User login
Cetuximab monotherapy ineffective in KRAS G13D-mutant mCRC
Cetuximab monotherapy had no activity in patients with metastatic colorectal cancer (mCRC) and KRAS G13D mutations, a finding that contradicts the theory that the G13D mutation differs from other RAS mutations and confers EGFR-1 monoclonal antibody sensitivity.
None of the patients who received cetuximab monotherapy had a response, and the 6-month progression-free survival rate was 10%.
Combined with recent similar reports of cetuximab monotherapy in G13D-mutated mCRC, the findings, “definitively exclude a clinical rationale for treating patients who have G13D-mutant CRC with single-agent cetuximab. It is reasonable to extrapolate this to an EGFR-I monoclonal antibody class effect, given the retrospective panitumumab data that also failed to show benefit in the G13D cohort, together with the head-to-head comparison of EGFR-I monoclonal antibodies showing no substantive differences between cetuximab and panitumumab in the refractory setting,” wrote Dr. Eva Segelov of University of New South Wales, Australia, and colleagues (J Clin Oncol. 2016 Apr 25. doi: 10.1200/JCO.2015.65.6843).
As part of the ICECREAM (Irinotecan Cetuximab Evaluation and Cetuximab Response Evaluation Among Patients with a G13D Mutation) prospective trial, the analysis included 51 patients with chemotherapy-refractory mCRC and KRAS G13D mutation; 25 received cetuximab monotherapy and 26 received cetuximab plus irinotecan.
In the cetuximab plus irinotecan arm, partial responses were observed in two patients (9%) and the 6-month PFS was 23%. Although both patients with partial responses had irinotecan-free periods of more than 12 months, in general, the time since previous irinotecan treatment did not seem to influence the response to combination therapy. The investigators noted the growing interest in retreating patients with previous chemotherapy and targeted agents, potentially aided by ultrasensitive liquid-biopsy measurements of resistant subclones, “which seem to wax and wane with drug exposure and treatment breaks,” they wrote.
To help discern whether the combination therapy has true synergy or there is an irinotecan rechallenge effect, additional data from the wild-type cohort of the ICECREAM study is awaited.
In addition to similar 6-month PFS in the cetuximab monotherapy and cetuximab plus irinotecan arms, no significant difference in overall survival was observed between the two arms (6-month survival, 56% vs. 42%; HR, 0.95; 95% CI, 0.53-1.68).
Dr. Segelov reported having financial ties to Roche, Bayer Pharmaceuticals Australia, Ipsen, Pfizer, and Merck Serono. Several of her coauthors reported ties to industry sources.
Cetuximab monotherapy had no activity in patients with metastatic colorectal cancer (mCRC) and KRAS G13D mutations, a finding that contradicts the theory that the G13D mutation differs from other RAS mutations and confers EGFR-1 monoclonal antibody sensitivity.
None of the patients who received cetuximab monotherapy had a response, and the 6-month progression-free survival rate was 10%.
Combined with recent similar reports of cetuximab monotherapy in G13D-mutated mCRC, the findings, “definitively exclude a clinical rationale for treating patients who have G13D-mutant CRC with single-agent cetuximab. It is reasonable to extrapolate this to an EGFR-I monoclonal antibody class effect, given the retrospective panitumumab data that also failed to show benefit in the G13D cohort, together with the head-to-head comparison of EGFR-I monoclonal antibodies showing no substantive differences between cetuximab and panitumumab in the refractory setting,” wrote Dr. Eva Segelov of University of New South Wales, Australia, and colleagues (J Clin Oncol. 2016 Apr 25. doi: 10.1200/JCO.2015.65.6843).
As part of the ICECREAM (Irinotecan Cetuximab Evaluation and Cetuximab Response Evaluation Among Patients with a G13D Mutation) prospective trial, the analysis included 51 patients with chemotherapy-refractory mCRC and KRAS G13D mutation; 25 received cetuximab monotherapy and 26 received cetuximab plus irinotecan.
In the cetuximab plus irinotecan arm, partial responses were observed in two patients (9%) and the 6-month PFS was 23%. Although both patients with partial responses had irinotecan-free periods of more than 12 months, in general, the time since previous irinotecan treatment did not seem to influence the response to combination therapy. The investigators noted the growing interest in retreating patients with previous chemotherapy and targeted agents, potentially aided by ultrasensitive liquid-biopsy measurements of resistant subclones, “which seem to wax and wane with drug exposure and treatment breaks,” they wrote.
To help discern whether the combination therapy has true synergy or there is an irinotecan rechallenge effect, additional data from the wild-type cohort of the ICECREAM study is awaited.
In addition to similar 6-month PFS in the cetuximab monotherapy and cetuximab plus irinotecan arms, no significant difference in overall survival was observed between the two arms (6-month survival, 56% vs. 42%; HR, 0.95; 95% CI, 0.53-1.68).
Dr. Segelov reported having financial ties to Roche, Bayer Pharmaceuticals Australia, Ipsen, Pfizer, and Merck Serono. Several of her coauthors reported ties to industry sources.
Cetuximab monotherapy had no activity in patients with metastatic colorectal cancer (mCRC) and KRAS G13D mutations, a finding that contradicts the theory that the G13D mutation differs from other RAS mutations and confers EGFR-1 monoclonal antibody sensitivity.
None of the patients who received cetuximab monotherapy had a response, and the 6-month progression-free survival rate was 10%.
Combined with recent similar reports of cetuximab monotherapy in G13D-mutated mCRC, the findings, “definitively exclude a clinical rationale for treating patients who have G13D-mutant CRC with single-agent cetuximab. It is reasonable to extrapolate this to an EGFR-I monoclonal antibody class effect, given the retrospective panitumumab data that also failed to show benefit in the G13D cohort, together with the head-to-head comparison of EGFR-I monoclonal antibodies showing no substantive differences between cetuximab and panitumumab in the refractory setting,” wrote Dr. Eva Segelov of University of New South Wales, Australia, and colleagues (J Clin Oncol. 2016 Apr 25. doi: 10.1200/JCO.2015.65.6843).
As part of the ICECREAM (Irinotecan Cetuximab Evaluation and Cetuximab Response Evaluation Among Patients with a G13D Mutation) prospective trial, the analysis included 51 patients with chemotherapy-refractory mCRC and KRAS G13D mutation; 25 received cetuximab monotherapy and 26 received cetuximab plus irinotecan.
In the cetuximab plus irinotecan arm, partial responses were observed in two patients (9%) and the 6-month PFS was 23%. Although both patients with partial responses had irinotecan-free periods of more than 12 months, in general, the time since previous irinotecan treatment did not seem to influence the response to combination therapy. The investigators noted the growing interest in retreating patients with previous chemotherapy and targeted agents, potentially aided by ultrasensitive liquid-biopsy measurements of resistant subclones, “which seem to wax and wane with drug exposure and treatment breaks,” they wrote.
To help discern whether the combination therapy has true synergy or there is an irinotecan rechallenge effect, additional data from the wild-type cohort of the ICECREAM study is awaited.
In addition to similar 6-month PFS in the cetuximab monotherapy and cetuximab plus irinotecan arms, no significant difference in overall survival was observed between the two arms (6-month survival, 56% vs. 42%; HR, 0.95; 95% CI, 0.53-1.68).
Dr. Segelov reported having financial ties to Roche, Bayer Pharmaceuticals Australia, Ipsen, Pfizer, and Merck Serono. Several of her coauthors reported ties to industry sources.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In patients with metastatic colorectal cancer and KRAS G13D mutation, cetuximab monotherapy showed no activity, and cetuximab plus irinotecan showed modest activity.
Major finding: In the cetuximab arm, 6-month progression-free survival (PFS) was 10% with a 0% response rate; in the cetuximab plus irinotecan arm, 6-month PFS was 23% with a 9% partial response rate.
Data sources: As part of the ICECREAM prospective trial, the analysis included 51 patients with chemotherapy-refractory mCRC and KRAS G13D mutation; 25 received cetuximab monotherapy and 26 received cetuximab plus irinotecan.
Disclosures: Dr. Segelov reported having financial ties to Roche, Bayer Pharmaceuticals Australia, Ipsen, Pfizer, and Merck Serono. Several of her coauthors reported ties to industry sources.
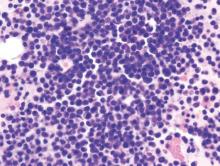
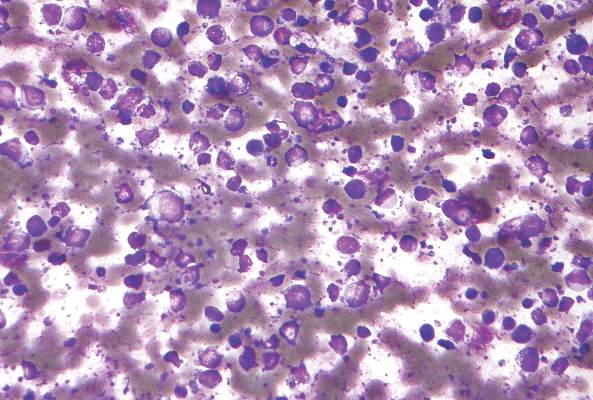
Daratumumab well tolerated, effective in heavily treated multiple myeloma
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
With its novel mechanism of action, single-agent activity, absence of crossresistance, and tolerability, daratumumab may prove to be a transformative new treatment for multiple myeloma.
 |
| Patrice Wendling/Frontline Medical News Dr. S. Vincent Rajkumar |
The single-agent activity of daratumumab (29%) exceeds that of bortezomib (27%), lenalidomide (26%), carfilzomib (24%), or pomalidomide (18%), even in a heavily pretreated population.
The safety profile is outstanding, and therein lies the reason for enthusiasm: Daratumumab can probably be combined with currently used triplet combinations in multiple myeloma, and can potentially take these highly active regimens to new heights.
Similar to rituximab, daratumumab will probably be added to many active triplet combinations. Daratumumab will likely move rapidly to a front-line setting in clinical trials for treatment of newly diagnosed multiple myeloma, maintenance therapy, and even smoldering multiple myeloma.
However, the data are insufficient to determine the cytogenetic subtypes that respond best to daratumumab. That information will be necessary in order to best sequence drugs according to the subtype of myeloma.
It will be important also to understand how daratumumab, an anti-CD38 drug, can work optimally with elotuzumab, another newly approved monoclonal antibody that targets SLAMF7.
Dr. S. Vincent Rajkumar is with the Mayo Clinic, Rochester, Minn. These remarks were part of an editorial (Lancet 2016; 387:1490-91) accompanying the study in the Lancet.
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
Daratumumab monotherapy was associated with an overall response rate of 29.2% and was well tolerated in 106 heavily treated patients with multiple myeloma, based on results from the SIRIUS trial.
Of 106 patients who received daratumumab at 16 mg/kg, 3% achieved a stringent complete response, 9% had a very good partial response, and 17% had a partial response. The median progression-free survival was 3.7 months and median duration of response was 7.4 months. The 12-month overall survival was 64·8%, and, at a subsequent cutoff, median overall survival was 17.5 months.
All of the study patients had been treated with proteasome inhibitors and immunomodulatory drugs, with a median of five previous therapies. Most patients (80%) had received autologous stem cell transplantation, and 97% were refractory to the last line of therapy before study enrollment.
“Resistance to any previous therapy had no effect on the activity of daratumumab, lending support to a novel mechanism of action, but these findings need to be confirmed in larger studies,” wrote Dr. Sagar Lonial of Emory University, Atlanta, and colleagues (Lancet 2016;387:1551-60). Response rates were similar for patients with moderate renal impairment, those over age 75, and those with extramedullary disease or high-risk baseline cytogenetic characteristics.
Daratumumab was well tolerated, and none of the patients discontinued treatment because of treatment-related adverse events. The most common adverse events of any grade were anemia (33%), thrombocytopenia (25%), and neutropenia (23%). Additional supportive care in the form of red blood cell transfusions was received by 38% of patients, platelet transfusions by 13%, and granulocyte colony-stimulating factor by 8%. Fatigue (40%) and nausea (29%) were the most common nonhematologic adverse events. Serious adverse events were observed in 30% of patients.
Daratumumab compares favorably with other regimens such as pomalidomide alone or with dexamethasone or carfilzomib monotherapy, according to the investigators.
The favorable safety profile of daratumumab makes it an attractive candidate for combination regimens, the authors noted, and daratumumab combined with other backbone agents are currently under investigation.
This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
FROM THE LANCET
Key clinical point: Daratumumab was well tolerated and showed encouraging activity in heavily treated patients with multiple myeloma.
Major finding: In 106 patients previously treated with a median of five lines of therapy, the overall response rate to daratumumab at 16 mg/kg was 29.2%; 3% achieved a stringent complete response, 9% a very good partial response, and 17% a partial response.
Data sources: Data from the SIRIUS trial for 106 patients in the 16-mg/kg group.
Disclosures: This study was sponsored by Janssen, maker of daratumumab (Darzalex). Dr. Lonial reported consulting or advisory roles with Janssen and several other drug companies.
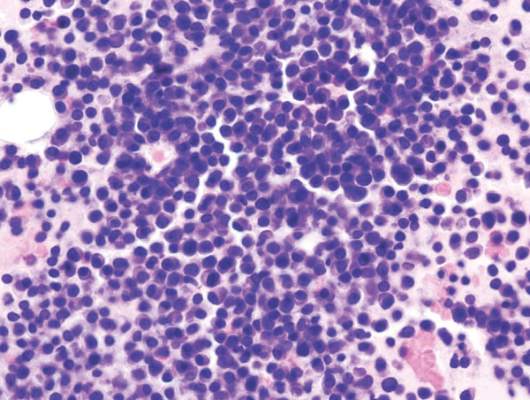
Dose-escalated blinatumomab plus dexamethasone induced responses in relapsed/refractory DLBCL
Blinatumomab, administered in a stepwise, dose-escalated regimen with prophylactic dexamethasone, induced responses in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a report published in Blood.
The phase II study included 25 patients who were refractory to their last treatment, had relapsed after autologous hematopoietic stem cell transplant (HSCT), or had relapsed disease and were ineligible for autologous HSCT.
In a previous phase I study that did not use a dose-escalated regimen, neurological adverse events were dose limiting at a maximum tolerated blinatumomab dose of 60 mcg/d. The current study used a 14-day stepwise dose escalation and corticosteroid premedication to minimize adverse events: blinatumomab was given at 9 mcg/d in the first week, 28 mcg/d in the second week, and 112 mcg/d thereafter.
Patients had received a median of three prior therapies. In total, 17 of 25 patients ended in cycle 1 (induction) because of disease progression, adverse events, or physician decision; 7 ended in cycle 2 (consolidation), and 1 ended in retreatment.
Among the 21 evaluable patients who received at least 1 week of blinatumomab at the target dose of 112 mcg/day or who discontinued treatment earlier because of progressive disease, the overall response rate was 43% (9/21) and the complete response rate was 19% (4/21). “At least 1 week of treatment at the target dose of 112 mcg/d appears to be required for efficacy,” wrote Dr. Andreas Viardot of the department of internal medicine III, University Hospital Ulm (Germany) and colleagues (Blood. 2016;127(11):1410-16).
The most common adverse events of grade 3 or higher were thrombocytopenia (17%) and leukopenia (17%). Grade 3 neurologic events included encephalopathy (9%) and aphasia (9%); no grade 4 or 5 neurologic events were reported. Cytokine release syndrome or cytokine storm were not reported.
Blinatumomab (Blincyto) is a bispecific T-cell engager antibody approved for the treatment of Philadelphia chromosome-negative relapsed or refractory B-cell precursor acute lymphoblastic leukemia. Blinatumomab transiently links CD3-positive T cells to CD19-positive B cells, which activates T cells and leads to T cell–mediated lysis of tumor cells and concomitant T-cell proliferation.
The study was supported by Amgen, the maker of Blincyto. Dr. Viardot reported having financial ties with Amgen and several other drug companies.
Blinatumomab, administered in a stepwise, dose-escalated regimen with prophylactic dexamethasone, induced responses in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a report published in Blood.
The phase II study included 25 patients who were refractory to their last treatment, had relapsed after autologous hematopoietic stem cell transplant (HSCT), or had relapsed disease and were ineligible for autologous HSCT.
In a previous phase I study that did not use a dose-escalated regimen, neurological adverse events were dose limiting at a maximum tolerated blinatumomab dose of 60 mcg/d. The current study used a 14-day stepwise dose escalation and corticosteroid premedication to minimize adverse events: blinatumomab was given at 9 mcg/d in the first week, 28 mcg/d in the second week, and 112 mcg/d thereafter.
Patients had received a median of three prior therapies. In total, 17 of 25 patients ended in cycle 1 (induction) because of disease progression, adverse events, or physician decision; 7 ended in cycle 2 (consolidation), and 1 ended in retreatment.
Among the 21 evaluable patients who received at least 1 week of blinatumomab at the target dose of 112 mcg/day or who discontinued treatment earlier because of progressive disease, the overall response rate was 43% (9/21) and the complete response rate was 19% (4/21). “At least 1 week of treatment at the target dose of 112 mcg/d appears to be required for efficacy,” wrote Dr. Andreas Viardot of the department of internal medicine III, University Hospital Ulm (Germany) and colleagues (Blood. 2016;127(11):1410-16).
The most common adverse events of grade 3 or higher were thrombocytopenia (17%) and leukopenia (17%). Grade 3 neurologic events included encephalopathy (9%) and aphasia (9%); no grade 4 or 5 neurologic events were reported. Cytokine release syndrome or cytokine storm were not reported.
Blinatumomab (Blincyto) is a bispecific T-cell engager antibody approved for the treatment of Philadelphia chromosome-negative relapsed or refractory B-cell precursor acute lymphoblastic leukemia. Blinatumomab transiently links CD3-positive T cells to CD19-positive B cells, which activates T cells and leads to T cell–mediated lysis of tumor cells and concomitant T-cell proliferation.
The study was supported by Amgen, the maker of Blincyto. Dr. Viardot reported having financial ties with Amgen and several other drug companies.
Blinatumomab, administered in a stepwise, dose-escalated regimen with prophylactic dexamethasone, induced responses in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to a report published in Blood.
The phase II study included 25 patients who were refractory to their last treatment, had relapsed after autologous hematopoietic stem cell transplant (HSCT), or had relapsed disease and were ineligible for autologous HSCT.
In a previous phase I study that did not use a dose-escalated regimen, neurological adverse events were dose limiting at a maximum tolerated blinatumomab dose of 60 mcg/d. The current study used a 14-day stepwise dose escalation and corticosteroid premedication to minimize adverse events: blinatumomab was given at 9 mcg/d in the first week, 28 mcg/d in the second week, and 112 mcg/d thereafter.
Patients had received a median of three prior therapies. In total, 17 of 25 patients ended in cycle 1 (induction) because of disease progression, adverse events, or physician decision; 7 ended in cycle 2 (consolidation), and 1 ended in retreatment.
Among the 21 evaluable patients who received at least 1 week of blinatumomab at the target dose of 112 mcg/day or who discontinued treatment earlier because of progressive disease, the overall response rate was 43% (9/21) and the complete response rate was 19% (4/21). “At least 1 week of treatment at the target dose of 112 mcg/d appears to be required for efficacy,” wrote Dr. Andreas Viardot of the department of internal medicine III, University Hospital Ulm (Germany) and colleagues (Blood. 2016;127(11):1410-16).
The most common adverse events of grade 3 or higher were thrombocytopenia (17%) and leukopenia (17%). Grade 3 neurologic events included encephalopathy (9%) and aphasia (9%); no grade 4 or 5 neurologic events were reported. Cytokine release syndrome or cytokine storm were not reported.
Blinatumomab (Blincyto) is a bispecific T-cell engager antibody approved for the treatment of Philadelphia chromosome-negative relapsed or refractory B-cell precursor acute lymphoblastic leukemia. Blinatumomab transiently links CD3-positive T cells to CD19-positive B cells, which activates T cells and leads to T cell–mediated lysis of tumor cells and concomitant T-cell proliferation.
The study was supported by Amgen, the maker of Blincyto. Dr. Viardot reported having financial ties with Amgen and several other drug companies.
FROM BLOOD
Key clinical point: Stepwise dose-escalated administration of blinatumomab plus dexamethasone may be effective in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Major finding: The overall response rate in 21 evaluable patients was 43% and the complete response rate was 19%.
Data sources: Phase II study of 25 patients who had received a median of three prior therapies.
Disclosures: The study was supported by Amgen, the maker of blinatumomab. Dr. Viardot reported having financial ties with Amgen and several other drug makers.
Older patients with soft tissue sarcoma may receive greater benefit from RT
Older patients appeared to receive greater benefit from adjuvant radiotherapy (RT) for soft tissue sarcoma (STS) than younger patients, according an analysis of the Surveillance, Epidemiology, and End Results (SEER) database.
Several STS subtypes were associated with significant RT benefits to overall survival (OS) and disease-specific survival (DSS) in patients older than 65 years, but survival differences were not significant in younger patients. These seven subtypes included leiomyosarcoma (hazard ratio, 0.84; P = .04), sarcoma not otherwise specified (HR, 0.66; P less than or equal to .001), liposarcoma not otherwise specified (HR, 0.72; P = .05), myxoid liposarcoma (HR, 0.50; P = .02), rhabdomyosarcoma (HR, 0.23; P less than or equal to .001), epithelioid (HR, 0.01; P less than .01) and myxoid chondrosarcoma (HR, 0.02; P = .04). One STS subtype, synovial sarcoma, was associated with significant RT benefit only in younger patients (HR, 0.73; P = .04). Malignant fibrous histiocytoma was the only subtype to show significant benefit in the overall cohort as well as both age groups.
“We observed a statistically significant improvement in OS and DSS in all patients receiving RT compared to surgery alone across the majority of histological subgroups. More importantly, there was no significant improvement in younger patients compared to a significant improvement in older patients, suggesting that survival benefits in response to RT are significantly affected by age-related differences,” wrote Dr. Noah K. Yuen of the Department of Surgery, University of California, Davis, and his colleagues (Anticancer Res. 2016 Apr;36(4):1745-50). The findings suggest that older patients may benefit more than previously appreciated, and while implementation of RT among the elderly may present challenges, according to the investigators, “our data suggest that this approach deserves greater attention.”
Previous population-based retrospective studies have demonstrated a similar benefit with surgery and adjuvant RT; however, randomized clinical trials have shown significant improvement in local control but have failed to show significant improvement in OS. The authors acknowledged the potential impact of unmeasured confounding factors on the retrospective study. Selection bias may be present if healthier older patients preferentially received RT; a subpopulation of healthier individuals would be expected to have better survival.
The SEER database analysis included 15,380 patients with non-metastatic STS who underwent surgery during 1990 to 2011. The mean age of the cohort was 56.6 years and one-third were age 65 years or more. As the most common histologic subtype, leiomyosarcoma accounted for 30.1% of all tumors. Most of the patients treated with RT (68.3%) had high-grade tumors.
Older patients appeared to receive greater benefit from adjuvant radiotherapy (RT) for soft tissue sarcoma (STS) than younger patients, according an analysis of the Surveillance, Epidemiology, and End Results (SEER) database.
Several STS subtypes were associated with significant RT benefits to overall survival (OS) and disease-specific survival (DSS) in patients older than 65 years, but survival differences were not significant in younger patients. These seven subtypes included leiomyosarcoma (hazard ratio, 0.84; P = .04), sarcoma not otherwise specified (HR, 0.66; P less than or equal to .001), liposarcoma not otherwise specified (HR, 0.72; P = .05), myxoid liposarcoma (HR, 0.50; P = .02), rhabdomyosarcoma (HR, 0.23; P less than or equal to .001), epithelioid (HR, 0.01; P less than .01) and myxoid chondrosarcoma (HR, 0.02; P = .04). One STS subtype, synovial sarcoma, was associated with significant RT benefit only in younger patients (HR, 0.73; P = .04). Malignant fibrous histiocytoma was the only subtype to show significant benefit in the overall cohort as well as both age groups.
“We observed a statistically significant improvement in OS and DSS in all patients receiving RT compared to surgery alone across the majority of histological subgroups. More importantly, there was no significant improvement in younger patients compared to a significant improvement in older patients, suggesting that survival benefits in response to RT are significantly affected by age-related differences,” wrote Dr. Noah K. Yuen of the Department of Surgery, University of California, Davis, and his colleagues (Anticancer Res. 2016 Apr;36(4):1745-50). The findings suggest that older patients may benefit more than previously appreciated, and while implementation of RT among the elderly may present challenges, according to the investigators, “our data suggest that this approach deserves greater attention.”
Previous population-based retrospective studies have demonstrated a similar benefit with surgery and adjuvant RT; however, randomized clinical trials have shown significant improvement in local control but have failed to show significant improvement in OS. The authors acknowledged the potential impact of unmeasured confounding factors on the retrospective study. Selection bias may be present if healthier older patients preferentially received RT; a subpopulation of healthier individuals would be expected to have better survival.
The SEER database analysis included 15,380 patients with non-metastatic STS who underwent surgery during 1990 to 2011. The mean age of the cohort was 56.6 years and one-third were age 65 years or more. As the most common histologic subtype, leiomyosarcoma accounted for 30.1% of all tumors. Most of the patients treated with RT (68.3%) had high-grade tumors.
Older patients appeared to receive greater benefit from adjuvant radiotherapy (RT) for soft tissue sarcoma (STS) than younger patients, according an analysis of the Surveillance, Epidemiology, and End Results (SEER) database.
Several STS subtypes were associated with significant RT benefits to overall survival (OS) and disease-specific survival (DSS) in patients older than 65 years, but survival differences were not significant in younger patients. These seven subtypes included leiomyosarcoma (hazard ratio, 0.84; P = .04), sarcoma not otherwise specified (HR, 0.66; P less than or equal to .001), liposarcoma not otherwise specified (HR, 0.72; P = .05), myxoid liposarcoma (HR, 0.50; P = .02), rhabdomyosarcoma (HR, 0.23; P less than or equal to .001), epithelioid (HR, 0.01; P less than .01) and myxoid chondrosarcoma (HR, 0.02; P = .04). One STS subtype, synovial sarcoma, was associated with significant RT benefit only in younger patients (HR, 0.73; P = .04). Malignant fibrous histiocytoma was the only subtype to show significant benefit in the overall cohort as well as both age groups.
“We observed a statistically significant improvement in OS and DSS in all patients receiving RT compared to surgery alone across the majority of histological subgroups. More importantly, there was no significant improvement in younger patients compared to a significant improvement in older patients, suggesting that survival benefits in response to RT are significantly affected by age-related differences,” wrote Dr. Noah K. Yuen of the Department of Surgery, University of California, Davis, and his colleagues (Anticancer Res. 2016 Apr;36(4):1745-50). The findings suggest that older patients may benefit more than previously appreciated, and while implementation of RT among the elderly may present challenges, according to the investigators, “our data suggest that this approach deserves greater attention.”
Previous population-based retrospective studies have demonstrated a similar benefit with surgery and adjuvant RT; however, randomized clinical trials have shown significant improvement in local control but have failed to show significant improvement in OS. The authors acknowledged the potential impact of unmeasured confounding factors on the retrospective study. Selection bias may be present if healthier older patients preferentially received RT; a subpopulation of healthier individuals would be expected to have better survival.
The SEER database analysis included 15,380 patients with non-metastatic STS who underwent surgery during 1990 to 2011. The mean age of the cohort was 56.6 years and one-third were age 65 years or more. As the most common histologic subtype, leiomyosarcoma accounted for 30.1% of all tumors. Most of the patients treated with RT (68.3%) had high-grade tumors.
FROM ANTICANCER RESEARCH
Key clinical point: For many subtypes of soft tissue sarcoma (STS), overall survival (OS) was significantly greater in older patients who received adjuvant RT, compared with those who received surgery alone.
Major finding: Among patients age 65 years and older who received RT, most STS subtypes were associated with significantly improved OS; among younger patients, only three subtypes were associated with significantly improved OS.
Data sources: The retrospective analysis of the Surveillance, Epidemiology, and End Results (SEER) database included 15,380 patients with non-metastatic STS who underwent surgery during 1990 to 2011.
Disclosures: Dr. Yuen and his coauthors reported having no disclosures.
Factor VIII–mimetic antibody effective in hemophilia A
The bispecific factor VIII–mimetic antibody ACE910 has a longer half-life than current hemophilia A treatments, potentially offering a more convenient once-weekly, subcutaneous injection, based on a study published in Blood.
In a phase I study, ACE910 was well tolerated at doses up to 1 mg/kg, with an average half life of 28 to 34 days. Based on tests in FVIII-depleted plasma, ACE910 shortened activated partial thromboplastin time (APTT) and increased peak height of thrombin generation, and exhibited a long-lasting response throughout the 24-week study period. ACE910 at 1 mg/kg resulted in APTT similar to that seen in normal plasma, although the peak height of thrombin generation did not reach normal levels.
The findings suggest “that ACE910 has the potential to reduce bleeding frequency in patients with severe hemophilia A to that of patients with mild hemophilia A, even at less frequent dosing, compared with existing FVIII and bypassing drugs. Furthermore, ACE910 may change the treatment paradigm from the current approach of maintaining trough levels of FVIII:C greater than 1% to a new approach of maintaining a constant hemostatic activity corresponding to a mild hemophilia A level,” wrote Dr. Naoki Uchida of Showa University Clinical Research Institute for Clinical Pharmacology and Therapeutics, Tokyo, and colleagues (Blood. 2016 Apr 7. doi: 10.1182/blood-2015-06-650226).
Adverse events were comparable with those of placebo; 13 of 48 subjects who received ACE910 reported 15 adverse events, compared with 6 adverse events reported by 4 of 16 subjects who received placebo. Except for moderate nasopharyngitis reported in one subject, all adverse events were mild, were not dose dependent, and were similar for Japanese and white subjects. Clinical and laboratory findings showed normal coagulability with ACE910 administered at any dose.
An anti-drug antibody response was observed in 2 of 48 patients (1 Japanese, 1 white) both at 0.1 mg/kg ACE910. The anti-drug antibody responses were not IgE mediated, and no allergic symptoms were observed.
This new nonsubstitutive therapy for hemophilia A has potential to become a disruptive technology that displaces the current therapeutic approach.
By binding to factor IXa and factor X, ACE910 bypasses factor VIII in the generation of factor Xa. Since ACE910 is a distinct entity from factor VIII, anti-FVIII antibodies do not neutralize the agent.
Infusion of recombinant factor VIII has an average half-life of 8 to 12 hours, or 1.5 to 1.7 hours longer with the recent introduction of extended half-life products. Patients who develop factor VIII allo- or autoantibodies require frequent, less effective intravenous therapies. ACE910 switches up the paradigm, with repeat doses given subcutaneously once per week.
Of concern is the potential for thrombosis and anti-drug antibodies (ADAs). Despite the long half-life of ACE910 and that the phase I study was conducted on healthy volunteers with normal coagulation systems, investigators observed no rise in D-dimer formation. Similarly, no rise in thrombin-antithrombin complex was observed.
Two of 48 subjects had anti-ACE910 antibodies, and in one of these subjects ACE910 half-life was reduced, as was APTT correction and thrombin generation. These findings suggest a functional ADA. A key issue for future studies will be the number of individuals who develop ADAs after repeated exposure to ACE910.
Dr. Michael Makris is professor of haemostasis and thrombosis at the University of Sheffield (England). These remarks were part of an editorial accompanying a report in Blood (2016 Apr 7. doi: 10.1182/blood-2016-01-691469).
This new nonsubstitutive therapy for hemophilia A has potential to become a disruptive technology that displaces the current therapeutic approach.
By binding to factor IXa and factor X, ACE910 bypasses factor VIII in the generation of factor Xa. Since ACE910 is a distinct entity from factor VIII, anti-FVIII antibodies do not neutralize the agent.
Infusion of recombinant factor VIII has an average half-life of 8 to 12 hours, or 1.5 to 1.7 hours longer with the recent introduction of extended half-life products. Patients who develop factor VIII allo- or autoantibodies require frequent, less effective intravenous therapies. ACE910 switches up the paradigm, with repeat doses given subcutaneously once per week.
Of concern is the potential for thrombosis and anti-drug antibodies (ADAs). Despite the long half-life of ACE910 and that the phase I study was conducted on healthy volunteers with normal coagulation systems, investigators observed no rise in D-dimer formation. Similarly, no rise in thrombin-antithrombin complex was observed.
Two of 48 subjects had anti-ACE910 antibodies, and in one of these subjects ACE910 half-life was reduced, as was APTT correction and thrombin generation. These findings suggest a functional ADA. A key issue for future studies will be the number of individuals who develop ADAs after repeated exposure to ACE910.
Dr. Michael Makris is professor of haemostasis and thrombosis at the University of Sheffield (England). These remarks were part of an editorial accompanying a report in Blood (2016 Apr 7. doi: 10.1182/blood-2016-01-691469).
This new nonsubstitutive therapy for hemophilia A has potential to become a disruptive technology that displaces the current therapeutic approach.
By binding to factor IXa and factor X, ACE910 bypasses factor VIII in the generation of factor Xa. Since ACE910 is a distinct entity from factor VIII, anti-FVIII antibodies do not neutralize the agent.
Infusion of recombinant factor VIII has an average half-life of 8 to 12 hours, or 1.5 to 1.7 hours longer with the recent introduction of extended half-life products. Patients who develop factor VIII allo- or autoantibodies require frequent, less effective intravenous therapies. ACE910 switches up the paradigm, with repeat doses given subcutaneously once per week.
Of concern is the potential for thrombosis and anti-drug antibodies (ADAs). Despite the long half-life of ACE910 and that the phase I study was conducted on healthy volunteers with normal coagulation systems, investigators observed no rise in D-dimer formation. Similarly, no rise in thrombin-antithrombin complex was observed.
Two of 48 subjects had anti-ACE910 antibodies, and in one of these subjects ACE910 half-life was reduced, as was APTT correction and thrombin generation. These findings suggest a functional ADA. A key issue for future studies will be the number of individuals who develop ADAs after repeated exposure to ACE910.
Dr. Michael Makris is professor of haemostasis and thrombosis at the University of Sheffield (England). These remarks were part of an editorial accompanying a report in Blood (2016 Apr 7. doi: 10.1182/blood-2016-01-691469).
The bispecific factor VIII–mimetic antibody ACE910 has a longer half-life than current hemophilia A treatments, potentially offering a more convenient once-weekly, subcutaneous injection, based on a study published in Blood.
In a phase I study, ACE910 was well tolerated at doses up to 1 mg/kg, with an average half life of 28 to 34 days. Based on tests in FVIII-depleted plasma, ACE910 shortened activated partial thromboplastin time (APTT) and increased peak height of thrombin generation, and exhibited a long-lasting response throughout the 24-week study period. ACE910 at 1 mg/kg resulted in APTT similar to that seen in normal plasma, although the peak height of thrombin generation did not reach normal levels.
The findings suggest “that ACE910 has the potential to reduce bleeding frequency in patients with severe hemophilia A to that of patients with mild hemophilia A, even at less frequent dosing, compared with existing FVIII and bypassing drugs. Furthermore, ACE910 may change the treatment paradigm from the current approach of maintaining trough levels of FVIII:C greater than 1% to a new approach of maintaining a constant hemostatic activity corresponding to a mild hemophilia A level,” wrote Dr. Naoki Uchida of Showa University Clinical Research Institute for Clinical Pharmacology and Therapeutics, Tokyo, and colleagues (Blood. 2016 Apr 7. doi: 10.1182/blood-2015-06-650226).
Adverse events were comparable with those of placebo; 13 of 48 subjects who received ACE910 reported 15 adverse events, compared with 6 adverse events reported by 4 of 16 subjects who received placebo. Except for moderate nasopharyngitis reported in one subject, all adverse events were mild, were not dose dependent, and were similar for Japanese and white subjects. Clinical and laboratory findings showed normal coagulability with ACE910 administered at any dose.
An anti-drug antibody response was observed in 2 of 48 patients (1 Japanese, 1 white) both at 0.1 mg/kg ACE910. The anti-drug antibody responses were not IgE mediated, and no allergic symptoms were observed.
The bispecific factor VIII–mimetic antibody ACE910 has a longer half-life than current hemophilia A treatments, potentially offering a more convenient once-weekly, subcutaneous injection, based on a study published in Blood.
In a phase I study, ACE910 was well tolerated at doses up to 1 mg/kg, with an average half life of 28 to 34 days. Based on tests in FVIII-depleted plasma, ACE910 shortened activated partial thromboplastin time (APTT) and increased peak height of thrombin generation, and exhibited a long-lasting response throughout the 24-week study period. ACE910 at 1 mg/kg resulted in APTT similar to that seen in normal plasma, although the peak height of thrombin generation did not reach normal levels.
The findings suggest “that ACE910 has the potential to reduce bleeding frequency in patients with severe hemophilia A to that of patients with mild hemophilia A, even at less frequent dosing, compared with existing FVIII and bypassing drugs. Furthermore, ACE910 may change the treatment paradigm from the current approach of maintaining trough levels of FVIII:C greater than 1% to a new approach of maintaining a constant hemostatic activity corresponding to a mild hemophilia A level,” wrote Dr. Naoki Uchida of Showa University Clinical Research Institute for Clinical Pharmacology and Therapeutics, Tokyo, and colleagues (Blood. 2016 Apr 7. doi: 10.1182/blood-2015-06-650226).
Adverse events were comparable with those of placebo; 13 of 48 subjects who received ACE910 reported 15 adverse events, compared with 6 adverse events reported by 4 of 16 subjects who received placebo. Except for moderate nasopharyngitis reported in one subject, all adverse events were mild, were not dose dependent, and were similar for Japanese and white subjects. Clinical and laboratory findings showed normal coagulability with ACE910 administered at any dose.
An anti-drug antibody response was observed in 2 of 48 patients (1 Japanese, 1 white) both at 0.1 mg/kg ACE910. The anti-drug antibody responses were not IgE mediated, and no allergic symptoms were observed.
FROM BLOOD
Key clinical point: The bispecific antibody ACE910 was safe and effective as a long-acting hemostatic drug for hemophilia A in a phase I trial of healthy subjects.
Major finding: ACE910 was well tolerated up to 1 mg/kg with an average half-life of 28 to 34 days; in factor VIII–depleted plasma, ACE910 at 1 mg/kg resulted in an APTT similar to normal plasma.
Data sources: The first-in-human, double-blind, randomized, placebo-controlled dose-escalation study included 40 Japanese men and 24 white men.
Disclosures: The study was sponsored by Chugai Pharmaceutical. Dr. Uchida reported having no disclosures. His coauthors reported ties to Chugai Pharmaceutical and F. Hoffmann-La Roche, as well as holding patents related to anti-FIXa/X bispecific antibodies.
Targeted therapy, immunotherapy may benefit patients with leptomeningeal metastases from melanoma
Patients with leptomeningeal metastases (LM) from melanoma have a poor prognosis, but treatment with targeted therapy and immune checkpoint inhibitors increased overall survival and resulted in long-term remission in a few patients, according to researchers.
The median survival for 21 patients who were treated with a BRAF inhibitor and/or ipilimumab was 21.7 weeks (range 2 to 235+ weeks); 24.9 weeks for treatment including a BRAF inhibitor (with and without a MEK inhibitor); 15.8 weeks for treatment including ipilimumab; and 4.3 weeks for radiotherapy (RT) only (Annals of Oncology 2016 March 8. doi: 10.1093/annonc/mdw134).
“A remarkable and encouraging new finding in our study is the long-term survival of patients who were treated with targeted treatment or immunotherapy. Moreover, the median survival of 22 weeks following these new therapies compares favorably to reported results of [intrathecal] chemotherapy for LM from melanoma,” wrote Dr. Marnix Geukes Foppen of Netherlands Cancer Institute, Amsterdam, and colleagues.
The retrospective analysis evaluated 39 consecutive patients treated at the Netherlands Cancer Institute during 2010-2015. Because of rapid disease progression or poor performance status, 14 patients did not receive treatment for LM, and their median survival was 2.9 weeks. Among 25 patients who were treated for LM, 15 received cranial or spinal RT and 21 received systemic therapy, and the median survival was 16.9 weeks.
Patients with performance status of 2 or 3 had worse survival than did those with performance status of 0 or 1 (3.6 vs. 18.8 weeks, P less than .001), and treatment did not significantly improve survival in this group (median 1.9 weeks for untreated vs. 3.9 weeks for treated). Patients with increased serum levels of lactate dehydrogenase and/or S100B had poorer survival compared with patients with normal levels.
The investigators noted that ipilimumab increases anti-tumor T cell activation in the lymph nodes, and activated T cells can cross the blood-brain or blood-CSF barrier. RT combined with ipilimumab may increase responses. Among 10 patients whose treatment included ipilimumab, median survival was 15.8 weeks; median survival was 47 weeks for ipilimumab with RT, and 6 weeks for ipilimumab without RT. A patient who had lymph node and lung metastasis, and LM without brain metastasis, was treated with whole brain RT and four cycles of ipilimumab, resulting in a complete radiological and clinical remission beyond 54 months.
Combining systemic targeted therapy and immunotherapy may result in long-term remissions, according the investigators.
“Especially in LM patients with a good performance score and low serum LDH and S100B levels these treatment options should be considered,” they wrote.
Patients with leptomeningeal metastases (LM) from melanoma have a poor prognosis, but treatment with targeted therapy and immune checkpoint inhibitors increased overall survival and resulted in long-term remission in a few patients, according to researchers.
The median survival for 21 patients who were treated with a BRAF inhibitor and/or ipilimumab was 21.7 weeks (range 2 to 235+ weeks); 24.9 weeks for treatment including a BRAF inhibitor (with and without a MEK inhibitor); 15.8 weeks for treatment including ipilimumab; and 4.3 weeks for radiotherapy (RT) only (Annals of Oncology 2016 March 8. doi: 10.1093/annonc/mdw134).
“A remarkable and encouraging new finding in our study is the long-term survival of patients who were treated with targeted treatment or immunotherapy. Moreover, the median survival of 22 weeks following these new therapies compares favorably to reported results of [intrathecal] chemotherapy for LM from melanoma,” wrote Dr. Marnix Geukes Foppen of Netherlands Cancer Institute, Amsterdam, and colleagues.
The retrospective analysis evaluated 39 consecutive patients treated at the Netherlands Cancer Institute during 2010-2015. Because of rapid disease progression or poor performance status, 14 patients did not receive treatment for LM, and their median survival was 2.9 weeks. Among 25 patients who were treated for LM, 15 received cranial or spinal RT and 21 received systemic therapy, and the median survival was 16.9 weeks.
Patients with performance status of 2 or 3 had worse survival than did those with performance status of 0 or 1 (3.6 vs. 18.8 weeks, P less than .001), and treatment did not significantly improve survival in this group (median 1.9 weeks for untreated vs. 3.9 weeks for treated). Patients with increased serum levels of lactate dehydrogenase and/or S100B had poorer survival compared with patients with normal levels.
The investigators noted that ipilimumab increases anti-tumor T cell activation in the lymph nodes, and activated T cells can cross the blood-brain or blood-CSF barrier. RT combined with ipilimumab may increase responses. Among 10 patients whose treatment included ipilimumab, median survival was 15.8 weeks; median survival was 47 weeks for ipilimumab with RT, and 6 weeks for ipilimumab without RT. A patient who had lymph node and lung metastasis, and LM without brain metastasis, was treated with whole brain RT and four cycles of ipilimumab, resulting in a complete radiological and clinical remission beyond 54 months.
Combining systemic targeted therapy and immunotherapy may result in long-term remissions, according the investigators.
“Especially in LM patients with a good performance score and low serum LDH and S100B levels these treatment options should be considered,” they wrote.
Patients with leptomeningeal metastases (LM) from melanoma have a poor prognosis, but treatment with targeted therapy and immune checkpoint inhibitors increased overall survival and resulted in long-term remission in a few patients, according to researchers.
The median survival for 21 patients who were treated with a BRAF inhibitor and/or ipilimumab was 21.7 weeks (range 2 to 235+ weeks); 24.9 weeks for treatment including a BRAF inhibitor (with and without a MEK inhibitor); 15.8 weeks for treatment including ipilimumab; and 4.3 weeks for radiotherapy (RT) only (Annals of Oncology 2016 March 8. doi: 10.1093/annonc/mdw134).
“A remarkable and encouraging new finding in our study is the long-term survival of patients who were treated with targeted treatment or immunotherapy. Moreover, the median survival of 22 weeks following these new therapies compares favorably to reported results of [intrathecal] chemotherapy for LM from melanoma,” wrote Dr. Marnix Geukes Foppen of Netherlands Cancer Institute, Amsterdam, and colleagues.
The retrospective analysis evaluated 39 consecutive patients treated at the Netherlands Cancer Institute during 2010-2015. Because of rapid disease progression or poor performance status, 14 patients did not receive treatment for LM, and their median survival was 2.9 weeks. Among 25 patients who were treated for LM, 15 received cranial or spinal RT and 21 received systemic therapy, and the median survival was 16.9 weeks.
Patients with performance status of 2 or 3 had worse survival than did those with performance status of 0 or 1 (3.6 vs. 18.8 weeks, P less than .001), and treatment did not significantly improve survival in this group (median 1.9 weeks for untreated vs. 3.9 weeks for treated). Patients with increased serum levels of lactate dehydrogenase and/or S100B had poorer survival compared with patients with normal levels.
The investigators noted that ipilimumab increases anti-tumor T cell activation in the lymph nodes, and activated T cells can cross the blood-brain or blood-CSF barrier. RT combined with ipilimumab may increase responses. Among 10 patients whose treatment included ipilimumab, median survival was 15.8 weeks; median survival was 47 weeks for ipilimumab with RT, and 6 weeks for ipilimumab without RT. A patient who had lymph node and lung metastasis, and LM without brain metastasis, was treated with whole brain RT and four cycles of ipilimumab, resulting in a complete radiological and clinical remission beyond 54 months.
Combining systemic targeted therapy and immunotherapy may result in long-term remissions, according the investigators.
“Especially in LM patients with a good performance score and low serum LDH and S100B levels these treatment options should be considered,” they wrote.
FROM ANNALS OF ONCOLOGY
Key clinical point: Leptomeningeal metastases from melanoma yield a poor prognosis, but patients may benefit from systemic targeted therapy and immunotherapy.
Major finding: Median survival for patients treated with systemic targeted therapy and/or immunotherapy (n = 21) was 21.7 weeks (range 2 to 235+ weeks).
Data source: Retrospective analysis of 39 consecutive patients treated at the Netherlands Cancer Institute during 2010-2015.
Disclosures: Dr. Geukes Foppen and coauthors reported having no disclosures.
Low Vitamin D Linked With Worse Outcome in Melanoma
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 mg/mL were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 mg/mL is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 mg/mL, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 mg/mL were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 mg/mL is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 mg/mL, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 mg/mL were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 mg/mL is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 mg/mL, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Farletuzumab may benefit patients with ovarian cancer and low CA-125 level
For patients with epithelial ovarian cancer in a platinum-sensitive first relapse, farletuzumab combined with carboplatin and taxane improved progression-free survival (PFS) and overall survival (OS) in a prespecified subgroup of patients with lower baseline levels of CA-125.
Primary analysis of the intention-to-treat population showed no significant difference in median PFS for placebo, farletuzumab at 1.25 mg/kg, and farletuzumab at 2.5 mg/kg (9.0, 9.5, and 9.7 months, respectively). However, in a prespecified subgroup analysis, patients with CA-125 not more than three times the upper limit of normal who received farletuzumab at 2.5 mg/kg had significantly improved PFS: median 13.6 months vs. 8.8 months for the placebo arm (hazard ratio, 0.49; P = .003).
“Despite these subgroup results not being a confirmatory statistical analysis according to ICH E9 guidelines, the observations warrant additional preclinical and clinical investigation,” wrote Dr. Ignace Vergote, professor in the department of gynecologic oncology at the Catholic University of Leuven, Belgium, and his colleagues. “Higher CA-125 levels may directly inhibit the immune response of farletuzumab-mediated [antibody-dependent cellular cytotoxicity] by suppressing natural killer-cell function; therefore, patients with lower CA-125 levels may exhibit a stronger farletuzumab mediated immune response,” they added (J Clin Oncol. 2016 Mar 21. doi:10.1200/JCO.2015.63.2596).
Patients with serum concentrations of farletuzumab above median levels of 57 mcg/mL had significantly improved PFS (HR, 0.679; 95% confidence interval, 0.55-0.83; P = .002). The investigators suggested that some patients may not accumulate adequate antibody levels to produce a pharmacologic effect, and they suggested that, given the observed absence of dose-limiting toxicities, higher doses of farletuzumab should be tested.
The randomized, double-blind, phase III study (MORAb-003-004) included 1,091 women with epithelial ovarian cancer in a platinum-sensitive first relapse: 361 received placebo, 367 received farletuzumab 1.25 mg/kg, and 363 received farletuzumab 2.5 mg/kg.
Overall safety profiles were similar for the three treatment arms. The most common adverse events were alopecia, nausea, neutropenia, fatigue, thrombocytopenia, and neuropathy. Anemia was more frequent in the farletuzumab groups (42.1%, 37.0%, 34.9% for farletuzumab 2.5 mg/kg, farletuzumab 1.25 mg/kg, and placebo, respectively).
For patients with epithelial ovarian cancer in a platinum-sensitive first relapse, farletuzumab combined with carboplatin and taxane improved progression-free survival (PFS) and overall survival (OS) in a prespecified subgroup of patients with lower baseline levels of CA-125.
Primary analysis of the intention-to-treat population showed no significant difference in median PFS for placebo, farletuzumab at 1.25 mg/kg, and farletuzumab at 2.5 mg/kg (9.0, 9.5, and 9.7 months, respectively). However, in a prespecified subgroup analysis, patients with CA-125 not more than three times the upper limit of normal who received farletuzumab at 2.5 mg/kg had significantly improved PFS: median 13.6 months vs. 8.8 months for the placebo arm (hazard ratio, 0.49; P = .003).
“Despite these subgroup results not being a confirmatory statistical analysis according to ICH E9 guidelines, the observations warrant additional preclinical and clinical investigation,” wrote Dr. Ignace Vergote, professor in the department of gynecologic oncology at the Catholic University of Leuven, Belgium, and his colleagues. “Higher CA-125 levels may directly inhibit the immune response of farletuzumab-mediated [antibody-dependent cellular cytotoxicity] by suppressing natural killer-cell function; therefore, patients with lower CA-125 levels may exhibit a stronger farletuzumab mediated immune response,” they added (J Clin Oncol. 2016 Mar 21. doi:10.1200/JCO.2015.63.2596).
Patients with serum concentrations of farletuzumab above median levels of 57 mcg/mL had significantly improved PFS (HR, 0.679; 95% confidence interval, 0.55-0.83; P = .002). The investigators suggested that some patients may not accumulate adequate antibody levels to produce a pharmacologic effect, and they suggested that, given the observed absence of dose-limiting toxicities, higher doses of farletuzumab should be tested.
The randomized, double-blind, phase III study (MORAb-003-004) included 1,091 women with epithelial ovarian cancer in a platinum-sensitive first relapse: 361 received placebo, 367 received farletuzumab 1.25 mg/kg, and 363 received farletuzumab 2.5 mg/kg.
Overall safety profiles were similar for the three treatment arms. The most common adverse events were alopecia, nausea, neutropenia, fatigue, thrombocytopenia, and neuropathy. Anemia was more frequent in the farletuzumab groups (42.1%, 37.0%, 34.9% for farletuzumab 2.5 mg/kg, farletuzumab 1.25 mg/kg, and placebo, respectively).
For patients with epithelial ovarian cancer in a platinum-sensitive first relapse, farletuzumab combined with carboplatin and taxane improved progression-free survival (PFS) and overall survival (OS) in a prespecified subgroup of patients with lower baseline levels of CA-125.
Primary analysis of the intention-to-treat population showed no significant difference in median PFS for placebo, farletuzumab at 1.25 mg/kg, and farletuzumab at 2.5 mg/kg (9.0, 9.5, and 9.7 months, respectively). However, in a prespecified subgroup analysis, patients with CA-125 not more than three times the upper limit of normal who received farletuzumab at 2.5 mg/kg had significantly improved PFS: median 13.6 months vs. 8.8 months for the placebo arm (hazard ratio, 0.49; P = .003).
“Despite these subgroup results not being a confirmatory statistical analysis according to ICH E9 guidelines, the observations warrant additional preclinical and clinical investigation,” wrote Dr. Ignace Vergote, professor in the department of gynecologic oncology at the Catholic University of Leuven, Belgium, and his colleagues. “Higher CA-125 levels may directly inhibit the immune response of farletuzumab-mediated [antibody-dependent cellular cytotoxicity] by suppressing natural killer-cell function; therefore, patients with lower CA-125 levels may exhibit a stronger farletuzumab mediated immune response,” they added (J Clin Oncol. 2016 Mar 21. doi:10.1200/JCO.2015.63.2596).
Patients with serum concentrations of farletuzumab above median levels of 57 mcg/mL had significantly improved PFS (HR, 0.679; 95% confidence interval, 0.55-0.83; P = .002). The investigators suggested that some patients may not accumulate adequate antibody levels to produce a pharmacologic effect, and they suggested that, given the observed absence of dose-limiting toxicities, higher doses of farletuzumab should be tested.
The randomized, double-blind, phase III study (MORAb-003-004) included 1,091 women with epithelial ovarian cancer in a platinum-sensitive first relapse: 361 received placebo, 367 received farletuzumab 1.25 mg/kg, and 363 received farletuzumab 2.5 mg/kg.
Overall safety profiles were similar for the three treatment arms. The most common adverse events were alopecia, nausea, neutropenia, fatigue, thrombocytopenia, and neuropathy. Anemia was more frequent in the farletuzumab groups (42.1%, 37.0%, 34.9% for farletuzumab 2.5 mg/kg, farletuzumab 1.25 mg/kg, and placebo, respectively).
Key clinical point: Farletuzumab combined with carboplatin and taxane improved progression-free survival (PFS) and overall survival (OS) in patients with lower baseline levels of CA-125.
Major finding: In patients with CA-125 not more than three times the upper limit of normal, median PFS was 13.6 months for the farletuzumab arm, compared with 8.8 months for the placebo arm, corresponding to a hazard ratio of 0.49 (P = .003).
Data sources: The randomized, double-blind, phase III study (MORAb-003-004) included 1,091 women with epithelial ovarian cancer in a platinum-sensitive first relapse.
Disclosures: Dr. Vergote reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
Low vitamin D linked with worse outcome in melanoma
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 ng/mL* were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 ng/mL* is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 ng/mL*, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
*Correction: An earlier version of this article used an incorrect unit of measurement for vitamin D deficiency.
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 ng/mL* were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 ng/mL* is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 ng/mL*, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
*Correction: An earlier version of this article used an incorrect unit of measurement for vitamin D deficiency.
Lower levels of vitamin D in patients with melanoma were associated with poorer survival, independent of effects from systemic inflammation indicated by simultaneous C-reactive protein (CRP) measures, according to researchers.
Multivariate analysis showed that vitamin D level was associated with overall survival (OS) (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (MSS) (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (DFS) (HR, 1.02; 95% CI, 1.00-1.04; P = .043). Patients with a vitamin D level less than 16 ng/mL* were 2.0 times more likely to die of all-cause disease than were patients with a higher level (95% CI, 1.50-2.66; P less than .001), investigators reported (J Clin Oncol. 2016 Mar 21. doi: 10.1200/JCO.2015.64.1357).
“Importantly, after adjustment for CRP, vitamin D remained an independent predictor of OS, MSS, and DFS. This suggests that, although blood levels of vitamin D and CRP are highly correlated with each other, each independently predicts clinical outcome in patients with melanoma,” wrote Dr. Shenying Fang of the University of Texas MD Anderson Cancer Center, Houston, and colleagues.
Although the role of the biomarkers in disease remains unclear and warrants further research, the authors added, “these data suggest that interventions to increase vitamin D or to reduce [systematic inflammatory response] and CRP could ultimately benefit patients with melanoma.”
Previous research has demonstrated an association between vitamin D deficiency and advanced melanoma stage, but investigations of vitamin D blood levels and melanoma risk have yielded inconsistent results. The researchers examined confounders, such as systemic inflammatory response (assessed by simultaneous CRP measurement), age, disease stage, and blood draw season to assess the relationship between vitamin D level and melanoma outcomes.
Decreased vitamin D was significantly associated with higher patient age, increased primary tumor thickness, ulcerated tumors, advanced-stage disease at blood draw, and increased CRP. Blood drawn in the fall/winter had lower vitamin D levels than that of spring/summer, reflecting average differences in sun exposure. These factors were included in the multivariable model.
A vitamin D level less than 20 ng/mL* is considered deficient, and deficient levels were significantly associated with poorer OS and DFS but not with poorer MSS. At levels below the optimal cutoff, determined by recursive partitioning, of 16 ng/mL*, patients had poorer OS (HR, 2.0; 95% CI, 1.50-2.66; P less than .001), MSS (HR, 1.76; 95% CI, 1.22-2.53; P = .003), and DFS (HR, 1.62; 95% CI, 1.04-2.53; P = .036) on univariate analysis, and associations remained significant on multivariable analysis.
The hospital-based investigation evaluated peripheral blood samples collected from 1,042 non-Hispanic white patients with melanoma from 1997 to 2009.
Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
*Correction: An earlier version of this article used an incorrect unit of measurement for vitamin D deficiency.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: After adjusting for C-reactive protein (CRP), lower vitamin D levels were independently associated with worse outcomes in melanoma patients.
Major finding: After adjusting for CRP and other confounders, vitamin D level was associated with overall survival (hazard ratio, 1.02 per unit decrease of vitamin D; 95% confidence interval, 1.01-1.04; P = .005), melanoma-specific survival (HR, 1.02; 95% CI, 1.00-1.04; P = .048), and disease-free survival (HR, 1.02; 95% CI, 1.00-1.04; P = .043).
Data sources: Peripheral blood samples from 1,042 non-Hispanic white patients with melanoma were collected from 1997 to 2009.
Disclosures: Dr. Fang reported having no disclosures. Several of his coauthors reported financial ties to industry sources.
RPS15 mutations prevalent in aggressive chronic lymphocytic leukemia
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
FROM BLOOD
Key clinical point: Aberrations in the RPS15 gene before therapy may be an indicator of aggressive pathobiology in chronic lymphocytic leukemia.
Major finding: Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing CLL, and the mutations were present before treatment in 7 of the 8.
Data sources: Whole exome sequencing of 110 samples collected before and after fludarabine, cyclophosphamide, and rituximab therapy from 41 patients with relapsed CLL.
Disclosures: Dr. Ljungström and coauthors reported having no relevant financial disclosures.