User login
Can Healthcare Go From Good to Great?
The American healthcare system produces a product whose quality, safety, reliability, and cost would be incompatible with corporate survival, were they created by a business operating in a competitive industry. Care fails to comport with best evidence nearly half of the time.1 Tens of thousands of Americans die yearly from preventable medical mistakes.2 The healthcare inflation rate is nearly twice that of the rest of the economy, rapidly outstripping the ability of employers, tax revenues, and consumers to pay the mounting bills.
Increasingly, the healthcare system is being held accountable for this lack of value. Whether through a more robust accreditation and regulatory environment, public reporting of quality and safety metrics, or pay for performance (or no pay for errors) initiatives, outside stakeholders are creating performance pressures that scarcely existed a decade ago.
Healthcare organizations and providers have begun to take notice and act, often by seeking answers from industries outside healthcare and thoughtfully importing these lessons into medicine. For example, the use of checklists has been adopted by healthcare (from aviation), with impressive results.3, 4 Many quality methods drawn from industry (Lean, Toyota, Six Sigma) have been used to try to improve performance and remove waste from complex processes.5, 6
While these efforts have been helpful, their focus has generally been at the point‐of‐careimproving the care of patients with acute myocardial infarction or decreasing readmissions. However, while the business community has long recognized that poor management and structure can thwart most efforts to improve individual processes, healthcare has paid relatively little attention to issues of organizational structure and leadership. The question arises: Could methods that have been used to learn from top‐performing businesses be helpful to healthcare's efforts to improve its own organizational performance?
In this article, we describe perhaps the best known effort to identify top‐performing corporations, compare them to carefully selected organizations that failed to achieve similar levels of performance, and glean lessons from these analyses. This effort, described in a book entitled Good to Great: Why Some Companies Make the Leapand Others Don't, has sold more than 3 million copies in its 35 languages, and is often cited by business leaders as a seminal work. We ask whether the methods of Good to Great might be applicable to healthcare organizations seeking to produce the kinds of value that patients and purchasers need and deserve.
GOOD TO GREAT METHODOLOGY
In 2001, business consultant Jim Collins published Good to Great. Its methods can be divided into 3 main components: (1) a gold standard metric to identify top organizations; (2) the creation of a control group of organizations that appeared similar to the top performers at the start of the study, but failed to match the successful organizations' performance over time; and (3) a detailed review of the methods, leadership, and structure of both the winning and laggard organizations, drawing lessons from their differences. Before discussing whether these methods could be used to analyze healthcare organizations, it is worth describing Collins' methods in more detail.
The first component of Good to Great's structure was the use of 4 metrics to identify top‐performing companies (Table 1). To select the good to great companies, Collins and his team began with a field of 1435 companies drawn from Fortune magazine's rankings of America's largest public companies. They then used the criteria in Table 1 to narrow the list to their final 11 companies, which formed the experimental group for the analysis.
|
| The company had to show a pattern of good performance punctuated by a transition point when it shifted to great performance. Great performance was defined as a cumulative total stock return of at least 3 times the general stock market for the period from the transition point through 15 years. |
| The transition from good to great had to be company‐specific, not an industry‐wide event. |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. |
| At the time of the selection (in 1996), the company still had to show an upward trend. |
After identifying these 11 top‐performing companies, Collins created a control group, composed of companies with similar attributes that could have made the transition, but failed to do so.7 To create the control group, Collins matched and scored a pool of control group candidates based on the following criteria: similarities of business model, size, age, and cumulative stock returns prior to the good to great transition. When there were several potential controls, Collins chose companies that were larger, more profitable, and had a stronger market position and reputation prior to the transition, in order to increase the probability that the experimental companies' successes were not incidental.8 Table 2 lists the paired experimental and control companies.
| Experimental Company | Control Company |
|---|---|
| |
| Abbott | Upjohn |
| Circuit City | Silo |
| Fannie Mae | Great Western |
| Gillette | Warner‐Lambert |
| Kimberly‐Clark | Scott Paper |
| Kroger | A&P |
| Nucor | Bethlehem Steel |
| Philip Morris | R.J. Reynolds |
| Pitney Bowes | Addressograph |
| Walgreen's | Eckerd |
| Wells Fargo | Bank of America |
Finally, Collins performed a detailed historical analysis on the experimental and control groups, using materials (such as major articles published on the company, books, academic case studies, analyst reports, and financial and annual reports) that assessed the companies in real time. Good to Great relied on evidence from the period of interest (ie, accrued prior to the transition point) to avoid biases that would likely result from relying on retrospective sources of data.9
This analysis identified a series of factors that were generally present in good to great companies and absent in the control organizations. In brief, they were: building a culture of discipline, making change through gradual and consistent improvement, having a leader with a paradoxical blend of personal humility and professional will, and relentlessly focusing on hiring and nurturing the best employees. Over 6000 articles and 5 years of analysis support these conclusions.8
EFFORTS TO DATE TO ANALYZE HEALTHCARE ORGANIZATIONAL CHARACTERISTICS
We reviewed a convenience sample of the literature on organizational change in healthcare, and found only 1 study that utilized a similar methodology to that of Good to Great: an analysis of the academic medical centers that participate in the University HealthSystem Consortium (UHC). Drawing inspiration from Collins' methodologies, the UHC study developed a holistic measure of quality, based on safety, mortality, compliance with evidence‐based practices, and equity of care. Using these criteria, the investigators selected 3 UHC member organizations that were performing extremely well, and 3 others performing toward the middle and bottom of the pack. Experts on health system organization then conducted detailed site visits to these 6 academic medical centers. The researchers were blinded to these rankings at the time of the visits, but were able to perfectly predict which cohort the organizations were in.
The investigators analyzed the factors that seemed to be present in the top‐performing organizations, but were absent in the laggards, and found: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, a concrete accountability structure for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration on quality.10
While the UHC study is among the most robust exploration of healthcare organization dynamics in the literature, it has a few limitations. The first is that it studied a small, relatively specialized population: UHC members, which are large, mostly urban, well‐resourced teaching hospitals. While studying segments of populations can limit the generalizability of some of the UHC studies' findings, their approach can be a useful model to apply to studying other types of healthcare institutions. (And, to be fair, Good to Great also studies a specialized populationFortune 500 companiesand thus its lessons need to be extrapolated to other businesses, such as small companies, with a degree of caution.) The study also suffers from the relative paucity of publicly accessible organizational data in healthcare. The fact that the UHC investigators depended on both top‐performing and laggard hospitals, to voluntarily release their organizational data and permit a detailed site visit, potentially introduces a selection bias into the survey population, a bias not present in Good to Great due to Collins' protocol for matching cases and controls.
There have been several other efforts, using different methods, to determine organizational predictors of success in healthcare. The results of several important studies are shown in Table 3. Taken together, they indicate that higher performing organizations make practitioners accountable for performance measurements, and implement systems designed to both reduce errors and facilitate adherence to evidence‐based guidelines. In addition to these studies, several consulting organizations and foundations have performed focused reviews of high‐performing healthcare organizations in an effort to identify key success factors.11 These studies, while elucidating factors that influence organizational performance, suffer from variable quality measures and subjective methods for gathering organizational data, both of which are addressed within a good to great‐style analysis.12
| Study | Key Findings |
|---|---|
| |
| Keroack et al.10 | Superior‐performing organizations were distinguished from average ones by having: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, concrete accountability structures for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration toward quality improvement measures. |
| Jha et al.22 | Factors that led to the VA's improved performance included: |
| Implementation of a systematic approach to measurement, management, and accountability for quality. | |
| Initiating routine performance measurements for high‐priority conditions. | |
| Creating performance contracts to hold managers accountable for meeting improvement goals. | |
| Having an independent agency gather and monitor data. | |
| Implementing process improvements, such as an integrated, comprehensive medical‐record system. | |
| Making performance data public and distributing these data widely within the VA and among other key stakeholders (veterans' service organizations, Congress). | |
| Shortell et al.20 | Focusing on reducing the barriers and encouraging the adoption of evidence‐based organizational management is associated with better patient outcomes. Examples of reducing barriers to encourage adoption of evidence‐based guidelines include: |
| Installing an IT system to improve chronic care management. | |
| Creating a culture where practitioners can help each other learn from their mistakes. | |
| Knaus et al.21 | The interaction and coordination of each hospital's ICU staff had a greater correlation with reduced mortality rates than did the unit's administrative structure, amount of specialized treatment used, or the hospital's teaching status. |
| Pronovost et al.3 | Introducing a checklist of 5 evidence‐based procedures into a healthcare team's operation can significantly reduce the rate of catheter‐associated infections. |
| Simple process change interventions, such as checklists, must be accompanied by efforts to improve team culture and create leadership accountability and engagement. | |
| Pronovost et al.30 | Implementing evidence‐based therapies by embedding them within a healthcare team's culture is more effective than simply focusing on changing physician behavior. |
| The authors proposed a 4‐step model for implementing evidence‐based therapies: select interventions with the largest benefit and lowest barriers to use, identify local barriers to implementation, measure performance, and ensure all patients receive the interventions. | |
Perhaps the best‐known study on healthcare organizational performance is The Dartmouth Atlas, an analysis that (though based on data accumulated over more than 30 years) has received tremendous public attention, in recent years, in the context of the debate over healthcare reform.13 However, by early 2010, the Dartmouth analysis was stirring controversy, with some observers expressing concerns over its focus on care toward the end of life, its methods for adjusting for case‐mix and sociodemographic predictors of outcomes and costs, and its exclusive use of Medicare data.14, 15 These limitations are also addressed by a good to great‐style analysis.
WOULD A GOOD TO GREAT ANALYSIS BE POSSIBLE IN HEALTHCARE?
While this review of prior research on organizational success factors in healthcare illustrates considerable interest in this area, none of the studies, to date, matches Good to Great in the robustness of the analysis or, obviously, its impact on the profession. Could a good to great analysis be carried out in healthcare? It is worth considering this by assessing each of Collins' 3 key steps: identifying the enterprises that made a good to great leap, selecting appropriate control organizations, and determining the factors that contributed to the successes of the former group.
Good to Great used an impressive elevation in stock price as a summary measure of organizational success. In the for‐profit business world, it is often assumed that Adam Smith's invisible hand makes corporate information available to investors, causing an organization's stock price to capture the overall success of its business strategy, including its product quality and operational efficiency.16 In the healthcare world, mostly populated by non‐profit organizations that are simultaneously working toward a bottom line and carrying out a social mission, there is no obvious equivalent to the stock price for measuring overall organizational performance and value. All of the methods for judging top hospitals, for example, are flaweda recent study found that the widely cited U.S. News & World Report's America's Best Hospitals list is largely driven by hospital reputation,17 while another study found glaring inconsistencies among methods used to calculate risk‐adjusted mortality rates.18 A generally accepted set of metrics defining the value of care produced by a healthcare organization (including quality, safety, access, patient satisfaction, and efficiency) would be needed to mirror the first good to great step: defining top‐performing organizations using a gold standard.19 The summary measure used in the UHC study is the closest we have seen to a good to great‐style summary performance measure in healthcare.10
While it is important to identify a gold‐standard measure of organizational quality, careful selection of a control organization may be the most important step in conducting a good to great analysis. Although Collins' use of stock price as a summary measure of organizational performance is the best measure available in business, it is by no means perfect. Despite this shortcoming, however, Collins believes that the central requirement is not finding a perfect measure of organizational success, but rather determining what correlates with a divergence of performance in stock price (J. Collins, oral communication, July 2010). Similar to clinical trials, meticulous matching of a good to great organization with a control has the advantage of canceling out extraneous environmental factors, thereby enabling the elucidation of organizational factors that contribute to divergent performance. Good to Great's methods depended on substantial historical background to define top performers and controls. Unfortunately, healthcare lacks an analog to the business world's robust historical and publicly accessible record of performance and organizational data. Therefore, even if a certain organization was determined to be a top performer based on a gold‐standard measure, selecting a control organization by matching its organizational and performance data to the top performer's would be unfeasible.
Finally, the lack of a historical record in healthcare also places substantial roadblocks in the way of looking under the organization's hood. Even in pioneering organizational analyses by Shortell et al.,20 Knaus et al.,21 and Jha et al.,22 substantial parts of their analyses relied on retrospective accounts to determine organizational characteristics. To remove the bias that comes from knowing the organization's ultimate performance, Collins was careful to base his analysis of organizational structures and leadership on documents available before the good to great transition. Equivalent data in healthcare are extremely difficult to find.
While it is best to rely on an historical record, it may be possible to carry out a good to great‐type analysis through meticulous structuring of personal interviews. Collins has endorsed a non‐healthcare study that utilized the good to great matching strategy but used personal interviews to make up for lack of access to a substantial historical record.23 To reduce the bias inherent in relying on interviews, the research team ensured that the good to great transition was sustained for many years, and that the practices elicited from the interviews started before the good to great transition. Both of these techniques helped increase the probability that the identified practices contributed to the transition to superior results (in this case, in public education outcomes) and, thus, that the adoption of these practices could result in improvements elsewhere (J. Collins, oral communication, July 2010).
To make such a study possible in healthcare, more organizational data are required. Without prodding by outside stakeholders, most healthcare organizations have been reluctant to publicize performance data for fear of malpractice risk,24 or based on their belief that current data paint an incomplete or inaccurate picture of their quality.25 Trends toward required reporting of quality data (such as via Medicare's Hospital Compare Web site) offer hope that future comparisons could rely on robust organizational quality and safety data. Instituting healthcare analogs to Securities & Exchange Commission (SEC) reporting mandates would further ameliorate this information deficit.26
While we believe that Good to Great offers lessons relevant to healthcare, there are limitations that are worth considering. First, the extraordinary complexity of healthcare organizations makes it likely that a matched‐pair‐type study would need to be accompanied by other types of analyses, including more quantitative analyses of large datasets, to give a full picture of structural and leadership predictors of strong performance. Moreover, before embracing the good to great method, some will undoubtedly point to the demise of Circuit City and Fannie Mae (2 of the Good to Great companies; Table 2) as a cautionary note. Collins addresses this issue with the commonsensical argument that the success of a company needs to be judged in the context of the era. By way of analogy, he points to the value of studying a sports team, such as the John Wooden‐coached UCLA teams of the 1960s and 1970s, notwithstanding the less stellar performance of today's UCLA team. In fact, Collins' recent book mines some of these failures for their important lessons.27
GOOD TO GREAT IN HEALTHCARE
Breaking through healthcare's myopia to explore solutions drawn from other industries, such as checklists, simulation, and industrial approaches to quality improvement, has yielded substantial insights and catalyzed major improvements in care. Similarly, we believe that finding ways to measure the performance of healthcare organizations on both cost and quality, to learn from those organizations achieving superior performance, and to create a policy and educational environment that rewards superior performance and helps poor performers improve, is a defining issue for healthcare. This will be particularly crucial as the policy environment changestransitions to Accountable Care Organizations28 and bundled payments29 are likely to increase the pressure on healthcare organizations to learn the secrets of their better‐performing brethren. These shifts are likely to put an even greater premium on the kinds of leadership, organizational structure, and ability to adapt to a changing environment that Collins highlighted in his analysis. After all, it is under the most challenging conditions that top organizations often prove their mettle.
Although there are considerable challenges in performing a good to great analysis in healthcare (Table 4), the overall point remains: Healthcare is likely to benefit from rigorous, unbiased methods to distinguish successful from less successful organizations, to learn the lessons of both, and to apply these lessons to improvement efforts.
| Issue* | Good to Great* | What Exists in Healthcare | How Healthcare Can Fill in the Gaps |
|---|---|---|---|
| |||
| Gold standard measure of quality | Cumulative total stock return of at least 3 times the general market for the period from the transition point through 15 years. | Risk‐adjusted patient outcomes data (eg, mortality), process data (eg, appropriate medication use), structural data (eg, stroke center). | Create a more robust constellation of quality criteria to measure organizational performance (risk‐adjusted patient outcomes, avoidable deaths, adherence to evidence‐based guidelines, cost effectiveness, patient satisfaction); develop a generally accepted roll‐up measure. Of the studies we reviewed, the UHC study's summary measure was the closest representation to a good to great‐summary performance measure. |
| At the time of the selection, the good to great company still had to show an upward trend. | The study of the VA's transformation and the ongoing UHC study stand out as examples of studying the upward trends of healthcare organizations.22 | Make sure that the high‐performing healthcare organizations are still improvingas indicated by gold standard measures. Once the organizations are identified, study the methods these organizations utilized to improve their performance. | |
| The turnaround had to be company‐specific, not an industry‐wide event. | A few organizations have been lauded for transformations (such as the VA system).22 In most circumstances, organizations praised for high quality (eg, Geisinger, Mayo Clinic, Cleveland Clinic) have long‐established corporate tradition and culture that would be difficult to imitate. The VA operates within a system that is unique and not replicable by most healthcare organizations. | Healthcare needs to identify more examples like the VA turnaround, particularly examples of hospitals or healthcare organizations operating in more typical environmentssuch as a community or rural hospital. | |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. | Most of the healthcare organizations of interest are large organizations with complex corporate cultures, not startups. | Not applicable. | |
| Comparison method | Collins selected a comparison company that was almost exactly the same as the good to great company, except for the transition. The selection criteria were business fit, size fit, age fit, stock chart fit, conservative test, and face validity.* | Healthcare organizational studies are mostly comparisons of organizations that all experience success; few studies compare high‐performing with nonhigh‐performing organizations. (Jha et al. compared Medicare data from non‐VA hospitals and the VA, but did not use similar criteria to select similar organizations22; Keroack and colleagues' comparison of 3 mediocre to 3 superior‐performing hospitals is the closest analog to the Good to Great methodology thus far.10) | Similar to the Good to Great study, a set of factors that can categorize healthcare organizations according to similarities must be devised (eg, outpatient care, inpatient care, academic affiliation, tertiary care center, patient demographics), but finding similar organizations whose performance diverged over time is challenging. |
| Analysis of factors that separated great companies from those that did not make the transition to greatness | Good to Great used annual reports, letters to shareholders, articles written about the company during the period of interest, books about the company, business school case studies, analyst reports written in real time. | Most of the research conducted thus far has been retrospective analyses of why organizations became top performers. | The historical source of data is almost nonexistent in comparison with the business world. A parallel effort would have to capture a mixture of structure and process changes, along with organizational variables. The most effective method would be a prospective organizational assessment of several organizations, following them over time to see which ones markedly improved their performance. |
- ,,, et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- ,,;for the Institute of Medicine (US), Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999. Available at: http://www.nap.edu/books/0309068371/html/. Accessed August 22, 2011.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Using industrial processes to improve patient care.BMJ.2004;328(7432):162–164.
- ,,,,.Lean six sigma in healthcare.J Healthc Qual.2006;28(2):4–11.
- .Good to great.Fast Company. September 30,2001. Available at: http://www.fastcompany.com/magazine/51/goodtogreat.html. Accessed August 22, 2011.
- .Good to Great: Why Some Companies Make the Leap… and Others Don't.New York, NY:HarperBusiness;2001.
- .It's in the research.Jim Collins. Available at: http://www.jimcollins.com/books/research.html. Accessed May 23,2010.
- ,,,,,.Organizational factors associated with high performance in quality and safety in academic medical centers.Acad Med.2007;82(12):1178–1186.
- ,,,,.Hosptial Quality: Ingredients for Success—a Case Study of Beth Israel Deaconess Medical Center.New York, NY:Commonwealth Fund;2004. Available at: http://www.commonwealthfund.org/Content/Publications/Fund‐Reports/2004/Jul/Hospital‐Quality–Ingredients‐for‐Success‐A‐Case‐Study‐of‐Beth‐Israel‐Deaconess‐Medical‐Center. aspx. Accessed August 22, 2011.
- ,,;for the Commonwealth Fund.Hospital quality improvement strategies and lessons from U.S. hospitals.New York, NY:Commonwealth Fund;2007. Available at: http://www.commonwealthfund.org/usr_doc/Silow‐Carroll_hosp_quality_ improve_strategies_lessons_1009.pdf?section=4039. Accessed August 22, 2011.
- .The cost conundrum: what a Texas town can teach us about healthcare.The New Yorker. June 1,2009.
- .A map to bad policy—hospital efficiency measures in the Dartmouth Atlas.N Engl J Med.2010;362(7):569–574.
- ,.Critics question study cited in health debate.The New York Times. June 2,2010.
- Smith A. Campbell RH, Skinner AS, eds.An Inquiry Into the Nature and Causes of the Wealth of Nations.Oxford, England:Clarendon Press;1976.
- .The role of reputation in U.S. News 152(8):521–525.
- ,,,,.Variability in the measurement of hospital‐wide mortality rates.N Engl J Med.2010;363(26):2530–2539.
- .The elephant of patient safety: what you see depends on how you look.Jt Comm J Qual Patient Saf.2010;36(9):399–401.
- ,,.Improving patient care by linking evidence‐based medicine and evidence‐based management.JAMA.2007;298(6):673–676.
- ,,,.An evaluation of outcome from intensive care in major medical centers.Ann Intern Med.1986;104(3):410–418.
- ,,,.Effect of the transformation of the Veterans Affairs Health Care System on the quality of care.N Engl J Med.2003;348(22):2218–2227.
- ;for the Morrison Institute for Public Policy, Center for the Future of Arizona.Why Some Schools With Latino Children Beat the Odds, and Others Don't.Tempe, AZ:Morrison Institute for Public Policy;2006.
- ,,, et al.Error reporting and disclosure systems: views from hospital leaders.JAMA.2005;293(11):1359–1366.
- .Public release of performance data: a progress report from the front.JAMA.2000;283(14):1884–1886.
- ,,.The GAAP in quality measurement and reporting.JAMA.2007;298(15):1800–1802.
- .How the Mighty Fall: And Why Some Companies Never Give in.New York, NY:Jim Collins [distributed in the US and Canada exclusively by HarperCollins Publishers];2009.
- ,,,.Creating accountable care organizations: the extended hospital medical staff.Health Aff (Millwood).2007;26(1):w44–w57.
- ,,,.Using Medicare payment policy to transform the health system: a framework for improving performance.Health Aff (Millwood).2009;28(2):w238–w250.
- ,,.Translating evidence into practice: a model for large scale knowledge translation.BMJ.2008;337:a1714.
The American healthcare system produces a product whose quality, safety, reliability, and cost would be incompatible with corporate survival, were they created by a business operating in a competitive industry. Care fails to comport with best evidence nearly half of the time.1 Tens of thousands of Americans die yearly from preventable medical mistakes.2 The healthcare inflation rate is nearly twice that of the rest of the economy, rapidly outstripping the ability of employers, tax revenues, and consumers to pay the mounting bills.
Increasingly, the healthcare system is being held accountable for this lack of value. Whether through a more robust accreditation and regulatory environment, public reporting of quality and safety metrics, or pay for performance (or no pay for errors) initiatives, outside stakeholders are creating performance pressures that scarcely existed a decade ago.
Healthcare organizations and providers have begun to take notice and act, often by seeking answers from industries outside healthcare and thoughtfully importing these lessons into medicine. For example, the use of checklists has been adopted by healthcare (from aviation), with impressive results.3, 4 Many quality methods drawn from industry (Lean, Toyota, Six Sigma) have been used to try to improve performance and remove waste from complex processes.5, 6
While these efforts have been helpful, their focus has generally been at the point‐of‐careimproving the care of patients with acute myocardial infarction or decreasing readmissions. However, while the business community has long recognized that poor management and structure can thwart most efforts to improve individual processes, healthcare has paid relatively little attention to issues of organizational structure and leadership. The question arises: Could methods that have been used to learn from top‐performing businesses be helpful to healthcare's efforts to improve its own organizational performance?
In this article, we describe perhaps the best known effort to identify top‐performing corporations, compare them to carefully selected organizations that failed to achieve similar levels of performance, and glean lessons from these analyses. This effort, described in a book entitled Good to Great: Why Some Companies Make the Leapand Others Don't, has sold more than 3 million copies in its 35 languages, and is often cited by business leaders as a seminal work. We ask whether the methods of Good to Great might be applicable to healthcare organizations seeking to produce the kinds of value that patients and purchasers need and deserve.
GOOD TO GREAT METHODOLOGY
In 2001, business consultant Jim Collins published Good to Great. Its methods can be divided into 3 main components: (1) a gold standard metric to identify top organizations; (2) the creation of a control group of organizations that appeared similar to the top performers at the start of the study, but failed to match the successful organizations' performance over time; and (3) a detailed review of the methods, leadership, and structure of both the winning and laggard organizations, drawing lessons from their differences. Before discussing whether these methods could be used to analyze healthcare organizations, it is worth describing Collins' methods in more detail.
The first component of Good to Great's structure was the use of 4 metrics to identify top‐performing companies (Table 1). To select the good to great companies, Collins and his team began with a field of 1435 companies drawn from Fortune magazine's rankings of America's largest public companies. They then used the criteria in Table 1 to narrow the list to their final 11 companies, which formed the experimental group for the analysis.
|
| The company had to show a pattern of good performance punctuated by a transition point when it shifted to great performance. Great performance was defined as a cumulative total stock return of at least 3 times the general stock market for the period from the transition point through 15 years. |
| The transition from good to great had to be company‐specific, not an industry‐wide event. |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. |
| At the time of the selection (in 1996), the company still had to show an upward trend. |
After identifying these 11 top‐performing companies, Collins created a control group, composed of companies with similar attributes that could have made the transition, but failed to do so.7 To create the control group, Collins matched and scored a pool of control group candidates based on the following criteria: similarities of business model, size, age, and cumulative stock returns prior to the good to great transition. When there were several potential controls, Collins chose companies that were larger, more profitable, and had a stronger market position and reputation prior to the transition, in order to increase the probability that the experimental companies' successes were not incidental.8 Table 2 lists the paired experimental and control companies.
| Experimental Company | Control Company |
|---|---|
| |
| Abbott | Upjohn |
| Circuit City | Silo |
| Fannie Mae | Great Western |
| Gillette | Warner‐Lambert |
| Kimberly‐Clark | Scott Paper |
| Kroger | A&P |
| Nucor | Bethlehem Steel |
| Philip Morris | R.J. Reynolds |
| Pitney Bowes | Addressograph |
| Walgreen's | Eckerd |
| Wells Fargo | Bank of America |
Finally, Collins performed a detailed historical analysis on the experimental and control groups, using materials (such as major articles published on the company, books, academic case studies, analyst reports, and financial and annual reports) that assessed the companies in real time. Good to Great relied on evidence from the period of interest (ie, accrued prior to the transition point) to avoid biases that would likely result from relying on retrospective sources of data.9
This analysis identified a series of factors that were generally present in good to great companies and absent in the control organizations. In brief, they were: building a culture of discipline, making change through gradual and consistent improvement, having a leader with a paradoxical blend of personal humility and professional will, and relentlessly focusing on hiring and nurturing the best employees. Over 6000 articles and 5 years of analysis support these conclusions.8
EFFORTS TO DATE TO ANALYZE HEALTHCARE ORGANIZATIONAL CHARACTERISTICS
We reviewed a convenience sample of the literature on organizational change in healthcare, and found only 1 study that utilized a similar methodology to that of Good to Great: an analysis of the academic medical centers that participate in the University HealthSystem Consortium (UHC). Drawing inspiration from Collins' methodologies, the UHC study developed a holistic measure of quality, based on safety, mortality, compliance with evidence‐based practices, and equity of care. Using these criteria, the investigators selected 3 UHC member organizations that were performing extremely well, and 3 others performing toward the middle and bottom of the pack. Experts on health system organization then conducted detailed site visits to these 6 academic medical centers. The researchers were blinded to these rankings at the time of the visits, but were able to perfectly predict which cohort the organizations were in.
The investigators analyzed the factors that seemed to be present in the top‐performing organizations, but were absent in the laggards, and found: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, a concrete accountability structure for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration on quality.10
While the UHC study is among the most robust exploration of healthcare organization dynamics in the literature, it has a few limitations. The first is that it studied a small, relatively specialized population: UHC members, which are large, mostly urban, well‐resourced teaching hospitals. While studying segments of populations can limit the generalizability of some of the UHC studies' findings, their approach can be a useful model to apply to studying other types of healthcare institutions. (And, to be fair, Good to Great also studies a specialized populationFortune 500 companiesand thus its lessons need to be extrapolated to other businesses, such as small companies, with a degree of caution.) The study also suffers from the relative paucity of publicly accessible organizational data in healthcare. The fact that the UHC investigators depended on both top‐performing and laggard hospitals, to voluntarily release their organizational data and permit a detailed site visit, potentially introduces a selection bias into the survey population, a bias not present in Good to Great due to Collins' protocol for matching cases and controls.
There have been several other efforts, using different methods, to determine organizational predictors of success in healthcare. The results of several important studies are shown in Table 3. Taken together, they indicate that higher performing organizations make practitioners accountable for performance measurements, and implement systems designed to both reduce errors and facilitate adherence to evidence‐based guidelines. In addition to these studies, several consulting organizations and foundations have performed focused reviews of high‐performing healthcare organizations in an effort to identify key success factors.11 These studies, while elucidating factors that influence organizational performance, suffer from variable quality measures and subjective methods for gathering organizational data, both of which are addressed within a good to great‐style analysis.12
| Study | Key Findings |
|---|---|
| |
| Keroack et al.10 | Superior‐performing organizations were distinguished from average ones by having: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, concrete accountability structures for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration toward quality improvement measures. |
| Jha et al.22 | Factors that led to the VA's improved performance included: |
| Implementation of a systematic approach to measurement, management, and accountability for quality. | |
| Initiating routine performance measurements for high‐priority conditions. | |
| Creating performance contracts to hold managers accountable for meeting improvement goals. | |
| Having an independent agency gather and monitor data. | |
| Implementing process improvements, such as an integrated, comprehensive medical‐record system. | |
| Making performance data public and distributing these data widely within the VA and among other key stakeholders (veterans' service organizations, Congress). | |
| Shortell et al.20 | Focusing on reducing the barriers and encouraging the adoption of evidence‐based organizational management is associated with better patient outcomes. Examples of reducing barriers to encourage adoption of evidence‐based guidelines include: |
| Installing an IT system to improve chronic care management. | |
| Creating a culture where practitioners can help each other learn from their mistakes. | |
| Knaus et al.21 | The interaction and coordination of each hospital's ICU staff had a greater correlation with reduced mortality rates than did the unit's administrative structure, amount of specialized treatment used, or the hospital's teaching status. |
| Pronovost et al.3 | Introducing a checklist of 5 evidence‐based procedures into a healthcare team's operation can significantly reduce the rate of catheter‐associated infections. |
| Simple process change interventions, such as checklists, must be accompanied by efforts to improve team culture and create leadership accountability and engagement. | |
| Pronovost et al.30 | Implementing evidence‐based therapies by embedding them within a healthcare team's culture is more effective than simply focusing on changing physician behavior. |
| The authors proposed a 4‐step model for implementing evidence‐based therapies: select interventions with the largest benefit and lowest barriers to use, identify local barriers to implementation, measure performance, and ensure all patients receive the interventions. | |
Perhaps the best‐known study on healthcare organizational performance is The Dartmouth Atlas, an analysis that (though based on data accumulated over more than 30 years) has received tremendous public attention, in recent years, in the context of the debate over healthcare reform.13 However, by early 2010, the Dartmouth analysis was stirring controversy, with some observers expressing concerns over its focus on care toward the end of life, its methods for adjusting for case‐mix and sociodemographic predictors of outcomes and costs, and its exclusive use of Medicare data.14, 15 These limitations are also addressed by a good to great‐style analysis.
WOULD A GOOD TO GREAT ANALYSIS BE POSSIBLE IN HEALTHCARE?
While this review of prior research on organizational success factors in healthcare illustrates considerable interest in this area, none of the studies, to date, matches Good to Great in the robustness of the analysis or, obviously, its impact on the profession. Could a good to great analysis be carried out in healthcare? It is worth considering this by assessing each of Collins' 3 key steps: identifying the enterprises that made a good to great leap, selecting appropriate control organizations, and determining the factors that contributed to the successes of the former group.
Good to Great used an impressive elevation in stock price as a summary measure of organizational success. In the for‐profit business world, it is often assumed that Adam Smith's invisible hand makes corporate information available to investors, causing an organization's stock price to capture the overall success of its business strategy, including its product quality and operational efficiency.16 In the healthcare world, mostly populated by non‐profit organizations that are simultaneously working toward a bottom line and carrying out a social mission, there is no obvious equivalent to the stock price for measuring overall organizational performance and value. All of the methods for judging top hospitals, for example, are flaweda recent study found that the widely cited U.S. News & World Report's America's Best Hospitals list is largely driven by hospital reputation,17 while another study found glaring inconsistencies among methods used to calculate risk‐adjusted mortality rates.18 A generally accepted set of metrics defining the value of care produced by a healthcare organization (including quality, safety, access, patient satisfaction, and efficiency) would be needed to mirror the first good to great step: defining top‐performing organizations using a gold standard.19 The summary measure used in the UHC study is the closest we have seen to a good to great‐style summary performance measure in healthcare.10
While it is important to identify a gold‐standard measure of organizational quality, careful selection of a control organization may be the most important step in conducting a good to great analysis. Although Collins' use of stock price as a summary measure of organizational performance is the best measure available in business, it is by no means perfect. Despite this shortcoming, however, Collins believes that the central requirement is not finding a perfect measure of organizational success, but rather determining what correlates with a divergence of performance in stock price (J. Collins, oral communication, July 2010). Similar to clinical trials, meticulous matching of a good to great organization with a control has the advantage of canceling out extraneous environmental factors, thereby enabling the elucidation of organizational factors that contribute to divergent performance. Good to Great's methods depended on substantial historical background to define top performers and controls. Unfortunately, healthcare lacks an analog to the business world's robust historical and publicly accessible record of performance and organizational data. Therefore, even if a certain organization was determined to be a top performer based on a gold‐standard measure, selecting a control organization by matching its organizational and performance data to the top performer's would be unfeasible.
Finally, the lack of a historical record in healthcare also places substantial roadblocks in the way of looking under the organization's hood. Even in pioneering organizational analyses by Shortell et al.,20 Knaus et al.,21 and Jha et al.,22 substantial parts of their analyses relied on retrospective accounts to determine organizational characteristics. To remove the bias that comes from knowing the organization's ultimate performance, Collins was careful to base his analysis of organizational structures and leadership on documents available before the good to great transition. Equivalent data in healthcare are extremely difficult to find.
While it is best to rely on an historical record, it may be possible to carry out a good to great‐type analysis through meticulous structuring of personal interviews. Collins has endorsed a non‐healthcare study that utilized the good to great matching strategy but used personal interviews to make up for lack of access to a substantial historical record.23 To reduce the bias inherent in relying on interviews, the research team ensured that the good to great transition was sustained for many years, and that the practices elicited from the interviews started before the good to great transition. Both of these techniques helped increase the probability that the identified practices contributed to the transition to superior results (in this case, in public education outcomes) and, thus, that the adoption of these practices could result in improvements elsewhere (J. Collins, oral communication, July 2010).
To make such a study possible in healthcare, more organizational data are required. Without prodding by outside stakeholders, most healthcare organizations have been reluctant to publicize performance data for fear of malpractice risk,24 or based on their belief that current data paint an incomplete or inaccurate picture of their quality.25 Trends toward required reporting of quality data (such as via Medicare's Hospital Compare Web site) offer hope that future comparisons could rely on robust organizational quality and safety data. Instituting healthcare analogs to Securities & Exchange Commission (SEC) reporting mandates would further ameliorate this information deficit.26
While we believe that Good to Great offers lessons relevant to healthcare, there are limitations that are worth considering. First, the extraordinary complexity of healthcare organizations makes it likely that a matched‐pair‐type study would need to be accompanied by other types of analyses, including more quantitative analyses of large datasets, to give a full picture of structural and leadership predictors of strong performance. Moreover, before embracing the good to great method, some will undoubtedly point to the demise of Circuit City and Fannie Mae (2 of the Good to Great companies; Table 2) as a cautionary note. Collins addresses this issue with the commonsensical argument that the success of a company needs to be judged in the context of the era. By way of analogy, he points to the value of studying a sports team, such as the John Wooden‐coached UCLA teams of the 1960s and 1970s, notwithstanding the less stellar performance of today's UCLA team. In fact, Collins' recent book mines some of these failures for their important lessons.27
GOOD TO GREAT IN HEALTHCARE
Breaking through healthcare's myopia to explore solutions drawn from other industries, such as checklists, simulation, and industrial approaches to quality improvement, has yielded substantial insights and catalyzed major improvements in care. Similarly, we believe that finding ways to measure the performance of healthcare organizations on both cost and quality, to learn from those organizations achieving superior performance, and to create a policy and educational environment that rewards superior performance and helps poor performers improve, is a defining issue for healthcare. This will be particularly crucial as the policy environment changestransitions to Accountable Care Organizations28 and bundled payments29 are likely to increase the pressure on healthcare organizations to learn the secrets of their better‐performing brethren. These shifts are likely to put an even greater premium on the kinds of leadership, organizational structure, and ability to adapt to a changing environment that Collins highlighted in his analysis. After all, it is under the most challenging conditions that top organizations often prove their mettle.
Although there are considerable challenges in performing a good to great analysis in healthcare (Table 4), the overall point remains: Healthcare is likely to benefit from rigorous, unbiased methods to distinguish successful from less successful organizations, to learn the lessons of both, and to apply these lessons to improvement efforts.
| Issue* | Good to Great* | What Exists in Healthcare | How Healthcare Can Fill in the Gaps |
|---|---|---|---|
| |||
| Gold standard measure of quality | Cumulative total stock return of at least 3 times the general market for the period from the transition point through 15 years. | Risk‐adjusted patient outcomes data (eg, mortality), process data (eg, appropriate medication use), structural data (eg, stroke center). | Create a more robust constellation of quality criteria to measure organizational performance (risk‐adjusted patient outcomes, avoidable deaths, adherence to evidence‐based guidelines, cost effectiveness, patient satisfaction); develop a generally accepted roll‐up measure. Of the studies we reviewed, the UHC study's summary measure was the closest representation to a good to great‐summary performance measure. |
| At the time of the selection, the good to great company still had to show an upward trend. | The study of the VA's transformation and the ongoing UHC study stand out as examples of studying the upward trends of healthcare organizations.22 | Make sure that the high‐performing healthcare organizations are still improvingas indicated by gold standard measures. Once the organizations are identified, study the methods these organizations utilized to improve their performance. | |
| The turnaround had to be company‐specific, not an industry‐wide event. | A few organizations have been lauded for transformations (such as the VA system).22 In most circumstances, organizations praised for high quality (eg, Geisinger, Mayo Clinic, Cleveland Clinic) have long‐established corporate tradition and culture that would be difficult to imitate. The VA operates within a system that is unique and not replicable by most healthcare organizations. | Healthcare needs to identify more examples like the VA turnaround, particularly examples of hospitals or healthcare organizations operating in more typical environmentssuch as a community or rural hospital. | |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. | Most of the healthcare organizations of interest are large organizations with complex corporate cultures, not startups. | Not applicable. | |
| Comparison method | Collins selected a comparison company that was almost exactly the same as the good to great company, except for the transition. The selection criteria were business fit, size fit, age fit, stock chart fit, conservative test, and face validity.* | Healthcare organizational studies are mostly comparisons of organizations that all experience success; few studies compare high‐performing with nonhigh‐performing organizations. (Jha et al. compared Medicare data from non‐VA hospitals and the VA, but did not use similar criteria to select similar organizations22; Keroack and colleagues' comparison of 3 mediocre to 3 superior‐performing hospitals is the closest analog to the Good to Great methodology thus far.10) | Similar to the Good to Great study, a set of factors that can categorize healthcare organizations according to similarities must be devised (eg, outpatient care, inpatient care, academic affiliation, tertiary care center, patient demographics), but finding similar organizations whose performance diverged over time is challenging. |
| Analysis of factors that separated great companies from those that did not make the transition to greatness | Good to Great used annual reports, letters to shareholders, articles written about the company during the period of interest, books about the company, business school case studies, analyst reports written in real time. | Most of the research conducted thus far has been retrospective analyses of why organizations became top performers. | The historical source of data is almost nonexistent in comparison with the business world. A parallel effort would have to capture a mixture of structure and process changes, along with organizational variables. The most effective method would be a prospective organizational assessment of several organizations, following them over time to see which ones markedly improved their performance. |
The American healthcare system produces a product whose quality, safety, reliability, and cost would be incompatible with corporate survival, were they created by a business operating in a competitive industry. Care fails to comport with best evidence nearly half of the time.1 Tens of thousands of Americans die yearly from preventable medical mistakes.2 The healthcare inflation rate is nearly twice that of the rest of the economy, rapidly outstripping the ability of employers, tax revenues, and consumers to pay the mounting bills.
Increasingly, the healthcare system is being held accountable for this lack of value. Whether through a more robust accreditation and regulatory environment, public reporting of quality and safety metrics, or pay for performance (or no pay for errors) initiatives, outside stakeholders are creating performance pressures that scarcely existed a decade ago.
Healthcare organizations and providers have begun to take notice and act, often by seeking answers from industries outside healthcare and thoughtfully importing these lessons into medicine. For example, the use of checklists has been adopted by healthcare (from aviation), with impressive results.3, 4 Many quality methods drawn from industry (Lean, Toyota, Six Sigma) have been used to try to improve performance and remove waste from complex processes.5, 6
While these efforts have been helpful, their focus has generally been at the point‐of‐careimproving the care of patients with acute myocardial infarction or decreasing readmissions. However, while the business community has long recognized that poor management and structure can thwart most efforts to improve individual processes, healthcare has paid relatively little attention to issues of organizational structure and leadership. The question arises: Could methods that have been used to learn from top‐performing businesses be helpful to healthcare's efforts to improve its own organizational performance?
In this article, we describe perhaps the best known effort to identify top‐performing corporations, compare them to carefully selected organizations that failed to achieve similar levels of performance, and glean lessons from these analyses. This effort, described in a book entitled Good to Great: Why Some Companies Make the Leapand Others Don't, has sold more than 3 million copies in its 35 languages, and is often cited by business leaders as a seminal work. We ask whether the methods of Good to Great might be applicable to healthcare organizations seeking to produce the kinds of value that patients and purchasers need and deserve.
GOOD TO GREAT METHODOLOGY
In 2001, business consultant Jim Collins published Good to Great. Its methods can be divided into 3 main components: (1) a gold standard metric to identify top organizations; (2) the creation of a control group of organizations that appeared similar to the top performers at the start of the study, but failed to match the successful organizations' performance over time; and (3) a detailed review of the methods, leadership, and structure of both the winning and laggard organizations, drawing lessons from their differences. Before discussing whether these methods could be used to analyze healthcare organizations, it is worth describing Collins' methods in more detail.
The first component of Good to Great's structure was the use of 4 metrics to identify top‐performing companies (Table 1). To select the good to great companies, Collins and his team began with a field of 1435 companies drawn from Fortune magazine's rankings of America's largest public companies. They then used the criteria in Table 1 to narrow the list to their final 11 companies, which formed the experimental group for the analysis.
|
| The company had to show a pattern of good performance punctuated by a transition point when it shifted to great performance. Great performance was defined as a cumulative total stock return of at least 3 times the general stock market for the period from the transition point through 15 years. |
| The transition from good to great had to be company‐specific, not an industry‐wide event. |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. |
| At the time of the selection (in 1996), the company still had to show an upward trend. |
After identifying these 11 top‐performing companies, Collins created a control group, composed of companies with similar attributes that could have made the transition, but failed to do so.7 To create the control group, Collins matched and scored a pool of control group candidates based on the following criteria: similarities of business model, size, age, and cumulative stock returns prior to the good to great transition. When there were several potential controls, Collins chose companies that were larger, more profitable, and had a stronger market position and reputation prior to the transition, in order to increase the probability that the experimental companies' successes were not incidental.8 Table 2 lists the paired experimental and control companies.
| Experimental Company | Control Company |
|---|---|
| |
| Abbott | Upjohn |
| Circuit City | Silo |
| Fannie Mae | Great Western |
| Gillette | Warner‐Lambert |
| Kimberly‐Clark | Scott Paper |
| Kroger | A&P |
| Nucor | Bethlehem Steel |
| Philip Morris | R.J. Reynolds |
| Pitney Bowes | Addressograph |
| Walgreen's | Eckerd |
| Wells Fargo | Bank of America |
Finally, Collins performed a detailed historical analysis on the experimental and control groups, using materials (such as major articles published on the company, books, academic case studies, analyst reports, and financial and annual reports) that assessed the companies in real time. Good to Great relied on evidence from the period of interest (ie, accrued prior to the transition point) to avoid biases that would likely result from relying on retrospective sources of data.9
This analysis identified a series of factors that were generally present in good to great companies and absent in the control organizations. In brief, they were: building a culture of discipline, making change through gradual and consistent improvement, having a leader with a paradoxical blend of personal humility and professional will, and relentlessly focusing on hiring and nurturing the best employees. Over 6000 articles and 5 years of analysis support these conclusions.8
EFFORTS TO DATE TO ANALYZE HEALTHCARE ORGANIZATIONAL CHARACTERISTICS
We reviewed a convenience sample of the literature on organizational change in healthcare, and found only 1 study that utilized a similar methodology to that of Good to Great: an analysis of the academic medical centers that participate in the University HealthSystem Consortium (UHC). Drawing inspiration from Collins' methodologies, the UHC study developed a holistic measure of quality, based on safety, mortality, compliance with evidence‐based practices, and equity of care. Using these criteria, the investigators selected 3 UHC member organizations that were performing extremely well, and 3 others performing toward the middle and bottom of the pack. Experts on health system organization then conducted detailed site visits to these 6 academic medical centers. The researchers were blinded to these rankings at the time of the visits, but were able to perfectly predict which cohort the organizations were in.
The investigators analyzed the factors that seemed to be present in the top‐performing organizations, but were absent in the laggards, and found: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, a concrete accountability structure for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration on quality.10
While the UHC study is among the most robust exploration of healthcare organization dynamics in the literature, it has a few limitations. The first is that it studied a small, relatively specialized population: UHC members, which are large, mostly urban, well‐resourced teaching hospitals. While studying segments of populations can limit the generalizability of some of the UHC studies' findings, their approach can be a useful model to apply to studying other types of healthcare institutions. (And, to be fair, Good to Great also studies a specialized populationFortune 500 companiesand thus its lessons need to be extrapolated to other businesses, such as small companies, with a degree of caution.) The study also suffers from the relative paucity of publicly accessible organizational data in healthcare. The fact that the UHC investigators depended on both top‐performing and laggard hospitals, to voluntarily release their organizational data and permit a detailed site visit, potentially introduces a selection bias into the survey population, a bias not present in Good to Great due to Collins' protocol for matching cases and controls.
There have been several other efforts, using different methods, to determine organizational predictors of success in healthcare. The results of several important studies are shown in Table 3. Taken together, they indicate that higher performing organizations make practitioners accountable for performance measurements, and implement systems designed to both reduce errors and facilitate adherence to evidence‐based guidelines. In addition to these studies, several consulting organizations and foundations have performed focused reviews of high‐performing healthcare organizations in an effort to identify key success factors.11 These studies, while elucidating factors that influence organizational performance, suffer from variable quality measures and subjective methods for gathering organizational data, both of which are addressed within a good to great‐style analysis.12
| Study | Key Findings |
|---|---|
| |
| Keroack et al.10 | Superior‐performing organizations were distinguished from average ones by having: hospital leadership emphasizing a patients‐first mission, an alignment of departmental objectives to reduce conflict, concrete accountability structures for quality, a relentless focus on measurable improvement, and a culture promoting interprofessional collaboration toward quality improvement measures. |
| Jha et al.22 | Factors that led to the VA's improved performance included: |
| Implementation of a systematic approach to measurement, management, and accountability for quality. | |
| Initiating routine performance measurements for high‐priority conditions. | |
| Creating performance contracts to hold managers accountable for meeting improvement goals. | |
| Having an independent agency gather and monitor data. | |
| Implementing process improvements, such as an integrated, comprehensive medical‐record system. | |
| Making performance data public and distributing these data widely within the VA and among other key stakeholders (veterans' service organizations, Congress). | |
| Shortell et al.20 | Focusing on reducing the barriers and encouraging the adoption of evidence‐based organizational management is associated with better patient outcomes. Examples of reducing barriers to encourage adoption of evidence‐based guidelines include: |
| Installing an IT system to improve chronic care management. | |
| Creating a culture where practitioners can help each other learn from their mistakes. | |
| Knaus et al.21 | The interaction and coordination of each hospital's ICU staff had a greater correlation with reduced mortality rates than did the unit's administrative structure, amount of specialized treatment used, or the hospital's teaching status. |
| Pronovost et al.3 | Introducing a checklist of 5 evidence‐based procedures into a healthcare team's operation can significantly reduce the rate of catheter‐associated infections. |
| Simple process change interventions, such as checklists, must be accompanied by efforts to improve team culture and create leadership accountability and engagement. | |
| Pronovost et al.30 | Implementing evidence‐based therapies by embedding them within a healthcare team's culture is more effective than simply focusing on changing physician behavior. |
| The authors proposed a 4‐step model for implementing evidence‐based therapies: select interventions with the largest benefit and lowest barriers to use, identify local barriers to implementation, measure performance, and ensure all patients receive the interventions. | |
Perhaps the best‐known study on healthcare organizational performance is The Dartmouth Atlas, an analysis that (though based on data accumulated over more than 30 years) has received tremendous public attention, in recent years, in the context of the debate over healthcare reform.13 However, by early 2010, the Dartmouth analysis was stirring controversy, with some observers expressing concerns over its focus on care toward the end of life, its methods for adjusting for case‐mix and sociodemographic predictors of outcomes and costs, and its exclusive use of Medicare data.14, 15 These limitations are also addressed by a good to great‐style analysis.
WOULD A GOOD TO GREAT ANALYSIS BE POSSIBLE IN HEALTHCARE?
While this review of prior research on organizational success factors in healthcare illustrates considerable interest in this area, none of the studies, to date, matches Good to Great in the robustness of the analysis or, obviously, its impact on the profession. Could a good to great analysis be carried out in healthcare? It is worth considering this by assessing each of Collins' 3 key steps: identifying the enterprises that made a good to great leap, selecting appropriate control organizations, and determining the factors that contributed to the successes of the former group.
Good to Great used an impressive elevation in stock price as a summary measure of organizational success. In the for‐profit business world, it is often assumed that Adam Smith's invisible hand makes corporate information available to investors, causing an organization's stock price to capture the overall success of its business strategy, including its product quality and operational efficiency.16 In the healthcare world, mostly populated by non‐profit organizations that are simultaneously working toward a bottom line and carrying out a social mission, there is no obvious equivalent to the stock price for measuring overall organizational performance and value. All of the methods for judging top hospitals, for example, are flaweda recent study found that the widely cited U.S. News & World Report's America's Best Hospitals list is largely driven by hospital reputation,17 while another study found glaring inconsistencies among methods used to calculate risk‐adjusted mortality rates.18 A generally accepted set of metrics defining the value of care produced by a healthcare organization (including quality, safety, access, patient satisfaction, and efficiency) would be needed to mirror the first good to great step: defining top‐performing organizations using a gold standard.19 The summary measure used in the UHC study is the closest we have seen to a good to great‐style summary performance measure in healthcare.10
While it is important to identify a gold‐standard measure of organizational quality, careful selection of a control organization may be the most important step in conducting a good to great analysis. Although Collins' use of stock price as a summary measure of organizational performance is the best measure available in business, it is by no means perfect. Despite this shortcoming, however, Collins believes that the central requirement is not finding a perfect measure of organizational success, but rather determining what correlates with a divergence of performance in stock price (J. Collins, oral communication, July 2010). Similar to clinical trials, meticulous matching of a good to great organization with a control has the advantage of canceling out extraneous environmental factors, thereby enabling the elucidation of organizational factors that contribute to divergent performance. Good to Great's methods depended on substantial historical background to define top performers and controls. Unfortunately, healthcare lacks an analog to the business world's robust historical and publicly accessible record of performance and organizational data. Therefore, even if a certain organization was determined to be a top performer based on a gold‐standard measure, selecting a control organization by matching its organizational and performance data to the top performer's would be unfeasible.
Finally, the lack of a historical record in healthcare also places substantial roadblocks in the way of looking under the organization's hood. Even in pioneering organizational analyses by Shortell et al.,20 Knaus et al.,21 and Jha et al.,22 substantial parts of their analyses relied on retrospective accounts to determine organizational characteristics. To remove the bias that comes from knowing the organization's ultimate performance, Collins was careful to base his analysis of organizational structures and leadership on documents available before the good to great transition. Equivalent data in healthcare are extremely difficult to find.
While it is best to rely on an historical record, it may be possible to carry out a good to great‐type analysis through meticulous structuring of personal interviews. Collins has endorsed a non‐healthcare study that utilized the good to great matching strategy but used personal interviews to make up for lack of access to a substantial historical record.23 To reduce the bias inherent in relying on interviews, the research team ensured that the good to great transition was sustained for many years, and that the practices elicited from the interviews started before the good to great transition. Both of these techniques helped increase the probability that the identified practices contributed to the transition to superior results (in this case, in public education outcomes) and, thus, that the adoption of these practices could result in improvements elsewhere (J. Collins, oral communication, July 2010).
To make such a study possible in healthcare, more organizational data are required. Without prodding by outside stakeholders, most healthcare organizations have been reluctant to publicize performance data for fear of malpractice risk,24 or based on their belief that current data paint an incomplete or inaccurate picture of their quality.25 Trends toward required reporting of quality data (such as via Medicare's Hospital Compare Web site) offer hope that future comparisons could rely on robust organizational quality and safety data. Instituting healthcare analogs to Securities & Exchange Commission (SEC) reporting mandates would further ameliorate this information deficit.26
While we believe that Good to Great offers lessons relevant to healthcare, there are limitations that are worth considering. First, the extraordinary complexity of healthcare organizations makes it likely that a matched‐pair‐type study would need to be accompanied by other types of analyses, including more quantitative analyses of large datasets, to give a full picture of structural and leadership predictors of strong performance. Moreover, before embracing the good to great method, some will undoubtedly point to the demise of Circuit City and Fannie Mae (2 of the Good to Great companies; Table 2) as a cautionary note. Collins addresses this issue with the commonsensical argument that the success of a company needs to be judged in the context of the era. By way of analogy, he points to the value of studying a sports team, such as the John Wooden‐coached UCLA teams of the 1960s and 1970s, notwithstanding the less stellar performance of today's UCLA team. In fact, Collins' recent book mines some of these failures for their important lessons.27
GOOD TO GREAT IN HEALTHCARE
Breaking through healthcare's myopia to explore solutions drawn from other industries, such as checklists, simulation, and industrial approaches to quality improvement, has yielded substantial insights and catalyzed major improvements in care. Similarly, we believe that finding ways to measure the performance of healthcare organizations on both cost and quality, to learn from those organizations achieving superior performance, and to create a policy and educational environment that rewards superior performance and helps poor performers improve, is a defining issue for healthcare. This will be particularly crucial as the policy environment changestransitions to Accountable Care Organizations28 and bundled payments29 are likely to increase the pressure on healthcare organizations to learn the secrets of their better‐performing brethren. These shifts are likely to put an even greater premium on the kinds of leadership, organizational structure, and ability to adapt to a changing environment that Collins highlighted in his analysis. After all, it is under the most challenging conditions that top organizations often prove their mettle.
Although there are considerable challenges in performing a good to great analysis in healthcare (Table 4), the overall point remains: Healthcare is likely to benefit from rigorous, unbiased methods to distinguish successful from less successful organizations, to learn the lessons of both, and to apply these lessons to improvement efforts.
| Issue* | Good to Great* | What Exists in Healthcare | How Healthcare Can Fill in the Gaps |
|---|---|---|---|
| |||
| Gold standard measure of quality | Cumulative total stock return of at least 3 times the general market for the period from the transition point through 15 years. | Risk‐adjusted patient outcomes data (eg, mortality), process data (eg, appropriate medication use), structural data (eg, stroke center). | Create a more robust constellation of quality criteria to measure organizational performance (risk‐adjusted patient outcomes, avoidable deaths, adherence to evidence‐based guidelines, cost effectiveness, patient satisfaction); develop a generally accepted roll‐up measure. Of the studies we reviewed, the UHC study's summary measure was the closest representation to a good to great‐summary performance measure. |
| At the time of the selection, the good to great company still had to show an upward trend. | The study of the VA's transformation and the ongoing UHC study stand out as examples of studying the upward trends of healthcare organizations.22 | Make sure that the high‐performing healthcare organizations are still improvingas indicated by gold standard measures. Once the organizations are identified, study the methods these organizations utilized to improve their performance. | |
| The turnaround had to be company‐specific, not an industry‐wide event. | A few organizations have been lauded for transformations (such as the VA system).22 In most circumstances, organizations praised for high quality (eg, Geisinger, Mayo Clinic, Cleveland Clinic) have long‐established corporate tradition and culture that would be difficult to imitate. The VA operates within a system that is unique and not replicable by most healthcare organizations. | Healthcare needs to identify more examples like the VA turnaround, particularly examples of hospitals or healthcare organizations operating in more typical environmentssuch as a community or rural hospital. | |
| The company had to be an established enterprise, not a startup, in business for at least 10 years prior to its transition. | Most of the healthcare organizations of interest are large organizations with complex corporate cultures, not startups. | Not applicable. | |
| Comparison method | Collins selected a comparison company that was almost exactly the same as the good to great company, except for the transition. The selection criteria were business fit, size fit, age fit, stock chart fit, conservative test, and face validity.* | Healthcare organizational studies are mostly comparisons of organizations that all experience success; few studies compare high‐performing with nonhigh‐performing organizations. (Jha et al. compared Medicare data from non‐VA hospitals and the VA, but did not use similar criteria to select similar organizations22; Keroack and colleagues' comparison of 3 mediocre to 3 superior‐performing hospitals is the closest analog to the Good to Great methodology thus far.10) | Similar to the Good to Great study, a set of factors that can categorize healthcare organizations according to similarities must be devised (eg, outpatient care, inpatient care, academic affiliation, tertiary care center, patient demographics), but finding similar organizations whose performance diverged over time is challenging. |
| Analysis of factors that separated great companies from those that did not make the transition to greatness | Good to Great used annual reports, letters to shareholders, articles written about the company during the period of interest, books about the company, business school case studies, analyst reports written in real time. | Most of the research conducted thus far has been retrospective analyses of why organizations became top performers. | The historical source of data is almost nonexistent in comparison with the business world. A parallel effort would have to capture a mixture of structure and process changes, along with organizational variables. The most effective method would be a prospective organizational assessment of several organizations, following them over time to see which ones markedly improved their performance. |
- ,,, et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- ,,;for the Institute of Medicine (US), Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999. Available at: http://www.nap.edu/books/0309068371/html/. Accessed August 22, 2011.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Using industrial processes to improve patient care.BMJ.2004;328(7432):162–164.
- ,,,,.Lean six sigma in healthcare.J Healthc Qual.2006;28(2):4–11.
- .Good to great.Fast Company. September 30,2001. Available at: http://www.fastcompany.com/magazine/51/goodtogreat.html. Accessed August 22, 2011.
- .Good to Great: Why Some Companies Make the Leap… and Others Don't.New York, NY:HarperBusiness;2001.
- .It's in the research.Jim Collins. Available at: http://www.jimcollins.com/books/research.html. Accessed May 23,2010.
- ,,,,,.Organizational factors associated with high performance in quality and safety in academic medical centers.Acad Med.2007;82(12):1178–1186.
- ,,,,.Hosptial Quality: Ingredients for Success—a Case Study of Beth Israel Deaconess Medical Center.New York, NY:Commonwealth Fund;2004. Available at: http://www.commonwealthfund.org/Content/Publications/Fund‐Reports/2004/Jul/Hospital‐Quality–Ingredients‐for‐Success‐A‐Case‐Study‐of‐Beth‐Israel‐Deaconess‐Medical‐Center. aspx. Accessed August 22, 2011.
- ,,;for the Commonwealth Fund.Hospital quality improvement strategies and lessons from U.S. hospitals.New York, NY:Commonwealth Fund;2007. Available at: http://www.commonwealthfund.org/usr_doc/Silow‐Carroll_hosp_quality_ improve_strategies_lessons_1009.pdf?section=4039. Accessed August 22, 2011.
- .The cost conundrum: what a Texas town can teach us about healthcare.The New Yorker. June 1,2009.
- .A map to bad policy—hospital efficiency measures in the Dartmouth Atlas.N Engl J Med.2010;362(7):569–574.
- ,.Critics question study cited in health debate.The New York Times. June 2,2010.
- Smith A. Campbell RH, Skinner AS, eds.An Inquiry Into the Nature and Causes of the Wealth of Nations.Oxford, England:Clarendon Press;1976.
- .The role of reputation in U.S. News 152(8):521–525.
- ,,,,.Variability in the measurement of hospital‐wide mortality rates.N Engl J Med.2010;363(26):2530–2539.
- .The elephant of patient safety: what you see depends on how you look.Jt Comm J Qual Patient Saf.2010;36(9):399–401.
- ,,.Improving patient care by linking evidence‐based medicine and evidence‐based management.JAMA.2007;298(6):673–676.
- ,,,.An evaluation of outcome from intensive care in major medical centers.Ann Intern Med.1986;104(3):410–418.
- ,,,.Effect of the transformation of the Veterans Affairs Health Care System on the quality of care.N Engl J Med.2003;348(22):2218–2227.
- ;for the Morrison Institute for Public Policy, Center for the Future of Arizona.Why Some Schools With Latino Children Beat the Odds, and Others Don't.Tempe, AZ:Morrison Institute for Public Policy;2006.
- ,,, et al.Error reporting and disclosure systems: views from hospital leaders.JAMA.2005;293(11):1359–1366.
- .Public release of performance data: a progress report from the front.JAMA.2000;283(14):1884–1886.
- ,,.The GAAP in quality measurement and reporting.JAMA.2007;298(15):1800–1802.
- .How the Mighty Fall: And Why Some Companies Never Give in.New York, NY:Jim Collins [distributed in the US and Canada exclusively by HarperCollins Publishers];2009.
- ,,,.Creating accountable care organizations: the extended hospital medical staff.Health Aff (Millwood).2007;26(1):w44–w57.
- ,,,.Using Medicare payment policy to transform the health system: a framework for improving performance.Health Aff (Millwood).2009;28(2):w238–w250.
- ,,.Translating evidence into practice: a model for large scale knowledge translation.BMJ.2008;337:a1714.
- ,,, et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- ,,;for the Institute of Medicine (US), Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999. Available at: http://www.nap.edu/books/0309068371/html/. Accessed August 22, 2011.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Using industrial processes to improve patient care.BMJ.2004;328(7432):162–164.
- ,,,,.Lean six sigma in healthcare.J Healthc Qual.2006;28(2):4–11.
- .Good to great.Fast Company. September 30,2001. Available at: http://www.fastcompany.com/magazine/51/goodtogreat.html. Accessed August 22, 2011.
- .Good to Great: Why Some Companies Make the Leap… and Others Don't.New York, NY:HarperBusiness;2001.
- .It's in the research.Jim Collins. Available at: http://www.jimcollins.com/books/research.html. Accessed May 23,2010.
- ,,,,,.Organizational factors associated with high performance in quality and safety in academic medical centers.Acad Med.2007;82(12):1178–1186.
- ,,,,.Hosptial Quality: Ingredients for Success—a Case Study of Beth Israel Deaconess Medical Center.New York, NY:Commonwealth Fund;2004. Available at: http://www.commonwealthfund.org/Content/Publications/Fund‐Reports/2004/Jul/Hospital‐Quality–Ingredients‐for‐Success‐A‐Case‐Study‐of‐Beth‐Israel‐Deaconess‐Medical‐Center. aspx. Accessed August 22, 2011.
- ,,;for the Commonwealth Fund.Hospital quality improvement strategies and lessons from U.S. hospitals.New York, NY:Commonwealth Fund;2007. Available at: http://www.commonwealthfund.org/usr_doc/Silow‐Carroll_hosp_quality_ improve_strategies_lessons_1009.pdf?section=4039. Accessed August 22, 2011.
- .The cost conundrum: what a Texas town can teach us about healthcare.The New Yorker. June 1,2009.
- .A map to bad policy—hospital efficiency measures in the Dartmouth Atlas.N Engl J Med.2010;362(7):569–574.
- ,.Critics question study cited in health debate.The New York Times. June 2,2010.
- Smith A. Campbell RH, Skinner AS, eds.An Inquiry Into the Nature and Causes of the Wealth of Nations.Oxford, England:Clarendon Press;1976.
- .The role of reputation in U.S. News 152(8):521–525.
- ,,,,.Variability in the measurement of hospital‐wide mortality rates.N Engl J Med.2010;363(26):2530–2539.
- .The elephant of patient safety: what you see depends on how you look.Jt Comm J Qual Patient Saf.2010;36(9):399–401.
- ,,.Improving patient care by linking evidence‐based medicine and evidence‐based management.JAMA.2007;298(6):673–676.
- ,,,.An evaluation of outcome from intensive care in major medical centers.Ann Intern Med.1986;104(3):410–418.
- ,,,.Effect of the transformation of the Veterans Affairs Health Care System on the quality of care.N Engl J Med.2003;348(22):2218–2227.
- ;for the Morrison Institute for Public Policy, Center for the Future of Arizona.Why Some Schools With Latino Children Beat the Odds, and Others Don't.Tempe, AZ:Morrison Institute for Public Policy;2006.
- ,,, et al.Error reporting and disclosure systems: views from hospital leaders.JAMA.2005;293(11):1359–1366.
- .Public release of performance data: a progress report from the front.JAMA.2000;283(14):1884–1886.
- ,,.The GAAP in quality measurement and reporting.JAMA.2007;298(15):1800–1802.
- .How the Mighty Fall: And Why Some Companies Never Give in.New York, NY:Jim Collins [distributed in the US and Canada exclusively by HarperCollins Publishers];2009.
- ,,,.Creating accountable care organizations: the extended hospital medical staff.Health Aff (Millwood).2007;26(1):w44–w57.
- ,,,.Using Medicare payment policy to transform the health system: a framework for improving performance.Health Aff (Millwood).2009;28(2):w238–w250.
- ,,.Translating evidence into practice: a model for large scale knowledge translation.BMJ.2008;337:a1714.
A Novel Approach to Physician Shortages
The demand for physician talent is intensifying as the US healthcare system confronts an unprecedented confluence of demographic pressures. Not only will 78 million retiring baby‐boomers require significant healthcare resources, but tens of thousands of practicing physicians will themselves reach retirement age within the next decade.1 At the same time, factors like the large increase in the percentage of female physicians (who are more likely to work part time), the growth of nonpractice opportunities for MDs, and generational demands for greater worklife balance are creating a major supply‐demand mismatch within the physician workforce.2 In this demographic atmosphere, the ability to recruit and retain physician leaders confers tremendous value to healthcare enterprisesboth public and private. Recruiting and retaining strategies already weigh heavily in the most palpable shortage areas, like primary care, but the system faces widespread unmet demand for a variety of specialist and generalist practitioners.36
This article does not address the public policy implications of the upcoming physician shortage, recognition of which will lead to the largest increase in new medical school slots in decades.7 Rather, we set out to illustrate how successful nonmedical businesses are embracing a thoughtful, systematic approach to retaining talent, based on the philosophy that keeping and engaging valued employees is more efficient than recruiting and orienting replacements. We posit that the innovations used by progressive companies could apply to recruitment and retention challenges confronting medicine.
How Industry Approaches the Talent Vacuum: Talent Facilitation
Leaders outside of medicine have long acknowledged that changing demographics and a global economy are driving unprecedented employee turnover.8 In confronting a talent vacuum, forward‐thinking managers have prioritized retaining key talent (rather than hiring anew) in planning for the future.9, 10 Doing so begins with attempts to understand the relationship between workers and the workplace, with a particular emphasis on appreciating workers' priorities. Indeed, new executive positions with titles like Chief Learning Officer and Chief Experience Officer are appearing as companies realize a need for focused expertise beyond traditional human resource departments. These companies understand that offering higher salaries is not the only retention strategyand often not even the most effective one.
The Four Actions of Talent Facilitation
The talent facilitation process centers on four actions: attract, engage, develop, and retain. None of these actions can stand alone, and all should be present, to some degree, at all stages of a worker's tenure. To attract or engage an employee or practice partner is not a 1‐time hook, but a constant and dynamic process.
Importantly, the concepts addressed here are not specific to 1 type of corporate system, size, or management level. Although the early business focus had been on upper‐level and executive talent within large corporate settings, there is an increasing recognition that a dedicated talent strategy is useful wherever recruiting and retaining talented people is important (and where is it not?).
The ideas presented here may seem most applicable to leaders of large physician corporations, hospital‐owned physician groups, or large integrated healthcare systems (such as Kaiser) that employ physicians. However, we also believe that the ideas apply across‐the‐board in medicine, including entities such as small, private, physician‐owned groups. We argue that regardless of the exact practice structure, a limited pool of resources must be dedicated to the attraction and retention of talented partners or employees, or to the cost of replacing those people if they pursue other opportunities (or the cost of inefficient and disengaged physicians). While an integrated health system may have the resources and scale to hire a Chief Experience Officer, we do not anticipate that a 5‐partner private practice would. Rather, we point to examples to illustrate the talent facilitation paradigm as a tool to systematically frame the allocation of those resources. Undoubtedly, the specific shape of a thoughtful talent facilitation effort will vary when applied in a large urban academic medical center vs. an integrated healthcare system vs. a small physician private practice, but the basic principles remain the same.
Attract
Increasingly, companies approach talented prospects with dedicated marketing campaigns to convey the value of a work environment.11 Silicon Valley employee lounges with free massages and foosball tables are the iconic example of attraction, but the concept runs deeper. Today's workers seek access to state‐of‐the‐art ideas and technology and often want to be part of a larger vision. Many seek opportunities to integrate their own professional and personal aspirations into a particular job description.
Hospital executives have long recognized the importance of attracting physicians to their facility (after all, the physicians draw patients and thus generate revenue). The traditional approach has surrounded perks, from comfortable doctor's lounges to the latest in surgical technology. But, the stakes seem greater now than before, and successful talent facilitation strategies are going beyond the tried and true.
Clearly, physicians seek financially stable practice settings with historical success. But they may also seek evidence of a defined strategic plan focused on more than mere profitability. Physicians may gravitate to practice environments that endorse progressive movements like the No One Dies Alone campaign.12 Similarly, recognition of movements beyond healthcarea commitment to Leadership in Energy and Environmental Design (LEED) (Green Building Rating System; US Green Building Council [USGBC];
The current recruitment campaign of California's prison healthcare system offers an unlikely source of inspiration. The prison system was placed in receivership to address a shortage of competent physician staff and other inadequacies. A central feature of the campaign is an attractive starting salary and good benefits. But, the campaign does not rely on money alone. For example, the campaign's website (
Engage
The corporate tool being employed at this stage is a strategy called on‐boarding, which emphasizes a streamlined integration of newcomers with existing workers and culture, and prioritizes aligning organizational roles with a worker's specific skills and interests. On‐boarding also emphasizes the value of early and frequent provision of constructive feedback from same‐level peers or managers with advanced coaching skills.
Many companies use formal survey tools to measure employee engagement and regularly evaluate the proficiency of system leaders in the ability to engage their employees. An engineering firm executive recently told us (P.K., C.K.) that he performs detailed and frequent on‐the‐job interviews, even with company veterans. The primary goal of these interviews is to ensure that engineers spend at least 85% of their time on work that: (1) they find interesting and (2) allows for the application of their best skills. Wherever possible, traditional job descriptions are altered to achieve this. Inevitably, there is still work (15% in this particular corporate vision) that no one prefers but needs to get done, but this process of active recalibration minimizes this fraction to the degree possible.
Even within a small physician practice group, one can imagine how a strategic approach of inviting and acknowledging individual physician's professional goals and particular talents may challenge the long‐held belief that everyone within a group enjoys and must do the exact same job. Once these goals and talents are articulated, groups may find that allowing for more customized roles within the practice enhances professional satisfaction.
Social networking, collaboration, and sharing of best practices are staples of engaging companies. The Cisco and Qualcomm companies, for example, utilize elaborate e‐networks (rough corporate equivalents to Facebook) to foster collegial interaction within and across traditional hierarchical boundaries so that managers and executives directly engage the ideas of employees at every level.14 The premise is logical: engaged employees will be more likely to contribute innovative ideas which, when listened to, are more likely to engage employees.
Most physicians will recognize the traditional resident report as a model for engagement. Beyond its educational value, interaction with program leadership, social bonding, collaborative effort, and exploration of best practices add tremendous value. Many companies would jump at the chance to engrain a similar cultural staple. Enhancing this type of interaction in a postresidency setting may promote engagement in a given system, especially if it facilitates interactions between physicians and senior hospital leaders. Absent these types of interactions, ensuring regular provision of peer review and/or constructive feedback can help systematically enhance 2‐way communication and enhance engagement.
Develop
Talent development relies on mentorship reflecting a genuine interest in an individual's future. Development strategies include pairing formal annual talent reviews or (in the case of practice partners) formal peer review with strategic development plans. Effective development strategy may include transparent succession planning so that individuals are aware they are being groomed for future roles.
A well‐known adage suggests, People quit the manager or administrator, not the job. Development in this sense relies on presenting new opportunities and knowing that people flourish when allowed to explore multiple paths forward. In many companies, the role of Chief Experience or Chief Learning Officers is to enhance development planning. Consider how career coaching of young hospitalists could transform an infinitely portable and volatile commodity job, prone to burnout, into an engaged specialist of sorts with immense value to a hospital. Hospitalists have already demonstrated their potential as quality improvement leaders.15 Imagine if hospital leadership enlisted a young hospitalist in a relevant quality improvement task force, such as one working on preventing falls. With appropriate support, the physician could obtain skills for quality improvement evaluation that would not only enhance his or her engagement with the hospital system but also provide a valuable analysis for the hospital.
As an example of development strategy within a small practice setting, consider the following real‐life anecdote: a group of 4 physicians recently completed a long and expensive recruitment of a new partner. The new partner, intrigued by the local hospital's surgical robot technology, sought the support of her partners (who are not currently using the technology) to partake in an expensive robotics training program. The partners decided not to provide the financial support. The new partner subsequently left the group for a nearby practice opportunity that would provide for the training, and the group was faced with the loss of a partner (one‐fourth of the practice!) and the cost of repeating the recruiting process. A preemptive evaluation of the value of investing in the development of the new partner and enhancing that partner's professional development may have proven wise despite the significant up‐front costs. In this case the manager the new partner quit was the inflexibility of the practice trajectory.
Retain
The economic incentive to retain talented workers is not subtle. If it was, companies would not be funneling resources into Chief Experience Officers. Likewise, the estimated cost for a medical practice to replace an individual physician is as at least $250,000.16, 17
In retention, as in attraction, salary is only part of the equation.18 People want fair and competitive compensation, and may leave if they are not getting it, but they will not stay (and will not stay engaged) only for a salary bump. Retention is enhanced when workers can advance according to skills and talent, rather than mere tenure. An effective retention policy responds to people's desire to incorporate individual professional goals into their work and allows for people to customize their career rather than simply occupy a job class. Effective retention policy respects worklife balance and recognizes that this balance might look different for 2 people with the same job. It may take the form of positive reinforcement (rather than subtle disdain) for using vacation time or allowing for participation in international service projects. Many literally feel that they need to quit their job in order to take time off or explore other interests.
Worklife balance has been a longstanding issue in medicine, and innovative augmentation strategies may well help retain top talent. Today's successful medical school applicants not only show aptitude in the classroom, they often have many well‐developed nonmedical skills. No one can expect that medical training will somehow convince them to leave everything else behind. Moreover, today's residency graduates, already with Generation Y sensibilities, have completed their entire training under the auspices of the Accreditation Council for Graduate Medical Education (ACGME) duty hours regulations, which has made residents far more comfortable with shift work and defined hours.
At the other end of the generation spectrum, as large numbers of physicians ready for retirement, effective talent facilitation strategies may evaluate how to reoffer medicine as a valid option for senior physicians who still wish to work. Retaining these physicians will require an appreciation of their lifestyle goals, as they will likely find continuing a traditional practice role untenable. A recent survey of orthopedic surgeons 50 years of age or older found that having a part‐time option was a common reason they continued practicing, and that the option to work part‐time would have the most impact on keeping these surgeons working past age 65 years.19 Those working part‐time were doing so in a wide range of practice arrangements including private practice. However, one‐third of those surveyed said a part‐time option was not available to them. Clearly, in an environment of workforce shortages, physician‐leaders must begin to think about worklife balance not only for new doctors but for those considering retirement.
Critics will point out the financial drawbacks in the provision of worklife balance. But the cost may pale in comparison to the cost of replacing physician leaders. Moreover, engaged physicians are more likely to add value in the form of intangible capital such as patient satisfaction and practice innovation. As such, we argue that effective retention strategy in medicine is likely to be cost‐effective, even if it requires significant new up‐front resources.
Lessons From Industry
Doctors frequently assume that the challenges and obstacles confronted in healthcare are unique to medicine. But, for every phrase like When I started practice, I decided how long office visits were, not the insurance company, or Young doctors just don't want to work as hard, there is a parallel utterance in the greater business world. Luckily, there are now examples of the healthcare world learning lessons from business. For example, innovators in medical quality improvement found value in the experience of other industries.20 Airlines and automakers have long honed systems for error prevention and possess expertise that may curb errors in the hospital.2123
We suspect that the ideas and practice of talent facilitation have already made their way into some medical settings. A Google search reveals multiple opportunities for hospital‐based talent managers, and websites advertise the availability of talent consultants ready to lend their expertise to the medical world. In the arena of academic medicine, the University of California, San Francisco (UCSF) Division of Hospital Medicine put some of the ideas of talent facilitation into practice over the past year, in part in response to an increasingly competitive market for academic hospitalists.24 Leaders introduced a formal faculty development program that links junior faculty with mentors and facilitates early and frequent feedback across hierarchical boundaries.25 These more intentional mentoring efforts were accompanied by a seminar series aimed at the needs of new faculty members, a research incubator program, divisional grand rounds, and other web‐based and in‐person forums for sharing best practices and innovations. Less formal social events have also been promoted. Importantly, these sweeping strategies seek to encompass the needs of both teaching and nonteaching hospitalists within UCSF.26
Clearly, an academic hospitalist group with 45 faculty physicians has unique characteristics that inform the specifics of its talent facilitation strategy. The interventions discussed above are meant to represent examples of the types of strategies that may be utilized by physician groups once a decision is made to focus on talent management. Undoubtedly, the shape of such efforts will vary in diverse practice settings, but physician leaders have much to gain through further exploration of where these core principles already exist within medicine and where they may be more effectively deployed. By examining how multinational businesses are systematically applying the concepts of talent facilitation to address a global talent shortage, the doctoring profession might again take an outside hint to help inform its future.
- Long Term Care: Aging Baby Boom Generation Will Increase Demand and Burden on Federal and State Budgets. United States General Accounting Office Testimony before the Special Committee on Aging, US Senate. Hearing Before the Special Committee on Aging of the US Senate,2002. Available at:http://www.gao.gov/new.items/d02544t.pdf. Accessed July 2009.
- ,.Physician workforce shortages: implications and issues for academic health centers and policymakers.Acad Med.2006;81(9):782–787.
- .New York moves to tackle shortage of primary‐care doctors.Lancet.2008;371(9615):801–802.
- ,.The US dermatology workforce: a specialty remains in shortage.J Am Acad Dermatol.2008;59(5):741–745.
- ,.Challenges and opportunities for recruiting a new generation of neurosurgeons.Neurosurgery.2007;61(6):1314–1319.
- ,.The developing crisis in the national general surgery workforce.J Am Coll Surg.2008;206(5):790–795.
- Medical School Enrollment Plans: Analysis of the 2007 AAMC Survey. Publication of the Association of American Medical Colleges, Center for Workforce Studies, April2008. Available at:http://www.aamc.org/workforce. Accessed July 2009.
- It's 2008: Do You Know Where Your Talent Is? Why acquisition and retention strategies don't work. Part 1 of a Deloitte Research Series on Talent Management.2008. Available at: http://www.deloitte.com/dtt/cda/content/UKConsulting_TalentMgtResearchReport.pdf. Accessed August 2009.
- ,,.The race for talent: retaining and engaging workers in the 21st century.Hum Resour Plann.2004;27(3):12–25.
- Expecting sales growth, CEOs cite worker retention as critical to success. March 1,2004. Available at:http://www.barometersurveys.com/production/barsurv.nsf/89343582e94adb6185256b84006c8ffe/9672ab2f54cf99f885256e5500768232?OpenDocument. Accessed July 2009.
- Jet Blue announces aviation university gateway program for pilot candidates: airline partners with Embry‐Riddle Aeronautical University, University of North Dakota, and Cape Air to fill pilot pipeline. January 30, 2008. Available at:http://investor.jetblue.com/phoenix.zhtml?c=131045287(4):487–494.
- ,,.A review of physician turnover: rates, causes, and consequences.Am J Med Qual.2004;19(2):56–66.
- ,,.The impact on revenue of physician turnover: an assessment model and experience in a large healthcare center.J Med Pract Manage.2006;21(6):351–355.
- ,,.Employee motivation: a powerful new model.Harv Bus Rev.2008;86(7–8):78,84,160.
- ,,.Work satisfaction and retirement plans of orthopaedic surgeons 50 years of age or older.Clin Orthop Relat Res.2008;466(1):231–238.
- ,,,.The long road to patient safety: a status report on patient safety systems.JAMA.2005(22);294:2858–2865.
- .Error reduction through team leadership: what surgeons can learn from the airline industry.Clin Neurosurg.2007;54:195–199.
- ,.Applying the Toyota production system: using a patient safety alert system to reduce error.Jt Comm J Qual Patient Saf.2007;33(7):376–386.
- ,,,.Improving Papanikolaou test quality and reducing medical errors by using Toyota production system methods.Am J Obstet Gynecol.2006;194(1):57–64.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction.2006; 1–45. Available at: http://www.hospitalmedicine.org. Accessed July 2009.
- UCSF Department of Medicine, Division of Hospital Medicine, Faculty Development. Available at: http://hospsrvr.ucsf.edu/cme/fds.html. Accessed July 2009.
- ,,, et al. Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–245.
The demand for physician talent is intensifying as the US healthcare system confronts an unprecedented confluence of demographic pressures. Not only will 78 million retiring baby‐boomers require significant healthcare resources, but tens of thousands of practicing physicians will themselves reach retirement age within the next decade.1 At the same time, factors like the large increase in the percentage of female physicians (who are more likely to work part time), the growth of nonpractice opportunities for MDs, and generational demands for greater worklife balance are creating a major supply‐demand mismatch within the physician workforce.2 In this demographic atmosphere, the ability to recruit and retain physician leaders confers tremendous value to healthcare enterprisesboth public and private. Recruiting and retaining strategies already weigh heavily in the most palpable shortage areas, like primary care, but the system faces widespread unmet demand for a variety of specialist and generalist practitioners.36
This article does not address the public policy implications of the upcoming physician shortage, recognition of which will lead to the largest increase in new medical school slots in decades.7 Rather, we set out to illustrate how successful nonmedical businesses are embracing a thoughtful, systematic approach to retaining talent, based on the philosophy that keeping and engaging valued employees is more efficient than recruiting and orienting replacements. We posit that the innovations used by progressive companies could apply to recruitment and retention challenges confronting medicine.
How Industry Approaches the Talent Vacuum: Talent Facilitation
Leaders outside of medicine have long acknowledged that changing demographics and a global economy are driving unprecedented employee turnover.8 In confronting a talent vacuum, forward‐thinking managers have prioritized retaining key talent (rather than hiring anew) in planning for the future.9, 10 Doing so begins with attempts to understand the relationship between workers and the workplace, with a particular emphasis on appreciating workers' priorities. Indeed, new executive positions with titles like Chief Learning Officer and Chief Experience Officer are appearing as companies realize a need for focused expertise beyond traditional human resource departments. These companies understand that offering higher salaries is not the only retention strategyand often not even the most effective one.
The Four Actions of Talent Facilitation
The talent facilitation process centers on four actions: attract, engage, develop, and retain. None of these actions can stand alone, and all should be present, to some degree, at all stages of a worker's tenure. To attract or engage an employee or practice partner is not a 1‐time hook, but a constant and dynamic process.
Importantly, the concepts addressed here are not specific to 1 type of corporate system, size, or management level. Although the early business focus had been on upper‐level and executive talent within large corporate settings, there is an increasing recognition that a dedicated talent strategy is useful wherever recruiting and retaining talented people is important (and where is it not?).
The ideas presented here may seem most applicable to leaders of large physician corporations, hospital‐owned physician groups, or large integrated healthcare systems (such as Kaiser) that employ physicians. However, we also believe that the ideas apply across‐the‐board in medicine, including entities such as small, private, physician‐owned groups. We argue that regardless of the exact practice structure, a limited pool of resources must be dedicated to the attraction and retention of talented partners or employees, or to the cost of replacing those people if they pursue other opportunities (or the cost of inefficient and disengaged physicians). While an integrated health system may have the resources and scale to hire a Chief Experience Officer, we do not anticipate that a 5‐partner private practice would. Rather, we point to examples to illustrate the talent facilitation paradigm as a tool to systematically frame the allocation of those resources. Undoubtedly, the specific shape of a thoughtful talent facilitation effort will vary when applied in a large urban academic medical center vs. an integrated healthcare system vs. a small physician private practice, but the basic principles remain the same.
Attract
Increasingly, companies approach talented prospects with dedicated marketing campaigns to convey the value of a work environment.11 Silicon Valley employee lounges with free massages and foosball tables are the iconic example of attraction, but the concept runs deeper. Today's workers seek access to state‐of‐the‐art ideas and technology and often want to be part of a larger vision. Many seek opportunities to integrate their own professional and personal aspirations into a particular job description.
Hospital executives have long recognized the importance of attracting physicians to their facility (after all, the physicians draw patients and thus generate revenue). The traditional approach has surrounded perks, from comfortable doctor's lounges to the latest in surgical technology. But, the stakes seem greater now than before, and successful talent facilitation strategies are going beyond the tried and true.
Clearly, physicians seek financially stable practice settings with historical success. But they may also seek evidence of a defined strategic plan focused on more than mere profitability. Physicians may gravitate to practice environments that endorse progressive movements like the No One Dies Alone campaign.12 Similarly, recognition of movements beyond healthcarea commitment to Leadership in Energy and Environmental Design (LEED) (Green Building Rating System; US Green Building Council [USGBC];
The current recruitment campaign of California's prison healthcare system offers an unlikely source of inspiration. The prison system was placed in receivership to address a shortage of competent physician staff and other inadequacies. A central feature of the campaign is an attractive starting salary and good benefits. But, the campaign does not rely on money alone. For example, the campaign's website (
Engage
The corporate tool being employed at this stage is a strategy called on‐boarding, which emphasizes a streamlined integration of newcomers with existing workers and culture, and prioritizes aligning organizational roles with a worker's specific skills and interests. On‐boarding also emphasizes the value of early and frequent provision of constructive feedback from same‐level peers or managers with advanced coaching skills.
Many companies use formal survey tools to measure employee engagement and regularly evaluate the proficiency of system leaders in the ability to engage their employees. An engineering firm executive recently told us (P.K., C.K.) that he performs detailed and frequent on‐the‐job interviews, even with company veterans. The primary goal of these interviews is to ensure that engineers spend at least 85% of their time on work that: (1) they find interesting and (2) allows for the application of their best skills. Wherever possible, traditional job descriptions are altered to achieve this. Inevitably, there is still work (15% in this particular corporate vision) that no one prefers but needs to get done, but this process of active recalibration minimizes this fraction to the degree possible.
Even within a small physician practice group, one can imagine how a strategic approach of inviting and acknowledging individual physician's professional goals and particular talents may challenge the long‐held belief that everyone within a group enjoys and must do the exact same job. Once these goals and talents are articulated, groups may find that allowing for more customized roles within the practice enhances professional satisfaction.
Social networking, collaboration, and sharing of best practices are staples of engaging companies. The Cisco and Qualcomm companies, for example, utilize elaborate e‐networks (rough corporate equivalents to Facebook) to foster collegial interaction within and across traditional hierarchical boundaries so that managers and executives directly engage the ideas of employees at every level.14 The premise is logical: engaged employees will be more likely to contribute innovative ideas which, when listened to, are more likely to engage employees.
Most physicians will recognize the traditional resident report as a model for engagement. Beyond its educational value, interaction with program leadership, social bonding, collaborative effort, and exploration of best practices add tremendous value. Many companies would jump at the chance to engrain a similar cultural staple. Enhancing this type of interaction in a postresidency setting may promote engagement in a given system, especially if it facilitates interactions between physicians and senior hospital leaders. Absent these types of interactions, ensuring regular provision of peer review and/or constructive feedback can help systematically enhance 2‐way communication and enhance engagement.
Develop
Talent development relies on mentorship reflecting a genuine interest in an individual's future. Development strategies include pairing formal annual talent reviews or (in the case of practice partners) formal peer review with strategic development plans. Effective development strategy may include transparent succession planning so that individuals are aware they are being groomed for future roles.
A well‐known adage suggests, People quit the manager or administrator, not the job. Development in this sense relies on presenting new opportunities and knowing that people flourish when allowed to explore multiple paths forward. In many companies, the role of Chief Experience or Chief Learning Officers is to enhance development planning. Consider how career coaching of young hospitalists could transform an infinitely portable and volatile commodity job, prone to burnout, into an engaged specialist of sorts with immense value to a hospital. Hospitalists have already demonstrated their potential as quality improvement leaders.15 Imagine if hospital leadership enlisted a young hospitalist in a relevant quality improvement task force, such as one working on preventing falls. With appropriate support, the physician could obtain skills for quality improvement evaluation that would not only enhance his or her engagement with the hospital system but also provide a valuable analysis for the hospital.
As an example of development strategy within a small practice setting, consider the following real‐life anecdote: a group of 4 physicians recently completed a long and expensive recruitment of a new partner. The new partner, intrigued by the local hospital's surgical robot technology, sought the support of her partners (who are not currently using the technology) to partake in an expensive robotics training program. The partners decided not to provide the financial support. The new partner subsequently left the group for a nearby practice opportunity that would provide for the training, and the group was faced with the loss of a partner (one‐fourth of the practice!) and the cost of repeating the recruiting process. A preemptive evaluation of the value of investing in the development of the new partner and enhancing that partner's professional development may have proven wise despite the significant up‐front costs. In this case the manager the new partner quit was the inflexibility of the practice trajectory.
Retain
The economic incentive to retain talented workers is not subtle. If it was, companies would not be funneling resources into Chief Experience Officers. Likewise, the estimated cost for a medical practice to replace an individual physician is as at least $250,000.16, 17
In retention, as in attraction, salary is only part of the equation.18 People want fair and competitive compensation, and may leave if they are not getting it, but they will not stay (and will not stay engaged) only for a salary bump. Retention is enhanced when workers can advance according to skills and talent, rather than mere tenure. An effective retention policy responds to people's desire to incorporate individual professional goals into their work and allows for people to customize their career rather than simply occupy a job class. Effective retention policy respects worklife balance and recognizes that this balance might look different for 2 people with the same job. It may take the form of positive reinforcement (rather than subtle disdain) for using vacation time or allowing for participation in international service projects. Many literally feel that they need to quit their job in order to take time off or explore other interests.
Worklife balance has been a longstanding issue in medicine, and innovative augmentation strategies may well help retain top talent. Today's successful medical school applicants not only show aptitude in the classroom, they often have many well‐developed nonmedical skills. No one can expect that medical training will somehow convince them to leave everything else behind. Moreover, today's residency graduates, already with Generation Y sensibilities, have completed their entire training under the auspices of the Accreditation Council for Graduate Medical Education (ACGME) duty hours regulations, which has made residents far more comfortable with shift work and defined hours.
At the other end of the generation spectrum, as large numbers of physicians ready for retirement, effective talent facilitation strategies may evaluate how to reoffer medicine as a valid option for senior physicians who still wish to work. Retaining these physicians will require an appreciation of their lifestyle goals, as they will likely find continuing a traditional practice role untenable. A recent survey of orthopedic surgeons 50 years of age or older found that having a part‐time option was a common reason they continued practicing, and that the option to work part‐time would have the most impact on keeping these surgeons working past age 65 years.19 Those working part‐time were doing so in a wide range of practice arrangements including private practice. However, one‐third of those surveyed said a part‐time option was not available to them. Clearly, in an environment of workforce shortages, physician‐leaders must begin to think about worklife balance not only for new doctors but for those considering retirement.
Critics will point out the financial drawbacks in the provision of worklife balance. But the cost may pale in comparison to the cost of replacing physician leaders. Moreover, engaged physicians are more likely to add value in the form of intangible capital such as patient satisfaction and practice innovation. As such, we argue that effective retention strategy in medicine is likely to be cost‐effective, even if it requires significant new up‐front resources.
Lessons From Industry
Doctors frequently assume that the challenges and obstacles confronted in healthcare are unique to medicine. But, for every phrase like When I started practice, I decided how long office visits were, not the insurance company, or Young doctors just don't want to work as hard, there is a parallel utterance in the greater business world. Luckily, there are now examples of the healthcare world learning lessons from business. For example, innovators in medical quality improvement found value in the experience of other industries.20 Airlines and automakers have long honed systems for error prevention and possess expertise that may curb errors in the hospital.2123
We suspect that the ideas and practice of talent facilitation have already made their way into some medical settings. A Google search reveals multiple opportunities for hospital‐based talent managers, and websites advertise the availability of talent consultants ready to lend their expertise to the medical world. In the arena of academic medicine, the University of California, San Francisco (UCSF) Division of Hospital Medicine put some of the ideas of talent facilitation into practice over the past year, in part in response to an increasingly competitive market for academic hospitalists.24 Leaders introduced a formal faculty development program that links junior faculty with mentors and facilitates early and frequent feedback across hierarchical boundaries.25 These more intentional mentoring efforts were accompanied by a seminar series aimed at the needs of new faculty members, a research incubator program, divisional grand rounds, and other web‐based and in‐person forums for sharing best practices and innovations. Less formal social events have also been promoted. Importantly, these sweeping strategies seek to encompass the needs of both teaching and nonteaching hospitalists within UCSF.26
Clearly, an academic hospitalist group with 45 faculty physicians has unique characteristics that inform the specifics of its talent facilitation strategy. The interventions discussed above are meant to represent examples of the types of strategies that may be utilized by physician groups once a decision is made to focus on talent management. Undoubtedly, the shape of such efforts will vary in diverse practice settings, but physician leaders have much to gain through further exploration of where these core principles already exist within medicine and where they may be more effectively deployed. By examining how multinational businesses are systematically applying the concepts of talent facilitation to address a global talent shortage, the doctoring profession might again take an outside hint to help inform its future.
The demand for physician talent is intensifying as the US healthcare system confronts an unprecedented confluence of demographic pressures. Not only will 78 million retiring baby‐boomers require significant healthcare resources, but tens of thousands of practicing physicians will themselves reach retirement age within the next decade.1 At the same time, factors like the large increase in the percentage of female physicians (who are more likely to work part time), the growth of nonpractice opportunities for MDs, and generational demands for greater worklife balance are creating a major supply‐demand mismatch within the physician workforce.2 In this demographic atmosphere, the ability to recruit and retain physician leaders confers tremendous value to healthcare enterprisesboth public and private. Recruiting and retaining strategies already weigh heavily in the most palpable shortage areas, like primary care, but the system faces widespread unmet demand for a variety of specialist and generalist practitioners.36
This article does not address the public policy implications of the upcoming physician shortage, recognition of which will lead to the largest increase in new medical school slots in decades.7 Rather, we set out to illustrate how successful nonmedical businesses are embracing a thoughtful, systematic approach to retaining talent, based on the philosophy that keeping and engaging valued employees is more efficient than recruiting and orienting replacements. We posit that the innovations used by progressive companies could apply to recruitment and retention challenges confronting medicine.
How Industry Approaches the Talent Vacuum: Talent Facilitation
Leaders outside of medicine have long acknowledged that changing demographics and a global economy are driving unprecedented employee turnover.8 In confronting a talent vacuum, forward‐thinking managers have prioritized retaining key talent (rather than hiring anew) in planning for the future.9, 10 Doing so begins with attempts to understand the relationship between workers and the workplace, with a particular emphasis on appreciating workers' priorities. Indeed, new executive positions with titles like Chief Learning Officer and Chief Experience Officer are appearing as companies realize a need for focused expertise beyond traditional human resource departments. These companies understand that offering higher salaries is not the only retention strategyand often not even the most effective one.
The Four Actions of Talent Facilitation
The talent facilitation process centers on four actions: attract, engage, develop, and retain. None of these actions can stand alone, and all should be present, to some degree, at all stages of a worker's tenure. To attract or engage an employee or practice partner is not a 1‐time hook, but a constant and dynamic process.
Importantly, the concepts addressed here are not specific to 1 type of corporate system, size, or management level. Although the early business focus had been on upper‐level and executive talent within large corporate settings, there is an increasing recognition that a dedicated talent strategy is useful wherever recruiting and retaining talented people is important (and where is it not?).
The ideas presented here may seem most applicable to leaders of large physician corporations, hospital‐owned physician groups, or large integrated healthcare systems (such as Kaiser) that employ physicians. However, we also believe that the ideas apply across‐the‐board in medicine, including entities such as small, private, physician‐owned groups. We argue that regardless of the exact practice structure, a limited pool of resources must be dedicated to the attraction and retention of talented partners or employees, or to the cost of replacing those people if they pursue other opportunities (or the cost of inefficient and disengaged physicians). While an integrated health system may have the resources and scale to hire a Chief Experience Officer, we do not anticipate that a 5‐partner private practice would. Rather, we point to examples to illustrate the talent facilitation paradigm as a tool to systematically frame the allocation of those resources. Undoubtedly, the specific shape of a thoughtful talent facilitation effort will vary when applied in a large urban academic medical center vs. an integrated healthcare system vs. a small physician private practice, but the basic principles remain the same.
Attract
Increasingly, companies approach talented prospects with dedicated marketing campaigns to convey the value of a work environment.11 Silicon Valley employee lounges with free massages and foosball tables are the iconic example of attraction, but the concept runs deeper. Today's workers seek access to state‐of‐the‐art ideas and technology and often want to be part of a larger vision. Many seek opportunities to integrate their own professional and personal aspirations into a particular job description.
Hospital executives have long recognized the importance of attracting physicians to their facility (after all, the physicians draw patients and thus generate revenue). The traditional approach has surrounded perks, from comfortable doctor's lounges to the latest in surgical technology. But, the stakes seem greater now than before, and successful talent facilitation strategies are going beyond the tried and true.
Clearly, physicians seek financially stable practice settings with historical success. But they may also seek evidence of a defined strategic plan focused on more than mere profitability. Physicians may gravitate to practice environments that endorse progressive movements like the No One Dies Alone campaign.12 Similarly, recognition of movements beyond healthcarea commitment to Leadership in Energy and Environmental Design (LEED) (Green Building Rating System; US Green Building Council [USGBC];
The current recruitment campaign of California's prison healthcare system offers an unlikely source of inspiration. The prison system was placed in receivership to address a shortage of competent physician staff and other inadequacies. A central feature of the campaign is an attractive starting salary and good benefits. But, the campaign does not rely on money alone. For example, the campaign's website (
Engage
The corporate tool being employed at this stage is a strategy called on‐boarding, which emphasizes a streamlined integration of newcomers with existing workers and culture, and prioritizes aligning organizational roles with a worker's specific skills and interests. On‐boarding also emphasizes the value of early and frequent provision of constructive feedback from same‐level peers or managers with advanced coaching skills.
Many companies use formal survey tools to measure employee engagement and regularly evaluate the proficiency of system leaders in the ability to engage their employees. An engineering firm executive recently told us (P.K., C.K.) that he performs detailed and frequent on‐the‐job interviews, even with company veterans. The primary goal of these interviews is to ensure that engineers spend at least 85% of their time on work that: (1) they find interesting and (2) allows for the application of their best skills. Wherever possible, traditional job descriptions are altered to achieve this. Inevitably, there is still work (15% in this particular corporate vision) that no one prefers but needs to get done, but this process of active recalibration minimizes this fraction to the degree possible.
Even within a small physician practice group, one can imagine how a strategic approach of inviting and acknowledging individual physician's professional goals and particular talents may challenge the long‐held belief that everyone within a group enjoys and must do the exact same job. Once these goals and talents are articulated, groups may find that allowing for more customized roles within the practice enhances professional satisfaction.
Social networking, collaboration, and sharing of best practices are staples of engaging companies. The Cisco and Qualcomm companies, for example, utilize elaborate e‐networks (rough corporate equivalents to Facebook) to foster collegial interaction within and across traditional hierarchical boundaries so that managers and executives directly engage the ideas of employees at every level.14 The premise is logical: engaged employees will be more likely to contribute innovative ideas which, when listened to, are more likely to engage employees.
Most physicians will recognize the traditional resident report as a model for engagement. Beyond its educational value, interaction with program leadership, social bonding, collaborative effort, and exploration of best practices add tremendous value. Many companies would jump at the chance to engrain a similar cultural staple. Enhancing this type of interaction in a postresidency setting may promote engagement in a given system, especially if it facilitates interactions between physicians and senior hospital leaders. Absent these types of interactions, ensuring regular provision of peer review and/or constructive feedback can help systematically enhance 2‐way communication and enhance engagement.
Develop
Talent development relies on mentorship reflecting a genuine interest in an individual's future. Development strategies include pairing formal annual talent reviews or (in the case of practice partners) formal peer review with strategic development plans. Effective development strategy may include transparent succession planning so that individuals are aware they are being groomed for future roles.
A well‐known adage suggests, People quit the manager or administrator, not the job. Development in this sense relies on presenting new opportunities and knowing that people flourish when allowed to explore multiple paths forward. In many companies, the role of Chief Experience or Chief Learning Officers is to enhance development planning. Consider how career coaching of young hospitalists could transform an infinitely portable and volatile commodity job, prone to burnout, into an engaged specialist of sorts with immense value to a hospital. Hospitalists have already demonstrated their potential as quality improvement leaders.15 Imagine if hospital leadership enlisted a young hospitalist in a relevant quality improvement task force, such as one working on preventing falls. With appropriate support, the physician could obtain skills for quality improvement evaluation that would not only enhance his or her engagement with the hospital system but also provide a valuable analysis for the hospital.
As an example of development strategy within a small practice setting, consider the following real‐life anecdote: a group of 4 physicians recently completed a long and expensive recruitment of a new partner. The new partner, intrigued by the local hospital's surgical robot technology, sought the support of her partners (who are not currently using the technology) to partake in an expensive robotics training program. The partners decided not to provide the financial support. The new partner subsequently left the group for a nearby practice opportunity that would provide for the training, and the group was faced with the loss of a partner (one‐fourth of the practice!) and the cost of repeating the recruiting process. A preemptive evaluation of the value of investing in the development of the new partner and enhancing that partner's professional development may have proven wise despite the significant up‐front costs. In this case the manager the new partner quit was the inflexibility of the practice trajectory.
Retain
The economic incentive to retain talented workers is not subtle. If it was, companies would not be funneling resources into Chief Experience Officers. Likewise, the estimated cost for a medical practice to replace an individual physician is as at least $250,000.16, 17
In retention, as in attraction, salary is only part of the equation.18 People want fair and competitive compensation, and may leave if they are not getting it, but they will not stay (and will not stay engaged) only for a salary bump. Retention is enhanced when workers can advance according to skills and talent, rather than mere tenure. An effective retention policy responds to people's desire to incorporate individual professional goals into their work and allows for people to customize their career rather than simply occupy a job class. Effective retention policy respects worklife balance and recognizes that this balance might look different for 2 people with the same job. It may take the form of positive reinforcement (rather than subtle disdain) for using vacation time or allowing for participation in international service projects. Many literally feel that they need to quit their job in order to take time off or explore other interests.
Worklife balance has been a longstanding issue in medicine, and innovative augmentation strategies may well help retain top talent. Today's successful medical school applicants not only show aptitude in the classroom, they often have many well‐developed nonmedical skills. No one can expect that medical training will somehow convince them to leave everything else behind. Moreover, today's residency graduates, already with Generation Y sensibilities, have completed their entire training under the auspices of the Accreditation Council for Graduate Medical Education (ACGME) duty hours regulations, which has made residents far more comfortable with shift work and defined hours.
At the other end of the generation spectrum, as large numbers of physicians ready for retirement, effective talent facilitation strategies may evaluate how to reoffer medicine as a valid option for senior physicians who still wish to work. Retaining these physicians will require an appreciation of their lifestyle goals, as they will likely find continuing a traditional practice role untenable. A recent survey of orthopedic surgeons 50 years of age or older found that having a part‐time option was a common reason they continued practicing, and that the option to work part‐time would have the most impact on keeping these surgeons working past age 65 years.19 Those working part‐time were doing so in a wide range of practice arrangements including private practice. However, one‐third of those surveyed said a part‐time option was not available to them. Clearly, in an environment of workforce shortages, physician‐leaders must begin to think about worklife balance not only for new doctors but for those considering retirement.
Critics will point out the financial drawbacks in the provision of worklife balance. But the cost may pale in comparison to the cost of replacing physician leaders. Moreover, engaged physicians are more likely to add value in the form of intangible capital such as patient satisfaction and practice innovation. As such, we argue that effective retention strategy in medicine is likely to be cost‐effective, even if it requires significant new up‐front resources.
Lessons From Industry
Doctors frequently assume that the challenges and obstacles confronted in healthcare are unique to medicine. But, for every phrase like When I started practice, I decided how long office visits were, not the insurance company, or Young doctors just don't want to work as hard, there is a parallel utterance in the greater business world. Luckily, there are now examples of the healthcare world learning lessons from business. For example, innovators in medical quality improvement found value in the experience of other industries.20 Airlines and automakers have long honed systems for error prevention and possess expertise that may curb errors in the hospital.2123
We suspect that the ideas and practice of talent facilitation have already made their way into some medical settings. A Google search reveals multiple opportunities for hospital‐based talent managers, and websites advertise the availability of talent consultants ready to lend their expertise to the medical world. In the arena of academic medicine, the University of California, San Francisco (UCSF) Division of Hospital Medicine put some of the ideas of talent facilitation into practice over the past year, in part in response to an increasingly competitive market for academic hospitalists.24 Leaders introduced a formal faculty development program that links junior faculty with mentors and facilitates early and frequent feedback across hierarchical boundaries.25 These more intentional mentoring efforts were accompanied by a seminar series aimed at the needs of new faculty members, a research incubator program, divisional grand rounds, and other web‐based and in‐person forums for sharing best practices and innovations. Less formal social events have also been promoted. Importantly, these sweeping strategies seek to encompass the needs of both teaching and nonteaching hospitalists within UCSF.26
Clearly, an academic hospitalist group with 45 faculty physicians has unique characteristics that inform the specifics of its talent facilitation strategy. The interventions discussed above are meant to represent examples of the types of strategies that may be utilized by physician groups once a decision is made to focus on talent management. Undoubtedly, the shape of such efforts will vary in diverse practice settings, but physician leaders have much to gain through further exploration of where these core principles already exist within medicine and where they may be more effectively deployed. By examining how multinational businesses are systematically applying the concepts of talent facilitation to address a global talent shortage, the doctoring profession might again take an outside hint to help inform its future.
- Long Term Care: Aging Baby Boom Generation Will Increase Demand and Burden on Federal and State Budgets. United States General Accounting Office Testimony before the Special Committee on Aging, US Senate. Hearing Before the Special Committee on Aging of the US Senate,2002. Available at:http://www.gao.gov/new.items/d02544t.pdf. Accessed July 2009.
- ,.Physician workforce shortages: implications and issues for academic health centers and policymakers.Acad Med.2006;81(9):782–787.
- .New York moves to tackle shortage of primary‐care doctors.Lancet.2008;371(9615):801–802.
- ,.The US dermatology workforce: a specialty remains in shortage.J Am Acad Dermatol.2008;59(5):741–745.
- ,.Challenges and opportunities for recruiting a new generation of neurosurgeons.Neurosurgery.2007;61(6):1314–1319.
- ,.The developing crisis in the national general surgery workforce.J Am Coll Surg.2008;206(5):790–795.
- Medical School Enrollment Plans: Analysis of the 2007 AAMC Survey. Publication of the Association of American Medical Colleges, Center for Workforce Studies, April2008. Available at:http://www.aamc.org/workforce. Accessed July 2009.
- It's 2008: Do You Know Where Your Talent Is? Why acquisition and retention strategies don't work. Part 1 of a Deloitte Research Series on Talent Management.2008. Available at: http://www.deloitte.com/dtt/cda/content/UKConsulting_TalentMgtResearchReport.pdf. Accessed August 2009.
- ,,.The race for talent: retaining and engaging workers in the 21st century.Hum Resour Plann.2004;27(3):12–25.
- Expecting sales growth, CEOs cite worker retention as critical to success. March 1,2004. Available at:http://www.barometersurveys.com/production/barsurv.nsf/89343582e94adb6185256b84006c8ffe/9672ab2f54cf99f885256e5500768232?OpenDocument. Accessed July 2009.
- Jet Blue announces aviation university gateway program for pilot candidates: airline partners with Embry‐Riddle Aeronautical University, University of North Dakota, and Cape Air to fill pilot pipeline. January 30, 2008. Available at:http://investor.jetblue.com/phoenix.zhtml?c=131045287(4):487–494.
- ,,.A review of physician turnover: rates, causes, and consequences.Am J Med Qual.2004;19(2):56–66.
- ,,.The impact on revenue of physician turnover: an assessment model and experience in a large healthcare center.J Med Pract Manage.2006;21(6):351–355.
- ,,.Employee motivation: a powerful new model.Harv Bus Rev.2008;86(7–8):78,84,160.
- ,,.Work satisfaction and retirement plans of orthopaedic surgeons 50 years of age or older.Clin Orthop Relat Res.2008;466(1):231–238.
- ,,,.The long road to patient safety: a status report on patient safety systems.JAMA.2005(22);294:2858–2865.
- .Error reduction through team leadership: what surgeons can learn from the airline industry.Clin Neurosurg.2007;54:195–199.
- ,.Applying the Toyota production system: using a patient safety alert system to reduce error.Jt Comm J Qual Patient Saf.2007;33(7):376–386.
- ,,,.Improving Papanikolaou test quality and reducing medical errors by using Toyota production system methods.Am J Obstet Gynecol.2006;194(1):57–64.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction.2006; 1–45. Available at: http://www.hospitalmedicine.org. Accessed July 2009.
- UCSF Department of Medicine, Division of Hospital Medicine, Faculty Development. Available at: http://hospsrvr.ucsf.edu/cme/fds.html. Accessed July 2009.
- ,,, et al. Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–245.
- Long Term Care: Aging Baby Boom Generation Will Increase Demand and Burden on Federal and State Budgets. United States General Accounting Office Testimony before the Special Committee on Aging, US Senate. Hearing Before the Special Committee on Aging of the US Senate,2002. Available at:http://www.gao.gov/new.items/d02544t.pdf. Accessed July 2009.
- ,.Physician workforce shortages: implications and issues for academic health centers and policymakers.Acad Med.2006;81(9):782–787.
- .New York moves to tackle shortage of primary‐care doctors.Lancet.2008;371(9615):801–802.
- ,.The US dermatology workforce: a specialty remains in shortage.J Am Acad Dermatol.2008;59(5):741–745.
- ,.Challenges and opportunities for recruiting a new generation of neurosurgeons.Neurosurgery.2007;61(6):1314–1319.
- ,.The developing crisis in the national general surgery workforce.J Am Coll Surg.2008;206(5):790–795.
- Medical School Enrollment Plans: Analysis of the 2007 AAMC Survey. Publication of the Association of American Medical Colleges, Center for Workforce Studies, April2008. Available at:http://www.aamc.org/workforce. Accessed July 2009.
- It's 2008: Do You Know Where Your Talent Is? Why acquisition and retention strategies don't work. Part 1 of a Deloitte Research Series on Talent Management.2008. Available at: http://www.deloitte.com/dtt/cda/content/UKConsulting_TalentMgtResearchReport.pdf. Accessed August 2009.
- ,,.The race for talent: retaining and engaging workers in the 21st century.Hum Resour Plann.2004;27(3):12–25.
- Expecting sales growth, CEOs cite worker retention as critical to success. March 1,2004. Available at:http://www.barometersurveys.com/production/barsurv.nsf/89343582e94adb6185256b84006c8ffe/9672ab2f54cf99f885256e5500768232?OpenDocument. Accessed July 2009.
- Jet Blue announces aviation university gateway program for pilot candidates: airline partners with Embry‐Riddle Aeronautical University, University of North Dakota, and Cape Air to fill pilot pipeline. January 30, 2008. Available at:http://investor.jetblue.com/phoenix.zhtml?c=131045287(4):487–494.
- ,,.A review of physician turnover: rates, causes, and consequences.Am J Med Qual.2004;19(2):56–66.
- ,,.The impact on revenue of physician turnover: an assessment model and experience in a large healthcare center.J Med Pract Manage.2006;21(6):351–355.
- ,,.Employee motivation: a powerful new model.Harv Bus Rev.2008;86(7–8):78,84,160.
- ,,.Work satisfaction and retirement plans of orthopaedic surgeons 50 years of age or older.Clin Orthop Relat Res.2008;466(1):231–238.
- ,,,.The long road to patient safety: a status report on patient safety systems.JAMA.2005(22);294:2858–2865.
- .Error reduction through team leadership: what surgeons can learn from the airline industry.Clin Neurosurg.2007;54:195–199.
- ,.Applying the Toyota production system: using a patient safety alert system to reduce error.Jt Comm J Qual Patient Saf.2007;33(7):376–386.
- ,,,.Improving Papanikolaou test quality and reducing medical errors by using Toyota production system methods.Am J Obstet Gynecol.2006;194(1):57–64.
- Society of Hospital Medicine Career Satisfaction Task Force. White Paper on Hospitalist Career Satisfaction.2006; 1–45. Available at: http://www.hospitalmedicine.org. Accessed July 2009.
- UCSF Department of Medicine, Division of Hospital Medicine, Faculty Development. Available at: http://hospsrvr.ucsf.edu/cme/fds.html. Accessed July 2009.
- ,,, et al. Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–245.
Hospitals and Recession
With the United States mired in its most severe recession in decades, stories of hospital struggles have emerged. Beaumont Hospital, located near the headquarters of major automakers and several assembly plants outside Detroit, recently cut hundreds of jobs and put major construction on indefinite hold.1 The CEO of Boston's Beth Israel Deaconess Medical Center made an agreement with employees to take large cuts in pay and vacation time to prevent laying off 10% of the staff.2 The University of Chicago Medical Center made plans to limit the number of emergency room beds, thereby decreasing low‐reimbursing emergency admissions while making beds available for higher‐paying elective hospitalizations.3
What is surprising about these stories is that hospitals have long been considered recession‐proof. Yet, with one‐half of US hospitals having reduced their staff to balance their budgets4 and with hospitals' financial margins falling dramatically,5 economic struggles are now a widespread problem.
Furthermore, it is difficult to determine if hospitals' clinical care has been damaged by the recession. The measurement of hospital quality is new and still under‐developed: there is virtually no reliable information on hospital quality from previous recessions, and even now it will be difficult to assess quality in real time.
Critics of waste and excess in the US health care system may see tough economic times as a Darwinian proving ground for hospitals, through which efficiency will improve and poor performers will close their doors. But more likely, hospital cutbacks will risk the quality and safety of health care delivery. For reasons of both public health and fiscal impact on communities, state and federal leaders may need to watch these trends closely to design and to be ready to implement potential government remedies for hospitals' fiscal woes.
In this commentary, we describe how hospitals have fared historically during recessions, how this recession could have different effectsfirst fiscally, then clinically, and we examine policy options to mitigate these untoward effects.
Decades of Recession‐Proof Hospitals
During the Great Depression, hospital insolvency was a national problem that prompted federal and state aid. Keeping hospitals alive was a critical policy goal and proved central to the early development of health insurance that focused on payment for hospital care.6
Since WWII, growth in America's hospitals has been only loosely related to national macroeconomic trends, with other changes like technological innovations and the advent of managed care far more influential to hospital finances. In fact, during recessions, hospital care spending growth often escalates in tandem with worsening unemployment (Figure 1). One explanation for this phenomenon is that economic pressures lead to declining primary care utilization, with adverse consequences for individuals' health.7
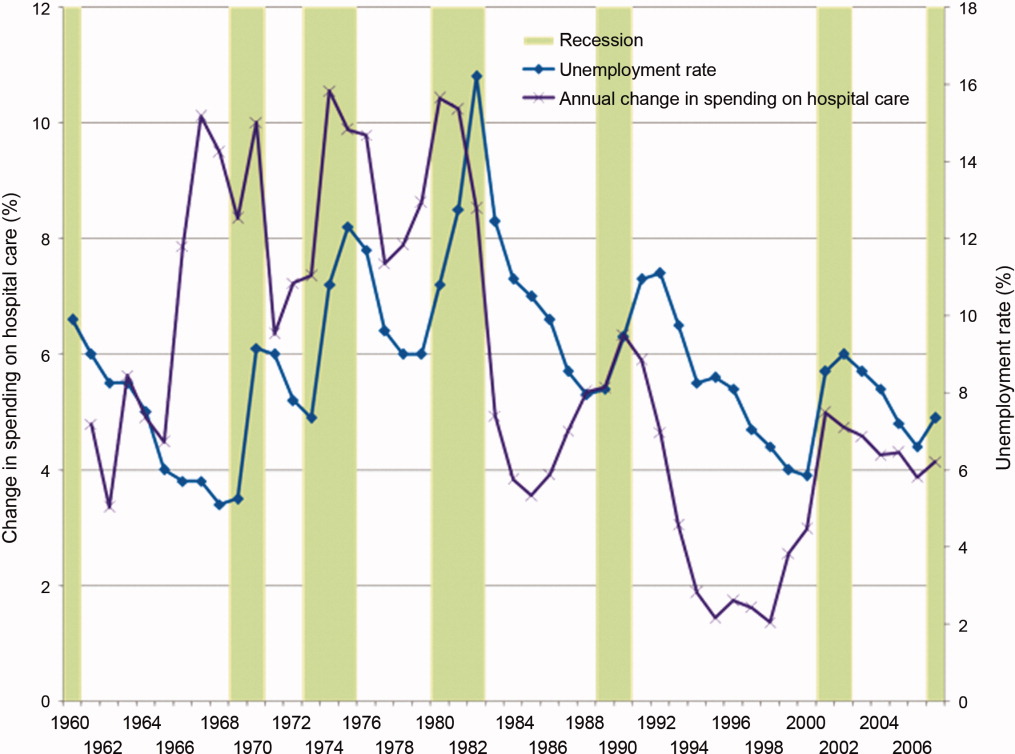
Hospitals' Current Fiscal Vulnerability
However, the current recession is the worst in 70 years. Every method of income generation available to hospitals appears at risk, including reimbursement per discharge (70% of hospitals report moderate or significant increases in uncompensated care), number of inpatient admissions (over one‐half report a moderate or significant decrease), difficulty obtaining bonds (60% report at least significant problems), and charitable donations.4 Over 50% of US hospitals had negative margins in the fourth quarter of 2008, though there has been some improvement since that time.8
Future hospital stability concerns remain. Growth in revenue per discharge is still below the norm.5 Because employment lags a recovering economy, further reimbursement decreases are possible from increasing proportions of patients with low‐reimbursing insurers or no coverage at all, decreasing payment rates from all payers, and decreasing elective care. The lower‐reimbursing payers, like state Medicaid programs, are experiencing increased enrollment as Americans lose their jobs and their better‐paying, employer‐sponsored private insurance.9 There's also evidence that reimbursement rates are declining from both Medicare and private insurers,10 which threatens the fragile cost‐shift through which hospitals have long used private insurance reimbursement to subsidize government reimbursements.11
Hospitals' specific financial challenges will likely vary across markets. The authors' state of Michigan has been hit particularly long and hard by the current recession. Unemployment rates exceeding 11% are expected to cause dramatic losses in private health insurance.9 Patients' increasing need with decreasing ability to pay will make markets in the deepest recession particularly vulnerable.
Hospital Quality and Safety at Risk?
The effect of the recession on the quality of hospital care is less clear. Until the 1990s, hospital quality was essentially assumed and virtually unmeasured. Even now, measuring hospital quality is difficult and rarely timely. Medicare data often take 1 to 2 years to become publicly available for analysis. Reports by trade organizations like the American Hospital Association are up‐to‐date but have conflicts of interest and are less rigorous. The most timely measures of hospitals' distressflawed as they may bewill come from the hospitals themselves, just like reports of economic woe from other businesses and government agencies during challenging economic times.
However, since the publication of the 1999 report To Err is Human,12 major improvements in hospital quality and safety have transformed the delivery of inpatient care. These improvements have taken the form of simple interventions like nationally consistent medical abbreviations, management initiatives like Six Sigma, and technological advances including computerized health records.
Nonetheless, during this recession and recovery, slashed hospital budgets may slow or even stop the momentum towards further improvements in quality and safety. Frontline care delivery could be at risk. Understaffed and under financed hospitals are rarely safe. Dissatisfaction and layoffs hurt the interactions between employees and patients. Robust nurse‐to‐patient ratios which have proven vital to patients' hospital outcomes could be at risk.13 Admittedly, recession‐induced threats to quality and safety are conjectures on our part: unfortunately, no recession measures of hospitals' specific spending on staffing, technology, or process improvements exist.
However, there are many small, evidence‐based changes that could improve hospital safety dramatically in the near future. Michigan's Keystone ICU Initiative showed that systematic interventions in routine care delivery could reduce the risk of catheter‐related bloodstream infections, which currently are implicated in the death of 28,000 Americans per year, to nearly zero.14 The Institute for Healthcare Improvement's 100,000 Lives Campaign also illustrated that dramatic improvements in hospital‐related mortality can occur with fairly focused interventions. In the month after discharge, more than one‐quarter of all hospitalized patients go to an emergency room or need to be rehospitalized. This rate can be cut by 30% by inserting a nurse discharge advocate into the discharge process.15 Instituting a simple safety checklist before surgery decreased surgery‐related mortality and complications by over one‐third.16
Such interventions are effective, reasonable, and widely accessible. Over the long‐term, many may even be cost‐saving. But, importantly, they all require an institutional investment in start‐up money and an organizational will to change how things have been done. In a period of recession with severe cost‐cutting, and a recovery period of cautious spending, this may not be possible.
A Possible Stimulus: Investing in Quality Initiatives at Fiscally Vulnerable Hospitals
It is not enough to keep hospitals' doors open in a recession. Hospitals must continue to improve the quality and safety of the care they delivervital for their future patients and also for their communities who depend on them as anchors of health systems. We believe there is a need for a new, federally supported alignment of hospital finance and hospital quality that can limit damage to hospitals, help community employment, and improve patient safety.
Timely, structural quality measures could speed the introduction of functional value‐based purchasing, promote hospital safety, and help local economies at the same time. There are many simple structural measures that could be examined, such as development of discharge coordinators, promoting effective nurse‐to‐patient ratios, and encouraging health information technology (IT). Importantly, this would not duplicate efforts already underway to promote quality with process measures. With effective financial monitoring in real time, these measures could focus on high‐risk, fiscally disadvantaged hospitals.
To its credit, the Obama administration has already reached out to support hospitals, although aid has not been targeted specifically to hospitals in the most dire financial circumstances. Along with support for Medicaid and community health centers to improve primary care during the recession, the administration has provided a $268 million increase in Disproportionate Share Hospital payments towards hospitals that care for vulnerable patients, an increase of about 3%.17 Concurrently, the Centers for Medicare and Medicaid Services are implementing a value‐based purchasing program that starts with a 5% withhold in reimbursement that institutions need to earn back through a combination of mortality, process, and patient satisfaction metrics.18 The administration also reserved $19 billion to promote improvement of health IT for American medicine.19
Using health IT investment to help hospitals is an appealing concept, but for many institutions the infrastructure required to make that transition directly competes with other patient needs, including bedside patient care. IT investments have large initial costs, at a time when bank loans are difficult to acquire and few organizations can make expensive capital improvements. In fact, one‐quarter of hospitals report scaling back health IT investments that they had already started, in spite of the stimulus funds available.4
Instead, the administration may have more influence on improving care delivery by focusing on connecting hospital safety with hospital financial stability, by appropriating stimulus funds to center on quality and safety programs like those described above. Here is how: a hospital that would receive stimulus money for employing nurse discharge advocates would preserve employment while advancing patient safety, as would a hospital that retains a nurse‐to‐patient ratio above a specified threshold. By focusing on measures of structural quality, the government could improve care in ways that are easy to measure and maximize local economic stimulus without difficult outcomes assessment, insurance reform, or duplicating process measure efforts. There could even be an innovation differential (ie, payment/reward) for hospitals that improve quality while holding flat or lowering overall costs.
Equally important is to use this national financial crisis as an opportunity to improve monitoring of hospital quality. While quality assessment of hospitals is difficult, increased federal awareness of local medical need, hospital financial stability, and government awareness of emergency services overcrowding, nurse‐to‐patient ratios, and IT utilization are all valuable and easy to measure.
None of these quality‐focused fiscal interventions would be guaranteed to prevent hospital closure. Especially in small population centers, hospital closures can affect an entire community's financial growth and clinical safety net,20 while leaving hundreds or even thousands unemployed. Hospital closure should be assessed by state and federal government officials in these larger terms, perhaps even encouraging closure when appropriate, and helping prevent it when necessary.
Conclusion
Hospitals, as complex pieces of America's health care system, are central to communities' safety and economic growth. While national health coverage reform, as currently being discussed in Washington, would make hospital infrastructure less sensitive to macroeconomic changes, major reform would not come fast enough if hospitals start closing. While the worst of the recession may be over, recovery and the continuing rise in unemployment is a tenuous lifeline for hospitals on the financial brink.
We are not arguing against all hospital layoffs, or even closures. Indeed, this recession is a lean time for most industries and is likely to lead to closures for hospitals that cannot compete on efficiency or quality. But a hospital closure is a major event for a community and should not be permitted to occur without thorough consideration of alternatives. Current data on hospitals' financial status and clinical safety are limited, potentially biased, and not timely enough for this rapidly changing economic crisis. Therefore, state and federal government officials should assess whether hospitals would be eligible not just for possible emergency loans, but for linking loans to quality of care and community need. In so doing, this difficult time could be an opportunity to help hospitals improve their care, rather than watching it diminish.
- Michigan's Health Care Safety Net: In Jeopardy.2009.
- .Final budget decisions.Running A Hospital. Vol 2009.Boston, MA;2009.
- .Doctors Plan to Limit Beds in ER.Wall Street Journal.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, DC2009.
- ,.Hospital Operational and Financial Performance Improving.Ann Arbor, MI:Thomson Reuters Center for Healthcare Improvement.2009.
- .The Social Transformation of American Medicine.New York, NY:Basic Books;1983.
- AAFP.Patient Care during the 2008‐2009 Recession – Online Survey.Leawood, KS:AAFP.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, D.C.:American Hospital Association.2009.
- The economic downturn and its impact on hospitals. American Hospital Association Trendwatch.2009.
- ,,.The Current Recession and U.S. Hospitals:Center for Healthcare Improvement.2009.
- ,,.The cost‐shift payment ‘hydraulic’: foundation, history, and implications.Health Aff (Millwood).2006;25(1):22–33.
- ,.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346(22):1715–1722.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- Disproportionate Share Hospital (DSH). Available at: http://www.hhs. gov/recovery/cms/dsh.html. Accessed December 2009.
- ,,.Measuring outcomes and efficiency in medicare value‐based purchasing.Health Aff (Millwood).2009;28(2):w251–w261.
- .Stimulating the adoption of health information technology.N Engl J Med.2009;360(15):1477–1479.
- ,,,.The effect of rural hospital closures on community economic health.Health Serv Res.2006;41(2):467–485.
With the United States mired in its most severe recession in decades, stories of hospital struggles have emerged. Beaumont Hospital, located near the headquarters of major automakers and several assembly plants outside Detroit, recently cut hundreds of jobs and put major construction on indefinite hold.1 The CEO of Boston's Beth Israel Deaconess Medical Center made an agreement with employees to take large cuts in pay and vacation time to prevent laying off 10% of the staff.2 The University of Chicago Medical Center made plans to limit the number of emergency room beds, thereby decreasing low‐reimbursing emergency admissions while making beds available for higher‐paying elective hospitalizations.3
What is surprising about these stories is that hospitals have long been considered recession‐proof. Yet, with one‐half of US hospitals having reduced their staff to balance their budgets4 and with hospitals' financial margins falling dramatically,5 economic struggles are now a widespread problem.
Furthermore, it is difficult to determine if hospitals' clinical care has been damaged by the recession. The measurement of hospital quality is new and still under‐developed: there is virtually no reliable information on hospital quality from previous recessions, and even now it will be difficult to assess quality in real time.
Critics of waste and excess in the US health care system may see tough economic times as a Darwinian proving ground for hospitals, through which efficiency will improve and poor performers will close their doors. But more likely, hospital cutbacks will risk the quality and safety of health care delivery. For reasons of both public health and fiscal impact on communities, state and federal leaders may need to watch these trends closely to design and to be ready to implement potential government remedies for hospitals' fiscal woes.
In this commentary, we describe how hospitals have fared historically during recessions, how this recession could have different effectsfirst fiscally, then clinically, and we examine policy options to mitigate these untoward effects.
Decades of Recession‐Proof Hospitals
During the Great Depression, hospital insolvency was a national problem that prompted federal and state aid. Keeping hospitals alive was a critical policy goal and proved central to the early development of health insurance that focused on payment for hospital care.6
Since WWII, growth in America's hospitals has been only loosely related to national macroeconomic trends, with other changes like technological innovations and the advent of managed care far more influential to hospital finances. In fact, during recessions, hospital care spending growth often escalates in tandem with worsening unemployment (Figure 1). One explanation for this phenomenon is that economic pressures lead to declining primary care utilization, with adverse consequences for individuals' health.7
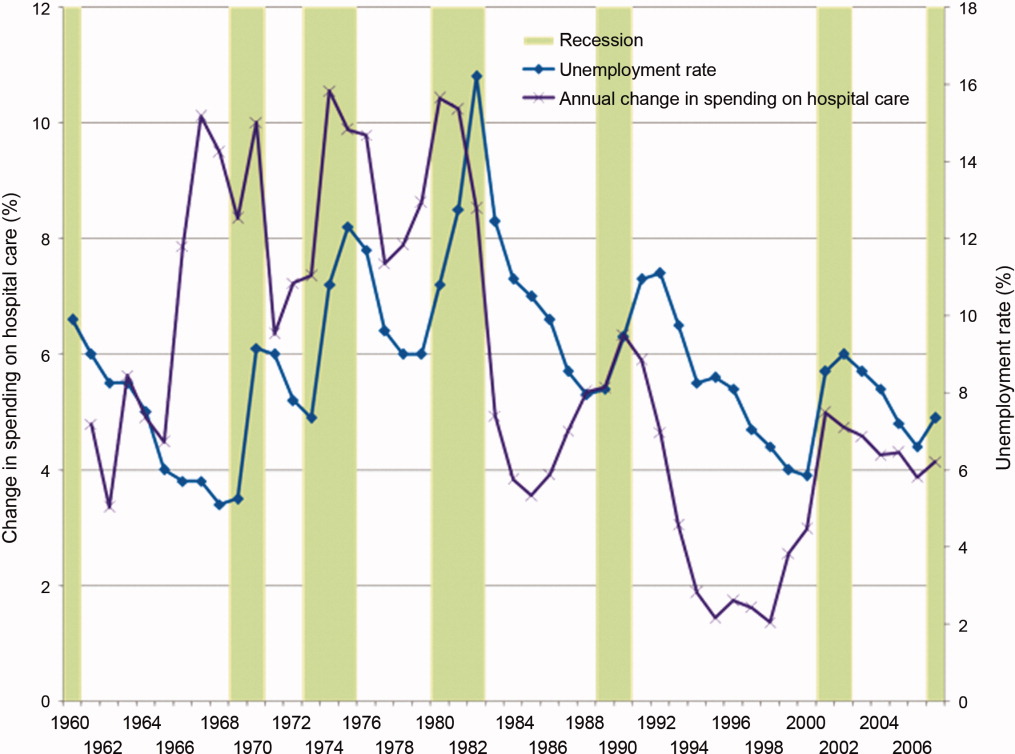
Hospitals' Current Fiscal Vulnerability
However, the current recession is the worst in 70 years. Every method of income generation available to hospitals appears at risk, including reimbursement per discharge (70% of hospitals report moderate or significant increases in uncompensated care), number of inpatient admissions (over one‐half report a moderate or significant decrease), difficulty obtaining bonds (60% report at least significant problems), and charitable donations.4 Over 50% of US hospitals had negative margins in the fourth quarter of 2008, though there has been some improvement since that time.8
Future hospital stability concerns remain. Growth in revenue per discharge is still below the norm.5 Because employment lags a recovering economy, further reimbursement decreases are possible from increasing proportions of patients with low‐reimbursing insurers or no coverage at all, decreasing payment rates from all payers, and decreasing elective care. The lower‐reimbursing payers, like state Medicaid programs, are experiencing increased enrollment as Americans lose their jobs and their better‐paying, employer‐sponsored private insurance.9 There's also evidence that reimbursement rates are declining from both Medicare and private insurers,10 which threatens the fragile cost‐shift through which hospitals have long used private insurance reimbursement to subsidize government reimbursements.11
Hospitals' specific financial challenges will likely vary across markets. The authors' state of Michigan has been hit particularly long and hard by the current recession. Unemployment rates exceeding 11% are expected to cause dramatic losses in private health insurance.9 Patients' increasing need with decreasing ability to pay will make markets in the deepest recession particularly vulnerable.
Hospital Quality and Safety at Risk?
The effect of the recession on the quality of hospital care is less clear. Until the 1990s, hospital quality was essentially assumed and virtually unmeasured. Even now, measuring hospital quality is difficult and rarely timely. Medicare data often take 1 to 2 years to become publicly available for analysis. Reports by trade organizations like the American Hospital Association are up‐to‐date but have conflicts of interest and are less rigorous. The most timely measures of hospitals' distressflawed as they may bewill come from the hospitals themselves, just like reports of economic woe from other businesses and government agencies during challenging economic times.
However, since the publication of the 1999 report To Err is Human,12 major improvements in hospital quality and safety have transformed the delivery of inpatient care. These improvements have taken the form of simple interventions like nationally consistent medical abbreviations, management initiatives like Six Sigma, and technological advances including computerized health records.
Nonetheless, during this recession and recovery, slashed hospital budgets may slow or even stop the momentum towards further improvements in quality and safety. Frontline care delivery could be at risk. Understaffed and under financed hospitals are rarely safe. Dissatisfaction and layoffs hurt the interactions between employees and patients. Robust nurse‐to‐patient ratios which have proven vital to patients' hospital outcomes could be at risk.13 Admittedly, recession‐induced threats to quality and safety are conjectures on our part: unfortunately, no recession measures of hospitals' specific spending on staffing, technology, or process improvements exist.
However, there are many small, evidence‐based changes that could improve hospital safety dramatically in the near future. Michigan's Keystone ICU Initiative showed that systematic interventions in routine care delivery could reduce the risk of catheter‐related bloodstream infections, which currently are implicated in the death of 28,000 Americans per year, to nearly zero.14 The Institute for Healthcare Improvement's 100,000 Lives Campaign also illustrated that dramatic improvements in hospital‐related mortality can occur with fairly focused interventions. In the month after discharge, more than one‐quarter of all hospitalized patients go to an emergency room or need to be rehospitalized. This rate can be cut by 30% by inserting a nurse discharge advocate into the discharge process.15 Instituting a simple safety checklist before surgery decreased surgery‐related mortality and complications by over one‐third.16
Such interventions are effective, reasonable, and widely accessible. Over the long‐term, many may even be cost‐saving. But, importantly, they all require an institutional investment in start‐up money and an organizational will to change how things have been done. In a period of recession with severe cost‐cutting, and a recovery period of cautious spending, this may not be possible.
A Possible Stimulus: Investing in Quality Initiatives at Fiscally Vulnerable Hospitals
It is not enough to keep hospitals' doors open in a recession. Hospitals must continue to improve the quality and safety of the care they delivervital for their future patients and also for their communities who depend on them as anchors of health systems. We believe there is a need for a new, federally supported alignment of hospital finance and hospital quality that can limit damage to hospitals, help community employment, and improve patient safety.
Timely, structural quality measures could speed the introduction of functional value‐based purchasing, promote hospital safety, and help local economies at the same time. There are many simple structural measures that could be examined, such as development of discharge coordinators, promoting effective nurse‐to‐patient ratios, and encouraging health information technology (IT). Importantly, this would not duplicate efforts already underway to promote quality with process measures. With effective financial monitoring in real time, these measures could focus on high‐risk, fiscally disadvantaged hospitals.
To its credit, the Obama administration has already reached out to support hospitals, although aid has not been targeted specifically to hospitals in the most dire financial circumstances. Along with support for Medicaid and community health centers to improve primary care during the recession, the administration has provided a $268 million increase in Disproportionate Share Hospital payments towards hospitals that care for vulnerable patients, an increase of about 3%.17 Concurrently, the Centers for Medicare and Medicaid Services are implementing a value‐based purchasing program that starts with a 5% withhold in reimbursement that institutions need to earn back through a combination of mortality, process, and patient satisfaction metrics.18 The administration also reserved $19 billion to promote improvement of health IT for American medicine.19
Using health IT investment to help hospitals is an appealing concept, but for many institutions the infrastructure required to make that transition directly competes with other patient needs, including bedside patient care. IT investments have large initial costs, at a time when bank loans are difficult to acquire and few organizations can make expensive capital improvements. In fact, one‐quarter of hospitals report scaling back health IT investments that they had already started, in spite of the stimulus funds available.4
Instead, the administration may have more influence on improving care delivery by focusing on connecting hospital safety with hospital financial stability, by appropriating stimulus funds to center on quality and safety programs like those described above. Here is how: a hospital that would receive stimulus money for employing nurse discharge advocates would preserve employment while advancing patient safety, as would a hospital that retains a nurse‐to‐patient ratio above a specified threshold. By focusing on measures of structural quality, the government could improve care in ways that are easy to measure and maximize local economic stimulus without difficult outcomes assessment, insurance reform, or duplicating process measure efforts. There could even be an innovation differential (ie, payment/reward) for hospitals that improve quality while holding flat or lowering overall costs.
Equally important is to use this national financial crisis as an opportunity to improve monitoring of hospital quality. While quality assessment of hospitals is difficult, increased federal awareness of local medical need, hospital financial stability, and government awareness of emergency services overcrowding, nurse‐to‐patient ratios, and IT utilization are all valuable and easy to measure.
None of these quality‐focused fiscal interventions would be guaranteed to prevent hospital closure. Especially in small population centers, hospital closures can affect an entire community's financial growth and clinical safety net,20 while leaving hundreds or even thousands unemployed. Hospital closure should be assessed by state and federal government officials in these larger terms, perhaps even encouraging closure when appropriate, and helping prevent it when necessary.
Conclusion
Hospitals, as complex pieces of America's health care system, are central to communities' safety and economic growth. While national health coverage reform, as currently being discussed in Washington, would make hospital infrastructure less sensitive to macroeconomic changes, major reform would not come fast enough if hospitals start closing. While the worst of the recession may be over, recovery and the continuing rise in unemployment is a tenuous lifeline for hospitals on the financial brink.
We are not arguing against all hospital layoffs, or even closures. Indeed, this recession is a lean time for most industries and is likely to lead to closures for hospitals that cannot compete on efficiency or quality. But a hospital closure is a major event for a community and should not be permitted to occur without thorough consideration of alternatives. Current data on hospitals' financial status and clinical safety are limited, potentially biased, and not timely enough for this rapidly changing economic crisis. Therefore, state and federal government officials should assess whether hospitals would be eligible not just for possible emergency loans, but for linking loans to quality of care and community need. In so doing, this difficult time could be an opportunity to help hospitals improve their care, rather than watching it diminish.
With the United States mired in its most severe recession in decades, stories of hospital struggles have emerged. Beaumont Hospital, located near the headquarters of major automakers and several assembly plants outside Detroit, recently cut hundreds of jobs and put major construction on indefinite hold.1 The CEO of Boston's Beth Israel Deaconess Medical Center made an agreement with employees to take large cuts in pay and vacation time to prevent laying off 10% of the staff.2 The University of Chicago Medical Center made plans to limit the number of emergency room beds, thereby decreasing low‐reimbursing emergency admissions while making beds available for higher‐paying elective hospitalizations.3
What is surprising about these stories is that hospitals have long been considered recession‐proof. Yet, with one‐half of US hospitals having reduced their staff to balance their budgets4 and with hospitals' financial margins falling dramatically,5 economic struggles are now a widespread problem.
Furthermore, it is difficult to determine if hospitals' clinical care has been damaged by the recession. The measurement of hospital quality is new and still under‐developed: there is virtually no reliable information on hospital quality from previous recessions, and even now it will be difficult to assess quality in real time.
Critics of waste and excess in the US health care system may see tough economic times as a Darwinian proving ground for hospitals, through which efficiency will improve and poor performers will close their doors. But more likely, hospital cutbacks will risk the quality and safety of health care delivery. For reasons of both public health and fiscal impact on communities, state and federal leaders may need to watch these trends closely to design and to be ready to implement potential government remedies for hospitals' fiscal woes.
In this commentary, we describe how hospitals have fared historically during recessions, how this recession could have different effectsfirst fiscally, then clinically, and we examine policy options to mitigate these untoward effects.
Decades of Recession‐Proof Hospitals
During the Great Depression, hospital insolvency was a national problem that prompted federal and state aid. Keeping hospitals alive was a critical policy goal and proved central to the early development of health insurance that focused on payment for hospital care.6
Since WWII, growth in America's hospitals has been only loosely related to national macroeconomic trends, with other changes like technological innovations and the advent of managed care far more influential to hospital finances. In fact, during recessions, hospital care spending growth often escalates in tandem with worsening unemployment (Figure 1). One explanation for this phenomenon is that economic pressures lead to declining primary care utilization, with adverse consequences for individuals' health.7
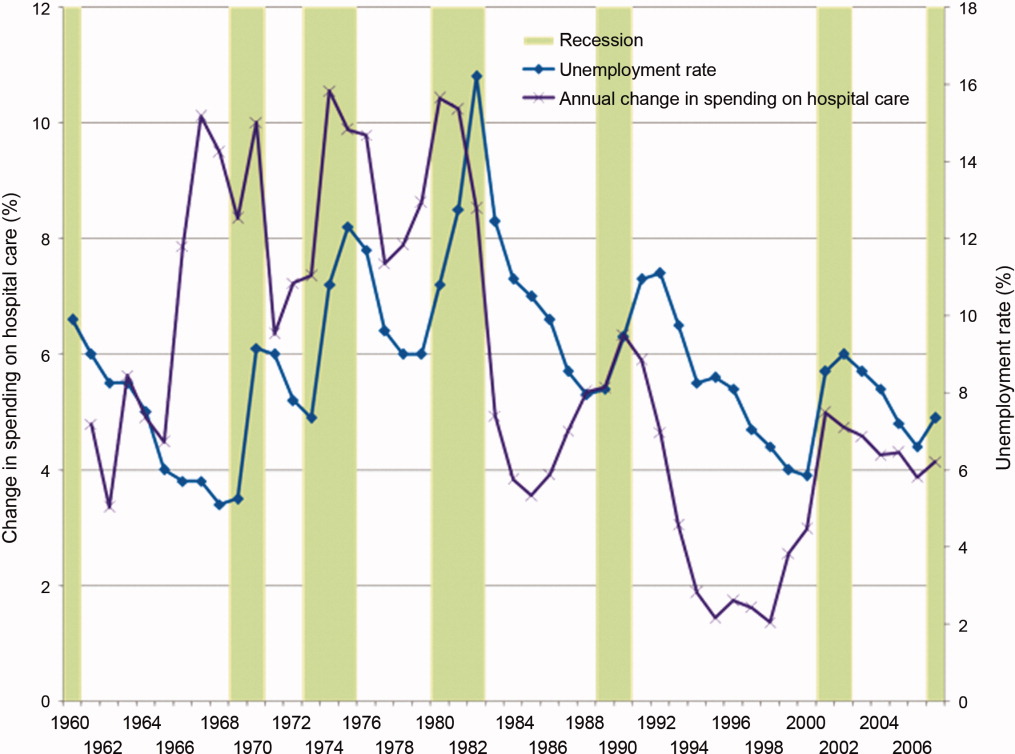
Hospitals' Current Fiscal Vulnerability
However, the current recession is the worst in 70 years. Every method of income generation available to hospitals appears at risk, including reimbursement per discharge (70% of hospitals report moderate or significant increases in uncompensated care), number of inpatient admissions (over one‐half report a moderate or significant decrease), difficulty obtaining bonds (60% report at least significant problems), and charitable donations.4 Over 50% of US hospitals had negative margins in the fourth quarter of 2008, though there has been some improvement since that time.8
Future hospital stability concerns remain. Growth in revenue per discharge is still below the norm.5 Because employment lags a recovering economy, further reimbursement decreases are possible from increasing proportions of patients with low‐reimbursing insurers or no coverage at all, decreasing payment rates from all payers, and decreasing elective care. The lower‐reimbursing payers, like state Medicaid programs, are experiencing increased enrollment as Americans lose their jobs and their better‐paying, employer‐sponsored private insurance.9 There's also evidence that reimbursement rates are declining from both Medicare and private insurers,10 which threatens the fragile cost‐shift through which hospitals have long used private insurance reimbursement to subsidize government reimbursements.11
Hospitals' specific financial challenges will likely vary across markets. The authors' state of Michigan has been hit particularly long and hard by the current recession. Unemployment rates exceeding 11% are expected to cause dramatic losses in private health insurance.9 Patients' increasing need with decreasing ability to pay will make markets in the deepest recession particularly vulnerable.
Hospital Quality and Safety at Risk?
The effect of the recession on the quality of hospital care is less clear. Until the 1990s, hospital quality was essentially assumed and virtually unmeasured. Even now, measuring hospital quality is difficult and rarely timely. Medicare data often take 1 to 2 years to become publicly available for analysis. Reports by trade organizations like the American Hospital Association are up‐to‐date but have conflicts of interest and are less rigorous. The most timely measures of hospitals' distressflawed as they may bewill come from the hospitals themselves, just like reports of economic woe from other businesses and government agencies during challenging economic times.
However, since the publication of the 1999 report To Err is Human,12 major improvements in hospital quality and safety have transformed the delivery of inpatient care. These improvements have taken the form of simple interventions like nationally consistent medical abbreviations, management initiatives like Six Sigma, and technological advances including computerized health records.
Nonetheless, during this recession and recovery, slashed hospital budgets may slow or even stop the momentum towards further improvements in quality and safety. Frontline care delivery could be at risk. Understaffed and under financed hospitals are rarely safe. Dissatisfaction and layoffs hurt the interactions between employees and patients. Robust nurse‐to‐patient ratios which have proven vital to patients' hospital outcomes could be at risk.13 Admittedly, recession‐induced threats to quality and safety are conjectures on our part: unfortunately, no recession measures of hospitals' specific spending on staffing, technology, or process improvements exist.
However, there are many small, evidence‐based changes that could improve hospital safety dramatically in the near future. Michigan's Keystone ICU Initiative showed that systematic interventions in routine care delivery could reduce the risk of catheter‐related bloodstream infections, which currently are implicated in the death of 28,000 Americans per year, to nearly zero.14 The Institute for Healthcare Improvement's 100,000 Lives Campaign also illustrated that dramatic improvements in hospital‐related mortality can occur with fairly focused interventions. In the month after discharge, more than one‐quarter of all hospitalized patients go to an emergency room or need to be rehospitalized. This rate can be cut by 30% by inserting a nurse discharge advocate into the discharge process.15 Instituting a simple safety checklist before surgery decreased surgery‐related mortality and complications by over one‐third.16
Such interventions are effective, reasonable, and widely accessible. Over the long‐term, many may even be cost‐saving. But, importantly, they all require an institutional investment in start‐up money and an organizational will to change how things have been done. In a period of recession with severe cost‐cutting, and a recovery period of cautious spending, this may not be possible.
A Possible Stimulus: Investing in Quality Initiatives at Fiscally Vulnerable Hospitals
It is not enough to keep hospitals' doors open in a recession. Hospitals must continue to improve the quality and safety of the care they delivervital for their future patients and also for their communities who depend on them as anchors of health systems. We believe there is a need for a new, federally supported alignment of hospital finance and hospital quality that can limit damage to hospitals, help community employment, and improve patient safety.
Timely, structural quality measures could speed the introduction of functional value‐based purchasing, promote hospital safety, and help local economies at the same time. There are many simple structural measures that could be examined, such as development of discharge coordinators, promoting effective nurse‐to‐patient ratios, and encouraging health information technology (IT). Importantly, this would not duplicate efforts already underway to promote quality with process measures. With effective financial monitoring in real time, these measures could focus on high‐risk, fiscally disadvantaged hospitals.
To its credit, the Obama administration has already reached out to support hospitals, although aid has not been targeted specifically to hospitals in the most dire financial circumstances. Along with support for Medicaid and community health centers to improve primary care during the recession, the administration has provided a $268 million increase in Disproportionate Share Hospital payments towards hospitals that care for vulnerable patients, an increase of about 3%.17 Concurrently, the Centers for Medicare and Medicaid Services are implementing a value‐based purchasing program that starts with a 5% withhold in reimbursement that institutions need to earn back through a combination of mortality, process, and patient satisfaction metrics.18 The administration also reserved $19 billion to promote improvement of health IT for American medicine.19
Using health IT investment to help hospitals is an appealing concept, but for many institutions the infrastructure required to make that transition directly competes with other patient needs, including bedside patient care. IT investments have large initial costs, at a time when bank loans are difficult to acquire and few organizations can make expensive capital improvements. In fact, one‐quarter of hospitals report scaling back health IT investments that they had already started, in spite of the stimulus funds available.4
Instead, the administration may have more influence on improving care delivery by focusing on connecting hospital safety with hospital financial stability, by appropriating stimulus funds to center on quality and safety programs like those described above. Here is how: a hospital that would receive stimulus money for employing nurse discharge advocates would preserve employment while advancing patient safety, as would a hospital that retains a nurse‐to‐patient ratio above a specified threshold. By focusing on measures of structural quality, the government could improve care in ways that are easy to measure and maximize local economic stimulus without difficult outcomes assessment, insurance reform, or duplicating process measure efforts. There could even be an innovation differential (ie, payment/reward) for hospitals that improve quality while holding flat or lowering overall costs.
Equally important is to use this national financial crisis as an opportunity to improve monitoring of hospital quality. While quality assessment of hospitals is difficult, increased federal awareness of local medical need, hospital financial stability, and government awareness of emergency services overcrowding, nurse‐to‐patient ratios, and IT utilization are all valuable and easy to measure.
None of these quality‐focused fiscal interventions would be guaranteed to prevent hospital closure. Especially in small population centers, hospital closures can affect an entire community's financial growth and clinical safety net,20 while leaving hundreds or even thousands unemployed. Hospital closure should be assessed by state and federal government officials in these larger terms, perhaps even encouraging closure when appropriate, and helping prevent it when necessary.
Conclusion
Hospitals, as complex pieces of America's health care system, are central to communities' safety and economic growth. While national health coverage reform, as currently being discussed in Washington, would make hospital infrastructure less sensitive to macroeconomic changes, major reform would not come fast enough if hospitals start closing. While the worst of the recession may be over, recovery and the continuing rise in unemployment is a tenuous lifeline for hospitals on the financial brink.
We are not arguing against all hospital layoffs, or even closures. Indeed, this recession is a lean time for most industries and is likely to lead to closures for hospitals that cannot compete on efficiency or quality. But a hospital closure is a major event for a community and should not be permitted to occur without thorough consideration of alternatives. Current data on hospitals' financial status and clinical safety are limited, potentially biased, and not timely enough for this rapidly changing economic crisis. Therefore, state and federal government officials should assess whether hospitals would be eligible not just for possible emergency loans, but for linking loans to quality of care and community need. In so doing, this difficult time could be an opportunity to help hospitals improve their care, rather than watching it diminish.
- Michigan's Health Care Safety Net: In Jeopardy.2009.
- .Final budget decisions.Running A Hospital. Vol 2009.Boston, MA;2009.
- .Doctors Plan to Limit Beds in ER.Wall Street Journal.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, DC2009.
- ,.Hospital Operational and Financial Performance Improving.Ann Arbor, MI:Thomson Reuters Center for Healthcare Improvement.2009.
- .The Social Transformation of American Medicine.New York, NY:Basic Books;1983.
- AAFP.Patient Care during the 2008‐2009 Recession – Online Survey.Leawood, KS:AAFP.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, D.C.:American Hospital Association.2009.
- The economic downturn and its impact on hospitals. American Hospital Association Trendwatch.2009.
- ,,.The Current Recession and U.S. Hospitals:Center for Healthcare Improvement.2009.
- ,,.The cost‐shift payment ‘hydraulic’: foundation, history, and implications.Health Aff (Millwood).2006;25(1):22–33.
- ,.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346(22):1715–1722.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- Disproportionate Share Hospital (DSH). Available at: http://www.hhs. gov/recovery/cms/dsh.html. Accessed December 2009.
- ,,.Measuring outcomes and efficiency in medicare value‐based purchasing.Health Aff (Millwood).2009;28(2):w251–w261.
- .Stimulating the adoption of health information technology.N Engl J Med.2009;360(15):1477–1479.
- ,,,.The effect of rural hospital closures on community economic health.Health Serv Res.2006;41(2):467–485.
- Michigan's Health Care Safety Net: In Jeopardy.2009.
- .Final budget decisions.Running A Hospital. Vol 2009.Boston, MA;2009.
- .Doctors Plan to Limit Beds in ER.Wall Street Journal.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, DC2009.
- ,.Hospital Operational and Financial Performance Improving.Ann Arbor, MI:Thomson Reuters Center for Healthcare Improvement.2009.
- .The Social Transformation of American Medicine.New York, NY:Basic Books;1983.
- AAFP.Patient Care during the 2008‐2009 Recession – Online Survey.Leawood, KS:AAFP.2009.
- The Impact of the Economic Crisis on Health Services for Patients and Communities.Washington, D.C.:American Hospital Association.2009.
- The economic downturn and its impact on hospitals. American Hospital Association Trendwatch.2009.
- ,,.The Current Recession and U.S. Hospitals:Center for Healthcare Improvement.2009.
- ,,.The cost‐shift payment ‘hydraulic’: foundation, history, and implications.Health Aff (Millwood).2006;25(1):22–33.
- ,.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346(22):1715–1722.
- ,,, et al.An intervention to decrease catheter‐related bloodstream infections in the ICU.N Engl J Med.2006;355(26):2725–2732.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- Disproportionate Share Hospital (DSH). Available at: http://www.hhs. gov/recovery/cms/dsh.html. Accessed December 2009.
- ,,.Measuring outcomes and efficiency in medicare value‐based purchasing.Health Aff (Millwood).2009;28(2):w251–w261.
- .Stimulating the adoption of health information technology.N Engl J Med.2009;360(15):1477–1479.
- ,,,.The effect of rural hospital closures on community economic health.Health Serv Res.2006;41(2):467–485.
Patient Hospital Financial Burden
Hospitalizations often impose a tremendous financial burden on patients and their families, adding to the stress and long‐term impact from medical illnesses. It is widely underappreciated that physicians can play an important role in substantially reducing patients' out‐of‐pocket expenses by participating in hospital‐based case review and utilization management. These topics are not a focus of most formal training curricula and unfortunately are typically viewed by medical staff as intrusive, time consuming, or only in terms of enhancing the facility's profitability. In reality, with strict rules governing insurance benefits the facility's interests are typically aligned with those of the patient.
One of the greatest impacts on a patient's financial liability is whether an admission is classified in observation vs. inpatient status, and is subject to much confusion. It is a common misperception that these are time‐based designations. Instead, they revolve around stringent medical necessity guidelines that examine the severity of the illness and the intensity of services provided.1 Inpatient stays may be brief, even a single day, if justified by medical need (although these short durations are closely scrutinized by the payors) or if involving a short list of procedures automatically triggering that status (ie, defibrillator placement).2 Conversely, observation status, although usually up to only 48 hours, can extend longer if inpatient criteria are never met and are then apt to generate large bills.
The key concept for the financial liability of patients in observation status is that their billing structure revolves around being categorized as outpatients, even though they stay overnight and are physically housed and cared for in the expensive hospital setting.3 This nonintuitive classification can culminate in unexpectedly high charges for which the patient is liable (Table 1): medications at inflated hospital pharmacy prices, especially when expensive antibiotics or immunosuppressive agents are administered (since outpatient prescriptions are not often covered by policies); ancillary services, radiology or laboratory tests with a high patient share of cost; and an hourly room charge that can easily exceed $30 per hour. The latter can be especially burdensome, as most insurance plans only cover the first 48 hours of observation. During that period the patient would be liable for just their copayment, but afterward they could be billed for the full amount. Hospitalizations well beyond the 48 hours can thus present tremendous hardships to those patients who never meet the stringent criteria for categorization as inpatients, and whose status thus must remain outpatient‐observation. Keeping patients over a weekend for procedures that are not available at the facility until the following Monday can put these individuals beyond the 48 hour observation interval and cause unintentional rapidly escalating out‐of‐pocket expenses. Other strategies to reduce the patient's financial liability include allowing patients to take their own medications from home (with pharmacy supervision and verification, per hospital guidelines), and limiting evaluations to just the admitting diagnosis (ie, pursuing other issues after discharge). In addition, an observation stay can never be ordered ahead of time for an outpatient procedure, as that type of admission is reserved for those individuals who unexpectedly need further care at the conclusion of the recovery period (typically 4 to 6 hours). Thus, the not uncommon practice of doing a patient a favor by letting them stay overnight after an outpatient procedure thereby can be a great disservice by dramatically increasing patient liability. One can well imagine how these scenarios lead to lay press exposs of the patient receiving a bill for a $25 aspirin and a night's stay 4 times more expensive than a luxury hotel. This is not to say that going home is the best or safest plan for a particular patient, but rather that the hospital is often an unnecessarily expensive (and in that sense inappropriate) location when there are alternatives. It is up to the individual hospital to determine how to handle rapidly escalating charges related to the admission status and the timeliness of a discharge. Many centers in effect write off highly select bills that are considered either uncollectible (ie, from indigent patients) or the fault of the facility's inefficiencies. So as not to have inconsistent billing policies across different insurers and patients, however, facilities are obligated to have uniform protocols for attempting to collect chargesa scenario that can be quite harsh for those individuals with significant and discoverable monetary resources.
| Observation (Outpatient Status) (Medicare Part B) | Inpatient (Medicare Part A) | |
|---|---|---|
| ||
| Room and board | Medicare deductible: $1068 per admission (waived if readmission in < 60 days) | |
| 48 hours | 20% of allowable charge (APC) | |
| >48 hours | 100% hospital charges | |
| Medications | 100% hospital charges | |
| Supplies | Up to 100% hospital charges | |
| Surgical | ||
| Operating room | Typically 20% copay of APC | |
| Recovery room | Typically 20% copay of APC | |
| Diagnostic | ||
| Laboratory | 20% copay of allowable charges | |
| Radiology | 20% copay of allowable charges | |
| Ancillary | ||
| Physical therapy | 20% copay of allowable charges | |
| Occupational therapy | 20% copay of allowable charges | |
| Speech therapy | 20% copay of allowable charges | |
Working with the physician for a timely discharge, hospital case managers and social workers are likely to arrive at creative solutions in the patient's best financial interest (ie, taxicab coupons and inexpensive hotels). As many patients simply do not have the resources to cope with unplanned overnight charges, it behooves the physician to make every effort to start outpatient procedures early in the day so as to minimize the chance of logistic problems triggering a potentially expensive overnight hospital stay.
Compare the observation patient's liability to that of the typically much‐preferred status of inpatient (Table 1) in which all expenses are rolled into one diagnosis‐related group (DRG) prospective payment.3 In the case of Medicare, the patient's bill would be the inpatient deductible, and this might be covered in its entirety by a supplemental policy. One absolutely cannot, however, simply avoid using the observation status and instead make all admissions inpatients; this would cause unnecessary resource utilization and expose the hospital to denial of payment for the entire episode of care. To prevent this situation, there are nationally‐recognized guidelines that strictly define when a hospitalization warrants an inpatient level of care. Integral to the individual qualifying for their policy's inpatient benefit, however, is that the chart must reflect not just the severity of illness but also intensity of services ordered by the physician.1 Similarly, changing a patient's status (ie, from observation to inpatient) must follow rigorous guidelines wherein the justification and timing are fully described in the body of the chart to an extent that would withstand audit.
Consider the example (Table 2) of a patient with a leg fracture admitted for pain due to edema and early compartment syndrome: a scenario appropriate for inpatient status, liability of just the $1092 Medicare deductible, and eligibility for postdischarge skilled nursing facility care. Had the charting erroneously only indicated pain and need for a new cast, then observation status would have yielded a bill for $3426, plus out of pocket nursing home expenses of over $150/day.
| Patient Liability for Observation Status (Medicare Part B) | Inpatient Charges (Covered by Medicare Part A Deductible) | |
|---|---|---|
| ||
| Room and board | $1788 | $1030 |
| Medications | $755 | $1196 |
| Supplies | $106 | $528 |
| Procedures and emergency room | $229 | $1145 |
| Diagnostic | ||
| Laboratory | $72 | $359 |
| Radiology | $159 | $795 |
| Ancillary | ||
| Electrocardiogram | $22 | $110 |
| Physical therapy | $295 | $1475 |
| Patient liability for hospitalization | $3426 | $1068 deductible for total charges of $6638 |
| Patient liability for subsequent skilled nursing facility | $159 per day* | Small daily co‐pay* |
Not only does the physician need to accurately chart the reasons for admission, but it is also extremely helpful to specifically document why the patient is not amenable to outpatient therapy. Examples include a clearly articulated history of failed attempts at home or emergency room treatment, or the need for close monitoring (ie, telemetry). In this regard case managers also provide a fresh set of eyes to evaluate the clarity and completeness of medical charting. What seems like obvious decision‐making to a physician may require expanded detailed notes to satisfy a third‐party review.
The work design of the case managers and utilization review team varies between facilities. Ideally, cases are reviewed upon admission (or within the first 24 hours), and then periodically thereafter. Many medical centers have this process computerized, wherein inpatient criteria are available online and status issues can be tracked daily. This nearly real‐time information serves as the basis for interacting with the attending physician, and is necessary because the chart documentation may not be amended after discharge. Having a robust database for all admissions is also immensely helpful in those hospitals which employ a Physician Advisor (PA) as a liaison and educator to the medical staff. This newly and now nationally recognized PA position serves an important role in educating the providers not just about these patient advocacy topics, but also other issues such as length‐of‐stay. Interestingly, having the infrastructure of a criteria‐driven database to follow the intensity of inpatient services on a daily basis gives case managers an objective perspective of when a patient requires less care and is ready for transfer to a lower acuity facility or discharge home. Physician participation is important when the patient thus runs out of intensities, since there will need to be early coordination of efforts for home health or skilled nursing care, durable medical equipment supplies, or outpatient infusions. It is important that physicians not view these activities as an inappropriate rush for discharge. In our experience most patients are in fact much happier to be out of the hospital and receiving home or skilled nursing care. Those in need of physical or occupational therapy may in fact have superior care in facilities dedicated to those activities. In addition, unnecessarily prolonged hospitalizations carry their own risks, such as hospital‐acquired infections and deep venous thromboses. An additional motivator for discharge is that, just as there are insurance plan limits for outpatient benefits, there can also be caps for inpatient services. Physicians thus have a role in preserving the limited and precious number of covered inpatient days of care, beyond which time the patient would be financially totally responsible. For example, most states limit the number of inpatient days covered by Medicaid. In Florida there is a cap of only 45 days per year (unless the patient is pediatric or within the first year of a transplant4). Similarly, there have been patients and families shocked and ill‐prepared to discover that all their Medicare hospital benefits were exhausted5: a not well‐publicized possibility, as in the setting of expensive intensive care units, transplantation, or chemotherapy. Timely discharges and careful resource utilization by physicians thus not only help the hospital but also are important for the patient.
In summary, physicians need to be aware that there can be tremendous financial hardship to patients caused by inappropriate or unnecessarily long observation stays, especially in cases where an inpatient designation would have been justified by appropriate documentation. Case managers, although employed by the facility, can thus assist physicians in this regard and together play an important role as patient advocates.
- Interqual® Level of Care Criteria: Acute Care Adult.Newton, MA:McKesson Health Solutions;2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Final changes to the hospital outpatient prospective payment system and CY 2009. Available at: http://www.cms.hhs.gov/HospitalOutpatientPPS/HORD/list.asp. Accessed September 2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Medicare Program; Changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/IPPS/itemdetail.asp. Accessed September 2009.
- Florida Medicaid covered services. Available at: http://www.fdhc.state. fl.us/Medicaid/MediPass/pdf/HealthyOutcomesCoveredServicesFlyerEnglish 0606.pdf. Accessed September 2009.
- Medicare Benefit Policy Manual: Chapter 5. Lifetime reserve days. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c05.pdf. Accessed September 2009.
Hospitalizations often impose a tremendous financial burden on patients and their families, adding to the stress and long‐term impact from medical illnesses. It is widely underappreciated that physicians can play an important role in substantially reducing patients' out‐of‐pocket expenses by participating in hospital‐based case review and utilization management. These topics are not a focus of most formal training curricula and unfortunately are typically viewed by medical staff as intrusive, time consuming, or only in terms of enhancing the facility's profitability. In reality, with strict rules governing insurance benefits the facility's interests are typically aligned with those of the patient.
One of the greatest impacts on a patient's financial liability is whether an admission is classified in observation vs. inpatient status, and is subject to much confusion. It is a common misperception that these are time‐based designations. Instead, they revolve around stringent medical necessity guidelines that examine the severity of the illness and the intensity of services provided.1 Inpatient stays may be brief, even a single day, if justified by medical need (although these short durations are closely scrutinized by the payors) or if involving a short list of procedures automatically triggering that status (ie, defibrillator placement).2 Conversely, observation status, although usually up to only 48 hours, can extend longer if inpatient criteria are never met and are then apt to generate large bills.
The key concept for the financial liability of patients in observation status is that their billing structure revolves around being categorized as outpatients, even though they stay overnight and are physically housed and cared for in the expensive hospital setting.3 This nonintuitive classification can culminate in unexpectedly high charges for which the patient is liable (Table 1): medications at inflated hospital pharmacy prices, especially when expensive antibiotics or immunosuppressive agents are administered (since outpatient prescriptions are not often covered by policies); ancillary services, radiology or laboratory tests with a high patient share of cost; and an hourly room charge that can easily exceed $30 per hour. The latter can be especially burdensome, as most insurance plans only cover the first 48 hours of observation. During that period the patient would be liable for just their copayment, but afterward they could be billed for the full amount. Hospitalizations well beyond the 48 hours can thus present tremendous hardships to those patients who never meet the stringent criteria for categorization as inpatients, and whose status thus must remain outpatient‐observation. Keeping patients over a weekend for procedures that are not available at the facility until the following Monday can put these individuals beyond the 48 hour observation interval and cause unintentional rapidly escalating out‐of‐pocket expenses. Other strategies to reduce the patient's financial liability include allowing patients to take their own medications from home (with pharmacy supervision and verification, per hospital guidelines), and limiting evaluations to just the admitting diagnosis (ie, pursuing other issues after discharge). In addition, an observation stay can never be ordered ahead of time for an outpatient procedure, as that type of admission is reserved for those individuals who unexpectedly need further care at the conclusion of the recovery period (typically 4 to 6 hours). Thus, the not uncommon practice of doing a patient a favor by letting them stay overnight after an outpatient procedure thereby can be a great disservice by dramatically increasing patient liability. One can well imagine how these scenarios lead to lay press exposs of the patient receiving a bill for a $25 aspirin and a night's stay 4 times more expensive than a luxury hotel. This is not to say that going home is the best or safest plan for a particular patient, but rather that the hospital is often an unnecessarily expensive (and in that sense inappropriate) location when there are alternatives. It is up to the individual hospital to determine how to handle rapidly escalating charges related to the admission status and the timeliness of a discharge. Many centers in effect write off highly select bills that are considered either uncollectible (ie, from indigent patients) or the fault of the facility's inefficiencies. So as not to have inconsistent billing policies across different insurers and patients, however, facilities are obligated to have uniform protocols for attempting to collect chargesa scenario that can be quite harsh for those individuals with significant and discoverable monetary resources.
| Observation (Outpatient Status) (Medicare Part B) | Inpatient (Medicare Part A) | |
|---|---|---|
| ||
| Room and board | Medicare deductible: $1068 per admission (waived if readmission in < 60 days) | |
| 48 hours | 20% of allowable charge (APC) | |
| >48 hours | 100% hospital charges | |
| Medications | 100% hospital charges | |
| Supplies | Up to 100% hospital charges | |
| Surgical | ||
| Operating room | Typically 20% copay of APC | |
| Recovery room | Typically 20% copay of APC | |
| Diagnostic | ||
| Laboratory | 20% copay of allowable charges | |
| Radiology | 20% copay of allowable charges | |
| Ancillary | ||
| Physical therapy | 20% copay of allowable charges | |
| Occupational therapy | 20% copay of allowable charges | |
| Speech therapy | 20% copay of allowable charges | |
Working with the physician for a timely discharge, hospital case managers and social workers are likely to arrive at creative solutions in the patient's best financial interest (ie, taxicab coupons and inexpensive hotels). As many patients simply do not have the resources to cope with unplanned overnight charges, it behooves the physician to make every effort to start outpatient procedures early in the day so as to minimize the chance of logistic problems triggering a potentially expensive overnight hospital stay.
Compare the observation patient's liability to that of the typically much‐preferred status of inpatient (Table 1) in which all expenses are rolled into one diagnosis‐related group (DRG) prospective payment.3 In the case of Medicare, the patient's bill would be the inpatient deductible, and this might be covered in its entirety by a supplemental policy. One absolutely cannot, however, simply avoid using the observation status and instead make all admissions inpatients; this would cause unnecessary resource utilization and expose the hospital to denial of payment for the entire episode of care. To prevent this situation, there are nationally‐recognized guidelines that strictly define when a hospitalization warrants an inpatient level of care. Integral to the individual qualifying for their policy's inpatient benefit, however, is that the chart must reflect not just the severity of illness but also intensity of services ordered by the physician.1 Similarly, changing a patient's status (ie, from observation to inpatient) must follow rigorous guidelines wherein the justification and timing are fully described in the body of the chart to an extent that would withstand audit.
Consider the example (Table 2) of a patient with a leg fracture admitted for pain due to edema and early compartment syndrome: a scenario appropriate for inpatient status, liability of just the $1092 Medicare deductible, and eligibility for postdischarge skilled nursing facility care. Had the charting erroneously only indicated pain and need for a new cast, then observation status would have yielded a bill for $3426, plus out of pocket nursing home expenses of over $150/day.
| Patient Liability for Observation Status (Medicare Part B) | Inpatient Charges (Covered by Medicare Part A Deductible) | |
|---|---|---|
| ||
| Room and board | $1788 | $1030 |
| Medications | $755 | $1196 |
| Supplies | $106 | $528 |
| Procedures and emergency room | $229 | $1145 |
| Diagnostic | ||
| Laboratory | $72 | $359 |
| Radiology | $159 | $795 |
| Ancillary | ||
| Electrocardiogram | $22 | $110 |
| Physical therapy | $295 | $1475 |
| Patient liability for hospitalization | $3426 | $1068 deductible for total charges of $6638 |
| Patient liability for subsequent skilled nursing facility | $159 per day* | Small daily co‐pay* |
Not only does the physician need to accurately chart the reasons for admission, but it is also extremely helpful to specifically document why the patient is not amenable to outpatient therapy. Examples include a clearly articulated history of failed attempts at home or emergency room treatment, or the need for close monitoring (ie, telemetry). In this regard case managers also provide a fresh set of eyes to evaluate the clarity and completeness of medical charting. What seems like obvious decision‐making to a physician may require expanded detailed notes to satisfy a third‐party review.
The work design of the case managers and utilization review team varies between facilities. Ideally, cases are reviewed upon admission (or within the first 24 hours), and then periodically thereafter. Many medical centers have this process computerized, wherein inpatient criteria are available online and status issues can be tracked daily. This nearly real‐time information serves as the basis for interacting with the attending physician, and is necessary because the chart documentation may not be amended after discharge. Having a robust database for all admissions is also immensely helpful in those hospitals which employ a Physician Advisor (PA) as a liaison and educator to the medical staff. This newly and now nationally recognized PA position serves an important role in educating the providers not just about these patient advocacy topics, but also other issues such as length‐of‐stay. Interestingly, having the infrastructure of a criteria‐driven database to follow the intensity of inpatient services on a daily basis gives case managers an objective perspective of when a patient requires less care and is ready for transfer to a lower acuity facility or discharge home. Physician participation is important when the patient thus runs out of intensities, since there will need to be early coordination of efforts for home health or skilled nursing care, durable medical equipment supplies, or outpatient infusions. It is important that physicians not view these activities as an inappropriate rush for discharge. In our experience most patients are in fact much happier to be out of the hospital and receiving home or skilled nursing care. Those in need of physical or occupational therapy may in fact have superior care in facilities dedicated to those activities. In addition, unnecessarily prolonged hospitalizations carry their own risks, such as hospital‐acquired infections and deep venous thromboses. An additional motivator for discharge is that, just as there are insurance plan limits for outpatient benefits, there can also be caps for inpatient services. Physicians thus have a role in preserving the limited and precious number of covered inpatient days of care, beyond which time the patient would be financially totally responsible. For example, most states limit the number of inpatient days covered by Medicaid. In Florida there is a cap of only 45 days per year (unless the patient is pediatric or within the first year of a transplant4). Similarly, there have been patients and families shocked and ill‐prepared to discover that all their Medicare hospital benefits were exhausted5: a not well‐publicized possibility, as in the setting of expensive intensive care units, transplantation, or chemotherapy. Timely discharges and careful resource utilization by physicians thus not only help the hospital but also are important for the patient.
In summary, physicians need to be aware that there can be tremendous financial hardship to patients caused by inappropriate or unnecessarily long observation stays, especially in cases where an inpatient designation would have been justified by appropriate documentation. Case managers, although employed by the facility, can thus assist physicians in this regard and together play an important role as patient advocates.
Hospitalizations often impose a tremendous financial burden on patients and their families, adding to the stress and long‐term impact from medical illnesses. It is widely underappreciated that physicians can play an important role in substantially reducing patients' out‐of‐pocket expenses by participating in hospital‐based case review and utilization management. These topics are not a focus of most formal training curricula and unfortunately are typically viewed by medical staff as intrusive, time consuming, or only in terms of enhancing the facility's profitability. In reality, with strict rules governing insurance benefits the facility's interests are typically aligned with those of the patient.
One of the greatest impacts on a patient's financial liability is whether an admission is classified in observation vs. inpatient status, and is subject to much confusion. It is a common misperception that these are time‐based designations. Instead, they revolve around stringent medical necessity guidelines that examine the severity of the illness and the intensity of services provided.1 Inpatient stays may be brief, even a single day, if justified by medical need (although these short durations are closely scrutinized by the payors) or if involving a short list of procedures automatically triggering that status (ie, defibrillator placement).2 Conversely, observation status, although usually up to only 48 hours, can extend longer if inpatient criteria are never met and are then apt to generate large bills.
The key concept for the financial liability of patients in observation status is that their billing structure revolves around being categorized as outpatients, even though they stay overnight and are physically housed and cared for in the expensive hospital setting.3 This nonintuitive classification can culminate in unexpectedly high charges for which the patient is liable (Table 1): medications at inflated hospital pharmacy prices, especially when expensive antibiotics or immunosuppressive agents are administered (since outpatient prescriptions are not often covered by policies); ancillary services, radiology or laboratory tests with a high patient share of cost; and an hourly room charge that can easily exceed $30 per hour. The latter can be especially burdensome, as most insurance plans only cover the first 48 hours of observation. During that period the patient would be liable for just their copayment, but afterward they could be billed for the full amount. Hospitalizations well beyond the 48 hours can thus present tremendous hardships to those patients who never meet the stringent criteria for categorization as inpatients, and whose status thus must remain outpatient‐observation. Keeping patients over a weekend for procedures that are not available at the facility until the following Monday can put these individuals beyond the 48 hour observation interval and cause unintentional rapidly escalating out‐of‐pocket expenses. Other strategies to reduce the patient's financial liability include allowing patients to take their own medications from home (with pharmacy supervision and verification, per hospital guidelines), and limiting evaluations to just the admitting diagnosis (ie, pursuing other issues after discharge). In addition, an observation stay can never be ordered ahead of time for an outpatient procedure, as that type of admission is reserved for those individuals who unexpectedly need further care at the conclusion of the recovery period (typically 4 to 6 hours). Thus, the not uncommon practice of doing a patient a favor by letting them stay overnight after an outpatient procedure thereby can be a great disservice by dramatically increasing patient liability. One can well imagine how these scenarios lead to lay press exposs of the patient receiving a bill for a $25 aspirin and a night's stay 4 times more expensive than a luxury hotel. This is not to say that going home is the best or safest plan for a particular patient, but rather that the hospital is often an unnecessarily expensive (and in that sense inappropriate) location when there are alternatives. It is up to the individual hospital to determine how to handle rapidly escalating charges related to the admission status and the timeliness of a discharge. Many centers in effect write off highly select bills that are considered either uncollectible (ie, from indigent patients) or the fault of the facility's inefficiencies. So as not to have inconsistent billing policies across different insurers and patients, however, facilities are obligated to have uniform protocols for attempting to collect chargesa scenario that can be quite harsh for those individuals with significant and discoverable monetary resources.
| Observation (Outpatient Status) (Medicare Part B) | Inpatient (Medicare Part A) | |
|---|---|---|
| ||
| Room and board | Medicare deductible: $1068 per admission (waived if readmission in < 60 days) | |
| 48 hours | 20% of allowable charge (APC) | |
| >48 hours | 100% hospital charges | |
| Medications | 100% hospital charges | |
| Supplies | Up to 100% hospital charges | |
| Surgical | ||
| Operating room | Typically 20% copay of APC | |
| Recovery room | Typically 20% copay of APC | |
| Diagnostic | ||
| Laboratory | 20% copay of allowable charges | |
| Radiology | 20% copay of allowable charges | |
| Ancillary | ||
| Physical therapy | 20% copay of allowable charges | |
| Occupational therapy | 20% copay of allowable charges | |
| Speech therapy | 20% copay of allowable charges | |
Working with the physician for a timely discharge, hospital case managers and social workers are likely to arrive at creative solutions in the patient's best financial interest (ie, taxicab coupons and inexpensive hotels). As many patients simply do not have the resources to cope with unplanned overnight charges, it behooves the physician to make every effort to start outpatient procedures early in the day so as to minimize the chance of logistic problems triggering a potentially expensive overnight hospital stay.
Compare the observation patient's liability to that of the typically much‐preferred status of inpatient (Table 1) in which all expenses are rolled into one diagnosis‐related group (DRG) prospective payment.3 In the case of Medicare, the patient's bill would be the inpatient deductible, and this might be covered in its entirety by a supplemental policy. One absolutely cannot, however, simply avoid using the observation status and instead make all admissions inpatients; this would cause unnecessary resource utilization and expose the hospital to denial of payment for the entire episode of care. To prevent this situation, there are nationally‐recognized guidelines that strictly define when a hospitalization warrants an inpatient level of care. Integral to the individual qualifying for their policy's inpatient benefit, however, is that the chart must reflect not just the severity of illness but also intensity of services ordered by the physician.1 Similarly, changing a patient's status (ie, from observation to inpatient) must follow rigorous guidelines wherein the justification and timing are fully described in the body of the chart to an extent that would withstand audit.
Consider the example (Table 2) of a patient with a leg fracture admitted for pain due to edema and early compartment syndrome: a scenario appropriate for inpatient status, liability of just the $1092 Medicare deductible, and eligibility for postdischarge skilled nursing facility care. Had the charting erroneously only indicated pain and need for a new cast, then observation status would have yielded a bill for $3426, plus out of pocket nursing home expenses of over $150/day.
| Patient Liability for Observation Status (Medicare Part B) | Inpatient Charges (Covered by Medicare Part A Deductible) | |
|---|---|---|
| ||
| Room and board | $1788 | $1030 |
| Medications | $755 | $1196 |
| Supplies | $106 | $528 |
| Procedures and emergency room | $229 | $1145 |
| Diagnostic | ||
| Laboratory | $72 | $359 |
| Radiology | $159 | $795 |
| Ancillary | ||
| Electrocardiogram | $22 | $110 |
| Physical therapy | $295 | $1475 |
| Patient liability for hospitalization | $3426 | $1068 deductible for total charges of $6638 |
| Patient liability for subsequent skilled nursing facility | $159 per day* | Small daily co‐pay* |
Not only does the physician need to accurately chart the reasons for admission, but it is also extremely helpful to specifically document why the patient is not amenable to outpatient therapy. Examples include a clearly articulated history of failed attempts at home or emergency room treatment, or the need for close monitoring (ie, telemetry). In this regard case managers also provide a fresh set of eyes to evaluate the clarity and completeness of medical charting. What seems like obvious decision‐making to a physician may require expanded detailed notes to satisfy a third‐party review.
The work design of the case managers and utilization review team varies between facilities. Ideally, cases are reviewed upon admission (or within the first 24 hours), and then periodically thereafter. Many medical centers have this process computerized, wherein inpatient criteria are available online and status issues can be tracked daily. This nearly real‐time information serves as the basis for interacting with the attending physician, and is necessary because the chart documentation may not be amended after discharge. Having a robust database for all admissions is also immensely helpful in those hospitals which employ a Physician Advisor (PA) as a liaison and educator to the medical staff. This newly and now nationally recognized PA position serves an important role in educating the providers not just about these patient advocacy topics, but also other issues such as length‐of‐stay. Interestingly, having the infrastructure of a criteria‐driven database to follow the intensity of inpatient services on a daily basis gives case managers an objective perspective of when a patient requires less care and is ready for transfer to a lower acuity facility or discharge home. Physician participation is important when the patient thus runs out of intensities, since there will need to be early coordination of efforts for home health or skilled nursing care, durable medical equipment supplies, or outpatient infusions. It is important that physicians not view these activities as an inappropriate rush for discharge. In our experience most patients are in fact much happier to be out of the hospital and receiving home or skilled nursing care. Those in need of physical or occupational therapy may in fact have superior care in facilities dedicated to those activities. In addition, unnecessarily prolonged hospitalizations carry their own risks, such as hospital‐acquired infections and deep venous thromboses. An additional motivator for discharge is that, just as there are insurance plan limits for outpatient benefits, there can also be caps for inpatient services. Physicians thus have a role in preserving the limited and precious number of covered inpatient days of care, beyond which time the patient would be financially totally responsible. For example, most states limit the number of inpatient days covered by Medicaid. In Florida there is a cap of only 45 days per year (unless the patient is pediatric or within the first year of a transplant4). Similarly, there have been patients and families shocked and ill‐prepared to discover that all their Medicare hospital benefits were exhausted5: a not well‐publicized possibility, as in the setting of expensive intensive care units, transplantation, or chemotherapy. Timely discharges and careful resource utilization by physicians thus not only help the hospital but also are important for the patient.
In summary, physicians need to be aware that there can be tremendous financial hardship to patients caused by inappropriate or unnecessarily long observation stays, especially in cases where an inpatient designation would have been justified by appropriate documentation. Case managers, although employed by the facility, can thus assist physicians in this regard and together play an important role as patient advocates.
- Interqual® Level of Care Criteria: Acute Care Adult.Newton, MA:McKesson Health Solutions;2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Final changes to the hospital outpatient prospective payment system and CY 2009. Available at: http://www.cms.hhs.gov/HospitalOutpatientPPS/HORD/list.asp. Accessed September 2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Medicare Program; Changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/IPPS/itemdetail.asp. Accessed September 2009.
- Florida Medicaid covered services. Available at: http://www.fdhc.state. fl.us/Medicaid/MediPass/pdf/HealthyOutcomesCoveredServicesFlyerEnglish 0606.pdf. Accessed September 2009.
- Medicare Benefit Policy Manual: Chapter 5. Lifetime reserve days. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c05.pdf. Accessed September 2009.
- Interqual® Level of Care Criteria: Acute Care Adult.Newton, MA:McKesson Health Solutions;2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Final changes to the hospital outpatient prospective payment system and CY 2009. Available at: http://www.cms.hhs.gov/HospitalOutpatientPPS/HORD/list.asp. Accessed September 2009.
- Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services (CMS).2008. Medicare Program; Changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/IPPS/itemdetail.asp. Accessed September 2009.
- Florida Medicaid covered services. Available at: http://www.fdhc.state. fl.us/Medicaid/MediPass/pdf/HealthyOutcomesCoveredServicesFlyerEnglish 0606.pdf. Accessed September 2009.
- Medicare Benefit Policy Manual: Chapter 5. Lifetime reserve days. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c05.pdf. Accessed September 2009.
Hospitalists and ACC in Pandemic Flu
Major natural disasters, such as Hurricane Rita and Hurricane Katrina in 2005, have reinforced the reality that health care workers may be asked to treat patients outside the traditional hospital setting.1 The emergence of H5N1 avian influenza in Southeast Asia has also raised concerns about a potential worldwide pandemic influenza.2 Since 2003, the number of avian influenza cases in humans has totaled 387, with 245 deaths.3 While H5N1 influenza has thus far been largely confined to avian populations, the virulence of this strain has raised concern regarding the possible emergence of enhanced human transmission.4 While impossible to accurately forecast the devastation of the next pandemic on the health system, anything similar to the pandemics of the past century will require a large coordinated response by the health system. The most severe pandemic in the past century occurred in 1918 to 1919. The estimated deaths attributed to this worldwide ranges from 20 to 100 million persons,57 with >500,000 of these deaths in the United States.6, 7 In comparison, the annual rate of deaths related to influenza in the United States ranges from 30,000 to 50,000.2, 5 It has been estimated that the next pandemic influenza could cause 75 to 100 million people to become ill, and lead to as many as 1.9 million deaths in the United States.8 In response, the Department of Health and Human Services (HHS) has stressed the importance of advanced planning,9 and the most recent Homeland Security Presidential Directive (HSPD‐21) directs health care organizations and the federal government to develop preparedness plans to provide surge capacity care in times of a catastrophic health event.10 A previous report by one of the authors emphasized the need for hospitalists to play a major role in institutional planning for a pandemic influenza.11
The Alternate Care Center
The concept of offsite care in an influenza pandemic has previously been described, and we will refer to these as Alternate Care Centers (ACCs). Although the literature describes different models of care at an ACC (Table 1),12 we believe an ACC should be activated as an extension of the supporting hospital, once the hospital becomes over capacity despite measures to grow its inpatient service volume.
| Overflow hospital providing full range of care |
| Patient isolation and alternative to home care for infectious patients |
| Expanded ambulatory care |
| Care for recovering, noninfectious patients |
| Limited supportive care for noncritical patients |
| Primary triage and rapid patient screening |
| Quarantine |
Our health system is a large academic medical center, and we have been working with our state to develop a plan to establish and operate an ACC for the next pandemic influenza. Our plans call for an ACC to be activated as an overflow hospital once our hospitals are beyond 120% capacity. We have gone through several functional and tabletop exercises to help identify critical issues that are likely to arise during a real pandemic. Subsequent to these exercises, we have convened an ACC Planning Work Group, reviewed the available literature on surge hospitals, and have focused our recent efforts on several key areas.13 First, it will be important to clearly outline the general services that will be available at this offsite location (Table 2), and this information should be disseminated to the local medical community and the general public. An informed public, with a clear understanding that the ACC is an extension of the hospital with hospitalists in charge of medical care, is more likely to accept getting healthcare in this setting.
|
| IVF administration |
| Parenteral medication administration (eg, antibiotics, steroids, narcotic analgesics, antiemetics) |
| Oxygen support |
| Palliative care services |
Second, hospitals and the ACCas an extension to the main hospitalwill be asked to provide care to patients referred from several external facilities. Thus, the relationship between the ACC and the main hospital is critical. In a situation where local and even national health care assets will be overwhelmed, having a traditional hospital take full ownership of the ACC and facilitate the transport of patients in and out of the center will be vital to the maintenance of operations. Figure 1 illustrates an example of how patients may be transitioned from 1 site of care to another.
Third, the logistics of establishing an ACC should include details regarding: (1) securing a location that is able to accommodate the needs of the ACC; (2) predetermining the scope of care that can be provided; (3) procuring the necessary equipment and supplies; (4) planning for an adequate number of workforce and staff members; and (5) ensuring a reliable communication plan within the local health system and with state and federal public health officials.14 Staffing shortages and communication barriers are worthy of further emphasis. Given conservative estimates that up to 35% of staff may become ill, refuse to work, or remain home to care for ill family members,15 it is essential that hospitals and regional emergency planners develop a staffing model for the ACC, well in advance of a pandemic. These may include scenarios in which the recommended provider‐to‐patient ratio can not be met. Among the essential lessons learned from the severe acute respiratory syndrome (SARS) outbreak in Toronto (Ontario, Canada) was the importance of developing redundant and reliable communication plans among the healthcare providers.16, 17
Last, healthcare workers' concerns about occupational health and safety must be addressed, and strict measures to protect providers in the ACC need to be implemented.16 This includes providing all exposed staff with adequate personal protective equipment (eg, N‐95 masks), ensuring that all staff are vaccinated against the influenza virus, and implementing strict infection control (eg, hand washing) practices.
For more information, we refer the reader to references that contain further details on our ACC exercises13 and documents that outline concepts of operations in an ACC, developed by the Joint Commission and a multiagency working group.1, 14
The Hospitalist Physician and the ACC
During an influenza pandemic, physicians from all specialties will be vital to the success of the health systems' response. General internists,18 family practitioners, and pediatricians will be overextended in the ambulatory setting to provide intravenous (IV) fluids, antibiotics, and vaccines. Emergency physicians will be called upon to provide care for a burgeoning number of patient arrivals to the Emergency Department (ED), whose acuity is higher than in nonpandemic times. These physicians' clinical expertise at their sites of practice may be severely tested. Hospitalists, given their inpatient focus will be ideally suited to provide medical care to patients admitted to the ACC.
Previous physician leadership at surge hospitals has come from multiple specialties. Case studies describing the heroic physician leadership after Hurricane Katrina and Hurricane Rita represented pediatricians, family physicians, emergency department physicians, and internists.1 In an influenza pandemic, patients in the ACC will require medical care that would, under nonsurge situations, warrant inpatient care. Hospitalists are well poised to lead the response in the ACC for pandemic flu. Hospitalists have expanded their presence into many clinical and administrative responsibilities in their local health systems,19 and the specialty of hospital medicine has evolved to incorporate many of the skills and expertise that would be required of physician leaders who manage an ACC during an influenza pandemic.
While the actual morbidity and mortality associated with the next pandemic are uncertain, it is likely that the number of patients who seek out medical care will exceed current capacity. With constrained space and resources, patients will require appropriate and safe transition to and from the hospital and the ACC. Hospitalists have become leaders in developing and promoting quality transition of care out of acute care settings.20, 21 Their expertise in optimizing this vulnerable time period in patients' healthcare experience should help hospitalists make efficient and appropriate transition care decisions even during busy times and in an alternate care location. Many hospitalists have also developed local and national expertise in quality improvement (QI) and patient safety (PS) initiatives in acute care settings.22 Hospitalists can lead the efforts to apply QI and PS practices in the ACC. These interventions should focus on the potential to be effective in improving patient care, but also consider issues such as ease of implementation, cost, and potential for harm.23
An influenza pandemic will require all levels of the healthcare system to work together to develop a coordinated approach to patient care. Previously, Kisuule et al.24 described how hospitalists can expand their role to include public health. The hospitalists' leadership in the ACC fits well with their descriptions, and hospitalists should work with local, state, and national public health officials in pandemic flu planning. Their scope of practice and clinical expertise will call on them to play key roles in recognition of the development of a pandemic; help lead the response efforts; provide education to staff, patients, and family members; develop clinical care guidelines and pathways for patients; utilize best practices in the use of antimicrobial therapy; and provide appropriate palliative care. Depending on the severity of the influenza pandemic, mortality could be considerable. Many hospitalists have expertise in palliative care at their hospitals,2527 and this skill set will be invaluable in providing compassionate end‐of‐life care to patients in the ACC.
In a pandemic, the most vulnerable patient populations will likely be disproportionately affected, including the elderly, children, and the immune‐compromised. Hospitalists who care regularly for these diverse groups of patients through the spectrum of illness and recovery will be able to address the variety of clinical and nonclinical issues that arise. If the ACC will provide care for children, hospitalists with training in pediatrics, medicine‐pediatrics, or family medicine should be available.
Additional Considerations
While many unanswered questions remain about how to best utilize the ACC, hospitalists are ideally suited to help lead planning efforts for an ACC for pandemic flu. Other issues that may require additional considerations include: (1) whether to strictly care for patients with influenza symptoms and influenza‐related illnesses or to provide care for all patients at the ACC; (2) what to do when patients refuse transfer to and from the ACC; (3) determining the optimal staffing model for patient care providers and to provide care for a wide range of age groups; (4) how the ACC will be funded; (5) how and where to store stockpiles; (6) developing redundant and coordinated communication plans; and (7) planning for reliable access to information and technology from the ACC.
Conclusions
We have introduced the concept of the ACC for the hospitalist community, and emphasized the benefits of engaging hospitalists to lead the ACC initiative at their own health organizations during pandemic flu. As hospitalists currently serve in many of these roles and possess the skills to provide care and lead these initiatives, we encourage hospitalists to contact their hospital administrators to volunteer to assist with preparation efforts.
- Joint Commission on Accreditation of Healthcare Organizations. Surge Hospitals: Providing Safe Care in Emergencies;2006. Available at: http://www.jointcommission.org/NR/rdonlyres/802E9DA4‐AE80‐4584‐A205‐48989C5BD684/0/surge_hospital.pdf. Accessed May 2009.
- .Pandemic influenza: are we ready?Disaster Manag Response.2005;3(3):61–67.
- Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO.2008. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2008_09_10/en/index.html. Accessed May 2009.
- ,,, et al.Human infection with highly pathogenic H5N1 influenza virus.Lancet.2008;371(9622):1464–1475.
- .Preparing for the next pandemic.N Engl J Med.2005;352(18):1839–1842.
- ,,.Influenza pandemic preparedness action plan for the United States: 2002 update.Clin Infect Dis.2002;35(5):590–596.
- ,,, et al.Nonpharmaceutical interventions implemented by US cities during the 1918‐1919 influenza pandemic.JAMA.2007;298(6):644–654.
- The Health Care Response to Pandemic Influenza: Position Paper.Philadelphia, PA:American College of Physicians;2006.
- U.S. Department of Health and Human Services (HHS). HHS Pandemic Influenza Plan. November2005. Available at: http://www.hhs.gov/pandemicflu/plan. Accessed May 2009.
- Homeland Security Presidential Directive/HSPD‐21.2007. Available at: http://www.whitehouse.gov/news/releases/2007/10/20071018‐10.html. Accessed May 2009.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1(2):118–123.
- ,,,,.The prospect of using alternative medical care facilities in an influenza pandemic.Biosecur Bioterror.2006;4(4):384–390.
- ,,, et al.Pandemic influenza and acute care centers (ACCs): taking care of sick patients in a non‐hospital setting.Biosecur Bioterror.2008;6(4):335–348.
- ,,.Acute Care Center. Modular Emergency Medical System: Concept of Operations for the Acute Care Center (ACC).Mass Casualty Care Strategy for A Biological Terrorism Incident. May2003. Available at: http://dms.dartmouth.edu/nnemmrs/resources/surge_capacity_guidance/documents/acute_care_center__concept_ of_operations. pdf. Accessed May 2009.
- Illinois Department of Public Health. Influenza.2007. Available at: http://www.idph.state.il.us/flu/pandemicfs.htm. Accessed May 2009.
- ,,.Learning from SARS in Hong Kong and Toronto.JAMA.2004;291(20):2483–2487.
- .Planning for epidemics—the lessons of SARS.N Engl J Med.2004;350(23):2332–2334.
- .The role of internists during epidemics, outbreaks, and bioterrorist attacks.J Gen Intern Med.2007;22(1):131–136.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37‐38):591–596.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,.Executing high‐quality care transitions: a call to do it right.J Hosp Med.2007;2(5):287–290.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- ,.Implementing patient safety interventions in your hospital: what to try and what to avoid.Med Clin North Am.2008;92(2):275–293, vii‐viii.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2(,2):93–101.
- ,,,,,.Evaluating the California hospital initiative in palliative services.Arch Intern Med.2006;166(2):227–230.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- .Palliative care in hospitals.J Hosp Med.2006;1(1):21–28.
Major natural disasters, such as Hurricane Rita and Hurricane Katrina in 2005, have reinforced the reality that health care workers may be asked to treat patients outside the traditional hospital setting.1 The emergence of H5N1 avian influenza in Southeast Asia has also raised concerns about a potential worldwide pandemic influenza.2 Since 2003, the number of avian influenza cases in humans has totaled 387, with 245 deaths.3 While H5N1 influenza has thus far been largely confined to avian populations, the virulence of this strain has raised concern regarding the possible emergence of enhanced human transmission.4 While impossible to accurately forecast the devastation of the next pandemic on the health system, anything similar to the pandemics of the past century will require a large coordinated response by the health system. The most severe pandemic in the past century occurred in 1918 to 1919. The estimated deaths attributed to this worldwide ranges from 20 to 100 million persons,57 with >500,000 of these deaths in the United States.6, 7 In comparison, the annual rate of deaths related to influenza in the United States ranges from 30,000 to 50,000.2, 5 It has been estimated that the next pandemic influenza could cause 75 to 100 million people to become ill, and lead to as many as 1.9 million deaths in the United States.8 In response, the Department of Health and Human Services (HHS) has stressed the importance of advanced planning,9 and the most recent Homeland Security Presidential Directive (HSPD‐21) directs health care organizations and the federal government to develop preparedness plans to provide surge capacity care in times of a catastrophic health event.10 A previous report by one of the authors emphasized the need for hospitalists to play a major role in institutional planning for a pandemic influenza.11
The Alternate Care Center
The concept of offsite care in an influenza pandemic has previously been described, and we will refer to these as Alternate Care Centers (ACCs). Although the literature describes different models of care at an ACC (Table 1),12 we believe an ACC should be activated as an extension of the supporting hospital, once the hospital becomes over capacity despite measures to grow its inpatient service volume.
| Overflow hospital providing full range of care |
| Patient isolation and alternative to home care for infectious patients |
| Expanded ambulatory care |
| Care for recovering, noninfectious patients |
| Limited supportive care for noncritical patients |
| Primary triage and rapid patient screening |
| Quarantine |
Our health system is a large academic medical center, and we have been working with our state to develop a plan to establish and operate an ACC for the next pandemic influenza. Our plans call for an ACC to be activated as an overflow hospital once our hospitals are beyond 120% capacity. We have gone through several functional and tabletop exercises to help identify critical issues that are likely to arise during a real pandemic. Subsequent to these exercises, we have convened an ACC Planning Work Group, reviewed the available literature on surge hospitals, and have focused our recent efforts on several key areas.13 First, it will be important to clearly outline the general services that will be available at this offsite location (Table 2), and this information should be disseminated to the local medical community and the general public. An informed public, with a clear understanding that the ACC is an extension of the hospital with hospitalists in charge of medical care, is more likely to accept getting healthcare in this setting.
|
| IVF administration |
| Parenteral medication administration (eg, antibiotics, steroids, narcotic analgesics, antiemetics) |
| Oxygen support |
| Palliative care services |
Second, hospitals and the ACCas an extension to the main hospitalwill be asked to provide care to patients referred from several external facilities. Thus, the relationship between the ACC and the main hospital is critical. In a situation where local and even national health care assets will be overwhelmed, having a traditional hospital take full ownership of the ACC and facilitate the transport of patients in and out of the center will be vital to the maintenance of operations. Figure 1 illustrates an example of how patients may be transitioned from 1 site of care to another.
Third, the logistics of establishing an ACC should include details regarding: (1) securing a location that is able to accommodate the needs of the ACC; (2) predetermining the scope of care that can be provided; (3) procuring the necessary equipment and supplies; (4) planning for an adequate number of workforce and staff members; and (5) ensuring a reliable communication plan within the local health system and with state and federal public health officials.14 Staffing shortages and communication barriers are worthy of further emphasis. Given conservative estimates that up to 35% of staff may become ill, refuse to work, or remain home to care for ill family members,15 it is essential that hospitals and regional emergency planners develop a staffing model for the ACC, well in advance of a pandemic. These may include scenarios in which the recommended provider‐to‐patient ratio can not be met. Among the essential lessons learned from the severe acute respiratory syndrome (SARS) outbreak in Toronto (Ontario, Canada) was the importance of developing redundant and reliable communication plans among the healthcare providers.16, 17
Last, healthcare workers' concerns about occupational health and safety must be addressed, and strict measures to protect providers in the ACC need to be implemented.16 This includes providing all exposed staff with adequate personal protective equipment (eg, N‐95 masks), ensuring that all staff are vaccinated against the influenza virus, and implementing strict infection control (eg, hand washing) practices.
For more information, we refer the reader to references that contain further details on our ACC exercises13 and documents that outline concepts of operations in an ACC, developed by the Joint Commission and a multiagency working group.1, 14
The Hospitalist Physician and the ACC
During an influenza pandemic, physicians from all specialties will be vital to the success of the health systems' response. General internists,18 family practitioners, and pediatricians will be overextended in the ambulatory setting to provide intravenous (IV) fluids, antibiotics, and vaccines. Emergency physicians will be called upon to provide care for a burgeoning number of patient arrivals to the Emergency Department (ED), whose acuity is higher than in nonpandemic times. These physicians' clinical expertise at their sites of practice may be severely tested. Hospitalists, given their inpatient focus will be ideally suited to provide medical care to patients admitted to the ACC.
Previous physician leadership at surge hospitals has come from multiple specialties. Case studies describing the heroic physician leadership after Hurricane Katrina and Hurricane Rita represented pediatricians, family physicians, emergency department physicians, and internists.1 In an influenza pandemic, patients in the ACC will require medical care that would, under nonsurge situations, warrant inpatient care. Hospitalists are well poised to lead the response in the ACC for pandemic flu. Hospitalists have expanded their presence into many clinical and administrative responsibilities in their local health systems,19 and the specialty of hospital medicine has evolved to incorporate many of the skills and expertise that would be required of physician leaders who manage an ACC during an influenza pandemic.
While the actual morbidity and mortality associated with the next pandemic are uncertain, it is likely that the number of patients who seek out medical care will exceed current capacity. With constrained space and resources, patients will require appropriate and safe transition to and from the hospital and the ACC. Hospitalists have become leaders in developing and promoting quality transition of care out of acute care settings.20, 21 Their expertise in optimizing this vulnerable time period in patients' healthcare experience should help hospitalists make efficient and appropriate transition care decisions even during busy times and in an alternate care location. Many hospitalists have also developed local and national expertise in quality improvement (QI) and patient safety (PS) initiatives in acute care settings.22 Hospitalists can lead the efforts to apply QI and PS practices in the ACC. These interventions should focus on the potential to be effective in improving patient care, but also consider issues such as ease of implementation, cost, and potential for harm.23
An influenza pandemic will require all levels of the healthcare system to work together to develop a coordinated approach to patient care. Previously, Kisuule et al.24 described how hospitalists can expand their role to include public health. The hospitalists' leadership in the ACC fits well with their descriptions, and hospitalists should work with local, state, and national public health officials in pandemic flu planning. Their scope of practice and clinical expertise will call on them to play key roles in recognition of the development of a pandemic; help lead the response efforts; provide education to staff, patients, and family members; develop clinical care guidelines and pathways for patients; utilize best practices in the use of antimicrobial therapy; and provide appropriate palliative care. Depending on the severity of the influenza pandemic, mortality could be considerable. Many hospitalists have expertise in palliative care at their hospitals,2527 and this skill set will be invaluable in providing compassionate end‐of‐life care to patients in the ACC.
In a pandemic, the most vulnerable patient populations will likely be disproportionately affected, including the elderly, children, and the immune‐compromised. Hospitalists who care regularly for these diverse groups of patients through the spectrum of illness and recovery will be able to address the variety of clinical and nonclinical issues that arise. If the ACC will provide care for children, hospitalists with training in pediatrics, medicine‐pediatrics, or family medicine should be available.
Additional Considerations
While many unanswered questions remain about how to best utilize the ACC, hospitalists are ideally suited to help lead planning efforts for an ACC for pandemic flu. Other issues that may require additional considerations include: (1) whether to strictly care for patients with influenza symptoms and influenza‐related illnesses or to provide care for all patients at the ACC; (2) what to do when patients refuse transfer to and from the ACC; (3) determining the optimal staffing model for patient care providers and to provide care for a wide range of age groups; (4) how the ACC will be funded; (5) how and where to store stockpiles; (6) developing redundant and coordinated communication plans; and (7) planning for reliable access to information and technology from the ACC.
Conclusions
We have introduced the concept of the ACC for the hospitalist community, and emphasized the benefits of engaging hospitalists to lead the ACC initiative at their own health organizations during pandemic flu. As hospitalists currently serve in many of these roles and possess the skills to provide care and lead these initiatives, we encourage hospitalists to contact their hospital administrators to volunteer to assist with preparation efforts.
Major natural disasters, such as Hurricane Rita and Hurricane Katrina in 2005, have reinforced the reality that health care workers may be asked to treat patients outside the traditional hospital setting.1 The emergence of H5N1 avian influenza in Southeast Asia has also raised concerns about a potential worldwide pandemic influenza.2 Since 2003, the number of avian influenza cases in humans has totaled 387, with 245 deaths.3 While H5N1 influenza has thus far been largely confined to avian populations, the virulence of this strain has raised concern regarding the possible emergence of enhanced human transmission.4 While impossible to accurately forecast the devastation of the next pandemic on the health system, anything similar to the pandemics of the past century will require a large coordinated response by the health system. The most severe pandemic in the past century occurred in 1918 to 1919. The estimated deaths attributed to this worldwide ranges from 20 to 100 million persons,57 with >500,000 of these deaths in the United States.6, 7 In comparison, the annual rate of deaths related to influenza in the United States ranges from 30,000 to 50,000.2, 5 It has been estimated that the next pandemic influenza could cause 75 to 100 million people to become ill, and lead to as many as 1.9 million deaths in the United States.8 In response, the Department of Health and Human Services (HHS) has stressed the importance of advanced planning,9 and the most recent Homeland Security Presidential Directive (HSPD‐21) directs health care organizations and the federal government to develop preparedness plans to provide surge capacity care in times of a catastrophic health event.10 A previous report by one of the authors emphasized the need for hospitalists to play a major role in institutional planning for a pandemic influenza.11
The Alternate Care Center
The concept of offsite care in an influenza pandemic has previously been described, and we will refer to these as Alternate Care Centers (ACCs). Although the literature describes different models of care at an ACC (Table 1),12 we believe an ACC should be activated as an extension of the supporting hospital, once the hospital becomes over capacity despite measures to grow its inpatient service volume.
| Overflow hospital providing full range of care |
| Patient isolation and alternative to home care for infectious patients |
| Expanded ambulatory care |
| Care for recovering, noninfectious patients |
| Limited supportive care for noncritical patients |
| Primary triage and rapid patient screening |
| Quarantine |
Our health system is a large academic medical center, and we have been working with our state to develop a plan to establish and operate an ACC for the next pandemic influenza. Our plans call for an ACC to be activated as an overflow hospital once our hospitals are beyond 120% capacity. We have gone through several functional and tabletop exercises to help identify critical issues that are likely to arise during a real pandemic. Subsequent to these exercises, we have convened an ACC Planning Work Group, reviewed the available literature on surge hospitals, and have focused our recent efforts on several key areas.13 First, it will be important to clearly outline the general services that will be available at this offsite location (Table 2), and this information should be disseminated to the local medical community and the general public. An informed public, with a clear understanding that the ACC is an extension of the hospital with hospitalists in charge of medical care, is more likely to accept getting healthcare in this setting.
|
| IVF administration |
| Parenteral medication administration (eg, antibiotics, steroids, narcotic analgesics, antiemetics) |
| Oxygen support |
| Palliative care services |
Second, hospitals and the ACCas an extension to the main hospitalwill be asked to provide care to patients referred from several external facilities. Thus, the relationship between the ACC and the main hospital is critical. In a situation where local and even national health care assets will be overwhelmed, having a traditional hospital take full ownership of the ACC and facilitate the transport of patients in and out of the center will be vital to the maintenance of operations. Figure 1 illustrates an example of how patients may be transitioned from 1 site of care to another.
Third, the logistics of establishing an ACC should include details regarding: (1) securing a location that is able to accommodate the needs of the ACC; (2) predetermining the scope of care that can be provided; (3) procuring the necessary equipment and supplies; (4) planning for an adequate number of workforce and staff members; and (5) ensuring a reliable communication plan within the local health system and with state and federal public health officials.14 Staffing shortages and communication barriers are worthy of further emphasis. Given conservative estimates that up to 35% of staff may become ill, refuse to work, or remain home to care for ill family members,15 it is essential that hospitals and regional emergency planners develop a staffing model for the ACC, well in advance of a pandemic. These may include scenarios in which the recommended provider‐to‐patient ratio can not be met. Among the essential lessons learned from the severe acute respiratory syndrome (SARS) outbreak in Toronto (Ontario, Canada) was the importance of developing redundant and reliable communication plans among the healthcare providers.16, 17
Last, healthcare workers' concerns about occupational health and safety must be addressed, and strict measures to protect providers in the ACC need to be implemented.16 This includes providing all exposed staff with adequate personal protective equipment (eg, N‐95 masks), ensuring that all staff are vaccinated against the influenza virus, and implementing strict infection control (eg, hand washing) practices.
For more information, we refer the reader to references that contain further details on our ACC exercises13 and documents that outline concepts of operations in an ACC, developed by the Joint Commission and a multiagency working group.1, 14
The Hospitalist Physician and the ACC
During an influenza pandemic, physicians from all specialties will be vital to the success of the health systems' response. General internists,18 family practitioners, and pediatricians will be overextended in the ambulatory setting to provide intravenous (IV) fluids, antibiotics, and vaccines. Emergency physicians will be called upon to provide care for a burgeoning number of patient arrivals to the Emergency Department (ED), whose acuity is higher than in nonpandemic times. These physicians' clinical expertise at their sites of practice may be severely tested. Hospitalists, given their inpatient focus will be ideally suited to provide medical care to patients admitted to the ACC.
Previous physician leadership at surge hospitals has come from multiple specialties. Case studies describing the heroic physician leadership after Hurricane Katrina and Hurricane Rita represented pediatricians, family physicians, emergency department physicians, and internists.1 In an influenza pandemic, patients in the ACC will require medical care that would, under nonsurge situations, warrant inpatient care. Hospitalists are well poised to lead the response in the ACC for pandemic flu. Hospitalists have expanded their presence into many clinical and administrative responsibilities in their local health systems,19 and the specialty of hospital medicine has evolved to incorporate many of the skills and expertise that would be required of physician leaders who manage an ACC during an influenza pandemic.
While the actual morbidity and mortality associated with the next pandemic are uncertain, it is likely that the number of patients who seek out medical care will exceed current capacity. With constrained space and resources, patients will require appropriate and safe transition to and from the hospital and the ACC. Hospitalists have become leaders in developing and promoting quality transition of care out of acute care settings.20, 21 Their expertise in optimizing this vulnerable time period in patients' healthcare experience should help hospitalists make efficient and appropriate transition care decisions even during busy times and in an alternate care location. Many hospitalists have also developed local and national expertise in quality improvement (QI) and patient safety (PS) initiatives in acute care settings.22 Hospitalists can lead the efforts to apply QI and PS practices in the ACC. These interventions should focus on the potential to be effective in improving patient care, but also consider issues such as ease of implementation, cost, and potential for harm.23
An influenza pandemic will require all levels of the healthcare system to work together to develop a coordinated approach to patient care. Previously, Kisuule et al.24 described how hospitalists can expand their role to include public health. The hospitalists' leadership in the ACC fits well with their descriptions, and hospitalists should work with local, state, and national public health officials in pandemic flu planning. Their scope of practice and clinical expertise will call on them to play key roles in recognition of the development of a pandemic; help lead the response efforts; provide education to staff, patients, and family members; develop clinical care guidelines and pathways for patients; utilize best practices in the use of antimicrobial therapy; and provide appropriate palliative care. Depending on the severity of the influenza pandemic, mortality could be considerable. Many hospitalists have expertise in palliative care at their hospitals,2527 and this skill set will be invaluable in providing compassionate end‐of‐life care to patients in the ACC.
In a pandemic, the most vulnerable patient populations will likely be disproportionately affected, including the elderly, children, and the immune‐compromised. Hospitalists who care regularly for these diverse groups of patients through the spectrum of illness and recovery will be able to address the variety of clinical and nonclinical issues that arise. If the ACC will provide care for children, hospitalists with training in pediatrics, medicine‐pediatrics, or family medicine should be available.
Additional Considerations
While many unanswered questions remain about how to best utilize the ACC, hospitalists are ideally suited to help lead planning efforts for an ACC for pandemic flu. Other issues that may require additional considerations include: (1) whether to strictly care for patients with influenza symptoms and influenza‐related illnesses or to provide care for all patients at the ACC; (2) what to do when patients refuse transfer to and from the ACC; (3) determining the optimal staffing model for patient care providers and to provide care for a wide range of age groups; (4) how the ACC will be funded; (5) how and where to store stockpiles; (6) developing redundant and coordinated communication plans; and (7) planning for reliable access to information and technology from the ACC.
Conclusions
We have introduced the concept of the ACC for the hospitalist community, and emphasized the benefits of engaging hospitalists to lead the ACC initiative at their own health organizations during pandemic flu. As hospitalists currently serve in many of these roles and possess the skills to provide care and lead these initiatives, we encourage hospitalists to contact their hospital administrators to volunteer to assist with preparation efforts.
- Joint Commission on Accreditation of Healthcare Organizations. Surge Hospitals: Providing Safe Care in Emergencies;2006. Available at: http://www.jointcommission.org/NR/rdonlyres/802E9DA4‐AE80‐4584‐A205‐48989C5BD684/0/surge_hospital.pdf. Accessed May 2009.
- .Pandemic influenza: are we ready?Disaster Manag Response.2005;3(3):61–67.
- Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO.2008. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2008_09_10/en/index.html. Accessed May 2009.
- ,,, et al.Human infection with highly pathogenic H5N1 influenza virus.Lancet.2008;371(9622):1464–1475.
- .Preparing for the next pandemic.N Engl J Med.2005;352(18):1839–1842.
- ,,.Influenza pandemic preparedness action plan for the United States: 2002 update.Clin Infect Dis.2002;35(5):590–596.
- ,,, et al.Nonpharmaceutical interventions implemented by US cities during the 1918‐1919 influenza pandemic.JAMA.2007;298(6):644–654.
- The Health Care Response to Pandemic Influenza: Position Paper.Philadelphia, PA:American College of Physicians;2006.
- U.S. Department of Health and Human Services (HHS). HHS Pandemic Influenza Plan. November2005. Available at: http://www.hhs.gov/pandemicflu/plan. Accessed May 2009.
- Homeland Security Presidential Directive/HSPD‐21.2007. Available at: http://www.whitehouse.gov/news/releases/2007/10/20071018‐10.html. Accessed May 2009.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1(2):118–123.
- ,,,,.The prospect of using alternative medical care facilities in an influenza pandemic.Biosecur Bioterror.2006;4(4):384–390.
- ,,, et al.Pandemic influenza and acute care centers (ACCs): taking care of sick patients in a non‐hospital setting.Biosecur Bioterror.2008;6(4):335–348.
- ,,.Acute Care Center. Modular Emergency Medical System: Concept of Operations for the Acute Care Center (ACC).Mass Casualty Care Strategy for A Biological Terrorism Incident. May2003. Available at: http://dms.dartmouth.edu/nnemmrs/resources/surge_capacity_guidance/documents/acute_care_center__concept_ of_operations. pdf. Accessed May 2009.
- Illinois Department of Public Health. Influenza.2007. Available at: http://www.idph.state.il.us/flu/pandemicfs.htm. Accessed May 2009.
- ,,.Learning from SARS in Hong Kong and Toronto.JAMA.2004;291(20):2483–2487.
- .Planning for epidemics—the lessons of SARS.N Engl J Med.2004;350(23):2332–2334.
- .The role of internists during epidemics, outbreaks, and bioterrorist attacks.J Gen Intern Med.2007;22(1):131–136.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37‐38):591–596.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,.Executing high‐quality care transitions: a call to do it right.J Hosp Med.2007;2(5):287–290.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- ,.Implementing patient safety interventions in your hospital: what to try and what to avoid.Med Clin North Am.2008;92(2):275–293, vii‐viii.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2(,2):93–101.
- ,,,,,.Evaluating the California hospital initiative in palliative services.Arch Intern Med.2006;166(2):227–230.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- .Palliative care in hospitals.J Hosp Med.2006;1(1):21–28.
- Joint Commission on Accreditation of Healthcare Organizations. Surge Hospitals: Providing Safe Care in Emergencies;2006. Available at: http://www.jointcommission.org/NR/rdonlyres/802E9DA4‐AE80‐4584‐A205‐48989C5BD684/0/surge_hospital.pdf. Accessed May 2009.
- .Pandemic influenza: are we ready?Disaster Manag Response.2005;3(3):61–67.
- Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO.2008. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2008_09_10/en/index.html. Accessed May 2009.
- ,,, et al.Human infection with highly pathogenic H5N1 influenza virus.Lancet.2008;371(9622):1464–1475.
- .Preparing for the next pandemic.N Engl J Med.2005;352(18):1839–1842.
- ,,.Influenza pandemic preparedness action plan for the United States: 2002 update.Clin Infect Dis.2002;35(5):590–596.
- ,,, et al.Nonpharmaceutical interventions implemented by US cities during the 1918‐1919 influenza pandemic.JAMA.2007;298(6):644–654.
- The Health Care Response to Pandemic Influenza: Position Paper.Philadelphia, PA:American College of Physicians;2006.
- U.S. Department of Health and Human Services (HHS). HHS Pandemic Influenza Plan. November2005. Available at: http://www.hhs.gov/pandemicflu/plan. Accessed May 2009.
- Homeland Security Presidential Directive/HSPD‐21.2007. Available at: http://www.whitehouse.gov/news/releases/2007/10/20071018‐10.html. Accessed May 2009.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1(2):118–123.
- ,,,,.The prospect of using alternative medical care facilities in an influenza pandemic.Biosecur Bioterror.2006;4(4):384–390.
- ,,, et al.Pandemic influenza and acute care centers (ACCs): taking care of sick patients in a non‐hospital setting.Biosecur Bioterror.2008;6(4):335–348.
- ,,.Acute Care Center. Modular Emergency Medical System: Concept of Operations for the Acute Care Center (ACC).Mass Casualty Care Strategy for A Biological Terrorism Incident. May2003. Available at: http://dms.dartmouth.edu/nnemmrs/resources/surge_capacity_guidance/documents/acute_care_center__concept_ of_operations. pdf. Accessed May 2009.
- Illinois Department of Public Health. Influenza.2007. Available at: http://www.idph.state.il.us/flu/pandemicfs.htm. Accessed May 2009.
- ,,.Learning from SARS in Hong Kong and Toronto.JAMA.2004;291(20):2483–2487.
- .Planning for epidemics—the lessons of SARS.N Engl J Med.2004;350(23):2332–2334.
- .The role of internists during epidemics, outbreaks, and bioterrorist attacks.J Gen Intern Med.2007;22(1):131–136.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37‐38):591–596.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,.Executing high‐quality care transitions: a call to do it right.J Hosp Med.2007;2(5):287–290.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- ,.Implementing patient safety interventions in your hospital: what to try and what to avoid.Med Clin North Am.2008;92(2):275–293, vii‐viii.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2(,2):93–101.
- ,,,,,.Evaluating the California hospital initiative in palliative services.Arch Intern Med.2006;166(2):227–230.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- .Palliative care in hospitals.J Hosp Med.2006;1(1):21–28.
Value‐Driven Health Care
It is estimated that the Medicare Part A trust fund will be exhausted by 2016 to 2019; also, the quality of care delivered in the United States is highly variable.13 Value is typically defined as the quality achieved for a given cost (ie, value = quality/cost). The focus on the 3 related concepts of value, quality, and cost of health care is likely to continue to increase. Previously, the U.S. Department of Health and Human Services (HHS) made value‐driven health care one of the Department's top priorities.4 Policymakers are in a period of transition but the publicly available plans of the President and Senate leadership indicate that the focus on value‐based initiatives will likely continue to increase as our nation strives to achieve better outcomes for our health care dollar.5, 6 Specifically, the federal government and other payers increasingly align payment incentives with value and quality, encourage public reporting on quality and Medicare payment costs, such as on the Hospital Compare website (
Since hospital care represented $648 billion in 2006, which is 37% of the total patient‐related U.S. health care expenditure, the trend to pay for value will likely have significant impact on hospitals and hospitalists.7 The Society of Hospital Medicine has a public policy committee that provides feedback to government on programs and policies related to value‐driven health care. The policies and programs need consideration and input from the broader community of hospitalists. This work outlines some of the major national initiatives and policies focused on value‐driven health care and their implications for hospitalists. Hospitalists will need to understand the policy landscape and trends, lead improvement in their individual hospitals to receive value‐based incentives, and assess the opportunities and challenges of current and potential payer programs and policies.
Policies and Initiatives: Implications for Hospitals and Hospitalists
Within the portfolio of value‐driven health care, there are at least 6 major government programs, initiatives, and policies with implications for hospitals and hospitalists: value‐based purchasing (VBP), quality and cost public reporting, Medicare demonstrations, hospital‐acquired conditions, incentives for use of effective HIT, and the physician quality reporting initiative (PQRI) (Table 1).
| Initiative or Policy | Description | Specific Examples | Potential Implications |
|---|---|---|---|
| Value‐based purchasing | At least a portion of hospital payment related to value instead of the traditional fee‐for‐service model | Performance score is based on domains such as process measures (eg, beta‐blocker at discharge for acute myocardial), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Hospital Survey, aka HCAHPS) | Hospitalists will influence hospital performance on Total Performance Score and could lead quality improvement efforts to improve score |
| Payment based on hospital Total Performance Score | |||
| Public reporting of quality and cost | Websites such as CMS HospitalCompare increasingly report on select quality and cost metrics | HospitalCompare reports process measures (eg, percent of heart failure patients given discharge instructions), outcome measures (eg, 30‐day risk‐adjusted mortality for AMI), survey of patients' hospital experience, and Medicare payment and volume for certain conditions | Many of these measures are directly related to care provided by hospitalists |
| Hospitalists could lead quality improvement initiatives focused on these measures | |||
| Medicare demonstrations | CMS has demonstration projects to test concepts, such as value‐based purchasing, incentive payments, and care management, aimed at improving the value of care delivered | Premier Hospital Quality Incentive Demonstration: Differentiates payment to hospitals based on performance on 30 metrics | Hospitals with their associated hospitalists can apply to participate in these and other demonstrations |
| Acute Care Episode (ACE) Demonstration: Provides bundled payments for select orthopedic and cardiovascular inpatient procedures | |||
| Medicare Hospital Gainsharing Demonstration: Hospitals can provide gainsharing payments to physicians based on savings from improving quality and efficiency | Successful demonstrations can be expanded or components incorporated into payment policy | ||
| Hospital‐acquired conditions | CMS rule that the presence of a select group of reasonably preventable conditions as the only complicating condition will not cause a higher‐paying diagnosis‐related group (DRG) to be assigned to the case | First 10 implemented: | Hospitalists can lead or participate in safety initiatives to decrease or eliminate these complications |
| Foreign object retained after surgery; | |||
| Air embolism; | |||
| Blood incompatibility; | |||
| Stage III and IV pressure ulcers; | |||
| Falls and trauma; | |||
| Manifestations of poor glycemic control; | |||
| Catheter‐associated urinary tract infections; | |||
| Vascular catheter‐associated infection; | |||
| Surgical site infection following specific surgeries; | |||
| Deep vein thrombosis and pulmonary embolus | |||
| Incentives for use of effective health information technology | Incentives for HIT use, often focused on certified interoperable systems and/or quality reporting, are provided by federal and private payers | The American Recovery and Reinvestment Act included over $17 billion of HIT incentives | Front line providers, including hospitalists, need to help guide implementation of HIT to be successful |
| Incentive money was directed at hospitals (hospital‐based physicians were excluded) and ambulatory physicians are eligible for direct incentives | Systems that include physician order entry, clinical decision support, and quality measurement capture and reporting can help hospitalists deliver higher quality care | ||
| Physician Quality Reporting Initiative (PQRI) | Quality measures linked to 2% incentive payment to physicians and other practitioners for reporting quality measures via claims or registry | Examples of measures hospitalists can report on include: | Hospitalists can drive performance on these measures, lead reporting efforts, and share in the financial rewards |
| Deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage; | |||
| Medication reconciliation at discharge; | |||
| Advance care plan documented; | |||
| Oral antiplatelet therapy for patients discharged with stroke diagnosis |
Value‐Based Purchasing
The Deficit Reduction Act Section 5001(b) authorized the Centers for Medicare and Medicaid Services (CMS) to develop a Medicare hospital VBP plan. The VBP plan is currently in the Presidents FY10 budget and the senate Committee's specification for health reform. VBP involves at least a portion of the payment being related to value instead of the traditional fee‐for‐service (FFS) model. CMS has consulted with external stakeholders on the measures, data infrastructure and validation, and incentive structure for the proposed program. Hospitals would submit data for all VBP measures that apply and performance scores would be given based on both attainment and improvement. The higher of the 2 scores (ie, attainment or improvement) would represent the hospital's performance in a given domain and the weighted domain scores would determine the hospital's total performance score. This total performance score would then be translated into an incentive payment for the hospital. Measure domains would include process measures (eg, beta‐blocker at discharge for acute myocardial infarction [AMI]), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Systems Hospital survey [HCAHPS]). Hospitalists are in a unique position to impact and improve performance in all of the above domains for hospitals. This has the potential to increase the value of high‐performing hospitalist groups to their respective hospitals. Most importantly, this program aligns incentives with rewarding the provision of high‐quality care as defined by these measures. Over time, CMS may consider expanding the measures to other domains such as efficiency, more patient‐centered outcomes, and care coordination. In terms of efficiency measurement, the Medicare Improvements for Patients and Providers Act (MIPPA) passed in 2008 called for CMS to provide confidential reports to physicians or groups of physicians on their relative resource use. This legislation also called for HHS to develop a plan for transitioning to VBP for Medicare professional services and a report to Congress on this plan.9 This lays the foundation for transforming Medicare to focus more on quality, resource use, and value and less on FFS.
Public Reporting of Quality and Cost
CMS is beginning to empower consumers with information on quality and Medicare payment costs so they can make educated decisions on where and how they seek care. The CMS website focused on hospitals is HospitalCompare (
Medicare Demonstrations
Several Medicare demonstration projects already implemented or in the planning stages are particularly relevant to hospitals and hospitalist practice. These demonstrations test concepts, such as VBP, incentive payments, and care management, aimed at improving the value of care delivered. If demonstrations are successful, they have potential for incorporation into federal policy. The Premier Hospital Quality Incentive Demonstration is an incentive program that differentiates payment to hospitals based on performance on 30 quality measures. Participation is voluntary. The top 20% of hospitals receive incentive payments.11 The success of this demonstration led to its current second phase. The Acute Care Episode (ACE) Demonstration will provide bundled payments (including Part A and B services) for ACEs within Medicare FFS. The demonstration includes gainsharing by allowing sites to reward individual clinicians, teams of clinicians, or other hospital staff who show measurable clinical quality improvement. The focus is on select orthopedic and cardiovascular inpatient procedures (eg, hip/knee replacement surgery and coronary artery bypass graft surgery).12 The demonstration also has potential to increase volume to participant physician‐hospital organizations through financial incentives to beneficiaries via payments to offset their Medicare cost‐sharing obligations. If this demonstration is successful and the concept of bundled payment is expanded to other conditions and additional geographies, this could have significant impact on hospitalists. Specifically, programs for care coordination and reducing readmissions and complications after discharge would be directly incentivized. The demonstration focuses on Texas, Oklahoma, Colorado, and New Mexico. The Medicare Hospital Gainsharing Demonstration program to test and evaluate arrangements between hospitals and physicians is designed improve the quality and efficiency of care provided to beneficiaries. The demonstration allows hospitals to provide gainsharing payments to physicians that represent solely a share of the savings incurred as a result of collaborative efforts to improve overall quality and efficiency. The demonstration was launched in 2007.13 Finally, the upcoming Medicare Medical Home Demonstration has the potential for direct or indirect hospitalist participation as facilitators in Tier 2 medical homes that take into account care coordination across inpatient and outpatient settings.14 These demonstrations represent attempts by the federal government to align incentives with high‐quality, high‐value delivery of care.
Hospital‐Acquired Conditions
Hospital‐acquired conditions (HACs) have significant cost and quality implications for U.S. healthcare, such as the estimated 99,000 deaths associated with hospital‐acquired infections annually.15 Therefore, CMS received statutory authority to not pay additional charges for reasonably preventable HACs. Beginning October 1, 2008, CMS implemented a rule that the presence of selected reasonably preventable conditions as the only complicating condition would not cause a higher‐paying DRG to be assigned to the case; therefore, the case would be paid as though the secondary diagnosis were not present. CMS also required the reporting of a new data element to delineate HACs from conditions present on admission. Hospitals can indicate to CMS if a condition was present on admission as a secondary diagnosis, allowing reimbursement for care provided to treat any condition present on admission. The first 10 HACs to be implemented were: foreign object retained after surgery, air embolism, blood incompatibility, stage III and IV pressure ulcers, falls and trauma, manifestations of poor glycemic control, catheter‐associated urinary tract infections, vascular catheterassociated infection, surgical site infection following specific surgeries, and deep vein thrombosis and pulmonary embolus.16 Since some complications are not absolutely preventable and evidence‐based guidelines for the prevention of some complications are lacking, this has generated some resistance from the provider community.17 The HAC payment policy is a step toward aligning incentives with quality performance, but any further HACs will need to be evaluated for their level of preventability and potential for unintended consequences.
Incentives for Use of Effective HIT
The use of HIT can be incentivized in 3 main ways, all of which are likely to increase over time. First, incentives can be implemented to reward reporting quality metrics via electronic health records or registries. Second, incentives based on quality performance may indirectly encourage the adoption of HIT because an electronic medical record, especially with computerized provider order entry and decision support, may enable higher performance on quality metrics. Finally, CMS has provided direct incentives for information technology adoption, such as certified electronic health records.18 The American Recovery and Reinvestment Act of 2009 created over $17 billion of potential incentive payments for HIT use by physicians and hospitals.19 Hospitals are eligible for significant incentives reaching estimates over $6 million per year, phasing out by 2015, so Congress excluded hospital‐based physicians from direct payments. Ambulatory physicians are eligible for up to $18,000 per year, phasing out by 2015, with subsequent payment reductions for nonuse. Since hospitalists often function at the nexus of clinical care, quality improvement, and technology use, they have the opportunity to lead or facilitate effective implementation of information technology in their hospitals. These efforts may be rewarded by hospitals.
PQRI
PQRI was authorized in 2006 and included a 1.5% incentive payment for satisfactorily reporting quality data. The incentive payment will increase to 2% in 2009. There are 153 PQRI measures in 2009 and a significant number of the measures focus on hospital‐based care. Examples of measures hospitalists can help report include: deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage, medication reconciliation at discharge, advance care plan documentation, oral antiplatelet therapy for patients discharged with stroke diagnosis, and anticoagulant therapy prescribed for atrial fibrillation in stroke patients at discharge. PQRI measures can be reported through claims‐based or registry‐based reporting. Reporting can be done on individual measures or for measure groups associated with specific conditions.20 Hospitalists have the potential to drive performance on these measures, lead reporting efforts, and share in the financial rewards.
Future Considerations
The political leadership at the federal and state level is beginning a new transition; however, the focus on quality and value for our health care dollar will likely continue to increase.5, 6 The U.S. health care system has untenable cost estimates, significant quality gaps, and a fractured payment system that fails to reward effective care coordination.2, 21, 22 This increased focus on quality and value should be viewed as an opportunity for hospitalists and hospitals. Hospitalist groups that can achieve high‐quality performance will be increasingly valued, and hospitals should further recognize the critical role hospitalists play in achieving high performance and the associated financial rewards. Hospitalists often lead quality improvement and safety programs in hospitals, and these programs are likely to be seen as progressively more important as payment is linked to performance. The Society of Hospital Medicine engages with policymakers and this role is increasingly significant as more policy and payment decisions impact hospitalists. The Society has focused on collaborative work with payers, policymakers, and other providers to find joint shared solutions. Hospitalists can serve as a link between providers and a focal point of care coordination, especially for the hospitalized patient. Finally, as our system and its incentives continue to progress toward alignment with value‐based high quality care, hospitalists should be leading the change and be an essential part of the solution to transform our health care system to provide high‐quality, efficient care to all Americans.
Acknowledgements
Dr. Tom Valuck is recognized for his thoughtful comments and edits in preparation, submission, and revision of this manuscript.
- Medicare Board of Trustees. A Summary of the 2008 Report. Available at: http://www.ssa.gov/OACT/TRSUM/trsummary.html. Accessed April 2009.
- , , , et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- Economy Likely to Move up Medicare's Insolvency. Available at: http://abcnews.go.com/Politics/Health/wireStory?id=6369658. Accessed April 2009.
- Value‐Driven Health Care. Available at: http://www.hhs.gov/valuedriven. Accessed April 2009.
- Obama‐Biden Full Health Care Plan. Available at: http://www.barackobama.com/issues/healthcare. Accessed April 2009.
- Senate Chairman Max Baucus Call to Action Health Reform 2009. Available at: http://finance.senate.gov/healthreform2009/finalwhitepaper.pdf. Accessed April 2009.
- , , , .National health spending in 2006: a year of change for prescription drugs.Health Aff (Millwood).2008;27(1):14–29.
- Medicare Hospital Value‐Based Purchasing Plan. October 31,2008. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/downloads/hospital_VBP_plan_issues_paper.pdf. Accessed April 2009.
- Medicare Improvements for Patients and Providers Act of 2008. Available at: http://www.asm.org/ASM/files/ccLibraryFiles/Filename/000000004120/HR6331.pdf. Accessed April 2009.
- HospitalCompare. Available at: www.hospitalcompare.hhs.gov. Accessed April 2009.
- Premier Hospital Quality Incentive Demonstration. Available at: http://www.cms.hhs.gov/HospitalQualityInits/35_hospitalpremier.asp. Accessed April 2009.
- Acute Care Episode Demonstration. Available at: http://www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none122(2):160–166.
- Hospital Acquired Conditions. Available at: http://www.cms.hhs.gov/HospitalAcqCond/06_Hospital‐Acquired_Conditions.asp. Accessed April 2009.
- , , .The wisdom and justice of not paying for “preventable complications”.JAMA.2008;299(18):2197–2199.
- E‐prescribing incentive program. Available at: http://www.cms.hhs.gov/ERXincentive. Accessed April 2009.
- American Recovery and Reinvestment Act. Available at: http://frwebgate.access.gpo.gov/cgi‐bin/getdoc.cgi?dbname=111_cong_bills299(19):2319–2321.
It is estimated that the Medicare Part A trust fund will be exhausted by 2016 to 2019; also, the quality of care delivered in the United States is highly variable.13 Value is typically defined as the quality achieved for a given cost (ie, value = quality/cost). The focus on the 3 related concepts of value, quality, and cost of health care is likely to continue to increase. Previously, the U.S. Department of Health and Human Services (HHS) made value‐driven health care one of the Department's top priorities.4 Policymakers are in a period of transition but the publicly available plans of the President and Senate leadership indicate that the focus on value‐based initiatives will likely continue to increase as our nation strives to achieve better outcomes for our health care dollar.5, 6 Specifically, the federal government and other payers increasingly align payment incentives with value and quality, encourage public reporting on quality and Medicare payment costs, such as on the Hospital Compare website (
Since hospital care represented $648 billion in 2006, which is 37% of the total patient‐related U.S. health care expenditure, the trend to pay for value will likely have significant impact on hospitals and hospitalists.7 The Society of Hospital Medicine has a public policy committee that provides feedback to government on programs and policies related to value‐driven health care. The policies and programs need consideration and input from the broader community of hospitalists. This work outlines some of the major national initiatives and policies focused on value‐driven health care and their implications for hospitalists. Hospitalists will need to understand the policy landscape and trends, lead improvement in their individual hospitals to receive value‐based incentives, and assess the opportunities and challenges of current and potential payer programs and policies.
Policies and Initiatives: Implications for Hospitals and Hospitalists
Within the portfolio of value‐driven health care, there are at least 6 major government programs, initiatives, and policies with implications for hospitals and hospitalists: value‐based purchasing (VBP), quality and cost public reporting, Medicare demonstrations, hospital‐acquired conditions, incentives for use of effective HIT, and the physician quality reporting initiative (PQRI) (Table 1).
| Initiative or Policy | Description | Specific Examples | Potential Implications |
|---|---|---|---|
| Value‐based purchasing | At least a portion of hospital payment related to value instead of the traditional fee‐for‐service model | Performance score is based on domains such as process measures (eg, beta‐blocker at discharge for acute myocardial), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Hospital Survey, aka HCAHPS) | Hospitalists will influence hospital performance on Total Performance Score and could lead quality improvement efforts to improve score |
| Payment based on hospital Total Performance Score | |||
| Public reporting of quality and cost | Websites such as CMS HospitalCompare increasingly report on select quality and cost metrics | HospitalCompare reports process measures (eg, percent of heart failure patients given discharge instructions), outcome measures (eg, 30‐day risk‐adjusted mortality for AMI), survey of patients' hospital experience, and Medicare payment and volume for certain conditions | Many of these measures are directly related to care provided by hospitalists |
| Hospitalists could lead quality improvement initiatives focused on these measures | |||
| Medicare demonstrations | CMS has demonstration projects to test concepts, such as value‐based purchasing, incentive payments, and care management, aimed at improving the value of care delivered | Premier Hospital Quality Incentive Demonstration: Differentiates payment to hospitals based on performance on 30 metrics | Hospitals with their associated hospitalists can apply to participate in these and other demonstrations |
| Acute Care Episode (ACE) Demonstration: Provides bundled payments for select orthopedic and cardiovascular inpatient procedures | |||
| Medicare Hospital Gainsharing Demonstration: Hospitals can provide gainsharing payments to physicians based on savings from improving quality and efficiency | Successful demonstrations can be expanded or components incorporated into payment policy | ||
| Hospital‐acquired conditions | CMS rule that the presence of a select group of reasonably preventable conditions as the only complicating condition will not cause a higher‐paying diagnosis‐related group (DRG) to be assigned to the case | First 10 implemented: | Hospitalists can lead or participate in safety initiatives to decrease or eliminate these complications |
| Foreign object retained after surgery; | |||
| Air embolism; | |||
| Blood incompatibility; | |||
| Stage III and IV pressure ulcers; | |||
| Falls and trauma; | |||
| Manifestations of poor glycemic control; | |||
| Catheter‐associated urinary tract infections; | |||
| Vascular catheter‐associated infection; | |||
| Surgical site infection following specific surgeries; | |||
| Deep vein thrombosis and pulmonary embolus | |||
| Incentives for use of effective health information technology | Incentives for HIT use, often focused on certified interoperable systems and/or quality reporting, are provided by federal and private payers | The American Recovery and Reinvestment Act included over $17 billion of HIT incentives | Front line providers, including hospitalists, need to help guide implementation of HIT to be successful |
| Incentive money was directed at hospitals (hospital‐based physicians were excluded) and ambulatory physicians are eligible for direct incentives | Systems that include physician order entry, clinical decision support, and quality measurement capture and reporting can help hospitalists deliver higher quality care | ||
| Physician Quality Reporting Initiative (PQRI) | Quality measures linked to 2% incentive payment to physicians and other practitioners for reporting quality measures via claims or registry | Examples of measures hospitalists can report on include: | Hospitalists can drive performance on these measures, lead reporting efforts, and share in the financial rewards |
| Deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage; | |||
| Medication reconciliation at discharge; | |||
| Advance care plan documented; | |||
| Oral antiplatelet therapy for patients discharged with stroke diagnosis |
Value‐Based Purchasing
The Deficit Reduction Act Section 5001(b) authorized the Centers for Medicare and Medicaid Services (CMS) to develop a Medicare hospital VBP plan. The VBP plan is currently in the Presidents FY10 budget and the senate Committee's specification for health reform. VBP involves at least a portion of the payment being related to value instead of the traditional fee‐for‐service (FFS) model. CMS has consulted with external stakeholders on the measures, data infrastructure and validation, and incentive structure for the proposed program. Hospitals would submit data for all VBP measures that apply and performance scores would be given based on both attainment and improvement. The higher of the 2 scores (ie, attainment or improvement) would represent the hospital's performance in a given domain and the weighted domain scores would determine the hospital's total performance score. This total performance score would then be translated into an incentive payment for the hospital. Measure domains would include process measures (eg, beta‐blocker at discharge for acute myocardial infarction [AMI]), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Systems Hospital survey [HCAHPS]). Hospitalists are in a unique position to impact and improve performance in all of the above domains for hospitals. This has the potential to increase the value of high‐performing hospitalist groups to their respective hospitals. Most importantly, this program aligns incentives with rewarding the provision of high‐quality care as defined by these measures. Over time, CMS may consider expanding the measures to other domains such as efficiency, more patient‐centered outcomes, and care coordination. In terms of efficiency measurement, the Medicare Improvements for Patients and Providers Act (MIPPA) passed in 2008 called for CMS to provide confidential reports to physicians or groups of physicians on their relative resource use. This legislation also called for HHS to develop a plan for transitioning to VBP for Medicare professional services and a report to Congress on this plan.9 This lays the foundation for transforming Medicare to focus more on quality, resource use, and value and less on FFS.
Public Reporting of Quality and Cost
CMS is beginning to empower consumers with information on quality and Medicare payment costs so they can make educated decisions on where and how they seek care. The CMS website focused on hospitals is HospitalCompare (
Medicare Demonstrations
Several Medicare demonstration projects already implemented or in the planning stages are particularly relevant to hospitals and hospitalist practice. These demonstrations test concepts, such as VBP, incentive payments, and care management, aimed at improving the value of care delivered. If demonstrations are successful, they have potential for incorporation into federal policy. The Premier Hospital Quality Incentive Demonstration is an incentive program that differentiates payment to hospitals based on performance on 30 quality measures. Participation is voluntary. The top 20% of hospitals receive incentive payments.11 The success of this demonstration led to its current second phase. The Acute Care Episode (ACE) Demonstration will provide bundled payments (including Part A and B services) for ACEs within Medicare FFS. The demonstration includes gainsharing by allowing sites to reward individual clinicians, teams of clinicians, or other hospital staff who show measurable clinical quality improvement. The focus is on select orthopedic and cardiovascular inpatient procedures (eg, hip/knee replacement surgery and coronary artery bypass graft surgery).12 The demonstration also has potential to increase volume to participant physician‐hospital organizations through financial incentives to beneficiaries via payments to offset their Medicare cost‐sharing obligations. If this demonstration is successful and the concept of bundled payment is expanded to other conditions and additional geographies, this could have significant impact on hospitalists. Specifically, programs for care coordination and reducing readmissions and complications after discharge would be directly incentivized. The demonstration focuses on Texas, Oklahoma, Colorado, and New Mexico. The Medicare Hospital Gainsharing Demonstration program to test and evaluate arrangements between hospitals and physicians is designed improve the quality and efficiency of care provided to beneficiaries. The demonstration allows hospitals to provide gainsharing payments to physicians that represent solely a share of the savings incurred as a result of collaborative efforts to improve overall quality and efficiency. The demonstration was launched in 2007.13 Finally, the upcoming Medicare Medical Home Demonstration has the potential for direct or indirect hospitalist participation as facilitators in Tier 2 medical homes that take into account care coordination across inpatient and outpatient settings.14 These demonstrations represent attempts by the federal government to align incentives with high‐quality, high‐value delivery of care.
Hospital‐Acquired Conditions
Hospital‐acquired conditions (HACs) have significant cost and quality implications for U.S. healthcare, such as the estimated 99,000 deaths associated with hospital‐acquired infections annually.15 Therefore, CMS received statutory authority to not pay additional charges for reasonably preventable HACs. Beginning October 1, 2008, CMS implemented a rule that the presence of selected reasonably preventable conditions as the only complicating condition would not cause a higher‐paying DRG to be assigned to the case; therefore, the case would be paid as though the secondary diagnosis were not present. CMS also required the reporting of a new data element to delineate HACs from conditions present on admission. Hospitals can indicate to CMS if a condition was present on admission as a secondary diagnosis, allowing reimbursement for care provided to treat any condition present on admission. The first 10 HACs to be implemented were: foreign object retained after surgery, air embolism, blood incompatibility, stage III and IV pressure ulcers, falls and trauma, manifestations of poor glycemic control, catheter‐associated urinary tract infections, vascular catheterassociated infection, surgical site infection following specific surgeries, and deep vein thrombosis and pulmonary embolus.16 Since some complications are not absolutely preventable and evidence‐based guidelines for the prevention of some complications are lacking, this has generated some resistance from the provider community.17 The HAC payment policy is a step toward aligning incentives with quality performance, but any further HACs will need to be evaluated for their level of preventability and potential for unintended consequences.
Incentives for Use of Effective HIT
The use of HIT can be incentivized in 3 main ways, all of which are likely to increase over time. First, incentives can be implemented to reward reporting quality metrics via electronic health records or registries. Second, incentives based on quality performance may indirectly encourage the adoption of HIT because an electronic medical record, especially with computerized provider order entry and decision support, may enable higher performance on quality metrics. Finally, CMS has provided direct incentives for information technology adoption, such as certified electronic health records.18 The American Recovery and Reinvestment Act of 2009 created over $17 billion of potential incentive payments for HIT use by physicians and hospitals.19 Hospitals are eligible for significant incentives reaching estimates over $6 million per year, phasing out by 2015, so Congress excluded hospital‐based physicians from direct payments. Ambulatory physicians are eligible for up to $18,000 per year, phasing out by 2015, with subsequent payment reductions for nonuse. Since hospitalists often function at the nexus of clinical care, quality improvement, and technology use, they have the opportunity to lead or facilitate effective implementation of information technology in their hospitals. These efforts may be rewarded by hospitals.
PQRI
PQRI was authorized in 2006 and included a 1.5% incentive payment for satisfactorily reporting quality data. The incentive payment will increase to 2% in 2009. There are 153 PQRI measures in 2009 and a significant number of the measures focus on hospital‐based care. Examples of measures hospitalists can help report include: deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage, medication reconciliation at discharge, advance care plan documentation, oral antiplatelet therapy for patients discharged with stroke diagnosis, and anticoagulant therapy prescribed for atrial fibrillation in stroke patients at discharge. PQRI measures can be reported through claims‐based or registry‐based reporting. Reporting can be done on individual measures or for measure groups associated with specific conditions.20 Hospitalists have the potential to drive performance on these measures, lead reporting efforts, and share in the financial rewards.
Future Considerations
The political leadership at the federal and state level is beginning a new transition; however, the focus on quality and value for our health care dollar will likely continue to increase.5, 6 The U.S. health care system has untenable cost estimates, significant quality gaps, and a fractured payment system that fails to reward effective care coordination.2, 21, 22 This increased focus on quality and value should be viewed as an opportunity for hospitalists and hospitals. Hospitalist groups that can achieve high‐quality performance will be increasingly valued, and hospitals should further recognize the critical role hospitalists play in achieving high performance and the associated financial rewards. Hospitalists often lead quality improvement and safety programs in hospitals, and these programs are likely to be seen as progressively more important as payment is linked to performance. The Society of Hospital Medicine engages with policymakers and this role is increasingly significant as more policy and payment decisions impact hospitalists. The Society has focused on collaborative work with payers, policymakers, and other providers to find joint shared solutions. Hospitalists can serve as a link between providers and a focal point of care coordination, especially for the hospitalized patient. Finally, as our system and its incentives continue to progress toward alignment with value‐based high quality care, hospitalists should be leading the change and be an essential part of the solution to transform our health care system to provide high‐quality, efficient care to all Americans.
Acknowledgements
Dr. Tom Valuck is recognized for his thoughtful comments and edits in preparation, submission, and revision of this manuscript.
It is estimated that the Medicare Part A trust fund will be exhausted by 2016 to 2019; also, the quality of care delivered in the United States is highly variable.13 Value is typically defined as the quality achieved for a given cost (ie, value = quality/cost). The focus on the 3 related concepts of value, quality, and cost of health care is likely to continue to increase. Previously, the U.S. Department of Health and Human Services (HHS) made value‐driven health care one of the Department's top priorities.4 Policymakers are in a period of transition but the publicly available plans of the President and Senate leadership indicate that the focus on value‐based initiatives will likely continue to increase as our nation strives to achieve better outcomes for our health care dollar.5, 6 Specifically, the federal government and other payers increasingly align payment incentives with value and quality, encourage public reporting on quality and Medicare payment costs, such as on the Hospital Compare website (
Since hospital care represented $648 billion in 2006, which is 37% of the total patient‐related U.S. health care expenditure, the trend to pay for value will likely have significant impact on hospitals and hospitalists.7 The Society of Hospital Medicine has a public policy committee that provides feedback to government on programs and policies related to value‐driven health care. The policies and programs need consideration and input from the broader community of hospitalists. This work outlines some of the major national initiatives and policies focused on value‐driven health care and their implications for hospitalists. Hospitalists will need to understand the policy landscape and trends, lead improvement in their individual hospitals to receive value‐based incentives, and assess the opportunities and challenges of current and potential payer programs and policies.
Policies and Initiatives: Implications for Hospitals and Hospitalists
Within the portfolio of value‐driven health care, there are at least 6 major government programs, initiatives, and policies with implications for hospitals and hospitalists: value‐based purchasing (VBP), quality and cost public reporting, Medicare demonstrations, hospital‐acquired conditions, incentives for use of effective HIT, and the physician quality reporting initiative (PQRI) (Table 1).
| Initiative or Policy | Description | Specific Examples | Potential Implications |
|---|---|---|---|
| Value‐based purchasing | At least a portion of hospital payment related to value instead of the traditional fee‐for‐service model | Performance score is based on domains such as process measures (eg, beta‐blocker at discharge for acute myocardial), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Hospital Survey, aka HCAHPS) | Hospitalists will influence hospital performance on Total Performance Score and could lead quality improvement efforts to improve score |
| Payment based on hospital Total Performance Score | |||
| Public reporting of quality and cost | Websites such as CMS HospitalCompare increasingly report on select quality and cost metrics | HospitalCompare reports process measures (eg, percent of heart failure patients given discharge instructions), outcome measures (eg, 30‐day risk‐adjusted mortality for AMI), survey of patients' hospital experience, and Medicare payment and volume for certain conditions | Many of these measures are directly related to care provided by hospitalists |
| Hospitalists could lead quality improvement initiatives focused on these measures | |||
| Medicare demonstrations | CMS has demonstration projects to test concepts, such as value‐based purchasing, incentive payments, and care management, aimed at improving the value of care delivered | Premier Hospital Quality Incentive Demonstration: Differentiates payment to hospitals based on performance on 30 metrics | Hospitals with their associated hospitalists can apply to participate in these and other demonstrations |
| Acute Care Episode (ACE) Demonstration: Provides bundled payments for select orthopedic and cardiovascular inpatient procedures | |||
| Medicare Hospital Gainsharing Demonstration: Hospitals can provide gainsharing payments to physicians based on savings from improving quality and efficiency | Successful demonstrations can be expanded or components incorporated into payment policy | ||
| Hospital‐acquired conditions | CMS rule that the presence of a select group of reasonably preventable conditions as the only complicating condition will not cause a higher‐paying diagnosis‐related group (DRG) to be assigned to the case | First 10 implemented: | Hospitalists can lead or participate in safety initiatives to decrease or eliminate these complications |
| Foreign object retained after surgery; | |||
| Air embolism; | |||
| Blood incompatibility; | |||
| Stage III and IV pressure ulcers; | |||
| Falls and trauma; | |||
| Manifestations of poor glycemic control; | |||
| Catheter‐associated urinary tract infections; | |||
| Vascular catheter‐associated infection; | |||
| Surgical site infection following specific surgeries; | |||
| Deep vein thrombosis and pulmonary embolus | |||
| Incentives for use of effective health information technology | Incentives for HIT use, often focused on certified interoperable systems and/or quality reporting, are provided by federal and private payers | The American Recovery and Reinvestment Act included over $17 billion of HIT incentives | Front line providers, including hospitalists, need to help guide implementation of HIT to be successful |
| Incentive money was directed at hospitals (hospital‐based physicians were excluded) and ambulatory physicians are eligible for direct incentives | Systems that include physician order entry, clinical decision support, and quality measurement capture and reporting can help hospitalists deliver higher quality care | ||
| Physician Quality Reporting Initiative (PQRI) | Quality measures linked to 2% incentive payment to physicians and other practitioners for reporting quality measures via claims or registry | Examples of measures hospitalists can report on include: | Hospitalists can drive performance on these measures, lead reporting efforts, and share in the financial rewards |
| Deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage; | |||
| Medication reconciliation at discharge; | |||
| Advance care plan documented; | |||
| Oral antiplatelet therapy for patients discharged with stroke diagnosis |
Value‐Based Purchasing
The Deficit Reduction Act Section 5001(b) authorized the Centers for Medicare and Medicaid Services (CMS) to develop a Medicare hospital VBP plan. The VBP plan is currently in the Presidents FY10 budget and the senate Committee's specification for health reform. VBP involves at least a portion of the payment being related to value instead of the traditional fee‐for‐service (FFS) model. CMS has consulted with external stakeholders on the measures, data infrastructure and validation, and incentive structure for the proposed program. Hospitals would submit data for all VBP measures that apply and performance scores would be given based on both attainment and improvement. The higher of the 2 scores (ie, attainment or improvement) would represent the hospital's performance in a given domain and the weighted domain scores would determine the hospital's total performance score. This total performance score would then be translated into an incentive payment for the hospital. Measure domains would include process measures (eg, beta‐blocker at discharge for acute myocardial infarction [AMI]), outcome measures (eg, 30‐day AMI mortality), and satisfaction measures (eg, Consumer Assessment of Healthcare Providers and Systems Hospital survey [HCAHPS]). Hospitalists are in a unique position to impact and improve performance in all of the above domains for hospitals. This has the potential to increase the value of high‐performing hospitalist groups to their respective hospitals. Most importantly, this program aligns incentives with rewarding the provision of high‐quality care as defined by these measures. Over time, CMS may consider expanding the measures to other domains such as efficiency, more patient‐centered outcomes, and care coordination. In terms of efficiency measurement, the Medicare Improvements for Patients and Providers Act (MIPPA) passed in 2008 called for CMS to provide confidential reports to physicians or groups of physicians on their relative resource use. This legislation also called for HHS to develop a plan for transitioning to VBP for Medicare professional services and a report to Congress on this plan.9 This lays the foundation for transforming Medicare to focus more on quality, resource use, and value and less on FFS.
Public Reporting of Quality and Cost
CMS is beginning to empower consumers with information on quality and Medicare payment costs so they can make educated decisions on where and how they seek care. The CMS website focused on hospitals is HospitalCompare (
Medicare Demonstrations
Several Medicare demonstration projects already implemented or in the planning stages are particularly relevant to hospitals and hospitalist practice. These demonstrations test concepts, such as VBP, incentive payments, and care management, aimed at improving the value of care delivered. If demonstrations are successful, they have potential for incorporation into federal policy. The Premier Hospital Quality Incentive Demonstration is an incentive program that differentiates payment to hospitals based on performance on 30 quality measures. Participation is voluntary. The top 20% of hospitals receive incentive payments.11 The success of this demonstration led to its current second phase. The Acute Care Episode (ACE) Demonstration will provide bundled payments (including Part A and B services) for ACEs within Medicare FFS. The demonstration includes gainsharing by allowing sites to reward individual clinicians, teams of clinicians, or other hospital staff who show measurable clinical quality improvement. The focus is on select orthopedic and cardiovascular inpatient procedures (eg, hip/knee replacement surgery and coronary artery bypass graft surgery).12 The demonstration also has potential to increase volume to participant physician‐hospital organizations through financial incentives to beneficiaries via payments to offset their Medicare cost‐sharing obligations. If this demonstration is successful and the concept of bundled payment is expanded to other conditions and additional geographies, this could have significant impact on hospitalists. Specifically, programs for care coordination and reducing readmissions and complications after discharge would be directly incentivized. The demonstration focuses on Texas, Oklahoma, Colorado, and New Mexico. The Medicare Hospital Gainsharing Demonstration program to test and evaluate arrangements between hospitals and physicians is designed improve the quality and efficiency of care provided to beneficiaries. The demonstration allows hospitals to provide gainsharing payments to physicians that represent solely a share of the savings incurred as a result of collaborative efforts to improve overall quality and efficiency. The demonstration was launched in 2007.13 Finally, the upcoming Medicare Medical Home Demonstration has the potential for direct or indirect hospitalist participation as facilitators in Tier 2 medical homes that take into account care coordination across inpatient and outpatient settings.14 These demonstrations represent attempts by the federal government to align incentives with high‐quality, high‐value delivery of care.
Hospital‐Acquired Conditions
Hospital‐acquired conditions (HACs) have significant cost and quality implications for U.S. healthcare, such as the estimated 99,000 deaths associated with hospital‐acquired infections annually.15 Therefore, CMS received statutory authority to not pay additional charges for reasonably preventable HACs. Beginning October 1, 2008, CMS implemented a rule that the presence of selected reasonably preventable conditions as the only complicating condition would not cause a higher‐paying DRG to be assigned to the case; therefore, the case would be paid as though the secondary diagnosis were not present. CMS also required the reporting of a new data element to delineate HACs from conditions present on admission. Hospitals can indicate to CMS if a condition was present on admission as a secondary diagnosis, allowing reimbursement for care provided to treat any condition present on admission. The first 10 HACs to be implemented were: foreign object retained after surgery, air embolism, blood incompatibility, stage III and IV pressure ulcers, falls and trauma, manifestations of poor glycemic control, catheter‐associated urinary tract infections, vascular catheterassociated infection, surgical site infection following specific surgeries, and deep vein thrombosis and pulmonary embolus.16 Since some complications are not absolutely preventable and evidence‐based guidelines for the prevention of some complications are lacking, this has generated some resistance from the provider community.17 The HAC payment policy is a step toward aligning incentives with quality performance, but any further HACs will need to be evaluated for their level of preventability and potential for unintended consequences.
Incentives for Use of Effective HIT
The use of HIT can be incentivized in 3 main ways, all of which are likely to increase over time. First, incentives can be implemented to reward reporting quality metrics via electronic health records or registries. Second, incentives based on quality performance may indirectly encourage the adoption of HIT because an electronic medical record, especially with computerized provider order entry and decision support, may enable higher performance on quality metrics. Finally, CMS has provided direct incentives for information technology adoption, such as certified electronic health records.18 The American Recovery and Reinvestment Act of 2009 created over $17 billion of potential incentive payments for HIT use by physicians and hospitals.19 Hospitals are eligible for significant incentives reaching estimates over $6 million per year, phasing out by 2015, so Congress excluded hospital‐based physicians from direct payments. Ambulatory physicians are eligible for up to $18,000 per year, phasing out by 2015, with subsequent payment reductions for nonuse. Since hospitalists often function at the nexus of clinical care, quality improvement, and technology use, they have the opportunity to lead or facilitate effective implementation of information technology in their hospitals. These efforts may be rewarded by hospitals.
PQRI
PQRI was authorized in 2006 and included a 1.5% incentive payment for satisfactorily reporting quality data. The incentive payment will increase to 2% in 2009. There are 153 PQRI measures in 2009 and a significant number of the measures focus on hospital‐based care. Examples of measures hospitalists can help report include: deep vein thrombosis prophylaxis for ischemic stroke or intracranial hemorrhage, medication reconciliation at discharge, advance care plan documentation, oral antiplatelet therapy for patients discharged with stroke diagnosis, and anticoagulant therapy prescribed for atrial fibrillation in stroke patients at discharge. PQRI measures can be reported through claims‐based or registry‐based reporting. Reporting can be done on individual measures or for measure groups associated with specific conditions.20 Hospitalists have the potential to drive performance on these measures, lead reporting efforts, and share in the financial rewards.
Future Considerations
The political leadership at the federal and state level is beginning a new transition; however, the focus on quality and value for our health care dollar will likely continue to increase.5, 6 The U.S. health care system has untenable cost estimates, significant quality gaps, and a fractured payment system that fails to reward effective care coordination.2, 21, 22 This increased focus on quality and value should be viewed as an opportunity for hospitalists and hospitals. Hospitalist groups that can achieve high‐quality performance will be increasingly valued, and hospitals should further recognize the critical role hospitalists play in achieving high performance and the associated financial rewards. Hospitalists often lead quality improvement and safety programs in hospitals, and these programs are likely to be seen as progressively more important as payment is linked to performance. The Society of Hospital Medicine engages with policymakers and this role is increasingly significant as more policy and payment decisions impact hospitalists. The Society has focused on collaborative work with payers, policymakers, and other providers to find joint shared solutions. Hospitalists can serve as a link between providers and a focal point of care coordination, especially for the hospitalized patient. Finally, as our system and its incentives continue to progress toward alignment with value‐based high quality care, hospitalists should be leading the change and be an essential part of the solution to transform our health care system to provide high‐quality, efficient care to all Americans.
Acknowledgements
Dr. Tom Valuck is recognized for his thoughtful comments and edits in preparation, submission, and revision of this manuscript.
- Medicare Board of Trustees. A Summary of the 2008 Report. Available at: http://www.ssa.gov/OACT/TRSUM/trsummary.html. Accessed April 2009.
- , , , et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- Economy Likely to Move up Medicare's Insolvency. Available at: http://abcnews.go.com/Politics/Health/wireStory?id=6369658. Accessed April 2009.
- Value‐Driven Health Care. Available at: http://www.hhs.gov/valuedriven. Accessed April 2009.
- Obama‐Biden Full Health Care Plan. Available at: http://www.barackobama.com/issues/healthcare. Accessed April 2009.
- Senate Chairman Max Baucus Call to Action Health Reform 2009. Available at: http://finance.senate.gov/healthreform2009/finalwhitepaper.pdf. Accessed April 2009.
- , , , .National health spending in 2006: a year of change for prescription drugs.Health Aff (Millwood).2008;27(1):14–29.
- Medicare Hospital Value‐Based Purchasing Plan. October 31,2008. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/downloads/hospital_VBP_plan_issues_paper.pdf. Accessed April 2009.
- Medicare Improvements for Patients and Providers Act of 2008. Available at: http://www.asm.org/ASM/files/ccLibraryFiles/Filename/000000004120/HR6331.pdf. Accessed April 2009.
- HospitalCompare. Available at: www.hospitalcompare.hhs.gov. Accessed April 2009.
- Premier Hospital Quality Incentive Demonstration. Available at: http://www.cms.hhs.gov/HospitalQualityInits/35_hospitalpremier.asp. Accessed April 2009.
- Acute Care Episode Demonstration. Available at: http://www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none122(2):160–166.
- Hospital Acquired Conditions. Available at: http://www.cms.hhs.gov/HospitalAcqCond/06_Hospital‐Acquired_Conditions.asp. Accessed April 2009.
- , , .The wisdom and justice of not paying for “preventable complications”.JAMA.2008;299(18):2197–2199.
- E‐prescribing incentive program. Available at: http://www.cms.hhs.gov/ERXincentive. Accessed April 2009.
- American Recovery and Reinvestment Act. Available at: http://frwebgate.access.gpo.gov/cgi‐bin/getdoc.cgi?dbname=111_cong_bills299(19):2319–2321.
- Medicare Board of Trustees. A Summary of the 2008 Report. Available at: http://www.ssa.gov/OACT/TRSUM/trsummary.html. Accessed April 2009.
- , , , et al.The quality of health care delivered to adults in the United States.N Engl J Med.2003;348(26):2635–2645.
- Economy Likely to Move up Medicare's Insolvency. Available at: http://abcnews.go.com/Politics/Health/wireStory?id=6369658. Accessed April 2009.
- Value‐Driven Health Care. Available at: http://www.hhs.gov/valuedriven. Accessed April 2009.
- Obama‐Biden Full Health Care Plan. Available at: http://www.barackobama.com/issues/healthcare. Accessed April 2009.
- Senate Chairman Max Baucus Call to Action Health Reform 2009. Available at: http://finance.senate.gov/healthreform2009/finalwhitepaper.pdf. Accessed April 2009.
- , , , .National health spending in 2006: a year of change for prescription drugs.Health Aff (Millwood).2008;27(1):14–29.
- Medicare Hospital Value‐Based Purchasing Plan. October 31,2008. Available at: http://www.cms.hhs.gov/AcuteInpatientPPS/downloads/hospital_VBP_plan_issues_paper.pdf. Accessed April 2009.
- Medicare Improvements for Patients and Providers Act of 2008. Available at: http://www.asm.org/ASM/files/ccLibraryFiles/Filename/000000004120/HR6331.pdf. Accessed April 2009.
- HospitalCompare. Available at: www.hospitalcompare.hhs.gov. Accessed April 2009.
- Premier Hospital Quality Incentive Demonstration. Available at: http://www.cms.hhs.gov/HospitalQualityInits/35_hospitalpremier.asp. Accessed April 2009.
- Acute Care Episode Demonstration. Available at: http://www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none122(2):160–166.
- Hospital Acquired Conditions. Available at: http://www.cms.hhs.gov/HospitalAcqCond/06_Hospital‐Acquired_Conditions.asp. Accessed April 2009.
- , , .The wisdom and justice of not paying for “preventable complications”.JAMA.2008;299(18):2197–2199.
- E‐prescribing incentive program. Available at: http://www.cms.hhs.gov/ERXincentive. Accessed April 2009.
- American Recovery and Reinvestment Act. Available at: http://frwebgate.access.gpo.gov/cgi‐bin/getdoc.cgi?dbname=111_cong_bills299(19):2319–2321.
Trivialization of Diagnosis
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
Historically, diagnosis has been central to patient care. Making the correct diagnosis serves as a guide to the choice of treatment, permits assessment of prognosis, and indicates what complications to expect. Arriving at the correct diagnosis has been a major goalthe Holy Grail, as it were. Accurate diagnosis continues to be a major focus of medical practice, and accurate diagnoses are routinely made every day. Still, many experienced clinicians have the impression that in recent years the primacy of diagnosis has been coming under attack from several sources.
A decade ago, Thomas Szasz pointed out that disease is a fact of nature, while diagnosis is man made.1 The noun diagnosis is derived from the Greek verb diagignoskeinindicating knowledge attained through analysis. As defined in Merriam‐Webster's Collegiate Dictionary, the diagnosis essentially means the conclusion arrived at by the art of identifying a disease. It is the product of an intellectual effort of a particular analytic type. The response to the question What is the diagnosis? has been the name of the specific disease entity with which the patient is afflicted.
Disease entities represent coherent, organizing concepts.2 A specific disease is a condition with characteristic manifestationsclinical, histologic, or pathophysiologic. If untreated, it results in dysfunction or, in some cases, death. Differentiation of one disease from another is enhanced when there is some sort of understanding, even if incomplete, of the specific pathophysiology at play. Admittedly, concepts of what constitute specific disease entities are not fixed; they evolve with time. Not all diseases have been identified. The underlying etiology may or may not be known. Nonetheless, diseases are recognized as specific entities, distinct from other diseases. Thus, anemia is not regarded as a disease, while pernicious anemia and iron deficiency anemia are diseases. Fever is not a disease, while typhoid fever is. Arthritis is not a disease, while gonococcal arthritis is.
Billable Terms Are Replacing Traditional Medical Diagnoses
The term diagnosis has been redefined to comply with the need to enter a diagnosis for billing purposes. Use of this term for this purpose has confused the issue. Diagnoses entered for such purposes are largely derived from International Classification of Diseases (ICD) lists.3 However, the ICD was not intended to definitively identify underlying diseases, nor to serve as a guide to management and prognostication. The 6th revision of the ICD in 1948, the first revision to be widely employed, was designed for epidemiologic purposes and achieved widespread use to obtain mortality and morbidity statistics.4 It was subsequently also used as a tool to index hospital medical records.
Significantly, it was also employed for billing purposes, with far‐reaching pernicious consequences. Although the ICD purports to be a list of diseases, it actually includes symptoms and signs. Consequently, in the billing context, diagnosis no longer necessarily refers to specific disease states; it now refers to billable termsoften the manifestation that was responsible for the patient seeking medical assistance. Far from being the product of an intellectual effort, it is often merely a justification for submitting a bill. Examples of such diagnoses are shown in Table 1. Many of them represent symptoms, signs, or laboratory abnormalities. The importance of accurate medical diagnosis has been cheapened by this change. The effect is to devalue diagnosisto lessen its status as the Holy Grail.
| Abdominal pain | General symptoms | Special symptom |
| Abnormal blood test | Immune disorders | Splenomegaly |
| Back disorder | Joint disorder | Throat pain |
| Coagulation defects | Myoneural disorder | Urinary symptoms |
| Diseases of esophagus | Otalgia | Visual disturbance |
| Eye disorders | Pain in joint | Vomiting |
| Fluid/electrolyte disorders | Right lower quadrant mass | Wheezing |
The effect of this on trainees is invidious, and predictable. The traditional meaning of diagnosis is being replaced in our minds. Physicians in training are tempted to deceive themselves into believing that they have arrived at an understanding of what they are dealing with when they enter such a diagnosis. After all, have they not responded to the question: what is the diagnosis?
We do not mean to imply that physicians are doing anything wrong by entering ICD terms for billing purposes. What must be done for billing purposes must be done. It is important to be aware, however, and to continually remind ourselves, that what has been entered for this purpose is often not a true medical diagnosis.
Further, when the diagnosis is not yet known, it is not possible to enter a true diagnosis. There is no way to say I don't know. It would be preferable to simply admit that the diagnosis is not yet established, as a medical resident has recently emphasized.5
Diagnosis Often Gets Short Shrift Because of the Perceived Urgency of Discharge
The emphasis on diagnosis several generations ago may have resulted, at least in part, from the relative paucity of effective therapeutic interventions before the 1930s. Things have changed; therapeutic capabilities are much more powerful now. Making the correct diagnosis seems to have lost its urgency. Instead of the major question being what is the diagnosis? it now is often what do we do now? The diagnosis is often an afterthought. Indeed, it is sometimes not even mentioned in discharge summaries, where, not uncommonly, one sees nondiagnoses such as blood in stool or polyarthritis.
In addition, we are under pressure to shorten the inpatient stay of hospitalized patients. At least a portion of the public is aware of this; thus, it has been noted in the New York Times that: The pressure to get patients out of the hospital rapidly can focus medical attention on treatment rather than diagnosis.6 We commonly seek to ameliorate the patients' status to permit discharge before (or often without) learning what we are dealing with. Sometimes one senses that the primary question has become how soon can we discharge this patient?
A price is paid for this. In the absence of a valid diagnosis, patients may be subjected to a broad array of nonessential investigations and therapeutic interventions, each with its own possible complications. Patients are often discharged without a diagnosis having been made, presenting a serious challenge to outpatient physicians who are left to manage them without a clear idea of what they are dealing with. It often falls to the outpatient physicians to make the diagnosis. This is somewhat problematic, since they themselves are under harsh time pressure. Patients often require rehospitalization for the same as‐yet‐undiagnosed condition.
The Problem‐Oriented Record Poses Problems
The widespread use of the problem‐oriented record, originated by Lawrence Weed,7 has led to problems of its own.8 It has evolved, away from its original intent. In practice, its major emphasis often seems to be on identification of problems and tracking their progress, rather than on synthesis. This often leads to muddy rather than clear diagnostic thinking. Assessments and progress notes frequently consist of lists of symptoms, organs, abnormal laboratory findings, or even medical specialties. The net effect is often fragmented thinkingas Weed7 put it, failure to integrate findings into a single entity. Synthesizing diverse findings into a single entity, when possible, is necessary to define a diagnosis. Failure to do so may have serious consequences. In a recent study of diagnostic errors in internal medicine, cognitive errors were frequently found to contribute to such errors.9 The most common cognitive problem was faulty synthesis. How much worse than faulty synthesis is failure to synthesize at all!
Presumptive Diagnoses, Even if Incorrect, Metamorphose into Established Diagnoses
We must often treat empirically. When there is no firm diagnosis, presumptive diagnoses must be made and acted upon. Unfortunately, there are not always mechanisms for the physician to make it clear that his or her diagnosis is only presumptive. (A common example is acute viral syndrome, generally an educated guess.) All too often, presumptive diagnoses are entered, without qualification, as definitive diagnoses, and then achieve immortality. Thus, if a patient is incorrectly diagnosed as having rheumatoid arthritis, all subsequent presentations will start: A so‐and‐so year‐old woman with rheumatoid arthritis for many years Presumptive diagnoses are frequently not questioned. It is easier to assume that they were arrived at after due consideration. Once entered in the medical record, they may be difficult to remove.
It is true that the need to arrive at a precise diagnosis is less pressing for some medical specialties than for others. Emergency physicians, critical care physicians, and frequently, surgeons, must commonly act on the basis of presumptive diagnoses. In contrast, internists, family physicians, psychiatrists, and indeed all physicians who care for patients with chronic illnesses can, with time, be expected to sort out accurate from inaccurate presumptive diagnoses.
A specific example of the problem of presumptive diagnosis is of interest. It is not uncommon, following a first encounter, for a diagnosis to be entered based on the patient's history alone. While such diagnoses are frequently correct, they are not invariably correct. The patient may have arrived at the conclusion herself; she may have misunderstood what she was told by her physician, or her physician may have been in error. Such inaccurate diagnoses also often achieve immortality in the medical record.
Apparent Disparaging of the Importance of Diagnosis
Further trivialization has come from a number of publications expressing concerns about the importance of diagnosis. Thus we read that there are negative consequences of emphasis on diagnosis. When we know what is wrong, we focus less on the individual and more on the disease.10 In his recent book Our Present Complaint. American Medicine, Then and Now, the scholar C.E. Rosenberg11 includes a chapter with the provocative title The Tyranny of Diagnosis. He points out that even a century ago the fear was expressed that burgeoning scientific medicine would lead to denigration of physicians' holistic and intuitive skills.11 Other authors maintain that firm diagnoses may be misleading, since many diseases are a matter of degree in a continuuma spectrumthat are best defined employing a statistical model of risk prediction.12 The suggestion is made that the usefulness of diagnostic tests should not be related to the presence or absence of a disease, but rather to whether they influence outcome.13
Scientific medicine is focused on diagnosis. Denigration of diagnosis has often come, as a philosophical posture, from opponents of reductionist thinking. As Rosenberg11 points out: It has become fashionable among humanistic and social science‐oriented commentators to dwell on the distinction between illness and disease, between the patient's felt experience and the constructions placed on that experience by the world of medicine. Their opposition, he feels, reflects the value‐laden mutual incompatibility (real or apparent) of art and science, of holism and reductionism.2
It is true that medicine is more than just biology. There is a great deal to be said for the view that scientific medicine tends to deemphasize the humanistic, holistic aspects of medical practice. However, despite all these concerns, most physiciansand, to be fair, most criticsagree that making an accurate diagnosis is important. Thus, though the title of his relevant chapter is The Tyranny of Diagnosis, Rosenberg11 states: I might just as well have used the term indispensability. Indeed, the opening words of that chapter are: Diagnosis has always played a pivotal role in medicine.11 Other authors cited above issue this disclaimer: We are not against diagnosis. Diagnosis does and always will play a central role in clinical medicine.12
The importance of diagnosis is underscored by the vigorous debate about how to assess diagnostic tests;14 apparently, diagnosis does indeed matter. While it is true that diagnoses are not always precise, objective, and quantifiable,10 abundant evidence points to the unavoidable conclusion that identifying the patient's disease is heuristically useful; that is, it works.2 The track record of modern scientific medicine in improving mortality and morbidity speaks for itself. It hardly seems necessary to defend it. In addition to representing a valuable intellectual challenge in its own right, diagnosis is pivotal to the scientific mission of medicine.
What Can Be Done?
The net effect of all these forces: the use of billable terms as diagnoses, the pressures of managed care, fragmented problem lists, persistence of incorrect presumptive diagnoses in medical records, and antireductionist criticisms is to encourage sloppy diagnostic thinking in some physicians. What can be done to emphasize the proper use of differential diagnosis in arriving at a definitive diagnosis? What can be done to underscore the importance of differentiating between presumptive and definitive diagnoses? Most importantly, how can we instill the respect for the intellectual honesty necessary to acquire and retain these skills?
Above all, we should relentlessly impress on our students and trainees the importance of arriving at an accurate definitive diagnosis. They should be aware that the job is only half done if the diagnosis has not been made. We should do this repeatedly, both by word and by example. We ourselves must display intellectual honesty.
In addition, we ought to be able to enter diagnosis uncertain, so coded, or to append the phrase cause unknown after the manifestation of concern, when we don't really know what is going on. We should routinely indicate when a diagnosis is merely presumptive. Perhaps we need a way to indicate: This diagnosis is definitive or to indicate the specific evidence that led to the diagnosis (eg, biopsy, laboratory result, radiographic finding). Finally, we need to correct the current confusion between diseases and billable terms, to differentiate the disease from the symptom, perhaps by labeling ICD‐9‐CM codes simply as billing codes, with a separate entry for actual medical diagnoses.
Although powerful historical forces have brought us to this state, we believe that arriving at the correct diagnosis is at least as important now as it has been in the past, and that its primacy should be recognized, celebrated, and fought for. We owe our patients no less.
Acknowledgements
The authors thank Drs. James Pile, Neal Dawson, and David Samols for their helpful suggestions.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.
- .What counts as disease? Rationales and rationalizations for treatment.Forsch Komplementarmed.1998;5(suppl S1):40–46.
- .What is disease? In memory of Owsei Temkin.Bull Hist Med.2003;77:491–505.
- World Health Organization (WHO). International Classification of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en. Accessed June2009.
- World Health Organization (WHO). History of the development of the ICD. Available at: http://www.who.int/classifications/icd/en/HistoryOfICD. pdf. Accessed June2009.
- .Living unlabeled—diagnosis and disorder.N Engl J Med.2008;359:1650–1653.
- . Poison Pill. New York Times Magazine. 2008: 24–26. Available at: http://www.nytimes.com/2008/04/13/magazine/13wwln‐diagnosis‐t.html. Accessed June2009.
- .Medical records that guide and teach.N Engl J Med.1968;278:593–600.
- .Clear writing, clear thinking and the disappearing art of the problem list.J Hosp Med.2007;2:199–202.
- , , .Diagnostic error in internal medicine.Arch Intern Med.2005;165:1493–1499.
- . The Tyranny of Diagnosis. New York Times. Available at: http://www.nytimes.com/2008/09/19/health/chen9‐18.html?partner=rssnyt2007.
- , , .Against diagnosis.Ann Intern Med.2008;149:200–203.
- , , .A philosophical perspective supports the need for patient‐outcome studies in diagnostic test evaluation.J Clin Epidemiol.2009;62:58–61.
- , .Evidence based diagnostics.BMJ.2005;330:724–726.
Academic Hospital Medicine
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
Penetrating Point
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
Reflections on Hospitalist Movement
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.