User login
Endocrine Society: Annual Meeting (ENDO 2014)
Program prevented antipsychotic-induced weight gain in youth
CHICAGO – An innovative multidisciplinary lifestyle intervention in youth with first-episode psychosis can prevent the marked weight gain and other adverse cardiometabolic effects that typically arise during the first months of treatment with antipsychotic agents.
"Antipsychotic-induced weight gain can be halted through individualized lifestyle and life-skills interventions. Weight stability in the face of antipsychotic therapy is a realistic and attainable goal," Dr. Katherine Samaras said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The multidisciplinary Australian effort, known as the Keeping the Body in Mind Program, is carried out by Dr. Samaras, an endocrinologist at St. Vincent’s Hospital in Sydney, Australia, together with a psychiatrist, a dietician, and an exercise physiologist. Their motivation in developing the program stems from studies documenting a 20-year life expectancy shortfall in patients with major mental illness, compared with the general population, which Dr. Sue Bailey, past president of the Royal College of Psychiatrists, has called "one of the biggest health scandals of our time."
In addition, as an endocrinologist Dr. Samaras was disturbed to see children and youth on antipsychotic agents in the diabetes clinic on virtually a daily basis. Her own clinical experience was underscored in a recent Tennessee Medicaid program study which found that 6- to 17-year-olds using antipsychotics were at more than threefold increased risk of type 2 diabetes. The risk was evident within the first year and grew with increasing cumulative dose (JAMA Psychiatry 2013;70:1067-75).
"As an endocrinologist, I expect youth with type 1 diabetes to have parity with respect to life expectancy, to maintain their current health, and to develop in education and life skills and have fulfilling life experiences. Imagine if we applied the diabetes care and prevention models we use every day in children with type 1 diabetes to youth with severe mental illness on antipsychotic medications," she mused.
The program is restricted to youth with first-episode psychosis who have been on antipsychotic medication for less than 4 weeks at enrollment. The program entailed weekly individualized counseling and monitoring by a dietician and an exercise physiologist, daily access to a gym converted from a staff conference room in the first-episode psychosis unit, and weekly group life-skills training classes in cooking, shopping, and budgeting.
"There may be very little family support for these people. They’re often living in shelters," Dr. Samaras explained.
She presented a 12-week pilot study involving 16 patients in the Keeping the Body in Mind Program and 12 sociodemographically similar controls in a more conventional Sydney first-episode psychosis program without lifestyle interventions. The subjects were 15-25 years old (mean age, 20 years). The most common psychiatric diagnosis was schizophreniform disorder, followed by bipolar disorder and major depression with psychotic features.
Over the course of 12 weeks, the lifestyle intervention group gained an average of 1.2 kg, compared with 7.3 kg in controls. Moreover, just 12% of the Keeping the Body in Mind Program participants experienced clinically significant weight gain, predefined by the investigators as a greater than 7% increase, compared with 75% of controls. Waist circumference, body mass index, lipids, blood pressure, and fasting blood glucose all remained essentially unchanged over time in the program participants. The group’s aerobic fitness as reflected in peak oxygen intake (VO2max) improved significantly. In contrast, all of these cardiometabolic parameters deteriorated significantly in the control group.
Dr. Samaras noted that most antipsychotic-induced weight gain occurs relatively early in the course of chronic treatment: In one representative study, the average gain was 12 kg during the first 24 months, another 4 kg in the following year, and an additional 3 kg at the 4-year mark.
However, when asked how long young patients with a first episode of major mental illness should remain involved in a lifestyle intervention program such as Keeping the Body in Mind, she was adamant: "I believe that as long as they’re on an antipsychotic agent they should receive dietetic and exercise physiologist support. The key is for us to walk along the path every step of the way for as long as these people need antipsychotics, and not to abandon them to the neglect that I think has characterized the physical health care of mental patients."
The study was supported by the Mental Health and Drug and Alcohol Office of the Ministry of Health for New South Wales. The presenter reported having no financial conflicts.
CHICAGO – An innovative multidisciplinary lifestyle intervention in youth with first-episode psychosis can prevent the marked weight gain and other adverse cardiometabolic effects that typically arise during the first months of treatment with antipsychotic agents.
"Antipsychotic-induced weight gain can be halted through individualized lifestyle and life-skills interventions. Weight stability in the face of antipsychotic therapy is a realistic and attainable goal," Dr. Katherine Samaras said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The multidisciplinary Australian effort, known as the Keeping the Body in Mind Program, is carried out by Dr. Samaras, an endocrinologist at St. Vincent’s Hospital in Sydney, Australia, together with a psychiatrist, a dietician, and an exercise physiologist. Their motivation in developing the program stems from studies documenting a 20-year life expectancy shortfall in patients with major mental illness, compared with the general population, which Dr. Sue Bailey, past president of the Royal College of Psychiatrists, has called "one of the biggest health scandals of our time."
In addition, as an endocrinologist Dr. Samaras was disturbed to see children and youth on antipsychotic agents in the diabetes clinic on virtually a daily basis. Her own clinical experience was underscored in a recent Tennessee Medicaid program study which found that 6- to 17-year-olds using antipsychotics were at more than threefold increased risk of type 2 diabetes. The risk was evident within the first year and grew with increasing cumulative dose (JAMA Psychiatry 2013;70:1067-75).
"As an endocrinologist, I expect youth with type 1 diabetes to have parity with respect to life expectancy, to maintain their current health, and to develop in education and life skills and have fulfilling life experiences. Imagine if we applied the diabetes care and prevention models we use every day in children with type 1 diabetes to youth with severe mental illness on antipsychotic medications," she mused.
The program is restricted to youth with first-episode psychosis who have been on antipsychotic medication for less than 4 weeks at enrollment. The program entailed weekly individualized counseling and monitoring by a dietician and an exercise physiologist, daily access to a gym converted from a staff conference room in the first-episode psychosis unit, and weekly group life-skills training classes in cooking, shopping, and budgeting.
"There may be very little family support for these people. They’re often living in shelters," Dr. Samaras explained.
She presented a 12-week pilot study involving 16 patients in the Keeping the Body in Mind Program and 12 sociodemographically similar controls in a more conventional Sydney first-episode psychosis program without lifestyle interventions. The subjects were 15-25 years old (mean age, 20 years). The most common psychiatric diagnosis was schizophreniform disorder, followed by bipolar disorder and major depression with psychotic features.
Over the course of 12 weeks, the lifestyle intervention group gained an average of 1.2 kg, compared with 7.3 kg in controls. Moreover, just 12% of the Keeping the Body in Mind Program participants experienced clinically significant weight gain, predefined by the investigators as a greater than 7% increase, compared with 75% of controls. Waist circumference, body mass index, lipids, blood pressure, and fasting blood glucose all remained essentially unchanged over time in the program participants. The group’s aerobic fitness as reflected in peak oxygen intake (VO2max) improved significantly. In contrast, all of these cardiometabolic parameters deteriorated significantly in the control group.
Dr. Samaras noted that most antipsychotic-induced weight gain occurs relatively early in the course of chronic treatment: In one representative study, the average gain was 12 kg during the first 24 months, another 4 kg in the following year, and an additional 3 kg at the 4-year mark.
However, when asked how long young patients with a first episode of major mental illness should remain involved in a lifestyle intervention program such as Keeping the Body in Mind, she was adamant: "I believe that as long as they’re on an antipsychotic agent they should receive dietetic and exercise physiologist support. The key is for us to walk along the path every step of the way for as long as these people need antipsychotics, and not to abandon them to the neglect that I think has characterized the physical health care of mental patients."
The study was supported by the Mental Health and Drug and Alcohol Office of the Ministry of Health for New South Wales. The presenter reported having no financial conflicts.
CHICAGO – An innovative multidisciplinary lifestyle intervention in youth with first-episode psychosis can prevent the marked weight gain and other adverse cardiometabolic effects that typically arise during the first months of treatment with antipsychotic agents.
"Antipsychotic-induced weight gain can be halted through individualized lifestyle and life-skills interventions. Weight stability in the face of antipsychotic therapy is a realistic and attainable goal," Dr. Katherine Samaras said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The multidisciplinary Australian effort, known as the Keeping the Body in Mind Program, is carried out by Dr. Samaras, an endocrinologist at St. Vincent’s Hospital in Sydney, Australia, together with a psychiatrist, a dietician, and an exercise physiologist. Their motivation in developing the program stems from studies documenting a 20-year life expectancy shortfall in patients with major mental illness, compared with the general population, which Dr. Sue Bailey, past president of the Royal College of Psychiatrists, has called "one of the biggest health scandals of our time."
In addition, as an endocrinologist Dr. Samaras was disturbed to see children and youth on antipsychotic agents in the diabetes clinic on virtually a daily basis. Her own clinical experience was underscored in a recent Tennessee Medicaid program study which found that 6- to 17-year-olds using antipsychotics were at more than threefold increased risk of type 2 diabetes. The risk was evident within the first year and grew with increasing cumulative dose (JAMA Psychiatry 2013;70:1067-75).
"As an endocrinologist, I expect youth with type 1 diabetes to have parity with respect to life expectancy, to maintain their current health, and to develop in education and life skills and have fulfilling life experiences. Imagine if we applied the diabetes care and prevention models we use every day in children with type 1 diabetes to youth with severe mental illness on antipsychotic medications," she mused.
The program is restricted to youth with first-episode psychosis who have been on antipsychotic medication for less than 4 weeks at enrollment. The program entailed weekly individualized counseling and monitoring by a dietician and an exercise physiologist, daily access to a gym converted from a staff conference room in the first-episode psychosis unit, and weekly group life-skills training classes in cooking, shopping, and budgeting.
"There may be very little family support for these people. They’re often living in shelters," Dr. Samaras explained.
She presented a 12-week pilot study involving 16 patients in the Keeping the Body in Mind Program and 12 sociodemographically similar controls in a more conventional Sydney first-episode psychosis program without lifestyle interventions. The subjects were 15-25 years old (mean age, 20 years). The most common psychiatric diagnosis was schizophreniform disorder, followed by bipolar disorder and major depression with psychotic features.
Over the course of 12 weeks, the lifestyle intervention group gained an average of 1.2 kg, compared with 7.3 kg in controls. Moreover, just 12% of the Keeping the Body in Mind Program participants experienced clinically significant weight gain, predefined by the investigators as a greater than 7% increase, compared with 75% of controls. Waist circumference, body mass index, lipids, blood pressure, and fasting blood glucose all remained essentially unchanged over time in the program participants. The group’s aerobic fitness as reflected in peak oxygen intake (VO2max) improved significantly. In contrast, all of these cardiometabolic parameters deteriorated significantly in the control group.
Dr. Samaras noted that most antipsychotic-induced weight gain occurs relatively early in the course of chronic treatment: In one representative study, the average gain was 12 kg during the first 24 months, another 4 kg in the following year, and an additional 3 kg at the 4-year mark.
However, when asked how long young patients with a first episode of major mental illness should remain involved in a lifestyle intervention program such as Keeping the Body in Mind, she was adamant: "I believe that as long as they’re on an antipsychotic agent they should receive dietetic and exercise physiologist support. The key is for us to walk along the path every step of the way for as long as these people need antipsychotics, and not to abandon them to the neglect that I think has characterized the physical health care of mental patients."
The study was supported by the Mental Health and Drug and Alcohol Office of the Ministry of Health for New South Wales. The presenter reported having no financial conflicts.
AT ICE/ENDO 2014
Key clinical point: Prescribing antipsychotics for children and youth is associated with a high risk of clinically significant weight gain and cardiometabolic deterioration, which can be prevented through an early lifestyle intervention.
Major finding: Twelve percent of young patients on antipsychotic agents for first-episode psychosis experienced a greater than 7% weight gain after 12 weeks in a novel lifestyle intervention program, compared with 75% of nonparticipating controls.
Data source: This pilot study compared outcomes in 16 youth who participated in a 12-week multidisciplinary lifestyle intervention and 12 controls who received usual care. All had gone on antipsychotic medications less than 4 weeks earlier for first-episode psychosis.
Disclosures: The study was supported by the Mental Health and Drug and Alcohol Office of the Ministry of Health for New South Wales. The presenter reported having no financial conflicts.
Thiazide diuretics commonly unmask primary hyperparathyroidism
CHICAGO – More than half of patients who discontinue thiazide diuretics due to hypercalcemia will remain hypercalcemic even after stopping the drugs, and will eventually be diagnosed with primary hyperparathyroidism, according to a retrospective review from the Mayo Clinic in Rochester, Minn.
Those patients probably have subclinical primary hyperparathyroidism (PHP) disease before starting thiazides, and it may have contributed to their hypertension. In the study, PHP was likely unmasked by thiazide treatment, which reduces calcium excretion. "In our clinical practice, it’s not uncommon for us to stop thiazides, and then find calcium levels don’t normalize. Now we have data to confirm our clinical impression," said senior investigator Dr. Robert Wermers, an endocrinologist in the departments of endocrinology, diabetes, metabolism and nutrition at Mayo.
The finding is something to keep in mind when prescribing thiazides. In almost all patients, they were prescribed for hypertension. Hypercalcemia was an incidental finding in the study; none of the patients were symptomatic. Older women were most at risk for PHP, and surgery was the usual treatment, he said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
In all, the team reviewed 220 patients diagnosed with thiazide-associated hypercalcemia between 1992 and 2010. They were a median of 68 years old; 190 (86%) were women.
Eighty-one (37%) of those patients were taken off the drug; hypercalcemia persisted in 49 (60%) patients, of whom 43 (88%) were subsequently diagnosed with PHP.
The findings suggest that "primary hyperparathyroidism is common in patients who develop hypercalcemia while taking thiazide diuretics," the investigators said.
Compared with the overall patient population of 220, those who were diagnosed with PHP had a slightly higher maximum serum calcium while on thiazides (mean 10.9 vs. 10.7 mg/dL) and had been on thiazides a shorter period of time when hypercalcemia was detected (median 2.9 vs. 3.9 years). More than 80% of the patients in both groups were women, and the mean age at onset of hypercalcemia was about 67 years. Serum calcium was normal in both groups before thiazide treatment (median 9.7 mg/dL for both groups).
Of the 139 (63%) patients who stayed on thiazides despite hypercalcemia, 71 (51%) remained hypercalcemic, seven (5%) were eventually diagnosed with PHP, and calcium normalized in 68 (48.9%).
The overall incidence of thiazide associated hypercalcemia was 17 cases per 100,000 person-years. The highest rate was 314.3/100,000 person-years in women 65-74 years old. The incidence started climbing in the mid-1990s and peaked in 1999 at 31.7 cases per 100,000 person-years, perhaps because the guidelines released at the time that called for increased osteoporosis screening. In 2010, the incidence was about 20 cases per 100,000 person-years.
The investigators have no disclosures, and had no outside funding for the project.
CHICAGO – More than half of patients who discontinue thiazide diuretics due to hypercalcemia will remain hypercalcemic even after stopping the drugs, and will eventually be diagnosed with primary hyperparathyroidism, according to a retrospective review from the Mayo Clinic in Rochester, Minn.
Those patients probably have subclinical primary hyperparathyroidism (PHP) disease before starting thiazides, and it may have contributed to their hypertension. In the study, PHP was likely unmasked by thiazide treatment, which reduces calcium excretion. "In our clinical practice, it’s not uncommon for us to stop thiazides, and then find calcium levels don’t normalize. Now we have data to confirm our clinical impression," said senior investigator Dr. Robert Wermers, an endocrinologist in the departments of endocrinology, diabetes, metabolism and nutrition at Mayo.
The finding is something to keep in mind when prescribing thiazides. In almost all patients, they were prescribed for hypertension. Hypercalcemia was an incidental finding in the study; none of the patients were symptomatic. Older women were most at risk for PHP, and surgery was the usual treatment, he said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
In all, the team reviewed 220 patients diagnosed with thiazide-associated hypercalcemia between 1992 and 2010. They were a median of 68 years old; 190 (86%) were women.
Eighty-one (37%) of those patients were taken off the drug; hypercalcemia persisted in 49 (60%) patients, of whom 43 (88%) were subsequently diagnosed with PHP.
The findings suggest that "primary hyperparathyroidism is common in patients who develop hypercalcemia while taking thiazide diuretics," the investigators said.
Compared with the overall patient population of 220, those who were diagnosed with PHP had a slightly higher maximum serum calcium while on thiazides (mean 10.9 vs. 10.7 mg/dL) and had been on thiazides a shorter period of time when hypercalcemia was detected (median 2.9 vs. 3.9 years). More than 80% of the patients in both groups were women, and the mean age at onset of hypercalcemia was about 67 years. Serum calcium was normal in both groups before thiazide treatment (median 9.7 mg/dL for both groups).
Of the 139 (63%) patients who stayed on thiazides despite hypercalcemia, 71 (51%) remained hypercalcemic, seven (5%) were eventually diagnosed with PHP, and calcium normalized in 68 (48.9%).
The overall incidence of thiazide associated hypercalcemia was 17 cases per 100,000 person-years. The highest rate was 314.3/100,000 person-years in women 65-74 years old. The incidence started climbing in the mid-1990s and peaked in 1999 at 31.7 cases per 100,000 person-years, perhaps because the guidelines released at the time that called for increased osteoporosis screening. In 2010, the incidence was about 20 cases per 100,000 person-years.
The investigators have no disclosures, and had no outside funding for the project.
CHICAGO – More than half of patients who discontinue thiazide diuretics due to hypercalcemia will remain hypercalcemic even after stopping the drugs, and will eventually be diagnosed with primary hyperparathyroidism, according to a retrospective review from the Mayo Clinic in Rochester, Minn.
Those patients probably have subclinical primary hyperparathyroidism (PHP) disease before starting thiazides, and it may have contributed to their hypertension. In the study, PHP was likely unmasked by thiazide treatment, which reduces calcium excretion. "In our clinical practice, it’s not uncommon for us to stop thiazides, and then find calcium levels don’t normalize. Now we have data to confirm our clinical impression," said senior investigator Dr. Robert Wermers, an endocrinologist in the departments of endocrinology, diabetes, metabolism and nutrition at Mayo.
The finding is something to keep in mind when prescribing thiazides. In almost all patients, they were prescribed for hypertension. Hypercalcemia was an incidental finding in the study; none of the patients were symptomatic. Older women were most at risk for PHP, and surgery was the usual treatment, he said at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
In all, the team reviewed 220 patients diagnosed with thiazide-associated hypercalcemia between 1992 and 2010. They were a median of 68 years old; 190 (86%) were women.
Eighty-one (37%) of those patients were taken off the drug; hypercalcemia persisted in 49 (60%) patients, of whom 43 (88%) were subsequently diagnosed with PHP.
The findings suggest that "primary hyperparathyroidism is common in patients who develop hypercalcemia while taking thiazide diuretics," the investigators said.
Compared with the overall patient population of 220, those who were diagnosed with PHP had a slightly higher maximum serum calcium while on thiazides (mean 10.9 vs. 10.7 mg/dL) and had been on thiazides a shorter period of time when hypercalcemia was detected (median 2.9 vs. 3.9 years). More than 80% of the patients in both groups were women, and the mean age at onset of hypercalcemia was about 67 years. Serum calcium was normal in both groups before thiazide treatment (median 9.7 mg/dL for both groups).
Of the 139 (63%) patients who stayed on thiazides despite hypercalcemia, 71 (51%) remained hypercalcemic, seven (5%) were eventually diagnosed with PHP, and calcium normalized in 68 (48.9%).
The overall incidence of thiazide associated hypercalcemia was 17 cases per 100,000 person-years. The highest rate was 314.3/100,000 person-years in women 65-74 years old. The incidence started climbing in the mid-1990s and peaked in 1999 at 31.7 cases per 100,000 person-years, perhaps because the guidelines released at the time that called for increased osteoporosis screening. In 2010, the incidence was about 20 cases per 100,000 person-years.
The investigators have no disclosures, and had no outside funding for the project.
AT ICE/ENDO 2014
Key clinical point: Be on the lookout for primary hyperparathyroidism when patients come off thiazides due to elevated serum calcium.
Major finding: Among patients taken off thiazide diuretics because of high serum calcium, hypercalcemia persisted in 49 (60%) patients, of whom 43 (88%) were subsequently diagnosed with primary hyperparathyroidism.
Data Source: Retrospective review of 220 patients diagnosed with thiazide-associated hypercalcemia
Disclosures: The investigators have no disclosures and had no outside funding for their work.
Statin use linked to memory decline in elderly
CHICAGO – More liberal lipid targets in elderly patients and lower statin doses might offset the risk of memory decline associated with statin use in these patients, Australian investigators suggested.
Dr. Katherine Samaras and her associates did neuropsychometric testing on 377 subjects 70-90 years old who had been on statins for 2-22 years, and 301 controls who had not taken the drugs. They then repeated the assessments at 2 and 4 years, and calculated composite, normalized z scores for various cognitive functions.
The team found a significantly greater decline in memory z score from baseline among statin users at both 2 and 4 years (4-year z score –0.27 vs. –0.07).
However, statin use was not associated with greater 4-year declines in language, processing speed, or visuospatial or executive functions. Also, metabolic syndrome was not associated with accelerated cognitive decline, Dr. Samaras reported at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The analysis controlled for age, sex, education, smoking, the presence of hypertension, diabetes, heart disease, stroke, obesity, and the presence of apolipoprotein E e4 genotype (APOEe4), which increases the risk for Alzheimer’s disease.
Previous stroke was significantly associated with an even greater memory decline among statin users. Smoking and APOEe4 seemed to be, as well, but the trends were not significant.
The subjects were part of the Sydney Memory and Ageing Study, a longitudinal cohort of community-dwelling, well elderly from the affluent part of Sydney. None had dementia.
The findings add weight to the Food and Drug Administration's warning about statin use and memory loss in 2012.
This has "made me look very closely at who I prescribe statins for. People do report cognitive changes" if asked, said Dr. Samaras of the Garvan Institute of Medical Research and the University of New South Wales in Sydney.
To forestall memory loss, "I wonder if we should have a greater range of appropriate lipid targets for the elderly, just as we have for hemoglobin A1c," she said. For now, if an elderly person is "really tightly controlled and well under the benchmark we are trying to reach [with statins], then I reduce the dose," with appropriate follow-up, Dr. Samaras said.
Trials of lipid-lowering therapy should include formal cognitive measurements, as well. "As a prescriber, I’d like to know that data," she said.
The subjects in the study were about 80 years old on average, and about equally split between men and women. The average body mass index was 27.1 kg/m2, and the average fasting glucose level was 5.6 mmol/L. Sixty percent of statin users and 45.9% of nonusers had metabolic syndrome; 15.2% of statin users and 5.5% of nonusers had diabetes.
Australia’s National Health and Medical Research Council funded the work. Dr. Samaras and her colleagues said they had no disclosures.
CHICAGO – More liberal lipid targets in elderly patients and lower statin doses might offset the risk of memory decline associated with statin use in these patients, Australian investigators suggested.
Dr. Katherine Samaras and her associates did neuropsychometric testing on 377 subjects 70-90 years old who had been on statins for 2-22 years, and 301 controls who had not taken the drugs. They then repeated the assessments at 2 and 4 years, and calculated composite, normalized z scores for various cognitive functions.
The team found a significantly greater decline in memory z score from baseline among statin users at both 2 and 4 years (4-year z score –0.27 vs. –0.07).
However, statin use was not associated with greater 4-year declines in language, processing speed, or visuospatial or executive functions. Also, metabolic syndrome was not associated with accelerated cognitive decline, Dr. Samaras reported at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The analysis controlled for age, sex, education, smoking, the presence of hypertension, diabetes, heart disease, stroke, obesity, and the presence of apolipoprotein E e4 genotype (APOEe4), which increases the risk for Alzheimer’s disease.
Previous stroke was significantly associated with an even greater memory decline among statin users. Smoking and APOEe4 seemed to be, as well, but the trends were not significant.
The subjects were part of the Sydney Memory and Ageing Study, a longitudinal cohort of community-dwelling, well elderly from the affluent part of Sydney. None had dementia.
The findings add weight to the Food and Drug Administration's warning about statin use and memory loss in 2012.
This has "made me look very closely at who I prescribe statins for. People do report cognitive changes" if asked, said Dr. Samaras of the Garvan Institute of Medical Research and the University of New South Wales in Sydney.
To forestall memory loss, "I wonder if we should have a greater range of appropriate lipid targets for the elderly, just as we have for hemoglobin A1c," she said. For now, if an elderly person is "really tightly controlled and well under the benchmark we are trying to reach [with statins], then I reduce the dose," with appropriate follow-up, Dr. Samaras said.
Trials of lipid-lowering therapy should include formal cognitive measurements, as well. "As a prescriber, I’d like to know that data," she said.
The subjects in the study were about 80 years old on average, and about equally split between men and women. The average body mass index was 27.1 kg/m2, and the average fasting glucose level was 5.6 mmol/L. Sixty percent of statin users and 45.9% of nonusers had metabolic syndrome; 15.2% of statin users and 5.5% of nonusers had diabetes.
Australia’s National Health and Medical Research Council funded the work. Dr. Samaras and her colleagues said they had no disclosures.
CHICAGO – More liberal lipid targets in elderly patients and lower statin doses might offset the risk of memory decline associated with statin use in these patients, Australian investigators suggested.
Dr. Katherine Samaras and her associates did neuropsychometric testing on 377 subjects 70-90 years old who had been on statins for 2-22 years, and 301 controls who had not taken the drugs. They then repeated the assessments at 2 and 4 years, and calculated composite, normalized z scores for various cognitive functions.
The team found a significantly greater decline in memory z score from baseline among statin users at both 2 and 4 years (4-year z score –0.27 vs. –0.07).
However, statin use was not associated with greater 4-year declines in language, processing speed, or visuospatial or executive functions. Also, metabolic syndrome was not associated with accelerated cognitive decline, Dr. Samaras reported at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The analysis controlled for age, sex, education, smoking, the presence of hypertension, diabetes, heart disease, stroke, obesity, and the presence of apolipoprotein E e4 genotype (APOEe4), which increases the risk for Alzheimer’s disease.
Previous stroke was significantly associated with an even greater memory decline among statin users. Smoking and APOEe4 seemed to be, as well, but the trends were not significant.
The subjects were part of the Sydney Memory and Ageing Study, a longitudinal cohort of community-dwelling, well elderly from the affluent part of Sydney. None had dementia.
The findings add weight to the Food and Drug Administration's warning about statin use and memory loss in 2012.
This has "made me look very closely at who I prescribe statins for. People do report cognitive changes" if asked, said Dr. Samaras of the Garvan Institute of Medical Research and the University of New South Wales in Sydney.
To forestall memory loss, "I wonder if we should have a greater range of appropriate lipid targets for the elderly, just as we have for hemoglobin A1c," she said. For now, if an elderly person is "really tightly controlled and well under the benchmark we are trying to reach [with statins], then I reduce the dose," with appropriate follow-up, Dr. Samaras said.
Trials of lipid-lowering therapy should include formal cognitive measurements, as well. "As a prescriber, I’d like to know that data," she said.
The subjects in the study were about 80 years old on average, and about equally split between men and women. The average body mass index was 27.1 kg/m2, and the average fasting glucose level was 5.6 mmol/L. Sixty percent of statin users and 45.9% of nonusers had metabolic syndrome; 15.2% of statin users and 5.5% of nonusers had diabetes.
Australia’s National Health and Medical Research Council funded the work. Dr. Samaras and her colleagues said they had no disclosures.
AT ICE/ENDO 2014
Key clinical point: Looser treatment targets for statins in the elderly may help reduce drug-associated memory loss.
Major finding: Compared with their peers, elderly statin users have a significantly greater decline in memory z scores from baseline at both 2 and 4 years (4-year z score –0.27 vs. –0.07).
Data source: Neuropsychometric testing in almost 700 patients aged 70-90 years.
Disclosures: Australia’s National Health and Medical Research Council funded the work. The investigators have no disclosures.
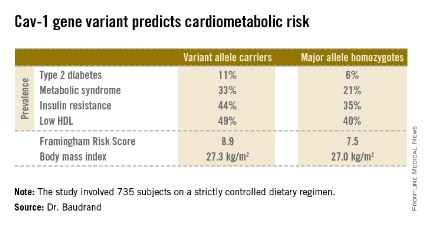
Gene variant detects increased cardiometabolic risk among nonobese
CHICAGO – Normal-weight individuals who carry a common variant of the caveolin-1 gene are at nearly fourfold increased risk of the metabolic syndrome compared with those who are homozygous for the major allele, according to a cross-sectional case-control study.
"This particular genotype may improve individual risk profiling and help detect nonobese subjects who are metabolically unhealthy and at increased cardiovascular risk before they experience severe clinical events," Dr. Rene Baudrand observed at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
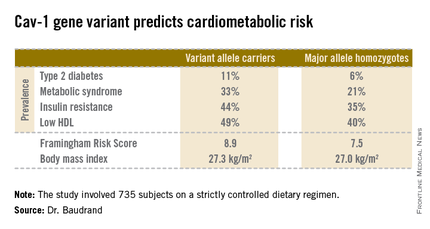
These findings take on added clinical import in light of mounting evidence that the long-term risks of cardiovascular events and type 2 diabetes in patients with the metabolic syndrome are of similar magnitude regardless of whether an individual is lean, overweight, or obese.
"There is no linear relationship between cardiovascular risk and BMI [body mass index]. So assessment of individual cardiovascular risk should involve more in-depth consideration than BMI alone," said Dr. Baudrand of Brigham and Women’s Hospital, Boston, and the Pontifical Catholic University of Chile, Santiago.
He and others have previously shown that caveolin-1 (cav-1) plays a critical role in cholesterol trafficking and signal transduction. It interacts with insulin receptors, steroid receptors, and ion channels.
The objective of the new study was to investigate the role of a suspected culprit cav-1 gene variant known as cav-1 rs926198 in terms of cardiometabolic risk. Expression of cav-1 has been shown to be significantly diminished in carriers of the variant allele.
The study included 735 white and Hispanic subjects on a strictly controlled dietary regimen. They averaged 45 years of age, with a mean BMI of 27.2 kg/m2. Two-thirds of participants were hypertensive, 9% had type 2 diabetes, and 30% had metabolic syndrome. Among the 200 obese subjects, the prevalence of metabolic syndrome was 62%, compared with 18% among the 535 nonobese subjects.
Fully 57% of subjects were found to carry the cav-1 gene variant. The other 43% were homozygous for what is known as the major allele. Carriers of the cav-1 gene variant were found to have significantly higher rates of type 2 diabetes, prediabetes, metabolic syndrome, and other abnormalities than those with the major allele (see chart). These differences were not explainable by differences in BMI; indeed, the average BMI in the two groups was nearly identical, according to Dr. Baudrand.
He and his coworkers also sought to learn whether study participants with metabolic syndrome would be more likely to have a sibling with metabolic syndrome if they were concordant for the cav-1 gene variant. This proved to be the case. In evaluating 348 subjects belonging to 142 sibships, the likelihood of concordance for metabolic syndrome was threefold greater if the siblings shared the cav-1 risk allele than if they were cav-1 discordant.
Upon closer scrutiny of the data, it became apparent that the seriously unfavorable cardiometabolic profile associated with the cav-1 gene variant was confined to the nonobese subjects. In a multivariate analysis adjusted for age, gender, BMI, and study site, the likelihood of metabolic syndrome among nonobese subjects with the variant allele was 3.86-fold higher than in nonobese individuals carrying the major allele. In addition, the adjusted likelihood of type 2 diabetes was 2.26-fold greater and that of low HDL was 1.78-fold greater, with all differences highly statistically significant. In contrast, the risk of these cardiometabolic problems in obese subjects didn’t vary regardless of the form of the cav-1 gene they possessed.
On the basis of these encouraging findings, the next step will be to conduct prospective studies to see if cav-1 genotyping is useful as a screening tool for cardiometabolic risk in nonobese patients. Further investigation is also warranted to identify the specific mechanisms by which the cav-1 risk allele results in cardiometabolic impairment. Among the leading possibilities are defects in aldosterone signaling, the insulin receptor, or adipocyte function, Dr. Baudrand said.
This study was supported by the National Institutes of Health and the Chilean National Science and Technology Research Fund. Dr. Baudrand reported having no financial conflicts.
CHICAGO – Normal-weight individuals who carry a common variant of the caveolin-1 gene are at nearly fourfold increased risk of the metabolic syndrome compared with those who are homozygous for the major allele, according to a cross-sectional case-control study.
"This particular genotype may improve individual risk profiling and help detect nonobese subjects who are metabolically unhealthy and at increased cardiovascular risk before they experience severe clinical events," Dr. Rene Baudrand observed at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
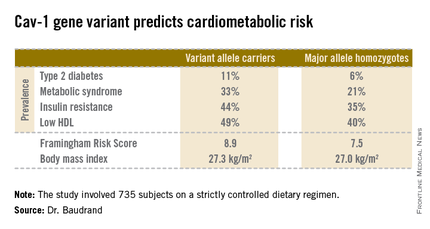
These findings take on added clinical import in light of mounting evidence that the long-term risks of cardiovascular events and type 2 diabetes in patients with the metabolic syndrome are of similar magnitude regardless of whether an individual is lean, overweight, or obese.
"There is no linear relationship between cardiovascular risk and BMI [body mass index]. So assessment of individual cardiovascular risk should involve more in-depth consideration than BMI alone," said Dr. Baudrand of Brigham and Women’s Hospital, Boston, and the Pontifical Catholic University of Chile, Santiago.
He and others have previously shown that caveolin-1 (cav-1) plays a critical role in cholesterol trafficking and signal transduction. It interacts with insulin receptors, steroid receptors, and ion channels.
The objective of the new study was to investigate the role of a suspected culprit cav-1 gene variant known as cav-1 rs926198 in terms of cardiometabolic risk. Expression of cav-1 has been shown to be significantly diminished in carriers of the variant allele.
The study included 735 white and Hispanic subjects on a strictly controlled dietary regimen. They averaged 45 years of age, with a mean BMI of 27.2 kg/m2. Two-thirds of participants were hypertensive, 9% had type 2 diabetes, and 30% had metabolic syndrome. Among the 200 obese subjects, the prevalence of metabolic syndrome was 62%, compared with 18% among the 535 nonobese subjects.
Fully 57% of subjects were found to carry the cav-1 gene variant. The other 43% were homozygous for what is known as the major allele. Carriers of the cav-1 gene variant were found to have significantly higher rates of type 2 diabetes, prediabetes, metabolic syndrome, and other abnormalities than those with the major allele (see chart). These differences were not explainable by differences in BMI; indeed, the average BMI in the two groups was nearly identical, according to Dr. Baudrand.
He and his coworkers also sought to learn whether study participants with metabolic syndrome would be more likely to have a sibling with metabolic syndrome if they were concordant for the cav-1 gene variant. This proved to be the case. In evaluating 348 subjects belonging to 142 sibships, the likelihood of concordance for metabolic syndrome was threefold greater if the siblings shared the cav-1 risk allele than if they were cav-1 discordant.
Upon closer scrutiny of the data, it became apparent that the seriously unfavorable cardiometabolic profile associated with the cav-1 gene variant was confined to the nonobese subjects. In a multivariate analysis adjusted for age, gender, BMI, and study site, the likelihood of metabolic syndrome among nonobese subjects with the variant allele was 3.86-fold higher than in nonobese individuals carrying the major allele. In addition, the adjusted likelihood of type 2 diabetes was 2.26-fold greater and that of low HDL was 1.78-fold greater, with all differences highly statistically significant. In contrast, the risk of these cardiometabolic problems in obese subjects didn’t vary regardless of the form of the cav-1 gene they possessed.
On the basis of these encouraging findings, the next step will be to conduct prospective studies to see if cav-1 genotyping is useful as a screening tool for cardiometabolic risk in nonobese patients. Further investigation is also warranted to identify the specific mechanisms by which the cav-1 risk allele results in cardiometabolic impairment. Among the leading possibilities are defects in aldosterone signaling, the insulin receptor, or adipocyte function, Dr. Baudrand said.
This study was supported by the National Institutes of Health and the Chilean National Science and Technology Research Fund. Dr. Baudrand reported having no financial conflicts.
CHICAGO – Normal-weight individuals who carry a common variant of the caveolin-1 gene are at nearly fourfold increased risk of the metabolic syndrome compared with those who are homozygous for the major allele, according to a cross-sectional case-control study.
"This particular genotype may improve individual risk profiling and help detect nonobese subjects who are metabolically unhealthy and at increased cardiovascular risk before they experience severe clinical events," Dr. Rene Baudrand observed at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
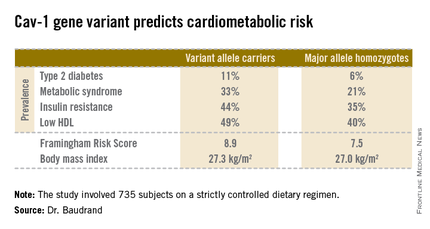
These findings take on added clinical import in light of mounting evidence that the long-term risks of cardiovascular events and type 2 diabetes in patients with the metabolic syndrome are of similar magnitude regardless of whether an individual is lean, overweight, or obese.
"There is no linear relationship between cardiovascular risk and BMI [body mass index]. So assessment of individual cardiovascular risk should involve more in-depth consideration than BMI alone," said Dr. Baudrand of Brigham and Women’s Hospital, Boston, and the Pontifical Catholic University of Chile, Santiago.
He and others have previously shown that caveolin-1 (cav-1) plays a critical role in cholesterol trafficking and signal transduction. It interacts with insulin receptors, steroid receptors, and ion channels.
The objective of the new study was to investigate the role of a suspected culprit cav-1 gene variant known as cav-1 rs926198 in terms of cardiometabolic risk. Expression of cav-1 has been shown to be significantly diminished in carriers of the variant allele.
The study included 735 white and Hispanic subjects on a strictly controlled dietary regimen. They averaged 45 years of age, with a mean BMI of 27.2 kg/m2. Two-thirds of participants were hypertensive, 9% had type 2 diabetes, and 30% had metabolic syndrome. Among the 200 obese subjects, the prevalence of metabolic syndrome was 62%, compared with 18% among the 535 nonobese subjects.
Fully 57% of subjects were found to carry the cav-1 gene variant. The other 43% were homozygous for what is known as the major allele. Carriers of the cav-1 gene variant were found to have significantly higher rates of type 2 diabetes, prediabetes, metabolic syndrome, and other abnormalities than those with the major allele (see chart). These differences were not explainable by differences in BMI; indeed, the average BMI in the two groups was nearly identical, according to Dr. Baudrand.
He and his coworkers also sought to learn whether study participants with metabolic syndrome would be more likely to have a sibling with metabolic syndrome if they were concordant for the cav-1 gene variant. This proved to be the case. In evaluating 348 subjects belonging to 142 sibships, the likelihood of concordance for metabolic syndrome was threefold greater if the siblings shared the cav-1 risk allele than if they were cav-1 discordant.
Upon closer scrutiny of the data, it became apparent that the seriously unfavorable cardiometabolic profile associated with the cav-1 gene variant was confined to the nonobese subjects. In a multivariate analysis adjusted for age, gender, BMI, and study site, the likelihood of metabolic syndrome among nonobese subjects with the variant allele was 3.86-fold higher than in nonobese individuals carrying the major allele. In addition, the adjusted likelihood of type 2 diabetes was 2.26-fold greater and that of low HDL was 1.78-fold greater, with all differences highly statistically significant. In contrast, the risk of these cardiometabolic problems in obese subjects didn’t vary regardless of the form of the cav-1 gene they possessed.
On the basis of these encouraging findings, the next step will be to conduct prospective studies to see if cav-1 genotyping is useful as a screening tool for cardiometabolic risk in nonobese patients. Further investigation is also warranted to identify the specific mechanisms by which the cav-1 risk allele results in cardiometabolic impairment. Among the leading possibilities are defects in aldosterone signaling, the insulin receptor, or adipocyte function, Dr. Baudrand said.
This study was supported by the National Institutes of Health and the Chilean National Science and Technology Research Fund. Dr. Baudrand reported having no financial conflicts.
AT ICE/ENDO 2014
Key clinical point: A genetic screening test shows promise as a means of identifying lean individuals at elevated risk for metabolic syndrome and type 2 diabetes.
Major finding: Nonobese individuals carrying a common variant of the caveolin-1 gene were at nearly fourfold increased risk for prevalent metabolic syndrome as well as 2.26-fold increased risk for type 2 diabetes, compared with those who were homozygous for the major allele.
Data source: This cross-sectional study entailed caveolin-1 genotyping of 735 subjects.
Disclosures: The study was supported by the National Institutes of Health and the Chilean National Science and Technology Research Fund. The presenter reported having no financial conflicts.
Hyponatremia linked to osteoporosis, fragility fractures
CHICAGO – Hyponatremia quadruples the risk of osteoporosis and fragility fractures, according to a retrospective database study presented at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
A team from Georgetown University in Washington matched 30,517 patients diagnosed with osteoporosis to 30,517 controls for age, race, sex, and how long they had been in the database of the MedStar Health System, which serves Baltimore and Washington.
The investigators found that patients with chronic hyponatremia – at least two sodium values below 135 mmol/L at least 1 year apart – were far more likely to be later diagnosed with osteoporosis (adjusted odds ratio, 3.99). Recent hyponatremia – at least one value below 135 mmol/L in the previous 30 days – also increased the risk (aOR, 3.08). In contrast, glucocorticoid use, a known osteoporosis risk factor, was associated with a far lower risk (aOR, 1.4), the team reported in a poster session at the meeting.
The researchers had similar results when they matched 46,256 patients with fragility fractures to 46,256 without: The fracture risk was substantially increased in patients with chronic hyponatremia (aOR, 4.71) and recent hyponatremia (aOR, 3.08). A previous diagnosis of osteoporosis – again, a known risk factor – increased the risk only moderately (aOR, 1.8).
The severity of hyponatremia played a role, too; patients with at least one value below 125 mmol/L had the highest risk for osteoporosis and fragility fractures.
The findings were all statistically significant.
"The results of this study support the hypothesis that hyponatremia is a significant and clinically important risk factor for both osteoporosis and bone fractures in inpatients and outpatients," the team concluded.
"We were surprised by the odds ratios and how strong a factor this was. Right now, hyponatremia is not an indication for bone mineral density [testing] because it’s never been considered to be a risk factor. It ought to be added as an indication. Patients with hyponatremia beyond an isolated single event should be evaluated for their bone density and fracture risk" no matter their age or sex, said senior investigator Dr. Joseph Verbalis, chief of the division on endocrinology and metabolism at Georgetown.
Based on the findings, "we [speculate] that early treatment of hyponatremia will prevent progression of bone disease and decrease fracture risk," and perhaps even obviate the need for bisphosphonates. "It’s an implication that needs to be followed up with definitive studies," he said.
Chronic hyponatremia increases osteoclast proliferation and activity, while recent hyponatremia reduces reaction time and makes it less likely people will catch themselves if they stumble. Elderly people are most at risk, either from overzealous salt restriction, sodium-depleting drugs like thiazide diuretics, or the syndrome of inappropriate antidiuretic hormone secretion (Indian J. Endocrinol. Metab. 2011;15(Suppl3):S208-S215).
The mean age of subjects in the osteoporosis analysis was about 75 years, and almost 90% were women. In the fragility fracture analysis, the mean age was about 60 years, and just over half the subjects were women.
Among the roughly 3 million patients the team initially sampled at the start of their work, there was a more than twofold increase in the prevalence of osteoporosis in hyponatremic (4.6%) vs. nonhyponatremic (1.8%) subjects, and a similar increase in vertebral or long-bone fractures (9.5% vs. 3.7%).
Dr. Verbalis is a consultant, investigator, speaker, and adviser for Otsuka, the maker of the hyponatremia drug tolvaptan. He is also a consultant for Cornerstone Therapeutics and Ferring Pharmaceuticals. The study had no outside funding.
CHICAGO – Hyponatremia quadruples the risk of osteoporosis and fragility fractures, according to a retrospective database study presented at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
A team from Georgetown University in Washington matched 30,517 patients diagnosed with osteoporosis to 30,517 controls for age, race, sex, and how long they had been in the database of the MedStar Health System, which serves Baltimore and Washington.
The investigators found that patients with chronic hyponatremia – at least two sodium values below 135 mmol/L at least 1 year apart – were far more likely to be later diagnosed with osteoporosis (adjusted odds ratio, 3.99). Recent hyponatremia – at least one value below 135 mmol/L in the previous 30 days – also increased the risk (aOR, 3.08). In contrast, glucocorticoid use, a known osteoporosis risk factor, was associated with a far lower risk (aOR, 1.4), the team reported in a poster session at the meeting.
The researchers had similar results when they matched 46,256 patients with fragility fractures to 46,256 without: The fracture risk was substantially increased in patients with chronic hyponatremia (aOR, 4.71) and recent hyponatremia (aOR, 3.08). A previous diagnosis of osteoporosis – again, a known risk factor – increased the risk only moderately (aOR, 1.8).
The severity of hyponatremia played a role, too; patients with at least one value below 125 mmol/L had the highest risk for osteoporosis and fragility fractures.
The findings were all statistically significant.
"The results of this study support the hypothesis that hyponatremia is a significant and clinically important risk factor for both osteoporosis and bone fractures in inpatients and outpatients," the team concluded.
"We were surprised by the odds ratios and how strong a factor this was. Right now, hyponatremia is not an indication for bone mineral density [testing] because it’s never been considered to be a risk factor. It ought to be added as an indication. Patients with hyponatremia beyond an isolated single event should be evaluated for their bone density and fracture risk" no matter their age or sex, said senior investigator Dr. Joseph Verbalis, chief of the division on endocrinology and metabolism at Georgetown.
Based on the findings, "we [speculate] that early treatment of hyponatremia will prevent progression of bone disease and decrease fracture risk," and perhaps even obviate the need for bisphosphonates. "It’s an implication that needs to be followed up with definitive studies," he said.
Chronic hyponatremia increases osteoclast proliferation and activity, while recent hyponatremia reduces reaction time and makes it less likely people will catch themselves if they stumble. Elderly people are most at risk, either from overzealous salt restriction, sodium-depleting drugs like thiazide diuretics, or the syndrome of inappropriate antidiuretic hormone secretion (Indian J. Endocrinol. Metab. 2011;15(Suppl3):S208-S215).
The mean age of subjects in the osteoporosis analysis was about 75 years, and almost 90% were women. In the fragility fracture analysis, the mean age was about 60 years, and just over half the subjects were women.
Among the roughly 3 million patients the team initially sampled at the start of their work, there was a more than twofold increase in the prevalence of osteoporosis in hyponatremic (4.6%) vs. nonhyponatremic (1.8%) subjects, and a similar increase in vertebral or long-bone fractures (9.5% vs. 3.7%).
Dr. Verbalis is a consultant, investigator, speaker, and adviser for Otsuka, the maker of the hyponatremia drug tolvaptan. He is also a consultant for Cornerstone Therapeutics and Ferring Pharmaceuticals. The study had no outside funding.
CHICAGO – Hyponatremia quadruples the risk of osteoporosis and fragility fractures, according to a retrospective database study presented at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
A team from Georgetown University in Washington matched 30,517 patients diagnosed with osteoporosis to 30,517 controls for age, race, sex, and how long they had been in the database of the MedStar Health System, which serves Baltimore and Washington.
The investigators found that patients with chronic hyponatremia – at least two sodium values below 135 mmol/L at least 1 year apart – were far more likely to be later diagnosed with osteoporosis (adjusted odds ratio, 3.99). Recent hyponatremia – at least one value below 135 mmol/L in the previous 30 days – also increased the risk (aOR, 3.08). In contrast, glucocorticoid use, a known osteoporosis risk factor, was associated with a far lower risk (aOR, 1.4), the team reported in a poster session at the meeting.
The researchers had similar results when they matched 46,256 patients with fragility fractures to 46,256 without: The fracture risk was substantially increased in patients with chronic hyponatremia (aOR, 4.71) and recent hyponatremia (aOR, 3.08). A previous diagnosis of osteoporosis – again, a known risk factor – increased the risk only moderately (aOR, 1.8).
The severity of hyponatremia played a role, too; patients with at least one value below 125 mmol/L had the highest risk for osteoporosis and fragility fractures.
The findings were all statistically significant.
"The results of this study support the hypothesis that hyponatremia is a significant and clinically important risk factor for both osteoporosis and bone fractures in inpatients and outpatients," the team concluded.
"We were surprised by the odds ratios and how strong a factor this was. Right now, hyponatremia is not an indication for bone mineral density [testing] because it’s never been considered to be a risk factor. It ought to be added as an indication. Patients with hyponatremia beyond an isolated single event should be evaluated for their bone density and fracture risk" no matter their age or sex, said senior investigator Dr. Joseph Verbalis, chief of the division on endocrinology and metabolism at Georgetown.
Based on the findings, "we [speculate] that early treatment of hyponatremia will prevent progression of bone disease and decrease fracture risk," and perhaps even obviate the need for bisphosphonates. "It’s an implication that needs to be followed up with definitive studies," he said.
Chronic hyponatremia increases osteoclast proliferation and activity, while recent hyponatremia reduces reaction time and makes it less likely people will catch themselves if they stumble. Elderly people are most at risk, either from overzealous salt restriction, sodium-depleting drugs like thiazide diuretics, or the syndrome of inappropriate antidiuretic hormone secretion (Indian J. Endocrinol. Metab. 2011;15(Suppl3):S208-S215).
The mean age of subjects in the osteoporosis analysis was about 75 years, and almost 90% were women. In the fragility fracture analysis, the mean age was about 60 years, and just over half the subjects were women.
Among the roughly 3 million patients the team initially sampled at the start of their work, there was a more than twofold increase in the prevalence of osteoporosis in hyponatremic (4.6%) vs. nonhyponatremic (1.8%) subjects, and a similar increase in vertebral or long-bone fractures (9.5% vs. 3.7%).
Dr. Verbalis is a consultant, investigator, speaker, and adviser for Otsuka, the maker of the hyponatremia drug tolvaptan. He is also a consultant for Cornerstone Therapeutics and Ferring Pharmaceuticals. The study had no outside funding.
AT ICE/ENDO 2014
Key clinical point: Early treatment of hyponatremia may one day prove to slow the progression of osteoporosis and reduce the need for bisphosphonates.
Major finding: In patients with chronic hyponatremia, the adjusted odds ratio for developing osteoporosis was 3.99, compared with those without.
Data Source: Retrospective case-control study involving more than 150,000 subjects.
Disclosures: Dr. Verbalis is a consultant, investigator, speaker, and adviser for Otsuka, the maker of the hyponatremia drug tolvaptan. The study had no outside funding.
Monitor elderly for bone loss after gastric bypass
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
AT ICE/ENDO 2014
Key clinical point: Gastric bypass puts some older patients at risk for osteoporosis.
Major finding: Two years after surgery, spine BMD in 30 patients was about 7% lower on quantitative CT and 6% lower on DXA when compared with 20 well-matched, morbidly obese controls.
Data Source: Retrospective case-control study with 2 years follow-up
Disclosures: The work was funded the National Institutes of Health. Dr. Yu is a consultant for Amgen.
Monitor elderly for bone loss after gastric bypass
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
CHICAGO – Older adults who undergo Roux-en-Y gastric bypass are at risk for lessened bone mineral density for at least 2 years after their surgery and should be monitored appropriately for osteoporosis or fragility fractures, according to investigators from Massachusetts General Hospital in Boston.
Two years postoperatively, vertebral bone mineral density (BMD) in 30 patients was about 7% lower on quantitative computed tomography (QCT) and 6% lower on dual-energy x-ray absorptiometry (DXA) – both methods were used to ensure accuracy – when compared with 20 well-matched, morbidly obese controls. Total hip BMD was 6% lower on QCT and 10% lower on DXA. Femoral neck BMD was about 6% lower by both measures.
Biomarkers of bone turnover remained markedly elevated in surgery patients, as well, but unchanged in controls (C-telopeptide 0.65 ng/mL vs. 0.3 ng/mL; amino-terminal propeptide of type I collagen 65 ng/mL vs. 40 ng/mL). The findings were all statistically significant.
The groups started to separate early on BMD, and there’s concern that bone loss will continue for more than 2 years after surgery. Preoperatively, most Roux-en-Y gastric bypass patients have a higher than normal BMD, "so even a loss of 10% over 2 years is not going to put most of them in the osteopenic or osteoporotic range. The caveat now is that we are [offering surgery] to older patients and adolescents. Elderly patients are starting with lower bone mass, so there are concerns about [post-op] skeletal fragility. The oldest patient in our study was 72. She became osteoporotic after surgery because her bone density was low to begin with," said lead investigator Dr. Elaine W. Yu, an endocrinologist at Massachusetts General.
"In adolescents, there are implications for achieving peak bone mass. Even if you have a normal bone density 2 years after surgery, what’s going to happen in 10 years, 20 years?" she asked.
In short, "people should pay attention to bone density and bone loss and discuss this as one of the potential negative effects of bariatric surgery. For patients at risk, you should definitely consider serial bone density monitoring and osteoporosis therapy if needed," she said at the joint meeting of the International Society of Endocrinology and the Endocrine Society.
At baseline, both subjects and controls were about 47 years old and 270 pounds, with a mean a mean body mass index of 45 kg/m2. About 85% were women. The study excluded patients with histories of bone disorders or use of bone-affecting medications.
Surgery patients lost a mean of about 85 pounds in the first 6 months; their weight loss then stabilized, but they continued to lose bone. Controls stayed about the same weight.
The findings can’t be explained by post-op calcium or vitamin D depletion. "These subjects were aggressively supplemented with both," and both groups maintained normal levels throughout the study. Also, there were no statistical differences in parathyroid hormone levels between the groups.
"Our theory is that there are changes in gut hormones after gastric bypass that have direct effects on bone, like ghrelin," Dr. Yu said.
The National Institutes of Health funded the work. Dr. Yu is a consultant for Amgen.
AT ICE/ENDO 2014
Key clinical point: Gastric bypass puts some older patients at risk for osteoporosis.
Major finding: Two years after surgery, spine BMD in 30 patients was about 7% lower on quantitative CT and 6% lower on DXA when compared with 20 well-matched, morbidly obese controls.
Data Source: Retrospective case-control study with 2 years follow-up
Disclosures: The work was funded the National Institutes of Health. Dr. Yu is a consultant for Amgen.
Effects of IV bisphosphonates last 2-3 years in children
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
AT ICE/ENDO 2014
Key clinical point: In children, osteocalcin is the first bone turnover marker that indicates it’s time to consider another round of IV bisphosphonate treatment.
Major finding: After initial improvement, serum osteocalcin begins to return to baseline about a year later (P = 0.007).
Data Source: Retrospective study of 104 children followed for up to 5 years.
Disclosures: The investigators have no disclosures, and received no outside funding for their work.
Effects of IV bisphosphonates last 2-3 years in children
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
CHICAGO – Serum osteocalcin is the first bone turnover marker to recover after intravenous bisphosphonate therapy in children with primary osteoporosis, secondary osteoporosis, or osteogenesis imperfecta, making it a good indicator that it’s time to consider a second round of treatment, according to investigators from Children’s Mercy Hospitals and Clinics in Kansas City, Mo.
In a review of 104 children followed for up to 5 years, they found that the benefits of IV bisphosphonates – for children, usually two or three 2-day courses about 4 months apart – remain durable for up to 3 years. After an initial decrease, serum osteocalcin starts to return to baseline 1 year after the start of treatment (P = 0.007); improvements in lumbar spine bone mineral density z scores on dual energy x-ray absorptiometry (DXA) start to plateau at about 2 years and then reverse after 3 years (P less than 0.0001). Decreases in urine N-telopeptide, a bone resorption marker, plateau at 2-3 years, then start to increase after 3 years (P less than 0.0001). Serum bone-specific alkaline phosphatase, a marker of bone formation like osteocalcin, continues to decrease for about 4.8-5 years (P less than 0.0001).
Although alkaline phosphatase, urine N-telopeptide, and lumbar z scores had begun to recover by the end of follow-up, they were still significantly improved over baseline. For instance, baseline lumbar z scores, more than two standard deviations below normal before treatment, were 1.31 standard deviations below normal at last follow up (P = 0.002).
However, after initial improvement, there was no statistically significant change in serum osteocalcin from baseline; the mean baseline value was 52.7 ng/mL, and mean value at last follow up was 54.5 ng/mL (P = 0.48).
"Osteocalcin is the first marker to increase within the first year after start of bisphosphonate therapy. The results of the study," perhaps the first to define the drug holiday window for bisphosphonates in children, "provide a framework [for] when to anticipate reinitiation of bisphosphonate therapy," the investigators concluded at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
"After 3 years, we should consider reinitiation of bisphosphonates in these children," said lead investigator Dr. Naziya Tahseen of the department of pediatric endocrinology at Children’s Mercy Hospitals and Clinics.
The subjects’ mean age was 11.6 years, 61 (58.7%) were girls, 67 (64.4%) were in puberty, and 75 (72.1%) were ambulatory; 59 (56.7%) children had primary or secondary osteoporosis, 26 (25%) had osteopenia, and 19 (18.3%) osteogenesis imperfecta. Lab values were followed every 4 months, with DXA scans repeated every 6-12 months.
Overall, children did better if they were ambulatory, but puberty status and gender had no effect.
The investigators had no relevant disclosures, and no outside funding was used for the project.
AT ICE/ENDO 2014
Key clinical point: In children, osteocalcin is the first bone turnover marker that indicates it’s time to consider another round of IV bisphosphonate treatment.
Major finding: After initial improvement, serum osteocalcin begins to return to baseline about a year later (P = 0.007).
Data Source: Retrospective study of 104 children followed for up to 5 years.
Disclosures: The investigators have no disclosures, and received no outside funding for their work.
VIDEO: Use late-night salivary cortisol to catch recurrent Cushing’s
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ICE/ENDO 2014