User login
When It Comes to Medicine, ‘Women Are Not Small Men’
Welcome everyone. I’m Dr. John White. I’m the chief medical officer at WebMD. Does your biologic sex impact your health? Does it have any play in how you’re diagnosed, how you’re treated in terms of what symptoms you have? Of course it does. We all know that. But that’s not something that many people believed 5, 10 years ago, certainly not 20 years ago. And it was only because of leaders like my guest today, Phyllis Greenberger, who really championed the need for research on women’s health. She has a new book out, which I love. It’s called Sex Cells: the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Please welcome my very good friend, Phyllis Greenberger.
Thank you.
Phyllis, It’s great to see you today.
It’s great to see you as well.
Now, you and I have been talking about this for easily 2 decades.
At least.
And some people think, oh, of course it makes sense. Although I saw you disagreeing that not everyone still believes that. But what has been that journey? Why has it been so hard to make people understand, as you point out early on in your book, women are not smaller men?
I think the basic reason was that it was just believed that men and women were the same except for their reproductive organs. So minus the reproductive organs, whether it was a device, a diagnostic, or therapeutic, if it was used and successful on a male, that it would be successful on a female. We’re really very far from understanding the differences, and there’s still a lot of distrust and disbelief and ignorance about it. And so there’s still a long way to go.
But you talk about that in the book, that there’s still a long way to go. Why is that? What’s the biggest obstacle? Is it just misinformation, lack of information? People don’t understand the science? There’s still resistance in some areas. Why is that?
I think it’s misinformation, and I gave a presentation, I don’t know how many years ago, at least 20 years ago, about the curriculum. And at the time, there was no women’s health in the curriculum. It was health. So if it was on cardiovascular issues or on osteoporosis, it was sort of the basic. And at the time, there would maybe be one woman whose job was women’s health, and she’d have an office, and otherwise there was nothing. And maybe they talked about breast cancer, who knows. But I spoke to someone just the other day, in view of all the attention that the book is getting now, whether that’s changed, whether it’s necessary and required. And she said it’s not. So, it’s not necessarily on the curriculum of all research and medical institutions, and even if women’s health, quote unquote, is on the curriculum, it doesn’t mean that they’re really looking at sex differences. And the difference is obvious. I mean, gender is really, it’s a social construct, but biological sex is how disease occurs and develops. And so if you’re not looking, and because there’s so little research now on sex differences that I don’t even know, I mean, how much you could actually teach.
So what needs to change? This book is a manifesto in many ways in how we need to include women; we need to make research more inclusive of everyone. But we’re not there yet. So what needs to change, Phyllis?
During this whole saga of trying to get people to listen to me and to the society, we really started out just looking at clinical trials and that, as you mentioned, I mean, there are issues in rural communities. There’s travel issues for women and child care. There’s a lot of disbelief or fear of clinical trials in some ethnicities. I do think, going to the future, that technology can help that. I mean, if people have broadband, which of course is also an issue in rural areas.
What could women do today? What should women listeners hear and then be doing? Should they be saying something to their doctor? Should they be asking specific questions? When they interact with the health care system, how can they make sure they’re getting the best care that’s appropriate for them when we know that sex cells matter?
Well, that’s a good question. It depends on, frankly, if your doctor is aware of this, if he or she has learned anything about this in school, which, I had already said, we’re not sure about that because research is still ongoing and there’s so much we don’t know. So I mean, you used to think, or I used to think, that you go to, you want a physician who’s older and more experienced. But now I think you should be going to a physician who’s younger and hopefully has learned about this, because the physicians that were educated years ago and have been practicing for 20, 30 years, I don’t know how much they know about this, whether they’re even aware of it.
Phyllis, you are a woman of action. You’ve lived in the DC area. You have championed legislative reforms, executive agendas. What do you want done now? What needs to be changed today? The curriculum is going to take time, but what else needs to change?
That’s a good question. I mean, if curriculum is going to take a while and you can ask your doctor if he prescribes the medication, whether it’s been tested on women, but then if it hasn’t been tested on women, but it’s the only thing that there is for your condition, I mean, so it’s very difficult. The Biden administration, as you know, just allocated a hundred million dollars for women’s health research.
What do you hope to accomplish with this book?
Well, what I’m hoping is that I spoke to someone at AMWA and I’m hoping — and AMWA is an association for women medical students. And I’m hoping that’s the audience. The audience needs to be. I mean, obviously everybody that I know that’s not a doctor that’s read it, found it fascinating and didn’t know a lot of the stuff that was in it. So I think it’s an interesting book anyway, and I think women should be aware of it. But really I think it needs to be for medical students.
And to your credit, you built the Society for Women’s Health Research into a powerful force in Washington under your tenure in really promoting the need for Office of Women’s Health and Research in general. The book is entitled Sex Cells, the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Phyllis Greenberger, thank you so much for all that you’ve done for women’s health, for women’s research. We wouldn’t be where we are today if it wasn’t for you. So thanks.
Thank you very much, John. Thank you. I appreciate the opportunity.
Dr. Whyte, is chief medical officer, WebMD, New York, NY. He has disclosed no relevant financial relationships. Ms. Greenberger is a women’s health advocate and author of “Sex Cells: The Fight to Overcome Bias and Discrimination in Women’s Healthcare”
This interview originally appeared on WebMD on May 23, 2024. A version of this article appeared on Medscape.com .
Welcome everyone. I’m Dr. John White. I’m the chief medical officer at WebMD. Does your biologic sex impact your health? Does it have any play in how you’re diagnosed, how you’re treated in terms of what symptoms you have? Of course it does. We all know that. But that’s not something that many people believed 5, 10 years ago, certainly not 20 years ago. And it was only because of leaders like my guest today, Phyllis Greenberger, who really championed the need for research on women’s health. She has a new book out, which I love. It’s called Sex Cells: the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Please welcome my very good friend, Phyllis Greenberger.
Thank you.
Phyllis, It’s great to see you today.
It’s great to see you as well.
Now, you and I have been talking about this for easily 2 decades.
At least.
And some people think, oh, of course it makes sense. Although I saw you disagreeing that not everyone still believes that. But what has been that journey? Why has it been so hard to make people understand, as you point out early on in your book, women are not smaller men?
I think the basic reason was that it was just believed that men and women were the same except for their reproductive organs. So minus the reproductive organs, whether it was a device, a diagnostic, or therapeutic, if it was used and successful on a male, that it would be successful on a female. We’re really very far from understanding the differences, and there’s still a lot of distrust and disbelief and ignorance about it. And so there’s still a long way to go.
But you talk about that in the book, that there’s still a long way to go. Why is that? What’s the biggest obstacle? Is it just misinformation, lack of information? People don’t understand the science? There’s still resistance in some areas. Why is that?
I think it’s misinformation, and I gave a presentation, I don’t know how many years ago, at least 20 years ago, about the curriculum. And at the time, there was no women’s health in the curriculum. It was health. So if it was on cardiovascular issues or on osteoporosis, it was sort of the basic. And at the time, there would maybe be one woman whose job was women’s health, and she’d have an office, and otherwise there was nothing. And maybe they talked about breast cancer, who knows. But I spoke to someone just the other day, in view of all the attention that the book is getting now, whether that’s changed, whether it’s necessary and required. And she said it’s not. So, it’s not necessarily on the curriculum of all research and medical institutions, and even if women’s health, quote unquote, is on the curriculum, it doesn’t mean that they’re really looking at sex differences. And the difference is obvious. I mean, gender is really, it’s a social construct, but biological sex is how disease occurs and develops. And so if you’re not looking, and because there’s so little research now on sex differences that I don’t even know, I mean, how much you could actually teach.
So what needs to change? This book is a manifesto in many ways in how we need to include women; we need to make research more inclusive of everyone. But we’re not there yet. So what needs to change, Phyllis?
During this whole saga of trying to get people to listen to me and to the society, we really started out just looking at clinical trials and that, as you mentioned, I mean, there are issues in rural communities. There’s travel issues for women and child care. There’s a lot of disbelief or fear of clinical trials in some ethnicities. I do think, going to the future, that technology can help that. I mean, if people have broadband, which of course is also an issue in rural areas.
What could women do today? What should women listeners hear and then be doing? Should they be saying something to their doctor? Should they be asking specific questions? When they interact with the health care system, how can they make sure they’re getting the best care that’s appropriate for them when we know that sex cells matter?
Well, that’s a good question. It depends on, frankly, if your doctor is aware of this, if he or she has learned anything about this in school, which, I had already said, we’re not sure about that because research is still ongoing and there’s so much we don’t know. So I mean, you used to think, or I used to think, that you go to, you want a physician who’s older and more experienced. But now I think you should be going to a physician who’s younger and hopefully has learned about this, because the physicians that were educated years ago and have been practicing for 20, 30 years, I don’t know how much they know about this, whether they’re even aware of it.
Phyllis, you are a woman of action. You’ve lived in the DC area. You have championed legislative reforms, executive agendas. What do you want done now? What needs to be changed today? The curriculum is going to take time, but what else needs to change?
That’s a good question. I mean, if curriculum is going to take a while and you can ask your doctor if he prescribes the medication, whether it’s been tested on women, but then if it hasn’t been tested on women, but it’s the only thing that there is for your condition, I mean, so it’s very difficult. The Biden administration, as you know, just allocated a hundred million dollars for women’s health research.
What do you hope to accomplish with this book?
Well, what I’m hoping is that I spoke to someone at AMWA and I’m hoping — and AMWA is an association for women medical students. And I’m hoping that’s the audience. The audience needs to be. I mean, obviously everybody that I know that’s not a doctor that’s read it, found it fascinating and didn’t know a lot of the stuff that was in it. So I think it’s an interesting book anyway, and I think women should be aware of it. But really I think it needs to be for medical students.
And to your credit, you built the Society for Women’s Health Research into a powerful force in Washington under your tenure in really promoting the need for Office of Women’s Health and Research in general. The book is entitled Sex Cells, the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Phyllis Greenberger, thank you so much for all that you’ve done for women’s health, for women’s research. We wouldn’t be where we are today if it wasn’t for you. So thanks.
Thank you very much, John. Thank you. I appreciate the opportunity.
Dr. Whyte, is chief medical officer, WebMD, New York, NY. He has disclosed no relevant financial relationships. Ms. Greenberger is a women’s health advocate and author of “Sex Cells: The Fight to Overcome Bias and Discrimination in Women’s Healthcare”
This interview originally appeared on WebMD on May 23, 2024. A version of this article appeared on Medscape.com .
Welcome everyone. I’m Dr. John White. I’m the chief medical officer at WebMD. Does your biologic sex impact your health? Does it have any play in how you’re diagnosed, how you’re treated in terms of what symptoms you have? Of course it does. We all know that. But that’s not something that many people believed 5, 10 years ago, certainly not 20 years ago. And it was only because of leaders like my guest today, Phyllis Greenberger, who really championed the need for research on women’s health. She has a new book out, which I love. It’s called Sex Cells: the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Please welcome my very good friend, Phyllis Greenberger.
Thank you.
Phyllis, It’s great to see you today.
It’s great to see you as well.
Now, you and I have been talking about this for easily 2 decades.
At least.
And some people think, oh, of course it makes sense. Although I saw you disagreeing that not everyone still believes that. But what has been that journey? Why has it been so hard to make people understand, as you point out early on in your book, women are not smaller men?
I think the basic reason was that it was just believed that men and women were the same except for their reproductive organs. So minus the reproductive organs, whether it was a device, a diagnostic, or therapeutic, if it was used and successful on a male, that it would be successful on a female. We’re really very far from understanding the differences, and there’s still a lot of distrust and disbelief and ignorance about it. And so there’s still a long way to go.
But you talk about that in the book, that there’s still a long way to go. Why is that? What’s the biggest obstacle? Is it just misinformation, lack of information? People don’t understand the science? There’s still resistance in some areas. Why is that?
I think it’s misinformation, and I gave a presentation, I don’t know how many years ago, at least 20 years ago, about the curriculum. And at the time, there was no women’s health in the curriculum. It was health. So if it was on cardiovascular issues or on osteoporosis, it was sort of the basic. And at the time, there would maybe be one woman whose job was women’s health, and she’d have an office, and otherwise there was nothing. And maybe they talked about breast cancer, who knows. But I spoke to someone just the other day, in view of all the attention that the book is getting now, whether that’s changed, whether it’s necessary and required. And she said it’s not. So, it’s not necessarily on the curriculum of all research and medical institutions, and even if women’s health, quote unquote, is on the curriculum, it doesn’t mean that they’re really looking at sex differences. And the difference is obvious. I mean, gender is really, it’s a social construct, but biological sex is how disease occurs and develops. And so if you’re not looking, and because there’s so little research now on sex differences that I don’t even know, I mean, how much you could actually teach.
So what needs to change? This book is a manifesto in many ways in how we need to include women; we need to make research more inclusive of everyone. But we’re not there yet. So what needs to change, Phyllis?
During this whole saga of trying to get people to listen to me and to the society, we really started out just looking at clinical trials and that, as you mentioned, I mean, there are issues in rural communities. There’s travel issues for women and child care. There’s a lot of disbelief or fear of clinical trials in some ethnicities. I do think, going to the future, that technology can help that. I mean, if people have broadband, which of course is also an issue in rural areas.
What could women do today? What should women listeners hear and then be doing? Should they be saying something to their doctor? Should they be asking specific questions? When they interact with the health care system, how can they make sure they’re getting the best care that’s appropriate for them when we know that sex cells matter?
Well, that’s a good question. It depends on, frankly, if your doctor is aware of this, if he or she has learned anything about this in school, which, I had already said, we’re not sure about that because research is still ongoing and there’s so much we don’t know. So I mean, you used to think, or I used to think, that you go to, you want a physician who’s older and more experienced. But now I think you should be going to a physician who’s younger and hopefully has learned about this, because the physicians that were educated years ago and have been practicing for 20, 30 years, I don’t know how much they know about this, whether they’re even aware of it.
Phyllis, you are a woman of action. You’ve lived in the DC area. You have championed legislative reforms, executive agendas. What do you want done now? What needs to be changed today? The curriculum is going to take time, but what else needs to change?
That’s a good question. I mean, if curriculum is going to take a while and you can ask your doctor if he prescribes the medication, whether it’s been tested on women, but then if it hasn’t been tested on women, but it’s the only thing that there is for your condition, I mean, so it’s very difficult. The Biden administration, as you know, just allocated a hundred million dollars for women’s health research.
What do you hope to accomplish with this book?
Well, what I’m hoping is that I spoke to someone at AMWA and I’m hoping — and AMWA is an association for women medical students. And I’m hoping that’s the audience. The audience needs to be. I mean, obviously everybody that I know that’s not a doctor that’s read it, found it fascinating and didn’t know a lot of the stuff that was in it. So I think it’s an interesting book anyway, and I think women should be aware of it. But really I think it needs to be for medical students.
And to your credit, you built the Society for Women’s Health Research into a powerful force in Washington under your tenure in really promoting the need for Office of Women’s Health and Research in general. The book is entitled Sex Cells, the Fight to Overcome Bias and Discrimination in Women’s Healthcare. Phyllis Greenberger, thank you so much for all that you’ve done for women’s health, for women’s research. We wouldn’t be where we are today if it wasn’t for you. So thanks.
Thank you very much, John. Thank you. I appreciate the opportunity.
Dr. Whyte, is chief medical officer, WebMD, New York, NY. He has disclosed no relevant financial relationships. Ms. Greenberger is a women’s health advocate and author of “Sex Cells: The Fight to Overcome Bias and Discrimination in Women’s Healthcare”
This interview originally appeared on WebMD on May 23, 2024. A version of this article appeared on Medscape.com .
The 5-year survival rate for pancreatic cancer is increasing
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
ESMO’s new focus on cancer prevention
This transcript has been edited for clarity.
John Whyte, MD: Welcome, everyone. I’m Dr John Whyte. I’m the chief medical officer at WebMD, and I’m joined today by Fabrice André. He is the chair of the scientific committee at the European Society for Medical Oncology, where we are today in Paris, France. Bonjour, Fabrice.
So, remind our viewers: What is ESMO? What does it do? And why is it so important?
Fabrice André, MD, PhD: First ESMO, is a scientific society – a member-based organization with around 25,000 members.
Dr. Whyte: Equivalent to ASCO (American Society of Clinical Oncology) in the United States, correct?
Dr. André: It has members worldwide, from all over the world. And it aims at disseminating science, educating. The name is European, so it has some roots in Europe; but it is really a global organization for education, dissemination, and also more and more to generate frameworks for the standards of treatment and the common terminology for healthcare professionals to better care for patients.
Dr. Whyte: What are you most excited by at this conference in terms of the innovations that are being discussed?
Dr. André: Today we are at ESMO 2022 in Paris, with 28,000 people registered and the vast majority on site, and what has been the editorial line – the tagline – for the scientific committee is “understand the disease to better treat the patient.” This is extremely important; What are the determinants of outcomes if we want to integrate all the wealth of innovation that is coming?
So, then, what are the new things? In the Presidential Symposium, where we usually have the very new things, we will have very important presentations on the role of pollution on cancer and the biological mechanism that induces cancer. Why is it important? First, it has impact on public health. But also, it’s important because, for us, it’s raising the signal that the oncology community must start to invest in this field of prevention.
Dr. Whyte: I was at your booth, by the way, the ESMO booth here, and you have two bicycles, which impressed me. Nobody was on them, I might point out, but the focus was on prevention. But let’s also address how historically, the academic community, the scientific community hasn’t really been focused on prevention. It’s about treatment. So it’s fascinating that you’re talking about prevention, because usually we talk about precision medicine, right? We talk about checkpoint inhibitors; we talk about immunomodulators. And here you’re saying, “Hey, John, we need to understand how we prevent cancer,” which is really a misnomer in a way, because there are many different diseases. Would you agree with that?
Dr. André: I fully agree with you. But what is the premise we are trying to address here? The premise is that prevention has always been very low in the agenda of international conferences. And we think we want to give the signal that it’s really time now that clinical infrastructure, hospitals, invest in this field, create teams dedicated to prevention, new structures for prevention. Why? Because we are discovering step by step that it could be that some drugs we use for patients with cancer could also be developed in the field of prevention. And for this, we need the oncologists. So, more and more, our conviction is that it is the oncology community that will transform the field of prevention, and we need to invest now. Having said that, we have two very important abstracts on this question. The other one is about early cancer detection. But of course, we have our traditional session on immunotherapeutics, precision medicine, and all the wealth of randomized trials. And so in this field, for patients with cancer, what is the new information?
Dr. Whyte: We have this whole continuum. So you talk about prevention – how much cancer is preventable? Eighty percent? Seventy percent? What do you estimate?
Dr. André: You know, I’m also a scientist. So as a scientist, I will say that there is no limit for this question. No, the only limit is the knowledge.
Dr. Whyte: Well, there is some inherited mutation, so we do know that.
Dr. André: We can just go to the current status – what we know now – but I don’t see why we would put some limit on how much we can prevent cancer. But indeed, so far, what are the risk factors? Genetics, hereditary cancer, all habits, and we know them. It’s about tobacco, alcohol, sun, some sexual behavior, etc., that indeed account. In France, we say that around 40% of cancer could be preventable.
Dr. Whyte: More and more, we learn about the issues of gout, other inflammatory diseases; it can have an association, but then we have early screening as well. So, if we’re on this continuum, how excited are you by what’s happening with liquid biopsies, with other testing? Because if we can get a cancer instead of at 500,000 cells at the time of imaging, at 10 or 50 cells, while there are fragments, that’s revolutionary, isn’t it?
Dr. André: I fully agree with you. We will have an important trial presented during ESMO that is the first prospective trial testing the device called Galleri, a tool for early cancer detection based on ctDNA (circulating tumor DNA) analysis by methylation pattern.
Dr. Whyte: General screening of the population or a more tailored population with certain indications? Because right now, most of those have focused on a limited population or are used for patients who already have a cancer, and testing that way – you think it’s going to be broader?
Dr. André: What this trial is investigating is in participants who do not have cancer, 6,000 participants ...
Dr. Whyte: Pas de tout? No cancer at all?
Dr. André: No cancer.
Dr. Whyte: No family history?
Dr. André: They can have family history, but no detectable cancer – can ctDNA analysis detect cancer? And the answer is, indeed, there is around 1% positivity, and around 40% of them, indeed, had cancer. So why is it important? Because it’s really a landmark prospective trial that is telling us that a device based on ctDNA can detect cancer at early stage. Then, how many cancers? What percentage?
Dr. Whyte: Which type of cancer?
Dr. André: And is it going to have an impact on outcome? And for all the questions, we don’t have the answer here. But the answer we have here today is that with this device, done prospectively, you can detect some cancer that would not be detectable without symptoms.
Dr. Whyte: It’s only going to get better, too.
Dr. André: Yeah. So then the next step is improving technology, integrating this technology with other ones we already have, in order to increase the percentage of patients in which we detect cancer at an earlier stage.
Dr. Whyte: What about pancreatic cancer, cancers we can’t detect through screening? People forget that most cancers cannot be detected through screening, so we need better tools. We do know that there are inherited mutations. Those really aren’t preventable in many ways; the goal is to get them early. So then we move to treatments, and you talked about precision medicine. What excites you about what’s going on these days at ESMO right now.
Dr. André: We have many trials on precision medicine. We will have two randomized trials that investigate two new targets; one is gamma secretase inhibitor. So, it’s a first-in-class, first time we even hear about this target at a clinical conference. And the second highly expected trial is a clinical trial in patients with metastatic lung cancer, KRAS mutated, testing sotorasib, which is a KRAS inhibitor, and showing the magnitude of improvement associated with sotorasib. The trial is positive, and it improved PFS [progression-free survival] in these patients. So these are two new targets that are validated at this conference.
Then, if we go on another topic of genomics, there is a question that is extremely important: Can we define patients who present an outlier sensitivity to immunotherapeutics? There will be one trial presented in the Presidential Symposium of immunotherapeutics in patients with colon cancer and microsatellite instability (MSI), showing that a few weeks of immunotherapeutics followed by surgery can cure patients. Why is it important? It’s important because we are all facing a shortage in the healthcare workforce. We have fewer nurses, fewer doctors, and we all have issues of sustainability. So, really now is the time to think about precision medicine, how precision medicine, by identifying outlier responders, can decrease the amount of resources we need to cure a patient. And this trial on immunotherapeutics, guided by genomics, is exactly this point: 8 weeks of treatment to cure a patient.
Dr. Whyte: Do you think there’s going to be a cure for cancer 10 years from now?
Dr. André: What I’m convinced of is that, in the 10 years that are coming, we are going step by step; we’re going to continue to increase the life expectancy of patients with cancer.
Dr. Whyte: And quality of life too, right?
Dr. André: Quality of life is a major issue. We had today a keynote on digital medicine and how ePRO (electronic patient-reported outcomes) can help the patient to really decrease the burden of symptoms. Quality of life is, of course, extremely important because of the very high number of patients who are cured of cancer; we need to decrease the burden of symptom in patients.
Dr. Whyte: And even though cancer rates are going down in most areas of the world, we still globally have millions of deaths from cancer every year. And sometimes people forget that, because they hear about some of the innovations. But I want to end with this: Are we investing enough in cancer care? Because let’s be honest – there are other diseases that we also need to spend time on. Cardiovascular disease is a global burden; infectious disease is a global burden. Are governments, are industries spending enough on cancer research and development?
Dr. André: Well, we can always claim for more, no? This is how everyone is trying to be, I think. But the reality is that we are living in a world where we have limited resources. I think what is more important for me is to be sure that any euro or dollar invested in cancer research is well used and generates an impact for patients. That is the most important, I think.
Dr. Whyte: And that’s why outcomes are so important in this research.
Dr. André: My conviction is that we have the tools, meaning the knowledge, the biotechnology, to really go the next step in terms of improving outcomes for patients. And for this, we now need clinical trials and translational research, but the tools, meaning basic science, basic knowledge, biotechnology – the basement for progress is here. We need now to transform this into direct impact for the patient. But I would not like to finish by saying we need more money in the field; what we need are people who can transform one euro, one dollar into concrete and measurable advances.
Dr. Whyte: We’re going to need more time on another day because I want to ask you about diversity in clinical trials, how important that is. I want to ask you about pediatric cancers; there are a whole bunch of things that I want to talk to you about. So hopefully we’ll find more time when we’re not at a big international conference such as ESMO. So, Dr Fabrice André, I want to thank you for taking time today.
Dr. André: Thank you and have a nice day.
Dr. Whyte: Stay tuned for a future discussion with Dr André on more about where we’re going in terms of cancer research and development. Thanks for watching, everyone.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
John Whyte, MD: Welcome, everyone. I’m Dr John Whyte. I’m the chief medical officer at WebMD, and I’m joined today by Fabrice André. He is the chair of the scientific committee at the European Society for Medical Oncology, where we are today in Paris, France. Bonjour, Fabrice.
So, remind our viewers: What is ESMO? What does it do? And why is it so important?
Fabrice André, MD, PhD: First ESMO, is a scientific society – a member-based organization with around 25,000 members.
Dr. Whyte: Equivalent to ASCO (American Society of Clinical Oncology) in the United States, correct?
Dr. André: It has members worldwide, from all over the world. And it aims at disseminating science, educating. The name is European, so it has some roots in Europe; but it is really a global organization for education, dissemination, and also more and more to generate frameworks for the standards of treatment and the common terminology for healthcare professionals to better care for patients.
Dr. Whyte: What are you most excited by at this conference in terms of the innovations that are being discussed?
Dr. André: Today we are at ESMO 2022 in Paris, with 28,000 people registered and the vast majority on site, and what has been the editorial line – the tagline – for the scientific committee is “understand the disease to better treat the patient.” This is extremely important; What are the determinants of outcomes if we want to integrate all the wealth of innovation that is coming?
So, then, what are the new things? In the Presidential Symposium, where we usually have the very new things, we will have very important presentations on the role of pollution on cancer and the biological mechanism that induces cancer. Why is it important? First, it has impact on public health. But also, it’s important because, for us, it’s raising the signal that the oncology community must start to invest in this field of prevention.
Dr. Whyte: I was at your booth, by the way, the ESMO booth here, and you have two bicycles, which impressed me. Nobody was on them, I might point out, but the focus was on prevention. But let’s also address how historically, the academic community, the scientific community hasn’t really been focused on prevention. It’s about treatment. So it’s fascinating that you’re talking about prevention, because usually we talk about precision medicine, right? We talk about checkpoint inhibitors; we talk about immunomodulators. And here you’re saying, “Hey, John, we need to understand how we prevent cancer,” which is really a misnomer in a way, because there are many different diseases. Would you agree with that?
Dr. André: I fully agree with you. But what is the premise we are trying to address here? The premise is that prevention has always been very low in the agenda of international conferences. And we think we want to give the signal that it’s really time now that clinical infrastructure, hospitals, invest in this field, create teams dedicated to prevention, new structures for prevention. Why? Because we are discovering step by step that it could be that some drugs we use for patients with cancer could also be developed in the field of prevention. And for this, we need the oncologists. So, more and more, our conviction is that it is the oncology community that will transform the field of prevention, and we need to invest now. Having said that, we have two very important abstracts on this question. The other one is about early cancer detection. But of course, we have our traditional session on immunotherapeutics, precision medicine, and all the wealth of randomized trials. And so in this field, for patients with cancer, what is the new information?
Dr. Whyte: We have this whole continuum. So you talk about prevention – how much cancer is preventable? Eighty percent? Seventy percent? What do you estimate?
Dr. André: You know, I’m also a scientist. So as a scientist, I will say that there is no limit for this question. No, the only limit is the knowledge.
Dr. Whyte: Well, there is some inherited mutation, so we do know that.
Dr. André: We can just go to the current status – what we know now – but I don’t see why we would put some limit on how much we can prevent cancer. But indeed, so far, what are the risk factors? Genetics, hereditary cancer, all habits, and we know them. It’s about tobacco, alcohol, sun, some sexual behavior, etc., that indeed account. In France, we say that around 40% of cancer could be preventable.
Dr. Whyte: More and more, we learn about the issues of gout, other inflammatory diseases; it can have an association, but then we have early screening as well. So, if we’re on this continuum, how excited are you by what’s happening with liquid biopsies, with other testing? Because if we can get a cancer instead of at 500,000 cells at the time of imaging, at 10 or 50 cells, while there are fragments, that’s revolutionary, isn’t it?
Dr. André: I fully agree with you. We will have an important trial presented during ESMO that is the first prospective trial testing the device called Galleri, a tool for early cancer detection based on ctDNA (circulating tumor DNA) analysis by methylation pattern.
Dr. Whyte: General screening of the population or a more tailored population with certain indications? Because right now, most of those have focused on a limited population or are used for patients who already have a cancer, and testing that way – you think it’s going to be broader?
Dr. André: What this trial is investigating is in participants who do not have cancer, 6,000 participants ...
Dr. Whyte: Pas de tout? No cancer at all?
Dr. André: No cancer.
Dr. Whyte: No family history?
Dr. André: They can have family history, but no detectable cancer – can ctDNA analysis detect cancer? And the answer is, indeed, there is around 1% positivity, and around 40% of them, indeed, had cancer. So why is it important? Because it’s really a landmark prospective trial that is telling us that a device based on ctDNA can detect cancer at early stage. Then, how many cancers? What percentage?
Dr. Whyte: Which type of cancer?
Dr. André: And is it going to have an impact on outcome? And for all the questions, we don’t have the answer here. But the answer we have here today is that with this device, done prospectively, you can detect some cancer that would not be detectable without symptoms.
Dr. Whyte: It’s only going to get better, too.
Dr. André: Yeah. So then the next step is improving technology, integrating this technology with other ones we already have, in order to increase the percentage of patients in which we detect cancer at an earlier stage.
Dr. Whyte: What about pancreatic cancer, cancers we can’t detect through screening? People forget that most cancers cannot be detected through screening, so we need better tools. We do know that there are inherited mutations. Those really aren’t preventable in many ways; the goal is to get them early. So then we move to treatments, and you talked about precision medicine. What excites you about what’s going on these days at ESMO right now.
Dr. André: We have many trials on precision medicine. We will have two randomized trials that investigate two new targets; one is gamma secretase inhibitor. So, it’s a first-in-class, first time we even hear about this target at a clinical conference. And the second highly expected trial is a clinical trial in patients with metastatic lung cancer, KRAS mutated, testing sotorasib, which is a KRAS inhibitor, and showing the magnitude of improvement associated with sotorasib. The trial is positive, and it improved PFS [progression-free survival] in these patients. So these are two new targets that are validated at this conference.
Then, if we go on another topic of genomics, there is a question that is extremely important: Can we define patients who present an outlier sensitivity to immunotherapeutics? There will be one trial presented in the Presidential Symposium of immunotherapeutics in patients with colon cancer and microsatellite instability (MSI), showing that a few weeks of immunotherapeutics followed by surgery can cure patients. Why is it important? It’s important because we are all facing a shortage in the healthcare workforce. We have fewer nurses, fewer doctors, and we all have issues of sustainability. So, really now is the time to think about precision medicine, how precision medicine, by identifying outlier responders, can decrease the amount of resources we need to cure a patient. And this trial on immunotherapeutics, guided by genomics, is exactly this point: 8 weeks of treatment to cure a patient.
Dr. Whyte: Do you think there’s going to be a cure for cancer 10 years from now?
Dr. André: What I’m convinced of is that, in the 10 years that are coming, we are going step by step; we’re going to continue to increase the life expectancy of patients with cancer.
Dr. Whyte: And quality of life too, right?
Dr. André: Quality of life is a major issue. We had today a keynote on digital medicine and how ePRO (electronic patient-reported outcomes) can help the patient to really decrease the burden of symptoms. Quality of life is, of course, extremely important because of the very high number of patients who are cured of cancer; we need to decrease the burden of symptom in patients.
Dr. Whyte: And even though cancer rates are going down in most areas of the world, we still globally have millions of deaths from cancer every year. And sometimes people forget that, because they hear about some of the innovations. But I want to end with this: Are we investing enough in cancer care? Because let’s be honest – there are other diseases that we also need to spend time on. Cardiovascular disease is a global burden; infectious disease is a global burden. Are governments, are industries spending enough on cancer research and development?
Dr. André: Well, we can always claim for more, no? This is how everyone is trying to be, I think. But the reality is that we are living in a world where we have limited resources. I think what is more important for me is to be sure that any euro or dollar invested in cancer research is well used and generates an impact for patients. That is the most important, I think.
Dr. Whyte: And that’s why outcomes are so important in this research.
Dr. André: My conviction is that we have the tools, meaning the knowledge, the biotechnology, to really go the next step in terms of improving outcomes for patients. And for this, we now need clinical trials and translational research, but the tools, meaning basic science, basic knowledge, biotechnology – the basement for progress is here. We need now to transform this into direct impact for the patient. But I would not like to finish by saying we need more money in the field; what we need are people who can transform one euro, one dollar into concrete and measurable advances.
Dr. Whyte: We’re going to need more time on another day because I want to ask you about diversity in clinical trials, how important that is. I want to ask you about pediatric cancers; there are a whole bunch of things that I want to talk to you about. So hopefully we’ll find more time when we’re not at a big international conference such as ESMO. So, Dr Fabrice André, I want to thank you for taking time today.
Dr. André: Thank you and have a nice day.
Dr. Whyte: Stay tuned for a future discussion with Dr André on more about where we’re going in terms of cancer research and development. Thanks for watching, everyone.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
John Whyte, MD: Welcome, everyone. I’m Dr John Whyte. I’m the chief medical officer at WebMD, and I’m joined today by Fabrice André. He is the chair of the scientific committee at the European Society for Medical Oncology, where we are today in Paris, France. Bonjour, Fabrice.
So, remind our viewers: What is ESMO? What does it do? And why is it so important?
Fabrice André, MD, PhD: First ESMO, is a scientific society – a member-based organization with around 25,000 members.
Dr. Whyte: Equivalent to ASCO (American Society of Clinical Oncology) in the United States, correct?
Dr. André: It has members worldwide, from all over the world. And it aims at disseminating science, educating. The name is European, so it has some roots in Europe; but it is really a global organization for education, dissemination, and also more and more to generate frameworks for the standards of treatment and the common terminology for healthcare professionals to better care for patients.
Dr. Whyte: What are you most excited by at this conference in terms of the innovations that are being discussed?
Dr. André: Today we are at ESMO 2022 in Paris, with 28,000 people registered and the vast majority on site, and what has been the editorial line – the tagline – for the scientific committee is “understand the disease to better treat the patient.” This is extremely important; What are the determinants of outcomes if we want to integrate all the wealth of innovation that is coming?
So, then, what are the new things? In the Presidential Symposium, where we usually have the very new things, we will have very important presentations on the role of pollution on cancer and the biological mechanism that induces cancer. Why is it important? First, it has impact on public health. But also, it’s important because, for us, it’s raising the signal that the oncology community must start to invest in this field of prevention.
Dr. Whyte: I was at your booth, by the way, the ESMO booth here, and you have two bicycles, which impressed me. Nobody was on them, I might point out, but the focus was on prevention. But let’s also address how historically, the academic community, the scientific community hasn’t really been focused on prevention. It’s about treatment. So it’s fascinating that you’re talking about prevention, because usually we talk about precision medicine, right? We talk about checkpoint inhibitors; we talk about immunomodulators. And here you’re saying, “Hey, John, we need to understand how we prevent cancer,” which is really a misnomer in a way, because there are many different diseases. Would you agree with that?
Dr. André: I fully agree with you. But what is the premise we are trying to address here? The premise is that prevention has always been very low in the agenda of international conferences. And we think we want to give the signal that it’s really time now that clinical infrastructure, hospitals, invest in this field, create teams dedicated to prevention, new structures for prevention. Why? Because we are discovering step by step that it could be that some drugs we use for patients with cancer could also be developed in the field of prevention. And for this, we need the oncologists. So, more and more, our conviction is that it is the oncology community that will transform the field of prevention, and we need to invest now. Having said that, we have two very important abstracts on this question. The other one is about early cancer detection. But of course, we have our traditional session on immunotherapeutics, precision medicine, and all the wealth of randomized trials. And so in this field, for patients with cancer, what is the new information?
Dr. Whyte: We have this whole continuum. So you talk about prevention – how much cancer is preventable? Eighty percent? Seventy percent? What do you estimate?
Dr. André: You know, I’m also a scientist. So as a scientist, I will say that there is no limit for this question. No, the only limit is the knowledge.
Dr. Whyte: Well, there is some inherited mutation, so we do know that.
Dr. André: We can just go to the current status – what we know now – but I don’t see why we would put some limit on how much we can prevent cancer. But indeed, so far, what are the risk factors? Genetics, hereditary cancer, all habits, and we know them. It’s about tobacco, alcohol, sun, some sexual behavior, etc., that indeed account. In France, we say that around 40% of cancer could be preventable.
Dr. Whyte: More and more, we learn about the issues of gout, other inflammatory diseases; it can have an association, but then we have early screening as well. So, if we’re on this continuum, how excited are you by what’s happening with liquid biopsies, with other testing? Because if we can get a cancer instead of at 500,000 cells at the time of imaging, at 10 or 50 cells, while there are fragments, that’s revolutionary, isn’t it?
Dr. André: I fully agree with you. We will have an important trial presented during ESMO that is the first prospective trial testing the device called Galleri, a tool for early cancer detection based on ctDNA (circulating tumor DNA) analysis by methylation pattern.
Dr. Whyte: General screening of the population or a more tailored population with certain indications? Because right now, most of those have focused on a limited population or are used for patients who already have a cancer, and testing that way – you think it’s going to be broader?
Dr. André: What this trial is investigating is in participants who do not have cancer, 6,000 participants ...
Dr. Whyte: Pas de tout? No cancer at all?
Dr. André: No cancer.
Dr. Whyte: No family history?
Dr. André: They can have family history, but no detectable cancer – can ctDNA analysis detect cancer? And the answer is, indeed, there is around 1% positivity, and around 40% of them, indeed, had cancer. So why is it important? Because it’s really a landmark prospective trial that is telling us that a device based on ctDNA can detect cancer at early stage. Then, how many cancers? What percentage?
Dr. Whyte: Which type of cancer?
Dr. André: And is it going to have an impact on outcome? And for all the questions, we don’t have the answer here. But the answer we have here today is that with this device, done prospectively, you can detect some cancer that would not be detectable without symptoms.
Dr. Whyte: It’s only going to get better, too.
Dr. André: Yeah. So then the next step is improving technology, integrating this technology with other ones we already have, in order to increase the percentage of patients in which we detect cancer at an earlier stage.
Dr. Whyte: What about pancreatic cancer, cancers we can’t detect through screening? People forget that most cancers cannot be detected through screening, so we need better tools. We do know that there are inherited mutations. Those really aren’t preventable in many ways; the goal is to get them early. So then we move to treatments, and you talked about precision medicine. What excites you about what’s going on these days at ESMO right now.
Dr. André: We have many trials on precision medicine. We will have two randomized trials that investigate two new targets; one is gamma secretase inhibitor. So, it’s a first-in-class, first time we even hear about this target at a clinical conference. And the second highly expected trial is a clinical trial in patients with metastatic lung cancer, KRAS mutated, testing sotorasib, which is a KRAS inhibitor, and showing the magnitude of improvement associated with sotorasib. The trial is positive, and it improved PFS [progression-free survival] in these patients. So these are two new targets that are validated at this conference.
Then, if we go on another topic of genomics, there is a question that is extremely important: Can we define patients who present an outlier sensitivity to immunotherapeutics? There will be one trial presented in the Presidential Symposium of immunotherapeutics in patients with colon cancer and microsatellite instability (MSI), showing that a few weeks of immunotherapeutics followed by surgery can cure patients. Why is it important? It’s important because we are all facing a shortage in the healthcare workforce. We have fewer nurses, fewer doctors, and we all have issues of sustainability. So, really now is the time to think about precision medicine, how precision medicine, by identifying outlier responders, can decrease the amount of resources we need to cure a patient. And this trial on immunotherapeutics, guided by genomics, is exactly this point: 8 weeks of treatment to cure a patient.
Dr. Whyte: Do you think there’s going to be a cure for cancer 10 years from now?
Dr. André: What I’m convinced of is that, in the 10 years that are coming, we are going step by step; we’re going to continue to increase the life expectancy of patients with cancer.
Dr. Whyte: And quality of life too, right?
Dr. André: Quality of life is a major issue. We had today a keynote on digital medicine and how ePRO (electronic patient-reported outcomes) can help the patient to really decrease the burden of symptoms. Quality of life is, of course, extremely important because of the very high number of patients who are cured of cancer; we need to decrease the burden of symptom in patients.
Dr. Whyte: And even though cancer rates are going down in most areas of the world, we still globally have millions of deaths from cancer every year. And sometimes people forget that, because they hear about some of the innovations. But I want to end with this: Are we investing enough in cancer care? Because let’s be honest – there are other diseases that we also need to spend time on. Cardiovascular disease is a global burden; infectious disease is a global burden. Are governments, are industries spending enough on cancer research and development?
Dr. André: Well, we can always claim for more, no? This is how everyone is trying to be, I think. But the reality is that we are living in a world where we have limited resources. I think what is more important for me is to be sure that any euro or dollar invested in cancer research is well used and generates an impact for patients. That is the most important, I think.
Dr. Whyte: And that’s why outcomes are so important in this research.
Dr. André: My conviction is that we have the tools, meaning the knowledge, the biotechnology, to really go the next step in terms of improving outcomes for patients. And for this, we now need clinical trials and translational research, but the tools, meaning basic science, basic knowledge, biotechnology – the basement for progress is here. We need now to transform this into direct impact for the patient. But I would not like to finish by saying we need more money in the field; what we need are people who can transform one euro, one dollar into concrete and measurable advances.
Dr. Whyte: We’re going to need more time on another day because I want to ask you about diversity in clinical trials, how important that is. I want to ask you about pediatric cancers; there are a whole bunch of things that I want to talk to you about. So hopefully we’ll find more time when we’re not at a big international conference such as ESMO. So, Dr Fabrice André, I want to thank you for taking time today.
Dr. André: Thank you and have a nice day.
Dr. Whyte: Stay tuned for a future discussion with Dr André on more about where we’re going in terms of cancer research and development. Thanks for watching, everyone.
A version of this article first appeared on Medscape.com.
Dispelling four myths about the FDA
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte, is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte, is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte, is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Dispelling four myths about the FDA
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
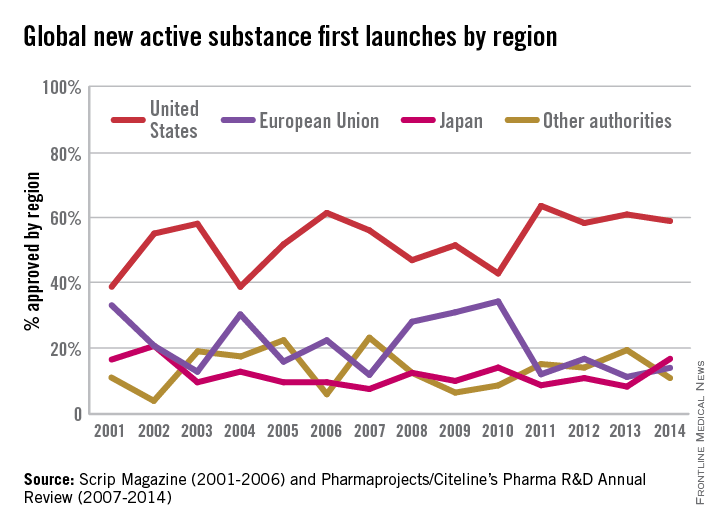
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
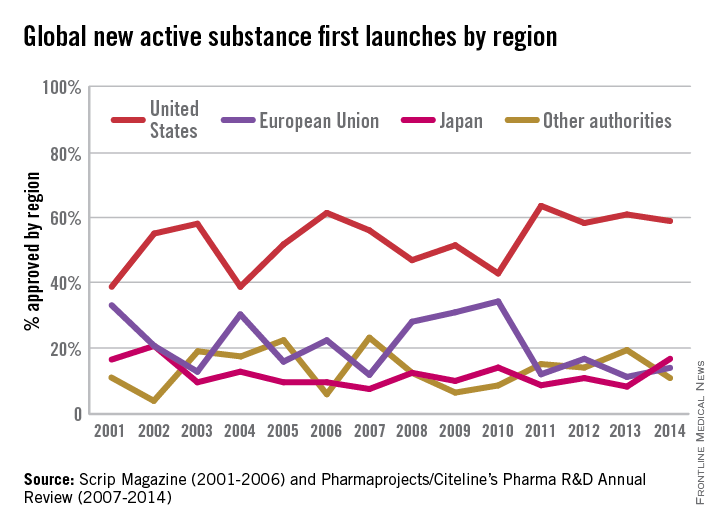
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
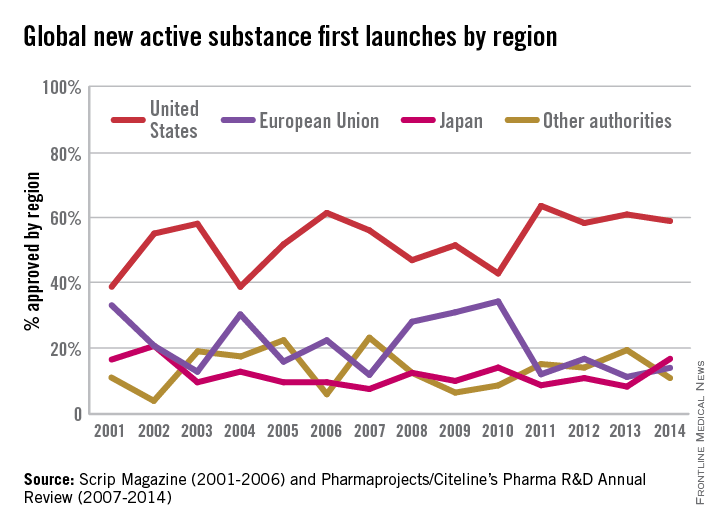
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).