User login
Child murder by parents: Toward prevention
Deaths of children who are killed by their parents often make the news. Cases of maternal infanticide may be particularly shocking, since women are expected to be selfless nurturers. Yet when a child is murdered, the most common perpetrator is their parent, and mothers and fathers kill at similar rates.1
As psychiatrists, we may see these cases in the news and worry about the risks of our own patients killing their children. In approximately 500 cases annually, an American parent is arrested for the homicide of their child.2 This is not even the entire story, since a large percentage of such cases end in suicide—and no arrest. This article reviews the reasons parents kill their children, and considers common characteristics of these parents, dispelling some myths, before discussing the importance of prevention efforts.
Types of child murder by parents
Child murder by parents is termed filicide. Infanticide has various meanings but often refers to the murder of a child younger than age 1. Approximately 2 dozen nations (but not the United States) have Infanticide Acts that decrease the penalty for mothers who kill their young child.3 Neonaticide refers to murder of the infant at birth or in the first day of life.4
Epidemiology and common characteristics
Approximately 15%—or 1 in 7 murders with an arrest—is a filicide.2 The younger the child, the greater the risk, but older children are killed as well.2 Internationally, fathers and mothers are found to kill at similar rates. For other types of homicide, offenders are overwhelmingly male. This makes child murder by parents the singular type of murder in which women and men perpetrate in equal numbers. Fathers are more likely than mothers to also commit suicide after they kill their children.5 The “Cinderella effect” refers to the elevated risk of a stepchild being killed compared to the risk for a biological child.6
In the general international population, mothers who commit filicide tend to have multiple stressors and limited resources. They may be socially isolated and may be victims themselves as well as potentially experiencing substance abuse.1 Some mothers view the child they killed as abnormal.
Less research has been conducted about fathers who kill. Fathers are more likely to also commit partner homicide.5,7 They are more likely to complete filicide-suicide and use firearms or other violent means.5,7-9 Fathers may have a history of violence, substance abuse, and/or mental illness.7
Neonaticide
Mothers are the most common perpetrator of neonaticide.4 It is unusual for a father to be involved in a neonaticide, or for the father and mother to perpetrate the act together. Rates of neonaticide are considered underestimates because of the number of hidden pregnancies, hidden corpses, and the difficulty that forensic pathologists may have in determining whether a baby was born alive or dead.
Continue to: Perpetrators of neonaticide...
Perpetrators of neonaticide tend to be single, relatively young women acting alone. They often live with their parents and are fearful of the repercussions of being pregnant. Pregnancies are often hidden, with no prenatal care. This includes both denial and concealment of pregnancy.4 Perpetrators of neonaticide commonly lack a premorbid serious mental illness, though after the homicide they may develop anxiety, depression, posttraumatic stress disorder (PTSD), or adjustment disorder.4 (Individuals who unwittingly find a murdered baby’s corpse may also be at risk of PTSD.)
Hidden pregnancies may be due to concealment or denial of pregnancy.10,11 Concealment of pregnancy involves a woman knowing she is pregnant, but purposely hiding from others. Concealment may occur after a period of denial of pregnancy. Denial of pregnancy has several subtypes: pervasive denial, affective denial, and psychotic denial. In cases of pervasive denial, the existence of the pregnancy and the pregnancy’s emotional significance is outside the woman’s awareness. Alternatively, in affective denial, she is intellectually aware that she is pregnant but makes little emotional or physical preparation. In the rarest form, psychotic denial, a woman with a psychotic disorder such as schizophrenia may intermittently deny her pregnancy. This may be correlated with a history of custody loss.10,11 Unlike denial of other medical conditions, in cases of denial of pregnancy, there will exist a very specific point in time (delivery) when the reality of the baby confronts the woman. Risks in cases of hidden pregnancies include those from lack of prenatal care and an assisted delivery as well as neonaticide. An FBI study12 of law enforcement files found most neonaticide offenders were single young women with no criminal or psychological history. A caveat is that in the rare cases in which a woman with psychotic illness commits neonaticide, she may have different characteristics from those generally reported.13
Motives
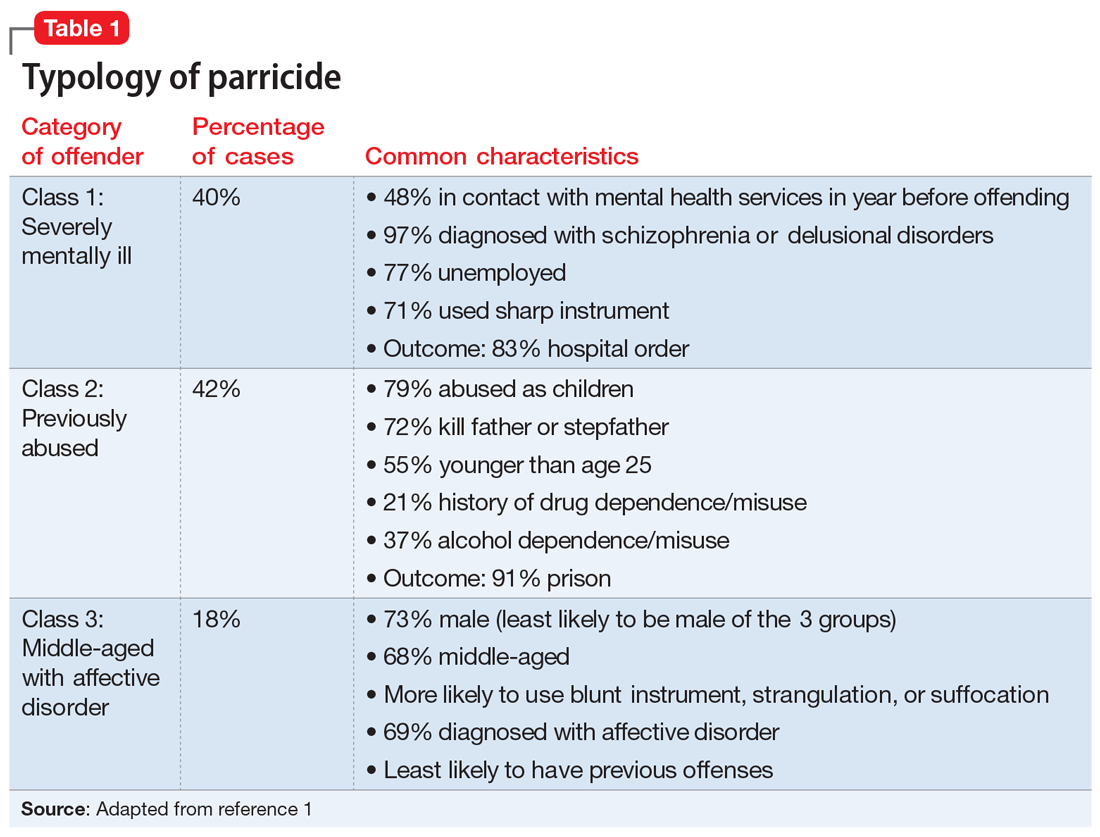
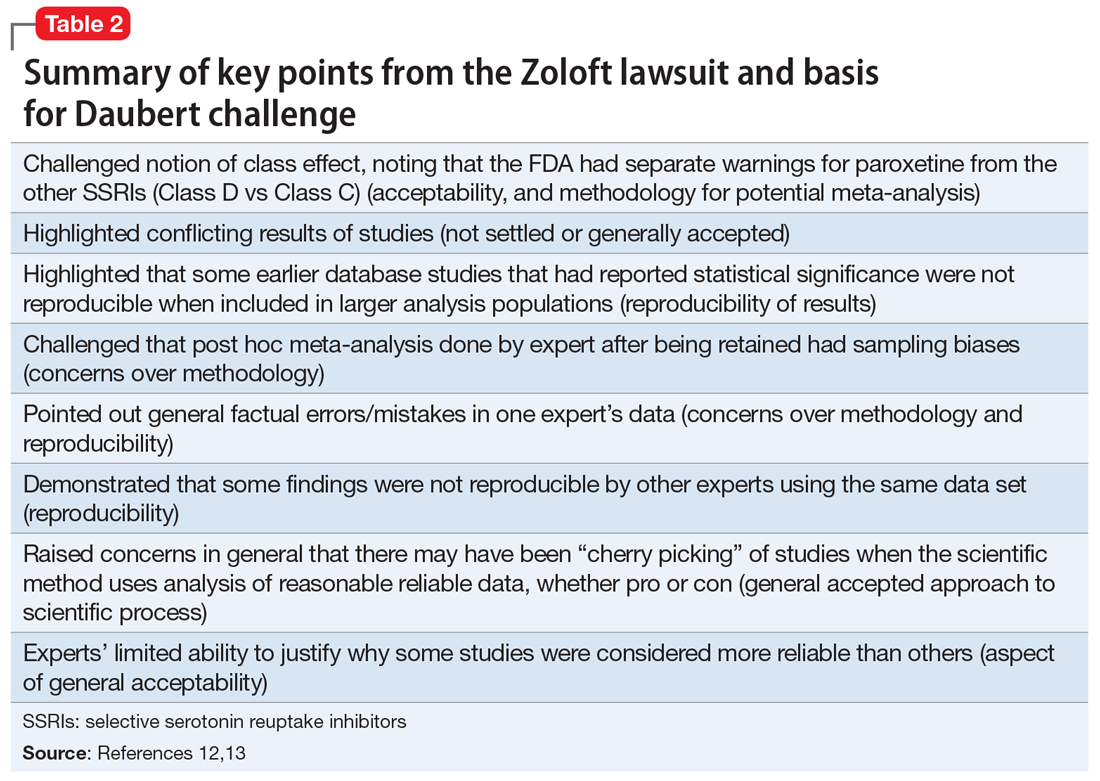
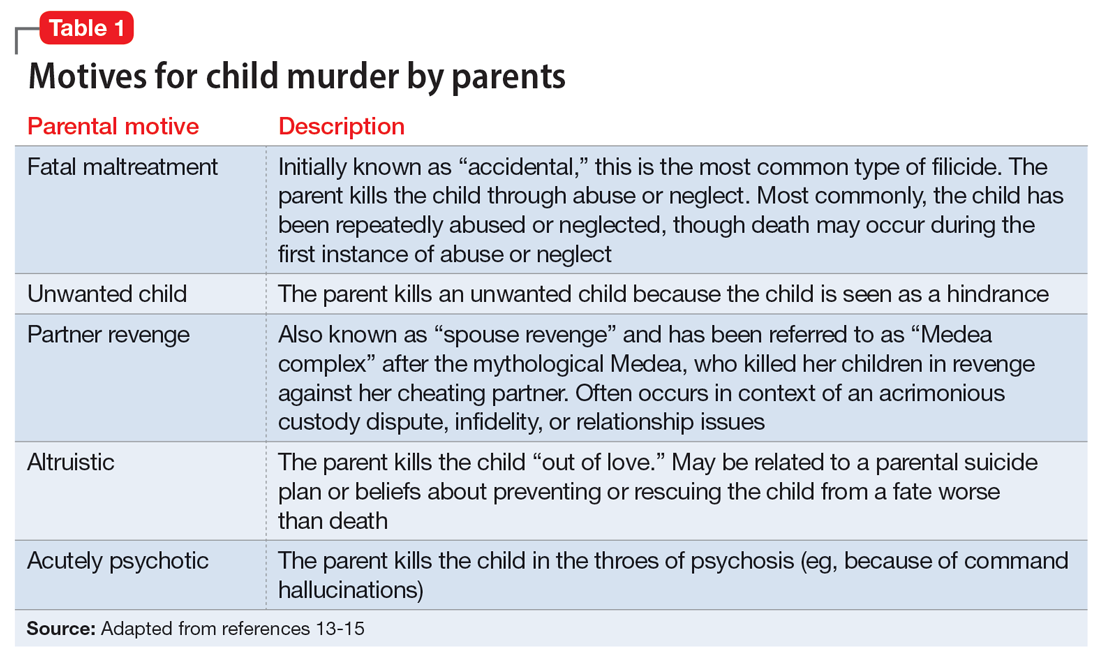
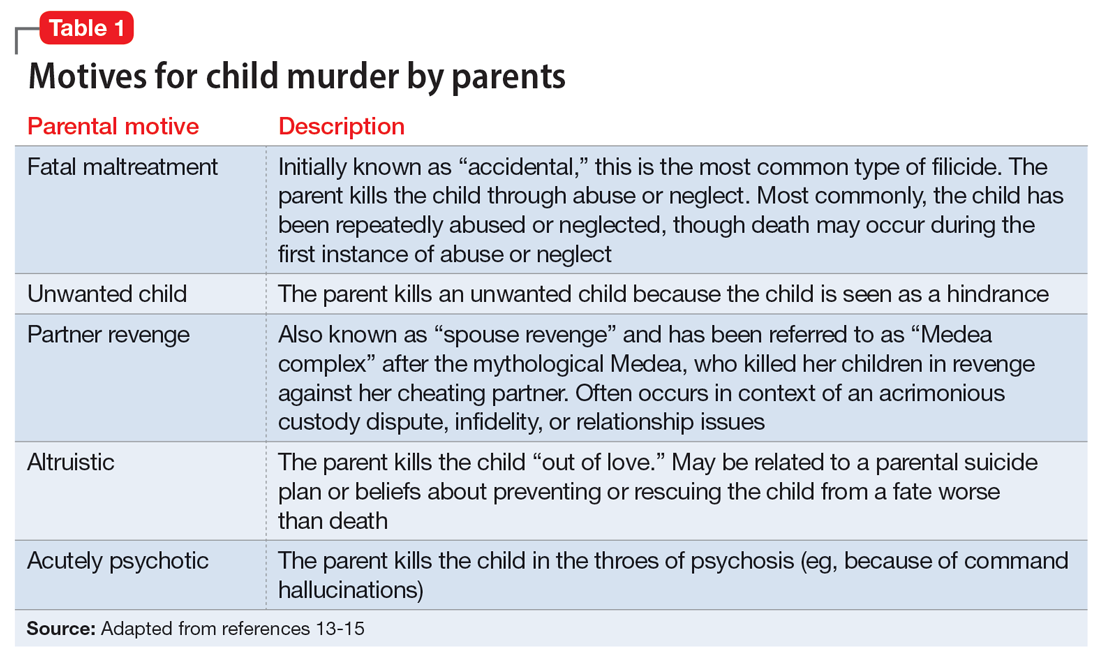
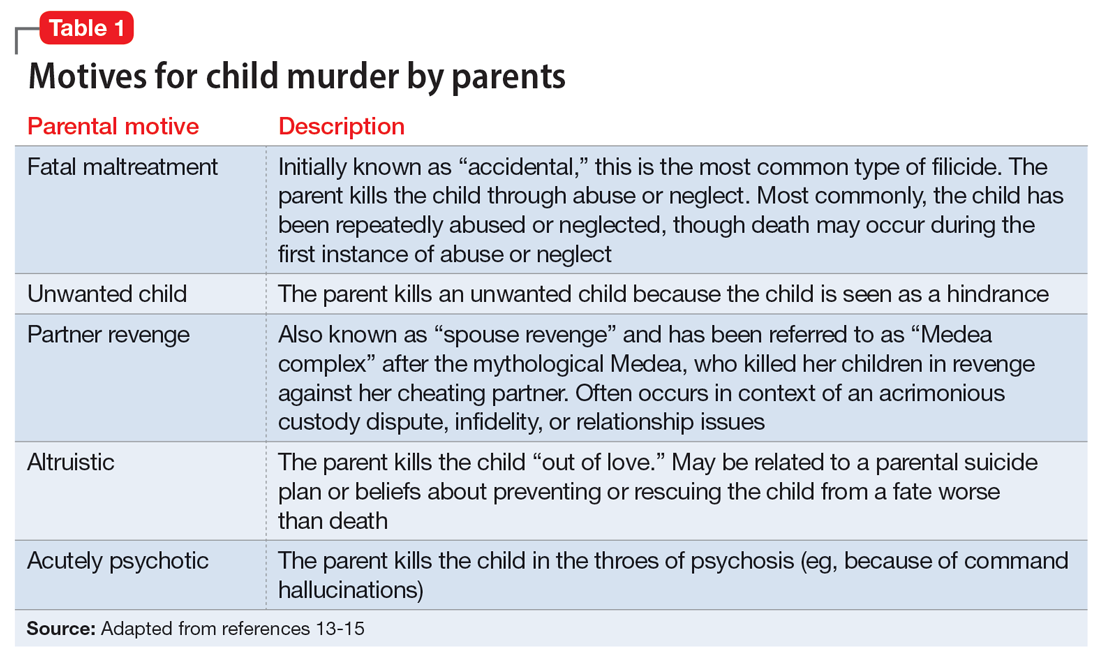
Fathers and mothers have a similar set of motives for killing their child (Table 113-15). Motives are critical to understand not only within forensics, but also for prevention. In performing assessments after a filicide, forensic psychiatrists must be mindful of gender bias.7,16 Resnick15 initially described 5 motives based on his 1969 review of the world literature. Our work5,17 has subsequently further explored these motives.
In child homicides from “fatal maltreatment,” the child has often been a chronic victim of abuse or neglect. National American data indicate that approximately 2 per 100,000 children are killed from child maltreatment annually. Of note in conceptualizing prevention, out of the same population of 100,000, there will be 471 referrals to Child Protective Services and 91 substantiated cases.18 However, only a minority of children who die from maltreatment had previous Child Protective Services involvement. While a child may be killed by fatal maltreatment at any age, one-half are younger than age 1, and three-quarters are younger than age 3.18 In rare cases, a parent who engages in medical child abuse (including factitious disorder imposed upon another) kills the child. Depending on the location and whether or not the death appeared to be intended, parents who kill because of fatal maltreatment might face charges of various levels of murder or manslaughter.
“Unwanted child” homicides occur when the parent has determined that they do not want to have the child, especially in comparison to another need or want. Unwanted child motive is the most common in neonaticide cases, occurring after a hidden pregnancy.4
Continue to: In "partner revenge" cases...
In “partner revenge” cases, parenting disputes, a custody battle, infidelity, or a difficult relationship breakup is often present. The parent wants to make the other parent suffer, and does so by killing their child. A parent may make statements such as “If I can’t have [the child], no one can,” and the child is used as a pawn.
In the final 2 motives—“altruistic” and “acutely psychotic”—mental illness is common. These are the populations we tend to find in samples of filicide-suicide cases where the parent has killed themselves and their child, and those found not guilty by reason of insanity.5,17 Altruistic filicide has been described as “murder out of love.” How can a parent kill their child out of love? Our research has shown several ways. First, the parent may be severely depressed and suicidal. They may be planning their own suicide, and as a parent who loves their child, they plan to take their child with them in death and not leave them alone in the “cruel world” that they themselves are departing. Or the parent may believe they are killing the child out of love to prevent or relieve the child’s suffering. The psychotic parent may believe that a terrible fate will befall their child, and they are killing them “gently.” For example, the parent may believe the child will be tortured or sex trafficked. Some parents may believe that their child has a devastating disease and think they would be better off dead. (Similar thinking of misguided altruism is seen in some cases of intimate partner homicide among older adults.19)
Alternatively, in rare cases of acutely psychotic filicide, parents with psychosis kill their child with no comprehensible motive. For example, they may be in a postictal state or may hear a command hallucination from God in the context of their psychosis.15
Myths vs realities of filicide
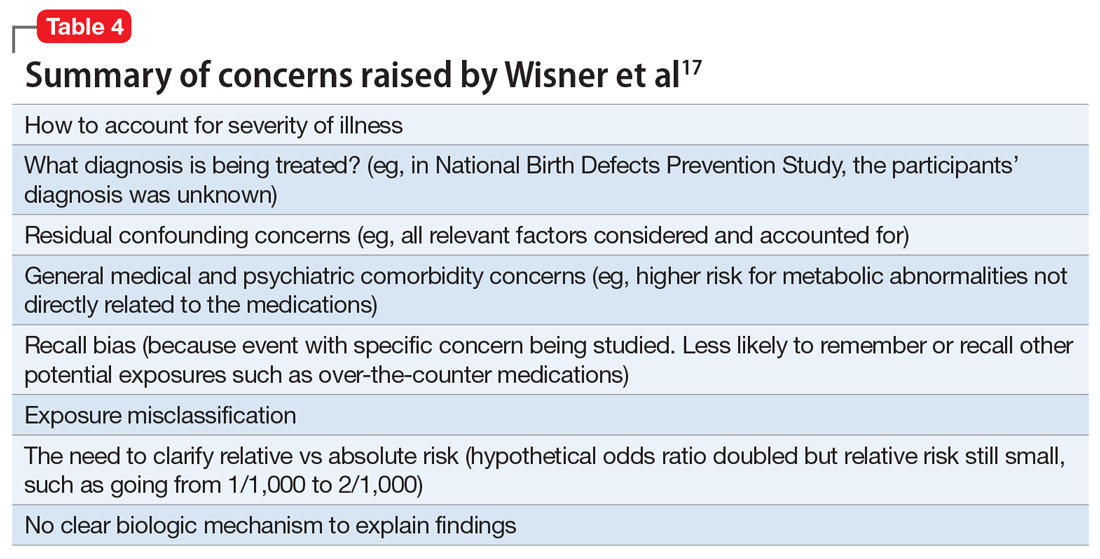
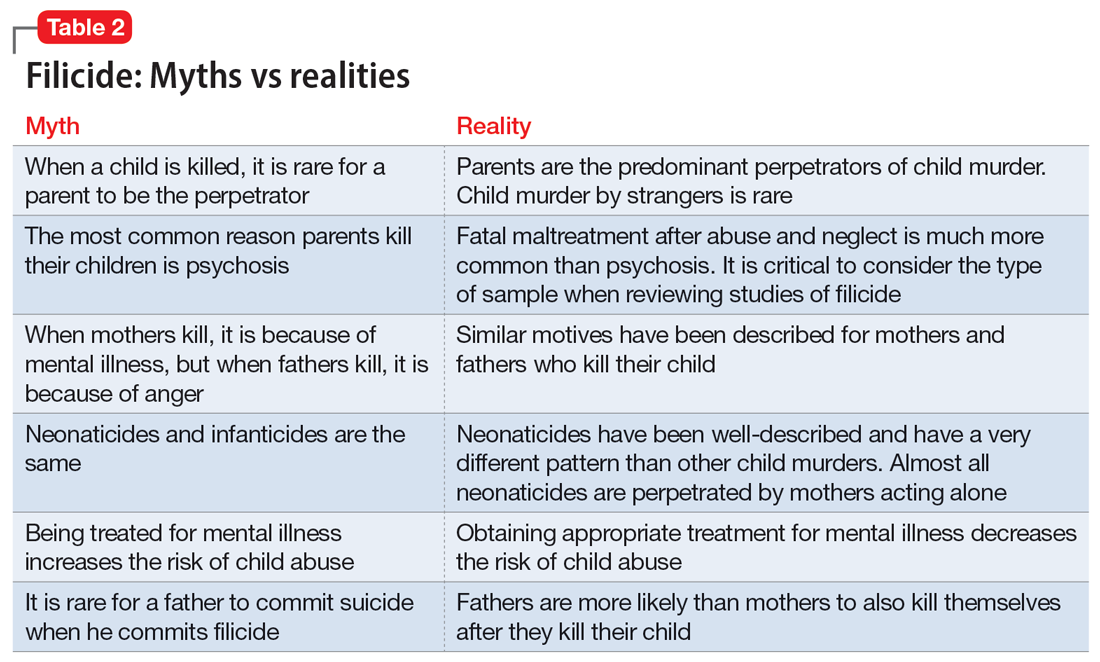
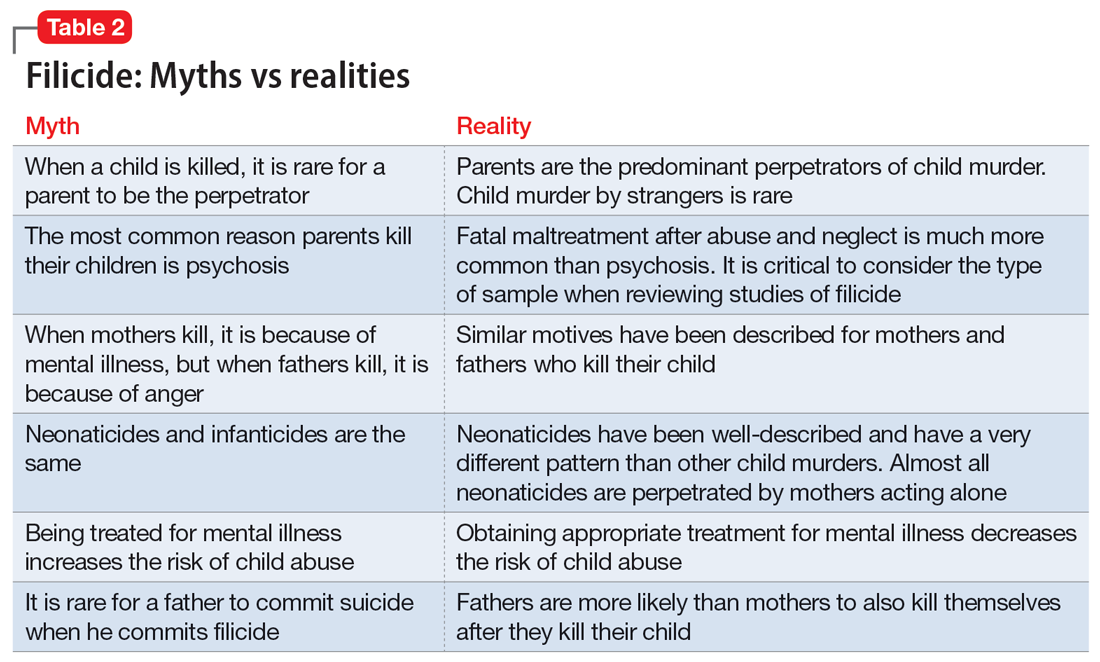
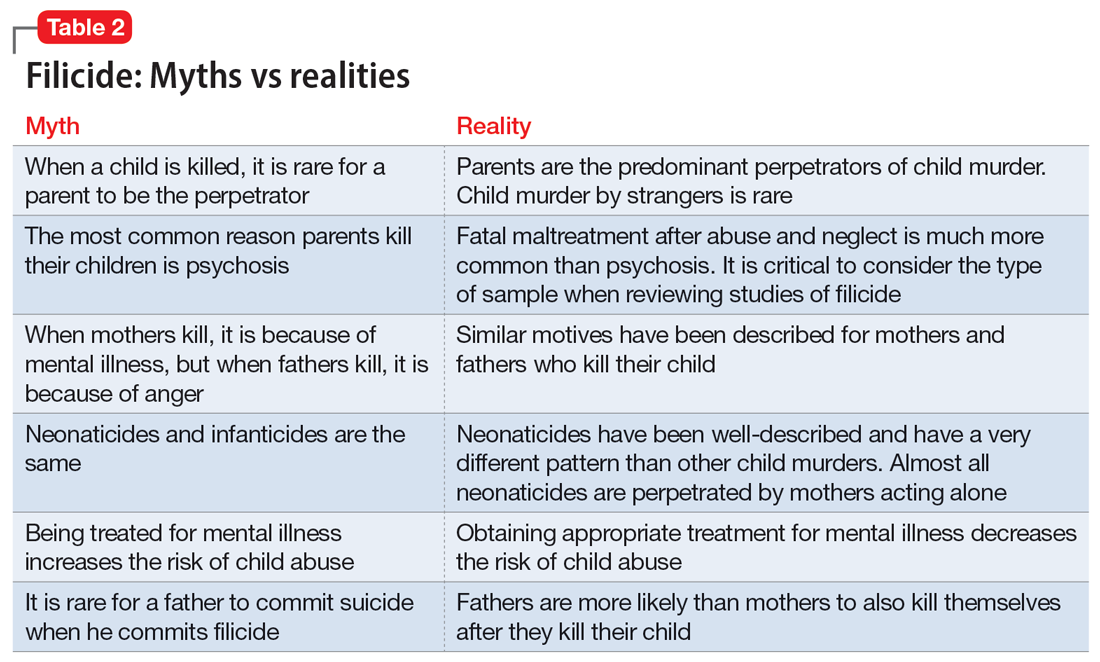
Common myths vs the realities of filicide are noted in Table 2. There are issues with believing these myths. For example, if we believe that most parents who kill their child have mental illness, this conflates mental illness and child homicide in our minds as well as the mind of the public. This can lead to further stigmatization of mental illness, and a lack of help-seeking behaviors because parents experiencing psychiatric symptoms may be afraid that if they report their symptoms, their child will be removed by Child Protective Services. However, treated mental illness decreases the risks of child abuse, similar to how treating mental illness decreases risks of other types of violence.20,21
Focusing on prevention
On a local level, we need to understand these tragedies to better understand prevention. To this end, across the United States, counties have Child Fatality Review teams.22 These teams are a partnership across sectors and disciplines, including professionals from health services, law enforcement, and social services—among others—working together to understand cases and consider preventive strategies and additional services needed within our communities.
Continue to: When conceptualizing prevention...
When conceptualizing prevention of child murder by parents, we can think of primary, secondary, and tertiary prevention. This means we want to encourage healthy families and healthy relationships within the family, as well as screening for risk and targeting interventions for families that have experienced difficulties, as well as for parents who have mental illness or substance use disorders.
Understanding the motive behind an individual committing filicide is also critical so that we do not conflate filicide and mental illness. Conflating these concepts leads to increased stigmatization and less help-seeking behavior.
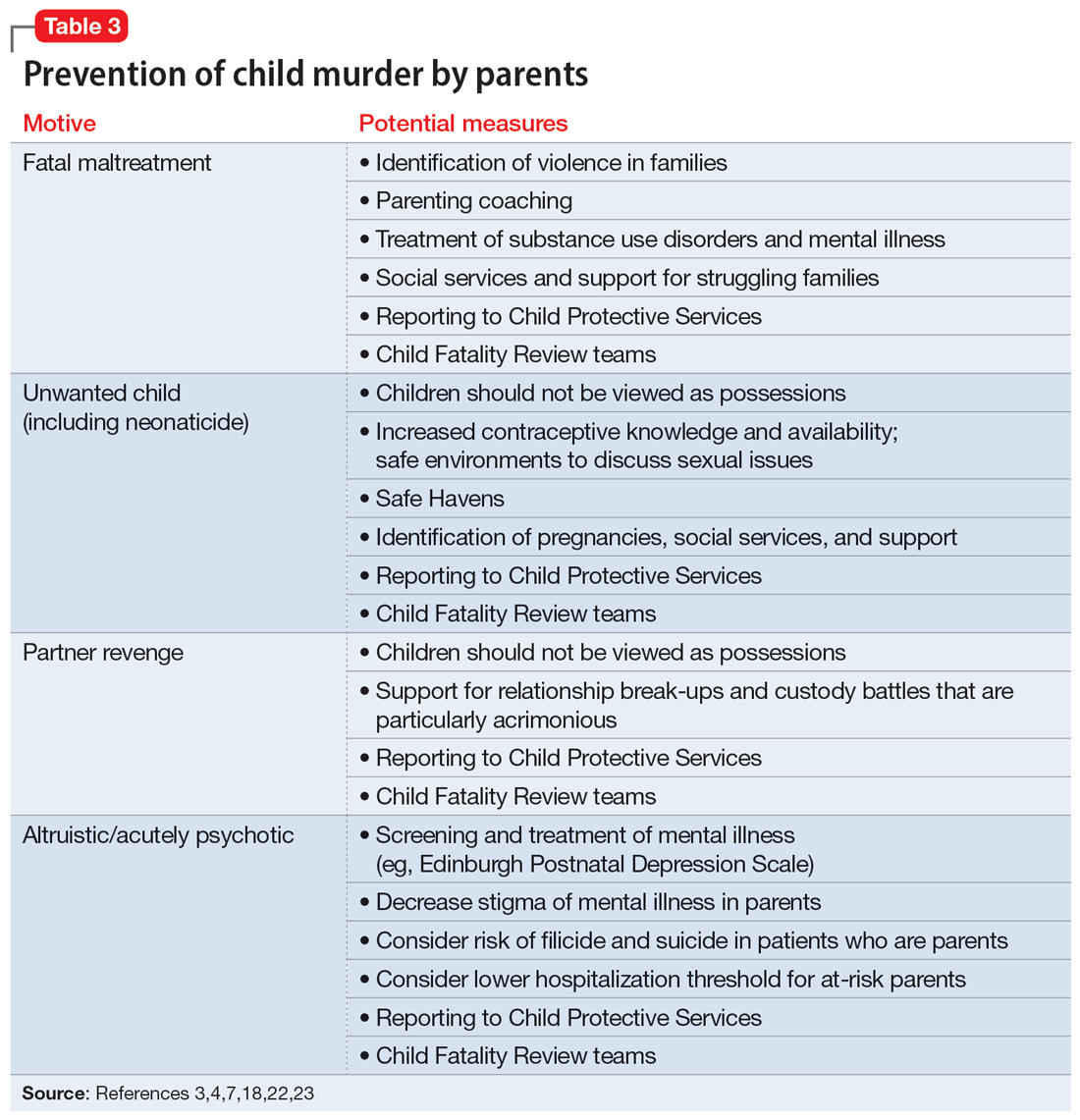
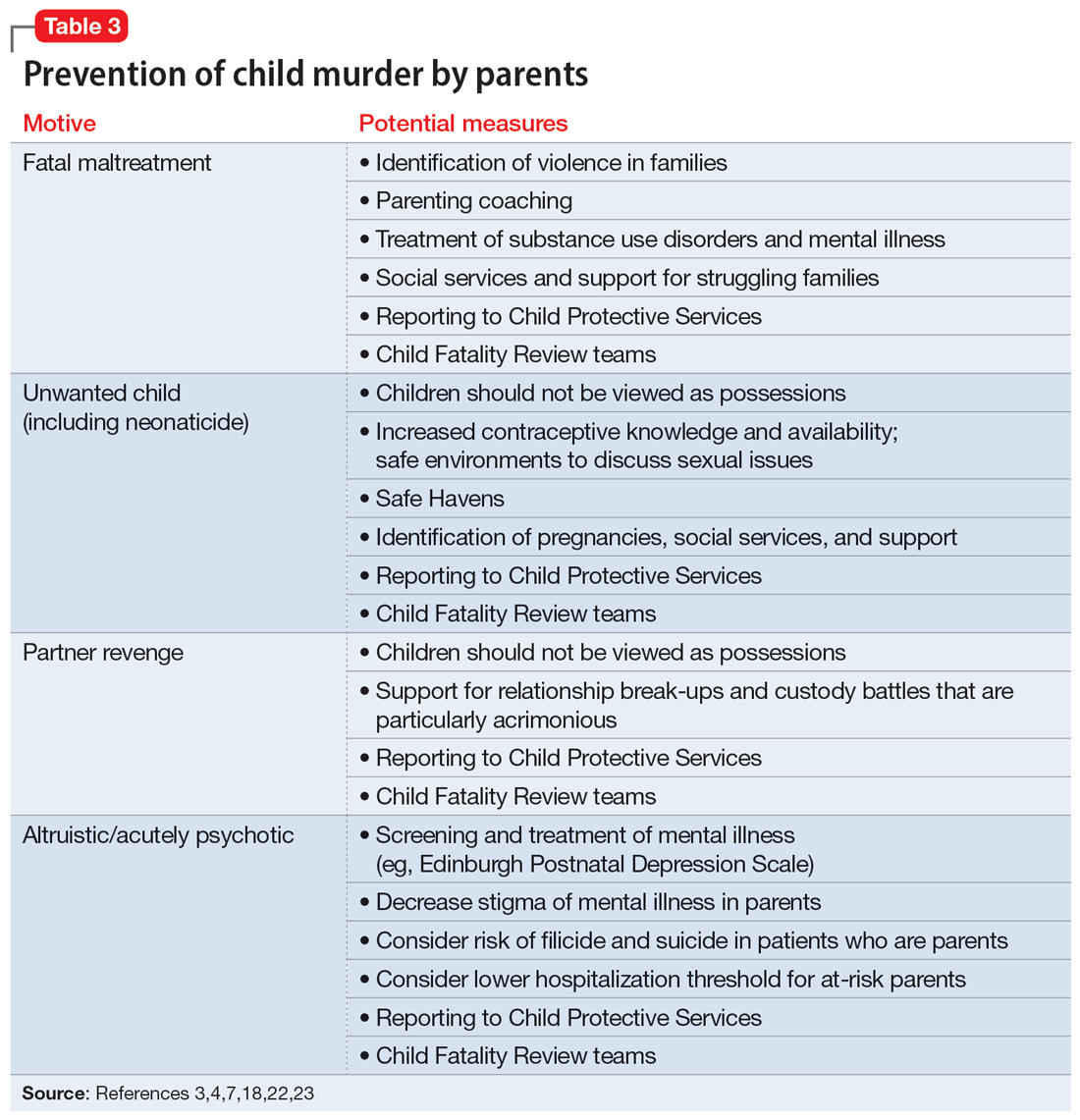
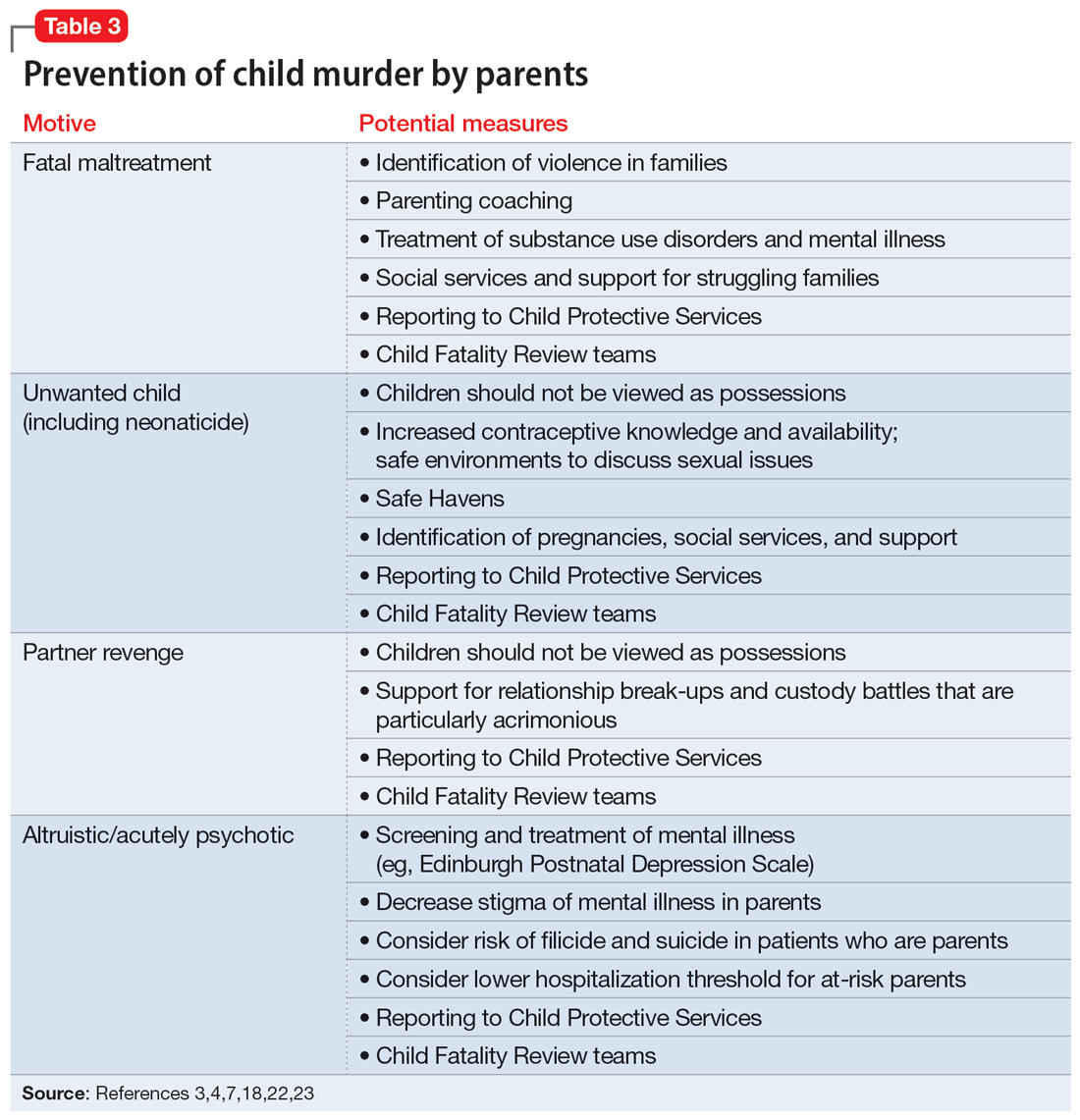
Table 33,4,7,18,22,23 describes the importance of understanding the motives for child murder by a parent in order to conceptualize appropriate prevention. Prevention efforts for 1 type of child murder will not necessarily help prevent murders that occur due to the other motives. Regarding prevention for fatal maltreatment cases, poor parenting skills, including inappropriate expressions of discipline, anger, and frustration, are common. In some cases, substance abuse is involved or the parent was acutely mentally unwell. Reporting to Child Protective Services can be helpful, but as previously noted, it is difficult to ascertain which cases will lead to a homicide. Recommendations from Child Fatality Review teams also are valuable.
Though many parents have frustrations with their children or thoughts of child harm, the act of filicide is rare, and individual cases may be difficult to predict. Regarding prediction, some mothers who committed filicide saw their psychiatrist within days to weeks before the murders.17 A small New Zealand study found that psychotic mothers reported no plans for killing their children in advance, whereas depressed mothers had contemplated the killing for days to weeks.24
Several studies have asked mothers about thoughts of harming their child. Among mothers with colicky infants, 70% reported “explicit aggressive thoughts and fantasies” while 26% had “infanticidal thoughts” during a colic episode.25 Another study26 found that among depressed mothers of infants and toddlers, 41% revealed thoughts of harming their child. Women with postpartum depression preferred not to share infanticidal thoughts with their doctor but were more likely to disclose that they were having suicidal thoughts in order to get needed help.27 Psychiatrists need to feel comfortable asking mothers about their coping skills, their suicidal thoughts, and their filicidal thoughts.14,23,28 Screening and treatment of mental illness is critical. Postpartum psychosis is well-known to pose an elevated risk of filicide and suicide.23 Obsessive-compulsive disorder may cause a parent to ruminate over ego-dystonic child harm but should be treated and the risk conceptualized very differently than in postpartum psychosis.23,29 Screening for postpartum depression and appropriate treatment of depression during pregnancy and the postpartum period decrease risk.30
Continue to: Regarding prevention of neonaticide...
Regarding prevention of neonaticide, Safe Haven laws, baby boxes, anonymous birth options, and increased contraceptive information and availability can help decrease the risk of this well-defined type of homicide.4 Safe Haven laws originated from Child Fatality Review teams.24 Though each state has its own variation, in general, parents can drop off an unharmed unwanted infant into Safe Havens in their state, which may include hospitals, police stations, or fire stations. In general, the mother remains anonymous and has immunity from prosecution for (safe) abandonment. There are drawbacks, such as lack of information regarding adoption and paternal rights. Safe Haven laws do not prevent all deaths and all unsafe abandonments. Baby boxes and baby hatches are used in various nations, including in Europe, and in some places have been used for centuries. In anonymous birth options, such as in France, a mother is not identified but is able to give birth at a hospital. This can decrease the risk from unattended delivery, but many women with denial of pregnancy report that they did not realize when they were about to give birth.4
Bottom Line
Knowledge about the intersection of mental illness and filicide can help in prevention. Parents who experience mental health concerns should be encouraged to obtain needed treatment, which aids prevention. However, many other factors elevate the risk of child murder by parents.
Related Resources
- National Center for Fatality Review and Prevention. https://ncfrp.org/
- Child Welfare Information Gateway. https://www.childwelfare.gov/topics/preventing/overview/federal-agencies/
1. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psych. 2005;162(9):1578-1587.
2. Mariano TY, Chan HC, Myers WC. Toward a more holistic understanding of filicide: a multidisciplinary analysis of 32 years of US arrest data [published corrections appears in Forensic Sci Int. 2014;245:92-94]. Forensic Sci Int. 2014;236:46-53.
3. Hatters Friedman S, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
4. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. 2009;32(1):43-47.
5. Hatters Friedman S, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
6. Daly M, Wilson M. Is the “Cinderella effect” controversial? A case study of evolution-minded research and critiques thereof. In: Crawford C, Krebs D, eds. Foundations of Evolutionary Psychology. Taylor & Francis Group/Lawrence Erlbaum Associates; 2008:383-400.
7. Friedman SH. Fathers and filicide: Mental illness and outcomes. In: Wong G, Parnham G, eds. Infanticide and Filicide: Foundations in Maternal Mental Health Forensics. 1st ed. American Psychiatric Association Publishing; 2020:85-107.
8. West SG, Friedman SH, Resnick PJ. Fathers who kill their children: an analysis of the literature. J Forensic Sci. 2009;54(2):463-468.
9. Putkonen H, Amon S, Eronen M, et al. Gender differences in filicide offense characteristics--a comprehensive register-based study of child murder in two European countries. Child Abuse Neglect. 2011;35(5):319-328.
10. Miller LJ. Denial of pregnancy. In: Spinelli MG, ed. Infanticide: Psychosocial and Legal Perspectives on Mothers Who Kill. American Psychiatric Association Publishing; 2003:81-104.
11. Friedman SH, Heneghan A, Rosenthal M. Characteristics of women who deny or conceal pregnancy. Psychosomatics. 2007;48(2):117-122.
12. Beyer K, Mack SM, Shelton JL. Investigative analysis of neonaticide: an exploratory study. Criminal Justice and Behavior. 2008;35(4):522-535.
13. Putkonen H, Weizmann-Henelius G, Collander J, et al. Neonaticides may be more preventable and heterogeneous than previously thought--neonaticides in Finland 1980-2000. Arch Womens Ment Health. 2007;10(1):15-23.
14. Friedman SH, Resnick PJ. Child murder and mental illness in parents: implications for psychiatrists. J Clin Psychiatry. 2011;72(5):587-588.
15. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126(3):325-334.
16. Friedman SH. Searching for the whole truth: considering culture and gender in forensic psychiatric practice. J Am Acad Psychiatry Law. 2023;51(1):23-34.
17. Friedman SH, Hrouda DR, Holden CE, et al. Child murder committed by severely mentally ill mothers: an examination of mothers found not guilty by reason of insanity. J Forensic Sci. 2005;50(6):1466-1471.
18. Ash P. Fatal maltreatment and child abuse turned to murder. In: Friedman SH, ed. Family Murder: Pathologies of Love and Hate. Group for the Advancement Psychiatry; 2018.
19. Friedman SH, Appel JM. Murder in the family: intimate partner homicide in the elderly. Psychiatric News. 2018. Accessed April 8, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a21
20. Friedman SH, McEwan MV. Treated mental illness and the risk of child abuse perpetration. Psychiatr Serv. 2018;69(2):211-216.
21. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
22. Hatters Friedman S, Beaman JW, Friedman JB. Fatality review and the role of the forensic psychiatrist. J Am Acad Psychiatry Law. 2021;49(3):396-405.
23. Friedman SH, Prakash C, Nagle-Yang S. Postpartum psychosis: protecting mother and infant. Current Psychiatry. 2019;18(4):12-21.
24. Stanton J, Simpson AI, Wouldes T. A qualitative study of filicide by mentally ill mothers. Child Abuse Negl. 2000;24(11):1451-1460.
25. Levitzky S, Cooper R. Infant colic syndrome—maternal fantasies of aggression and infanticide. Clin Pediatr (Phila). 2000;39(7):395-400.
26. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
27. Barr JA, Beck CT. Infanticide secrets: qualitative study on postpartum depression. Can Fam Physician. 2008;54(12):1716-1717.e5.
28. Friedman SH, Sorrentino RM, Stankowski JE, et al. Psychiatrists’ knowledge about maternal filicidal thoughts. Compr Psychiatry. 2008;49(1):106-110.
29. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
30. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20(8):30-36.
Deaths of children who are killed by their parents often make the news. Cases of maternal infanticide may be particularly shocking, since women are expected to be selfless nurturers. Yet when a child is murdered, the most common perpetrator is their parent, and mothers and fathers kill at similar rates.1
As psychiatrists, we may see these cases in the news and worry about the risks of our own patients killing their children. In approximately 500 cases annually, an American parent is arrested for the homicide of their child.2 This is not even the entire story, since a large percentage of such cases end in suicide—and no arrest. This article reviews the reasons parents kill their children, and considers common characteristics of these parents, dispelling some myths, before discussing the importance of prevention efforts.
Types of child murder by parents
Child murder by parents is termed filicide. Infanticide has various meanings but often refers to the murder of a child younger than age 1. Approximately 2 dozen nations (but not the United States) have Infanticide Acts that decrease the penalty for mothers who kill their young child.3 Neonaticide refers to murder of the infant at birth or in the first day of life.4
Epidemiology and common characteristics
Approximately 15%—or 1 in 7 murders with an arrest—is a filicide.2 The younger the child, the greater the risk, but older children are killed as well.2 Internationally, fathers and mothers are found to kill at similar rates. For other types of homicide, offenders are overwhelmingly male. This makes child murder by parents the singular type of murder in which women and men perpetrate in equal numbers. Fathers are more likely than mothers to also commit suicide after they kill their children.5 The “Cinderella effect” refers to the elevated risk of a stepchild being killed compared to the risk for a biological child.6
In the general international population, mothers who commit filicide tend to have multiple stressors and limited resources. They may be socially isolated and may be victims themselves as well as potentially experiencing substance abuse.1 Some mothers view the child they killed as abnormal.
Less research has been conducted about fathers who kill. Fathers are more likely to also commit partner homicide.5,7 They are more likely to complete filicide-suicide and use firearms or other violent means.5,7-9 Fathers may have a history of violence, substance abuse, and/or mental illness.7
Neonaticide
Mothers are the most common perpetrator of neonaticide.4 It is unusual for a father to be involved in a neonaticide, or for the father and mother to perpetrate the act together. Rates of neonaticide are considered underestimates because of the number of hidden pregnancies, hidden corpses, and the difficulty that forensic pathologists may have in determining whether a baby was born alive or dead.
Continue to: Perpetrators of neonaticide...
Perpetrators of neonaticide tend to be single, relatively young women acting alone. They often live with their parents and are fearful of the repercussions of being pregnant. Pregnancies are often hidden, with no prenatal care. This includes both denial and concealment of pregnancy.4 Perpetrators of neonaticide commonly lack a premorbid serious mental illness, though after the homicide they may develop anxiety, depression, posttraumatic stress disorder (PTSD), or adjustment disorder.4 (Individuals who unwittingly find a murdered baby’s corpse may also be at risk of PTSD.)
Hidden pregnancies may be due to concealment or denial of pregnancy.10,11 Concealment of pregnancy involves a woman knowing she is pregnant, but purposely hiding from others. Concealment may occur after a period of denial of pregnancy. Denial of pregnancy has several subtypes: pervasive denial, affective denial, and psychotic denial. In cases of pervasive denial, the existence of the pregnancy and the pregnancy’s emotional significance is outside the woman’s awareness. Alternatively, in affective denial, she is intellectually aware that she is pregnant but makes little emotional or physical preparation. In the rarest form, psychotic denial, a woman with a psychotic disorder such as schizophrenia may intermittently deny her pregnancy. This may be correlated with a history of custody loss.10,11 Unlike denial of other medical conditions, in cases of denial of pregnancy, there will exist a very specific point in time (delivery) when the reality of the baby confronts the woman. Risks in cases of hidden pregnancies include those from lack of prenatal care and an assisted delivery as well as neonaticide. An FBI study12 of law enforcement files found most neonaticide offenders were single young women with no criminal or psychological history. A caveat is that in the rare cases in which a woman with psychotic illness commits neonaticide, she may have different characteristics from those generally reported.13
Motives
Fathers and mothers have a similar set of motives for killing their child (Table 113-15). Motives are critical to understand not only within forensics, but also for prevention. In performing assessments after a filicide, forensic psychiatrists must be mindful of gender bias.7,16 Resnick15 initially described 5 motives based on his 1969 review of the world literature. Our work5,17 has subsequently further explored these motives.
In child homicides from “fatal maltreatment,” the child has often been a chronic victim of abuse or neglect. National American data indicate that approximately 2 per 100,000 children are killed from child maltreatment annually. Of note in conceptualizing prevention, out of the same population of 100,000, there will be 471 referrals to Child Protective Services and 91 substantiated cases.18 However, only a minority of children who die from maltreatment had previous Child Protective Services involvement. While a child may be killed by fatal maltreatment at any age, one-half are younger than age 1, and three-quarters are younger than age 3.18 In rare cases, a parent who engages in medical child abuse (including factitious disorder imposed upon another) kills the child. Depending on the location and whether or not the death appeared to be intended, parents who kill because of fatal maltreatment might face charges of various levels of murder or manslaughter.
“Unwanted child” homicides occur when the parent has determined that they do not want to have the child, especially in comparison to another need or want. Unwanted child motive is the most common in neonaticide cases, occurring after a hidden pregnancy.4
Continue to: In "partner revenge" cases...
In “partner revenge” cases, parenting disputes, a custody battle, infidelity, or a difficult relationship breakup is often present. The parent wants to make the other parent suffer, and does so by killing their child. A parent may make statements such as “If I can’t have [the child], no one can,” and the child is used as a pawn.
In the final 2 motives—“altruistic” and “acutely psychotic”—mental illness is common. These are the populations we tend to find in samples of filicide-suicide cases where the parent has killed themselves and their child, and those found not guilty by reason of insanity.5,17 Altruistic filicide has been described as “murder out of love.” How can a parent kill their child out of love? Our research has shown several ways. First, the parent may be severely depressed and suicidal. They may be planning their own suicide, and as a parent who loves their child, they plan to take their child with them in death and not leave them alone in the “cruel world” that they themselves are departing. Or the parent may believe they are killing the child out of love to prevent or relieve the child’s suffering. The psychotic parent may believe that a terrible fate will befall their child, and they are killing them “gently.” For example, the parent may believe the child will be tortured or sex trafficked. Some parents may believe that their child has a devastating disease and think they would be better off dead. (Similar thinking of misguided altruism is seen in some cases of intimate partner homicide among older adults.19)
Alternatively, in rare cases of acutely psychotic filicide, parents with psychosis kill their child with no comprehensible motive. For example, they may be in a postictal state or may hear a command hallucination from God in the context of their psychosis.15
Myths vs realities of filicide
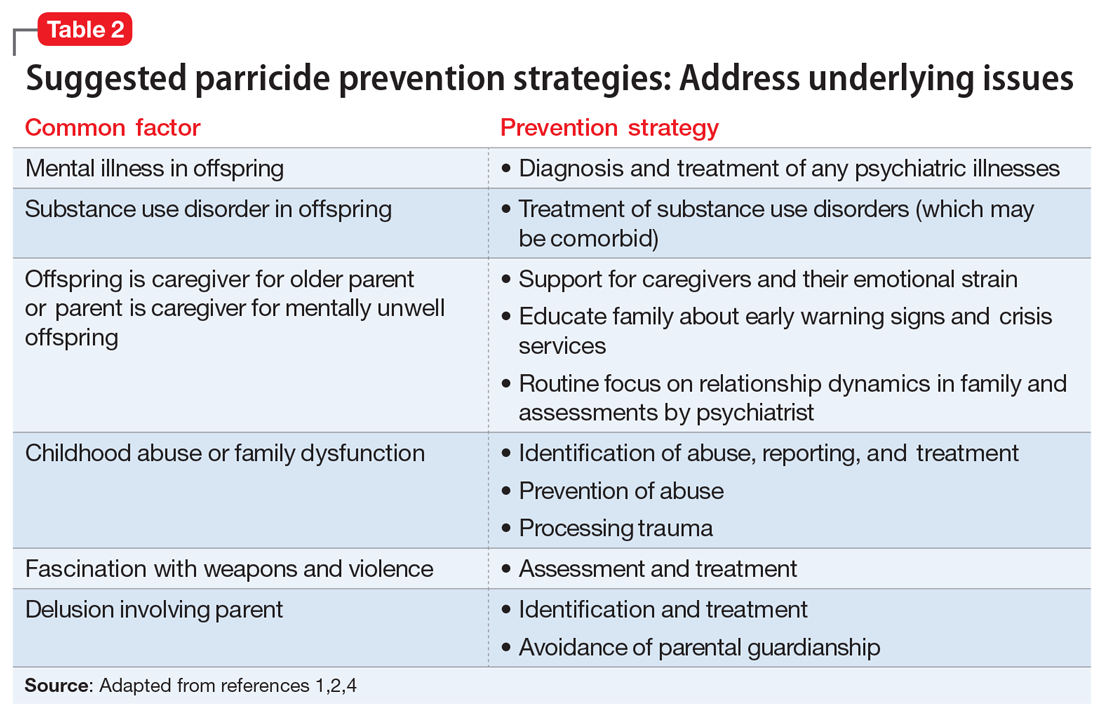
Common myths vs the realities of filicide are noted in Table 2. There are issues with believing these myths. For example, if we believe that most parents who kill their child have mental illness, this conflates mental illness and child homicide in our minds as well as the mind of the public. This can lead to further stigmatization of mental illness, and a lack of help-seeking behaviors because parents experiencing psychiatric symptoms may be afraid that if they report their symptoms, their child will be removed by Child Protective Services. However, treated mental illness decreases the risks of child abuse, similar to how treating mental illness decreases risks of other types of violence.20,21
Focusing on prevention
On a local level, we need to understand these tragedies to better understand prevention. To this end, across the United States, counties have Child Fatality Review teams.22 These teams are a partnership across sectors and disciplines, including professionals from health services, law enforcement, and social services—among others—working together to understand cases and consider preventive strategies and additional services needed within our communities.
Continue to: When conceptualizing prevention...
When conceptualizing prevention of child murder by parents, we can think of primary, secondary, and tertiary prevention. This means we want to encourage healthy families and healthy relationships within the family, as well as screening for risk and targeting interventions for families that have experienced difficulties, as well as for parents who have mental illness or substance use disorders.
Understanding the motive behind an individual committing filicide is also critical so that we do not conflate filicide and mental illness. Conflating these concepts leads to increased stigmatization and less help-seeking behavior.
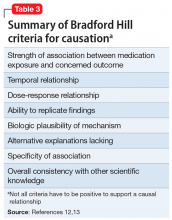
Table 33,4,7,18,22,23 describes the importance of understanding the motives for child murder by a parent in order to conceptualize appropriate prevention. Prevention efforts for 1 type of child murder will not necessarily help prevent murders that occur due to the other motives. Regarding prevention for fatal maltreatment cases, poor parenting skills, including inappropriate expressions of discipline, anger, and frustration, are common. In some cases, substance abuse is involved or the parent was acutely mentally unwell. Reporting to Child Protective Services can be helpful, but as previously noted, it is difficult to ascertain which cases will lead to a homicide. Recommendations from Child Fatality Review teams also are valuable.
Though many parents have frustrations with their children or thoughts of child harm, the act of filicide is rare, and individual cases may be difficult to predict. Regarding prediction, some mothers who committed filicide saw their psychiatrist within days to weeks before the murders.17 A small New Zealand study found that psychotic mothers reported no plans for killing their children in advance, whereas depressed mothers had contemplated the killing for days to weeks.24
Several studies have asked mothers about thoughts of harming their child. Among mothers with colicky infants, 70% reported “explicit aggressive thoughts and fantasies” while 26% had “infanticidal thoughts” during a colic episode.25 Another study26 found that among depressed mothers of infants and toddlers, 41% revealed thoughts of harming their child. Women with postpartum depression preferred not to share infanticidal thoughts with their doctor but were more likely to disclose that they were having suicidal thoughts in order to get needed help.27 Psychiatrists need to feel comfortable asking mothers about their coping skills, their suicidal thoughts, and their filicidal thoughts.14,23,28 Screening and treatment of mental illness is critical. Postpartum psychosis is well-known to pose an elevated risk of filicide and suicide.23 Obsessive-compulsive disorder may cause a parent to ruminate over ego-dystonic child harm but should be treated and the risk conceptualized very differently than in postpartum psychosis.23,29 Screening for postpartum depression and appropriate treatment of depression during pregnancy and the postpartum period decrease risk.30
Continue to: Regarding prevention of neonaticide...
Regarding prevention of neonaticide, Safe Haven laws, baby boxes, anonymous birth options, and increased contraceptive information and availability can help decrease the risk of this well-defined type of homicide.4 Safe Haven laws originated from Child Fatality Review teams.24 Though each state has its own variation, in general, parents can drop off an unharmed unwanted infant into Safe Havens in their state, which may include hospitals, police stations, or fire stations. In general, the mother remains anonymous and has immunity from prosecution for (safe) abandonment. There are drawbacks, such as lack of information regarding adoption and paternal rights. Safe Haven laws do not prevent all deaths and all unsafe abandonments. Baby boxes and baby hatches are used in various nations, including in Europe, and in some places have been used for centuries. In anonymous birth options, such as in France, a mother is not identified but is able to give birth at a hospital. This can decrease the risk from unattended delivery, but many women with denial of pregnancy report that they did not realize when they were about to give birth.4
Bottom Line
Knowledge about the intersection of mental illness and filicide can help in prevention. Parents who experience mental health concerns should be encouraged to obtain needed treatment, which aids prevention. However, many other factors elevate the risk of child murder by parents.
Related Resources
- National Center for Fatality Review and Prevention. https://ncfrp.org/
- Child Welfare Information Gateway. https://www.childwelfare.gov/topics/preventing/overview/federal-agencies/
Deaths of children who are killed by their parents often make the news. Cases of maternal infanticide may be particularly shocking, since women are expected to be selfless nurturers. Yet when a child is murdered, the most common perpetrator is their parent, and mothers and fathers kill at similar rates.1
As psychiatrists, we may see these cases in the news and worry about the risks of our own patients killing their children. In approximately 500 cases annually, an American parent is arrested for the homicide of their child.2 This is not even the entire story, since a large percentage of such cases end in suicide—and no arrest. This article reviews the reasons parents kill their children, and considers common characteristics of these parents, dispelling some myths, before discussing the importance of prevention efforts.
Types of child murder by parents
Child murder by parents is termed filicide. Infanticide has various meanings but often refers to the murder of a child younger than age 1. Approximately 2 dozen nations (but not the United States) have Infanticide Acts that decrease the penalty for mothers who kill their young child.3 Neonaticide refers to murder of the infant at birth or in the first day of life.4
Epidemiology and common characteristics
Approximately 15%—or 1 in 7 murders with an arrest—is a filicide.2 The younger the child, the greater the risk, but older children are killed as well.2 Internationally, fathers and mothers are found to kill at similar rates. For other types of homicide, offenders are overwhelmingly male. This makes child murder by parents the singular type of murder in which women and men perpetrate in equal numbers. Fathers are more likely than mothers to also commit suicide after they kill their children.5 The “Cinderella effect” refers to the elevated risk of a stepchild being killed compared to the risk for a biological child.6
In the general international population, mothers who commit filicide tend to have multiple stressors and limited resources. They may be socially isolated and may be victims themselves as well as potentially experiencing substance abuse.1 Some mothers view the child they killed as abnormal.
Less research has been conducted about fathers who kill. Fathers are more likely to also commit partner homicide.5,7 They are more likely to complete filicide-suicide and use firearms or other violent means.5,7-9 Fathers may have a history of violence, substance abuse, and/or mental illness.7
Neonaticide
Mothers are the most common perpetrator of neonaticide.4 It is unusual for a father to be involved in a neonaticide, or for the father and mother to perpetrate the act together. Rates of neonaticide are considered underestimates because of the number of hidden pregnancies, hidden corpses, and the difficulty that forensic pathologists may have in determining whether a baby was born alive or dead.
Continue to: Perpetrators of neonaticide...
Perpetrators of neonaticide tend to be single, relatively young women acting alone. They often live with their parents and are fearful of the repercussions of being pregnant. Pregnancies are often hidden, with no prenatal care. This includes both denial and concealment of pregnancy.4 Perpetrators of neonaticide commonly lack a premorbid serious mental illness, though after the homicide they may develop anxiety, depression, posttraumatic stress disorder (PTSD), or adjustment disorder.4 (Individuals who unwittingly find a murdered baby’s corpse may also be at risk of PTSD.)
Hidden pregnancies may be due to concealment or denial of pregnancy.10,11 Concealment of pregnancy involves a woman knowing she is pregnant, but purposely hiding from others. Concealment may occur after a period of denial of pregnancy. Denial of pregnancy has several subtypes: pervasive denial, affective denial, and psychotic denial. In cases of pervasive denial, the existence of the pregnancy and the pregnancy’s emotional significance is outside the woman’s awareness. Alternatively, in affective denial, she is intellectually aware that she is pregnant but makes little emotional or physical preparation. In the rarest form, psychotic denial, a woman with a psychotic disorder such as schizophrenia may intermittently deny her pregnancy. This may be correlated with a history of custody loss.10,11 Unlike denial of other medical conditions, in cases of denial of pregnancy, there will exist a very specific point in time (delivery) when the reality of the baby confronts the woman. Risks in cases of hidden pregnancies include those from lack of prenatal care and an assisted delivery as well as neonaticide. An FBI study12 of law enforcement files found most neonaticide offenders were single young women with no criminal or psychological history. A caveat is that in the rare cases in which a woman with psychotic illness commits neonaticide, she may have different characteristics from those generally reported.13
Motives
Fathers and mothers have a similar set of motives for killing their child (Table 113-15). Motives are critical to understand not only within forensics, but also for prevention. In performing assessments after a filicide, forensic psychiatrists must be mindful of gender bias.7,16 Resnick15 initially described 5 motives based on his 1969 review of the world literature. Our work5,17 has subsequently further explored these motives.
In child homicides from “fatal maltreatment,” the child has often been a chronic victim of abuse or neglect. National American data indicate that approximately 2 per 100,000 children are killed from child maltreatment annually. Of note in conceptualizing prevention, out of the same population of 100,000, there will be 471 referrals to Child Protective Services and 91 substantiated cases.18 However, only a minority of children who die from maltreatment had previous Child Protective Services involvement. While a child may be killed by fatal maltreatment at any age, one-half are younger than age 1, and three-quarters are younger than age 3.18 In rare cases, a parent who engages in medical child abuse (including factitious disorder imposed upon another) kills the child. Depending on the location and whether or not the death appeared to be intended, parents who kill because of fatal maltreatment might face charges of various levels of murder or manslaughter.
“Unwanted child” homicides occur when the parent has determined that they do not want to have the child, especially in comparison to another need or want. Unwanted child motive is the most common in neonaticide cases, occurring after a hidden pregnancy.4
Continue to: In "partner revenge" cases...
In “partner revenge” cases, parenting disputes, a custody battle, infidelity, or a difficult relationship breakup is often present. The parent wants to make the other parent suffer, and does so by killing their child. A parent may make statements such as “If I can’t have [the child], no one can,” and the child is used as a pawn.
In the final 2 motives—“altruistic” and “acutely psychotic”—mental illness is common. These are the populations we tend to find in samples of filicide-suicide cases where the parent has killed themselves and their child, and those found not guilty by reason of insanity.5,17 Altruistic filicide has been described as “murder out of love.” How can a parent kill their child out of love? Our research has shown several ways. First, the parent may be severely depressed and suicidal. They may be planning their own suicide, and as a parent who loves their child, they plan to take their child with them in death and not leave them alone in the “cruel world” that they themselves are departing. Or the parent may believe they are killing the child out of love to prevent or relieve the child’s suffering. The psychotic parent may believe that a terrible fate will befall their child, and they are killing them “gently.” For example, the parent may believe the child will be tortured or sex trafficked. Some parents may believe that their child has a devastating disease and think they would be better off dead. (Similar thinking of misguided altruism is seen in some cases of intimate partner homicide among older adults.19)
Alternatively, in rare cases of acutely psychotic filicide, parents with psychosis kill their child with no comprehensible motive. For example, they may be in a postictal state or may hear a command hallucination from God in the context of their psychosis.15
Myths vs realities of filicide
Common myths vs the realities of filicide are noted in Table 2. There are issues with believing these myths. For example, if we believe that most parents who kill their child have mental illness, this conflates mental illness and child homicide in our minds as well as the mind of the public. This can lead to further stigmatization of mental illness, and a lack of help-seeking behaviors because parents experiencing psychiatric symptoms may be afraid that if they report their symptoms, their child will be removed by Child Protective Services. However, treated mental illness decreases the risks of child abuse, similar to how treating mental illness decreases risks of other types of violence.20,21
Focusing on prevention
On a local level, we need to understand these tragedies to better understand prevention. To this end, across the United States, counties have Child Fatality Review teams.22 These teams are a partnership across sectors and disciplines, including professionals from health services, law enforcement, and social services—among others—working together to understand cases and consider preventive strategies and additional services needed within our communities.
Continue to: When conceptualizing prevention...
When conceptualizing prevention of child murder by parents, we can think of primary, secondary, and tertiary prevention. This means we want to encourage healthy families and healthy relationships within the family, as well as screening for risk and targeting interventions for families that have experienced difficulties, as well as for parents who have mental illness or substance use disorders.
Understanding the motive behind an individual committing filicide is also critical so that we do not conflate filicide and mental illness. Conflating these concepts leads to increased stigmatization and less help-seeking behavior.
Table 33,4,7,18,22,23 describes the importance of understanding the motives for child murder by a parent in order to conceptualize appropriate prevention. Prevention efforts for 1 type of child murder will not necessarily help prevent murders that occur due to the other motives. Regarding prevention for fatal maltreatment cases, poor parenting skills, including inappropriate expressions of discipline, anger, and frustration, are common. In some cases, substance abuse is involved or the parent was acutely mentally unwell. Reporting to Child Protective Services can be helpful, but as previously noted, it is difficult to ascertain which cases will lead to a homicide. Recommendations from Child Fatality Review teams also are valuable.
Though many parents have frustrations with their children or thoughts of child harm, the act of filicide is rare, and individual cases may be difficult to predict. Regarding prediction, some mothers who committed filicide saw their psychiatrist within days to weeks before the murders.17 A small New Zealand study found that psychotic mothers reported no plans for killing their children in advance, whereas depressed mothers had contemplated the killing for days to weeks.24
Several studies have asked mothers about thoughts of harming their child. Among mothers with colicky infants, 70% reported “explicit aggressive thoughts and fantasies” while 26% had “infanticidal thoughts” during a colic episode.25 Another study26 found that among depressed mothers of infants and toddlers, 41% revealed thoughts of harming their child. Women with postpartum depression preferred not to share infanticidal thoughts with their doctor but were more likely to disclose that they were having suicidal thoughts in order to get needed help.27 Psychiatrists need to feel comfortable asking mothers about their coping skills, their suicidal thoughts, and their filicidal thoughts.14,23,28 Screening and treatment of mental illness is critical. Postpartum psychosis is well-known to pose an elevated risk of filicide and suicide.23 Obsessive-compulsive disorder may cause a parent to ruminate over ego-dystonic child harm but should be treated and the risk conceptualized very differently than in postpartum psychosis.23,29 Screening for postpartum depression and appropriate treatment of depression during pregnancy and the postpartum period decrease risk.30
Continue to: Regarding prevention of neonaticide...
Regarding prevention of neonaticide, Safe Haven laws, baby boxes, anonymous birth options, and increased contraceptive information and availability can help decrease the risk of this well-defined type of homicide.4 Safe Haven laws originated from Child Fatality Review teams.24 Though each state has its own variation, in general, parents can drop off an unharmed unwanted infant into Safe Havens in their state, which may include hospitals, police stations, or fire stations. In general, the mother remains anonymous and has immunity from prosecution for (safe) abandonment. There are drawbacks, such as lack of information regarding adoption and paternal rights. Safe Haven laws do not prevent all deaths and all unsafe abandonments. Baby boxes and baby hatches are used in various nations, including in Europe, and in some places have been used for centuries. In anonymous birth options, such as in France, a mother is not identified but is able to give birth at a hospital. This can decrease the risk from unattended delivery, but many women with denial of pregnancy report that they did not realize when they were about to give birth.4
Bottom Line
Knowledge about the intersection of mental illness and filicide can help in prevention. Parents who experience mental health concerns should be encouraged to obtain needed treatment, which aids prevention. However, many other factors elevate the risk of child murder by parents.
Related Resources
- National Center for Fatality Review and Prevention. https://ncfrp.org/
- Child Welfare Information Gateway. https://www.childwelfare.gov/topics/preventing/overview/federal-agencies/
1. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psych. 2005;162(9):1578-1587.
2. Mariano TY, Chan HC, Myers WC. Toward a more holistic understanding of filicide: a multidisciplinary analysis of 32 years of US arrest data [published corrections appears in Forensic Sci Int. 2014;245:92-94]. Forensic Sci Int. 2014;236:46-53.
3. Hatters Friedman S, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
4. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. 2009;32(1):43-47.
5. Hatters Friedman S, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
6. Daly M, Wilson M. Is the “Cinderella effect” controversial? A case study of evolution-minded research and critiques thereof. In: Crawford C, Krebs D, eds. Foundations of Evolutionary Psychology. Taylor & Francis Group/Lawrence Erlbaum Associates; 2008:383-400.
7. Friedman SH. Fathers and filicide: Mental illness and outcomes. In: Wong G, Parnham G, eds. Infanticide and Filicide: Foundations in Maternal Mental Health Forensics. 1st ed. American Psychiatric Association Publishing; 2020:85-107.
8. West SG, Friedman SH, Resnick PJ. Fathers who kill their children: an analysis of the literature. J Forensic Sci. 2009;54(2):463-468.
9. Putkonen H, Amon S, Eronen M, et al. Gender differences in filicide offense characteristics--a comprehensive register-based study of child murder in two European countries. Child Abuse Neglect. 2011;35(5):319-328.
10. Miller LJ. Denial of pregnancy. In: Spinelli MG, ed. Infanticide: Psychosocial and Legal Perspectives on Mothers Who Kill. American Psychiatric Association Publishing; 2003:81-104.
11. Friedman SH, Heneghan A, Rosenthal M. Characteristics of women who deny or conceal pregnancy. Psychosomatics. 2007;48(2):117-122.
12. Beyer K, Mack SM, Shelton JL. Investigative analysis of neonaticide: an exploratory study. Criminal Justice and Behavior. 2008;35(4):522-535.
13. Putkonen H, Weizmann-Henelius G, Collander J, et al. Neonaticides may be more preventable and heterogeneous than previously thought--neonaticides in Finland 1980-2000. Arch Womens Ment Health. 2007;10(1):15-23.
14. Friedman SH, Resnick PJ. Child murder and mental illness in parents: implications for psychiatrists. J Clin Psychiatry. 2011;72(5):587-588.
15. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126(3):325-334.
16. Friedman SH. Searching for the whole truth: considering culture and gender in forensic psychiatric practice. J Am Acad Psychiatry Law. 2023;51(1):23-34.
17. Friedman SH, Hrouda DR, Holden CE, et al. Child murder committed by severely mentally ill mothers: an examination of mothers found not guilty by reason of insanity. J Forensic Sci. 2005;50(6):1466-1471.
18. Ash P. Fatal maltreatment and child abuse turned to murder. In: Friedman SH, ed. Family Murder: Pathologies of Love and Hate. Group for the Advancement Psychiatry; 2018.
19. Friedman SH, Appel JM. Murder in the family: intimate partner homicide in the elderly. Psychiatric News. 2018. Accessed April 8, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a21
20. Friedman SH, McEwan MV. Treated mental illness and the risk of child abuse perpetration. Psychiatr Serv. 2018;69(2):211-216.
21. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
22. Hatters Friedman S, Beaman JW, Friedman JB. Fatality review and the role of the forensic psychiatrist. J Am Acad Psychiatry Law. 2021;49(3):396-405.
23. Friedman SH, Prakash C, Nagle-Yang S. Postpartum psychosis: protecting mother and infant. Current Psychiatry. 2019;18(4):12-21.
24. Stanton J, Simpson AI, Wouldes T. A qualitative study of filicide by mentally ill mothers. Child Abuse Negl. 2000;24(11):1451-1460.
25. Levitzky S, Cooper R. Infant colic syndrome—maternal fantasies of aggression and infanticide. Clin Pediatr (Phila). 2000;39(7):395-400.
26. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
27. Barr JA, Beck CT. Infanticide secrets: qualitative study on postpartum depression. Can Fam Physician. 2008;54(12):1716-1717.e5.
28. Friedman SH, Sorrentino RM, Stankowski JE, et al. Psychiatrists’ knowledge about maternal filicidal thoughts. Compr Psychiatry. 2008;49(1):106-110.
29. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
30. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20(8):30-36.
1. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psych. 2005;162(9):1578-1587.
2. Mariano TY, Chan HC, Myers WC. Toward a more holistic understanding of filicide: a multidisciplinary analysis of 32 years of US arrest data [published corrections appears in Forensic Sci Int. 2014;245:92-94]. Forensic Sci Int. 2014;236:46-53.
3. Hatters Friedman S, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
4. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. 2009;32(1):43-47.
5. Hatters Friedman S, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
6. Daly M, Wilson M. Is the “Cinderella effect” controversial? A case study of evolution-minded research and critiques thereof. In: Crawford C, Krebs D, eds. Foundations of Evolutionary Psychology. Taylor & Francis Group/Lawrence Erlbaum Associates; 2008:383-400.
7. Friedman SH. Fathers and filicide: Mental illness and outcomes. In: Wong G, Parnham G, eds. Infanticide and Filicide: Foundations in Maternal Mental Health Forensics. 1st ed. American Psychiatric Association Publishing; 2020:85-107.
8. West SG, Friedman SH, Resnick PJ. Fathers who kill their children: an analysis of the literature. J Forensic Sci. 2009;54(2):463-468.
9. Putkonen H, Amon S, Eronen M, et al. Gender differences in filicide offense characteristics--a comprehensive register-based study of child murder in two European countries. Child Abuse Neglect. 2011;35(5):319-328.
10. Miller LJ. Denial of pregnancy. In: Spinelli MG, ed. Infanticide: Psychosocial and Legal Perspectives on Mothers Who Kill. American Psychiatric Association Publishing; 2003:81-104.
11. Friedman SH, Heneghan A, Rosenthal M. Characteristics of women who deny or conceal pregnancy. Psychosomatics. 2007;48(2):117-122.
12. Beyer K, Mack SM, Shelton JL. Investigative analysis of neonaticide: an exploratory study. Criminal Justice and Behavior. 2008;35(4):522-535.
13. Putkonen H, Weizmann-Henelius G, Collander J, et al. Neonaticides may be more preventable and heterogeneous than previously thought--neonaticides in Finland 1980-2000. Arch Womens Ment Health. 2007;10(1):15-23.
14. Friedman SH, Resnick PJ. Child murder and mental illness in parents: implications for psychiatrists. J Clin Psychiatry. 2011;72(5):587-588.
15. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126(3):325-334.
16. Friedman SH. Searching for the whole truth: considering culture and gender in forensic psychiatric practice. J Am Acad Psychiatry Law. 2023;51(1):23-34.
17. Friedman SH, Hrouda DR, Holden CE, et al. Child murder committed by severely mentally ill mothers: an examination of mothers found not guilty by reason of insanity. J Forensic Sci. 2005;50(6):1466-1471.
18. Ash P. Fatal maltreatment and child abuse turned to murder. In: Friedman SH, ed. Family Murder: Pathologies of Love and Hate. Group for the Advancement Psychiatry; 2018.
19. Friedman SH, Appel JM. Murder in the family: intimate partner homicide in the elderly. Psychiatric News. 2018. Accessed April 8, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a21
20. Friedman SH, McEwan MV. Treated mental illness and the risk of child abuse perpetration. Psychiatr Serv. 2018;69(2):211-216.
21. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
22. Hatters Friedman S, Beaman JW, Friedman JB. Fatality review and the role of the forensic psychiatrist. J Am Acad Psychiatry Law. 2021;49(3):396-405.
23. Friedman SH, Prakash C, Nagle-Yang S. Postpartum psychosis: protecting mother and infant. Current Psychiatry. 2019;18(4):12-21.
24. Stanton J, Simpson AI, Wouldes T. A qualitative study of filicide by mentally ill mothers. Child Abuse Negl. 2000;24(11):1451-1460.
25. Levitzky S, Cooper R. Infant colic syndrome—maternal fantasies of aggression and infanticide. Clin Pediatr (Phila). 2000;39(7):395-400.
26. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
27. Barr JA, Beck CT. Infanticide secrets: qualitative study on postpartum depression. Can Fam Physician. 2008;54(12):1716-1717.e5.
28. Friedman SH, Sorrentino RM, Stankowski JE, et al. Psychiatrists’ knowledge about maternal filicidal thoughts. Compr Psychiatry. 2008;49(1):106-110.
29. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
30. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20(8):30-36.
Emergency contraception for psychiatric patients
Ms. A, age 22, is a college student who presents for an initial psychiatric evaluation. Her body mass index (BMI) is 20 (normal range: 18.5 to 24.9), and her medical history is positive only for childhood asthma. She has been treated for major depressive disorder with venlafaxine by her previous psychiatrist. While this antidepressant has been effective for some symptoms, she has experienced adverse effects and is interested in a different medication. During the evaluation, Ms. A remarks that she had a “scare” last night when the condom broke while having sex with her boyfriend. She says that she is interested in having children at some point, but not at present; she is concerned that getting pregnant now would cause her depression to “spiral out of control.”
Unwanted or mistimed pregnancies account for 45% of all pregnancies.1 While there are ramifications for any unintended pregnancy, the risks for patients with mental illness are greater and include potential adverse effects on the neonate from both psychiatric disease and psychiatric medication use, worse obstetrical outcomes for patients with untreated mental illness, and worsening of psychiatric symptoms and suicide risk in the peripartum period.2 These risks become even more pronounced when psychiatric medications are reflexively discontinued or reduced in pregnancy, which is commonly done contrary to best practice recommendations. In the United States, the recent Supreme Court decision in Dobbs v Jackson Women’s Health Organization has erased federal protections for abortion previously conferred by Roe v Wade. As a result, as of early October 2022, abortion had been made illegal in 11 states, and was likely to be banned in many others, most commonly in states where there is limited support for either parents or children. Thus, preventing unplanned pregnancies should be a treatment consideration for all medical disciplines.3
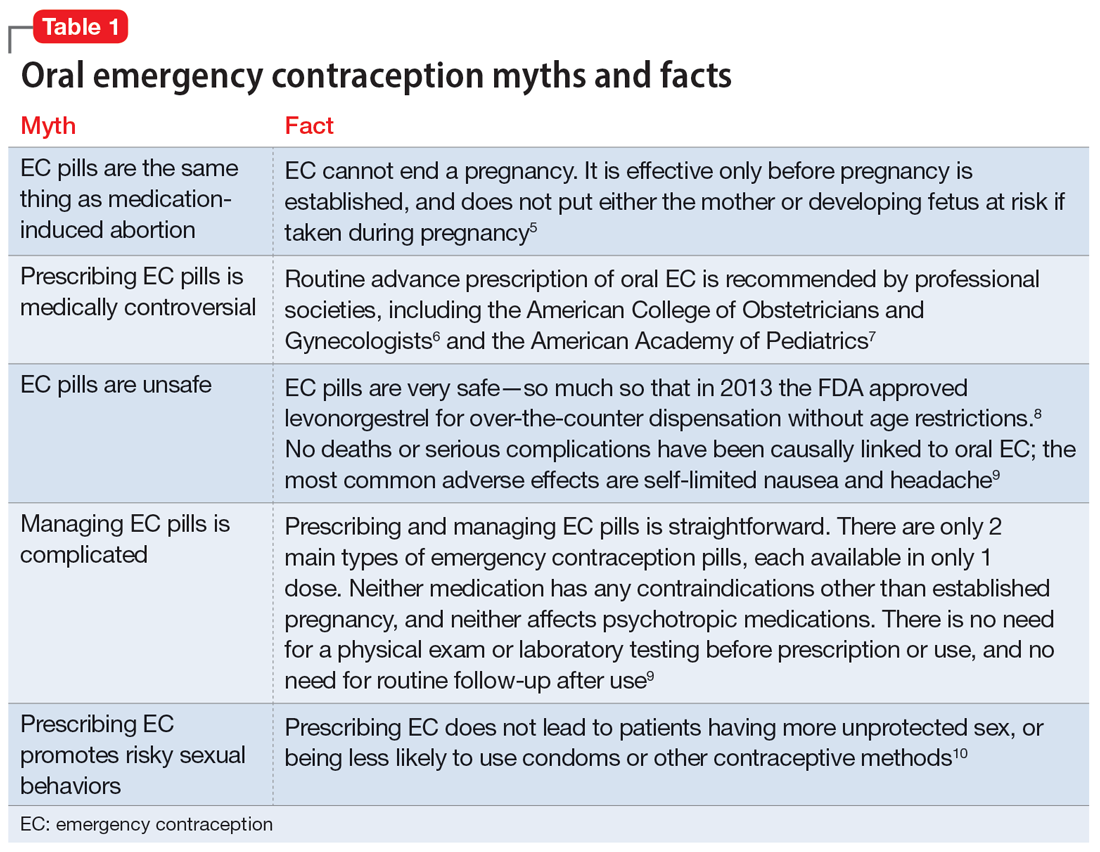
Psychiatrists may hesitate to prescribe emergency contraception (EC) due to fears it falls outside the scope of their practice. However, psychiatry has already moved towards prescribing nonpsychiatric medications when doing so clearly benefits the patient. One example is prescribing metformin to address metabolic syndrome related to the use of second-generation antipsychotics. Emergency contraceptives have strong safety profiles and are easy to prescribe. Unfortunately, there are many barriers to increasing access to emergency contraceptives for psychiatric patients.4 These include the erroneous belief that laboratory and physical exams are needed before starting EC, cost and/or limited stock of emergency contraceptives at pharmacies, and general confusion regarding what constitutes EC vs an oral abortive (Table 15-10). Psychiatrists are particularly well-positioned to support the reproductive autonomy and well-being of patients who struggle to engage with other clinicians. This article aims to help psychiatrists better understand EC so they can comfortably prescribe it before their patients need it.
What is emergency contraception?
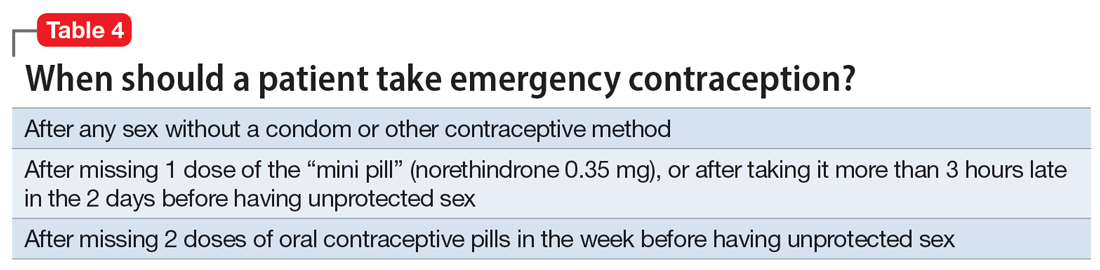
EC is medications or devices that patients can use after sexual intercourse to prevent pregnancy. They do not impede the development of an established pregnancy and thus are not abortifacients. EC is not recommended as a primary means of contraception,9 but it can be extremely valuable to reduce pregnancy risk after unprotected intercourse or contraceptive failures such as broken condoms or missed doses of birth control pills. EC can prevent ≥95% of pregnancies when taken within 5 days of at-risk intercourse.11
Methods of EC fall into 2 categories: oral medications (sometimes referred to as “morning after pills”) and intrauterine devices (IUDs). IUDs are the most effective means of EC, especially for patients with higher BMIs or who may be taking medications such as cytochrome P450 (CYP)3A4 inducers that could interfere with the effectiveness of oral methods. IUDs also have the advantage of providing highly effective ongoing contraception.6 However, IUDs require in-office placement by a trained clinician, and patients may experience difficulty obtaining placement within 5 days of unprotected sex. Therefore, oral medication is the most common form of EC.
Oral EC is safe and effective, and professional societies (including the American College of Obstetricians and Gynecologists6 and the American Academy of Pediatrics7) recommend routinely prescribing oral EC for patients in advance of need. Advance prescribing eliminates barriers to accessing EC, increases the use of EC, and does not encourage risky sexual behaviors.10
Overview of oral emergency contraception
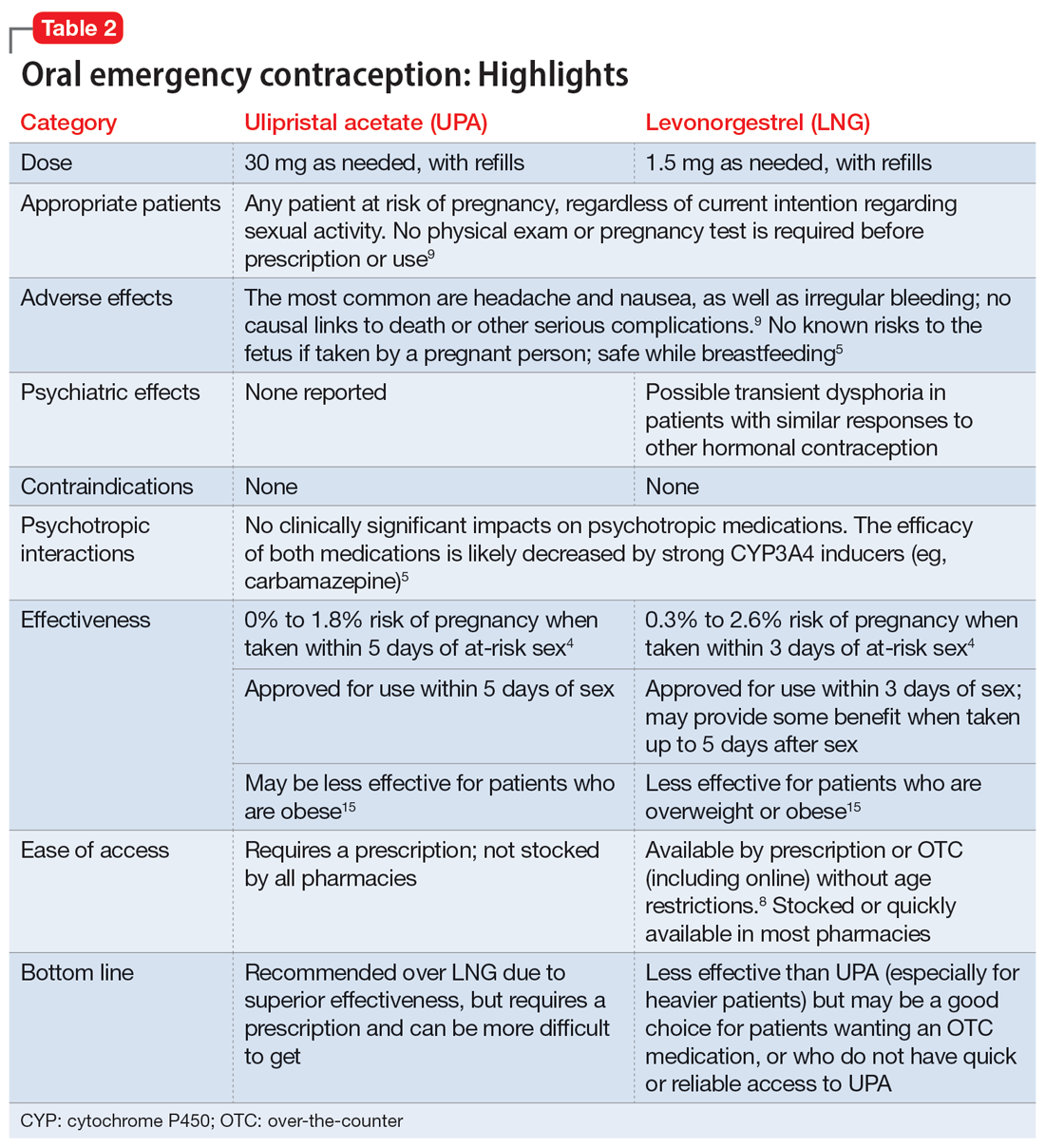
Two medications are FDA-approved for use as oral EC: ulipristal acetate and levonorgestrel. Both are available in generic and branded versions. While many common birth control pills can also be safely used off-label as emergency contraception (an approach known as the Yuzpe method), they are less effective, not as well-tolerated, and require knowledge of the specific type of pill the patient has available.9 Oral EC appears to work primarily through delay or inhibition of ovulation, and is unlikely to prevent implantation of a fertilized egg.9
Continue to: Ulipristal acetate
Ulipristal acetate (UPA) is an oral progesterone receptor agonist-antagonist taken as a single 30 mg dose up to 5 days after unprotected sex. Pregnancy rates from a single act of unprotected sex followed by UPA use range from 0% to 1.8%.4 Many pharmacies stock UPA, and others (especially chain pharmacies) report being able to order and fill it within 24 hours.12
Levonorgestrel (LNG) is an oral progestin that is available by prescription and has also been approved for over-the-counter sale to patients of all ages and sexes (without the need to show identification) since 2013.8 It is administered as a single 1.5 mg dose taken as soon as possible up to 3 days after unprotected sex, although it may continue to provide benefits when taken within 5 days. Pregnancy rates from a single act of unprotected sex followed by LNG use range from 0.3% to 2.6%, with much higher odds among women who are obese.4 LNG is available both by prescription or over-the-counter,13 although it is often kept in a locked cabinet or behind the counter, and staff are often misinformed regarding the lack of age restrictions for sale without a prescription.14
Safety and adverse effects. According to the CDC, there are no conditions for which the risks outweigh the advantages of use of either UPA or LNG,5 and patients for whom hormonal birth control is otherwise contraindicated can still use them safely. If a pregnancy has already occurred, taking EC will not harm the developing fetus; it is also safe to use when breastfeeding.5 Both medications are generally well-tolerated—neither has been causally linked to deaths or serious complications,5 and the most common adverse effects are headache (approximately 19%) and nausea (approximately 12%), in addition to irregular bleeding, fatigue, dizziness, and abdominal pain.15 Oral EC may be used more than once, even within the same menstrual cycle. Patients who use EC repeatedly should be encouraged to discuss more efficacious contraceptive options with their primary physician or gynecologist.
Will oral EC affect psychiatric treatment?
Oral EC is unlikely to have a meaningful effect on psychiatric symptoms or management, particularly when compared to the significant impacts of unintended pregnancies. Neither medication is known to have any clinically significant impacts on the pharmacokinetics or pharmacodynamics of psychotropic medications, although the effectiveness of both medications can be impaired by CYP3A4 inducers such as carbamazepine.5 In addition, while research has not specifically examined the impact of EC on psychiatric symptoms, the broader literature on hormonal contraception indicates that most patients with psychiatric disorders generally report similar or lower rates of mood symptoms associated with their use.16 Some women treated with hormonal contraceptives do develop dysphoric mood,16 but any such effects resulting from LNG would likely be transient. Mood disruptions or other psychiatric symptoms have not been associated with UPA use.
How to prescribe oral emergency contraception
Who and when. Women of reproductive age should be counseled about EC as part of anticipatory guidance, regardless of their current intentions for sexual behaviors. Patients do not need a physical examination or pregnancy test before being prescribed or using oral EC.9 Much like how intranasal naloxone is prescribed, prescriptions should be provided in advance of need, with multiple refills to facilitate ready access when needed.
Continue to: Which to prescribe
Which to prescribe. UPA is more effective in preventing pregnancy than LNG at all time points up to 120 hours after sex, including for women who are overweight or obese.15 As such, it is recommended as the first-line choice. However, because LNG is available without prescription and is more readily available (including via online order), it may be a good choice for patients who need rapid EC or who prefer a medication that does not require a prescription (Table 24,5,8,9,15).
What to tell patients. Patients should be instructed to fill their prescription before they expect to use it, to ensure ready availability when desired (Table 35,9). Oral EC is shelf stable for at least 3 years when stored in a cool, dry environment. Patients should take the medication as soon as possible following at-risk sexual intercourse (Table 4). Tell them that if they vomit within 3 hours of taking the medication, they should take a second dose. Remind patients that EC does not protect against sexually transmitted infections, or from sex that occurs after the medication is taken (in fact, they can increase the possibility of pregnancy later in that menstrual cycle due to delayed ovulation).9 Counsel patients to abstain from sex or to use barrier contraception for 7 days after use. Those who take birth control pills can resume use immediately after using LNG; they should wait 5 days after taking UPA.
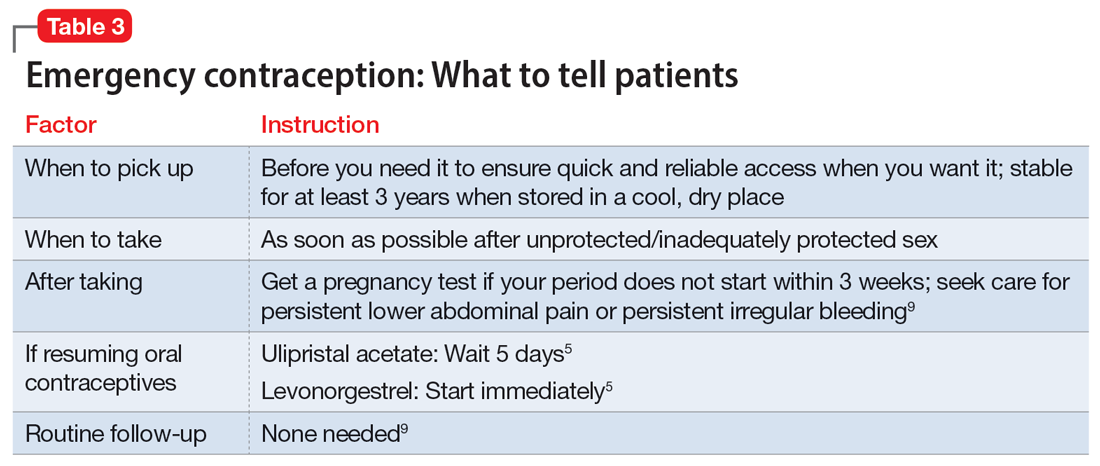
No routine follow-up is needed after taking UPA or LNG. However, patients should get a pregnancy test if their period does not start within 3 weeks, and should seek medical evaluation if they experience significant lower abdominal pain or persistent irregular bleeding in order to rule out pregnancy-related complications. Patients who use EC repeatedly should be recommended to pursue routine contraceptive care.
Billing. Counseling your patients about contraception can increase the reimbursement you receive by adding to the complexity of the encounter (regardless of whether you prescribe a medication) through use of the ICD-10 code Z30.0.
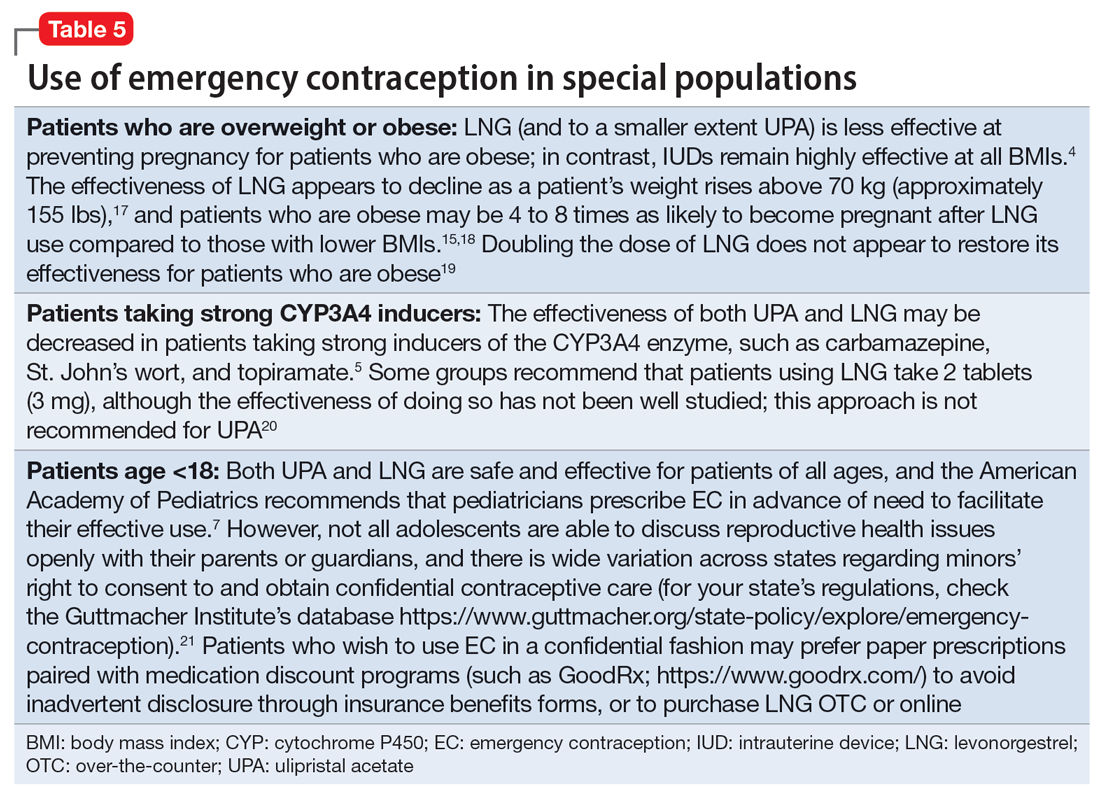
Emergency contraception for special populations
Some patients face additional challenges to effective EC that should be considered when counseling and prescribing. Table 54,5,7,15,17-21 discusses the use of EC in these special populations. Of particular importance for psychiatrists, LNG is less effective at preventing undesired pregnancy among patients who are overweight or obese,15,17,18 and strong CYP3A4-inducing agents may decrease the effectiveness of both LNG and UPA.5 Keep in mind, however, that the advantages of using either UPA or LNG outweigh the risks for all populations.5 Patients must be aware of appropriate information in order to make informed decisions, but should not be discouraged from using EC.
Continue to: Other groups of patients...
Other groups of patients may face barriers due to some clinicians’ hesitancy regarding their ability to consent to reproductive care. Most patients with psychiatric illnesses have decision-making capacity regarding reproductive issues.22 Although EC is supported by the American Academy of Pediatrics,7 patients age <18 have varying rights to consent across states,21 and merit special consideration.
CASE CONTINUED
Ms. A does not wish to get pregnant at this time, and expresses fears that her recent contraceptive failure could lead to an unintended pregnancy. In addition to her psychiatric treatment, her psychiatrist should discuss EC options with her. She has a healthy BMI and had inadequately protected sex <1 day ago, so her clinician may prescribe LNG (to ensure rapid access for immediate use) in addition to UPA for her to have available in case of future “scares.” The psychiatrist should consider pharmacologic treatment with an antidepressant with a relatively safe reproductive record (eg, sertraline).23 This is considered preventive ethics, since Ms. A is of reproductive age, even if she is not presently planning to get pregnant, due to the aforementioned high rate of unplanned pregnancy.23,24 It is also important for the psychiatrist to continue the dialogue in future sessions about preventing unintended pregnancy. Since Ms. A has benefited from a psychotropic medication when not pregnant, it will be important to discuss with her the risks and benefits of medication should she plan a pregnancy.
Bottom Line
Patients with mental illnesses are at increased risk of adverse outcomes resulting from unintended pregnancies. Clinicians should counsel patients about emergency contraception (EC) as a part of routine psychiatric care, and should prescribe oral EC in advance of patient need to facilitate effective use.
Related Resources
- American College of Obstetricians and Gynecologists Practice Bulletin on Emergency Contraception. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/ articles/2015/09/emergency-contraception
- State policies on emergency contraception. https://www.guttmacher.org/state-policy/explore/emergency-contraception
- State policies on minors’ access to contraceptive services. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
- Patient-oriented contraceptive education materials (in English and Spanish). https://shop.powertodecide.org/ptd-category/educational-materials
Drug Brand Names
Carbamazepine • Tegretol
Levonorgestrel • Plan B One-Step, Fallback
Metformin • Glucophage
Naloxone • Narcan
Norethindrone • Aygestin
Sertraline • Zoloft
Topiramate • Topamax
Ulipristal acetate • Ella
Venlafaxine • Effexor
1. Grossman D. Expanding access to short-acting hormonal contraceptive methods in the United States. JAMA Intern Med. 2019;179:1209-1210.
2. Gur TL, Kim DR, Epperson CN. Central nervous system effects of prenatal selective serotonin reuptake inhibitors: sensing the signal through the noise. Psychopharmacology (Berl). 2013;227:567-582.
3. Ross N, Landess J, Kaempf A, et al. Pregnancy termination: what psychiatrists need to know. Current Psychiatry. 2022;21:8-9.
4. Haeger KO, Lamme J, Cleland K. State of emergency contraception in the US, 2018. Contracept Reprod Med. 2018;3:20.
5. Curtis KM, Tepper NK, Jatlaoui TC, et al. US medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65:1-3.
6. American College of Obstetricians and Gynecologists. Committee Opinion No 707: Access to emergency contraception. Obstet Gynecol. 2017;130:e48-e52.
7. Upadhya KK, Breuner CC, Alderman EM, et al. Emergency contraception. Pediatrics. 2019;144:e20193149.
8. Rowan A. Obama administration yields to the courts and the evidence, allows emergency contraception to be sold without restrictions. Guttmacher Institute. Published June 25, 2013. Accessed July 31, 2022. https://www.guttmacher.org/gpr/2013/06/obama-administration-yields-courts-and-evidence-allows-emergency-contraception-be-sold#
9. American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
10. Rodriguez MI, Curtis KM, Gaffield ML, et al. Advance supply of emergency contraception: a systematic review. Contraception. 2013;87:590-601.
11. World Health Organization. Emergency contraception. Published November 9, 2021. Accessed August 4, 2022. https://www.who.int/news-room/fact-sheets/detail/emergency-contraception
12. Shigesato M, Elia J, Tschann M, et al. Pharmacy access to ulipristal acetate in major cities throughout the United States. Contraception. 2018;97:264-269.
13. Wilkinson TA, Clark P, Rafie S, et al. Access to emergency contraception after removal of age restrictions. Pediatrics. 2017;140:e20164262.
14. Cleland K, Bass J, Doci F, et al. Access to emergency contraception in the over-the-counter era. Women’s Health Issues. 2016;26:622-627.
15. Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet. 2010;375:555-562.
16. McCloskey LR, Wisner KL, Cattan MK, et al. Contraception for women with psychiatric disorders. Am J Psychiatry. 2021;178:247-255.
17. Kapp N, Abitbol JL, Mathé H, et al. Effect of body weight and BMI on the efficacy of levonorgestrel emergency contraception. Contraception. 2015;91:97-104.
18. Festin MP, Peregoudov A, Seuc A, et al. Effect of BMI and body weight on pregnancy rates with LNG as emergency contraception: analysis of four WHO HRP studies. Contraception. 2017;95:50-54.
19. Edelman AB, Hennebold JD, Bond K, et al. Double dosing levonorgestrel-based emergency contraception for individuals with obesity: a randomized controlled trial. Obstet Gynecol. 2022;140(1):48-54.
20. FSRH Clinical Effectiveness Unit. FSRH clinical guideline: Emergency contraception. Published March 2017. Amended December 2020. Faculty of Sexual & Reproductive Healthcare. Accessed August 4, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-emergency-contraception-march-2017/
21. Guttmacher Institute. Minors’ access to contraceptive services. Guttmacher Institute. Accessed August 4, 2022. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
22. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022;63:61-70.
23. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20:30-36.
24. Friedman SH. The ethics of treating depression in pregnancy. J Primary Healthcare. 2015;7:81-83.
Ms. A, age 22, is a college student who presents for an initial psychiatric evaluation. Her body mass index (BMI) is 20 (normal range: 18.5 to 24.9), and her medical history is positive only for childhood asthma. She has been treated for major depressive disorder with venlafaxine by her previous psychiatrist. While this antidepressant has been effective for some symptoms, she has experienced adverse effects and is interested in a different medication. During the evaluation, Ms. A remarks that she had a “scare” last night when the condom broke while having sex with her boyfriend. She says that she is interested in having children at some point, but not at present; she is concerned that getting pregnant now would cause her depression to “spiral out of control.”
Unwanted or mistimed pregnancies account for 45% of all pregnancies.1 While there are ramifications for any unintended pregnancy, the risks for patients with mental illness are greater and include potential adverse effects on the neonate from both psychiatric disease and psychiatric medication use, worse obstetrical outcomes for patients with untreated mental illness, and worsening of psychiatric symptoms and suicide risk in the peripartum period.2 These risks become even more pronounced when psychiatric medications are reflexively discontinued or reduced in pregnancy, which is commonly done contrary to best practice recommendations. In the United States, the recent Supreme Court decision in Dobbs v Jackson Women’s Health Organization has erased federal protections for abortion previously conferred by Roe v Wade. As a result, as of early October 2022, abortion had been made illegal in 11 states, and was likely to be banned in many others, most commonly in states where there is limited support for either parents or children. Thus, preventing unplanned pregnancies should be a treatment consideration for all medical disciplines.3
Psychiatrists may hesitate to prescribe emergency contraception (EC) due to fears it falls outside the scope of their practice. However, psychiatry has already moved towards prescribing nonpsychiatric medications when doing so clearly benefits the patient. One example is prescribing metformin to address metabolic syndrome related to the use of second-generation antipsychotics. Emergency contraceptives have strong safety profiles and are easy to prescribe. Unfortunately, there are many barriers to increasing access to emergency contraceptives for psychiatric patients.4 These include the erroneous belief that laboratory and physical exams are needed before starting EC, cost and/or limited stock of emergency contraceptives at pharmacies, and general confusion regarding what constitutes EC vs an oral abortive (Table 15-10). Psychiatrists are particularly well-positioned to support the reproductive autonomy and well-being of patients who struggle to engage with other clinicians. This article aims to help psychiatrists better understand EC so they can comfortably prescribe it before their patients need it.
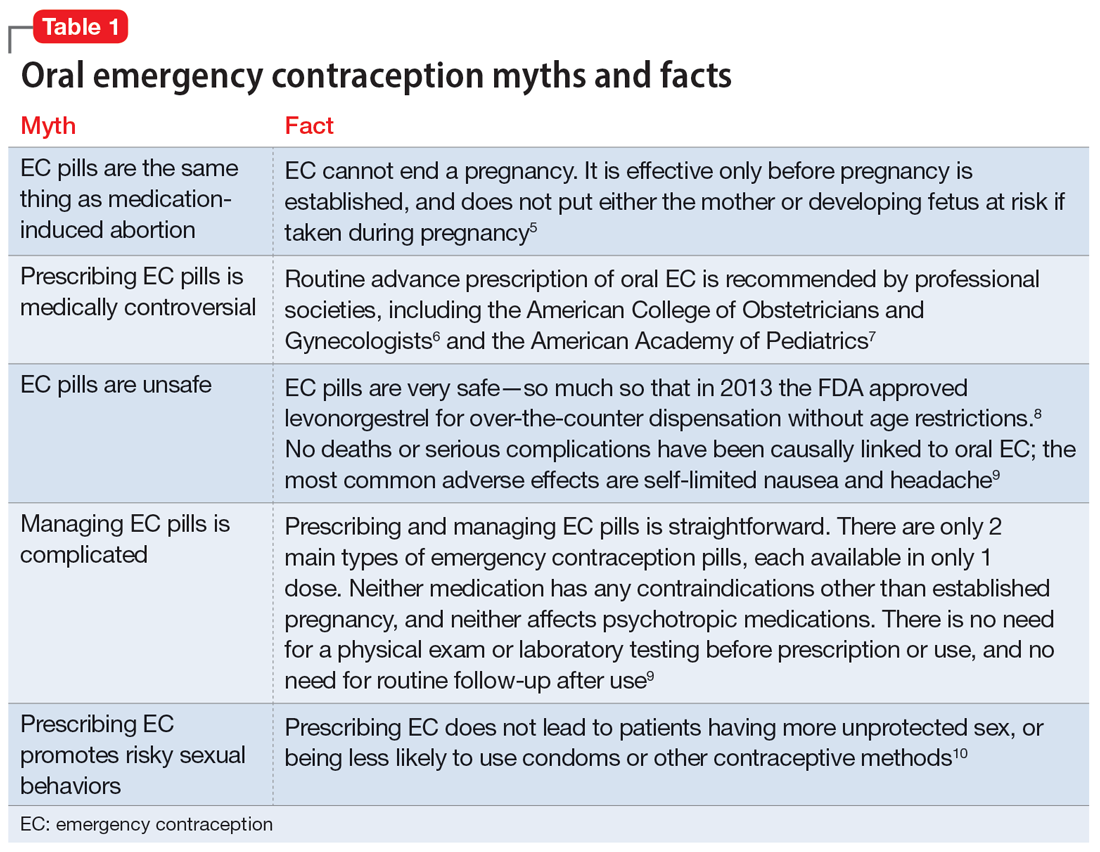
What is emergency contraception?
EC is medications or devices that patients can use after sexual intercourse to prevent pregnancy. They do not impede the development of an established pregnancy and thus are not abortifacients. EC is not recommended as a primary means of contraception,9 but it can be extremely valuable to reduce pregnancy risk after unprotected intercourse or contraceptive failures such as broken condoms or missed doses of birth control pills. EC can prevent ≥95% of pregnancies when taken within 5 days of at-risk intercourse.11
Methods of EC fall into 2 categories: oral medications (sometimes referred to as “morning after pills”) and intrauterine devices (IUDs). IUDs are the most effective means of EC, especially for patients with higher BMIs or who may be taking medications such as cytochrome P450 (CYP)3A4 inducers that could interfere with the effectiveness of oral methods. IUDs also have the advantage of providing highly effective ongoing contraception.6 However, IUDs require in-office placement by a trained clinician, and patients may experience difficulty obtaining placement within 5 days of unprotected sex. Therefore, oral medication is the most common form of EC.
Oral EC is safe and effective, and professional societies (including the American College of Obstetricians and Gynecologists6 and the American Academy of Pediatrics7) recommend routinely prescribing oral EC for patients in advance of need. Advance prescribing eliminates barriers to accessing EC, increases the use of EC, and does not encourage risky sexual behaviors.10
Overview of oral emergency contraception
Two medications are FDA-approved for use as oral EC: ulipristal acetate and levonorgestrel. Both are available in generic and branded versions. While many common birth control pills can also be safely used off-label as emergency contraception (an approach known as the Yuzpe method), they are less effective, not as well-tolerated, and require knowledge of the specific type of pill the patient has available.9 Oral EC appears to work primarily through delay or inhibition of ovulation, and is unlikely to prevent implantation of a fertilized egg.9
Continue to: Ulipristal acetate
Ulipristal acetate (UPA) is an oral progesterone receptor agonist-antagonist taken as a single 30 mg dose up to 5 days after unprotected sex. Pregnancy rates from a single act of unprotected sex followed by UPA use range from 0% to 1.8%.4 Many pharmacies stock UPA, and others (especially chain pharmacies) report being able to order and fill it within 24 hours.12
Levonorgestrel (LNG) is an oral progestin that is available by prescription and has also been approved for over-the-counter sale to patients of all ages and sexes (without the need to show identification) since 2013.8 It is administered as a single 1.5 mg dose taken as soon as possible up to 3 days after unprotected sex, although it may continue to provide benefits when taken within 5 days. Pregnancy rates from a single act of unprotected sex followed by LNG use range from 0.3% to 2.6%, with much higher odds among women who are obese.4 LNG is available both by prescription or over-the-counter,13 although it is often kept in a locked cabinet or behind the counter, and staff are often misinformed regarding the lack of age restrictions for sale without a prescription.14
Safety and adverse effects. According to the CDC, there are no conditions for which the risks outweigh the advantages of use of either UPA or LNG,5 and patients for whom hormonal birth control is otherwise contraindicated can still use them safely. If a pregnancy has already occurred, taking EC will not harm the developing fetus; it is also safe to use when breastfeeding.5 Both medications are generally well-tolerated—neither has been causally linked to deaths or serious complications,5 and the most common adverse effects are headache (approximately 19%) and nausea (approximately 12%), in addition to irregular bleeding, fatigue, dizziness, and abdominal pain.15 Oral EC may be used more than once, even within the same menstrual cycle. Patients who use EC repeatedly should be encouraged to discuss more efficacious contraceptive options with their primary physician or gynecologist.
Will oral EC affect psychiatric treatment?
Oral EC is unlikely to have a meaningful effect on psychiatric symptoms or management, particularly when compared to the significant impacts of unintended pregnancies. Neither medication is known to have any clinically significant impacts on the pharmacokinetics or pharmacodynamics of psychotropic medications, although the effectiveness of both medications can be impaired by CYP3A4 inducers such as carbamazepine.5 In addition, while research has not specifically examined the impact of EC on psychiatric symptoms, the broader literature on hormonal contraception indicates that most patients with psychiatric disorders generally report similar or lower rates of mood symptoms associated with their use.16 Some women treated with hormonal contraceptives do develop dysphoric mood,16 but any such effects resulting from LNG would likely be transient. Mood disruptions or other psychiatric symptoms have not been associated with UPA use.
How to prescribe oral emergency contraception
Who and when. Women of reproductive age should be counseled about EC as part of anticipatory guidance, regardless of their current intentions for sexual behaviors. Patients do not need a physical examination or pregnancy test before being prescribed or using oral EC.9 Much like how intranasal naloxone is prescribed, prescriptions should be provided in advance of need, with multiple refills to facilitate ready access when needed.
Continue to: Which to prescribe
Which to prescribe. UPA is more effective in preventing pregnancy than LNG at all time points up to 120 hours after sex, including for women who are overweight or obese.15 As such, it is recommended as the first-line choice. However, because LNG is available without prescription and is more readily available (including via online order), it may be a good choice for patients who need rapid EC or who prefer a medication that does not require a prescription (Table 24,5,8,9,15).
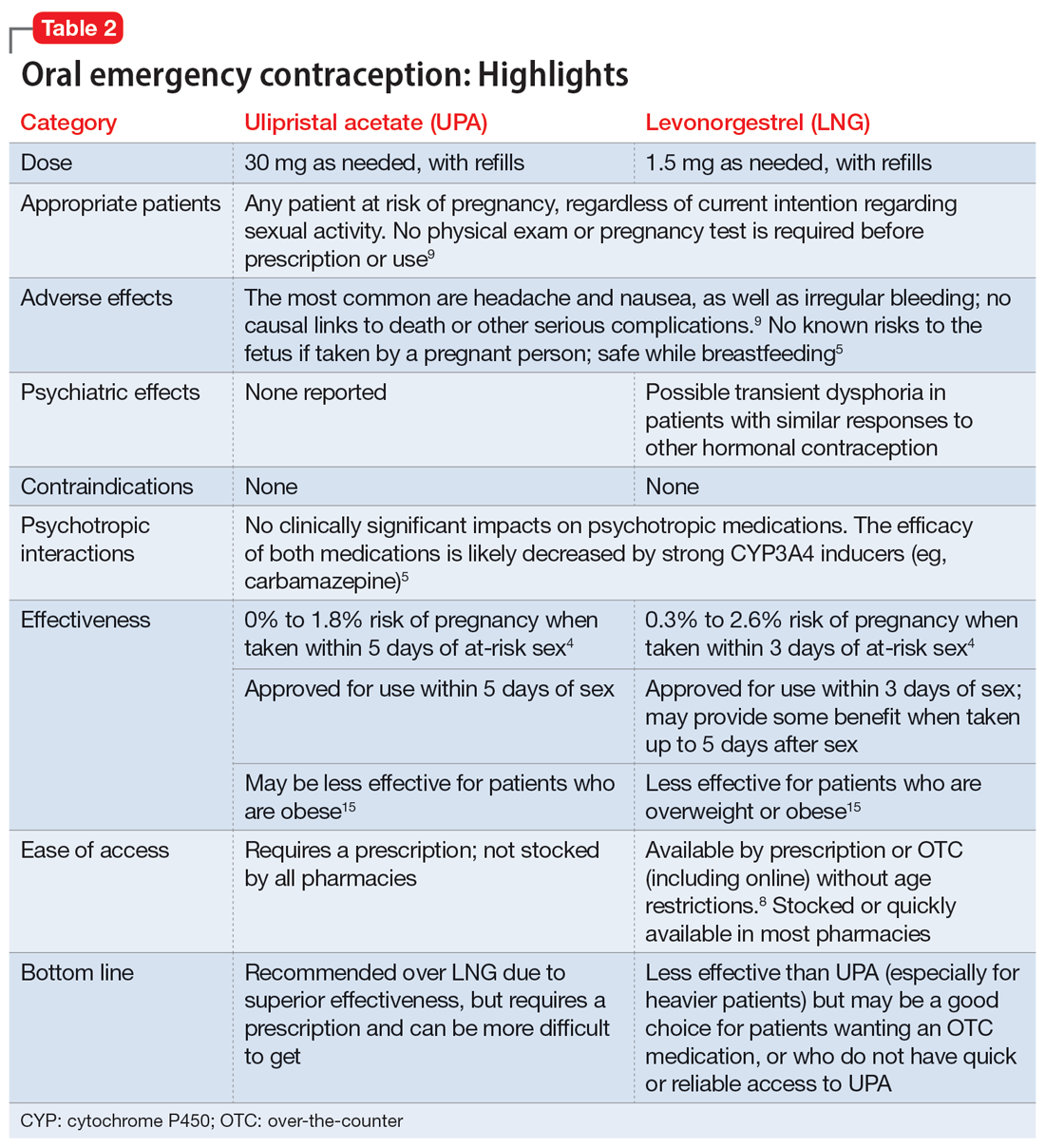
What to tell patients. Patients should be instructed to fill their prescription before they expect to use it, to ensure ready availability when desired (Table 35,9). Oral EC is shelf stable for at least 3 years when stored in a cool, dry environment. Patients should take the medication as soon as possible following at-risk sexual intercourse (Table 4). Tell them that if they vomit within 3 hours of taking the medication, they should take a second dose. Remind patients that EC does not protect against sexually transmitted infections, or from sex that occurs after the medication is taken (in fact, they can increase the possibility of pregnancy later in that menstrual cycle due to delayed ovulation).9 Counsel patients to abstain from sex or to use barrier contraception for 7 days after use. Those who take birth control pills can resume use immediately after using LNG; they should wait 5 days after taking UPA.
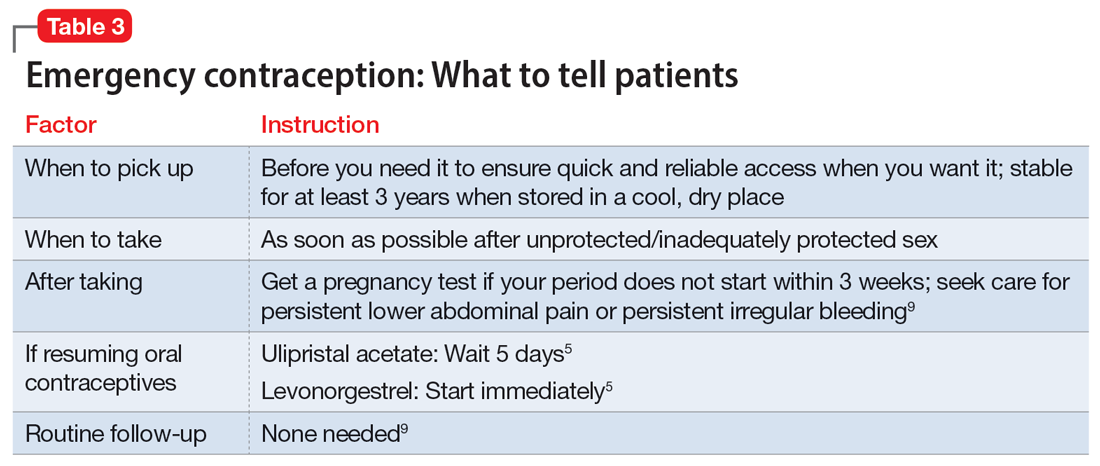
No routine follow-up is needed after taking UPA or LNG. However, patients should get a pregnancy test if their period does not start within 3 weeks, and should seek medical evaluation if they experience significant lower abdominal pain or persistent irregular bleeding in order to rule out pregnancy-related complications. Patients who use EC repeatedly should be recommended to pursue routine contraceptive care.
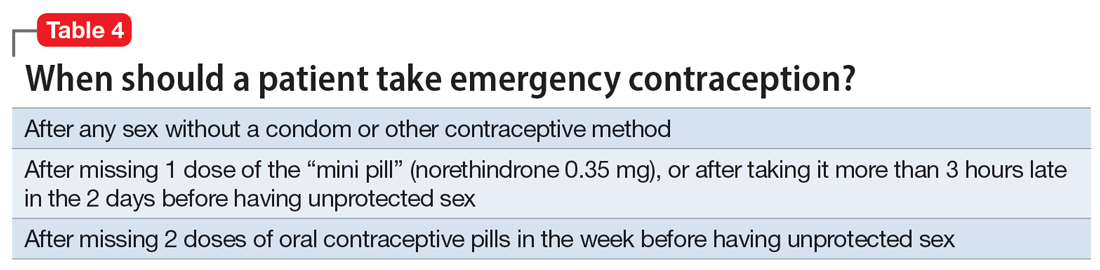
Billing. Counseling your patients about contraception can increase the reimbursement you receive by adding to the complexity of the encounter (regardless of whether you prescribe a medication) through use of the ICD-10 code Z30.0.
Emergency contraception for special populations
Some patients face additional challenges to effective EC that should be considered when counseling and prescribing. Table 54,5,7,15,17-21 discusses the use of EC in these special populations. Of particular importance for psychiatrists, LNG is less effective at preventing undesired pregnancy among patients who are overweight or obese,15,17,18 and strong CYP3A4-inducing agents may decrease the effectiveness of both LNG and UPA.5 Keep in mind, however, that the advantages of using either UPA or LNG outweigh the risks for all populations.5 Patients must be aware of appropriate information in order to make informed decisions, but should not be discouraged from using EC.
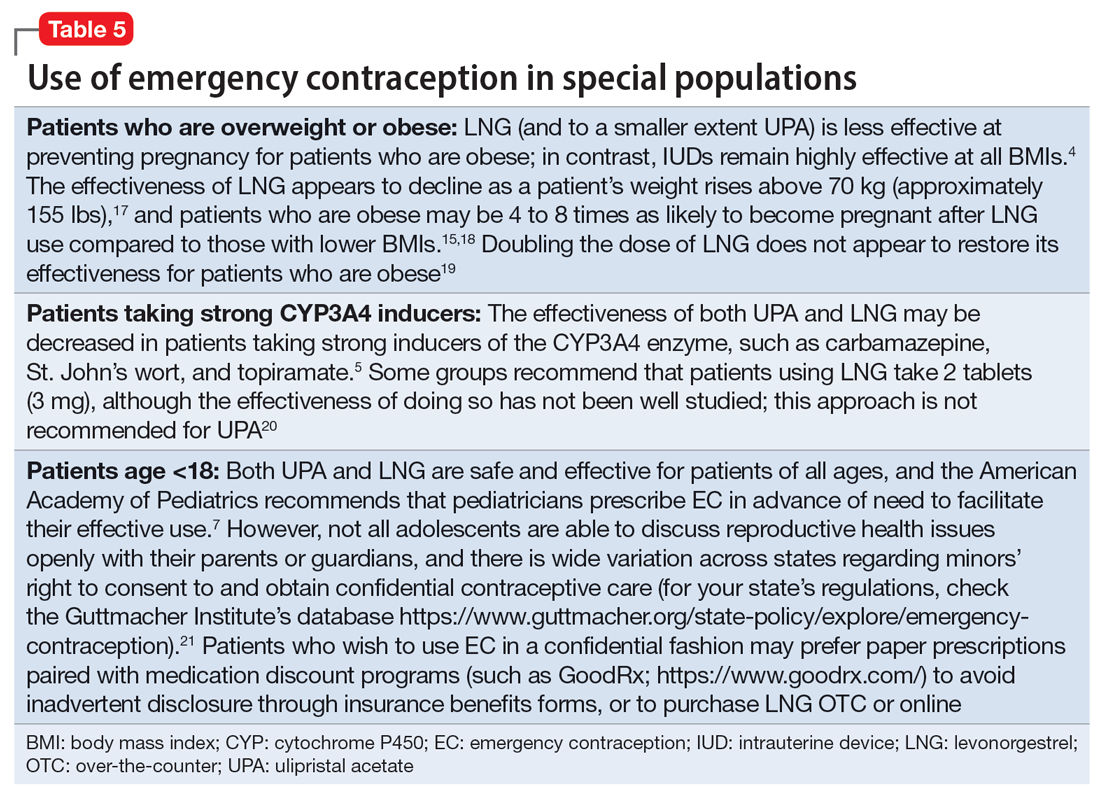
Continue to: Other groups of patients...
Other groups of patients may face barriers due to some clinicians’ hesitancy regarding their ability to consent to reproductive care. Most patients with psychiatric illnesses have decision-making capacity regarding reproductive issues.22 Although EC is supported by the American Academy of Pediatrics,7 patients age <18 have varying rights to consent across states,21 and merit special consideration.
CASE CONTINUED
Ms. A does not wish to get pregnant at this time, and expresses fears that her recent contraceptive failure could lead to an unintended pregnancy. In addition to her psychiatric treatment, her psychiatrist should discuss EC options with her. She has a healthy BMI and had inadequately protected sex <1 day ago, so her clinician may prescribe LNG (to ensure rapid access for immediate use) in addition to UPA for her to have available in case of future “scares.” The psychiatrist should consider pharmacologic treatment with an antidepressant with a relatively safe reproductive record (eg, sertraline).23 This is considered preventive ethics, since Ms. A is of reproductive age, even if she is not presently planning to get pregnant, due to the aforementioned high rate of unplanned pregnancy.23,24 It is also important for the psychiatrist to continue the dialogue in future sessions about preventing unintended pregnancy. Since Ms. A has benefited from a psychotropic medication when not pregnant, it will be important to discuss with her the risks and benefits of medication should she plan a pregnancy.
Bottom Line
Patients with mental illnesses are at increased risk of adverse outcomes resulting from unintended pregnancies. Clinicians should counsel patients about emergency contraception (EC) as a part of routine psychiatric care, and should prescribe oral EC in advance of patient need to facilitate effective use.
Related Resources
- American College of Obstetricians and Gynecologists Practice Bulletin on Emergency Contraception. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/ articles/2015/09/emergency-contraception
- State policies on emergency contraception. https://www.guttmacher.org/state-policy/explore/emergency-contraception
- State policies on minors’ access to contraceptive services. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
- Patient-oriented contraceptive education materials (in English and Spanish). https://shop.powertodecide.org/ptd-category/educational-materials
Drug Brand Names
Carbamazepine • Tegretol
Levonorgestrel • Plan B One-Step, Fallback
Metformin • Glucophage
Naloxone • Narcan
Norethindrone • Aygestin
Sertraline • Zoloft
Topiramate • Topamax
Ulipristal acetate • Ella
Venlafaxine • Effexor
Ms. A, age 22, is a college student who presents for an initial psychiatric evaluation. Her body mass index (BMI) is 20 (normal range: 18.5 to 24.9), and her medical history is positive only for childhood asthma. She has been treated for major depressive disorder with venlafaxine by her previous psychiatrist. While this antidepressant has been effective for some symptoms, she has experienced adverse effects and is interested in a different medication. During the evaluation, Ms. A remarks that she had a “scare” last night when the condom broke while having sex with her boyfriend. She says that she is interested in having children at some point, but not at present; she is concerned that getting pregnant now would cause her depression to “spiral out of control.”
Unwanted or mistimed pregnancies account for 45% of all pregnancies.1 While there are ramifications for any unintended pregnancy, the risks for patients with mental illness are greater and include potential adverse effects on the neonate from both psychiatric disease and psychiatric medication use, worse obstetrical outcomes for patients with untreated mental illness, and worsening of psychiatric symptoms and suicide risk in the peripartum period.2 These risks become even more pronounced when psychiatric medications are reflexively discontinued or reduced in pregnancy, which is commonly done contrary to best practice recommendations. In the United States, the recent Supreme Court decision in Dobbs v Jackson Women’s Health Organization has erased federal protections for abortion previously conferred by Roe v Wade. As a result, as of early October 2022, abortion had been made illegal in 11 states, and was likely to be banned in many others, most commonly in states where there is limited support for either parents or children. Thus, preventing unplanned pregnancies should be a treatment consideration for all medical disciplines.3
Psychiatrists may hesitate to prescribe emergency contraception (EC) due to fears it falls outside the scope of their practice. However, psychiatry has already moved towards prescribing nonpsychiatric medications when doing so clearly benefits the patient. One example is prescribing metformin to address metabolic syndrome related to the use of second-generation antipsychotics. Emergency contraceptives have strong safety profiles and are easy to prescribe. Unfortunately, there are many barriers to increasing access to emergency contraceptives for psychiatric patients.4 These include the erroneous belief that laboratory and physical exams are needed before starting EC, cost and/or limited stock of emergency contraceptives at pharmacies, and general confusion regarding what constitutes EC vs an oral abortive (Table 15-10). Psychiatrists are particularly well-positioned to support the reproductive autonomy and well-being of patients who struggle to engage with other clinicians. This article aims to help psychiatrists better understand EC so they can comfortably prescribe it before their patients need it.
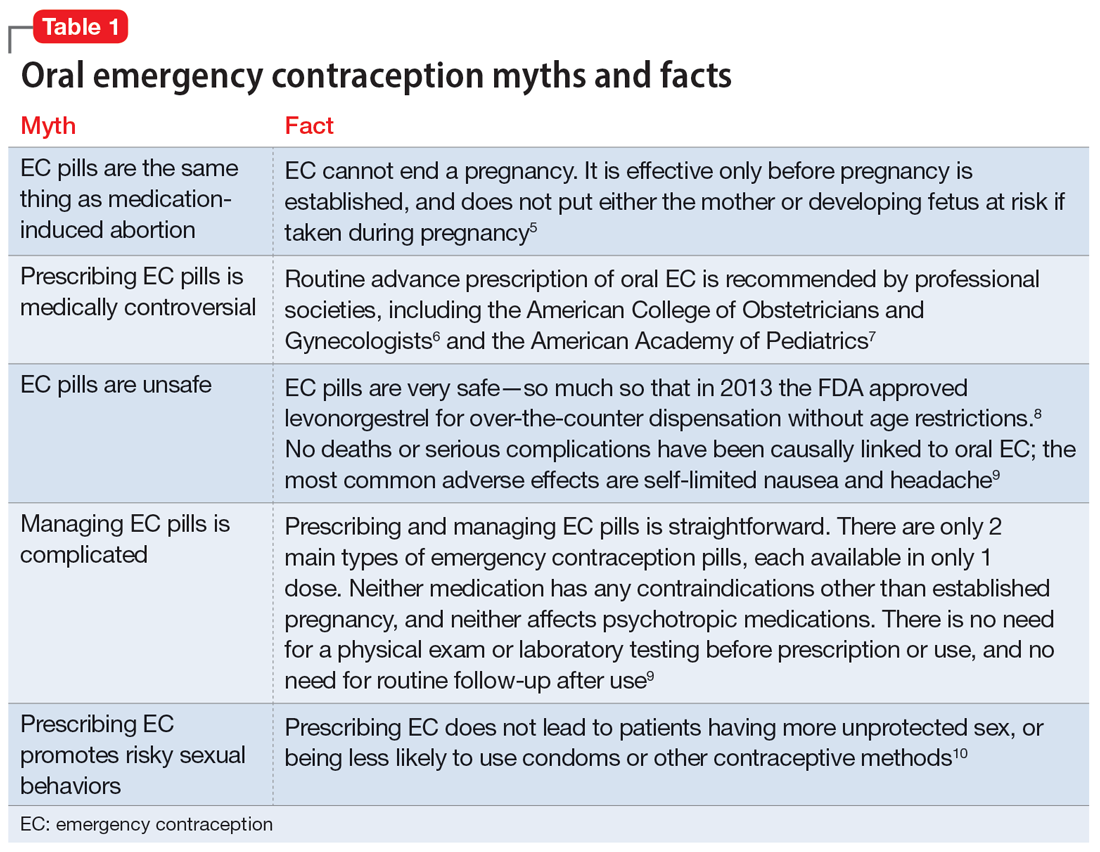
What is emergency contraception?
EC is medications or devices that patients can use after sexual intercourse to prevent pregnancy. They do not impede the development of an established pregnancy and thus are not abortifacients. EC is not recommended as a primary means of contraception,9 but it can be extremely valuable to reduce pregnancy risk after unprotected intercourse or contraceptive failures such as broken condoms or missed doses of birth control pills. EC can prevent ≥95% of pregnancies when taken within 5 days of at-risk intercourse.11
Methods of EC fall into 2 categories: oral medications (sometimes referred to as “morning after pills”) and intrauterine devices (IUDs). IUDs are the most effective means of EC, especially for patients with higher BMIs or who may be taking medications such as cytochrome P450 (CYP)3A4 inducers that could interfere with the effectiveness of oral methods. IUDs also have the advantage of providing highly effective ongoing contraception.6 However, IUDs require in-office placement by a trained clinician, and patients may experience difficulty obtaining placement within 5 days of unprotected sex. Therefore, oral medication is the most common form of EC.
Oral EC is safe and effective, and professional societies (including the American College of Obstetricians and Gynecologists6 and the American Academy of Pediatrics7) recommend routinely prescribing oral EC for patients in advance of need. Advance prescribing eliminates barriers to accessing EC, increases the use of EC, and does not encourage risky sexual behaviors.10
Overview of oral emergency contraception
Two medications are FDA-approved for use as oral EC: ulipristal acetate and levonorgestrel. Both are available in generic and branded versions. While many common birth control pills can also be safely used off-label as emergency contraception (an approach known as the Yuzpe method), they are less effective, not as well-tolerated, and require knowledge of the specific type of pill the patient has available.9 Oral EC appears to work primarily through delay or inhibition of ovulation, and is unlikely to prevent implantation of a fertilized egg.9
Continue to: Ulipristal acetate
Ulipristal acetate (UPA) is an oral progesterone receptor agonist-antagonist taken as a single 30 mg dose up to 5 days after unprotected sex. Pregnancy rates from a single act of unprotected sex followed by UPA use range from 0% to 1.8%.4 Many pharmacies stock UPA, and others (especially chain pharmacies) report being able to order and fill it within 24 hours.12
Levonorgestrel (LNG) is an oral progestin that is available by prescription and has also been approved for over-the-counter sale to patients of all ages and sexes (without the need to show identification) since 2013.8 It is administered as a single 1.5 mg dose taken as soon as possible up to 3 days after unprotected sex, although it may continue to provide benefits when taken within 5 days. Pregnancy rates from a single act of unprotected sex followed by LNG use range from 0.3% to 2.6%, with much higher odds among women who are obese.4 LNG is available both by prescription or over-the-counter,13 although it is often kept in a locked cabinet or behind the counter, and staff are often misinformed regarding the lack of age restrictions for sale without a prescription.14
Safety and adverse effects. According to the CDC, there are no conditions for which the risks outweigh the advantages of use of either UPA or LNG,5 and patients for whom hormonal birth control is otherwise contraindicated can still use them safely. If a pregnancy has already occurred, taking EC will not harm the developing fetus; it is also safe to use when breastfeeding.5 Both medications are generally well-tolerated—neither has been causally linked to deaths or serious complications,5 and the most common adverse effects are headache (approximately 19%) and nausea (approximately 12%), in addition to irregular bleeding, fatigue, dizziness, and abdominal pain.15 Oral EC may be used more than once, even within the same menstrual cycle. Patients who use EC repeatedly should be encouraged to discuss more efficacious contraceptive options with their primary physician or gynecologist.
Will oral EC affect psychiatric treatment?
Oral EC is unlikely to have a meaningful effect on psychiatric symptoms or management, particularly when compared to the significant impacts of unintended pregnancies. Neither medication is known to have any clinically significant impacts on the pharmacokinetics or pharmacodynamics of psychotropic medications, although the effectiveness of both medications can be impaired by CYP3A4 inducers such as carbamazepine.5 In addition, while research has not specifically examined the impact of EC on psychiatric symptoms, the broader literature on hormonal contraception indicates that most patients with psychiatric disorders generally report similar or lower rates of mood symptoms associated with their use.16 Some women treated with hormonal contraceptives do develop dysphoric mood,16 but any such effects resulting from LNG would likely be transient. Mood disruptions or other psychiatric symptoms have not been associated with UPA use.
How to prescribe oral emergency contraception
Who and when. Women of reproductive age should be counseled about EC as part of anticipatory guidance, regardless of their current intentions for sexual behaviors. Patients do not need a physical examination or pregnancy test before being prescribed or using oral EC.9 Much like how intranasal naloxone is prescribed, prescriptions should be provided in advance of need, with multiple refills to facilitate ready access when needed.
Continue to: Which to prescribe
Which to prescribe. UPA is more effective in preventing pregnancy than LNG at all time points up to 120 hours after sex, including for women who are overweight or obese.15 As such, it is recommended as the first-line choice. However, because LNG is available without prescription and is more readily available (including via online order), it may be a good choice for patients who need rapid EC or who prefer a medication that does not require a prescription (Table 24,5,8,9,15).
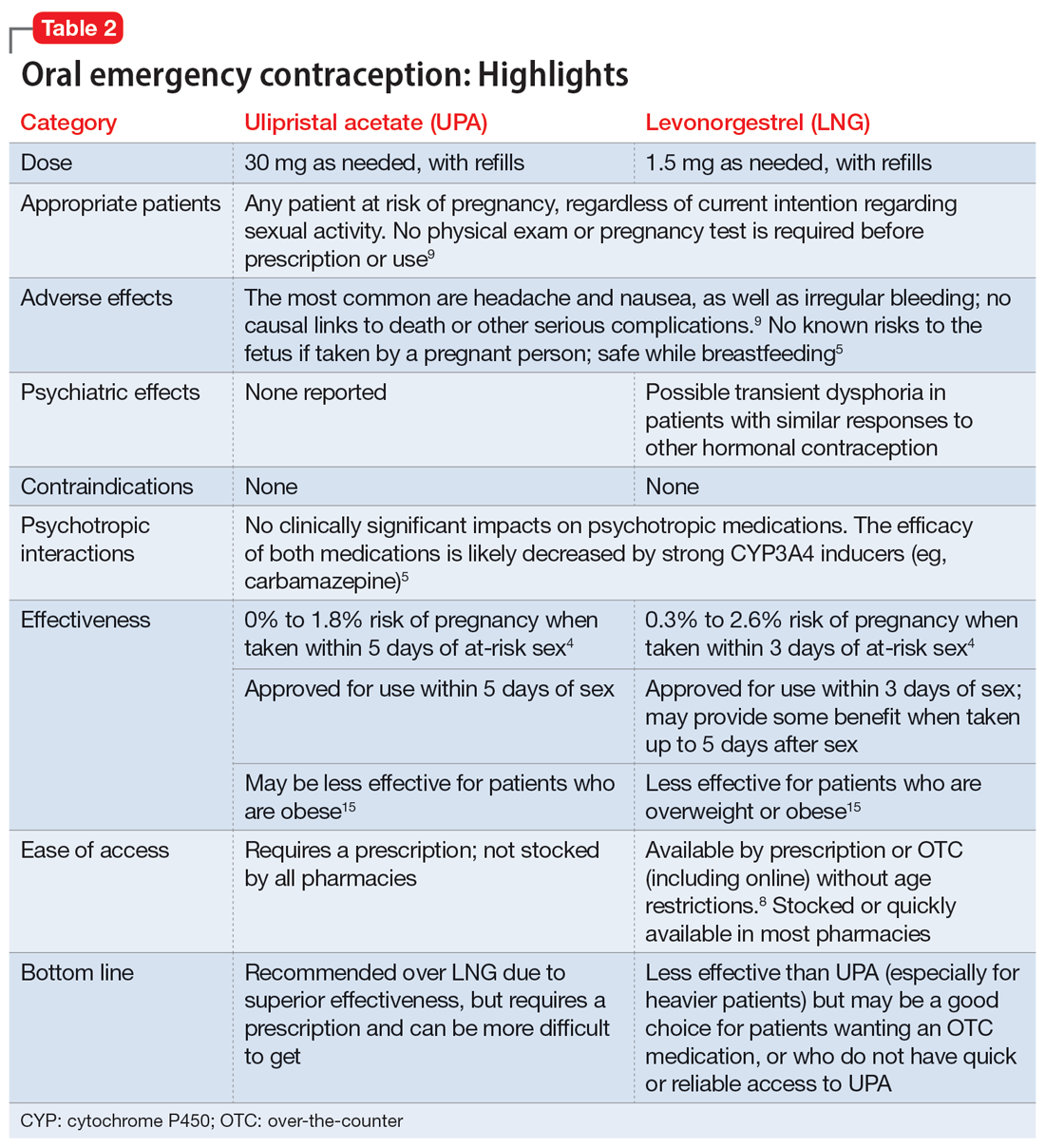
What to tell patients. Patients should be instructed to fill their prescription before they expect to use it, to ensure ready availability when desired (Table 35,9). Oral EC is shelf stable for at least 3 years when stored in a cool, dry environment. Patients should take the medication as soon as possible following at-risk sexual intercourse (Table 4). Tell them that if they vomit within 3 hours of taking the medication, they should take a second dose. Remind patients that EC does not protect against sexually transmitted infections, or from sex that occurs after the medication is taken (in fact, they can increase the possibility of pregnancy later in that menstrual cycle due to delayed ovulation).9 Counsel patients to abstain from sex or to use barrier contraception for 7 days after use. Those who take birth control pills can resume use immediately after using LNG; they should wait 5 days after taking UPA.
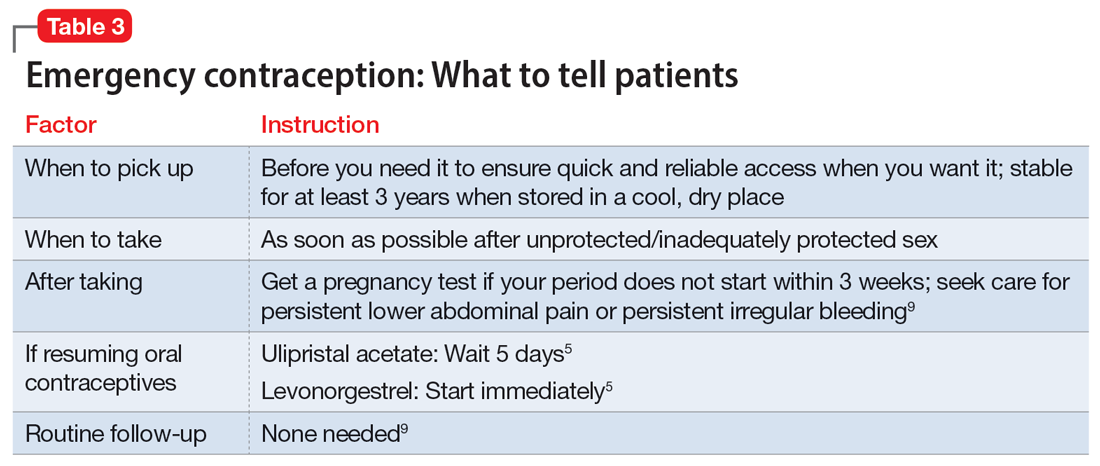
No routine follow-up is needed after taking UPA or LNG. However, patients should get a pregnancy test if their period does not start within 3 weeks, and should seek medical evaluation if they experience significant lower abdominal pain or persistent irregular bleeding in order to rule out pregnancy-related complications. Patients who use EC repeatedly should be recommended to pursue routine contraceptive care.
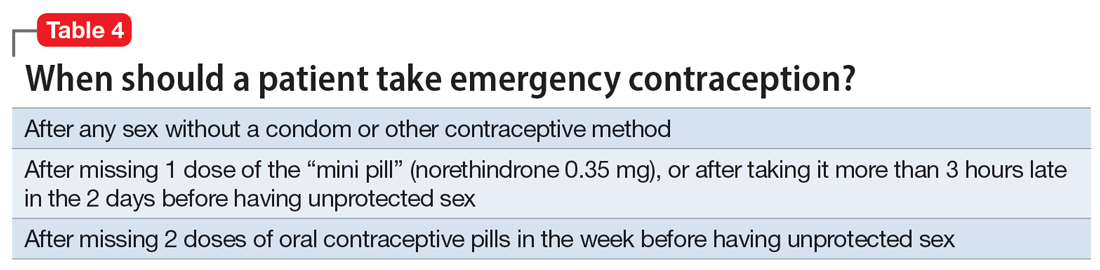
Billing. Counseling your patients about contraception can increase the reimbursement you receive by adding to the complexity of the encounter (regardless of whether you prescribe a medication) through use of the ICD-10 code Z30.0.
Emergency contraception for special populations
Some patients face additional challenges to effective EC that should be considered when counseling and prescribing. Table 54,5,7,15,17-21 discusses the use of EC in these special populations. Of particular importance for psychiatrists, LNG is less effective at preventing undesired pregnancy among patients who are overweight or obese,15,17,18 and strong CYP3A4-inducing agents may decrease the effectiveness of both LNG and UPA.5 Keep in mind, however, that the advantages of using either UPA or LNG outweigh the risks for all populations.5 Patients must be aware of appropriate information in order to make informed decisions, but should not be discouraged from using EC.
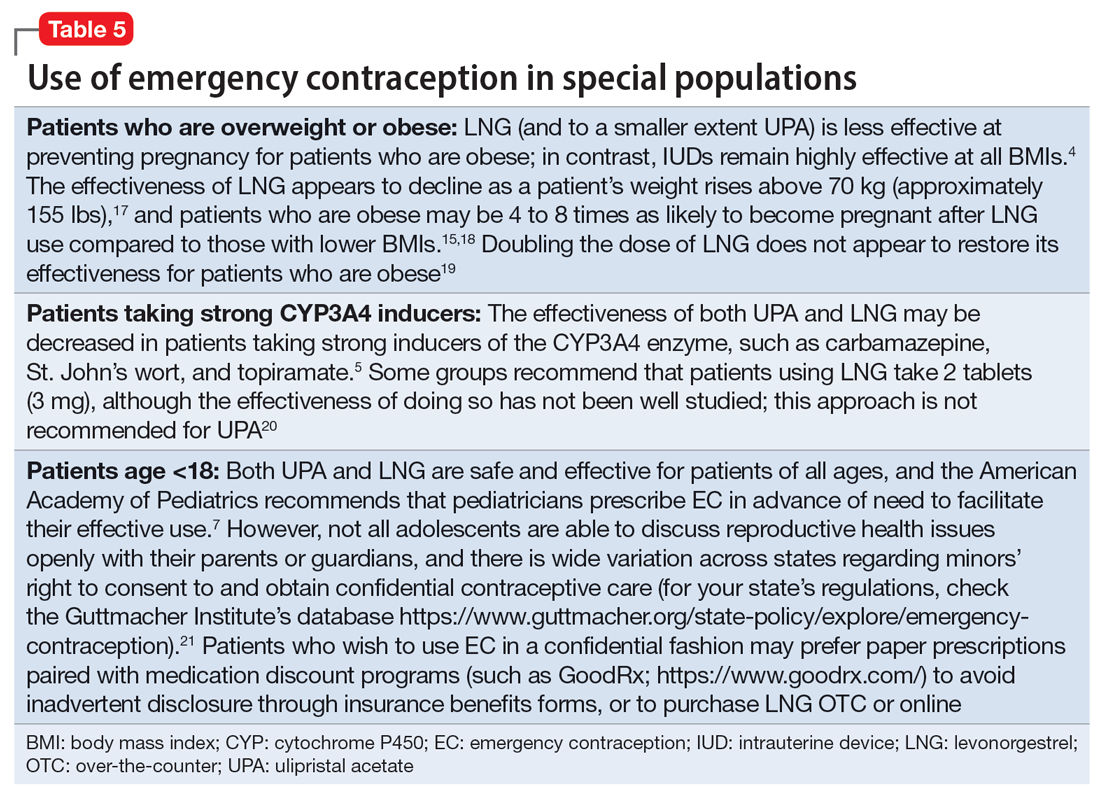
Continue to: Other groups of patients...
Other groups of patients may face barriers due to some clinicians’ hesitancy regarding their ability to consent to reproductive care. Most patients with psychiatric illnesses have decision-making capacity regarding reproductive issues.22 Although EC is supported by the American Academy of Pediatrics,7 patients age <18 have varying rights to consent across states,21 and merit special consideration.
CASE CONTINUED
Ms. A does not wish to get pregnant at this time, and expresses fears that her recent contraceptive failure could lead to an unintended pregnancy. In addition to her psychiatric treatment, her psychiatrist should discuss EC options with her. She has a healthy BMI and had inadequately protected sex <1 day ago, so her clinician may prescribe LNG (to ensure rapid access for immediate use) in addition to UPA for her to have available in case of future “scares.” The psychiatrist should consider pharmacologic treatment with an antidepressant with a relatively safe reproductive record (eg, sertraline).23 This is considered preventive ethics, since Ms. A is of reproductive age, even if she is not presently planning to get pregnant, due to the aforementioned high rate of unplanned pregnancy.23,24 It is also important for the psychiatrist to continue the dialogue in future sessions about preventing unintended pregnancy. Since Ms. A has benefited from a psychotropic medication when not pregnant, it will be important to discuss with her the risks and benefits of medication should she plan a pregnancy.
Bottom Line
Patients with mental illnesses are at increased risk of adverse outcomes resulting from unintended pregnancies. Clinicians should counsel patients about emergency contraception (EC) as a part of routine psychiatric care, and should prescribe oral EC in advance of patient need to facilitate effective use.
Related Resources
- American College of Obstetricians and Gynecologists Practice Bulletin on Emergency Contraception. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/ articles/2015/09/emergency-contraception
- State policies on emergency contraception. https://www.guttmacher.org/state-policy/explore/emergency-contraception
- State policies on minors’ access to contraceptive services. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
- Patient-oriented contraceptive education materials (in English and Spanish). https://shop.powertodecide.org/ptd-category/educational-materials
Drug Brand Names
Carbamazepine • Tegretol
Levonorgestrel • Plan B One-Step, Fallback
Metformin • Glucophage
Naloxone • Narcan
Norethindrone • Aygestin
Sertraline • Zoloft
Topiramate • Topamax
Ulipristal acetate • Ella
Venlafaxine • Effexor
1. Grossman D. Expanding access to short-acting hormonal contraceptive methods in the United States. JAMA Intern Med. 2019;179:1209-1210.
2. Gur TL, Kim DR, Epperson CN. Central nervous system effects of prenatal selective serotonin reuptake inhibitors: sensing the signal through the noise. Psychopharmacology (Berl). 2013;227:567-582.
3. Ross N, Landess J, Kaempf A, et al. Pregnancy termination: what psychiatrists need to know. Current Psychiatry. 2022;21:8-9.
4. Haeger KO, Lamme J, Cleland K. State of emergency contraception in the US, 2018. Contracept Reprod Med. 2018;3:20.
5. Curtis KM, Tepper NK, Jatlaoui TC, et al. US medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65:1-3.
6. American College of Obstetricians and Gynecologists. Committee Opinion No 707: Access to emergency contraception. Obstet Gynecol. 2017;130:e48-e52.
7. Upadhya KK, Breuner CC, Alderman EM, et al. Emergency contraception. Pediatrics. 2019;144:e20193149.
8. Rowan A. Obama administration yields to the courts and the evidence, allows emergency contraception to be sold without restrictions. Guttmacher Institute. Published June 25, 2013. Accessed July 31, 2022. https://www.guttmacher.org/gpr/2013/06/obama-administration-yields-courts-and-evidence-allows-emergency-contraception-be-sold#
9. American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
10. Rodriguez MI, Curtis KM, Gaffield ML, et al. Advance supply of emergency contraception: a systematic review. Contraception. 2013;87:590-601.
11. World Health Organization. Emergency contraception. Published November 9, 2021. Accessed August 4, 2022. https://www.who.int/news-room/fact-sheets/detail/emergency-contraception
12. Shigesato M, Elia J, Tschann M, et al. Pharmacy access to ulipristal acetate in major cities throughout the United States. Contraception. 2018;97:264-269.
13. Wilkinson TA, Clark P, Rafie S, et al. Access to emergency contraception after removal of age restrictions. Pediatrics. 2017;140:e20164262.
14. Cleland K, Bass J, Doci F, et al. Access to emergency contraception in the over-the-counter era. Women’s Health Issues. 2016;26:622-627.
15. Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet. 2010;375:555-562.
16. McCloskey LR, Wisner KL, Cattan MK, et al. Contraception for women with psychiatric disorders. Am J Psychiatry. 2021;178:247-255.
17. Kapp N, Abitbol JL, Mathé H, et al. Effect of body weight and BMI on the efficacy of levonorgestrel emergency contraception. Contraception. 2015;91:97-104.
18. Festin MP, Peregoudov A, Seuc A, et al. Effect of BMI and body weight on pregnancy rates with LNG as emergency contraception: analysis of four WHO HRP studies. Contraception. 2017;95:50-54.
19. Edelman AB, Hennebold JD, Bond K, et al. Double dosing levonorgestrel-based emergency contraception for individuals with obesity: a randomized controlled trial. Obstet Gynecol. 2022;140(1):48-54.
20. FSRH Clinical Effectiveness Unit. FSRH clinical guideline: Emergency contraception. Published March 2017. Amended December 2020. Faculty of Sexual & Reproductive Healthcare. Accessed August 4, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-emergency-contraception-march-2017/
21. Guttmacher Institute. Minors’ access to contraceptive services. Guttmacher Institute. Accessed August 4, 2022. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
22. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022;63:61-70.
23. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20:30-36.
24. Friedman SH. The ethics of treating depression in pregnancy. J Primary Healthcare. 2015;7:81-83.
1. Grossman D. Expanding access to short-acting hormonal contraceptive methods in the United States. JAMA Intern Med. 2019;179:1209-1210.
2. Gur TL, Kim DR, Epperson CN. Central nervous system effects of prenatal selective serotonin reuptake inhibitors: sensing the signal through the noise. Psychopharmacology (Berl). 2013;227:567-582.
3. Ross N, Landess J, Kaempf A, et al. Pregnancy termination: what psychiatrists need to know. Current Psychiatry. 2022;21:8-9.
4. Haeger KO, Lamme J, Cleland K. State of emergency contraception in the US, 2018. Contracept Reprod Med. 2018;3:20.
5. Curtis KM, Tepper NK, Jatlaoui TC, et al. US medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65:1-3.
6. American College of Obstetricians and Gynecologists. Committee Opinion No 707: Access to emergency contraception. Obstet Gynecol. 2017;130:e48-e52.
7. Upadhya KK, Breuner CC, Alderman EM, et al. Emergency contraception. Pediatrics. 2019;144:e20193149.
8. Rowan A. Obama administration yields to the courts and the evidence, allows emergency contraception to be sold without restrictions. Guttmacher Institute. Published June 25, 2013. Accessed July 31, 2022. https://www.guttmacher.org/gpr/2013/06/obama-administration-yields-courts-and-evidence-allows-emergency-contraception-be-sold#
9. American College of Obstetricians and Gynecologists. Practice Bulletin No. 152: Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
10. Rodriguez MI, Curtis KM, Gaffield ML, et al. Advance supply of emergency contraception: a systematic review. Contraception. 2013;87:590-601.
11. World Health Organization. Emergency contraception. Published November 9, 2021. Accessed August 4, 2022. https://www.who.int/news-room/fact-sheets/detail/emergency-contraception
12. Shigesato M, Elia J, Tschann M, et al. Pharmacy access to ulipristal acetate in major cities throughout the United States. Contraception. 2018;97:264-269.
13. Wilkinson TA, Clark P, Rafie S, et al. Access to emergency contraception after removal of age restrictions. Pediatrics. 2017;140:e20164262.
14. Cleland K, Bass J, Doci F, et al. Access to emergency contraception in the over-the-counter era. Women’s Health Issues. 2016;26:622-627.
15. Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet. 2010;375:555-562.
16. McCloskey LR, Wisner KL, Cattan MK, et al. Contraception for women with psychiatric disorders. Am J Psychiatry. 2021;178:247-255.
17. Kapp N, Abitbol JL, Mathé H, et al. Effect of body weight and BMI on the efficacy of levonorgestrel emergency contraception. Contraception. 2015;91:97-104.
18. Festin MP, Peregoudov A, Seuc A, et al. Effect of BMI and body weight on pregnancy rates with LNG as emergency contraception: analysis of four WHO HRP studies. Contraception. 2017;95:50-54.
19. Edelman AB, Hennebold JD, Bond K, et al. Double dosing levonorgestrel-based emergency contraception for individuals with obesity: a randomized controlled trial. Obstet Gynecol. 2022;140(1):48-54.
20. FSRH Clinical Effectiveness Unit. FSRH clinical guideline: Emergency contraception. Published March 2017. Amended December 2020. Faculty of Sexual & Reproductive Healthcare. Accessed August 4, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-emergency-contraception-march-2017/
21. Guttmacher Institute. Minors’ access to contraceptive services. Guttmacher Institute. Accessed August 4, 2022. https://www.guttmacher.org/state-policy/explore/minors-access-contraceptive-services
22. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022;63:61-70.
23. Friedman SH, Hall RCW. Avoiding malpractice while treating depression in pregnant women. Current Psychiatry. 2021;20:30-36.
24. Friedman SH. The ethics of treating depression in pregnancy. J Primary Healthcare. 2015;7:81-83.
Pregnancy termination: What psychiatrists need to know
Approximately half of pregnancies in the United States are unplanned, and approximately one-fifth of pregnancies end in elective termination.1 Psychiatrists who treat women of childbearing potential should understand critical aspects of abortion that could affect their patients’ mental health.
Discuss the potential for pregnancy with your patients. Individuals with psychiatric illness are less likely to adhere to contraceptive methods and are more likely to have unplanned pregnancies and detect pregnancies late.2 Women receiving psychiatric care could be at risk of not detecting pregnancy early enough to meet state laws that restrict the time frames in which abortions are allowed.
Understand that patients face barriers to abortion. Almost immediately after the Supreme Court overturned Roe v Wade in June 2022, abortion became illegal in several states. Even if abortion remains legal and available in your jurisdiction, patients could face barriers, including strict limits on abortion timing, monetary and travel challenges, preabortion counseling mandates, and timely access to an abortion provider.
Know that most patients can provide informed consent. Most patients with psychiatric illness have capacity to make medical decisions, including whether to consent to an abortion. Pro forma assessment is not necessary. Assessing capacity to consent to abortion should be the same as any other capacity assessment. If a woman lacks medical decision-making capacity, a substitute decision-maker must be used.
Recognize that ambivalence is normal. Even when a woman is certain about her decision to terminate a pregnancy, she might experience ambivalence. Ambivalence about important life decisions is common and should be validated and explored.3
Be aware of bias. As psychiatrists, we must ensure that our personal opinions about abortion do not impact patient care. An impartial and nondirective approach is key, and any effort to persuade or manipulate a woman’s decision is unethical. Because women with mental illness might be vulnerable to coercion, it is important to ensure that the woman’s choice is voluntary.
Accurately communicate information about mental health and abortion to your patients. Abortion does not worsen mental health. Research on abortion and mental health is rife with poorly designed studies that contain methodological flaws, including failure to control for confounding effects, such as pre-existing mental illness, and inadequate control group comparisons.4 For example, the correct comparison group in which to consider mental health outcomes for women who are seeking an abortion is those who sought an abortion but were not able to have one—not women with planned and desired pregnancies. The best predictor of postabortion mental wellness is preabortion mental health.5 Well-designed studies, such as the Turnaway Study, have demonstrated that abortion does not cause a significant increase in mental illness.6 The Turnaway Study was a well-designed, prospective study of thousands of women who obtained a wanted abortion. It compared many outcomes, including mental health, among women who wanted an abortion vs women who could not obtain a wanted abortion.
Continue to: Know that patients might not receive accurate information about the risks and impact of abortion
Know that patients might not receive accurate information about the risks and impact of abortion. A number of states have requirements—known as “informed consent laws”—that mandate physicians to provide state-authored informational packets about the risks and alternatives to abortion to patients seeking abortions. Some of this information is scientifically inaccurate, which poses a significant ethical dilemma for doctors who must choose between legal requirements and an obligation to scientific integrity.7
Recognize that abortion being illegal could negatively impact mental health. The consequences of being forced to carry out an unwanted pregnancy are profound. Women unable to obtain an abortion are more likely to have adverse health and pregnancy outcomes, live in poverty, stay with an abusive partner, and have difficulty bonding with the child.6 Abortion is highly stigmatized in the United States, and belonging to a stigmatized group is a risk factor for adverse mental health sequalae, including anxiety, depression, substance use, and cognitive deficits.4-6
Stay up-to-date on your state’s abortion laws. The legal landscape regarding abortion is changing rapidly, and it is important to stay abreast of these changes.
Restrictions on abortion likely will significantly affect women with psychiatric illness. As psychiatrists, we must be aware of the impact of the country’s changing laws will have on our patients and their mental health.
1. Guttmacher Institute. Accessed July 21, 2022. https://www.guttmacher.org/
2. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635. doi:10.1093/schbul/23.4.623
3. Brody BD, Chaudhry SK, Penzner JB, et al. A woman with major depression with psychotic features requesting a termination of pregnancy. Am J Psychiatry. 2016;173(1):12-15. doi:10.1176/appi.ajp.2015.15030380
4. Major B, Appelbaum M, Beckman L, et al. Abortion and mental health: Evaluating the evidence. Am Psychol. 2009;64(9):863-890. doi:10.1037/a0017497
5. Steinberg JR, Tschann JM, Furgerson D, et al. Psychosocial factors and pre-abortion psychological health: the significance of stigma. Soc Sci Med. 2016;150:67-75. doi:10.1016/j.socscimed.2015.12.007
6. ANSIRH. The Turnaway Study. Accessed June 29, 2022. https://www.ansirh.org/research/ongoing/turnaway-study
7. Daniels CR, Ferguson J, Howard G, et al. Informed or misinformed consent? Abortion policy in the United States. J Health Polit Policy Law. 2016;41(2):181-209. doi:10.1215/03616878-3476105
Approximately half of pregnancies in the United States are unplanned, and approximately one-fifth of pregnancies end in elective termination.1 Psychiatrists who treat women of childbearing potential should understand critical aspects of abortion that could affect their patients’ mental health.
Discuss the potential for pregnancy with your patients. Individuals with psychiatric illness are less likely to adhere to contraceptive methods and are more likely to have unplanned pregnancies and detect pregnancies late.2 Women receiving psychiatric care could be at risk of not detecting pregnancy early enough to meet state laws that restrict the time frames in which abortions are allowed.
Understand that patients face barriers to abortion. Almost immediately after the Supreme Court overturned Roe v Wade in June 2022, abortion became illegal in several states. Even if abortion remains legal and available in your jurisdiction, patients could face barriers, including strict limits on abortion timing, monetary and travel challenges, preabortion counseling mandates, and timely access to an abortion provider.
Know that most patients can provide informed consent. Most patients with psychiatric illness have capacity to make medical decisions, including whether to consent to an abortion. Pro forma assessment is not necessary. Assessing capacity to consent to abortion should be the same as any other capacity assessment. If a woman lacks medical decision-making capacity, a substitute decision-maker must be used.
Recognize that ambivalence is normal. Even when a woman is certain about her decision to terminate a pregnancy, she might experience ambivalence. Ambivalence about important life decisions is common and should be validated and explored.3
Be aware of bias. As psychiatrists, we must ensure that our personal opinions about abortion do not impact patient care. An impartial and nondirective approach is key, and any effort to persuade or manipulate a woman’s decision is unethical. Because women with mental illness might be vulnerable to coercion, it is important to ensure that the woman’s choice is voluntary.
Accurately communicate information about mental health and abortion to your patients. Abortion does not worsen mental health. Research on abortion and mental health is rife with poorly designed studies that contain methodological flaws, including failure to control for confounding effects, such as pre-existing mental illness, and inadequate control group comparisons.4 For example, the correct comparison group in which to consider mental health outcomes for women who are seeking an abortion is those who sought an abortion but were not able to have one—not women with planned and desired pregnancies. The best predictor of postabortion mental wellness is preabortion mental health.5 Well-designed studies, such as the Turnaway Study, have demonstrated that abortion does not cause a significant increase in mental illness.6 The Turnaway Study was a well-designed, prospective study of thousands of women who obtained a wanted abortion. It compared many outcomes, including mental health, among women who wanted an abortion vs women who could not obtain a wanted abortion.
Continue to: Know that patients might not receive accurate information about the risks and impact of abortion
Know that patients might not receive accurate information about the risks and impact of abortion. A number of states have requirements—known as “informed consent laws”—that mandate physicians to provide state-authored informational packets about the risks and alternatives to abortion to patients seeking abortions. Some of this information is scientifically inaccurate, which poses a significant ethical dilemma for doctors who must choose between legal requirements and an obligation to scientific integrity.7
Recognize that abortion being illegal could negatively impact mental health. The consequences of being forced to carry out an unwanted pregnancy are profound. Women unable to obtain an abortion are more likely to have adverse health and pregnancy outcomes, live in poverty, stay with an abusive partner, and have difficulty bonding with the child.6 Abortion is highly stigmatized in the United States, and belonging to a stigmatized group is a risk factor for adverse mental health sequalae, including anxiety, depression, substance use, and cognitive deficits.4-6
Stay up-to-date on your state’s abortion laws. The legal landscape regarding abortion is changing rapidly, and it is important to stay abreast of these changes.
Restrictions on abortion likely will significantly affect women with psychiatric illness. As psychiatrists, we must be aware of the impact of the country’s changing laws will have on our patients and their mental health.
Approximately half of pregnancies in the United States are unplanned, and approximately one-fifth of pregnancies end in elective termination.1 Psychiatrists who treat women of childbearing potential should understand critical aspects of abortion that could affect their patients’ mental health.
Discuss the potential for pregnancy with your patients. Individuals with psychiatric illness are less likely to adhere to contraceptive methods and are more likely to have unplanned pregnancies and detect pregnancies late.2 Women receiving psychiatric care could be at risk of not detecting pregnancy early enough to meet state laws that restrict the time frames in which abortions are allowed.
Understand that patients face barriers to abortion. Almost immediately after the Supreme Court overturned Roe v Wade in June 2022, abortion became illegal in several states. Even if abortion remains legal and available in your jurisdiction, patients could face barriers, including strict limits on abortion timing, monetary and travel challenges, preabortion counseling mandates, and timely access to an abortion provider.
Know that most patients can provide informed consent. Most patients with psychiatric illness have capacity to make medical decisions, including whether to consent to an abortion. Pro forma assessment is not necessary. Assessing capacity to consent to abortion should be the same as any other capacity assessment. If a woman lacks medical decision-making capacity, a substitute decision-maker must be used.
Recognize that ambivalence is normal. Even when a woman is certain about her decision to terminate a pregnancy, she might experience ambivalence. Ambivalence about important life decisions is common and should be validated and explored.3
Be aware of bias. As psychiatrists, we must ensure that our personal opinions about abortion do not impact patient care. An impartial and nondirective approach is key, and any effort to persuade or manipulate a woman’s decision is unethical. Because women with mental illness might be vulnerable to coercion, it is important to ensure that the woman’s choice is voluntary.
Accurately communicate information about mental health and abortion to your patients. Abortion does not worsen mental health. Research on abortion and mental health is rife with poorly designed studies that contain methodological flaws, including failure to control for confounding effects, such as pre-existing mental illness, and inadequate control group comparisons.4 For example, the correct comparison group in which to consider mental health outcomes for women who are seeking an abortion is those who sought an abortion but were not able to have one—not women with planned and desired pregnancies. The best predictor of postabortion mental wellness is preabortion mental health.5 Well-designed studies, such as the Turnaway Study, have demonstrated that abortion does not cause a significant increase in mental illness.6 The Turnaway Study was a well-designed, prospective study of thousands of women who obtained a wanted abortion. It compared many outcomes, including mental health, among women who wanted an abortion vs women who could not obtain a wanted abortion.
Continue to: Know that patients might not receive accurate information about the risks and impact of abortion
Know that patients might not receive accurate information about the risks and impact of abortion. A number of states have requirements—known as “informed consent laws”—that mandate physicians to provide state-authored informational packets about the risks and alternatives to abortion to patients seeking abortions. Some of this information is scientifically inaccurate, which poses a significant ethical dilemma for doctors who must choose between legal requirements and an obligation to scientific integrity.7
Recognize that abortion being illegal could negatively impact mental health. The consequences of being forced to carry out an unwanted pregnancy are profound. Women unable to obtain an abortion are more likely to have adverse health and pregnancy outcomes, live in poverty, stay with an abusive partner, and have difficulty bonding with the child.6 Abortion is highly stigmatized in the United States, and belonging to a stigmatized group is a risk factor for adverse mental health sequalae, including anxiety, depression, substance use, and cognitive deficits.4-6
Stay up-to-date on your state’s abortion laws. The legal landscape regarding abortion is changing rapidly, and it is important to stay abreast of these changes.
Restrictions on abortion likely will significantly affect women with psychiatric illness. As psychiatrists, we must be aware of the impact of the country’s changing laws will have on our patients and their mental health.
1. Guttmacher Institute. Accessed July 21, 2022. https://www.guttmacher.org/
2. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635. doi:10.1093/schbul/23.4.623
3. Brody BD, Chaudhry SK, Penzner JB, et al. A woman with major depression with psychotic features requesting a termination of pregnancy. Am J Psychiatry. 2016;173(1):12-15. doi:10.1176/appi.ajp.2015.15030380
4. Major B, Appelbaum M, Beckman L, et al. Abortion and mental health: Evaluating the evidence. Am Psychol. 2009;64(9):863-890. doi:10.1037/a0017497
5. Steinberg JR, Tschann JM, Furgerson D, et al. Psychosocial factors and pre-abortion psychological health: the significance of stigma. Soc Sci Med. 2016;150:67-75. doi:10.1016/j.socscimed.2015.12.007
6. ANSIRH. The Turnaway Study. Accessed June 29, 2022. https://www.ansirh.org/research/ongoing/turnaway-study
7. Daniels CR, Ferguson J, Howard G, et al. Informed or misinformed consent? Abortion policy in the United States. J Health Polit Policy Law. 2016;41(2):181-209. doi:10.1215/03616878-3476105
1. Guttmacher Institute. Accessed July 21, 2022. https://www.guttmacher.org/
2. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635. doi:10.1093/schbul/23.4.623
3. Brody BD, Chaudhry SK, Penzner JB, et al. A woman with major depression with psychotic features requesting a termination of pregnancy. Am J Psychiatry. 2016;173(1):12-15. doi:10.1176/appi.ajp.2015.15030380
4. Major B, Appelbaum M, Beckman L, et al. Abortion and mental health: Evaluating the evidence. Am Psychol. 2009;64(9):863-890. doi:10.1037/a0017497
5. Steinberg JR, Tschann JM, Furgerson D, et al. Psychosocial factors and pre-abortion psychological health: the significance of stigma. Soc Sci Med. 2016;150:67-75. doi:10.1016/j.socscimed.2015.12.007
6. ANSIRH. The Turnaway Study. Accessed June 29, 2022. https://www.ansirh.org/research/ongoing/turnaway-study
7. Daniels CR, Ferguson J, Howard G, et al. Informed or misinformed consent? Abortion policy in the United States. J Health Polit Policy Law. 2016;41(2):181-209. doi:10.1215/03616878-3476105
Managing bipolar disorder in women who are pregnant
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
Honor thy parents? Understanding parricide and associated spree killings
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
Avoiding malpractice while treating depression in pregnant women
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Treating psychosis in pregnant women: A measured approach
The peak age of onset of schizophrenia coincides with the peak childbearing age of 25 to 35 years.1 So it would not be unusual for your patient with schizophrenia to tell you she is trying to get pregnant, or thinks she might be pregnant. In these situations, you must carefully weigh the risks to the mother (eg, relapse, complications) and to the fetus (eg, possible miscarriage, teratogenesis) when deciding whether to continue or change her treatment regimen. When faced with making these decisions, keep the following factors in mind.
1. Most importantly: Do not make knee-jerk changes. Do not suddenly stop medications. Proceed in a thoughtful and measured way.
2. Discuss the risks with your patient. There is no such thing as a risk-free decision. There are potential risks from untreated psychosis as well as from medications. Mothers with untreated psychosis have an increased risk of suicide and violence, as well as poor self-care. Schizophrenia may be associated with an increased risk of poor birth outcomes, including preterm delivery, low birthweight, and neonatal complications.2 Avoid making absolute statements about specific medications during pregnancy; there needs to be an individualized risk-benefit discussion for each patient, and for each medication.
3. Involve the patient’s partner and family in treatment planning if possible. The patient’s family can be important in promoting mental health during pregnancy and the postpartum. Educating the family as well as the patient regarding medications and the risks of untreated mental illness can go a long way toward compliance.
4. Do not rely on what pregnancy category a medication was. There are multiple dimensions to evaluate when considering the use of an antipsychotic agent during pregnancy. Does it increase the risk of miscarriage? Malformations? Preterm birth? Perinatal toxicity? Behavioral teratogenesis (neurodevelopmental sequelae)? Looking for a simple summary or single letter grade minimizes the understanding of the specific outcome of concern in the specific mother. Instead, look at the Pregnancy section under Use in Specific Populations on the medication’s package insert (prescribing information), consult a web site such as MotherToBaby (mothertobaby.org/healthcare-professionals/), and/or search for the latest research on PubMed.
5. Collaborate with the patient’s obstetrician or family medicine physician. Make sure that you are on the same page regarding treating the patient’s psychosis. Other clinicians often will agree with your treatment plan because they understand the risks of untreated psychosis compared with other risks the patient is facing. However, if you don’t communicate with your patient’s other health care professionals, she might receive mixed messages.
6. As for medication choice, pregnancy is the most important time to conduct a careful medication history to inform your choice of medication. Was Medication X ineffective, or did the patient not pick it up from the pharmacy? Did she really have a trial of 3 months, or did she only take it for a week before she decided to stop?
Continue to: Determine which medication has worked for the patient in the past
7. Determine which medication has worked for the patient in the past. If Medication Y worked before she was pregnant, it is likely to still work during pregnancy. If it is a relatively safe option, it may be the best choice.
8. Avoid multiple medication exposures wherever possible. If a patient is taking Medication Z, it is working, and she tells you she is 3 months pregnant, it is often better to continue it (assuming it is a relatively safe medication) than to switch to Medication A, which has slightly better “safety data.” By switching to a different antipsychotic, you would be exposing the fetus to a second agent that may not even work for the mother.
9. Focus on treating the patient’s present symptoms. Medication doses may need to change due to pregnancy-related changes in symptoms, drug distribution, and/or metabolism.
10. Remain vigilant for other risks. Keep in mind that pregnant women with psychosis often face risks other than psychiatric medications and psychosis. Comorbidities such as substance use disorders, obesity, and poor prenatal care must also be addressed.3
11. Follow your patient more closely during pregnancy. Pregnancy is an uncertain time for any new mother. Be sure to have an open line of communication with the patient, and be responsive to her concerns.
Continue to: Provide psychoeducation about the postpartum period
12. Provide psychoeducation about the postpartum period. Pregnancy is the time to educate your patient about the importance of sleep, warning signs of exacerbation of psychosis, and breastfeeding safety.
13. Be proactive with future female patients of childbearing age, regardless of whether they tell you they are sexually active. Women with psychosis have higher rates of unplanned pregnancy.3,4 When initiating treatment of psychosis in a woman of childbearing age, rather than treating her with the newest available medication that does not yet have safety data in pregnancy, it is best to start with a medication already known to be relatively safe in pregnancy. This way, if she were to become pregnant, your treatment plan would already be safe and appropriate.
14. Consult a reproductive psychiatrist if needed.
1. Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15(3):183-192.
2. Galbally M, Crabb C. Schizophrenia and psychotic disorders. O&G. 2018;20(3). https://www.ogmagazine.org.au/20/3-20/schizophrenia-and-psychotic-disorders/
3. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635.
4. Friedman SH, Hall RCW, Sorrentino RM. Involuntary treatment of psychosis in pregnancy. J Am Acad Psychiatry Law. 2018;46(2):217-223.
The peak age of onset of schizophrenia coincides with the peak childbearing age of 25 to 35 years.1 So it would not be unusual for your patient with schizophrenia to tell you she is trying to get pregnant, or thinks she might be pregnant. In these situations, you must carefully weigh the risks to the mother (eg, relapse, complications) and to the fetus (eg, possible miscarriage, teratogenesis) when deciding whether to continue or change her treatment regimen. When faced with making these decisions, keep the following factors in mind.
1. Most importantly: Do not make knee-jerk changes. Do not suddenly stop medications. Proceed in a thoughtful and measured way.
2. Discuss the risks with your patient. There is no such thing as a risk-free decision. There are potential risks from untreated psychosis as well as from medications. Mothers with untreated psychosis have an increased risk of suicide and violence, as well as poor self-care. Schizophrenia may be associated with an increased risk of poor birth outcomes, including preterm delivery, low birthweight, and neonatal complications.2 Avoid making absolute statements about specific medications during pregnancy; there needs to be an individualized risk-benefit discussion for each patient, and for each medication.
3. Involve the patient’s partner and family in treatment planning if possible. The patient’s family can be important in promoting mental health during pregnancy and the postpartum. Educating the family as well as the patient regarding medications and the risks of untreated mental illness can go a long way toward compliance.
4. Do not rely on what pregnancy category a medication was. There are multiple dimensions to evaluate when considering the use of an antipsychotic agent during pregnancy. Does it increase the risk of miscarriage? Malformations? Preterm birth? Perinatal toxicity? Behavioral teratogenesis (neurodevelopmental sequelae)? Looking for a simple summary or single letter grade minimizes the understanding of the specific outcome of concern in the specific mother. Instead, look at the Pregnancy section under Use in Specific Populations on the medication’s package insert (prescribing information), consult a web site such as MotherToBaby (mothertobaby.org/healthcare-professionals/), and/or search for the latest research on PubMed.
5. Collaborate with the patient’s obstetrician or family medicine physician. Make sure that you are on the same page regarding treating the patient’s psychosis. Other clinicians often will agree with your treatment plan because they understand the risks of untreated psychosis compared with other risks the patient is facing. However, if you don’t communicate with your patient’s other health care professionals, she might receive mixed messages.
6. As for medication choice, pregnancy is the most important time to conduct a careful medication history to inform your choice of medication. Was Medication X ineffective, or did the patient not pick it up from the pharmacy? Did she really have a trial of 3 months, or did she only take it for a week before she decided to stop?
Continue to: Determine which medication has worked for the patient in the past
7. Determine which medication has worked for the patient in the past. If Medication Y worked before she was pregnant, it is likely to still work during pregnancy. If it is a relatively safe option, it may be the best choice.
8. Avoid multiple medication exposures wherever possible. If a patient is taking Medication Z, it is working, and she tells you she is 3 months pregnant, it is often better to continue it (assuming it is a relatively safe medication) than to switch to Medication A, which has slightly better “safety data.” By switching to a different antipsychotic, you would be exposing the fetus to a second agent that may not even work for the mother.
9. Focus on treating the patient’s present symptoms. Medication doses may need to change due to pregnancy-related changes in symptoms, drug distribution, and/or metabolism.
10. Remain vigilant for other risks. Keep in mind that pregnant women with psychosis often face risks other than psychiatric medications and psychosis. Comorbidities such as substance use disorders, obesity, and poor prenatal care must also be addressed.3
11. Follow your patient more closely during pregnancy. Pregnancy is an uncertain time for any new mother. Be sure to have an open line of communication with the patient, and be responsive to her concerns.
Continue to: Provide psychoeducation about the postpartum period
12. Provide psychoeducation about the postpartum period. Pregnancy is the time to educate your patient about the importance of sleep, warning signs of exacerbation of psychosis, and breastfeeding safety.
13. Be proactive with future female patients of childbearing age, regardless of whether they tell you they are sexually active. Women with psychosis have higher rates of unplanned pregnancy.3,4 When initiating treatment of psychosis in a woman of childbearing age, rather than treating her with the newest available medication that does not yet have safety data in pregnancy, it is best to start with a medication already known to be relatively safe in pregnancy. This way, if she were to become pregnant, your treatment plan would already be safe and appropriate.
14. Consult a reproductive psychiatrist if needed.
The peak age of onset of schizophrenia coincides with the peak childbearing age of 25 to 35 years.1 So it would not be unusual for your patient with schizophrenia to tell you she is trying to get pregnant, or thinks she might be pregnant. In these situations, you must carefully weigh the risks to the mother (eg, relapse, complications) and to the fetus (eg, possible miscarriage, teratogenesis) when deciding whether to continue or change her treatment regimen. When faced with making these decisions, keep the following factors in mind.
1. Most importantly: Do not make knee-jerk changes. Do not suddenly stop medications. Proceed in a thoughtful and measured way.
2. Discuss the risks with your patient. There is no such thing as a risk-free decision. There are potential risks from untreated psychosis as well as from medications. Mothers with untreated psychosis have an increased risk of suicide and violence, as well as poor self-care. Schizophrenia may be associated with an increased risk of poor birth outcomes, including preterm delivery, low birthweight, and neonatal complications.2 Avoid making absolute statements about specific medications during pregnancy; there needs to be an individualized risk-benefit discussion for each patient, and for each medication.
3. Involve the patient’s partner and family in treatment planning if possible. The patient’s family can be important in promoting mental health during pregnancy and the postpartum. Educating the family as well as the patient regarding medications and the risks of untreated mental illness can go a long way toward compliance.
4. Do not rely on what pregnancy category a medication was. There are multiple dimensions to evaluate when considering the use of an antipsychotic agent during pregnancy. Does it increase the risk of miscarriage? Malformations? Preterm birth? Perinatal toxicity? Behavioral teratogenesis (neurodevelopmental sequelae)? Looking for a simple summary or single letter grade minimizes the understanding of the specific outcome of concern in the specific mother. Instead, look at the Pregnancy section under Use in Specific Populations on the medication’s package insert (prescribing information), consult a web site such as MotherToBaby (mothertobaby.org/healthcare-professionals/), and/or search for the latest research on PubMed.
5. Collaborate with the patient’s obstetrician or family medicine physician. Make sure that you are on the same page regarding treating the patient’s psychosis. Other clinicians often will agree with your treatment plan because they understand the risks of untreated psychosis compared with other risks the patient is facing. However, if you don’t communicate with your patient’s other health care professionals, she might receive mixed messages.
6. As for medication choice, pregnancy is the most important time to conduct a careful medication history to inform your choice of medication. Was Medication X ineffective, or did the patient not pick it up from the pharmacy? Did she really have a trial of 3 months, or did she only take it for a week before she decided to stop?
Continue to: Determine which medication has worked for the patient in the past
7. Determine which medication has worked for the patient in the past. If Medication Y worked before she was pregnant, it is likely to still work during pregnancy. If it is a relatively safe option, it may be the best choice.
8. Avoid multiple medication exposures wherever possible. If a patient is taking Medication Z, it is working, and she tells you she is 3 months pregnant, it is often better to continue it (assuming it is a relatively safe medication) than to switch to Medication A, which has slightly better “safety data.” By switching to a different antipsychotic, you would be exposing the fetus to a second agent that may not even work for the mother.
9. Focus on treating the patient’s present symptoms. Medication doses may need to change due to pregnancy-related changes in symptoms, drug distribution, and/or metabolism.
10. Remain vigilant for other risks. Keep in mind that pregnant women with psychosis often face risks other than psychiatric medications and psychosis. Comorbidities such as substance use disorders, obesity, and poor prenatal care must also be addressed.3
11. Follow your patient more closely during pregnancy. Pregnancy is an uncertain time for any new mother. Be sure to have an open line of communication with the patient, and be responsive to her concerns.
Continue to: Provide psychoeducation about the postpartum period
12. Provide psychoeducation about the postpartum period. Pregnancy is the time to educate your patient about the importance of sleep, warning signs of exacerbation of psychosis, and breastfeeding safety.
13. Be proactive with future female patients of childbearing age, regardless of whether they tell you they are sexually active. Women with psychosis have higher rates of unplanned pregnancy.3,4 When initiating treatment of psychosis in a woman of childbearing age, rather than treating her with the newest available medication that does not yet have safety data in pregnancy, it is best to start with a medication already known to be relatively safe in pregnancy. This way, if she were to become pregnant, your treatment plan would already be safe and appropriate.
14. Consult a reproductive psychiatrist if needed.
1. Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15(3):183-192.
2. Galbally M, Crabb C. Schizophrenia and psychotic disorders. O&G. 2018;20(3). https://www.ogmagazine.org.au/20/3-20/schizophrenia-and-psychotic-disorders/
3. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635.
4. Friedman SH, Hall RCW, Sorrentino RM. Involuntary treatment of psychosis in pregnancy. J Am Acad Psychiatry Law. 2018;46(2):217-223.
1. Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15(3):183-192.
2. Galbally M, Crabb C. Schizophrenia and psychotic disorders. O&G. 2018;20(3). https://www.ogmagazine.org.au/20/3-20/schizophrenia-and-psychotic-disorders/
3. Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull. 1997;23(4):623-635.
4. Friedman SH, Hall RCW, Sorrentino RM. Involuntary treatment of psychosis in pregnancy. J Am Acad Psychiatry Law. 2018;46(2):217-223.
‘The Undoing’: A dramatization of ‘You Should Have Known’
Jean Hanff Korelitz’s ironic psychological thriller, “You Should Have Known,” (New York: Grand Central Publishing, 2014) was transformed into an HBO miniseries called “The Undoing,” written and produced by David E. Kelley and directed by Susanne Bier, which premiered on Oct. 25, 2020.
The television drama differed from the novel in fundamental ways, but both have themes related to the therapeutic process. In the novel, a New York City–based couples therapist, Grace Reinhart Sachs, had recently written a book called “You Should Have Known,” about women who married their spouses disregarding their gut instinct that their partner was not fundamentally right for them, or might potentially cheat on them, or whose stories contained contradictions. In the miniseries, Grace (played by Nicole Kidman), is a therapist but there is no mention of her having written a book. Grace in both the novel and the miniseries is married to a pediatric oncologist, Jonathan (his ethnicity and surname were changed in the miniseries from a Jewish New Yorker in the novel to a British Dr. Jonathan Fraser in the series, played by Hugh Grant).
[Spoiler alert]: Prepandemic New York City’s Upper East Side is scandalized when a murdered mother is found by her young son the day after a lavish fund-raising auction party for a private school. Grace and Jonathan’s son, Henry, attends this school as well, and Grace had served on the auction committee with the murdered mother. When two detectives question Grace in the course of their investigation, she assumes that they are questioning her as they would any parent in the school. However, when she tries to reach her husband about the news and the investigation, she cannot. She thought he was at a medical conference in Cleveland, but she realizes that she does not know exactly what conference and exactly where. After many failed attempts at calling and texting, she hears a familiar alert sound coming from his nightstand drawer where she retrieves the cell phone that had been deliberately placed.
In the novel, Jonathan never reappears from “Cleveland,” and although it takes Grace a while to understand that her husband is not who she thought he was, she eventually does. In the miniseries, Jonathan appears in their lake house and a trial ensues with Jonathan adamantly proclaiming his innocence despite all evidence to the contrary.
The Oxford Reference defines undoing as “an emotional conflict associated with an action is dealt with by negating the action or attempting ‘magically’ to cause it not to have occurred by substituting an approximately opposite action.” It is not that the consequences of the action are attempted to be negated (as in making amends or showing remorse), but the action itself. In this way, the miniseries is aptly named since both main characters, Grace and Jonathan, use this defense mechanism. Grace has difficulty acknowledging that her husband could be capable of any wrongdoing, even as she is faced with fact after fact that contradicts this premise – and counsels others about their relationship choices. Similarly, Jonathan’s choice of profession is likely an attempt to undo his 4-year-old sister’s death that occurred on his watch when he was 14. However, even treating children’s cancer cannot undo the many indiscretions he has apparently committed in his adult life.
In the portrayal of a doctor with narcissistic, and possibly psychopathic, traits, “The Undoing” joins multiple recent podcasts that document real-life bad doctors, including Wondery’s “The Shrink Next Door,” “Dr. Death” (seasons 1 and 2), and “Do No Harm.” While most physicians go into medicine to heal and improve peoples’ lives, others, such as the character of Dr. Jonathan Fraser, appear to become physicians for ulterior and sinister motivations. Jonathan’s difficulty with empathy was present when he was a child as a character trait – rather than being attributable to any childhood traumatic event, as Grace had let herself believe.
In a Dec. 11, 2020, New York Times op-ed, Richard A. Friedman, MD, a psychiatrist affiliated with New York Presbyterian-Cornell University, discussed three “dangerous doctors” during the pandemic who are potentially harming the nation. Scott Atlas, MD, a radiologist on leave from Stanford (Calif.) University, advised President Trump on the coronavirus despite having no training in public health or infectious disease. Before resigning, he questioned the use of face masks, contradicting scientific proof of their prevention of disease. Another doctor, a cardiologist in Washington, also publicly disputed scientific evidence of the efficacy of face masks and social distancing, and a third physician promoted hydroxychloroquine as a treatment for coronavirus despite scientific evidence that it has been ineffective and possibly even harmful to patients with the virus.
Both the novel “You Should Have Known” and the series “The Undoing” will be of interest to psychiatrists, especially therapists and forensic psychiatrists, because of the themes portrayed, such as defense mechanisms, therapeutic process, and a homicide investigation – as well as the common human experience of being an expert in something in one’s professional life, yet occasionally falling short of recognizing the same phenomena in one’s personal life.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and is on the faculty at Weill-Cornell Medical Center. She has no conflicts of interest. Dr. Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law, and which was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association. She has no conflicts of interest.
Jean Hanff Korelitz’s ironic psychological thriller, “You Should Have Known,” (New York: Grand Central Publishing, 2014) was transformed into an HBO miniseries called “The Undoing,” written and produced by David E. Kelley and directed by Susanne Bier, which premiered on Oct. 25, 2020.
The television drama differed from the novel in fundamental ways, but both have themes related to the therapeutic process. In the novel, a New York City–based couples therapist, Grace Reinhart Sachs, had recently written a book called “You Should Have Known,” about women who married their spouses disregarding their gut instinct that their partner was not fundamentally right for them, or might potentially cheat on them, or whose stories contained contradictions. In the miniseries, Grace (played by Nicole Kidman), is a therapist but there is no mention of her having written a book. Grace in both the novel and the miniseries is married to a pediatric oncologist, Jonathan (his ethnicity and surname were changed in the miniseries from a Jewish New Yorker in the novel to a British Dr. Jonathan Fraser in the series, played by Hugh Grant).
[Spoiler alert]: Prepandemic New York City’s Upper East Side is scandalized when a murdered mother is found by her young son the day after a lavish fund-raising auction party for a private school. Grace and Jonathan’s son, Henry, attends this school as well, and Grace had served on the auction committee with the murdered mother. When two detectives question Grace in the course of their investigation, she assumes that they are questioning her as they would any parent in the school. However, when she tries to reach her husband about the news and the investigation, she cannot. She thought he was at a medical conference in Cleveland, but she realizes that she does not know exactly what conference and exactly where. After many failed attempts at calling and texting, she hears a familiar alert sound coming from his nightstand drawer where she retrieves the cell phone that had been deliberately placed.
In the novel, Jonathan never reappears from “Cleveland,” and although it takes Grace a while to understand that her husband is not who she thought he was, she eventually does. In the miniseries, Jonathan appears in their lake house and a trial ensues with Jonathan adamantly proclaiming his innocence despite all evidence to the contrary.
The Oxford Reference defines undoing as “an emotional conflict associated with an action is dealt with by negating the action or attempting ‘magically’ to cause it not to have occurred by substituting an approximately opposite action.” It is not that the consequences of the action are attempted to be negated (as in making amends or showing remorse), but the action itself. In this way, the miniseries is aptly named since both main characters, Grace and Jonathan, use this defense mechanism. Grace has difficulty acknowledging that her husband could be capable of any wrongdoing, even as she is faced with fact after fact that contradicts this premise – and counsels others about their relationship choices. Similarly, Jonathan’s choice of profession is likely an attempt to undo his 4-year-old sister’s death that occurred on his watch when he was 14. However, even treating children’s cancer cannot undo the many indiscretions he has apparently committed in his adult life.
In the portrayal of a doctor with narcissistic, and possibly psychopathic, traits, “The Undoing” joins multiple recent podcasts that document real-life bad doctors, including Wondery’s “The Shrink Next Door,” “Dr. Death” (seasons 1 and 2), and “Do No Harm.” While most physicians go into medicine to heal and improve peoples’ lives, others, such as the character of Dr. Jonathan Fraser, appear to become physicians for ulterior and sinister motivations. Jonathan’s difficulty with empathy was present when he was a child as a character trait – rather than being attributable to any childhood traumatic event, as Grace had let herself believe.
In a Dec. 11, 2020, New York Times op-ed, Richard A. Friedman, MD, a psychiatrist affiliated with New York Presbyterian-Cornell University, discussed three “dangerous doctors” during the pandemic who are potentially harming the nation. Scott Atlas, MD, a radiologist on leave from Stanford (Calif.) University, advised President Trump on the coronavirus despite having no training in public health or infectious disease. Before resigning, he questioned the use of face masks, contradicting scientific proof of their prevention of disease. Another doctor, a cardiologist in Washington, also publicly disputed scientific evidence of the efficacy of face masks and social distancing, and a third physician promoted hydroxychloroquine as a treatment for coronavirus despite scientific evidence that it has been ineffective and possibly even harmful to patients with the virus.
Both the novel “You Should Have Known” and the series “The Undoing” will be of interest to psychiatrists, especially therapists and forensic psychiatrists, because of the themes portrayed, such as defense mechanisms, therapeutic process, and a homicide investigation – as well as the common human experience of being an expert in something in one’s professional life, yet occasionally falling short of recognizing the same phenomena in one’s personal life.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and is on the faculty at Weill-Cornell Medical Center. She has no conflicts of interest. Dr. Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law, and which was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association. She has no conflicts of interest.
Jean Hanff Korelitz’s ironic psychological thriller, “You Should Have Known,” (New York: Grand Central Publishing, 2014) was transformed into an HBO miniseries called “The Undoing,” written and produced by David E. Kelley and directed by Susanne Bier, which premiered on Oct. 25, 2020.
The television drama differed from the novel in fundamental ways, but both have themes related to the therapeutic process. In the novel, a New York City–based couples therapist, Grace Reinhart Sachs, had recently written a book called “You Should Have Known,” about women who married their spouses disregarding their gut instinct that their partner was not fundamentally right for them, or might potentially cheat on them, or whose stories contained contradictions. In the miniseries, Grace (played by Nicole Kidman), is a therapist but there is no mention of her having written a book. Grace in both the novel and the miniseries is married to a pediatric oncologist, Jonathan (his ethnicity and surname were changed in the miniseries from a Jewish New Yorker in the novel to a British Dr. Jonathan Fraser in the series, played by Hugh Grant).
[Spoiler alert]: Prepandemic New York City’s Upper East Side is scandalized when a murdered mother is found by her young son the day after a lavish fund-raising auction party for a private school. Grace and Jonathan’s son, Henry, attends this school as well, and Grace had served on the auction committee with the murdered mother. When two detectives question Grace in the course of their investigation, she assumes that they are questioning her as they would any parent in the school. However, when she tries to reach her husband about the news and the investigation, she cannot. She thought he was at a medical conference in Cleveland, but she realizes that she does not know exactly what conference and exactly where. After many failed attempts at calling and texting, she hears a familiar alert sound coming from his nightstand drawer where she retrieves the cell phone that had been deliberately placed.
In the novel, Jonathan never reappears from “Cleveland,” and although it takes Grace a while to understand that her husband is not who she thought he was, she eventually does. In the miniseries, Jonathan appears in their lake house and a trial ensues with Jonathan adamantly proclaiming his innocence despite all evidence to the contrary.
The Oxford Reference defines undoing as “an emotional conflict associated with an action is dealt with by negating the action or attempting ‘magically’ to cause it not to have occurred by substituting an approximately opposite action.” It is not that the consequences of the action are attempted to be negated (as in making amends or showing remorse), but the action itself. In this way, the miniseries is aptly named since both main characters, Grace and Jonathan, use this defense mechanism. Grace has difficulty acknowledging that her husband could be capable of any wrongdoing, even as she is faced with fact after fact that contradicts this premise – and counsels others about their relationship choices. Similarly, Jonathan’s choice of profession is likely an attempt to undo his 4-year-old sister’s death that occurred on his watch when he was 14. However, even treating children’s cancer cannot undo the many indiscretions he has apparently committed in his adult life.
In the portrayal of a doctor with narcissistic, and possibly psychopathic, traits, “The Undoing” joins multiple recent podcasts that document real-life bad doctors, including Wondery’s “The Shrink Next Door,” “Dr. Death” (seasons 1 and 2), and “Do No Harm.” While most physicians go into medicine to heal and improve peoples’ lives, others, such as the character of Dr. Jonathan Fraser, appear to become physicians for ulterior and sinister motivations. Jonathan’s difficulty with empathy was present when he was a child as a character trait – rather than being attributable to any childhood traumatic event, as Grace had let herself believe.
In a Dec. 11, 2020, New York Times op-ed, Richard A. Friedman, MD, a psychiatrist affiliated with New York Presbyterian-Cornell University, discussed three “dangerous doctors” during the pandemic who are potentially harming the nation. Scott Atlas, MD, a radiologist on leave from Stanford (Calif.) University, advised President Trump on the coronavirus despite having no training in public health or infectious disease. Before resigning, he questioned the use of face masks, contradicting scientific proof of their prevention of disease. Another doctor, a cardiologist in Washington, also publicly disputed scientific evidence of the efficacy of face masks and social distancing, and a third physician promoted hydroxychloroquine as a treatment for coronavirus despite scientific evidence that it has been ineffective and possibly even harmful to patients with the virus.
Both the novel “You Should Have Known” and the series “The Undoing” will be of interest to psychiatrists, especially therapists and forensic psychiatrists, because of the themes portrayed, such as defense mechanisms, therapeutic process, and a homicide investigation – as well as the common human experience of being an expert in something in one’s professional life, yet occasionally falling short of recognizing the same phenomena in one’s personal life.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and is on the faculty at Weill-Cornell Medical Center. She has no conflicts of interest. Dr. Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law, and which was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association. She has no conflicts of interest.
‘Defending Jacob’ and defending psychiatry
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
The 2012 crime fiction novel, “Defending Jacob,” by William Landay was dramatized into a miniseries created by Mark Bomback that premiered on April 24, 2020, on Apple TV+ (and for those resisting a subscription, “The Morning Show” and “Defending Jacob” are both worth it). Both the “Defending Jacob” novel and the miniseries have themes that are of interest to psychiatry, especially to child and forensic psychiatrists, and both the literary and TV versions are excellent, albeit disturbing, diversions from the current pandemic.
(Spoiler alert!) The story is set in the affluent town of Newton, Mass., where crime is generally low and homicides extremely infrequent. Protagonist Andy Barber, a 51-year-old Jewish assistant district attorney, is played by a younger Chris Evans in the miniseries. His wife, Laurie Gold Barber, a 51-year-old Jewish former schoolteacher and stay-at-home mom, is played by a younger Michelle Dockery of Downton Abbey fame. In the miniseries, her character is actively working as a teacher and social activist for children. Other differences between the novel and the miniseries will be pointed out when relevant, but the overall narrative is similar. Both stories are cleverly told through Andy Barber speaking in retrospect as he is being questioned in front of a grand jury for a potential indictment.
When 14-year-old Ben Rifkin is found stabbed to death in Cold Spring Park before school one morning, Andy Barber initially takes the case despite his boss’s reservations that there may be a conflict because Andy’s son Jacob is a student in Ben’s class at school. As the title suggests, it soon becomes clear that Jacob may have had something to do with the murder. At that point, Andy is taken off the case and it is given to a junior colleague, Neal Logiudice, who demonstrates both admiration and contempt for his former mentor, perhaps because of underlying jealousy and insecurity. Neal Logiudice becomes the DA questioning Andy Barber.
Prior to Jacob’s formal accusation of murder, the Barbers appear to be fiercely loyal and unable to fully see and understand their son. The difficulty with objectivity and the reasons why family member physicians should never treat family members – and why family member attorneys should never represent loved ones – is abundantly clear in this story. When Andy receives an anonymous tip that Jacob’s childhood best friend, Derek Yoo, posted on Facebook, “Jake, everyone knows you did it. You have a knife. I’ve seen it,’ ” Andy then looks through Jacob’s drawers and finds a folding knife in one of his T-shirts. In the chapter aptly titled “Denial,” Andy, an experienced prosecutor, does not turn the knife over as evidence, but instead disposes of it – believing Jacob that he did not take the knife to school the day his classmate was stabbed.
After Jacob is indicted, Andy Barber confesses to his wife, Laurie, that his estranged father who left when he was 6 is actually in prison convicted of murdering and raping a woman. In the novel, his grandfather and great-grandfather are also convicted felons. Laurie reveals this family history to Jacob’s attorney, and the attorney subsequently refers the family to a forensic psychologist. In the novel, she is a large Jewish woman; in the miniseries she is played by a very thin Poorna Jagannathan (who incidentally has portrayed a therapist in the television series “Sorry for your Loss,” and a doctor in “The Act,” “Better Call Saul,” “NCIS: Los Angeles,” “House of Cards,” “The Game,” “Law and Order: Criminal Intent,” “Rescue Me,” “Jonny Zero,” “An Actor Prepares,” “The Circle,” “Thanks for Sharing,” and “Montclair.”) Although the goal of the defense was a finding of “not guilty,” a psychiatric defense was going to be used as a last resort if necessary.
Laurie had already googled and learned of “the murder gene,” which was further explained by the forensic psychologist as a mutation called:
“MAOA Knockout. It has been argued in court as a trigger for violence before, but the argument was too simplistic, and it was rejected. Our understanding of the gene-environment interplay has improved since then – the science is getting better and very quickly – and we may have better testimony now. The second mutation is located in what’s called the serotonin transporter gene. The official name for the gene is SLC6A4. It’s located on chromosome 17. It encodes a protein that facilitates the activity of the serotonin transporter system, which is what enables the reuptake of serotonin from the synapse back into the neuron.”1
She further explains that there have been many studies on the “nurture” side of the nature/nurture question and that, with new developments in DNA studies, it is now becoming possible to study the “nature” side.
“Defending Jacob” explores the nature/nurture issue, as well as issues with forensic testimony in court and the criminal justice system in general. The issue of repressing feelings and hiding secrets and then having to confront both in a brutal manner is another theme addressed in the story. Andy tried to hide and forget that his father was in prison and the criminal history in his family, but he was forced to face this and his feelings about it when confronted with his own son being accused of murder. Of note, he does not seek help from a therapist despite these life-altering events. (Humongous spoiler alert:) The story that began with a murder of an unrelated child may end with a family murder, one that would be well described and could be understood by psychiatrists using the categories of motives initially described by Phillip Resnick, MD.2
Once again, and unfortunately, as we have pointed out in other media reviews, the portrayal of psychiatric/psychological themes is problematic. Using a psychologist to explain the science of DNA and not a psychiatrist is an interesting choice. Diagnosing a 14-year-old with personality disorders also contributes to misunderstanding and stigma. In addition, no timely attempt is made to refer the accused Jacob for mental health treatment. The stigmatization of psychiatry in the media was addressed by the World Psychiatric Association task force guidance on how to combat stigmatization of psychiatry and psychiatrists,3 including breaking down negative views of psychiatrists and psychiatry in the general public, among medical students, other health professionals, and patients and relatives. The task force made recommendations for national psychiatric societies and for individual practitioners to help reduce stigma of the profession of psychiatry. We would argue that speaking to the media, including fiction authors, to help educate about mental health is an important role for psychiatrists. It would lead to more realistic portrayals in film and books.
Overall, “Defending Jacob” is a compelling story in both the novel and the miniseries. Despite some problems with how it depicts mental health issues, both are engaging and contain thoughtful, extremely well-written themes of interest to many clinical and forensic psychiatrists.
References
1. Landay W. Defending Jacob, a novel. New York: Delacorte Press, 2012.
2. Friedman SH. Family Murder: Pathologies of Love and Hate. Washington: American Psychiatric Association Publishing, 2019.
3. Sartorius N et al. World Psychiatry. 2010 Oct;9(3):131-44.
Dr. Rosenbaum is a clinical and forensic psychiatrist in private practice in New York. She is an assistant clinical professor at New York University Langone Medical Center and on the faculty at Weill Cornell Medical Center. Dr. Hatters Friedman serves as the Phillip Resnick Professor of Forensic Psychiatry at Case Western Reserve University, Cleveland. She is also editor of Family Murder: Pathologies of Love and Hate (Washington: American Psychiatric Association Publishing, 2019), which was written by the Group for the Advancement of Psychiatry’s Committee on Psychiatry & Law and was awarded the 2020 Manfred Gutmacher Award by the American Psychiatric Association.
‘After Life’ and before good treatment
Portrayal of psychiatry in Netflix series could deter people from getting help
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.
Portrayal of psychiatry in Netflix series could deter people from getting help
Portrayal of psychiatry in Netflix series could deter people from getting help
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.