User login
American College of Gastroenterology (ACG): Annual Scientific Meeting
VIDEO: Expert outlines new thinking on irritable bowel syndrome
HONOLULU – New medications and more patient-focused strategies are changing the treatment of irritable bowel syndrome, as physicians move away from simply treating symptoms and gain a better understanding of IBS processes and mechanisms of action.
“I think there’s kind of an explosion in medications for functional bowel disease, specifically irritable bowel syndrome, over the last couple years, because we’ve gotten a lot smarter about how we think about these patients and how we treat these patients,” explained Dr. Darren M. Brenner, director of the functional bowel program at Northwestern University, Chicago.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Brenner discussed new approaches to target the syndrome’s mechanisms of action, new thinking by the Food and Drug Administration on IBS drug approval, and the wide range of traditional, complementary and alternative, and diet-related therapeutic options now available to patients.
HONOLULU – New medications and more patient-focused strategies are changing the treatment of irritable bowel syndrome, as physicians move away from simply treating symptoms and gain a better understanding of IBS processes and mechanisms of action.
“I think there’s kind of an explosion in medications for functional bowel disease, specifically irritable bowel syndrome, over the last couple years, because we’ve gotten a lot smarter about how we think about these patients and how we treat these patients,” explained Dr. Darren M. Brenner, director of the functional bowel program at Northwestern University, Chicago.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Brenner discussed new approaches to target the syndrome’s mechanisms of action, new thinking by the Food and Drug Administration on IBS drug approval, and the wide range of traditional, complementary and alternative, and diet-related therapeutic options now available to patients.
HONOLULU – New medications and more patient-focused strategies are changing the treatment of irritable bowel syndrome, as physicians move away from simply treating symptoms and gain a better understanding of IBS processes and mechanisms of action.
“I think there’s kind of an explosion in medications for functional bowel disease, specifically irritable bowel syndrome, over the last couple years, because we’ve gotten a lot smarter about how we think about these patients and how we treat these patients,” explained Dr. Darren M. Brenner, director of the functional bowel program at Northwestern University, Chicago.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Brenner discussed new approaches to target the syndrome’s mechanisms of action, new thinking by the Food and Drug Administration on IBS drug approval, and the wide range of traditional, complementary and alternative, and diet-related therapeutic options now available to patients.
AT ACG 2015
VIDEO: Serum amyloid A could be IBD biomarker
HONOLULU – Serum amyloid A levels may offer an effective biomarker to gauge disease activity in inflammatory bowel disease, while baseline fecal calprotectin levels could help predict how patients with IBD will respond to anti-tumor necrosis factor therapy, according to two studies presented at the annual meeting of the American College of Gastroenterology.
“There’s a really high need for biomarkers in order to have a better assessment and better control of disease activity, before treatment and then throughout therapy,” explained the studies’ lead author, Dr. Andres Yarur of the University of Chicago.
In an interview at the meeting, Dr. Yarur discussed the two studies’ results, and how serum amyloid A levels, in combination with C-reactive protein levels, may improve clinicians’ ability to identify active endoscopic disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Serum amyloid A levels may offer an effective biomarker to gauge disease activity in inflammatory bowel disease, while baseline fecal calprotectin levels could help predict how patients with IBD will respond to anti-tumor necrosis factor therapy, according to two studies presented at the annual meeting of the American College of Gastroenterology.
“There’s a really high need for biomarkers in order to have a better assessment and better control of disease activity, before treatment and then throughout therapy,” explained the studies’ lead author, Dr. Andres Yarur of the University of Chicago.
In an interview at the meeting, Dr. Yarur discussed the two studies’ results, and how serum amyloid A levels, in combination with C-reactive protein levels, may improve clinicians’ ability to identify active endoscopic disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Serum amyloid A levels may offer an effective biomarker to gauge disease activity in inflammatory bowel disease, while baseline fecal calprotectin levels could help predict how patients with IBD will respond to anti-tumor necrosis factor therapy, according to two studies presented at the annual meeting of the American College of Gastroenterology.
“There’s a really high need for biomarkers in order to have a better assessment and better control of disease activity, before treatment and then throughout therapy,” explained the studies’ lead author, Dr. Andres Yarur of the University of Chicago.
In an interview at the meeting, Dr. Yarur discussed the two studies’ results, and how serum amyloid A levels, in combination with C-reactive protein levels, may improve clinicians’ ability to identify active endoscopic disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACG 2015
Gut Microbiota May Predict C diff Treatment Response
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At ACG 2015
VIDEO: Gut microbiota may predict C. diff treatment response
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At ACG 2015
New targeted Crohn’s therapy performs well in phase III trial
HONOLULU – Ustekinumab, a monoclonal antibody targeted against interleukins 12 and 23 (IL-12 and IL-23), met its primary endpoint for control of Crohn’s disease in a multinational phase III trial presented at the annual meeting of the American College of Gastroenterology.
The trial, called UNITI-2, enrolled patients with moderate to severe Crohn’s disease who had failed traditional therapies but were naive to or at least had not failed a tumor necrosis factor (TNF) inhibitor, reported Dr. Brian Feagan, professor of medicine, University of Western Ontario, London. Results of a second and parallel phase III trial with ustekinumab, called UNITI-1, which enrolled TNF inhibitor failures, have not yet been reported.
In UNITI-2, 628 patients were randomized to placebo, 130 mg of ustekinumab in a fixed subcutaneous dose of 130 mg, or a weight-based dose of 6 mg/kg of subcutaneous ustekinumab. Major enrollment criteria, other than failure of a non-TNF inhibitor therapy, included a Crohn’s disease activity index (CDAI) score between 220 and 450. The primary endpoint was a CDAI reduction of at least 100 points at 6 weeks. Clinical remission at 8 weeks, defined as CDAI less than 150, was a secondary endpoint.
The primary endpoint was reached by 28.7% randomized to placebo, 51.7% of those randomized to the fixed dose of ustekinumab, and 55.5% of those randomized to weight-based dosing. The advantage for the active treatment arms was statistically significant (both P less than .001). For the secondary endpoint of clinical remission at 8 weeks, the rates were 19.6% for placebo, 30.6% (P = .009 vs. placebo) for fixed-dose ustekinumab, and 40.2% (P less than .001 vs. placebo) for the weight-based dose.
The anti-inflammatory effect of ustekinumab, which inhibits signal transduction of IL-12 and IL-23 by binding to the p40 subunit that both cytokines employ for receptor binding, was reflected in the rapid reduction in C-reactive protein (CRP) concentrations observed with both doses but not with placebo, according to Dr. Feagan. He noted that the greater CRP reduction on the weight-based dosing, which nearly doubles ustekinumab exposure for some individuals, supports the dose-response anti-inflammatory mechanism of the drug.
Ustekinumab was well tolerated with similar rates and types of adverse events reported in the active treatment and placebo groups. This included infections, serious infections, and infusion reactions. There was a theoretical concern about an increased risk for cardiovascular events that was not substantiated in this study. No malignancies were observed in this short-term study.
Nearly 70% of the patients were naive to a biologic treatment. Of the 31.4% with prior exposure to a TNF inhibitor, none had met criteria for failure. About 80% had failed corticosteroids after what was considered to be an adequate course, while nearly 70% had failed one or more immunomodulators. About half had failed both.
Details about quality of life measures were not presented at the ACG, but Dr. Feagan said, summarizing the data, they “also confirmed the clinical efficacy of ustekinumab,” which was approved for the treatment of psoriatic arthritis more than 2 years ago.
The data, which suggest a level of efficacy comparable to other targeted therapies in Crohn’s disease, appear to encourage a filing for Food and Drug Administration approval in Crohn’s disease. However, data about the relative efficacy of this drug in those who have failed a TNF inhibitor is expected to provide greater insight about how this agent will add to current options.
“It is encouraging to see disease control with agents targeting novel cytokines in the inflammatory pathway, but we need to begin thinking about how these biologics fit with each other,” said Dr. David Rubin, chief, section of gastroenterology, hepatology, and nutrition, University of Chicago. Dr. Rubin was a moderator of the ACG session in which the UNITI-2 data were presented.
Dr. Feagan has financial relationships with Millennium, Merck, Centocor, Elan/Biogen, Janssen-Ortho, Teva Pharmaceuticals, Bristol-Myers Squibb, Celgene, and many other pharmaceutical companies.
HONOLULU – Ustekinumab, a monoclonal antibody targeted against interleukins 12 and 23 (IL-12 and IL-23), met its primary endpoint for control of Crohn’s disease in a multinational phase III trial presented at the annual meeting of the American College of Gastroenterology.
The trial, called UNITI-2, enrolled patients with moderate to severe Crohn’s disease who had failed traditional therapies but were naive to or at least had not failed a tumor necrosis factor (TNF) inhibitor, reported Dr. Brian Feagan, professor of medicine, University of Western Ontario, London. Results of a second and parallel phase III trial with ustekinumab, called UNITI-1, which enrolled TNF inhibitor failures, have not yet been reported.
In UNITI-2, 628 patients were randomized to placebo, 130 mg of ustekinumab in a fixed subcutaneous dose of 130 mg, or a weight-based dose of 6 mg/kg of subcutaneous ustekinumab. Major enrollment criteria, other than failure of a non-TNF inhibitor therapy, included a Crohn’s disease activity index (CDAI) score between 220 and 450. The primary endpoint was a CDAI reduction of at least 100 points at 6 weeks. Clinical remission at 8 weeks, defined as CDAI less than 150, was a secondary endpoint.
The primary endpoint was reached by 28.7% randomized to placebo, 51.7% of those randomized to the fixed dose of ustekinumab, and 55.5% of those randomized to weight-based dosing. The advantage for the active treatment arms was statistically significant (both P less than .001). For the secondary endpoint of clinical remission at 8 weeks, the rates were 19.6% for placebo, 30.6% (P = .009 vs. placebo) for fixed-dose ustekinumab, and 40.2% (P less than .001 vs. placebo) for the weight-based dose.
The anti-inflammatory effect of ustekinumab, which inhibits signal transduction of IL-12 and IL-23 by binding to the p40 subunit that both cytokines employ for receptor binding, was reflected in the rapid reduction in C-reactive protein (CRP) concentrations observed with both doses but not with placebo, according to Dr. Feagan. He noted that the greater CRP reduction on the weight-based dosing, which nearly doubles ustekinumab exposure for some individuals, supports the dose-response anti-inflammatory mechanism of the drug.
Ustekinumab was well tolerated with similar rates and types of adverse events reported in the active treatment and placebo groups. This included infections, serious infections, and infusion reactions. There was a theoretical concern about an increased risk for cardiovascular events that was not substantiated in this study. No malignancies were observed in this short-term study.
Nearly 70% of the patients were naive to a biologic treatment. Of the 31.4% with prior exposure to a TNF inhibitor, none had met criteria for failure. About 80% had failed corticosteroids after what was considered to be an adequate course, while nearly 70% had failed one or more immunomodulators. About half had failed both.
Details about quality of life measures were not presented at the ACG, but Dr. Feagan said, summarizing the data, they “also confirmed the clinical efficacy of ustekinumab,” which was approved for the treatment of psoriatic arthritis more than 2 years ago.
The data, which suggest a level of efficacy comparable to other targeted therapies in Crohn’s disease, appear to encourage a filing for Food and Drug Administration approval in Crohn’s disease. However, data about the relative efficacy of this drug in those who have failed a TNF inhibitor is expected to provide greater insight about how this agent will add to current options.
“It is encouraging to see disease control with agents targeting novel cytokines in the inflammatory pathway, but we need to begin thinking about how these biologics fit with each other,” said Dr. David Rubin, chief, section of gastroenterology, hepatology, and nutrition, University of Chicago. Dr. Rubin was a moderator of the ACG session in which the UNITI-2 data were presented.
Dr. Feagan has financial relationships with Millennium, Merck, Centocor, Elan/Biogen, Janssen-Ortho, Teva Pharmaceuticals, Bristol-Myers Squibb, Celgene, and many other pharmaceutical companies.
HONOLULU – Ustekinumab, a monoclonal antibody targeted against interleukins 12 and 23 (IL-12 and IL-23), met its primary endpoint for control of Crohn’s disease in a multinational phase III trial presented at the annual meeting of the American College of Gastroenterology.
The trial, called UNITI-2, enrolled patients with moderate to severe Crohn’s disease who had failed traditional therapies but were naive to or at least had not failed a tumor necrosis factor (TNF) inhibitor, reported Dr. Brian Feagan, professor of medicine, University of Western Ontario, London. Results of a second and parallel phase III trial with ustekinumab, called UNITI-1, which enrolled TNF inhibitor failures, have not yet been reported.
In UNITI-2, 628 patients were randomized to placebo, 130 mg of ustekinumab in a fixed subcutaneous dose of 130 mg, or a weight-based dose of 6 mg/kg of subcutaneous ustekinumab. Major enrollment criteria, other than failure of a non-TNF inhibitor therapy, included a Crohn’s disease activity index (CDAI) score between 220 and 450. The primary endpoint was a CDAI reduction of at least 100 points at 6 weeks. Clinical remission at 8 weeks, defined as CDAI less than 150, was a secondary endpoint.
The primary endpoint was reached by 28.7% randomized to placebo, 51.7% of those randomized to the fixed dose of ustekinumab, and 55.5% of those randomized to weight-based dosing. The advantage for the active treatment arms was statistically significant (both P less than .001). For the secondary endpoint of clinical remission at 8 weeks, the rates were 19.6% for placebo, 30.6% (P = .009 vs. placebo) for fixed-dose ustekinumab, and 40.2% (P less than .001 vs. placebo) for the weight-based dose.
The anti-inflammatory effect of ustekinumab, which inhibits signal transduction of IL-12 and IL-23 by binding to the p40 subunit that both cytokines employ for receptor binding, was reflected in the rapid reduction in C-reactive protein (CRP) concentrations observed with both doses but not with placebo, according to Dr. Feagan. He noted that the greater CRP reduction on the weight-based dosing, which nearly doubles ustekinumab exposure for some individuals, supports the dose-response anti-inflammatory mechanism of the drug.
Ustekinumab was well tolerated with similar rates and types of adverse events reported in the active treatment and placebo groups. This included infections, serious infections, and infusion reactions. There was a theoretical concern about an increased risk for cardiovascular events that was not substantiated in this study. No malignancies were observed in this short-term study.
Nearly 70% of the patients were naive to a biologic treatment. Of the 31.4% with prior exposure to a TNF inhibitor, none had met criteria for failure. About 80% had failed corticosteroids after what was considered to be an adequate course, while nearly 70% had failed one or more immunomodulators. About half had failed both.
Details about quality of life measures were not presented at the ACG, but Dr. Feagan said, summarizing the data, they “also confirmed the clinical efficacy of ustekinumab,” which was approved for the treatment of psoriatic arthritis more than 2 years ago.
The data, which suggest a level of efficacy comparable to other targeted therapies in Crohn’s disease, appear to encourage a filing for Food and Drug Administration approval in Crohn’s disease. However, data about the relative efficacy of this drug in those who have failed a TNF inhibitor is expected to provide greater insight about how this agent will add to current options.
“It is encouraging to see disease control with agents targeting novel cytokines in the inflammatory pathway, but we need to begin thinking about how these biologics fit with each other,” said Dr. David Rubin, chief, section of gastroenterology, hepatology, and nutrition, University of Chicago. Dr. Rubin was a moderator of the ACG session in which the UNITI-2 data were presented.
Dr. Feagan has financial relationships with Millennium, Merck, Centocor, Elan/Biogen, Janssen-Ortho, Teva Pharmaceuticals, Bristol-Myers Squibb, Celgene, and many other pharmaceutical companies.
AT ACG 2015
Key clinical point: Ustekinumab, a novel monoclonal antibody for the treatment of Crohn’s disease, met its primary endpoint in a phase III trial.
Major finding: A reduction of 100 points or greater in the Crohn’s disease activity index (CDAI) was achieved by more than 50% patients on either dosing strategy of ustekinumab versus 28.7% of those in the placebo group (P less than .001).
Data source: Double-blind, placebo-controlled multicenter phase III trial.
Disclosures: The trial was sponsored by Janssen. Dr. Feagan has financial relationships with Millennium, Merck, Centocor, Elan/Biogen, Janssen-Ortho, Teva Pharmaceuticals, Bristol-Myers Squibb, and many others.
Early TIPS tied to mortality reduction in esophageal bleeds
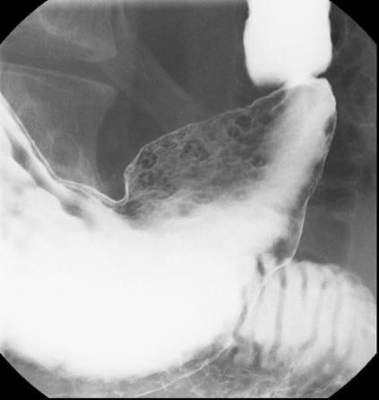
HONOLULU – Early use of a transjugular intrahepatic portosystemic shunt (TIPS) is associated with substantial reductions in mortality, according to an analysis of a national inpatient database.
Based on this study, “early use of TIPS, together with patient and physician education on current guidelines and protocols, should continue to be a priority to improve patient outcomes” in patients with hepatic cirrhosis and risk of recurrent esophageal variceal bleeds, reported Dr. Basile Njei, a gastroenterology fellow at Yale University, New Haven, Conn.
In this study, the Nationwide Inpatient Sample database was queried by ICD-9 codes to identify patients with esophageal variceal bleeding treated between the years 2000 and 2010. The goal was to compare early use of TIPS, defined as TIPS administered within 72 hours of the bleeding, relative to rescue TIPS, defined as TIPS after two or more episodes of bleeding or one bleeding episode followed by another endoscopic intervention, such as balloon tamponade or surgery.
Over the period of study, a Poisson regression analysis used to control for multiple variables associated any TIPS utilization with an inverse association with overall mortality, producing a relative risk of 0.88 (95% confidence interval, 0.83-0.92). In the context of timing of TIPS, in-hospital mortality fell from 5.6% for those who received rescue TIPS to 1.5% in those who underwent early TIPS.
On multivariate analysis, an advantage was observed for early TIPS relative to rescue TIPS for in-hospital mortality (RR, 0.85; P less than .01), in-hospital rebleeding (RR, 0.57; P less than .01), and length of hospital stay (RR, 0.87; P less than .01). Rates of sepsis (RR, 0.83; P = .32) and hepatic encephalopathy (RR, 0.87; P = .22) were not significantly lower in the early TIPS group, but they were also not increased. For early TIPS versus no TIPS, the advantages on multivariate analysis were similar for both in-hospital deaths (RR, 0.87; P less than .01) and in-hospital rebleeding (RR, 0.57; P less than .01), but no advantage was seen for length of stay for TIPS versus no TIPS (RR, 0.99; P = .18).
Overall, there was a steady decline in mortality associated with esophageal variceal bleeding over the period of evaluation, falling incrementally over time from 656 deaths per 100,000 hospitalizations in 2000 to 412 deaths per 100,000 in 2010. This 37.2% reduction was statistically significant (P less than .01). The reduction in mortality was inversely associated with an increasing use of TIPS over the study period.
The data from this analysis are consistent with a multicenter randomized trial conducted several years ago in Europe (N Engl J Med. 2010;362:2370-9). In that study 63 patients with hepatic cirrhosis and acute variceal bleeding who had been treated with vasoactive drugs plus endoscopic therapy were randomized to early TIPS or rescue TIPS. At 1 year, 86% of those in the early TIPS group were alive versus 61% (P = .01) of those randomized to receive TIPS as a rescue strategy.
Relative to the previous study, the key finding of this study is that early TIPS “is associated with significant short-term reductions in rebleeding and mortality without a significant increase in encephalopathy in real world U.S. clinical practice,” according to Dr. Njei. It substantiates the European study and encourages a protocol that emphasizes early TIPS, particularly in those with a high risk of repeat esophageal variceal bleeding.
In the discussion that followed the presentation of these results at the annual meeting of the American College of Gastroenterology, the moderator, Dr. Paul Y. Kwo, medical director of liver transplantation, Indiana University, Indianapolis, pointed out, that some of those in the rescue TIPS group might simply have been poor candidates for this intervention. Although he praised the methodology of this study, which won the 2015 ACG Fellows-In-Training Award, he questioned whether rescue TIPS was a last resort salvage therapy in those initially considered poor risks for TIPS. Dr. Njei responded that the multivariate analysis was specifically designed to control for variables such as risk status to diminish this potential bias. Indeed, he said he believes TIPS is underemployed.
“The relatively small percentage of eligible cases receiving early TIPS suggests that there is room for further improvement in the treatment of patients with decompensated cirrhosis and esophageal variceal bleeding,” Dr. Njei concluded.
Dr. Njei reported that he had no relevant financial relationships to disclose.
HONOLULU – Early use of a transjugular intrahepatic portosystemic shunt (TIPS) is associated with substantial reductions in mortality, according to an analysis of a national inpatient database.
Based on this study, “early use of TIPS, together with patient and physician education on current guidelines and protocols, should continue to be a priority to improve patient outcomes” in patients with hepatic cirrhosis and risk of recurrent esophageal variceal bleeds, reported Dr. Basile Njei, a gastroenterology fellow at Yale University, New Haven, Conn.
In this study, the Nationwide Inpatient Sample database was queried by ICD-9 codes to identify patients with esophageal variceal bleeding treated between the years 2000 and 2010. The goal was to compare early use of TIPS, defined as TIPS administered within 72 hours of the bleeding, relative to rescue TIPS, defined as TIPS after two or more episodes of bleeding or one bleeding episode followed by another endoscopic intervention, such as balloon tamponade or surgery.
Over the period of study, a Poisson regression analysis used to control for multiple variables associated any TIPS utilization with an inverse association with overall mortality, producing a relative risk of 0.88 (95% confidence interval, 0.83-0.92). In the context of timing of TIPS, in-hospital mortality fell from 5.6% for those who received rescue TIPS to 1.5% in those who underwent early TIPS.
On multivariate analysis, an advantage was observed for early TIPS relative to rescue TIPS for in-hospital mortality (RR, 0.85; P less than .01), in-hospital rebleeding (RR, 0.57; P less than .01), and length of hospital stay (RR, 0.87; P less than .01). Rates of sepsis (RR, 0.83; P = .32) and hepatic encephalopathy (RR, 0.87; P = .22) were not significantly lower in the early TIPS group, but they were also not increased. For early TIPS versus no TIPS, the advantages on multivariate analysis were similar for both in-hospital deaths (RR, 0.87; P less than .01) and in-hospital rebleeding (RR, 0.57; P less than .01), but no advantage was seen for length of stay for TIPS versus no TIPS (RR, 0.99; P = .18).
Overall, there was a steady decline in mortality associated with esophageal variceal bleeding over the period of evaluation, falling incrementally over time from 656 deaths per 100,000 hospitalizations in 2000 to 412 deaths per 100,000 in 2010. This 37.2% reduction was statistically significant (P less than .01). The reduction in mortality was inversely associated with an increasing use of TIPS over the study period.
The data from this analysis are consistent with a multicenter randomized trial conducted several years ago in Europe (N Engl J Med. 2010;362:2370-9). In that study 63 patients with hepatic cirrhosis and acute variceal bleeding who had been treated with vasoactive drugs plus endoscopic therapy were randomized to early TIPS or rescue TIPS. At 1 year, 86% of those in the early TIPS group were alive versus 61% (P = .01) of those randomized to receive TIPS as a rescue strategy.
Relative to the previous study, the key finding of this study is that early TIPS “is associated with significant short-term reductions in rebleeding and mortality without a significant increase in encephalopathy in real world U.S. clinical practice,” according to Dr. Njei. It substantiates the European study and encourages a protocol that emphasizes early TIPS, particularly in those with a high risk of repeat esophageal variceal bleeding.
In the discussion that followed the presentation of these results at the annual meeting of the American College of Gastroenterology, the moderator, Dr. Paul Y. Kwo, medical director of liver transplantation, Indiana University, Indianapolis, pointed out, that some of those in the rescue TIPS group might simply have been poor candidates for this intervention. Although he praised the methodology of this study, which won the 2015 ACG Fellows-In-Training Award, he questioned whether rescue TIPS was a last resort salvage therapy in those initially considered poor risks for TIPS. Dr. Njei responded that the multivariate analysis was specifically designed to control for variables such as risk status to diminish this potential bias. Indeed, he said he believes TIPS is underemployed.
“The relatively small percentage of eligible cases receiving early TIPS suggests that there is room for further improvement in the treatment of patients with decompensated cirrhosis and esophageal variceal bleeding,” Dr. Njei concluded.
Dr. Njei reported that he had no relevant financial relationships to disclose.
HONOLULU – Early use of a transjugular intrahepatic portosystemic shunt (TIPS) is associated with substantial reductions in mortality, according to an analysis of a national inpatient database.
Based on this study, “early use of TIPS, together with patient and physician education on current guidelines and protocols, should continue to be a priority to improve patient outcomes” in patients with hepatic cirrhosis and risk of recurrent esophageal variceal bleeds, reported Dr. Basile Njei, a gastroenterology fellow at Yale University, New Haven, Conn.
In this study, the Nationwide Inpatient Sample database was queried by ICD-9 codes to identify patients with esophageal variceal bleeding treated between the years 2000 and 2010. The goal was to compare early use of TIPS, defined as TIPS administered within 72 hours of the bleeding, relative to rescue TIPS, defined as TIPS after two or more episodes of bleeding or one bleeding episode followed by another endoscopic intervention, such as balloon tamponade or surgery.
Over the period of study, a Poisson regression analysis used to control for multiple variables associated any TIPS utilization with an inverse association with overall mortality, producing a relative risk of 0.88 (95% confidence interval, 0.83-0.92). In the context of timing of TIPS, in-hospital mortality fell from 5.6% for those who received rescue TIPS to 1.5% in those who underwent early TIPS.
On multivariate analysis, an advantage was observed for early TIPS relative to rescue TIPS for in-hospital mortality (RR, 0.85; P less than .01), in-hospital rebleeding (RR, 0.57; P less than .01), and length of hospital stay (RR, 0.87; P less than .01). Rates of sepsis (RR, 0.83; P = .32) and hepatic encephalopathy (RR, 0.87; P = .22) were not significantly lower in the early TIPS group, but they were also not increased. For early TIPS versus no TIPS, the advantages on multivariate analysis were similar for both in-hospital deaths (RR, 0.87; P less than .01) and in-hospital rebleeding (RR, 0.57; P less than .01), but no advantage was seen for length of stay for TIPS versus no TIPS (RR, 0.99; P = .18).
Overall, there was a steady decline in mortality associated with esophageal variceal bleeding over the period of evaluation, falling incrementally over time from 656 deaths per 100,000 hospitalizations in 2000 to 412 deaths per 100,000 in 2010. This 37.2% reduction was statistically significant (P less than .01). The reduction in mortality was inversely associated with an increasing use of TIPS over the study period.
The data from this analysis are consistent with a multicenter randomized trial conducted several years ago in Europe (N Engl J Med. 2010;362:2370-9). In that study 63 patients with hepatic cirrhosis and acute variceal bleeding who had been treated with vasoactive drugs plus endoscopic therapy were randomized to early TIPS or rescue TIPS. At 1 year, 86% of those in the early TIPS group were alive versus 61% (P = .01) of those randomized to receive TIPS as a rescue strategy.
Relative to the previous study, the key finding of this study is that early TIPS “is associated with significant short-term reductions in rebleeding and mortality without a significant increase in encephalopathy in real world U.S. clinical practice,” according to Dr. Njei. It substantiates the European study and encourages a protocol that emphasizes early TIPS, particularly in those with a high risk of repeat esophageal variceal bleeding.
In the discussion that followed the presentation of these results at the annual meeting of the American College of Gastroenterology, the moderator, Dr. Paul Y. Kwo, medical director of liver transplantation, Indiana University, Indianapolis, pointed out, that some of those in the rescue TIPS group might simply have been poor candidates for this intervention. Although he praised the methodology of this study, which won the 2015 ACG Fellows-In-Training Award, he questioned whether rescue TIPS was a last resort salvage therapy in those initially considered poor risks for TIPS. Dr. Njei responded that the multivariate analysis was specifically designed to control for variables such as risk status to diminish this potential bias. Indeed, he said he believes TIPS is underemployed.
“The relatively small percentage of eligible cases receiving early TIPS suggests that there is room for further improvement in the treatment of patients with decompensated cirrhosis and esophageal variceal bleeding,” Dr. Njei concluded.
Dr. Njei reported that he had no relevant financial relationships to disclose.
AT ACG 2015
Key clinical point:Early use of a transjugular intrahepatic portosystemic shunt to reduce the risk of esophageal variceal rebleeding is associated with reduced mortality.
Major finding: In those receiving early TIPS (TIPS administered within 72 hours of the bleeding) mortality was 1.5% vs. 5.6% for those receiving TIPS as rescue therapy.
Data source: A retrospective evaluation of a national inpatient database.
Disclosures: Dr. Njei reported that he had no relevant financial relationships to disclose.
Disparity found in PPI risk perception among physicians
HONOLULU – A survey of almost 500 physicians found that primary care physicians (PCPs) are far more concerned about the reported adverse effects of proton pump inhibitors (PPIs) than are gastroenterologists and use them more sparingly. The results of the survey were presented at the 2015 American College of Gastroenterology (ACG) Annual Scientific Meeting and Postgraduate Course.
“We asked physicians about a broad array of adverse effects from long-term use of PPIs and PCPs expressed greater concern for all of them,” reported Dr. Samir Kapadia, division of gastroenterology and hepatology, State University of New York at Stony Brook. “Alternatively, significantly more gastroenterologists responded that they really had no concerns for any of these adverse effects.”
The evidence may be on the side of the gastroenterologists, according to Dr. Kapadia. Although PPIs have been associated with hypomagnesemia, iron deficiency, vitamin B12 deficiency, diarrhea caused by Clostridium difficile infection, and interactions with the platelet inhibitor clopidogrel, Dr. Kapadia noted that few associations have been made on the basis of prospective trials.
“Much of the available literature is observational or based on studies that are heterogeneous and small,” Dr. Kapadia. “Confounding factors in these studies also limit interpretation.”
In this study for which surveys are still being collected, a 19-item questionnaire was distributed to 384 gastroenterologists and 88 PCPs. In addition to demographic information, the surveys were designed to capture opinions about the safety of PPIs as well as elicit information about how these agents are being used in clinical practice.
Of side effects associated with PPIs, significantly more PCPs than gastroenterologists expressed concern about hypomagnesemia (41.7% vs. 6.3%; P less than .001), iron deficiency (33.3% vs. 11.4%; P = .014) and vitamin B12 deficiency (47.6% vs. 17.3%; P = .005). From the other perspective, when asked about their concern for these and other safety issues, the answer was “none of the above” for 26.2% of PCPs and 67.1% of gastroenterologists (P less than .001).
When given specific risk scenarios, PCPs were consistently more prepared to discontinue PPI therapy than were gastroenterologists. For example, in a hypothetical 65-year-old with GERD symptoms expressing concern about risk of hip fracture, 64.5% of PCPs vs. 30.7% of gastroenterologists (P less than .001) responded that they would discontinue the PPI. In a patient of the same age about to start broad-spectrum antibiotics for cellulitis, 16.1% of PCPs, but only 4.3% of gastroenterologists (P = .001) reported that they would discontinue PPIs. Conversely, 68.5% of gastroenterologists vs. 54.2% of PCPs (P = .028) would continue therapy.
For a hypothetical 65-year-old with symptomatic gastroesophageal reflux disease (GERD) initiating clopidogrel, 50% of PCPs vs. 27.6% of gastroenterologists (P = .001) would switch to an H2-receptor antagonist. Only 27.3% of PCPs vs. 46.4% of gastroenterologists (P = .001) would continue the PPI. When the age of the hypothetical patient is raised to 75 years, PCPs, but not gastroenterologists, were even more likely to discontinue PPI therapy.
Using PPIs appropriately is an important goal, Dr. Kapadia emphasized. However, he suggested that many warnings about the risks of PPIs, including those issued by the Food and Drug Administration, are incompletely substantiated and are not being evaluated with an appropriate attention to benefit-to-risk ratio of a drug that not only controls symptoms but may also reduce risk of GI bleeding. Others share this point of view.
“The pendulum has moved too far in regard to the fear of potential side effects,” agreed Dr. Philip Katz, chairman, division of gastroenterology, Albert Einstein Medical Center, Philadelphia. First author of the 2013 ACG guidelines on GERD, which addresses the safety of PPIs (Am J Gastroenterol. 2013;108:308-28), Dr. Katz said in an interview that the data generated by this survey suggest that PCPs are misinterpreting the relative risks and need to be given more information about indications in which benefits are well established.
Making the same point, Dr. Nicholas J. Shaheen, chief, division of gastroenterology and hepatology, University of North Carolina, Chapel Hill, suggested “This may be a failure on our part [as gastroenterologists] to educate our colleagues about the role of these drugs.”
Dr. Kapadia reported no potential conflicts.
HONOLULU – A survey of almost 500 physicians found that primary care physicians (PCPs) are far more concerned about the reported adverse effects of proton pump inhibitors (PPIs) than are gastroenterologists and use them more sparingly. The results of the survey were presented at the 2015 American College of Gastroenterology (ACG) Annual Scientific Meeting and Postgraduate Course.
“We asked physicians about a broad array of adverse effects from long-term use of PPIs and PCPs expressed greater concern for all of them,” reported Dr. Samir Kapadia, division of gastroenterology and hepatology, State University of New York at Stony Brook. “Alternatively, significantly more gastroenterologists responded that they really had no concerns for any of these adverse effects.”
The evidence may be on the side of the gastroenterologists, according to Dr. Kapadia. Although PPIs have been associated with hypomagnesemia, iron deficiency, vitamin B12 deficiency, diarrhea caused by Clostridium difficile infection, and interactions with the platelet inhibitor clopidogrel, Dr. Kapadia noted that few associations have been made on the basis of prospective trials.
“Much of the available literature is observational or based on studies that are heterogeneous and small,” Dr. Kapadia. “Confounding factors in these studies also limit interpretation.”
In this study for which surveys are still being collected, a 19-item questionnaire was distributed to 384 gastroenterologists and 88 PCPs. In addition to demographic information, the surveys were designed to capture opinions about the safety of PPIs as well as elicit information about how these agents are being used in clinical practice.
Of side effects associated with PPIs, significantly more PCPs than gastroenterologists expressed concern about hypomagnesemia (41.7% vs. 6.3%; P less than .001), iron deficiency (33.3% vs. 11.4%; P = .014) and vitamin B12 deficiency (47.6% vs. 17.3%; P = .005). From the other perspective, when asked about their concern for these and other safety issues, the answer was “none of the above” for 26.2% of PCPs and 67.1% of gastroenterologists (P less than .001).
When given specific risk scenarios, PCPs were consistently more prepared to discontinue PPI therapy than were gastroenterologists. For example, in a hypothetical 65-year-old with GERD symptoms expressing concern about risk of hip fracture, 64.5% of PCPs vs. 30.7% of gastroenterologists (P less than .001) responded that they would discontinue the PPI. In a patient of the same age about to start broad-spectrum antibiotics for cellulitis, 16.1% of PCPs, but only 4.3% of gastroenterologists (P = .001) reported that they would discontinue PPIs. Conversely, 68.5% of gastroenterologists vs. 54.2% of PCPs (P = .028) would continue therapy.
For a hypothetical 65-year-old with symptomatic gastroesophageal reflux disease (GERD) initiating clopidogrel, 50% of PCPs vs. 27.6% of gastroenterologists (P = .001) would switch to an H2-receptor antagonist. Only 27.3% of PCPs vs. 46.4% of gastroenterologists (P = .001) would continue the PPI. When the age of the hypothetical patient is raised to 75 years, PCPs, but not gastroenterologists, were even more likely to discontinue PPI therapy.
Using PPIs appropriately is an important goal, Dr. Kapadia emphasized. However, he suggested that many warnings about the risks of PPIs, including those issued by the Food and Drug Administration, are incompletely substantiated and are not being evaluated with an appropriate attention to benefit-to-risk ratio of a drug that not only controls symptoms but may also reduce risk of GI bleeding. Others share this point of view.
“The pendulum has moved too far in regard to the fear of potential side effects,” agreed Dr. Philip Katz, chairman, division of gastroenterology, Albert Einstein Medical Center, Philadelphia. First author of the 2013 ACG guidelines on GERD, which addresses the safety of PPIs (Am J Gastroenterol. 2013;108:308-28), Dr. Katz said in an interview that the data generated by this survey suggest that PCPs are misinterpreting the relative risks and need to be given more information about indications in which benefits are well established.
Making the same point, Dr. Nicholas J. Shaheen, chief, division of gastroenterology and hepatology, University of North Carolina, Chapel Hill, suggested “This may be a failure on our part [as gastroenterologists] to educate our colleagues about the role of these drugs.”
Dr. Kapadia reported no potential conflicts.
HONOLULU – A survey of almost 500 physicians found that primary care physicians (PCPs) are far more concerned about the reported adverse effects of proton pump inhibitors (PPIs) than are gastroenterologists and use them more sparingly. The results of the survey were presented at the 2015 American College of Gastroenterology (ACG) Annual Scientific Meeting and Postgraduate Course.
“We asked physicians about a broad array of adverse effects from long-term use of PPIs and PCPs expressed greater concern for all of them,” reported Dr. Samir Kapadia, division of gastroenterology and hepatology, State University of New York at Stony Brook. “Alternatively, significantly more gastroenterologists responded that they really had no concerns for any of these adverse effects.”
The evidence may be on the side of the gastroenterologists, according to Dr. Kapadia. Although PPIs have been associated with hypomagnesemia, iron deficiency, vitamin B12 deficiency, diarrhea caused by Clostridium difficile infection, and interactions with the platelet inhibitor clopidogrel, Dr. Kapadia noted that few associations have been made on the basis of prospective trials.
“Much of the available literature is observational or based on studies that are heterogeneous and small,” Dr. Kapadia. “Confounding factors in these studies also limit interpretation.”
In this study for which surveys are still being collected, a 19-item questionnaire was distributed to 384 gastroenterologists and 88 PCPs. In addition to demographic information, the surveys were designed to capture opinions about the safety of PPIs as well as elicit information about how these agents are being used in clinical practice.
Of side effects associated with PPIs, significantly more PCPs than gastroenterologists expressed concern about hypomagnesemia (41.7% vs. 6.3%; P less than .001), iron deficiency (33.3% vs. 11.4%; P = .014) and vitamin B12 deficiency (47.6% vs. 17.3%; P = .005). From the other perspective, when asked about their concern for these and other safety issues, the answer was “none of the above” for 26.2% of PCPs and 67.1% of gastroenterologists (P less than .001).
When given specific risk scenarios, PCPs were consistently more prepared to discontinue PPI therapy than were gastroenterologists. For example, in a hypothetical 65-year-old with GERD symptoms expressing concern about risk of hip fracture, 64.5% of PCPs vs. 30.7% of gastroenterologists (P less than .001) responded that they would discontinue the PPI. In a patient of the same age about to start broad-spectrum antibiotics for cellulitis, 16.1% of PCPs, but only 4.3% of gastroenterologists (P = .001) reported that they would discontinue PPIs. Conversely, 68.5% of gastroenterologists vs. 54.2% of PCPs (P = .028) would continue therapy.
For a hypothetical 65-year-old with symptomatic gastroesophageal reflux disease (GERD) initiating clopidogrel, 50% of PCPs vs. 27.6% of gastroenterologists (P = .001) would switch to an H2-receptor antagonist. Only 27.3% of PCPs vs. 46.4% of gastroenterologists (P = .001) would continue the PPI. When the age of the hypothetical patient is raised to 75 years, PCPs, but not gastroenterologists, were even more likely to discontinue PPI therapy.
Using PPIs appropriately is an important goal, Dr. Kapadia emphasized. However, he suggested that many warnings about the risks of PPIs, including those issued by the Food and Drug Administration, are incompletely substantiated and are not being evaluated with an appropriate attention to benefit-to-risk ratio of a drug that not only controls symptoms but may also reduce risk of GI bleeding. Others share this point of view.
“The pendulum has moved too far in regard to the fear of potential side effects,” agreed Dr. Philip Katz, chairman, division of gastroenterology, Albert Einstein Medical Center, Philadelphia. First author of the 2013 ACG guidelines on GERD, which addresses the safety of PPIs (Am J Gastroenterol. 2013;108:308-28), Dr. Katz said in an interview that the data generated by this survey suggest that PCPs are misinterpreting the relative risks and need to be given more information about indications in which benefits are well established.
Making the same point, Dr. Nicholas J. Shaheen, chief, division of gastroenterology and hepatology, University of North Carolina, Chapel Hill, suggested “This may be a failure on our part [as gastroenterologists] to educate our colleagues about the role of these drugs.”
Dr. Kapadia reported no potential conflicts.
FROM THE AMERICAN COLLEGE OF GASTROENTEROLOGY 2015 SCIENTIFIC MEETING AND POSTGRADUATE COURSE
Key clinical point: Primary care physicians used proton pump inhibitors more sparingly, were more concerned about reported adverse effects than were gastroenterologists, but are perhaps too cautious in the cost-benefit analysis.
Major finding: Primary care physicians (PCPs) are far more concerned about the reported adverse effects of proton pump inhibitors than are gastroenterologists.
Data source: A survey of nearly 500 physicians, weighted toward gastroenterologists.
Disclosures: Dr. Kapadia reported no potential conflicts of interest.
DNA-based pancreatic cyst test guides treatment
HONOLULU – A DNA-based molecular diagnostic test that stratifies pancreatic cysts for their malignant potential better than current alternatives can help guide management, according to two sets of corroborating data presented at the annual meeting of the American College of Gastroenterology.
The test was associated with a high degree of accuracy for identifying those pancreatic cysts with a high as well as those with a low potential for malignant transformation, according to Dr. David E. Loren, codirector, pancreaticobiliary section, Thomas Jefferson University, Philadelphia.
“This test can be recommended across the board to patients with a pancreatic cyst. The exception would be those with a positive cytology for malignancy in which no further diagnostic study is needed,” said Dr. Loren.
The proprietary test, marketed under the name PancraGEN (Interpace Diagnostics), uses genetic and molecular information, such as oncogene mutations and loss of heterozygosity (LOH) markers, to stratify pancreatic cysts as high risk on the basis of malignant transformation potential or low risk on the basis of characteristics predicting a benign course. It is commercially available and has been used in more than 14,000 patients worldwide, according to Dr. Loren.
In the first of two studies presented at ACG 2015, the performance of the diagnostic test was compared to AGA criteria for managing pancreatic cysts, which were published earlier this year (Gastroenterology 2015;148:819-22). Using registry data with known outcomes, researchers compared the performance of the AGA criteria and the PancraGEN test in 417 patients.
The AGA criteria, which require assessment of cytological atypia and endoscopic ultrasound imaging features, were falsely negative in 57% of cases and falsely positive in 4%, producing a positive predictive value of 59% and a negative predictive value of 93%. Of the 27 malignancies missed by the AGA criteria, the PancraGEN test identified 21. As a result, it generated far greater sensitivity (87% vs. 43%; P less than .0001) even though the specificity of the PancraGEN test and the AGA criteria were similar (92% vs. 96%, respectively).
“The DNA-based approach helped identify false-negative cases otherwise missed by AGA-recommended imaging and cytology,” Dr. Loren confirmed.
In a second study using the same registry data, the goal was to determine whether the DNA-based diagnostic test would provide more accurate management decisions. In this study, the DNA-based diagnostic test was compared to the International Consensus Guidelines (ICG), which were most recently updated in 2012 (Pancreatology 2012;12:183-197). The study evaluated outcomes in the context of recommendations by the ICG as well as the risk status established with the PancraGEN test.
In cysts recommended for surveillance by ICG but identified as high-risk by PancraGEN testing, 57% had malignant outcomes. In cysts recommended for Surgery by ICG guidelines but identified as low-risk by PancraGEN test, 99% had a benign outcome.
Whether compared to AGA or ICG criteria, the DNA-based test is more accurate for detecting malignant potential “without drastically overdiagnosing malignancy in patients with benign lesions,” said Dr. Loren, who said the second study confirmed its utility “in real-life management decisions.”
Cost efficacy data were not presented at the ACG meeting, but Dr. Loren said that models predict cost savings from PancraGEN testing because of more appropriate care, particularly a reduction in unnecessary surgeries. Although it is also theoretically possible that a reduction in false-negative diagnoses could lead to a mortality benefit through earlier treatment of lesions with a high likelihood of malignant transformation, Dr. Loren cautioned that this advantage would be difficult to show without extended follow-up because of the slow growth of many tumors.
It is estimated that about 120,000 pancreatic cysts are identified annually. On cytology, results are often ambiguous, complicating the decision to incur the risks and costs of surgery relative to a watch-and-wait approach. A more precise test has the potential both to avoid unnecessary surgeries and to ensure that those at high risk are treated appropriately. Overall, Dr. Loren said he believes that the PancraGEN test will improve care in this population.
“We think this is a better approach relative to current alternatives,” he asserted.
Dr. Loren received research support from Interpace Diagnostics
HONOLULU – A DNA-based molecular diagnostic test that stratifies pancreatic cysts for their malignant potential better than current alternatives can help guide management, according to two sets of corroborating data presented at the annual meeting of the American College of Gastroenterology.
The test was associated with a high degree of accuracy for identifying those pancreatic cysts with a high as well as those with a low potential for malignant transformation, according to Dr. David E. Loren, codirector, pancreaticobiliary section, Thomas Jefferson University, Philadelphia.
“This test can be recommended across the board to patients with a pancreatic cyst. The exception would be those with a positive cytology for malignancy in which no further diagnostic study is needed,” said Dr. Loren.
The proprietary test, marketed under the name PancraGEN (Interpace Diagnostics), uses genetic and molecular information, such as oncogene mutations and loss of heterozygosity (LOH) markers, to stratify pancreatic cysts as high risk on the basis of malignant transformation potential or low risk on the basis of characteristics predicting a benign course. It is commercially available and has been used in more than 14,000 patients worldwide, according to Dr. Loren.
In the first of two studies presented at ACG 2015, the performance of the diagnostic test was compared to AGA criteria for managing pancreatic cysts, which were published earlier this year (Gastroenterology 2015;148:819-22). Using registry data with known outcomes, researchers compared the performance of the AGA criteria and the PancraGEN test in 417 patients.
The AGA criteria, which require assessment of cytological atypia and endoscopic ultrasound imaging features, were falsely negative in 57% of cases and falsely positive in 4%, producing a positive predictive value of 59% and a negative predictive value of 93%. Of the 27 malignancies missed by the AGA criteria, the PancraGEN test identified 21. As a result, it generated far greater sensitivity (87% vs. 43%; P less than .0001) even though the specificity of the PancraGEN test and the AGA criteria were similar (92% vs. 96%, respectively).
“The DNA-based approach helped identify false-negative cases otherwise missed by AGA-recommended imaging and cytology,” Dr. Loren confirmed.
In a second study using the same registry data, the goal was to determine whether the DNA-based diagnostic test would provide more accurate management decisions. In this study, the DNA-based diagnostic test was compared to the International Consensus Guidelines (ICG), which were most recently updated in 2012 (Pancreatology 2012;12:183-197). The study evaluated outcomes in the context of recommendations by the ICG as well as the risk status established with the PancraGEN test.
In cysts recommended for surveillance by ICG but identified as high-risk by PancraGEN testing, 57% had malignant outcomes. In cysts recommended for Surgery by ICG guidelines but identified as low-risk by PancraGEN test, 99% had a benign outcome.
Whether compared to AGA or ICG criteria, the DNA-based test is more accurate for detecting malignant potential “without drastically overdiagnosing malignancy in patients with benign lesions,” said Dr. Loren, who said the second study confirmed its utility “in real-life management decisions.”
Cost efficacy data were not presented at the ACG meeting, but Dr. Loren said that models predict cost savings from PancraGEN testing because of more appropriate care, particularly a reduction in unnecessary surgeries. Although it is also theoretically possible that a reduction in false-negative diagnoses could lead to a mortality benefit through earlier treatment of lesions with a high likelihood of malignant transformation, Dr. Loren cautioned that this advantage would be difficult to show without extended follow-up because of the slow growth of many tumors.
It is estimated that about 120,000 pancreatic cysts are identified annually. On cytology, results are often ambiguous, complicating the decision to incur the risks and costs of surgery relative to a watch-and-wait approach. A more precise test has the potential both to avoid unnecessary surgeries and to ensure that those at high risk are treated appropriately. Overall, Dr. Loren said he believes that the PancraGEN test will improve care in this population.
“We think this is a better approach relative to current alternatives,” he asserted.
Dr. Loren received research support from Interpace Diagnostics
HONOLULU – A DNA-based molecular diagnostic test that stratifies pancreatic cysts for their malignant potential better than current alternatives can help guide management, according to two sets of corroborating data presented at the annual meeting of the American College of Gastroenterology.
The test was associated with a high degree of accuracy for identifying those pancreatic cysts with a high as well as those with a low potential for malignant transformation, according to Dr. David E. Loren, codirector, pancreaticobiliary section, Thomas Jefferson University, Philadelphia.
“This test can be recommended across the board to patients with a pancreatic cyst. The exception would be those with a positive cytology for malignancy in which no further diagnostic study is needed,” said Dr. Loren.
The proprietary test, marketed under the name PancraGEN (Interpace Diagnostics), uses genetic and molecular information, such as oncogene mutations and loss of heterozygosity (LOH) markers, to stratify pancreatic cysts as high risk on the basis of malignant transformation potential or low risk on the basis of characteristics predicting a benign course. It is commercially available and has been used in more than 14,000 patients worldwide, according to Dr. Loren.
In the first of two studies presented at ACG 2015, the performance of the diagnostic test was compared to AGA criteria for managing pancreatic cysts, which were published earlier this year (Gastroenterology 2015;148:819-22). Using registry data with known outcomes, researchers compared the performance of the AGA criteria and the PancraGEN test in 417 patients.
The AGA criteria, which require assessment of cytological atypia and endoscopic ultrasound imaging features, were falsely negative in 57% of cases and falsely positive in 4%, producing a positive predictive value of 59% and a negative predictive value of 93%. Of the 27 malignancies missed by the AGA criteria, the PancraGEN test identified 21. As a result, it generated far greater sensitivity (87% vs. 43%; P less than .0001) even though the specificity of the PancraGEN test and the AGA criteria were similar (92% vs. 96%, respectively).
“The DNA-based approach helped identify false-negative cases otherwise missed by AGA-recommended imaging and cytology,” Dr. Loren confirmed.
In a second study using the same registry data, the goal was to determine whether the DNA-based diagnostic test would provide more accurate management decisions. In this study, the DNA-based diagnostic test was compared to the International Consensus Guidelines (ICG), which were most recently updated in 2012 (Pancreatology 2012;12:183-197). The study evaluated outcomes in the context of recommendations by the ICG as well as the risk status established with the PancraGEN test.
In cysts recommended for surveillance by ICG but identified as high-risk by PancraGEN testing, 57% had malignant outcomes. In cysts recommended for Surgery by ICG guidelines but identified as low-risk by PancraGEN test, 99% had a benign outcome.
Whether compared to AGA or ICG criteria, the DNA-based test is more accurate for detecting malignant potential “without drastically overdiagnosing malignancy in patients with benign lesions,” said Dr. Loren, who said the second study confirmed its utility “in real-life management decisions.”
Cost efficacy data were not presented at the ACG meeting, but Dr. Loren said that models predict cost savings from PancraGEN testing because of more appropriate care, particularly a reduction in unnecessary surgeries. Although it is also theoretically possible that a reduction in false-negative diagnoses could lead to a mortality benefit through earlier treatment of lesions with a high likelihood of malignant transformation, Dr. Loren cautioned that this advantage would be difficult to show without extended follow-up because of the slow growth of many tumors.
It is estimated that about 120,000 pancreatic cysts are identified annually. On cytology, results are often ambiguous, complicating the decision to incur the risks and costs of surgery relative to a watch-and-wait approach. A more precise test has the potential both to avoid unnecessary surgeries and to ensure that those at high risk are treated appropriately. Overall, Dr. Loren said he believes that the PancraGEN test will improve care in this population.
“We think this is a better approach relative to current alternatives,” he asserted.
Dr. Loren received research support from Interpace Diagnostics
EXPERT ANALYSIS FROM ACG 2015
Risk score assesses likelihood of fecal transplant failure
HONOLULU – Fecal transplant was shown to be effective in the treatment of recurrent or refractory episodes of Clostridium difficile infection in a double-blind trial for the first time, and a second study isolated predictors of treatment failure.
The results of the double-blind study were expected. Several studies, although none double blind, have previously shown this therapy to be efficacious. The study of predictors of failure may be of more immediate practical application, because it is relevant to patient selection, according to the investigators, some of whom were involved in both studies.
In the double-blind study, 46 patients were randomized at two centers to receive a fecal microbiota transplant from donor stool or to a placebo, which was a transplant of the patient’s own stool.
The primary outcome was clinical cure at the end of 8 weeks, achieved in 91% of those randomized to the active therapy and 63% of those randomized to placebo (P = .024). Most of those who had treatment failure, which occurred on average 10 days after the procedure (range, 1-62 days), received the active therapy subsequently and also achieved clinical cure after donor transplantation.
“There were no significant differences in any adverse event rates between the donor transplant and placebo groups,” Dr. Colleen Kelly reported at the annual meeting of the American College of Gastroenterology. Dr. Kelly, a gastroenterologist with the Miriam Hospital, Brown University, Providence, R.I., was also a coauthor of the study of risk factors for the failure of fecal transplant.
Underlining the importance of a double-blind trial to provide confirmation of the efficacy of fecal transplant, Dr. Christina M. Surawicz, who moderated the ACG session at which both studies were presented, said, “We have been waiting for these results.”
However, a disparity in results at the two participating centers is notable. In Providence, cure was achieved in 90% of those receiving fecal transplant versus 43% receiving placebo (P = .019). At the other participating institution, Montefiore Medical Center, New York, the cure rate was 92% with fecal transplant, but 90% of the placebo patients were also cured (P = .89). The data were not intended for a separate analysis, so Dr. Kelly said this did not affect her final conclusion that this trial confirmed the efficacy of this treatment.
In the separate study evaluating predictors of failure to achieve cure after fecal transplant, the retrospective analysis was performed with 345 patients treated for C. difficile infection with fecal transplant. In this population, the overall failure rate was 23.7%, but there was a wide variability observed upon univariate and multivariate analysis of risk factors, Dr. Monika Fischer, a gastroenterologist at Indiana University Hospital, Indianapolis, said at the meeting.
For example, in patients with nonsevere recurrent C. difficile infection, the failure rate was 18%. In contrast, the failure rate was approximately 50% among those with severe refractory C. difficile infection.
Upon multivariate analysis, three risk factors were independent predictors of fecal transplant failure: inpatient status, which was associated with an odds ratio of 6.92 (P = .001); being immunosuppressed (OR, 3.28; P = .0004); and previous hospitalization for C. difficile infection (OR, 1.45 for each prior hospitalization; P less than .001).
With the use of these three factors, a risk score was found to be highly predictive of failure. In this risk score, 5 points were attributed to inpatient status, 3 points to immunosuppression, and 1 point to each prior hospitalization for C. difficile infection. On a scale of 0-12 points, the risk of failure was 13% in those with 0 points, 17% in those with 1-3 points, and 44% in those with 4 or more points.
“Our data suggest that the risk of fecal transplant failure is predictable based on pretransplant characteristics. We hope that this risk stratification model will prove helpful,” said Dr. Fischer, whose coauthors included Dr. Kelly.
Although she did not directly endorse this risk stratification tool for patient management, Dr. Surawicz called this presentation “very clinically relevant.” Practical tools are needed to guide the use of this therapy as it becomes more widely used in the treatment of C. difficile, said Dr. Surawicz, professor of gastroenterology, University of Washington, Seattle.
Dr. Kelly reported no relevant financial conflicts. Dr. Fischer reported a financial relationship with Rebiotix.
HONOLULU – Fecal transplant was shown to be effective in the treatment of recurrent or refractory episodes of Clostridium difficile infection in a double-blind trial for the first time, and a second study isolated predictors of treatment failure.
The results of the double-blind study were expected. Several studies, although none double blind, have previously shown this therapy to be efficacious. The study of predictors of failure may be of more immediate practical application, because it is relevant to patient selection, according to the investigators, some of whom were involved in both studies.
In the double-blind study, 46 patients were randomized at two centers to receive a fecal microbiota transplant from donor stool or to a placebo, which was a transplant of the patient’s own stool.
The primary outcome was clinical cure at the end of 8 weeks, achieved in 91% of those randomized to the active therapy and 63% of those randomized to placebo (P = .024). Most of those who had treatment failure, which occurred on average 10 days after the procedure (range, 1-62 days), received the active therapy subsequently and also achieved clinical cure after donor transplantation.
“There were no significant differences in any adverse event rates between the donor transplant and placebo groups,” Dr. Colleen Kelly reported at the annual meeting of the American College of Gastroenterology. Dr. Kelly, a gastroenterologist with the Miriam Hospital, Brown University, Providence, R.I., was also a coauthor of the study of risk factors for the failure of fecal transplant.
Underlining the importance of a double-blind trial to provide confirmation of the efficacy of fecal transplant, Dr. Christina M. Surawicz, who moderated the ACG session at which both studies were presented, said, “We have been waiting for these results.”
However, a disparity in results at the two participating centers is notable. In Providence, cure was achieved in 90% of those receiving fecal transplant versus 43% receiving placebo (P = .019). At the other participating institution, Montefiore Medical Center, New York, the cure rate was 92% with fecal transplant, but 90% of the placebo patients were also cured (P = .89). The data were not intended for a separate analysis, so Dr. Kelly said this did not affect her final conclusion that this trial confirmed the efficacy of this treatment.
In the separate study evaluating predictors of failure to achieve cure after fecal transplant, the retrospective analysis was performed with 345 patients treated for C. difficile infection with fecal transplant. In this population, the overall failure rate was 23.7%, but there was a wide variability observed upon univariate and multivariate analysis of risk factors, Dr. Monika Fischer, a gastroenterologist at Indiana University Hospital, Indianapolis, said at the meeting.
For example, in patients with nonsevere recurrent C. difficile infection, the failure rate was 18%. In contrast, the failure rate was approximately 50% among those with severe refractory C. difficile infection.
Upon multivariate analysis, three risk factors were independent predictors of fecal transplant failure: inpatient status, which was associated with an odds ratio of 6.92 (P = .001); being immunosuppressed (OR, 3.28; P = .0004); and previous hospitalization for C. difficile infection (OR, 1.45 for each prior hospitalization; P less than .001).
With the use of these three factors, a risk score was found to be highly predictive of failure. In this risk score, 5 points were attributed to inpatient status, 3 points to immunosuppression, and 1 point to each prior hospitalization for C. difficile infection. On a scale of 0-12 points, the risk of failure was 13% in those with 0 points, 17% in those with 1-3 points, and 44% in those with 4 or more points.
“Our data suggest that the risk of fecal transplant failure is predictable based on pretransplant characteristics. We hope that this risk stratification model will prove helpful,” said Dr. Fischer, whose coauthors included Dr. Kelly.
Although she did not directly endorse this risk stratification tool for patient management, Dr. Surawicz called this presentation “very clinically relevant.” Practical tools are needed to guide the use of this therapy as it becomes more widely used in the treatment of C. difficile, said Dr. Surawicz, professor of gastroenterology, University of Washington, Seattle.
Dr. Kelly reported no relevant financial conflicts. Dr. Fischer reported a financial relationship with Rebiotix.
HONOLULU – Fecal transplant was shown to be effective in the treatment of recurrent or refractory episodes of Clostridium difficile infection in a double-blind trial for the first time, and a second study isolated predictors of treatment failure.
The results of the double-blind study were expected. Several studies, although none double blind, have previously shown this therapy to be efficacious. The study of predictors of failure may be of more immediate practical application, because it is relevant to patient selection, according to the investigators, some of whom were involved in both studies.
In the double-blind study, 46 patients were randomized at two centers to receive a fecal microbiota transplant from donor stool or to a placebo, which was a transplant of the patient’s own stool.
The primary outcome was clinical cure at the end of 8 weeks, achieved in 91% of those randomized to the active therapy and 63% of those randomized to placebo (P = .024). Most of those who had treatment failure, which occurred on average 10 days after the procedure (range, 1-62 days), received the active therapy subsequently and also achieved clinical cure after donor transplantation.
“There were no significant differences in any adverse event rates between the donor transplant and placebo groups,” Dr. Colleen Kelly reported at the annual meeting of the American College of Gastroenterology. Dr. Kelly, a gastroenterologist with the Miriam Hospital, Brown University, Providence, R.I., was also a coauthor of the study of risk factors for the failure of fecal transplant.
Underlining the importance of a double-blind trial to provide confirmation of the efficacy of fecal transplant, Dr. Christina M. Surawicz, who moderated the ACG session at which both studies were presented, said, “We have been waiting for these results.”
However, a disparity in results at the two participating centers is notable. In Providence, cure was achieved in 90% of those receiving fecal transplant versus 43% receiving placebo (P = .019). At the other participating institution, Montefiore Medical Center, New York, the cure rate was 92% with fecal transplant, but 90% of the placebo patients were also cured (P = .89). The data were not intended for a separate analysis, so Dr. Kelly said this did not affect her final conclusion that this trial confirmed the efficacy of this treatment.
In the separate study evaluating predictors of failure to achieve cure after fecal transplant, the retrospective analysis was performed with 345 patients treated for C. difficile infection with fecal transplant. In this population, the overall failure rate was 23.7%, but there was a wide variability observed upon univariate and multivariate analysis of risk factors, Dr. Monika Fischer, a gastroenterologist at Indiana University Hospital, Indianapolis, said at the meeting.
For example, in patients with nonsevere recurrent C. difficile infection, the failure rate was 18%. In contrast, the failure rate was approximately 50% among those with severe refractory C. difficile infection.
Upon multivariate analysis, three risk factors were independent predictors of fecal transplant failure: inpatient status, which was associated with an odds ratio of 6.92 (P = .001); being immunosuppressed (OR, 3.28; P = .0004); and previous hospitalization for C. difficile infection (OR, 1.45 for each prior hospitalization; P less than .001).
With the use of these three factors, a risk score was found to be highly predictive of failure. In this risk score, 5 points were attributed to inpatient status, 3 points to immunosuppression, and 1 point to each prior hospitalization for C. difficile infection. On a scale of 0-12 points, the risk of failure was 13% in those with 0 points, 17% in those with 1-3 points, and 44% in those with 4 or more points.
“Our data suggest that the risk of fecal transplant failure is predictable based on pretransplant characteristics. We hope that this risk stratification model will prove helpful,” said Dr. Fischer, whose coauthors included Dr. Kelly.
Although she did not directly endorse this risk stratification tool for patient management, Dr. Surawicz called this presentation “very clinically relevant.” Practical tools are needed to guide the use of this therapy as it becomes more widely used in the treatment of C. difficile, said Dr. Surawicz, professor of gastroenterology, University of Washington, Seattle.
Dr. Kelly reported no relevant financial conflicts. Dr. Fischer reported a financial relationship with Rebiotix.
AT ACG 2015
GI bleeds in obese patients more complicated but no more fatal
HONOLULU – Obese patients who develop an upper GI bleed receive more treatment, are more likely to develop hemorrhagic shock, and are more likely to require admission to an intensive care unit than those who are not obese, but they do not have higher in-hospital mortality, according to analysis of a large national database that was presented at the annual meeting of the American College of Gastroenterology.
The significantly greater odds ratio of most major complications from upper GI bleeds in patients with obesity relative to those who are not obese was expected but so was an increased rate of in-hospital mortality, according to the first author of the study, Dr. Marwan S. Abou Gergi of Catalyst Medical Consulting, Baltimore.
“In this study, patients with obesity received more frequent endoscopic interventions, which could explain why mortality rates were not significantly higher,” Dr. Abou Gergi reported.
In the analysis, characterized as the first study to evaluate the impact of obesity on outcomes in upper GI hemorrhage, data were drawn from the 2012 Nationwide Inpatient Sample database, which is considered to provide a representative sample of U.S. hospital experience. Drawn from more than 7 million hospitalizations, the study focused on patients 18 or over with a primary ICD-9 code for upper GI hemorrhage. The primary outcome was mortality. Secondary outcomes included interventions, ICU admissions, and length of stay.
Of the 132,545 discharges with upper GI hemorrhage, 11,220 (8.5%) were identified as obese. The in-hospital mortality overall was 1.97%, but the proportion of those who died was slightly lower among patients identified as obese, producing a nonsignificant adjusted odds ratio (OR) of 0.87 (P greater than .1). Yet the rates of hemorrhage shock (OR 1.31; P = .02) and admission to the ICU (OR 1.35; P less than .02) were greater in the obese. The median length of stay of 0.35 days for obese patients was also significantly longer.
One reason for the lower rate of mortality may be more aggressive treatment. In particular, repeat endoscopy therapy was more common in those who were obese (P less than .01), suggesting, “Our treatments are working,” Dr. Abou Gergi said.
The proportion of patients with a score of 3 or greater on the Charlson comorbidity index was higher in the obese than in those not identified as obese (49% vs. 39%; P less than .01). This along with previously published evidence that obese patients take more anticoagulants, take more antiplatelets, and may face delays in endoscopy due to greater difficulty in administering sedation, were among considerations predicting a higher mortality, according to Dr. Abou Gergi.
However, there are several potential explanations for these unexpected findings. One is that mortality rates overall were low, making it difficult to show differences on this outcome. In addition, ICD-9 codes may be effective for isolating a group with obesity but not in identifying a control group without obesity.
“It is likely that not all patients who are obese received this code, so we may be seeing a population of obese patients be compared to another population that includes at least some patients who also have obesity,” explained Dr. John R. Saltzman, director of endoscopy, Brigham and Women’s Hospital, Boston. A coauthor of this study, Dr. Saltzman noted that despite a comparable rate of in-hospital mortality, most of the findings in the study argued that patients who develop upper GI bleeding have a more difficult course. He noted that this is reflected in the cost of care, which was significantly higher in those who were obese.
Although he acknowledged that he was surprised that this was “essentially a negative study,” he believes that mortality may have been “too tough” as a primary endpoint for demonstrating a difference. However, he also believes that it may be appropriate to give credit for effective treatments.
“I think that may be the key. We are just getting better at taking care of these patients,” Dr. Saltzman said.
Dr. Abou Gergi reported he has no relevant financial relationships.
HONOLULU – Obese patients who develop an upper GI bleed receive more treatment, are more likely to develop hemorrhagic shock, and are more likely to require admission to an intensive care unit than those who are not obese, but they do not have higher in-hospital mortality, according to analysis of a large national database that was presented at the annual meeting of the American College of Gastroenterology.
The significantly greater odds ratio of most major complications from upper GI bleeds in patients with obesity relative to those who are not obese was expected but so was an increased rate of in-hospital mortality, according to the first author of the study, Dr. Marwan S. Abou Gergi of Catalyst Medical Consulting, Baltimore.
“In this study, patients with obesity received more frequent endoscopic interventions, which could explain why mortality rates were not significantly higher,” Dr. Abou Gergi reported.
In the analysis, characterized as the first study to evaluate the impact of obesity on outcomes in upper GI hemorrhage, data were drawn from the 2012 Nationwide Inpatient Sample database, which is considered to provide a representative sample of U.S. hospital experience. Drawn from more than 7 million hospitalizations, the study focused on patients 18 or over with a primary ICD-9 code for upper GI hemorrhage. The primary outcome was mortality. Secondary outcomes included interventions, ICU admissions, and length of stay.
Of the 132,545 discharges with upper GI hemorrhage, 11,220 (8.5%) were identified as obese. The in-hospital mortality overall was 1.97%, but the proportion of those who died was slightly lower among patients identified as obese, producing a nonsignificant adjusted odds ratio (OR) of 0.87 (P greater than .1). Yet the rates of hemorrhage shock (OR 1.31; P = .02) and admission to the ICU (OR 1.35; P less than .02) were greater in the obese. The median length of stay of 0.35 days for obese patients was also significantly longer.
One reason for the lower rate of mortality may be more aggressive treatment. In particular, repeat endoscopy therapy was more common in those who were obese (P less than .01), suggesting, “Our treatments are working,” Dr. Abou Gergi said.
The proportion of patients with a score of 3 or greater on the Charlson comorbidity index was higher in the obese than in those not identified as obese (49% vs. 39%; P less than .01). This along with previously published evidence that obese patients take more anticoagulants, take more antiplatelets, and may face delays in endoscopy due to greater difficulty in administering sedation, were among considerations predicting a higher mortality, according to Dr. Abou Gergi.
However, there are several potential explanations for these unexpected findings. One is that mortality rates overall were low, making it difficult to show differences on this outcome. In addition, ICD-9 codes may be effective for isolating a group with obesity but not in identifying a control group without obesity.
“It is likely that not all patients who are obese received this code, so we may be seeing a population of obese patients be compared to another population that includes at least some patients who also have obesity,” explained Dr. John R. Saltzman, director of endoscopy, Brigham and Women’s Hospital, Boston. A coauthor of this study, Dr. Saltzman noted that despite a comparable rate of in-hospital mortality, most of the findings in the study argued that patients who develop upper GI bleeding have a more difficult course. He noted that this is reflected in the cost of care, which was significantly higher in those who were obese.
Although he acknowledged that he was surprised that this was “essentially a negative study,” he believes that mortality may have been “too tough” as a primary endpoint for demonstrating a difference. However, he also believes that it may be appropriate to give credit for effective treatments.
“I think that may be the key. We are just getting better at taking care of these patients,” Dr. Saltzman said.
Dr. Abou Gergi reported he has no relevant financial relationships.
HONOLULU – Obese patients who develop an upper GI bleed receive more treatment, are more likely to develop hemorrhagic shock, and are more likely to require admission to an intensive care unit than those who are not obese, but they do not have higher in-hospital mortality, according to analysis of a large national database that was presented at the annual meeting of the American College of Gastroenterology.
The significantly greater odds ratio of most major complications from upper GI bleeds in patients with obesity relative to those who are not obese was expected but so was an increased rate of in-hospital mortality, according to the first author of the study, Dr. Marwan S. Abou Gergi of Catalyst Medical Consulting, Baltimore.
“In this study, patients with obesity received more frequent endoscopic interventions, which could explain why mortality rates were not significantly higher,” Dr. Abou Gergi reported.
In the analysis, characterized as the first study to evaluate the impact of obesity on outcomes in upper GI hemorrhage, data were drawn from the 2012 Nationwide Inpatient Sample database, which is considered to provide a representative sample of U.S. hospital experience. Drawn from more than 7 million hospitalizations, the study focused on patients 18 or over with a primary ICD-9 code for upper GI hemorrhage. The primary outcome was mortality. Secondary outcomes included interventions, ICU admissions, and length of stay.
Of the 132,545 discharges with upper GI hemorrhage, 11,220 (8.5%) were identified as obese. The in-hospital mortality overall was 1.97%, but the proportion of those who died was slightly lower among patients identified as obese, producing a nonsignificant adjusted odds ratio (OR) of 0.87 (P greater than .1). Yet the rates of hemorrhage shock (OR 1.31; P = .02) and admission to the ICU (OR 1.35; P less than .02) were greater in the obese. The median length of stay of 0.35 days for obese patients was also significantly longer.
One reason for the lower rate of mortality may be more aggressive treatment. In particular, repeat endoscopy therapy was more common in those who were obese (P less than .01), suggesting, “Our treatments are working,” Dr. Abou Gergi said.
The proportion of patients with a score of 3 or greater on the Charlson comorbidity index was higher in the obese than in those not identified as obese (49% vs. 39%; P less than .01). This along with previously published evidence that obese patients take more anticoagulants, take more antiplatelets, and may face delays in endoscopy due to greater difficulty in administering sedation, were among considerations predicting a higher mortality, according to Dr. Abou Gergi.
However, there are several potential explanations for these unexpected findings. One is that mortality rates overall were low, making it difficult to show differences on this outcome. In addition, ICD-9 codes may be effective for isolating a group with obesity but not in identifying a control group without obesity.
“It is likely that not all patients who are obese received this code, so we may be seeing a population of obese patients be compared to another population that includes at least some patients who also have obesity,” explained Dr. John R. Saltzman, director of endoscopy, Brigham and Women’s Hospital, Boston. A coauthor of this study, Dr. Saltzman noted that despite a comparable rate of in-hospital mortality, most of the findings in the study argued that patients who develop upper GI bleeding have a more difficult course. He noted that this is reflected in the cost of care, which was significantly higher in those who were obese.
Although he acknowledged that he was surprised that this was “essentially a negative study,” he believes that mortality may have been “too tough” as a primary endpoint for demonstrating a difference. However, he also believes that it may be appropriate to give credit for effective treatments.
“I think that may be the key. We are just getting better at taking care of these patients,” Dr. Saltzman said.
Dr. Abou Gergi reported he has no relevant financial relationships.
AT ACG 2015