User login
Combined hormonal contraceptives and migraine: An update on the evidence
Combined hormonal contraceptives are contraindicated in women who have migraine with aura because they pose a risk of stroke. But how great is the risk, and how strong is the evidence, particularly with today’s low-dose contraceptives? Can we view migraine with aura as a relative contraindication rather than an absolute one?
This article reviews migraine diagnosis, the effects of estrogen and the menstrual cycle on migraine, the evidence of stroke risk with combined hormonal contraceptive use, and how the frequency of aura may affect risk. It offers practical advice on choosing contraceptive formulations and counseling patients on risks and benefits.
WHAT THE GUIDELINES SAY
Current guidelines restrict the use of combined hormonal contraceptives in the setting of migraine with aura, but not in migraine without aura.
A practice bulletin from the American College of Obstetrics and Gynecology in 2010 noted that extended-cycle or continuous hormonal contraceptives, including oral and parenteral products, might provide relief of migraines by eliminating the drops in estrogen levels that precipitate them.1 However, the bulletin also cautioned that though cerebrovascular accidents in women are rare, the impact of a stroke is so devastating that clinicians should consider intrauterine devices, progestin-only options, and other nonestrogen methods in women who have migraine with focal neurologic signs, women who smoke, and women age 35 or older.1
In 2016, the US Centers for Disease Control and Prevention published updates to its medical eligibility criteria for contraceptive use in various medical conditions. In the case of migraine without aura, the guidelines note no limitation to the use of combined hormonal contraceptives, regardless of the patient’s age. In the case of migraine with aura, the consensus was that the risk associated with combined hormonal contraception typically outweighs its benefits, noting “an unacceptable health risk if the contraceptive method is used.”2
We believe a fresh look at the data is warranted.
EARLY ORAL CONTRACEPTIVES WERE ALL HIGH-DOSE
This issue first surfaced in the decade and a half after the initial launch of oral contraceptives in 1960. The products then were all high-dose pills, containing up to 150 µg of mestranol. In subsequent decades, the dose of estrogen was successively reduced, so that now some pills contain only 10 µg of ethinyl estradiol. High-dose pills—which today contain 50 µg of ethinyl estradiol—account for less than 1% of pills currently sold in the United States and have been eliminated in many countries.
DIAGNOSTIC CRITERIA FOR MIGRAINE
According to the International Classification of Headache Disorders (ICHD),3 the diagnosis of migraine requires 2 of the 4 following criteria:
- Unilateral location
- Pulsating or throbbing pain
- Pain of at least moderate intensity
- Pain aggravated by activity, or causing a preference to avoid activity.
An additional criterion is either nausea or a combination of photophobia and phonophobia with the episode. This criterion can be met if the patient prefers to avoid bright lights and loud noises during an attack.
Headache experts have suggested that patients with a stable pattern of episodic, disabling headache and normal findings on physical examination should be considered to have migraine if there is no contradictory evidence.4,5
Migraine with aura requires at least 2 of the following 4 characteristics3:
- 1 aura symptom, spreading gradually over 5 minutes, or 2 or more aura symptoms occurring in succession, or both
- Each aura symptom lasting 5 to 60 minutes (not “a few seconds,” not “hours”)
- The aura followed by the onset of headache within 60 minutes
- At least 1 aura symptom is unilateral.
Visual blurring, floaters, or split-second flashes before or during a migraine headache do not meet the criteria for aura.
MIGRAINE IS COMMON AND UNDERRECOGNIZED
In a study of 1,203 patients seeking care from a primary care provider for headache,6 94% of the 377 who turned in a diary with enough data to make a diagnosis were diagnosed with a migraine or probable migraine by an expert panel. A quarter of patients who likely had migraine based on an expert review of symptoms did not receive a migraine diagnosis at the time of their office visit.
Similarly, in a large epidemiologic study,7 30,758 adults were asked if they had headaches and, if so, how they named them. Headaches were reported by 23,564 of the participants and were subsequently diagnosed by formal ICHD criteria. Of the 3,074 individuals who met the criteria for migraine, only 53.4% correctly recognized their headaches as migraine. The most common erroneous labels were “sinus headache” and “stress headache.”7
HOW ESTROGEN AFFECTS MIGRAINE
Of note, migraine can be exacerbated during times of cycle irregularity, such as adolescence and perimenopause, the 2 times during a woman’s life associated with the highest risk of unintended pregnancy.10,11
STROKE RISK: ESTROGEN DOSE MATTERS
Shortly after the first combined oral contraceptives were released, reports of adverse events began to appear, although serious events were relatively rare. In response, prescribing guidelines advised against giving oral contraceptives to women with a history of deep vein thrombosis, myocardial infarction, stroke, or hypertension. Also, over the years, the hormonal content of the formulations was successively reduced, and with each reduction in estrogen, a decrease was observed in venous thrombosis and pulmonary embolism.12,13 Current low-dose formulations are considerably safer than high-dose options but are not entirely without risk.14
Stroke risk with combined oral contraceptives was first highlighted in a landmark article in 1975.15 However, the authors were unable to correlate the risk with the estrogen concentration of the pill, since 23 of the 25 women who suffered thrombotic stroke while taking the mestranol-containing formulation took 100-μg pills, and all 20 women who had strokes while taking the ethinyl estradiol formulation took 50-μg pills. Thus, by today’s standards, they were all taking high-dose pills. The risk of thrombotic stroke was 4 to 5 times higher in users than in nonusers.
In 1996, a study from the World Health Organization16 reported an increased risk of stroke with high-dose combined oral contraceptives (odds ratio [OR] 5.30, 95% confidence interval [CI] 2.56–11.0). With preparations containing less than 50 μg of ethinyl estradiol, the risk was not statistically significant (OR 1.53, 95% CI 0.71–3.31). These numbers were for Europe only; in developing countries, the risk was elevated regardless of dose, presumably due to additional risk factors in combined oral contraceptive users. The majority of strokes were in smokers taking 50-μg pills, with an average age greater than 35.
In 2002, a 5-year case-control study in Denmark found that the risk of stroke with combined oral contraceptives correlated directly with the estrogen content, from no increased risk with the newest and lowest-dose formulation (containing ethinyl estradiol 20 µg) to an OR of 4.5 with the older high-dose (50 µg) formulations.17
Reassuringly, a 2012 retrospective review of the Danish national registry13 revealed a low absolute risk of arterial events in users of combined oral contraceptives: 21.4 per 100,000 person-years for thrombotic stroke, and 10.1 per 100,000 person-years for myocardial infarction. Further, these risks were substantially lower with 20-μg ethinyl estradiol products than with those containing 30 to 40 μg.13 An important limitation of this large database review is that it did not control for important stroke risk factors such as obesity and smoking.
Although international studies14,16 continue to show a small but increased risk, more than 30 years have passed since a US study found an increased risk of stroke with combined oral contraceptives.
The discrepancy between US and international studies is possibly explained by the strong relative contraindication in the United States to the use of combined oral contraceptives in smokers over the age of 35 and the more prevalent use of high-dose pills in international studies. High-dose pills had been used in most of the stroke cases in the 1996 World Health Organization study16 but were used by only 0.7% of the women in the case and control groups in 2 pooled US studies from the same time period.18 Similarly, in these US studies, only 17% of the women were smokers on combined oral contraceptives, whereas in the international study, 51% of the women who had strokes and 38% of those in the control groups were smokers.
A large US study19 reviewing 3.6 million woman-years of use found no increased stroke risk (OR 0.96) in current users of low-dose combined oral contraceptives, results similar to those of a pooled analysis of US studies.18 Though this pooled analysis showed an adjusted increased risk of ischemic stroke in women reporting a history of migraine (OR 2.08, 95% CI 1.19–3.65), these conclusions were based on only 4 cases. The prevalence of migraine was identical in women who did or did not have strokes, 7.8% vs 7.7%, respectively, but the risk was judged to be increased after adjusting for other factors. But one important factor was not adjusted for: only 11 of the 1,017 women in the case and control groups were using 50-μg ethinyl estradiol pills, and 4 of the strokes were in this group of 11 women.
STROKE RISK INCREASES WITH FREQUENCY OF MIGRAINE AURA
Use of combined hormonal contraceptives in women who have migraine with aura remains controversial, based on good evidence that aura increases stroke risk20 and good evidence that high-dose oral contraceptives increase stroke risk.15
A cohort study encompassing more than 470,000 person-years with a median follow-up of 26 years found that while migraine without aura conferred no increase in risk of all-cause mortality, migraine with aura did.21
The longitudinal Women’s Health Study analyzed data from 27,798 women over age 45 and found that migraine with aura conferred an increased risk of cardiovascular disease (including stroke) that varied directly with aura frequency.22 Aura frequency less than once a month conferred a risk 2 times higher than in women without migraine, and the risk was more than 4 times higher when aura frequency exceeded once a week.
Similarly, an analysis of the World Health Organization study of stroke in young women found that the adjusted risk of ischemic stroke was significantly and directly associated with aura frequency.20
Potential explanations for this increased risk with greater aura frequency include changes induced during spreading cortical depression, shared genetic predispositions, and common underlying comorbidities such as patent foramen ovale.23–26
Though studies have shown that combined oral contraceptives in continuous regimens27 or in regimens that minimize drops in estrogen levels28 can help improve general headache and menstrual-related migraine, these studies have excluded patients who have migraine with aura.
In a pilot study,29 28 women referred to a tertiary headache clinic who had migraine with aura and intractable menstrual-related migraine were offered combined hormonal contraception in the form of a vaginal ring that releases only 15 μg ethinyl estradiol per 24 hours, thereby reducing peak estrogen exposure to a level lower than those encountered with the native menstrual cycle (with the suppression of ovulation). The women used this continuous ultra-low-dose hormonal contraception without placebo days. After a mean follow-up of 8 months, this regimen reduced aura frequency from a baseline average of 3.2 per month to only 0.2 per month. No woman had an increase in aura frequency, and menstrual-related migraine was eliminated in 21 (91.3%) of the 23 evaluable patients.
CHOOSING THE OPTIMAL CONTRACEPTIVE FORMULATION
Today, ultra-low-dose combined oral contraceptives (containing 10–15 µg of ethinyl estradiol) inhibit ovulation with doses of estrogen that are in a midphysiologic range. Consequently, they expose women to lower peak concentrations of estrogen than they would experience in their natural menstrual cycle (Figure 1). If a combined oral contraceptive is used in women with migraine with aura, lower estrogen doses (≤ 20 µg ethinyl estradiol) are preferred to decrease aura frequency and minimize the risk of stroke associated with high-dose ethinyl estradiol formulations.
Does the progestin matter?
Though there has been debate about whether different types of progestins alter the risk of venous thromboembolism,30,31 the chosen progestin does not seem to affect arterial risks such as stroke and myocardial infarction.14
All current guidelines note that progestin-only pills can be safely offered to women with migraine with aura. However, progestin-only pills have a shorter half-life than combined hormonal contraceptives and must be taken consistently and on time to ensure contraceptive efficacy and minimize abnormal bleeding. Patients who cannot adhere to a strict daily pill regimen may increase their risk of unintended pregnancy. In addition, progestin-only pills do not help with reducing episodes of migraine because they prevent ovulation only about half of the time.2 In contrast, a progestin-only arm implant is not only considered safe to use in women with migraine with aura, it may also prevent ovulation more reliably. Though progestin arm implants have the potential to reduce menstrual migraine and aura, this requires further study to confirm.
For menstrual-related migraine
In clinical practice, providers may offer certain combined hormonal contraceptives to women with debilitating menstrual-related migraine to prevent attacks. Although menstrual-related migraine rarely if ever is accompanied by aura, these patients may still have migraine with aura at other times of the month.
In women with menstrual-related migraine, any decrease in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-withdrawal migraine. All currently available regimens of combined hormonal contraceptives that follow a 21-days-on, 7-days-off plan entail a drop in ethinyl estradiol of more than 10 µg (Figure 1).
Continuous regimens: Who needs a menstrual cycle anyway?
Of note: ultra-low-estrogen combined hormonal contraceptives that have placebo intervals may not inhibit ovulation consistently in all women.32 Contraceptive efficacy is still maintained, as contraception does not require inhibition of ovulation. Other mechanisms such as thickening of cervical mucus help with pregnancy prevention.
However, if ovulation is not inhibited, the consequent postovulatory decline in estrogen will continue to contribute to estrogen-withdrawal migraine.33,34 Reducing the number of placebo days may help inhibit ovulation. Adding back adequate estrogen during the placebo break (eg, either 0.9 mg conjugated equine estrogen with a 20-µg ethinyl estradiol combined oral contraceptive, or 0.075 mg transdermal 17B estradiol with a 15-µg combined hormonal contraceptive) can prevent these migraines.33,34
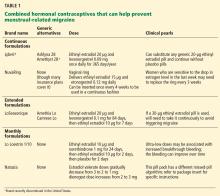
Some extended-cycle regimens, which give 4 withdrawal bleeds per year, will likewise prevent estrogen-withdrawal migraine if the decline in estrogen is limited to 10 µg (Table 1). Unfortunately, most extended regimens (Seasonale, Seasonique, and their generics) entail a 20- or 30-µg drop.
Continuous or extended-cycle regimens can be prescribed using any generic 20-µg combined hormonal contraceptive that the patient tolerates, along with specific instructions on the prescription to take the pills in a continuous fashion, eg, “Do not take the placebo pills; start the next pill pack immediately after 21 days.”
Postmenopausal hormone therapy
Neither smoking nor migraine is a contraindication to the use of postmenopausal hormone therapy, which is substantially lower in dosage than combined hormonal contraceptives.
ADVISING PATIENTS ON RISKS VS BENEFITS
It is important to remember that the risks of unintended pregnancy are always greater than the risks of any contraceptive, especially in women with chronic medical conditions, including those who have migraine with aura. Other benefits include the following:
Lower mortality risk. A 2010 analysis demonstrated that in nearly 46,000 women followed since 1968, those taking combined oral contraceptives had statistically significantly lower death rates from any cause and a lower risk of death from cancer and cardiovascular diseases than women who had never taken combined oral contraceptives.36
Stroke. Though the absolute risk of stroke to an individual woman taking a low-dose or ultra-low-dose combined hormonal contraceptive has been shown to be similar to that in women who are not taking combined hormonal contraception, its impact on an otherwise healthy woman could be devastating. Clinicians must remember that current guidelines still caution against prescribing combined hormonal contraceptives in women with migraine with aura and thus should counsel their patients accordingly and document the discussion in the medical record.
Noncontraceptive benefits. Women may be prescribed a combined hormonal contraceptive for benefits beyond contraception. The obvious reasons include beneficial effects on endometriosis, anemia, acne, hirsutism, dysmenorrhea, and prevention of ovarian cysts. But other important major benefits2 include substantial reductions in the risk of ovarian cancer (> 50% decrease after 10 years)37 and endometrial cancer (additional 24% reduction for each 5 years of use),38 and a modest decrease in the risk of colon cancer (37% less risk in ever-users).39 Further, combined oral contraceptive use has been associated with a decrease in mortality rates,40,41 with no increased risk of nonreproductive cancers.41
Ultra-low-dose, continuous formulations may benefit women by decreasing the frequency of migraine with aura and menstrual-related migraine. There is no evidence that reducing aura frequency also reduces stroke risk, but this represents an important area for future research.
WHAT WOULD WE DO?
For a patient who has a history of migraine with aura, if the goal is only to prevent pregnancy, we would recommend another contraceptive option that does not involve estrogen. However, we would consider prescribing a combined hormonal contraceptive in a low-dose regimen if the patient prefers this regimen for other health benefits (eg, acne control), if she has no other risk factors for stroke, and if she gives her informed consent after a discussion of the risks and benefits. Women who have menstrual-related migraine refractory to or who cannot tolerate other migraine therapies are often willing to try a low-dose estrogen-containing contraceptive for control of their migraine, especially if they have tried it in the past and believe that it helped prevent migraine. Patients should have follow-up within 3 months to discuss whether they have benefited from the regimen in terms of headache frequency or severity.
- ACOG Practice Bulletin No. 110: noncontraceptive uses of hormonal contraceptives. Obstet Gynecol 2010; 115:206–218.
- Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports/Centers for Disease Control 2016; 65:1–104.
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013; 33:629–808.
- Lipton RB, Cady RK, Stewart WF, Wilks K, Hall C. Diagnostic lessons from the Spectrum study. Neurology 2002; 58(suppl 6):S27–S31.
- Lipton RB, Stewart WF, Cady R, et al. 2000 Wolfe Award. Sumatriptan for the range of headaches in migraine sufferers: results of the Spectrum Study. Headache 2000; 40:783–791.
- Tepper SJ, Dahlof CG, Dowson A, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the Landmark Study. Headache 2004; 44:856–864.
- Lipton RB, Stewart WF, Liberman JN. Self-awareness of migraine: interpreting the labels that headache sufferers apply to their headaches. Neurology 2002; 58(suppl 6):S21–S26.
- Chai NC, Peterlin BL, Calhoun AH. Migraine and estrogen. Curr Opin Neurol 2014; 27:315–324.
- Calhoun AH. Menstrual migraine: update on pathophysiology and approach to therapy and management. Curr Treat Options Neurol 2012; 14:1–14.
- McNamara M, Batur P, DeSapri KT. In the clinic. Perimenopause. Ann Intern Med 2015; 162:ITC1–ITC15.
- O’Brien HL, Cohen JM. Young adults with headaches: the transition from adolescents to adults. Headache 2015; 55:1404–1409.
- Vessey M, Mant D, Smith A, Yeates D. Oral contraceptives and venous thromboembolism: findings in a large prospective study. Br Med J (Clin Res Ed) 1986; 292:526.
- Lidegaard O, Lokkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- MacGregor EA. Contraception and headache. Headache 2013; 53:247–276.
- Oral contraceptives and stroke in young women. Associated risk factors. JAMA 1975; 231:718–722.
- Ischaemic stroke and combined oral contraceptives: results of an international, multicentre, case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet 1996; 348:498–505.
- Lidegaard O, Kreiner S. Contraceptives and cerebral thrombosis: a five-year national case-control study. Contraception 2002; 65:197–205.
- Schwartz SM, Petitti DB, Siscovick DS, et al. Stroke and use of low-dose oral contraceptives in young women: a pooled analysis of two US studies. Stroke 1998; 29:2277–2284.
- Petitti DB, Sidney S, Bernstein A, Wolf S, Quesenberry C, Ziel HK. Stroke in users of low-dose oral contraceptives. N Engl J Med 1996; 335:8–15.
- Donaghy M, Chang CL, Poulter N; European Collaborators of the World Health Organisation Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Duration, frequency, recency, and type of migraine and the risk of ischaemic stroke in women of childbearing age. J Neurol Neurosurg Psychiatry 2002; 73:747–750.
- Gudmundsson LS, Scher AI, Aspelund T, et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ 2010; 341:c3966.
- Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology 2005; 64:1020–1026.
- Lee ST, Chu K, Jung KH, et al. Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology 2008; 70:1510–1517.
- Kunz GA, Liang G, Cuculi F, et al. Circulating endothelial progenitor cells predict coronary artery disease severity. Am Heart J 2006; 152:190–195.
- Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA 2006; 296:283–291.
- Pezzini A, Del Zotto E, Giossi A, Volonghi I, Grassi M, Padovani A. The migraine-ischemic stroke connection: potential pathogenic mechanisms. Curr Mol Med 2009; 9:215–226.
- Sulak P, Willis S, Kuehl T, Coffee A, Clark J. Headaches and oral contraceptives: impact of eliminating the standard 7-day placebo interval. Headache 2007; 47:27–37.
- Nappi RE, Terreno E, Sances G, et al. Effect of a contraceptive pill containing estradiol valerate and dienogest (E2V/DNG) in women with menstrually-related migraine (MRM). Contraception 2013; 88:369–375.
- Calhoun A, Ford S, Pruitt A. The impact of extended-cycle vaginal ring contraception on migraine aura: a retrospective case series. Headache 2012; 52:1246–1253.
- Wu CQ, Grandi SM, Filion KB, Abenhaim HA, Joseph L, Eisenberg MJ. Drospirenone-containing oral contraceptive pills and the risk of venous and arterial thrombosis: a systematic review. BJOG 2013; 120:801–810.
- Dinger J, Bardenheuer K, Heinemann K. Cardiovascular and general safety of a 24-day regimen of drospirenone-containing combined oral contraceptives: final results from the International Active Surveillance Study of Women Taking Oral Contraceptives. Contraception 2014; 89:253–263.
- Benson LS, Micks EA. Why stop now? Extended and continuous regimens of combined hormonal contraceptive methods. Obstet Gynecol Clin North Am 2015; 42:669–681.
- Mannix LK, Calhoun AH. Menstrual migraine. Curr Treat Options Neurol 2004; 6:489–498.
- Calhoun AH. A novel specific prophylaxis for menstrual-associated migraine. South Med J 2004; 97:819–822.
- Calhoun AH. Current topics and controversies in menstrual migraine. Headache 2012; 52(suppl 1):8–11.
- Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V, Lee AJ. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ 2010; 340:c927.
- Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive pills as primary prevention for ovarian cancer: a systematic review and meta-analysis. Obstet Gynecol 2013; 122:139 -147.
- Collaborative Group on Epidemiological Studies on Endometrial Cancer. Endometrial cancer and oral contraceptives: an individual participant meta-analysis of 27,276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol 2015; 16:1061–1070.
- Fernandez E, La Vecchia C, Franceschi S, et al. Oral contraceptive use and risk of colorectal cancer. Epidemiology 1998; 9:295–300.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition; a cohort study. BMC Med 2015; 13:252.
- Vessey M, Yeates D. Oral contraceptive use and cancer: final report from the Oxford-Family Planning Association Contraceptive Study. Contraception 2013; 88:678–683.
Combined hormonal contraceptives are contraindicated in women who have migraine with aura because they pose a risk of stroke. But how great is the risk, and how strong is the evidence, particularly with today’s low-dose contraceptives? Can we view migraine with aura as a relative contraindication rather than an absolute one?
This article reviews migraine diagnosis, the effects of estrogen and the menstrual cycle on migraine, the evidence of stroke risk with combined hormonal contraceptive use, and how the frequency of aura may affect risk. It offers practical advice on choosing contraceptive formulations and counseling patients on risks and benefits.
WHAT THE GUIDELINES SAY
Current guidelines restrict the use of combined hormonal contraceptives in the setting of migraine with aura, but not in migraine without aura.
A practice bulletin from the American College of Obstetrics and Gynecology in 2010 noted that extended-cycle or continuous hormonal contraceptives, including oral and parenteral products, might provide relief of migraines by eliminating the drops in estrogen levels that precipitate them.1 However, the bulletin also cautioned that though cerebrovascular accidents in women are rare, the impact of a stroke is so devastating that clinicians should consider intrauterine devices, progestin-only options, and other nonestrogen methods in women who have migraine with focal neurologic signs, women who smoke, and women age 35 or older.1
In 2016, the US Centers for Disease Control and Prevention published updates to its medical eligibility criteria for contraceptive use in various medical conditions. In the case of migraine without aura, the guidelines note no limitation to the use of combined hormonal contraceptives, regardless of the patient’s age. In the case of migraine with aura, the consensus was that the risk associated with combined hormonal contraception typically outweighs its benefits, noting “an unacceptable health risk if the contraceptive method is used.”2
We believe a fresh look at the data is warranted.
EARLY ORAL CONTRACEPTIVES WERE ALL HIGH-DOSE
This issue first surfaced in the decade and a half after the initial launch of oral contraceptives in 1960. The products then were all high-dose pills, containing up to 150 µg of mestranol. In subsequent decades, the dose of estrogen was successively reduced, so that now some pills contain only 10 µg of ethinyl estradiol. High-dose pills—which today contain 50 µg of ethinyl estradiol—account for less than 1% of pills currently sold in the United States and have been eliminated in many countries.
DIAGNOSTIC CRITERIA FOR MIGRAINE
According to the International Classification of Headache Disorders (ICHD),3 the diagnosis of migraine requires 2 of the 4 following criteria:
- Unilateral location
- Pulsating or throbbing pain
- Pain of at least moderate intensity
- Pain aggravated by activity, or causing a preference to avoid activity.
An additional criterion is either nausea or a combination of photophobia and phonophobia with the episode. This criterion can be met if the patient prefers to avoid bright lights and loud noises during an attack.
Headache experts have suggested that patients with a stable pattern of episodic, disabling headache and normal findings on physical examination should be considered to have migraine if there is no contradictory evidence.4,5
Migraine with aura requires at least 2 of the following 4 characteristics3:
- 1 aura symptom, spreading gradually over 5 minutes, or 2 or more aura symptoms occurring in succession, or both
- Each aura symptom lasting 5 to 60 minutes (not “a few seconds,” not “hours”)
- The aura followed by the onset of headache within 60 minutes
- At least 1 aura symptom is unilateral.
Visual blurring, floaters, or split-second flashes before or during a migraine headache do not meet the criteria for aura.
MIGRAINE IS COMMON AND UNDERRECOGNIZED
In a study of 1,203 patients seeking care from a primary care provider for headache,6 94% of the 377 who turned in a diary with enough data to make a diagnosis were diagnosed with a migraine or probable migraine by an expert panel. A quarter of patients who likely had migraine based on an expert review of symptoms did not receive a migraine diagnosis at the time of their office visit.
Similarly, in a large epidemiologic study,7 30,758 adults were asked if they had headaches and, if so, how they named them. Headaches were reported by 23,564 of the participants and were subsequently diagnosed by formal ICHD criteria. Of the 3,074 individuals who met the criteria for migraine, only 53.4% correctly recognized their headaches as migraine. The most common erroneous labels were “sinus headache” and “stress headache.”7
HOW ESTROGEN AFFECTS MIGRAINE
Of note, migraine can be exacerbated during times of cycle irregularity, such as adolescence and perimenopause, the 2 times during a woman’s life associated with the highest risk of unintended pregnancy.10,11
STROKE RISK: ESTROGEN DOSE MATTERS
Shortly after the first combined oral contraceptives were released, reports of adverse events began to appear, although serious events were relatively rare. In response, prescribing guidelines advised against giving oral contraceptives to women with a history of deep vein thrombosis, myocardial infarction, stroke, or hypertension. Also, over the years, the hormonal content of the formulations was successively reduced, and with each reduction in estrogen, a decrease was observed in venous thrombosis and pulmonary embolism.12,13 Current low-dose formulations are considerably safer than high-dose options but are not entirely without risk.14
Stroke risk with combined oral contraceptives was first highlighted in a landmark article in 1975.15 However, the authors were unable to correlate the risk with the estrogen concentration of the pill, since 23 of the 25 women who suffered thrombotic stroke while taking the mestranol-containing formulation took 100-μg pills, and all 20 women who had strokes while taking the ethinyl estradiol formulation took 50-μg pills. Thus, by today’s standards, they were all taking high-dose pills. The risk of thrombotic stroke was 4 to 5 times higher in users than in nonusers.
In 1996, a study from the World Health Organization16 reported an increased risk of stroke with high-dose combined oral contraceptives (odds ratio [OR] 5.30, 95% confidence interval [CI] 2.56–11.0). With preparations containing less than 50 μg of ethinyl estradiol, the risk was not statistically significant (OR 1.53, 95% CI 0.71–3.31). These numbers were for Europe only; in developing countries, the risk was elevated regardless of dose, presumably due to additional risk factors in combined oral contraceptive users. The majority of strokes were in smokers taking 50-μg pills, with an average age greater than 35.
In 2002, a 5-year case-control study in Denmark found that the risk of stroke with combined oral contraceptives correlated directly with the estrogen content, from no increased risk with the newest and lowest-dose formulation (containing ethinyl estradiol 20 µg) to an OR of 4.5 with the older high-dose (50 µg) formulations.17
Reassuringly, a 2012 retrospective review of the Danish national registry13 revealed a low absolute risk of arterial events in users of combined oral contraceptives: 21.4 per 100,000 person-years for thrombotic stroke, and 10.1 per 100,000 person-years for myocardial infarction. Further, these risks were substantially lower with 20-μg ethinyl estradiol products than with those containing 30 to 40 μg.13 An important limitation of this large database review is that it did not control for important stroke risk factors such as obesity and smoking.
Although international studies14,16 continue to show a small but increased risk, more than 30 years have passed since a US study found an increased risk of stroke with combined oral contraceptives.
The discrepancy between US and international studies is possibly explained by the strong relative contraindication in the United States to the use of combined oral contraceptives in smokers over the age of 35 and the more prevalent use of high-dose pills in international studies. High-dose pills had been used in most of the stroke cases in the 1996 World Health Organization study16 but were used by only 0.7% of the women in the case and control groups in 2 pooled US studies from the same time period.18 Similarly, in these US studies, only 17% of the women were smokers on combined oral contraceptives, whereas in the international study, 51% of the women who had strokes and 38% of those in the control groups were smokers.
A large US study19 reviewing 3.6 million woman-years of use found no increased stroke risk (OR 0.96) in current users of low-dose combined oral contraceptives, results similar to those of a pooled analysis of US studies.18 Though this pooled analysis showed an adjusted increased risk of ischemic stroke in women reporting a history of migraine (OR 2.08, 95% CI 1.19–3.65), these conclusions were based on only 4 cases. The prevalence of migraine was identical in women who did or did not have strokes, 7.8% vs 7.7%, respectively, but the risk was judged to be increased after adjusting for other factors. But one important factor was not adjusted for: only 11 of the 1,017 women in the case and control groups were using 50-μg ethinyl estradiol pills, and 4 of the strokes were in this group of 11 women.
STROKE RISK INCREASES WITH FREQUENCY OF MIGRAINE AURA
Use of combined hormonal contraceptives in women who have migraine with aura remains controversial, based on good evidence that aura increases stroke risk20 and good evidence that high-dose oral contraceptives increase stroke risk.15
A cohort study encompassing more than 470,000 person-years with a median follow-up of 26 years found that while migraine without aura conferred no increase in risk of all-cause mortality, migraine with aura did.21
The longitudinal Women’s Health Study analyzed data from 27,798 women over age 45 and found that migraine with aura conferred an increased risk of cardiovascular disease (including stroke) that varied directly with aura frequency.22 Aura frequency less than once a month conferred a risk 2 times higher than in women without migraine, and the risk was more than 4 times higher when aura frequency exceeded once a week.
Similarly, an analysis of the World Health Organization study of stroke in young women found that the adjusted risk of ischemic stroke was significantly and directly associated with aura frequency.20
Potential explanations for this increased risk with greater aura frequency include changes induced during spreading cortical depression, shared genetic predispositions, and common underlying comorbidities such as patent foramen ovale.23–26
Though studies have shown that combined oral contraceptives in continuous regimens27 or in regimens that minimize drops in estrogen levels28 can help improve general headache and menstrual-related migraine, these studies have excluded patients who have migraine with aura.
In a pilot study,29 28 women referred to a tertiary headache clinic who had migraine with aura and intractable menstrual-related migraine were offered combined hormonal contraception in the form of a vaginal ring that releases only 15 μg ethinyl estradiol per 24 hours, thereby reducing peak estrogen exposure to a level lower than those encountered with the native menstrual cycle (with the suppression of ovulation). The women used this continuous ultra-low-dose hormonal contraception without placebo days. After a mean follow-up of 8 months, this regimen reduced aura frequency from a baseline average of 3.2 per month to only 0.2 per month. No woman had an increase in aura frequency, and menstrual-related migraine was eliminated in 21 (91.3%) of the 23 evaluable patients.
CHOOSING THE OPTIMAL CONTRACEPTIVE FORMULATION
Today, ultra-low-dose combined oral contraceptives (containing 10–15 µg of ethinyl estradiol) inhibit ovulation with doses of estrogen that are in a midphysiologic range. Consequently, they expose women to lower peak concentrations of estrogen than they would experience in their natural menstrual cycle (Figure 1). If a combined oral contraceptive is used in women with migraine with aura, lower estrogen doses (≤ 20 µg ethinyl estradiol) are preferred to decrease aura frequency and minimize the risk of stroke associated with high-dose ethinyl estradiol formulations.
Does the progestin matter?
Though there has been debate about whether different types of progestins alter the risk of venous thromboembolism,30,31 the chosen progestin does not seem to affect arterial risks such as stroke and myocardial infarction.14
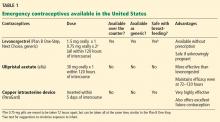
All current guidelines note that progestin-only pills can be safely offered to women with migraine with aura. However, progestin-only pills have a shorter half-life than combined hormonal contraceptives and must be taken consistently and on time to ensure contraceptive efficacy and minimize abnormal bleeding. Patients who cannot adhere to a strict daily pill regimen may increase their risk of unintended pregnancy. In addition, progestin-only pills do not help with reducing episodes of migraine because they prevent ovulation only about half of the time.2 In contrast, a progestin-only arm implant is not only considered safe to use in women with migraine with aura, it may also prevent ovulation more reliably. Though progestin arm implants have the potential to reduce menstrual migraine and aura, this requires further study to confirm.
For menstrual-related migraine
In clinical practice, providers may offer certain combined hormonal contraceptives to women with debilitating menstrual-related migraine to prevent attacks. Although menstrual-related migraine rarely if ever is accompanied by aura, these patients may still have migraine with aura at other times of the month.
In women with menstrual-related migraine, any decrease in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-withdrawal migraine. All currently available regimens of combined hormonal contraceptives that follow a 21-days-on, 7-days-off plan entail a drop in ethinyl estradiol of more than 10 µg (Figure 1).
Continuous regimens: Who needs a menstrual cycle anyway?
Of note: ultra-low-estrogen combined hormonal contraceptives that have placebo intervals may not inhibit ovulation consistently in all women.32 Contraceptive efficacy is still maintained, as contraception does not require inhibition of ovulation. Other mechanisms such as thickening of cervical mucus help with pregnancy prevention.
However, if ovulation is not inhibited, the consequent postovulatory decline in estrogen will continue to contribute to estrogen-withdrawal migraine.33,34 Reducing the number of placebo days may help inhibit ovulation. Adding back adequate estrogen during the placebo break (eg, either 0.9 mg conjugated equine estrogen with a 20-µg ethinyl estradiol combined oral contraceptive, or 0.075 mg transdermal 17B estradiol with a 15-µg combined hormonal contraceptive) can prevent these migraines.33,34
Some extended-cycle regimens, which give 4 withdrawal bleeds per year, will likewise prevent estrogen-withdrawal migraine if the decline in estrogen is limited to 10 µg (Table 1). Unfortunately, most extended regimens (Seasonale, Seasonique, and their generics) entail a 20- or 30-µg drop.
Continuous or extended-cycle regimens can be prescribed using any generic 20-µg combined hormonal contraceptive that the patient tolerates, along with specific instructions on the prescription to take the pills in a continuous fashion, eg, “Do not take the placebo pills; start the next pill pack immediately after 21 days.”
Postmenopausal hormone therapy
Neither smoking nor migraine is a contraindication to the use of postmenopausal hormone therapy, which is substantially lower in dosage than combined hormonal contraceptives.
ADVISING PATIENTS ON RISKS VS BENEFITS
It is important to remember that the risks of unintended pregnancy are always greater than the risks of any contraceptive, especially in women with chronic medical conditions, including those who have migraine with aura. Other benefits include the following:
Lower mortality risk. A 2010 analysis demonstrated that in nearly 46,000 women followed since 1968, those taking combined oral contraceptives had statistically significantly lower death rates from any cause and a lower risk of death from cancer and cardiovascular diseases than women who had never taken combined oral contraceptives.36
Stroke. Though the absolute risk of stroke to an individual woman taking a low-dose or ultra-low-dose combined hormonal contraceptive has been shown to be similar to that in women who are not taking combined hormonal contraception, its impact on an otherwise healthy woman could be devastating. Clinicians must remember that current guidelines still caution against prescribing combined hormonal contraceptives in women with migraine with aura and thus should counsel their patients accordingly and document the discussion in the medical record.
Noncontraceptive benefits. Women may be prescribed a combined hormonal contraceptive for benefits beyond contraception. The obvious reasons include beneficial effects on endometriosis, anemia, acne, hirsutism, dysmenorrhea, and prevention of ovarian cysts. But other important major benefits2 include substantial reductions in the risk of ovarian cancer (> 50% decrease after 10 years)37 and endometrial cancer (additional 24% reduction for each 5 years of use),38 and a modest decrease in the risk of colon cancer (37% less risk in ever-users).39 Further, combined oral contraceptive use has been associated with a decrease in mortality rates,40,41 with no increased risk of nonreproductive cancers.41
Ultra-low-dose, continuous formulations may benefit women by decreasing the frequency of migraine with aura and menstrual-related migraine. There is no evidence that reducing aura frequency also reduces stroke risk, but this represents an important area for future research.
WHAT WOULD WE DO?
For a patient who has a history of migraine with aura, if the goal is only to prevent pregnancy, we would recommend another contraceptive option that does not involve estrogen. However, we would consider prescribing a combined hormonal contraceptive in a low-dose regimen if the patient prefers this regimen for other health benefits (eg, acne control), if she has no other risk factors for stroke, and if she gives her informed consent after a discussion of the risks and benefits. Women who have menstrual-related migraine refractory to or who cannot tolerate other migraine therapies are often willing to try a low-dose estrogen-containing contraceptive for control of their migraine, especially if they have tried it in the past and believe that it helped prevent migraine. Patients should have follow-up within 3 months to discuss whether they have benefited from the regimen in terms of headache frequency or severity.
Combined hormonal contraceptives are contraindicated in women who have migraine with aura because they pose a risk of stroke. But how great is the risk, and how strong is the evidence, particularly with today’s low-dose contraceptives? Can we view migraine with aura as a relative contraindication rather than an absolute one?
This article reviews migraine diagnosis, the effects of estrogen and the menstrual cycle on migraine, the evidence of stroke risk with combined hormonal contraceptive use, and how the frequency of aura may affect risk. It offers practical advice on choosing contraceptive formulations and counseling patients on risks and benefits.
WHAT THE GUIDELINES SAY
Current guidelines restrict the use of combined hormonal contraceptives in the setting of migraine with aura, but not in migraine without aura.
A practice bulletin from the American College of Obstetrics and Gynecology in 2010 noted that extended-cycle or continuous hormonal contraceptives, including oral and parenteral products, might provide relief of migraines by eliminating the drops in estrogen levels that precipitate them.1 However, the bulletin also cautioned that though cerebrovascular accidents in women are rare, the impact of a stroke is so devastating that clinicians should consider intrauterine devices, progestin-only options, and other nonestrogen methods in women who have migraine with focal neurologic signs, women who smoke, and women age 35 or older.1
In 2016, the US Centers for Disease Control and Prevention published updates to its medical eligibility criteria for contraceptive use in various medical conditions. In the case of migraine without aura, the guidelines note no limitation to the use of combined hormonal contraceptives, regardless of the patient’s age. In the case of migraine with aura, the consensus was that the risk associated with combined hormonal contraception typically outweighs its benefits, noting “an unacceptable health risk if the contraceptive method is used.”2
We believe a fresh look at the data is warranted.
EARLY ORAL CONTRACEPTIVES WERE ALL HIGH-DOSE
This issue first surfaced in the decade and a half after the initial launch of oral contraceptives in 1960. The products then were all high-dose pills, containing up to 150 µg of mestranol. In subsequent decades, the dose of estrogen was successively reduced, so that now some pills contain only 10 µg of ethinyl estradiol. High-dose pills—which today contain 50 µg of ethinyl estradiol—account for less than 1% of pills currently sold in the United States and have been eliminated in many countries.
DIAGNOSTIC CRITERIA FOR MIGRAINE
According to the International Classification of Headache Disorders (ICHD),3 the diagnosis of migraine requires 2 of the 4 following criteria:
- Unilateral location
- Pulsating or throbbing pain
- Pain of at least moderate intensity
- Pain aggravated by activity, or causing a preference to avoid activity.
An additional criterion is either nausea or a combination of photophobia and phonophobia with the episode. This criterion can be met if the patient prefers to avoid bright lights and loud noises during an attack.
Headache experts have suggested that patients with a stable pattern of episodic, disabling headache and normal findings on physical examination should be considered to have migraine if there is no contradictory evidence.4,5
Migraine with aura requires at least 2 of the following 4 characteristics3:
- 1 aura symptom, spreading gradually over 5 minutes, or 2 or more aura symptoms occurring in succession, or both
- Each aura symptom lasting 5 to 60 minutes (not “a few seconds,” not “hours”)
- The aura followed by the onset of headache within 60 minutes
- At least 1 aura symptom is unilateral.
Visual blurring, floaters, or split-second flashes before or during a migraine headache do not meet the criteria for aura.
MIGRAINE IS COMMON AND UNDERRECOGNIZED
In a study of 1,203 patients seeking care from a primary care provider for headache,6 94% of the 377 who turned in a diary with enough data to make a diagnosis were diagnosed with a migraine or probable migraine by an expert panel. A quarter of patients who likely had migraine based on an expert review of symptoms did not receive a migraine diagnosis at the time of their office visit.
Similarly, in a large epidemiologic study,7 30,758 adults were asked if they had headaches and, if so, how they named them. Headaches were reported by 23,564 of the participants and were subsequently diagnosed by formal ICHD criteria. Of the 3,074 individuals who met the criteria for migraine, only 53.4% correctly recognized their headaches as migraine. The most common erroneous labels were “sinus headache” and “stress headache.”7
HOW ESTROGEN AFFECTS MIGRAINE
Of note, migraine can be exacerbated during times of cycle irregularity, such as adolescence and perimenopause, the 2 times during a woman’s life associated with the highest risk of unintended pregnancy.10,11
STROKE RISK: ESTROGEN DOSE MATTERS
Shortly after the first combined oral contraceptives were released, reports of adverse events began to appear, although serious events were relatively rare. In response, prescribing guidelines advised against giving oral contraceptives to women with a history of deep vein thrombosis, myocardial infarction, stroke, or hypertension. Also, over the years, the hormonal content of the formulations was successively reduced, and with each reduction in estrogen, a decrease was observed in venous thrombosis and pulmonary embolism.12,13 Current low-dose formulations are considerably safer than high-dose options but are not entirely without risk.14
Stroke risk with combined oral contraceptives was first highlighted in a landmark article in 1975.15 However, the authors were unable to correlate the risk with the estrogen concentration of the pill, since 23 of the 25 women who suffered thrombotic stroke while taking the mestranol-containing formulation took 100-μg pills, and all 20 women who had strokes while taking the ethinyl estradiol formulation took 50-μg pills. Thus, by today’s standards, they were all taking high-dose pills. The risk of thrombotic stroke was 4 to 5 times higher in users than in nonusers.
In 1996, a study from the World Health Organization16 reported an increased risk of stroke with high-dose combined oral contraceptives (odds ratio [OR] 5.30, 95% confidence interval [CI] 2.56–11.0). With preparations containing less than 50 μg of ethinyl estradiol, the risk was not statistically significant (OR 1.53, 95% CI 0.71–3.31). These numbers were for Europe only; in developing countries, the risk was elevated regardless of dose, presumably due to additional risk factors in combined oral contraceptive users. The majority of strokes were in smokers taking 50-μg pills, with an average age greater than 35.
In 2002, a 5-year case-control study in Denmark found that the risk of stroke with combined oral contraceptives correlated directly with the estrogen content, from no increased risk with the newest and lowest-dose formulation (containing ethinyl estradiol 20 µg) to an OR of 4.5 with the older high-dose (50 µg) formulations.17
Reassuringly, a 2012 retrospective review of the Danish national registry13 revealed a low absolute risk of arterial events in users of combined oral contraceptives: 21.4 per 100,000 person-years for thrombotic stroke, and 10.1 per 100,000 person-years for myocardial infarction. Further, these risks were substantially lower with 20-μg ethinyl estradiol products than with those containing 30 to 40 μg.13 An important limitation of this large database review is that it did not control for important stroke risk factors such as obesity and smoking.
Although international studies14,16 continue to show a small but increased risk, more than 30 years have passed since a US study found an increased risk of stroke with combined oral contraceptives.
The discrepancy between US and international studies is possibly explained by the strong relative contraindication in the United States to the use of combined oral contraceptives in smokers over the age of 35 and the more prevalent use of high-dose pills in international studies. High-dose pills had been used in most of the stroke cases in the 1996 World Health Organization study16 but were used by only 0.7% of the women in the case and control groups in 2 pooled US studies from the same time period.18 Similarly, in these US studies, only 17% of the women were smokers on combined oral contraceptives, whereas in the international study, 51% of the women who had strokes and 38% of those in the control groups were smokers.
A large US study19 reviewing 3.6 million woman-years of use found no increased stroke risk (OR 0.96) in current users of low-dose combined oral contraceptives, results similar to those of a pooled analysis of US studies.18 Though this pooled analysis showed an adjusted increased risk of ischemic stroke in women reporting a history of migraine (OR 2.08, 95% CI 1.19–3.65), these conclusions were based on only 4 cases. The prevalence of migraine was identical in women who did or did not have strokes, 7.8% vs 7.7%, respectively, but the risk was judged to be increased after adjusting for other factors. But one important factor was not adjusted for: only 11 of the 1,017 women in the case and control groups were using 50-μg ethinyl estradiol pills, and 4 of the strokes were in this group of 11 women.
STROKE RISK INCREASES WITH FREQUENCY OF MIGRAINE AURA
Use of combined hormonal contraceptives in women who have migraine with aura remains controversial, based on good evidence that aura increases stroke risk20 and good evidence that high-dose oral contraceptives increase stroke risk.15
A cohort study encompassing more than 470,000 person-years with a median follow-up of 26 years found that while migraine without aura conferred no increase in risk of all-cause mortality, migraine with aura did.21
The longitudinal Women’s Health Study analyzed data from 27,798 women over age 45 and found that migraine with aura conferred an increased risk of cardiovascular disease (including stroke) that varied directly with aura frequency.22 Aura frequency less than once a month conferred a risk 2 times higher than in women without migraine, and the risk was more than 4 times higher when aura frequency exceeded once a week.
Similarly, an analysis of the World Health Organization study of stroke in young women found that the adjusted risk of ischemic stroke was significantly and directly associated with aura frequency.20
Potential explanations for this increased risk with greater aura frequency include changes induced during spreading cortical depression, shared genetic predispositions, and common underlying comorbidities such as patent foramen ovale.23–26
Though studies have shown that combined oral contraceptives in continuous regimens27 or in regimens that minimize drops in estrogen levels28 can help improve general headache and menstrual-related migraine, these studies have excluded patients who have migraine with aura.
In a pilot study,29 28 women referred to a tertiary headache clinic who had migraine with aura and intractable menstrual-related migraine were offered combined hormonal contraception in the form of a vaginal ring that releases only 15 μg ethinyl estradiol per 24 hours, thereby reducing peak estrogen exposure to a level lower than those encountered with the native menstrual cycle (with the suppression of ovulation). The women used this continuous ultra-low-dose hormonal contraception without placebo days. After a mean follow-up of 8 months, this regimen reduced aura frequency from a baseline average of 3.2 per month to only 0.2 per month. No woman had an increase in aura frequency, and menstrual-related migraine was eliminated in 21 (91.3%) of the 23 evaluable patients.
CHOOSING THE OPTIMAL CONTRACEPTIVE FORMULATION
Today, ultra-low-dose combined oral contraceptives (containing 10–15 µg of ethinyl estradiol) inhibit ovulation with doses of estrogen that are in a midphysiologic range. Consequently, they expose women to lower peak concentrations of estrogen than they would experience in their natural menstrual cycle (Figure 1). If a combined oral contraceptive is used in women with migraine with aura, lower estrogen doses (≤ 20 µg ethinyl estradiol) are preferred to decrease aura frequency and minimize the risk of stroke associated with high-dose ethinyl estradiol formulations.
Does the progestin matter?
Though there has been debate about whether different types of progestins alter the risk of venous thromboembolism,30,31 the chosen progestin does not seem to affect arterial risks such as stroke and myocardial infarction.14
All current guidelines note that progestin-only pills can be safely offered to women with migraine with aura. However, progestin-only pills have a shorter half-life than combined hormonal contraceptives and must be taken consistently and on time to ensure contraceptive efficacy and minimize abnormal bleeding. Patients who cannot adhere to a strict daily pill regimen may increase their risk of unintended pregnancy. In addition, progestin-only pills do not help with reducing episodes of migraine because they prevent ovulation only about half of the time.2 In contrast, a progestin-only arm implant is not only considered safe to use in women with migraine with aura, it may also prevent ovulation more reliably. Though progestin arm implants have the potential to reduce menstrual migraine and aura, this requires further study to confirm.
For menstrual-related migraine
In clinical practice, providers may offer certain combined hormonal contraceptives to women with debilitating menstrual-related migraine to prevent attacks. Although menstrual-related migraine rarely if ever is accompanied by aura, these patients may still have migraine with aura at other times of the month.
In women with menstrual-related migraine, any decrease in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-withdrawal migraine. All currently available regimens of combined hormonal contraceptives that follow a 21-days-on, 7-days-off plan entail a drop in ethinyl estradiol of more than 10 µg (Figure 1).
Continuous regimens: Who needs a menstrual cycle anyway?
Of note: ultra-low-estrogen combined hormonal contraceptives that have placebo intervals may not inhibit ovulation consistently in all women.32 Contraceptive efficacy is still maintained, as contraception does not require inhibition of ovulation. Other mechanisms such as thickening of cervical mucus help with pregnancy prevention.
However, if ovulation is not inhibited, the consequent postovulatory decline in estrogen will continue to contribute to estrogen-withdrawal migraine.33,34 Reducing the number of placebo days may help inhibit ovulation. Adding back adequate estrogen during the placebo break (eg, either 0.9 mg conjugated equine estrogen with a 20-µg ethinyl estradiol combined oral contraceptive, or 0.075 mg transdermal 17B estradiol with a 15-µg combined hormonal contraceptive) can prevent these migraines.33,34
Some extended-cycle regimens, which give 4 withdrawal bleeds per year, will likewise prevent estrogen-withdrawal migraine if the decline in estrogen is limited to 10 µg (Table 1). Unfortunately, most extended regimens (Seasonale, Seasonique, and their generics) entail a 20- or 30-µg drop.
Continuous or extended-cycle regimens can be prescribed using any generic 20-µg combined hormonal contraceptive that the patient tolerates, along with specific instructions on the prescription to take the pills in a continuous fashion, eg, “Do not take the placebo pills; start the next pill pack immediately after 21 days.”
Postmenopausal hormone therapy
Neither smoking nor migraine is a contraindication to the use of postmenopausal hormone therapy, which is substantially lower in dosage than combined hormonal contraceptives.
ADVISING PATIENTS ON RISKS VS BENEFITS
It is important to remember that the risks of unintended pregnancy are always greater than the risks of any contraceptive, especially in women with chronic medical conditions, including those who have migraine with aura. Other benefits include the following:
Lower mortality risk. A 2010 analysis demonstrated that in nearly 46,000 women followed since 1968, those taking combined oral contraceptives had statistically significantly lower death rates from any cause and a lower risk of death from cancer and cardiovascular diseases than women who had never taken combined oral contraceptives.36
Stroke. Though the absolute risk of stroke to an individual woman taking a low-dose or ultra-low-dose combined hormonal contraceptive has been shown to be similar to that in women who are not taking combined hormonal contraception, its impact on an otherwise healthy woman could be devastating. Clinicians must remember that current guidelines still caution against prescribing combined hormonal contraceptives in women with migraine with aura and thus should counsel their patients accordingly and document the discussion in the medical record.
Noncontraceptive benefits. Women may be prescribed a combined hormonal contraceptive for benefits beyond contraception. The obvious reasons include beneficial effects on endometriosis, anemia, acne, hirsutism, dysmenorrhea, and prevention of ovarian cysts. But other important major benefits2 include substantial reductions in the risk of ovarian cancer (> 50% decrease after 10 years)37 and endometrial cancer (additional 24% reduction for each 5 years of use),38 and a modest decrease in the risk of colon cancer (37% less risk in ever-users).39 Further, combined oral contraceptive use has been associated with a decrease in mortality rates,40,41 with no increased risk of nonreproductive cancers.41
Ultra-low-dose, continuous formulations may benefit women by decreasing the frequency of migraine with aura and menstrual-related migraine. There is no evidence that reducing aura frequency also reduces stroke risk, but this represents an important area for future research.
WHAT WOULD WE DO?
For a patient who has a history of migraine with aura, if the goal is only to prevent pregnancy, we would recommend another contraceptive option that does not involve estrogen. However, we would consider prescribing a combined hormonal contraceptive in a low-dose regimen if the patient prefers this regimen for other health benefits (eg, acne control), if she has no other risk factors for stroke, and if she gives her informed consent after a discussion of the risks and benefits. Women who have menstrual-related migraine refractory to or who cannot tolerate other migraine therapies are often willing to try a low-dose estrogen-containing contraceptive for control of their migraine, especially if they have tried it in the past and believe that it helped prevent migraine. Patients should have follow-up within 3 months to discuss whether they have benefited from the regimen in terms of headache frequency or severity.
- ACOG Practice Bulletin No. 110: noncontraceptive uses of hormonal contraceptives. Obstet Gynecol 2010; 115:206–218.
- Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports/Centers for Disease Control 2016; 65:1–104.
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013; 33:629–808.
- Lipton RB, Cady RK, Stewart WF, Wilks K, Hall C. Diagnostic lessons from the Spectrum study. Neurology 2002; 58(suppl 6):S27–S31.
- Lipton RB, Stewart WF, Cady R, et al. 2000 Wolfe Award. Sumatriptan for the range of headaches in migraine sufferers: results of the Spectrum Study. Headache 2000; 40:783–791.
- Tepper SJ, Dahlof CG, Dowson A, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the Landmark Study. Headache 2004; 44:856–864.
- Lipton RB, Stewart WF, Liberman JN. Self-awareness of migraine: interpreting the labels that headache sufferers apply to their headaches. Neurology 2002; 58(suppl 6):S21–S26.
- Chai NC, Peterlin BL, Calhoun AH. Migraine and estrogen. Curr Opin Neurol 2014; 27:315–324.
- Calhoun AH. Menstrual migraine: update on pathophysiology and approach to therapy and management. Curr Treat Options Neurol 2012; 14:1–14.
- McNamara M, Batur P, DeSapri KT. In the clinic. Perimenopause. Ann Intern Med 2015; 162:ITC1–ITC15.
- O’Brien HL, Cohen JM. Young adults with headaches: the transition from adolescents to adults. Headache 2015; 55:1404–1409.
- Vessey M, Mant D, Smith A, Yeates D. Oral contraceptives and venous thromboembolism: findings in a large prospective study. Br Med J (Clin Res Ed) 1986; 292:526.
- Lidegaard O, Lokkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- MacGregor EA. Contraception and headache. Headache 2013; 53:247–276.
- Oral contraceptives and stroke in young women. Associated risk factors. JAMA 1975; 231:718–722.
- Ischaemic stroke and combined oral contraceptives: results of an international, multicentre, case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet 1996; 348:498–505.
- Lidegaard O, Kreiner S. Contraceptives and cerebral thrombosis: a five-year national case-control study. Contraception 2002; 65:197–205.
- Schwartz SM, Petitti DB, Siscovick DS, et al. Stroke and use of low-dose oral contraceptives in young women: a pooled analysis of two US studies. Stroke 1998; 29:2277–2284.
- Petitti DB, Sidney S, Bernstein A, Wolf S, Quesenberry C, Ziel HK. Stroke in users of low-dose oral contraceptives. N Engl J Med 1996; 335:8–15.
- Donaghy M, Chang CL, Poulter N; European Collaborators of the World Health Organisation Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Duration, frequency, recency, and type of migraine and the risk of ischaemic stroke in women of childbearing age. J Neurol Neurosurg Psychiatry 2002; 73:747–750.
- Gudmundsson LS, Scher AI, Aspelund T, et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ 2010; 341:c3966.
- Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology 2005; 64:1020–1026.
- Lee ST, Chu K, Jung KH, et al. Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology 2008; 70:1510–1517.
- Kunz GA, Liang G, Cuculi F, et al. Circulating endothelial progenitor cells predict coronary artery disease severity. Am Heart J 2006; 152:190–195.
- Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA 2006; 296:283–291.
- Pezzini A, Del Zotto E, Giossi A, Volonghi I, Grassi M, Padovani A. The migraine-ischemic stroke connection: potential pathogenic mechanisms. Curr Mol Med 2009; 9:215–226.
- Sulak P, Willis S, Kuehl T, Coffee A, Clark J. Headaches and oral contraceptives: impact of eliminating the standard 7-day placebo interval. Headache 2007; 47:27–37.
- Nappi RE, Terreno E, Sances G, et al. Effect of a contraceptive pill containing estradiol valerate and dienogest (E2V/DNG) in women with menstrually-related migraine (MRM). Contraception 2013; 88:369–375.
- Calhoun A, Ford S, Pruitt A. The impact of extended-cycle vaginal ring contraception on migraine aura: a retrospective case series. Headache 2012; 52:1246–1253.
- Wu CQ, Grandi SM, Filion KB, Abenhaim HA, Joseph L, Eisenberg MJ. Drospirenone-containing oral contraceptive pills and the risk of venous and arterial thrombosis: a systematic review. BJOG 2013; 120:801–810.
- Dinger J, Bardenheuer K, Heinemann K. Cardiovascular and general safety of a 24-day regimen of drospirenone-containing combined oral contraceptives: final results from the International Active Surveillance Study of Women Taking Oral Contraceptives. Contraception 2014; 89:253–263.
- Benson LS, Micks EA. Why stop now? Extended and continuous regimens of combined hormonal contraceptive methods. Obstet Gynecol Clin North Am 2015; 42:669–681.
- Mannix LK, Calhoun AH. Menstrual migraine. Curr Treat Options Neurol 2004; 6:489–498.
- Calhoun AH. A novel specific prophylaxis for menstrual-associated migraine. South Med J 2004; 97:819–822.
- Calhoun AH. Current topics and controversies in menstrual migraine. Headache 2012; 52(suppl 1):8–11.
- Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V, Lee AJ. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ 2010; 340:c927.
- Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive pills as primary prevention for ovarian cancer: a systematic review and meta-analysis. Obstet Gynecol 2013; 122:139 -147.
- Collaborative Group on Epidemiological Studies on Endometrial Cancer. Endometrial cancer and oral contraceptives: an individual participant meta-analysis of 27,276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol 2015; 16:1061–1070.
- Fernandez E, La Vecchia C, Franceschi S, et al. Oral contraceptive use and risk of colorectal cancer. Epidemiology 1998; 9:295–300.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition; a cohort study. BMC Med 2015; 13:252.
- Vessey M, Yeates D. Oral contraceptive use and cancer: final report from the Oxford-Family Planning Association Contraceptive Study. Contraception 2013; 88:678–683.
- ACOG Practice Bulletin No. 110: noncontraceptive uses of hormonal contraceptives. Obstet Gynecol 2010; 115:206–218.
- Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports/Centers for Disease Control 2016; 65:1–104.
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013; 33:629–808.
- Lipton RB, Cady RK, Stewart WF, Wilks K, Hall C. Diagnostic lessons from the Spectrum study. Neurology 2002; 58(suppl 6):S27–S31.
- Lipton RB, Stewart WF, Cady R, et al. 2000 Wolfe Award. Sumatriptan for the range of headaches in migraine sufferers: results of the Spectrum Study. Headache 2000; 40:783–791.
- Tepper SJ, Dahlof CG, Dowson A, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the Landmark Study. Headache 2004; 44:856–864.
- Lipton RB, Stewart WF, Liberman JN. Self-awareness of migraine: interpreting the labels that headache sufferers apply to their headaches. Neurology 2002; 58(suppl 6):S21–S26.
- Chai NC, Peterlin BL, Calhoun AH. Migraine and estrogen. Curr Opin Neurol 2014; 27:315–324.
- Calhoun AH. Menstrual migraine: update on pathophysiology and approach to therapy and management. Curr Treat Options Neurol 2012; 14:1–14.
- McNamara M, Batur P, DeSapri KT. In the clinic. Perimenopause. Ann Intern Med 2015; 162:ITC1–ITC15.
- O’Brien HL, Cohen JM. Young adults with headaches: the transition from adolescents to adults. Headache 2015; 55:1404–1409.
- Vessey M, Mant D, Smith A, Yeates D. Oral contraceptives and venous thromboembolism: findings in a large prospective study. Br Med J (Clin Res Ed) 1986; 292:526.
- Lidegaard O, Lokkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- MacGregor EA. Contraception and headache. Headache 2013; 53:247–276.
- Oral contraceptives and stroke in young women. Associated risk factors. JAMA 1975; 231:718–722.
- Ischaemic stroke and combined oral contraceptives: results of an international, multicentre, case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet 1996; 348:498–505.
- Lidegaard O, Kreiner S. Contraceptives and cerebral thrombosis: a five-year national case-control study. Contraception 2002; 65:197–205.
- Schwartz SM, Petitti DB, Siscovick DS, et al. Stroke and use of low-dose oral contraceptives in young women: a pooled analysis of two US studies. Stroke 1998; 29:2277–2284.
- Petitti DB, Sidney S, Bernstein A, Wolf S, Quesenberry C, Ziel HK. Stroke in users of low-dose oral contraceptives. N Engl J Med 1996; 335:8–15.
- Donaghy M, Chang CL, Poulter N; European Collaborators of the World Health Organisation Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Duration, frequency, recency, and type of migraine and the risk of ischaemic stroke in women of childbearing age. J Neurol Neurosurg Psychiatry 2002; 73:747–750.
- Gudmundsson LS, Scher AI, Aspelund T, et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ 2010; 341:c3966.
- Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology 2005; 64:1020–1026.
- Lee ST, Chu K, Jung KH, et al. Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology 2008; 70:1510–1517.
- Kunz GA, Liang G, Cuculi F, et al. Circulating endothelial progenitor cells predict coronary artery disease severity. Am Heart J 2006; 152:190–195.
- Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA 2006; 296:283–291.
- Pezzini A, Del Zotto E, Giossi A, Volonghi I, Grassi M, Padovani A. The migraine-ischemic stroke connection: potential pathogenic mechanisms. Curr Mol Med 2009; 9:215–226.
- Sulak P, Willis S, Kuehl T, Coffee A, Clark J. Headaches and oral contraceptives: impact of eliminating the standard 7-day placebo interval. Headache 2007; 47:27–37.
- Nappi RE, Terreno E, Sances G, et al. Effect of a contraceptive pill containing estradiol valerate and dienogest (E2V/DNG) in women with menstrually-related migraine (MRM). Contraception 2013; 88:369–375.
- Calhoun A, Ford S, Pruitt A. The impact of extended-cycle vaginal ring contraception on migraine aura: a retrospective case series. Headache 2012; 52:1246–1253.
- Wu CQ, Grandi SM, Filion KB, Abenhaim HA, Joseph L, Eisenberg MJ. Drospirenone-containing oral contraceptive pills and the risk of venous and arterial thrombosis: a systematic review. BJOG 2013; 120:801–810.
- Dinger J, Bardenheuer K, Heinemann K. Cardiovascular and general safety of a 24-day regimen of drospirenone-containing combined oral contraceptives: final results from the International Active Surveillance Study of Women Taking Oral Contraceptives. Contraception 2014; 89:253–263.
- Benson LS, Micks EA. Why stop now? Extended and continuous regimens of combined hormonal contraceptive methods. Obstet Gynecol Clin North Am 2015; 42:669–681.
- Mannix LK, Calhoun AH. Menstrual migraine. Curr Treat Options Neurol 2004; 6:489–498.
- Calhoun AH. A novel specific prophylaxis for menstrual-associated migraine. South Med J 2004; 97:819–822.
- Calhoun AH. Current topics and controversies in menstrual migraine. Headache 2012; 52(suppl 1):8–11.
- Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V, Lee AJ. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ 2010; 340:c927.
- Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive pills as primary prevention for ovarian cancer: a systematic review and meta-analysis. Obstet Gynecol 2013; 122:139 -147.
- Collaborative Group on Epidemiological Studies on Endometrial Cancer. Endometrial cancer and oral contraceptives: an individual participant meta-analysis of 27,276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol 2015; 16:1061–1070.
- Fernandez E, La Vecchia C, Franceschi S, et al. Oral contraceptive use and risk of colorectal cancer. Epidemiology 1998; 9:295–300.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition; a cohort study. BMC Med 2015; 13:252.
- Vessey M, Yeates D. Oral contraceptive use and cancer: final report from the Oxford-Family Planning Association Contraceptive Study. Contraception 2013; 88:678–683.
KEY POINTS
- There is no restriction on the use of combined hormonal contraceptives by women with migraine without aura, and the risk vs benefit for women with aura is debatable.
- Migraine with aura—but not migraine without aura—is associated with a twofold increased risk of ischemic stroke, although the absolute risk is small in healthy women who do not smoke.
- Combined hormonal contraceptives are associated with ischemic stroke, but the risk is dose-dependent. Ultra-low-dose formulations (containing ≤ 20 μg of ethinyl estradiol) do not pose an increased risk of stroke in healthy nonsmokers.
Annual mammography starting at age 40: More talk, less action?
National societies agree on the value of mammographic screening at age 50 through 69 (though the frequency is still debated), but there is no consensus about whether to screen at age 40 through 49, or age 70 and older. The US Preventive Services Task Force (USPSTF) recommends against routinely screening women age 40 through 49, while the American Academy of Family Physicians and the American College of Physicians recommend screening every 1 to 2 years for women in this age group. The American Cancer Society, the American Medical Association, the National Cancer Institute, the American College of Radiology, and the American Congress of Obstetricians and Gynecologists recommend yearly mammography starting at age 40.1
Besides female sex, the major risk factor for breast cancer is increasing age. Thus, women in their 40s are at significantly lower risk of breast cancer than those in their 50s. As emerging evidence focuses on the potential harms and benefits from screening, we must question the practice of annual screening starting at age 40.
DOES MAMMOGRAPHIC SCREENING SAVE LIVES?
The main goal of screening for any type of cancer is to reduce the death rate. A 2014 meta-analysis of randomized controlled trials found a 15% to 20% relative decrease in the breast cancer mortality rate with screening mammography, approximately 15% for women in their 40s and 32% for women in their 60s.2 Since the prevalence of breast cancer is lower in younger women, many more women in their 40s must be screened to prevent one breast cancer death. For women age 60 to 69, 377 must be screened to prevent one breast cancer death, whereas for women age 39 to 49 the number is 1,904.3
Whether screening for breast cancer reduces the death rate has been questioned following the 2014 publication of 25-year follow-up data from the Canadian National Breast Screening Study.4 This randomized controlled trial of screening mammography and clinical breast examination, launched in 1980, involved 89,835 women and 5 years of screening. Women age 40 to 49 were randomly assigned to undergo either five annual mammographic screenings and annual clinical breast examinations or no mammography and a single clinical breast examination, followed by usual care in the community. Those age 50 to 59 received annual clinical breast examinations and were randomized to either mammography or no mammography.
During 25 years of follow-up, 3,250 women in the mammography group and 3,133 in the control group were diagnosed with breast cancer, and 500 and 505, respectively, died of breast cancer. No difference in mortality rate was found between the mammography and control groups (hazard ratio 0.99, 95% confidence interval 0.88–1.12), and the findings in both age cohorts were similar.4
Criticisms of this study include that it was performed using outdated imaging technology, and that a significant proportion of the control group also received mammography, although it is also possible that the mortality benefit from mammographic screening alone may not be as high as once predicted.
Reduction in breast cancer mortality is likely from a combination of screening mammography and better treatment. The number of women presenting with late-stage cancers has decreased in the past 3 decades, but only slightly; and most of the decrease has been in regional, node-positive disease, a stage that can now often be treated successfully (the expected 5-year survival rate is 85% in women age 40 or older).5 For women with estrogen receptor-positive tumors, the combination of hormonal therapy and adjuvant chemotherapy has reduced the death rate by half.6
It has been 50 years since a large randomized controlled trial of mammographic screening has been done in the United States. Thus, further study is needed to understand whether screening is less valuable now that better treatments are available.
DOES MAMMOGRAPHIC SCREENING REDUCE LATE-STAGE CANCERS?
To be effective, screening must detect disease at an earlier, more curable stage. Although screening mammography has substantially increased the number of early-stage breast cancers detected, it has only marginally decreased the rate of diagnosis of late-stage cancers.5
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) data5 show that between 1976 and 2008 screening mammography was associated with a doubling in early-stage breast cancer cases detected (from 112 to 234 cases per 100,000 women per year, an absolute increase of 122 cases per 100,000 per year). In contrast, late-stage cancer diagnoses decreased by 8% (from 102 to 94 cases per 100,000 women per year, or an absolute decrease of 8 per 100,000 women per year). Assuming a constant underlying disease burden, only 8 of the 122 early-stage cancers diagnosed would be expected to progress to advanced disease, suggesting that the rest would have never harmed these women—ie, they were overdiagnosed. The authors estimated that in 2008, breast cancer was overdiagnosed in more than 70,000 women, accounting for 31% of all diagnosed breast cancers.5
HARMS OF OVERDIAGNOSIS
Based on SEER data, Bleyer and Welch5 estimated that more than 1 million US women may have been overdiagnosed with breast cancer in the past 3 decades. Many women in this situation subsequently undergo surgery, radiation therapy, hormonal therapy, chemotherapy, or a combination of these for a cancer that may never become clinically significant. Until we can differentiate deadly from indolent cancers, highly sensitive screening tests will increase the risk of overtreatment.
Breast cancer has increased in incidence since the 1990s, mostly from the detection of more early-stage cancer or ductal carcinoma in situ (DCIS). Rare before widespread screening, DCIS now accounts for 20% to 30% of all breast cancer diagnoses.6,7 However, DCIS is not always a precursor to invasive cancer: untreated, it progresses to invasive disease in half of cases or fewer. Because DCIS is usually diagnosed only with mammography, its incidence has been steadily on the rise since screening became widespread.1
Welch and Passow6 reviewed the available evidence and attempted to provide a range of estimates for three outcomes important to the mammography decision: breast cancer deaths avoided, false alarms, and overdiagnosis. For every 1,000 US women screened yearly for a decade starting at age 50, an estimated 0.3 to 3.2 avoided breast cancer death, 490 to 670 had at least one false alarm, and 3 to 14 were overdiagnosed and treated needlessly.
Esserman et al7 calculated that in women age 50 to 70, prevention of one breast cancer death would require that 838 women be screened for 6 years, leading to 5,866 screening visits, 535 recalls, 90 biopsies, and 24 cancers treated (18 invasive, 6 DCIS).
SCREENING EVERY YEAR VS EVERY 2 YEARS
Also controversial is whether screening mammography should be done annually or every 2 years. For women in their 50s, the American Cancer Society recommends mammography every year, the American College of Physicians and American Academy of Family Physicians recommend it every 1 to 2 years, and the USPSTF recommends it every 2 years.
A prospective analysis of 11,474 women with breast cancer and 922,624 controls8 found that performing mammography every 2 years instead of annually for women age 50 to 74 did not increase the risk of advanced-stage or large-size tumors regardless of breast density or hormone therapy use. But women undergoing annual mammography had a higher risk of false-positive results and biopsy recommendations.8 Women age 40 to 49 with extremely dense breasts were the only subgroup who derived additional benefit from annual screening, as they had a higher risk of advanced-stage cancer if they were screened every 2 years instead of yearly (odds ratio [OR] 1.89; 95% CI 1.06–3.39) and a higher risk of larger tumors (OR 2.39; 95% CI 1.37–4.18). However, the probability of a false-positive result in these younger women undergoing annual mammography was also very high at 65.5%.8
For most women in their 40s (other than those with extremely dense breasts) and 50s, biennial and annual mammography were associated with a similar risk of advanced-stage disease. Women with fatty breasts are at low risk of breast cancer regardless of other risk factors and did not appear to benefit from annual screening.8 The 12% to 15% of women in their 40s with extremely dense breasts (whose risk of breast cancer is similar to that in average-risk women in their 50s) should decide if the added benefit of annual screening is outweighed by the additional harms, including doubling the number of mammograms, as well as more false-positive results and breast biopsy recommendations.8
Mandelblatt et al9 statistically evaluated 20 screening strategies, ie, screening every year or every 2 years, and starting and stopping at various ages. On average, screening every 2 years was 81% as beneficial as annual screening but caused only about half as many false-positive results. Women age 50 through 69 who were screened every 2 years achieved a median 16.5% (range 15%–23%) reduction in breast cancer deaths compared with no screening. Initiating screening every 2 years at age 40 reduced the death rate by an additional 3% (range 1%–6%) compared with starting at age 50. Not surprisingly, starting screening at age 40 consumed more resources and yielded more false-positive results. After age 69, screening every 2 years yielded some additional mortality reduction in all models, but overdiagnosis increased most substantially at older ages, as the ratio of slow- to fast-growing tumors increases with age. The authors concluded that screening every 2 years achieves most of the benefit of annual screening with less harm.
FALSE-POSITIVE RESULTS AND ANXIETY
False-positive results on mammography can increase distress and anxiety about breast cancer and perceived breast cancer risk in some women.3 After 10 years of annual screening, more than half of women receive at least one false-positive recall, and 7% to 9% receive a false-positive biopsy recommendation. It is helpful for women to understand this risk when deciding whether to start mammographic screening.10
OUR VIEWS
There are two major issues to address in clinical practice regarding mammographic screening: at what age to start, and how often to screen. For years, women have been instructed to start annual mammographic screening at age 40, and such established patterns can be difficult to change.
When deciding whether to have a mammogram at age 40, women should be aware of the full range of risks and benefits. Assessing a woman’s individual risk of breast cancer (based on family history and number and age of pregnancies) can be an important starting point for assessing the potential benefits and risks of screening.
Although a shared decision-making approach is intuitively appealing, it takes much more time than simply ordering a mammogram. Time constraints during a medical appointment may make it challenging to have a prolonged discussion about the pros and cons of screening. Patient education materials about the risks vs benefits of screening initiation may be useful, and because the decision does not usually need to be made urgently, women can be given the opportunity to consider the decision outside of the primary care appointment.
The issue of annual vs biennial screening presents an additional challenge, because women have come to expect annual screening. Studies show that the only subgroup of women who appear to benefit from annual screening are those in their 40s with dense breasts. Although breast cancer is rarer in younger women, when it does develop, it is often more aggressive, so offering annual screening to this subpopulation may make sense. For all other women, since there is no evidence that annual mammography offers clinical benefit over biennial screening, clinicians can be comfortable with offering screening every 2 years.
Future research must focus on developing better tools for differentiating women who are at higher vs lower risk for breast cancer and on developing methods to determine which DCIS cancers are more likely to be indolent and therefore amenable to watchful waiting.
In the interim, we must continue to identify women at high risk who will benefit from magnetic resonance imaging, genetic testing, and prophylactic medications, in accordance with USPSTF recommendations. Women with new breast symptoms or concerns should continue to undergo evaluation with diagnostic imaging, including mammography. However, for most women who are at average risk and have no symptoms, we must ensure that they are fully aware of the possible benefits and risks of screening mammography so that they can make an informed decision about when to start screening and how often to be screened.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726.
- Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014; 311:1327–1335.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L; US Preventive Services Task Force. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med 2009; 151:727–737.
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014; 348:g366.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 2012; 367:1998–2005.
- Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med 2014; 174:448–454.
- Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA 2009; 302:1685–1692.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med 2013; 173:807–816.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 2009; 151:738–747.
- Hubbard RA, Kerlikowske K, Flowers CI, Yankaskas BC, Zhu W, Miglioretti DL. Cumulative probability of false-positive recall or biopsy recommendation after 10 years of screening mammography: a cohort study. Ann Intern Med 2011; 155:481–492.
National societies agree on the value of mammographic screening at age 50 through 69 (though the frequency is still debated), but there is no consensus about whether to screen at age 40 through 49, or age 70 and older. The US Preventive Services Task Force (USPSTF) recommends against routinely screening women age 40 through 49, while the American Academy of Family Physicians and the American College of Physicians recommend screening every 1 to 2 years for women in this age group. The American Cancer Society, the American Medical Association, the National Cancer Institute, the American College of Radiology, and the American Congress of Obstetricians and Gynecologists recommend yearly mammography starting at age 40.1
Besides female sex, the major risk factor for breast cancer is increasing age. Thus, women in their 40s are at significantly lower risk of breast cancer than those in their 50s. As emerging evidence focuses on the potential harms and benefits from screening, we must question the practice of annual screening starting at age 40.
DOES MAMMOGRAPHIC SCREENING SAVE LIVES?
The main goal of screening for any type of cancer is to reduce the death rate. A 2014 meta-analysis of randomized controlled trials found a 15% to 20% relative decrease in the breast cancer mortality rate with screening mammography, approximately 15% for women in their 40s and 32% for women in their 60s.2 Since the prevalence of breast cancer is lower in younger women, many more women in their 40s must be screened to prevent one breast cancer death. For women age 60 to 69, 377 must be screened to prevent one breast cancer death, whereas for women age 39 to 49 the number is 1,904.3
Whether screening for breast cancer reduces the death rate has been questioned following the 2014 publication of 25-year follow-up data from the Canadian National Breast Screening Study.4 This randomized controlled trial of screening mammography and clinical breast examination, launched in 1980, involved 89,835 women and 5 years of screening. Women age 40 to 49 were randomly assigned to undergo either five annual mammographic screenings and annual clinical breast examinations or no mammography and a single clinical breast examination, followed by usual care in the community. Those age 50 to 59 received annual clinical breast examinations and were randomized to either mammography or no mammography.
During 25 years of follow-up, 3,250 women in the mammography group and 3,133 in the control group were diagnosed with breast cancer, and 500 and 505, respectively, died of breast cancer. No difference in mortality rate was found between the mammography and control groups (hazard ratio 0.99, 95% confidence interval 0.88–1.12), and the findings in both age cohorts were similar.4
Criticisms of this study include that it was performed using outdated imaging technology, and that a significant proportion of the control group also received mammography, although it is also possible that the mortality benefit from mammographic screening alone may not be as high as once predicted.
Reduction in breast cancer mortality is likely from a combination of screening mammography and better treatment. The number of women presenting with late-stage cancers has decreased in the past 3 decades, but only slightly; and most of the decrease has been in regional, node-positive disease, a stage that can now often be treated successfully (the expected 5-year survival rate is 85% in women age 40 or older).5 For women with estrogen receptor-positive tumors, the combination of hormonal therapy and adjuvant chemotherapy has reduced the death rate by half.6
It has been 50 years since a large randomized controlled trial of mammographic screening has been done in the United States. Thus, further study is needed to understand whether screening is less valuable now that better treatments are available.
DOES MAMMOGRAPHIC SCREENING REDUCE LATE-STAGE CANCERS?
To be effective, screening must detect disease at an earlier, more curable stage. Although screening mammography has substantially increased the number of early-stage breast cancers detected, it has only marginally decreased the rate of diagnosis of late-stage cancers.5
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) data5 show that between 1976 and 2008 screening mammography was associated with a doubling in early-stage breast cancer cases detected (from 112 to 234 cases per 100,000 women per year, an absolute increase of 122 cases per 100,000 per year). In contrast, late-stage cancer diagnoses decreased by 8% (from 102 to 94 cases per 100,000 women per year, or an absolute decrease of 8 per 100,000 women per year). Assuming a constant underlying disease burden, only 8 of the 122 early-stage cancers diagnosed would be expected to progress to advanced disease, suggesting that the rest would have never harmed these women—ie, they were overdiagnosed. The authors estimated that in 2008, breast cancer was overdiagnosed in more than 70,000 women, accounting for 31% of all diagnosed breast cancers.5
HARMS OF OVERDIAGNOSIS
Based on SEER data, Bleyer and Welch5 estimated that more than 1 million US women may have been overdiagnosed with breast cancer in the past 3 decades. Many women in this situation subsequently undergo surgery, radiation therapy, hormonal therapy, chemotherapy, or a combination of these for a cancer that may never become clinically significant. Until we can differentiate deadly from indolent cancers, highly sensitive screening tests will increase the risk of overtreatment.
Breast cancer has increased in incidence since the 1990s, mostly from the detection of more early-stage cancer or ductal carcinoma in situ (DCIS). Rare before widespread screening, DCIS now accounts for 20% to 30% of all breast cancer diagnoses.6,7 However, DCIS is not always a precursor to invasive cancer: untreated, it progresses to invasive disease in half of cases or fewer. Because DCIS is usually diagnosed only with mammography, its incidence has been steadily on the rise since screening became widespread.1
Welch and Passow6 reviewed the available evidence and attempted to provide a range of estimates for three outcomes important to the mammography decision: breast cancer deaths avoided, false alarms, and overdiagnosis. For every 1,000 US women screened yearly for a decade starting at age 50, an estimated 0.3 to 3.2 avoided breast cancer death, 490 to 670 had at least one false alarm, and 3 to 14 were overdiagnosed and treated needlessly.
Esserman et al7 calculated that in women age 50 to 70, prevention of one breast cancer death would require that 838 women be screened for 6 years, leading to 5,866 screening visits, 535 recalls, 90 biopsies, and 24 cancers treated (18 invasive, 6 DCIS).
SCREENING EVERY YEAR VS EVERY 2 YEARS
Also controversial is whether screening mammography should be done annually or every 2 years. For women in their 50s, the American Cancer Society recommends mammography every year, the American College of Physicians and American Academy of Family Physicians recommend it every 1 to 2 years, and the USPSTF recommends it every 2 years.
A prospective analysis of 11,474 women with breast cancer and 922,624 controls8 found that performing mammography every 2 years instead of annually for women age 50 to 74 did not increase the risk of advanced-stage or large-size tumors regardless of breast density or hormone therapy use. But women undergoing annual mammography had a higher risk of false-positive results and biopsy recommendations.8 Women age 40 to 49 with extremely dense breasts were the only subgroup who derived additional benefit from annual screening, as they had a higher risk of advanced-stage cancer if they were screened every 2 years instead of yearly (odds ratio [OR] 1.89; 95% CI 1.06–3.39) and a higher risk of larger tumors (OR 2.39; 95% CI 1.37–4.18). However, the probability of a false-positive result in these younger women undergoing annual mammography was also very high at 65.5%.8
For most women in their 40s (other than those with extremely dense breasts) and 50s, biennial and annual mammography were associated with a similar risk of advanced-stage disease. Women with fatty breasts are at low risk of breast cancer regardless of other risk factors and did not appear to benefit from annual screening.8 The 12% to 15% of women in their 40s with extremely dense breasts (whose risk of breast cancer is similar to that in average-risk women in their 50s) should decide if the added benefit of annual screening is outweighed by the additional harms, including doubling the number of mammograms, as well as more false-positive results and breast biopsy recommendations.8
Mandelblatt et al9 statistically evaluated 20 screening strategies, ie, screening every year or every 2 years, and starting and stopping at various ages. On average, screening every 2 years was 81% as beneficial as annual screening but caused only about half as many false-positive results. Women age 50 through 69 who were screened every 2 years achieved a median 16.5% (range 15%–23%) reduction in breast cancer deaths compared with no screening. Initiating screening every 2 years at age 40 reduced the death rate by an additional 3% (range 1%–6%) compared with starting at age 50. Not surprisingly, starting screening at age 40 consumed more resources and yielded more false-positive results. After age 69, screening every 2 years yielded some additional mortality reduction in all models, but overdiagnosis increased most substantially at older ages, as the ratio of slow- to fast-growing tumors increases with age. The authors concluded that screening every 2 years achieves most of the benefit of annual screening with less harm.
FALSE-POSITIVE RESULTS AND ANXIETY
False-positive results on mammography can increase distress and anxiety about breast cancer and perceived breast cancer risk in some women.3 After 10 years of annual screening, more than half of women receive at least one false-positive recall, and 7% to 9% receive a false-positive biopsy recommendation. It is helpful for women to understand this risk when deciding whether to start mammographic screening.10
OUR VIEWS
There are two major issues to address in clinical practice regarding mammographic screening: at what age to start, and how often to screen. For years, women have been instructed to start annual mammographic screening at age 40, and such established patterns can be difficult to change.
When deciding whether to have a mammogram at age 40, women should be aware of the full range of risks and benefits. Assessing a woman’s individual risk of breast cancer (based on family history and number and age of pregnancies) can be an important starting point for assessing the potential benefits and risks of screening.
Although a shared decision-making approach is intuitively appealing, it takes much more time than simply ordering a mammogram. Time constraints during a medical appointment may make it challenging to have a prolonged discussion about the pros and cons of screening. Patient education materials about the risks vs benefits of screening initiation may be useful, and because the decision does not usually need to be made urgently, women can be given the opportunity to consider the decision outside of the primary care appointment.
The issue of annual vs biennial screening presents an additional challenge, because women have come to expect annual screening. Studies show that the only subgroup of women who appear to benefit from annual screening are those in their 40s with dense breasts. Although breast cancer is rarer in younger women, when it does develop, it is often more aggressive, so offering annual screening to this subpopulation may make sense. For all other women, since there is no evidence that annual mammography offers clinical benefit over biennial screening, clinicians can be comfortable with offering screening every 2 years.
Future research must focus on developing better tools for differentiating women who are at higher vs lower risk for breast cancer and on developing methods to determine which DCIS cancers are more likely to be indolent and therefore amenable to watchful waiting.
In the interim, we must continue to identify women at high risk who will benefit from magnetic resonance imaging, genetic testing, and prophylactic medications, in accordance with USPSTF recommendations. Women with new breast symptoms or concerns should continue to undergo evaluation with diagnostic imaging, including mammography. However, for most women who are at average risk and have no symptoms, we must ensure that they are fully aware of the possible benefits and risks of screening mammography so that they can make an informed decision about when to start screening and how often to be screened.
National societies agree on the value of mammographic screening at age 50 through 69 (though the frequency is still debated), but there is no consensus about whether to screen at age 40 through 49, or age 70 and older. The US Preventive Services Task Force (USPSTF) recommends against routinely screening women age 40 through 49, while the American Academy of Family Physicians and the American College of Physicians recommend screening every 1 to 2 years for women in this age group. The American Cancer Society, the American Medical Association, the National Cancer Institute, the American College of Radiology, and the American Congress of Obstetricians and Gynecologists recommend yearly mammography starting at age 40.1
Besides female sex, the major risk factor for breast cancer is increasing age. Thus, women in their 40s are at significantly lower risk of breast cancer than those in their 50s. As emerging evidence focuses on the potential harms and benefits from screening, we must question the practice of annual screening starting at age 40.
DOES MAMMOGRAPHIC SCREENING SAVE LIVES?
The main goal of screening for any type of cancer is to reduce the death rate. A 2014 meta-analysis of randomized controlled trials found a 15% to 20% relative decrease in the breast cancer mortality rate with screening mammography, approximately 15% for women in their 40s and 32% for women in their 60s.2 Since the prevalence of breast cancer is lower in younger women, many more women in their 40s must be screened to prevent one breast cancer death. For women age 60 to 69, 377 must be screened to prevent one breast cancer death, whereas for women age 39 to 49 the number is 1,904.3
Whether screening for breast cancer reduces the death rate has been questioned following the 2014 publication of 25-year follow-up data from the Canadian National Breast Screening Study.4 This randomized controlled trial of screening mammography and clinical breast examination, launched in 1980, involved 89,835 women and 5 years of screening. Women age 40 to 49 were randomly assigned to undergo either five annual mammographic screenings and annual clinical breast examinations or no mammography and a single clinical breast examination, followed by usual care in the community. Those age 50 to 59 received annual clinical breast examinations and were randomized to either mammography or no mammography.
During 25 years of follow-up, 3,250 women in the mammography group and 3,133 in the control group were diagnosed with breast cancer, and 500 and 505, respectively, died of breast cancer. No difference in mortality rate was found between the mammography and control groups (hazard ratio 0.99, 95% confidence interval 0.88–1.12), and the findings in both age cohorts were similar.4
Criticisms of this study include that it was performed using outdated imaging technology, and that a significant proportion of the control group also received mammography, although it is also possible that the mortality benefit from mammographic screening alone may not be as high as once predicted.
Reduction in breast cancer mortality is likely from a combination of screening mammography and better treatment. The number of women presenting with late-stage cancers has decreased in the past 3 decades, but only slightly; and most of the decrease has been in regional, node-positive disease, a stage that can now often be treated successfully (the expected 5-year survival rate is 85% in women age 40 or older).5 For women with estrogen receptor-positive tumors, the combination of hormonal therapy and adjuvant chemotherapy has reduced the death rate by half.6
It has been 50 years since a large randomized controlled trial of mammographic screening has been done in the United States. Thus, further study is needed to understand whether screening is less valuable now that better treatments are available.
DOES MAMMOGRAPHIC SCREENING REDUCE LATE-STAGE CANCERS?
To be effective, screening must detect disease at an earlier, more curable stage. Although screening mammography has substantially increased the number of early-stage breast cancers detected, it has only marginally decreased the rate of diagnosis of late-stage cancers.5
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) data5 show that between 1976 and 2008 screening mammography was associated with a doubling in early-stage breast cancer cases detected (from 112 to 234 cases per 100,000 women per year, an absolute increase of 122 cases per 100,000 per year). In contrast, late-stage cancer diagnoses decreased by 8% (from 102 to 94 cases per 100,000 women per year, or an absolute decrease of 8 per 100,000 women per year). Assuming a constant underlying disease burden, only 8 of the 122 early-stage cancers diagnosed would be expected to progress to advanced disease, suggesting that the rest would have never harmed these women—ie, they were overdiagnosed. The authors estimated that in 2008, breast cancer was overdiagnosed in more than 70,000 women, accounting for 31% of all diagnosed breast cancers.5
HARMS OF OVERDIAGNOSIS
Based on SEER data, Bleyer and Welch5 estimated that more than 1 million US women may have been overdiagnosed with breast cancer in the past 3 decades. Many women in this situation subsequently undergo surgery, radiation therapy, hormonal therapy, chemotherapy, or a combination of these for a cancer that may never become clinically significant. Until we can differentiate deadly from indolent cancers, highly sensitive screening tests will increase the risk of overtreatment.
Breast cancer has increased in incidence since the 1990s, mostly from the detection of more early-stage cancer or ductal carcinoma in situ (DCIS). Rare before widespread screening, DCIS now accounts for 20% to 30% of all breast cancer diagnoses.6,7 However, DCIS is not always a precursor to invasive cancer: untreated, it progresses to invasive disease in half of cases or fewer. Because DCIS is usually diagnosed only with mammography, its incidence has been steadily on the rise since screening became widespread.1
Welch and Passow6 reviewed the available evidence and attempted to provide a range of estimates for three outcomes important to the mammography decision: breast cancer deaths avoided, false alarms, and overdiagnosis. For every 1,000 US women screened yearly for a decade starting at age 50, an estimated 0.3 to 3.2 avoided breast cancer death, 490 to 670 had at least one false alarm, and 3 to 14 were overdiagnosed and treated needlessly.
Esserman et al7 calculated that in women age 50 to 70, prevention of one breast cancer death would require that 838 women be screened for 6 years, leading to 5,866 screening visits, 535 recalls, 90 biopsies, and 24 cancers treated (18 invasive, 6 DCIS).
SCREENING EVERY YEAR VS EVERY 2 YEARS
Also controversial is whether screening mammography should be done annually or every 2 years. For women in their 50s, the American Cancer Society recommends mammography every year, the American College of Physicians and American Academy of Family Physicians recommend it every 1 to 2 years, and the USPSTF recommends it every 2 years.
A prospective analysis of 11,474 women with breast cancer and 922,624 controls8 found that performing mammography every 2 years instead of annually for women age 50 to 74 did not increase the risk of advanced-stage or large-size tumors regardless of breast density or hormone therapy use. But women undergoing annual mammography had a higher risk of false-positive results and biopsy recommendations.8 Women age 40 to 49 with extremely dense breasts were the only subgroup who derived additional benefit from annual screening, as they had a higher risk of advanced-stage cancer if they were screened every 2 years instead of yearly (odds ratio [OR] 1.89; 95% CI 1.06–3.39) and a higher risk of larger tumors (OR 2.39; 95% CI 1.37–4.18). However, the probability of a false-positive result in these younger women undergoing annual mammography was also very high at 65.5%.8
For most women in their 40s (other than those with extremely dense breasts) and 50s, biennial and annual mammography were associated with a similar risk of advanced-stage disease. Women with fatty breasts are at low risk of breast cancer regardless of other risk factors and did not appear to benefit from annual screening.8 The 12% to 15% of women in their 40s with extremely dense breasts (whose risk of breast cancer is similar to that in average-risk women in their 50s) should decide if the added benefit of annual screening is outweighed by the additional harms, including doubling the number of mammograms, as well as more false-positive results and breast biopsy recommendations.8
Mandelblatt et al9 statistically evaluated 20 screening strategies, ie, screening every year or every 2 years, and starting and stopping at various ages. On average, screening every 2 years was 81% as beneficial as annual screening but caused only about half as many false-positive results. Women age 50 through 69 who were screened every 2 years achieved a median 16.5% (range 15%–23%) reduction in breast cancer deaths compared with no screening. Initiating screening every 2 years at age 40 reduced the death rate by an additional 3% (range 1%–6%) compared with starting at age 50. Not surprisingly, starting screening at age 40 consumed more resources and yielded more false-positive results. After age 69, screening every 2 years yielded some additional mortality reduction in all models, but overdiagnosis increased most substantially at older ages, as the ratio of slow- to fast-growing tumors increases with age. The authors concluded that screening every 2 years achieves most of the benefit of annual screening with less harm.
FALSE-POSITIVE RESULTS AND ANXIETY
False-positive results on mammography can increase distress and anxiety about breast cancer and perceived breast cancer risk in some women.3 After 10 years of annual screening, more than half of women receive at least one false-positive recall, and 7% to 9% receive a false-positive biopsy recommendation. It is helpful for women to understand this risk when deciding whether to start mammographic screening.10
OUR VIEWS
There are two major issues to address in clinical practice regarding mammographic screening: at what age to start, and how often to screen. For years, women have been instructed to start annual mammographic screening at age 40, and such established patterns can be difficult to change.
When deciding whether to have a mammogram at age 40, women should be aware of the full range of risks and benefits. Assessing a woman’s individual risk of breast cancer (based on family history and number and age of pregnancies) can be an important starting point for assessing the potential benefits and risks of screening.
Although a shared decision-making approach is intuitively appealing, it takes much more time than simply ordering a mammogram. Time constraints during a medical appointment may make it challenging to have a prolonged discussion about the pros and cons of screening. Patient education materials about the risks vs benefits of screening initiation may be useful, and because the decision does not usually need to be made urgently, women can be given the opportunity to consider the decision outside of the primary care appointment.
The issue of annual vs biennial screening presents an additional challenge, because women have come to expect annual screening. Studies show that the only subgroup of women who appear to benefit from annual screening are those in their 40s with dense breasts. Although breast cancer is rarer in younger women, when it does develop, it is often more aggressive, so offering annual screening to this subpopulation may make sense. For all other women, since there is no evidence that annual mammography offers clinical benefit over biennial screening, clinicians can be comfortable with offering screening every 2 years.
Future research must focus on developing better tools for differentiating women who are at higher vs lower risk for breast cancer and on developing methods to determine which DCIS cancers are more likely to be indolent and therefore amenable to watchful waiting.
In the interim, we must continue to identify women at high risk who will benefit from magnetic resonance imaging, genetic testing, and prophylactic medications, in accordance with USPSTF recommendations. Women with new breast symptoms or concerns should continue to undergo evaluation with diagnostic imaging, including mammography. However, for most women who are at average risk and have no symptoms, we must ensure that they are fully aware of the possible benefits and risks of screening mammography so that they can make an informed decision about when to start screening and how often to be screened.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726.
- Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014; 311:1327–1335.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L; US Preventive Services Task Force. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med 2009; 151:727–737.
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014; 348:g366.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 2012; 367:1998–2005.
- Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med 2014; 174:448–454.
- Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA 2009; 302:1685–1692.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med 2013; 173:807–816.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 2009; 151:738–747.
- Hubbard RA, Kerlikowske K, Flowers CI, Yankaskas BC, Zhu W, Miglioretti DL. Cumulative probability of false-positive recall or biopsy recommendation after 10 years of screening mammography: a cohort study. Ann Intern Med 2011; 155:481–492.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726.
- Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014; 311:1327–1335.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L; US Preventive Services Task Force. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med 2009; 151:727–737.
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014; 348:g366.
- Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 2012; 367:1998–2005.
- Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med 2014; 174:448–454.
- Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA 2009; 302:1685–1692.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med 2013; 173:807–816.
- Mandelblatt JS, Cronin KA, Bailey S, et al; Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 2009; 151:738–747.
- Hubbard RA, Kerlikowske K, Flowers CI, Yankaskas BC, Zhu W, Miglioretti DL. Cumulative probability of false-positive recall or biopsy recommendation after 10 years of screening mammography: a cohort study. Ann Intern Med 2011; 155:481–492.
In reply: Emergency contraception
In Reply: I thank Drs. Kahlenborn and Severs for their comments. Controversy surrounds emergency contraception; thus, it is important to use peer-reviewed, current medical literature to reference mechanism of action. The product label is an unreliable resource, as it was written before current studies that clarified how emergency contraception works. The Noé study concluded that “levonorgestrel emergency contraception does not prevent embryo implantation and therefore cannot be labeled as abortifacient.”1 They monitored ovulation via ultrasonography and hormonal assays, so they knew in which women ovulation had occurred when emergency contraception was taken. Of those who took it before ovulation, 16 pregnancies were expected and none occurred. When it was taken the day of ovulation or after, 8.7 pregnancies were expected and 8 pregnancies occurred. Because emergency contraception was ineffective after ovulation, a postfertilization effect is unlikely.
Although Drs. Kahlenborn and Severs cited 2004 Croxatto data, they did not cite the 2007 study by Novikova et al,2 which concluded that levonorgestrel emergency contraception “has little or no effect on post-ovulation events, but is highly effective when taken before ovulation.”2 In this study, when levonorgestrel emergency contraception was taken pre-ovulation, 0 out of 4 expected pregnancies occurred. When it was taken post-ovulation, 3 out of the 3 to 4 expected pregnancies occurred.2
The Frequently Asked Question 114 that Drs. Kahlenborn and Severs cited from the American Congress of Obstetricians and Gynecologists was updated in August 2011 and no longer cites prevention of implantation as a potential mechanism of action. Instead, it reads, “Progestin-only pills are thought to prevent pregnancy mainly by preventing ovulation.” 3 Another ACOG committee opinion, from November 2012, states, “A common misconception is that emergency contraception causes an abortion. Inhibition or delay of ovulation is the principal mechanism of action. Review of evidence suggests that emergency contraception cannot prevent implantation of a fertilized egg. Emergency contraception is not effective after implantation; therefore, it is not an abortifacient.”4
The International Federation of Gynecology & Obstetrics and the International Consortium for Emergency Contraception have issued a joint statement on emergency contraception, including mechanism of action.5 This is a good resource for providers and patients. We owe our patients an honest discussion about the current science, from current references and guidelines, so they can make educated decisions based on their own comfort level with emergency contraception.
- Noé G, Croxatto HB, Salvatierra AM, et al. Contraceptive efficacy of emergency contraception with levonorgestrel given before or after ovulation. Contraception 2011; 84:486–492.
- Novikova N, Weisberg E, Stanczyk FZ, Croxatto HB, Fraser IS. Effectiveness of levonorgestrel emergency contraception given before or after ovulation—a pilot study. Contraception 2007; 75:112–118.
- ACOG Frequently Asked Questions #114, Emergency Contraception. http://www.acog.org/~/media/For%20Patients/faq114.pdf?dmc=1&ts=20121127T1830130312. Accessed January 6, 2013.
- ACOG Committee Opinion. Access to Emergency Contraception. Number 542, November 2012. www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Health_Care_for_Underserved_Women/Access_to_Emergency_Contraception. Accessed January 10, 2013.
- International Federation of Gynecology and Obstetrics (FIGO) and International Consortium for Emergency Contraception (ICEC). Emergency Contraception Statement, March 2011. http://www.emergencycontraception.org/publications/PDFs/policy/MOA_ENG_2011.pdf. Accessed January 10, 2013.
In Reply: I thank Drs. Kahlenborn and Severs for their comments. Controversy surrounds emergency contraception; thus, it is important to use peer-reviewed, current medical literature to reference mechanism of action. The product label is an unreliable resource, as it was written before current studies that clarified how emergency contraception works. The Noé study concluded that “levonorgestrel emergency contraception does not prevent embryo implantation and therefore cannot be labeled as abortifacient.”1 They monitored ovulation via ultrasonography and hormonal assays, so they knew in which women ovulation had occurred when emergency contraception was taken. Of those who took it before ovulation, 16 pregnancies were expected and none occurred. When it was taken the day of ovulation or after, 8.7 pregnancies were expected and 8 pregnancies occurred. Because emergency contraception was ineffective after ovulation, a postfertilization effect is unlikely.
Although Drs. Kahlenborn and Severs cited 2004 Croxatto data, they did not cite the 2007 study by Novikova et al,2 which concluded that levonorgestrel emergency contraception “has little or no effect on post-ovulation events, but is highly effective when taken before ovulation.”2 In this study, when levonorgestrel emergency contraception was taken pre-ovulation, 0 out of 4 expected pregnancies occurred. When it was taken post-ovulation, 3 out of the 3 to 4 expected pregnancies occurred.2
The Frequently Asked Question 114 that Drs. Kahlenborn and Severs cited from the American Congress of Obstetricians and Gynecologists was updated in August 2011 and no longer cites prevention of implantation as a potential mechanism of action. Instead, it reads, “Progestin-only pills are thought to prevent pregnancy mainly by preventing ovulation.” 3 Another ACOG committee opinion, from November 2012, states, “A common misconception is that emergency contraception causes an abortion. Inhibition or delay of ovulation is the principal mechanism of action. Review of evidence suggests that emergency contraception cannot prevent implantation of a fertilized egg. Emergency contraception is not effective after implantation; therefore, it is not an abortifacient.”4
The International Federation of Gynecology & Obstetrics and the International Consortium for Emergency Contraception have issued a joint statement on emergency contraception, including mechanism of action.5 This is a good resource for providers and patients. We owe our patients an honest discussion about the current science, from current references and guidelines, so they can make educated decisions based on their own comfort level with emergency contraception.
In Reply: I thank Drs. Kahlenborn and Severs for their comments. Controversy surrounds emergency contraception; thus, it is important to use peer-reviewed, current medical literature to reference mechanism of action. The product label is an unreliable resource, as it was written before current studies that clarified how emergency contraception works. The Noé study concluded that “levonorgestrel emergency contraception does not prevent embryo implantation and therefore cannot be labeled as abortifacient.”1 They monitored ovulation via ultrasonography and hormonal assays, so they knew in which women ovulation had occurred when emergency contraception was taken. Of those who took it before ovulation, 16 pregnancies were expected and none occurred. When it was taken the day of ovulation or after, 8.7 pregnancies were expected and 8 pregnancies occurred. Because emergency contraception was ineffective after ovulation, a postfertilization effect is unlikely.
Although Drs. Kahlenborn and Severs cited 2004 Croxatto data, they did not cite the 2007 study by Novikova et al,2 which concluded that levonorgestrel emergency contraception “has little or no effect on post-ovulation events, but is highly effective when taken before ovulation.”2 In this study, when levonorgestrel emergency contraception was taken pre-ovulation, 0 out of 4 expected pregnancies occurred. When it was taken post-ovulation, 3 out of the 3 to 4 expected pregnancies occurred.2
The Frequently Asked Question 114 that Drs. Kahlenborn and Severs cited from the American Congress of Obstetricians and Gynecologists was updated in August 2011 and no longer cites prevention of implantation as a potential mechanism of action. Instead, it reads, “Progestin-only pills are thought to prevent pregnancy mainly by preventing ovulation.” 3 Another ACOG committee opinion, from November 2012, states, “A common misconception is that emergency contraception causes an abortion. Inhibition or delay of ovulation is the principal mechanism of action. Review of evidence suggests that emergency contraception cannot prevent implantation of a fertilized egg. Emergency contraception is not effective after implantation; therefore, it is not an abortifacient.”4
The International Federation of Gynecology & Obstetrics and the International Consortium for Emergency Contraception have issued a joint statement on emergency contraception, including mechanism of action.5 This is a good resource for providers and patients. We owe our patients an honest discussion about the current science, from current references and guidelines, so they can make educated decisions based on their own comfort level with emergency contraception.
- Noé G, Croxatto HB, Salvatierra AM, et al. Contraceptive efficacy of emergency contraception with levonorgestrel given before or after ovulation. Contraception 2011; 84:486–492.
- Novikova N, Weisberg E, Stanczyk FZ, Croxatto HB, Fraser IS. Effectiveness of levonorgestrel emergency contraception given before or after ovulation—a pilot study. Contraception 2007; 75:112–118.
- ACOG Frequently Asked Questions #114, Emergency Contraception. http://www.acog.org/~/media/For%20Patients/faq114.pdf?dmc=1&ts=20121127T1830130312. Accessed January 6, 2013.
- ACOG Committee Opinion. Access to Emergency Contraception. Number 542, November 2012. www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Health_Care_for_Underserved_Women/Access_to_Emergency_Contraception. Accessed January 10, 2013.
- International Federation of Gynecology and Obstetrics (FIGO) and International Consortium for Emergency Contraception (ICEC). Emergency Contraception Statement, March 2011. http://www.emergencycontraception.org/publications/PDFs/policy/MOA_ENG_2011.pdf. Accessed January 10, 2013.
- Noé G, Croxatto HB, Salvatierra AM, et al. Contraceptive efficacy of emergency contraception with levonorgestrel given before or after ovulation. Contraception 2011; 84:486–492.
- Novikova N, Weisberg E, Stanczyk FZ, Croxatto HB, Fraser IS. Effectiveness of levonorgestrel emergency contraception given before or after ovulation—a pilot study. Contraception 2007; 75:112–118.
- ACOG Frequently Asked Questions #114, Emergency Contraception. http://www.acog.org/~/media/For%20Patients/faq114.pdf?dmc=1&ts=20121127T1830130312. Accessed January 6, 2013.
- ACOG Committee Opinion. Access to Emergency Contraception. Number 542, November 2012. www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Health_Care_for_Underserved_Women/Access_to_Emergency_Contraception. Accessed January 10, 2013.
- International Federation of Gynecology and Obstetrics (FIGO) and International Consortium for Emergency Contraception (ICEC). Emergency Contraception Statement, March 2011. http://www.emergencycontraception.org/publications/PDFs/policy/MOA_ENG_2011.pdf. Accessed January 10, 2013.
Emergency contraception: Separating fact from fiction
In the United States, nearly 50 million legal abortions were performed between 1973 and 2008.1 About half of pregnancies in American women are unintended, and 4 out of 10 unintended pregnancies are terminated by abortion.2 Of the women who had abortions, 54% had used a contraceptive method during the month they became pregnant.3
It is hoped that the expanded use of emergency contraception will translate into fewer abortions. However, in a 2006–2008 survey conducted by the US Centers for Disease Control and Prevention, only 9.7% of women ages 15 to 44 reported ever having used emergency contraception.4 (To put this figure in perspective, a similar number—about 10%—of women in this age group become pregnant in any given year, half of them unintentionally.4) Clearly, patients need to be better educated in the methods of contraception and emergency contraception.
Hospitals are not meeting the need. Pretending to be in need of emergency contraception, Harrison5 called the emergency departments of all 597 Catholic hospitals in the United States and 615 (17%) of the non-Catholic hospitals. About half of the staff she spoke to said they do not dispense emergency contraception, even in cases of sexual assault. This was the case for both Catholic and non-Catholic hospitals. Of the people she talked to who said they did not provide emergency contraception under any circumstance, only about half gave her a phone number for another facility to try, and most of these phone numbers were wrong, were for facilities that were not open on weekends, or were for facilities that did not offer emergency contraception either. This is in spite of legal precedent, which indicates that failure to provide complete post-rape counseling, including emergency contraception, constitutes inadequate care and gives a woman the standing to sue the hospital.6
Clearly, better provider education is also needed in the area of emergency contraception. The Association of Reproductive Health Professionals has a helpful Web site for providers and for patients. In addition to up-to-date information about contraceptive and emergency contraceptive choices, it provides advice on how to discuss emergency contraception with patients (www.arhp.org). We can test our own knowledge of this topic by reviewing the following questions.
WHICH PRODUCT IS MOST EFFECTIVE?
Q: True or false? Levonorgestrel monotherapy (Plan B One-Step, Next Choice) is the most effective oral emergency contraceptive.
A: False, although this statement was true before the US approval of ulipristal acetate (ella) in August 2010.
For many years levonorgestrel monotherapy has been the mainstay of emergency contraception, having replaced the combination estrogen-progestin (Yuzpe) regimen because of better tolerability and improved efficacy.7 Its main mechanism of action involves delaying ovulation. Levonorgestrel is given in two doses of 0.75 mg 12 hours apart, or as a single 1.5-mg dose (Table 1). Both formulations of levonorgestrel are available over the counter to women age 17 and older, or by prescription if they are under age 17.
However, a randomized controlled trial showed that women treated with ulipristal had about half the number of pregnancies than in those treated with levonorgestrel, with pregnancy rates of 0.9% vs 1.7%.8
HOW WIDE IS THE WINDOW OF OPPORTUNITY?
Q: True or false? Both ulipristal and levonorgestrel can be taken up to 120 hours (5 days) after unprotected intercourse. However, ulipristal maintains its effectiveness throughout this time, whereas levonorgestrel becomes less effective the longer a patient waits to take it.
A: True. Ulipristal is a second-generation selective progesterone receptor modulator. These drugs can function as agonists, antagonists, or mixed agonist-antagonists at the progesterone receptor, depending on the tissue affected. Ulipristal is given as a one-time, 30-mg dose within 120 hours of intercourse.
In a study of 1,696 women, 844 of whom received ulipristal acetate and 852 of whom received levonorgestrel, ulipristal was at least as effective as levonorgestrel when used within 72 hours of intercourse for emergency contraception, with 15 pregnancies in the ulipristal group and 22 pregnancies in the levonorgestrel group (odds ratio [OR] 0.68, 95% confidence interval [CI] 0.35–1.31]). However, ulipristal prevented significantly more pregnancies than levonorgestrel at 72 to 120 hours, with no pregnancies in the ulipristal group and three pregnancies in the levonorgestrel group.9
Because ulipristal has a long half-life (32 hours), it can delay ovulation beyond the life span of sperm, thereby extending the window of opportunity for emergency contraception. However, patients should be advised to avoid further unprotected intercourse after the use of emergency contraception. Because emergency contraception works mainly by delaying ovulation, it may increase the likelihood of pregnancy if the patient has unprotected intercourse again several days later.
IS MIFEPRISTONE AN EMERGENCY CONTRACEPTIVE?
Q: True or false? In the United States, mifepristone (Mifeprex), also known as RU-486, is available for use as an emergency contraceptive in addition to its use in abortion.
A: False, even though mifepristone, another selective progesterone receptor modulator, is highly effective when used up to 120 hours after intercourse. In fact, it might be effective up to 17 days after unprotected intercourse.10
Although mifepristone is one of the most effective forms of emergency contraception, social and political controversy has prevented its approval in the United States. However, it is approved for use as an abortifacient, at a higher dose than would be used for emergency contraception.
Unlike levonorgestrel, mifepristone exerts its effect via two potential mechanisms: delaying ovulation and preventing implantation.11
IUDs AS EMERGENCY CONTRACEPTION
Q: True or false? Insertion of a 5-year intrauterine device (IUD), ie, the levonorgestrel-releasing intrauterine system (Mirena), is 99.8% effective at preventing pregnancy when used within 5 days of unprotected intercourse.
A: False. The Mirena IUD has not been studied as a form of emergency contraception. However, this statement would be true for the 10-year copper IUD ParaGard. Copper-releasing IUDs are considered a very effective method of emergency contraception, with associated pregnancy rates of 0.0% to 0.2% when inserted up until implantation (within 5 days after ovulation).12,13 If desired, the IUD can then be kept in place for up to 10 years as a method of birth control.
However, this method requires the ready availability of a health professional trained to do the insertion. It is also important to make sure that the patient will not be at increased risk of sexually transmitted infections from further unprotected intercourse. The American Congress of Obstetricians and Gynecologists (ACOG) recommends that an IUD be placed within 5 days of unprotected intercourse for use as emergency contraception.
A recent review looked at 42 published studies of copper IUDs used for emergency contraception around the world. It found copper IUDs to be a safe and highly effective method of emergency contraception, with the additional advantage of simultaneously offering one of the most reliable and cost-effective contraceptive options.14
EMERGENCY CONTRACEPTION AT MID-CYCLE
Q: True or false? When choosing a method of emergency contraception, it is important to consider whether a woman is near ovulation during the time of intercourse.
A: True. Emergency contraception can prevent pregnancy after unprotected intercourse, but it does not always work. The most widely used method, levonorgestrel 1.5 mg orally within 72 hours of intercourse, prevents at least 50% of pregnancies that would have occurred in the absence of its use.15 Glasier et al16 showed that emergency contraception was more likely to fail if a woman had unprotected intercourse around the time of ovulation.16
Though it can be difficult for women to tell if they are in the fertile times of their cycle, it might be helpful to try to identify women who have intercourse at mid-cycle, when the risk of pregnancy is greatest. Because insertion of an IUD and use of ulipristal acetate probably prevent more pregnancies, these methods might be preferred over levonorgestrel-based regimens during these higher-risk situations.
OBESE PATIENTS
Q: True or false? Hormonal emergency contraception is more likely to fail in obese patients.
A: True. Most recent evidence shows that whichever oral emergency contraceptive drug is taken, the risk of pregnancy is more than 3 times greater for obese women (OR 3.60, 95% CI 1.96–6.53) and 1.5 times greater for overweight women (OR 1.53, 95% CI 0.75–2.95).16 Of all covariates tested, those that were shown to increase the odds of failure of the emergency contraception were higher body mass index, further unprotected intercourse, and conception probability (based on time of fertility cycle). In fact, among obese women treated with levonorgestrel, the observed pregnancy rate was 5.8%, which is slightly above the overall pregnancy rate expected in the absence of emergency contraception, suggesting that for obese women levonorgestrel-based emergency contraception may even be ineffective.
This is in line with recent reports suggesting that oral contraceptives are less effective in obese women. More effective regimens such as an IUD or ulipristal might be preferred in these women. However, obesity should not be used as a reason not to offer emergency contraception, as this is the last chance these women have to prevent pregnancy.
IS IT ABORTION?
Q: True or false? Emergency contraception does not cause abortion.
A: True, but patients may ask for more details about this. Hormonal emergency contraception works primarily by delaying or inhibiting ovulation and inhibiting fertilization.
Levonorgestrel or combined estrogen-progestin-based methods would be unlikely to have any adverse effects on the endometrium after fertilization, since they would only serve to enhance the progesterone effect. Therefore, they are unlikely to affect the ability of the embryo to attach to the endometrium.
Ulipristal, on the other hand, can have just the opposite effect on the postovulatory endometrium because of its inhibitory action on progesterone. Ulipristal is structurally similar to mifepristone, and its mechanism of action varies depending on the time of administration during the menstrual cycle. When unprotected intercourse occurs during a time when fertility is not possible, ulipristal behaves like a placebo. When intercourse occurs just before ovulation, ulipristal acts by delaying ovulation and thereby preventing fertilization (similar to levonorgestrel). Ulipristal may have an additional action of affecting the ability of the embryo to either attach to the endometrium or maintain its attachment, by a variety of mechanisms of action.17,18 Because of this, some in the popular press and on the Internet have spoken out against the use of ulipristal.
The ACOG considers pregnancy to begin not with fertilization of the egg but with implantation, as demonstrated by a positive pregnancy test.
Of note, the copper IUD also prevents implantation after fertilization, which likely explains its high efficacy.
Women who have detailed questions about this can be counseled that levonorgestrel works mostly by preventing ovulation, and that ulipristal and the copper IUD might also work via postfertilization mechanisms. However, they are not considered to be abortive, based on standard definitions of pregnancy.
If a woman is pregnant and she takes levonorgestrel-based emergency contraception, this has not been shown to have any adverse effects on the fetus (similar to oral contraceptives).
Ulipristal is classified as pregnancy category X, and therefore its use during pregnancy is contraindicated. Based on information provided by the manufacturer, there are no adequate, well-controlled studies of ulipristal use in pregnant women. Although fetal loss was observed in animal studies after ulipristal administration (during the period of organogenesis), no malformations or adverse events were present in the surviving fetuses. Ulipristal is not indicated for termination of an existing pregnancy.
DO THE USUAL CONTRAINDICATIONS TO HORMONAL CONTRACEPTIVES APPLY?
Q: True or false? Because emergency contraception has such a short duration of exposure, the usual medical contraindications to hormonal therapies do not apply to it.
A: True. The usual contraindications to the use of hormonal contraceptives (eg, migraine with aura, hypertension, history of venous thromboembolism) do not apply to emergency contraception because of the short time of exposure.19 Furthermore, the risks associated with pregnancy in these women would likely outweigh any risks associated with emergency contraception.
However, one must be cognizant of potential drug interactions. According to the manufacturer, the use of ulipristal did not inhibit or induce cytochrome P 450 enzymes in vitro; therefore, in vivo studies were not performed. But because ulipristal is metabolized primarily via CYP3A4, an interaction between agents that induce or inhibit CYP3A4 could occur.20 Thus, concomitant use of drugs such as barbiturates, rifampin (Rifadin), St. John’s wort, or antiseizure drugs such as topiramate (Topamax) may lower ulipristal concentrations. These medications may also affect levonorgestrel levels, similar to their effects on combined hormonal contraception. However, it is not known whether this translates to decreased efficacy.
When a woman is taking medications that can potentially decrease the effectiveness of hormonal emergency contraception, a more effective method such as a copper IUD might be more strongly considered. If a woman is not interested in an IUD, oral emergency contraception should still be offered, given that this is one of the last chances to prevent pregnancy, especially if she is on a potential teratogen.
Oral contraceptive pills have not been studied in combination with ulipristal. However, because ulipristal binds with high affinity to progesterone receptors (thus competing with the contraceptive), use of additional barrier contraceptives is recommended for the remainder of the menstrual cycle.
EMERGENCY CONTRACEPTION AND BREASTFEEDING
Q: True of false? Emergency contraceptives can be used if a woman is breastfeeding.
A: That depends on which method is used. Both the ACOG and the World Health Organization state that it is safe for breastfeeding women to use emergency contraception, but these are older guidelines addressing progestin-only regimens (ie, levonorgestrel).19,21 It is unknown whether ulipristal is secreted into human breast milk, although excretion was seen in animal studies. Therefore, ulipristal is not recommended for use by women who are breastfeeding.20,22 To minimize the infant’s exposure to levonorgestrel, mothers should consider not nursing for at least 8 hours after ingestion, but no more than 24 hours is needed.23
- Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health 2011; 43:41–50.
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011; 84:478–485.
- Jones RK, Darroch JE, Henshaw SK. Contraceptive use among US women having abortions in 2000–2001. Perspect Sex Reprod Health 2002; 34:294–303.
- Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. National Center for Health Statistics. Vital Health Stat 2010; 23. http://www.cdc.gov/NCHS/data/series/sr_23/sr23_029.pdf. Accessed October 1, 2012.
- Harrison T. Availability of emergency contraception: a survey of hospital emergency department staff. Ann Emerg Med 2005; 46:105–110.
- Goldenring JM, Allred G. Post-rape care in hospital emergency rooms. Am J Public Health 2001; 91:1169–1170.
- Randomised controlled trial of levonorgestrel versus the Yuzpe regimen of combined oral contraceptives for emergency contraception. Task Force on Postovulatory Methods of Fertility Regulation. Lancet 1998; 352:428–433.
- Creinin MD, Schlaff W, Archer DF, et al. Progesterone receptor modulator for emergency contraception: a randomized controlled trial. Obstet Gynecol 2006; 108:1089–1097.
- Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet 2010; 375:555–562.
- Glasier A, Thong KJ, Dewar M, Mackie M, Baird DT. Mifepristone (RU 486) compared with high-dose estrogen and progestogen for emergency postcoital contraception. N Engl J Med 1992; 327:1041–1044.
- Glasier A. Emergency postcoital contraception. N Engl J Med 1997; 337:1058–1064.
- Stanford JB, Mikolajczyk RT. Mechanisms of action of intrauterine devices: update and estimation of postfertilization effects. Am J Obstet Gynecol 2002; 187:1699–1708.
- Zhou L, Xiao B. Emergency contraception with Multiload Cu-375 SL IUD: a multicenter clinical trial. Contraception 2001; 64:107–112.
- Cleland K, Zhu H, Goldstuck N, Cheng L, Trussell J. The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod 2012; 27:1994–2000.
- Trussell J, Ellertson C, von Hertzen H, et al. Estimating the effectiveness of emergency contraceptive pills. Contraception 2003; 67:259–265.
- Glasier A, Cameron ST, Blithe D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel. Contraception 2011; 84:363–367.
- Miech RP. Immunopharmacology of ulipristal as an emergency contraceptive. Int J Womens Health 2011; 3:391–397.
- Keenan JA. Ulipristal acetate: contraceptive or contragestive? Ann Pharmacother 2011; 45:813–815.
- Medical eligibility criteria for contraceptive use. 3rd ed. Geneva: Reproductive Health and Research, World Health Organization; 2004.
- Ella package insert. Morristown, NJ: Watson Pharmaceuticals; August 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022474s000lbl.pdf. Accessed July 6, 2012.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 112: emergency contraception. Obstet Gynecol 2010; 115:1100–1109.
- Orleans RJ. Clinical review. NDA22-474. Ella (ulipristal acetate 30 mg). US Food and Drug Administration, July 27, 2010. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/UCM295393.pdf. Accessed October 1, 2012.
- Gainer E, Massai R, Lillo S, et al. Levonorgestrel pharmacokinetics in plasma and milk of lactating women who take 1.5 mg for emergency contraception. Hum Reprod 2007; 22:1578–1584.
In the United States, nearly 50 million legal abortions were performed between 1973 and 2008.1 About half of pregnancies in American women are unintended, and 4 out of 10 unintended pregnancies are terminated by abortion.2 Of the women who had abortions, 54% had used a contraceptive method during the month they became pregnant.3
It is hoped that the expanded use of emergency contraception will translate into fewer abortions. However, in a 2006–2008 survey conducted by the US Centers for Disease Control and Prevention, only 9.7% of women ages 15 to 44 reported ever having used emergency contraception.4 (To put this figure in perspective, a similar number—about 10%—of women in this age group become pregnant in any given year, half of them unintentionally.4) Clearly, patients need to be better educated in the methods of contraception and emergency contraception.
Hospitals are not meeting the need. Pretending to be in need of emergency contraception, Harrison5 called the emergency departments of all 597 Catholic hospitals in the United States and 615 (17%) of the non-Catholic hospitals. About half of the staff she spoke to said they do not dispense emergency contraception, even in cases of sexual assault. This was the case for both Catholic and non-Catholic hospitals. Of the people she talked to who said they did not provide emergency contraception under any circumstance, only about half gave her a phone number for another facility to try, and most of these phone numbers were wrong, were for facilities that were not open on weekends, or were for facilities that did not offer emergency contraception either. This is in spite of legal precedent, which indicates that failure to provide complete post-rape counseling, including emergency contraception, constitutes inadequate care and gives a woman the standing to sue the hospital.6
Clearly, better provider education is also needed in the area of emergency contraception. The Association of Reproductive Health Professionals has a helpful Web site for providers and for patients. In addition to up-to-date information about contraceptive and emergency contraceptive choices, it provides advice on how to discuss emergency contraception with patients (www.arhp.org). We can test our own knowledge of this topic by reviewing the following questions.
WHICH PRODUCT IS MOST EFFECTIVE?
Q: True or false? Levonorgestrel monotherapy (Plan B One-Step, Next Choice) is the most effective oral emergency contraceptive.
A: False, although this statement was true before the US approval of ulipristal acetate (ella) in August 2010.
For many years levonorgestrel monotherapy has been the mainstay of emergency contraception, having replaced the combination estrogen-progestin (Yuzpe) regimen because of better tolerability and improved efficacy.7 Its main mechanism of action involves delaying ovulation. Levonorgestrel is given in two doses of 0.75 mg 12 hours apart, or as a single 1.5-mg dose (Table 1). Both formulations of levonorgestrel are available over the counter to women age 17 and older, or by prescription if they are under age 17.
However, a randomized controlled trial showed that women treated with ulipristal had about half the number of pregnancies than in those treated with levonorgestrel, with pregnancy rates of 0.9% vs 1.7%.8
HOW WIDE IS THE WINDOW OF OPPORTUNITY?
Q: True or false? Both ulipristal and levonorgestrel can be taken up to 120 hours (5 days) after unprotected intercourse. However, ulipristal maintains its effectiveness throughout this time, whereas levonorgestrel becomes less effective the longer a patient waits to take it.
A: True. Ulipristal is a second-generation selective progesterone receptor modulator. These drugs can function as agonists, antagonists, or mixed agonist-antagonists at the progesterone receptor, depending on the tissue affected. Ulipristal is given as a one-time, 30-mg dose within 120 hours of intercourse.
In a study of 1,696 women, 844 of whom received ulipristal acetate and 852 of whom received levonorgestrel, ulipristal was at least as effective as levonorgestrel when used within 72 hours of intercourse for emergency contraception, with 15 pregnancies in the ulipristal group and 22 pregnancies in the levonorgestrel group (odds ratio [OR] 0.68, 95% confidence interval [CI] 0.35–1.31]). However, ulipristal prevented significantly more pregnancies than levonorgestrel at 72 to 120 hours, with no pregnancies in the ulipristal group and three pregnancies in the levonorgestrel group.9
Because ulipristal has a long half-life (32 hours), it can delay ovulation beyond the life span of sperm, thereby extending the window of opportunity for emergency contraception. However, patients should be advised to avoid further unprotected intercourse after the use of emergency contraception. Because emergency contraception works mainly by delaying ovulation, it may increase the likelihood of pregnancy if the patient has unprotected intercourse again several days later.
IS MIFEPRISTONE AN EMERGENCY CONTRACEPTIVE?
Q: True or false? In the United States, mifepristone (Mifeprex), also known as RU-486, is available for use as an emergency contraceptive in addition to its use in abortion.
A: False, even though mifepristone, another selective progesterone receptor modulator, is highly effective when used up to 120 hours after intercourse. In fact, it might be effective up to 17 days after unprotected intercourse.10
Although mifepristone is one of the most effective forms of emergency contraception, social and political controversy has prevented its approval in the United States. However, it is approved for use as an abortifacient, at a higher dose than would be used for emergency contraception.
Unlike levonorgestrel, mifepristone exerts its effect via two potential mechanisms: delaying ovulation and preventing implantation.11
IUDs AS EMERGENCY CONTRACEPTION
Q: True or false? Insertion of a 5-year intrauterine device (IUD), ie, the levonorgestrel-releasing intrauterine system (Mirena), is 99.8% effective at preventing pregnancy when used within 5 days of unprotected intercourse.
A: False. The Mirena IUD has not been studied as a form of emergency contraception. However, this statement would be true for the 10-year copper IUD ParaGard. Copper-releasing IUDs are considered a very effective method of emergency contraception, with associated pregnancy rates of 0.0% to 0.2% when inserted up until implantation (within 5 days after ovulation).12,13 If desired, the IUD can then be kept in place for up to 10 years as a method of birth control.
However, this method requires the ready availability of a health professional trained to do the insertion. It is also important to make sure that the patient will not be at increased risk of sexually transmitted infections from further unprotected intercourse. The American Congress of Obstetricians and Gynecologists (ACOG) recommends that an IUD be placed within 5 days of unprotected intercourse for use as emergency contraception.
A recent review looked at 42 published studies of copper IUDs used for emergency contraception around the world. It found copper IUDs to be a safe and highly effective method of emergency contraception, with the additional advantage of simultaneously offering one of the most reliable and cost-effective contraceptive options.14
EMERGENCY CONTRACEPTION AT MID-CYCLE
Q: True or false? When choosing a method of emergency contraception, it is important to consider whether a woman is near ovulation during the time of intercourse.
A: True. Emergency contraception can prevent pregnancy after unprotected intercourse, but it does not always work. The most widely used method, levonorgestrel 1.5 mg orally within 72 hours of intercourse, prevents at least 50% of pregnancies that would have occurred in the absence of its use.15 Glasier et al16 showed that emergency contraception was more likely to fail if a woman had unprotected intercourse around the time of ovulation.16
Though it can be difficult for women to tell if they are in the fertile times of their cycle, it might be helpful to try to identify women who have intercourse at mid-cycle, when the risk of pregnancy is greatest. Because insertion of an IUD and use of ulipristal acetate probably prevent more pregnancies, these methods might be preferred over levonorgestrel-based regimens during these higher-risk situations.
OBESE PATIENTS
Q: True or false? Hormonal emergency contraception is more likely to fail in obese patients.
A: True. Most recent evidence shows that whichever oral emergency contraceptive drug is taken, the risk of pregnancy is more than 3 times greater for obese women (OR 3.60, 95% CI 1.96–6.53) and 1.5 times greater for overweight women (OR 1.53, 95% CI 0.75–2.95).16 Of all covariates tested, those that were shown to increase the odds of failure of the emergency contraception were higher body mass index, further unprotected intercourse, and conception probability (based on time of fertility cycle). In fact, among obese women treated with levonorgestrel, the observed pregnancy rate was 5.8%, which is slightly above the overall pregnancy rate expected in the absence of emergency contraception, suggesting that for obese women levonorgestrel-based emergency contraception may even be ineffective.
This is in line with recent reports suggesting that oral contraceptives are less effective in obese women. More effective regimens such as an IUD or ulipristal might be preferred in these women. However, obesity should not be used as a reason not to offer emergency contraception, as this is the last chance these women have to prevent pregnancy.
IS IT ABORTION?
Q: True or false? Emergency contraception does not cause abortion.
A: True, but patients may ask for more details about this. Hormonal emergency contraception works primarily by delaying or inhibiting ovulation and inhibiting fertilization.
Levonorgestrel or combined estrogen-progestin-based methods would be unlikely to have any adverse effects on the endometrium after fertilization, since they would only serve to enhance the progesterone effect. Therefore, they are unlikely to affect the ability of the embryo to attach to the endometrium.
Ulipristal, on the other hand, can have just the opposite effect on the postovulatory endometrium because of its inhibitory action on progesterone. Ulipristal is structurally similar to mifepristone, and its mechanism of action varies depending on the time of administration during the menstrual cycle. When unprotected intercourse occurs during a time when fertility is not possible, ulipristal behaves like a placebo. When intercourse occurs just before ovulation, ulipristal acts by delaying ovulation and thereby preventing fertilization (similar to levonorgestrel). Ulipristal may have an additional action of affecting the ability of the embryo to either attach to the endometrium or maintain its attachment, by a variety of mechanisms of action.17,18 Because of this, some in the popular press and on the Internet have spoken out against the use of ulipristal.
The ACOG considers pregnancy to begin not with fertilization of the egg but with implantation, as demonstrated by a positive pregnancy test.
Of note, the copper IUD also prevents implantation after fertilization, which likely explains its high efficacy.
Women who have detailed questions about this can be counseled that levonorgestrel works mostly by preventing ovulation, and that ulipristal and the copper IUD might also work via postfertilization mechanisms. However, they are not considered to be abortive, based on standard definitions of pregnancy.
If a woman is pregnant and she takes levonorgestrel-based emergency contraception, this has not been shown to have any adverse effects on the fetus (similar to oral contraceptives).
Ulipristal is classified as pregnancy category X, and therefore its use during pregnancy is contraindicated. Based on information provided by the manufacturer, there are no adequate, well-controlled studies of ulipristal use in pregnant women. Although fetal loss was observed in animal studies after ulipristal administration (during the period of organogenesis), no malformations or adverse events were present in the surviving fetuses. Ulipristal is not indicated for termination of an existing pregnancy.
DO THE USUAL CONTRAINDICATIONS TO HORMONAL CONTRACEPTIVES APPLY?
Q: True or false? Because emergency contraception has such a short duration of exposure, the usual medical contraindications to hormonal therapies do not apply to it.
A: True. The usual contraindications to the use of hormonal contraceptives (eg, migraine with aura, hypertension, history of venous thromboembolism) do not apply to emergency contraception because of the short time of exposure.19 Furthermore, the risks associated with pregnancy in these women would likely outweigh any risks associated with emergency contraception.
However, one must be cognizant of potential drug interactions. According to the manufacturer, the use of ulipristal did not inhibit or induce cytochrome P 450 enzymes in vitro; therefore, in vivo studies were not performed. But because ulipristal is metabolized primarily via CYP3A4, an interaction between agents that induce or inhibit CYP3A4 could occur.20 Thus, concomitant use of drugs such as barbiturates, rifampin (Rifadin), St. John’s wort, or antiseizure drugs such as topiramate (Topamax) may lower ulipristal concentrations. These medications may also affect levonorgestrel levels, similar to their effects on combined hormonal contraception. However, it is not known whether this translates to decreased efficacy.
When a woman is taking medications that can potentially decrease the effectiveness of hormonal emergency contraception, a more effective method such as a copper IUD might be more strongly considered. If a woman is not interested in an IUD, oral emergency contraception should still be offered, given that this is one of the last chances to prevent pregnancy, especially if she is on a potential teratogen.
Oral contraceptive pills have not been studied in combination with ulipristal. However, because ulipristal binds with high affinity to progesterone receptors (thus competing with the contraceptive), use of additional barrier contraceptives is recommended for the remainder of the menstrual cycle.
EMERGENCY CONTRACEPTION AND BREASTFEEDING
Q: True of false? Emergency contraceptives can be used if a woman is breastfeeding.
A: That depends on which method is used. Both the ACOG and the World Health Organization state that it is safe for breastfeeding women to use emergency contraception, but these are older guidelines addressing progestin-only regimens (ie, levonorgestrel).19,21 It is unknown whether ulipristal is secreted into human breast milk, although excretion was seen in animal studies. Therefore, ulipristal is not recommended for use by women who are breastfeeding.20,22 To minimize the infant’s exposure to levonorgestrel, mothers should consider not nursing for at least 8 hours after ingestion, but no more than 24 hours is needed.23
In the United States, nearly 50 million legal abortions were performed between 1973 and 2008.1 About half of pregnancies in American women are unintended, and 4 out of 10 unintended pregnancies are terminated by abortion.2 Of the women who had abortions, 54% had used a contraceptive method during the month they became pregnant.3
It is hoped that the expanded use of emergency contraception will translate into fewer abortions. However, in a 2006–2008 survey conducted by the US Centers for Disease Control and Prevention, only 9.7% of women ages 15 to 44 reported ever having used emergency contraception.4 (To put this figure in perspective, a similar number—about 10%—of women in this age group become pregnant in any given year, half of them unintentionally.4) Clearly, patients need to be better educated in the methods of contraception and emergency contraception.
Hospitals are not meeting the need. Pretending to be in need of emergency contraception, Harrison5 called the emergency departments of all 597 Catholic hospitals in the United States and 615 (17%) of the non-Catholic hospitals. About half of the staff she spoke to said they do not dispense emergency contraception, even in cases of sexual assault. This was the case for both Catholic and non-Catholic hospitals. Of the people she talked to who said they did not provide emergency contraception under any circumstance, only about half gave her a phone number for another facility to try, and most of these phone numbers were wrong, were for facilities that were not open on weekends, or were for facilities that did not offer emergency contraception either. This is in spite of legal precedent, which indicates that failure to provide complete post-rape counseling, including emergency contraception, constitutes inadequate care and gives a woman the standing to sue the hospital.6
Clearly, better provider education is also needed in the area of emergency contraception. The Association of Reproductive Health Professionals has a helpful Web site for providers and for patients. In addition to up-to-date information about contraceptive and emergency contraceptive choices, it provides advice on how to discuss emergency contraception with patients (www.arhp.org). We can test our own knowledge of this topic by reviewing the following questions.
WHICH PRODUCT IS MOST EFFECTIVE?
Q: True or false? Levonorgestrel monotherapy (Plan B One-Step, Next Choice) is the most effective oral emergency contraceptive.
A: False, although this statement was true before the US approval of ulipristal acetate (ella) in August 2010.
For many years levonorgestrel monotherapy has been the mainstay of emergency contraception, having replaced the combination estrogen-progestin (Yuzpe) regimen because of better tolerability and improved efficacy.7 Its main mechanism of action involves delaying ovulation. Levonorgestrel is given in two doses of 0.75 mg 12 hours apart, or as a single 1.5-mg dose (Table 1). Both formulations of levonorgestrel are available over the counter to women age 17 and older, or by prescription if they are under age 17.
However, a randomized controlled trial showed that women treated with ulipristal had about half the number of pregnancies than in those treated with levonorgestrel, with pregnancy rates of 0.9% vs 1.7%.8
HOW WIDE IS THE WINDOW OF OPPORTUNITY?
Q: True or false? Both ulipristal and levonorgestrel can be taken up to 120 hours (5 days) after unprotected intercourse. However, ulipristal maintains its effectiveness throughout this time, whereas levonorgestrel becomes less effective the longer a patient waits to take it.
A: True. Ulipristal is a second-generation selective progesterone receptor modulator. These drugs can function as agonists, antagonists, or mixed agonist-antagonists at the progesterone receptor, depending on the tissue affected. Ulipristal is given as a one-time, 30-mg dose within 120 hours of intercourse.
In a study of 1,696 women, 844 of whom received ulipristal acetate and 852 of whom received levonorgestrel, ulipristal was at least as effective as levonorgestrel when used within 72 hours of intercourse for emergency contraception, with 15 pregnancies in the ulipristal group and 22 pregnancies in the levonorgestrel group (odds ratio [OR] 0.68, 95% confidence interval [CI] 0.35–1.31]). However, ulipristal prevented significantly more pregnancies than levonorgestrel at 72 to 120 hours, with no pregnancies in the ulipristal group and three pregnancies in the levonorgestrel group.9
Because ulipristal has a long half-life (32 hours), it can delay ovulation beyond the life span of sperm, thereby extending the window of opportunity for emergency contraception. However, patients should be advised to avoid further unprotected intercourse after the use of emergency contraception. Because emergency contraception works mainly by delaying ovulation, it may increase the likelihood of pregnancy if the patient has unprotected intercourse again several days later.
IS MIFEPRISTONE AN EMERGENCY CONTRACEPTIVE?
Q: True or false? In the United States, mifepristone (Mifeprex), also known as RU-486, is available for use as an emergency contraceptive in addition to its use in abortion.
A: False, even though mifepristone, another selective progesterone receptor modulator, is highly effective when used up to 120 hours after intercourse. In fact, it might be effective up to 17 days after unprotected intercourse.10
Although mifepristone is one of the most effective forms of emergency contraception, social and political controversy has prevented its approval in the United States. However, it is approved for use as an abortifacient, at a higher dose than would be used for emergency contraception.
Unlike levonorgestrel, mifepristone exerts its effect via two potential mechanisms: delaying ovulation and preventing implantation.11
IUDs AS EMERGENCY CONTRACEPTION
Q: True or false? Insertion of a 5-year intrauterine device (IUD), ie, the levonorgestrel-releasing intrauterine system (Mirena), is 99.8% effective at preventing pregnancy when used within 5 days of unprotected intercourse.
A: False. The Mirena IUD has not been studied as a form of emergency contraception. However, this statement would be true for the 10-year copper IUD ParaGard. Copper-releasing IUDs are considered a very effective method of emergency contraception, with associated pregnancy rates of 0.0% to 0.2% when inserted up until implantation (within 5 days after ovulation).12,13 If desired, the IUD can then be kept in place for up to 10 years as a method of birth control.
However, this method requires the ready availability of a health professional trained to do the insertion. It is also important to make sure that the patient will not be at increased risk of sexually transmitted infections from further unprotected intercourse. The American Congress of Obstetricians and Gynecologists (ACOG) recommends that an IUD be placed within 5 days of unprotected intercourse for use as emergency contraception.
A recent review looked at 42 published studies of copper IUDs used for emergency contraception around the world. It found copper IUDs to be a safe and highly effective method of emergency contraception, with the additional advantage of simultaneously offering one of the most reliable and cost-effective contraceptive options.14
EMERGENCY CONTRACEPTION AT MID-CYCLE
Q: True or false? When choosing a method of emergency contraception, it is important to consider whether a woman is near ovulation during the time of intercourse.
A: True. Emergency contraception can prevent pregnancy after unprotected intercourse, but it does not always work. The most widely used method, levonorgestrel 1.5 mg orally within 72 hours of intercourse, prevents at least 50% of pregnancies that would have occurred in the absence of its use.15 Glasier et al16 showed that emergency contraception was more likely to fail if a woman had unprotected intercourse around the time of ovulation.16
Though it can be difficult for women to tell if they are in the fertile times of their cycle, it might be helpful to try to identify women who have intercourse at mid-cycle, when the risk of pregnancy is greatest. Because insertion of an IUD and use of ulipristal acetate probably prevent more pregnancies, these methods might be preferred over levonorgestrel-based regimens during these higher-risk situations.
OBESE PATIENTS
Q: True or false? Hormonal emergency contraception is more likely to fail in obese patients.
A: True. Most recent evidence shows that whichever oral emergency contraceptive drug is taken, the risk of pregnancy is more than 3 times greater for obese women (OR 3.60, 95% CI 1.96–6.53) and 1.5 times greater for overweight women (OR 1.53, 95% CI 0.75–2.95).16 Of all covariates tested, those that were shown to increase the odds of failure of the emergency contraception were higher body mass index, further unprotected intercourse, and conception probability (based on time of fertility cycle). In fact, among obese women treated with levonorgestrel, the observed pregnancy rate was 5.8%, which is slightly above the overall pregnancy rate expected in the absence of emergency contraception, suggesting that for obese women levonorgestrel-based emergency contraception may even be ineffective.
This is in line with recent reports suggesting that oral contraceptives are less effective in obese women. More effective regimens such as an IUD or ulipristal might be preferred in these women. However, obesity should not be used as a reason not to offer emergency contraception, as this is the last chance these women have to prevent pregnancy.
IS IT ABORTION?
Q: True or false? Emergency contraception does not cause abortion.
A: True, but patients may ask for more details about this. Hormonal emergency contraception works primarily by delaying or inhibiting ovulation and inhibiting fertilization.
Levonorgestrel or combined estrogen-progestin-based methods would be unlikely to have any adverse effects on the endometrium after fertilization, since they would only serve to enhance the progesterone effect. Therefore, they are unlikely to affect the ability of the embryo to attach to the endometrium.
Ulipristal, on the other hand, can have just the opposite effect on the postovulatory endometrium because of its inhibitory action on progesterone. Ulipristal is structurally similar to mifepristone, and its mechanism of action varies depending on the time of administration during the menstrual cycle. When unprotected intercourse occurs during a time when fertility is not possible, ulipristal behaves like a placebo. When intercourse occurs just before ovulation, ulipristal acts by delaying ovulation and thereby preventing fertilization (similar to levonorgestrel). Ulipristal may have an additional action of affecting the ability of the embryo to either attach to the endometrium or maintain its attachment, by a variety of mechanisms of action.17,18 Because of this, some in the popular press and on the Internet have spoken out against the use of ulipristal.
The ACOG considers pregnancy to begin not with fertilization of the egg but with implantation, as demonstrated by a positive pregnancy test.
Of note, the copper IUD also prevents implantation after fertilization, which likely explains its high efficacy.
Women who have detailed questions about this can be counseled that levonorgestrel works mostly by preventing ovulation, and that ulipristal and the copper IUD might also work via postfertilization mechanisms. However, they are not considered to be abortive, based on standard definitions of pregnancy.
If a woman is pregnant and she takes levonorgestrel-based emergency contraception, this has not been shown to have any adverse effects on the fetus (similar to oral contraceptives).
Ulipristal is classified as pregnancy category X, and therefore its use during pregnancy is contraindicated. Based on information provided by the manufacturer, there are no adequate, well-controlled studies of ulipristal use in pregnant women. Although fetal loss was observed in animal studies after ulipristal administration (during the period of organogenesis), no malformations or adverse events were present in the surviving fetuses. Ulipristal is not indicated for termination of an existing pregnancy.
DO THE USUAL CONTRAINDICATIONS TO HORMONAL CONTRACEPTIVES APPLY?
Q: True or false? Because emergency contraception has such a short duration of exposure, the usual medical contraindications to hormonal therapies do not apply to it.
A: True. The usual contraindications to the use of hormonal contraceptives (eg, migraine with aura, hypertension, history of venous thromboembolism) do not apply to emergency contraception because of the short time of exposure.19 Furthermore, the risks associated with pregnancy in these women would likely outweigh any risks associated with emergency contraception.
However, one must be cognizant of potential drug interactions. According to the manufacturer, the use of ulipristal did not inhibit or induce cytochrome P 450 enzymes in vitro; therefore, in vivo studies were not performed. But because ulipristal is metabolized primarily via CYP3A4, an interaction between agents that induce or inhibit CYP3A4 could occur.20 Thus, concomitant use of drugs such as barbiturates, rifampin (Rifadin), St. John’s wort, or antiseizure drugs such as topiramate (Topamax) may lower ulipristal concentrations. These medications may also affect levonorgestrel levels, similar to their effects on combined hormonal contraception. However, it is not known whether this translates to decreased efficacy.
When a woman is taking medications that can potentially decrease the effectiveness of hormonal emergency contraception, a more effective method such as a copper IUD might be more strongly considered. If a woman is not interested in an IUD, oral emergency contraception should still be offered, given that this is one of the last chances to prevent pregnancy, especially if she is on a potential teratogen.
Oral contraceptive pills have not been studied in combination with ulipristal. However, because ulipristal binds with high affinity to progesterone receptors (thus competing with the contraceptive), use of additional barrier contraceptives is recommended for the remainder of the menstrual cycle.
EMERGENCY CONTRACEPTION AND BREASTFEEDING
Q: True of false? Emergency contraceptives can be used if a woman is breastfeeding.
A: That depends on which method is used. Both the ACOG and the World Health Organization state that it is safe for breastfeeding women to use emergency contraception, but these are older guidelines addressing progestin-only regimens (ie, levonorgestrel).19,21 It is unknown whether ulipristal is secreted into human breast milk, although excretion was seen in animal studies. Therefore, ulipristal is not recommended for use by women who are breastfeeding.20,22 To minimize the infant’s exposure to levonorgestrel, mothers should consider not nursing for at least 8 hours after ingestion, but no more than 24 hours is needed.23
- Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health 2011; 43:41–50.
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011; 84:478–485.
- Jones RK, Darroch JE, Henshaw SK. Contraceptive use among US women having abortions in 2000–2001. Perspect Sex Reprod Health 2002; 34:294–303.
- Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. National Center for Health Statistics. Vital Health Stat 2010; 23. http://www.cdc.gov/NCHS/data/series/sr_23/sr23_029.pdf. Accessed October 1, 2012.
- Harrison T. Availability of emergency contraception: a survey of hospital emergency department staff. Ann Emerg Med 2005; 46:105–110.
- Goldenring JM, Allred G. Post-rape care in hospital emergency rooms. Am J Public Health 2001; 91:1169–1170.
- Randomised controlled trial of levonorgestrel versus the Yuzpe regimen of combined oral contraceptives for emergency contraception. Task Force on Postovulatory Methods of Fertility Regulation. Lancet 1998; 352:428–433.
- Creinin MD, Schlaff W, Archer DF, et al. Progesterone receptor modulator for emergency contraception: a randomized controlled trial. Obstet Gynecol 2006; 108:1089–1097.
- Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet 2010; 375:555–562.
- Glasier A, Thong KJ, Dewar M, Mackie M, Baird DT. Mifepristone (RU 486) compared with high-dose estrogen and progestogen for emergency postcoital contraception. N Engl J Med 1992; 327:1041–1044.
- Glasier A. Emergency postcoital contraception. N Engl J Med 1997; 337:1058–1064.
- Stanford JB, Mikolajczyk RT. Mechanisms of action of intrauterine devices: update and estimation of postfertilization effects. Am J Obstet Gynecol 2002; 187:1699–1708.
- Zhou L, Xiao B. Emergency contraception with Multiload Cu-375 SL IUD: a multicenter clinical trial. Contraception 2001; 64:107–112.
- Cleland K, Zhu H, Goldstuck N, Cheng L, Trussell J. The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod 2012; 27:1994–2000.
- Trussell J, Ellertson C, von Hertzen H, et al. Estimating the effectiveness of emergency contraceptive pills. Contraception 2003; 67:259–265.
- Glasier A, Cameron ST, Blithe D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel. Contraception 2011; 84:363–367.
- Miech RP. Immunopharmacology of ulipristal as an emergency contraceptive. Int J Womens Health 2011; 3:391–397.
- Keenan JA. Ulipristal acetate: contraceptive or contragestive? Ann Pharmacother 2011; 45:813–815.
- Medical eligibility criteria for contraceptive use. 3rd ed. Geneva: Reproductive Health and Research, World Health Organization; 2004.
- Ella package insert. Morristown, NJ: Watson Pharmaceuticals; August 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022474s000lbl.pdf. Accessed July 6, 2012.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 112: emergency contraception. Obstet Gynecol 2010; 115:1100–1109.
- Orleans RJ. Clinical review. NDA22-474. Ella (ulipristal acetate 30 mg). US Food and Drug Administration, July 27, 2010. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/UCM295393.pdf. Accessed October 1, 2012.
- Gainer E, Massai R, Lillo S, et al. Levonorgestrel pharmacokinetics in plasma and milk of lactating women who take 1.5 mg for emergency contraception. Hum Reprod 2007; 22:1578–1584.
- Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health 2011; 43:41–50.
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011; 84:478–485.
- Jones RK, Darroch JE, Henshaw SK. Contraceptive use among US women having abortions in 2000–2001. Perspect Sex Reprod Health 2002; 34:294–303.
- Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. National Center for Health Statistics. Vital Health Stat 2010; 23. http://www.cdc.gov/NCHS/data/series/sr_23/sr23_029.pdf. Accessed October 1, 2012.
- Harrison T. Availability of emergency contraception: a survey of hospital emergency department staff. Ann Emerg Med 2005; 46:105–110.
- Goldenring JM, Allred G. Post-rape care in hospital emergency rooms. Am J Public Health 2001; 91:1169–1170.
- Randomised controlled trial of levonorgestrel versus the Yuzpe regimen of combined oral contraceptives for emergency contraception. Task Force on Postovulatory Methods of Fertility Regulation. Lancet 1998; 352:428–433.
- Creinin MD, Schlaff W, Archer DF, et al. Progesterone receptor modulator for emergency contraception: a randomized controlled trial. Obstet Gynecol 2006; 108:1089–1097.
- Glasier AF, Cameron ST, Fine PM, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet 2010; 375:555–562.
- Glasier A, Thong KJ, Dewar M, Mackie M, Baird DT. Mifepristone (RU 486) compared with high-dose estrogen and progestogen for emergency postcoital contraception. N Engl J Med 1992; 327:1041–1044.
- Glasier A. Emergency postcoital contraception. N Engl J Med 1997; 337:1058–1064.
- Stanford JB, Mikolajczyk RT. Mechanisms of action of intrauterine devices: update and estimation of postfertilization effects. Am J Obstet Gynecol 2002; 187:1699–1708.
- Zhou L, Xiao B. Emergency contraception with Multiload Cu-375 SL IUD: a multicenter clinical trial. Contraception 2001; 64:107–112.
- Cleland K, Zhu H, Goldstuck N, Cheng L, Trussell J. The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod 2012; 27:1994–2000.
- Trussell J, Ellertson C, von Hertzen H, et al. Estimating the effectiveness of emergency contraceptive pills. Contraception 2003; 67:259–265.
- Glasier A, Cameron ST, Blithe D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel. Contraception 2011; 84:363–367.
- Miech RP. Immunopharmacology of ulipristal as an emergency contraceptive. Int J Womens Health 2011; 3:391–397.
- Keenan JA. Ulipristal acetate: contraceptive or contragestive? Ann Pharmacother 2011; 45:813–815.
- Medical eligibility criteria for contraceptive use. 3rd ed. Geneva: Reproductive Health and Research, World Health Organization; 2004.
- Ella package insert. Morristown, NJ: Watson Pharmaceuticals; August 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022474s000lbl.pdf. Accessed July 6, 2012.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 112: emergency contraception. Obstet Gynecol 2010; 115:1100–1109.
- Orleans RJ. Clinical review. NDA22-474. Ella (ulipristal acetate 30 mg). US Food and Drug Administration, July 27, 2010. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/UCM295393.pdf. Accessed October 1, 2012.
- Gainer E, Massai R, Lillo S, et al. Levonorgestrel pharmacokinetics in plasma and milk of lactating women who take 1.5 mg for emergency contraception. Hum Reprod 2007; 22:1578–1584.
KEY POINTS
- Levonorgestrel-based emergency contraceptives such as Plan B One-Step, Next Choice, and generics are now available over the counter, which has the advantage of avoiding the delays and hassles of calling the doctor’s office and waiting for prescriptions. But patients still need our guidance on how and when to use emergency contraception.
- Even if patients now have easy access to over-the-counter emergency contraceptives, we physicians should take every opportunity to discuss effective contraceptive options with our patients.
- Ulipristal and copper intrauterine devices (ParaGard) are likely to be more effective than levonorgestrel and should be considered in women at highest risk of pregnancy, such as those who are obese.
- Prescribers should feel comfortable addressing tough questions about mechanisms of action, as controversies and myths about emergency contraception are regularly discussed in the media and on the Internet.