User login
Density: The quality or state of being dense; the quantity per unit volume, unit area, or unit length; the degree of opacity of a translucent medium, or the common logarithm of the opacity.
—Merriam-Webster’s dictionary1
For more than a decade, federal law in the United States has compelled breast imaging centers to give every mammography patient a letter explaining her result.2
Often, however, the first person a woman speaks to about her findings is her primary care clinician, particularly if she has had a screening mammogram at a center where films are “batch-read” and are not viewed by the radiologist at the time of the appointment. Internal medicine physicians are often called on to help women understand their findings and to order follow-up tests recommended by the radiologist—a not uncommon occurrence. Also, internists often need to address patients’ anxieties about the possibility of breast cancer and provide them with enough information to make an informed decision about an appropriate action plan.
Meanwhile, discussing mammography has become more complicated. In 2009, the United States Preventive Services Task Force stopped recommending that women under age 50 be routinely screened for breast cancer, and instead stated that the decision to begin screening these women should consider “patient context” and the patient’s personal “values”3—with the implication that women’s primary clinicians would play an important role in helping them weigh the test’s potential benefits and harms.
More and more, internists must grapple with the task of how to help women decipher the concept of “breast density,” understand their personal density results, and make an informed decision about whether to undergo additional imaging studies, such as ultrasonography and magnetic resonance imaging (MRI).
LEGISLATION REQUIRING DENSITY NOTIFICATION
The impetus for this change in practice has been spurred in large part by patient advocates, who have argued that women deserve to know their density because mammography is less sensitive in women with dense breasts. So far, at least 12 states have enacted laws requiring breast imaging centers to add information about breast density in the result notification letters they mail to patients. Legislatures in several other states are considering breast density notification laws,4 and federal legislation has been proposed.
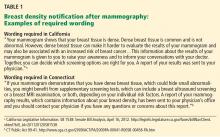
Some of the state laws, such as those in Connecticut, Texas, and Virginia, require informing all mammography patients about their density findings, whether or not they have dense breast tissue. Other states, such as California, Hawaii, and New York, require informing only those found to have dense tissue. And some states, such as California, Connecticut, Hawaii, Texas, and Virginia, require specific wording in the density notification letter (Table 1).
The details of all these notification laws may differ in how they specify which patients must be notified and in how the information should be worded, but the goal is the same: to raise women’s awareness so that they can embark on an informed decision with their physician about whether to undergo further testing.
Because of liability concerns, some breast imaging centers in states that currently lack such notification laws have begun informing women about their density results.
Unfortunately, at this point clinicians have no clear guidelines for helping patients with dense breasts decide whether to undergo additional testing. In addition, the evidence is equivocal, and the tests have risks as well as benefits. The patient needs to understand all this by discussing it with her physician. And to discuss this decision effectively, the physician must be well versed in the evolving literature on breast density. Below, we present important points to keep in mind as we foster these discussions with our patients.
BREAST TISSUE DENSITY IS STILL A SUBJECTIVE MEASUREMENT
Breast density limits the sensitivity of mammography. This is widely established. Yet the interpretation of breast density today is subjective. It is determined by the interpreting radiologist based on the Breast Imaging and Reporting Data System (BI-RADS), which defines “heterogeneously dense” breasts as those containing 50% to 75% dense tissue and “dense” breasts as those with more than 75%5 (Figure 1). This subjective measurement is based on two-dimensional imaging, which may underestimate or overestimate the percentage of breast density because of tissue summation. Ideally, density should be measured using three-dimensional imaging with automated software,6 but this technology is not yet widely available.
INCREASED DETECTION OF BENIGN LESIONS
Although adding ultrasonography to mammography in patients with dense breast tissue detects additional cancers,7,8 it also leads to a significant increase in the detection of lesions that are not malignant yet require additional workup or biopsy.
The largest study to examine this was the American College of Radiology Imaging Network Protocol 6666 (ACRIN 6666),7 a multi-institutional study evaluating the diagnostic yield, sensitivity, and specificity of adding ultrasonography in high-risk patients who presented with negative mammograms and had heterogeneously dense tissue in at least one quadrant.7 (High risk was defined as a threefold higher risk of breast cancer as determined by risk factors such as personal history of breast cancer or high-risk lesions, or elevated risk using the Gail or Claus model.) The supplemental yield was 4.2 cancers per 1,000 women (95% confidence interval 1.1 to 7.2 per 1,000) on a single prevalent screen. Of 12 cancers detected solely by ultrasonography, 11 were invasive and had a median size of 10 mm. Of those reported, 8 of 9 were node-negative. Despite this additional yield, the positive predictive value of biopsy prompted by ultrasonography was only 8.9%.7 Other investigators have reported similar findings.8
RELATIONSHIP BETWEEN DENSITY AND CANCER RISK STILL NOT CLEAR
The relationship between breast density and cancer risk is not entirely clear. Higher breast density has been associated with a higher risk of breast cancer,9,10 presumably because cancer usually develops in parenchyma, and not fatty tissue. Yet obesity and age, which are inversely associated with density, are also risk factors for the development of breast cancer. Some prominent radiologists have cast doubt on the methodology used in these density studies, which relied on density measurements calculated by two-dimensional views of the breast, and have called for a re-evaluation of the relationship between density and cancer risk.6
LIMITED HEALTH LITERACY: A CHALLENGE
The term “breast density” is unfamiliar to most lay people. As physicians, we need to keep in mind that more than a third of US adults have limited health literacy and thus have difficulty processing basic health information.11 But even the 1 in 10 US women with “proficient” health literacy skills may find the term “density” confusing.
As the definition at the opening of this article suggests, the word itself is nuanced and has different meanings. Anecdotally, both of the authors, a general internist (E.M.) and a breast imaging specialist (M.Y.), have encountered numerous quizzical and sometimes distrustful reactions when telling patients—including some with graduate degrees—that they have “dense” breast tissue and might benefit from additional ultrasonographic testing. Avoiding jargon is key; studies have found that terms such as “benign” can be confusing when used in a mammogram result notification letter.12
How can we explain the concept of breast density to our patients?
Supplemental educational materials that feature simple pictures can also be helpful in conveying complex health information,13 although their effect on the communication of breast density has not been studied. The American College of Radiology and the Society of Breast Imaging produce a freely available, downloadable patient brochure on breast density that includes photographs of mammograms with high and low breast density. The brochure is available from the American College of Radiology online at www.acr.org, under “Tools you can use.”
We recommend introducing women to the concept of breast density before they undergo mammography—at the time the test is ordered—and provide them with supplemental materials such as the above-mentioned brochure. About 1 out of every 10 women who undergo screening mammography has a result requiring additional testing that does not result in a cancer diagnosis. Yet a body of research suggests that many women don’t realize that mammograms don’t always yield a cut-and-dried “cancer” or “no cancer” result. In past studies, women have said they were unaware of how common it is to be called back after routine screening mammography, and they wanted to be prepared for this in advance.12,14 Similarly, many women are unaware of the concept of breast density and don’t know that they may be told about these findings when they get their mammogram report.
Avoid causing anxiety
When explaining results to women with dense breasts, we should emphasize that there are no abnormalities on the current mammogram, and that the only reason to consider additional imaging is the breast density. But regardless of the ultimate outcome, an abnormal mammogram can trigger long-standing anxiety, 15 and it is reasonable to assume that some women will become anxious when told they have highly dense breasts. It is important that clinicians be aware of this potential anxiety and inquire about any personal cancer-related concerns at the time they discuss their findings.16
Helping the patient choose the type of additional screening
If a patient is found to have dense breasts and chooses to undergo additional screening, the decision about which test—ultrasonography or MRI—can be based on the woman’s lifetime risk of breast cancer.
The American Cancer Society recommends that patients with a lifetime risk of 20% or greater—according to a risk model such as BRCAPRO, Tyrer-Cuzick, or BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm)—should be screened annually with breast MRI regardless of breast density. Patients in this category are those who carry the BRCA gene mutations and their untested first-degree relatives, and patients with Li-Fraumeni, Cowden, or Bannayan-Riley-Ruvalcaba syndrome. Also considered are women who underwent chest radiation between the ages of 10 and 30, and patients who have more than one first-degree relative with breast cancer but who do not have an identifiable genetic mutation.17
Patients with dense breasts who have an increased lifetime risk but who do not meet these criteria and those who are at average risk may be offered breast ultrasonography. If risk factors are unclear, genetic counseling can help determine the lifetime risk and thus help the patient choose the additional screening test.18
MORE WORK TO DO
Clearly, we still do not know how to explain breast density results to our patients in a way that will help them make a fully informed decision about additional screening. Research suggests that letters alone are insufficient,13,19,20 and there is no guarantee that simply adding breast density notification language to result letters will enhance a woman’s understanding and empower her to choose a course of action that is sensitive to her personal preferences.
As more states adopt notification legislation, we must develop effective methods to improve our patients’ understanding of the meaning and implications of having dense breasts and to help them decide how to proceed. Such tools could include videos, Web sites, and pictorials, as well as specialized training for patient educators and health navigators. Otherwise, including this additional, conceptually difficult information to result notification letters could make the doctor-patient interaction even more “dense”—and could increase women’s uncertainty and anxiety about their personal risk of cancer.21
- Merriam-Webster online dictionary. Density http://www.merriam-webster.com/dictionary/density. Accessed November 12, 2013.
- US Food and Drug Administration (FDA). Radiation-emitting products: Frequently asked questions about MQSA. http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/ConsumerInformation/ucm113968.htm. Accessed November 12, 2013.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726, W–236.
- Are You Dense Advocacy Inc. Are you dense? http://areyoudenseadvocacy.org. Accessed November 12, 2013.
- American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS). 4th ed. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/BIRADS/MammoBIRADS.pdf. Accessed November 12, 2013.
- Kopans DB. Basic physics and doubts about relationship between mammographically determined tissue density and breast cancer risk. Radiology 2008; 246:348–353.
- Berg WA, Blume JD, Cormack JB, et al; ACRIN 6666 Investigators. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 2008; 299:2151–2163.
- Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology 2012; 265:59–69.
- Vacek PM, Geller BM. A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomarkers Prev 2004; 13:715–722.
- Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med 2007; 356:227–236.
- Kutner M, Greenberg E, Jin Y, Paulsen C; National Center for Education Statistics. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy. US Department of Education. http://nces.ed.gov/pubs2006/2006483.pdf. Accessed November 12, 2013.
- Marcus EN, Drummond D, Dietz N. Urban women’s p for learning of their mammogram result: a qualitative study. J Cancer Educ 2012; 27:156–164.
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006; 61:173–190.
- Nekhlyudov L, Li R, Fletcher SW. Information and involvement p of women in their 40s before their first screening mammogram. Arch Intern Med 2005; 165:1370–1374.
- Barton MB, Moore S, Polk S, Shtatland E, Elmore JG, Fletcher SW. Increased patient concern after false-positive mammograms: clinician documentation and subsequent ambulatory visits. J Gen Intern Med 2001; 16:150–156.
- Politi MC, Street RL. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract 2011; 17:579–584.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57:75–89.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol 2009; 192:390–399.
- Jones BA, Reams K, Calvocoressi L, Dailey A, Kasl SV, Liston NM. Adequacy of communicating results from screening mammograms to African American and white women. Am J Public Health 2007; 97:531–538.
- Karliner LS, Patricia Kaplan C, Juarbe T, Pasick R, Pérez-Stable EJ. Poor patient comprehension of abnormal mammography results. J Gen Intern Med 2005; 20:432–437.
- Marcus EN. Post-mammogram letters often confuse more than they help. Washington Post, February 25, 2013. http://articles.washingtonpost.com/2013-02-25/national/37287736_1_mammogram-letters-densebreasts/2. Accessed November 12, 2013.
Density: The quality or state of being dense; the quantity per unit volume, unit area, or unit length; the degree of opacity of a translucent medium, or the common logarithm of the opacity.
—Merriam-Webster’s dictionary1
For more than a decade, federal law in the United States has compelled breast imaging centers to give every mammography patient a letter explaining her result.2
Often, however, the first person a woman speaks to about her findings is her primary care clinician, particularly if she has had a screening mammogram at a center where films are “batch-read” and are not viewed by the radiologist at the time of the appointment. Internal medicine physicians are often called on to help women understand their findings and to order follow-up tests recommended by the radiologist—a not uncommon occurrence. Also, internists often need to address patients’ anxieties about the possibility of breast cancer and provide them with enough information to make an informed decision about an appropriate action plan.
Meanwhile, discussing mammography has become more complicated. In 2009, the United States Preventive Services Task Force stopped recommending that women under age 50 be routinely screened for breast cancer, and instead stated that the decision to begin screening these women should consider “patient context” and the patient’s personal “values”3—with the implication that women’s primary clinicians would play an important role in helping them weigh the test’s potential benefits and harms.
More and more, internists must grapple with the task of how to help women decipher the concept of “breast density,” understand their personal density results, and make an informed decision about whether to undergo additional imaging studies, such as ultrasonography and magnetic resonance imaging (MRI).
LEGISLATION REQUIRING DENSITY NOTIFICATION
The impetus for this change in practice has been spurred in large part by patient advocates, who have argued that women deserve to know their density because mammography is less sensitive in women with dense breasts. So far, at least 12 states have enacted laws requiring breast imaging centers to add information about breast density in the result notification letters they mail to patients. Legislatures in several other states are considering breast density notification laws,4 and federal legislation has been proposed.
Some of the state laws, such as those in Connecticut, Texas, and Virginia, require informing all mammography patients about their density findings, whether or not they have dense breast tissue. Other states, such as California, Hawaii, and New York, require informing only those found to have dense tissue. And some states, such as California, Connecticut, Hawaii, Texas, and Virginia, require specific wording in the density notification letter (Table 1).
The details of all these notification laws may differ in how they specify which patients must be notified and in how the information should be worded, but the goal is the same: to raise women’s awareness so that they can embark on an informed decision with their physician about whether to undergo further testing.
Because of liability concerns, some breast imaging centers in states that currently lack such notification laws have begun informing women about their density results.
Unfortunately, at this point clinicians have no clear guidelines for helping patients with dense breasts decide whether to undergo additional testing. In addition, the evidence is equivocal, and the tests have risks as well as benefits. The patient needs to understand all this by discussing it with her physician. And to discuss this decision effectively, the physician must be well versed in the evolving literature on breast density. Below, we present important points to keep in mind as we foster these discussions with our patients.
BREAST TISSUE DENSITY IS STILL A SUBJECTIVE MEASUREMENT
Breast density limits the sensitivity of mammography. This is widely established. Yet the interpretation of breast density today is subjective. It is determined by the interpreting radiologist based on the Breast Imaging and Reporting Data System (BI-RADS), which defines “heterogeneously dense” breasts as those containing 50% to 75% dense tissue and “dense” breasts as those with more than 75%5 (Figure 1). This subjective measurement is based on two-dimensional imaging, which may underestimate or overestimate the percentage of breast density because of tissue summation. Ideally, density should be measured using three-dimensional imaging with automated software,6 but this technology is not yet widely available.
INCREASED DETECTION OF BENIGN LESIONS
Although adding ultrasonography to mammography in patients with dense breast tissue detects additional cancers,7,8 it also leads to a significant increase in the detection of lesions that are not malignant yet require additional workup or biopsy.
The largest study to examine this was the American College of Radiology Imaging Network Protocol 6666 (ACRIN 6666),7 a multi-institutional study evaluating the diagnostic yield, sensitivity, and specificity of adding ultrasonography in high-risk patients who presented with negative mammograms and had heterogeneously dense tissue in at least one quadrant.7 (High risk was defined as a threefold higher risk of breast cancer as determined by risk factors such as personal history of breast cancer or high-risk lesions, or elevated risk using the Gail or Claus model.) The supplemental yield was 4.2 cancers per 1,000 women (95% confidence interval 1.1 to 7.2 per 1,000) on a single prevalent screen. Of 12 cancers detected solely by ultrasonography, 11 were invasive and had a median size of 10 mm. Of those reported, 8 of 9 were node-negative. Despite this additional yield, the positive predictive value of biopsy prompted by ultrasonography was only 8.9%.7 Other investigators have reported similar findings.8
RELATIONSHIP BETWEEN DENSITY AND CANCER RISK STILL NOT CLEAR
The relationship between breast density and cancer risk is not entirely clear. Higher breast density has been associated with a higher risk of breast cancer,9,10 presumably because cancer usually develops in parenchyma, and not fatty tissue. Yet obesity and age, which are inversely associated with density, are also risk factors for the development of breast cancer. Some prominent radiologists have cast doubt on the methodology used in these density studies, which relied on density measurements calculated by two-dimensional views of the breast, and have called for a re-evaluation of the relationship between density and cancer risk.6
LIMITED HEALTH LITERACY: A CHALLENGE
The term “breast density” is unfamiliar to most lay people. As physicians, we need to keep in mind that more than a third of US adults have limited health literacy and thus have difficulty processing basic health information.11 But even the 1 in 10 US women with “proficient” health literacy skills may find the term “density” confusing.
As the definition at the opening of this article suggests, the word itself is nuanced and has different meanings. Anecdotally, both of the authors, a general internist (E.M.) and a breast imaging specialist (M.Y.), have encountered numerous quizzical and sometimes distrustful reactions when telling patients—including some with graduate degrees—that they have “dense” breast tissue and might benefit from additional ultrasonographic testing. Avoiding jargon is key; studies have found that terms such as “benign” can be confusing when used in a mammogram result notification letter.12
How can we explain the concept of breast density to our patients?
Supplemental educational materials that feature simple pictures can also be helpful in conveying complex health information,13 although their effect on the communication of breast density has not been studied. The American College of Radiology and the Society of Breast Imaging produce a freely available, downloadable patient brochure on breast density that includes photographs of mammograms with high and low breast density. The brochure is available from the American College of Radiology online at www.acr.org, under “Tools you can use.”
We recommend introducing women to the concept of breast density before they undergo mammography—at the time the test is ordered—and provide them with supplemental materials such as the above-mentioned brochure. About 1 out of every 10 women who undergo screening mammography has a result requiring additional testing that does not result in a cancer diagnosis. Yet a body of research suggests that many women don’t realize that mammograms don’t always yield a cut-and-dried “cancer” or “no cancer” result. In past studies, women have said they were unaware of how common it is to be called back after routine screening mammography, and they wanted to be prepared for this in advance.12,14 Similarly, many women are unaware of the concept of breast density and don’t know that they may be told about these findings when they get their mammogram report.
Avoid causing anxiety
When explaining results to women with dense breasts, we should emphasize that there are no abnormalities on the current mammogram, and that the only reason to consider additional imaging is the breast density. But regardless of the ultimate outcome, an abnormal mammogram can trigger long-standing anxiety, 15 and it is reasonable to assume that some women will become anxious when told they have highly dense breasts. It is important that clinicians be aware of this potential anxiety and inquire about any personal cancer-related concerns at the time they discuss their findings.16
Helping the patient choose the type of additional screening
If a patient is found to have dense breasts and chooses to undergo additional screening, the decision about which test—ultrasonography or MRI—can be based on the woman’s lifetime risk of breast cancer.
The American Cancer Society recommends that patients with a lifetime risk of 20% or greater—according to a risk model such as BRCAPRO, Tyrer-Cuzick, or BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm)—should be screened annually with breast MRI regardless of breast density. Patients in this category are those who carry the BRCA gene mutations and their untested first-degree relatives, and patients with Li-Fraumeni, Cowden, or Bannayan-Riley-Ruvalcaba syndrome. Also considered are women who underwent chest radiation between the ages of 10 and 30, and patients who have more than one first-degree relative with breast cancer but who do not have an identifiable genetic mutation.17
Patients with dense breasts who have an increased lifetime risk but who do not meet these criteria and those who are at average risk may be offered breast ultrasonography. If risk factors are unclear, genetic counseling can help determine the lifetime risk and thus help the patient choose the additional screening test.18
MORE WORK TO DO
Clearly, we still do not know how to explain breast density results to our patients in a way that will help them make a fully informed decision about additional screening. Research suggests that letters alone are insufficient,13,19,20 and there is no guarantee that simply adding breast density notification language to result letters will enhance a woman’s understanding and empower her to choose a course of action that is sensitive to her personal preferences.
As more states adopt notification legislation, we must develop effective methods to improve our patients’ understanding of the meaning and implications of having dense breasts and to help them decide how to proceed. Such tools could include videos, Web sites, and pictorials, as well as specialized training for patient educators and health navigators. Otherwise, including this additional, conceptually difficult information to result notification letters could make the doctor-patient interaction even more “dense”—and could increase women’s uncertainty and anxiety about their personal risk of cancer.21
Density: The quality or state of being dense; the quantity per unit volume, unit area, or unit length; the degree of opacity of a translucent medium, or the common logarithm of the opacity.
—Merriam-Webster’s dictionary1
For more than a decade, federal law in the United States has compelled breast imaging centers to give every mammography patient a letter explaining her result.2
Often, however, the first person a woman speaks to about her findings is her primary care clinician, particularly if she has had a screening mammogram at a center where films are “batch-read” and are not viewed by the radiologist at the time of the appointment. Internal medicine physicians are often called on to help women understand their findings and to order follow-up tests recommended by the radiologist—a not uncommon occurrence. Also, internists often need to address patients’ anxieties about the possibility of breast cancer and provide them with enough information to make an informed decision about an appropriate action plan.
Meanwhile, discussing mammography has become more complicated. In 2009, the United States Preventive Services Task Force stopped recommending that women under age 50 be routinely screened for breast cancer, and instead stated that the decision to begin screening these women should consider “patient context” and the patient’s personal “values”3—with the implication that women’s primary clinicians would play an important role in helping them weigh the test’s potential benefits and harms.
More and more, internists must grapple with the task of how to help women decipher the concept of “breast density,” understand their personal density results, and make an informed decision about whether to undergo additional imaging studies, such as ultrasonography and magnetic resonance imaging (MRI).
LEGISLATION REQUIRING DENSITY NOTIFICATION
The impetus for this change in practice has been spurred in large part by patient advocates, who have argued that women deserve to know their density because mammography is less sensitive in women with dense breasts. So far, at least 12 states have enacted laws requiring breast imaging centers to add information about breast density in the result notification letters they mail to patients. Legislatures in several other states are considering breast density notification laws,4 and federal legislation has been proposed.
Some of the state laws, such as those in Connecticut, Texas, and Virginia, require informing all mammography patients about their density findings, whether or not they have dense breast tissue. Other states, such as California, Hawaii, and New York, require informing only those found to have dense tissue. And some states, such as California, Connecticut, Hawaii, Texas, and Virginia, require specific wording in the density notification letter (Table 1).
The details of all these notification laws may differ in how they specify which patients must be notified and in how the information should be worded, but the goal is the same: to raise women’s awareness so that they can embark on an informed decision with their physician about whether to undergo further testing.
Because of liability concerns, some breast imaging centers in states that currently lack such notification laws have begun informing women about their density results.
Unfortunately, at this point clinicians have no clear guidelines for helping patients with dense breasts decide whether to undergo additional testing. In addition, the evidence is equivocal, and the tests have risks as well as benefits. The patient needs to understand all this by discussing it with her physician. And to discuss this decision effectively, the physician must be well versed in the evolving literature on breast density. Below, we present important points to keep in mind as we foster these discussions with our patients.
BREAST TISSUE DENSITY IS STILL A SUBJECTIVE MEASUREMENT
Breast density limits the sensitivity of mammography. This is widely established. Yet the interpretation of breast density today is subjective. It is determined by the interpreting radiologist based on the Breast Imaging and Reporting Data System (BI-RADS), which defines “heterogeneously dense” breasts as those containing 50% to 75% dense tissue and “dense” breasts as those with more than 75%5 (Figure 1). This subjective measurement is based on two-dimensional imaging, which may underestimate or overestimate the percentage of breast density because of tissue summation. Ideally, density should be measured using three-dimensional imaging with automated software,6 but this technology is not yet widely available.
INCREASED DETECTION OF BENIGN LESIONS
Although adding ultrasonography to mammography in patients with dense breast tissue detects additional cancers,7,8 it also leads to a significant increase in the detection of lesions that are not malignant yet require additional workup or biopsy.
The largest study to examine this was the American College of Radiology Imaging Network Protocol 6666 (ACRIN 6666),7 a multi-institutional study evaluating the diagnostic yield, sensitivity, and specificity of adding ultrasonography in high-risk patients who presented with negative mammograms and had heterogeneously dense tissue in at least one quadrant.7 (High risk was defined as a threefold higher risk of breast cancer as determined by risk factors such as personal history of breast cancer or high-risk lesions, or elevated risk using the Gail or Claus model.) The supplemental yield was 4.2 cancers per 1,000 women (95% confidence interval 1.1 to 7.2 per 1,000) on a single prevalent screen. Of 12 cancers detected solely by ultrasonography, 11 were invasive and had a median size of 10 mm. Of those reported, 8 of 9 were node-negative. Despite this additional yield, the positive predictive value of biopsy prompted by ultrasonography was only 8.9%.7 Other investigators have reported similar findings.8
RELATIONSHIP BETWEEN DENSITY AND CANCER RISK STILL NOT CLEAR
The relationship between breast density and cancer risk is not entirely clear. Higher breast density has been associated with a higher risk of breast cancer,9,10 presumably because cancer usually develops in parenchyma, and not fatty tissue. Yet obesity and age, which are inversely associated with density, are also risk factors for the development of breast cancer. Some prominent radiologists have cast doubt on the methodology used in these density studies, which relied on density measurements calculated by two-dimensional views of the breast, and have called for a re-evaluation of the relationship between density and cancer risk.6
LIMITED HEALTH LITERACY: A CHALLENGE
The term “breast density” is unfamiliar to most lay people. As physicians, we need to keep in mind that more than a third of US adults have limited health literacy and thus have difficulty processing basic health information.11 But even the 1 in 10 US women with “proficient” health literacy skills may find the term “density” confusing.
As the definition at the opening of this article suggests, the word itself is nuanced and has different meanings. Anecdotally, both of the authors, a general internist (E.M.) and a breast imaging specialist (M.Y.), have encountered numerous quizzical and sometimes distrustful reactions when telling patients—including some with graduate degrees—that they have “dense” breast tissue and might benefit from additional ultrasonographic testing. Avoiding jargon is key; studies have found that terms such as “benign” can be confusing when used in a mammogram result notification letter.12
How can we explain the concept of breast density to our patients?
Supplemental educational materials that feature simple pictures can also be helpful in conveying complex health information,13 although their effect on the communication of breast density has not been studied. The American College of Radiology and the Society of Breast Imaging produce a freely available, downloadable patient brochure on breast density that includes photographs of mammograms with high and low breast density. The brochure is available from the American College of Radiology online at www.acr.org, under “Tools you can use.”
We recommend introducing women to the concept of breast density before they undergo mammography—at the time the test is ordered—and provide them with supplemental materials such as the above-mentioned brochure. About 1 out of every 10 women who undergo screening mammography has a result requiring additional testing that does not result in a cancer diagnosis. Yet a body of research suggests that many women don’t realize that mammograms don’t always yield a cut-and-dried “cancer” or “no cancer” result. In past studies, women have said they were unaware of how common it is to be called back after routine screening mammography, and they wanted to be prepared for this in advance.12,14 Similarly, many women are unaware of the concept of breast density and don’t know that they may be told about these findings when they get their mammogram report.
Avoid causing anxiety
When explaining results to women with dense breasts, we should emphasize that there are no abnormalities on the current mammogram, and that the only reason to consider additional imaging is the breast density. But regardless of the ultimate outcome, an abnormal mammogram can trigger long-standing anxiety, 15 and it is reasonable to assume that some women will become anxious when told they have highly dense breasts. It is important that clinicians be aware of this potential anxiety and inquire about any personal cancer-related concerns at the time they discuss their findings.16
Helping the patient choose the type of additional screening
If a patient is found to have dense breasts and chooses to undergo additional screening, the decision about which test—ultrasonography or MRI—can be based on the woman’s lifetime risk of breast cancer.
The American Cancer Society recommends that patients with a lifetime risk of 20% or greater—according to a risk model such as BRCAPRO, Tyrer-Cuzick, or BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm)—should be screened annually with breast MRI regardless of breast density. Patients in this category are those who carry the BRCA gene mutations and their untested first-degree relatives, and patients with Li-Fraumeni, Cowden, or Bannayan-Riley-Ruvalcaba syndrome. Also considered are women who underwent chest radiation between the ages of 10 and 30, and patients who have more than one first-degree relative with breast cancer but who do not have an identifiable genetic mutation.17
Patients with dense breasts who have an increased lifetime risk but who do not meet these criteria and those who are at average risk may be offered breast ultrasonography. If risk factors are unclear, genetic counseling can help determine the lifetime risk and thus help the patient choose the additional screening test.18
MORE WORK TO DO
Clearly, we still do not know how to explain breast density results to our patients in a way that will help them make a fully informed decision about additional screening. Research suggests that letters alone are insufficient,13,19,20 and there is no guarantee that simply adding breast density notification language to result letters will enhance a woman’s understanding and empower her to choose a course of action that is sensitive to her personal preferences.
As more states adopt notification legislation, we must develop effective methods to improve our patients’ understanding of the meaning and implications of having dense breasts and to help them decide how to proceed. Such tools could include videos, Web sites, and pictorials, as well as specialized training for patient educators and health navigators. Otherwise, including this additional, conceptually difficult information to result notification letters could make the doctor-patient interaction even more “dense”—and could increase women’s uncertainty and anxiety about their personal risk of cancer.21
- Merriam-Webster online dictionary. Density http://www.merriam-webster.com/dictionary/density. Accessed November 12, 2013.
- US Food and Drug Administration (FDA). Radiation-emitting products: Frequently asked questions about MQSA. http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/ConsumerInformation/ucm113968.htm. Accessed November 12, 2013.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726, W–236.
- Are You Dense Advocacy Inc. Are you dense? http://areyoudenseadvocacy.org. Accessed November 12, 2013.
- American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS). 4th ed. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/BIRADS/MammoBIRADS.pdf. Accessed November 12, 2013.
- Kopans DB. Basic physics and doubts about relationship between mammographically determined tissue density and breast cancer risk. Radiology 2008; 246:348–353.
- Berg WA, Blume JD, Cormack JB, et al; ACRIN 6666 Investigators. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 2008; 299:2151–2163.
- Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology 2012; 265:59–69.
- Vacek PM, Geller BM. A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomarkers Prev 2004; 13:715–722.
- Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med 2007; 356:227–236.
- Kutner M, Greenberg E, Jin Y, Paulsen C; National Center for Education Statistics. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy. US Department of Education. http://nces.ed.gov/pubs2006/2006483.pdf. Accessed November 12, 2013.
- Marcus EN, Drummond D, Dietz N. Urban women’s p for learning of their mammogram result: a qualitative study. J Cancer Educ 2012; 27:156–164.
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006; 61:173–190.
- Nekhlyudov L, Li R, Fletcher SW. Information and involvement p of women in their 40s before their first screening mammogram. Arch Intern Med 2005; 165:1370–1374.
- Barton MB, Moore S, Polk S, Shtatland E, Elmore JG, Fletcher SW. Increased patient concern after false-positive mammograms: clinician documentation and subsequent ambulatory visits. J Gen Intern Med 2001; 16:150–156.
- Politi MC, Street RL. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract 2011; 17:579–584.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57:75–89.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol 2009; 192:390–399.
- Jones BA, Reams K, Calvocoressi L, Dailey A, Kasl SV, Liston NM. Adequacy of communicating results from screening mammograms to African American and white women. Am J Public Health 2007; 97:531–538.
- Karliner LS, Patricia Kaplan C, Juarbe T, Pasick R, Pérez-Stable EJ. Poor patient comprehension of abnormal mammography results. J Gen Intern Med 2005; 20:432–437.
- Marcus EN. Post-mammogram letters often confuse more than they help. Washington Post, February 25, 2013. http://articles.washingtonpost.com/2013-02-25/national/37287736_1_mammogram-letters-densebreasts/2. Accessed November 12, 2013.
- Merriam-Webster online dictionary. Density http://www.merriam-webster.com/dictionary/density. Accessed November 12, 2013.
- US Food and Drug Administration (FDA). Radiation-emitting products: Frequently asked questions about MQSA. http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/ConsumerInformation/ucm113968.htm. Accessed November 12, 2013.
- US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151:716–726, W–236.
- Are You Dense Advocacy Inc. Are you dense? http://areyoudenseadvocacy.org. Accessed November 12, 2013.
- American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS). 4th ed. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/BIRADS/MammoBIRADS.pdf. Accessed November 12, 2013.
- Kopans DB. Basic physics and doubts about relationship between mammographically determined tissue density and breast cancer risk. Radiology 2008; 246:348–353.
- Berg WA, Blume JD, Cormack JB, et al; ACRIN 6666 Investigators. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 2008; 299:2151–2163.
- Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology 2012; 265:59–69.
- Vacek PM, Geller BM. A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomarkers Prev 2004; 13:715–722.
- Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med 2007; 356:227–236.
- Kutner M, Greenberg E, Jin Y, Paulsen C; National Center for Education Statistics. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy. US Department of Education. http://nces.ed.gov/pubs2006/2006483.pdf. Accessed November 12, 2013.
- Marcus EN, Drummond D, Dietz N. Urban women’s p for learning of their mammogram result: a qualitative study. J Cancer Educ 2012; 27:156–164.
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006; 61:173–190.
- Nekhlyudov L, Li R, Fletcher SW. Information and involvement p of women in their 40s before their first screening mammogram. Arch Intern Med 2005; 165:1370–1374.
- Barton MB, Moore S, Polk S, Shtatland E, Elmore JG, Fletcher SW. Increased patient concern after false-positive mammograms: clinician documentation and subsequent ambulatory visits. J Gen Intern Med 2001; 16:150–156.
- Politi MC, Street RL. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract 2011; 17:579–584.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57:75–89.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol 2009; 192:390–399.
- Jones BA, Reams K, Calvocoressi L, Dailey A, Kasl SV, Liston NM. Adequacy of communicating results from screening mammograms to African American and white women. Am J Public Health 2007; 97:531–538.
- Karliner LS, Patricia Kaplan C, Juarbe T, Pasick R, Pérez-Stable EJ. Poor patient comprehension of abnormal mammography results. J Gen Intern Med 2005; 20:432–437.
- Marcus EN. Post-mammogram letters often confuse more than they help. Washington Post, February 25, 2013. http://articles.washingtonpost.com/2013-02-25/national/37287736_1_mammogram-letters-densebreasts/2. Accessed November 12, 2013.