User login
High ankylosing spondylitis activity linked to cardiovascular risk
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
AT THE EULAR CONGRESS 2013
Tight inflammation control could reduce CV risk in men with gout
MADRID – Optimizing anti-inflammatory treatment may help to reduce the risk of heart-related problems in men with crystal-proven gout, judging from 7-year follow up data from a prospective study.
Five factors were found to increase substantially the risk for cardiovascular (CV) events in the 251-patient study: including: high levels of C-reactive protein (CRP); renal insufficiency; daily intake of more than 20 g of alcohol; current coronary heart disease (CHD); and a family history of premature CV events.
The odds ratio (OR) for any CV event was 5.71 for CRP levels greater than 5 mg/L on multivariate analysis. This increased to 10.31 and 14.26 when nonfatal and fatal CV events were considered separately.
Odds ratios for renal insufficiency, defined as a creatinine clearance of less than 60 mL/min per 1.73 m2, were 4.76 for any CV event and 8.42 for fatal CV events. Respective values for a family history of CV events before the age of 55 years was 3.09 considering any CV event, but 7.53 if consideration was limited to fatal events only. Current CHD also increased the risk for any CV event (OR, 3.67) and for nonfatal events (OR, 10.41).
Alcohol intake of more than 20g/day carried an OR of 4.23 for any CV event.
"We have a cardiologist in our team to ensure the reliability of the cardiovascular outcomes," said Dr. Victoria Barskova of the Research Institute of Rheumatology in Moscow, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72[suppl. 3]:95). She explained that the study was designed to prospectively determine baseline factors that might influence the development of CV events in male patients with crystal-proven gout.
Between 2003 and 2006, a total of 407 men were screened and 301 deemed eligible for the study. Of these, 251 had follow-up data to 2010-2012. Data collected at baseline and at follow-up included patient demographics, including family history of gout and early CV disease, smoking history, and alcohol consumption. Comorbidities and gout characteristics were also assessed and all patients had an ECG and echocardiogram.
Comparing baseline clinical features with follow-up visit data, Dr. Barskova noted that the number of allopurinol users increased from 16% to 57% (P = .00001), although regular allopurinol use was not found to decrease the risk for CV events.
There was an increase in the percentage of patients with diabetes from 18% to 43% (P = .00001), chronic heart disease from 35% to 53% (P = .00001), and heart failure from 10% to 28% (P = .0001). Alcohol use significantly decreased (92% vs. 63%; P less than .0001).
The frequency of subcutaneous tophi and chronic arthritis comparing the first and last visits was the same.
Just under a quarter (23.1%, n = 58) of patients experienced a CV event. There were 32 (13%) deaths reported of which 22 were from cardiovascular causes. There were 36 nonfatal CV events.
"In our cohort of patients with crystal proven gout, the following independent risk factors for all CV events have been highlighted: CRP, renal insufficiency, alcohol intake, coronary heart disease, and a family history of CV events," Dr. Barskova said in conclusion.
The key message for rheumatologists, she added, is that "tight control of inflammation, which is measured not only by the obvious arthritis, but also by the serum CRP level, may have a positive effect on cardiovascular events in patients with gout."
MADRID – Optimizing anti-inflammatory treatment may help to reduce the risk of heart-related problems in men with crystal-proven gout, judging from 7-year follow up data from a prospective study.
Five factors were found to increase substantially the risk for cardiovascular (CV) events in the 251-patient study: including: high levels of C-reactive protein (CRP); renal insufficiency; daily intake of more than 20 g of alcohol; current coronary heart disease (CHD); and a family history of premature CV events.
The odds ratio (OR) for any CV event was 5.71 for CRP levels greater than 5 mg/L on multivariate analysis. This increased to 10.31 and 14.26 when nonfatal and fatal CV events were considered separately.
Odds ratios for renal insufficiency, defined as a creatinine clearance of less than 60 mL/min per 1.73 m2, were 4.76 for any CV event and 8.42 for fatal CV events. Respective values for a family history of CV events before the age of 55 years was 3.09 considering any CV event, but 7.53 if consideration was limited to fatal events only. Current CHD also increased the risk for any CV event (OR, 3.67) and for nonfatal events (OR, 10.41).
Alcohol intake of more than 20g/day carried an OR of 4.23 for any CV event.
"We have a cardiologist in our team to ensure the reliability of the cardiovascular outcomes," said Dr. Victoria Barskova of the Research Institute of Rheumatology in Moscow, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72[suppl. 3]:95). She explained that the study was designed to prospectively determine baseline factors that might influence the development of CV events in male patients with crystal-proven gout.
Between 2003 and 2006, a total of 407 men were screened and 301 deemed eligible for the study. Of these, 251 had follow-up data to 2010-2012. Data collected at baseline and at follow-up included patient demographics, including family history of gout and early CV disease, smoking history, and alcohol consumption. Comorbidities and gout characteristics were also assessed and all patients had an ECG and echocardiogram.
Comparing baseline clinical features with follow-up visit data, Dr. Barskova noted that the number of allopurinol users increased from 16% to 57% (P = .00001), although regular allopurinol use was not found to decrease the risk for CV events.
There was an increase in the percentage of patients with diabetes from 18% to 43% (P = .00001), chronic heart disease from 35% to 53% (P = .00001), and heart failure from 10% to 28% (P = .0001). Alcohol use significantly decreased (92% vs. 63%; P less than .0001).
The frequency of subcutaneous tophi and chronic arthritis comparing the first and last visits was the same.
Just under a quarter (23.1%, n = 58) of patients experienced a CV event. There were 32 (13%) deaths reported of which 22 were from cardiovascular causes. There were 36 nonfatal CV events.
"In our cohort of patients with crystal proven gout, the following independent risk factors for all CV events have been highlighted: CRP, renal insufficiency, alcohol intake, coronary heart disease, and a family history of CV events," Dr. Barskova said in conclusion.
The key message for rheumatologists, she added, is that "tight control of inflammation, which is measured not only by the obvious arthritis, but also by the serum CRP level, may have a positive effect on cardiovascular events in patients with gout."
MADRID – Optimizing anti-inflammatory treatment may help to reduce the risk of heart-related problems in men with crystal-proven gout, judging from 7-year follow up data from a prospective study.
Five factors were found to increase substantially the risk for cardiovascular (CV) events in the 251-patient study: including: high levels of C-reactive protein (CRP); renal insufficiency; daily intake of more than 20 g of alcohol; current coronary heart disease (CHD); and a family history of premature CV events.
The odds ratio (OR) for any CV event was 5.71 for CRP levels greater than 5 mg/L on multivariate analysis. This increased to 10.31 and 14.26 when nonfatal and fatal CV events were considered separately.
Odds ratios for renal insufficiency, defined as a creatinine clearance of less than 60 mL/min per 1.73 m2, were 4.76 for any CV event and 8.42 for fatal CV events. Respective values for a family history of CV events before the age of 55 years was 3.09 considering any CV event, but 7.53 if consideration was limited to fatal events only. Current CHD also increased the risk for any CV event (OR, 3.67) and for nonfatal events (OR, 10.41).
Alcohol intake of more than 20g/day carried an OR of 4.23 for any CV event.
"We have a cardiologist in our team to ensure the reliability of the cardiovascular outcomes," said Dr. Victoria Barskova of the Research Institute of Rheumatology in Moscow, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72[suppl. 3]:95). She explained that the study was designed to prospectively determine baseline factors that might influence the development of CV events in male patients with crystal-proven gout.
Between 2003 and 2006, a total of 407 men were screened and 301 deemed eligible for the study. Of these, 251 had follow-up data to 2010-2012. Data collected at baseline and at follow-up included patient demographics, including family history of gout and early CV disease, smoking history, and alcohol consumption. Comorbidities and gout characteristics were also assessed and all patients had an ECG and echocardiogram.
Comparing baseline clinical features with follow-up visit data, Dr. Barskova noted that the number of allopurinol users increased from 16% to 57% (P = .00001), although regular allopurinol use was not found to decrease the risk for CV events.
There was an increase in the percentage of patients with diabetes from 18% to 43% (P = .00001), chronic heart disease from 35% to 53% (P = .00001), and heart failure from 10% to 28% (P = .0001). Alcohol use significantly decreased (92% vs. 63%; P less than .0001).
The frequency of subcutaneous tophi and chronic arthritis comparing the first and last visits was the same.
Just under a quarter (23.1%, n = 58) of patients experienced a CV event. There were 32 (13%) deaths reported of which 22 were from cardiovascular causes. There were 36 nonfatal CV events.
"In our cohort of patients with crystal proven gout, the following independent risk factors for all CV events have been highlighted: CRP, renal insufficiency, alcohol intake, coronary heart disease, and a family history of CV events," Dr. Barskova said in conclusion.
The key message for rheumatologists, she added, is that "tight control of inflammation, which is measured not only by the obvious arthritis, but also by the serum CRP level, may have a positive effect on cardiovascular events in patients with gout."
AT THE EULAR CONGRESS 2013
Major finding: The odds ratio for any CV event was 5.71 for CRP levels greater than 5 mg/L on multivariate analysis. This increased to 10.31 and 14.26 when nonfatal and fatal CV events were considered separately.
Data source: Single-center, prospective cohort study of 251 male patients with crystal-proven gout with 6.9 years’ mean follow-up.
Disclosures: The research was supported by the Russian Academy of Medical Sciences. Dr. Barskova has not relevant conflicts of interest.
Scoring method assesses large-joint damage in treated RA
MADRID – A new radiographic scoring method successfully assessed damage in the large joints of patients with rheumatoid arthritis who were being treated with biologic therapy, according to research presented at the annual European Congress of Rheumatology.
The ARASHI (Assessment of Rheumatoid Arthritis by Scoring of Large-Joint Destruction and Healing in Radiographic Imaging) method, developed by a team in Japan, was tested over a period of 2 years in 51 patients who were being newly treated with tumor necrosis factor–alpha (TNF-alpha) inhibitors.
"Evaluation of radiographic damage of the small joints in the hands and feet using the van der Heijde total Sharp score in patients with early RA has been established," said Dr. Isao Matsushita, assistant professor in the orthopedic surgery department at the University of Toyama, Japan.
While the Larsen grade is most often used to assess large joints, this radiographic grading system has several limitations, including a "ceiling effect," resulting from the substantial variation found within each of the six Larsen grades (scored 0-5), he said in an interview at the meeting. Dr. Matsushita and his colleagues developed the ARASHI method to offer a more sensitive means of determining radiographic progression in the large joints.
The ARASHI method is composed of two parts (Mod. Rheumatol. 2013 April 27 [doi: 10.1007/s10165-012-0823-6]), Dr. Matsushita explained. First, there is a status score, which takes into account four categories: joint space narrowing (scored 0-3), erosion (scored 0-3), joint surface (0-6), and joint stability (0-4). Second, there is a change score, which assesses the same four categories plus the porosity of the joint.
A total of 57 patients with early RA who were about to be treated with TNF-alpha inhibitors were included in the study, and 51 completed 2 years’ treatment with these agents. The most frequently prescribed TNF-alpha inhibitors were infliximab, in 24 patients, and etanercept, used in 14. Another 7 patients switched from infliximab to etanercept, and 6 patients were treated with adalimumab. The mean age of the patients was 60 years, with a mean RA duration of 10.6 years.
The investigators used the ARASHI status score to assess 96 hip and 86 knee joints at baseline (before TNF-alpha inhibitor treatment was started). They later computed the ARASHI change score for the joints at both 1-year and 2-year follow-up visits. A 1-point or more increase in the ARASHI change score constituted radiographic progression. Higher scores indicated higher levels of joint damage.
All of the hip and knee joints with a status score of greater than 2 showed progression of joint damage under TNF-blocking therapies, Dr. Matsushita said. He added that of the joints with a low baseline ARASHI status score (0-2), only 6.5% showed progressive damage over the course of the study. Furthermore, the joint space narrowing score was more closely related to the joint damage subsequently seen than was the erosion score.
Taken together, these findings demonstrate that the "ARASHI scoring method is useful for the evaluation of radiographic damage in large weight-bearing joints, and to predict the risk for progression in patients with RA," Dr. Matsushita said. The next step is to look at the utility of the score in other large joints, perhaps the shoulder, elbow, and ankle joints, he noted.
Dr. Matsushita had no disclosures.
MADRID – A new radiographic scoring method successfully assessed damage in the large joints of patients with rheumatoid arthritis who were being treated with biologic therapy, according to research presented at the annual European Congress of Rheumatology.
The ARASHI (Assessment of Rheumatoid Arthritis by Scoring of Large-Joint Destruction and Healing in Radiographic Imaging) method, developed by a team in Japan, was tested over a period of 2 years in 51 patients who were being newly treated with tumor necrosis factor–alpha (TNF-alpha) inhibitors.
"Evaluation of radiographic damage of the small joints in the hands and feet using the van der Heijde total Sharp score in patients with early RA has been established," said Dr. Isao Matsushita, assistant professor in the orthopedic surgery department at the University of Toyama, Japan.
While the Larsen grade is most often used to assess large joints, this radiographic grading system has several limitations, including a "ceiling effect," resulting from the substantial variation found within each of the six Larsen grades (scored 0-5), he said in an interview at the meeting. Dr. Matsushita and his colleagues developed the ARASHI method to offer a more sensitive means of determining radiographic progression in the large joints.
The ARASHI method is composed of two parts (Mod. Rheumatol. 2013 April 27 [doi: 10.1007/s10165-012-0823-6]), Dr. Matsushita explained. First, there is a status score, which takes into account four categories: joint space narrowing (scored 0-3), erosion (scored 0-3), joint surface (0-6), and joint stability (0-4). Second, there is a change score, which assesses the same four categories plus the porosity of the joint.
A total of 57 patients with early RA who were about to be treated with TNF-alpha inhibitors were included in the study, and 51 completed 2 years’ treatment with these agents. The most frequently prescribed TNF-alpha inhibitors were infliximab, in 24 patients, and etanercept, used in 14. Another 7 patients switched from infliximab to etanercept, and 6 patients were treated with adalimumab. The mean age of the patients was 60 years, with a mean RA duration of 10.6 years.
The investigators used the ARASHI status score to assess 96 hip and 86 knee joints at baseline (before TNF-alpha inhibitor treatment was started). They later computed the ARASHI change score for the joints at both 1-year and 2-year follow-up visits. A 1-point or more increase in the ARASHI change score constituted radiographic progression. Higher scores indicated higher levels of joint damage.
All of the hip and knee joints with a status score of greater than 2 showed progression of joint damage under TNF-blocking therapies, Dr. Matsushita said. He added that of the joints with a low baseline ARASHI status score (0-2), only 6.5% showed progressive damage over the course of the study. Furthermore, the joint space narrowing score was more closely related to the joint damage subsequently seen than was the erosion score.
Taken together, these findings demonstrate that the "ARASHI scoring method is useful for the evaluation of radiographic damage in large weight-bearing joints, and to predict the risk for progression in patients with RA," Dr. Matsushita said. The next step is to look at the utility of the score in other large joints, perhaps the shoulder, elbow, and ankle joints, he noted.
Dr. Matsushita had no disclosures.
MADRID – A new radiographic scoring method successfully assessed damage in the large joints of patients with rheumatoid arthritis who were being treated with biologic therapy, according to research presented at the annual European Congress of Rheumatology.
The ARASHI (Assessment of Rheumatoid Arthritis by Scoring of Large-Joint Destruction and Healing in Radiographic Imaging) method, developed by a team in Japan, was tested over a period of 2 years in 51 patients who were being newly treated with tumor necrosis factor–alpha (TNF-alpha) inhibitors.
"Evaluation of radiographic damage of the small joints in the hands and feet using the van der Heijde total Sharp score in patients with early RA has been established," said Dr. Isao Matsushita, assistant professor in the orthopedic surgery department at the University of Toyama, Japan.
While the Larsen grade is most often used to assess large joints, this radiographic grading system has several limitations, including a "ceiling effect," resulting from the substantial variation found within each of the six Larsen grades (scored 0-5), he said in an interview at the meeting. Dr. Matsushita and his colleagues developed the ARASHI method to offer a more sensitive means of determining radiographic progression in the large joints.
The ARASHI method is composed of two parts (Mod. Rheumatol. 2013 April 27 [doi: 10.1007/s10165-012-0823-6]), Dr. Matsushita explained. First, there is a status score, which takes into account four categories: joint space narrowing (scored 0-3), erosion (scored 0-3), joint surface (0-6), and joint stability (0-4). Second, there is a change score, which assesses the same four categories plus the porosity of the joint.
A total of 57 patients with early RA who were about to be treated with TNF-alpha inhibitors were included in the study, and 51 completed 2 years’ treatment with these agents. The most frequently prescribed TNF-alpha inhibitors were infliximab, in 24 patients, and etanercept, used in 14. Another 7 patients switched from infliximab to etanercept, and 6 patients were treated with adalimumab. The mean age of the patients was 60 years, with a mean RA duration of 10.6 years.
The investigators used the ARASHI status score to assess 96 hip and 86 knee joints at baseline (before TNF-alpha inhibitor treatment was started). They later computed the ARASHI change score for the joints at both 1-year and 2-year follow-up visits. A 1-point or more increase in the ARASHI change score constituted radiographic progression. Higher scores indicated higher levels of joint damage.
All of the hip and knee joints with a status score of greater than 2 showed progression of joint damage under TNF-blocking therapies, Dr. Matsushita said. He added that of the joints with a low baseline ARASHI status score (0-2), only 6.5% showed progressive damage over the course of the study. Furthermore, the joint space narrowing score was more closely related to the joint damage subsequently seen than was the erosion score.
Taken together, these findings demonstrate that the "ARASHI scoring method is useful for the evaluation of radiographic damage in large weight-bearing joints, and to predict the risk for progression in patients with RA," Dr. Matsushita said. The next step is to look at the utility of the score in other large joints, perhaps the shoulder, elbow, and ankle joints, he noted.
Dr. Matsushita had no disclosures.
AT THE EULAR CONGRESS 2013
Major finding: Only 6.5% of patients with a low (0-2) baseline ARASHI status score showed progressive radiographic damage over the course of the study.
Data source: Study of 51 consecutive patients with active rheumatoid arthritis who underwent 2 years of treatment with TNF-alpha inhibitors.
Disclosures: Dr. Matsushita had no disclosures.
Childbirth increases odds of ACPA-negative, not positive, RA
MADRID – Having a child was associated with ACPA-negative but not ACPA-positive rheumatoid arthritis in a case-control study of almost 5,000 women living in Sweden.
The odds ratio (OR) for ACPA (anti–citrullinated protein antibody)–negative rheumatoid arthritis (RA) comparing parous with nulliparous women was 2.1 in women aged 18-44 years. The effect was not seen in older women, with an OR of 0.9 for women aged 45-70 years.
"The risk seems to be more pronounced in the postpartum period [in the] 2 years before the onset of [RA] symptoms," Cecilia Orellana reported at the annual European Congress of Rheumatology. Indeed, the odds of developing ACPA-positive disease within the first year of childbirth (OR = 2.6) was higher than within 2 years (OR = 1.8).
Ms. Orellana, a second-year postgraduate student within the Institute of Environmental Medicine at the Karolinska Institutet in Stockholm, also noted that the risk of ACPA-negative RA appeared higher in women who had their first child at a young age. The OR for ACPA-negative RA in women younger than 23 years was 2.5, followed by 2.1 for those aged 23-26 years, 1.8 for those aged 27-30 years, and 1.5 for those older than 30 years.
The link between parity and RA has been studied before with some findings suggesting no association and others finding a possible protective effect of parity on the risk of RA. This is the only study to date to look at parity in relation to ACPA status (Ann. Rheum. Dis. 2013;72[Suppl. 3]:102).
The case-control study involved 2,035 women with RA and 2,911 age-matched controls enrolled in the ongoing Swedish EIRA (Epidemiological Investigation of RA) study during 1996-2009. Nearly two-thirds (64%) of women with RA were ACPA positive.
ORs were adjusted for smoking status, education, body mass index, age of menarche, and oral contraceptive use, but none of these adjustments altered the risk of developing RA.
The biological mechanisms behind the increased risk for ACPA-negative RA in women who have given birth needs further study, Ms. Orellana concluded.
The findings appear "counterintuitive" to what clinicians might assume, Dr. Christopher Buckley, professor of rheumatology at the University of Birmingham, England, said in an interview.
"I would have predicted that if women had had more children, there might have been more [ACPA-positive] disease, because you are more likely to have immune suppression, but this [study] actually suggests that women are protected from [ACPA-positive] disease," said Dr. Buckley, who was not involved in the study. "This might mean that pregnancy is not a bad thing," he said, adding that if women do get pregnant they are more likely to have ACPA-negative disease, which actually carries a better prognosis.
As for how these data could help clinicians advise women, Dr. Buckley noted that it is of course very likely that there is more than a single factor at play. Other factors would almost certainly be influencing the risk of RA. But these data beg the question as to how many children a woman might need to have to produce an effect. Since parity seems to influence ACPA-negative RA risk in younger women, the findings might be most relevant in the developing world where women tend to have their children at a younger age.
"It’s one of those results that is completely counterintuitive," Dr. Buckley said, "which usually tells you that there is something going on."
Ms. Orellana and Dr. Buckley had no disclosures. The study was supported by grants from the Swedish Medical Research Council, the Swedish Council for Working Life and Social Research, King Gustav V’s 80-year Foundation, the Swedish Rheumatic Foundation, the Stockholm County Council, and the insurance company AFA.
MADRID – Having a child was associated with ACPA-negative but not ACPA-positive rheumatoid arthritis in a case-control study of almost 5,000 women living in Sweden.
The odds ratio (OR) for ACPA (anti–citrullinated protein antibody)–negative rheumatoid arthritis (RA) comparing parous with nulliparous women was 2.1 in women aged 18-44 years. The effect was not seen in older women, with an OR of 0.9 for women aged 45-70 years.
"The risk seems to be more pronounced in the postpartum period [in the] 2 years before the onset of [RA] symptoms," Cecilia Orellana reported at the annual European Congress of Rheumatology. Indeed, the odds of developing ACPA-positive disease within the first year of childbirth (OR = 2.6) was higher than within 2 years (OR = 1.8).
Ms. Orellana, a second-year postgraduate student within the Institute of Environmental Medicine at the Karolinska Institutet in Stockholm, also noted that the risk of ACPA-negative RA appeared higher in women who had their first child at a young age. The OR for ACPA-negative RA in women younger than 23 years was 2.5, followed by 2.1 for those aged 23-26 years, 1.8 for those aged 27-30 years, and 1.5 for those older than 30 years.
The link between parity and RA has been studied before with some findings suggesting no association and others finding a possible protective effect of parity on the risk of RA. This is the only study to date to look at parity in relation to ACPA status (Ann. Rheum. Dis. 2013;72[Suppl. 3]:102).
The case-control study involved 2,035 women with RA and 2,911 age-matched controls enrolled in the ongoing Swedish EIRA (Epidemiological Investigation of RA) study during 1996-2009. Nearly two-thirds (64%) of women with RA were ACPA positive.
ORs were adjusted for smoking status, education, body mass index, age of menarche, and oral contraceptive use, but none of these adjustments altered the risk of developing RA.
The biological mechanisms behind the increased risk for ACPA-negative RA in women who have given birth needs further study, Ms. Orellana concluded.
The findings appear "counterintuitive" to what clinicians might assume, Dr. Christopher Buckley, professor of rheumatology at the University of Birmingham, England, said in an interview.
"I would have predicted that if women had had more children, there might have been more [ACPA-positive] disease, because you are more likely to have immune suppression, but this [study] actually suggests that women are protected from [ACPA-positive] disease," said Dr. Buckley, who was not involved in the study. "This might mean that pregnancy is not a bad thing," he said, adding that if women do get pregnant they are more likely to have ACPA-negative disease, which actually carries a better prognosis.
As for how these data could help clinicians advise women, Dr. Buckley noted that it is of course very likely that there is more than a single factor at play. Other factors would almost certainly be influencing the risk of RA. But these data beg the question as to how many children a woman might need to have to produce an effect. Since parity seems to influence ACPA-negative RA risk in younger women, the findings might be most relevant in the developing world where women tend to have their children at a younger age.
"It’s one of those results that is completely counterintuitive," Dr. Buckley said, "which usually tells you that there is something going on."
Ms. Orellana and Dr. Buckley had no disclosures. The study was supported by grants from the Swedish Medical Research Council, the Swedish Council for Working Life and Social Research, King Gustav V’s 80-year Foundation, the Swedish Rheumatic Foundation, the Stockholm County Council, and the insurance company AFA.
MADRID – Having a child was associated with ACPA-negative but not ACPA-positive rheumatoid arthritis in a case-control study of almost 5,000 women living in Sweden.
The odds ratio (OR) for ACPA (anti–citrullinated protein antibody)–negative rheumatoid arthritis (RA) comparing parous with nulliparous women was 2.1 in women aged 18-44 years. The effect was not seen in older women, with an OR of 0.9 for women aged 45-70 years.
"The risk seems to be more pronounced in the postpartum period [in the] 2 years before the onset of [RA] symptoms," Cecilia Orellana reported at the annual European Congress of Rheumatology. Indeed, the odds of developing ACPA-positive disease within the first year of childbirth (OR = 2.6) was higher than within 2 years (OR = 1.8).
Ms. Orellana, a second-year postgraduate student within the Institute of Environmental Medicine at the Karolinska Institutet in Stockholm, also noted that the risk of ACPA-negative RA appeared higher in women who had their first child at a young age. The OR for ACPA-negative RA in women younger than 23 years was 2.5, followed by 2.1 for those aged 23-26 years, 1.8 for those aged 27-30 years, and 1.5 for those older than 30 years.
The link between parity and RA has been studied before with some findings suggesting no association and others finding a possible protective effect of parity on the risk of RA. This is the only study to date to look at parity in relation to ACPA status (Ann. Rheum. Dis. 2013;72[Suppl. 3]:102).
The case-control study involved 2,035 women with RA and 2,911 age-matched controls enrolled in the ongoing Swedish EIRA (Epidemiological Investigation of RA) study during 1996-2009. Nearly two-thirds (64%) of women with RA were ACPA positive.
ORs were adjusted for smoking status, education, body mass index, age of menarche, and oral contraceptive use, but none of these adjustments altered the risk of developing RA.
The biological mechanisms behind the increased risk for ACPA-negative RA in women who have given birth needs further study, Ms. Orellana concluded.
The findings appear "counterintuitive" to what clinicians might assume, Dr. Christopher Buckley, professor of rheumatology at the University of Birmingham, England, said in an interview.
"I would have predicted that if women had had more children, there might have been more [ACPA-positive] disease, because you are more likely to have immune suppression, but this [study] actually suggests that women are protected from [ACPA-positive] disease," said Dr. Buckley, who was not involved in the study. "This might mean that pregnancy is not a bad thing," he said, adding that if women do get pregnant they are more likely to have ACPA-negative disease, which actually carries a better prognosis.
As for how these data could help clinicians advise women, Dr. Buckley noted that it is of course very likely that there is more than a single factor at play. Other factors would almost certainly be influencing the risk of RA. But these data beg the question as to how many children a woman might need to have to produce an effect. Since parity seems to influence ACPA-negative RA risk in younger women, the findings might be most relevant in the developing world where women tend to have their children at a younger age.
"It’s one of those results that is completely counterintuitive," Dr. Buckley said, "which usually tells you that there is something going on."
Ms. Orellana and Dr. Buckley had no disclosures. The study was supported by grants from the Swedish Medical Research Council, the Swedish Council for Working Life and Social Research, King Gustav V’s 80-year Foundation, the Swedish Rheumatic Foundation, the Stockholm County Council, and the insurance company AFA.
AT THE EULAR CONGRESS 2013
Major finding: Odds ratios for ACPA-negative and ACPA-positive RA after childbirth were 2.1 and 0.9, respectively, comparing parous with nulliparous women aged 18 years to 44 years.
Data source: Study of 2,035 women with RA and 2,911 age-matched controls from the Swedish EIRA (Epidemiological Investigation of RA) database.
Disclosures: Ms. Orellana and Dr. Buckley had no disclosures. The study was supported by grants from the Swedish Medical Research Council, the Swedish Council for Working Life and Social Research, King Gustav V’s 80-year Foundation, the Swedish Rheumatic Foundation, the Stockholm County Council, and the insurance company AFA.
Evidence grows for TNF inhibitors in spondyloarthritis
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE EULAR CONGRESS 2013
Improved definition boosts peripheral spondyloarthritis diagnoses
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
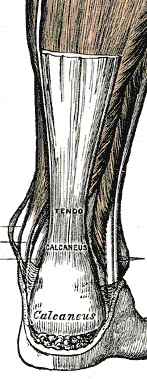
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
ACPA-positivity in RA does not preclude drug-free remission
MADRID – Drug-free remission is possible for rheumatoid arthritis patients with anticitrullinated protein antibodies, although they may not be able to sustain it for as long as ACPA-negative patients.
Still, after treatment with methotrexate and tapered prednisone, more than one-third of ACPA-positive patients experienced drug-free remission for at least some period of time, Dr. Kirsten Wevers-de Boer said at the annual European Congress of Rheumatology.
"With this treatment strategy, the presence of ACPA appears not to preclude drug discontinuation," said Dr. Wevers-de Boer of the department of rheumatology at Leiden University Medical Center in the Netherlands.
She and her colleagues conducted a subanalysis of patients who achieved remission in the IMPROVED study, which examined remission rates in 610 patients with recent-onset rheumatoid or undifferentiated arthritis. They were treated with a two-step regimen of 7 weeks of methotrexate 25 mg/week along with a tapered course of prednisone. Prednisone was started at 60 mg/day and tapered to 7.5 mg/day by the end of the treatment period (Ann. Rheum. Dis. 2013 May 28 [doi:10.1136/annrheumdis-2013-203243]).
Patients not in remission 4 months after the treatment cycle were randomized to either one of two regimens – methotrexate, hydroxychloroquine, sulfasalazine, and low-dose prednisone, or methotrexate plus adalimumab.
Dr. Wevers-de Boer’s subanalysis focused on the 375 patients (61%) who achieved early drug-free remission. They were followed for up to 16 months.
At 1 year, 119 (32%) had remained in drug-free remission. Significantly more of the patients who were in drug-free remission at 1 year were ACPA negative than were those who were not in remission (62% vs. 50%).
At 16 months, 77 patients (65% of the entire group) were still in drug-free remission. Again, ACPA negativity was more often present among those who were still in drug-free remission than it was in those who were not in remission (80% vs. 58%).
Dr. Wevers-de Boer conducted regression analyses to look for any significant baseline factors that might predict the inability to sustain drug-free remission.
In the univariate analysis, significant factors were a high tender joint count at baseline, being ACPA-positive, and fulfilling the 2010 American College of Rheumatology-European League Against Rheumatism diagnostic criteria. In the multivariate analysis, the combination of high tender joint count and meeting the 2010 diagnostic criteria was significantly associated with an inability to sustain remission.
"Patients who are ACPA positive can achieve drug-free remission almost as often as patients who are ACPA negative, although they are somewhat less often able to sustain that," she said.
Dr. Wevers-de Boer disclosed that she has received grant funding from Abbott, which sponsored the IMPROVED study.
MADRID – Drug-free remission is possible for rheumatoid arthritis patients with anticitrullinated protein antibodies, although they may not be able to sustain it for as long as ACPA-negative patients.
Still, after treatment with methotrexate and tapered prednisone, more than one-third of ACPA-positive patients experienced drug-free remission for at least some period of time, Dr. Kirsten Wevers-de Boer said at the annual European Congress of Rheumatology.
"With this treatment strategy, the presence of ACPA appears not to preclude drug discontinuation," said Dr. Wevers-de Boer of the department of rheumatology at Leiden University Medical Center in the Netherlands.
She and her colleagues conducted a subanalysis of patients who achieved remission in the IMPROVED study, which examined remission rates in 610 patients with recent-onset rheumatoid or undifferentiated arthritis. They were treated with a two-step regimen of 7 weeks of methotrexate 25 mg/week along with a tapered course of prednisone. Prednisone was started at 60 mg/day and tapered to 7.5 mg/day by the end of the treatment period (Ann. Rheum. Dis. 2013 May 28 [doi:10.1136/annrheumdis-2013-203243]).
Patients not in remission 4 months after the treatment cycle were randomized to either one of two regimens – methotrexate, hydroxychloroquine, sulfasalazine, and low-dose prednisone, or methotrexate plus adalimumab.
Dr. Wevers-de Boer’s subanalysis focused on the 375 patients (61%) who achieved early drug-free remission. They were followed for up to 16 months.
At 1 year, 119 (32%) had remained in drug-free remission. Significantly more of the patients who were in drug-free remission at 1 year were ACPA negative than were those who were not in remission (62% vs. 50%).
At 16 months, 77 patients (65% of the entire group) were still in drug-free remission. Again, ACPA negativity was more often present among those who were still in drug-free remission than it was in those who were not in remission (80% vs. 58%).
Dr. Wevers-de Boer conducted regression analyses to look for any significant baseline factors that might predict the inability to sustain drug-free remission.
In the univariate analysis, significant factors were a high tender joint count at baseline, being ACPA-positive, and fulfilling the 2010 American College of Rheumatology-European League Against Rheumatism diagnostic criteria. In the multivariate analysis, the combination of high tender joint count and meeting the 2010 diagnostic criteria was significantly associated with an inability to sustain remission.
"Patients who are ACPA positive can achieve drug-free remission almost as often as patients who are ACPA negative, although they are somewhat less often able to sustain that," she said.
Dr. Wevers-de Boer disclosed that she has received grant funding from Abbott, which sponsored the IMPROVED study.
MADRID – Drug-free remission is possible for rheumatoid arthritis patients with anticitrullinated protein antibodies, although they may not be able to sustain it for as long as ACPA-negative patients.
Still, after treatment with methotrexate and tapered prednisone, more than one-third of ACPA-positive patients experienced drug-free remission for at least some period of time, Dr. Kirsten Wevers-de Boer said at the annual European Congress of Rheumatology.
"With this treatment strategy, the presence of ACPA appears not to preclude drug discontinuation," said Dr. Wevers-de Boer of the department of rheumatology at Leiden University Medical Center in the Netherlands.
She and her colleagues conducted a subanalysis of patients who achieved remission in the IMPROVED study, which examined remission rates in 610 patients with recent-onset rheumatoid or undifferentiated arthritis. They were treated with a two-step regimen of 7 weeks of methotrexate 25 mg/week along with a tapered course of prednisone. Prednisone was started at 60 mg/day and tapered to 7.5 mg/day by the end of the treatment period (Ann. Rheum. Dis. 2013 May 28 [doi:10.1136/annrheumdis-2013-203243]).
Patients not in remission 4 months after the treatment cycle were randomized to either one of two regimens – methotrexate, hydroxychloroquine, sulfasalazine, and low-dose prednisone, or methotrexate plus adalimumab.
Dr. Wevers-de Boer’s subanalysis focused on the 375 patients (61%) who achieved early drug-free remission. They were followed for up to 16 months.
At 1 year, 119 (32%) had remained in drug-free remission. Significantly more of the patients who were in drug-free remission at 1 year were ACPA negative than were those who were not in remission (62% vs. 50%).
At 16 months, 77 patients (65% of the entire group) were still in drug-free remission. Again, ACPA negativity was more often present among those who were still in drug-free remission than it was in those who were not in remission (80% vs. 58%).
Dr. Wevers-de Boer conducted regression analyses to look for any significant baseline factors that might predict the inability to sustain drug-free remission.
In the univariate analysis, significant factors were a high tender joint count at baseline, being ACPA-positive, and fulfilling the 2010 American College of Rheumatology-European League Against Rheumatism diagnostic criteria. In the multivariate analysis, the combination of high tender joint count and meeting the 2010 diagnostic criteria was significantly associated with an inability to sustain remission.
"Patients who are ACPA positive can achieve drug-free remission almost as often as patients who are ACPA negative, although they are somewhat less often able to sustain that," she said.
Dr. Wevers-de Boer disclosed that she has received grant funding from Abbott, which sponsored the IMPROVED study.
AT THE EULAR CONGRESS 2013
Major finding: Significantly more of these patients who were in drug-free remission at 1 year were ACPA-negative than were those who were not in remission (62% vs. 50%).
Data source: A subanalysis of 375 patients who achieved early drug-free remission in the IMPROVED study.
Disclosures: Dr. Wevers-de Boer reported receiving grant funding from Abbott, the IMPROVED study sponsor.
Scleroderma patients suffer from small bowel bacterial overgrowth
MADRID – More than a third of patients with systemic sclerosis and intestinal symptoms have an increase in gastrointestinal tract bacteria, an alteration in the type of gut microbes present, or both, based on data from a French study presented at the annual European Congress of Rheumatology.
Small intestinal bacterial overgrowth (SIBO) was found to affect 14 (38%) of 37 patients included in the study. These patients had been recruited from a larger group of 120 scleroderma patients who complained of gastrointestinal symptoms over a 2-year period.
"SIBO can compromise patients’ quality of life and be responsible for mortality," study investigator Dr. Marie Tauber said. SIBO can cause GI symptoms such as bloating, diarrhea, malabsorption, weight loss, and malnutrition, which may have a significant impact on patients’ overall prognosis, she noted.
Dr. Tauber, a dermatologist who took part in the research as part of an internship within the rheumatology department of the Hôpital Cochin in Paris, explained the three goals of the study. The first was to examine the prevalence of SIBO in patients with systemic sclerosis exhibiting GI symptoms, and the second was to identify subsets of patients who might be at increased risk. A third goal was to observe the impact of optimal SIBO treatment on the patients’ conditions.
The median age of participants was 59 years, and 79% were women. The median disease duration was approximately 10 years, and 49% of patients had diffuse cutaneous disease.
A diagnosis of SIBO was based on positive hydrogen and methane breath tests, and blood assays were used to assess the presence of malabsorption.
The researchers also administered two questionnaires – the generic SF-36 (Short Form 36) Health Survey and the disease-specific UCLA SCTC GIT (University of California, Los Angeles, Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument) – to patients at the time of their breath testing visits.
All patients with SIBO were treated with a rotating regimen of amoxicillin, ciprofloxacin, and metronidazole, each given for 1 month at a time. Breath tests, as well as the UCLA SCTC GIT, were repeated. Fewer than 50% of patients had a negative breath test after antibody treatment, which highlighted a need to repeat the test after antibiotic treatment to determine whether a second course is required, Dr. Tauber noted.
Three clinical parameters separated patients with and without SIBO: longer disease duration (11 vs. 7 years; P = .02), lower prevalence of anti-topoisomerase I antibodies (Anti-Scl-70 Ab, 7% vs. 39%; P = .04), and higher prevalence of definite pulmonary arterial hypertension (PAH, 21% vs. 0%; P = .04).
Total UCLA SCTC GIT scores were higher in patients with SIBO than in those without it (0.79 vs. 0.31; P = .03). SIBO-affected patients also were more likely to have weight loss of 5% or more (43% vs. 8%; P = .03).
Given the small number of patients, it is difficult to draw firm conclusions from these data, and larger studies are needed, Dr. Tauber observed. However, the findings suggest that there may be factors associated with SIBO that could be targeted in an intervention program.
Two patients with SIBO died despite antibiotic treatment, which "underscores, unfortunately, the association between SIBO and mortality," Dr. Tauber said.
"To our knowledge, this is the first study using the UCLA SCTC GIT to identify patients at risk of SIBO in systemic sclerosis," and the data support the systematic use of this score, together with regular weight evaluation in these patients, she concluded.
Dr. Tauber had no financial conflicts to disclose.
MADRID – More than a third of patients with systemic sclerosis and intestinal symptoms have an increase in gastrointestinal tract bacteria, an alteration in the type of gut microbes present, or both, based on data from a French study presented at the annual European Congress of Rheumatology.
Small intestinal bacterial overgrowth (SIBO) was found to affect 14 (38%) of 37 patients included in the study. These patients had been recruited from a larger group of 120 scleroderma patients who complained of gastrointestinal symptoms over a 2-year period.
"SIBO can compromise patients’ quality of life and be responsible for mortality," study investigator Dr. Marie Tauber said. SIBO can cause GI symptoms such as bloating, diarrhea, malabsorption, weight loss, and malnutrition, which may have a significant impact on patients’ overall prognosis, she noted.
Dr. Tauber, a dermatologist who took part in the research as part of an internship within the rheumatology department of the Hôpital Cochin in Paris, explained the three goals of the study. The first was to examine the prevalence of SIBO in patients with systemic sclerosis exhibiting GI symptoms, and the second was to identify subsets of patients who might be at increased risk. A third goal was to observe the impact of optimal SIBO treatment on the patients’ conditions.
The median age of participants was 59 years, and 79% were women. The median disease duration was approximately 10 years, and 49% of patients had diffuse cutaneous disease.
A diagnosis of SIBO was based on positive hydrogen and methane breath tests, and blood assays were used to assess the presence of malabsorption.
The researchers also administered two questionnaires – the generic SF-36 (Short Form 36) Health Survey and the disease-specific UCLA SCTC GIT (University of California, Los Angeles, Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument) – to patients at the time of their breath testing visits.
All patients with SIBO were treated with a rotating regimen of amoxicillin, ciprofloxacin, and metronidazole, each given for 1 month at a time. Breath tests, as well as the UCLA SCTC GIT, were repeated. Fewer than 50% of patients had a negative breath test after antibody treatment, which highlighted a need to repeat the test after antibiotic treatment to determine whether a second course is required, Dr. Tauber noted.
Three clinical parameters separated patients with and without SIBO: longer disease duration (11 vs. 7 years; P = .02), lower prevalence of anti-topoisomerase I antibodies (Anti-Scl-70 Ab, 7% vs. 39%; P = .04), and higher prevalence of definite pulmonary arterial hypertension (PAH, 21% vs. 0%; P = .04).
Total UCLA SCTC GIT scores were higher in patients with SIBO than in those without it (0.79 vs. 0.31; P = .03). SIBO-affected patients also were more likely to have weight loss of 5% or more (43% vs. 8%; P = .03).
Given the small number of patients, it is difficult to draw firm conclusions from these data, and larger studies are needed, Dr. Tauber observed. However, the findings suggest that there may be factors associated with SIBO that could be targeted in an intervention program.
Two patients with SIBO died despite antibiotic treatment, which "underscores, unfortunately, the association between SIBO and mortality," Dr. Tauber said.
"To our knowledge, this is the first study using the UCLA SCTC GIT to identify patients at risk of SIBO in systemic sclerosis," and the data support the systematic use of this score, together with regular weight evaluation in these patients, she concluded.
Dr. Tauber had no financial conflicts to disclose.
MADRID – More than a third of patients with systemic sclerosis and intestinal symptoms have an increase in gastrointestinal tract bacteria, an alteration in the type of gut microbes present, or both, based on data from a French study presented at the annual European Congress of Rheumatology.
Small intestinal bacterial overgrowth (SIBO) was found to affect 14 (38%) of 37 patients included in the study. These patients had been recruited from a larger group of 120 scleroderma patients who complained of gastrointestinal symptoms over a 2-year period.
"SIBO can compromise patients’ quality of life and be responsible for mortality," study investigator Dr. Marie Tauber said. SIBO can cause GI symptoms such as bloating, diarrhea, malabsorption, weight loss, and malnutrition, which may have a significant impact on patients’ overall prognosis, she noted.
Dr. Tauber, a dermatologist who took part in the research as part of an internship within the rheumatology department of the Hôpital Cochin in Paris, explained the three goals of the study. The first was to examine the prevalence of SIBO in patients with systemic sclerosis exhibiting GI symptoms, and the second was to identify subsets of patients who might be at increased risk. A third goal was to observe the impact of optimal SIBO treatment on the patients’ conditions.
The median age of participants was 59 years, and 79% were women. The median disease duration was approximately 10 years, and 49% of patients had diffuse cutaneous disease.
A diagnosis of SIBO was based on positive hydrogen and methane breath tests, and blood assays were used to assess the presence of malabsorption.
The researchers also administered two questionnaires – the generic SF-36 (Short Form 36) Health Survey and the disease-specific UCLA SCTC GIT (University of California, Los Angeles, Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument) – to patients at the time of their breath testing visits.
All patients with SIBO were treated with a rotating regimen of amoxicillin, ciprofloxacin, and metronidazole, each given for 1 month at a time. Breath tests, as well as the UCLA SCTC GIT, were repeated. Fewer than 50% of patients had a negative breath test after antibody treatment, which highlighted a need to repeat the test after antibiotic treatment to determine whether a second course is required, Dr. Tauber noted.
Three clinical parameters separated patients with and without SIBO: longer disease duration (11 vs. 7 years; P = .02), lower prevalence of anti-topoisomerase I antibodies (Anti-Scl-70 Ab, 7% vs. 39%; P = .04), and higher prevalence of definite pulmonary arterial hypertension (PAH, 21% vs. 0%; P = .04).
Total UCLA SCTC GIT scores were higher in patients with SIBO than in those without it (0.79 vs. 0.31; P = .03). SIBO-affected patients also were more likely to have weight loss of 5% or more (43% vs. 8%; P = .03).
Given the small number of patients, it is difficult to draw firm conclusions from these data, and larger studies are needed, Dr. Tauber observed. However, the findings suggest that there may be factors associated with SIBO that could be targeted in an intervention program.
Two patients with SIBO died despite antibiotic treatment, which "underscores, unfortunately, the association between SIBO and mortality," Dr. Tauber said.
"To our knowledge, this is the first study using the UCLA SCTC GIT to identify patients at risk of SIBO in systemic sclerosis," and the data support the systematic use of this score, together with regular weight evaluation in these patients, she concluded.
Dr. Tauber had no financial conflicts to disclose.
AT THE EULAR CONGRESS 2013
Major finding: SIBO affected 14 (38%) of 37 scleroderma patients with gastrointestinal symptoms.
Data source: Observational study of 120 adults with systemic sclerosis and intestinal symptoms.
Disclosures: Dr. Tauber had no financial conflicts to disclose.
New biomarkers find 8% more patients with early RA
MADRID – Four newly identified serologic biomarkers have the potential to increase the chances of an early diagnosis for patients with rheumatoid arthritis.
When added to the standard biomarker panel, the new markers – UH-RA.1, UH-RA.9, UH-RA.14, and UH-RA.21 – found about 8% more patients with new-onset RA, Dr. Liesbeth De Winter reported at the annual European Congress of Rheumatology.
The current diagnostic methods, based on 2010 RA Classification Criteria and a two-antibody serological panel, miss about one-third of patients with new-onset disease, said Dr. De Winter of the Biomedical Research Institute of Hasselt University, Diepenbeek, Belgium. The resulting delay in diagnosis decreases the chance of a good outcome for the group.
"Early diagnosis is important, because there is a therapeutic window in the first few years during which early intervention and treatment yield a better outcome, and patients are much more likely to go into remission when treated at this time," she said.
Researchers at the same institute first published on these new biomarkers in 2011 (J. Autoimmun. 2011;36:33-46). Since then, Dr. De Winter said, they have been validated and found to be significantly associated with early-onset disease.
The team used the current diagnostic criteria in a group of 292 patients with RA, 97 healthy controls, and 90 rheumatic controls (including patients with arthritis, ankylosing spondylitis, osteoarthritis, and Sjögren’s syndrome). About one-third (34%) of the RA patients were seronegative for the diagnostic biomarkers of rheumatoid factor and anti-citrullinated protein antibodies (ACPAs). This 34% was termed the "serological gap."
But 26% of these patients were also positive for at least one of the four new biomarkers, "narrowing the serological gap by 8%," Dr. De Winter said. Of the 39 patients with very early RA, 13% were also positive for the new biomarkers, she added.
The test should be easy and inexpensive to implement, as it could simply be added to the current biomarker panel in a routine patient workup, she added.
The next step is to examine whether the markers can predict either disease course or therapeutic response, she said. "It’s already been shown that patients who are positive for ACPA respond differently to treatment. We also want to try and identify their role in the disease process, to help us gain some additional knowledge about it."
Identifying more early-stage patients could have a large impact on disease burden, Dr. Maya Buch said during a press briefing on the study.
"There’s currently a risk that some of our early-stage patients are being neglected because the diagnostic criteria as they are now are weighted toward ACPA-positive patients," said Dr. Buch of the University of Leeds, England. "I think it’s likely that even more biomarkers will be identified over time, further increasing our ability to catch these patients early. Incremental work like this fills the need for patients that we are not currently able to diagnose as early as necessary."
Dr. De Winter had no financial disclosures.
MADRID – Four newly identified serologic biomarkers have the potential to increase the chances of an early diagnosis for patients with rheumatoid arthritis.
When added to the standard biomarker panel, the new markers – UH-RA.1, UH-RA.9, UH-RA.14, and UH-RA.21 – found about 8% more patients with new-onset RA, Dr. Liesbeth De Winter reported at the annual European Congress of Rheumatology.
The current diagnostic methods, based on 2010 RA Classification Criteria and a two-antibody serological panel, miss about one-third of patients with new-onset disease, said Dr. De Winter of the Biomedical Research Institute of Hasselt University, Diepenbeek, Belgium. The resulting delay in diagnosis decreases the chance of a good outcome for the group.
"Early diagnosis is important, because there is a therapeutic window in the first few years during which early intervention and treatment yield a better outcome, and patients are much more likely to go into remission when treated at this time," she said.
Researchers at the same institute first published on these new biomarkers in 2011 (J. Autoimmun. 2011;36:33-46). Since then, Dr. De Winter said, they have been validated and found to be significantly associated with early-onset disease.
The team used the current diagnostic criteria in a group of 292 patients with RA, 97 healthy controls, and 90 rheumatic controls (including patients with arthritis, ankylosing spondylitis, osteoarthritis, and Sjögren’s syndrome). About one-third (34%) of the RA patients were seronegative for the diagnostic biomarkers of rheumatoid factor and anti-citrullinated protein antibodies (ACPAs). This 34% was termed the "serological gap."
But 26% of these patients were also positive for at least one of the four new biomarkers, "narrowing the serological gap by 8%," Dr. De Winter said. Of the 39 patients with very early RA, 13% were also positive for the new biomarkers, she added.
The test should be easy and inexpensive to implement, as it could simply be added to the current biomarker panel in a routine patient workup, she added.
The next step is to examine whether the markers can predict either disease course or therapeutic response, she said. "It’s already been shown that patients who are positive for ACPA respond differently to treatment. We also want to try and identify their role in the disease process, to help us gain some additional knowledge about it."
Identifying more early-stage patients could have a large impact on disease burden, Dr. Maya Buch said during a press briefing on the study.
"There’s currently a risk that some of our early-stage patients are being neglected because the diagnostic criteria as they are now are weighted toward ACPA-positive patients," said Dr. Buch of the University of Leeds, England. "I think it’s likely that even more biomarkers will be identified over time, further increasing our ability to catch these patients early. Incremental work like this fills the need for patients that we are not currently able to diagnose as early as necessary."
Dr. De Winter had no financial disclosures.
MADRID – Four newly identified serologic biomarkers have the potential to increase the chances of an early diagnosis for patients with rheumatoid arthritis.
When added to the standard biomarker panel, the new markers – UH-RA.1, UH-RA.9, UH-RA.14, and UH-RA.21 – found about 8% more patients with new-onset RA, Dr. Liesbeth De Winter reported at the annual European Congress of Rheumatology.
The current diagnostic methods, based on 2010 RA Classification Criteria and a two-antibody serological panel, miss about one-third of patients with new-onset disease, said Dr. De Winter of the Biomedical Research Institute of Hasselt University, Diepenbeek, Belgium. The resulting delay in diagnosis decreases the chance of a good outcome for the group.
"Early diagnosis is important, because there is a therapeutic window in the first few years during which early intervention and treatment yield a better outcome, and patients are much more likely to go into remission when treated at this time," she said.
Researchers at the same institute first published on these new biomarkers in 2011 (J. Autoimmun. 2011;36:33-46). Since then, Dr. De Winter said, they have been validated and found to be significantly associated with early-onset disease.
The team used the current diagnostic criteria in a group of 292 patients with RA, 97 healthy controls, and 90 rheumatic controls (including patients with arthritis, ankylosing spondylitis, osteoarthritis, and Sjögren’s syndrome). About one-third (34%) of the RA patients were seronegative for the diagnostic biomarkers of rheumatoid factor and anti-citrullinated protein antibodies (ACPAs). This 34% was termed the "serological gap."
But 26% of these patients were also positive for at least one of the four new biomarkers, "narrowing the serological gap by 8%," Dr. De Winter said. Of the 39 patients with very early RA, 13% were also positive for the new biomarkers, she added.
The test should be easy and inexpensive to implement, as it could simply be added to the current biomarker panel in a routine patient workup, she added.
The next step is to examine whether the markers can predict either disease course or therapeutic response, she said. "It’s already been shown that patients who are positive for ACPA respond differently to treatment. We also want to try and identify their role in the disease process, to help us gain some additional knowledge about it."
Identifying more early-stage patients could have a large impact on disease burden, Dr. Maya Buch said during a press briefing on the study.
"There’s currently a risk that some of our early-stage patients are being neglected because the diagnostic criteria as they are now are weighted toward ACPA-positive patients," said Dr. Buch of the University of Leeds, England. "I think it’s likely that even more biomarkers will be identified over time, further increasing our ability to catch these patients early. Incremental work like this fills the need for patients that we are not currently able to diagnose as early as necessary."
Dr. De Winter had no financial disclosures.
AT THE EULAR CONGRESS 2013
Major finding: A panel of four new serologic biomarkers found about 8% more patients with early rheumatoid arthritis, improving the rate of missed diagnosis from 34% to 26%.
Data source: A diagnostic study of 292 patients with RA, 97 healthy controls, and 90 rheumatic controls (including patients with arthritis, ankylosing spondylitis, osteoarthritis, and Sjögren’s syndrome).
Disclosures: Dr. De Winter had no financial disclosures.
Apremilast effects sustained at 1 year in psoriatic arthritis
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
AT THE EULAR CONGRESS 2013
Major finding: ACR 20 response at 1 year was 57%-63% for patients given apremilast.
Data source: PALACE 1, a 504-patient, phase III, multicenter, double blind, placebo-controlled study of apremilast for the treatment of active psoriatic arthritis.
Disclosures: Celgene funded the study. Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.