation after 1 year of therapy with urine dipstick monitoring for relapse, as lifelong therapy may pose unnecessary expense and risk for infection. In fact, given the financial burden of prolonged therapy on society, we believe it is unethical to continue treatment in a patient with unknown risk for relapse without a trial of discontinuation, as evidence has shown good response to re-initiation of therapy in the event of relapse.28 Agencies that have negotiated or attempted to regulate the cost of eculizumab have been met with public media campaigns featuring afflicted children at risk of death without eculizumab. The public relations company behind these efforts received support from Alexion.29-31
Conclusion
Given the formidable cost and the international monopoly status of eculizumab for a life-threatening condition, prospective discontinuation trials supported by the manufacturer would seem warranted in select cases. Delineating which patients will have a chronic relapsing course and those who will not should be one of these clinical trials. For now, one can only wonder: What’s worse than having a rare disease like aHUS? Perhaps the cost of treatment for a potentially indefinite period of time—now that’s a “bitter pill.”32
A 59-year-old man with a 20-year history (1994) of HIV well controlled on highly active antiretroviral therapy (HAART) therapy (baseline viral load undetectable, CD4+ cell count 781), presented to a community hospital (May 7, 2014) with abdominal pain. The patient’s girlfriend reported unusual behavior for 1 week before admission, including decreased appetite, binge drinking, and nonadherence to HAART therapy.
There was no history of fever, illegal medication use, or diarrhea. In addition to HIV, his past history was remarkable for hepatitis B, hypertension, and left lower extremity amputation secondary to a motor vehicle accident. He had a remote history of cocaine, PCP (phencyclidine), LSD (lysergic acid diethylamide), marijuana, and alcohol misuse and a 50 pack-year smoking history. His family history was remarkable for a mother who died of pancreatic cancer.
During his hospitalization, he developed pronounced expressive aphasia and lethargy but was able to follow simple commands. A computed tomography (CT) scan of the head revealed a left lacunar infarction, and he was transferred to the VA Long Beach Healthcare System in California for further care of a possible stroke.
Shortly after arrival, he developed a fever of 100.9º F. His pulse was 100 bpm and regular, blood pressure was 164/92 mm Hg, and respiratory rate was 14 breaths per minute. A physical examination was remarkable for somnolence, disorientation, and aphasia. He was grimacing to light palpation in all 4 quadrants of the abdomen and had diffuse purpura on skin examination. Laboratory results showed worsening thrombocytopenia, acute kidney injury with proteinuria and hemoglobinuria, and hemolysis (schistocytes, low haptoglobin level, and elevated lactate dehydrogenase [LDH]).
The patient’s changes in baseline laboratory results were platelet count 206,000 mm3 to 64,000 mm3, serum creatinine level 0.98 mg/dL to 1.55 mg/dL. His hemogram showed normochromic normocytic anemia (hemoglobin [Hb] level 10.2 g/dL) with schistocytes. Serum samples were initially unreportable by the laboratory due to severe hemolysis, but his haptoglobin level was found to be low and, conversely, LDH remarkably high. Fifteen days after admission, his CD4+ cell count was 141. An abdominal CT scan showed right lower quadrant abdominal free fluid and thickening of the terminal ileum with surrounding stranding, suggestive of terminal ileitis, and he was started on piperacillin-tazobactam. A lumbar puncture was unremarkable, and HAART medications were resumed. The patient required intubation and a ventilator for acute respiratory failure.
Empiric treatment for presumed thrombotic thrombocytopenic purpura (TTP) with plasmapheresis and methylprednisolone was ineffective, and the patient required mechanical ventilation and hemodialysis.
In refractory cases of TTP-hemolytic uremic syndrome, rituximab, a monoclonal antibody directed at CD20 present on B lymphocytes, is added empirically as effective salvage therapy and was therefore tried in this case.1
However, the addition of rituximab failed to improve the patient’s condition, and he developed further seizure activity and evidence of new lacunar infarctions as seen on magnetic resonance imaging of the brain. His hospital course was complicated by recurrent hemoptysis and respiratory failure, requiring assisted ventilation and eventually tracheostomy.
A normal ADAMTS13 level (72%) and negative Shiga toxin test changed the diagnosis to atypical hemolytic uremic syndrome (aHUS). Mean complement C3 (74 mg/dL) and C4 (9 mg/dL) levels were low. Plasmapheresis was discontinued, and treatment with eculizumab (Soliris, Alexion Pharmaceuticals) was initiated. Meningococcal vaccine was administered post-eculizumab, aimed at reducing but not eliminating the risk of meningococcemia.2 Two weeks later, the patient’s platelet count normalized, renal function improved, hemolysis resolved, and the patient regained full mental status. Eight weeks after initiating eculizumab, he no longer required dialysis.
Discussion
Generalized thrombosis of smaller blood vessels (thrombotic microangiopathy [TMA]) occurs in 3 uncommon syndromes—TTP, HUS, and aHUS—all with similar clinical presentations but distinct pathologic etiologies and treatment. These syndromes share a clinical picture of thrombocytopenia, hemolytic anemia, and renal failure. Hemolysis in these conditions is manifested by schistocytes, elevated lactate dehydrogenase from damaged cells, decreased haptoglobin, anemia, and hemoglobinuria.
Thrombotic Thrombocytopenic Purpura
Thrombocytopenic purpura occurs in about 3 cases per 1,000,000 adults per year.3 It occurs when the metalloproteinase enzyme ADAMTS13 activity is impaired, interrupting its function to cleave large sticky von Willebrand factor (vWF) multimers, resulting in coagulation in microvasculature by increased platelet aggregation, hemolysis from shearing of red blood cells, and compromised circulation to the highly vascularized kidney and other vital organs.4 The hallmark of TTP is a severely decreased ADAMTS13 activity (< 5% of normal) secondary to coexisting conditions, such as cancer, pregnancy, HIV infection, adverse effects (AEs), or antibodies to ADAMTS13.5
The TTP pentad of thrombocytopenia, hemolytic anemia, neurologic symptoms, renal failure, and fever were present in our patient. The patient had a known HIV infection but no exposure to medications associated with TTP (such as acyclovir, quinine, oxymorphone, platelet aggregation inhibitors, or immunosuppressants). Prior to obtaining ADAMTS13 level, the patient was treated empirically for TTP with early and daily plasma exchange to remove the inhibitor of ADAMTS13 and replace it with fresh frozen plasma. Rituximab also was used to inhibit production of antibodies to ADAMTS13 from CD20 B lymphocytes. These empiric clinical measures were not effective in stopping his decline in renal and neurologic functions.
Hemolytic Uremic Syndrome
Like TTP, HUS is also a consequence of thrombotic microangiopathy. However, in contrast to TTP, which is more commonly seen in adults,3 HUS is usually seen in young children secondary to Shiga toxin-producing Escherichia coli (STEC).6 Hemolytic uremic syndrome, also referred to as STEC-HUS or typical HUS, is a rare disease affecting 10 to 20 people per million annually. About 10% of these patients are classified as having aHUS because STEC is not implicated in their disease. It is of interest that, unlike aHUS, STEC-HUS is usually a self-limited disease of children, the majority of whom recover without relapse, and evidence that eculizumab improves prognosis in STEC-HUS is not compelling.5
Atypical Hemolytic Uremic Syndrome
Atypical HUS is a complement-mediated disease. The usual function of complement proteins is to destroy foreign cells and activate immune cells. However, in aHUS this protective defense system goes awry resulting in a pathologic thrombotic milieu. Specifically, aHUS is a continuous complement mediated attack on vascular endothelial beds due to the failure of protein regulators to terminate the complement cascade. Unlike typical HUS, which is usually associated with a Shiga-toxin producing gastrointestinal infection, the trigger in aHUS is unknown and thought to be associated with a genetic predisposition.
Atypical HUS distinguishes itself from TTP and HUS in that it does not respond to plasma exchange, corticosteroids, rituximab, or other immunosupressants. This is due to the distinct underlying pathophysiology of aHUS in which the problem is the unbridled activation of the alternate arm of the complement system.
The complement system is part of the innate immune system, which acts with or without the adaptive immune system it “complements” by amplifying a cascade of responses to eliminate the trigger pathogen. There are 3 complement pathways—classical, lectin, and alternate. The alternate complement pathway, whose activation generates C5a complement (anaphylotoxin), was most pertinent to this case. This precipitates a number of downstream protein cleaving events that lead to the cell lysing membrane attack complex (MAC), which creates a pore in the cell membrane of pathogens seen as foreign. In aHUS, the patient’s own cells come under attack by their own complement, which is no longer inhibited due to mutations in regulatory proteins of the alternate pathway.
With the foot off the complement brake (the hallmark feature underlying aHUS), endothelial cells, leukocytes, and platelets become hyperactive and thrombogenic, thereby resulting in microangiopathy and ischemia of involved organs.7 These mutations may be sporadic or familial and occur in a genetically susceptible host.8 It should be emphasized that genetic testing in complement mediated HUS is a specialized and slow process (weeks); the initial clinical diagnosis is one of exclusion and does not rest on genetic testing. Furthermore, serum complement levels may be normal in cases of complement mediated aHUS.9-11
This patient had a life-threatening condition that required distinguishing it from 2 rare diseases with very similar presentations; failure to do so in a timely fashion could easily have resulted in his demise. TTP or HUS was the important question, and ADAMTS13 level was one of the determining diagnostic tests. The usual interventions for TTP and HUS (plasmapheresis/plasma exchange and, in some cases, rituximab) were ineffective in this patient with aHUS. The patient achieved full recovery of neurologic, renal, and hematologic impairments after treatment with eculizumab, the recombinant humanized monoclonal antibody that binds to the complement protein C5 brake and inhibits its enzymatic cleavage, thereby interfering with the production of the MAC and cell lysis.
Although the patient did not have an identifiable mutation in the panel of complement regulatory genes tested, the rather dramatic efficacy of the orphan drug eculizumab was in a sense confirmation of his complement related hemolytic uremia. Left undecided are the questions of how long to continue eculizumab, the potential risk of relapse with discontinuation, and the ethical dilemma of proper length of treatment with the most expensive medication in the world given its total cost and no clear discontinuation criteria.12-15 The cost of medications for rare and ultra-rare orphan drugs have approached unsustainable levels, posing ethical challenges to many developed countries.16
Eculizumab and Orphan Drugs
Several months before his assassination, President Kennedy awarded Frances Kathleen Oldham Kelsey, MD, PhD, the President’s Award for Distinguished Federal Civilian Service (August 7, 1962) for her insistence that more safety evidence for thalidomide be presented before she would approve its use in the U.S. As a result of the thalidomide tragedy, the Kefauver Harris amendment was passed unanimously by Congress and signed into law by President Kennedy on October 10, 1962. It required stringent evidence of safety and efficacy for FDA approval of a new medication, reporting of AEs to the FDA, truth in drug advertising, rules governing generic drugs, and informed consent from patients participating in clinical trials.
An unintended consequence was that the development of medications for uncommon diseases became fiscally unattractive to the pharmaceutical industry, ie, “orphaned.” The Orphan Drug Act was enacted by Congress in 1983 to encourage development of drugs to treat less common diseases (diseases/disorders affecting fewer than 200,000 people in the U.S.) through incentives such as exclusive use approval for 7 years, reduced taxes, grants, and favorable laws. Ironically, thalidomide was designated an orphan drug on October 14, 1998 for treatment of multiple myeloma. Since its enactment in 1983, more than 400 orphan drugs and biologic products have been marketed. There may be as many as 7,000 orphan diseases to target for drug therapy, and the 17 of the 20 most expensive drugs in the world in 2013 were for rare orphan diseases.16
Paroxysmal nocturnal hemoglobinuria (PNH) is one of those rare diseases. Mutations of hematopoietic stem cells produce red blood cell membranes deficient in the glycoprotein to which signaling proteins attach (glycosyl phosphatidylinositol) and serve to inhibit complement-induced lysis. This results in intravascular hemolysis (increased LDH and decreased haptoglobin) and increased thrombosis. The FDA approved the orphan drug eculizumab for the treatment of the orphan disease PNH on March 16, 2007.
Eculizumab is a humanized mouse monoclonal antibody that gained FDA orphan drug approval (and exclusivity rights until 2019) for the treatment of aHUS on September 23, 2011, based on 2 industry-sponsored small trials of 17 and 20 patients, and it remains the primary and only known effective treatment for this disease.17-19
Eculizumab has raised many interesting questions. Its mechanism of action wets the appetite of pharmacologists and unveils more basic science questions regarding other related mechanisms of disease, recognition of foreign vs self, genetic influences, virulence of organisms, and more. National and international dilemmas have arisen because of the extreme cost of eculizumab, its position as the only effective treatment for this rare and often fatal disease, and the manufacturer’s recommendation and promotion that it be continued indefinitely. How should the price of a drug, developed in large part by government-supported research and tax incentives, and without competition, be determined and justified?
Pharmaceutical Inflation
A marketplace for pharmaceuticals is simply not analogous to other industries. Advances in pharmacotherapy, some miraculous, have come at a substantial cost. The high cost of drugs became newsworthy with the AIDS pandemic and the approval of the lifesaving azidothymidine (AZT) in 1989 (Burroughs Wellcome–also the developer of pyrimethamine [Daraprim]) and its then record price. Cancer treatment that used to cost $10,000 per year now costs $10,000 per month while the oncology community extolls a 2- or 3-month progression free survival benefit. Patients must now deal with the shock of a cancer diagnosis followed by the shock of an exorbitant copayment.
Recent media attention focused derision on Martin Shkreli, chief executive officer of Turing Pharmaceuticals, for purchasing pyrimethamine and then raising the price of the 62-year-old treatment for protozoan infection toxoplasmosis from $13.50 to $750 per pill. The debacle may also serve to highlight the complexities and ethical issues involved when profit intersects with health care. Some drug costs have dramatically increased in the U.S. because of greed, a belief that a marketplace can control costs, and the lack of regulation. The usual suspects, such as cost of research, length of development, stimulus to innovation, and return on investment, are difficult to apply to old medications whose marketing rights were acquired by purchase of another company. Can marketplace economics be applied in health situations where there is no competition, legal protections afforded manufacturers, consumers unable to make an informed decision?
While pharmacy and therapeutics committees were debating treatment of hepatitis C with either of 2 drugs approved in 2011, boceprevir (Victrelis, Merck) or telapravir (Incivek, Vertex and Johnson & Johnson), Gilead Pharmaceuticals acquired Pharmasset Inc. and its hepatitis C drug sofosbuvir (Sovaldi) for a whopping $11.2 billion in 2012. It received FDA approval April 8, 2013, under Breakthrough Therapy Designation.
While economists argued over the wisdom of such a high-cost acquisition, Gilead generated $9 billion in sales during the first 3 quarters of 2014, surpassing adalimumab (Humira), which had been the highest earning drug in 2014. Hepatitis C could now be quickly treated with truly unprecedented efficacy and without the AEs of interferon. The oft-quoted cost $1,000 per pill or about $84,000 per treatment in the U.S. drew international attention. Prior options for hepatitis C treatment, which preceded sofosbuvir by a mere couple of years, fell into pharmaceutical extinction. Telapravir succumbed to competition and ceased to be manufactured on August 12, 2014. Shortly after approval of sofosbuvir, Gilead also gained approval of its combination product for hepatitis C ledipasvir 90 mg/sofosbuvir 400 mg (Harvoni) on October 10, 2014.
The Most Expensive Drug in the World
Although there are no shortages of contenders for the coveted most expensive title, eculizumab is the current champion. Drugs that offer a cure, such as antibiotics, usually involve a relatively short, onetime course. Lack of return on the cost of development of curative agents may have reduced industrial incentives to develop antibiotics. On the other hand, the extent of infectious diseases, such as malaria, Ebola, tuberculosis, HIV, hepatitis, and the proliferation of drug-resistant organisms, continues to fuel industrial interest for this lifesaving class of medications.
Cancer medications touting a brief interruption of the race to death have raised questions of affordability, equitable access, and quality vs quantity of life. The $11,000 per month endothelial growth factor inhibitor aflibercept (Zaltrap, Regeneron, and Sanofi) was approved by the FDA in November 2012 for colorectal cancer and was followed by a historic rejection by Memorial Sloan-Kettering Cancer Center, since its cost was nearly double that of a similar medication bevacizumab (Avastin) with similar meager benefit of a median progression free survival of 1.4 months.20 Moreover Medicare is mandated to cover the price the manufacturers charge plus a 6% cushion for any cancer drug that the FDA approves.21 Patients with private insurance, often elderly and on a fixed income, are burdened with a copayment requirement of 20% of the cost of the drug. The nonnegotiation clause of Medicare has not reduced cost of medications, particularly for cancer, which many of the elderly will likely face.
The VA, a single-payer system distinguished by bipartisan congressional support, can directly negotiate with pharmaceutical companies, resulting in lower drug prices than discounts guaranteed by federal law; but what if there is no competitor? Biosimilar drugs are currently being debated by those seeking to prolong their patent protection. Stem cell therapies that offer a cure for some rare diseases or hope for common diseases are certain to command astronomical prices. Gene therapy offers hope for cure of both rare and common afflictions but at astounding prices.
The medication alipogene tiparvovec (Glybera, UniQure) delivered by adenovirus, for example, has been approved for use in the rare disorder lipoprotein lipase deficiency and is anticipated to cost $1.6 million for a onetime curative treatment. The pharmaceutical industry has joined the gene therapy race. While this is indeed a record acquisition sum for alipogene tiparvovec, at least it offers a cure. Eculizumab, although unique and effective, offers indefinite administration at a cost exceeding $600,000 per year, every year, for life. In 2014, sales of eculizumab climbed 44% to $2.234 billion.
To Continue or Discontinue Treatment
The duration of treatment with eculizumab poses a challenging dilemma for patients, clinicians, and health care providers. Eculizumab is the only effective treatment for a life-threatening condition, and the manufacturer, Alexion, recommends lifelong therapy of its product that has no competitors. Our patient was treated with 47 fixed-dose infusions of eculizumab at 2-week intervals from May 31, 2014, to February 18, 2016, at a cost of $737,957.80. The commercial cost outside the VA would be about 1.8 times this amount ($1.3 million). This extraordinary cost is the basic ethical issue. Without competition there is little to negotiate.
Need the treatment be lifelong? The AEs of eculizumab are not trivial, and some clinicians felt evidence for indefinite use in this patient was not compelling. Our patient’s initial critical and unstable condition had completely resolved after 2 months of eculizumab. The initial unknown precipitating event triggering the patient’s aHUS probably had resolved. His genetic testing did not disclose any HUS-related mutation. The patient’s serum was sent to Cincinnati Children’s Hospital (CCH) Clinical Laboratory Service to determine his eculizumab level and complement inhibition. His complement inhibition, as measured by CH50 activity, was adequately suppressed at 6% on eculizumab (target of < 10%) in spite of a free serum eculizumab level (81 mg/mL) that was somewhat below the therapeutic range of > 100 mg/mL.
Arguments for lifelong eculizumab therapy are based in part on the theoretical development of anti-eculizumab antibodies that could render reinstitution of eculizumab ineffective.22 Monitoring patients for relapse of their aHUS involves following markers of disease activity (levels of creatinine, LDH, haptoglobin, platelet counts, and Hb in urine). A report of 10 adult patients with aHUS who were treated effectively with eculizumab supports a trial of discontinuation.23 Seven of the 10 patients did not relapse following discontinuation of eculizumab. Three of 10 patients experienced a relapse when monitored for a cumulative 95 months, but all 3 had immediate and complete recovery after resuming therapy. All 3 patients who experienced relapse carried a complement factor H mutation. Their relapses occurred within 6 weeks from the last dose and were detected simply by performing home urine dipstick monitoring for haptoglobin 3 times per week. The 3 patients who relapsed promptly responded to eculizumab reinstitution with return of their labs to baseline.
Monitoring of complement function in patients with aHUS can guide clinically appropriate dosing intervals without changing disease activity markers.24 The half-life of eculizumab is about 11 days, and dosing intervals may be safely extended beyond 2 weeks in select patients.25 The target minimum inhibitory serum eculizumab level necessary to inhibit complement-mediated hemolysis is 50 µg/mL and 35 mg/mL for aHUS and PNH, respectively. In a small pharmacokinetic pilot study, Gatault and colleagues noted that trough levels during eculizumab maintenance by enzyme-linked immunoabsorbent assay (ELISA) of 44 mg/mL to 59 mg/mL inhibited the complement cascade.26 We suggested that weight-based dosing aiming at a trough > 50 mg/mL (rather than fixed dosing at a fixed interval) would be a better maintenance strategy.
In select patients, a trial of gradual discontinuation by lengthening the dosing interval of eculizumab seems a reasonable and safe alternative to indefinite continuation of the drug. After a patient’s successful recovery, the initial and unknown trigger of aHUS may no longer play a role. Improvement in the patient’s medical condition may permit the restoration of the patient’s defenses to once again function normally. Eculizumab seemed to retain its efficacy in the small number of patients who relapsed. Those who relapsed had positive genetic markers.
Further arguments favoring trial discontinuation in patients without known genetic predisposition are that continuation is not without risk, particularly of meningococcal infection, necessity for infusion every 2 weeks for life, little is known regarding long-term risk of the drug, and a lot is known of its extreme cost. Suppression of C5 inhibitory effect can lead to increased susceptibility to infections, whereas increased C5 activity may lead to a continued autoimmune attack on native cells.
As proposed by others, we suggest that this decision be made on a case by case basis, tailoring treatment based on an individual’s genetics and medical history.27 Although the European Medicines Agency has approved lifelong therapy for aHUS, this may be appropriate only for patients who have aHUS complement mutations associated with poor outcomes.27 This approach may not be warranted, however, in a patient, such as the one presented with no genetic mutations, or in those with mutations of uncertain clinical consequence. In such cases, given that 90% of adults who have a relapse experience within the first year after an aHUS episode, a reasonable alternative may be a trial discontinuation.27,28 After 1 year of eculizumab therapy, a trial of discontinuation with urine dipstick monitoring for Hb (Hemastix) 3 times a week for relapse may avoid the unnecessary expense and risk for infection posed by lifelong therapy, and eculizumab may be effectively restarted in case of relapse.
We propose that in these cases it would be reasonable to perform a trial of discontinuation after 1 year of therapy with urine dipstick monitoring for relapse, as lifelong therapy may pose unnecessary expense and risk for infection. In fact, given the financial burden of prolonged therapy on society, we believe it is unethical to continue treatment in a patient with unknown risk for relapse without a trial of discontinuation, as evidence has shown good response to re-initiation of therapy in the event of relapse.28 Agencies that have negotiated or attempted to regulate the cost of eculizumab have been met with public media campaigns featuring afflicted children at risk of death without eculizumab. The public relations company behind these efforts received support from Alexion.29-31
Conclusion
Given the formidable cost and the international monopoly status of eculizumab for a life-threatening condition, prospective discontinuation trials supported by the manufacturer would seem warranted in select cases. Delineating which patients will have a chronic relapsing course and those who will not should be one of these clinical trials. For now, one can only wonder: What’s worse than having a rare disease like aHUS? Perhaps the cost of treatment for a potentially indefinite period of time—now that’s a “bitter pill.”32
1. Caramazza D, Quintini G, Abbene I, et al. Relapsing or refractory idiopathic thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: the role of rituximab. Transfusion. 2010;50(12):2753-2760.
2. Köse O, Zimmerhackl LB, Jungraithmayr T, Mache C, Nürnberger J. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin Thromb Hemost. 2010;36(6):669-672.
3. Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, George JN. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer. 2013;60(10):1676-1682.
4. Sadler JE. Von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood. 2008;112(1):11-18.
5. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19.
6. Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035-1050.
7. Liszewski MK, Atkinson JP. Exploring the complement system in human disease. The Rheumatologist website. http://www.the-rheumatologist.org/article/exploring-the-complement-system-in-human-disease. Published February 1, 2010. Accessed May 9, 2016.
8. Mayer CL, Leibowitz CS, Kurosawa S, Stearns-Kurosawa DJ. Shiga toxins and the pathophysiology of hemolytic uremic syndrome in humans and animals. Toxins (Basel). 2012;4(11):1261-1287.
9. Noris M, Mescia F, Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nat Rev Nephrol. 2012;8(11):622-633.
10. Geerdink LM, Westra D, van Wijk JA, et al. Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol. 2012;27(8):1283-1291.
11. Sellier-Leclerc AL, Frémeaux-Bacchi V, Dragon-Durey MA, et al; French Society of Pediatric Nephrology. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007;18(8):2392-2400.
12. Herper M. The worlds most expensive drugs. Forbes. February 22, 2010.
13. Nordrum A. Drug prices: world's most expensive medicine costs $440,000 a year, but is it worth the expense? International Business Times website. http://www.ibtimes.com/drug-prices-worlds-most-expensive-medicine-costs-440000-year-it-worth-expense-2302609. Updated February 13, 2016. Published June 24, 2015. Accessed June 15, 2016.
14. CBC News. The real cost of the world's most expensive drug [video]. CBC/Radio Canada website. http://www.cbc.ca/player/play/2670383596. Accessed June 15, 2016.
15. EvaluatePharma. Orphan Drug Report 2014. EvaluatePharma website. http://www.evaluategroup.com/orphandrug2014. Published 2014. Accessed June 15, 2016.
16. Isaacs D. Ethical dilemmas about orphan drugs for orphan diseases. J Paediatr Child Health. 2014;50(4):249-250.
17. Licht C, Muus P, Legendre CM, et al. Eculizumab (ECU) safety and efficacy in atypical hemolytic uremic syndrome (aHUS) patients with long disease duration and chronic kidney disease (CKD): 2-year results. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
18. Greenbaum L, Legendre CM, Babu S, et al. Eculizumab (ECU) in atypical hemolytic uremic syndrome (aHUS) patients with progressing thrombotic microangiopathy (TMA): 2-year data. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
19. Legendre CM, Licht C, Muus P, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Eng J Med. 2013;368(23):2169-2181.
20. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters. New York Times. October 14, 2012:Opinion Pages.
21. Medicare Prescription Drug, Improvement, and Modernization Act of 2003, Public Law 108-173;117 Stat 2066. U.S. Government Printing Office website. https://www.gpo.gov/fdsys/pkg/PLAW-108publ173/pdf/PLAW-108publ173.pdf. Approved December 8, 2003. Accessed June 6, 2016.
22. Jodele S, Fukuda T, Vinks A, et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2014;20(4):518-525.
23. Ardissino G, Testa S, Possenti I, et al. Discontinuation of eculizumab maintenance treatment for atypical hemolytic uremic syndrome: a report of 10 cases. Am J Kidney Dis. 2014;64(4):633-637.
24. Cugno M, Gualtierotti R, Possenti I, et al. Complement functional tests for monitoring eculizumab treatment in patients with atypical hemolytic uremic syndrome. J Thromb Haemost. 2014;12(9):1440-1448.
25. Waters AM, Licht C. aHUS caused by complement dysregulation: new therapies on the horizon. Pediatr Nephrol. 2011;26(1):41-57.
26. Gatault P, Brachet G, Ternant D, et al. Therapeutic drug monitoring of eculizumab: rational for an individualized dosing schedule. MAbs. 2015;7(6):1205-1211.
27. Zuber J, Fakhouri F, Roumenina LT, Loirat C, Frémeaux-Bacchi V; French Study Group for aHUS/C3G. Use of eculizumab for atypical haemolytic uraemic syndrome and C3 glomerulopathies. Nat Rev Nephrol. 2012;8(11):643-657.
28. Fakhouri F, Frémeaux-Bacchi V, Loirat C. Atypical hemolytic uremic syndrome: from the rediscovery of complement to targeted therapy. Eur J Intern Med. 2013;24(6):492-495.
29. Crowe K. Analysis: how pharmaceutical company Alexion set the price of the world's most expensive drug. CBC/Radio Canada website. http://www.cbc.ca/news/health/how-pharmaceutical-company-alexion-set-the-price-of-the-world-s-most-expensive-drug-1.3125251 Updated June 25, 2015. Accessed June 21, 2016.
30. Drug campaign for sick child was a PR stunt. FlandersToday website. http://www.flanderstoday.eu/business/drug-campaign-sick-child-was-pr-stunt. Published May 8, 2013. Accessed June 21, 2016.
31. Herald on Sunday editorial: miracle cure, morally derelect. New Zealand Herald website. http://www.nzherald.co.nz/opinion/news/article.cfm?c_id=466&objectid=10861630. Published January 27, 2013. Accessed June 21, 2016.
32. Brill S. Bitter pill: why medical bills are killing us. http://healthland.time.com/2013/02/20/bitter-pill-why-medical-bills-are-killing-us/print/[2/26/2013. Time website. Published February 20, 2013. Accessed June 6, 2016.
1. Caramazza D, Quintini G, Abbene I, et al. Relapsing or refractory idiopathic thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: the role of rituximab. Transfusion. 2010;50(12):2753-2760.
2. Köse O, Zimmerhackl LB, Jungraithmayr T, Mache C, Nürnberger J. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin Thromb Hemost. 2010;36(6):669-672.
3. Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, George JN. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer. 2013;60(10):1676-1682.
4. Sadler JE. Von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood. 2008;112(1):11-18.
5. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19.
6. Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035-1050.
7. Liszewski MK, Atkinson JP. Exploring the complement system in human disease. The Rheumatologist website. http://www.the-rheumatologist.org/article/exploring-the-complement-system-in-human-disease. Published February 1, 2010. Accessed May 9, 2016.
8. Mayer CL, Leibowitz CS, Kurosawa S, Stearns-Kurosawa DJ. Shiga toxins and the pathophysiology of hemolytic uremic syndrome in humans and animals. Toxins (Basel). 2012;4(11):1261-1287.
9. Noris M, Mescia F, Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nat Rev Nephrol. 2012;8(11):622-633.
10. Geerdink LM, Westra D, van Wijk JA, et al. Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol. 2012;27(8):1283-1291.
11. Sellier-Leclerc AL, Frémeaux-Bacchi V, Dragon-Durey MA, et al; French Society of Pediatric Nephrology. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007;18(8):2392-2400.
12. Herper M. The worlds most expensive drugs. Forbes. February 22, 2010.
13. Nordrum A. Drug prices: world's most expensive medicine costs $440,000 a year, but is it worth the expense? International Business Times website. http://www.ibtimes.com/drug-prices-worlds-most-expensive-medicine-costs-440000-year-it-worth-expense-2302609. Updated February 13, 2016. Published June 24, 2015. Accessed June 15, 2016.
14. CBC News. The real cost of the world's most expensive drug [video]. CBC/Radio Canada website. http://www.cbc.ca/player/play/2670383596. Accessed June 15, 2016.
15. EvaluatePharma. Orphan Drug Report 2014. EvaluatePharma website. http://www.evaluategroup.com/orphandrug2014. Published 2014. Accessed June 15, 2016.
16. Isaacs D. Ethical dilemmas about orphan drugs for orphan diseases. J Paediatr Child Health. 2014;50(4):249-250.
17. Licht C, Muus P, Legendre CM, et al. Eculizumab (ECU) safety and efficacy in atypical hemolytic uremic syndrome (aHUS) patients with long disease duration and chronic kidney disease (CKD): 2-year results. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
18. Greenbaum L, Legendre CM, Babu S, et al. Eculizumab (ECU) in atypical hemolytic uremic syndrome (aHUS) patients with progressing thrombotic microangiopathy (TMA): 2-year data. Poster presented at: 54th Annual Meeting of the American Society of Hematology; December 8-12, 2012; Atlanta, GA.
19. Legendre CM, Licht C, Muus P, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Eng J Med. 2013;368(23):2169-2181.
20. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters. New York Times. October 14, 2012:Opinion Pages.
21. Medicare Prescription Drug, Improvement, and Modernization Act of 2003, Public Law 108-173;117 Stat 2066. U.S. Government Printing Office website. https://www.gpo.gov/fdsys/pkg/PLAW-108publ173/pdf/PLAW-108publ173.pdf. Approved December 8, 2003. Accessed June 6, 2016.
22. Jodele S, Fukuda T, Vinks A, et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2014;20(4):518-525.
23. Ardissino G, Testa S, Possenti I, et al. Discontinuation of eculizumab maintenance treatment for atypical hemolytic uremic syndrome: a report of 10 cases. Am J Kidney Dis. 2014;64(4):633-637.
24. Cugno M, Gualtierotti R, Possenti I, et al. Complement functional tests for monitoring eculizumab treatment in patients with atypical hemolytic uremic syndrome. J Thromb Haemost. 2014;12(9):1440-1448.
25. Waters AM, Licht C. aHUS caused by complement dysregulation: new therapies on the horizon. Pediatr Nephrol. 2011;26(1):41-57.
26. Gatault P, Brachet G, Ternant D, et al. Therapeutic drug monitoring of eculizumab: rational for an individualized dosing schedule. MAbs. 2015;7(6):1205-1211.
27. Zuber J, Fakhouri F, Roumenina LT, Loirat C, Frémeaux-Bacchi V; French Study Group for aHUS/C3G. Use of eculizumab for atypical haemolytic uraemic syndrome and C3 glomerulopathies. Nat Rev Nephrol. 2012;8(11):643-657.
28. Fakhouri F, Frémeaux-Bacchi V, Loirat C. Atypical hemolytic uremic syndrome: from the rediscovery of complement to targeted therapy. Eur J Intern Med. 2013;24(6):492-495.
29. Crowe K. Analysis: how pharmaceutical company Alexion set the price of the world's most expensive drug. CBC/Radio Canada website. http://www.cbc.ca/news/health/how-pharmaceutical-company-alexion-set-the-price-of-the-world-s-most-expensive-drug-1.3125251 Updated June 25, 2015. Accessed June 21, 2016.
30. Drug campaign for sick child was a PR stunt. FlandersToday website. http://www.flanderstoday.eu/business/drug-campaign-sick-child-was-pr-stunt. Published May 8, 2013. Accessed June 21, 2016.
31. Herald on Sunday editorial: miracle cure, morally derelect. New Zealand Herald website. http://www.nzherald.co.nz/opinion/news/article.cfm?c_id=466&objectid=10861630. Published January 27, 2013. Accessed June 21, 2016.
32. Brill S. Bitter pill: why medical bills are killing us. http://healthland.time.com/2013/02/20/bitter-pill-why-medical-bills-are-killing-us/print/[2/26/2013. Time website. Published February 20, 2013. Accessed June 6, 2016.
Expanding Treatment Options
Q) One of my diabetic patients read about finerenone in The New York Times. Apparently, it’s the “newest cure for albuminuria”! Is this just hype, or do the trials on this medication really show progress against kidney disease? Should I buy stock in the company?
Albuminuria (> 500 mg/d) associated with diabetic nephropathy and other glomerular diseases increases patient risk for chronic kidney disease (CKD) and its progression to end-stage renal disease (ESRD). Reduction of albuminuria has been shown to slow the progression of CKD.
Renin-angiotensin-aldosterone system (RAAS) blockers, such as ACE inhibitors or angiotensin receptor blockers, are considered firstline therapy to reduce albuminuria. Additional treatment modalities include diuretics, nondihydropyridine calcium channel blockers, ß-blockers, and aldosterone antagonist therapy. Limiting dietary sodium helps control blood pressure, thus slowing disease progression. In addition, some studies show that limiting phosphorus and protein (for the latter, intake of no more than 0.7 g/kg ideal body weight per day) may slow the progression of CKD. Unfortunately, despite these interventions, patients may still advance to ESRD.1
The aldosterone and steroidal mineralocorticoid receptor antagonists (MRA) spironolactone and eplerenone have been found to reduce albuminuria when used in conjunction with RAAS blockade. However, patients using this combination are up to eight times more likely to experience hyperkalemia—a serious, potentially life-threatening adverse condition—than those not using an MRA.2 The presence of hyperkalemia requires discontinuation of the RAAS blocker and the MRA, at least temporarily.
Finerenone, a nonsteroidal MRA with “greater receptor selectivity than spironolactone and better receptor affinity than eplerenone in vitro,” is in phase III trials for the treatment of systolic and diastolic dysfunction and reduction of morbidity and mortality associated with heart failure.2 One study has already demonstrated that finerenone (5 to 10 mg/d) is at least as effective as spironolactone (25 mg/d) for heart failure patients.3
The Mineralocorticoid Receptor Antagonist Tolerability Study-Diabetic Nephropathy (ARTS-DN) found that finerenone at 10 to 20 mg/d was superior to spironolactone and eplerenone, partly due to the decreased incidence of hyperkalemia. However, it should be noted that the lower incidence of hyperkalemia may be attributable to the fact that 66% of the study participants had an estimated glomerular filtration rate (eGFR) greater than 60 mL/min and that potential participants with a serum potassium level of more than 4.8 mEq/L were not included in the study.2
Additional research is needed to confirm superiority of finerenone over spironolactone and eplerenone, in conjunction with RAAS blockers, in the treatment of albuminuria and hyperkalemia. Including subjects with lower eGFR (such as patients with stage IV CKD who are at higher risk for hyperkalemia) would give a better indication of finerenone’s efficacy. In the meantime, it’s probably too soon to corner the market on this stock! —SEB
Susan E. Brown, MS, ARNP, ACNP-BC, CCRN
Great River Nephrology, West Burlington, Iowa
References
1. Parikh SV, Haddad NJ, Hebert LA. Retarding progression of kidney disease. In: Johnson RJ, Feehally J, Floege J, eds. Comprehensive Clinical Nephrology. 5th ed. Philadelphia, PA: Saunders; 2015:931-940.
2. Bakris GL, Agarwal R, Chan JC, et al. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314(9):884-894.
3. Kolkhof P, Delbeck M, Kretschmer A, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist, protects from rat cardiorenal injury. J Cardiovasc Pharmacol. 2014;64(1):69-78.
Q) One of my diabetic patients read about finerenone in The New York Times. Apparently, it’s the “newest cure for albuminuria”! Is this just hype, or do the trials on this medication really show progress against kidney disease? Should I buy stock in the company?
Albuminuria (> 500 mg/d) associated with diabetic nephropathy and other glomerular diseases increases patient risk for chronic kidney disease (CKD) and its progression to end-stage renal disease (ESRD). Reduction of albuminuria has been shown to slow the progression of CKD.
Renin-angiotensin-aldosterone system (RAAS) blockers, such as ACE inhibitors or angiotensin receptor blockers, are considered firstline therapy to reduce albuminuria. Additional treatment modalities include diuretics, nondihydropyridine calcium channel blockers, ß-blockers, and aldosterone antagonist therapy. Limiting dietary sodium helps control blood pressure, thus slowing disease progression. In addition, some studies show that limiting phosphorus and protein (for the latter, intake of no more than 0.7 g/kg ideal body weight per day) may slow the progression of CKD. Unfortunately, despite these interventions, patients may still advance to ESRD.1
The aldosterone and steroidal mineralocorticoid receptor antagonists (MRA) spironolactone and eplerenone have been found to reduce albuminuria when used in conjunction with RAAS blockade. However, patients using this combination are up to eight times more likely to experience hyperkalemia—a serious, potentially life-threatening adverse condition—than those not using an MRA.2 The presence of hyperkalemia requires discontinuation of the RAAS blocker and the MRA, at least temporarily.
Finerenone, a nonsteroidal MRA with “greater receptor selectivity than spironolactone and better receptor affinity than eplerenone in vitro,” is in phase III trials for the treatment of systolic and diastolic dysfunction and reduction of morbidity and mortality associated with heart failure.2 One study has already demonstrated that finerenone (5 to 10 mg/d) is at least as effective as spironolactone (25 mg/d) for heart failure patients.3
The Mineralocorticoid Receptor Antagonist Tolerability Study-Diabetic Nephropathy (ARTS-DN) found that finerenone at 10 to 20 mg/d was superior to spironolactone and eplerenone, partly due to the decreased incidence of hyperkalemia. However, it should be noted that the lower incidence of hyperkalemia may be attributable to the fact that 66% of the study participants had an estimated glomerular filtration rate (eGFR) greater than 60 mL/min and that potential participants with a serum potassium level of more than 4.8 mEq/L were not included in the study.2
Additional research is needed to confirm superiority of finerenone over spironolactone and eplerenone, in conjunction with RAAS blockers, in the treatment of albuminuria and hyperkalemia. Including subjects with lower eGFR (such as patients with stage IV CKD who are at higher risk for hyperkalemia) would give a better indication of finerenone’s efficacy. In the meantime, it’s probably too soon to corner the market on this stock! —SEB
Susan E. Brown, MS, ARNP, ACNP-BC, CCRN
Great River Nephrology, West Burlington, Iowa
References
1. Parikh SV, Haddad NJ, Hebert LA. Retarding progression of kidney disease. In: Johnson RJ, Feehally J, Floege J, eds. Comprehensive Clinical Nephrology. 5th ed. Philadelphia, PA: Saunders; 2015:931-940.
2. Bakris GL, Agarwal R, Chan JC, et al. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314(9):884-894.
3. Kolkhof P, Delbeck M, Kretschmer A, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist, protects from rat cardiorenal injury. J Cardiovasc Pharmacol. 2014;64(1):69-78.
Q) One of my diabetic patients read about finerenone in The New York Times. Apparently, it’s the “newest cure for albuminuria”! Is this just hype, or do the trials on this medication really show progress against kidney disease? Should I buy stock in the company?
Albuminuria (> 500 mg/d) associated with diabetic nephropathy and other glomerular diseases increases patient risk for chronic kidney disease (CKD) and its progression to end-stage renal disease (ESRD). Reduction of albuminuria has been shown to slow the progression of CKD.
Renin-angiotensin-aldosterone system (RAAS) blockers, such as ACE inhibitors or angiotensin receptor blockers, are considered firstline therapy to reduce albuminuria. Additional treatment modalities include diuretics, nondihydropyridine calcium channel blockers, ß-blockers, and aldosterone antagonist therapy. Limiting dietary sodium helps control blood pressure, thus slowing disease progression. In addition, some studies show that limiting phosphorus and protein (for the latter, intake of no more than 0.7 g/kg ideal body weight per day) may slow the progression of CKD. Unfortunately, despite these interventions, patients may still advance to ESRD.1
The aldosterone and steroidal mineralocorticoid receptor antagonists (MRA) spironolactone and eplerenone have been found to reduce albuminuria when used in conjunction with RAAS blockade. However, patients using this combination are up to eight times more likely to experience hyperkalemia—a serious, potentially life-threatening adverse condition—than those not using an MRA.2 The presence of hyperkalemia requires discontinuation of the RAAS blocker and the MRA, at least temporarily.
Finerenone, a nonsteroidal MRA with “greater receptor selectivity than spironolactone and better receptor affinity than eplerenone in vitro,” is in phase III trials for the treatment of systolic and diastolic dysfunction and reduction of morbidity and mortality associated with heart failure.2 One study has already demonstrated that finerenone (5 to 10 mg/d) is at least as effective as spironolactone (25 mg/d) for heart failure patients.3
The Mineralocorticoid Receptor Antagonist Tolerability Study-Diabetic Nephropathy (ARTS-DN) found that finerenone at 10 to 20 mg/d was superior to spironolactone and eplerenone, partly due to the decreased incidence of hyperkalemia. However, it should be noted that the lower incidence of hyperkalemia may be attributable to the fact that 66% of the study participants had an estimated glomerular filtration rate (eGFR) greater than 60 mL/min and that potential participants with a serum potassium level of more than 4.8 mEq/L were not included in the study.2
Additional research is needed to confirm superiority of finerenone over spironolactone and eplerenone, in conjunction with RAAS blockers, in the treatment of albuminuria and hyperkalemia. Including subjects with lower eGFR (such as patients with stage IV CKD who are at higher risk for hyperkalemia) would give a better indication of finerenone’s efficacy. In the meantime, it’s probably too soon to corner the market on this stock! —SEB
Susan E. Brown, MS, ARNP, ACNP-BC, CCRN
Great River Nephrology, West Burlington, Iowa
References
1. Parikh SV, Haddad NJ, Hebert LA. Retarding progression of kidney disease. In: Johnson RJ, Feehally J, Floege J, eds. Comprehensive Clinical Nephrology. 5th ed. Philadelphia, PA: Saunders; 2015:931-940.
2. Bakris GL, Agarwal R, Chan JC, et al. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314(9):884-894.
3. Kolkhof P, Delbeck M, Kretschmer A, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist, protects from rat cardiorenal injury. J Cardiovasc Pharmacol. 2014;64(1):69-78.
Nutrition Guidelines for CKD
Q) I see patients with diabetes, hypertension, chronic kidney disease (CKD), obesity ... often all within the same patient! I keep hearing that the DASH diet is best for these patients. Is this true? Do you have any suggestions (or handouts) for teaching good eating habits in a 15-minute office visit?
It is always nice to focus on what patients can do, rather than what they can’t. Patients with diabetes, kidney disease, heart disease, and obesity hear a lot of “can’t” messages, making “can” messages particularly important to emphasize.
Healthy diets for diabetes, heart, and kidney patients include foods low in trans and saturated fats and sodium. Not all CKD patients are required to follow a low-potassium diet; dietary restrictions are based on laboratory values, medications, and other factors. As we know, adding an ACE inhibitor or an angiotensin receptor blocker (ARB) to the treatment regimen can cause an elevation in serum potassium.
For adults with CKD, it is recommended that sodium intake be restricted to < 2,000 mg/d.4 And in this population, salt substitutes are not recommended, since they often contain large amounts of potassium chloride, which increases risk for hyperkalemia.5 Other spices (eg, garlic, pepper, lemon) are better substitutes for salt.
The late Paul Prudhomme, an award-winning chef from New Orleans, struggled with obesity and health issues for years. He developed wonderful, kidney-friendly spices free of salt and potassium. His line of spices, Magic Seasoning Blends, is sold in many grocery stores. You can recommend them without worry.
Studies have shown that the usual Western diet (which features an abundance of processed foods, fats, and sugars) contributes to kidney disease.6 The DASH (Dietary Approaches to Stop Hypertension) diet, developed by cardio experts, replaces these foods with healthier alternatives.
Recent research has shown that the DASH diet does, in fact, slow the progression of kidney disease.7 It also lowers blood pressure and decreases kidney stone formation, which are risk factors for kidney disease.
So, the DASH diet is protective for your patients (from both a kidney and a cardiac standpoint)—but how do you explain this in a 15-minute office visit?
Here are a few quick tips:
• Increase fruit and vegetable intake to include all colors on your plate (and no, tan is not really a color)
• If you eat meat, the cooking method should start with “B” (ie, bake, boil, broil, barbeque [without salty sauce]) ... Note that “fried” does not start with “B”!
• Use a smaller plate and you will not eat as much
• Use technology in your favor. There are great apps and downloads you can recommend (see Table). —CC
Christine Corbett, MSN, APRN, FNP-BC, CNN-NP
Kansas City Veterans Affairs, Kansas City, Missouri
References
4. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;(3):1-150.
5. National Kidney Disease Education Program. Potassium: tips for people with chronic kidney disease (CKD). www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/nutrition-potassium/Documents/nutrition-potassium-508.pdf. Accessed June 20, 2016.
6. Odermatt A. The Western-style diet: a major risk factor for impaired kidney function and chronic kidney disease. Am J Physiol Renal Physiol. 2011;301(5):F919-F931.
7. Steiber A. DASH-style diet effective in preventing, delaying CKD progression. Renal and Urology News. 2012.
Q) I see patients with diabetes, hypertension, chronic kidney disease (CKD), obesity ... often all within the same patient! I keep hearing that the DASH diet is best for these patients. Is this true? Do you have any suggestions (or handouts) for teaching good eating habits in a 15-minute office visit?
It is always nice to focus on what patients can do, rather than what they can’t. Patients with diabetes, kidney disease, heart disease, and obesity hear a lot of “can’t” messages, making “can” messages particularly important to emphasize.
Healthy diets for diabetes, heart, and kidney patients include foods low in trans and saturated fats and sodium. Not all CKD patients are required to follow a low-potassium diet; dietary restrictions are based on laboratory values, medications, and other factors. As we know, adding an ACE inhibitor or an angiotensin receptor blocker (ARB) to the treatment regimen can cause an elevation in serum potassium.
For adults with CKD, it is recommended that sodium intake be restricted to < 2,000 mg/d.4 And in this population, salt substitutes are not recommended, since they often contain large amounts of potassium chloride, which increases risk for hyperkalemia.5 Other spices (eg, garlic, pepper, lemon) are better substitutes for salt.
The late Paul Prudhomme, an award-winning chef from New Orleans, struggled with obesity and health issues for years. He developed wonderful, kidney-friendly spices free of salt and potassium. His line of spices, Magic Seasoning Blends, is sold in many grocery stores. You can recommend them without worry.
Studies have shown that the usual Western diet (which features an abundance of processed foods, fats, and sugars) contributes to kidney disease.6 The DASH (Dietary Approaches to Stop Hypertension) diet, developed by cardio experts, replaces these foods with healthier alternatives.
Recent research has shown that the DASH diet does, in fact, slow the progression of kidney disease.7 It also lowers blood pressure and decreases kidney stone formation, which are risk factors for kidney disease.
So, the DASH diet is protective for your patients (from both a kidney and a cardiac standpoint)—but how do you explain this in a 15-minute office visit?
Here are a few quick tips:
• Increase fruit and vegetable intake to include all colors on your plate (and no, tan is not really a color)
• If you eat meat, the cooking method should start with “B” (ie, bake, boil, broil, barbeque [without salty sauce]) ... Note that “fried” does not start with “B”!
• Use a smaller plate and you will not eat as much
• Use technology in your favor. There are great apps and downloads you can recommend (see Table). —CC
Christine Corbett, MSN, APRN, FNP-BC, CNN-NP
Kansas City Veterans Affairs, Kansas City, Missouri
References
4. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;(3):1-150.
5. National Kidney Disease Education Program. Potassium: tips for people with chronic kidney disease (CKD). www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/nutrition-potassium/Documents/nutrition-potassium-508.pdf. Accessed June 20, 2016.
6. Odermatt A. The Western-style diet: a major risk factor for impaired kidney function and chronic kidney disease. Am J Physiol Renal Physiol. 2011;301(5):F919-F931.
7. Steiber A. DASH-style diet effective in preventing, delaying CKD progression. Renal and Urology News. 2012.
Q) I see patients with diabetes, hypertension, chronic kidney disease (CKD), obesity ... often all within the same patient! I keep hearing that the DASH diet is best for these patients. Is this true? Do you have any suggestions (or handouts) for teaching good eating habits in a 15-minute office visit?
It is always nice to focus on what patients can do, rather than what they can’t. Patients with diabetes, kidney disease, heart disease, and obesity hear a lot of “can’t” messages, making “can” messages particularly important to emphasize.
Healthy diets for diabetes, heart, and kidney patients include foods low in trans and saturated fats and sodium. Not all CKD patients are required to follow a low-potassium diet; dietary restrictions are based on laboratory values, medications, and other factors. As we know, adding an ACE inhibitor or an angiotensin receptor blocker (ARB) to the treatment regimen can cause an elevation in serum potassium.
For adults with CKD, it is recommended that sodium intake be restricted to < 2,000 mg/d.4 And in this population, salt substitutes are not recommended, since they often contain large amounts of potassium chloride, which increases risk for hyperkalemia.5 Other spices (eg, garlic, pepper, lemon) are better substitutes for salt.
The late Paul Prudhomme, an award-winning chef from New Orleans, struggled with obesity and health issues for years. He developed wonderful, kidney-friendly spices free of salt and potassium. His line of spices, Magic Seasoning Blends, is sold in many grocery stores. You can recommend them without worry.
Studies have shown that the usual Western diet (which features an abundance of processed foods, fats, and sugars) contributes to kidney disease.6 The DASH (Dietary Approaches to Stop Hypertension) diet, developed by cardio experts, replaces these foods with healthier alternatives.
Recent research has shown that the DASH diet does, in fact, slow the progression of kidney disease.7 It also lowers blood pressure and decreases kidney stone formation, which are risk factors for kidney disease.
So, the DASH diet is protective for your patients (from both a kidney and a cardiac standpoint)—but how do you explain this in a 15-minute office visit?
Here are a few quick tips:
• Increase fruit and vegetable intake to include all colors on your plate (and no, tan is not really a color)
• If you eat meat, the cooking method should start with “B” (ie, bake, boil, broil, barbeque [without salty sauce]) ... Note that “fried” does not start with “B”!
• Use a smaller plate and you will not eat as much
• Use technology in your favor. There are great apps and downloads you can recommend (see Table). —CC
Christine Corbett, MSN, APRN, FNP-BC, CNN-NP
Kansas City Veterans Affairs, Kansas City, Missouri
References
4. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;(3):1-150.
5. National Kidney Disease Education Program. Potassium: tips for people with chronic kidney disease (CKD). www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/nutrition-potassium/Documents/nutrition-potassium-508.pdf. Accessed June 20, 2016.
6. Odermatt A. The Western-style diet: a major risk factor for impaired kidney function and chronic kidney disease. Am J Physiol Renal Physiol. 2011;301(5):F919-F931.
7. Steiber A. DASH-style diet effective in preventing, delaying CKD progression. Renal and Urology News. 2012.
Lipoprotein(a) and Cardiovascular Disease
Cardiovascular disease (CVD) is the leading cause of death in the United States. CVD-related diseases affect 83.6 million people in the US and are responsible for almost 800,000 deaths annually.1 The myriad underlying causes for these disorders range from inadequate lifestyle management to genetic abnormalities. One genetically determined abnormality is lipoprotein(a), or Lp(a).2-4
It is estimated that 25% of the US population has elevated Lp(a) levels (> 30 mg/dL) that are clinically significant.5 Lp(a) is recognized as an independent risk factor for CVD, stroke, retinal artery occlusions, and restenosis of vein grafts.2-5
Regardless of practice type, clinicians at some point in their career will see a “vasculopath.” Many of these patients have undiagnosed familial hypercholesterolemia, which affects 1 in 200 to 300 patients in the US and manifests with LDL cholesterol (LDL-C) levels ≥ 190 mg/dL.6-8 Other patients may have CVD with relatively “normal” traditional lipids, more aggressive premature disease, and/or progressive disease despite “usual therapy.”
As clinical lipid specialists working both in cardiology and endocrinology, the authors find the lack of evaluation for additional abnormalities in high-risk patients to be quite disturbing. The patient most commonly seen with the Lp(a) abnormality is one with CVD onset approximately one decade earlier than expected, along with a family history of premature CVD or closure of recently placed stents. Unfortunately, this may result in disease in the second or third decade for men and third or fourth decade for women.
Of course, CVD can leave patients with less productive lives and increase the burden to the health care system and to society. A positive outcome of identification of this apolipoprotein abnormality is that it may prompt evaluation of other family members prior to the inception of vascular disease. When it is identified in the asymptomatic, disease-free patient, aggressive risk reduction—in the form of lifestyle management and medication—may delay or prevent disease onset.
Continue for identification of the problem >>
Identification of the problem
Office visits seldom include a thorough and complete patient history. A “good” family history should include first-degree relatives. Time-constrained practitioners may take a rudimentary family history of immediate relatives when a pedigree of the patient would be more appropriate.
Pedigree assessment offers a more specific picture of disease in families and identifies prevalence and incidence. Busy clinicians could have patients use an online resource to generate their own family pedigree. Or, as in most practices, a medical assistant or other appropriate office staff could initiate the process in the chart.
Patients with premature or advanced disease and significant family history need further investigation. A suspect history would include multiple family members with disease earlier in life than expected and perhaps early cardiovascular death. The personal history of the patient may include multiple cardiovascular incidents despite therapeutic intervention; despite taking lipid-lowering and/or antiplatelet therapy, the patient will present with progressive disease. Often, disease manifests in multiple areas of the vasculature or as restenosis of previous interventions.
Genetics
Lp(a) results from a genetic variation of the apolipoprotein(a) (LPA) locus on chromosome 6q27. Lp(a) is comprised of an apolipoprotein(b) (apoB)–containing LDL molecule that is bonded to LPA. LPA is structurally similar to plasminogen, the precursor for plasmin that degrades fibrin in blood clots. Due to this similarity, LPA can competitively inhibit plasmin activity and thereby increase risk for thrombosis.4,9
Continue for physical examination >>
Physical Examination
Patients with very elevated LDL-C levels in whom Lp(a) is also high may present with other outward stigmata of dyslipidemia. Visualization of the eye may reveal evidence of severe dyslipidemia with arcus cornea. This arcus can present as unilateral, bilateral, inferior, superior, or mixed and is representative of the buildup of cholesterol that cannot be removed from the body by normal means. Further examination may reveal tendon xanthomas, which are also representative of a genetic cholesterol disorder—in most cases, familial hypercholesterolemia.7
Laboratory Workup
In patients who are known or suspected to be at high risk for CVD, the laboratory workup should include a fasting lipid panel, with Lp(a) and apoB; a comprehensive metabolic profile to establish renal and liver function (as therapeutic interventions utilize these organs for metabolism); and a fasting glucose measurement to rule out occult diabetes, which enhances risk factors. Thyroid function is also assessed, secondary to its deleterious effects on lipid metabolism.
Lp(a) results must be interpreted in the context of ethnicity; significance will vary. For example, both the African-American and Asian populations have been found to have high levels of Lp(a), but these are generally felt to be less atherogenic in African Americans. No major differences have been identified for other populations. It is, however, important to note that those patients with nephropathies and elevated Lp(a) carry a higher risk for coronary artery disease.
Lp(a) levels will remain relatively steady throughout life, negating the need for routine monitoring once a patient’s levels have been established. The exception is postmenopausal women, in whom Lp(a) levels may increase due to changes in estrogen. It is prudent to assess Lp(a) in women both pre- and postmenopause, based on data from the Women’s Health Study.10
Continue for diagnosis and treatment >>
Diagnosis and Treatment
Elevated Lp(a), which is found in 25% to 35% of the population, is diagnosed at a level > 30 mg/dL, regardless of sex.4,9 In conjunction with known disease, elevated Lp(a) is sufficient to warrant consideration of very aggressive treatment. In these circumstances, the provider may consider a target LDL-C level ≤ 70 mg/dL.6,7,11 In primary prevention, clinicians should consider lowering this threshold. Levels that may have been considered appropriate in a low- or moderate-risk patient (≤ 160 mg/dL and ≤ 130 mg/dL, respectively) may be reduced to ≤ 130 mg/dL and ≤ 100 mg/dL, respectively.6,11
There is no peer-reviewed evidence with regard to lifestyle management (exercise and diet) for reduction of Lp(a). However, it is reasonable to recommend that high-risk patients adopt healthier regimens.
Management of elevated Lp(a) includes consideration of pharmacologic intervention. Since Lp(a) is prothrombotic, all patients without contraindications should at least be taking low-dose (81-mg) aspirin. Those with evidence of thrombotic events may need lifetime antiplatelet therapy.12 Statin therapy has mixed and minimal effects on Lp(a), although it remains the mainstay of treatment due to its effects on LDL-C and other lipoproteins.13 Although long-term data are lacking, there is some anecdotal evidence of improvement with fibrate therapy. However, it is not recommended for treatment of elevated Lp(a).14
Nicotinic acid has had the longest and most robust history for reduction of Lp(a).9,12 However, recent studies examining combination therapy with statins and nicotinic acid have yielded discouraging results—and in some cases have suggested negative outcomes with this combination.15,16 High doses (4-5 g for immediate release and 2-3 g for sustained release) of nicotinic acid are necessary to produce beneficial results on Lp(a) or other lipid abnormalities (eg, elevated triglycerides, low HDL cholesterol).17 Use of OTC nicotinic acid is not recommended, since these products are considered dietary supplements and regulated as such, raising the potential for untoward adverse effects and/or the possibility that little to no active ingredient is present.18-20
Results from the Women’s Health Study and the Heart and Estrogen/progestin Replacement Study suggested that estrogen might be an effective therapy. In one analysis, women with elevated Lp(a) derived greater potential cardioprotective effects from hormone replacement therapy (HRT) than those with lower Lp(a), and the researchers noted a “significant interaction” between baseline Lp(a), HRT treatment, and CVD risk. However, use of HRT is not approved for treatment of vascular risk today, due to the potential for adverse effects.10,21
A novel therapy, in the form of PCSK9 inhibition, has been shown to reduce LDL-C significantly; reduction in Lp(a) was also observed. The FDA recently approved two PCSK9 inhibitors (alirocumab and evolocumab) for use, although the primary indication is for further reduction in LDL-C on top of the maximally tolerated dose of statin therapy, not for reduction of Lp(a).22,23
Apheresis has been shown to have positive effects in reducing ongoing vascular events in select patient populations. It is approved by the FDA for treatment of refractory LDL-C, mostly in patients with familial hypercholesterolemia, but it is not indicated for treatment of elevated Lp(a). However, since Lp(a) tracks with LDL-C, it is also removed during the process; about a 50% reduction in Lp(a) levels has been noted, although levels rebound posttreatment. To date, reimbursement issues remain in the absence of an FDA indication and due to the paucity of treatment centers in the US.24,25
Follow-up. The therapies mentioned require routine evaluation to assess tolerability and safety, as recommended in the prescribing information. Patients with known CVD should undergo an appropriate cardiac workup annually to evaluate for occult progression of disease. Patients require further evaluation of related cardiovascular risk factors and adherence with medication regimens. For primary prevention patients, annual follow-up is also recommended to assess for any changes in health status, lifestyle, or medication adherence.
Continue for conclusion >>
Conclusion
The average health care provider frequently performs the standard evaluation of a patient at risk for, or with, CVD. However, a subset of this population may be at increased cardiovascular risk due to Lp(a), a common genetic risk factor that can be responsible for premature or progressive CVD. Because of the aggressive nature of this disorder and the young age at which it influences the development of vascular disease, health care providers must be more vigilant about looking beyond the obvious in patients with familial hypercholesterolemia or family history of premature CVD.
Patients with progressive disease must be more thoroughly evaluated; there are already more than 63 million persons with elevated Lp(a) in the US—and many more undiagnosed—who may benefit from aggressive care. Underdiagnosis has been associated with decreased quality and productivity in the work environment, decreased quality of life, increased use of health dollars, and possibly early loss of life.
While the test for Lp(a) is readily available, the cost may not be covered by insurance and therefore may be passed on to the patient. It would behoove health care professionals to lobby for coverage as a means to reduce the prevalence of CVD, the number one cause of mortality in the US.
References
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive Summary: heart disease and stroke statistics—2014 Update: a report from the American Heart Association. Circulation. 2014;129:399-410.
2. Bennet A, Di Angelantonio E, Erqou S, et al. Lipoprotein(a) levels and risk of future coronary heart disease: large-scale prospective data [published corrections appear in Arch Intern Med. 2008;168(10):1089 and Arch Intern Med. 2008;168(10):1096]. Arch Intern Med. 2008;168(6):598-608.
3. Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301(22):2331-2339.
4. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), hormone replacement therapy, and risk of future cardiovascular events. J Am Coll Cardiol. 2008;52(2):124-131.
5. Scanu AM. Lipoprotein(a). A genetic risk factor for premature coronary heart disease. JAMA. 1992;267(24):3326-3329.
6. Goldberg AC, Hopkins PN, Toth PP; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S1-S8.
7. Ito M, McGowan MP, Moriarty PM; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Management of familial hypercholesterolemias in adult patients: recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S38-S45.
8. Sjouke B, Kusters DM, Kindt I, et al. Homozygous autosomal dominant hypercholesterolaemia in the Netherlands: prevalence, genotype-phenotype relationship, and clinical outcome. Eur Heart J. 2014 Feb 28. [Epub ahead of print]
9. Nordestgaard BG, Chapman MJ, Ray K, et al; European Atherosclerosis Society Consensus Panel. Lipoprotein (a) as a cardiovascular risk factor: current status. Eur Heart J. 2010; 31(23):2844-2853.
10. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), measured with an assay independent of apolipoprotein(a) isoform size, and risk of future cardiovascular events among initially healthy women. JAMA. 2006;296 (11):1363-1370.
11. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227-239.
12. Jacobson TA. Lipoprotein (a), cardiovascular disease, and contemporary management. Mayo Clin Proc. 2013;88(11):1294-1311.
13. Hunninghake DB, Stein EA, Mellies MJ. Effects of one year of treatment with pravastatin, an HMG-CoA reductase inhibitor, on lipoprotein a. J Clin Pharmacol. 1993;33 (6):574-580.
14. Jones PH, Pownall HJ, Patsch W, et al. Effect of gemfibrozil on levels of lipoprotein[a] in type 2 hyperlipoproteinemic subjects. J Lipid Res. 1996;37(6):1298-1308.
15. Boden WE, Probstfield JL, Anderson T, et al; AIM-HIGH investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365(24):2255-2267.
16. Landray MJ, Haynes R, Hopewell JC, et al; HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371 (3):203-212.
17. Morgan JM, Capuzzi DM, Guyton JR. A new extended-release niacin (Niaspan): efficacy, tolerability, and safety in hypercholesterolemic patients. Am J Cardiol. 1998;82 (12A): 29U-34U.
18. Piepho RW. The pharmacokinetics and pharmacodynamics of agents proven to raise high-density lipoprotein cholesterol. Am J Cardiol. 2000;86(12A):35L-40L.
19. Guyton JR, Bays HE. Safety considerations with niacin therapy. Am J Cardiol. 2007; 99(6A):22C-31C.
20. McKenney JM, Proctor JD, Harris S, Chinchili VM. A comparison of the efficacy and toxic effects of sustained- vs immediate-release niacin in hypercholesterolemic patients. JAMA. 1994;271(9):672-677.
21. Shlipak MG, Simon JA, Vittinghoff E, et al. Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA. 2000;283 (14):1845-1852.
22. Marbach JA, McKeon JL, Ross JL, Duffy D. Novel treatments for familial hypercholesterolemia: pharmacogenetics at work. Pharmacotherapy. 2014;34(9):961-972.
23. Stein EA, Mellis S, Yancopoulos GD, et al. Effect of a monoclonal antibody to PCSK9 on LDL cholesterol. N Engl J Med. 2012;366(12): 1108-1118.
24. Sachais BS, Katz J, Ross J, Rader DJ. Long-term effects of LDL apheresis in patients with severe hypercholesterolemia. J Clin Apher. 2005;20:252-255.
25. Waldmann E, Parhofer K. Lipoprotein apheresis to treat elevated lipoprotein(a). J Lipid Res. 2016 Feb 17. [Epub ahead of print]
Cardiovascular disease (CVD) is the leading cause of death in the United States. CVD-related diseases affect 83.6 million people in the US and are responsible for almost 800,000 deaths annually.1 The myriad underlying causes for these disorders range from inadequate lifestyle management to genetic abnormalities. One genetically determined abnormality is lipoprotein(a), or Lp(a).2-4
It is estimated that 25% of the US population has elevated Lp(a) levels (> 30 mg/dL) that are clinically significant.5 Lp(a) is recognized as an independent risk factor for CVD, stroke, retinal artery occlusions, and restenosis of vein grafts.2-5
Regardless of practice type, clinicians at some point in their career will see a “vasculopath.” Many of these patients have undiagnosed familial hypercholesterolemia, which affects 1 in 200 to 300 patients in the US and manifests with LDL cholesterol (LDL-C) levels ≥ 190 mg/dL.6-8 Other patients may have CVD with relatively “normal” traditional lipids, more aggressive premature disease, and/or progressive disease despite “usual therapy.”
As clinical lipid specialists working both in cardiology and endocrinology, the authors find the lack of evaluation for additional abnormalities in high-risk patients to be quite disturbing. The patient most commonly seen with the Lp(a) abnormality is one with CVD onset approximately one decade earlier than expected, along with a family history of premature CVD or closure of recently placed stents. Unfortunately, this may result in disease in the second or third decade for men and third or fourth decade for women.
Of course, CVD can leave patients with less productive lives and increase the burden to the health care system and to society. A positive outcome of identification of this apolipoprotein abnormality is that it may prompt evaluation of other family members prior to the inception of vascular disease. When it is identified in the asymptomatic, disease-free patient, aggressive risk reduction—in the form of lifestyle management and medication—may delay or prevent disease onset.
Continue for identification of the problem >>
Identification of the problem
Office visits seldom include a thorough and complete patient history. A “good” family history should include first-degree relatives. Time-constrained practitioners may take a rudimentary family history of immediate relatives when a pedigree of the patient would be more appropriate.
Pedigree assessment offers a more specific picture of disease in families and identifies prevalence and incidence. Busy clinicians could have patients use an online resource to generate their own family pedigree. Or, as in most practices, a medical assistant or other appropriate office staff could initiate the process in the chart.
Patients with premature or advanced disease and significant family history need further investigation. A suspect history would include multiple family members with disease earlier in life than expected and perhaps early cardiovascular death. The personal history of the patient may include multiple cardiovascular incidents despite therapeutic intervention; despite taking lipid-lowering and/or antiplatelet therapy, the patient will present with progressive disease. Often, disease manifests in multiple areas of the vasculature or as restenosis of previous interventions.
Genetics
Lp(a) results from a genetic variation of the apolipoprotein(a) (LPA) locus on chromosome 6q27. Lp(a) is comprised of an apolipoprotein(b) (apoB)–containing LDL molecule that is bonded to LPA. LPA is structurally similar to plasminogen, the precursor for plasmin that degrades fibrin in blood clots. Due to this similarity, LPA can competitively inhibit plasmin activity and thereby increase risk for thrombosis.4,9
Continue for physical examination >>
Physical Examination
Patients with very elevated LDL-C levels in whom Lp(a) is also high may present with other outward stigmata of dyslipidemia. Visualization of the eye may reveal evidence of severe dyslipidemia with arcus cornea. This arcus can present as unilateral, bilateral, inferior, superior, or mixed and is representative of the buildup of cholesterol that cannot be removed from the body by normal means. Further examination may reveal tendon xanthomas, which are also representative of a genetic cholesterol disorder—in most cases, familial hypercholesterolemia.7
Laboratory Workup
In patients who are known or suspected to be at high risk for CVD, the laboratory workup should include a fasting lipid panel, with Lp(a) and apoB; a comprehensive metabolic profile to establish renal and liver function (as therapeutic interventions utilize these organs for metabolism); and a fasting glucose measurement to rule out occult diabetes, which enhances risk factors. Thyroid function is also assessed, secondary to its deleterious effects on lipid metabolism.
Lp(a) results must be interpreted in the context of ethnicity; significance will vary. For example, both the African-American and Asian populations have been found to have high levels of Lp(a), but these are generally felt to be less atherogenic in African Americans. No major differences have been identified for other populations. It is, however, important to note that those patients with nephropathies and elevated Lp(a) carry a higher risk for coronary artery disease.
Lp(a) levels will remain relatively steady throughout life, negating the need for routine monitoring once a patient’s levels have been established. The exception is postmenopausal women, in whom Lp(a) levels may increase due to changes in estrogen. It is prudent to assess Lp(a) in women both pre- and postmenopause, based on data from the Women’s Health Study.10
Continue for diagnosis and treatment >>
Diagnosis and Treatment
Elevated Lp(a), which is found in 25% to 35% of the population, is diagnosed at a level > 30 mg/dL, regardless of sex.4,9 In conjunction with known disease, elevated Lp(a) is sufficient to warrant consideration of very aggressive treatment. In these circumstances, the provider may consider a target LDL-C level ≤ 70 mg/dL.6,7,11 In primary prevention, clinicians should consider lowering this threshold. Levels that may have been considered appropriate in a low- or moderate-risk patient (≤ 160 mg/dL and ≤ 130 mg/dL, respectively) may be reduced to ≤ 130 mg/dL and ≤ 100 mg/dL, respectively.6,11
There is no peer-reviewed evidence with regard to lifestyle management (exercise and diet) for reduction of Lp(a). However, it is reasonable to recommend that high-risk patients adopt healthier regimens.
Management of elevated Lp(a) includes consideration of pharmacologic intervention. Since Lp(a) is prothrombotic, all patients without contraindications should at least be taking low-dose (81-mg) aspirin. Those with evidence of thrombotic events may need lifetime antiplatelet therapy.12 Statin therapy has mixed and minimal effects on Lp(a), although it remains the mainstay of treatment due to its effects on LDL-C and other lipoproteins.13 Although long-term data are lacking, there is some anecdotal evidence of improvement with fibrate therapy. However, it is not recommended for treatment of elevated Lp(a).14
Nicotinic acid has had the longest and most robust history for reduction of Lp(a).9,12 However, recent studies examining combination therapy with statins and nicotinic acid have yielded discouraging results—and in some cases have suggested negative outcomes with this combination.15,16 High doses (4-5 g for immediate release and 2-3 g for sustained release) of nicotinic acid are necessary to produce beneficial results on Lp(a) or other lipid abnormalities (eg, elevated triglycerides, low HDL cholesterol).17 Use of OTC nicotinic acid is not recommended, since these products are considered dietary supplements and regulated as such, raising the potential for untoward adverse effects and/or the possibility that little to no active ingredient is present.18-20
Results from the Women’s Health Study and the Heart and Estrogen/progestin Replacement Study suggested that estrogen might be an effective therapy. In one analysis, women with elevated Lp(a) derived greater potential cardioprotective effects from hormone replacement therapy (HRT) than those with lower Lp(a), and the researchers noted a “significant interaction” between baseline Lp(a), HRT treatment, and CVD risk. However, use of HRT is not approved for treatment of vascular risk today, due to the potential for adverse effects.10,21
A novel therapy, in the form of PCSK9 inhibition, has been shown to reduce LDL-C significantly; reduction in Lp(a) was also observed. The FDA recently approved two PCSK9 inhibitors (alirocumab and evolocumab) for use, although the primary indication is for further reduction in LDL-C on top of the maximally tolerated dose of statin therapy, not for reduction of Lp(a).22,23
Apheresis has been shown to have positive effects in reducing ongoing vascular events in select patient populations. It is approved by the FDA for treatment of refractory LDL-C, mostly in patients with familial hypercholesterolemia, but it is not indicated for treatment of elevated Lp(a). However, since Lp(a) tracks with LDL-C, it is also removed during the process; about a 50% reduction in Lp(a) levels has been noted, although levels rebound posttreatment. To date, reimbursement issues remain in the absence of an FDA indication and due to the paucity of treatment centers in the US.24,25
Follow-up. The therapies mentioned require routine evaluation to assess tolerability and safety, as recommended in the prescribing information. Patients with known CVD should undergo an appropriate cardiac workup annually to evaluate for occult progression of disease. Patients require further evaluation of related cardiovascular risk factors and adherence with medication regimens. For primary prevention patients, annual follow-up is also recommended to assess for any changes in health status, lifestyle, or medication adherence.
Continue for conclusion >>
Conclusion
The average health care provider frequently performs the standard evaluation of a patient at risk for, or with, CVD. However, a subset of this population may be at increased cardiovascular risk due to Lp(a), a common genetic risk factor that can be responsible for premature or progressive CVD. Because of the aggressive nature of this disorder and the young age at which it influences the development of vascular disease, health care providers must be more vigilant about looking beyond the obvious in patients with familial hypercholesterolemia or family history of premature CVD.
Patients with progressive disease must be more thoroughly evaluated; there are already more than 63 million persons with elevated Lp(a) in the US—and many more undiagnosed—who may benefit from aggressive care. Underdiagnosis has been associated with decreased quality and productivity in the work environment, decreased quality of life, increased use of health dollars, and possibly early loss of life.
While the test for Lp(a) is readily available, the cost may not be covered by insurance and therefore may be passed on to the patient. It would behoove health care professionals to lobby for coverage as a means to reduce the prevalence of CVD, the number one cause of mortality in the US.
References
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive Summary: heart disease and stroke statistics—2014 Update: a report from the American Heart Association. Circulation. 2014;129:399-410.
2. Bennet A, Di Angelantonio E, Erqou S, et al. Lipoprotein(a) levels and risk of future coronary heart disease: large-scale prospective data [published corrections appear in Arch Intern Med. 2008;168(10):1089 and Arch Intern Med. 2008;168(10):1096]. Arch Intern Med. 2008;168(6):598-608.
3. Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301(22):2331-2339.
4. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), hormone replacement therapy, and risk of future cardiovascular events. J Am Coll Cardiol. 2008;52(2):124-131.
5. Scanu AM. Lipoprotein(a). A genetic risk factor for premature coronary heart disease. JAMA. 1992;267(24):3326-3329.
6. Goldberg AC, Hopkins PN, Toth PP; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S1-S8.
7. Ito M, McGowan MP, Moriarty PM; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Management of familial hypercholesterolemias in adult patients: recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S38-S45.
8. Sjouke B, Kusters DM, Kindt I, et al. Homozygous autosomal dominant hypercholesterolaemia in the Netherlands: prevalence, genotype-phenotype relationship, and clinical outcome. Eur Heart J. 2014 Feb 28. [Epub ahead of print]
9. Nordestgaard BG, Chapman MJ, Ray K, et al; European Atherosclerosis Society Consensus Panel. Lipoprotein (a) as a cardiovascular risk factor: current status. Eur Heart J. 2010; 31(23):2844-2853.
10. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), measured with an assay independent of apolipoprotein(a) isoform size, and risk of future cardiovascular events among initially healthy women. JAMA. 2006;296 (11):1363-1370.
11. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227-239.
12. Jacobson TA. Lipoprotein (a), cardiovascular disease, and contemporary management. Mayo Clin Proc. 2013;88(11):1294-1311.
13. Hunninghake DB, Stein EA, Mellies MJ. Effects of one year of treatment with pravastatin, an HMG-CoA reductase inhibitor, on lipoprotein a. J Clin Pharmacol. 1993;33 (6):574-580.
14. Jones PH, Pownall HJ, Patsch W, et al. Effect of gemfibrozil on levels of lipoprotein[a] in type 2 hyperlipoproteinemic subjects. J Lipid Res. 1996;37(6):1298-1308.
15. Boden WE, Probstfield JL, Anderson T, et al; AIM-HIGH investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365(24):2255-2267.
16. Landray MJ, Haynes R, Hopewell JC, et al; HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371 (3):203-212.
17. Morgan JM, Capuzzi DM, Guyton JR. A new extended-release niacin (Niaspan): efficacy, tolerability, and safety in hypercholesterolemic patients. Am J Cardiol. 1998;82 (12A): 29U-34U.
18. Piepho RW. The pharmacokinetics and pharmacodynamics of agents proven to raise high-density lipoprotein cholesterol. Am J Cardiol. 2000;86(12A):35L-40L.
19. Guyton JR, Bays HE. Safety considerations with niacin therapy. Am J Cardiol. 2007; 99(6A):22C-31C.
20. McKenney JM, Proctor JD, Harris S, Chinchili VM. A comparison of the efficacy and toxic effects of sustained- vs immediate-release niacin in hypercholesterolemic patients. JAMA. 1994;271(9):672-677.
21. Shlipak MG, Simon JA, Vittinghoff E, et al. Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA. 2000;283 (14):1845-1852.
22. Marbach JA, McKeon JL, Ross JL, Duffy D. Novel treatments for familial hypercholesterolemia: pharmacogenetics at work. Pharmacotherapy. 2014;34(9):961-972.
23. Stein EA, Mellis S, Yancopoulos GD, et al. Effect of a monoclonal antibody to PCSK9 on LDL cholesterol. N Engl J Med. 2012;366(12): 1108-1118.
24. Sachais BS, Katz J, Ross J, Rader DJ. Long-term effects of LDL apheresis in patients with severe hypercholesterolemia. J Clin Apher. 2005;20:252-255.
25. Waldmann E, Parhofer K. Lipoprotein apheresis to treat elevated lipoprotein(a). J Lipid Res. 2016 Feb 17. [Epub ahead of print]
Cardiovascular disease (CVD) is the leading cause of death in the United States. CVD-related diseases affect 83.6 million people in the US and are responsible for almost 800,000 deaths annually.1 The myriad underlying causes for these disorders range from inadequate lifestyle management to genetic abnormalities. One genetically determined abnormality is lipoprotein(a), or Lp(a).2-4
It is estimated that 25% of the US population has elevated Lp(a) levels (> 30 mg/dL) that are clinically significant.5 Lp(a) is recognized as an independent risk factor for CVD, stroke, retinal artery occlusions, and restenosis of vein grafts.2-5
Regardless of practice type, clinicians at some point in their career will see a “vasculopath.” Many of these patients have undiagnosed familial hypercholesterolemia, which affects 1 in 200 to 300 patients in the US and manifests with LDL cholesterol (LDL-C) levels ≥ 190 mg/dL.6-8 Other patients may have CVD with relatively “normal” traditional lipids, more aggressive premature disease, and/or progressive disease despite “usual therapy.”
As clinical lipid specialists working both in cardiology and endocrinology, the authors find the lack of evaluation for additional abnormalities in high-risk patients to be quite disturbing. The patient most commonly seen with the Lp(a) abnormality is one with CVD onset approximately one decade earlier than expected, along with a family history of premature CVD or closure of recently placed stents. Unfortunately, this may result in disease in the second or third decade for men and third or fourth decade for women.
Of course, CVD can leave patients with less productive lives and increase the burden to the health care system and to society. A positive outcome of identification of this apolipoprotein abnormality is that it may prompt evaluation of other family members prior to the inception of vascular disease. When it is identified in the asymptomatic, disease-free patient, aggressive risk reduction—in the form of lifestyle management and medication—may delay or prevent disease onset.
Continue for identification of the problem >>
Identification of the problem
Office visits seldom include a thorough and complete patient history. A “good” family history should include first-degree relatives. Time-constrained practitioners may take a rudimentary family history of immediate relatives when a pedigree of the patient would be more appropriate.
Pedigree assessment offers a more specific picture of disease in families and identifies prevalence and incidence. Busy clinicians could have patients use an online resource to generate their own family pedigree. Or, as in most practices, a medical assistant or other appropriate office staff could initiate the process in the chart.
Patients with premature or advanced disease and significant family history need further investigation. A suspect history would include multiple family members with disease earlier in life than expected and perhaps early cardiovascular death. The personal history of the patient may include multiple cardiovascular incidents despite therapeutic intervention; despite taking lipid-lowering and/or antiplatelet therapy, the patient will present with progressive disease. Often, disease manifests in multiple areas of the vasculature or as restenosis of previous interventions.
Genetics
Lp(a) results from a genetic variation of the apolipoprotein(a) (LPA) locus on chromosome 6q27. Lp(a) is comprised of an apolipoprotein(b) (apoB)–containing LDL molecule that is bonded to LPA. LPA is structurally similar to plasminogen, the precursor for plasmin that degrades fibrin in blood clots. Due to this similarity, LPA can competitively inhibit plasmin activity and thereby increase risk for thrombosis.4,9
Continue for physical examination >>
Physical Examination
Patients with very elevated LDL-C levels in whom Lp(a) is also high may present with other outward stigmata of dyslipidemia. Visualization of the eye may reveal evidence of severe dyslipidemia with arcus cornea. This arcus can present as unilateral, bilateral, inferior, superior, or mixed and is representative of the buildup of cholesterol that cannot be removed from the body by normal means. Further examination may reveal tendon xanthomas, which are also representative of a genetic cholesterol disorder—in most cases, familial hypercholesterolemia.7
Laboratory Workup
In patients who are known or suspected to be at high risk for CVD, the laboratory workup should include a fasting lipid panel, with Lp(a) and apoB; a comprehensive metabolic profile to establish renal and liver function (as therapeutic interventions utilize these organs for metabolism); and a fasting glucose measurement to rule out occult diabetes, which enhances risk factors. Thyroid function is also assessed, secondary to its deleterious effects on lipid metabolism.
Lp(a) results must be interpreted in the context of ethnicity; significance will vary. For example, both the African-American and Asian populations have been found to have high levels of Lp(a), but these are generally felt to be less atherogenic in African Americans. No major differences have been identified for other populations. It is, however, important to note that those patients with nephropathies and elevated Lp(a) carry a higher risk for coronary artery disease.
Lp(a) levels will remain relatively steady throughout life, negating the need for routine monitoring once a patient’s levels have been established. The exception is postmenopausal women, in whom Lp(a) levels may increase due to changes in estrogen. It is prudent to assess Lp(a) in women both pre- and postmenopause, based on data from the Women’s Health Study.10
Continue for diagnosis and treatment >>
Diagnosis and Treatment
Elevated Lp(a), which is found in 25% to 35% of the population, is diagnosed at a level > 30 mg/dL, regardless of sex.4,9 In conjunction with known disease, elevated Lp(a) is sufficient to warrant consideration of very aggressive treatment. In these circumstances, the provider may consider a target LDL-C level ≤ 70 mg/dL.6,7,11 In primary prevention, clinicians should consider lowering this threshold. Levels that may have been considered appropriate in a low- or moderate-risk patient (≤ 160 mg/dL and ≤ 130 mg/dL, respectively) may be reduced to ≤ 130 mg/dL and ≤ 100 mg/dL, respectively.6,11
There is no peer-reviewed evidence with regard to lifestyle management (exercise and diet) for reduction of Lp(a). However, it is reasonable to recommend that high-risk patients adopt healthier regimens.
Management of elevated Lp(a) includes consideration of pharmacologic intervention. Since Lp(a) is prothrombotic, all patients without contraindications should at least be taking low-dose (81-mg) aspirin. Those with evidence of thrombotic events may need lifetime antiplatelet therapy.12 Statin therapy has mixed and minimal effects on Lp(a), although it remains the mainstay of treatment due to its effects on LDL-C and other lipoproteins.13 Although long-term data are lacking, there is some anecdotal evidence of improvement with fibrate therapy. However, it is not recommended for treatment of elevated Lp(a).14
Nicotinic acid has had the longest and most robust history for reduction of Lp(a).9,12 However, recent studies examining combination therapy with statins and nicotinic acid have yielded discouraging results—and in some cases have suggested negative outcomes with this combination.15,16 High doses (4-5 g for immediate release and 2-3 g for sustained release) of nicotinic acid are necessary to produce beneficial results on Lp(a) or other lipid abnormalities (eg, elevated triglycerides, low HDL cholesterol).17 Use of OTC nicotinic acid is not recommended, since these products are considered dietary supplements and regulated as such, raising the potential for untoward adverse effects and/or the possibility that little to no active ingredient is present.18-20
Results from the Women’s Health Study and the Heart and Estrogen/progestin Replacement Study suggested that estrogen might be an effective therapy. In one analysis, women with elevated Lp(a) derived greater potential cardioprotective effects from hormone replacement therapy (HRT) than those with lower Lp(a), and the researchers noted a “significant interaction” between baseline Lp(a), HRT treatment, and CVD risk. However, use of HRT is not approved for treatment of vascular risk today, due to the potential for adverse effects.10,21
A novel therapy, in the form of PCSK9 inhibition, has been shown to reduce LDL-C significantly; reduction in Lp(a) was also observed. The FDA recently approved two PCSK9 inhibitors (alirocumab and evolocumab) for use, although the primary indication is for further reduction in LDL-C on top of the maximally tolerated dose of statin therapy, not for reduction of Lp(a).22,23
Apheresis has been shown to have positive effects in reducing ongoing vascular events in select patient populations. It is approved by the FDA for treatment of refractory LDL-C, mostly in patients with familial hypercholesterolemia, but it is not indicated for treatment of elevated Lp(a). However, since Lp(a) tracks with LDL-C, it is also removed during the process; about a 50% reduction in Lp(a) levels has been noted, although levels rebound posttreatment. To date, reimbursement issues remain in the absence of an FDA indication and due to the paucity of treatment centers in the US.24,25
Follow-up. The therapies mentioned require routine evaluation to assess tolerability and safety, as recommended in the prescribing information. Patients with known CVD should undergo an appropriate cardiac workup annually to evaluate for occult progression of disease. Patients require further evaluation of related cardiovascular risk factors and adherence with medication regimens. For primary prevention patients, annual follow-up is also recommended to assess for any changes in health status, lifestyle, or medication adherence.
Continue for conclusion >>
Conclusion
The average health care provider frequently performs the standard evaluation of a patient at risk for, or with, CVD. However, a subset of this population may be at increased cardiovascular risk due to Lp(a), a common genetic risk factor that can be responsible for premature or progressive CVD. Because of the aggressive nature of this disorder and the young age at which it influences the development of vascular disease, health care providers must be more vigilant about looking beyond the obvious in patients with familial hypercholesterolemia or family history of premature CVD.
Patients with progressive disease must be more thoroughly evaluated; there are already more than 63 million persons with elevated Lp(a) in the US—and many more undiagnosed—who may benefit from aggressive care. Underdiagnosis has been associated with decreased quality and productivity in the work environment, decreased quality of life, increased use of health dollars, and possibly early loss of life.
While the test for Lp(a) is readily available, the cost may not be covered by insurance and therefore may be passed on to the patient. It would behoove health care professionals to lobby for coverage as a means to reduce the prevalence of CVD, the number one cause of mortality in the US.
References
1. Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive Summary: heart disease and stroke statistics—2014 Update: a report from the American Heart Association. Circulation. 2014;129:399-410.
2. Bennet A, Di Angelantonio E, Erqou S, et al. Lipoprotein(a) levels and risk of future coronary heart disease: large-scale prospective data [published corrections appear in Arch Intern Med. 2008;168(10):1089 and Arch Intern Med. 2008;168(10):1096]. Arch Intern Med. 2008;168(6):598-608.
3. Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301(22):2331-2339.
4. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), hormone replacement therapy, and risk of future cardiovascular events. J Am Coll Cardiol. 2008;52(2):124-131.
5. Scanu AM. Lipoprotein(a). A genetic risk factor for premature coronary heart disease. JAMA. 1992;267(24):3326-3329.
6. Goldberg AC, Hopkins PN, Toth PP; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S1-S8.
7. Ito M, McGowan MP, Moriarty PM; National Lipid Association Expert Panel on Familial Hypercholesterolemia. Management of familial hypercholesterolemias in adult patients: recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipid. 2011;5(3 suppl):S38-S45.
8. Sjouke B, Kusters DM, Kindt I, et al. Homozygous autosomal dominant hypercholesterolaemia in the Netherlands: prevalence, genotype-phenotype relationship, and clinical outcome. Eur Heart J. 2014 Feb 28. [Epub ahead of print]
9. Nordestgaard BG, Chapman MJ, Ray K, et al; European Atherosclerosis Society Consensus Panel. Lipoprotein (a) as a cardiovascular risk factor: current status. Eur Heart J. 2010; 31(23):2844-2853.
10. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), measured with an assay independent of apolipoprotein(a) isoform size, and risk of future cardiovascular events among initially healthy women. JAMA. 2006;296 (11):1363-1370.
11. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227-239.
12. Jacobson TA. Lipoprotein (a), cardiovascular disease, and contemporary management. Mayo Clin Proc. 2013;88(11):1294-1311.
13. Hunninghake DB, Stein EA, Mellies MJ. Effects of one year of treatment with pravastatin, an HMG-CoA reductase inhibitor, on lipoprotein a. J Clin Pharmacol. 1993;33 (6):574-580.
14. Jones PH, Pownall HJ, Patsch W, et al. Effect of gemfibrozil on levels of lipoprotein[a] in type 2 hyperlipoproteinemic subjects. J Lipid Res. 1996;37(6):1298-1308.
15. Boden WE, Probstfield JL, Anderson T, et al; AIM-HIGH investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365(24):2255-2267.
16. Landray MJ, Haynes R, Hopewell JC, et al; HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371 (3):203-212.
17. Morgan JM, Capuzzi DM, Guyton JR. A new extended-release niacin (Niaspan): efficacy, tolerability, and safety in hypercholesterolemic patients. Am J Cardiol. 1998;82 (12A): 29U-34U.
18. Piepho RW. The pharmacokinetics and pharmacodynamics of agents proven to raise high-density lipoprotein cholesterol. Am J Cardiol. 2000;86(12A):35L-40L.
19. Guyton JR, Bays HE. Safety considerations with niacin therapy. Am J Cardiol. 2007; 99(6A):22C-31C.
20. McKenney JM, Proctor JD, Harris S, Chinchili VM. A comparison of the efficacy and toxic effects of sustained- vs immediate-release niacin in hypercholesterolemic patients. JAMA. 1994;271(9):672-677.
21. Shlipak MG, Simon JA, Vittinghoff E, et al. Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA. 2000;283 (14):1845-1852.
22. Marbach JA, McKeon JL, Ross JL, Duffy D. Novel treatments for familial hypercholesterolemia: pharmacogenetics at work. Pharmacotherapy. 2014;34(9):961-972.
23. Stein EA, Mellis S, Yancopoulos GD, et al. Effect of a monoclonal antibody to PCSK9 on LDL cholesterol. N Engl J Med. 2012;366(12): 1108-1118.
24. Sachais BS, Katz J, Ross J, Rader DJ. Long-term effects of LDL apheresis in patients with severe hypercholesterolemia. J Clin Apher. 2005;20:252-255.
25. Waldmann E, Parhofer K. Lipoprotein apheresis to treat elevated lipoprotein(a). J Lipid Res. 2016 Feb 17. [Epub ahead of print]
CKD: Latest on Screening
Q) suPAR, a new screening tool for chronic kidney disease, has gotten a lot of press recently. My practice is interested in implementing it, but we can’t find information on how to obtain it. Is it commercially available yet? How can we order it? And importantly for our patients, do insurance plans cover it?
Research has been ongoing regarding biomarkers that could identify those at risk for chronic kidney disease (CKD) long before loss of renal function is apparent. A recently published study suggests that the circulating protein, soluble urokinase-type plasminogen activator receptor (suPAR), may be such a biomarker.
In a study of 3,683 subjects (ages 20 to 90) undergoing cardiac catheterization, and a further evaluation of 347 subjects in the Women’s Interagency HIV Study, Hayek et al found that elevated levels of suPAR were independently associated with CKD and with accelerated loss of renal function. At five-year follow-up, 24% of the 1,335 subjects with an initial estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m2 had developed CKD. Risk for progression to CKD was about 41% in those with a baseline suPAR level ≥ 3,040 ng/mL, compared to 12% in those with lower baseline suPAR levels.1 Thus, the cutoff for high versus low risk appears to be 3,040 ng/mL.
Hayek and associates are not the first or the only investigators studying the connection between suPAR and kidney disease. Evolving research has suggested suPAR may be an initiating factor in the development of focal segmental glomerulosclerosis (FSGS).2 However, a recent study did not support this association.3
Currently, in the United States, laboratory testing for suPAR is available only for research purposes and has not been approved by the FDA for direct patient care.4 While more research is needed with different cohorts, there is much excitement in the field of nephrology regarding the potential role of suPAR as a biomarker for predicting CKD. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
1. Hayek SS, Sever S, Ko Y-A, et al. Soluble urokinase receptor and chronic kidney disease. N Engl J Med. 2015;373:1916-1925.
2. Spinale JM, Mariani LH, Kapoor S, et al. A reassessment of soluble urokinase-type plasminogen activator receptor in glomerular disease. Kidney Int. 2015;87(3):564-574.
3. Wei C, El Hindi S, Li J, et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis.Nature Med. 2011;17: 952-960.
4. Rush University Medical Center. Early warning found for chronic kidney disease: common protein in blood rises months or years before disease develops [news release]. November 5, 2015. www.rush.edu/news/press-releases/early-warning-found-chronic-kidney-disease. Accessed April 11, 2016.
Q) suPAR, a new screening tool for chronic kidney disease, has gotten a lot of press recently. My practice is interested in implementing it, but we can’t find information on how to obtain it. Is it commercially available yet? How can we order it? And importantly for our patients, do insurance plans cover it?
Research has been ongoing regarding biomarkers that could identify those at risk for chronic kidney disease (CKD) long before loss of renal function is apparent. A recently published study suggests that the circulating protein, soluble urokinase-type plasminogen activator receptor (suPAR), may be such a biomarker.
In a study of 3,683 subjects (ages 20 to 90) undergoing cardiac catheterization, and a further evaluation of 347 subjects in the Women’s Interagency HIV Study, Hayek et al found that elevated levels of suPAR were independently associated with CKD and with accelerated loss of renal function. At five-year follow-up, 24% of the 1,335 subjects with an initial estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m2 had developed CKD. Risk for progression to CKD was about 41% in those with a baseline suPAR level ≥ 3,040 ng/mL, compared to 12% in those with lower baseline suPAR levels.1 Thus, the cutoff for high versus low risk appears to be 3,040 ng/mL.
Hayek and associates are not the first or the only investigators studying the connection between suPAR and kidney disease. Evolving research has suggested suPAR may be an initiating factor in the development of focal segmental glomerulosclerosis (FSGS).2 However, a recent study did not support this association.3
Currently, in the United States, laboratory testing for suPAR is available only for research purposes and has not been approved by the FDA for direct patient care.4 While more research is needed with different cohorts, there is much excitement in the field of nephrology regarding the potential role of suPAR as a biomarker for predicting CKD. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
1. Hayek SS, Sever S, Ko Y-A, et al. Soluble urokinase receptor and chronic kidney disease. N Engl J Med. 2015;373:1916-1925.
2. Spinale JM, Mariani LH, Kapoor S, et al. A reassessment of soluble urokinase-type plasminogen activator receptor in glomerular disease. Kidney Int. 2015;87(3):564-574.
3. Wei C, El Hindi S, Li J, et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis.Nature Med. 2011;17: 952-960.
4. Rush University Medical Center. Early warning found for chronic kidney disease: common protein in blood rises months or years before disease develops [news release]. November 5, 2015. www.rush.edu/news/press-releases/early-warning-found-chronic-kidney-disease. Accessed April 11, 2016.
Q) suPAR, a new screening tool for chronic kidney disease, has gotten a lot of press recently. My practice is interested in implementing it, but we can’t find information on how to obtain it. Is it commercially available yet? How can we order it? And importantly for our patients, do insurance plans cover it?
Research has been ongoing regarding biomarkers that could identify those at risk for chronic kidney disease (CKD) long before loss of renal function is apparent. A recently published study suggests that the circulating protein, soluble urokinase-type plasminogen activator receptor (suPAR), may be such a biomarker.
In a study of 3,683 subjects (ages 20 to 90) undergoing cardiac catheterization, and a further evaluation of 347 subjects in the Women’s Interagency HIV Study, Hayek et al found that elevated levels of suPAR were independently associated with CKD and with accelerated loss of renal function. At five-year follow-up, 24% of the 1,335 subjects with an initial estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m2 had developed CKD. Risk for progression to CKD was about 41% in those with a baseline suPAR level ≥ 3,040 ng/mL, compared to 12% in those with lower baseline suPAR levels.1 Thus, the cutoff for high versus low risk appears to be 3,040 ng/mL.
Hayek and associates are not the first or the only investigators studying the connection between suPAR and kidney disease. Evolving research has suggested suPAR may be an initiating factor in the development of focal segmental glomerulosclerosis (FSGS).2 However, a recent study did not support this association.3
Currently, in the United States, laboratory testing for suPAR is available only for research purposes and has not been approved by the FDA for direct patient care.4 While more research is needed with different cohorts, there is much excitement in the field of nephrology regarding the potential role of suPAR as a biomarker for predicting CKD. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
1. Hayek SS, Sever S, Ko Y-A, et al. Soluble urokinase receptor and chronic kidney disease. N Engl J Med. 2015;373:1916-1925.
2. Spinale JM, Mariani LH, Kapoor S, et al. A reassessment of soluble urokinase-type plasminogen activator receptor in glomerular disease. Kidney Int. 2015;87(3):564-574.
3. Wei C, El Hindi S, Li J, et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis.Nature Med. 2011;17: 952-960.
4. Rush University Medical Center. Early warning found for chronic kidney disease: common protein in blood rises months or years before disease develops [news release]. November 5, 2015. www.rush.edu/news/press-releases/early-warning-found-chronic-kidney-disease. Accessed April 11, 2016.
CKD: Latest on Management
Q) I have a patient with stage 3a chronic kidney disease (glomerular filtration rate, 45-60 mL/min/1.73 m2). I have her on a statin and an ACE inhibitor. Is there anything else I can do to slow the progression of kidney disease?
For patients with stage 3a chronic kidney disease (CKD), ongoing evaluation of risk factors and management can impact the rate of disease progression. The cornerstones of CKD care include identification and treatment of the cause; management of hypertension, albuminuria, and diabetes (if applicable); reduction of cardiovascular (CV) risk; and correction of metabolic abnormalities.5
When considering factors that can contribute to kidney injury, clinicians should consider possible pre-, intra-, and post-renal processes that could potentially cause injury.
Prerenal: Approximately 20% of cardiac output is directed to the kidneys. Reduced left ventricular function, diastolic dysfunction, and pulmonary hypertension can all contribute to a reduction in renal blood flow and subsequent kidney injury.6
Intrarenal: Exploration of possible intra-renal processes begins with a thorough history of any familial disease, hematuria, stones, proteinuria, and exposure to nephrotoxins. The nephrotoxicity profile of all medications should be examined, and patients should be educated about products, particularly OTC medications (eg, NSAIDs, common cold preparations, and herbal or weight-loss products), that can be harmful to the kidneys. Patients should also be made aware of the risk for contrast-induced renal injury, especially when considering imaging or cardiac testing. Since diabetes is a leading cause of kidney disease, good diabetic control can reduce nephropathy and slow disease progression.
Postrenal: Benign prostatic hypertrophy, kidney stones, and neurogenic bladder can all cause injury. These warrant further evaluation and treatment.
CKD often worsens existing hypertension, which is an independent risk factor for kidney failure.7 Goal blood pressure (BP) for all patients without significant albuminuria should be < 140/90 mm Hg; for those with urinary albumin ≥ 30 mg/24 h, the goal is < 130/80 mm Hg.8 Choice of antihypertensive agents can be tailored to other comorbidities, but an ACE inhibitor or angiotensin receptor blocker should be considered firstline treatment. Nocturnal hypertension is common in patients with CKD and an independent marker of CV risk. By dosing antihypertensive medications at bedtime, the clinician supports CV risk reduction.9
CKD is an independent risk factor for CV disease, thus risk factor modification should be aggressively pursued. Regardless of the cause of CKD, cigarette smoking has been associated with a more rapid decline in renal function. Patients should be counseled on the risks and offered interventions to assist in smoking cessation.10 There is also emerging evidence that exercise likely benefits the vascular health of the kidneys and appears to slow the rate of kidney decline.11,12 Overall, lifestyle interventions that help mitigate CV risk may directly benefit preservation of kidney function as well.
Metabolic abnormalities increase with CKD progression. Maintaining proper bone health through control of phosphate/acidosis and calcium equilibrium reduces morbidity as it relates to vascular and soft-tissue calcification. This can often be effectively managed through dietary modifications in early to moderate CKD. As the number of functioning nephrons decrease in CKD, so does the ability of the kidney to maintain proper acid/base balance. Persistent metabolic acidosis is related to CKD progression. Acid buffering with oral bicarbonate may be needed to achieve a goal CO2 of 22 to 32 mEq/L.8
Through adoption of a comprehensive approach—one that is inclusive of the patient—optimal outcomes can be achieved for this rapidly growing and often underrecognized population. —CJ, AH-B, IS, BB
Crystal Johnson, PA-C
Angela Harker-Bacchus, FNP-BC
Irina Sadovskaya, PA-C
Beverly Benmoussa, FNP-BC
Transplant Nephrology Extra-Renal CKD Clinic, University of Michigan
References
5. Murphree DD, Thelen SM. Chronic kidney disease in primary care. J Am Board Fam Med. 2010;23(4):542-550.
6. Coppolino G, Presta P, Saturno L, Fuiano G. Acute kidney injury in patients undergoing cardiac surgery. J Nephrol. 2013;26(1):32-40.
7. Ravera M, Re M, Defarri L, et al. Importance of blood pressure control in chronic kidney disease. J Am Soc Nephrol. 2006;17(4 suppl 2):S98-S103.
8. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2013;3(suppl):1-150.
9. Hermida RC, Ayala DE, Mojón A, Fernández JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol. 2011;22(12):2313-2321.
10. Ricardo AC, Anderson CA, Yang W, et al. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2015;65(3):412-424.
11. Gould DW, Graham-Brown MPM, Watson EL, et al. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrology (Carlton). 2014;19(9):519-527.
12. Robinson-Cohen C, Littman AJ, Duncan GE, et al. Physical activity and change in estimated GFR among persons with CKD. J Am Soc Nephrol. 2014;25(2):399-406.
Q) I have a patient with stage 3a chronic kidney disease (glomerular filtration rate, 45-60 mL/min/1.73 m2). I have her on a statin and an ACE inhibitor. Is there anything else I can do to slow the progression of kidney disease?
For patients with stage 3a chronic kidney disease (CKD), ongoing evaluation of risk factors and management can impact the rate of disease progression. The cornerstones of CKD care include identification and treatment of the cause; management of hypertension, albuminuria, and diabetes (if applicable); reduction of cardiovascular (CV) risk; and correction of metabolic abnormalities.5
When considering factors that can contribute to kidney injury, clinicians should consider possible pre-, intra-, and post-renal processes that could potentially cause injury.
Prerenal: Approximately 20% of cardiac output is directed to the kidneys. Reduced left ventricular function, diastolic dysfunction, and pulmonary hypertension can all contribute to a reduction in renal blood flow and subsequent kidney injury.6
Intrarenal: Exploration of possible intra-renal processes begins with a thorough history of any familial disease, hematuria, stones, proteinuria, and exposure to nephrotoxins. The nephrotoxicity profile of all medications should be examined, and patients should be educated about products, particularly OTC medications (eg, NSAIDs, common cold preparations, and herbal or weight-loss products), that can be harmful to the kidneys. Patients should also be made aware of the risk for contrast-induced renal injury, especially when considering imaging or cardiac testing. Since diabetes is a leading cause of kidney disease, good diabetic control can reduce nephropathy and slow disease progression.
Postrenal: Benign prostatic hypertrophy, kidney stones, and neurogenic bladder can all cause injury. These warrant further evaluation and treatment.
CKD often worsens existing hypertension, which is an independent risk factor for kidney failure.7 Goal blood pressure (BP) for all patients without significant albuminuria should be < 140/90 mm Hg; for those with urinary albumin ≥ 30 mg/24 h, the goal is < 130/80 mm Hg.8 Choice of antihypertensive agents can be tailored to other comorbidities, but an ACE inhibitor or angiotensin receptor blocker should be considered firstline treatment. Nocturnal hypertension is common in patients with CKD and an independent marker of CV risk. By dosing antihypertensive medications at bedtime, the clinician supports CV risk reduction.9
CKD is an independent risk factor for CV disease, thus risk factor modification should be aggressively pursued. Regardless of the cause of CKD, cigarette smoking has been associated with a more rapid decline in renal function. Patients should be counseled on the risks and offered interventions to assist in smoking cessation.10 There is also emerging evidence that exercise likely benefits the vascular health of the kidneys and appears to slow the rate of kidney decline.11,12 Overall, lifestyle interventions that help mitigate CV risk may directly benefit preservation of kidney function as well.
Metabolic abnormalities increase with CKD progression. Maintaining proper bone health through control of phosphate/acidosis and calcium equilibrium reduces morbidity as it relates to vascular and soft-tissue calcification. This can often be effectively managed through dietary modifications in early to moderate CKD. As the number of functioning nephrons decrease in CKD, so does the ability of the kidney to maintain proper acid/base balance. Persistent metabolic acidosis is related to CKD progression. Acid buffering with oral bicarbonate may be needed to achieve a goal CO2 of 22 to 32 mEq/L.8
Through adoption of a comprehensive approach—one that is inclusive of the patient—optimal outcomes can be achieved for this rapidly growing and often underrecognized population. —CJ, AH-B, IS, BB
Crystal Johnson, PA-C
Angela Harker-Bacchus, FNP-BC
Irina Sadovskaya, PA-C
Beverly Benmoussa, FNP-BC
Transplant Nephrology Extra-Renal CKD Clinic, University of Michigan
References
5. Murphree DD, Thelen SM. Chronic kidney disease in primary care. J Am Board Fam Med. 2010;23(4):542-550.
6. Coppolino G, Presta P, Saturno L, Fuiano G. Acute kidney injury in patients undergoing cardiac surgery. J Nephrol. 2013;26(1):32-40.
7. Ravera M, Re M, Defarri L, et al. Importance of blood pressure control in chronic kidney disease. J Am Soc Nephrol. 2006;17(4 suppl 2):S98-S103.
8. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2013;3(suppl):1-150.
9. Hermida RC, Ayala DE, Mojón A, Fernández JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol. 2011;22(12):2313-2321.
10. Ricardo AC, Anderson CA, Yang W, et al. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2015;65(3):412-424.
11. Gould DW, Graham-Brown MPM, Watson EL, et al. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrology (Carlton). 2014;19(9):519-527.
12. Robinson-Cohen C, Littman AJ, Duncan GE, et al. Physical activity and change in estimated GFR among persons with CKD. J Am Soc Nephrol. 2014;25(2):399-406.
Q) I have a patient with stage 3a chronic kidney disease (glomerular filtration rate, 45-60 mL/min/1.73 m2). I have her on a statin and an ACE inhibitor. Is there anything else I can do to slow the progression of kidney disease?
For patients with stage 3a chronic kidney disease (CKD), ongoing evaluation of risk factors and management can impact the rate of disease progression. The cornerstones of CKD care include identification and treatment of the cause; management of hypertension, albuminuria, and diabetes (if applicable); reduction of cardiovascular (CV) risk; and correction of metabolic abnormalities.5
When considering factors that can contribute to kidney injury, clinicians should consider possible pre-, intra-, and post-renal processes that could potentially cause injury.
Prerenal: Approximately 20% of cardiac output is directed to the kidneys. Reduced left ventricular function, diastolic dysfunction, and pulmonary hypertension can all contribute to a reduction in renal blood flow and subsequent kidney injury.6
Intrarenal: Exploration of possible intra-renal processes begins with a thorough history of any familial disease, hematuria, stones, proteinuria, and exposure to nephrotoxins. The nephrotoxicity profile of all medications should be examined, and patients should be educated about products, particularly OTC medications (eg, NSAIDs, common cold preparations, and herbal or weight-loss products), that can be harmful to the kidneys. Patients should also be made aware of the risk for contrast-induced renal injury, especially when considering imaging or cardiac testing. Since diabetes is a leading cause of kidney disease, good diabetic control can reduce nephropathy and slow disease progression.
Postrenal: Benign prostatic hypertrophy, kidney stones, and neurogenic bladder can all cause injury. These warrant further evaluation and treatment.
CKD often worsens existing hypertension, which is an independent risk factor for kidney failure.7 Goal blood pressure (BP) for all patients without significant albuminuria should be < 140/90 mm Hg; for those with urinary albumin ≥ 30 mg/24 h, the goal is < 130/80 mm Hg.8 Choice of antihypertensive agents can be tailored to other comorbidities, but an ACE inhibitor or angiotensin receptor blocker should be considered firstline treatment. Nocturnal hypertension is common in patients with CKD and an independent marker of CV risk. By dosing antihypertensive medications at bedtime, the clinician supports CV risk reduction.9
CKD is an independent risk factor for CV disease, thus risk factor modification should be aggressively pursued. Regardless of the cause of CKD, cigarette smoking has been associated with a more rapid decline in renal function. Patients should be counseled on the risks and offered interventions to assist in smoking cessation.10 There is also emerging evidence that exercise likely benefits the vascular health of the kidneys and appears to slow the rate of kidney decline.11,12 Overall, lifestyle interventions that help mitigate CV risk may directly benefit preservation of kidney function as well.
Metabolic abnormalities increase with CKD progression. Maintaining proper bone health through control of phosphate/acidosis and calcium equilibrium reduces morbidity as it relates to vascular and soft-tissue calcification. This can often be effectively managed through dietary modifications in early to moderate CKD. As the number of functioning nephrons decrease in CKD, so does the ability of the kidney to maintain proper acid/base balance. Persistent metabolic acidosis is related to CKD progression. Acid buffering with oral bicarbonate may be needed to achieve a goal CO2 of 22 to 32 mEq/L.8
Through adoption of a comprehensive approach—one that is inclusive of the patient—optimal outcomes can be achieved for this rapidly growing and often underrecognized population. —CJ, AH-B, IS, BB
Crystal Johnson, PA-C
Angela Harker-Bacchus, FNP-BC
Irina Sadovskaya, PA-C
Beverly Benmoussa, FNP-BC
Transplant Nephrology Extra-Renal CKD Clinic, University of Michigan
References
5. Murphree DD, Thelen SM. Chronic kidney disease in primary care. J Am Board Fam Med. 2010;23(4):542-550.
6. Coppolino G, Presta P, Saturno L, Fuiano G. Acute kidney injury in patients undergoing cardiac surgery. J Nephrol. 2013;26(1):32-40.
7. Ravera M, Re M, Defarri L, et al. Importance of blood pressure control in chronic kidney disease. J Am Soc Nephrol. 2006;17(4 suppl 2):S98-S103.
8. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2013;3(suppl):1-150.
9. Hermida RC, Ayala DE, Mojón A, Fernández JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol. 2011;22(12):2313-2321.
10. Ricardo AC, Anderson CA, Yang W, et al. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2015;65(3):412-424.
11. Gould DW, Graham-Brown MPM, Watson EL, et al. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrology (Carlton). 2014;19(9):519-527.
12. Robinson-Cohen C, Littman AJ, Duncan GE, et al. Physical activity and change in estimated GFR among persons with CKD. J Am Soc Nephrol. 2014;25(2):399-406.
Kidney Disease: Surprising Patients
Q) Recently, I have seen four or five Asian-American patients with really bad kidney function. All of them were thin but had diabetes, hypertension, and a serum creatinine > 2 mg/dL. The kidney disease was a shock to them (and me). Am I missing something here?
Diabetes and hypertension are the most common causes of chronic kidney disease (CKD), with diabetes slightly edging out hypertension for the number 1 slot.1 Although Asian Americans have a tendency toward a lower body mass index (BMI) than the general population, this does not exclude them from developing diabetes or hypertension.
About 20% (1 in 5) of Asian-American adults have both diabetes and hypertension. In fact, Asian Americans with a BMI ≤ 25 often develop type 2 diabetes (T2DM), which is a direct contrast to other racial and ethnic groups in whom T2DM is more prevalent at higher BMIs. The current thinking is that Asian Americans have a higher percentage of body fat at lower BMIs.2 Among racial and ethnic subgroups, Asian Americans have the highest prevalence of undiagnosed diabetes (close to 50%).2
In 2004, after adjusting for lower BMI, McNeely and Boyko found that the incidence of diabetes in Asian Americans was 60% higher than in the Hispanic population.3 In 2015, this influenced the American Diabetes Association (ADA) to change its recommendation for diabetes screening in Asian Americans, lowering the threshold to a BMI of 23.4
Since abdominal or visceral fat is a risk factor for heart disease, hypertension, and diabetes, and it appears that the Asian-American population carries excess fat centrally, this population is also at risk for cardiac disease.5 For that reason, in this population, the American Heart Association recommends measuring waist circumference to screen for hidden abdominal adiposity.6
Thus, the trend you are seeing in your patient population is really only the tip of the iceberg. The Asian-American population is the fastest-growing ethnic group in the United States.3 It’s time to update your diabetes screening protocols. —SWM
Shushanne Wynter-Minott, DNP, FNP-BC
Memorial Healthcare System, Hollywood, Florida
References
1. CDC. National Chronic Kidney Disease Fact Sheet, 2014. www.cdc.gov/diabetes/pubs/pdf/kidney_Factsheet.pdf. Accessed February 3, 2016.
2. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029.
3. McNeely MJ, Boyko EJ. Type 2 diabetes prevalence in Asian Americans: results of a national health survey. Diabetes Care. 2004;27(1):66-69.
4. American Diabetes Association. Standards of medical care in diabetes—2015: summary of revisions. Diabetes Care. 2015;38(suppl):S4.
5. Park YW, Allison DB, Heymsfield SB, Gallagher D. Larger amounts of visceral adipose tissue in Asian Americans. Obes Res. 2001;9(7):381-387.
6. Rao G, Powell-Wiley TM, Ancheta I, et al; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health. Identification of obesity and cardiovascular risk in ethnically and racially diverse populations: a scientific statement from the American Heart Association. Circulation. 2015;132(5):457-472.
Q) Recently, I have seen four or five Asian-American patients with really bad kidney function. All of them were thin but had diabetes, hypertension, and a serum creatinine > 2 mg/dL. The kidney disease was a shock to them (and me). Am I missing something here?
Diabetes and hypertension are the most common causes of chronic kidney disease (CKD), with diabetes slightly edging out hypertension for the number 1 slot.1 Although Asian Americans have a tendency toward a lower body mass index (BMI) than the general population, this does not exclude them from developing diabetes or hypertension.
About 20% (1 in 5) of Asian-American adults have both diabetes and hypertension. In fact, Asian Americans with a BMI ≤ 25 often develop type 2 diabetes (T2DM), which is a direct contrast to other racial and ethnic groups in whom T2DM is more prevalent at higher BMIs. The current thinking is that Asian Americans have a higher percentage of body fat at lower BMIs.2 Among racial and ethnic subgroups, Asian Americans have the highest prevalence of undiagnosed diabetes (close to 50%).2
In 2004, after adjusting for lower BMI, McNeely and Boyko found that the incidence of diabetes in Asian Americans was 60% higher than in the Hispanic population.3 In 2015, this influenced the American Diabetes Association (ADA) to change its recommendation for diabetes screening in Asian Americans, lowering the threshold to a BMI of 23.4
Since abdominal or visceral fat is a risk factor for heart disease, hypertension, and diabetes, and it appears that the Asian-American population carries excess fat centrally, this population is also at risk for cardiac disease.5 For that reason, in this population, the American Heart Association recommends measuring waist circumference to screen for hidden abdominal adiposity.6
Thus, the trend you are seeing in your patient population is really only the tip of the iceberg. The Asian-American population is the fastest-growing ethnic group in the United States.3 It’s time to update your diabetes screening protocols. —SWM
Shushanne Wynter-Minott, DNP, FNP-BC
Memorial Healthcare System, Hollywood, Florida
References
1. CDC. National Chronic Kidney Disease Fact Sheet, 2014. www.cdc.gov/diabetes/pubs/pdf/kidney_Factsheet.pdf. Accessed February 3, 2016.
2. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029.
3. McNeely MJ, Boyko EJ. Type 2 diabetes prevalence in Asian Americans: results of a national health survey. Diabetes Care. 2004;27(1):66-69.
4. American Diabetes Association. Standards of medical care in diabetes—2015: summary of revisions. Diabetes Care. 2015;38(suppl):S4.
5. Park YW, Allison DB, Heymsfield SB, Gallagher D. Larger amounts of visceral adipose tissue in Asian Americans. Obes Res. 2001;9(7):381-387.
6. Rao G, Powell-Wiley TM, Ancheta I, et al; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health. Identification of obesity and cardiovascular risk in ethnically and racially diverse populations: a scientific statement from the American Heart Association. Circulation. 2015;132(5):457-472.
Q) Recently, I have seen four or five Asian-American patients with really bad kidney function. All of them were thin but had diabetes, hypertension, and a serum creatinine > 2 mg/dL. The kidney disease was a shock to them (and me). Am I missing something here?
Diabetes and hypertension are the most common causes of chronic kidney disease (CKD), with diabetes slightly edging out hypertension for the number 1 slot.1 Although Asian Americans have a tendency toward a lower body mass index (BMI) than the general population, this does not exclude them from developing diabetes or hypertension.
About 20% (1 in 5) of Asian-American adults have both diabetes and hypertension. In fact, Asian Americans with a BMI ≤ 25 often develop type 2 diabetes (T2DM), which is a direct contrast to other racial and ethnic groups in whom T2DM is more prevalent at higher BMIs. The current thinking is that Asian Americans have a higher percentage of body fat at lower BMIs.2 Among racial and ethnic subgroups, Asian Americans have the highest prevalence of undiagnosed diabetes (close to 50%).2
In 2004, after adjusting for lower BMI, McNeely and Boyko found that the incidence of diabetes in Asian Americans was 60% higher than in the Hispanic population.3 In 2015, this influenced the American Diabetes Association (ADA) to change its recommendation for diabetes screening in Asian Americans, lowering the threshold to a BMI of 23.4
Since abdominal or visceral fat is a risk factor for heart disease, hypertension, and diabetes, and it appears that the Asian-American population carries excess fat centrally, this population is also at risk for cardiac disease.5 For that reason, in this population, the American Heart Association recommends measuring waist circumference to screen for hidden abdominal adiposity.6
Thus, the trend you are seeing in your patient population is really only the tip of the iceberg. The Asian-American population is the fastest-growing ethnic group in the United States.3 It’s time to update your diabetes screening protocols. —SWM
Shushanne Wynter-Minott, DNP, FNP-BC
Memorial Healthcare System, Hollywood, Florida
References
1. CDC. National Chronic Kidney Disease Fact Sheet, 2014. www.cdc.gov/diabetes/pubs/pdf/kidney_Factsheet.pdf. Accessed February 3, 2016.
2. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029.
3. McNeely MJ, Boyko EJ. Type 2 diabetes prevalence in Asian Americans: results of a national health survey. Diabetes Care. 2004;27(1):66-69.
4. American Diabetes Association. Standards of medical care in diabetes—2015: summary of revisions. Diabetes Care. 2015;38(suppl):S4.
5. Park YW, Allison DB, Heymsfield SB, Gallagher D. Larger amounts of visceral adipose tissue in Asian Americans. Obes Res. 2001;9(7):381-387.
6. Rao G, Powell-Wiley TM, Ancheta I, et al; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health. Identification of obesity and cardiovascular risk in ethnically and racially diverse populations: a scientific statement from the American Heart Association. Circulation. 2015;132(5):457-472.
Kidney Disease: Unexpected Consequences
Q) We were operating on a 58-year-old woman for a subcapital fracture of her right hip. The orthopedist mentioned that the patient had kidney disease and that it probably caused her hip fracture. I didn’t know kidney disease causes hip fractures. Is this true?
Evolving evidence suggests an association between diminishing renal function and increased risk for fracture. Here’s a look at the available data:
Atherosclerosis Risk in Communities (ARIC) Study. During a median 13 years’ follow-up of 10,955 community-based older adults, investigators identified higher albuminuria level and decreased creatinine-based estimated glomerular filtration rate (eGFR) as significant risk factors for fracture. Other risk factors included older age, race (Caucasians had the highest incidence), and sex (women were more likely than men to sustain a fracture). A nonlinear relationship was observed between eGFR and fracture diagnosis, with a graded association between fracture and albuminuria level.7
Cardiovascular Health Study. In this study of 4,699 older community-based adults, kidney function was assessed by measurement of serum cystatin C. During a mean follow-up of 7.1 years, higher cystatin C levels correlated to a higher risk for hip fracture in both sexes. In women, there was a significant association between diminishing renal function and hip fracture status: Those with lower eGFRs had a higher incidence of fractures. There was a similar magnitude of association among men, but it was not significant.8
Health, Aging and Body Composite Study. In 2,754 older adults, an association was noted between decreased femoral neck bone mineral density (BMD) and increased risk for fracture in those with and without CKD stage 3 to 5. With a concurrent diagnosis of osteoporosis, there was a 110% increased risk for nonspinal fracture in those with CKD and a 63% increased risk for those without CKD.9 In a study of 485 adult hemodialysis patients, decreased total hip and femoral neck BMD was associated with an increased risk for fractures in women with parathyroid hormone levels on the lower range of acceptable in this population (intact parathyroid hormone level [IPTH] < 204 pg/mL) and for spinal fractures in both genders.10
Bone changes associated with deterioration of renal function are complex and multifactorial. Human bone is a composite of protein fused to mineral crystals, primarily calcium and phosphate. Bone is dynamic, being broken down and rebuilt throughout adulthood, with the skeleton almost completely rebuilt every 10 years.11
CKD–mineral and bone disorder (CKD–MBD) is a systemic disorder seen in those with kidney disease that affects bone and mineral metabolism. Its manifestations include abnormalities in the bone, calcifications of vascular and/or soft tissues, abnormal vitamin D metabolism, and disruptions in the phosphorus, calcium, and parathyroid hormone levels. These components, and the severity of the condition, vary by stage of CKD. One component of CKD–MBD, renal osteodystrophy, is associated with changes in bone morphology and is definitively diagnosed by bone biopsy.12
Care of these patients is complex and can be compounded by osteoporosis and/or loss of bone strength. Osteoporosis, like CKD, increases in incidence with age and is associated with fracture risk.11
While useful for diagnosing osteoporosis and predicting fracture risk in the general population, dual-energy X-ray densitometry (DXA) has not been recommended in those with CKD due to the type of bone changes that occur with diminished renal function.12 However, evolving evidence regarding use of DXA in these patients prompted a Kidney Disease: Improving Global Outcomes (KDIGO) “controversies” conference to recommend reexamination of the evidence regarding this recommendation.13 KDIGO’s 2009 clinical practice guideline on CKD–MBD (http://kdigo.org/home/mineral-bone-disorder/) can be of benefit in the assessment and care of affected patients. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
7. Daya NR, Voskertchian A, Schneider ALC, et al. Kidney function and fracture risk: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2016;67(2):218-226.
8. Fried LF, Biggs ML, Shlipak MG, et al. Association of kidney function with incident hip fracture in older adults. J Am Soc Nephrol. 2007;18:282-286.
9. Yenchek RH, Ix JH, Shlipak MG, et al. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7(7):1130-1136.
10. Iimori S, Mori Y, Akita W, et al. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients—a single-center cohort study. Nephrol Dial Transplant. 2012;27:345-351.
11. Office of the Surgeon General (US). Bone Health and Osteoporosis: a Report of the Surgeon General. Rockville, MD: Office of the Surgeon General; 2004.
12. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1-S130.
13. Ketteler M, Elder GJ, Evenepoel P, et al. Revisiting KDIGO clinical practice guideline on chronic kidney disease-mineral and bone disorder: a commentary from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int. 2015;87(3):502-528.
Q) We were operating on a 58-year-old woman for a subcapital fracture of her right hip. The orthopedist mentioned that the patient had kidney disease and that it probably caused her hip fracture. I didn’t know kidney disease causes hip fractures. Is this true?
Evolving evidence suggests an association between diminishing renal function and increased risk for fracture. Here’s a look at the available data:
Atherosclerosis Risk in Communities (ARIC) Study. During a median 13 years’ follow-up of 10,955 community-based older adults, investigators identified higher albuminuria level and decreased creatinine-based estimated glomerular filtration rate (eGFR) as significant risk factors for fracture. Other risk factors included older age, race (Caucasians had the highest incidence), and sex (women were more likely than men to sustain a fracture). A nonlinear relationship was observed between eGFR and fracture diagnosis, with a graded association between fracture and albuminuria level.7
Cardiovascular Health Study. In this study of 4,699 older community-based adults, kidney function was assessed by measurement of serum cystatin C. During a mean follow-up of 7.1 years, higher cystatin C levels correlated to a higher risk for hip fracture in both sexes. In women, there was a significant association between diminishing renal function and hip fracture status: Those with lower eGFRs had a higher incidence of fractures. There was a similar magnitude of association among men, but it was not significant.8
Health, Aging and Body Composite Study. In 2,754 older adults, an association was noted between decreased femoral neck bone mineral density (BMD) and increased risk for fracture in those with and without CKD stage 3 to 5. With a concurrent diagnosis of osteoporosis, there was a 110% increased risk for nonspinal fracture in those with CKD and a 63% increased risk for those without CKD.9 In a study of 485 adult hemodialysis patients, decreased total hip and femoral neck BMD was associated with an increased risk for fractures in women with parathyroid hormone levels on the lower range of acceptable in this population (intact parathyroid hormone level [IPTH] < 204 pg/mL) and for spinal fractures in both genders.10
Bone changes associated with deterioration of renal function are complex and multifactorial. Human bone is a composite of protein fused to mineral crystals, primarily calcium and phosphate. Bone is dynamic, being broken down and rebuilt throughout adulthood, with the skeleton almost completely rebuilt every 10 years.11
CKD–mineral and bone disorder (CKD–MBD) is a systemic disorder seen in those with kidney disease that affects bone and mineral metabolism. Its manifestations include abnormalities in the bone, calcifications of vascular and/or soft tissues, abnormal vitamin D metabolism, and disruptions in the phosphorus, calcium, and parathyroid hormone levels. These components, and the severity of the condition, vary by stage of CKD. One component of CKD–MBD, renal osteodystrophy, is associated with changes in bone morphology and is definitively diagnosed by bone biopsy.12
Care of these patients is complex and can be compounded by osteoporosis and/or loss of bone strength. Osteoporosis, like CKD, increases in incidence with age and is associated with fracture risk.11
While useful for diagnosing osteoporosis and predicting fracture risk in the general population, dual-energy X-ray densitometry (DXA) has not been recommended in those with CKD due to the type of bone changes that occur with diminished renal function.12 However, evolving evidence regarding use of DXA in these patients prompted a Kidney Disease: Improving Global Outcomes (KDIGO) “controversies” conference to recommend reexamination of the evidence regarding this recommendation.13 KDIGO’s 2009 clinical practice guideline on CKD–MBD (http://kdigo.org/home/mineral-bone-disorder/) can be of benefit in the assessment and care of affected patients. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
7. Daya NR, Voskertchian A, Schneider ALC, et al. Kidney function and fracture risk: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2016;67(2):218-226.
8. Fried LF, Biggs ML, Shlipak MG, et al. Association of kidney function with incident hip fracture in older adults. J Am Soc Nephrol. 2007;18:282-286.
9. Yenchek RH, Ix JH, Shlipak MG, et al. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7(7):1130-1136.
10. Iimori S, Mori Y, Akita W, et al. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients—a single-center cohort study. Nephrol Dial Transplant. 2012;27:345-351.
11. Office of the Surgeon General (US). Bone Health and Osteoporosis: a Report of the Surgeon General. Rockville, MD: Office of the Surgeon General; 2004.
12. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1-S130.
13. Ketteler M, Elder GJ, Evenepoel P, et al. Revisiting KDIGO clinical practice guideline on chronic kidney disease-mineral and bone disorder: a commentary from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int. 2015;87(3):502-528.
Q) We were operating on a 58-year-old woman for a subcapital fracture of her right hip. The orthopedist mentioned that the patient had kidney disease and that it probably caused her hip fracture. I didn’t know kidney disease causes hip fractures. Is this true?
Evolving evidence suggests an association between diminishing renal function and increased risk for fracture. Here’s a look at the available data:
Atherosclerosis Risk in Communities (ARIC) Study. During a median 13 years’ follow-up of 10,955 community-based older adults, investigators identified higher albuminuria level and decreased creatinine-based estimated glomerular filtration rate (eGFR) as significant risk factors for fracture. Other risk factors included older age, race (Caucasians had the highest incidence), and sex (women were more likely than men to sustain a fracture). A nonlinear relationship was observed between eGFR and fracture diagnosis, with a graded association between fracture and albuminuria level.7
Cardiovascular Health Study. In this study of 4,699 older community-based adults, kidney function was assessed by measurement of serum cystatin C. During a mean follow-up of 7.1 years, higher cystatin C levels correlated to a higher risk for hip fracture in both sexes. In women, there was a significant association between diminishing renal function and hip fracture status: Those with lower eGFRs had a higher incidence of fractures. There was a similar magnitude of association among men, but it was not significant.8
Health, Aging and Body Composite Study. In 2,754 older adults, an association was noted between decreased femoral neck bone mineral density (BMD) and increased risk for fracture in those with and without CKD stage 3 to 5. With a concurrent diagnosis of osteoporosis, there was a 110% increased risk for nonspinal fracture in those with CKD and a 63% increased risk for those without CKD.9 In a study of 485 adult hemodialysis patients, decreased total hip and femoral neck BMD was associated with an increased risk for fractures in women with parathyroid hormone levels on the lower range of acceptable in this population (intact parathyroid hormone level [IPTH] < 204 pg/mL) and for spinal fractures in both genders.10
Bone changes associated with deterioration of renal function are complex and multifactorial. Human bone is a composite of protein fused to mineral crystals, primarily calcium and phosphate. Bone is dynamic, being broken down and rebuilt throughout adulthood, with the skeleton almost completely rebuilt every 10 years.11
CKD–mineral and bone disorder (CKD–MBD) is a systemic disorder seen in those with kidney disease that affects bone and mineral metabolism. Its manifestations include abnormalities in the bone, calcifications of vascular and/or soft tissues, abnormal vitamin D metabolism, and disruptions in the phosphorus, calcium, and parathyroid hormone levels. These components, and the severity of the condition, vary by stage of CKD. One component of CKD–MBD, renal osteodystrophy, is associated with changes in bone morphology and is definitively diagnosed by bone biopsy.12
Care of these patients is complex and can be compounded by osteoporosis and/or loss of bone strength. Osteoporosis, like CKD, increases in incidence with age and is associated with fracture risk.11
While useful for diagnosing osteoporosis and predicting fracture risk in the general population, dual-energy X-ray densitometry (DXA) has not been recommended in those with CKD due to the type of bone changes that occur with diminished renal function.12 However, evolving evidence regarding use of DXA in these patients prompted a Kidney Disease: Improving Global Outcomes (KDIGO) “controversies” conference to recommend reexamination of the evidence regarding this recommendation.13 KDIGO’s 2009 clinical practice guideline on CKD–MBD (http://kdigo.org/home/mineral-bone-disorder/) can be of benefit in the assessment and care of affected patients. —CS
Cindy Smith, DNP, APRN, CNN-NP, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virgina
References
7. Daya NR, Voskertchian A, Schneider ALC, et al. Kidney function and fracture risk: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2016;67(2):218-226.
8. Fried LF, Biggs ML, Shlipak MG, et al. Association of kidney function with incident hip fracture in older adults. J Am Soc Nephrol. 2007;18:282-286.
9. Yenchek RH, Ix JH, Shlipak MG, et al. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7(7):1130-1136.
10. Iimori S, Mori Y, Akita W, et al. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients—a single-center cohort study. Nephrol Dial Transplant. 2012;27:345-351.
11. Office of the Surgeon General (US). Bone Health and Osteoporosis: a Report of the Surgeon General. Rockville, MD: Office of the Surgeon General; 2004.
12. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1-S130.
13. Ketteler M, Elder GJ, Evenepoel P, et al. Revisiting KDIGO clinical practice guideline on chronic kidney disease-mineral and bone disorder: a commentary from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int. 2015;87(3):502-528.