User login
Counterphobia and Poor Sun Protection Practices in First-Degree Relatives of Melanoma Patients
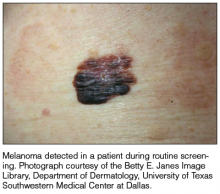
It is widely accepted that there are several factors that may independently elevate an individual’s risk for melanoma, such as a history of childhood sunburns, family history of melanoma, and poor sun protection practices. Several studies have examined risk behaviors in melanoma patients following their diagnosis and have reported findings such as increased UV exposure patterns, persistent tanning bed use, and sun-protective behaviors similar to those of the general population (Figure).1-4
Although first-degree relatives (FDRs) of melanoma patients are at an increased risk for melanoma, they also have been found to exhibit surprisingly poor sun protection practices. In one retrospective analysis, Geller et al5 found that frequent sunburns, high rates of tanning bed use, and low rates of sunscreen use were common among children of health care workers who reported a personal or family history of skin cancer. An independent study reported that merely 37% (37/100) of FDRs of melanoma patients use sunscreen more than half of the time, and considerably fewer wear protective clothing or seek shade while outdoors.6 Given their increased risk for developing melanoma, it is likely to be assumed that FDRs of melanoma patients practice diligent sun protection. The underlying reasons for the failure of this at-risk population to adhere strongly to sun protection practices warrants special attention.
Manne et al7 conducted a survey in a group of FDRs of melanoma patients with self-reported poor sun protection practices to evaluate the demographic, medical, psychological, educational (knowledge of sun protection guidelines), and social influences that correlate with sun protection and sunbathing practices. More effective sun protective behaviors were identified in FDRs with higher education, fewer perceived benefits of sunbathing, more prominent photoaging concerns, and greater sunscreen self-efficacy. The authors concluded that sun-protective behavior in FDRs was not associated with prior knowledge about sunscreen or UV exposure, their relative’s melanoma stage, or physician recommendations for sun protection.7
Factors that have been documented as influencing sun-protective behavior in the general population include knowledge of the benefits of sun protection; attitudes toward tanning and sun protection; subjective norms regarding the beauty and perceived health of a tan; and optimistic bias, which is a cognitive mechanism that causes a person to believe that he/she is at lesser risk for experiencing a negative outcome compared to others. Additionally, sun protection behaviors are influenced by the immediacy of getting the reward (the perceived benefits of tanning) versus the delayed punishment (development of skin cancer).6 Although all of these elements may be important for some individuals, we believe that a subset of FDRs of melanoma patients may be susceptible to the phenomenon known as counterphobia.
Counterphobia is a neurotic response to anxiety in which an individual actively pursues situations that heighten his/her fear rather than fleeing from a feared object or behavior.8 Most insight into counterphobia has come from the experiences of children who have parent(s) with a debilitating or fatal diagnosis. Due to their immature coping mechanisms, some children are at risk for maladaptive behavioral responses. The loss of a parent typically produces severe psychological trauma in all children, but in those who develop counterphobia, it manifests as a heightened fear of death and vulnerability to their parent’s illness. This maladaptive response is dependent on self-identification with the parent, especially among daughters of lost mothers and sons of lost fathers, and this fear remains with the child through adulthood. A survey of 154 motherless daughters found that women aged 19 to 35 years have the highest level of obsessive thoughts of mortality and more than 75% believe they will succumb to their mother’s illness (92% in the case of cancer).9 Despite this fear, children may exhibit health-compromising behaviors related to the diagnoses that led to their parents’ deaths; for example, counterphobia has been identified as a pathologic factor behind sexually promiscuous practices in the children of patients with AIDS, and it also may explain high-risk drinking behavior in a child whose parent died from hepatocellular carcinoma due to a history of alcoholic cirrhosis. Similarly, counterphobia can manifest as the deliberate refusal to undergo a mammogram in a woman whose mother died of breast cancer.9 Psychologists have hypothesized that counterphobic pursuits may result from attempts to master the anxiety associated with fear of injury or death as well as from the notion that attempts at risk-factor reduction are futile, as their death is certain.10
The strong influence of counterphobia on perspectives of health and mortality among individuals affected by early loss of a parent is well documented. An assessment of the subjective life expectancy, death anxiety, and health-related behaviors of college students who lost a parent revealed that these individuals estimated their own life spans to be shorter than college students with 2 living parents.11 Moreover, when students were explicitly instructed to predict their life expectancy based on a purely objective mentality rather than one influenced by personal feelings, the exclusion of emotion yielded a longer projected life span. This finding highlights the magnitude of the psychological forces influencing the ethos of individuals affected by premature parental loss. In the same study, individuals who had experienced early loss of a parent believed they would die of the same condition that caused their parent’s death, a finding accompanied by notably poorer diet and smoking behaviors, which might be expected among those with counterphobic defenses.11
Although Manne et al7 did not find an association between melanoma disease severity and sun-protective behavior in FDRs, the study design did not allow for assessment of potential counterphobic responses, which are most likely to develop in younger individuals who strongly identify with the family member whose disease was disabling or fatal. For example, the study included adult relatives (mean age, 46 years) of melanoma patients diagnosed in the preceding 4 years. Furthermore, fewer than 20% (108/545) of the patients had stage III or IV melanoma, and it was not known if melanoma patients communicated the diagnosis to their family members.7
A practice gap exists in FDRs of melanoma patients who are largely assumed to be practicing adequate, if not heightened, sun protection practices. Given that this group demonstrates poor sun protection practices, it is important to identify reasons for such behavior that may extend beyond what is currently known and may include counterphobia. Based on research performed in other medical conditions, the individuals most at risk for counterphobic responses are young children of patients diagnosed with a disabling or fatal condition, but whether in cases of melanoma counterphobia exists as a maladaptive response and whether such a response may occur in all close relatives, not just offspring, is unknown. Currently, the type of measure(s) that may mitigate poor risk factor modification due to counterphobia, including sun protection practices, is unknown. However, physician knowledge of counterphobic responses as a possibility in close relatives of melanoma patients may improve physician efforts to modify behavior in this unique, high-risk population.
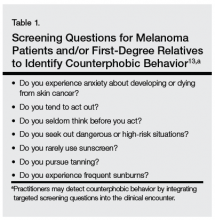
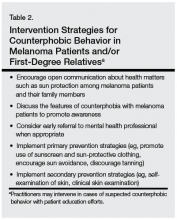
The multimodal pathway of melanoma development suggests that individuals with an underlying genetic predisposition for melanoma who also neglect sun-protective measures are an especially high-risk group.12 As such, targeted education and screening of this patient population may be warranted (Table 1). Although it is incumbent on physicians to incorporate concerted screening, counseling, and focused interventions for newly diagnosed melanoma patients, taking similar measures to counsel and educate immediate relatives who may be at high risk for poor sun protection practices also is encouraged (Table 2).
We believe that recognition of counterphobic behavior is critical in the evaluation of FDRs of melanoma patients. Heightened awareness may bolster primary prevention efforts, especially in our patients with genetic diatheses toward melanoma development.
1. Idorn L, Datta P, Heydenreich J, et al. A 3-year follow-up of sun behavior in patients with cutaneous malignant melanoma [published online ahead of print October 2, 2013]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.5098.
2. Idorn LW, Datta P, Heydenreich J, et al. Sun behaviour after cutaneous malignant melanoma: a study based on ultraviolet radiation measurements and sun diary data [published online ahead of print]. Br J Dermatol. 2013;168:367-373.
3. Mayer D, Layman A, Carlson J. Sun-protection behaviors of melanoma survivors. J Am Acad Dermatol. 2012;66:e9-e10.
4. Lee TK, Brazier AS, Shoveller JA, et al. Sun-related behavior after a diagnosis of cutaneous malignant melanoma. Melanoma Res. 2007;17:51-55.
5. Geller AC, Brooks DR, Colditz GA, et al. Sun protection practices among offspring of women with personal or family history of skin cancer. Pediatrics. 2006;117:e688-e694.
6. Azzarello LM, Dessureault S, Jacobsen PB. Sun-protective behavior among individuals with a family history of melanoma. Cancer Epidemiol Boomarkers Prev. 2006;15:142-145.
7. Manne SL, Coups EJ, Jacobsen PB, et al. Sun protection and sunbathing practices among at-risk family members of patients with melanoma. BMC Public Health. 2011;11:122.
8. Fenichel O. The Psychoanalytic Theory of Neurosis. Oxford, United Kingdom: Taylor & Francis; 1999.
9. Edelman H. Motherless Daughters: The Legacy of Loss. 2nd ed. Cambridge, MA: Da Capo Press; 2006.
10. Poznanski E, Arthur B. The counterphobic defense in children. Child Psychiatry Hum Dev. 1971;1:178-191.
11. Denes-Raj V, Ehrlichman H. Effects of premature parental death on subjective life expectancy, death anxiety, and health behavior. Omega: Journal of Death and Dying. 1991;23:309-321.
12. Hayward NK. Genetics of melanoma predisposition. Oncogene. 2003;22:3053-3062.
13. Arthey S, Clarke VA. Suntanning and sun protection: a review of the psychologial literature. Soc Sci Med. 1995;40:265-274.
It is widely accepted that there are several factors that may independently elevate an individual’s risk for melanoma, such as a history of childhood sunburns, family history of melanoma, and poor sun protection practices. Several studies have examined risk behaviors in melanoma patients following their diagnosis and have reported findings such as increased UV exposure patterns, persistent tanning bed use, and sun-protective behaviors similar to those of the general population (Figure).1-4
Although first-degree relatives (FDRs) of melanoma patients are at an increased risk for melanoma, they also have been found to exhibit surprisingly poor sun protection practices. In one retrospective analysis, Geller et al5 found that frequent sunburns, high rates of tanning bed use, and low rates of sunscreen use were common among children of health care workers who reported a personal or family history of skin cancer. An independent study reported that merely 37% (37/100) of FDRs of melanoma patients use sunscreen more than half of the time, and considerably fewer wear protective clothing or seek shade while outdoors.6 Given their increased risk for developing melanoma, it is likely to be assumed that FDRs of melanoma patients practice diligent sun protection. The underlying reasons for the failure of this at-risk population to adhere strongly to sun protection practices warrants special attention.
Manne et al7 conducted a survey in a group of FDRs of melanoma patients with self-reported poor sun protection practices to evaluate the demographic, medical, psychological, educational (knowledge of sun protection guidelines), and social influences that correlate with sun protection and sunbathing practices. More effective sun protective behaviors were identified in FDRs with higher education, fewer perceived benefits of sunbathing, more prominent photoaging concerns, and greater sunscreen self-efficacy. The authors concluded that sun-protective behavior in FDRs was not associated with prior knowledge about sunscreen or UV exposure, their relative’s melanoma stage, or physician recommendations for sun protection.7
Factors that have been documented as influencing sun-protective behavior in the general population include knowledge of the benefits of sun protection; attitudes toward tanning and sun protection; subjective norms regarding the beauty and perceived health of a tan; and optimistic bias, which is a cognitive mechanism that causes a person to believe that he/she is at lesser risk for experiencing a negative outcome compared to others. Additionally, sun protection behaviors are influenced by the immediacy of getting the reward (the perceived benefits of tanning) versus the delayed punishment (development of skin cancer).6 Although all of these elements may be important for some individuals, we believe that a subset of FDRs of melanoma patients may be susceptible to the phenomenon known as counterphobia.
Counterphobia is a neurotic response to anxiety in which an individual actively pursues situations that heighten his/her fear rather than fleeing from a feared object or behavior.8 Most insight into counterphobia has come from the experiences of children who have parent(s) with a debilitating or fatal diagnosis. Due to their immature coping mechanisms, some children are at risk for maladaptive behavioral responses. The loss of a parent typically produces severe psychological trauma in all children, but in those who develop counterphobia, it manifests as a heightened fear of death and vulnerability to their parent’s illness. This maladaptive response is dependent on self-identification with the parent, especially among daughters of lost mothers and sons of lost fathers, and this fear remains with the child through adulthood. A survey of 154 motherless daughters found that women aged 19 to 35 years have the highest level of obsessive thoughts of mortality and more than 75% believe they will succumb to their mother’s illness (92% in the case of cancer).9 Despite this fear, children may exhibit health-compromising behaviors related to the diagnoses that led to their parents’ deaths; for example, counterphobia has been identified as a pathologic factor behind sexually promiscuous practices in the children of patients with AIDS, and it also may explain high-risk drinking behavior in a child whose parent died from hepatocellular carcinoma due to a history of alcoholic cirrhosis. Similarly, counterphobia can manifest as the deliberate refusal to undergo a mammogram in a woman whose mother died of breast cancer.9 Psychologists have hypothesized that counterphobic pursuits may result from attempts to master the anxiety associated with fear of injury or death as well as from the notion that attempts at risk-factor reduction are futile, as their death is certain.10
The strong influence of counterphobia on perspectives of health and mortality among individuals affected by early loss of a parent is well documented. An assessment of the subjective life expectancy, death anxiety, and health-related behaviors of college students who lost a parent revealed that these individuals estimated their own life spans to be shorter than college students with 2 living parents.11 Moreover, when students were explicitly instructed to predict their life expectancy based on a purely objective mentality rather than one influenced by personal feelings, the exclusion of emotion yielded a longer projected life span. This finding highlights the magnitude of the psychological forces influencing the ethos of individuals affected by premature parental loss. In the same study, individuals who had experienced early loss of a parent believed they would die of the same condition that caused their parent’s death, a finding accompanied by notably poorer diet and smoking behaviors, which might be expected among those with counterphobic defenses.11
Although Manne et al7 did not find an association between melanoma disease severity and sun-protective behavior in FDRs, the study design did not allow for assessment of potential counterphobic responses, which are most likely to develop in younger individuals who strongly identify with the family member whose disease was disabling or fatal. For example, the study included adult relatives (mean age, 46 years) of melanoma patients diagnosed in the preceding 4 years. Furthermore, fewer than 20% (108/545) of the patients had stage III or IV melanoma, and it was not known if melanoma patients communicated the diagnosis to their family members.7
A practice gap exists in FDRs of melanoma patients who are largely assumed to be practicing adequate, if not heightened, sun protection practices. Given that this group demonstrates poor sun protection practices, it is important to identify reasons for such behavior that may extend beyond what is currently known and may include counterphobia. Based on research performed in other medical conditions, the individuals most at risk for counterphobic responses are young children of patients diagnosed with a disabling or fatal condition, but whether in cases of melanoma counterphobia exists as a maladaptive response and whether such a response may occur in all close relatives, not just offspring, is unknown. Currently, the type of measure(s) that may mitigate poor risk factor modification due to counterphobia, including sun protection practices, is unknown. However, physician knowledge of counterphobic responses as a possibility in close relatives of melanoma patients may improve physician efforts to modify behavior in this unique, high-risk population.
The multimodal pathway of melanoma development suggests that individuals with an underlying genetic predisposition for melanoma who also neglect sun-protective measures are an especially high-risk group.12 As such, targeted education and screening of this patient population may be warranted (Table 1). Although it is incumbent on physicians to incorporate concerted screening, counseling, and focused interventions for newly diagnosed melanoma patients, taking similar measures to counsel and educate immediate relatives who may be at high risk for poor sun protection practices also is encouraged (Table 2).
We believe that recognition of counterphobic behavior is critical in the evaluation of FDRs of melanoma patients. Heightened awareness may bolster primary prevention efforts, especially in our patients with genetic diatheses toward melanoma development.
It is widely accepted that there are several factors that may independently elevate an individual’s risk for melanoma, such as a history of childhood sunburns, family history of melanoma, and poor sun protection practices. Several studies have examined risk behaviors in melanoma patients following their diagnosis and have reported findings such as increased UV exposure patterns, persistent tanning bed use, and sun-protective behaviors similar to those of the general population (Figure).1-4
Although first-degree relatives (FDRs) of melanoma patients are at an increased risk for melanoma, they also have been found to exhibit surprisingly poor sun protection practices. In one retrospective analysis, Geller et al5 found that frequent sunburns, high rates of tanning bed use, and low rates of sunscreen use were common among children of health care workers who reported a personal or family history of skin cancer. An independent study reported that merely 37% (37/100) of FDRs of melanoma patients use sunscreen more than half of the time, and considerably fewer wear protective clothing or seek shade while outdoors.6 Given their increased risk for developing melanoma, it is likely to be assumed that FDRs of melanoma patients practice diligent sun protection. The underlying reasons for the failure of this at-risk population to adhere strongly to sun protection practices warrants special attention.
Manne et al7 conducted a survey in a group of FDRs of melanoma patients with self-reported poor sun protection practices to evaluate the demographic, medical, psychological, educational (knowledge of sun protection guidelines), and social influences that correlate with sun protection and sunbathing practices. More effective sun protective behaviors were identified in FDRs with higher education, fewer perceived benefits of sunbathing, more prominent photoaging concerns, and greater sunscreen self-efficacy. The authors concluded that sun-protective behavior in FDRs was not associated with prior knowledge about sunscreen or UV exposure, their relative’s melanoma stage, or physician recommendations for sun protection.7
Factors that have been documented as influencing sun-protective behavior in the general population include knowledge of the benefits of sun protection; attitudes toward tanning and sun protection; subjective norms regarding the beauty and perceived health of a tan; and optimistic bias, which is a cognitive mechanism that causes a person to believe that he/she is at lesser risk for experiencing a negative outcome compared to others. Additionally, sun protection behaviors are influenced by the immediacy of getting the reward (the perceived benefits of tanning) versus the delayed punishment (development of skin cancer).6 Although all of these elements may be important for some individuals, we believe that a subset of FDRs of melanoma patients may be susceptible to the phenomenon known as counterphobia.
Counterphobia is a neurotic response to anxiety in which an individual actively pursues situations that heighten his/her fear rather than fleeing from a feared object or behavior.8 Most insight into counterphobia has come from the experiences of children who have parent(s) with a debilitating or fatal diagnosis. Due to their immature coping mechanisms, some children are at risk for maladaptive behavioral responses. The loss of a parent typically produces severe psychological trauma in all children, but in those who develop counterphobia, it manifests as a heightened fear of death and vulnerability to their parent’s illness. This maladaptive response is dependent on self-identification with the parent, especially among daughters of lost mothers and sons of lost fathers, and this fear remains with the child through adulthood. A survey of 154 motherless daughters found that women aged 19 to 35 years have the highest level of obsessive thoughts of mortality and more than 75% believe they will succumb to their mother’s illness (92% in the case of cancer).9 Despite this fear, children may exhibit health-compromising behaviors related to the diagnoses that led to their parents’ deaths; for example, counterphobia has been identified as a pathologic factor behind sexually promiscuous practices in the children of patients with AIDS, and it also may explain high-risk drinking behavior in a child whose parent died from hepatocellular carcinoma due to a history of alcoholic cirrhosis. Similarly, counterphobia can manifest as the deliberate refusal to undergo a mammogram in a woman whose mother died of breast cancer.9 Psychologists have hypothesized that counterphobic pursuits may result from attempts to master the anxiety associated with fear of injury or death as well as from the notion that attempts at risk-factor reduction are futile, as their death is certain.10
The strong influence of counterphobia on perspectives of health and mortality among individuals affected by early loss of a parent is well documented. An assessment of the subjective life expectancy, death anxiety, and health-related behaviors of college students who lost a parent revealed that these individuals estimated their own life spans to be shorter than college students with 2 living parents.11 Moreover, when students were explicitly instructed to predict their life expectancy based on a purely objective mentality rather than one influenced by personal feelings, the exclusion of emotion yielded a longer projected life span. This finding highlights the magnitude of the psychological forces influencing the ethos of individuals affected by premature parental loss. In the same study, individuals who had experienced early loss of a parent believed they would die of the same condition that caused their parent’s death, a finding accompanied by notably poorer diet and smoking behaviors, which might be expected among those with counterphobic defenses.11
Although Manne et al7 did not find an association between melanoma disease severity and sun-protective behavior in FDRs, the study design did not allow for assessment of potential counterphobic responses, which are most likely to develop in younger individuals who strongly identify with the family member whose disease was disabling or fatal. For example, the study included adult relatives (mean age, 46 years) of melanoma patients diagnosed in the preceding 4 years. Furthermore, fewer than 20% (108/545) of the patients had stage III or IV melanoma, and it was not known if melanoma patients communicated the diagnosis to their family members.7
A practice gap exists in FDRs of melanoma patients who are largely assumed to be practicing adequate, if not heightened, sun protection practices. Given that this group demonstrates poor sun protection practices, it is important to identify reasons for such behavior that may extend beyond what is currently known and may include counterphobia. Based on research performed in other medical conditions, the individuals most at risk for counterphobic responses are young children of patients diagnosed with a disabling or fatal condition, but whether in cases of melanoma counterphobia exists as a maladaptive response and whether such a response may occur in all close relatives, not just offspring, is unknown. Currently, the type of measure(s) that may mitigate poor risk factor modification due to counterphobia, including sun protection practices, is unknown. However, physician knowledge of counterphobic responses as a possibility in close relatives of melanoma patients may improve physician efforts to modify behavior in this unique, high-risk population.
The multimodal pathway of melanoma development suggests that individuals with an underlying genetic predisposition for melanoma who also neglect sun-protective measures are an especially high-risk group.12 As such, targeted education and screening of this patient population may be warranted (Table 1). Although it is incumbent on physicians to incorporate concerted screening, counseling, and focused interventions for newly diagnosed melanoma patients, taking similar measures to counsel and educate immediate relatives who may be at high risk for poor sun protection practices also is encouraged (Table 2).
We believe that recognition of counterphobic behavior is critical in the evaluation of FDRs of melanoma patients. Heightened awareness may bolster primary prevention efforts, especially in our patients with genetic diatheses toward melanoma development.
1. Idorn L, Datta P, Heydenreich J, et al. A 3-year follow-up of sun behavior in patients with cutaneous malignant melanoma [published online ahead of print October 2, 2013]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.5098.
2. Idorn LW, Datta P, Heydenreich J, et al. Sun behaviour after cutaneous malignant melanoma: a study based on ultraviolet radiation measurements and sun diary data [published online ahead of print]. Br J Dermatol. 2013;168:367-373.
3. Mayer D, Layman A, Carlson J. Sun-protection behaviors of melanoma survivors. J Am Acad Dermatol. 2012;66:e9-e10.
4. Lee TK, Brazier AS, Shoveller JA, et al. Sun-related behavior after a diagnosis of cutaneous malignant melanoma. Melanoma Res. 2007;17:51-55.
5. Geller AC, Brooks DR, Colditz GA, et al. Sun protection practices among offspring of women with personal or family history of skin cancer. Pediatrics. 2006;117:e688-e694.
6. Azzarello LM, Dessureault S, Jacobsen PB. Sun-protective behavior among individuals with a family history of melanoma. Cancer Epidemiol Boomarkers Prev. 2006;15:142-145.
7. Manne SL, Coups EJ, Jacobsen PB, et al. Sun protection and sunbathing practices among at-risk family members of patients with melanoma. BMC Public Health. 2011;11:122.
8. Fenichel O. The Psychoanalytic Theory of Neurosis. Oxford, United Kingdom: Taylor & Francis; 1999.
9. Edelman H. Motherless Daughters: The Legacy of Loss. 2nd ed. Cambridge, MA: Da Capo Press; 2006.
10. Poznanski E, Arthur B. The counterphobic defense in children. Child Psychiatry Hum Dev. 1971;1:178-191.
11. Denes-Raj V, Ehrlichman H. Effects of premature parental death on subjective life expectancy, death anxiety, and health behavior. Omega: Journal of Death and Dying. 1991;23:309-321.
12. Hayward NK. Genetics of melanoma predisposition. Oncogene. 2003;22:3053-3062.
13. Arthey S, Clarke VA. Suntanning and sun protection: a review of the psychologial literature. Soc Sci Med. 1995;40:265-274.
1. Idorn L, Datta P, Heydenreich J, et al. A 3-year follow-up of sun behavior in patients with cutaneous malignant melanoma [published online ahead of print October 2, 2013]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.5098.
2. Idorn LW, Datta P, Heydenreich J, et al. Sun behaviour after cutaneous malignant melanoma: a study based on ultraviolet radiation measurements and sun diary data [published online ahead of print]. Br J Dermatol. 2013;168:367-373.
3. Mayer D, Layman A, Carlson J. Sun-protection behaviors of melanoma survivors. J Am Acad Dermatol. 2012;66:e9-e10.
4. Lee TK, Brazier AS, Shoveller JA, et al. Sun-related behavior after a diagnosis of cutaneous malignant melanoma. Melanoma Res. 2007;17:51-55.
5. Geller AC, Brooks DR, Colditz GA, et al. Sun protection practices among offspring of women with personal or family history of skin cancer. Pediatrics. 2006;117:e688-e694.
6. Azzarello LM, Dessureault S, Jacobsen PB. Sun-protective behavior among individuals with a family history of melanoma. Cancer Epidemiol Boomarkers Prev. 2006;15:142-145.
7. Manne SL, Coups EJ, Jacobsen PB, et al. Sun protection and sunbathing practices among at-risk family members of patients with melanoma. BMC Public Health. 2011;11:122.
8. Fenichel O. The Psychoanalytic Theory of Neurosis. Oxford, United Kingdom: Taylor & Francis; 1999.
9. Edelman H. Motherless Daughters: The Legacy of Loss. 2nd ed. Cambridge, MA: Da Capo Press; 2006.
10. Poznanski E, Arthur B. The counterphobic defense in children. Child Psychiatry Hum Dev. 1971;1:178-191.
11. Denes-Raj V, Ehrlichman H. Effects of premature parental death on subjective life expectancy, death anxiety, and health behavior. Omega: Journal of Death and Dying. 1991;23:309-321.
12. Hayward NK. Genetics of melanoma predisposition. Oncogene. 2003;22:3053-3062.
13. Arthey S, Clarke VA. Suntanning and sun protection: a review of the psychologial literature. Soc Sci Med. 1995;40:265-274.