User login
Erythrodermic psoriasis is a severe form of psoriasis associated with higher morbidity and mortality rates compared to other forms of psoriasis. Cutaneous signs of erythrodermic psoriasis include erythema, edema, and superficial desquamation. Scabies is a common ectoparasitic disease that is diagnosed by the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. The course of scabies may be altered in patients with desquamative inflammatory skin disease such as psoriasis. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis.
Case Reports
Patient 1
A 13-year-old adolescent boy with psoriasis of 4 years’ duration presented to our outpatient clinic with severe widespread erythema and mild desquamation (Figure 1). The patient was hospitalized following a diagnosis of erythrodermic psoriasis. His medical history was remarkable for recurrent episodes of bronchitis, and his family history included 2 siblings with psoriasis. Physical examination revealed no abnormalities, except for a fever (temperature, 38.0°C). A complete blood cell count revealed an elevated absolute eosinophil count (9260 cells/µL [reference range, 0–700 cells/µL]) corresponding to 48.4% (reference range, 0%–7%) of blood cells. There were no pathological findings in the serum biochemistry; complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Peripheral blood smear, abdominal ultrasonography, electrocardiography, and echocardiography were performed; no cardiac pathology was observed. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis.
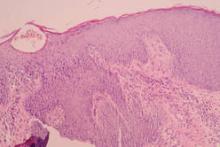
One week after the initiation of treatment the patient’s fever improved. At 2-week follow-up, a complete blood cell count demonstrated more marked eosinophilia, and the percentage of eosinophils at weekly intervals over the next 3 weeks increased to 51.2%, 63.0%, and 71.7%, respectively. The patient presented 2 weeks later with a chief concern of pruritus. Histologic examination of a lesional biopsy specimen revealed psoriasiform epithelial hyperplasia with scabies mites in the stratum corneum (Figure 2). Mites also were noted on direct microscopic examination of scrapings performed with the suspicion of scabies. The patient was treated with permethrin cream 5%. Although all of the patients and staff in the ward also were administered topical permethrin to prevent a scabies epidemic, 2 inpatients who had been discharged before the diagnosis of scabies presented to our outpatient clinic approximately 1 month later with scabies. At 6-month follow-up, the patient’s eosinophil count was within reference range (0.237cells/µL; 3.78%); pruritus and lesions were not observed.
Patient 2
A 26-year-old woman with psoriasis of 5 years’ duration was hospitalized for treatment of erythrodermic psoriasis at the same time as patient 1, her brother. On dermatologic examination, severe widespread erythema, scaling, and edema were noted (Figure 3). Physical examination revealed a fever (temperature, 38.5°C). Hypoalbuminemia and high C-reactive protein levels were present in serum biochemistry. Eosinophil counts were within reference range (0.346 cells/µL; 1.88%). No pathological findings were noted in the complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis. On days 20 and 45 of treatment, eosinophil levels were 8.26% (0.994 cells/mL) and 17.5% (1620 cells/mL), respectively. The patient’s erythema and edema remarkably decreased at the end of the first month of treatment with cyclosporine, but simultaneous onset of pruritus and increasing eosinophil levels despite treatment with cyclosporine were noted. Scabies mites were demonstrated on microscopic examination of skin scrapings from the dorsal aspect of the hand (Figure 4), and the patient was treated with permethrin cream 5%. At 6-month follow-up, eosinophil levels were within reference range (0.317 cells/mL; 4.75%); pruritus and lesions were not observed.
 |
| Figure 3. Severe widespread erythema, scaling, and edema in a 26-year-old woman with psoriasis. |
 |
Figure 4. A mite and an egg were noted on direct microscopic examination of skin scrapings from the dorsal aspect of the hand (original magnification ×400). |
Comment
Erythrodermic psoriasis is a severe form of psoriasis. In the 2010 consensus of the National Psoriasis Foundation medical board, it was reported that cyclosporine and infliximab are the fastest and most effective agents in treating erythrodermic psoriasis.1
Progressive increases in the number of eosinophils prompted us to screen our patients for causes of hypereosinophilia. Increased eosinophil counts have not been linked to treatment with cyclosporine. In contrast, it has been detected that cyclosporine reduces the number of eosinophils in many eosinophilic dermatoses.2
There is no hematologic finding for scabies; therefore, clinical findings are most important in the diagnosis. Crusted scabies is a special form of scabies seen in immunocompromised patients that is characterized by excessive numbers of scabies mites. Peripheral eosinophilia may be observed in this form of the disease.3 In classic scabies, eosinophilia is uncommon in peripheral blood. In contrast with these data, there are 2 cases in the literature of scabies secondary to disorders of keratinization without immune deficiency with different clinical presentations.4 In these patients, the most striking and only finding at the time of diagnosis was substantial eosinophilia. These cases were reported with emphasis on eosinophilia as the first sign of scabies infestation in patients with severe hyperkeratosis.4 In our patients, the spread of infection may have been facilitated by the immunosuppressive effects of cyclosporine in addition to the existing disease. Crusted scabies after use of cyclosporine for atopic dermatitis has been reported. It was emphasized that suppression of scratching and immunosuppression due to cyclospor-ine caused the spread of scabies mites in the skin.5
Burrows, vesicles, and erythematous papules are typical lesions seen in scabies. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. In our patients, widespread erythema and scaling were noted, and pruritus was thought to be due to psoriasis lesions. Because of excessive scaling in the stratum corneum from psoriasis, the clinical features of scabies were concealed and the classic clinical signs of scabies were not present. The patients’ hypereosinophilia led us to investigate the cause. A lesional biopsy and direct microscopy demonstrated scabies mites.
Conclusion
The relationship between psoriasis and scabies previously has been reported in the literature as scabies with crusts mimicking rupioid psoriasis.6 However, our patients developed scabies in the setting of psoriasis. Severe scabies can present as erythroderma.7 We believe the diagnosis of scabies in our patients would have been more complicated without the preexisting psoriasis, as biopsies of erythrodermic psoriasis often are nonspecific and may contain eosinophils in the inflammatory infiltrate. Although pruritus may be interpreted as a result of the primary dermatologic disease, the presence of hypereosinophilia may suggest scabies in erythrodermic patients. For this reason, peripheral eosinophilia may suggest scabies in patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents, and a search for scabies mites in skin scrapings should be undertaken.
1. Rosenbach M, Hsu S, Korman NJ, et al. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation [published online ahead of print August 8, 2009]. J Am Acad Dermatol. 2010;62:655-662.
2. Maleki D, Sayyah A, Rahimi-Rad MH, et al. Kimura’s disease with eosinophilic panniculitis–treated with cyclosporine: a case report. Allergy Asthma Clin Immunol. 2010;6:5.
3. Roberts LJ, Huffam SE, Walton SF, et al. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect. 2005;50:375-381.
4. Sluzevich JC, Sheth AP, Lucky AV. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol. 2007;143:670-673.
5. Monari P, Sala R, Calzavara-Pinton P. Norwegian scabies in a healthy woman during oral cyclosporine therapy [published online ahead of print March 2, 2007]. Eur J Dermatol. 2007;17:173.
6. Costa JB, Rocha de Sousa VL, da Trindade Neto PB, et al. Norwegian scabies mimicking rupioid psoriasis. An Bras Dermatol. 2012;87:910-913.
7. Mehta V, Balachandran C, Monga P, et al. Images in clinical practice. Norwegian scabies presenting as erythroderma. Indian J Dermatol Venereol Leprol. 2009;75:609-610.
Erythrodermic psoriasis is a severe form of psoriasis associated with higher morbidity and mortality rates compared to other forms of psoriasis. Cutaneous signs of erythrodermic psoriasis include erythema, edema, and superficial desquamation. Scabies is a common ectoparasitic disease that is diagnosed by the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. The course of scabies may be altered in patients with desquamative inflammatory skin disease such as psoriasis. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis.
Case Reports
Patient 1
A 13-year-old adolescent boy with psoriasis of 4 years’ duration presented to our outpatient clinic with severe widespread erythema and mild desquamation (Figure 1). The patient was hospitalized following a diagnosis of erythrodermic psoriasis. His medical history was remarkable for recurrent episodes of bronchitis, and his family history included 2 siblings with psoriasis. Physical examination revealed no abnormalities, except for a fever (temperature, 38.0°C). A complete blood cell count revealed an elevated absolute eosinophil count (9260 cells/µL [reference range, 0–700 cells/µL]) corresponding to 48.4% (reference range, 0%–7%) of blood cells. There were no pathological findings in the serum biochemistry; complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Peripheral blood smear, abdominal ultrasonography, electrocardiography, and echocardiography were performed; no cardiac pathology was observed. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis.
One week after the initiation of treatment the patient’s fever improved. At 2-week follow-up, a complete blood cell count demonstrated more marked eosinophilia, and the percentage of eosinophils at weekly intervals over the next 3 weeks increased to 51.2%, 63.0%, and 71.7%, respectively. The patient presented 2 weeks later with a chief concern of pruritus. Histologic examination of a lesional biopsy specimen revealed psoriasiform epithelial hyperplasia with scabies mites in the stratum corneum (Figure 2). Mites also were noted on direct microscopic examination of scrapings performed with the suspicion of scabies. The patient was treated with permethrin cream 5%. Although all of the patients and staff in the ward also were administered topical permethrin to prevent a scabies epidemic, 2 inpatients who had been discharged before the diagnosis of scabies presented to our outpatient clinic approximately 1 month later with scabies. At 6-month follow-up, the patient’s eosinophil count was within reference range (0.237cells/µL; 3.78%); pruritus and lesions were not observed.
Patient 2
A 26-year-old woman with psoriasis of 5 years’ duration was hospitalized for treatment of erythrodermic psoriasis at the same time as patient 1, her brother. On dermatologic examination, severe widespread erythema, scaling, and edema were noted (Figure 3). Physical examination revealed a fever (temperature, 38.5°C). Hypoalbuminemia and high C-reactive protein levels were present in serum biochemistry. Eosinophil counts were within reference range (0.346 cells/µL; 1.88%). No pathological findings were noted in the complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis. On days 20 and 45 of treatment, eosinophil levels were 8.26% (0.994 cells/mL) and 17.5% (1620 cells/mL), respectively. The patient’s erythema and edema remarkably decreased at the end of the first month of treatment with cyclosporine, but simultaneous onset of pruritus and increasing eosinophil levels despite treatment with cyclosporine were noted. Scabies mites were demonstrated on microscopic examination of skin scrapings from the dorsal aspect of the hand (Figure 4), and the patient was treated with permethrin cream 5%. At 6-month follow-up, eosinophil levels were within reference range (0.317 cells/mL; 4.75%); pruritus and lesions were not observed.
 |
| Figure 3. Severe widespread erythema, scaling, and edema in a 26-year-old woman with psoriasis. |
 |
Figure 4. A mite and an egg were noted on direct microscopic examination of skin scrapings from the dorsal aspect of the hand (original magnification ×400). |
Comment
Erythrodermic psoriasis is a severe form of psoriasis. In the 2010 consensus of the National Psoriasis Foundation medical board, it was reported that cyclosporine and infliximab are the fastest and most effective agents in treating erythrodermic psoriasis.1
Progressive increases in the number of eosinophils prompted us to screen our patients for causes of hypereosinophilia. Increased eosinophil counts have not been linked to treatment with cyclosporine. In contrast, it has been detected that cyclosporine reduces the number of eosinophils in many eosinophilic dermatoses.2
There is no hematologic finding for scabies; therefore, clinical findings are most important in the diagnosis. Crusted scabies is a special form of scabies seen in immunocompromised patients that is characterized by excessive numbers of scabies mites. Peripheral eosinophilia may be observed in this form of the disease.3 In classic scabies, eosinophilia is uncommon in peripheral blood. In contrast with these data, there are 2 cases in the literature of scabies secondary to disorders of keratinization without immune deficiency with different clinical presentations.4 In these patients, the most striking and only finding at the time of diagnosis was substantial eosinophilia. These cases were reported with emphasis on eosinophilia as the first sign of scabies infestation in patients with severe hyperkeratosis.4 In our patients, the spread of infection may have been facilitated by the immunosuppressive effects of cyclosporine in addition to the existing disease. Crusted scabies after use of cyclosporine for atopic dermatitis has been reported. It was emphasized that suppression of scratching and immunosuppression due to cyclospor-ine caused the spread of scabies mites in the skin.5
Burrows, vesicles, and erythematous papules are typical lesions seen in scabies. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. In our patients, widespread erythema and scaling were noted, and pruritus was thought to be due to psoriasis lesions. Because of excessive scaling in the stratum corneum from psoriasis, the clinical features of scabies were concealed and the classic clinical signs of scabies were not present. The patients’ hypereosinophilia led us to investigate the cause. A lesional biopsy and direct microscopy demonstrated scabies mites.
Conclusion
The relationship between psoriasis and scabies previously has been reported in the literature as scabies with crusts mimicking rupioid psoriasis.6 However, our patients developed scabies in the setting of psoriasis. Severe scabies can present as erythroderma.7 We believe the diagnosis of scabies in our patients would have been more complicated without the preexisting psoriasis, as biopsies of erythrodermic psoriasis often are nonspecific and may contain eosinophils in the inflammatory infiltrate. Although pruritus may be interpreted as a result of the primary dermatologic disease, the presence of hypereosinophilia may suggest scabies in erythrodermic patients. For this reason, peripheral eosinophilia may suggest scabies in patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents, and a search for scabies mites in skin scrapings should be undertaken.
Erythrodermic psoriasis is a severe form of psoriasis associated with higher morbidity and mortality rates compared to other forms of psoriasis. Cutaneous signs of erythrodermic psoriasis include erythema, edema, and superficial desquamation. Scabies is a common ectoparasitic disease that is diagnosed by the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. The course of scabies may be altered in patients with desquamative inflammatory skin disease such as psoriasis. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis.
Case Reports
Patient 1
A 13-year-old adolescent boy with psoriasis of 4 years’ duration presented to our outpatient clinic with severe widespread erythema and mild desquamation (Figure 1). The patient was hospitalized following a diagnosis of erythrodermic psoriasis. His medical history was remarkable for recurrent episodes of bronchitis, and his family history included 2 siblings with psoriasis. Physical examination revealed no abnormalities, except for a fever (temperature, 38.0°C). A complete blood cell count revealed an elevated absolute eosinophil count (9260 cells/µL [reference range, 0–700 cells/µL]) corresponding to 48.4% (reference range, 0%–7%) of blood cells. There were no pathological findings in the serum biochemistry; complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Peripheral blood smear, abdominal ultrasonography, electrocardiography, and echocardiography were performed; no cardiac pathology was observed. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis.
One week after the initiation of treatment the patient’s fever improved. At 2-week follow-up, a complete blood cell count demonstrated more marked eosinophilia, and the percentage of eosinophils at weekly intervals over the next 3 weeks increased to 51.2%, 63.0%, and 71.7%, respectively. The patient presented 2 weeks later with a chief concern of pruritus. Histologic examination of a lesional biopsy specimen revealed psoriasiform epithelial hyperplasia with scabies mites in the stratum corneum (Figure 2). Mites also were noted on direct microscopic examination of scrapings performed with the suspicion of scabies. The patient was treated with permethrin cream 5%. Although all of the patients and staff in the ward also were administered topical permethrin to prevent a scabies epidemic, 2 inpatients who had been discharged before the diagnosis of scabies presented to our outpatient clinic approximately 1 month later with scabies. At 6-month follow-up, the patient’s eosinophil count was within reference range (0.237cells/µL; 3.78%); pruritus and lesions were not observed.
Patient 2
A 26-year-old woman with psoriasis of 5 years’ duration was hospitalized for treatment of erythrodermic psoriasis at the same time as patient 1, her brother. On dermatologic examination, severe widespread erythema, scaling, and edema were noted (Figure 3). Physical examination revealed a fever (temperature, 38.5°C). Hypoalbuminemia and high C-reactive protein levels were present in serum biochemistry. Eosinophil counts were within reference range (0.346 cells/µL; 1.88%). No pathological findings were noted in the complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis. On days 20 and 45 of treatment, eosinophil levels were 8.26% (0.994 cells/mL) and 17.5% (1620 cells/mL), respectively. The patient’s erythema and edema remarkably decreased at the end of the first month of treatment with cyclosporine, but simultaneous onset of pruritus and increasing eosinophil levels despite treatment with cyclosporine were noted. Scabies mites were demonstrated on microscopic examination of skin scrapings from the dorsal aspect of the hand (Figure 4), and the patient was treated with permethrin cream 5%. At 6-month follow-up, eosinophil levels were within reference range (0.317 cells/mL; 4.75%); pruritus and lesions were not observed.
 |
| Figure 3. Severe widespread erythema, scaling, and edema in a 26-year-old woman with psoriasis. |
 |
Figure 4. A mite and an egg were noted on direct microscopic examination of skin scrapings from the dorsal aspect of the hand (original magnification ×400). |
Comment
Erythrodermic psoriasis is a severe form of psoriasis. In the 2010 consensus of the National Psoriasis Foundation medical board, it was reported that cyclosporine and infliximab are the fastest and most effective agents in treating erythrodermic psoriasis.1
Progressive increases in the number of eosinophils prompted us to screen our patients for causes of hypereosinophilia. Increased eosinophil counts have not been linked to treatment with cyclosporine. In contrast, it has been detected that cyclosporine reduces the number of eosinophils in many eosinophilic dermatoses.2
There is no hematologic finding for scabies; therefore, clinical findings are most important in the diagnosis. Crusted scabies is a special form of scabies seen in immunocompromised patients that is characterized by excessive numbers of scabies mites. Peripheral eosinophilia may be observed in this form of the disease.3 In classic scabies, eosinophilia is uncommon in peripheral blood. In contrast with these data, there are 2 cases in the literature of scabies secondary to disorders of keratinization without immune deficiency with different clinical presentations.4 In these patients, the most striking and only finding at the time of diagnosis was substantial eosinophilia. These cases were reported with emphasis on eosinophilia as the first sign of scabies infestation in patients with severe hyperkeratosis.4 In our patients, the spread of infection may have been facilitated by the immunosuppressive effects of cyclosporine in addition to the existing disease. Crusted scabies after use of cyclosporine for atopic dermatitis has been reported. It was emphasized that suppression of scratching and immunosuppression due to cyclospor-ine caused the spread of scabies mites in the skin.5
Burrows, vesicles, and erythematous papules are typical lesions seen in scabies. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. In our patients, widespread erythema and scaling were noted, and pruritus was thought to be due to psoriasis lesions. Because of excessive scaling in the stratum corneum from psoriasis, the clinical features of scabies were concealed and the classic clinical signs of scabies were not present. The patients’ hypereosinophilia led us to investigate the cause. A lesional biopsy and direct microscopy demonstrated scabies mites.
Conclusion
The relationship between psoriasis and scabies previously has been reported in the literature as scabies with crusts mimicking rupioid psoriasis.6 However, our patients developed scabies in the setting of psoriasis. Severe scabies can present as erythroderma.7 We believe the diagnosis of scabies in our patients would have been more complicated without the preexisting psoriasis, as biopsies of erythrodermic psoriasis often are nonspecific and may contain eosinophils in the inflammatory infiltrate. Although pruritus may be interpreted as a result of the primary dermatologic disease, the presence of hypereosinophilia may suggest scabies in erythrodermic patients. For this reason, peripheral eosinophilia may suggest scabies in patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents, and a search for scabies mites in skin scrapings should be undertaken.
1. Rosenbach M, Hsu S, Korman NJ, et al. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation [published online ahead of print August 8, 2009]. J Am Acad Dermatol. 2010;62:655-662.
2. Maleki D, Sayyah A, Rahimi-Rad MH, et al. Kimura’s disease with eosinophilic panniculitis–treated with cyclosporine: a case report. Allergy Asthma Clin Immunol. 2010;6:5.
3. Roberts LJ, Huffam SE, Walton SF, et al. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect. 2005;50:375-381.
4. Sluzevich JC, Sheth AP, Lucky AV. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol. 2007;143:670-673.
5. Monari P, Sala R, Calzavara-Pinton P. Norwegian scabies in a healthy woman during oral cyclosporine therapy [published online ahead of print March 2, 2007]. Eur J Dermatol. 2007;17:173.
6. Costa JB, Rocha de Sousa VL, da Trindade Neto PB, et al. Norwegian scabies mimicking rupioid psoriasis. An Bras Dermatol. 2012;87:910-913.
7. Mehta V, Balachandran C, Monga P, et al. Images in clinical practice. Norwegian scabies presenting as erythroderma. Indian J Dermatol Venereol Leprol. 2009;75:609-610.
1. Rosenbach M, Hsu S, Korman NJ, et al. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation [published online ahead of print August 8, 2009]. J Am Acad Dermatol. 2010;62:655-662.
2. Maleki D, Sayyah A, Rahimi-Rad MH, et al. Kimura’s disease with eosinophilic panniculitis–treated with cyclosporine: a case report. Allergy Asthma Clin Immunol. 2010;6:5.
3. Roberts LJ, Huffam SE, Walton SF, et al. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect. 2005;50:375-381.
4. Sluzevich JC, Sheth AP, Lucky AV. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol. 2007;143:670-673.
5. Monari P, Sala R, Calzavara-Pinton P. Norwegian scabies in a healthy woman during oral cyclosporine therapy [published online ahead of print March 2, 2007]. Eur J Dermatol. 2007;17:173.
6. Costa JB, Rocha de Sousa VL, da Trindade Neto PB, et al. Norwegian scabies mimicking rupioid psoriasis. An Bras Dermatol. 2012;87:910-913.
7. Mehta V, Balachandran C, Monga P, et al. Images in clinical practice. Norwegian scabies presenting as erythroderma. Indian J Dermatol Venereol Leprol. 2009;75:609-610.
- If a desquamative disease such as psoriasis precedes scabies, then the disease course may be altered. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis.
- The presence of hypereosinophilia may suggest scabies in patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents; therefore, a search for sarcoptic mites in skin scrapings should be undertaken.