User login
American Society for Reproductive Medicine (ASRM)
Despite incentives, many couples aim for twins with IVF
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
BOSTON – For many couples undergoing in vitro fertilization, the desire to rapidly complete a family apparently outweighs concerns over medical risks and the lure of cash savings, according to Dr. Fady I. Sharara.
Despite being offered free gonadotropins (Menopur) for one cycle and a free year of freezing and storage of all extra blastocysts, 48% of couples who were paying out of pocket opted for multiple- rather than single-embryo transfer, and 23.5% of those who had at least one reproductive cycle covered by insurance also refused the free offer, said Dr. Sharara, a reproductive endocrinologist and infertility specialist in group practice in Reston.
The medication alone could cost as much as $6,000, with freezing adding another $1,800 or so and storage, approximately $750, Dr. Sharara said in an interview.
The patients made the decision to proceed with multiples despite being informed about the higher risk of maternal, fetal, and perinatal problems.
"Twins are associated with significant morbidities: early delivery, cerebral palsy, mental retardation if they’re delivered very early, diabetes in the mom, and hypertension, so [there are] a lot of issues, and I tell my patients that twins are not twice the fun," he said.
"We were not meant to bear litters," he added.
New mothers of twins are more susceptible to postpartum depression, especially if they do not have help at home, and parents of twins have been shown in at least one study (Obstet. Gynecol. 2011;117:892-7) to be slightly but significantly more likely to get divorced than parents of singletons.
"One is hard enough; two at the same time is a killer for a lot of people. Some marriages don’t survive this," he said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Sharara offered patients – all women under age 38 who were proceeding with assisted reproductive technology (ART) – the chance to participate in the study. The free drugs and services were offered without regard to the patient’s insurance coverage or to her ovarian reserve status.
Of 48 couples offered a single-embryo transfer, 18 refused to take part in the trial. Of those who had double-embryo transfer, the ongoing pregnancy rate (approximately 10 weeks’ duration) was 80%, compared with 58.3% for the women who had single-embryo transfer, a difference that was not significant. Dr. Sharara noted, however, that two additional patients who had single-embryo transfer are now pregnant, and he estimated that the updated ongoing pregnancy rate for singletons will be about 60%-65%.
In all, 7 of the 18 women who opted for dual-embryo transfer are pregnant with twins, whereas none of the single-embryo pregnancies have resulted in twins. In a series of 500 single-embryo transfers at his center, the rate of twin pregnancies was 1.5%.
Dr. Sharara noted that some of the women offered single-embryo transfer did not meet the ASRM definitions for good-prognosis patients, including women aged 35 years and older who had a failed prior reproductive cycle, one ovary, prior uterine surgery, or diminished ovarian reserve.
One of the hardest parts of his job, he said, is getting the message through.
"When I sit down and talk to patients about the risks of having twins, they don’t want to hear it," Dr. Sharara said.
The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Of 48 couples offered approximately $8,500 in savings if they opted for single-embryo transfer, 18 refused and chose dual transfers.
Data source: An ongoing, prospective single-center study of patient attitudes regarding the relative merits of single-embryo transfer in 48 couples.
Disclosures: The study was supported by Ferring Pharmaceuticals. Dr. Sharara disclosed receiving grants from the company.
Many women physicians regret delaying reproduction
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
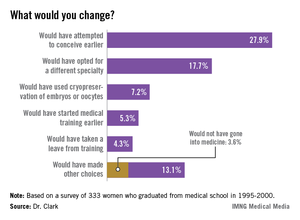
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
The fact that 25% of physicians have infertility is a slight increase over the percentage of general population (15%), and it reinforces to physicians that they are not immune to the diseases we treat.
The study utilizes graduates from medical school between 1995 and 2000, and it doesn't reflect the working environment that today's graduates face, 13-18 years later. Duty hours, Gen X graduates, and the increasing number of women in medicine, especially in obstetrics and gynecology, have changed the workplace. Residents and young physicians in practice are no longer willing to work the hours that their predecessors did. To me, this is mostly a positive trend, as the desire for work-life balance is something young physicians are teaching older physicians, by example. In my own department, we see many physicians of all ages leading fuller, happier lives because of these changes. That is not to say that being a resident or young physician in practice and being pregnant is easy. It is just more acceptable than it was for the physicians in the study cohort.
 |
| Dr. David Forstein |
As to the option of oocyte freezing early in their career, this option is becoming more and more available to women. We have seen a number of women in their mid- to late 20s, with no partner in place, freeze oocytes "just in case." As the technology improves and allows higher pregnancy rates from unstimulated oocytes, more women will choose this option. Currently, the best pregnancy rates come from frozen embryos, then from oocytes frozen following an ovarian stimulation cycle. The stimulation still requires multiple medication injections, and ultrasound and hormone-level monitoring. These requirements are an additional hurdle for women with busy schedules to navigate.
The cost of an oocyte harvest is significant and not often covered by insurance or, even if it is covered, there are copays and deductibles that make it difficult for residents to manage. This is a challenge to which there are no easy answers.
In my residency program director's role, I have frequently been challenged by resident and attending physicians about what the response to "another pregnant resident" should be. Often frustration ensues amongst the team because a maternity leave stretches the manpower of a program. In my mind, the appropriate response is that as ob.gyns., we should celebrate every pregnancy! If we can't lead by example about how to treat professional women during pregnancy and with their young families, who is going to do it? Respect for the challenge of multitasking a residency or a practice and a family is the way forward.
David Forstein, D.O., is an infertility specialist who is associate professor of obstetrics and gynecology at the University of South Carolina, Greenville. He said he had no financial disclosures relevant to this commentary.
Ob.Gyns. should be leading the way
Regarding this intriguing research performed by Clark and her colleagues, these women physicians had their first child about 7 years later than women in the general population, and just over a quarter of respondents indicated, in retrospect, that they would have attempted to conceive earlier. This paper highlights the bind that professional women often find themselves in - that there is no "ideal" time to have a child.
 |
| Dr. Eve Espey |
Women pursuing professions may be discouraged from childbearing during their education and may hear the message that it is irresponsible to detract from their study time or professional development by having children during their undergraduate education or medical school. During residency, the "system" is not designed to accommodate absences, and fellow residents usually absorb the workload for women taking maternity leave, sometimes leading to resentment and an unspoken bias against childbearing.
Our society is only beginning to accommodate the women who wish to "have it all," both professional fulfillment in a rewarding career and the personal happiness that comes with parenthood.
As women's physicians, ob.gyns. should lead the way in encouraging women professionals to have children whenever during their professional development or careers they see fit, whether that be in college, medical school, residency, or beyond. Because there is no "ideal" time, we should support women in their personal and professional fulfillment, and develop flexible systems that do not punish women for electing to have children at any point in their reproductive lives.
Eve Espey, M.D., is an associate professor of obstetrics and gynecology at the University of New Mexico, Albuquerque. She said she had no financial disclosures relevant to this commentary.
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
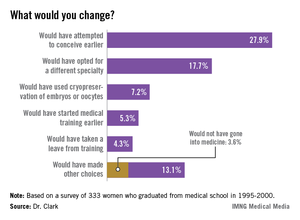
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
BOSTON – Many female physicians say that if they had to do it over again, they might have tried to have children sooner, chosen a different specialty, or elected to have embryos frozen "just in case" they had later fertility problems, an investigator said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Dr. Natalie A. Clark and her colleagues surveyed a random sample of female physicians in the United States to ask about their choices for timing of conception, their basic knowledge of reproductive limitations, and how reproductive choices factor into their professional and personal decision making. The investigators randomly selected 600 women who graduated from medical school from 1995 through 2000 from the American Medical Association (AMA) physicians’ database, and mailed surveys to them. A total of 333 (55.5%) responded.
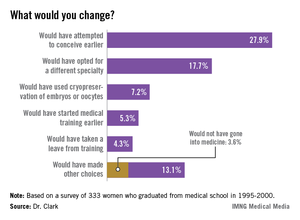
Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training. Of the 13.1% who said they would have made other, unspecified choices, 3.6% independently reported that they would not have gone into medicine.
The survey of female physicians highlights the unique challenges that women of childbearing age face when trying to balance the demands of education, training, and career advancement, said Dr. Clark, a third-year resident at the University of Michigan department of obstetrics and gynecology in Ann Arbor.
"We have a number of highly educated patients who come into our clinic who have finished their MDs or PhDs, and have done a great amount of postgraduate work, and they present at very late reproductive ages. They say, "I’m ready to start reproducing, and I don’t want to be too aggressive, but what can I do?’ – not fully realizing that they’ve missed their ideal reproductive window," Dr. Clark said in an interview.
The majority of respondents (55%) work in specialties for women, children, and families, including family medicine, obstetrics and gynecology, and pediatrics; 31% work in other medical specialties; 10% in hospital-based specialties; and 4% in surgical specialties.
In all, 80% of the respondents said they had attempted to conceive, and 77% had at least one biological child. The physicians on average had their first child 7.4 years later than did women in the general population, according to data from the Centers for Disease Control and Prevention.
One-fourth (25%) of all respondents had been diagnosed with infertility. Ovulatory dysfunction was the most common cause, followed by male factor, age-related diminished ovarian reserve, endometriosis, tubal factor, and uterine factor.
"Despite having a medical background, 44% of infertile respondents were surprised about their diagnosis of infertility," Dr. Clark said. In every age range, physicians consistently underestimated their chances for conceiving, she added.
"I think that if we can change the culture of medicine such that we can support those decisions at a biologically advantageous time point, it could change the field of medicine," Dr. Clark said.
The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Asked whether they would in retrospect have changed anything about their reproductive choices, 27.9% of female physicians said they would have attempted to conceive earlier, 17.7% would have opted for a different specialty, 7.2% would have used cryopreservation of embryos or oocytes, 5.3% would have started medical training earlier, and 4.3% would have taken a leave from training.
Data source: Mailed survey of 333 U.S. women physicians who graduated from medical school from 1995 through 2000.
Disclosures: The study was supported by a grant from the AMA Joan F. Giambalvo Memorial Scholarship Fund. Dr. Clark was a 2012 recipient of a research award from the fund.
ART linked to increases in risk of some congenital malformations
BOSTON – Assisted reproductive technologies are associated with a small but significant risk for congenital malformations in some organ systems, reported investigators from a consortium of Nordic countries at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Singleton children born to parents who used assisted reproductive technology (ART) were significantly more likely than were children born through spontaneous pregnancies to have malformations of the heart, gastrointestinal tract, or urinary tract, reported Dr. Anna-Karina Aaris Henningsen of the Fertility Clinic at the Rigshospitalet in Copenhagen.
Combined data from the extensive medical registries in Denmark, Sweden, Norway, and Finland showed that, compared with controls, singletons born with the help of ART had a 20% increase in risk for any heart malformation, 56% increase in risk for gastrointestinal anomalies, and 49% increase in risk for urinary tract malformations.
In contrast, congenital malformations of the nervous system, abdominal wall, genitals, orofacial region, limbs, or chromosomes were not more common in ART-conceived children than in spontaneously conceived controls, the investigators found.
"It’s still a very small increased risk, and there are many things we can’t answer yet, things we need to look into," Dr. Henningsen said, speaking on behalf of colleagues in the CoNARTas Study Group.
For example, it’s unclear whether the differences might be a causal effect of ART or related to underlying fertility problems of the couples using ART. In addition, there may be differences in rates of malformations between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) techniques, or between fresh- and frozen-embryo transfer methods, she said.
In the matched cohort study, the authors also found that ART was associated with a small but significant risk for placental abruption in both singleton and twin pregnancies, compared with unassisted pregnancies, findings that were consistent across the Nordic countries.
The authors looked at population-based data on 58,714 singletons and 27,919 twins born after the introduction of IVF, ICSI, and frozen-embryo transfer in each of the participating countries. Data on ART came from national ART registers. Singletons born from ART pregnancies were matched on the mother’s parity and year of birth with a fourfold larger control group of spontaneously conceived singletons. All spontaneously conceived twins born during the study period also were counted as controls.
They used the European surveillance of congenital anomalies (EUROCAT) system to classify malformations and group them according to organ system.
In analyses looking at all children born after ART – both twins and singletons – the odds ratio for congenital heart malformations (such as common arterial truncus, transposition of great vessels, presence of a single ventricle, atrioventricular septal defect, etc.) was 1.12, with a confidence interval indicating significance. No other organ system anomalies, however, were associated with ART in the overall population.
In a multivariate analysis controlling for mother’s parity, year of birth, maternal age, child’s sex and country, the authors found that ART in singletons was associated with an odds ratio of 1.20 for congenital heart malformations, 1.56 for gastrointestinal malformations (esophageal atresia, duodenal atresia or stenosis, etc.), and 1.49 for urogenital malformations (such as bilateral renal agenesis, renal dysplasia, or congenital hydronephrosis).
In the question-and-answer portion following Dr. Henningsen’s presentation, an audience member asked whether ascertainment bias might account for the differences seen, because ART-born children may be scrutinized more closely than are spontaneously-born children for congenital malformations.
"If the child has a major malformation, it will be registered, regardless if it’s an ART child or a spontaneously conceived child," she replied.
The study was supported by the European Society of Human Reproduction and Embryology (ESHRE), the University of Copenhagen, the Danish Agency for Science, Technology and Innovation, and the Nordic Federation of Obstetrics and Gynecology (NFOG). Dr. Henningsen reported having no conflict of interest disclosures.
BOSTON – Assisted reproductive technologies are associated with a small but significant risk for congenital malformations in some organ systems, reported investigators from a consortium of Nordic countries at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Singleton children born to parents who used assisted reproductive technology (ART) were significantly more likely than were children born through spontaneous pregnancies to have malformations of the heart, gastrointestinal tract, or urinary tract, reported Dr. Anna-Karina Aaris Henningsen of the Fertility Clinic at the Rigshospitalet in Copenhagen.
Combined data from the extensive medical registries in Denmark, Sweden, Norway, and Finland showed that, compared with controls, singletons born with the help of ART had a 20% increase in risk for any heart malformation, 56% increase in risk for gastrointestinal anomalies, and 49% increase in risk for urinary tract malformations.
In contrast, congenital malformations of the nervous system, abdominal wall, genitals, orofacial region, limbs, or chromosomes were not more common in ART-conceived children than in spontaneously conceived controls, the investigators found.
"It’s still a very small increased risk, and there are many things we can’t answer yet, things we need to look into," Dr. Henningsen said, speaking on behalf of colleagues in the CoNARTas Study Group.
For example, it’s unclear whether the differences might be a causal effect of ART or related to underlying fertility problems of the couples using ART. In addition, there may be differences in rates of malformations between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) techniques, or between fresh- and frozen-embryo transfer methods, she said.
In the matched cohort study, the authors also found that ART was associated with a small but significant risk for placental abruption in both singleton and twin pregnancies, compared with unassisted pregnancies, findings that were consistent across the Nordic countries.
The authors looked at population-based data on 58,714 singletons and 27,919 twins born after the introduction of IVF, ICSI, and frozen-embryo transfer in each of the participating countries. Data on ART came from national ART registers. Singletons born from ART pregnancies were matched on the mother’s parity and year of birth with a fourfold larger control group of spontaneously conceived singletons. All spontaneously conceived twins born during the study period also were counted as controls.
They used the European surveillance of congenital anomalies (EUROCAT) system to classify malformations and group them according to organ system.
In analyses looking at all children born after ART – both twins and singletons – the odds ratio for congenital heart malformations (such as common arterial truncus, transposition of great vessels, presence of a single ventricle, atrioventricular septal defect, etc.) was 1.12, with a confidence interval indicating significance. No other organ system anomalies, however, were associated with ART in the overall population.
In a multivariate analysis controlling for mother’s parity, year of birth, maternal age, child’s sex and country, the authors found that ART in singletons was associated with an odds ratio of 1.20 for congenital heart malformations, 1.56 for gastrointestinal malformations (esophageal atresia, duodenal atresia or stenosis, etc.), and 1.49 for urogenital malformations (such as bilateral renal agenesis, renal dysplasia, or congenital hydronephrosis).
In the question-and-answer portion following Dr. Henningsen’s presentation, an audience member asked whether ascertainment bias might account for the differences seen, because ART-born children may be scrutinized more closely than are spontaneously-born children for congenital malformations.
"If the child has a major malformation, it will be registered, regardless if it’s an ART child or a spontaneously conceived child," she replied.
The study was supported by the European Society of Human Reproduction and Embryology (ESHRE), the University of Copenhagen, the Danish Agency for Science, Technology and Innovation, and the Nordic Federation of Obstetrics and Gynecology (NFOG). Dr. Henningsen reported having no conflict of interest disclosures.
BOSTON – Assisted reproductive technologies are associated with a small but significant risk for congenital malformations in some organ systems, reported investigators from a consortium of Nordic countries at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
Singleton children born to parents who used assisted reproductive technology (ART) were significantly more likely than were children born through spontaneous pregnancies to have malformations of the heart, gastrointestinal tract, or urinary tract, reported Dr. Anna-Karina Aaris Henningsen of the Fertility Clinic at the Rigshospitalet in Copenhagen.
Combined data from the extensive medical registries in Denmark, Sweden, Norway, and Finland showed that, compared with controls, singletons born with the help of ART had a 20% increase in risk for any heart malformation, 56% increase in risk for gastrointestinal anomalies, and 49% increase in risk for urinary tract malformations.
In contrast, congenital malformations of the nervous system, abdominal wall, genitals, orofacial region, limbs, or chromosomes were not more common in ART-conceived children than in spontaneously conceived controls, the investigators found.
"It’s still a very small increased risk, and there are many things we can’t answer yet, things we need to look into," Dr. Henningsen said, speaking on behalf of colleagues in the CoNARTas Study Group.
For example, it’s unclear whether the differences might be a causal effect of ART or related to underlying fertility problems of the couples using ART. In addition, there may be differences in rates of malformations between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) techniques, or between fresh- and frozen-embryo transfer methods, she said.
In the matched cohort study, the authors also found that ART was associated with a small but significant risk for placental abruption in both singleton and twin pregnancies, compared with unassisted pregnancies, findings that were consistent across the Nordic countries.
The authors looked at population-based data on 58,714 singletons and 27,919 twins born after the introduction of IVF, ICSI, and frozen-embryo transfer in each of the participating countries. Data on ART came from national ART registers. Singletons born from ART pregnancies were matched on the mother’s parity and year of birth with a fourfold larger control group of spontaneously conceived singletons. All spontaneously conceived twins born during the study period also were counted as controls.
They used the European surveillance of congenital anomalies (EUROCAT) system to classify malformations and group them according to organ system.
In analyses looking at all children born after ART – both twins and singletons – the odds ratio for congenital heart malformations (such as common arterial truncus, transposition of great vessels, presence of a single ventricle, atrioventricular septal defect, etc.) was 1.12, with a confidence interval indicating significance. No other organ system anomalies, however, were associated with ART in the overall population.
In a multivariate analysis controlling for mother’s parity, year of birth, maternal age, child’s sex and country, the authors found that ART in singletons was associated with an odds ratio of 1.20 for congenital heart malformations, 1.56 for gastrointestinal malformations (esophageal atresia, duodenal atresia or stenosis, etc.), and 1.49 for urogenital malformations (such as bilateral renal agenesis, renal dysplasia, or congenital hydronephrosis).
In the question-and-answer portion following Dr. Henningsen’s presentation, an audience member asked whether ascertainment bias might account for the differences seen, because ART-born children may be scrutinized more closely than are spontaneously-born children for congenital malformations.
"If the child has a major malformation, it will be registered, regardless if it’s an ART child or a spontaneously conceived child," she replied.
The study was supported by the European Society of Human Reproduction and Embryology (ESHRE), the University of Copenhagen, the Danish Agency for Science, Technology and Innovation, and the Nordic Federation of Obstetrics and Gynecology (NFOG). Dr. Henningsen reported having no conflict of interest disclosures.
AT THE JOINT IFFS/ASRM ANNUAL MEETING
Major finding: Assisted reproductive technology in singletons was associated with an odds ratio of 1.20 for congenital heart malformations, 1.56 for gastrointestinal malformations, and 1.49 for urogenital malformations
Data source: Population-based cohort study of 58,714 singletons and 27,919 twins born in Denmark, Finland, Norway, and Sweden.
Disclosures: The study was supported by the ESHRE, the University of Copenhagen, the Danish Agency for Science, Technology and Innovation, and the NFOG. Dr. Henningsen reported having no conflict of interest disclosures.
Oocyte donations in United States rise, with good results
BOSTON – A substantial increase in the number of donor oocyte cycles in the United States from 2000 to 2010 was accompanied by an increase in good perinatal outcomes, reported investigators at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A review of data from 93% of all fertility centers in the United States showed that the annual number of reproductive cycles using donor rather than autologous oocytes grew from 10,801 in 2000, to 18,306 in 2010.
The trend was accompanied by increases in the proportion of cycles using frozen rather than fresh embryos, as well as elective single-embryo transfer (eSET) vs. multiple transfers, said Dr. Jennifer F. Kawwass, a reproductive endocrinology and infertility fellow at Emory University in Atlanta, and her colleagues. The findings were published simultaneously in JAMA online (2013 [doi:10.1001/jama.2013.280924]).
The data show that single-embryo transfers were associated with a more than twofold improvement in the odds of a good outcome, compared with multiple transfers, and that embryo transfer at day 5 vs. day 3 was associated with a smaller but still significant increase in the chance of a favorable outcome.
Factors associated with lower likelihood of success included tubal- or uterine-factor infertility, and race/ethnicity with non-Hispanic black women having about half the number of successful pregnancies as non-Hispanic white women had.
Societal trends
The findings reflect both societal trends and the evolution of assisted reproductive technologies (ART), commented Dr. William D. Schlaff, Paul and Eloise Bowers Professor and chair of obstetrics and gynecology at Thomas Jefferson University in Philadelphia.
"This shows that people who are doing ART, particularly in the United States, are really putting weight behind the goal of having a single, healthy term pregnancy by transferring a single embryo," he said in an interview.
The data also show that, despite the attendant risks of multiple-fetus pregnancies for mothers and children, some patients may have better outcomes with multiple-embryo transfers.
"If you can identify a subgroup of people with a very good prognosis, particularly if they’re on the fence as to how they would like to proceed, I think you can help them make decisions that would minimize the risk of higher multiples or twins, while not affecting their overall prognosis," Dr. Schlaff said.
The data suggest that oocyte donation is here to stay for the foreseeable future, Dr. Evan R. Myers of the department of obstetrics and gynecology at Duke University in Durham, N.C., noted in a JAMA editorial (2013 [doi:10.1001/jama.2013.280925]).
"More complete data on both short-and long-term outcomes of donation are needed so donors can make truly informed choices and, once those data are available, mechanisms can be put in place to ensure that the donor recruitment and consent process at clinics is conducted according to the highest ethical standards," he wrote.
Dr. Kawwass and her colleagues drew on data reported by fertility centers under mandate to the Centers for Disease Control and Prevention’s National ART Surveillance System. They defined a good perinatal outcome as a singleton born live at 37 weeks’ gestation or later, weighing at least 2,500 g.
Data from the 443 reporting clinics showed the increase in donor oocyte cycles noted before. In addition, the proportion of cycles using frozen embryos increased from 26.7% in 2000 to 40.3% in 2010, and the number of cycles with eSET grew over the same period from just 0.8% to 14.5% (P less than .001 for both trends).
In 2000, 18.5% of cycles resulted in good perinatal outcomes; by 2010, the percentage of good outcomes had improved to 24.4% (P less than .001).
There was no change over time in the mean age of either donors (28 years), or recipients (41 years).
In multivariate analysis controlling for recipient and donor age, race, infertility diagnosis, and number of prior pregnancies, miscarriages, preterm and full-term births and other factors, factors significantly favoring a good outcome were day 5 embryo transfer (adjusted odds ratio 1.17) and eSET (adjusted OR, 2.32).
Conversely, factors negatively associated with good outcomes were tubal-factor infertility (adjusted OR, 0.72), uterine-factor infertility (adjusted OR, 0.74), and non-Hispanic black recipient race/ethnicity (adjusted OR, 0.48).
Sister, can you spare an egg?
In his editorial, Dr. Myers noted that the surveillance data do not include data on health outcomes for oocyte donors.
"Donors are at risk for all of the complications associated with ovulation induction, including the potentially life-threatening ovarian hyperstimulation syndrome. In addition, there is uncertainty about longer-term issues such as effects on the donor’s own fertility or the need to inform recipients about the discovery of health issues not known at the time of donation," he wrote.
The study was supported by the CDC. The authors reported having no conflict of interest disclosures. Dr. Myers disclosed serving as a consultant for AbbVie, Merck, and the CDC, and receiving grants or grants pending from the Patient-Centered Outcomes Research Institute and Hologic-GenProbe.
BOSTON – A substantial increase in the number of donor oocyte cycles in the United States from 2000 to 2010 was accompanied by an increase in good perinatal outcomes, reported investigators at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A review of data from 93% of all fertility centers in the United States showed that the annual number of reproductive cycles using donor rather than autologous oocytes grew from 10,801 in 2000, to 18,306 in 2010.
The trend was accompanied by increases in the proportion of cycles using frozen rather than fresh embryos, as well as elective single-embryo transfer (eSET) vs. multiple transfers, said Dr. Jennifer F. Kawwass, a reproductive endocrinology and infertility fellow at Emory University in Atlanta, and her colleagues. The findings were published simultaneously in JAMA online (2013 [doi:10.1001/jama.2013.280924]).
The data show that single-embryo transfers were associated with a more than twofold improvement in the odds of a good outcome, compared with multiple transfers, and that embryo transfer at day 5 vs. day 3 was associated with a smaller but still significant increase in the chance of a favorable outcome.
Factors associated with lower likelihood of success included tubal- or uterine-factor infertility, and race/ethnicity with non-Hispanic black women having about half the number of successful pregnancies as non-Hispanic white women had.
Societal trends
The findings reflect both societal trends and the evolution of assisted reproductive technologies (ART), commented Dr. William D. Schlaff, Paul and Eloise Bowers Professor and chair of obstetrics and gynecology at Thomas Jefferson University in Philadelphia.
"This shows that people who are doing ART, particularly in the United States, are really putting weight behind the goal of having a single, healthy term pregnancy by transferring a single embryo," he said in an interview.
The data also show that, despite the attendant risks of multiple-fetus pregnancies for mothers and children, some patients may have better outcomes with multiple-embryo transfers.
"If you can identify a subgroup of people with a very good prognosis, particularly if they’re on the fence as to how they would like to proceed, I think you can help them make decisions that would minimize the risk of higher multiples or twins, while not affecting their overall prognosis," Dr. Schlaff said.
The data suggest that oocyte donation is here to stay for the foreseeable future, Dr. Evan R. Myers of the department of obstetrics and gynecology at Duke University in Durham, N.C., noted in a JAMA editorial (2013 [doi:10.1001/jama.2013.280925]).
"More complete data on both short-and long-term outcomes of donation are needed so donors can make truly informed choices and, once those data are available, mechanisms can be put in place to ensure that the donor recruitment and consent process at clinics is conducted according to the highest ethical standards," he wrote.
Dr. Kawwass and her colleagues drew on data reported by fertility centers under mandate to the Centers for Disease Control and Prevention’s National ART Surveillance System. They defined a good perinatal outcome as a singleton born live at 37 weeks’ gestation or later, weighing at least 2,500 g.
Data from the 443 reporting clinics showed the increase in donor oocyte cycles noted before. In addition, the proportion of cycles using frozen embryos increased from 26.7% in 2000 to 40.3% in 2010, and the number of cycles with eSET grew over the same period from just 0.8% to 14.5% (P less than .001 for both trends).
In 2000, 18.5% of cycles resulted in good perinatal outcomes; by 2010, the percentage of good outcomes had improved to 24.4% (P less than .001).
There was no change over time in the mean age of either donors (28 years), or recipients (41 years).
In multivariate analysis controlling for recipient and donor age, race, infertility diagnosis, and number of prior pregnancies, miscarriages, preterm and full-term births and other factors, factors significantly favoring a good outcome were day 5 embryo transfer (adjusted odds ratio 1.17) and eSET (adjusted OR, 2.32).
Conversely, factors negatively associated with good outcomes were tubal-factor infertility (adjusted OR, 0.72), uterine-factor infertility (adjusted OR, 0.74), and non-Hispanic black recipient race/ethnicity (adjusted OR, 0.48).
Sister, can you spare an egg?
In his editorial, Dr. Myers noted that the surveillance data do not include data on health outcomes for oocyte donors.
"Donors are at risk for all of the complications associated with ovulation induction, including the potentially life-threatening ovarian hyperstimulation syndrome. In addition, there is uncertainty about longer-term issues such as effects on the donor’s own fertility or the need to inform recipients about the discovery of health issues not known at the time of donation," he wrote.
The study was supported by the CDC. The authors reported having no conflict of interest disclosures. Dr. Myers disclosed serving as a consultant for AbbVie, Merck, and the CDC, and receiving grants or grants pending from the Patient-Centered Outcomes Research Institute and Hologic-GenProbe.
BOSTON – A substantial increase in the number of donor oocyte cycles in the United States from 2000 to 2010 was accompanied by an increase in good perinatal outcomes, reported investigators at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A review of data from 93% of all fertility centers in the United States showed that the annual number of reproductive cycles using donor rather than autologous oocytes grew from 10,801 in 2000, to 18,306 in 2010.
The trend was accompanied by increases in the proportion of cycles using frozen rather than fresh embryos, as well as elective single-embryo transfer (eSET) vs. multiple transfers, said Dr. Jennifer F. Kawwass, a reproductive endocrinology and infertility fellow at Emory University in Atlanta, and her colleagues. The findings were published simultaneously in JAMA online (2013 [doi:10.1001/jama.2013.280924]).
The data show that single-embryo transfers were associated with a more than twofold improvement in the odds of a good outcome, compared with multiple transfers, and that embryo transfer at day 5 vs. day 3 was associated with a smaller but still significant increase in the chance of a favorable outcome.
Factors associated with lower likelihood of success included tubal- or uterine-factor infertility, and race/ethnicity with non-Hispanic black women having about half the number of successful pregnancies as non-Hispanic white women had.
Societal trends
The findings reflect both societal trends and the evolution of assisted reproductive technologies (ART), commented Dr. William D. Schlaff, Paul and Eloise Bowers Professor and chair of obstetrics and gynecology at Thomas Jefferson University in Philadelphia.
"This shows that people who are doing ART, particularly in the United States, are really putting weight behind the goal of having a single, healthy term pregnancy by transferring a single embryo," he said in an interview.
The data also show that, despite the attendant risks of multiple-fetus pregnancies for mothers and children, some patients may have better outcomes with multiple-embryo transfers.
"If you can identify a subgroup of people with a very good prognosis, particularly if they’re on the fence as to how they would like to proceed, I think you can help them make decisions that would minimize the risk of higher multiples or twins, while not affecting their overall prognosis," Dr. Schlaff said.
The data suggest that oocyte donation is here to stay for the foreseeable future, Dr. Evan R. Myers of the department of obstetrics and gynecology at Duke University in Durham, N.C., noted in a JAMA editorial (2013 [doi:10.1001/jama.2013.280925]).
"More complete data on both short-and long-term outcomes of donation are needed so donors can make truly informed choices and, once those data are available, mechanisms can be put in place to ensure that the donor recruitment and consent process at clinics is conducted according to the highest ethical standards," he wrote.
Dr. Kawwass and her colleagues drew on data reported by fertility centers under mandate to the Centers for Disease Control and Prevention’s National ART Surveillance System. They defined a good perinatal outcome as a singleton born live at 37 weeks’ gestation or later, weighing at least 2,500 g.
Data from the 443 reporting clinics showed the increase in donor oocyte cycles noted before. In addition, the proportion of cycles using frozen embryos increased from 26.7% in 2000 to 40.3% in 2010, and the number of cycles with eSET grew over the same period from just 0.8% to 14.5% (P less than .001 for both trends).
In 2000, 18.5% of cycles resulted in good perinatal outcomes; by 2010, the percentage of good outcomes had improved to 24.4% (P less than .001).
There was no change over time in the mean age of either donors (28 years), or recipients (41 years).
In multivariate analysis controlling for recipient and donor age, race, infertility diagnosis, and number of prior pregnancies, miscarriages, preterm and full-term births and other factors, factors significantly favoring a good outcome were day 5 embryo transfer (adjusted odds ratio 1.17) and eSET (adjusted OR, 2.32).
Conversely, factors negatively associated with good outcomes were tubal-factor infertility (adjusted OR, 0.72), uterine-factor infertility (adjusted OR, 0.74), and non-Hispanic black recipient race/ethnicity (adjusted OR, 0.48).
Sister, can you spare an egg?
In his editorial, Dr. Myers noted that the surveillance data do not include data on health outcomes for oocyte donors.
"Donors are at risk for all of the complications associated with ovulation induction, including the potentially life-threatening ovarian hyperstimulation syndrome. In addition, there is uncertainty about longer-term issues such as effects on the donor’s own fertility or the need to inform recipients about the discovery of health issues not known at the time of donation," he wrote.
The study was supported by the CDC. The authors reported having no conflict of interest disclosures. Dr. Myers disclosed serving as a consultant for AbbVie, Merck, and the CDC, and receiving grants or grants pending from the Patient-Centered Outcomes Research Institute and Hologic-GenProbe.
AT THE IFFS/ASRM ANNUAL MEETING
Major finding: The annual number of reproductive cycles using donor rather than autologous oocytes grew from 10,801 in 2000, to 18,306 in 2010.
Data source: Surveillance data from a CDC database of 443 infertility clinics in the United States.
Disclosures: The study was supported by the CDC. The authors reported having no conflict of interest disclosures. Dr. Myers disclosed serving as a consultant for AbbVie, Merck, and the CDC, and receiving grants or grants pending from the Patient-Centered Outcomes Research Institute and Hologic-GenProbe.
Live births higher with letrozole than clomiphene in women with PCOS
BOSTON – Letrozole is superior to clomiphene for stimulating ovulation and should be considered the new standard of care for treating anovulatory infertility in women with the polycystic ovary syndrome, investigators said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
In a randomized prospective study, 27.5% of women with polycystic ovary syndrome (PCOS) who received letrozole (Femara) had a live birth, compared with 19.5% of women treated with clomipheme. The rate ratio for live births, the primary endpoint, was 1.44 in favor of letrozole (P =.011), said Dr. Richard S. Legro, professor of obstetrics and gynecology at the Pennsylvania State University in Hershey.
"We think that this is going to be a pivotal trial that changes practice," he said.
The Pregnancy in Polycystic Ovary Syndrome (PPCOS I) trial, published in 2007, showed that clomiphene, a selective estrogen receptor modulator (SERM), was superior to the insulin sensitizer metformin for treatment of infertility in women with PCOS, but at the cost of higher-risk multiple births, Dr. Legro noted (N. Engl. J. Med. 2007;356:551-66).
In addition, clomiphene resistance was common in that study: 25% of participants never ovulated once in up to six treatment cycles, and 78% of patients treated with clomiphene were not able to conceive.
The rationale behind the use of letrozole, an aromatase inhibitor normally prescribed as an adjuvant therapy in women with hormone-responsive breast cancer, is that it interferes with inappropriate estrogen feedback at the hypothalamus, causing a corresponding rise in the secretion of follicle-stimulating hormone.
Letrozole also has a shorter half-life than clomiphene, meaning that there is a lower risk of fetal exposure to the drug in early pregnancy. In addition, Dr. Legro said that aromatase inhibitors were shown in a systematic review to induce more monofollicular ovulation and have more favorable endometrial effects than SERMs (J. Clin. Endocrinol. Metab. 2006;91:760-71).
For the current study, the investigators enrolled 750 infertile women with a diagnosis of PCOS according to modified Rotterdam criteria: ovulatory dysfunction with either hyperandrogenism or polycystic ovaries. The women, aged of 18-39 years, were in good health and did not have other potentially confounding endocrinopathies. There were no body mass index (BMI) limits in the study, but patients with high BMIs were counseled about the effects of excess weight on fertility.
A total of 376 patients were assigned to receive clomiphene 50 mg/day and 374 were assigned to receive letrozole 2.5 mg/day in doses escalating to 7.5 mg/day for a total of 5 days per cycle for up to five cycles. The drugs were provided in identical capsules over the same schedule.
Apart from the cumulative incidence of live births, there were no significant differences between the two drug groups in pregnancy duration, infant birth weight, proportion of male infants (including twins), or twin live births.
Ovulation rates with letrozole were significantly superior to clomiphene beginning at the second cycle and continuing through the fifth and final cycle (P less than .01).
Fecundity also was better with letrozole, with rate ratios compared with clomiphene of 1.31 for conception, 1.31 for singleton pregnancy, and 1.29 for singleton live birth.
There were four major congenital abnormalities in the children of women who took letrozole, including cerebral palsy with arrested hydrocephalus with polycythemia and neutropenia, imperforate anus with perineal fistula and spina bifida with a tethered spinal cord, right hemimegancephaly and dysgenesis of the left frontal and temporal lobes without hydrocephalus, and a large cardiac ventricular septal defect that required surgical repair.
There was only one major abnormality in the clomiphene group – an atrial ventricular septal cardiac defect with pulmonary stenosis.
There was one minor birth defect – ankyloglossia – in the letrozole group. There were two intrauterine fetal or neonatal deaths in the letrozole group and three in the clomiphene group.
In the question-and-response session following the presentation, Dr. Frederick Licciardi, director of the oocyte donation program at NYU Fertility Center in New York City, questioned the need for a randomized trial, noting that previous studies have shown that letrozole is superior to clomiphene in this population.
"I think the studies were too small, and didn’t focus on live birth. It takes a study like this to detect this sort of advantage," Dr. Legro replied.
The study was funded by the National Institutes of Health. Dr. Legro reported receiving consulting fees from GlaxoSmithKline, Ferring, and Abbott; lecture fees from Serono; and grant support from Pfizer.
BOSTON – Letrozole is superior to clomiphene for stimulating ovulation and should be considered the new standard of care for treating anovulatory infertility in women with the polycystic ovary syndrome, investigators said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
In a randomized prospective study, 27.5% of women with polycystic ovary syndrome (PCOS) who received letrozole (Femara) had a live birth, compared with 19.5% of women treated with clomipheme. The rate ratio for live births, the primary endpoint, was 1.44 in favor of letrozole (P =.011), said Dr. Richard S. Legro, professor of obstetrics and gynecology at the Pennsylvania State University in Hershey.
"We think that this is going to be a pivotal trial that changes practice," he said.
The Pregnancy in Polycystic Ovary Syndrome (PPCOS I) trial, published in 2007, showed that clomiphene, a selective estrogen receptor modulator (SERM), was superior to the insulin sensitizer metformin for treatment of infertility in women with PCOS, but at the cost of higher-risk multiple births, Dr. Legro noted (N. Engl. J. Med. 2007;356:551-66).
In addition, clomiphene resistance was common in that study: 25% of participants never ovulated once in up to six treatment cycles, and 78% of patients treated with clomiphene were not able to conceive.
The rationale behind the use of letrozole, an aromatase inhibitor normally prescribed as an adjuvant therapy in women with hormone-responsive breast cancer, is that it interferes with inappropriate estrogen feedback at the hypothalamus, causing a corresponding rise in the secretion of follicle-stimulating hormone.
Letrozole also has a shorter half-life than clomiphene, meaning that there is a lower risk of fetal exposure to the drug in early pregnancy. In addition, Dr. Legro said that aromatase inhibitors were shown in a systematic review to induce more monofollicular ovulation and have more favorable endometrial effects than SERMs (J. Clin. Endocrinol. Metab. 2006;91:760-71).
For the current study, the investigators enrolled 750 infertile women with a diagnosis of PCOS according to modified Rotterdam criteria: ovulatory dysfunction with either hyperandrogenism or polycystic ovaries. The women, aged of 18-39 years, were in good health and did not have other potentially confounding endocrinopathies. There were no body mass index (BMI) limits in the study, but patients with high BMIs were counseled about the effects of excess weight on fertility.
A total of 376 patients were assigned to receive clomiphene 50 mg/day and 374 were assigned to receive letrozole 2.5 mg/day in doses escalating to 7.5 mg/day for a total of 5 days per cycle for up to five cycles. The drugs were provided in identical capsules over the same schedule.
Apart from the cumulative incidence of live births, there were no significant differences between the two drug groups in pregnancy duration, infant birth weight, proportion of male infants (including twins), or twin live births.
Ovulation rates with letrozole were significantly superior to clomiphene beginning at the second cycle and continuing through the fifth and final cycle (P less than .01).
Fecundity also was better with letrozole, with rate ratios compared with clomiphene of 1.31 for conception, 1.31 for singleton pregnancy, and 1.29 for singleton live birth.
There were four major congenital abnormalities in the children of women who took letrozole, including cerebral palsy with arrested hydrocephalus with polycythemia and neutropenia, imperforate anus with perineal fistula and spina bifida with a tethered spinal cord, right hemimegancephaly and dysgenesis of the left frontal and temporal lobes without hydrocephalus, and a large cardiac ventricular septal defect that required surgical repair.
There was only one major abnormality in the clomiphene group – an atrial ventricular septal cardiac defect with pulmonary stenosis.
There was one minor birth defect – ankyloglossia – in the letrozole group. There were two intrauterine fetal or neonatal deaths in the letrozole group and three in the clomiphene group.
In the question-and-response session following the presentation, Dr. Frederick Licciardi, director of the oocyte donation program at NYU Fertility Center in New York City, questioned the need for a randomized trial, noting that previous studies have shown that letrozole is superior to clomiphene in this population.
"I think the studies were too small, and didn’t focus on live birth. It takes a study like this to detect this sort of advantage," Dr. Legro replied.
The study was funded by the National Institutes of Health. Dr. Legro reported receiving consulting fees from GlaxoSmithKline, Ferring, and Abbott; lecture fees from Serono; and grant support from Pfizer.
BOSTON – Letrozole is superior to clomiphene for stimulating ovulation and should be considered the new standard of care for treating anovulatory infertility in women with the polycystic ovary syndrome, investigators said at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
In a randomized prospective study, 27.5% of women with polycystic ovary syndrome (PCOS) who received letrozole (Femara) had a live birth, compared with 19.5% of women treated with clomipheme. The rate ratio for live births, the primary endpoint, was 1.44 in favor of letrozole (P =.011), said Dr. Richard S. Legro, professor of obstetrics and gynecology at the Pennsylvania State University in Hershey.
"We think that this is going to be a pivotal trial that changes practice," he said.
The Pregnancy in Polycystic Ovary Syndrome (PPCOS I) trial, published in 2007, showed that clomiphene, a selective estrogen receptor modulator (SERM), was superior to the insulin sensitizer metformin for treatment of infertility in women with PCOS, but at the cost of higher-risk multiple births, Dr. Legro noted (N. Engl. J. Med. 2007;356:551-66).
In addition, clomiphene resistance was common in that study: 25% of participants never ovulated once in up to six treatment cycles, and 78% of patients treated with clomiphene were not able to conceive.
The rationale behind the use of letrozole, an aromatase inhibitor normally prescribed as an adjuvant therapy in women with hormone-responsive breast cancer, is that it interferes with inappropriate estrogen feedback at the hypothalamus, causing a corresponding rise in the secretion of follicle-stimulating hormone.
Letrozole also has a shorter half-life than clomiphene, meaning that there is a lower risk of fetal exposure to the drug in early pregnancy. In addition, Dr. Legro said that aromatase inhibitors were shown in a systematic review to induce more monofollicular ovulation and have more favorable endometrial effects than SERMs (J. Clin. Endocrinol. Metab. 2006;91:760-71).
For the current study, the investigators enrolled 750 infertile women with a diagnosis of PCOS according to modified Rotterdam criteria: ovulatory dysfunction with either hyperandrogenism or polycystic ovaries. The women, aged of 18-39 years, were in good health and did not have other potentially confounding endocrinopathies. There were no body mass index (BMI) limits in the study, but patients with high BMIs were counseled about the effects of excess weight on fertility.
A total of 376 patients were assigned to receive clomiphene 50 mg/day and 374 were assigned to receive letrozole 2.5 mg/day in doses escalating to 7.5 mg/day for a total of 5 days per cycle for up to five cycles. The drugs were provided in identical capsules over the same schedule.
Apart from the cumulative incidence of live births, there were no significant differences between the two drug groups in pregnancy duration, infant birth weight, proportion of male infants (including twins), or twin live births.
Ovulation rates with letrozole were significantly superior to clomiphene beginning at the second cycle and continuing through the fifth and final cycle (P less than .01).
Fecundity also was better with letrozole, with rate ratios compared with clomiphene of 1.31 for conception, 1.31 for singleton pregnancy, and 1.29 for singleton live birth.
There were four major congenital abnormalities in the children of women who took letrozole, including cerebral palsy with arrested hydrocephalus with polycythemia and neutropenia, imperforate anus with perineal fistula and spina bifida with a tethered spinal cord, right hemimegancephaly and dysgenesis of the left frontal and temporal lobes without hydrocephalus, and a large cardiac ventricular septal defect that required surgical repair.
There was only one major abnormality in the clomiphene group – an atrial ventricular septal cardiac defect with pulmonary stenosis.
There was one minor birth defect – ankyloglossia – in the letrozole group. There were two intrauterine fetal or neonatal deaths in the letrozole group and three in the clomiphene group.
In the question-and-response session following the presentation, Dr. Frederick Licciardi, director of the oocyte donation program at NYU Fertility Center in New York City, questioned the need for a randomized trial, noting that previous studies have shown that letrozole is superior to clomiphene in this population.
"I think the studies were too small, and didn’t focus on live birth. It takes a study like this to detect this sort of advantage," Dr. Legro replied.
The study was funded by the National Institutes of Health. Dr. Legro reported receiving consulting fees from GlaxoSmithKline, Ferring, and Abbott; lecture fees from Serono; and grant support from Pfizer.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Compared with clomiphene, the rate ratio for live births for women with polycystic ovary syndrome treated with letrozole was 1.44.
Data source: Randomized, blinded study in 750 women with the polycystic ovary syndrome.
Disclosures: The study was funded by the National Institutes of Health. Dr. Legro reported receiving consulting fees from GlaxoSmithKline, Ferring, and Abbott; lecture fees from Serono; and grant support from Pfizer.
Many women with cancer not told about impaired fertility risk
BOSTON – Less than half of all women of child-bearing age who are diagnosed with cancer discuss with their physicians the potential effects of cancer therapy on fertility, and even fewer are referred to reproductive specialists, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A survey of 1,282 female survivors of various cancers showed that more than 50% did not have a discussion with their oncologists about the possible deleterious effects of chemotherapy or radiation on fertility, and few patients received referrals to reproductive specialists, said Penelope P. Howards, Ph.D., assistant professor of epidemiology at Emory University’s Rollins School of Public Health in Atlanta.
"In our cohort, which was women who were diagnosed between 1990 and 2009, a large proportion is not getting the message about how treatments may affect their fertility," Dr. Howards said in an interview.
The likelihood that women would have been counseled about fertility varied by the type of cancer and by the typical treatment approach. For example, nearly 70% of women with cervical cancer said they had talked about fertility with their physicians, whereas women with cancers more typically managed by surgery – such as melanoma and thyroid cancer – were the least likely to be informed about potentially compromised fertility.
Only 60% of women with uterine cancers and 42% of women with ovarian cancers were told about the effects of treatment on fertility, despite having cancers of the reproductive system. Among women with breast cancer, the most common cancer type represented in the study, only 44% said they received fertility counseling.
Women who had at least one child by the time of diagnosis were less likely to be counseled than were women with no children (42% vs. 50%, respectively), and women aged 20-24 years were less likely to be informed about potentially compromised fertility than were women in their 30s, the investigators found.
Dr. Howards speculated that oncologists may assume that younger cancer patients are less likely to need counseling because they have a longer time to recover reproductive function than women who are approaching the age of menopause. Additionally, they may observe that young women who are rendered amenorrheic by cancer treatment may eventually resume menses, and wrongly assume that a return to menstruation indicates a return to full reproductive health.
Of those women who reported having a fertility discussion, 33% said they had initiated it themselves, 44% said that their oncologists had brought it up, and 23% said someone else initiated the discussion.
Dr. Howards and her colleagues searched the Georgia Cancer Registry to identify and interview women with a first diagnosis of cancer between the ages of 20 and 35 years. The interviews included questions about their reproductive histories, whether they had discussed with a clinician how cancer therapies might affect their fertility, and whether they had received a referral to a fertility specialist.
Factors that significantly predicted which women would be less likely to be counseled about infertility included having a child at diagnosis (adjusted odds ratio, 1.7), younger age at diagnosis (aOR, 1.5), being African American vs. white (aOR, 1.2), and not receiving chemotherapy or radiation (aOR, 3.1).
Of those women who did have a fertility discussion, only 6% of those with a child and 19% of those without children were referred to a fertility specialist.
An investigator who was not involved in the study said that the problem is not limited to women.
"With regard to men who get a diagnosis of cancer, we have seen that the discussion about their fertility status is not often had prior to getting a therapy that would affect their fertility status, such as chemotherapy, radiotherapy, or surgery," said Dr. Anand Shridharani, a urologist at the Erlanger Health System in Chattanooga, Tenn.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Development. Dr. Howards and Dr. Shridharani reported having no relevant disclosures.
BOSTON – Less than half of all women of child-bearing age who are diagnosed with cancer discuss with their physicians the potential effects of cancer therapy on fertility, and even fewer are referred to reproductive specialists, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A survey of 1,282 female survivors of various cancers showed that more than 50% did not have a discussion with their oncologists about the possible deleterious effects of chemotherapy or radiation on fertility, and few patients received referrals to reproductive specialists, said Penelope P. Howards, Ph.D., assistant professor of epidemiology at Emory University’s Rollins School of Public Health in Atlanta.
"In our cohort, which was women who were diagnosed between 1990 and 2009, a large proportion is not getting the message about how treatments may affect their fertility," Dr. Howards said in an interview.
The likelihood that women would have been counseled about fertility varied by the type of cancer and by the typical treatment approach. For example, nearly 70% of women with cervical cancer said they had talked about fertility with their physicians, whereas women with cancers more typically managed by surgery – such as melanoma and thyroid cancer – were the least likely to be informed about potentially compromised fertility.
Only 60% of women with uterine cancers and 42% of women with ovarian cancers were told about the effects of treatment on fertility, despite having cancers of the reproductive system. Among women with breast cancer, the most common cancer type represented in the study, only 44% said they received fertility counseling.
Women who had at least one child by the time of diagnosis were less likely to be counseled than were women with no children (42% vs. 50%, respectively), and women aged 20-24 years were less likely to be informed about potentially compromised fertility than were women in their 30s, the investigators found.
Dr. Howards speculated that oncologists may assume that younger cancer patients are less likely to need counseling because they have a longer time to recover reproductive function than women who are approaching the age of menopause. Additionally, they may observe that young women who are rendered amenorrheic by cancer treatment may eventually resume menses, and wrongly assume that a return to menstruation indicates a return to full reproductive health.
Of those women who reported having a fertility discussion, 33% said they had initiated it themselves, 44% said that their oncologists had brought it up, and 23% said someone else initiated the discussion.
Dr. Howards and her colleagues searched the Georgia Cancer Registry to identify and interview women with a first diagnosis of cancer between the ages of 20 and 35 years. The interviews included questions about their reproductive histories, whether they had discussed with a clinician how cancer therapies might affect their fertility, and whether they had received a referral to a fertility specialist.
Factors that significantly predicted which women would be less likely to be counseled about infertility included having a child at diagnosis (adjusted odds ratio, 1.7), younger age at diagnosis (aOR, 1.5), being African American vs. white (aOR, 1.2), and not receiving chemotherapy or radiation (aOR, 3.1).
Of those women who did have a fertility discussion, only 6% of those with a child and 19% of those without children were referred to a fertility specialist.
An investigator who was not involved in the study said that the problem is not limited to women.
"With regard to men who get a diagnosis of cancer, we have seen that the discussion about their fertility status is not often had prior to getting a therapy that would affect their fertility status, such as chemotherapy, radiotherapy, or surgery," said Dr. Anand Shridharani, a urologist at the Erlanger Health System in Chattanooga, Tenn.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Development. Dr. Howards and Dr. Shridharani reported having no relevant disclosures.
BOSTON – Less than half of all women of child-bearing age who are diagnosed with cancer discuss with their physicians the potential effects of cancer therapy on fertility, and even fewer are referred to reproductive specialists, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A survey of 1,282 female survivors of various cancers showed that more than 50% did not have a discussion with their oncologists about the possible deleterious effects of chemotherapy or radiation on fertility, and few patients received referrals to reproductive specialists, said Penelope P. Howards, Ph.D., assistant professor of epidemiology at Emory University’s Rollins School of Public Health in Atlanta.
"In our cohort, which was women who were diagnosed between 1990 and 2009, a large proportion is not getting the message about how treatments may affect their fertility," Dr. Howards said in an interview.
The likelihood that women would have been counseled about fertility varied by the type of cancer and by the typical treatment approach. For example, nearly 70% of women with cervical cancer said they had talked about fertility with their physicians, whereas women with cancers more typically managed by surgery – such as melanoma and thyroid cancer – were the least likely to be informed about potentially compromised fertility.
Only 60% of women with uterine cancers and 42% of women with ovarian cancers were told about the effects of treatment on fertility, despite having cancers of the reproductive system. Among women with breast cancer, the most common cancer type represented in the study, only 44% said they received fertility counseling.
Women who had at least one child by the time of diagnosis were less likely to be counseled than were women with no children (42% vs. 50%, respectively), and women aged 20-24 years were less likely to be informed about potentially compromised fertility than were women in their 30s, the investigators found.
Dr. Howards speculated that oncologists may assume that younger cancer patients are less likely to need counseling because they have a longer time to recover reproductive function than women who are approaching the age of menopause. Additionally, they may observe that young women who are rendered amenorrheic by cancer treatment may eventually resume menses, and wrongly assume that a return to menstruation indicates a return to full reproductive health.
Of those women who reported having a fertility discussion, 33% said they had initiated it themselves, 44% said that their oncologists had brought it up, and 23% said someone else initiated the discussion.
Dr. Howards and her colleagues searched the Georgia Cancer Registry to identify and interview women with a first diagnosis of cancer between the ages of 20 and 35 years. The interviews included questions about their reproductive histories, whether they had discussed with a clinician how cancer therapies might affect their fertility, and whether they had received a referral to a fertility specialist.
Factors that significantly predicted which women would be less likely to be counseled about infertility included having a child at diagnosis (adjusted odds ratio, 1.7), younger age at diagnosis (aOR, 1.5), being African American vs. white (aOR, 1.2), and not receiving chemotherapy or radiation (aOR, 3.1).
Of those women who did have a fertility discussion, only 6% of those with a child and 19% of those without children were referred to a fertility specialist.
An investigator who was not involved in the study said that the problem is not limited to women.
"With regard to men who get a diagnosis of cancer, we have seen that the discussion about their fertility status is not often had prior to getting a therapy that would affect their fertility status, such as chemotherapy, radiotherapy, or surgery," said Dr. Anand Shridharani, a urologist at the Erlanger Health System in Chattanooga, Tenn.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Development. Dr. Howards and Dr. Shridharani reported having no relevant disclosures.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Less than half of all women of reproductive age with a diagnosis of cancer were told by physicians that treatment might affect their fertility.
Data source: Telephone-based survey of 1,282 women in a cancer registry.
Disclosures: The study was supported by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Development. Dr. Howards and Dr. Shridharani reported having no relevant disclosures.
Phthalate effect on fecundity varies according to gender
BOSTON – Men exposed to environmental phthalate compounds may have about a 20% reduction in fertility, but women exposed to similar chemicals may have an increase in fecundity, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A study of couples trying to conceive showed that for men, exposure to some phthalates – esters of phthalic acid used widely in plastics, soaps, and cosmetics – resulted in a fecundity odds ratio (FOR) ranging from 0.77 to 0.82, indicating that a longer than normal time would be required to achieve a pregnancy. In contrast, women exposed to phthalates had an FOR ranging from 1.09 to 1.20, indicating increased fertility.
The investigators found, however, no associations between exposure to bisphenol A (BPA), an estrogen-mimicking plasticizing compound, and fertility in either men or women.
The findings show the importance of assessing both partners when trying to determine the source of reproductive problems, said Michael S. Bloom, Ph.D., assistant professor of environmental health sciences at the University at Albany, The State University of New York.
"If the authors had just measured women, they would be thinking that phthalates enhanced fecundity, as measured by a shorter time to pregnancy; had only men been observed, they would be thinking that phthalates diminished fecundity, as measured by a longer time to pregnancy," said Dr. Bloom.
Dr. Bloom was not involved in the study, but he presented the data on behalf of Dr. Germaine Buck Louis, an epidemiologist at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, who was unable to attend due to the federal government shutdown.
Previous studies have shown that persistent environmental chemicals such as polychlorinated biphenyls (PCBs) and perfluorooctanesulfonamide (PFOSA) are associated with diminished fecundity in couples as measured by a longer time to pregnancy. Yet despite their presence in everything from baby bottles to shampoo, short-lived chemicals such as BPA and phthalates have not been widely investigated for their effects on human fertility, Dr. Bloom said.
Nonetheless, emerging evidence suggests that BPA is associated with decreased semen quality and hormonal abnormalities in men, and with ovulatory and embryo implantation problems in women. Similarly, phthalates have been associated with sperm damage and decreased sperm motility among men attending fertility clinics and in the general population, and with a threefold increase in pregnancy loss among women, he noted.
The investigators looked at a prospective cohort of 501 couples in committed relationships who were stopping contraception. The female partners ranged in age from 18 to 44 years. The authors conducted a baseline interview; conducted anthropometric assessments; collected blood and urine samples at baseline to assess environmental exposures; and asked the couples to keep a daily journal on sexual intercourse and lifestyles, the female partner’s menstruation, and pregnancy test results.
The couples were followed until they either achieved a pregnancy confirmed by a positive human chorionic gonadotropin (HCG) or had 12 reproductive cycles without a pregnancy.
In multivariate analyses controlling for age, body mass index, serum cotinine and creatinine levels, research site, and time off contraception, they found that BPA was not significantly associated with fecundity in either sex.
In contrast, mono-(3-carboxypropyl) phthalate (mCPP) was significantly associated) with an FOR of 1.20 in women, and mono-n-octyl phthalate (mOP) was associated with an FOR of 1.09.
Among men, three phthalates – monomethyl phthalate, monobutyl phthalate, and monobenzyl phthalate – were associated with respective FORs of 0.80, 0.82, and 0.77. All these associations were statistically significant.
Although the authors did not find an association between BPA and fecundity in either sex, there was a data signal that suggested a possible negative effect of BPA exposure in women, and that with a large sample size the association might be statistically significant, the investigators said.
The study was supported by the Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Buck Louis is a senior investigator at the NICHD. Dr. Bloom reported having no relevant disclosures.
BOSTON – Men exposed to environmental phthalate compounds may have about a 20% reduction in fertility, but women exposed to similar chemicals may have an increase in fecundity, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A study of couples trying to conceive showed that for men, exposure to some phthalates – esters of phthalic acid used widely in plastics, soaps, and cosmetics – resulted in a fecundity odds ratio (FOR) ranging from 0.77 to 0.82, indicating that a longer than normal time would be required to achieve a pregnancy. In contrast, women exposed to phthalates had an FOR ranging from 1.09 to 1.20, indicating increased fertility.
The investigators found, however, no associations between exposure to bisphenol A (BPA), an estrogen-mimicking plasticizing compound, and fertility in either men or women.
The findings show the importance of assessing both partners when trying to determine the source of reproductive problems, said Michael S. Bloom, Ph.D., assistant professor of environmental health sciences at the University at Albany, The State University of New York.
"If the authors had just measured women, they would be thinking that phthalates enhanced fecundity, as measured by a shorter time to pregnancy; had only men been observed, they would be thinking that phthalates diminished fecundity, as measured by a longer time to pregnancy," said Dr. Bloom.
Dr. Bloom was not involved in the study, but he presented the data on behalf of Dr. Germaine Buck Louis, an epidemiologist at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, who was unable to attend due to the federal government shutdown.
Previous studies have shown that persistent environmental chemicals such as polychlorinated biphenyls (PCBs) and perfluorooctanesulfonamide (PFOSA) are associated with diminished fecundity in couples as measured by a longer time to pregnancy. Yet despite their presence in everything from baby bottles to shampoo, short-lived chemicals such as BPA and phthalates have not been widely investigated for their effects on human fertility, Dr. Bloom said.
Nonetheless, emerging evidence suggests that BPA is associated with decreased semen quality and hormonal abnormalities in men, and with ovulatory and embryo implantation problems in women. Similarly, phthalates have been associated with sperm damage and decreased sperm motility among men attending fertility clinics and in the general population, and with a threefold increase in pregnancy loss among women, he noted.
The investigators looked at a prospective cohort of 501 couples in committed relationships who were stopping contraception. The female partners ranged in age from 18 to 44 years. The authors conducted a baseline interview; conducted anthropometric assessments; collected blood and urine samples at baseline to assess environmental exposures; and asked the couples to keep a daily journal on sexual intercourse and lifestyles, the female partner’s menstruation, and pregnancy test results.
The couples were followed until they either achieved a pregnancy confirmed by a positive human chorionic gonadotropin (HCG) or had 12 reproductive cycles without a pregnancy.
In multivariate analyses controlling for age, body mass index, serum cotinine and creatinine levels, research site, and time off contraception, they found that BPA was not significantly associated with fecundity in either sex.
In contrast, mono-(3-carboxypropyl) phthalate (mCPP) was significantly associated) with an FOR of 1.20 in women, and mono-n-octyl phthalate (mOP) was associated with an FOR of 1.09.
Among men, three phthalates – monomethyl phthalate, monobutyl phthalate, and monobenzyl phthalate – were associated with respective FORs of 0.80, 0.82, and 0.77. All these associations were statistically significant.
Although the authors did not find an association between BPA and fecundity in either sex, there was a data signal that suggested a possible negative effect of BPA exposure in women, and that with a large sample size the association might be statistically significant, the investigators said.
The study was supported by the Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Buck Louis is a senior investigator at the NICHD. Dr. Bloom reported having no relevant disclosures.
BOSTON – Men exposed to environmental phthalate compounds may have about a 20% reduction in fertility, but women exposed to similar chemicals may have an increase in fecundity, investigators reported at the conjoint meeting of the International Federation of Fertility Societies and the American Society for Reproductive Medicine.
A study of couples trying to conceive showed that for men, exposure to some phthalates – esters of phthalic acid used widely in plastics, soaps, and cosmetics – resulted in a fecundity odds ratio (FOR) ranging from 0.77 to 0.82, indicating that a longer than normal time would be required to achieve a pregnancy. In contrast, women exposed to phthalates had an FOR ranging from 1.09 to 1.20, indicating increased fertility.
The investigators found, however, no associations between exposure to bisphenol A (BPA), an estrogen-mimicking plasticizing compound, and fertility in either men or women.
The findings show the importance of assessing both partners when trying to determine the source of reproductive problems, said Michael S. Bloom, Ph.D., assistant professor of environmental health sciences at the University at Albany, The State University of New York.
"If the authors had just measured women, they would be thinking that phthalates enhanced fecundity, as measured by a shorter time to pregnancy; had only men been observed, they would be thinking that phthalates diminished fecundity, as measured by a longer time to pregnancy," said Dr. Bloom.
Dr. Bloom was not involved in the study, but he presented the data on behalf of Dr. Germaine Buck Louis, an epidemiologist at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, who was unable to attend due to the federal government shutdown.
Previous studies have shown that persistent environmental chemicals such as polychlorinated biphenyls (PCBs) and perfluorooctanesulfonamide (PFOSA) are associated with diminished fecundity in couples as measured by a longer time to pregnancy. Yet despite their presence in everything from baby bottles to shampoo, short-lived chemicals such as BPA and phthalates have not been widely investigated for their effects on human fertility, Dr. Bloom said.
Nonetheless, emerging evidence suggests that BPA is associated with decreased semen quality and hormonal abnormalities in men, and with ovulatory and embryo implantation problems in women. Similarly, phthalates have been associated with sperm damage and decreased sperm motility among men attending fertility clinics and in the general population, and with a threefold increase in pregnancy loss among women, he noted.
The investigators looked at a prospective cohort of 501 couples in committed relationships who were stopping contraception. The female partners ranged in age from 18 to 44 years. The authors conducted a baseline interview; conducted anthropometric assessments; collected blood and urine samples at baseline to assess environmental exposures; and asked the couples to keep a daily journal on sexual intercourse and lifestyles, the female partner’s menstruation, and pregnancy test results.
The couples were followed until they either achieved a pregnancy confirmed by a positive human chorionic gonadotropin (HCG) or had 12 reproductive cycles without a pregnancy.
In multivariate analyses controlling for age, body mass index, serum cotinine and creatinine levels, research site, and time off contraception, they found that BPA was not significantly associated with fecundity in either sex.
In contrast, mono-(3-carboxypropyl) phthalate (mCPP) was significantly associated) with an FOR of 1.20 in women, and mono-n-octyl phthalate (mOP) was associated with an FOR of 1.09.
Among men, three phthalates – monomethyl phthalate, monobutyl phthalate, and monobenzyl phthalate – were associated with respective FORs of 0.80, 0.82, and 0.77. All these associations were statistically significant.
Although the authors did not find an association between BPA and fecundity in either sex, there was a data signal that suggested a possible negative effect of BPA exposure in women, and that with a large sample size the association might be statistically significant, the investigators said.
The study was supported by the Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Buck Louis is a senior investigator at the NICHD. Dr. Bloom reported having no relevant disclosures.
AT THE JOINT IFFS/ASRM MEETING
Major finding: Certain mono-esters of phthalate were associated with increased fecundity among women, while others were associated with decreased fertility in men.
Data source: Prospective study of 501 couples stopping contraception.
Disclosures: The study was supported by the Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Buck Louis is a senior investigator at the NICHD. Dr. Bloom reported having no relevant disclosures.








