User login
Methotrexate enhances pegloticase response in uncontrolled gout
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
FROM THE EULAR 2022 CONGRESS
European AxSpA guidelines reflect recent changes in drug therapy
COPENHAGEN – European recommendations and overarching principles for the management of patients with axial spondyloarthritis (axSpA) have remained largely unchanged since 2016 – with a few notable but very important exceptions.
The 2022 updated recommendations include a new point regarding which biologic agents to use for patients with recurrent uveitis, active inflammatory bowel disease (IBD), or significant psoriasis, as well as new advice to reevaluate the diagnosis and consider the presence of comorbidities if the disease doesn’t respond to current therapies, reported Sofia Ramiro, MD, PhD, from Leiden (Netherlands) University Medical Center.
She summarized the 2022 updates at the annual European Congress of Rheumatology on behalf of colleagues in the ASAS (Assessment of SpondyloArthritis International Society)/EULAR committee.
Among other significant updates are a recommendation for managing patients with persistently high disease activity despite conventional therapy, and a recommendation as to what to do when a first biologic or targeted synthetic disease-modifying antirheumatic drug (DMARD) fails, Dr. Ramiro said at the meeting.
“Although we have more changes in the pharmacological part, I would like to emphasize the importance of nonpharmacological treatment in axial SpA,” she said.
Overarching principles
The members of the committee that created the recommendations were in complete agreement that axSpA, as they state in the overarching principles, “is a potentially severe disease with diverse manifestations, usually requiring multidisciplinary management coordinated by the rheumatologist.”
They also universally acknowledged that “the primary goal of treating the patient with axSpA is to maximize health-related quality of life through control of symptoms and inflammation, prevention of progressive structural damage, preservation/normalization of function, and social participation.”
The overarching principles include the aforementioned emphasis on both pharmacologic and nonpharmacologic management, shared decision-making between patients and rheumatologists, and awareness of the potential financial toxicities and societal problems that patients face.
A closer look: New recommendations
As noted before, there are two new recommendations since the 2016 iteration.
Recommendation No. 10 states, “If there is a history of recurrent uveitis or active IBD, preference should be given to a monoclonal antibody against TNF-alpha [tumor necrosis factor–alpha]. For patients with significant psoriasis, an IL-17 [interleukin-17] inhibitor may be preferred.”
This recommendation stipulates that it refers only to IL-17A inhibitors.
The other new recommendation, No. 11, seems like plain common sense. It states, “Absence of response to treatment should trigger reevaluation of the diagnosis and consideration of the presence of comorbidities.”
Revised recommendations
The two significantly revised recommendations deal with drug therapy.
Recommendation No. 9 holds that for patients with persistently high disease activity despite conventional therapy, a TNF inhibitor, including the pegylated humanized antigen-binding fragment certolizumab pegol (Cimzia), an IL-17 inhibitor, or Janus kinase (JAK) inhibitor, should be considered.
Recommendation No. 12 states that if the first biologic or targeted synthetic DMARD fails, switching to another biologic DMARD (TNF inhibitor or IL-17 inhibitor) or JAK inhibitor should be considered.
Transatlantic similarities, differences
Lianne Gensler, MD, a rheumatologist and professor of medicine at the University of California, San Francisco, who served on the committee that developed the 2019 American College of Rheumatology guidelines for the treatment of ankylosing spondylitis and nonradiographic axSpA, said that, while there are similarities between some of the recommendations promulgated on each side of the Atlantic, there are significant differences and even opposing viewpoints.
A primary difference between the two is the methodology used to arrive at the recommendations in the first place, she said in an interview with this news organization.
“ACR uses a very robust approach to guideline development, where each question is addressed by a ‘PICO’ ” population, intervention, control, and outcomes – and that’s good if you have good evidence, but sometimes – often, in fact – we don’t have strong evidence that would lead everyone to choose the same approach every time, and that’s true especially in inflammatory arthritis, where there’s a lot of shared decision-making, so many of the recommendations out of ACR are conditional,” she said.
In contrast, the ASAS/EULAR recommendations are based largely on broader levels of evidence and on consensus. In developing the European recommendations, the authors were able to take into account drugs that were newly approved since the 2019 ACR guidelines were issued, she noted.
Although many of the broader recommendations are similar, they diverge when it comes to specific issues, such as whether to treat to target.
“ACR guidelines say, ‘Do not treat to target.’ EULAR guidelines say it’s okay to treat to target. ACR guidelines made that decision because at that time, there was no treat-to-target data,” Dr, Gensler said.
“I think, as rheumatologists, we always want to aim for a goal in a patient, so it’s not unreasonable, but I think we shouldn’t attach too much to a number,” she said.
Another difference is that the ACR guidelines recommend against switching to a biosimilar agent when a patient’s condition is stable with the originator biologic.
Dr. Gensler said that she particularly appreciated the new EULAR recommendation (No. 11) to reconsider the diagnosis for patients for whom therapies have failed.
“The sense that nonresponse means ongoing disease activity and therefore drug escalation or change needs to happen is not always the right answer,” she said.
The process for developing the recommendations was supported by EULAR. Dr. Ramiro has received research grants and consulting and/or speaking fees from AbbVie, Eli Lilly, Galapagos, Merck Sharp and Dohme, Novartis, Pfizer, Sanofi, and UCB. Dr. Gensler has received research grant support from Novartis, Pfizer, and UCB and has consulting relationships with AbbVie, Gilead, Janssen, MoonLake, Novartis, and Pfizer.
A version of this article first appeared on Medscape.com.
COPENHAGEN – European recommendations and overarching principles for the management of patients with axial spondyloarthritis (axSpA) have remained largely unchanged since 2016 – with a few notable but very important exceptions.
The 2022 updated recommendations include a new point regarding which biologic agents to use for patients with recurrent uveitis, active inflammatory bowel disease (IBD), or significant psoriasis, as well as new advice to reevaluate the diagnosis and consider the presence of comorbidities if the disease doesn’t respond to current therapies, reported Sofia Ramiro, MD, PhD, from Leiden (Netherlands) University Medical Center.
She summarized the 2022 updates at the annual European Congress of Rheumatology on behalf of colleagues in the ASAS (Assessment of SpondyloArthritis International Society)/EULAR committee.
Among other significant updates are a recommendation for managing patients with persistently high disease activity despite conventional therapy, and a recommendation as to what to do when a first biologic or targeted synthetic disease-modifying antirheumatic drug (DMARD) fails, Dr. Ramiro said at the meeting.
“Although we have more changes in the pharmacological part, I would like to emphasize the importance of nonpharmacological treatment in axial SpA,” she said.
Overarching principles
The members of the committee that created the recommendations were in complete agreement that axSpA, as they state in the overarching principles, “is a potentially severe disease with diverse manifestations, usually requiring multidisciplinary management coordinated by the rheumatologist.”
They also universally acknowledged that “the primary goal of treating the patient with axSpA is to maximize health-related quality of life through control of symptoms and inflammation, prevention of progressive structural damage, preservation/normalization of function, and social participation.”
The overarching principles include the aforementioned emphasis on both pharmacologic and nonpharmacologic management, shared decision-making between patients and rheumatologists, and awareness of the potential financial toxicities and societal problems that patients face.
A closer look: New recommendations
As noted before, there are two new recommendations since the 2016 iteration.
Recommendation No. 10 states, “If there is a history of recurrent uveitis or active IBD, preference should be given to a monoclonal antibody against TNF-alpha [tumor necrosis factor–alpha]. For patients with significant psoriasis, an IL-17 [interleukin-17] inhibitor may be preferred.”
This recommendation stipulates that it refers only to IL-17A inhibitors.
The other new recommendation, No. 11, seems like plain common sense. It states, “Absence of response to treatment should trigger reevaluation of the diagnosis and consideration of the presence of comorbidities.”
Revised recommendations
The two significantly revised recommendations deal with drug therapy.
Recommendation No. 9 holds that for patients with persistently high disease activity despite conventional therapy, a TNF inhibitor, including the pegylated humanized antigen-binding fragment certolizumab pegol (Cimzia), an IL-17 inhibitor, or Janus kinase (JAK) inhibitor, should be considered.
Recommendation No. 12 states that if the first biologic or targeted synthetic DMARD fails, switching to another biologic DMARD (TNF inhibitor or IL-17 inhibitor) or JAK inhibitor should be considered.
Transatlantic similarities, differences
Lianne Gensler, MD, a rheumatologist and professor of medicine at the University of California, San Francisco, who served on the committee that developed the 2019 American College of Rheumatology guidelines for the treatment of ankylosing spondylitis and nonradiographic axSpA, said that, while there are similarities between some of the recommendations promulgated on each side of the Atlantic, there are significant differences and even opposing viewpoints.
A primary difference between the two is the methodology used to arrive at the recommendations in the first place, she said in an interview with this news organization.
“ACR uses a very robust approach to guideline development, where each question is addressed by a ‘PICO’ ” population, intervention, control, and outcomes – and that’s good if you have good evidence, but sometimes – often, in fact – we don’t have strong evidence that would lead everyone to choose the same approach every time, and that’s true especially in inflammatory arthritis, where there’s a lot of shared decision-making, so many of the recommendations out of ACR are conditional,” she said.
In contrast, the ASAS/EULAR recommendations are based largely on broader levels of evidence and on consensus. In developing the European recommendations, the authors were able to take into account drugs that were newly approved since the 2019 ACR guidelines were issued, she noted.
Although many of the broader recommendations are similar, they diverge when it comes to specific issues, such as whether to treat to target.
“ACR guidelines say, ‘Do not treat to target.’ EULAR guidelines say it’s okay to treat to target. ACR guidelines made that decision because at that time, there was no treat-to-target data,” Dr, Gensler said.
“I think, as rheumatologists, we always want to aim for a goal in a patient, so it’s not unreasonable, but I think we shouldn’t attach too much to a number,” she said.
Another difference is that the ACR guidelines recommend against switching to a biosimilar agent when a patient’s condition is stable with the originator biologic.
Dr. Gensler said that she particularly appreciated the new EULAR recommendation (No. 11) to reconsider the diagnosis for patients for whom therapies have failed.
“The sense that nonresponse means ongoing disease activity and therefore drug escalation or change needs to happen is not always the right answer,” she said.
The process for developing the recommendations was supported by EULAR. Dr. Ramiro has received research grants and consulting and/or speaking fees from AbbVie, Eli Lilly, Galapagos, Merck Sharp and Dohme, Novartis, Pfizer, Sanofi, and UCB. Dr. Gensler has received research grant support from Novartis, Pfizer, and UCB and has consulting relationships with AbbVie, Gilead, Janssen, MoonLake, Novartis, and Pfizer.
A version of this article first appeared on Medscape.com.
COPENHAGEN – European recommendations and overarching principles for the management of patients with axial spondyloarthritis (axSpA) have remained largely unchanged since 2016 – with a few notable but very important exceptions.
The 2022 updated recommendations include a new point regarding which biologic agents to use for patients with recurrent uveitis, active inflammatory bowel disease (IBD), or significant psoriasis, as well as new advice to reevaluate the diagnosis and consider the presence of comorbidities if the disease doesn’t respond to current therapies, reported Sofia Ramiro, MD, PhD, from Leiden (Netherlands) University Medical Center.
She summarized the 2022 updates at the annual European Congress of Rheumatology on behalf of colleagues in the ASAS (Assessment of SpondyloArthritis International Society)/EULAR committee.
Among other significant updates are a recommendation for managing patients with persistently high disease activity despite conventional therapy, and a recommendation as to what to do when a first biologic or targeted synthetic disease-modifying antirheumatic drug (DMARD) fails, Dr. Ramiro said at the meeting.
“Although we have more changes in the pharmacological part, I would like to emphasize the importance of nonpharmacological treatment in axial SpA,” she said.
Overarching principles
The members of the committee that created the recommendations were in complete agreement that axSpA, as they state in the overarching principles, “is a potentially severe disease with diverse manifestations, usually requiring multidisciplinary management coordinated by the rheumatologist.”
They also universally acknowledged that “the primary goal of treating the patient with axSpA is to maximize health-related quality of life through control of symptoms and inflammation, prevention of progressive structural damage, preservation/normalization of function, and social participation.”
The overarching principles include the aforementioned emphasis on both pharmacologic and nonpharmacologic management, shared decision-making between patients and rheumatologists, and awareness of the potential financial toxicities and societal problems that patients face.
A closer look: New recommendations
As noted before, there are two new recommendations since the 2016 iteration.
Recommendation No. 10 states, “If there is a history of recurrent uveitis or active IBD, preference should be given to a monoclonal antibody against TNF-alpha [tumor necrosis factor–alpha]. For patients with significant psoriasis, an IL-17 [interleukin-17] inhibitor may be preferred.”
This recommendation stipulates that it refers only to IL-17A inhibitors.
The other new recommendation, No. 11, seems like plain common sense. It states, “Absence of response to treatment should trigger reevaluation of the diagnosis and consideration of the presence of comorbidities.”
Revised recommendations
The two significantly revised recommendations deal with drug therapy.
Recommendation No. 9 holds that for patients with persistently high disease activity despite conventional therapy, a TNF inhibitor, including the pegylated humanized antigen-binding fragment certolizumab pegol (Cimzia), an IL-17 inhibitor, or Janus kinase (JAK) inhibitor, should be considered.
Recommendation No. 12 states that if the first biologic or targeted synthetic DMARD fails, switching to another biologic DMARD (TNF inhibitor or IL-17 inhibitor) or JAK inhibitor should be considered.
Transatlantic similarities, differences
Lianne Gensler, MD, a rheumatologist and professor of medicine at the University of California, San Francisco, who served on the committee that developed the 2019 American College of Rheumatology guidelines for the treatment of ankylosing spondylitis and nonradiographic axSpA, said that, while there are similarities between some of the recommendations promulgated on each side of the Atlantic, there are significant differences and even opposing viewpoints.
A primary difference between the two is the methodology used to arrive at the recommendations in the first place, she said in an interview with this news organization.
“ACR uses a very robust approach to guideline development, where each question is addressed by a ‘PICO’ ” population, intervention, control, and outcomes – and that’s good if you have good evidence, but sometimes – often, in fact – we don’t have strong evidence that would lead everyone to choose the same approach every time, and that’s true especially in inflammatory arthritis, where there’s a lot of shared decision-making, so many of the recommendations out of ACR are conditional,” she said.
In contrast, the ASAS/EULAR recommendations are based largely on broader levels of evidence and on consensus. In developing the European recommendations, the authors were able to take into account drugs that were newly approved since the 2019 ACR guidelines were issued, she noted.
Although many of the broader recommendations are similar, they diverge when it comes to specific issues, such as whether to treat to target.
“ACR guidelines say, ‘Do not treat to target.’ EULAR guidelines say it’s okay to treat to target. ACR guidelines made that decision because at that time, there was no treat-to-target data,” Dr, Gensler said.
“I think, as rheumatologists, we always want to aim for a goal in a patient, so it’s not unreasonable, but I think we shouldn’t attach too much to a number,” she said.
Another difference is that the ACR guidelines recommend against switching to a biosimilar agent when a patient’s condition is stable with the originator biologic.
Dr. Gensler said that she particularly appreciated the new EULAR recommendation (No. 11) to reconsider the diagnosis for patients for whom therapies have failed.
“The sense that nonresponse means ongoing disease activity and therefore drug escalation or change needs to happen is not always the right answer,” she said.
The process for developing the recommendations was supported by EULAR. Dr. Ramiro has received research grants and consulting and/or speaking fees from AbbVie, Eli Lilly, Galapagos, Merck Sharp and Dohme, Novartis, Pfizer, Sanofi, and UCB. Dr. Gensler has received research grant support from Novartis, Pfizer, and UCB and has consulting relationships with AbbVie, Gilead, Janssen, MoonLake, Novartis, and Pfizer.
A version of this article first appeared on Medscape.com.
THE EULAR 2022 CONGRESS
TNF placental transfer makes little difference in offspring infections
COPENHAGEN – Here’s reassuring news for pregnant women with rheumatic diseases treated with tumor necrosis factor (TNF)–alpha inhibitors: Although the drugs vary widely in their transmissibility across the placenta, there appears to be no excess risk for serious infections in children exposed in utero to TNF inhibitors with high, compared with low, placental transfer.
That’s according to investigators at McGill University in Montreal, who studied outcomes for nearly 3,000 infants who were exposed to TNF inhibitors during gestation.
“Our data are reassuring as we saw no strong signal, which suggests that there is no need to switch the mother’s drugs. More studies are needed, but this is a step in the right direction to reduce maternal stress and reassure physicians,” said Leah K. Flatman, MSc, a PhD candidate in epidemiology at McGill.
Ms. Flatman presented the findings in an oral abstract session at the annual European Congress of Rheumatology.
Not without risks
Approximately 20% of pregnant women with chronic inflammatory diseases are prescribed a TNF inhibitor, a class of drug that is effective for disease control but also increases risk for infection because of immunosuppressive effects.
“Similarly, offspring exposed in utero to TNF inhibitors may also experience immunosuppression and subsequent serious infections in their first year of life. This is the result of the TNF inhibitor entering the fetal bloodstream at different concentrations,» Ms. Flatman said.
Anti-TNF monoclonal immunoglobulins, such as infliximab (Remicade and biosimilars), adalimumab (Humira and biosimilars), and golimumab (Simponi) have the highest placental transfer, reaching higher levels in fetal circulation than in maternal circulation, she noted.
In contrast, certolizumab (Cimzia), a pegylated humanized antigen-binding fragment, and etanercept (Enbrel and biosimilars), a fusion protein, have the lowest placental penetration, Ms. Flatman said.
Population study
The investigators conducted a population cohort study using the IBM MarketScan database of commercial claims from employer-provided health insurance plans in the United States.
They looked at data on offspring of mothers with rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and/or inflammatory bowel diseases (IBD; Crohn’s disease, and ulcerative colitis). The children were born from Jan. 1, 2011 through Dec. 31, 2019.
The exposure was at least one filled prescription and/or infusion procedure claim for TNF inhibitors in the 6 months before delivery. The exposures were divided into high and low placental-transfer categories.
A total of 26,088 offspring were identified, of whom 2,902 (11.1%) were exposed to a TNF inhibitor in utero. A little more than half of these children were born to mothers treated with TNF inhibitors for IBD.
For the primary outcome of serious infections (based on at least one hospitalization with infection in the first year of life), the investigators plotted Kaplan-Meier curves, which showed that the survival probability of serious infections in the high and low groups overlapped, indicating no large differences.
Of 2,105 offspring of mothers treated with a high–placental-transfer drug, 38 (1.8%) had serious infections, compared with 10 of 797 offspring (1.3%) of mothers who received low–placental-transfer drugs.
In multivariable analysis that controlled for maternal age at delivery, any RA diagnosis without an IBD diagnosis, and IBD diagnosis, gestational or pregestational diabetes, maternal asthma, preterm delivery, corticosteroid use, and disease-modifying antirheumatic drug use, the investigators saw that the hazard ratio for risk for serious infection in the high–, compared with the low–placental-transfer group was 1.20, with a confidence interval crossing 1, indicating nonsignificance.
Similar results reported
Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented, told this news organization that the findings were in line with those of a recent meta-analysis looking at the safety of biologic agents in pregnant women with IBD.
She added, however, that although the meta-analysis also showed little difference in outcomes for the children of women treated with high– compared with low–placental-transfer drugs, “we need more data to be sure about this.”
Comoderator Gabriela Riemekasten, MD, director of the clinic for rheumatology and clinical immunology at University Hospital in Lübeck, Germany, told this news organization that she was surprised to see that more women received high– than low–placental-transfer drugs.
Although there was a 20% difference between the groups, the numbers were relatively low, and “I would consider this in my practice and give my patients the advice of these data,” she said.
The study was supported by an Arthritis Society PhD Salary Award, and a Canadian Institutes of Health Project grant. Ms. Flatman, Dr. Förger, and Dr. Riemekasten reported having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Here’s reassuring news for pregnant women with rheumatic diseases treated with tumor necrosis factor (TNF)–alpha inhibitors: Although the drugs vary widely in their transmissibility across the placenta, there appears to be no excess risk for serious infections in children exposed in utero to TNF inhibitors with high, compared with low, placental transfer.
That’s according to investigators at McGill University in Montreal, who studied outcomes for nearly 3,000 infants who were exposed to TNF inhibitors during gestation.
“Our data are reassuring as we saw no strong signal, which suggests that there is no need to switch the mother’s drugs. More studies are needed, but this is a step in the right direction to reduce maternal stress and reassure physicians,” said Leah K. Flatman, MSc, a PhD candidate in epidemiology at McGill.
Ms. Flatman presented the findings in an oral abstract session at the annual European Congress of Rheumatology.
Not without risks
Approximately 20% of pregnant women with chronic inflammatory diseases are prescribed a TNF inhibitor, a class of drug that is effective for disease control but also increases risk for infection because of immunosuppressive effects.
“Similarly, offspring exposed in utero to TNF inhibitors may also experience immunosuppression and subsequent serious infections in their first year of life. This is the result of the TNF inhibitor entering the fetal bloodstream at different concentrations,» Ms. Flatman said.
Anti-TNF monoclonal immunoglobulins, such as infliximab (Remicade and biosimilars), adalimumab (Humira and biosimilars), and golimumab (Simponi) have the highest placental transfer, reaching higher levels in fetal circulation than in maternal circulation, she noted.
In contrast, certolizumab (Cimzia), a pegylated humanized antigen-binding fragment, and etanercept (Enbrel and biosimilars), a fusion protein, have the lowest placental penetration, Ms. Flatman said.
Population study
The investigators conducted a population cohort study using the IBM MarketScan database of commercial claims from employer-provided health insurance plans in the United States.
They looked at data on offspring of mothers with rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and/or inflammatory bowel diseases (IBD; Crohn’s disease, and ulcerative colitis). The children were born from Jan. 1, 2011 through Dec. 31, 2019.
The exposure was at least one filled prescription and/or infusion procedure claim for TNF inhibitors in the 6 months before delivery. The exposures were divided into high and low placental-transfer categories.
A total of 26,088 offspring were identified, of whom 2,902 (11.1%) were exposed to a TNF inhibitor in utero. A little more than half of these children were born to mothers treated with TNF inhibitors for IBD.
For the primary outcome of serious infections (based on at least one hospitalization with infection in the first year of life), the investigators plotted Kaplan-Meier curves, which showed that the survival probability of serious infections in the high and low groups overlapped, indicating no large differences.
Of 2,105 offspring of mothers treated with a high–placental-transfer drug, 38 (1.8%) had serious infections, compared with 10 of 797 offspring (1.3%) of mothers who received low–placental-transfer drugs.
In multivariable analysis that controlled for maternal age at delivery, any RA diagnosis without an IBD diagnosis, and IBD diagnosis, gestational or pregestational diabetes, maternal asthma, preterm delivery, corticosteroid use, and disease-modifying antirheumatic drug use, the investigators saw that the hazard ratio for risk for serious infection in the high–, compared with the low–placental-transfer group was 1.20, with a confidence interval crossing 1, indicating nonsignificance.
Similar results reported
Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented, told this news organization that the findings were in line with those of a recent meta-analysis looking at the safety of biologic agents in pregnant women with IBD.
She added, however, that although the meta-analysis also showed little difference in outcomes for the children of women treated with high– compared with low–placental-transfer drugs, “we need more data to be sure about this.”
Comoderator Gabriela Riemekasten, MD, director of the clinic for rheumatology and clinical immunology at University Hospital in Lübeck, Germany, told this news organization that she was surprised to see that more women received high– than low–placental-transfer drugs.
Although there was a 20% difference between the groups, the numbers were relatively low, and “I would consider this in my practice and give my patients the advice of these data,” she said.
The study was supported by an Arthritis Society PhD Salary Award, and a Canadian Institutes of Health Project grant. Ms. Flatman, Dr. Förger, and Dr. Riemekasten reported having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Here’s reassuring news for pregnant women with rheumatic diseases treated with tumor necrosis factor (TNF)–alpha inhibitors: Although the drugs vary widely in their transmissibility across the placenta, there appears to be no excess risk for serious infections in children exposed in utero to TNF inhibitors with high, compared with low, placental transfer.
That’s according to investigators at McGill University in Montreal, who studied outcomes for nearly 3,000 infants who were exposed to TNF inhibitors during gestation.
“Our data are reassuring as we saw no strong signal, which suggests that there is no need to switch the mother’s drugs. More studies are needed, but this is a step in the right direction to reduce maternal stress and reassure physicians,” said Leah K. Flatman, MSc, a PhD candidate in epidemiology at McGill.
Ms. Flatman presented the findings in an oral abstract session at the annual European Congress of Rheumatology.
Not without risks
Approximately 20% of pregnant women with chronic inflammatory diseases are prescribed a TNF inhibitor, a class of drug that is effective for disease control but also increases risk for infection because of immunosuppressive effects.
“Similarly, offspring exposed in utero to TNF inhibitors may also experience immunosuppression and subsequent serious infections in their first year of life. This is the result of the TNF inhibitor entering the fetal bloodstream at different concentrations,» Ms. Flatman said.
Anti-TNF monoclonal immunoglobulins, such as infliximab (Remicade and biosimilars), adalimumab (Humira and biosimilars), and golimumab (Simponi) have the highest placental transfer, reaching higher levels in fetal circulation than in maternal circulation, she noted.
In contrast, certolizumab (Cimzia), a pegylated humanized antigen-binding fragment, and etanercept (Enbrel and biosimilars), a fusion protein, have the lowest placental penetration, Ms. Flatman said.
Population study
The investigators conducted a population cohort study using the IBM MarketScan database of commercial claims from employer-provided health insurance plans in the United States.
They looked at data on offspring of mothers with rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and/or inflammatory bowel diseases (IBD; Crohn’s disease, and ulcerative colitis). The children were born from Jan. 1, 2011 through Dec. 31, 2019.
The exposure was at least one filled prescription and/or infusion procedure claim for TNF inhibitors in the 6 months before delivery. The exposures were divided into high and low placental-transfer categories.
A total of 26,088 offspring were identified, of whom 2,902 (11.1%) were exposed to a TNF inhibitor in utero. A little more than half of these children were born to mothers treated with TNF inhibitors for IBD.
For the primary outcome of serious infections (based on at least one hospitalization with infection in the first year of life), the investigators plotted Kaplan-Meier curves, which showed that the survival probability of serious infections in the high and low groups overlapped, indicating no large differences.
Of 2,105 offspring of mothers treated with a high–placental-transfer drug, 38 (1.8%) had serious infections, compared with 10 of 797 offspring (1.3%) of mothers who received low–placental-transfer drugs.
In multivariable analysis that controlled for maternal age at delivery, any RA diagnosis without an IBD diagnosis, and IBD diagnosis, gestational or pregestational diabetes, maternal asthma, preterm delivery, corticosteroid use, and disease-modifying antirheumatic drug use, the investigators saw that the hazard ratio for risk for serious infection in the high–, compared with the low–placental-transfer group was 1.20, with a confidence interval crossing 1, indicating nonsignificance.
Similar results reported
Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented, told this news organization that the findings were in line with those of a recent meta-analysis looking at the safety of biologic agents in pregnant women with IBD.
She added, however, that although the meta-analysis also showed little difference in outcomes for the children of women treated with high– compared with low–placental-transfer drugs, “we need more data to be sure about this.”
Comoderator Gabriela Riemekasten, MD, director of the clinic for rheumatology and clinical immunology at University Hospital in Lübeck, Germany, told this news organization that she was surprised to see that more women received high– than low–placental-transfer drugs.
Although there was a 20% difference between the groups, the numbers were relatively low, and “I would consider this in my practice and give my patients the advice of these data,” she said.
The study was supported by an Arthritis Society PhD Salary Award, and a Canadian Institutes of Health Project grant. Ms. Flatman, Dr. Förger, and Dr. Riemekasten reported having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
THE EULAR 2022 CONGRESS
‘Encouraging’ results of baricitinib in juvenile idiopathic arthritis
COPENHAGEN – Baricitinib (Olumiant), a Janus kinase (JAK) inhibitor, significantly increases time to disease flare and decreases frequency of flares in patients with juvenile idiopathic arthritis (JIA), according to the results of a phase 3, placebo-controlled study.
The results support use of baricitinib when biologic or conventional synthetic disease-modifying antirheumatic drugs (DMARDs) fail.
The difference in the proportion of patients who flared between baricitinib and placebo was seen as soon as 4 weeks after half of the patients switched from active drug to placebo, at 3.7% versus 23.5% respectively, reported Athimalaipet Ramanan, MD, from the University of Bristol (England) who presented the findings of the withdrawal, efficacy, and safety study at the annual European Congress of Rheumatology.
“Our patients and parents have been waiting for alternative drugs for JIA, so JAK inhibitors have come at the right time,” he said. “These are really very encouraging findings for families, caregivers, and patients with JIA, to have an effective oral JAK inhibitor for managing these children.”
In reporting the key findings, Dr. Ramanan added that the majority of patients (76%) achieved a JIA-ACR (American College of Rheumatology) 30 score during the 12-week open-label phase and went on to enter the double-blind withdrawal phase of the trial.
Baricitinib 2-mg tablets are already Food and Drug Administration approved for the treatment of adults with moderately to severely active rheumatoid arthritis. This study, sponsored by the drug manufacturer Eli Lilly, aimed to investigate the efficacy and safety in pediatric patients with JIA who have shown an inadequate response to conventional synthetic or biologic DMARDs.
“For juvenile patients we need to make a dose adjustment [from the adult dosing], especially because we don’t have long-term safety data from JAK inhibitors in general,” said Osama Elfayad, MD, rheumatologist from Mouwasat Hospital, Dammam, Saudi Arabia who attended the presentation and commented on the findings.
He emphasized that safety was of primary concern in the pediatric population who have a long life expectancy. “For me it is essential to have good long-term safety data in juvenile patients. If we start with 4 mg and if the patient is controlled, we should shift to 2 mg which will be much better. I understand some clinicians are asking for 1 mg.”
Study details
The study population included patients aged from 2 to 17 years old with extended oligo- or polyarticular JIA, enthesitis-related juvenile idiopathic arthritis (ERA) and juvenile psoriatic arthritis.
The trial was divided into three periods: a 2-week safety assessment, a 12-week open-label lead-in phase, and an up-to 32-week double-blind withdrawal phase. After confirmation of dose and safety, children were enrolled in the open-label phase receiving age-based, oral, once daily doses of baricitinib.
“The primary endpoint is really concerned with the next phase of the study [double-blind withdrawal phase] looking at the proportion of patients who have shown a response at week 12 [achieved JIA-ACR30] but when switched from active drug to placebo have a flare,” explained Dr. Ramanan.
Patients were randomized 1:1 to continuing baricitinib or newly starting placebo until disease flare or up to week 32. The time to flare during the double-blind phase was the primary endpoint, while secondary endpoints included JIA-ACR30/50/70/90 response rates at week 12, and the proportion of patients with a flare during the double-blind phase.
“These secondary endpoints are more relevant to the clinic,” noted Dr. Ramanan.
A total of 219 patients entered the open-label phase, and of these, 163 achieved a JIA-ACR 30. These 163 children entered the double-blind stage and were randomized to baricitinib four times a day (56 completed), or placebo (32 completed).
Two-thirds of patients were female, which is typical of the disease, explained Dr. Ramanan, and over two-thirds were White. “Most patients had had disease for around 4 years, and about half had had prior biologic therapy. About half were on baseline methotrexate and almost one-third had used corticosteroids although at doses of under 0.2mg/kg.
“It’s gratifying to see that over 75% achieved a JIA-ACR 30 [76.3%]. More importantly, two-thirds of the patients have a JIA-ACR 50 [63.5%], and almost half of the patients have a JIA-ACR 70 [46.1%]. This is pretty significant at 12 weeks only,” he remarked.
The key finding, however, was in the withdrawal phase, said Dr. Ramanan. “We see that those patients who had a response at week 12 and were then switched to placebo, about half [50.6%] flared on placebo, compared to only 17% of those who continued with baricitinib. So not only do those who switch to placebo have a higher frequency of flares but they are more likely to flare quickly, as early as 4 weeks.”
With respect to safety, he said: “This shows short-term safety, but what we really need is medium and long-term safety data. It is no surprise that most of the events seen were as expected in children including nasopharyngitis, upper respiratory tract infections, and nausea.”
In the baricitinib versus placebo phase, 4.9% had serious adverse events in the baricitinib group compared to 3.7% in the placebo group. “There was nothing we didn’t expect to see which was mainly infection,” said Dr. Ramanan.
Dr. Elfayad has no disclosures. Professor Ramanan is a consultant for Eli Lilly, Abbvie, Roche, UCB, Novartis, Pfizer, and Sobi. He has received grant/research support from Eli Lilly.
COPENHAGEN – Baricitinib (Olumiant), a Janus kinase (JAK) inhibitor, significantly increases time to disease flare and decreases frequency of flares in patients with juvenile idiopathic arthritis (JIA), according to the results of a phase 3, placebo-controlled study.
The results support use of baricitinib when biologic or conventional synthetic disease-modifying antirheumatic drugs (DMARDs) fail.
The difference in the proportion of patients who flared between baricitinib and placebo was seen as soon as 4 weeks after half of the patients switched from active drug to placebo, at 3.7% versus 23.5% respectively, reported Athimalaipet Ramanan, MD, from the University of Bristol (England) who presented the findings of the withdrawal, efficacy, and safety study at the annual European Congress of Rheumatology.
“Our patients and parents have been waiting for alternative drugs for JIA, so JAK inhibitors have come at the right time,” he said. “These are really very encouraging findings for families, caregivers, and patients with JIA, to have an effective oral JAK inhibitor for managing these children.”
In reporting the key findings, Dr. Ramanan added that the majority of patients (76%) achieved a JIA-ACR (American College of Rheumatology) 30 score during the 12-week open-label phase and went on to enter the double-blind withdrawal phase of the trial.
Baricitinib 2-mg tablets are already Food and Drug Administration approved for the treatment of adults with moderately to severely active rheumatoid arthritis. This study, sponsored by the drug manufacturer Eli Lilly, aimed to investigate the efficacy and safety in pediatric patients with JIA who have shown an inadequate response to conventional synthetic or biologic DMARDs.
“For juvenile patients we need to make a dose adjustment [from the adult dosing], especially because we don’t have long-term safety data from JAK inhibitors in general,” said Osama Elfayad, MD, rheumatologist from Mouwasat Hospital, Dammam, Saudi Arabia who attended the presentation and commented on the findings.
He emphasized that safety was of primary concern in the pediatric population who have a long life expectancy. “For me it is essential to have good long-term safety data in juvenile patients. If we start with 4 mg and if the patient is controlled, we should shift to 2 mg which will be much better. I understand some clinicians are asking for 1 mg.”
Study details
The study population included patients aged from 2 to 17 years old with extended oligo- or polyarticular JIA, enthesitis-related juvenile idiopathic arthritis (ERA) and juvenile psoriatic arthritis.
The trial was divided into three periods: a 2-week safety assessment, a 12-week open-label lead-in phase, and an up-to 32-week double-blind withdrawal phase. After confirmation of dose and safety, children were enrolled in the open-label phase receiving age-based, oral, once daily doses of baricitinib.
“The primary endpoint is really concerned with the next phase of the study [double-blind withdrawal phase] looking at the proportion of patients who have shown a response at week 12 [achieved JIA-ACR30] but when switched from active drug to placebo have a flare,” explained Dr. Ramanan.
Patients were randomized 1:1 to continuing baricitinib or newly starting placebo until disease flare or up to week 32. The time to flare during the double-blind phase was the primary endpoint, while secondary endpoints included JIA-ACR30/50/70/90 response rates at week 12, and the proportion of patients with a flare during the double-blind phase.
“These secondary endpoints are more relevant to the clinic,” noted Dr. Ramanan.
A total of 219 patients entered the open-label phase, and of these, 163 achieved a JIA-ACR 30. These 163 children entered the double-blind stage and were randomized to baricitinib four times a day (56 completed), or placebo (32 completed).
Two-thirds of patients were female, which is typical of the disease, explained Dr. Ramanan, and over two-thirds were White. “Most patients had had disease for around 4 years, and about half had had prior biologic therapy. About half were on baseline methotrexate and almost one-third had used corticosteroids although at doses of under 0.2mg/kg.
“It’s gratifying to see that over 75% achieved a JIA-ACR 30 [76.3%]. More importantly, two-thirds of the patients have a JIA-ACR 50 [63.5%], and almost half of the patients have a JIA-ACR 70 [46.1%]. This is pretty significant at 12 weeks only,” he remarked.
The key finding, however, was in the withdrawal phase, said Dr. Ramanan. “We see that those patients who had a response at week 12 and were then switched to placebo, about half [50.6%] flared on placebo, compared to only 17% of those who continued with baricitinib. So not only do those who switch to placebo have a higher frequency of flares but they are more likely to flare quickly, as early as 4 weeks.”
With respect to safety, he said: “This shows short-term safety, but what we really need is medium and long-term safety data. It is no surprise that most of the events seen were as expected in children including nasopharyngitis, upper respiratory tract infections, and nausea.”
In the baricitinib versus placebo phase, 4.9% had serious adverse events in the baricitinib group compared to 3.7% in the placebo group. “There was nothing we didn’t expect to see which was mainly infection,” said Dr. Ramanan.
Dr. Elfayad has no disclosures. Professor Ramanan is a consultant for Eli Lilly, Abbvie, Roche, UCB, Novartis, Pfizer, and Sobi. He has received grant/research support from Eli Lilly.
COPENHAGEN – Baricitinib (Olumiant), a Janus kinase (JAK) inhibitor, significantly increases time to disease flare and decreases frequency of flares in patients with juvenile idiopathic arthritis (JIA), according to the results of a phase 3, placebo-controlled study.
The results support use of baricitinib when biologic or conventional synthetic disease-modifying antirheumatic drugs (DMARDs) fail.
The difference in the proportion of patients who flared between baricitinib and placebo was seen as soon as 4 weeks after half of the patients switched from active drug to placebo, at 3.7% versus 23.5% respectively, reported Athimalaipet Ramanan, MD, from the University of Bristol (England) who presented the findings of the withdrawal, efficacy, and safety study at the annual European Congress of Rheumatology.
“Our patients and parents have been waiting for alternative drugs for JIA, so JAK inhibitors have come at the right time,” he said. “These are really very encouraging findings for families, caregivers, and patients with JIA, to have an effective oral JAK inhibitor for managing these children.”
In reporting the key findings, Dr. Ramanan added that the majority of patients (76%) achieved a JIA-ACR (American College of Rheumatology) 30 score during the 12-week open-label phase and went on to enter the double-blind withdrawal phase of the trial.
Baricitinib 2-mg tablets are already Food and Drug Administration approved for the treatment of adults with moderately to severely active rheumatoid arthritis. This study, sponsored by the drug manufacturer Eli Lilly, aimed to investigate the efficacy and safety in pediatric patients with JIA who have shown an inadequate response to conventional synthetic or biologic DMARDs.
“For juvenile patients we need to make a dose adjustment [from the adult dosing], especially because we don’t have long-term safety data from JAK inhibitors in general,” said Osama Elfayad, MD, rheumatologist from Mouwasat Hospital, Dammam, Saudi Arabia who attended the presentation and commented on the findings.
He emphasized that safety was of primary concern in the pediatric population who have a long life expectancy. “For me it is essential to have good long-term safety data in juvenile patients. If we start with 4 mg and if the patient is controlled, we should shift to 2 mg which will be much better. I understand some clinicians are asking for 1 mg.”
Study details
The study population included patients aged from 2 to 17 years old with extended oligo- or polyarticular JIA, enthesitis-related juvenile idiopathic arthritis (ERA) and juvenile psoriatic arthritis.
The trial was divided into three periods: a 2-week safety assessment, a 12-week open-label lead-in phase, and an up-to 32-week double-blind withdrawal phase. After confirmation of dose and safety, children were enrolled in the open-label phase receiving age-based, oral, once daily doses of baricitinib.
“The primary endpoint is really concerned with the next phase of the study [double-blind withdrawal phase] looking at the proportion of patients who have shown a response at week 12 [achieved JIA-ACR30] but when switched from active drug to placebo have a flare,” explained Dr. Ramanan.
Patients were randomized 1:1 to continuing baricitinib or newly starting placebo until disease flare or up to week 32. The time to flare during the double-blind phase was the primary endpoint, while secondary endpoints included JIA-ACR30/50/70/90 response rates at week 12, and the proportion of patients with a flare during the double-blind phase.
“These secondary endpoints are more relevant to the clinic,” noted Dr. Ramanan.
A total of 219 patients entered the open-label phase, and of these, 163 achieved a JIA-ACR 30. These 163 children entered the double-blind stage and were randomized to baricitinib four times a day (56 completed), or placebo (32 completed).
Two-thirds of patients were female, which is typical of the disease, explained Dr. Ramanan, and over two-thirds were White. “Most patients had had disease for around 4 years, and about half had had prior biologic therapy. About half were on baseline methotrexate and almost one-third had used corticosteroids although at doses of under 0.2mg/kg.
“It’s gratifying to see that over 75% achieved a JIA-ACR 30 [76.3%]. More importantly, two-thirds of the patients have a JIA-ACR 50 [63.5%], and almost half of the patients have a JIA-ACR 70 [46.1%]. This is pretty significant at 12 weeks only,” he remarked.
The key finding, however, was in the withdrawal phase, said Dr. Ramanan. “We see that those patients who had a response at week 12 and were then switched to placebo, about half [50.6%] flared on placebo, compared to only 17% of those who continued with baricitinib. So not only do those who switch to placebo have a higher frequency of flares but they are more likely to flare quickly, as early as 4 weeks.”
With respect to safety, he said: “This shows short-term safety, but what we really need is medium and long-term safety data. It is no surprise that most of the events seen were as expected in children including nasopharyngitis, upper respiratory tract infections, and nausea.”
In the baricitinib versus placebo phase, 4.9% had serious adverse events in the baricitinib group compared to 3.7% in the placebo group. “There was nothing we didn’t expect to see which was mainly infection,” said Dr. Ramanan.
Dr. Elfayad has no disclosures. Professor Ramanan is a consultant for Eli Lilly, Abbvie, Roche, UCB, Novartis, Pfizer, and Sobi. He has received grant/research support from Eli Lilly.
AT THE EULAR 2022 CONGRESS
Izokibep improves multiple psoriatic arthritis symptoms in phase 2 study
A host of psoriatic arthritis symptoms can be improved by the investigational interleukin (IL)-17 blocker izokibep, according to the results of a phase 2 trial presented at the annual European Congress of Rheumatology.
Around half of all participants in the trial who were treated with izokibep achieved a 50% or higher improvement in American College of Rheumatology response criteria (ACR50) at week 16, the trial’s primary endpoint. This was highly significant (P = .0003) when compared to the control group, where only 13% of patients given a placebo achieved an ACR50.
There was also a significant improvement in skin symptoms, as assessed by the Psoriasis Area and Severity Index (PASI) and resolution of enthesitis in 88% of patients given the highest dose of izokibep.
Aurelie Najm, MD, PhD, of the Institute of Infection, Immunity and Inflammation at the University of Glasgow, who tweeted about the main results, said that the data also looked “promising for the enthesitis domain” with a “safety profile similar to that observed in PsO [psoriasis].”Peter Taylor, MA, PhD, FRCP, FRCPE, of the University of Oxford in England, said: “The improvements demonstrated in arthritis, psoriasis, and enthesitis are exciting relative to responses reported for the current standard of care.”
He continued, in a statement issued jointly by Affibody, Acelyrin, and Immagene Biopharmaceuticals – the three companies assessing izokibep’s therapeutic potential – that the drug “seems promising” and that he was “eager to see its continued development for patients.”
Small and potent, a novel IL-17 inhibitor
Izokibep is an antibody mimetic that inhibits IL-17A designed to “overcome the limitations of monoclonal antibodies,” according to its developers.
Due to its small molecular size – reportedly about one-tenth of the size of a monoclonal antibody – they say that levels of high drug exposure can be achieved from a single, subcutaneous injection rather than an intravenous infusion, which is needed for monoclonal antibodies.
Moreover, izokibep’s small size means it could potentially reach target tissues “that may otherwise be inaccessible to the much larger monoclonal antibodies.”
So far more than 300 patients have been treated with izokibep, some for up to 3 years, but not all have had psoriatic arthritis. Indeed, the drug has been tested in patients with psoriasis, and there are a few actively recruiting trials including one in ankylosing spondylitis, another in noninfective uveitis, and one in the rare and painful skin condition hidradenitis suppurativa.
Testing two doses of izokibep in psoriatic arthritis
The trial presented at the EULAR 2022 Congress tested two doses of izokibep – 40 mg and 80 mg – given by subcutaneous injection every 2 weeks – against placebo in 135 adult patients with active psoriatic arthritis. For inclusion in the trial patients had to have at least three swollen and at least three tender joints and have had an inadequate response to prior therapy including nonsteroidal anti-inflammatory drugs, conventional synthetic disease-modifying antirheumatic drugs, or tumor necrosis factor inhibitors.
Principle investigator Frank Behrens, MD, of Goethe University Frankfurt, Germany, reported that it was a multicenter effort conducted at 22 European sites with the primary endpoint being an ACR50 response at 16 weeks. This was met by 52% of patients given the 80-mg dose of izokibep, 48% of patients given the 40-mg dose of izokibep, and just 13% of patients who had been randomized to placebo.
ACR20 and ACR70 response were one of several key secondary endpoints tested, again at 16 weeks, with a respective 75%, 60%, and 20% of patients in each group achieving the lower response target and 20%, 32%, and 5%, achieving the more stringent response target.
“Izokibep demonstrated a robust efficacy in the musculoskeletal arthritic domains, but also in the extra-articular musculoskeletal domain,” Dr. Behrens said.
Not only that, but the values were “at the top end” of what’s been demonstrated for drugs currently regarded as the standard of care.
More than 80% of patients achieved a PASI75 response and 57% a PASI50 response with the two doses of izokibep, and 63%-88% achieved a resolution of enthesitis. The latter was measured using the Leeds Enthesitis Index.
There was also improvement in quality of life, measured using the Psoriatic Impact of Disease questionnaire, with a percentage increase beyond the MCID of 31%-41% with izokibep versus 12% for placebo.
“These are the first data of the phase 2 study in psoriatic arthritis,” Dr. Behrens reported.
“The safety profile was consistent with placebo,” with the only “standout aspect” being a higher number of injection-site reactions with izokibep versus placebo; but there were no serious infections, no serious adverse events,” he added.
“The interesting thing is from the preclinical research there was no dose-limiting toxicity with izokibep, therefore, I think the plan in the future is maybe to increase the dose to optimize treatment outcome based on the really robust effectiveness we see here in the first study in this clinical trial,” he said.
As a small study, stratifying results by gender wasn’t an option, Dr. Behrens noted in answering a question during the discussion period, but might be something that will be included in future and larger trials based on the post-hoc findings of other IL-17 trials.
Moving forward, the next step will involve a phase 2b/3 pivotal study which will likely include a higher dosing regimen of 160 mg once weekly alongside the twice-weekly dosing used in this trial.
Izokibep is an investigational treatment being developed by Affibody AB, Sweden, and ACELYRIN, USA. All three companies funded the phase 2 trial and were involved in the study design, conduct and reporting of results.
Dr. Behrens and Dr. Taylor were investigators in the study.
Dr. Behrens disclosed he was a shareholder of Pfizer, Sanofi, GlaxoSmithKline, Gilead Sciences, Inc. and Novartis; part of the speakers’ bureau for Amgen, Horizon, Lilly, Novartis, Pfizer, Sanofi, Genzyme, Flexion and AbbVie; a consultant of AbbVie, Boehringer Ingelheim, Flexion, Janssen, Pfizer, Sanofi, Regeneron, SUN Pharma Advanced Research, Gilead Sciences, Inc.; and had received grant or research support from Pfizer, Janssen, Chugai, Celgene and Roche
Dr. Taylor acknowledged grant or research support from: Celgene and Galapagos, and acted as a consultant for AbbVie, Biogen, Bristol Myers Squibb, Fresenius, Galapagos, Gilead, GlaxoSmithKline, Janssen, Lilly, Nordic Pharma, Pfizer, Roche, Sanofi and UCB.
A host of psoriatic arthritis symptoms can be improved by the investigational interleukin (IL)-17 blocker izokibep, according to the results of a phase 2 trial presented at the annual European Congress of Rheumatology.
Around half of all participants in the trial who were treated with izokibep achieved a 50% or higher improvement in American College of Rheumatology response criteria (ACR50) at week 16, the trial’s primary endpoint. This was highly significant (P = .0003) when compared to the control group, where only 13% of patients given a placebo achieved an ACR50.
There was also a significant improvement in skin symptoms, as assessed by the Psoriasis Area and Severity Index (PASI) and resolution of enthesitis in 88% of patients given the highest dose of izokibep.
Aurelie Najm, MD, PhD, of the Institute of Infection, Immunity and Inflammation at the University of Glasgow, who tweeted about the main results, said that the data also looked “promising for the enthesitis domain” with a “safety profile similar to that observed in PsO [psoriasis].”Peter Taylor, MA, PhD, FRCP, FRCPE, of the University of Oxford in England, said: “The improvements demonstrated in arthritis, psoriasis, and enthesitis are exciting relative to responses reported for the current standard of care.”
He continued, in a statement issued jointly by Affibody, Acelyrin, and Immagene Biopharmaceuticals – the three companies assessing izokibep’s therapeutic potential – that the drug “seems promising” and that he was “eager to see its continued development for patients.”
Small and potent, a novel IL-17 inhibitor
Izokibep is an antibody mimetic that inhibits IL-17A designed to “overcome the limitations of monoclonal antibodies,” according to its developers.
Due to its small molecular size – reportedly about one-tenth of the size of a monoclonal antibody – they say that levels of high drug exposure can be achieved from a single, subcutaneous injection rather than an intravenous infusion, which is needed for monoclonal antibodies.
Moreover, izokibep’s small size means it could potentially reach target tissues “that may otherwise be inaccessible to the much larger monoclonal antibodies.”
So far more than 300 patients have been treated with izokibep, some for up to 3 years, but not all have had psoriatic arthritis. Indeed, the drug has been tested in patients with psoriasis, and there are a few actively recruiting trials including one in ankylosing spondylitis, another in noninfective uveitis, and one in the rare and painful skin condition hidradenitis suppurativa.
Testing two doses of izokibep in psoriatic arthritis
The trial presented at the EULAR 2022 Congress tested two doses of izokibep – 40 mg and 80 mg – given by subcutaneous injection every 2 weeks – against placebo in 135 adult patients with active psoriatic arthritis. For inclusion in the trial patients had to have at least three swollen and at least three tender joints and have had an inadequate response to prior therapy including nonsteroidal anti-inflammatory drugs, conventional synthetic disease-modifying antirheumatic drugs, or tumor necrosis factor inhibitors.
Principle investigator Frank Behrens, MD, of Goethe University Frankfurt, Germany, reported that it was a multicenter effort conducted at 22 European sites with the primary endpoint being an ACR50 response at 16 weeks. This was met by 52% of patients given the 80-mg dose of izokibep, 48% of patients given the 40-mg dose of izokibep, and just 13% of patients who had been randomized to placebo.
ACR20 and ACR70 response were one of several key secondary endpoints tested, again at 16 weeks, with a respective 75%, 60%, and 20% of patients in each group achieving the lower response target and 20%, 32%, and 5%, achieving the more stringent response target.
“Izokibep demonstrated a robust efficacy in the musculoskeletal arthritic domains, but also in the extra-articular musculoskeletal domain,” Dr. Behrens said.
Not only that, but the values were “at the top end” of what’s been demonstrated for drugs currently regarded as the standard of care.
More than 80% of patients achieved a PASI75 response and 57% a PASI50 response with the two doses of izokibep, and 63%-88% achieved a resolution of enthesitis. The latter was measured using the Leeds Enthesitis Index.
There was also improvement in quality of life, measured using the Psoriatic Impact of Disease questionnaire, with a percentage increase beyond the MCID of 31%-41% with izokibep versus 12% for placebo.
“These are the first data of the phase 2 study in psoriatic arthritis,” Dr. Behrens reported.
“The safety profile was consistent with placebo,” with the only “standout aspect” being a higher number of injection-site reactions with izokibep versus placebo; but there were no serious infections, no serious adverse events,” he added.
“The interesting thing is from the preclinical research there was no dose-limiting toxicity with izokibep, therefore, I think the plan in the future is maybe to increase the dose to optimize treatment outcome based on the really robust effectiveness we see here in the first study in this clinical trial,” he said.
As a small study, stratifying results by gender wasn’t an option, Dr. Behrens noted in answering a question during the discussion period, but might be something that will be included in future and larger trials based on the post-hoc findings of other IL-17 trials.
Moving forward, the next step will involve a phase 2b/3 pivotal study which will likely include a higher dosing regimen of 160 mg once weekly alongside the twice-weekly dosing used in this trial.
Izokibep is an investigational treatment being developed by Affibody AB, Sweden, and ACELYRIN, USA. All three companies funded the phase 2 trial and were involved in the study design, conduct and reporting of results.
Dr. Behrens and Dr. Taylor were investigators in the study.
Dr. Behrens disclosed he was a shareholder of Pfizer, Sanofi, GlaxoSmithKline, Gilead Sciences, Inc. and Novartis; part of the speakers’ bureau for Amgen, Horizon, Lilly, Novartis, Pfizer, Sanofi, Genzyme, Flexion and AbbVie; a consultant of AbbVie, Boehringer Ingelheim, Flexion, Janssen, Pfizer, Sanofi, Regeneron, SUN Pharma Advanced Research, Gilead Sciences, Inc.; and had received grant or research support from Pfizer, Janssen, Chugai, Celgene and Roche
Dr. Taylor acknowledged grant or research support from: Celgene and Galapagos, and acted as a consultant for AbbVie, Biogen, Bristol Myers Squibb, Fresenius, Galapagos, Gilead, GlaxoSmithKline, Janssen, Lilly, Nordic Pharma, Pfizer, Roche, Sanofi and UCB.
A host of psoriatic arthritis symptoms can be improved by the investigational interleukin (IL)-17 blocker izokibep, according to the results of a phase 2 trial presented at the annual European Congress of Rheumatology.
Around half of all participants in the trial who were treated with izokibep achieved a 50% or higher improvement in American College of Rheumatology response criteria (ACR50) at week 16, the trial’s primary endpoint. This was highly significant (P = .0003) when compared to the control group, where only 13% of patients given a placebo achieved an ACR50.
There was also a significant improvement in skin symptoms, as assessed by the Psoriasis Area and Severity Index (PASI) and resolution of enthesitis in 88% of patients given the highest dose of izokibep.
Aurelie Najm, MD, PhD, of the Institute of Infection, Immunity and Inflammation at the University of Glasgow, who tweeted about the main results, said that the data also looked “promising for the enthesitis domain” with a “safety profile similar to that observed in PsO [psoriasis].”Peter Taylor, MA, PhD, FRCP, FRCPE, of the University of Oxford in England, said: “The improvements demonstrated in arthritis, psoriasis, and enthesitis are exciting relative to responses reported for the current standard of care.”
He continued, in a statement issued jointly by Affibody, Acelyrin, and Immagene Biopharmaceuticals – the three companies assessing izokibep’s therapeutic potential – that the drug “seems promising” and that he was “eager to see its continued development for patients.”
Small and potent, a novel IL-17 inhibitor
Izokibep is an antibody mimetic that inhibits IL-17A designed to “overcome the limitations of monoclonal antibodies,” according to its developers.
Due to its small molecular size – reportedly about one-tenth of the size of a monoclonal antibody – they say that levels of high drug exposure can be achieved from a single, subcutaneous injection rather than an intravenous infusion, which is needed for monoclonal antibodies.
Moreover, izokibep’s small size means it could potentially reach target tissues “that may otherwise be inaccessible to the much larger monoclonal antibodies.”
So far more than 300 patients have been treated with izokibep, some for up to 3 years, but not all have had psoriatic arthritis. Indeed, the drug has been tested in patients with psoriasis, and there are a few actively recruiting trials including one in ankylosing spondylitis, another in noninfective uveitis, and one in the rare and painful skin condition hidradenitis suppurativa.
Testing two doses of izokibep in psoriatic arthritis
The trial presented at the EULAR 2022 Congress tested two doses of izokibep – 40 mg and 80 mg – given by subcutaneous injection every 2 weeks – against placebo in 135 adult patients with active psoriatic arthritis. For inclusion in the trial patients had to have at least three swollen and at least three tender joints and have had an inadequate response to prior therapy including nonsteroidal anti-inflammatory drugs, conventional synthetic disease-modifying antirheumatic drugs, or tumor necrosis factor inhibitors.
Principle investigator Frank Behrens, MD, of Goethe University Frankfurt, Germany, reported that it was a multicenter effort conducted at 22 European sites with the primary endpoint being an ACR50 response at 16 weeks. This was met by 52% of patients given the 80-mg dose of izokibep, 48% of patients given the 40-mg dose of izokibep, and just 13% of patients who had been randomized to placebo.
ACR20 and ACR70 response were one of several key secondary endpoints tested, again at 16 weeks, with a respective 75%, 60%, and 20% of patients in each group achieving the lower response target and 20%, 32%, and 5%, achieving the more stringent response target.
“Izokibep demonstrated a robust efficacy in the musculoskeletal arthritic domains, but also in the extra-articular musculoskeletal domain,” Dr. Behrens said.
Not only that, but the values were “at the top end” of what’s been demonstrated for drugs currently regarded as the standard of care.
More than 80% of patients achieved a PASI75 response and 57% a PASI50 response with the two doses of izokibep, and 63%-88% achieved a resolution of enthesitis. The latter was measured using the Leeds Enthesitis Index.
There was also improvement in quality of life, measured using the Psoriatic Impact of Disease questionnaire, with a percentage increase beyond the MCID of 31%-41% with izokibep versus 12% for placebo.
“These are the first data of the phase 2 study in psoriatic arthritis,” Dr. Behrens reported.
“The safety profile was consistent with placebo,” with the only “standout aspect” being a higher number of injection-site reactions with izokibep versus placebo; but there were no serious infections, no serious adverse events,” he added.
“The interesting thing is from the preclinical research there was no dose-limiting toxicity with izokibep, therefore, I think the plan in the future is maybe to increase the dose to optimize treatment outcome based on the really robust effectiveness we see here in the first study in this clinical trial,” he said.
As a small study, stratifying results by gender wasn’t an option, Dr. Behrens noted in answering a question during the discussion period, but might be something that will be included in future and larger trials based on the post-hoc findings of other IL-17 trials.
Moving forward, the next step will involve a phase 2b/3 pivotal study which will likely include a higher dosing regimen of 160 mg once weekly alongside the twice-weekly dosing used in this trial.
Izokibep is an investigational treatment being developed by Affibody AB, Sweden, and ACELYRIN, USA. All three companies funded the phase 2 trial and were involved in the study design, conduct and reporting of results.
Dr. Behrens and Dr. Taylor were investigators in the study.
Dr. Behrens disclosed he was a shareholder of Pfizer, Sanofi, GlaxoSmithKline, Gilead Sciences, Inc. and Novartis; part of the speakers’ bureau for Amgen, Horizon, Lilly, Novartis, Pfizer, Sanofi, Genzyme, Flexion and AbbVie; a consultant of AbbVie, Boehringer Ingelheim, Flexion, Janssen, Pfizer, Sanofi, Regeneron, SUN Pharma Advanced Research, Gilead Sciences, Inc.; and had received grant or research support from Pfizer, Janssen, Chugai, Celgene and Roche
Dr. Taylor acknowledged grant or research support from: Celgene and Galapagos, and acted as a consultant for AbbVie, Biogen, Bristol Myers Squibb, Fresenius, Galapagos, Gilead, GlaxoSmithKline, Janssen, Lilly, Nordic Pharma, Pfizer, Roche, Sanofi and UCB.
FROM THE EULAR 2022 CONGRESS
First evidence of disease modification with methotrexate in pre-RA
COPENHAGEN – Temporary methotrexate in clinically suspected arthralgia delays but does not prevent clinical arthritis development; however, it does lead to sustained reduction of disease burden and MRI-detected inflammation in all at-risk groups, shows the 2-year Treat Earlier study.
“These data provide the first evidence for disease modification when intervening in ‘pre-RA [rheumatoid arthritis]’ or arthralgia,” said Doortje Krijbolder, MD, of Leiden (the Netherlands) University Medical Center, who presented her study at the annual European Congress of Rheumatology.
The randomized, double-blind, study aimed to find out if giving methotrexate in the pre-arthritis phase of arthralgia (with subclinical joint inflammation) prevents the development of clinical arthritis or reduces the burden of disease.
“This is the first trial that aims to reduce the burden of disease, and as such, in pre-RA, it is important that disease modification is sustained after temporary treatment otherwise patients will start regressing with disease activity,” said Dr. Krijbolder.
She explained that methotrexate is usually initiated as first-line treatment when arthritis becomes clinically apparent with joint swelling, but “disease processes begin long before this, and only become clinically recognizable when patients develop symptoms.”
Clinically detectable arthritis development
All 236 patients included in the study had arthralgia of the small joints that, because of the character of the symptoms, was found clinically suspect for progression to RA over time.
“Importantly, these participants had not yet developed clinical arthritis that could be detected on physical joint examination, and were clinically suspected of progressing to RA. They had all undergone an MRI and subclinical joint-inflammation had been detected that was more than prevalent in symptom-free controls,” said Dr. Krijbolder.
Patients were randomized (1:1) to either a single intramuscular glucocorticoid injection (120 mg methylprednisolone [Depo Medrol]) and a 1-year course of oral methotrexate (up to 25 mg/week), or to placebo injection and placebo tablets, and were then followed for a further year without medication to see whether disease progressed.
Treatment and placebo groups were matched with an average age of 46-47 years, 62%-68% were women, they had had symptoms (joint pain) for 27-28 weeks, C-reactive protein was increased in 27%-30%, and 20%-26% were anti-citrullinated protein autoantibody (ACPA) positive.
The primary endpoint was the development of clinically detectable arthritis (fulfilling the 2010 RA-criteria or involving ≥ 2 joints) that persisted for at least 2 weeks. The main secondary endpoints were related to disease burden, including patient-reported physical functioning, along with symptoms and workability (presenteeism at work – the percentage of productivity lost caused by the joint complaints), and measured every 4 months, said Dr. Krijbolder.
She and her colleagues also followed the course of MRI-detected inflammation, which comprised the sum of tenosynovitis, synovitis, and osteitis scored with the RA-MRI Scoring (RAMRIS) method.
Analysis was carried out on an intention-to-treat basis, and two prespecified subgroup analyses were also performed to obtain a better understanding of the effect of methotrexate and glucocorticoids in participants with high risk of clinical arthritis development (positive predictive value (PPV) ≥ 70%), and in patients stratified for ACPA status.
Delays but does not prevent
There was no difference between treatment and placebo groups in the development of persistent clinical arthritis over 2 years (80% vs. 82%, hazard ratio [HR] 0.81; 95% confidence interval [CI], 0.45, 1.48]); however, in the high-risk group subanalysis, 67% in the placebo group developed persistent clinical arthritis. For the treatment group, 7%developed persistent clinical arthritis at 6 months, 27% at 12 months, 40% at 18 months, and 67% at 24 months. For the placebo group: 56% developed persistent clinical arthritis at 6 months, and 67% at 12 months, 18 months, and 24 months.
“Strikingly, in the treatment group there was a statistically significant difference between 6 and 12 months, but in year 2, this difference disappeared, suggesting a delayed arthritis development but no prevention,” said Dr. Krijbolder.
Persistent clinical arthritis became similar at 24 months, at 67% in both groups. A similar, but less pronounced, delaying effect was seen with the ACPA-positive patients, with 48% and 52% developing persistent clinical arthritis at 24 months.
In joint pain, there was a decline in the treatment group compared with the placebo group and this persisted over 2 years (–9 on scale of 0 to 100: (95%CI, –12,–4; P < .001), and a similar effect was seen in high-risk and ACPA subgroups, reported Dr. Krijbolder.
Physical functioning improved more in the treatment-group compared with the placebo group during the first months and remained better (mean between-group difference over 2 years HAQ [health assessment questionnaire] –0.1 [–0.2, –0.03; P = .004]), and morning stiffness (–12 [95%CI, –16, –8; P < .001]), and presenteeism (–8% [95%CI, –13%, –3%; P = .001]) also showed improvement over time compared with placebo.
MRI-detected joint-inflammation was also persistently improved with a mean difference over 2 years –1.4 points (95%CI, –2.0, –0.9; P < .001). “As we know that symptoms and functional impairments are associated with MRI-detected joint inflammation, it was not surprising that treatment induced a decline in joint inflammation that persisted over time, also after the stop of the treatment in the second year,” explained Dr. Krijbolder.
In the high-risk subgroup, as well as in both ACPA-positive and ACPA-negative participants, a comparable statistically significant decline in MRI-detected inflammation was found.
“It may seem counterintuitive that on the one hand we found a delaying effect of treatment on persistent clinical arthritis but no prevention, while on the other, we saw a sustained treatment effect on MRI-detected joint-inflammation and related symptoms and functional impairments,” added Dr. Krijbolder.
To help understand this, the researchers performed a post hoc analysis in high-risk participants, comparing those who did not progress with those who did progress to arthritis. “Both progressors and nonprogressors showed a sustained treatment effect for pain and MRI-detected joint-inflammation, and in nonprogressors, there was almost a complete relief of pain and they nearly returned to the normal range of MRI-detected joint-inflammation as seen in symptom-free controls,” reported Dr. Krijbolder.
“In those who progressed to arthritis, there was less pain and less MRI-detected joint inflammation in the treatment group, but also at the time when they developed clinical arthritis. So both progressors and nonprogressors benefit from treatment,” she noted.
The number of serious adverse events was the same between the groups and adverse events were as expected from methotrexate.
Dr. Krijbolder said, “the results are encouraging and will open up a new treatment landscape in pre-RA at the future, but at the moment it is too early to give recommendations for clinical practice; we definitely do not want to advocate the start of treatment in all at-risk individuals from now on.”
More research should unravel the mechanisms within the joint that contribute to the development of clinical arthritis and disease chronicity, she said. “If we understand these, we may be able to use more targeted interventions in the future and prevent the development of clinical arthritis all together.
“We are also looking forward to learning more about the long-term beneficial effects of this early treatment in our ongoing observational extension of the trial.”
Hendrik Schulze-Koops, MD, of Ludwig-Maximilians-University of Munich, who moderated the session, asked Dr. Krijbolder, “As well as giving methotrexate to the participants in the treatment group, you also gave a single glucocorticoid injection at baseline, and a placebo injection in the placebo group, can you comment on that?”
Dr. Krijbolder replied that by the first study visit of 4 months, methotrexate would have already started working, and as such from her data it was not possible to distinguish what effect arose from the Depo Medrol injection, and what was from the methotrexate.
“Maybe there even is a synergetic effect, meaning that the two medications together work even better. To learn more about this would require a novel trial with a study design that would, for example, collect data quickly after the injection, for example after 2-4 weeks, because than the effect of the methotrexate would still be limited, or, of course, a novel trial with a treatment arm that only consists of a glucocorticoid injection,” she added.
No conflicts of interest were declared.
COPENHAGEN – Temporary methotrexate in clinically suspected arthralgia delays but does not prevent clinical arthritis development; however, it does lead to sustained reduction of disease burden and MRI-detected inflammation in all at-risk groups, shows the 2-year Treat Earlier study.
“These data provide the first evidence for disease modification when intervening in ‘pre-RA [rheumatoid arthritis]’ or arthralgia,” said Doortje Krijbolder, MD, of Leiden (the Netherlands) University Medical Center, who presented her study at the annual European Congress of Rheumatology.
The randomized, double-blind, study aimed to find out if giving methotrexate in the pre-arthritis phase of arthralgia (with subclinical joint inflammation) prevents the development of clinical arthritis or reduces the burden of disease.
“This is the first trial that aims to reduce the burden of disease, and as such, in pre-RA, it is important that disease modification is sustained after temporary treatment otherwise patients will start regressing with disease activity,” said Dr. Krijbolder.
She explained that methotrexate is usually initiated as first-line treatment when arthritis becomes clinically apparent with joint swelling, but “disease processes begin long before this, and only become clinically recognizable when patients develop symptoms.”
Clinically detectable arthritis development
All 236 patients included in the study had arthralgia of the small joints that, because of the character of the symptoms, was found clinically suspect for progression to RA over time.
“Importantly, these participants had not yet developed clinical arthritis that could be detected on physical joint examination, and were clinically suspected of progressing to RA. They had all undergone an MRI and subclinical joint-inflammation had been detected that was more than prevalent in symptom-free controls,” said Dr. Krijbolder.
Patients were randomized (1:1) to either a single intramuscular glucocorticoid injection (120 mg methylprednisolone [Depo Medrol]) and a 1-year course of oral methotrexate (up to 25 mg/week), or to placebo injection and placebo tablets, and were then followed for a further year without medication to see whether disease progressed.
Treatment and placebo groups were matched with an average age of 46-47 years, 62%-68% were women, they had had symptoms (joint pain) for 27-28 weeks, C-reactive protein was increased in 27%-30%, and 20%-26% were anti-citrullinated protein autoantibody (ACPA) positive.
The primary endpoint was the development of clinically detectable arthritis (fulfilling the 2010 RA-criteria or involving ≥ 2 joints) that persisted for at least 2 weeks. The main secondary endpoints were related to disease burden, including patient-reported physical functioning, along with symptoms and workability (presenteeism at work – the percentage of productivity lost caused by the joint complaints), and measured every 4 months, said Dr. Krijbolder.
She and her colleagues also followed the course of MRI-detected inflammation, which comprised the sum of tenosynovitis, synovitis, and osteitis scored with the RA-MRI Scoring (RAMRIS) method.
Analysis was carried out on an intention-to-treat basis, and two prespecified subgroup analyses were also performed to obtain a better understanding of the effect of methotrexate and glucocorticoids in participants with high risk of clinical arthritis development (positive predictive value (PPV) ≥ 70%), and in patients stratified for ACPA status.
Delays but does not prevent
There was no difference between treatment and placebo groups in the development of persistent clinical arthritis over 2 years (80% vs. 82%, hazard ratio [HR] 0.81; 95% confidence interval [CI], 0.45, 1.48]); however, in the high-risk group subanalysis, 67% in the placebo group developed persistent clinical arthritis. For the treatment group, 7%developed persistent clinical arthritis at 6 months, 27% at 12 months, 40% at 18 months, and 67% at 24 months. For the placebo group: 56% developed persistent clinical arthritis at 6 months, and 67% at 12 months, 18 months, and 24 months.
“Strikingly, in the treatment group there was a statistically significant difference between 6 and 12 months, but in year 2, this difference disappeared, suggesting a delayed arthritis development but no prevention,” said Dr. Krijbolder.
Persistent clinical arthritis became similar at 24 months, at 67% in both groups. A similar, but less pronounced, delaying effect was seen with the ACPA-positive patients, with 48% and 52% developing persistent clinical arthritis at 24 months.
In joint pain, there was a decline in the treatment group compared with the placebo group and this persisted over 2 years (–9 on scale of 0 to 100: (95%CI, –12,–4; P < .001), and a similar effect was seen in high-risk and ACPA subgroups, reported Dr. Krijbolder.
Physical functioning improved more in the treatment-group compared with the placebo group during the first months and remained better (mean between-group difference over 2 years HAQ [health assessment questionnaire] –0.1 [–0.2, –0.03; P = .004]), and morning stiffness (–12 [95%CI, –16, –8; P < .001]), and presenteeism (–8% [95%CI, –13%, –3%; P = .001]) also showed improvement over time compared with placebo.
MRI-detected joint-inflammation was also persistently improved with a mean difference over 2 years –1.4 points (95%CI, –2.0, –0.9; P < .001). “As we know that symptoms and functional impairments are associated with MRI-detected joint inflammation, it was not surprising that treatment induced a decline in joint inflammation that persisted over time, also after the stop of the treatment in the second year,” explained Dr. Krijbolder.
In the high-risk subgroup, as well as in both ACPA-positive and ACPA-negative participants, a comparable statistically significant decline in MRI-detected inflammation was found.
“It may seem counterintuitive that on the one hand we found a delaying effect of treatment on persistent clinical arthritis but no prevention, while on the other, we saw a sustained treatment effect on MRI-detected joint-inflammation and related symptoms and functional impairments,” added Dr. Krijbolder.
To help understand this, the researchers performed a post hoc analysis in high-risk participants, comparing those who did not progress with those who did progress to arthritis. “Both progressors and nonprogressors showed a sustained treatment effect for pain and MRI-detected joint-inflammation, and in nonprogressors, there was almost a complete relief of pain and they nearly returned to the normal range of MRI-detected joint-inflammation as seen in symptom-free controls,” reported Dr. Krijbolder.
“In those who progressed to arthritis, there was less pain and less MRI-detected joint inflammation in the treatment group, but also at the time when they developed clinical arthritis. So both progressors and nonprogressors benefit from treatment,” she noted.
The number of serious adverse events was the same between the groups and adverse events were as expected from methotrexate.
Dr. Krijbolder said, “the results are encouraging and will open up a new treatment landscape in pre-RA at the future, but at the moment it is too early to give recommendations for clinical practice; we definitely do not want to advocate the start of treatment in all at-risk individuals from now on.”
More research should unravel the mechanisms within the joint that contribute to the development of clinical arthritis and disease chronicity, she said. “If we understand these, we may be able to use more targeted interventions in the future and prevent the development of clinical arthritis all together.
“We are also looking forward to learning more about the long-term beneficial effects of this early treatment in our ongoing observational extension of the trial.”
Hendrik Schulze-Koops, MD, of Ludwig-Maximilians-University of Munich, who moderated the session, asked Dr. Krijbolder, “As well as giving methotrexate to the participants in the treatment group, you also gave a single glucocorticoid injection at baseline, and a placebo injection in the placebo group, can you comment on that?”
Dr. Krijbolder replied that by the first study visit of 4 months, methotrexate would have already started working, and as such from her data it was not possible to distinguish what effect arose from the Depo Medrol injection, and what was from the methotrexate.
“Maybe there even is a synergetic effect, meaning that the two medications together work even better. To learn more about this would require a novel trial with a study design that would, for example, collect data quickly after the injection, for example after 2-4 weeks, because than the effect of the methotrexate would still be limited, or, of course, a novel trial with a treatment arm that only consists of a glucocorticoid injection,” she added.
No conflicts of interest were declared.
COPENHAGEN – Temporary methotrexate in clinically suspected arthralgia delays but does not prevent clinical arthritis development; however, it does lead to sustained reduction of disease burden and MRI-detected inflammation in all at-risk groups, shows the 2-year Treat Earlier study.
“These data provide the first evidence for disease modification when intervening in ‘pre-RA [rheumatoid arthritis]’ or arthralgia,” said Doortje Krijbolder, MD, of Leiden (the Netherlands) University Medical Center, who presented her study at the annual European Congress of Rheumatology.
The randomized, double-blind, study aimed to find out if giving methotrexate in the pre-arthritis phase of arthralgia (with subclinical joint inflammation) prevents the development of clinical arthritis or reduces the burden of disease.
“This is the first trial that aims to reduce the burden of disease, and as such, in pre-RA, it is important that disease modification is sustained after temporary treatment otherwise patients will start regressing with disease activity,” said Dr. Krijbolder.
She explained that methotrexate is usually initiated as first-line treatment when arthritis becomes clinically apparent with joint swelling, but “disease processes begin long before this, and only become clinically recognizable when patients develop symptoms.”
Clinically detectable arthritis development
All 236 patients included in the study had arthralgia of the small joints that, because of the character of the symptoms, was found clinically suspect for progression to RA over time.
“Importantly, these participants had not yet developed clinical arthritis that could be detected on physical joint examination, and were clinically suspected of progressing to RA. They had all undergone an MRI and subclinical joint-inflammation had been detected that was more than prevalent in symptom-free controls,” said Dr. Krijbolder.
Patients were randomized (1:1) to either a single intramuscular glucocorticoid injection (120 mg methylprednisolone [Depo Medrol]) and a 1-year course of oral methotrexate (up to 25 mg/week), or to placebo injection and placebo tablets, and were then followed for a further year without medication to see whether disease progressed.
Treatment and placebo groups were matched with an average age of 46-47 years, 62%-68% were women, they had had symptoms (joint pain) for 27-28 weeks, C-reactive protein was increased in 27%-30%, and 20%-26% were anti-citrullinated protein autoantibody (ACPA) positive.
The primary endpoint was the development of clinically detectable arthritis (fulfilling the 2010 RA-criteria or involving ≥ 2 joints) that persisted for at least 2 weeks. The main secondary endpoints were related to disease burden, including patient-reported physical functioning, along with symptoms and workability (presenteeism at work – the percentage of productivity lost caused by the joint complaints), and measured every 4 months, said Dr. Krijbolder.
She and her colleagues also followed the course of MRI-detected inflammation, which comprised the sum of tenosynovitis, synovitis, and osteitis scored with the RA-MRI Scoring (RAMRIS) method.
Analysis was carried out on an intention-to-treat basis, and two prespecified subgroup analyses were also performed to obtain a better understanding of the effect of methotrexate and glucocorticoids in participants with high risk of clinical arthritis development (positive predictive value (PPV) ≥ 70%), and in patients stratified for ACPA status.
Delays but does not prevent
There was no difference between treatment and placebo groups in the development of persistent clinical arthritis over 2 years (80% vs. 82%, hazard ratio [HR] 0.81; 95% confidence interval [CI], 0.45, 1.48]); however, in the high-risk group subanalysis, 67% in the placebo group developed persistent clinical arthritis. For the treatment group, 7%developed persistent clinical arthritis at 6 months, 27% at 12 months, 40% at 18 months, and 67% at 24 months. For the placebo group: 56% developed persistent clinical arthritis at 6 months, and 67% at 12 months, 18 months, and 24 months.
“Strikingly, in the treatment group there was a statistically significant difference between 6 and 12 months, but in year 2, this difference disappeared, suggesting a delayed arthritis development but no prevention,” said Dr. Krijbolder.
Persistent clinical arthritis became similar at 24 months, at 67% in both groups. A similar, but less pronounced, delaying effect was seen with the ACPA-positive patients, with 48% and 52% developing persistent clinical arthritis at 24 months.
In joint pain, there was a decline in the treatment group compared with the placebo group and this persisted over 2 years (–9 on scale of 0 to 100: (95%CI, –12,–4; P < .001), and a similar effect was seen in high-risk and ACPA subgroups, reported Dr. Krijbolder.
Physical functioning improved more in the treatment-group compared with the placebo group during the first months and remained better (mean between-group difference over 2 years HAQ [health assessment questionnaire] –0.1 [–0.2, –0.03; P = .004]), and morning stiffness (–12 [95%CI, –16, –8; P < .001]), and presenteeism (–8% [95%CI, –13%, –3%; P = .001]) also showed improvement over time compared with placebo.
MRI-detected joint-inflammation was also persistently improved with a mean difference over 2 years –1.4 points (95%CI, –2.0, –0.9; P < .001). “As we know that symptoms and functional impairments are associated with MRI-detected joint inflammation, it was not surprising that treatment induced a decline in joint inflammation that persisted over time, also after the stop of the treatment in the second year,” explained Dr. Krijbolder.
In the high-risk subgroup, as well as in both ACPA-positive and ACPA-negative participants, a comparable statistically significant decline in MRI-detected inflammation was found.
“It may seem counterintuitive that on the one hand we found a delaying effect of treatment on persistent clinical arthritis but no prevention, while on the other, we saw a sustained treatment effect on MRI-detected joint-inflammation and related symptoms and functional impairments,” added Dr. Krijbolder.
To help understand this, the researchers performed a post hoc analysis in high-risk participants, comparing those who did not progress with those who did progress to arthritis. “Both progressors and nonprogressors showed a sustained treatment effect for pain and MRI-detected joint-inflammation, and in nonprogressors, there was almost a complete relief of pain and they nearly returned to the normal range of MRI-detected joint-inflammation as seen in symptom-free controls,” reported Dr. Krijbolder.
“In those who progressed to arthritis, there was less pain and less MRI-detected joint inflammation in the treatment group, but also at the time when they developed clinical arthritis. So both progressors and nonprogressors benefit from treatment,” she noted.
The number of serious adverse events was the same between the groups and adverse events were as expected from methotrexate.
Dr. Krijbolder said, “the results are encouraging and will open up a new treatment landscape in pre-RA at the future, but at the moment it is too early to give recommendations for clinical practice; we definitely do not want to advocate the start of treatment in all at-risk individuals from now on.”
More research should unravel the mechanisms within the joint that contribute to the development of clinical arthritis and disease chronicity, she said. “If we understand these, we may be able to use more targeted interventions in the future and prevent the development of clinical arthritis all together.
“We are also looking forward to learning more about the long-term beneficial effects of this early treatment in our ongoing observational extension of the trial.”
Hendrik Schulze-Koops, MD, of Ludwig-Maximilians-University of Munich, who moderated the session, asked Dr. Krijbolder, “As well as giving methotrexate to the participants in the treatment group, you also gave a single glucocorticoid injection at baseline, and a placebo injection in the placebo group, can you comment on that?”
Dr. Krijbolder replied that by the first study visit of 4 months, methotrexate would have already started working, and as such from her data it was not possible to distinguish what effect arose from the Depo Medrol injection, and what was from the methotrexate.
“Maybe there even is a synergetic effect, meaning that the two medications together work even better. To learn more about this would require a novel trial with a study design that would, for example, collect data quickly after the injection, for example after 2-4 weeks, because than the effect of the methotrexate would still be limited, or, of course, a novel trial with a treatment arm that only consists of a glucocorticoid injection,” she added.
No conflicts of interest were declared.
AT THE EULAR 2022 CONGRESS
High maternal, fetal morbidity rates in SLE pregnancies
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
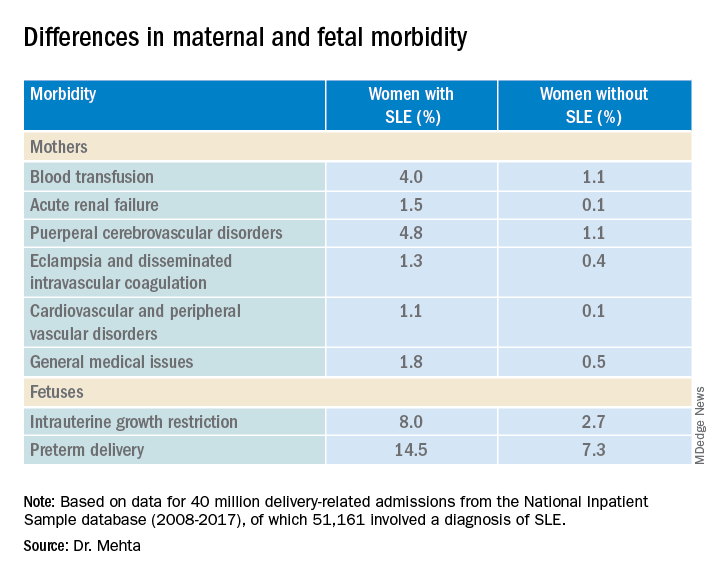
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
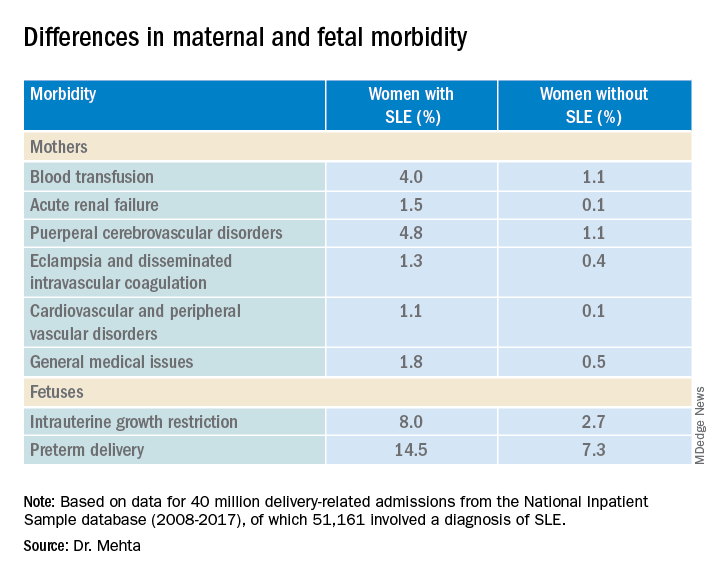
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COPENHAGEN – Pregnant women with systemic lupus erythematosus (SLE) are at significantly higher risk of requiring transfusion, developing a cerebrovascular disorder, or developing acute renal failure than pregnant women without SLE, a review of data from an American national sample indicates.
Pregnant women with SLE also have a twofold-higher risk for premature delivery, and a threefold risk of having a fetus with intrauterine growth restriction than their pregnant counterparts without SLE, reported Bella Mehta, MBBS, MS, MD, a rheumatologist at the Hospital for Special Surgery in New York.
“Severe maternal morbidity and fetal morbidity still remain high, but this work can help inform physicians and counsel patients for pregnancy planning and management,” she said at the annual European Congress of Rheumatology.
Although in-hospital maternal and fetal mortality rates for women with SLE have declined over the past 2 decades, the same cannot be said for morbidities, prompting the investigators to conduct a study to determine the proportion of fetal and maternal morbidity in SLE deliveries, compared with non-SLE deliveries over a decade.
Inpatient Sample
Dr. Mehta and colleagues studied retrospective data on 40 million delivery-related admissions from the National Inpatient Sample database. Of these patients, 51,161 had a diagnosis of SLE.
They identified all delivery-related hospital admissions for patients with and without SLE from 2008 through 2017 using diagnostic codes.
The researchers looked at fetal morbidity indicators, including preterm delivery and intrauterine growth restriction, and used the Centers for Disease Control and Prevention standard definition of severe maternal morbidity as “unexpected outcomes of labor and delivery that result in significant short- or long- term consequences to a woman’s health.”
They identified 21 severe maternal morbidity outcomes, including blood transfusion requirements, acute renal failure, eclampsia and disseminated intravascular coagulation, cardiovascular and peripheral vascular disorders, and general medical issues (hysterectomy, shock, sepsis, adult respiratory distress syndrome, severe anesthesia complications, temporary tracheostomy, and ventilation).
Study results
Women with SLE were slightly older at the time of delivery (mean age, 30.05 vs. 29.19 years) and had more comorbidities, according to the Elixhauser Comorbidity Scale, with 97.84% of women in this group having one to four comorbidities, compared with 19.4% of women without SLE.
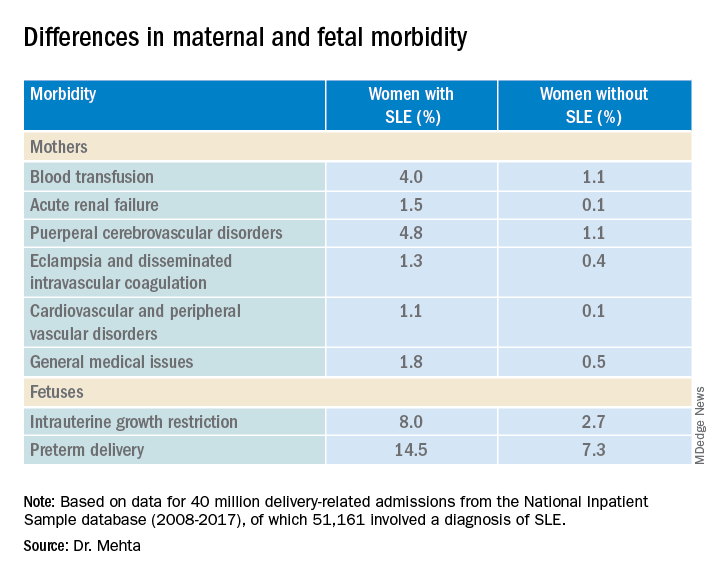
Dr. Mehta acknowledged that the study was limited by the inability to capture outpatient deliveries, although she noted that only about 1.3% of deliveries in the United States occur outside the inpatient setting.
In addition, she noted that the database does not include information on lupus disease activity, Apgar scores, SLE flares, the presence of nephritis, antiphospholipid or anti-Ro/SSA antibodies, or medication use.
A rheumatologist who was not involved in the study said in an interview that the data from this study are in line with those in other recently published studies.
“The problem is that these data were not corrected for further disease activity or drugs,” said Frauke Förger, MD, professor of rheumatology and immunology at the University of Bern (Switzerland), who comoderated the oral abstract session where the data were presented.
She said prospective studies that adjusted for factors such as SLE disease activity and medication use will be required to give clinicians a better understanding of how to manage pregnancies in women with SLE.
The study was supported by an award from Weill Cornell Medicine. Dr. Mehta and Dr. Förger reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
AT THE EULAR 2022 CONGRESS
EULAR recommends starting methotrexate and glucocorticoids in RA management
COPENHAGEN – New recommendations for the management of rheumatoid arthritis from the European Alliance of Associations for Rheumatology suggest starting short-term methotrexate and glucocorticoids when starting or changing conventional synthetic disease-modifying antirheumatic drugs (DMARDs), although rapid glucocorticoid dose reduction and discontinuation is also emphasized.
“In this respect we are at odds with the American College of Rheumatology guideline,” said Josef S. Smolen, MD, professor of internal medicine at the Medical University of Vienna, who presented the update at the annual European Congress of Rheumatology.
More evidence supports the recommendation to start methotrexate plus glucocorticoids since this is not surpassed by several biologic DMARDs (bDMARDs) plus methotrexate, said Dr. Smolen, who spoke on behalf of his coauthors, Robert Landewe, MD, PhD, from Amsterdam Rheumatology and Clinical Immunology Center, and the rest of the Global Task Force for the 2022 Update of the EULAR RA-Management Recommendations.
In addition, “JAK [Janus kinase] inhibitors are now only recommended for patients who do not have risk factors for cardiovascular or malignant diseases, but otherwise they remain on the same level [phase 2] as bDMARDS,” he said.
“Registries hitherto do not observe what is reported in the ORAL Surveillance randomized controlled trial [RCT],” but, he added, “RCTs are the decisive studies and we await the baricitinib data on a similar population at risk.”
Dr. Smolen also noted that the ENTRACTE trial comparing tocilizumab with tumor necrosis factor (TNF)–alpha inhibitors did not report similar data as ORAL Surveillance.
“Tapering b/ts [biologic/targeted synthetic] and cs [conventional synthetic] DMARDs in sustained remission have been brought together with the need to discontinue glucocorticoids before other drugs are tapered has been more strongly emphasized,” he explained.
Most of the recommendations from the 2019 update remain unchanged, including all five overarching principles and 6 of the 12 individual items.
Rheumatologist Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, joined the meeting remotely and commented on the working draft of the treatment recommendations. “While much was retained from the previous version, there were several important updates,” he said. “Regarding the use of steroids, it is recommended that when they are used, they should be stopped as soon as possible. Regarding jakinibs, which EULAR considers as a class, they recommended consideration of risk factors for MACE events prior to their utilization,” he said.
Methotrexate plus glucocorticoids (Recommendation 6)
In recent years, many recommendations have suggested combining methotrexate with glucocorticoids as a first-treatment strategy upon diagnosis of RA, said Dr. Smolen, and initially “guidance from the ACR was in agreement.”
In 2021, however, “the ACR published a paper, albeit with a very low level of evidence, that one should not primarily use a combination of methotrexate plus glucocorticoids,” he added, with an emphasis on the “very low level of evidence.”
“Some people on the task force even interpreted it as being in favor of using expensive drugs,” he explained. “This needed to be addressed in the 2022 update.”
The global task force wanted to look further at the benefit-to-risk ratio, despite it being discussed in the 2019 recommendations. “We wanted to check that short-term use of glucocorticoids was not associated with major risks,” said Dr. Smolen. “Glucocorticoids are not used for a long time if used as a bridging therapy. We felt we had to more clearly define what we meant by short term.”
A systematic review of around 7,000 papers, led to consideration of 10 unique studies. “One study published a few years ago in PLOS One, did not find any evidence of increased cardiovascular risk,” Dr. Smolen reported, “however, use of over 1,000 mg of glucocorticoid was associated with a trend for high cardiovascular risk.”
“This trend was confirmed by data from the CorEvitas registry, which shows that up to 1,100 mg of cumulative dose was associated with no increased risk, but above this with increasing dose there was an increased and significant risk,” he added.
When the task force looked at trials that mandated and prespecified a reduction and stopping of glucocorticoids, they found less than 10% persistence of glucocorticoids at 12 months in all trials, some even reduced use to zero.
Dr. Smolen and colleagues also looked at data from the NORD-STAR trial, that compared methotrexate and glucocorticoids with methotrexate and three bDMARDs, namely an anti-TNF inhibitor, certolizumab pegol; anti–co-stimulation, abatacept; and an anti–interleukin-6 receptor, tocilizumab.
“These data prove the validity of the EULAR RA management recommendations regarding the unsurpassed benefit of methotrexate plus glucocorticoids in early RA,” Dr. Smolen said.
“This is confirmation of efficacy and that if you induce tapering and stopping it is not dangerous,” he added. “The level of evidence was very high, and it is the highest level of agreement we have had for any glucocorticoid recommendation over recent years.”
As such, Recommendation 6 says that shortening glucocorticoids should be considered when initiating or changing csDMARDS, in different dose regimens and routes of administration, but should be tapered and discontinued as rapidly as clinically feasible.
JAK inhibitor placed relative to DMARDs (Recommendation 10)
A paper published in the New England Journal of Medicine suggested cardiovascular risks and malignancy risks were higher with the JAK inhibitor, tofacitinib, compared with TNF-alpha inhibitors.
The task force therefore felt the need to evaluate the place of JAK inhibitors next to biologic DMARDs “once phase one with methotrexate plus glucocorticoids has failed,” Dr. Smolen said.
After a systematic literature review of around 4,500 papers, the researchers evaluated 88 safety papers including the ORAL Surveillance study. “This very clearly showed that tocilizumab was not noninferior according to the noninferiority criteria with an upper limit of 1.8 [hazard ratio] and this was independent of dose, compared with TNF-alpha inhibitor,” said Dr. Smolen. “The major adverse cardiovascular events [MACE] were not different, nor were malignancies and overall mortality.”
Dr. Smolen also referred to the ENTRACTE trial that compared etanercept with tocilizumab, and again, there was no evidence of an increased risk of MACE nor mortality for tocilizumab compared with a TNF-alpha inhibitor.
“The increased MACE risk in the ORAL Surveillance trial is unlikely due to inhibition of IL-6 and must be due to some other effects than IL-6 signaling,” he said.
As such, the agreed-on recommendation was that, “if the treatment target is not achieved with the first csDMARD strategy, when poor prognostic factors are present, a bDMARD should be added; JAK inhibitors may be considered but pertinent risk factors must be taken into account [aged over 65 years, history of current or past smoking, either cardiovascular or malignancy risk factors, and risk factors for thromboembolic events].”
There was a high level of agreement by the group for this recommendation.
Switching DMARDs
The task force considered their recommendations on switching DMARDs based on a systematic literature review of 47 papers.
EULAR previously strongly recommended a combination of csDMARDs with bDMARDs (including JAK inhibitors), and this recommendation remains the same except for a note added about risks of tsDMARDs.
Recommendation 10 relates to failure of phase 2 treatment and what to do when the first bDMARD or a tsDMARD has failed (including as per new recommendations, a JAK inhibitor), and if one TNF or IL-6 receptor inhibitor therapy has failed. In this case, patients may receive an agent with another mode of action or a second TNF/IL-6 receptor inhibitor, said Dr. Smolen.
Recommendation 11 has been combined with recommendation 12, he added. “If a patient is in persistent remission after having tapered glucocorticoids, one can consider tapering bDMARDs, or tsDMARDs especially if this treatment is combined with a csDMARD.
“We decided to put more emphasis on the stopping of glucocorticoids, namely not saying ‘tapering’ but ‘discontinued,’ and if the patient is in sustained remission, then consider reduction of DMARDs [biologic, targeted synthetic or conventional synthetic DMARDs],” he explained. “This is left to the discretion of the patient and the physician as to which one should be tapered first. We don’t recommend to taper everything because the patient might be affected by flares but this needs further discussion.”
Dr. Smolen ended his presentation by looking ahead to the next set of recommendations: “With the current rate of evidence development, we expect an update of the recommendations to be necessary in about 3-4 years.”
This article was updated on 6/9/2022.
COPENHAGEN – New recommendations for the management of rheumatoid arthritis from the European Alliance of Associations for Rheumatology suggest starting short-term methotrexate and glucocorticoids when starting or changing conventional synthetic disease-modifying antirheumatic drugs (DMARDs), although rapid glucocorticoid dose reduction and discontinuation is also emphasized.
“In this respect we are at odds with the American College of Rheumatology guideline,” said Josef S. Smolen, MD, professor of internal medicine at the Medical University of Vienna, who presented the update at the annual European Congress of Rheumatology.
More evidence supports the recommendation to start methotrexate plus glucocorticoids since this is not surpassed by several biologic DMARDs (bDMARDs) plus methotrexate, said Dr. Smolen, who spoke on behalf of his coauthors, Robert Landewe, MD, PhD, from Amsterdam Rheumatology and Clinical Immunology Center, and the rest of the Global Task Force for the 2022 Update of the EULAR RA-Management Recommendations.
In addition, “JAK [Janus kinase] inhibitors are now only recommended for patients who do not have risk factors for cardiovascular or malignant diseases, but otherwise they remain on the same level [phase 2] as bDMARDS,” he said.
“Registries hitherto do not observe what is reported in the ORAL Surveillance randomized controlled trial [RCT],” but, he added, “RCTs are the decisive studies and we await the baricitinib data on a similar population at risk.”
Dr. Smolen also noted that the ENTRACTE trial comparing tocilizumab with tumor necrosis factor (TNF)–alpha inhibitors did not report similar data as ORAL Surveillance.
“Tapering b/ts [biologic/targeted synthetic] and cs [conventional synthetic] DMARDs in sustained remission have been brought together with the need to discontinue glucocorticoids before other drugs are tapered has been more strongly emphasized,” he explained.
Most of the recommendations from the 2019 update remain unchanged, including all five overarching principles and 6 of the 12 individual items.
Rheumatologist Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, joined the meeting remotely and commented on the working draft of the treatment recommendations. “While much was retained from the previous version, there were several important updates,” he said. “Regarding the use of steroids, it is recommended that when they are used, they should be stopped as soon as possible. Regarding jakinibs, which EULAR considers as a class, they recommended consideration of risk factors for MACE events prior to their utilization,” he said.
Methotrexate plus glucocorticoids (Recommendation 6)
In recent years, many recommendations have suggested combining methotrexate with glucocorticoids as a first-treatment strategy upon diagnosis of RA, said Dr. Smolen, and initially “guidance from the ACR was in agreement.”
In 2021, however, “the ACR published a paper, albeit with a very low level of evidence, that one should not primarily use a combination of methotrexate plus glucocorticoids,” he added, with an emphasis on the “very low level of evidence.”
“Some people on the task force even interpreted it as being in favor of using expensive drugs,” he explained. “This needed to be addressed in the 2022 update.”
The global task force wanted to look further at the benefit-to-risk ratio, despite it being discussed in the 2019 recommendations. “We wanted to check that short-term use of glucocorticoids was not associated with major risks,” said Dr. Smolen. “Glucocorticoids are not used for a long time if used as a bridging therapy. We felt we had to more clearly define what we meant by short term.”
A systematic review of around 7,000 papers, led to consideration of 10 unique studies. “One study published a few years ago in PLOS One, did not find any evidence of increased cardiovascular risk,” Dr. Smolen reported, “however, use of over 1,000 mg of glucocorticoid was associated with a trend for high cardiovascular risk.”
“This trend was confirmed by data from the CorEvitas registry, which shows that up to 1,100 mg of cumulative dose was associated with no increased risk, but above this with increasing dose there was an increased and significant risk,” he added.
When the task force looked at trials that mandated and prespecified a reduction and stopping of glucocorticoids, they found less than 10% persistence of glucocorticoids at 12 months in all trials, some even reduced use to zero.
Dr. Smolen and colleagues also looked at data from the NORD-STAR trial, that compared methotrexate and glucocorticoids with methotrexate and three bDMARDs, namely an anti-TNF inhibitor, certolizumab pegol; anti–co-stimulation, abatacept; and an anti–interleukin-6 receptor, tocilizumab.
“These data prove the validity of the EULAR RA management recommendations regarding the unsurpassed benefit of methotrexate plus glucocorticoids in early RA,” Dr. Smolen said.
“This is confirmation of efficacy and that if you induce tapering and stopping it is not dangerous,” he added. “The level of evidence was very high, and it is the highest level of agreement we have had for any glucocorticoid recommendation over recent years.”
As such, Recommendation 6 says that shortening glucocorticoids should be considered when initiating or changing csDMARDS, in different dose regimens and routes of administration, but should be tapered and discontinued as rapidly as clinically feasible.
JAK inhibitor placed relative to DMARDs (Recommendation 10)
A paper published in the New England Journal of Medicine suggested cardiovascular risks and malignancy risks were higher with the JAK inhibitor, tofacitinib, compared with TNF-alpha inhibitors.
The task force therefore felt the need to evaluate the place of JAK inhibitors next to biologic DMARDs “once phase one with methotrexate plus glucocorticoids has failed,” Dr. Smolen said.
After a systematic literature review of around 4,500 papers, the researchers evaluated 88 safety papers including the ORAL Surveillance study. “This very clearly showed that tocilizumab was not noninferior according to the noninferiority criteria with an upper limit of 1.8 [hazard ratio] and this was independent of dose, compared with TNF-alpha inhibitor,” said Dr. Smolen. “The major adverse cardiovascular events [MACE] were not different, nor were malignancies and overall mortality.”
Dr. Smolen also referred to the ENTRACTE trial that compared etanercept with tocilizumab, and again, there was no evidence of an increased risk of MACE nor mortality for tocilizumab compared with a TNF-alpha inhibitor.
“The increased MACE risk in the ORAL Surveillance trial is unlikely due to inhibition of IL-6 and must be due to some other effects than IL-6 signaling,” he said.
As such, the agreed-on recommendation was that, “if the treatment target is not achieved with the first csDMARD strategy, when poor prognostic factors are present, a bDMARD should be added; JAK inhibitors may be considered but pertinent risk factors must be taken into account [aged over 65 years, history of current or past smoking, either cardiovascular or malignancy risk factors, and risk factors for thromboembolic events].”
There was a high level of agreement by the group for this recommendation.
Switching DMARDs
The task force considered their recommendations on switching DMARDs based on a systematic literature review of 47 papers.
EULAR previously strongly recommended a combination of csDMARDs with bDMARDs (including JAK inhibitors), and this recommendation remains the same except for a note added about risks of tsDMARDs.
Recommendation 10 relates to failure of phase 2 treatment and what to do when the first bDMARD or a tsDMARD has failed (including as per new recommendations, a JAK inhibitor), and if one TNF or IL-6 receptor inhibitor therapy has failed. In this case, patients may receive an agent with another mode of action or a second TNF/IL-6 receptor inhibitor, said Dr. Smolen.
Recommendation 11 has been combined with recommendation 12, he added. “If a patient is in persistent remission after having tapered glucocorticoids, one can consider tapering bDMARDs, or tsDMARDs especially if this treatment is combined with a csDMARD.
“We decided to put more emphasis on the stopping of glucocorticoids, namely not saying ‘tapering’ but ‘discontinued,’ and if the patient is in sustained remission, then consider reduction of DMARDs [biologic, targeted synthetic or conventional synthetic DMARDs],” he explained. “This is left to the discretion of the patient and the physician as to which one should be tapered first. We don’t recommend to taper everything because the patient might be affected by flares but this needs further discussion.”
Dr. Smolen ended his presentation by looking ahead to the next set of recommendations: “With the current rate of evidence development, we expect an update of the recommendations to be necessary in about 3-4 years.”
This article was updated on 6/9/2022.
COPENHAGEN – New recommendations for the management of rheumatoid arthritis from the European Alliance of Associations for Rheumatology suggest starting short-term methotrexate and glucocorticoids when starting or changing conventional synthetic disease-modifying antirheumatic drugs (DMARDs), although rapid glucocorticoid dose reduction and discontinuation is also emphasized.
“In this respect we are at odds with the American College of Rheumatology guideline,” said Josef S. Smolen, MD, professor of internal medicine at the Medical University of Vienna, who presented the update at the annual European Congress of Rheumatology.
More evidence supports the recommendation to start methotrexate plus glucocorticoids since this is not surpassed by several biologic DMARDs (bDMARDs) plus methotrexate, said Dr. Smolen, who spoke on behalf of his coauthors, Robert Landewe, MD, PhD, from Amsterdam Rheumatology and Clinical Immunology Center, and the rest of the Global Task Force for the 2022 Update of the EULAR RA-Management Recommendations.
In addition, “JAK [Janus kinase] inhibitors are now only recommended for patients who do not have risk factors for cardiovascular or malignant diseases, but otherwise they remain on the same level [phase 2] as bDMARDS,” he said.
“Registries hitherto do not observe what is reported in the ORAL Surveillance randomized controlled trial [RCT],” but, he added, “RCTs are the decisive studies and we await the baricitinib data on a similar population at risk.”
Dr. Smolen also noted that the ENTRACTE trial comparing tocilizumab with tumor necrosis factor (TNF)–alpha inhibitors did not report similar data as ORAL Surveillance.
“Tapering b/ts [biologic/targeted synthetic] and cs [conventional synthetic] DMARDs in sustained remission have been brought together with the need to discontinue glucocorticoids before other drugs are tapered has been more strongly emphasized,” he explained.
Most of the recommendations from the 2019 update remain unchanged, including all five overarching principles and 6 of the 12 individual items.
Rheumatologist Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, joined the meeting remotely and commented on the working draft of the treatment recommendations. “While much was retained from the previous version, there were several important updates,” he said. “Regarding the use of steroids, it is recommended that when they are used, they should be stopped as soon as possible. Regarding jakinibs, which EULAR considers as a class, they recommended consideration of risk factors for MACE events prior to their utilization,” he said.
Methotrexate plus glucocorticoids (Recommendation 6)
In recent years, many recommendations have suggested combining methotrexate with glucocorticoids as a first-treatment strategy upon diagnosis of RA, said Dr. Smolen, and initially “guidance from the ACR was in agreement.”
In 2021, however, “the ACR published a paper, albeit with a very low level of evidence, that one should not primarily use a combination of methotrexate plus glucocorticoids,” he added, with an emphasis on the “very low level of evidence.”
“Some people on the task force even interpreted it as being in favor of using expensive drugs,” he explained. “This needed to be addressed in the 2022 update.”
The global task force wanted to look further at the benefit-to-risk ratio, despite it being discussed in the 2019 recommendations. “We wanted to check that short-term use of glucocorticoids was not associated with major risks,” said Dr. Smolen. “Glucocorticoids are not used for a long time if used as a bridging therapy. We felt we had to more clearly define what we meant by short term.”
A systematic review of around 7,000 papers, led to consideration of 10 unique studies. “One study published a few years ago in PLOS One, did not find any evidence of increased cardiovascular risk,” Dr. Smolen reported, “however, use of over 1,000 mg of glucocorticoid was associated with a trend for high cardiovascular risk.”
“This trend was confirmed by data from the CorEvitas registry, which shows that up to 1,100 mg of cumulative dose was associated with no increased risk, but above this with increasing dose there was an increased and significant risk,” he added.
When the task force looked at trials that mandated and prespecified a reduction and stopping of glucocorticoids, they found less than 10% persistence of glucocorticoids at 12 months in all trials, some even reduced use to zero.
Dr. Smolen and colleagues also looked at data from the NORD-STAR trial, that compared methotrexate and glucocorticoids with methotrexate and three bDMARDs, namely an anti-TNF inhibitor, certolizumab pegol; anti–co-stimulation, abatacept; and an anti–interleukin-6 receptor, tocilizumab.
“These data prove the validity of the EULAR RA management recommendations regarding the unsurpassed benefit of methotrexate plus glucocorticoids in early RA,” Dr. Smolen said.
“This is confirmation of efficacy and that if you induce tapering and stopping it is not dangerous,” he added. “The level of evidence was very high, and it is the highest level of agreement we have had for any glucocorticoid recommendation over recent years.”
As such, Recommendation 6 says that shortening glucocorticoids should be considered when initiating or changing csDMARDS, in different dose regimens and routes of administration, but should be tapered and discontinued as rapidly as clinically feasible.
JAK inhibitor placed relative to DMARDs (Recommendation 10)
A paper published in the New England Journal of Medicine suggested cardiovascular risks and malignancy risks were higher with the JAK inhibitor, tofacitinib, compared with TNF-alpha inhibitors.
The task force therefore felt the need to evaluate the place of JAK inhibitors next to biologic DMARDs “once phase one with methotrexate plus glucocorticoids has failed,” Dr. Smolen said.
After a systematic literature review of around 4,500 papers, the researchers evaluated 88 safety papers including the ORAL Surveillance study. “This very clearly showed that tocilizumab was not noninferior according to the noninferiority criteria with an upper limit of 1.8 [hazard ratio] and this was independent of dose, compared with TNF-alpha inhibitor,” said Dr. Smolen. “The major adverse cardiovascular events [MACE] were not different, nor were malignancies and overall mortality.”
Dr. Smolen also referred to the ENTRACTE trial that compared etanercept with tocilizumab, and again, there was no evidence of an increased risk of MACE nor mortality for tocilizumab compared with a TNF-alpha inhibitor.
“The increased MACE risk in the ORAL Surveillance trial is unlikely due to inhibition of IL-6 and must be due to some other effects than IL-6 signaling,” he said.
As such, the agreed-on recommendation was that, “if the treatment target is not achieved with the first csDMARD strategy, when poor prognostic factors are present, a bDMARD should be added; JAK inhibitors may be considered but pertinent risk factors must be taken into account [aged over 65 years, history of current or past smoking, either cardiovascular or malignancy risk factors, and risk factors for thromboembolic events].”
There was a high level of agreement by the group for this recommendation.
Switching DMARDs
The task force considered their recommendations on switching DMARDs based on a systematic literature review of 47 papers.
EULAR previously strongly recommended a combination of csDMARDs with bDMARDs (including JAK inhibitors), and this recommendation remains the same except for a note added about risks of tsDMARDs.
Recommendation 10 relates to failure of phase 2 treatment and what to do when the first bDMARD or a tsDMARD has failed (including as per new recommendations, a JAK inhibitor), and if one TNF or IL-6 receptor inhibitor therapy has failed. In this case, patients may receive an agent with another mode of action or a second TNF/IL-6 receptor inhibitor, said Dr. Smolen.
Recommendation 11 has been combined with recommendation 12, he added. “If a patient is in persistent remission after having tapered glucocorticoids, one can consider tapering bDMARDs, or tsDMARDs especially if this treatment is combined with a csDMARD.
“We decided to put more emphasis on the stopping of glucocorticoids, namely not saying ‘tapering’ but ‘discontinued,’ and if the patient is in sustained remission, then consider reduction of DMARDs [biologic, targeted synthetic or conventional synthetic DMARDs],” he explained. “This is left to the discretion of the patient and the physician as to which one should be tapered first. We don’t recommend to taper everything because the patient might be affected by flares but this needs further discussion.”
Dr. Smolen ended his presentation by looking ahead to the next set of recommendations: “With the current rate of evidence development, we expect an update of the recommendations to be necessary in about 3-4 years.”
This article was updated on 6/9/2022.
AT THE EULAR 2022 CONGRESS
Updated EULAR recommendations for AAV include new drugs, practices
The
The 2022 revision – which was unveiled at the annual European Congress of Rheumatology – includes guidance on using new drugs, such as avacopan (Tavneos) and mepolizumab (Nucala), as well as revised recommendations on the use of rituximab and glucocorticosteroids.

The overhaul also contains specific recommendations for treating eosinophilic granulomatosis with polyangiitis (EGPA), separating it out from granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) for the first time.
“Until now, EGPA has usually been managed in the same way as [the] other diseases,” Bernhard Hellmich, MD, of the University of Tübingen (Germany) said in an interview ahead of his presentation at the congress.
“But we now have data on each type specifically, so there is good reason to make separate recommendations,” he added.
Indeed, so much new data has become available in the past few years there are only three recommendations that remain unchanged from the previous iteration published in 2016.
Since then, “several high-impact studies in AAV have been published and the results of these studies required an update of the existing recommendations,” Dr. Hellmich said.
Developed in record time – just 7 months from start to finish – the process of updating the recommendations on AAV followed EULAR’s standard operating procedures. An important step in this process is to perform a systemic literature review. Perhaps crucially, and in contrast to the first U.S. vasculitis guidelines published only in 2021, the most recent literature search was able to include data on avacopan, which was approved for use in Europe in January as an adjunctive treatment for adults with severe active GPA and MPA.
The results of the literature review were reported separately at the EULAR 2022 Congress, with separate presentations highlighting the data behind the amended treatment and diagnostic and follow-up procedure recommendations.
Highlights of the changes
A key change is the introduction of four overarching principles, which weren’t included in the previous update, said Dr. Hellmich.
“We moved some of the existing recommendations with low level of evidence to overarching principles,” he added, stating that the first general principle was that all patients should be offered “the best care which must be based on shared decision-making between the patient and the physician considering efficacy, safety, and costs.”
The second principle states that patients should have access to education that covers the prognosis and impact of AAV, including recognizing warning symptoms and treatment options.
The third focuses on screening for adverse effects and comorbidities, recommending that patients are given appropriate prophylaxis and lifestyle advice.
Finally, the fourth general principle recognizes that AAV is a rare group of heterogenous and potentially life-threatening diseases that need multidisciplinary care, with access to specific vasculitis expertise.
New recommendations
Of the 17 recommendations made, 6 are completely new, including one on ANCA testing in patients who are suspected of having AAV.
“We recommend testing for both PR3- and MPO-ANCA using a high-quality antigen-specific assay as the primary method of testing,” Dr. Hellmich said. This is based on strong new evidence that antigen-specific assays have superior diagnostic accuracy, compared with indirect immunofluorescence.
“We also want to emphasize that ANCA testing should be done in patients with signs and symptoms in order to minimize the risk of false-positive results,” Dr. Hellmich said.
Also new is the recommendation to use oral steroids to induce remission in GPA/MPA, followed by a stepwise reduction in the dose, aiming for a dose of not more than 5 mg prednisolone per day by 4-5 months of treatment.
“Glucocorticoids are very effective, but also are the major trigger of infections in AAV,” said Dr. Hellmich. This is important since infections are a major driver of early mortality in AAV.
“Another possibility to reduce glucocorticoid exposure is avacopan,” he said. It’s recommended to be used in combination with rituximab or cyclophosphamide for remission induction in GPA/MPA as a strategy to basically “get rid of steroids.”
Indeed, “for patients who really have a high burden of glucocorticoid-associated adverse effects, especially relapsing patients, I think it would make sense just to give avacopan and no steroids,” Dr. Hellmich said.
Other new recommendations concern remission induction and maintenance therapy in new-onset EGPA. Regarding the latter, the choice of treatment depends on whether there is an organ- or life-threatening situation, with methotrexate, azathioprine, mepolizumab, or rituximab all recommended equally, or if there is no organ- or life-threatening situation, then mepolizumab is preferred.
Revised and unchanged recommendations
Eight of the recommendations have been revised, with rituximab being placed more prominently as a treatment in some. For remission induction in GPA and MPA with organ- or life threatening disease, rituximab is now the preferred option for relapsing disease. Rituximab also replaced methotrexate as the preferred option for maintaining remission, although methotrexate and azathioprine can still be considered as alternatives.
Another changed statement is on the duration of maintenance treatment in GPA and MPA, which now advocates 1-2 years of treatment after achieving remission. Longer therapy might be needed in relapsing cases, but the benefits and risks need to be carefully considered and patient preferences taken into account.
Prophylaxis against pneumonia and other infections is still recommended, with the revised guidance noting that patients receiving cyclophosphamide, rituximab, or high-dose steroids, should be treated with trimethoprim-sulfamethoxazole (co-trimoxazole).
“There are retrospective data in the AAV population that the administration of co-trimoxazole reduces not only the incidence of pneumocystis, but also of other infections. So, this is important recommendation for clinical practice,” Dr. Hellmich said.
Summing up
“For a rare disease group, I think this is very good progress,” said Dr. Hellmich, but “there are still many open questions, so we have a long research agenda.”
There is purposefully no recommendation on COVID-19, however, as “the conditions that impact COVID outcomes change rapidly and any recommendation made now is likely to be outdated soon; the AAV recommendations are intended to last for at least a couple of years.”
In a press release issued by the German Society for Rheumatology, which was unrelated to Dr. Hellmich’s talk, experts commented on vasculitis guidelines generally, noting that there has been a move toward using biologic therapies such as rituximab and mepolizumab as a new standard of therapy.
DGRh President and chief physician at the Immanuel Hospital in Berlin Andreas Krause, MD, observed that “cyclophosphamide, which was used in the past and which inhibits blood formation in the bone marrow and can lead to infertility, can now often be dispensed with.”
Julia Holle, MD, of Rheumazentrum Schleswig-Holstein Mitte in Neumünster, Germany, was also quoted in the press release, saying that, “for patients, the successful use of biologics and the reduction in the glucocorticoid dose is important progress.”
Dr. Holle was involved in the development of revised European guidelines. She is also the lead author of a recent publication on treatment of vasculitis on available evidence. Dr. Hellmich acknowledged having ties to multiple pharma companies, acting as speaker, consultant, or both to Abbvie, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai, GlaxoSmithKline, InflaRx, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and Vifor.
The
The 2022 revision – which was unveiled at the annual European Congress of Rheumatology – includes guidance on using new drugs, such as avacopan (Tavneos) and mepolizumab (Nucala), as well as revised recommendations on the use of rituximab and glucocorticosteroids.

The overhaul also contains specific recommendations for treating eosinophilic granulomatosis with polyangiitis (EGPA), separating it out from granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) for the first time.
“Until now, EGPA has usually been managed in the same way as [the] other diseases,” Bernhard Hellmich, MD, of the University of Tübingen (Germany) said in an interview ahead of his presentation at the congress.
“But we now have data on each type specifically, so there is good reason to make separate recommendations,” he added.
Indeed, so much new data has become available in the past few years there are only three recommendations that remain unchanged from the previous iteration published in 2016.
Since then, “several high-impact studies in AAV have been published and the results of these studies required an update of the existing recommendations,” Dr. Hellmich said.
Developed in record time – just 7 months from start to finish – the process of updating the recommendations on AAV followed EULAR’s standard operating procedures. An important step in this process is to perform a systemic literature review. Perhaps crucially, and in contrast to the first U.S. vasculitis guidelines published only in 2021, the most recent literature search was able to include data on avacopan, which was approved for use in Europe in January as an adjunctive treatment for adults with severe active GPA and MPA.
The results of the literature review were reported separately at the EULAR 2022 Congress, with separate presentations highlighting the data behind the amended treatment and diagnostic and follow-up procedure recommendations.
Highlights of the changes
A key change is the introduction of four overarching principles, which weren’t included in the previous update, said Dr. Hellmich.
“We moved some of the existing recommendations with low level of evidence to overarching principles,” he added, stating that the first general principle was that all patients should be offered “the best care which must be based on shared decision-making between the patient and the physician considering efficacy, safety, and costs.”
The second principle states that patients should have access to education that covers the prognosis and impact of AAV, including recognizing warning symptoms and treatment options.
The third focuses on screening for adverse effects and comorbidities, recommending that patients are given appropriate prophylaxis and lifestyle advice.
Finally, the fourth general principle recognizes that AAV is a rare group of heterogenous and potentially life-threatening diseases that need multidisciplinary care, with access to specific vasculitis expertise.
New recommendations
Of the 17 recommendations made, 6 are completely new, including one on ANCA testing in patients who are suspected of having AAV.
“We recommend testing for both PR3- and MPO-ANCA using a high-quality antigen-specific assay as the primary method of testing,” Dr. Hellmich said. This is based on strong new evidence that antigen-specific assays have superior diagnostic accuracy, compared with indirect immunofluorescence.
“We also want to emphasize that ANCA testing should be done in patients with signs and symptoms in order to minimize the risk of false-positive results,” Dr. Hellmich said.
Also new is the recommendation to use oral steroids to induce remission in GPA/MPA, followed by a stepwise reduction in the dose, aiming for a dose of not more than 5 mg prednisolone per day by 4-5 months of treatment.
“Glucocorticoids are very effective, but also are the major trigger of infections in AAV,” said Dr. Hellmich. This is important since infections are a major driver of early mortality in AAV.
“Another possibility to reduce glucocorticoid exposure is avacopan,” he said. It’s recommended to be used in combination with rituximab or cyclophosphamide for remission induction in GPA/MPA as a strategy to basically “get rid of steroids.”
Indeed, “for patients who really have a high burden of glucocorticoid-associated adverse effects, especially relapsing patients, I think it would make sense just to give avacopan and no steroids,” Dr. Hellmich said.
Other new recommendations concern remission induction and maintenance therapy in new-onset EGPA. Regarding the latter, the choice of treatment depends on whether there is an organ- or life-threatening situation, with methotrexate, azathioprine, mepolizumab, or rituximab all recommended equally, or if there is no organ- or life-threatening situation, then mepolizumab is preferred.
Revised and unchanged recommendations
Eight of the recommendations have been revised, with rituximab being placed more prominently as a treatment in some. For remission induction in GPA and MPA with organ- or life threatening disease, rituximab is now the preferred option for relapsing disease. Rituximab also replaced methotrexate as the preferred option for maintaining remission, although methotrexate and azathioprine can still be considered as alternatives.
Another changed statement is on the duration of maintenance treatment in GPA and MPA, which now advocates 1-2 years of treatment after achieving remission. Longer therapy might be needed in relapsing cases, but the benefits and risks need to be carefully considered and patient preferences taken into account.
Prophylaxis against pneumonia and other infections is still recommended, with the revised guidance noting that patients receiving cyclophosphamide, rituximab, or high-dose steroids, should be treated with trimethoprim-sulfamethoxazole (co-trimoxazole).
“There are retrospective data in the AAV population that the administration of co-trimoxazole reduces not only the incidence of pneumocystis, but also of other infections. So, this is important recommendation for clinical practice,” Dr. Hellmich said.
Summing up
“For a rare disease group, I think this is very good progress,” said Dr. Hellmich, but “there are still many open questions, so we have a long research agenda.”
There is purposefully no recommendation on COVID-19, however, as “the conditions that impact COVID outcomes change rapidly and any recommendation made now is likely to be outdated soon; the AAV recommendations are intended to last for at least a couple of years.”
In a press release issued by the German Society for Rheumatology, which was unrelated to Dr. Hellmich’s talk, experts commented on vasculitis guidelines generally, noting that there has been a move toward using biologic therapies such as rituximab and mepolizumab as a new standard of therapy.
DGRh President and chief physician at the Immanuel Hospital in Berlin Andreas Krause, MD, observed that “cyclophosphamide, which was used in the past and which inhibits blood formation in the bone marrow and can lead to infertility, can now often be dispensed with.”
Julia Holle, MD, of Rheumazentrum Schleswig-Holstein Mitte in Neumünster, Germany, was also quoted in the press release, saying that, “for patients, the successful use of biologics and the reduction in the glucocorticoid dose is important progress.”
Dr. Holle was involved in the development of revised European guidelines. She is also the lead author of a recent publication on treatment of vasculitis on available evidence. Dr. Hellmich acknowledged having ties to multiple pharma companies, acting as speaker, consultant, or both to Abbvie, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai, GlaxoSmithKline, InflaRx, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and Vifor.
The
The 2022 revision – which was unveiled at the annual European Congress of Rheumatology – includes guidance on using new drugs, such as avacopan (Tavneos) and mepolizumab (Nucala), as well as revised recommendations on the use of rituximab and glucocorticosteroids.

The overhaul also contains specific recommendations for treating eosinophilic granulomatosis with polyangiitis (EGPA), separating it out from granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) for the first time.
“Until now, EGPA has usually been managed in the same way as [the] other diseases,” Bernhard Hellmich, MD, of the University of Tübingen (Germany) said in an interview ahead of his presentation at the congress.
“But we now have data on each type specifically, so there is good reason to make separate recommendations,” he added.
Indeed, so much new data has become available in the past few years there are only three recommendations that remain unchanged from the previous iteration published in 2016.
Since then, “several high-impact studies in AAV have been published and the results of these studies required an update of the existing recommendations,” Dr. Hellmich said.
Developed in record time – just 7 months from start to finish – the process of updating the recommendations on AAV followed EULAR’s standard operating procedures. An important step in this process is to perform a systemic literature review. Perhaps crucially, and in contrast to the first U.S. vasculitis guidelines published only in 2021, the most recent literature search was able to include data on avacopan, which was approved for use in Europe in January as an adjunctive treatment for adults with severe active GPA and MPA.
The results of the literature review were reported separately at the EULAR 2022 Congress, with separate presentations highlighting the data behind the amended treatment and diagnostic and follow-up procedure recommendations.
Highlights of the changes
A key change is the introduction of four overarching principles, which weren’t included in the previous update, said Dr. Hellmich.
“We moved some of the existing recommendations with low level of evidence to overarching principles,” he added, stating that the first general principle was that all patients should be offered “the best care which must be based on shared decision-making between the patient and the physician considering efficacy, safety, and costs.”
The second principle states that patients should have access to education that covers the prognosis and impact of AAV, including recognizing warning symptoms and treatment options.
The third focuses on screening for adverse effects and comorbidities, recommending that patients are given appropriate prophylaxis and lifestyle advice.
Finally, the fourth general principle recognizes that AAV is a rare group of heterogenous and potentially life-threatening diseases that need multidisciplinary care, with access to specific vasculitis expertise.
New recommendations
Of the 17 recommendations made, 6 are completely new, including one on ANCA testing in patients who are suspected of having AAV.
“We recommend testing for both PR3- and MPO-ANCA using a high-quality antigen-specific assay as the primary method of testing,” Dr. Hellmich said. This is based on strong new evidence that antigen-specific assays have superior diagnostic accuracy, compared with indirect immunofluorescence.
“We also want to emphasize that ANCA testing should be done in patients with signs and symptoms in order to minimize the risk of false-positive results,” Dr. Hellmich said.
Also new is the recommendation to use oral steroids to induce remission in GPA/MPA, followed by a stepwise reduction in the dose, aiming for a dose of not more than 5 mg prednisolone per day by 4-5 months of treatment.
“Glucocorticoids are very effective, but also are the major trigger of infections in AAV,” said Dr. Hellmich. This is important since infections are a major driver of early mortality in AAV.
“Another possibility to reduce glucocorticoid exposure is avacopan,” he said. It’s recommended to be used in combination with rituximab or cyclophosphamide for remission induction in GPA/MPA as a strategy to basically “get rid of steroids.”
Indeed, “for patients who really have a high burden of glucocorticoid-associated adverse effects, especially relapsing patients, I think it would make sense just to give avacopan and no steroids,” Dr. Hellmich said.
Other new recommendations concern remission induction and maintenance therapy in new-onset EGPA. Regarding the latter, the choice of treatment depends on whether there is an organ- or life-threatening situation, with methotrexate, azathioprine, mepolizumab, or rituximab all recommended equally, or if there is no organ- or life-threatening situation, then mepolizumab is preferred.
Revised and unchanged recommendations
Eight of the recommendations have been revised, with rituximab being placed more prominently as a treatment in some. For remission induction in GPA and MPA with organ- or life threatening disease, rituximab is now the preferred option for relapsing disease. Rituximab also replaced methotrexate as the preferred option for maintaining remission, although methotrexate and azathioprine can still be considered as alternatives.
Another changed statement is on the duration of maintenance treatment in GPA and MPA, which now advocates 1-2 years of treatment after achieving remission. Longer therapy might be needed in relapsing cases, but the benefits and risks need to be carefully considered and patient preferences taken into account.
Prophylaxis against pneumonia and other infections is still recommended, with the revised guidance noting that patients receiving cyclophosphamide, rituximab, or high-dose steroids, should be treated with trimethoprim-sulfamethoxazole (co-trimoxazole).
“There are retrospective data in the AAV population that the administration of co-trimoxazole reduces not only the incidence of pneumocystis, but also of other infections. So, this is important recommendation for clinical practice,” Dr. Hellmich said.
Summing up
“For a rare disease group, I think this is very good progress,” said Dr. Hellmich, but “there are still many open questions, so we have a long research agenda.”
There is purposefully no recommendation on COVID-19, however, as “the conditions that impact COVID outcomes change rapidly and any recommendation made now is likely to be outdated soon; the AAV recommendations are intended to last for at least a couple of years.”
In a press release issued by the German Society for Rheumatology, which was unrelated to Dr. Hellmich’s talk, experts commented on vasculitis guidelines generally, noting that there has been a move toward using biologic therapies such as rituximab and mepolizumab as a new standard of therapy.
DGRh President and chief physician at the Immanuel Hospital in Berlin Andreas Krause, MD, observed that “cyclophosphamide, which was used in the past and which inhibits blood formation in the bone marrow and can lead to infertility, can now often be dispensed with.”
Julia Holle, MD, of Rheumazentrum Schleswig-Holstein Mitte in Neumünster, Germany, was also quoted in the press release, saying that, “for patients, the successful use of biologics and the reduction in the glucocorticoid dose is important progress.”
Dr. Holle was involved in the development of revised European guidelines. She is also the lead author of a recent publication on treatment of vasculitis on available evidence. Dr. Hellmich acknowledged having ties to multiple pharma companies, acting as speaker, consultant, or both to Abbvie, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai, GlaxoSmithKline, InflaRx, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and Vifor.
FROM THE EULAR 2022 CONGRESS
Upadacitinib effective against nonradiographic AxSpA
COPENHAGEN – The Janus kinase (JAK) inhibitor upadacitinib (Rinvoq, AbbVie) was associated with significant improvements in disease activity, pain, function, and quality of life, compared with placebo, in patients with nonradiographic axial spondyloarthritis (nr-axSpA), results of the first efficacy analysis of the phase 3, randomized SELECT-AXIS-2 trial showed.
The trial met its primary endpoint of an improvement of Assessment of SpondyloArthritis International Society 40% (ASAS 40) response criteria in the prespecified efficacy analysis at week 14, reported Filip Van den Bosch, MD, PhD, Ghent (Belgium) University.
In all, 45% of patients randomized to receive upadacitinib achieved an ASAS 40, compared with 23% of those assigned to placebo (P < .001).
“This is the first study showing efficacy and showing that the JAK inhibitor upadacitinib might be a therapeutic option in patients with active, nonradiographic spondyloarthritis,” Van den Bosch said at the annual European Congress of Rheumatology.
Although JAK inhibitors have previously been shown to be efficacious and safe for the treatment of ankylosing spondylitis, the SELECT-AXIS-2 trial is the first to evaluate a JAK inhibitor in nonradiographic axSpA, he added.
Study details
Patients 18 years and older with rheumatologist-diagnosed nr-axSpA were eligible for the study if they also met 2009 ASAS classification criteria for axSpA but not the radiologic criterion of modified New York criteria; had objective signs of active inflammation consistent with axSpA on MRI of the sacroiliac joints and/or high-sensitivity C-reactive protein above the upper limit of normal (2.87 mg/L) at screening; and had Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and patient-assessment of total back pain scores of 4 or greater based on a 0-10 numeric rating scale at study entry.
Patients were screened with MRI imaging of the spine and x-rays of the sacroiliac joints and spine, and then randomized to receive either placebo (157 patients) or upadacitinib 15 mg daily (158 patients) for 52 weeks. At the end of 52 weeks, all patients on upadacitinib will continue on the drug at the same dose level, and those assigned to placebo will be switched over to 15 mg upadacitinib daily maintenance.
As well as meeting the primary endpoint at week 14, response rates with the JAK inhibitor were higher at all time points over this initial time period, Dr. Van den Bosch noted.
Most targets hit
Of 14 multiplicity-controlled secondary endpoints, 12 were statistically better with upadacitinib, including change from baseline in patient’s assessment of total back pain, Bath Ankylosing Spondylitis Functional Index, Ankylosing Spondylitis Disease Activity Score, Low Disease Activity, Ankylosing Spondylitis Quality of Life, and MRI Spondyloarthritis Research Consortium of Canada score for sacroiliac joints.
Only the BASDAI and Maastricht Ankylosing Spondylitis Enthesitis Score were not significantly better with the JAK inhibitor.
The safety of upadacitinib in this setting was consistent with its known safety profile, Dr. Van den Bosch said.
Approximately half of all patients in each trial arm had an adverse event. Serious adverse events were reported in four patients assigned to upadacitinib versus two on placebo, and serious adverse events requiring drug discontinuation occurred in two and four patients, respectively.
‘Important’ data
Fabian Proft, MD, head of the clinical trials unit at Charite University Hospital, Berlin, who was not involved in the study, said in an interview that the findings were not surprising.
“We know the efficacy of upadacitinib already in radiographic axial spondyloarthritis, and from all the other drugs that we also know that are effective in radiographic axial spondyloarthritis that are similarly effective in nonradiographic disease,” he said.
“I think it is really important because it is the first data on JAK inhibition also in non-radiographic axial spondyloarthritis – an important step,” said Dr. Proft, who was comoderator of the oral abstract session where Van den Bosch reported the data.
The trial was supported by AbbVie. Dr. Van den Bosch disclosed speaker and consulting fees from AbbVie and others. Dr. Proft disclosed speaker and consulting fees from AbbVie as well.
A version of this article first appeared on Medscape.com.
COPENHAGEN – The Janus kinase (JAK) inhibitor upadacitinib (Rinvoq, AbbVie) was associated with significant improvements in disease activity, pain, function, and quality of life, compared with placebo, in patients with nonradiographic axial spondyloarthritis (nr-axSpA), results of the first efficacy analysis of the phase 3, randomized SELECT-AXIS-2 trial showed.
The trial met its primary endpoint of an improvement of Assessment of SpondyloArthritis International Society 40% (ASAS 40) response criteria in the prespecified efficacy analysis at week 14, reported Filip Van den Bosch, MD, PhD, Ghent (Belgium) University.
In all, 45% of patients randomized to receive upadacitinib achieved an ASAS 40, compared with 23% of those assigned to placebo (P < .001).
“This is the first study showing efficacy and showing that the JAK inhibitor upadacitinib might be a therapeutic option in patients with active, nonradiographic spondyloarthritis,” Van den Bosch said at the annual European Congress of Rheumatology.
Although JAK inhibitors have previously been shown to be efficacious and safe for the treatment of ankylosing spondylitis, the SELECT-AXIS-2 trial is the first to evaluate a JAK inhibitor in nonradiographic axSpA, he added.
Study details
Patients 18 years and older with rheumatologist-diagnosed nr-axSpA were eligible for the study if they also met 2009 ASAS classification criteria for axSpA but not the radiologic criterion of modified New York criteria; had objective signs of active inflammation consistent with axSpA on MRI of the sacroiliac joints and/or high-sensitivity C-reactive protein above the upper limit of normal (2.87 mg/L) at screening; and had Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and patient-assessment of total back pain scores of 4 or greater based on a 0-10 numeric rating scale at study entry.
Patients were screened with MRI imaging of the spine and x-rays of the sacroiliac joints and spine, and then randomized to receive either placebo (157 patients) or upadacitinib 15 mg daily (158 patients) for 52 weeks. At the end of 52 weeks, all patients on upadacitinib will continue on the drug at the same dose level, and those assigned to placebo will be switched over to 15 mg upadacitinib daily maintenance.
As well as meeting the primary endpoint at week 14, response rates with the JAK inhibitor were higher at all time points over this initial time period, Dr. Van den Bosch noted.
Most targets hit
Of 14 multiplicity-controlled secondary endpoints, 12 were statistically better with upadacitinib, including change from baseline in patient’s assessment of total back pain, Bath Ankylosing Spondylitis Functional Index, Ankylosing Spondylitis Disease Activity Score, Low Disease Activity, Ankylosing Spondylitis Quality of Life, and MRI Spondyloarthritis Research Consortium of Canada score for sacroiliac joints.
Only the BASDAI and Maastricht Ankylosing Spondylitis Enthesitis Score were not significantly better with the JAK inhibitor.
The safety of upadacitinib in this setting was consistent with its known safety profile, Dr. Van den Bosch said.
Approximately half of all patients in each trial arm had an adverse event. Serious adverse events were reported in four patients assigned to upadacitinib versus two on placebo, and serious adverse events requiring drug discontinuation occurred in two and four patients, respectively.
‘Important’ data
Fabian Proft, MD, head of the clinical trials unit at Charite University Hospital, Berlin, who was not involved in the study, said in an interview that the findings were not surprising.
“We know the efficacy of upadacitinib already in radiographic axial spondyloarthritis, and from all the other drugs that we also know that are effective in radiographic axial spondyloarthritis that are similarly effective in nonradiographic disease,” he said.
“I think it is really important because it is the first data on JAK inhibition also in non-radiographic axial spondyloarthritis – an important step,” said Dr. Proft, who was comoderator of the oral abstract session where Van den Bosch reported the data.
The trial was supported by AbbVie. Dr. Van den Bosch disclosed speaker and consulting fees from AbbVie and others. Dr. Proft disclosed speaker and consulting fees from AbbVie as well.
A version of this article first appeared on Medscape.com.
COPENHAGEN – The Janus kinase (JAK) inhibitor upadacitinib (Rinvoq, AbbVie) was associated with significant improvements in disease activity, pain, function, and quality of life, compared with placebo, in patients with nonradiographic axial spondyloarthritis (nr-axSpA), results of the first efficacy analysis of the phase 3, randomized SELECT-AXIS-2 trial showed.
The trial met its primary endpoint of an improvement of Assessment of SpondyloArthritis International Society 40% (ASAS 40) response criteria in the prespecified efficacy analysis at week 14, reported Filip Van den Bosch, MD, PhD, Ghent (Belgium) University.
In all, 45% of patients randomized to receive upadacitinib achieved an ASAS 40, compared with 23% of those assigned to placebo (P < .001).
“This is the first study showing efficacy and showing that the JAK inhibitor upadacitinib might be a therapeutic option in patients with active, nonradiographic spondyloarthritis,” Van den Bosch said at the annual European Congress of Rheumatology.
Although JAK inhibitors have previously been shown to be efficacious and safe for the treatment of ankylosing spondylitis, the SELECT-AXIS-2 trial is the first to evaluate a JAK inhibitor in nonradiographic axSpA, he added.
Study details
Patients 18 years and older with rheumatologist-diagnosed nr-axSpA were eligible for the study if they also met 2009 ASAS classification criteria for axSpA but not the radiologic criterion of modified New York criteria; had objective signs of active inflammation consistent with axSpA on MRI of the sacroiliac joints and/or high-sensitivity C-reactive protein above the upper limit of normal (2.87 mg/L) at screening; and had Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and patient-assessment of total back pain scores of 4 or greater based on a 0-10 numeric rating scale at study entry.
Patients were screened with MRI imaging of the spine and x-rays of the sacroiliac joints and spine, and then randomized to receive either placebo (157 patients) or upadacitinib 15 mg daily (158 patients) for 52 weeks. At the end of 52 weeks, all patients on upadacitinib will continue on the drug at the same dose level, and those assigned to placebo will be switched over to 15 mg upadacitinib daily maintenance.
As well as meeting the primary endpoint at week 14, response rates with the JAK inhibitor were higher at all time points over this initial time period, Dr. Van den Bosch noted.
Most targets hit
Of 14 multiplicity-controlled secondary endpoints, 12 were statistically better with upadacitinib, including change from baseline in patient’s assessment of total back pain, Bath Ankylosing Spondylitis Functional Index, Ankylosing Spondylitis Disease Activity Score, Low Disease Activity, Ankylosing Spondylitis Quality of Life, and MRI Spondyloarthritis Research Consortium of Canada score for sacroiliac joints.
Only the BASDAI and Maastricht Ankylosing Spondylitis Enthesitis Score were not significantly better with the JAK inhibitor.
The safety of upadacitinib in this setting was consistent with its known safety profile, Dr. Van den Bosch said.
Approximately half of all patients in each trial arm had an adverse event. Serious adverse events were reported in four patients assigned to upadacitinib versus two on placebo, and serious adverse events requiring drug discontinuation occurred in two and four patients, respectively.
‘Important’ data
Fabian Proft, MD, head of the clinical trials unit at Charite University Hospital, Berlin, who was not involved in the study, said in an interview that the findings were not surprising.
“We know the efficacy of upadacitinib already in radiographic axial spondyloarthritis, and from all the other drugs that we also know that are effective in radiographic axial spondyloarthritis that are similarly effective in nonradiographic disease,” he said.
“I think it is really important because it is the first data on JAK inhibition also in non-radiographic axial spondyloarthritis – an important step,” said Dr. Proft, who was comoderator of the oral abstract session where Van den Bosch reported the data.
The trial was supported by AbbVie. Dr. Van den Bosch disclosed speaker and consulting fees from AbbVie and others. Dr. Proft disclosed speaker and consulting fees from AbbVie as well.
A version of this article first appeared on Medscape.com.
AT THE EULAR 2022 CONGRESS