User login
Target childhood obesity now to prevent knee OA later
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
AT OARSI 2017
Key clinical point:
Major finding: The prevalence of patellar cartilage defects in young adults was 24.2% in those who were normal weight both as children and young adults, compared with 40% in subjects who were overweight at both time points.
Data source: A prospective population-based cohort study of 322 subjects followed from childhood to age 31-41 years, when they were assessed via MRI for knee cartilage defects.
Disclosures: The National Health and Medical Research Council of Australia supported the study. The presenter reported having no financial conflicts.
HIV-positive patients with metabolic syndrome have high rate of hand OA
LAS VEGAS – One of the most intriguing clues that suggest the metabolic syndrome or one of its components might cause hand osteoarthritis comes from a recent study of middle-aged HIV-positive patients, David T. Felson, MD, asserted at the World Congress on Osteoarthritis.
“This is an important study. The identification of an unusual cohort, which otherwise wasn’t supposed to get a particular disease, has really helped us to determine the cause of diseases in other circumstances,” said Dr. Felson, a rheumatologist who is professor of medicine and epidemiology and director of the clinical epidemiology research and training unit at Boston University. He cited an example that also happens to have been related to HIV: Kaposi’s sarcoma in gay men “that alerted us initially to the existence of HIV infection,” he commented.
Dr. Felson was a coinvestigator in the cross-sectional hand osteoarthritis (HOA) study, which included 152 HIV-positive patients with metabolic syndrome matched by age and gender to 149 HIV-infected individuals without it, with individuals in the Framingham (Mass.) Osteoarthritis Study serving as controls drawn from the general population. The prevalence of hand OA was 64.5% in HIV-positive subjects with metabolic syndrome – significantly greater than the 46.3% prevalence in HIV-positive patients without metabolic syndrome, and the 38.7% prevalence in the Framingham cohort.
In addition, the radiographic severity of hand OA was greater in the HIV-positive group with metabolic syndrome. In a logistic regression analysis, the presence of metabolic syndrome was associated with a 2.23-fold increased risk of hand OA in HIV-infected subjects (Ann Rheum Dis. 2016 Dec;75[12]:2101-7).
“It’s circumstantial evidence, but I would say that the report on this cohort provides us with potentially very important clues,” Dr. Felson said at the congress sponsored by the Osteoarthritis Research Society International.
Other evidence to suggest that metabolic factors are causally related to hand OA comes from animal models, as well as from large population-based cohort studies, including the Netherlands Epidemiology of Obesity (NEO) study. NEO involved 6,673 middle-aged Dutch men and women. Metabolic syndrome was associated with increased rates of both hand OA and knee OA in analyses unadjusted for body weight. However, when the Leiden University investigators adjusted for body weight, the association between metabolic syndrome and knee OA went away, whereas the association between metabolic syndrome and hand OA remained strong (Ann Rheum Dis. 2015 Oct;74[10]:1842-7).
This has uniformly been the case in other cohort studies reporting an association between metabolic syndrome and knee OA: upon adjusting for body mass index (BMI), there is no longer a residual relationship between metabolic syndrome and knee OA.
“One of the challenges in studying metabolic syndrome and knee osteoarthritis is that all the components of the metabolic syndrome are strongly correlated with obesity, and obesity is a major risk factor for knee osteoarthritis through its effects on joint loading. So obesity – at least for knee osteoarthritis – is an enormous confounder,” Dr. Felson said.
The findings from NEO and other large cohort studies underscore a key point: “Metabolic syndrome is not a risk factor for knee osteoarthritis, despite a lot of hullabaloo to the contrary. It doesn’t emerge in cohort studies as an important factor,” according to the rheum
“I’m not suggesting that there are different ultimate causes in the biology of hand osteoarthritis and knee osteoarthritis. I’m suggesting that the epidemiologic findings are different because joint load-bearing is a critical factor in knee osteoarthritis and that factor overwhelms much else. The message with regards to hand osteoarthritis is nowhere near as clear as it is for knee osteoarthritis, and the possibility that metabolic syndrome may cause hand osteoarthritis probably needs to be pursued further,” he continued.
Also worth pursuing is the possibility that hypertension increases the risk of OA. Several studies, including Framingham, have shown a modest signal of a relationship with both knee OA and hand OA that persists after adjusting for BMI. A hypothetical mechanism for such an effect might be reduced blood flow to the joints of hypertensive patients, with resultant adverse structural effects.
“Look at all the varied consequences of high blood pressure: stroke, blindness, MI, heart failure, kidney failure. Is osteoarthritis another one we need to be thinking about? I don’t know the answer, but I think it remains an open question based on the available data,” Dr. Felson observed.
As for the possibility that diabetes is causally linked to OA, he pronounced himself a skeptic.
“The diabetes association has been heralded by some, but in multiple studies, after adjustment for BMI the association goes away. I would strongly suggest to you that diabetes is not associated with osteoarthritis,” he declared.
He stressed that the possibility that metabolic factors are involved in the pathogenesis of OA isn’t simply of academic interest.
“We’re struggling in this field to find prevention and treatment opportunities. At present, there is no treatment that’s been shown to slow progression of osteoarthritis. If a causative metabolic factor could be identified, we might hope that it could reveal effective treatments for abrogating the disease,” he said.
Dr. Felson reported having no financial conflicts of interest.
LAS VEGAS – One of the most intriguing clues that suggest the metabolic syndrome or one of its components might cause hand osteoarthritis comes from a recent study of middle-aged HIV-positive patients, David T. Felson, MD, asserted at the World Congress on Osteoarthritis.
“This is an important study. The identification of an unusual cohort, which otherwise wasn’t supposed to get a particular disease, has really helped us to determine the cause of diseases in other circumstances,” said Dr. Felson, a rheumatologist who is professor of medicine and epidemiology and director of the clinical epidemiology research and training unit at Boston University. He cited an example that also happens to have been related to HIV: Kaposi’s sarcoma in gay men “that alerted us initially to the existence of HIV infection,” he commented.
Dr. Felson was a coinvestigator in the cross-sectional hand osteoarthritis (HOA) study, which included 152 HIV-positive patients with metabolic syndrome matched by age and gender to 149 HIV-infected individuals without it, with individuals in the Framingham (Mass.) Osteoarthritis Study serving as controls drawn from the general population. The prevalence of hand OA was 64.5% in HIV-positive subjects with metabolic syndrome – significantly greater than the 46.3% prevalence in HIV-positive patients without metabolic syndrome, and the 38.7% prevalence in the Framingham cohort.
In addition, the radiographic severity of hand OA was greater in the HIV-positive group with metabolic syndrome. In a logistic regression analysis, the presence of metabolic syndrome was associated with a 2.23-fold increased risk of hand OA in HIV-infected subjects (Ann Rheum Dis. 2016 Dec;75[12]:2101-7).
“It’s circumstantial evidence, but I would say that the report on this cohort provides us with potentially very important clues,” Dr. Felson said at the congress sponsored by the Osteoarthritis Research Society International.
Other evidence to suggest that metabolic factors are causally related to hand OA comes from animal models, as well as from large population-based cohort studies, including the Netherlands Epidemiology of Obesity (NEO) study. NEO involved 6,673 middle-aged Dutch men and women. Metabolic syndrome was associated with increased rates of both hand OA and knee OA in analyses unadjusted for body weight. However, when the Leiden University investigators adjusted for body weight, the association between metabolic syndrome and knee OA went away, whereas the association between metabolic syndrome and hand OA remained strong (Ann Rheum Dis. 2015 Oct;74[10]:1842-7).
This has uniformly been the case in other cohort studies reporting an association between metabolic syndrome and knee OA: upon adjusting for body mass index (BMI), there is no longer a residual relationship between metabolic syndrome and knee OA.
“One of the challenges in studying metabolic syndrome and knee osteoarthritis is that all the components of the metabolic syndrome are strongly correlated with obesity, and obesity is a major risk factor for knee osteoarthritis through its effects on joint loading. So obesity – at least for knee osteoarthritis – is an enormous confounder,” Dr. Felson said.
The findings from NEO and other large cohort studies underscore a key point: “Metabolic syndrome is not a risk factor for knee osteoarthritis, despite a lot of hullabaloo to the contrary. It doesn’t emerge in cohort studies as an important factor,” according to the rheum
“I’m not suggesting that there are different ultimate causes in the biology of hand osteoarthritis and knee osteoarthritis. I’m suggesting that the epidemiologic findings are different because joint load-bearing is a critical factor in knee osteoarthritis and that factor overwhelms much else. The message with regards to hand osteoarthritis is nowhere near as clear as it is for knee osteoarthritis, and the possibility that metabolic syndrome may cause hand osteoarthritis probably needs to be pursued further,” he continued.
Also worth pursuing is the possibility that hypertension increases the risk of OA. Several studies, including Framingham, have shown a modest signal of a relationship with both knee OA and hand OA that persists after adjusting for BMI. A hypothetical mechanism for such an effect might be reduced blood flow to the joints of hypertensive patients, with resultant adverse structural effects.
“Look at all the varied consequences of high blood pressure: stroke, blindness, MI, heart failure, kidney failure. Is osteoarthritis another one we need to be thinking about? I don’t know the answer, but I think it remains an open question based on the available data,” Dr. Felson observed.
As for the possibility that diabetes is causally linked to OA, he pronounced himself a skeptic.
“The diabetes association has been heralded by some, but in multiple studies, after adjustment for BMI the association goes away. I would strongly suggest to you that diabetes is not associated with osteoarthritis,” he declared.
He stressed that the possibility that metabolic factors are involved in the pathogenesis of OA isn’t simply of academic interest.
“We’re struggling in this field to find prevention and treatment opportunities. At present, there is no treatment that’s been shown to slow progression of osteoarthritis. If a causative metabolic factor could be identified, we might hope that it could reveal effective treatments for abrogating the disease,” he said.
Dr. Felson reported having no financial conflicts of interest.
LAS VEGAS – One of the most intriguing clues that suggest the metabolic syndrome or one of its components might cause hand osteoarthritis comes from a recent study of middle-aged HIV-positive patients, David T. Felson, MD, asserted at the World Congress on Osteoarthritis.
“This is an important study. The identification of an unusual cohort, which otherwise wasn’t supposed to get a particular disease, has really helped us to determine the cause of diseases in other circumstances,” said Dr. Felson, a rheumatologist who is professor of medicine and epidemiology and director of the clinical epidemiology research and training unit at Boston University. He cited an example that also happens to have been related to HIV: Kaposi’s sarcoma in gay men “that alerted us initially to the existence of HIV infection,” he commented.
Dr. Felson was a coinvestigator in the cross-sectional hand osteoarthritis (HOA) study, which included 152 HIV-positive patients with metabolic syndrome matched by age and gender to 149 HIV-infected individuals without it, with individuals in the Framingham (Mass.) Osteoarthritis Study serving as controls drawn from the general population. The prevalence of hand OA was 64.5% in HIV-positive subjects with metabolic syndrome – significantly greater than the 46.3% prevalence in HIV-positive patients without metabolic syndrome, and the 38.7% prevalence in the Framingham cohort.
In addition, the radiographic severity of hand OA was greater in the HIV-positive group with metabolic syndrome. In a logistic regression analysis, the presence of metabolic syndrome was associated with a 2.23-fold increased risk of hand OA in HIV-infected subjects (Ann Rheum Dis. 2016 Dec;75[12]:2101-7).
“It’s circumstantial evidence, but I would say that the report on this cohort provides us with potentially very important clues,” Dr. Felson said at the congress sponsored by the Osteoarthritis Research Society International.
Other evidence to suggest that metabolic factors are causally related to hand OA comes from animal models, as well as from large population-based cohort studies, including the Netherlands Epidemiology of Obesity (NEO) study. NEO involved 6,673 middle-aged Dutch men and women. Metabolic syndrome was associated with increased rates of both hand OA and knee OA in analyses unadjusted for body weight. However, when the Leiden University investigators adjusted for body weight, the association between metabolic syndrome and knee OA went away, whereas the association between metabolic syndrome and hand OA remained strong (Ann Rheum Dis. 2015 Oct;74[10]:1842-7).
This has uniformly been the case in other cohort studies reporting an association between metabolic syndrome and knee OA: upon adjusting for body mass index (BMI), there is no longer a residual relationship between metabolic syndrome and knee OA.
“One of the challenges in studying metabolic syndrome and knee osteoarthritis is that all the components of the metabolic syndrome are strongly correlated with obesity, and obesity is a major risk factor for knee osteoarthritis through its effects on joint loading. So obesity – at least for knee osteoarthritis – is an enormous confounder,” Dr. Felson said.
The findings from NEO and other large cohort studies underscore a key point: “Metabolic syndrome is not a risk factor for knee osteoarthritis, despite a lot of hullabaloo to the contrary. It doesn’t emerge in cohort studies as an important factor,” according to the rheum
“I’m not suggesting that there are different ultimate causes in the biology of hand osteoarthritis and knee osteoarthritis. I’m suggesting that the epidemiologic findings are different because joint load-bearing is a critical factor in knee osteoarthritis and that factor overwhelms much else. The message with regards to hand osteoarthritis is nowhere near as clear as it is for knee osteoarthritis, and the possibility that metabolic syndrome may cause hand osteoarthritis probably needs to be pursued further,” he continued.
Also worth pursuing is the possibility that hypertension increases the risk of OA. Several studies, including Framingham, have shown a modest signal of a relationship with both knee OA and hand OA that persists after adjusting for BMI. A hypothetical mechanism for such an effect might be reduced blood flow to the joints of hypertensive patients, with resultant adverse structural effects.
“Look at all the varied consequences of high blood pressure: stroke, blindness, MI, heart failure, kidney failure. Is osteoarthritis another one we need to be thinking about? I don’t know the answer, but I think it remains an open question based on the available data,” Dr. Felson observed.
As for the possibility that diabetes is causally linked to OA, he pronounced himself a skeptic.
“The diabetes association has been heralded by some, but in multiple studies, after adjustment for BMI the association goes away. I would strongly suggest to you that diabetes is not associated with osteoarthritis,” he declared.
He stressed that the possibility that metabolic factors are involved in the pathogenesis of OA isn’t simply of academic interest.
“We’re struggling in this field to find prevention and treatment opportunities. At present, there is no treatment that’s been shown to slow progression of osteoarthritis. If a causative metabolic factor could be identified, we might hope that it could reveal effective treatments for abrogating the disease,” he said.
Dr. Felson reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM OARSI 2017
Metabolic syndrome doesn’t cause hand osteoarthritis
LAS VEGAS – Metabolic syndrome is not causally related to hand osteoarthritis, according to data from the Framingham Offspring Study.
The new Framingham analysis, which features rigorous longitudinal follow-up, puts a serious dent in the popular hypothesis that metabolic syndrome is a risk factor for osteoarthritis through the proposed mechanism of systemic inflammation, Ida K. Haugen, MD, said at the World Congress on Osteoarthritis.
In recent years, the growing obesity epidemic and the related phenomenon of the metabolic syndrome have been posited to be the hub around which a variety of chronic diseases orbit, including type 2 diabetes, cardiovascular disease, some cancers, and osteoarthritis. Hand osteoarthritis is the phenotype of osteoarthritis best suited to investigation of whether metabolic syndrome promotes osteoarthritis by creating a systemic inflammatory state. Unlike knee, hip, or ankle osteoarthritis, the obesity that is a core feature of metabolic syndrome doesn’t cause much extra loading of the finger joints, Dr. Haugen explained at the meeting sponsored by the Osteoarthritis Research Society International.
Dr. Haugen, a rheumatologist at Diakonhjemmet Hospital in Oslo, presented an analysis of 1,089 Framingham Offspring Study participants aged 50-75 years at baseline, all free of rheumatoid arthritis and all with baseline hand radiographs. Of those patients, 41% met American Heart Association criteria for metabolic syndrome. In a cross-sectional analysis at baseline, the prevalence of metabolic syndrome in the subgroup with baseline hand osteoarthritis was no different from that in those without the disease.
The focus of the study involved the 785 patients who had both baseline hand radiographs and repeat hand x-rays at 7 years of follow-up. At baseline, 199 of these patients (25%) already had hand osteoarthritis, as defined by two or more interphalangeal joints with Kellgren-Lawrence grade 2-4 findings, and 49 patients had erosive hand osteoarthritis.
In a cross-sectional analysis at baseline, there was no association between metabolic syndrome and hand osteoarthritis. In contrast to the findings in earlier studies by other investigators, metabolic syndrome was actually associated with a significantly reduced risk of erosive hand osteoarthritis. Indeed, in a logistic regression analysis adjusted for age, sex, and body mass index, having metabolic syndrome was associated with a 58% reduction in the risk of prevalent erosive hand osteoarthritis.
During a mean follow-up of 7 years, 26% of patients who were free of hand osteoarthritis at baseline developed the condition. Of those, 8% developed incident erosive hand osteoarthritis. Metabolic syndrome was unrelated to the risk of these conditions.
Moreover, among patients with baseline hand osteoarthritis, there was no association between having metabolic syndrome and worsening Kellgren-Lawrence scores over time.
“We found no dose-response relationship between the number of metabolic syndrome components and the risk of developing hand osteoarthritis during follow-up,” according to the rheumatologist. “Those with all five components present did not have any higher risk of hand osteoarthritis, compared with those with no components.”
When she and her coinvestigators looked at the impact of the individual components of metabolic syndrome, they found a significant association between hypertension and worsening Kellgren-Lawrence scores over time. In an analysis adjusted for age, sex, and body mass index, having hypertension was associated with a 47% increased likelihood of radiographic worsening in patients with hand osteoarthritis at baseline. However, the association between hypertension and incident hand osteoarthritis was weaker and not statistically significant.
Drilling down further, the investigators found a dose-response relationship between the quartile of diastolic blood pressure and the risk of having hand osteoarthritis at baseline. This was not the case for systolic blood pressure, however. The apparent association between hypertension and hand osteoarthritis is worthy of further exploration, Dr. Haugen said.
None of the other elements of the metabolic syndrome showed any relationship with hand osteoarthritis risk.
The Framingham Offspring Study is supported by the National Heart, Lung, and Blood Institute. Dr. Haugen’s involvement was supported by Extrastiftelsen. She reported having no financial conflicts of interest.
LAS VEGAS – Metabolic syndrome is not causally related to hand osteoarthritis, according to data from the Framingham Offspring Study.
The new Framingham analysis, which features rigorous longitudinal follow-up, puts a serious dent in the popular hypothesis that metabolic syndrome is a risk factor for osteoarthritis through the proposed mechanism of systemic inflammation, Ida K. Haugen, MD, said at the World Congress on Osteoarthritis.
In recent years, the growing obesity epidemic and the related phenomenon of the metabolic syndrome have been posited to be the hub around which a variety of chronic diseases orbit, including type 2 diabetes, cardiovascular disease, some cancers, and osteoarthritis. Hand osteoarthritis is the phenotype of osteoarthritis best suited to investigation of whether metabolic syndrome promotes osteoarthritis by creating a systemic inflammatory state. Unlike knee, hip, or ankle osteoarthritis, the obesity that is a core feature of metabolic syndrome doesn’t cause much extra loading of the finger joints, Dr. Haugen explained at the meeting sponsored by the Osteoarthritis Research Society International.
Dr. Haugen, a rheumatologist at Diakonhjemmet Hospital in Oslo, presented an analysis of 1,089 Framingham Offspring Study participants aged 50-75 years at baseline, all free of rheumatoid arthritis and all with baseline hand radiographs. Of those patients, 41% met American Heart Association criteria for metabolic syndrome. In a cross-sectional analysis at baseline, the prevalence of metabolic syndrome in the subgroup with baseline hand osteoarthritis was no different from that in those without the disease.
The focus of the study involved the 785 patients who had both baseline hand radiographs and repeat hand x-rays at 7 years of follow-up. At baseline, 199 of these patients (25%) already had hand osteoarthritis, as defined by two or more interphalangeal joints with Kellgren-Lawrence grade 2-4 findings, and 49 patients had erosive hand osteoarthritis.
In a cross-sectional analysis at baseline, there was no association between metabolic syndrome and hand osteoarthritis. In contrast to the findings in earlier studies by other investigators, metabolic syndrome was actually associated with a significantly reduced risk of erosive hand osteoarthritis. Indeed, in a logistic regression analysis adjusted for age, sex, and body mass index, having metabolic syndrome was associated with a 58% reduction in the risk of prevalent erosive hand osteoarthritis.
During a mean follow-up of 7 years, 26% of patients who were free of hand osteoarthritis at baseline developed the condition. Of those, 8% developed incident erosive hand osteoarthritis. Metabolic syndrome was unrelated to the risk of these conditions.
Moreover, among patients with baseline hand osteoarthritis, there was no association between having metabolic syndrome and worsening Kellgren-Lawrence scores over time.
“We found no dose-response relationship between the number of metabolic syndrome components and the risk of developing hand osteoarthritis during follow-up,” according to the rheumatologist. “Those with all five components present did not have any higher risk of hand osteoarthritis, compared with those with no components.”
When she and her coinvestigators looked at the impact of the individual components of metabolic syndrome, they found a significant association between hypertension and worsening Kellgren-Lawrence scores over time. In an analysis adjusted for age, sex, and body mass index, having hypertension was associated with a 47% increased likelihood of radiographic worsening in patients with hand osteoarthritis at baseline. However, the association between hypertension and incident hand osteoarthritis was weaker and not statistically significant.
Drilling down further, the investigators found a dose-response relationship between the quartile of diastolic blood pressure and the risk of having hand osteoarthritis at baseline. This was not the case for systolic blood pressure, however. The apparent association between hypertension and hand osteoarthritis is worthy of further exploration, Dr. Haugen said.
None of the other elements of the metabolic syndrome showed any relationship with hand osteoarthritis risk.
The Framingham Offspring Study is supported by the National Heart, Lung, and Blood Institute. Dr. Haugen’s involvement was supported by Extrastiftelsen. She reported having no financial conflicts of interest.
LAS VEGAS – Metabolic syndrome is not causally related to hand osteoarthritis, according to data from the Framingham Offspring Study.
The new Framingham analysis, which features rigorous longitudinal follow-up, puts a serious dent in the popular hypothesis that metabolic syndrome is a risk factor for osteoarthritis through the proposed mechanism of systemic inflammation, Ida K. Haugen, MD, said at the World Congress on Osteoarthritis.
In recent years, the growing obesity epidemic and the related phenomenon of the metabolic syndrome have been posited to be the hub around which a variety of chronic diseases orbit, including type 2 diabetes, cardiovascular disease, some cancers, and osteoarthritis. Hand osteoarthritis is the phenotype of osteoarthritis best suited to investigation of whether metabolic syndrome promotes osteoarthritis by creating a systemic inflammatory state. Unlike knee, hip, or ankle osteoarthritis, the obesity that is a core feature of metabolic syndrome doesn’t cause much extra loading of the finger joints, Dr. Haugen explained at the meeting sponsored by the Osteoarthritis Research Society International.
Dr. Haugen, a rheumatologist at Diakonhjemmet Hospital in Oslo, presented an analysis of 1,089 Framingham Offspring Study participants aged 50-75 years at baseline, all free of rheumatoid arthritis and all with baseline hand radiographs. Of those patients, 41% met American Heart Association criteria for metabolic syndrome. In a cross-sectional analysis at baseline, the prevalence of metabolic syndrome in the subgroup with baseline hand osteoarthritis was no different from that in those without the disease.
The focus of the study involved the 785 patients who had both baseline hand radiographs and repeat hand x-rays at 7 years of follow-up. At baseline, 199 of these patients (25%) already had hand osteoarthritis, as defined by two or more interphalangeal joints with Kellgren-Lawrence grade 2-4 findings, and 49 patients had erosive hand osteoarthritis.
In a cross-sectional analysis at baseline, there was no association between metabolic syndrome and hand osteoarthritis. In contrast to the findings in earlier studies by other investigators, metabolic syndrome was actually associated with a significantly reduced risk of erosive hand osteoarthritis. Indeed, in a logistic regression analysis adjusted for age, sex, and body mass index, having metabolic syndrome was associated with a 58% reduction in the risk of prevalent erosive hand osteoarthritis.
During a mean follow-up of 7 years, 26% of patients who were free of hand osteoarthritis at baseline developed the condition. Of those, 8% developed incident erosive hand osteoarthritis. Metabolic syndrome was unrelated to the risk of these conditions.
Moreover, among patients with baseline hand osteoarthritis, there was no association between having metabolic syndrome and worsening Kellgren-Lawrence scores over time.
“We found no dose-response relationship between the number of metabolic syndrome components and the risk of developing hand osteoarthritis during follow-up,” according to the rheumatologist. “Those with all five components present did not have any higher risk of hand osteoarthritis, compared with those with no components.”
When she and her coinvestigators looked at the impact of the individual components of metabolic syndrome, they found a significant association between hypertension and worsening Kellgren-Lawrence scores over time. In an analysis adjusted for age, sex, and body mass index, having hypertension was associated with a 47% increased likelihood of radiographic worsening in patients with hand osteoarthritis at baseline. However, the association between hypertension and incident hand osteoarthritis was weaker and not statistically significant.
Drilling down further, the investigators found a dose-response relationship between the quartile of diastolic blood pressure and the risk of having hand osteoarthritis at baseline. This was not the case for systolic blood pressure, however. The apparent association between hypertension and hand osteoarthritis is worthy of further exploration, Dr. Haugen said.
None of the other elements of the metabolic syndrome showed any relationship with hand osteoarthritis risk.
The Framingham Offspring Study is supported by the National Heart, Lung, and Blood Institute. Dr. Haugen’s involvement was supported by Extrastiftelsen. She reported having no financial conflicts of interest.
AT OARSI 2017
Key clinical point:
Major finding: Patients with metabolic syndrome are not at increased risk of developing hand osteoarthritis, erosive hand osteoarthritis, or accelerated progression of existing hand osteoarthritis.
Data source: A prospective observational study of 785 patients with hand radiographs at baseline and 7 years’ follow-up, during which 26% developed new-onset hand osteoarthritis.
Disclosures: The Framingham Offspring Study is supported by the National Heart, Lung, and Blood Institute. Dr. Haugen’s involvement was supported by Extrastiftelsen. She reported having no financial conflicts of interest.
Knee bone density improved in osteoarthritis with load-reducing shoe
LAS VEGAS – Patients with medial compartment knee osteoarthritis who wore a patented flexible mobility shoe experienced a favorable reduction in medial tibial bone mineral density that directly correlated with their improved gait biomechanics and reduced peak knee adduction moment, Najia Shakoor, MD, reported at the World Congress on Osteoarthritis.
“Our results suggest that bone can be modified with sustained load reduction and that evaluation of tibial bone density may be an inexpensive tool for evaluating the consequences of load-reducing interventions,” said Dr. Shakoor, a rheumatologist at Rush University in Chicago.
Indeed, measuring changes in medial tibial bone density over time via serial dual x-ray absorptiometry is an attractive surrogate anatomic marker of a patient’s response to a biomechanical load-reducing intervention such as a special shoe or knee brace, Dr. Shakoor noted at the meeting sponsored by the Osteoarthritis Research Society International.
After all, she added, bone density measurement is simpler than sending a patient to a motion analysis laboratory for multicamera gait analysis using a force plate to evaluate changes in the peak external knee adduction moment (a validated marker of load distribution across the tibial plateau).
Studies suggest that bone, not cartilage, bears the bulk of the load burden across the knee joint. That’s why patients with knee osteoarthritis have increased proximal tibial bone mineral density. Dr. Shakoor presented evidence that sustained reduction in dynamic knee loading results in a proportionate reduction in medial tibial bone density over the course of 6 months.
She reported on 51 patients with mild to moderate radiographic and symptomatic medial compartment knee osteoarthritis who were randomized to wear a commercially available flexible mobility shoe or a similar-looking but nonflexible control shoe for 6 hours per day for at least 6 days per week for 6 months. At baseline and again at 6 months, the participants underwent knee bone density measurement and formal gait analysis.
Peak knee adduction moment decreased by 14% over the course of 6 months in the flexible shoe group, significantly greater than the 6% reduction in the controls. Moreover, Dr. Shakoor and her coinvestigators documented a significant reduction in medial tibial bone density in the flexible shoe group. The greater the improvement in knee adduction moment, the larger the reduction in bone density.
In contrast, medial tibial bone density didn’t change significantly in the controls.
Dr. Shakoor said that she had also expected to see a reduction in the ratio of medial to lateral tibial bone density in the flexible shoe group. However, there was no statistically significant change, although there was a trend in that direction.
Asked if reduction in knee adduction moment and/or medial tibial bone density correlated with improved knee pain scores, Dr. Shakoor replied that almost everyone in the study reported improvement in pain, suggesting a placebo effect for that endpoint. In any event, the relatively small study wasn’t powered to evaluate change in pain over time.
The Arthritis Foundation funded the study. Dr. Shakoor is coinventor of the flexible shoe used in the study. The patent, owned by Rush University, has been licensed to Dr. Comfort, which markets the shoe as the Dr. Comfort Flex-OA Mobility Shoe. A percentage of the proceeds from shoe sales is distributed to the university and the coinventors.
LAS VEGAS – Patients with medial compartment knee osteoarthritis who wore a patented flexible mobility shoe experienced a favorable reduction in medial tibial bone mineral density that directly correlated with their improved gait biomechanics and reduced peak knee adduction moment, Najia Shakoor, MD, reported at the World Congress on Osteoarthritis.
“Our results suggest that bone can be modified with sustained load reduction and that evaluation of tibial bone density may be an inexpensive tool for evaluating the consequences of load-reducing interventions,” said Dr. Shakoor, a rheumatologist at Rush University in Chicago.
Indeed, measuring changes in medial tibial bone density over time via serial dual x-ray absorptiometry is an attractive surrogate anatomic marker of a patient’s response to a biomechanical load-reducing intervention such as a special shoe or knee brace, Dr. Shakoor noted at the meeting sponsored by the Osteoarthritis Research Society International.
After all, she added, bone density measurement is simpler than sending a patient to a motion analysis laboratory for multicamera gait analysis using a force plate to evaluate changes in the peak external knee adduction moment (a validated marker of load distribution across the tibial plateau).
Studies suggest that bone, not cartilage, bears the bulk of the load burden across the knee joint. That’s why patients with knee osteoarthritis have increased proximal tibial bone mineral density. Dr. Shakoor presented evidence that sustained reduction in dynamic knee loading results in a proportionate reduction in medial tibial bone density over the course of 6 months.
She reported on 51 patients with mild to moderate radiographic and symptomatic medial compartment knee osteoarthritis who were randomized to wear a commercially available flexible mobility shoe or a similar-looking but nonflexible control shoe for 6 hours per day for at least 6 days per week for 6 months. At baseline and again at 6 months, the participants underwent knee bone density measurement and formal gait analysis.
Peak knee adduction moment decreased by 14% over the course of 6 months in the flexible shoe group, significantly greater than the 6% reduction in the controls. Moreover, Dr. Shakoor and her coinvestigators documented a significant reduction in medial tibial bone density in the flexible shoe group. The greater the improvement in knee adduction moment, the larger the reduction in bone density.
In contrast, medial tibial bone density didn’t change significantly in the controls.
Dr. Shakoor said that she had also expected to see a reduction in the ratio of medial to lateral tibial bone density in the flexible shoe group. However, there was no statistically significant change, although there was a trend in that direction.
Asked if reduction in knee adduction moment and/or medial tibial bone density correlated with improved knee pain scores, Dr. Shakoor replied that almost everyone in the study reported improvement in pain, suggesting a placebo effect for that endpoint. In any event, the relatively small study wasn’t powered to evaluate change in pain over time.
The Arthritis Foundation funded the study. Dr. Shakoor is coinventor of the flexible shoe used in the study. The patent, owned by Rush University, has been licensed to Dr. Comfort, which markets the shoe as the Dr. Comfort Flex-OA Mobility Shoe. A percentage of the proceeds from shoe sales is distributed to the university and the coinventors.
LAS VEGAS – Patients with medial compartment knee osteoarthritis who wore a patented flexible mobility shoe experienced a favorable reduction in medial tibial bone mineral density that directly correlated with their improved gait biomechanics and reduced peak knee adduction moment, Najia Shakoor, MD, reported at the World Congress on Osteoarthritis.
“Our results suggest that bone can be modified with sustained load reduction and that evaluation of tibial bone density may be an inexpensive tool for evaluating the consequences of load-reducing interventions,” said Dr. Shakoor, a rheumatologist at Rush University in Chicago.
Indeed, measuring changes in medial tibial bone density over time via serial dual x-ray absorptiometry is an attractive surrogate anatomic marker of a patient’s response to a biomechanical load-reducing intervention such as a special shoe or knee brace, Dr. Shakoor noted at the meeting sponsored by the Osteoarthritis Research Society International.
After all, she added, bone density measurement is simpler than sending a patient to a motion analysis laboratory for multicamera gait analysis using a force plate to evaluate changes in the peak external knee adduction moment (a validated marker of load distribution across the tibial plateau).
Studies suggest that bone, not cartilage, bears the bulk of the load burden across the knee joint. That’s why patients with knee osteoarthritis have increased proximal tibial bone mineral density. Dr. Shakoor presented evidence that sustained reduction in dynamic knee loading results in a proportionate reduction in medial tibial bone density over the course of 6 months.
She reported on 51 patients with mild to moderate radiographic and symptomatic medial compartment knee osteoarthritis who were randomized to wear a commercially available flexible mobility shoe or a similar-looking but nonflexible control shoe for 6 hours per day for at least 6 days per week for 6 months. At baseline and again at 6 months, the participants underwent knee bone density measurement and formal gait analysis.
Peak knee adduction moment decreased by 14% over the course of 6 months in the flexible shoe group, significantly greater than the 6% reduction in the controls. Moreover, Dr. Shakoor and her coinvestigators documented a significant reduction in medial tibial bone density in the flexible shoe group. The greater the improvement in knee adduction moment, the larger the reduction in bone density.
In contrast, medial tibial bone density didn’t change significantly in the controls.
Dr. Shakoor said that she had also expected to see a reduction in the ratio of medial to lateral tibial bone density in the flexible shoe group. However, there was no statistically significant change, although there was a trend in that direction.
Asked if reduction in knee adduction moment and/or medial tibial bone density correlated with improved knee pain scores, Dr. Shakoor replied that almost everyone in the study reported improvement in pain, suggesting a placebo effect for that endpoint. In any event, the relatively small study wasn’t powered to evaluate change in pain over time.
The Arthritis Foundation funded the study. Dr. Shakoor is coinventor of the flexible shoe used in the study. The patent, owned by Rush University, has been licensed to Dr. Comfort, which markets the shoe as the Dr. Comfort Flex-OA Mobility Shoe. A percentage of the proceeds from shoe sales is distributed to the university and the coinventors.
AT OARSI 2017
Key clinical point:
Major finding: Knee osteoarthritis patients who wore a flexible mobility shoe designed to reduce dynamic loading of the joint had a 14% reduction in peak external knee adduction moment over a 6-month period, with a parallel decrease in medial tibial bone density.
Data source: A 6-month randomized trial involving 51 patients with symptomatic radiographic medial compartment knee osteoarthritis, who were assigned to wear a shoe designed to reduce dynamic knee loading or a similar-looking control shoe.
Disclosures: The Arthritis Foundation funded the study. Dr. Shakoor is coinventor of the flexible shoe used in the study. The patent, owned by Rush University, has been licensed to Dr. Comfort, which markets the shoe as the Dr. Comfort Flex-OA Mobility Shoe. A percentage of the proceeds from shoe sales is distributed to the university and the coinventors.
CRPM may be promising predictive biomarker for knee osteoarthritis
LAS VEGAS – , Anne-Christine Bay-Jensen, PhD, said at the World Congress on Osteoarthritis.
That way, investigators maximize the likelihood of obtaining a positive outcome undiluted by giving the therapy to the wrong patients.
CRPM shows preliminary evidence of passing muster on both counts, according to Dr. Bay-Jensen, head of rheumatology at Nordic Bioscience in Herløv, Denmark.
The Danish researcher introduced herself to the Las Vegas audience by announcing, “My purpose in life is to develop biomarkers for identifying phenotypes in osteoarthritis.”
Indeed, she has been a pioneer in investigating the clinical utility of CRPM, a degradation fragment of C-reactive protein that is produced in the joint and thus reflects joint-specific tissue inflammation. Unlike C-reactive protein, which is an acute phase reactant, CRPM reflects chronic inflammation, she explained at the meeting sponsored by the Osteoarthritis Research Society International.
Her early work with CRPM explored its use as a biomarker in rheumatoid arthritis (RA) patients. She demonstrated, for example, in a secondary analysis of the phase III, double-blind, placebo-controlled LITHE trial that an 11% reduction in CRPM at week 4 of treatment with tocilizumab (Actemra) plus methotrexate was associated with a fourfold increased likelihood of a clinical response at week 16. That finding indicates that utilizing CRPM as an early predictor of tocilizumab efficacy promotes a more targeted, cost-effective, and personalized use of the biologic agent.
At OARSI 2017, Dr. Bay-Jensen presented evidence that even though the mean serum CRPM is significantly higher in patients with RA than in those with knee osteoarthritis (KOA), one-third or more of KOA patients have levels of joint tissue inflammation comparable to that seen in RA. That patient subset with a highly inflammatory KOA phenotype would be the logical focus of future clinical trials of agents having potent anti-inflammatory effects, rather than potential therapies with bone- or cartilage-modifying effects.
The data came from a biomarker study of 113 patients with early RA, as well as from two Nordic Bioscience–sponsored phase III randomized, multicenter, placebo-controlled clinical trials of oral salmon calcitonin in a total of 2,306 patients with knee osteoarthritis, both of which proved negative (Osteoarthritis Cartilage. 2015 Apr;23[4]:532-43). The mean baseline CRPM in the early RA patients was 17.1 ng/mL, compared with 8.5 ng/mL in the KOA patients. However, 31% of KOA patients in one phase III oral calcitonin trial and 41% in the other had a baseline serum CRPM greater than 9 ng/mL, a level that overlapped with 75% of the RA patients.
A related substudy of the oral calcitonin trials examined CRPM as a predictive biomarker. It included 153 knees without OA at baseline, 50 of which developed radiographic evidence of KOA, as evidenced by a Kellgren-Lawrence grade of 2 or 3 during 2 years of prospective follow-up. A serum CRPM of 9 ng/mL or more at baseline was associated with a 4.6-fold increased likelihood of incident KOA during follow-up.
Nordic Bioscience, Dr. Bay-Jensen’s employer, markets numerous proprietary biomarker assays, including one for CRPM.
LAS VEGAS – , Anne-Christine Bay-Jensen, PhD, said at the World Congress on Osteoarthritis.
That way, investigators maximize the likelihood of obtaining a positive outcome undiluted by giving the therapy to the wrong patients.
CRPM shows preliminary evidence of passing muster on both counts, according to Dr. Bay-Jensen, head of rheumatology at Nordic Bioscience in Herløv, Denmark.
The Danish researcher introduced herself to the Las Vegas audience by announcing, “My purpose in life is to develop biomarkers for identifying phenotypes in osteoarthritis.”
Indeed, she has been a pioneer in investigating the clinical utility of CRPM, a degradation fragment of C-reactive protein that is produced in the joint and thus reflects joint-specific tissue inflammation. Unlike C-reactive protein, which is an acute phase reactant, CRPM reflects chronic inflammation, she explained at the meeting sponsored by the Osteoarthritis Research Society International.
Her early work with CRPM explored its use as a biomarker in rheumatoid arthritis (RA) patients. She demonstrated, for example, in a secondary analysis of the phase III, double-blind, placebo-controlled LITHE trial that an 11% reduction in CRPM at week 4 of treatment with tocilizumab (Actemra) plus methotrexate was associated with a fourfold increased likelihood of a clinical response at week 16. That finding indicates that utilizing CRPM as an early predictor of tocilizumab efficacy promotes a more targeted, cost-effective, and personalized use of the biologic agent.
At OARSI 2017, Dr. Bay-Jensen presented evidence that even though the mean serum CRPM is significantly higher in patients with RA than in those with knee osteoarthritis (KOA), one-third or more of KOA patients have levels of joint tissue inflammation comparable to that seen in RA. That patient subset with a highly inflammatory KOA phenotype would be the logical focus of future clinical trials of agents having potent anti-inflammatory effects, rather than potential therapies with bone- or cartilage-modifying effects.
The data came from a biomarker study of 113 patients with early RA, as well as from two Nordic Bioscience–sponsored phase III randomized, multicenter, placebo-controlled clinical trials of oral salmon calcitonin in a total of 2,306 patients with knee osteoarthritis, both of which proved negative (Osteoarthritis Cartilage. 2015 Apr;23[4]:532-43). The mean baseline CRPM in the early RA patients was 17.1 ng/mL, compared with 8.5 ng/mL in the KOA patients. However, 31% of KOA patients in one phase III oral calcitonin trial and 41% in the other had a baseline serum CRPM greater than 9 ng/mL, a level that overlapped with 75% of the RA patients.
A related substudy of the oral calcitonin trials examined CRPM as a predictive biomarker. It included 153 knees without OA at baseline, 50 of which developed radiographic evidence of KOA, as evidenced by a Kellgren-Lawrence grade of 2 or 3 during 2 years of prospective follow-up. A serum CRPM of 9 ng/mL or more at baseline was associated with a 4.6-fold increased likelihood of incident KOA during follow-up.
Nordic Bioscience, Dr. Bay-Jensen’s employer, markets numerous proprietary biomarker assays, including one for CRPM.
LAS VEGAS – , Anne-Christine Bay-Jensen, PhD, said at the World Congress on Osteoarthritis.
That way, investigators maximize the likelihood of obtaining a positive outcome undiluted by giving the therapy to the wrong patients.
CRPM shows preliminary evidence of passing muster on both counts, according to Dr. Bay-Jensen, head of rheumatology at Nordic Bioscience in Herløv, Denmark.
The Danish researcher introduced herself to the Las Vegas audience by announcing, “My purpose in life is to develop biomarkers for identifying phenotypes in osteoarthritis.”
Indeed, she has been a pioneer in investigating the clinical utility of CRPM, a degradation fragment of C-reactive protein that is produced in the joint and thus reflects joint-specific tissue inflammation. Unlike C-reactive protein, which is an acute phase reactant, CRPM reflects chronic inflammation, she explained at the meeting sponsored by the Osteoarthritis Research Society International.
Her early work with CRPM explored its use as a biomarker in rheumatoid arthritis (RA) patients. She demonstrated, for example, in a secondary analysis of the phase III, double-blind, placebo-controlled LITHE trial that an 11% reduction in CRPM at week 4 of treatment with tocilizumab (Actemra) plus methotrexate was associated with a fourfold increased likelihood of a clinical response at week 16. That finding indicates that utilizing CRPM as an early predictor of tocilizumab efficacy promotes a more targeted, cost-effective, and personalized use of the biologic agent.
At OARSI 2017, Dr. Bay-Jensen presented evidence that even though the mean serum CRPM is significantly higher in patients with RA than in those with knee osteoarthritis (KOA), one-third or more of KOA patients have levels of joint tissue inflammation comparable to that seen in RA. That patient subset with a highly inflammatory KOA phenotype would be the logical focus of future clinical trials of agents having potent anti-inflammatory effects, rather than potential therapies with bone- or cartilage-modifying effects.
The data came from a biomarker study of 113 patients with early RA, as well as from two Nordic Bioscience–sponsored phase III randomized, multicenter, placebo-controlled clinical trials of oral salmon calcitonin in a total of 2,306 patients with knee osteoarthritis, both of which proved negative (Osteoarthritis Cartilage. 2015 Apr;23[4]:532-43). The mean baseline CRPM in the early RA patients was 17.1 ng/mL, compared with 8.5 ng/mL in the KOA patients. However, 31% of KOA patients in one phase III oral calcitonin trial and 41% in the other had a baseline serum CRPM greater than 9 ng/mL, a level that overlapped with 75% of the RA patients.
A related substudy of the oral calcitonin trials examined CRPM as a predictive biomarker. It included 153 knees without OA at baseline, 50 of which developed radiographic evidence of KOA, as evidenced by a Kellgren-Lawrence grade of 2 or 3 during 2 years of prospective follow-up. A serum CRPM of 9 ng/mL or more at baseline was associated with a 4.6-fold increased likelihood of incident KOA during follow-up.
Nordic Bioscience, Dr. Bay-Jensen’s employer, markets numerous proprietary biomarker assays, including one for CRPM.
EXPERT ANALYSIS FROM OARSI 2017
Novel ibuprofen formulation cuts GI side effects in patients with knee pain flares
LAS VEGAS – A novel lipid formulation of ibuprofen given at 1,200 mg/day proved noninferior to high-dose standard ibuprofen at 2,400 mg/day for management of episodic knee pain flares in a phase III randomized trial, and it accomplished this with significantly fewer gastrointestinal side effects, Sita M.A. Bierma-Zeinstra, MD, reported.
Episodic flares of knee pain are a disabling feature of knee osteoarthritis that can occur at all stages of the disease, including prior to clinical diagnosis. There is a need for a fast-acting analgesic designed for short-term use with minimal side effects to provide pain relief during these flares. This was the motivation for developing Flarin, a lipid formulation soft-gel capsule of ibuprofen that is effective at less-than-standard doses of the conventional NSAID, she explained at the World Congress on Osteoarthritis.
The primary outcome was change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale after 5 days of treatment. The score dropped from a mean of 5.72 at baseline out of a possible maximum of 10 to 3.05 in the lipid ibuprofen group, from 5.6 to 3.26 in patients on standard ibuprofen at 1,200 mg/day, and from 5.61 to 2.82 in subjects on standard ibuprofen at 2,400 mg/day. Those between-group differences were not statistically significant, reported Dr. Bierma-Zeinstra, professor of osteoarthritis and related disorders at Erasmus University Medical Center in Rotterdam.
In contrast, the rate of gastrointestinal side effects was significantly different across the three treatment arms: 16.2% in the lipid ibuprofen group, 22.6% with conventional ibuprofen at 1,200 mg/day, and 28.3% with ibuprofen at 2,400 mg/day, she said at the congress, which was sponsored by the Osteoarthritis Research Society International.
The group on the investigational formulation of ibuprofen also showed a consistent trend for superior results on the WOMAC swelling, pain, stiffness, and function subscales after 5 days of treatment, although only the improvement in swelling achieved statistical significance, Dr. Bierma-Zeinstra continued.
Flarin is approved and marketed in the United Kingdom. Infirst Healthcare, the novel NSAID’s developer and the sponsor of the phase III randomized trial, is seeking to gain regulatory approval throughout Europe. The U.K. company also has an agreement with McNeil Consumer Pharmaceuticals to market its products in the United States, once approved.
Dr. Bierma-Zeinstra reported having received a research grant from Infirst.
LAS VEGAS – A novel lipid formulation of ibuprofen given at 1,200 mg/day proved noninferior to high-dose standard ibuprofen at 2,400 mg/day for management of episodic knee pain flares in a phase III randomized trial, and it accomplished this with significantly fewer gastrointestinal side effects, Sita M.A. Bierma-Zeinstra, MD, reported.
Episodic flares of knee pain are a disabling feature of knee osteoarthritis that can occur at all stages of the disease, including prior to clinical diagnosis. There is a need for a fast-acting analgesic designed for short-term use with minimal side effects to provide pain relief during these flares. This was the motivation for developing Flarin, a lipid formulation soft-gel capsule of ibuprofen that is effective at less-than-standard doses of the conventional NSAID, she explained at the World Congress on Osteoarthritis.
The primary outcome was change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale after 5 days of treatment. The score dropped from a mean of 5.72 at baseline out of a possible maximum of 10 to 3.05 in the lipid ibuprofen group, from 5.6 to 3.26 in patients on standard ibuprofen at 1,200 mg/day, and from 5.61 to 2.82 in subjects on standard ibuprofen at 2,400 mg/day. Those between-group differences were not statistically significant, reported Dr. Bierma-Zeinstra, professor of osteoarthritis and related disorders at Erasmus University Medical Center in Rotterdam.
In contrast, the rate of gastrointestinal side effects was significantly different across the three treatment arms: 16.2% in the lipid ibuprofen group, 22.6% with conventional ibuprofen at 1,200 mg/day, and 28.3% with ibuprofen at 2,400 mg/day, she said at the congress, which was sponsored by the Osteoarthritis Research Society International.
The group on the investigational formulation of ibuprofen also showed a consistent trend for superior results on the WOMAC swelling, pain, stiffness, and function subscales after 5 days of treatment, although only the improvement in swelling achieved statistical significance, Dr. Bierma-Zeinstra continued.
Flarin is approved and marketed in the United Kingdom. Infirst Healthcare, the novel NSAID’s developer and the sponsor of the phase III randomized trial, is seeking to gain regulatory approval throughout Europe. The U.K. company also has an agreement with McNeil Consumer Pharmaceuticals to market its products in the United States, once approved.
Dr. Bierma-Zeinstra reported having received a research grant from Infirst.
LAS VEGAS – A novel lipid formulation of ibuprofen given at 1,200 mg/day proved noninferior to high-dose standard ibuprofen at 2,400 mg/day for management of episodic knee pain flares in a phase III randomized trial, and it accomplished this with significantly fewer gastrointestinal side effects, Sita M.A. Bierma-Zeinstra, MD, reported.
Episodic flares of knee pain are a disabling feature of knee osteoarthritis that can occur at all stages of the disease, including prior to clinical diagnosis. There is a need for a fast-acting analgesic designed for short-term use with minimal side effects to provide pain relief during these flares. This was the motivation for developing Flarin, a lipid formulation soft-gel capsule of ibuprofen that is effective at less-than-standard doses of the conventional NSAID, she explained at the World Congress on Osteoarthritis.
The primary outcome was change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale after 5 days of treatment. The score dropped from a mean of 5.72 at baseline out of a possible maximum of 10 to 3.05 in the lipid ibuprofen group, from 5.6 to 3.26 in patients on standard ibuprofen at 1,200 mg/day, and from 5.61 to 2.82 in subjects on standard ibuprofen at 2,400 mg/day. Those between-group differences were not statistically significant, reported Dr. Bierma-Zeinstra, professor of osteoarthritis and related disorders at Erasmus University Medical Center in Rotterdam.
In contrast, the rate of gastrointestinal side effects was significantly different across the three treatment arms: 16.2% in the lipid ibuprofen group, 22.6% with conventional ibuprofen at 1,200 mg/day, and 28.3% with ibuprofen at 2,400 mg/day, she said at the congress, which was sponsored by the Osteoarthritis Research Society International.
The group on the investigational formulation of ibuprofen also showed a consistent trend for superior results on the WOMAC swelling, pain, stiffness, and function subscales after 5 days of treatment, although only the improvement in swelling achieved statistical significance, Dr. Bierma-Zeinstra continued.
Flarin is approved and marketed in the United Kingdom. Infirst Healthcare, the novel NSAID’s developer and the sponsor of the phase III randomized trial, is seeking to gain regulatory approval throughout Europe. The U.K. company also has an agreement with McNeil Consumer Pharmaceuticals to market its products in the United States, once approved.
Dr. Bierma-Zeinstra reported having received a research grant from Infirst.
AT OARSI 2017
Key clinical point:
Major finding: The incidence of GI side effects in patients being treated for an episodic knee pain flare was 16.2% after 5 days of treatment with a novel lipid formulation of ibuprofen at 1,200 mg/day, significantly lower than in patients randomized to conventional ibuprofen soft-gel capsules at 1,200 or 2,400 mg/day.
Data source: This three-arm, multicenter, international randomized trial involved 462 patients experiencing a recent-onset episodic flare of knee pain.
Disclosures: The presenter reported having received a research grant from Infirst Healthcare, which funded the study.
How to prevent secondary posttraumatic knee osteoarthritis
LAS VEGAS – A variety of evidence-based strategies are available for preventing posttraumatic knee osteoarthritis (KOA) in patients who have already sustained an anterior cruciate ligament (ACL) injury. And they’re generally ignored, according to May Arna Risberg, PhD.
“We have a lot of knowledge. We can use secondary prevention strategies. And here I think we, as physical therapists, physicians, and orthopedic surgeons, are doing a lousy job because we are sending these ACL-injured patients back to sports before they have normalized knee function and quadriceps strength,” said Dr. Risberg, professor of sports medicine at the Norwegian School of Sport Sciences in Oslo.
With no proven disease-modifying therapy for KOA available to date, secondary prevention of posttraumatic KOA is worthy of high-priority status, she said at the World Congress on Osteoarthritis. An estimated 250,00 ACL injuries occur annually in the United States, and up to one-half of affected patients, most of whom are young, active people, will experience a second ACL rupture within the first few years after undergoing their initial reconstruction. This second ACL injury greatly increases their risk of developing posttraumatic KOA within 15-20 years, while they are still relatively young, she said.
Moreover, if the second ACL injury involves meniscus surgery, the 5-year risk of posttraumatic KOA roughly triples to up to 48%.
She highlighted a few effective strategies for preventing posttraumatic KOA in patients who already have an ACL injury.
Avoid reinjury
Dr. Risberg was senior author of a recent report from the prospective Delaware-Oslo Cohort Study involving 106 athletes who underwent ACL reconstruction following injury in what she termed level I sports. These are sports that entail lots of pivoting, jumping, and hard cutting, such as basketball, soccer, and handball.
In the first 2 years after ACL repair, 30% of patients who returned to participation in a level 1 sport experienced an ACL reinjury, compared with just 8% who opted for a lower-level sport. Athletes who returned to a level 1 sport had an adjusted 4.3 times greater ACL reinjury rate than those who didn’t, Dr. Risberg noted at the congress sponsored by the Osteoarthritis Research Society International.
The good news is that this sharply increased reinjury risk was mitigated if return to a level 1 sport was delayed for at least 9 months post surgery and if the patient had regained quadriceps strength comparable to the uninjured side. For every month that return to sport was delayed out until 9 months post ACL reconstruction, the knee reinjury rate was reduced by 51% (Br J Sports Med. 2016;50:804-8).
In a meta-analysis by other investigators of 12 studies including 5,707 participants, weakness of the knee extensor muscles was independently associated with a 1.65 times increased risk of developing KOA (Osteoarthritis Cartilage. 2015 Feb;23[2]:171-7).
Attend to BMI
A discussion of the importance of maintaining a healthy body weight is an important aspect of patient education for athletes with knee injuries. In a cohort study of 988 patients who underwent primary ACL reconstruction, being overweight or obese was associated with a significantly increased risk of subsequent meniscal tears and chondral lesions (Am J Sports Med. 2015 Dec;43[12]:2966-73).
Also, it’s well established that obesity is a risk factor for knee OA, and Canadian investigators have shown that young athletes with a sports-related intra-articular knee injury were 3.75 times more likely to be overweight or obese 3-10 years post injury, compared with matched uninjured controls (Osteoarthritis Cartilage. 2015 Jul;23[7]:1122-9).
Consider prehabilitative exercise training
Dr. Risberg and coinvestigators have reported that preoperative quadriceps muscle strength deficits are predictive of impaired knee function, as measured by the Cincinnati Knee Score 2 years post surgery. She said she believes ACL reconstruction shouldn’t be done until quadriceps muscle strength is at least 80% of that in the uninjured limb (Br J Sports Med. 2009 May;43[5]:371-6). She and her coinvestigators have published the details of a 5-week progressive exercise therapy program in which they have shown results in significantly improved early postoperative knee function (J Orthop Sports Phys Ther. 2010 Nov;40[11]:705-21). They now try to have patients complete the twice-weekly, 5-week program before final decisions are reached regarding whether to have ACL reconstruction.
Test all before okaying return to sport
It’s important to know if patients who have undergone ACL reconstruction have gotten full knee function back before determining if they’re ready for full-on sports participation. In the Delaware-Oslo Cohort Study, patients who delayed their return until at least 9 months after surgery and passed the return-to-sports test had a 5.6% reinjury rate within 2 years, while those who failed the return-to-sports criteria had a 38.2% ACL reinjury rate.
The return-to-sports testing utilized in this study entailed isokinetic quadriceps strength testing, the single hop leg test, the 14-item self-rated Knee Outcome Survey–Activities of Daily Living Scale, and a self-rated Global Rating Scale of perceived function on a 0-100 scale. To be cleared for return to sports, a patient had to demonstrate having regained at least 90% of quadriceps muscle strength and hop performance along with scoring in the normative range on both of the self-rating instruments.
Surgical vs. nonsurgical treatment of ACL rupture
The evidence on this score is conflicting, according to Dr. Risberg. While most physical therapists believe ACL reconstruction doesn’t protect against later development of KOA, as reflected in a meta-analysis of published studies (J Bone Joint Surg Am. 2014 Feb 19;96[4]:292-300), a more recent retrospective comparison of 964 patients with an isolated ACL tear and an equal number of matched controls concluded that patients treated nonoperatively were six times more likely to have been diagnosed with KOA and 16.7 times more likely to have undergone total knee replacement at a mean follow-up of 13.7 years than were those treated with ACL reconstruction (Am J Sports Med. 2016 Jul;44[7]:1699-707).
Dr. Risberg’s fellow panelist Jackie Whittaker, PhD, said that, as long as quadriceps muscle strengthening is a priority, it makes sense to strengthen the hamstring as well, particularly if the ACL reconstruction utilized the hamstring tendon.
“Also, I would add that it’s important to develop a relationship with these ACL-injured people, who are often very young. Preventing a disease that they’re going to get 20 years later isn’t a priority for them. You need to develop that relationship and build it up over time. Helping them set realistic expectations is very important. And we need to do what we can to help them find some sort of competitive outlet. A lot of these kids were very competitive, and now they’ve had an injury and can’t compete. They don’t want to go back to playing just any sport. They want to be able to be competitive, and if you don’t help them find another way to express that, they sort of give up on physical activity altogether,” according to Dr. Whittaker of the University of Alberta in Edmonton.
Dr. Risberg and Dr. Whittaker reported having no financial conflicts of interest.
LAS VEGAS – A variety of evidence-based strategies are available for preventing posttraumatic knee osteoarthritis (KOA) in patients who have already sustained an anterior cruciate ligament (ACL) injury. And they’re generally ignored, according to May Arna Risberg, PhD.
“We have a lot of knowledge. We can use secondary prevention strategies. And here I think we, as physical therapists, physicians, and orthopedic surgeons, are doing a lousy job because we are sending these ACL-injured patients back to sports before they have normalized knee function and quadriceps strength,” said Dr. Risberg, professor of sports medicine at the Norwegian School of Sport Sciences in Oslo.
With no proven disease-modifying therapy for KOA available to date, secondary prevention of posttraumatic KOA is worthy of high-priority status, she said at the World Congress on Osteoarthritis. An estimated 250,00 ACL injuries occur annually in the United States, and up to one-half of affected patients, most of whom are young, active people, will experience a second ACL rupture within the first few years after undergoing their initial reconstruction. This second ACL injury greatly increases their risk of developing posttraumatic KOA within 15-20 years, while they are still relatively young, she said.
Moreover, if the second ACL injury involves meniscus surgery, the 5-year risk of posttraumatic KOA roughly triples to up to 48%.
She highlighted a few effective strategies for preventing posttraumatic KOA in patients who already have an ACL injury.
Avoid reinjury
Dr. Risberg was senior author of a recent report from the prospective Delaware-Oslo Cohort Study involving 106 athletes who underwent ACL reconstruction following injury in what she termed level I sports. These are sports that entail lots of pivoting, jumping, and hard cutting, such as basketball, soccer, and handball.
In the first 2 years after ACL repair, 30% of patients who returned to participation in a level 1 sport experienced an ACL reinjury, compared with just 8% who opted for a lower-level sport. Athletes who returned to a level 1 sport had an adjusted 4.3 times greater ACL reinjury rate than those who didn’t, Dr. Risberg noted at the congress sponsored by the Osteoarthritis Research Society International.
The good news is that this sharply increased reinjury risk was mitigated if return to a level 1 sport was delayed for at least 9 months post surgery and if the patient had regained quadriceps strength comparable to the uninjured side. For every month that return to sport was delayed out until 9 months post ACL reconstruction, the knee reinjury rate was reduced by 51% (Br J Sports Med. 2016;50:804-8).
In a meta-analysis by other investigators of 12 studies including 5,707 participants, weakness of the knee extensor muscles was independently associated with a 1.65 times increased risk of developing KOA (Osteoarthritis Cartilage. 2015 Feb;23[2]:171-7).
Attend to BMI
A discussion of the importance of maintaining a healthy body weight is an important aspect of patient education for athletes with knee injuries. In a cohort study of 988 patients who underwent primary ACL reconstruction, being overweight or obese was associated with a significantly increased risk of subsequent meniscal tears and chondral lesions (Am J Sports Med. 2015 Dec;43[12]:2966-73).
Also, it’s well established that obesity is a risk factor for knee OA, and Canadian investigators have shown that young athletes with a sports-related intra-articular knee injury were 3.75 times more likely to be overweight or obese 3-10 years post injury, compared with matched uninjured controls (Osteoarthritis Cartilage. 2015 Jul;23[7]:1122-9).
Consider prehabilitative exercise training
Dr. Risberg and coinvestigators have reported that preoperative quadriceps muscle strength deficits are predictive of impaired knee function, as measured by the Cincinnati Knee Score 2 years post surgery. She said she believes ACL reconstruction shouldn’t be done until quadriceps muscle strength is at least 80% of that in the uninjured limb (Br J Sports Med. 2009 May;43[5]:371-6). She and her coinvestigators have published the details of a 5-week progressive exercise therapy program in which they have shown results in significantly improved early postoperative knee function (J Orthop Sports Phys Ther. 2010 Nov;40[11]:705-21). They now try to have patients complete the twice-weekly, 5-week program before final decisions are reached regarding whether to have ACL reconstruction.
Test all before okaying return to sport
It’s important to know if patients who have undergone ACL reconstruction have gotten full knee function back before determining if they’re ready for full-on sports participation. In the Delaware-Oslo Cohort Study, patients who delayed their return until at least 9 months after surgery and passed the return-to-sports test had a 5.6% reinjury rate within 2 years, while those who failed the return-to-sports criteria had a 38.2% ACL reinjury rate.
The return-to-sports testing utilized in this study entailed isokinetic quadriceps strength testing, the single hop leg test, the 14-item self-rated Knee Outcome Survey–Activities of Daily Living Scale, and a self-rated Global Rating Scale of perceived function on a 0-100 scale. To be cleared for return to sports, a patient had to demonstrate having regained at least 90% of quadriceps muscle strength and hop performance along with scoring in the normative range on both of the self-rating instruments.
Surgical vs. nonsurgical treatment of ACL rupture
The evidence on this score is conflicting, according to Dr. Risberg. While most physical therapists believe ACL reconstruction doesn’t protect against later development of KOA, as reflected in a meta-analysis of published studies (J Bone Joint Surg Am. 2014 Feb 19;96[4]:292-300), a more recent retrospective comparison of 964 patients with an isolated ACL tear and an equal number of matched controls concluded that patients treated nonoperatively were six times more likely to have been diagnosed with KOA and 16.7 times more likely to have undergone total knee replacement at a mean follow-up of 13.7 years than were those treated with ACL reconstruction (Am J Sports Med. 2016 Jul;44[7]:1699-707).
Dr. Risberg’s fellow panelist Jackie Whittaker, PhD, said that, as long as quadriceps muscle strengthening is a priority, it makes sense to strengthen the hamstring as well, particularly if the ACL reconstruction utilized the hamstring tendon.
“Also, I would add that it’s important to develop a relationship with these ACL-injured people, who are often very young. Preventing a disease that they’re going to get 20 years later isn’t a priority for them. You need to develop that relationship and build it up over time. Helping them set realistic expectations is very important. And we need to do what we can to help them find some sort of competitive outlet. A lot of these kids were very competitive, and now they’ve had an injury and can’t compete. They don’t want to go back to playing just any sport. They want to be able to be competitive, and if you don’t help them find another way to express that, they sort of give up on physical activity altogether,” according to Dr. Whittaker of the University of Alberta in Edmonton.
Dr. Risberg and Dr. Whittaker reported having no financial conflicts of interest.
LAS VEGAS – A variety of evidence-based strategies are available for preventing posttraumatic knee osteoarthritis (KOA) in patients who have already sustained an anterior cruciate ligament (ACL) injury. And they’re generally ignored, according to May Arna Risberg, PhD.
“We have a lot of knowledge. We can use secondary prevention strategies. And here I think we, as physical therapists, physicians, and orthopedic surgeons, are doing a lousy job because we are sending these ACL-injured patients back to sports before they have normalized knee function and quadriceps strength,” said Dr. Risberg, professor of sports medicine at the Norwegian School of Sport Sciences in Oslo.
With no proven disease-modifying therapy for KOA available to date, secondary prevention of posttraumatic KOA is worthy of high-priority status, she said at the World Congress on Osteoarthritis. An estimated 250,00 ACL injuries occur annually in the United States, and up to one-half of affected patients, most of whom are young, active people, will experience a second ACL rupture within the first few years after undergoing their initial reconstruction. This second ACL injury greatly increases their risk of developing posttraumatic KOA within 15-20 years, while they are still relatively young, she said.
Moreover, if the second ACL injury involves meniscus surgery, the 5-year risk of posttraumatic KOA roughly triples to up to 48%.
She highlighted a few effective strategies for preventing posttraumatic KOA in patients who already have an ACL injury.
Avoid reinjury
Dr. Risberg was senior author of a recent report from the prospective Delaware-Oslo Cohort Study involving 106 athletes who underwent ACL reconstruction following injury in what she termed level I sports. These are sports that entail lots of pivoting, jumping, and hard cutting, such as basketball, soccer, and handball.
In the first 2 years after ACL repair, 30% of patients who returned to participation in a level 1 sport experienced an ACL reinjury, compared with just 8% who opted for a lower-level sport. Athletes who returned to a level 1 sport had an adjusted 4.3 times greater ACL reinjury rate than those who didn’t, Dr. Risberg noted at the congress sponsored by the Osteoarthritis Research Society International.
The good news is that this sharply increased reinjury risk was mitigated if return to a level 1 sport was delayed for at least 9 months post surgery and if the patient had regained quadriceps strength comparable to the uninjured side. For every month that return to sport was delayed out until 9 months post ACL reconstruction, the knee reinjury rate was reduced by 51% (Br J Sports Med. 2016;50:804-8).
In a meta-analysis by other investigators of 12 studies including 5,707 participants, weakness of the knee extensor muscles was independently associated with a 1.65 times increased risk of developing KOA (Osteoarthritis Cartilage. 2015 Feb;23[2]:171-7).
Attend to BMI
A discussion of the importance of maintaining a healthy body weight is an important aspect of patient education for athletes with knee injuries. In a cohort study of 988 patients who underwent primary ACL reconstruction, being overweight or obese was associated with a significantly increased risk of subsequent meniscal tears and chondral lesions (Am J Sports Med. 2015 Dec;43[12]:2966-73).
Also, it’s well established that obesity is a risk factor for knee OA, and Canadian investigators have shown that young athletes with a sports-related intra-articular knee injury were 3.75 times more likely to be overweight or obese 3-10 years post injury, compared with matched uninjured controls (Osteoarthritis Cartilage. 2015 Jul;23[7]:1122-9).
Consider prehabilitative exercise training
Dr. Risberg and coinvestigators have reported that preoperative quadriceps muscle strength deficits are predictive of impaired knee function, as measured by the Cincinnati Knee Score 2 years post surgery. She said she believes ACL reconstruction shouldn’t be done until quadriceps muscle strength is at least 80% of that in the uninjured limb (Br J Sports Med. 2009 May;43[5]:371-6). She and her coinvestigators have published the details of a 5-week progressive exercise therapy program in which they have shown results in significantly improved early postoperative knee function (J Orthop Sports Phys Ther. 2010 Nov;40[11]:705-21). They now try to have patients complete the twice-weekly, 5-week program before final decisions are reached regarding whether to have ACL reconstruction.
Test all before okaying return to sport
It’s important to know if patients who have undergone ACL reconstruction have gotten full knee function back before determining if they’re ready for full-on sports participation. In the Delaware-Oslo Cohort Study, patients who delayed their return until at least 9 months after surgery and passed the return-to-sports test had a 5.6% reinjury rate within 2 years, while those who failed the return-to-sports criteria had a 38.2% ACL reinjury rate.
The return-to-sports testing utilized in this study entailed isokinetic quadriceps strength testing, the single hop leg test, the 14-item self-rated Knee Outcome Survey–Activities of Daily Living Scale, and a self-rated Global Rating Scale of perceived function on a 0-100 scale. To be cleared for return to sports, a patient had to demonstrate having regained at least 90% of quadriceps muscle strength and hop performance along with scoring in the normative range on both of the self-rating instruments.
Surgical vs. nonsurgical treatment of ACL rupture
The evidence on this score is conflicting, according to Dr. Risberg. While most physical therapists believe ACL reconstruction doesn’t protect against later development of KOA, as reflected in a meta-analysis of published studies (J Bone Joint Surg Am. 2014 Feb 19;96[4]:292-300), a more recent retrospective comparison of 964 patients with an isolated ACL tear and an equal number of matched controls concluded that patients treated nonoperatively were six times more likely to have been diagnosed with KOA and 16.7 times more likely to have undergone total knee replacement at a mean follow-up of 13.7 years than were those treated with ACL reconstruction (Am J Sports Med. 2016 Jul;44[7]:1699-707).
Dr. Risberg’s fellow panelist Jackie Whittaker, PhD, said that, as long as quadriceps muscle strengthening is a priority, it makes sense to strengthen the hamstring as well, particularly if the ACL reconstruction utilized the hamstring tendon.
“Also, I would add that it’s important to develop a relationship with these ACL-injured people, who are often very young. Preventing a disease that they’re going to get 20 years later isn’t a priority for them. You need to develop that relationship and build it up over time. Helping them set realistic expectations is very important. And we need to do what we can to help them find some sort of competitive outlet. A lot of these kids were very competitive, and now they’ve had an injury and can’t compete. They don’t want to go back to playing just any sport. They want to be able to be competitive, and if you don’t help them find another way to express that, they sort of give up on physical activity altogether,” according to Dr. Whittaker of the University of Alberta in Edmonton.
Dr. Risberg and Dr. Whittaker reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM OARSI 2017
Exercise tops NSAIDs for knee osteoarthritis
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
AT OARSI 2017
Key clinical point:
Major finding: At 12 months of follow-up, patients with knee osteoarthritis who had been assigned to an 8-week structured neuromuscular exercise therapy program had a mean 10.9-point improvement on the KOOS symptom subscale, significantly better than the 3.3-point improvement in patients assigned to primary therapy with NSAIDs and acetaminophen.
Data source: This randomized, single-blind clinical trial included 93 patients with mild to moderate knee osteoarthritis.
Disclosures: The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. The presenter reported having no financial conflicts of interest.
Knee injuries in youth sports bring double whammy
LAS VEGAS – Young people who sustain an intra-articular knee injury while participating in youth sports are not only at increased risk for early posttraumatic osteoarthritis 3-10 years later as young adults, but they also are more prone to develop obesity and other modifiable risk factors for osteoarthritis, according to Jackie Whittaker, PhD.
“It appears that some of these young active individuals, after sustaining an injury which is itself a risk factor for osteoarthritis, are going down a pathway where they’re developing a second risk factor for the disease. This may accelerate the rate at which they get the disease and may very well also accelerate the rate at which the disease progresses after its onset,” Dr. Whittaker of the University of Alberta, Edmonton, said at the World Congress on Osteoarthritis.
It’s well established from other studies that roughly 50% of youth who have a significant knee joint injury for which they seek medical attention go on to develop knee osteoarthritis within 10-15 years. The Alberta study focuses on the years between injury and OA onset in an effort to identify modifiable risk factors and develop interventions to delay or halt progression to the disease. There is a paucity of research regarding this crucial time period, Dr. Whittaker explained at the congress sponsored by the Osteoarthritis Research Society International.
“In Canada, we know that injury during sport and recreation is the No. 1 reason that youth between the ages of 11 and 18 seek medical attention, with an alarming one in three doing so. Knee injuries are among the most common of those injuries,” she said.
At follow-up, 29% of the group with a history of knee injury and 4% of controls already had OA as defined by MRI. The likelihood of MRI evidence of OA was 13.5-fold greater in patients who underwent knee surgery for their injury, compared with controls.
“We saw the highest risk, as expected, in patients with ACL [anterior cruciate ligament] and/or meniscal tears, but we also saw a twofold increased risk of OA in those with seemingly less severe injuries, like grade 1-3 medial and collateral ligament injuries,” said Dr. Whittaker.
“I don’t think we were really shocked that knee injury can lead to structural changes that can be associated with future symptomatic OA, but we were surprised to be seeing that as early as 3-10 years post injury. And we were also seeing greater adiposity, a higher rate of being overweight or obese, reduced physical activity, weaker knee muscular strength, and poorer performance on balance and physical function tests,” she continued.
Indeed, at follow-up the subjects with a history of a youth sports knee injury were 4.4-fold more likely to be in the top quartile of fat mass index, compared with uninjured controls, 5.7-fold more likely to be in the highest quartile for abdominal fat, 2.1 times more likely to be in the lowest quartile for total weekly physical activity, and 2.4-fold more likely to be overweight or obese by body mass index (BMI). They were significantly less aerobically fit as reflected in their performance on the 20-meter shuttle run. And they scored significantly worse on the validated Knee Injury and Osteoarthritis Outcome Score (KOOS), particularly on the knee-related quality of life, pain, and symptom subscales.
“The study is ongoing, but it has already contributed to identification of who we’re probably going to need to target for secondary prevention strategies: obviously, individuals who have torn their ACL and/or their meniscus, as was already well known, but perhaps also individuals that have had less severe injuries, those who have a high BMI or some other indicator of adiposity, and those at risk of becoming physically inactive,” Dr. Whittaker said.
She added that a key take-away message from the study, for which she is coprincipal investigator, is that reduced physical activity on the part of someone with a history of a youth sports knee injury is a big red flag. These patients need to address their modifiable risk factors for OA via physical therapy and rehabilitation, along with receiving education reinforcing the importance of lifelong musculoskeletal health.
“Reduced physical activity is a warning sign. Don’t wait for knee pain,” she emphasized.
The Alberta Youth Prevention in Early OA study is funded by the Canadian Institutes of Health Research and nonprofit organizations. Dr. Whittaker reported having no financial conflicts.
LAS VEGAS – Young people who sustain an intra-articular knee injury while participating in youth sports are not only at increased risk for early posttraumatic osteoarthritis 3-10 years later as young adults, but they also are more prone to develop obesity and other modifiable risk factors for osteoarthritis, according to Jackie Whittaker, PhD.
“It appears that some of these young active individuals, after sustaining an injury which is itself a risk factor for osteoarthritis, are going down a pathway where they’re developing a second risk factor for the disease. This may accelerate the rate at which they get the disease and may very well also accelerate the rate at which the disease progresses after its onset,” Dr. Whittaker of the University of Alberta, Edmonton, said at the World Congress on Osteoarthritis.
It’s well established from other studies that roughly 50% of youth who have a significant knee joint injury for which they seek medical attention go on to develop knee osteoarthritis within 10-15 years. The Alberta study focuses on the years between injury and OA onset in an effort to identify modifiable risk factors and develop interventions to delay or halt progression to the disease. There is a paucity of research regarding this crucial time period, Dr. Whittaker explained at the congress sponsored by the Osteoarthritis Research Society International.
“In Canada, we know that injury during sport and recreation is the No. 1 reason that youth between the ages of 11 and 18 seek medical attention, with an alarming one in three doing so. Knee injuries are among the most common of those injuries,” she said.
At follow-up, 29% of the group with a history of knee injury and 4% of controls already had OA as defined by MRI. The likelihood of MRI evidence of OA was 13.5-fold greater in patients who underwent knee surgery for their injury, compared with controls.
“We saw the highest risk, as expected, in patients with ACL [anterior cruciate ligament] and/or meniscal tears, but we also saw a twofold increased risk of OA in those with seemingly less severe injuries, like grade 1-3 medial and collateral ligament injuries,” said Dr. Whittaker.
“I don’t think we were really shocked that knee injury can lead to structural changes that can be associated with future symptomatic OA, but we were surprised to be seeing that as early as 3-10 years post injury. And we were also seeing greater adiposity, a higher rate of being overweight or obese, reduced physical activity, weaker knee muscular strength, and poorer performance on balance and physical function tests,” she continued.
Indeed, at follow-up the subjects with a history of a youth sports knee injury were 4.4-fold more likely to be in the top quartile of fat mass index, compared with uninjured controls, 5.7-fold more likely to be in the highest quartile for abdominal fat, 2.1 times more likely to be in the lowest quartile for total weekly physical activity, and 2.4-fold more likely to be overweight or obese by body mass index (BMI). They were significantly less aerobically fit as reflected in their performance on the 20-meter shuttle run. And they scored significantly worse on the validated Knee Injury and Osteoarthritis Outcome Score (KOOS), particularly on the knee-related quality of life, pain, and symptom subscales.
“The study is ongoing, but it has already contributed to identification of who we’re probably going to need to target for secondary prevention strategies: obviously, individuals who have torn their ACL and/or their meniscus, as was already well known, but perhaps also individuals that have had less severe injuries, those who have a high BMI or some other indicator of adiposity, and those at risk of becoming physically inactive,” Dr. Whittaker said.
She added that a key take-away message from the study, for which she is coprincipal investigator, is that reduced physical activity on the part of someone with a history of a youth sports knee injury is a big red flag. These patients need to address their modifiable risk factors for OA via physical therapy and rehabilitation, along with receiving education reinforcing the importance of lifelong musculoskeletal health.
“Reduced physical activity is a warning sign. Don’t wait for knee pain,” she emphasized.
The Alberta Youth Prevention in Early OA study is funded by the Canadian Institutes of Health Research and nonprofit organizations. Dr. Whittaker reported having no financial conflicts.
LAS VEGAS – Young people who sustain an intra-articular knee injury while participating in youth sports are not only at increased risk for early posttraumatic osteoarthritis 3-10 years later as young adults, but they also are more prone to develop obesity and other modifiable risk factors for osteoarthritis, according to Jackie Whittaker, PhD.
“It appears that some of these young active individuals, after sustaining an injury which is itself a risk factor for osteoarthritis, are going down a pathway where they’re developing a second risk factor for the disease. This may accelerate the rate at which they get the disease and may very well also accelerate the rate at which the disease progresses after its onset,” Dr. Whittaker of the University of Alberta, Edmonton, said at the World Congress on Osteoarthritis.
It’s well established from other studies that roughly 50% of youth who have a significant knee joint injury for which they seek medical attention go on to develop knee osteoarthritis within 10-15 years. The Alberta study focuses on the years between injury and OA onset in an effort to identify modifiable risk factors and develop interventions to delay or halt progression to the disease. There is a paucity of research regarding this crucial time period, Dr. Whittaker explained at the congress sponsored by the Osteoarthritis Research Society International.
“In Canada, we know that injury during sport and recreation is the No. 1 reason that youth between the ages of 11 and 18 seek medical attention, with an alarming one in three doing so. Knee injuries are among the most common of those injuries,” she said.
At follow-up, 29% of the group with a history of knee injury and 4% of controls already had OA as defined by MRI. The likelihood of MRI evidence of OA was 13.5-fold greater in patients who underwent knee surgery for their injury, compared with controls.
“We saw the highest risk, as expected, in patients with ACL [anterior cruciate ligament] and/or meniscal tears, but we also saw a twofold increased risk of OA in those with seemingly less severe injuries, like grade 1-3 medial and collateral ligament injuries,” said Dr. Whittaker.
“I don’t think we were really shocked that knee injury can lead to structural changes that can be associated with future symptomatic OA, but we were surprised to be seeing that as early as 3-10 years post injury. And we were also seeing greater adiposity, a higher rate of being overweight or obese, reduced physical activity, weaker knee muscular strength, and poorer performance on balance and physical function tests,” she continued.
Indeed, at follow-up the subjects with a history of a youth sports knee injury were 4.4-fold more likely to be in the top quartile of fat mass index, compared with uninjured controls, 5.7-fold more likely to be in the highest quartile for abdominal fat, 2.1 times more likely to be in the lowest quartile for total weekly physical activity, and 2.4-fold more likely to be overweight or obese by body mass index (BMI). They were significantly less aerobically fit as reflected in their performance on the 20-meter shuttle run. And they scored significantly worse on the validated Knee Injury and Osteoarthritis Outcome Score (KOOS), particularly on the knee-related quality of life, pain, and symptom subscales.
“The study is ongoing, but it has already contributed to identification of who we’re probably going to need to target for secondary prevention strategies: obviously, individuals who have torn their ACL and/or their meniscus, as was already well known, but perhaps also individuals that have had less severe injuries, those who have a high BMI or some other indicator of adiposity, and those at risk of becoming physically inactive,” Dr. Whittaker said.
She added that a key take-away message from the study, for which she is coprincipal investigator, is that reduced physical activity on the part of someone with a history of a youth sports knee injury is a big red flag. These patients need to address their modifiable risk factors for OA via physical therapy and rehabilitation, along with receiving education reinforcing the importance of lifelong musculoskeletal health.
“Reduced physical activity is a warning sign. Don’t wait for knee pain,” she emphasized.
The Alberta Youth Prevention in Early OA study is funded by the Canadian Institutes of Health Research and nonprofit organizations. Dr. Whittaker reported having no financial conflicts.
Key clinical point:
Major finding: Just 3-10 years after sustaining a knee injury while participating in youth sports, 29% of young people already have MRI evidence of knee osteoarthritis.
Data source: The Alberta Youth Prevention in Early OA study, an ongoing prospective 200-subject longitudinal cohort study of the long-term consequences of sports-related knee injury.
Disclosures: The study is funded by the Canadian Institutes of Health Research and nonprofit organizations. The presenter reported having no financial conflicts.
Think twice before recommending partial meniscectomy
LAS VEGAS – Patients with knee osteoarthritis (OA) and a meniscal tear who underwent arthroscopic partial meniscectomy (APM) subsequently experienced accelerated structural progression of their OA, compared with those randomized to physical therapy alone in the randomized METEOR trial.
“In discussing treatment options for symptomatic meniscal tear, patients and providers must weigh the potential benefits and risks of arthroscopic partial meniscectomy, including this increased risk of structural progression,” Jamie E. Collins, PhD, said at the World Congress on Osteoarthritis.
A thorough physician-patient discussion also needs to mention that several large randomized trials have suggested that patients with meniscal tear and osteoarthritic changes experience similar pain relief with APM plus physical therapy (PT) as compared with PT alone, she added at the congress sponsored by the Osteoarthritis Research Society International.
The METEOR trial was a seven-center U.S. randomized trial of APM plus PT or PT alone in patients with MRI or radiographic evidence of OA changes, a meniscal tear on MRI, and mechanical knee symptoms. Dr. Collins reported on 176 randomized patients with baseline and 18-month follow-up MRIs read by a specialist musculoskeletal radiologist. This analysis excluded the 37 patients in the PT group who crossed over to APM within 6 months after randomization.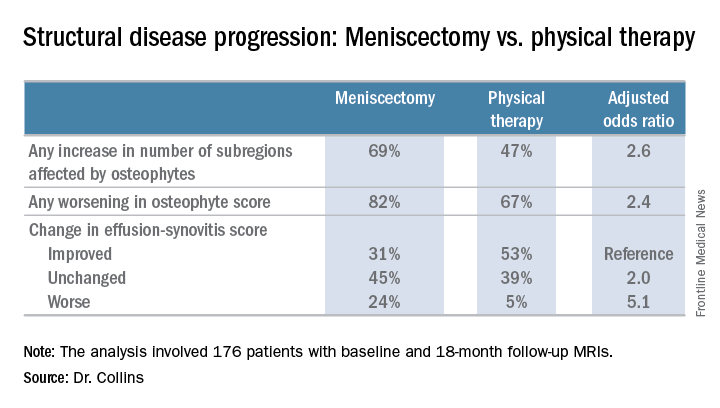
There was no significant difference between the two treatment groups in changes in bone marrow lesions or Hoffa-synovitis.
A secondary analysis that incorporated the 37 crossovers from PT to APM within 6 months showed similarly accelerated OA progression after arthroscopic surgery.
“Future work should focus on determining whether this accelerated structural progression is associated with changes in symptoms and ultimately with a higher risk of total knee replacement. In other words, is 2+ structural worsening something that’s noticeable or important for patients?” Dr. Collins concluded.
She reported having no financial conflicts regarding her study, which was sponsored by Brigham and Women’s Hospital.
LAS VEGAS – Patients with knee osteoarthritis (OA) and a meniscal tear who underwent arthroscopic partial meniscectomy (APM) subsequently experienced accelerated structural progression of their OA, compared with those randomized to physical therapy alone in the randomized METEOR trial.
“In discussing treatment options for symptomatic meniscal tear, patients and providers must weigh the potential benefits and risks of arthroscopic partial meniscectomy, including this increased risk of structural progression,” Jamie E. Collins, PhD, said at the World Congress on Osteoarthritis.
A thorough physician-patient discussion also needs to mention that several large randomized trials have suggested that patients with meniscal tear and osteoarthritic changes experience similar pain relief with APM plus physical therapy (PT) as compared with PT alone, she added at the congress sponsored by the Osteoarthritis Research Society International.
The METEOR trial was a seven-center U.S. randomized trial of APM plus PT or PT alone in patients with MRI or radiographic evidence of OA changes, a meniscal tear on MRI, and mechanical knee symptoms. Dr. Collins reported on 176 randomized patients with baseline and 18-month follow-up MRIs read by a specialist musculoskeletal radiologist. This analysis excluded the 37 patients in the PT group who crossed over to APM within 6 months after randomization.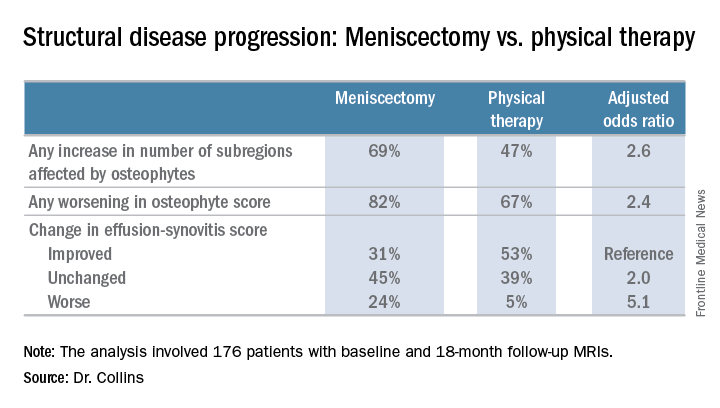
There was no significant difference between the two treatment groups in changes in bone marrow lesions or Hoffa-synovitis.
A secondary analysis that incorporated the 37 crossovers from PT to APM within 6 months showed similarly accelerated OA progression after arthroscopic surgery.
“Future work should focus on determining whether this accelerated structural progression is associated with changes in symptoms and ultimately with a higher risk of total knee replacement. In other words, is 2+ structural worsening something that’s noticeable or important for patients?” Dr. Collins concluded.
She reported having no financial conflicts regarding her study, which was sponsored by Brigham and Women’s Hospital.
LAS VEGAS – Patients with knee osteoarthritis (OA) and a meniscal tear who underwent arthroscopic partial meniscectomy (APM) subsequently experienced accelerated structural progression of their OA, compared with those randomized to physical therapy alone in the randomized METEOR trial.
“In discussing treatment options for symptomatic meniscal tear, patients and providers must weigh the potential benefits and risks of arthroscopic partial meniscectomy, including this increased risk of structural progression,” Jamie E. Collins, PhD, said at the World Congress on Osteoarthritis.
A thorough physician-patient discussion also needs to mention that several large randomized trials have suggested that patients with meniscal tear and osteoarthritic changes experience similar pain relief with APM plus physical therapy (PT) as compared with PT alone, she added at the congress sponsored by the Osteoarthritis Research Society International.
The METEOR trial was a seven-center U.S. randomized trial of APM plus PT or PT alone in patients with MRI or radiographic evidence of OA changes, a meniscal tear on MRI, and mechanical knee symptoms. Dr. Collins reported on 176 randomized patients with baseline and 18-month follow-up MRIs read by a specialist musculoskeletal radiologist. This analysis excluded the 37 patients in the PT group who crossed over to APM within 6 months after randomization.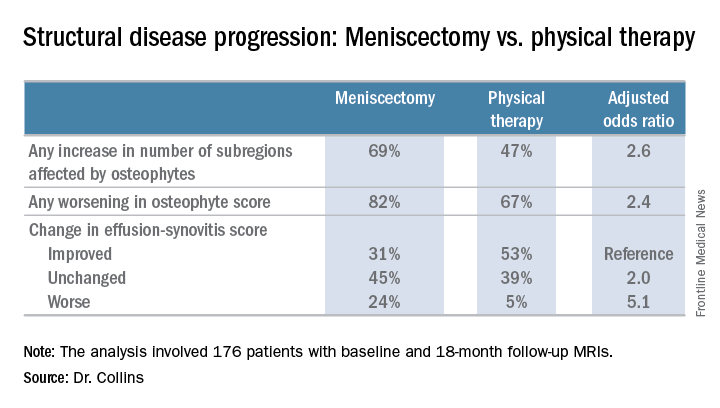
There was no significant difference between the two treatment groups in changes in bone marrow lesions or Hoffa-synovitis.
A secondary analysis that incorporated the 37 crossovers from PT to APM within 6 months showed similarly accelerated OA progression after arthroscopic surgery.
“Future work should focus on determining whether this accelerated structural progression is associated with changes in symptoms and ultimately with a higher risk of total knee replacement. In other words, is 2+ structural worsening something that’s noticeable or important for patients?” Dr. Collins concluded.
She reported having no financial conflicts regarding her study, which was sponsored by Brigham and Women’s Hospital.
AT OARSI 2017
Key clinical point:
Major finding: Surgically treated patients were 2.6 times more likely to demonstrate MRI evidence of structural disease progression at 18 months than those who received physical therapy alone.
Data source: This analysis from the multicenter METEOR trial included 176 patients with a symptomatic meniscal tear.
Disclosures: The presenter reported having no financial conflicts regarding her study, which was sponsored by Brigham and Women’s Hospital.