User login
Experts dispel incorrect dogmas in aesthetic medicine
At least once a week,
Those images may help Dr. Stankiewicz understand patient preferences in terms of lip size and proportion, but she points out that shape is unique to each person. “I tell them: ‘All we can do is enhance that lip shape with filler. We can’t give you somebody else’s lip shape with an injection of filler.’ ”
During a virtual course on laser and aesthetic skin therapy, she and Omar A. Ibrahimi, MD, PhD, dispelled this and other false dogmas that they hear from some clinicians who practice aesthetic medicine and the patients who see them.
Wait 1 year before treating traumatic and surgical scars with vascular and fractional CO2 lasers. “I don’t think this is controversial anymore, because there is a boatload of data, which has shown that early treatment can prevent hypertrophic scarring and promote scar maturation,” said Dr. Stankiewicz, who practices dermatology in Park City, Utah. “Histology has also shown more organized dermal collagen from early treatment. Of course, there will be situations where you may want to hold off, like doing an ablative fractional [laser treatment] over the scar of a joint replacement ... where you may risk infection.” In her clinic, she routinely treats scars on the same day as suture removal, “as long as the healing looks appropriate.”
Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, Stamford, also jumps on treating scars early. For a patient with postacne erythema, for example, he will use a pulsed-dye laser, which he believes will prevent scars from becoming atrophic.
Used equipment is a better investment than new equipment. While purchasing used laser and light devices can save money, especially when starting out, be wary of potential pitfalls, including the fact that many devices have disposable tips. “If your laser isn’t certified or you’re not the authorized owner of the device, you won’t be able to buy the disposables,” Dr. Stankiewicz noted. “So, before you buy a used device, ensure that you can buy them.”
Also, consider the cost of service if the device breaks down, she advised. Some lasers are complicated to service and others have codes set by the manufacturer so that only contracted engineers can work on them. “Otherwise, third-party engineers and service providers have to figure out how to crack the code to get into the machine,” she said. “If you’re in the situation where you have to ask the manufacturer to service your device, you have to pay a lot of money to recertify your device. Then you’ve lost all the savings you thought you made by buying a used machine.” She prefers to negotiate a good deal on a new device. “Often, a very good deal on a new device can rival the offer of a used one.”
Dr. Ibrahimi recalled buying a used fractional laser that came with a 30-day guarantee, but it stopped working around day 45. “I didn’t have much recourse there,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “You can’t go back to the company [for repair] unless you pay a recertification fee.”
Avoid exercise after Botox treatment. Although inverted yoga poses and lying down should be avoided for several hours after receiving Botox, there are no other limits to other forms of exercise post treatment, Dr. Stankiewicz said. If she suspects that a patient will develop bruising on one or more injection sites, she treats the areas with a laser. “Doing this on the same day as Botox treatment doesn’t always stop or treat bruising, many times it does.”
Another myth she hears is that it is not safe to fly in an airplane after Botox treatment. “That recommendation comes from the fact that the atmospheric pressure is lower in an airplane, so we worry about the risk of Botox spread,” Dr. Stankiewicz said. “But I practice at 7,000 feet above sea level, which is the same atmospheric pressure as that in an airplane,” she added, noting Botox is administered throughout the day in her practice and she does not see increased complications or worry about spread.
Clinician self-treatment is okay. In the opinion of Dr. Stankiewicz, aesthetic clinicians who treat themselves “have a fool for a patient.” She added: “Although no one is going to blame you and may not even know if you give yourself a little Botox touch-up at home, glorifying self-treatment on social media must stop. It’s dangerous and it can be ineffective.”
Self-treatment can also impair judgment and the objectivity of cosmetic therapies. “Also, when you’re pointing a laser at your own face and posting it on social media, it gives viewers the impression that this is not a serious medical treatment when it really is,” she emphasized. In addition, “when you treat yourself, you lose the ability to see the proper clinical endpoint. You also lose the ability to see the angle and the appropriate position for injection to avoid intervascular occlusion.”
Neither Dr. Stankiewicz nor Dr. Ibrahimi reported having relevant financial disclosures.
At least once a week,
Those images may help Dr. Stankiewicz understand patient preferences in terms of lip size and proportion, but she points out that shape is unique to each person. “I tell them: ‘All we can do is enhance that lip shape with filler. We can’t give you somebody else’s lip shape with an injection of filler.’ ”
During a virtual course on laser and aesthetic skin therapy, she and Omar A. Ibrahimi, MD, PhD, dispelled this and other false dogmas that they hear from some clinicians who practice aesthetic medicine and the patients who see them.
Wait 1 year before treating traumatic and surgical scars with vascular and fractional CO2 lasers. “I don’t think this is controversial anymore, because there is a boatload of data, which has shown that early treatment can prevent hypertrophic scarring and promote scar maturation,” said Dr. Stankiewicz, who practices dermatology in Park City, Utah. “Histology has also shown more organized dermal collagen from early treatment. Of course, there will be situations where you may want to hold off, like doing an ablative fractional [laser treatment] over the scar of a joint replacement ... where you may risk infection.” In her clinic, she routinely treats scars on the same day as suture removal, “as long as the healing looks appropriate.”
Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, Stamford, also jumps on treating scars early. For a patient with postacne erythema, for example, he will use a pulsed-dye laser, which he believes will prevent scars from becoming atrophic.
Used equipment is a better investment than new equipment. While purchasing used laser and light devices can save money, especially when starting out, be wary of potential pitfalls, including the fact that many devices have disposable tips. “If your laser isn’t certified or you’re not the authorized owner of the device, you won’t be able to buy the disposables,” Dr. Stankiewicz noted. “So, before you buy a used device, ensure that you can buy them.”
Also, consider the cost of service if the device breaks down, she advised. Some lasers are complicated to service and others have codes set by the manufacturer so that only contracted engineers can work on them. “Otherwise, third-party engineers and service providers have to figure out how to crack the code to get into the machine,” she said. “If you’re in the situation where you have to ask the manufacturer to service your device, you have to pay a lot of money to recertify your device. Then you’ve lost all the savings you thought you made by buying a used machine.” She prefers to negotiate a good deal on a new device. “Often, a very good deal on a new device can rival the offer of a used one.”
Dr. Ibrahimi recalled buying a used fractional laser that came with a 30-day guarantee, but it stopped working around day 45. “I didn’t have much recourse there,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “You can’t go back to the company [for repair] unless you pay a recertification fee.”
Avoid exercise after Botox treatment. Although inverted yoga poses and lying down should be avoided for several hours after receiving Botox, there are no other limits to other forms of exercise post treatment, Dr. Stankiewicz said. If she suspects that a patient will develop bruising on one or more injection sites, she treats the areas with a laser. “Doing this on the same day as Botox treatment doesn’t always stop or treat bruising, many times it does.”
Another myth she hears is that it is not safe to fly in an airplane after Botox treatment. “That recommendation comes from the fact that the atmospheric pressure is lower in an airplane, so we worry about the risk of Botox spread,” Dr. Stankiewicz said. “But I practice at 7,000 feet above sea level, which is the same atmospheric pressure as that in an airplane,” she added, noting Botox is administered throughout the day in her practice and she does not see increased complications or worry about spread.
Clinician self-treatment is okay. In the opinion of Dr. Stankiewicz, aesthetic clinicians who treat themselves “have a fool for a patient.” She added: “Although no one is going to blame you and may not even know if you give yourself a little Botox touch-up at home, glorifying self-treatment on social media must stop. It’s dangerous and it can be ineffective.”
Self-treatment can also impair judgment and the objectivity of cosmetic therapies. “Also, when you’re pointing a laser at your own face and posting it on social media, it gives viewers the impression that this is not a serious medical treatment when it really is,” she emphasized. In addition, “when you treat yourself, you lose the ability to see the proper clinical endpoint. You also lose the ability to see the angle and the appropriate position for injection to avoid intervascular occlusion.”
Neither Dr. Stankiewicz nor Dr. Ibrahimi reported having relevant financial disclosures.
At least once a week,
Those images may help Dr. Stankiewicz understand patient preferences in terms of lip size and proportion, but she points out that shape is unique to each person. “I tell them: ‘All we can do is enhance that lip shape with filler. We can’t give you somebody else’s lip shape with an injection of filler.’ ”
During a virtual course on laser and aesthetic skin therapy, she and Omar A. Ibrahimi, MD, PhD, dispelled this and other false dogmas that they hear from some clinicians who practice aesthetic medicine and the patients who see them.
Wait 1 year before treating traumatic and surgical scars with vascular and fractional CO2 lasers. “I don’t think this is controversial anymore, because there is a boatload of data, which has shown that early treatment can prevent hypertrophic scarring and promote scar maturation,” said Dr. Stankiewicz, who practices dermatology in Park City, Utah. “Histology has also shown more organized dermal collagen from early treatment. Of course, there will be situations where you may want to hold off, like doing an ablative fractional [laser treatment] over the scar of a joint replacement ... where you may risk infection.” In her clinic, she routinely treats scars on the same day as suture removal, “as long as the healing looks appropriate.”
Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, Stamford, also jumps on treating scars early. For a patient with postacne erythema, for example, he will use a pulsed-dye laser, which he believes will prevent scars from becoming atrophic.
Used equipment is a better investment than new equipment. While purchasing used laser and light devices can save money, especially when starting out, be wary of potential pitfalls, including the fact that many devices have disposable tips. “If your laser isn’t certified or you’re not the authorized owner of the device, you won’t be able to buy the disposables,” Dr. Stankiewicz noted. “So, before you buy a used device, ensure that you can buy them.”
Also, consider the cost of service if the device breaks down, she advised. Some lasers are complicated to service and others have codes set by the manufacturer so that only contracted engineers can work on them. “Otherwise, third-party engineers and service providers have to figure out how to crack the code to get into the machine,” she said. “If you’re in the situation where you have to ask the manufacturer to service your device, you have to pay a lot of money to recertify your device. Then you’ve lost all the savings you thought you made by buying a used machine.” She prefers to negotiate a good deal on a new device. “Often, a very good deal on a new device can rival the offer of a used one.”
Dr. Ibrahimi recalled buying a used fractional laser that came with a 30-day guarantee, but it stopped working around day 45. “I didn’t have much recourse there,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “You can’t go back to the company [for repair] unless you pay a recertification fee.”
Avoid exercise after Botox treatment. Although inverted yoga poses and lying down should be avoided for several hours after receiving Botox, there are no other limits to other forms of exercise post treatment, Dr. Stankiewicz said. If she suspects that a patient will develop bruising on one or more injection sites, she treats the areas with a laser. “Doing this on the same day as Botox treatment doesn’t always stop or treat bruising, many times it does.”
Another myth she hears is that it is not safe to fly in an airplane after Botox treatment. “That recommendation comes from the fact that the atmospheric pressure is lower in an airplane, so we worry about the risk of Botox spread,” Dr. Stankiewicz said. “But I practice at 7,000 feet above sea level, which is the same atmospheric pressure as that in an airplane,” she added, noting Botox is administered throughout the day in her practice and she does not see increased complications or worry about spread.
Clinician self-treatment is okay. In the opinion of Dr. Stankiewicz, aesthetic clinicians who treat themselves “have a fool for a patient.” She added: “Although no one is going to blame you and may not even know if you give yourself a little Botox touch-up at home, glorifying self-treatment on social media must stop. It’s dangerous and it can be ineffective.”
Self-treatment can also impair judgment and the objectivity of cosmetic therapies. “Also, when you’re pointing a laser at your own face and posting it on social media, it gives viewers the impression that this is not a serious medical treatment when it really is,” she emphasized. In addition, “when you treat yourself, you lose the ability to see the proper clinical endpoint. You also lose the ability to see the angle and the appropriate position for injection to avoid intervascular occlusion.”
Neither Dr. Stankiewicz nor Dr. Ibrahimi reported having relevant financial disclosures.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Novel platform harnesses 3D laser technology for skin treatments
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
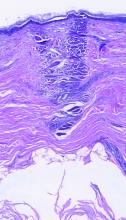
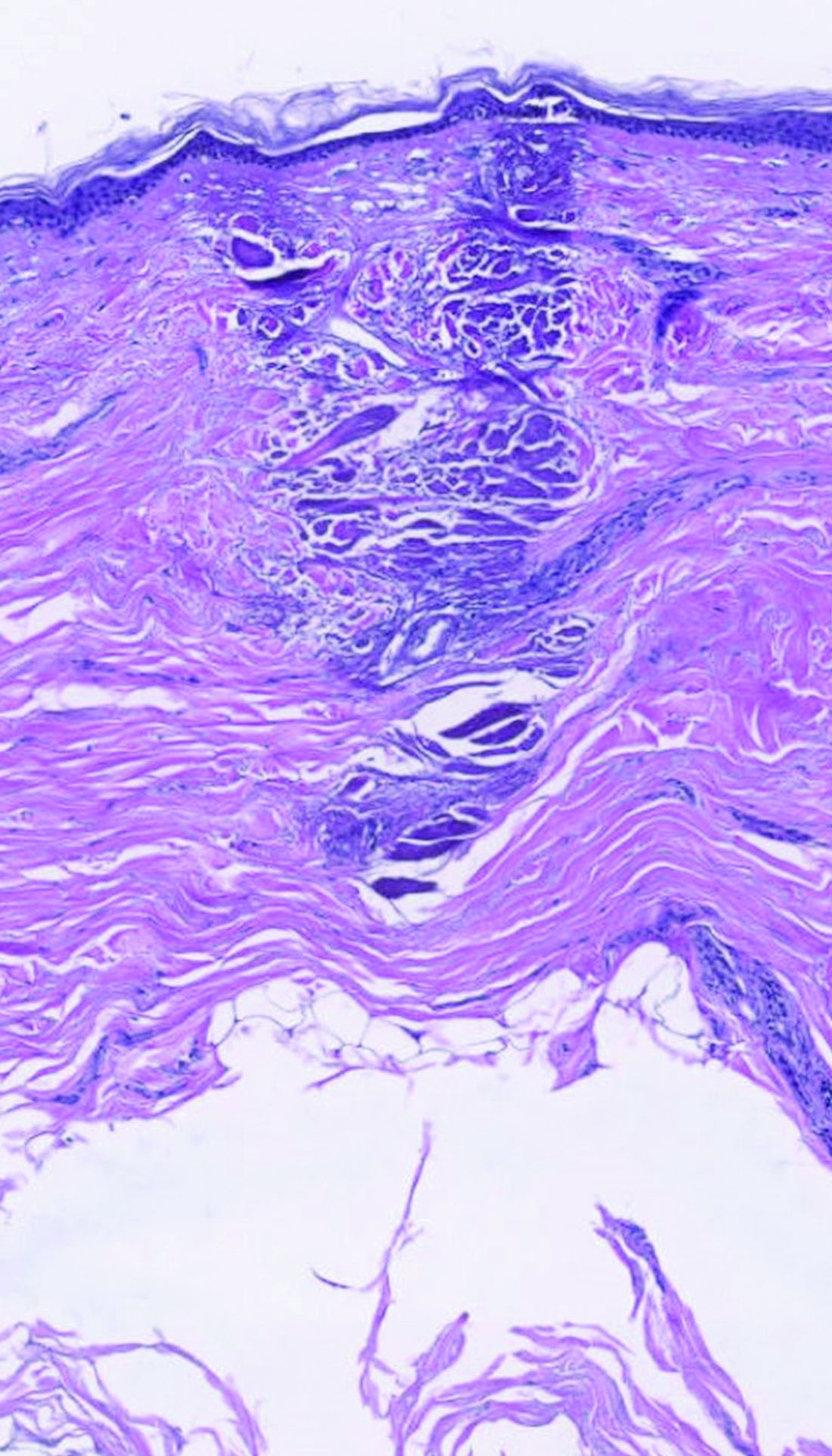
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Applications for laser-assisted drug delivery on the horizon, expert says
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Applications for nano-pulse stimulation continue to evolve
During a virtual course on laser and aesthetic skin therapy, Yakir Levin, MD, PhD, likened nano-pulse stimulation to microneedling or radiofrequency microneedling “in that you have an array of microneedles that go into the skin,” he said. “However, it is actually completely different.”
The CellFX System uses nano-pulse stimulation to deliver ultrashort electrical energy pulses into the skin of target lesions via a console-based handheld applicator. In September 2022, the Food and Drug Administration cleared the CellFX system for treatment of sebaceous hyperplasia in patients with Fitzpatrick skin types I-II. This followed a general clearance of the device in 2021 for dermatologic procedures requiring ablation and resurfacing of the skin.
Pulses from the device deliver a “constant electrical potential gradient across cell membranes and organelle membranes, causing them to break down,” explained Dr. Levin, a dermatologist and physician scientist at Massachusetts General Hospital, Boston, where he practices cosmetic dermatology and conducts research on birthmarks in children. This creates pores in those membranes “and leads to a controlled form of cell death,” he said. “As a result, this treatment is limited to cells, so you can do it in the dermis without damaging the collagen network. It spares tissue that’s outside of the field, and it’s nonthermal.”
Images from electron microscopy have demonstrated swelling of the mitochondria and breakdown of nuclei within 2 hours of treatment in a rat study. “Within 1 day of treatment you have death of the cells and the beginning of involution of the lesion,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “This presents us with the opportunity to treat dermal lesions without causing damage to the epidermis or to the acellular portion of the dermis.”
In published studies, nano-pulse stimulation has been shown to be effective for treating sebaceous hyperplasia and warts. According to Dr. Levin, clinicians typically treat sebaceous hyperplasia with an radiofrequency microneedle or electrodesiccation, “where we shave off the top but do not try to hit the bottom because we don’t want to cause scarring of the dermis,” he said. “Using the nano-pulse stimulation technology, however, you end up with involution of the sebaceous lesion without damaging the surrounding dermis.”
In a prospective, randomized study, 72 individuals with sebaceous gland hyperplasia received nano-pulse stimulation to 222 lesions and they returned for three to four follow-up evaluations with photographs. At the final study visit, investigators rated 99.6% of the sebaceous gland lesions as clear or mostly clear, while 79% of the study participants said they were “satisfied” or “mostly satisfied” with the outcome.
At posttreatment day 60, 55% of the lesions were judged to have no hyperpigmentation and 31% exhibited mild posttreatment hyperpigmentation.
In a more recent study, researchers used the CellFX System to treat 195 cutaneous warts up to 10 mm wide in 62 individuals enrolled at one of five sites. They found that 75% of common warts, 73% of flat warts, and 44% of plantar warts were completely clear 60 days following the last nano-pulse stimulation treatment and did not recur within the 120-day observation period.
The most common reactions at the treatment sites were erythema (51%) and eschar formation (23%) on day 30.
According to Dr. Levin, promising future applications of nano-pulse stimulation include treatment of syringomas, dermatofibromas, and basal cell carcinomas.
Dr. Levin reported financial interest in Accure Acne, Avava Medical, and Soltego. The CellFX system was developed and is marketed by Pulse Biosciences.
During a virtual course on laser and aesthetic skin therapy, Yakir Levin, MD, PhD, likened nano-pulse stimulation to microneedling or radiofrequency microneedling “in that you have an array of microneedles that go into the skin,” he said. “However, it is actually completely different.”
The CellFX System uses nano-pulse stimulation to deliver ultrashort electrical energy pulses into the skin of target lesions via a console-based handheld applicator. In September 2022, the Food and Drug Administration cleared the CellFX system for treatment of sebaceous hyperplasia in patients with Fitzpatrick skin types I-II. This followed a general clearance of the device in 2021 for dermatologic procedures requiring ablation and resurfacing of the skin.
Pulses from the device deliver a “constant electrical potential gradient across cell membranes and organelle membranes, causing them to break down,” explained Dr. Levin, a dermatologist and physician scientist at Massachusetts General Hospital, Boston, where he practices cosmetic dermatology and conducts research on birthmarks in children. This creates pores in those membranes “and leads to a controlled form of cell death,” he said. “As a result, this treatment is limited to cells, so you can do it in the dermis without damaging the collagen network. It spares tissue that’s outside of the field, and it’s nonthermal.”
Images from electron microscopy have demonstrated swelling of the mitochondria and breakdown of nuclei within 2 hours of treatment in a rat study. “Within 1 day of treatment you have death of the cells and the beginning of involution of the lesion,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “This presents us with the opportunity to treat dermal lesions without causing damage to the epidermis or to the acellular portion of the dermis.”
In published studies, nano-pulse stimulation has been shown to be effective for treating sebaceous hyperplasia and warts. According to Dr. Levin, clinicians typically treat sebaceous hyperplasia with an radiofrequency microneedle or electrodesiccation, “where we shave off the top but do not try to hit the bottom because we don’t want to cause scarring of the dermis,” he said. “Using the nano-pulse stimulation technology, however, you end up with involution of the sebaceous lesion without damaging the surrounding dermis.”
In a prospective, randomized study, 72 individuals with sebaceous gland hyperplasia received nano-pulse stimulation to 222 lesions and they returned for three to four follow-up evaluations with photographs. At the final study visit, investigators rated 99.6% of the sebaceous gland lesions as clear or mostly clear, while 79% of the study participants said they were “satisfied” or “mostly satisfied” with the outcome.
At posttreatment day 60, 55% of the lesions were judged to have no hyperpigmentation and 31% exhibited mild posttreatment hyperpigmentation.
In a more recent study, researchers used the CellFX System to treat 195 cutaneous warts up to 10 mm wide in 62 individuals enrolled at one of five sites. They found that 75% of common warts, 73% of flat warts, and 44% of plantar warts were completely clear 60 days following the last nano-pulse stimulation treatment and did not recur within the 120-day observation period.
The most common reactions at the treatment sites were erythema (51%) and eschar formation (23%) on day 30.
According to Dr. Levin, promising future applications of nano-pulse stimulation include treatment of syringomas, dermatofibromas, and basal cell carcinomas.
Dr. Levin reported financial interest in Accure Acne, Avava Medical, and Soltego. The CellFX system was developed and is marketed by Pulse Biosciences.
During a virtual course on laser and aesthetic skin therapy, Yakir Levin, MD, PhD, likened nano-pulse stimulation to microneedling or radiofrequency microneedling “in that you have an array of microneedles that go into the skin,” he said. “However, it is actually completely different.”
The CellFX System uses nano-pulse stimulation to deliver ultrashort electrical energy pulses into the skin of target lesions via a console-based handheld applicator. In September 2022, the Food and Drug Administration cleared the CellFX system for treatment of sebaceous hyperplasia in patients with Fitzpatrick skin types I-II. This followed a general clearance of the device in 2021 for dermatologic procedures requiring ablation and resurfacing of the skin.
Pulses from the device deliver a “constant electrical potential gradient across cell membranes and organelle membranes, causing them to break down,” explained Dr. Levin, a dermatologist and physician scientist at Massachusetts General Hospital, Boston, where he practices cosmetic dermatology and conducts research on birthmarks in children. This creates pores in those membranes “and leads to a controlled form of cell death,” he said. “As a result, this treatment is limited to cells, so you can do it in the dermis without damaging the collagen network. It spares tissue that’s outside of the field, and it’s nonthermal.”
Images from electron microscopy have demonstrated swelling of the mitochondria and breakdown of nuclei within 2 hours of treatment in a rat study. “Within 1 day of treatment you have death of the cells and the beginning of involution of the lesion,” he said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “This presents us with the opportunity to treat dermal lesions without causing damage to the epidermis or to the acellular portion of the dermis.”
In published studies, nano-pulse stimulation has been shown to be effective for treating sebaceous hyperplasia and warts. According to Dr. Levin, clinicians typically treat sebaceous hyperplasia with an radiofrequency microneedle or electrodesiccation, “where we shave off the top but do not try to hit the bottom because we don’t want to cause scarring of the dermis,” he said. “Using the nano-pulse stimulation technology, however, you end up with involution of the sebaceous lesion without damaging the surrounding dermis.”
In a prospective, randomized study, 72 individuals with sebaceous gland hyperplasia received nano-pulse stimulation to 222 lesions and they returned for three to four follow-up evaluations with photographs. At the final study visit, investigators rated 99.6% of the sebaceous gland lesions as clear or mostly clear, while 79% of the study participants said they were “satisfied” or “mostly satisfied” with the outcome.
At posttreatment day 60, 55% of the lesions were judged to have no hyperpigmentation and 31% exhibited mild posttreatment hyperpigmentation.
In a more recent study, researchers used the CellFX System to treat 195 cutaneous warts up to 10 mm wide in 62 individuals enrolled at one of five sites. They found that 75% of common warts, 73% of flat warts, and 44% of plantar warts were completely clear 60 days following the last nano-pulse stimulation treatment and did not recur within the 120-day observation period.
The most common reactions at the treatment sites were erythema (51%) and eschar formation (23%) on day 30.
According to Dr. Levin, promising future applications of nano-pulse stimulation include treatment of syringomas, dermatofibromas, and basal cell carcinomas.
Dr. Levin reported financial interest in Accure Acne, Avava Medical, and Soltego. The CellFX system was developed and is marketed by Pulse Biosciences.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Laser and light devices for acne treatment continue to advance
The calendar year
This was preceded by the FDA clearance of AviClear, marketed by Cutera, in March, and the commercial launch of TheraClearX, marketed by StrataSkin, in July.
“It’s an exciting time to be working with acne,” Fernanda H. Sakamoto, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. “We’ll see a lot of people using new devices. I’m looking forward to seeing results in the long term.”
AviClear and the Accure Laser System, marketed by Accure, are both powered by a 1,726-nm laser, but they work differently. AviClear, which was cleared for the treatment of mild, moderate, and severe acne, has a maximum fluence of 30 J/cm2 in single-pulse mode and a maximum fluence of 20 J/cm2 in double-pulse mode. The treatment handpiece has an integrated scanner for delivering treatment spot(s) in an operator-selected pattern. “It’s a little bit lower powered than the Accure and has a maximum pulse energy of 5 joules and a pulse duration of up to 50 milliseconds,” Dr. Sakamoto said. In the treatment of acne, laser and light treatments target the sebaceous gland.
In pivotal data submitted to the FDA, 104 patients with acne who were enrolled at 7 U.S. sites received 304 treatments with AviClear spaced 2-5 weeks apart. Each treatment took about 30 minutes. Treatment success was defined as having at least 50% fewer inflammatory acne lesions 12 weeks after the final treatment visit, compared with baseline. At the week 4 follow-up visit, there were median and mean reductions of 42% and 37%, respectively, in the inflammatory lesion counts from baseline (P < .001). The researchers found that, at the week 4 follow-up visit, 36% of patients had achieved treatment success, which increased to 78% at the 12-week follow-up visit. Treatment was considered safe and tolerable, according to the manufacturer.
The other newcomer device with a 1,726-nm wavelength is the Accure Laser System, which features a smart laser handpiece for real-time thermal monitoring and precise delivery of laser emissions. The device received CE Mark approval in 2020 for the treatment of moderate acne, and on Nov. 22, 2022, the manufacturer announced that it had been cleared by the FDA for the treatment of mild to severe inflammatory acne vulgaris.
Dr. Sakamoto and her Wellman colleagues have been working with five dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, and Mitchel Goldman, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2022, more than 50 patients with mild to severe acne were enrolled in four studies and an additional 30 were enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment after four monthly treatment sessions. The average lesion reduction at week 12 was 82% and the mean visual analog scale score immediately after treatment was 2.09 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device overall with no adverse events reported. At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histologic studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other skin structures.
Dr. Sakamoto emphasized that to date no direct clinical comparisons have been made between the AviClear and Accure devices. “Are all 1,726-nm lasers made equal? That is a question that we have to keep in our mind,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “They are using the same wavelength, but they are different types of lasers.”
For example, the Accure Laser treats to temperature, relies on air cooling, and is targeted to dermatologists and plastic surgeons, while the AviClear treats to fluence, relies on contact cooling, and includes med spas and other nonphysician providers as the target users. “Mathematically, the difference between the two devices is that the Accure can achieve deeper penetration in a single pulse, while the AviClear is a little more superficial,” she said. “Whether that is translated clinically is unknown at this point.”
Dr. Sakamoto also discussed the TheraClearX, which is FDA cleared for the treatment of mild, moderate, and severe acne, including comedonal, pustular, and inflammatory acne vulgaris. The device, which is a new version of the Palomar Acleara, uses a vacuum technique with up to 3 psi pressure in conjunction with broadband light with a wavelength spectrum of 500 nm–1,200 nm delivered through a liquid-cooled, handheld delivery system. The predicate device was the Aesthera Isolaz System. The vacuum extracts buildup of sebaceous material. “At the same time, it takes the blood out of the competing chromophore,” she said. “By doing so, it potentially damages the sebaceous glands and reduces the inflammatory lesions.”
Dr. Sakamoto disclosed that she is the founder of and science advisor for Lightwater Bioscience. She is also a science advisor for Accure Acne and has received portions of patent royalties from Massachusetts General Hospital.
The calendar year
This was preceded by the FDA clearance of AviClear, marketed by Cutera, in March, and the commercial launch of TheraClearX, marketed by StrataSkin, in July.
“It’s an exciting time to be working with acne,” Fernanda H. Sakamoto, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. “We’ll see a lot of people using new devices. I’m looking forward to seeing results in the long term.”
AviClear and the Accure Laser System, marketed by Accure, are both powered by a 1,726-nm laser, but they work differently. AviClear, which was cleared for the treatment of mild, moderate, and severe acne, has a maximum fluence of 30 J/cm2 in single-pulse mode and a maximum fluence of 20 J/cm2 in double-pulse mode. The treatment handpiece has an integrated scanner for delivering treatment spot(s) in an operator-selected pattern. “It’s a little bit lower powered than the Accure and has a maximum pulse energy of 5 joules and a pulse duration of up to 50 milliseconds,” Dr. Sakamoto said. In the treatment of acne, laser and light treatments target the sebaceous gland.
In pivotal data submitted to the FDA, 104 patients with acne who were enrolled at 7 U.S. sites received 304 treatments with AviClear spaced 2-5 weeks apart. Each treatment took about 30 minutes. Treatment success was defined as having at least 50% fewer inflammatory acne lesions 12 weeks after the final treatment visit, compared with baseline. At the week 4 follow-up visit, there were median and mean reductions of 42% and 37%, respectively, in the inflammatory lesion counts from baseline (P < .001). The researchers found that, at the week 4 follow-up visit, 36% of patients had achieved treatment success, which increased to 78% at the 12-week follow-up visit. Treatment was considered safe and tolerable, according to the manufacturer.
The other newcomer device with a 1,726-nm wavelength is the Accure Laser System, which features a smart laser handpiece for real-time thermal monitoring and precise delivery of laser emissions. The device received CE Mark approval in 2020 for the treatment of moderate acne, and on Nov. 22, 2022, the manufacturer announced that it had been cleared by the FDA for the treatment of mild to severe inflammatory acne vulgaris.
Dr. Sakamoto and her Wellman colleagues have been working with five dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, and Mitchel Goldman, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2022, more than 50 patients with mild to severe acne were enrolled in four studies and an additional 30 were enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment after four monthly treatment sessions. The average lesion reduction at week 12 was 82% and the mean visual analog scale score immediately after treatment was 2.09 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device overall with no adverse events reported. At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histologic studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other skin structures.
Dr. Sakamoto emphasized that to date no direct clinical comparisons have been made between the AviClear and Accure devices. “Are all 1,726-nm lasers made equal? That is a question that we have to keep in our mind,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “They are using the same wavelength, but they are different types of lasers.”
For example, the Accure Laser treats to temperature, relies on air cooling, and is targeted to dermatologists and plastic surgeons, while the AviClear treats to fluence, relies on contact cooling, and includes med spas and other nonphysician providers as the target users. “Mathematically, the difference between the two devices is that the Accure can achieve deeper penetration in a single pulse, while the AviClear is a little more superficial,” she said. “Whether that is translated clinically is unknown at this point.”
Dr. Sakamoto also discussed the TheraClearX, which is FDA cleared for the treatment of mild, moderate, and severe acne, including comedonal, pustular, and inflammatory acne vulgaris. The device, which is a new version of the Palomar Acleara, uses a vacuum technique with up to 3 psi pressure in conjunction with broadband light with a wavelength spectrum of 500 nm–1,200 nm delivered through a liquid-cooled, handheld delivery system. The predicate device was the Aesthera Isolaz System. The vacuum extracts buildup of sebaceous material. “At the same time, it takes the blood out of the competing chromophore,” she said. “By doing so, it potentially damages the sebaceous glands and reduces the inflammatory lesions.”
Dr. Sakamoto disclosed that she is the founder of and science advisor for Lightwater Bioscience. She is also a science advisor for Accure Acne and has received portions of patent royalties from Massachusetts General Hospital.
The calendar year
This was preceded by the FDA clearance of AviClear, marketed by Cutera, in March, and the commercial launch of TheraClearX, marketed by StrataSkin, in July.
“It’s an exciting time to be working with acne,” Fernanda H. Sakamoto, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. “We’ll see a lot of people using new devices. I’m looking forward to seeing results in the long term.”
AviClear and the Accure Laser System, marketed by Accure, are both powered by a 1,726-nm laser, but they work differently. AviClear, which was cleared for the treatment of mild, moderate, and severe acne, has a maximum fluence of 30 J/cm2 in single-pulse mode and a maximum fluence of 20 J/cm2 in double-pulse mode. The treatment handpiece has an integrated scanner for delivering treatment spot(s) in an operator-selected pattern. “It’s a little bit lower powered than the Accure and has a maximum pulse energy of 5 joules and a pulse duration of up to 50 milliseconds,” Dr. Sakamoto said. In the treatment of acne, laser and light treatments target the sebaceous gland.
In pivotal data submitted to the FDA, 104 patients with acne who were enrolled at 7 U.S. sites received 304 treatments with AviClear spaced 2-5 weeks apart. Each treatment took about 30 minutes. Treatment success was defined as having at least 50% fewer inflammatory acne lesions 12 weeks after the final treatment visit, compared with baseline. At the week 4 follow-up visit, there were median and mean reductions of 42% and 37%, respectively, in the inflammatory lesion counts from baseline (P < .001). The researchers found that, at the week 4 follow-up visit, 36% of patients had achieved treatment success, which increased to 78% at the 12-week follow-up visit. Treatment was considered safe and tolerable, according to the manufacturer.
The other newcomer device with a 1,726-nm wavelength is the Accure Laser System, which features a smart laser handpiece for real-time thermal monitoring and precise delivery of laser emissions. The device received CE Mark approval in 2020 for the treatment of moderate acne, and on Nov. 22, 2022, the manufacturer announced that it had been cleared by the FDA for the treatment of mild to severe inflammatory acne vulgaris.
Dr. Sakamoto and her Wellman colleagues have been working with five dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, and Mitchel Goldman, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2022, more than 50 patients with mild to severe acne were enrolled in four studies and an additional 30 were enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment after four monthly treatment sessions. The average lesion reduction at week 12 was 82% and the mean visual analog scale score immediately after treatment was 2.09 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device overall with no adverse events reported. At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histologic studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other skin structures.
Dr. Sakamoto emphasized that to date no direct clinical comparisons have been made between the AviClear and Accure devices. “Are all 1,726-nm lasers made equal? That is a question that we have to keep in our mind,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “They are using the same wavelength, but they are different types of lasers.”
For example, the Accure Laser treats to temperature, relies on air cooling, and is targeted to dermatologists and plastic surgeons, while the AviClear treats to fluence, relies on contact cooling, and includes med spas and other nonphysician providers as the target users. “Mathematically, the difference between the two devices is that the Accure can achieve deeper penetration in a single pulse, while the AviClear is a little more superficial,” she said. “Whether that is translated clinically is unknown at this point.”
Dr. Sakamoto also discussed the TheraClearX, which is FDA cleared for the treatment of mild, moderate, and severe acne, including comedonal, pustular, and inflammatory acne vulgaris. The device, which is a new version of the Palomar Acleara, uses a vacuum technique with up to 3 psi pressure in conjunction with broadband light with a wavelength spectrum of 500 nm–1,200 nm delivered through a liquid-cooled, handheld delivery system. The predicate device was the Aesthera Isolaz System. The vacuum extracts buildup of sebaceous material. “At the same time, it takes the blood out of the competing chromophore,” she said. “By doing so, it potentially damages the sebaceous glands and reduces the inflammatory lesions.”
Dr. Sakamoto disclosed that she is the founder of and science advisor for Lightwater Bioscience. She is also a science advisor for Accure Acne and has received portions of patent royalties from Massachusetts General Hospital.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
What does it take for men to embrace cosmetic treatments?
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE