User login
Trial supports combined androgen suppression, radiotherapy for prostate cancer
Adjuvant androgen suppression with goserelin and radiotherapy at doses of 70-78 Gy improved biochemical disease-free survival of men with intermediate- and high-risk localized prostate cancer when compared against radiotherapy alone, according to results of the EORTC 22991 trial.
“Our results suggest that adding 6-month AS as a concomitant and adjuvant modality improves biochemical disease-free survival even at a dose of 78 Gy, with acceptable adverse effects. Furthermore, for patients with low-volume high-risk localized prostate cancer, our results pave the way to using a combination approach with 78-Gy RT plus a short AS duration. Such an approach should be formally compared with long-term or intermediate duration of AS,” wrote Dr. Michel Bolla, professor of radiation oncology at Grenoble University Hospital, France, and colleagues.
The 5-year biochemical disease-free survival (DFS) for radiotherapy (RT) plus androgen suppression (AS), compared with RT alone, was 82.6% (95% CI, 78.4-86.1) vs. 69.8% (95% CI, 64.9-74.2), corresponding to a hazard ratio of 0.52 (95% CI, 0.41-0.66; P less than .001). At a median follow up of 7.2 years, 118 of 410 patients (28.8%) in the RT plus AS arm and 201 of 409 patients (49.1%) in the RT arm reported events for the primary endpoint of biochemical DFS. Radiation dose had no statistically significant impact on the unadjusted treatment affect, according to exploratory heterogeneity tests (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.64.8055).
The European Organisation for Research and Treatment of Cancer (EORTC) trial 22991 recruited 819 men, median age 70 years, from 37 centers in 14 countries during 2001-2008. Patients had prostate adenocarcinoma T1b to T2a with PSA greater than 10 ng/mL or Gleason score of 7 or higher. External radiation dose levels were selected by the centers: 70 Gy (24.6%), 74 Gy (51.1%), and 78 Gy (24.2%).
There was no significant interaction between RT dose and AS (P greater than .1) in a multivariate analysis. The two arms had similar proportions of second cancers: 57 of 410 patients (13.9%) in the RT plus AS group and 46 of 409 patients (11.2%) in the RT alone group.
The study was supported in part by AstraZeneca. Dr. Bolla reported consulting or advisory roles with Janssen and AstraZeneca. Several of his coauthors reported financial ties to industry sources.
The study by Dr. Bolla and colleagues adds to the body of evidence in support of including short-term adjuvant androgen suppression (AS) when external-beam radiation therapy (EBRT) is selected as the primary treatment for intermediate- to high-risk prostate cancer.
While dose-escalated EBRT has been shown to improve biochemical disease-free survival in intermediate- and high-risk disease, the impact of AS added to EBRT has been much more consistent and pronounced.
The dose escalation component of the study addresses the question of the balance between AS and radiation dose. In the exploratory analysis, each dose level showed benefit from AS, but multivariate analysis showed no significant interaction with EBRT dose. The results seem to support that addition of AS to dose-escalated EBRT is beneficial, but whether dose-escalated EBRT plus AS is superior to standard-dose EBRT plus AS was not demonstrated.
Another consideration is the impact of AS on micrometastasis. Previous studies showed a reduction in micrometastatic disease in patients with 6 months of AS plus EBRT, compared with 3 months of AS plus EBRT. High radiation doses would not be expected to confer such benefit as AS given for a sufficient duration.
Although eliminating AS is highly desirable due to morbidity associated with the therapy, it is not advisable for the vast majority of patients with intermediate- to high-risk prostate cancer.
Dr. Alan Pollack and Dr. Matthew Abramowitz are with the department of radiation oncology at the University of Miami (Fla.). These remarks were part of their editorial accompanying Dr. Bolla and colleagues’ report (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.66.2320).
The study by Dr. Bolla and colleagues adds to the body of evidence in support of including short-term adjuvant androgen suppression (AS) when external-beam radiation therapy (EBRT) is selected as the primary treatment for intermediate- to high-risk prostate cancer.
While dose-escalated EBRT has been shown to improve biochemical disease-free survival in intermediate- and high-risk disease, the impact of AS added to EBRT has been much more consistent and pronounced.
The dose escalation component of the study addresses the question of the balance between AS and radiation dose. In the exploratory analysis, each dose level showed benefit from AS, but multivariate analysis showed no significant interaction with EBRT dose. The results seem to support that addition of AS to dose-escalated EBRT is beneficial, but whether dose-escalated EBRT plus AS is superior to standard-dose EBRT plus AS was not demonstrated.
Another consideration is the impact of AS on micrometastasis. Previous studies showed a reduction in micrometastatic disease in patients with 6 months of AS plus EBRT, compared with 3 months of AS plus EBRT. High radiation doses would not be expected to confer such benefit as AS given for a sufficient duration.
Although eliminating AS is highly desirable due to morbidity associated with the therapy, it is not advisable for the vast majority of patients with intermediate- to high-risk prostate cancer.
Dr. Alan Pollack and Dr. Matthew Abramowitz are with the department of radiation oncology at the University of Miami (Fla.). These remarks were part of their editorial accompanying Dr. Bolla and colleagues’ report (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.66.2320).
The study by Dr. Bolla and colleagues adds to the body of evidence in support of including short-term adjuvant androgen suppression (AS) when external-beam radiation therapy (EBRT) is selected as the primary treatment for intermediate- to high-risk prostate cancer.
While dose-escalated EBRT has been shown to improve biochemical disease-free survival in intermediate- and high-risk disease, the impact of AS added to EBRT has been much more consistent and pronounced.
The dose escalation component of the study addresses the question of the balance between AS and radiation dose. In the exploratory analysis, each dose level showed benefit from AS, but multivariate analysis showed no significant interaction with EBRT dose. The results seem to support that addition of AS to dose-escalated EBRT is beneficial, but whether dose-escalated EBRT plus AS is superior to standard-dose EBRT plus AS was not demonstrated.
Another consideration is the impact of AS on micrometastasis. Previous studies showed a reduction in micrometastatic disease in patients with 6 months of AS plus EBRT, compared with 3 months of AS plus EBRT. High radiation doses would not be expected to confer such benefit as AS given for a sufficient duration.
Although eliminating AS is highly desirable due to morbidity associated with the therapy, it is not advisable for the vast majority of patients with intermediate- to high-risk prostate cancer.
Dr. Alan Pollack and Dr. Matthew Abramowitz are with the department of radiation oncology at the University of Miami (Fla.). These remarks were part of their editorial accompanying Dr. Bolla and colleagues’ report (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.66.2320).
Adjuvant androgen suppression with goserelin and radiotherapy at doses of 70-78 Gy improved biochemical disease-free survival of men with intermediate- and high-risk localized prostate cancer when compared against radiotherapy alone, according to results of the EORTC 22991 trial.
“Our results suggest that adding 6-month AS as a concomitant and adjuvant modality improves biochemical disease-free survival even at a dose of 78 Gy, with acceptable adverse effects. Furthermore, for patients with low-volume high-risk localized prostate cancer, our results pave the way to using a combination approach with 78-Gy RT plus a short AS duration. Such an approach should be formally compared with long-term or intermediate duration of AS,” wrote Dr. Michel Bolla, professor of radiation oncology at Grenoble University Hospital, France, and colleagues.
The 5-year biochemical disease-free survival (DFS) for radiotherapy (RT) plus androgen suppression (AS), compared with RT alone, was 82.6% (95% CI, 78.4-86.1) vs. 69.8% (95% CI, 64.9-74.2), corresponding to a hazard ratio of 0.52 (95% CI, 0.41-0.66; P less than .001). At a median follow up of 7.2 years, 118 of 410 patients (28.8%) in the RT plus AS arm and 201 of 409 patients (49.1%) in the RT arm reported events for the primary endpoint of biochemical DFS. Radiation dose had no statistically significant impact on the unadjusted treatment affect, according to exploratory heterogeneity tests (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.64.8055).
The European Organisation for Research and Treatment of Cancer (EORTC) trial 22991 recruited 819 men, median age 70 years, from 37 centers in 14 countries during 2001-2008. Patients had prostate adenocarcinoma T1b to T2a with PSA greater than 10 ng/mL or Gleason score of 7 or higher. External radiation dose levels were selected by the centers: 70 Gy (24.6%), 74 Gy (51.1%), and 78 Gy (24.2%).
There was no significant interaction between RT dose and AS (P greater than .1) in a multivariate analysis. The two arms had similar proportions of second cancers: 57 of 410 patients (13.9%) in the RT plus AS group and 46 of 409 patients (11.2%) in the RT alone group.
The study was supported in part by AstraZeneca. Dr. Bolla reported consulting or advisory roles with Janssen and AstraZeneca. Several of his coauthors reported financial ties to industry sources.
Adjuvant androgen suppression with goserelin and radiotherapy at doses of 70-78 Gy improved biochemical disease-free survival of men with intermediate- and high-risk localized prostate cancer when compared against radiotherapy alone, according to results of the EORTC 22991 trial.
“Our results suggest that adding 6-month AS as a concomitant and adjuvant modality improves biochemical disease-free survival even at a dose of 78 Gy, with acceptable adverse effects. Furthermore, for patients with low-volume high-risk localized prostate cancer, our results pave the way to using a combination approach with 78-Gy RT plus a short AS duration. Such an approach should be formally compared with long-term or intermediate duration of AS,” wrote Dr. Michel Bolla, professor of radiation oncology at Grenoble University Hospital, France, and colleagues.
The 5-year biochemical disease-free survival (DFS) for radiotherapy (RT) plus androgen suppression (AS), compared with RT alone, was 82.6% (95% CI, 78.4-86.1) vs. 69.8% (95% CI, 64.9-74.2), corresponding to a hazard ratio of 0.52 (95% CI, 0.41-0.66; P less than .001). At a median follow up of 7.2 years, 118 of 410 patients (28.8%) in the RT plus AS arm and 201 of 409 patients (49.1%) in the RT arm reported events for the primary endpoint of biochemical DFS. Radiation dose had no statistically significant impact on the unadjusted treatment affect, according to exploratory heterogeneity tests (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.64.8055).
The European Organisation for Research and Treatment of Cancer (EORTC) trial 22991 recruited 819 men, median age 70 years, from 37 centers in 14 countries during 2001-2008. Patients had prostate adenocarcinoma T1b to T2a with PSA greater than 10 ng/mL or Gleason score of 7 or higher. External radiation dose levels were selected by the centers: 70 Gy (24.6%), 74 Gy (51.1%), and 78 Gy (24.2%).
There was no significant interaction between RT dose and AS (P greater than .1) in a multivariate analysis. The two arms had similar proportions of second cancers: 57 of 410 patients (13.9%) in the RT plus AS group and 46 of 409 patients (11.2%) in the RT alone group.
The study was supported in part by AstraZeneca. Dr. Bolla reported consulting or advisory roles with Janssen and AstraZeneca. Several of his coauthors reported financial ties to industry sources.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Adding 6-month androgen suppression (AS) to radiotherapy (RT) at doses of 70 Gy, 74 Gy, or 78 Gy improved biochemical disease-free survival (DFS) in men with intermediate- and high-risk localized prostate cancer.
Major finding: The 5-year biochemical DFS for RT plus AS, compared with RT alone, was 82.6% (95% CI, 78.4-86.1) vs. 69.8% (95% CI, 64.9-74.2), corresponding to a hazard ratio of 0.52 (95% CI, 0.41-0.66; P less than .001).
Data sources: During 2001-2008, the European Organisation for Research and Treatment of Cancer (EORTC) trial 22991 randomized 409 patients to RT and 410 patients to RT plus AS.
Disclosures: The study was supported in part by AstraZeneca. Dr. Bolla reported consulting or advisory roles with Janssen and AstraZeneca. Several of his coauthors reported financial ties to industry sources.
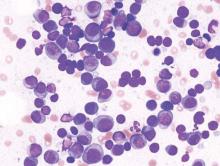
Lenalidomide-dexamethasone yields similar PFS as triplet regimens in elderly multiple myeloma patients
A comparison of lenalidomide-based treatments for multiple myeloma patients who were ineligible for stem cell transplantation showed similar progression-free survival (PFS) for two alkylator-containing triplet regimens and an alkylator-free doublet regimen but a higher risk of hematologic toxicity with a melphalan-prednisone-lenalidomide regimen.
For the triplet regimens, melphalan-prednisone-lenalidomide (MPR) and cyclophosphamide-prednisone-lenalidomide (CPR), the median PFS was 22 months, compared with 21 months for the doublet regimen lenalidomide plus low-dose dexamethasone (Rd). The hazard ratio (HR) was 0.906 (95% CI, 0.739-1.11; P = .344). The 4-year overall survival (OS) was 67% with triplet and 58% with doublet regimens (HR, 0.945; 95% CI, 0.700-1.274; P = .709) (Blood. 2016;127[9]:1102-8).
The major safety concern, according to the researchers, was the higher toxicity with MPR compared with CPR and Rd. The most frequent toxicities of grade 3 or more were hematologic, with at least one reported event in 68% of the MPR arm, 32% of CPR, and 29% or Rd patients (P less than .0001). In a post hoc analysis of safety according to patient fitness, the incidence of at least one hematologic adverse event ocurred in 75% of fit patients in the MPR arm occurred, 34% in CPR, and 29% in Rd; the incidence of at least one hematologic adverse event in intermediate fitness patients in the MPR arm was 61%, 33% in CPR, and 25% in Rd; in frail patients, 75% in MPR, 28% in CPR, and 3% in Rd (P = .001 for MPR vs. Rd and MPR vs. CPR). Nonhematologic adverse events were similar for the three groups and less than 10%.
Previous studies, such as the FIRST trial, showed the superiority of lenalidomide-containing regimens over standard treatments, but a question remained over the best drug to combine with lenalidomide – an alkylating agent or steroid. Separate analysis of the three arms further illustrated that the addition of an alkylating agent did not lead to better response or outcome. Median PFS for MPR, CPR, and Rd arms were 24, 20, and 21 months, respectively; 4-year OS rates were 65%, 68%, and 58%, respectively; overall response rates were 71%, 68%, and 74%, respectively.
Compared with the previous FIRST study, the less intense regimen in this study (Rd administered for only 9 months as induction treatment, followed by maintenance with lenalidomide at a lower dose) resulted in less hematological toxicity.
“This suggests that continuous treatment with Rd can be a valuable option for prolonging PFS and achieving a deeper response, and reducing the dose during maintenance can be a valuable strategy for improving tolerability,” wrote Dr. Valeria Magarotto of the myeloma unit in the division of hematology at the University of Torino (Italy), and colleagues. They added, “A more intensive induction treatment with Rd administered for a limited duration (9 months) followed by a less intensive continuous treatment with lenalidomide alone seems to be a sensible and effective choice.”
The phase III trial included 654 patients with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation due to advanced age (65 years and older) or comorbidities. Patients were randomized to receive MPR (n = 217), CPR (n = 220), or Rd (n = 217).
A comparison of lenalidomide-based treatments for multiple myeloma patients who were ineligible for stem cell transplantation showed similar progression-free survival (PFS) for two alkylator-containing triplet regimens and an alkylator-free doublet regimen but a higher risk of hematologic toxicity with a melphalan-prednisone-lenalidomide regimen.
For the triplet regimens, melphalan-prednisone-lenalidomide (MPR) and cyclophosphamide-prednisone-lenalidomide (CPR), the median PFS was 22 months, compared with 21 months for the doublet regimen lenalidomide plus low-dose dexamethasone (Rd). The hazard ratio (HR) was 0.906 (95% CI, 0.739-1.11; P = .344). The 4-year overall survival (OS) was 67% with triplet and 58% with doublet regimens (HR, 0.945; 95% CI, 0.700-1.274; P = .709) (Blood. 2016;127[9]:1102-8).
The major safety concern, according to the researchers, was the higher toxicity with MPR compared with CPR and Rd. The most frequent toxicities of grade 3 or more were hematologic, with at least one reported event in 68% of the MPR arm, 32% of CPR, and 29% or Rd patients (P less than .0001). In a post hoc analysis of safety according to patient fitness, the incidence of at least one hematologic adverse event ocurred in 75% of fit patients in the MPR arm occurred, 34% in CPR, and 29% in Rd; the incidence of at least one hematologic adverse event in intermediate fitness patients in the MPR arm was 61%, 33% in CPR, and 25% in Rd; in frail patients, 75% in MPR, 28% in CPR, and 3% in Rd (P = .001 for MPR vs. Rd and MPR vs. CPR). Nonhematologic adverse events were similar for the three groups and less than 10%.
Previous studies, such as the FIRST trial, showed the superiority of lenalidomide-containing regimens over standard treatments, but a question remained over the best drug to combine with lenalidomide – an alkylating agent or steroid. Separate analysis of the three arms further illustrated that the addition of an alkylating agent did not lead to better response or outcome. Median PFS for MPR, CPR, and Rd arms were 24, 20, and 21 months, respectively; 4-year OS rates were 65%, 68%, and 58%, respectively; overall response rates were 71%, 68%, and 74%, respectively.
Compared with the previous FIRST study, the less intense regimen in this study (Rd administered for only 9 months as induction treatment, followed by maintenance with lenalidomide at a lower dose) resulted in less hematological toxicity.
“This suggests that continuous treatment with Rd can be a valuable option for prolonging PFS and achieving a deeper response, and reducing the dose during maintenance can be a valuable strategy for improving tolerability,” wrote Dr. Valeria Magarotto of the myeloma unit in the division of hematology at the University of Torino (Italy), and colleagues. They added, “A more intensive induction treatment with Rd administered for a limited duration (9 months) followed by a less intensive continuous treatment with lenalidomide alone seems to be a sensible and effective choice.”
The phase III trial included 654 patients with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation due to advanced age (65 years and older) or comorbidities. Patients were randomized to receive MPR (n = 217), CPR (n = 220), or Rd (n = 217).
A comparison of lenalidomide-based treatments for multiple myeloma patients who were ineligible for stem cell transplantation showed similar progression-free survival (PFS) for two alkylator-containing triplet regimens and an alkylator-free doublet regimen but a higher risk of hematologic toxicity with a melphalan-prednisone-lenalidomide regimen.
For the triplet regimens, melphalan-prednisone-lenalidomide (MPR) and cyclophosphamide-prednisone-lenalidomide (CPR), the median PFS was 22 months, compared with 21 months for the doublet regimen lenalidomide plus low-dose dexamethasone (Rd). The hazard ratio (HR) was 0.906 (95% CI, 0.739-1.11; P = .344). The 4-year overall survival (OS) was 67% with triplet and 58% with doublet regimens (HR, 0.945; 95% CI, 0.700-1.274; P = .709) (Blood. 2016;127[9]:1102-8).
The major safety concern, according to the researchers, was the higher toxicity with MPR compared with CPR and Rd. The most frequent toxicities of grade 3 or more were hematologic, with at least one reported event in 68% of the MPR arm, 32% of CPR, and 29% or Rd patients (P less than .0001). In a post hoc analysis of safety according to patient fitness, the incidence of at least one hematologic adverse event ocurred in 75% of fit patients in the MPR arm occurred, 34% in CPR, and 29% in Rd; the incidence of at least one hematologic adverse event in intermediate fitness patients in the MPR arm was 61%, 33% in CPR, and 25% in Rd; in frail patients, 75% in MPR, 28% in CPR, and 3% in Rd (P = .001 for MPR vs. Rd and MPR vs. CPR). Nonhematologic adverse events were similar for the three groups and less than 10%.
Previous studies, such as the FIRST trial, showed the superiority of lenalidomide-containing regimens over standard treatments, but a question remained over the best drug to combine with lenalidomide – an alkylating agent or steroid. Separate analysis of the three arms further illustrated that the addition of an alkylating agent did not lead to better response or outcome. Median PFS for MPR, CPR, and Rd arms were 24, 20, and 21 months, respectively; 4-year OS rates were 65%, 68%, and 58%, respectively; overall response rates were 71%, 68%, and 74%, respectively.
Compared with the previous FIRST study, the less intense regimen in this study (Rd administered for only 9 months as induction treatment, followed by maintenance with lenalidomide at a lower dose) resulted in less hematological toxicity.
“This suggests that continuous treatment with Rd can be a valuable option for prolonging PFS and achieving a deeper response, and reducing the dose during maintenance can be a valuable strategy for improving tolerability,” wrote Dr. Valeria Magarotto of the myeloma unit in the division of hematology at the University of Torino (Italy), and colleagues. They added, “A more intensive induction treatment with Rd administered for a limited duration (9 months) followed by a less intensive continuous treatment with lenalidomide alone seems to be a sensible and effective choice.”
The phase III trial included 654 patients with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation due to advanced age (65 years and older) or comorbidities. Patients were randomized to receive MPR (n = 217), CPR (n = 220), or Rd (n = 217).
FROM BLOOD
Key clinical point: In elderly patients with newly diagnosed multiple myeloma, progression-free survival was similar for alkylator-containing triplet regimens and an alkylator-free doublet regimen, but the doublet resulted in less hematologic toxicity.
Major finding: Median PFS for MPR, CPR and Rd arms were 24, 20, and 21 months, respectively; 4-year OS rates were 65%, 68%, and 58%, respectively.
Data sources: Phase III trial of 654 patients randomized to receive melphalan-prednisone-lenalidomide (n = 217), cyclophosphamide-prednisone-lenalidomide (n = 220), or lenalidomide plus low-dose dexamethasone (n = 217).
Disclosures: Dr. Magarotto reported having no disclosures. Several of her coauthors reported financial ties to industry sources.
RECIST underestimates benefit of pembrolizumab in subset of melanoma patients
Certain patients with advanced melanoma treated with pembrolizumab had unique response patterns, such as early or delayed tumor pseudoprogression, and Response Evaluation Criteria in Solid Tumors (RECIST) criteria might underestimate the immunotherapy benefit in this subset.
Among 592 patients who survived 12 weeks or more, 84 (14%) had progressive disease per RECIST v1.1 but nonprogressive disease per immune-related response criteria (irRC). Overall survival (OS) was longer in this group compared with the 177 patients who had progressive disease per both RECIST v1.1 and irRC: median OS was 22.5 months (95% CI, 16.5 to not yet reached) vs. 8.4 months (95% CI, 6.6 to 9.9), investigators reported (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.0391).
“RECIST v1.1 might underestimate the benefit of pembrolizumab in approximately 15% of patients. These data suggest that patients may benefit from receiving treatment beyond initial evidence of radiographic progression and thus support the use of modified response criteria on the basis of immune-related response patterns. Furthermore, clinicians aware to these criteria might be able to avoid otherwise premature termination of potentially effective treatment,” wrote Dr. F. Stephen Hodi Jr., director of immuno-oncology at Dana Farber Cancer Institute, Boston, and colleagues.
Two-year OS rates for patients with nonprogressive disease per both criteria, progressive disease per RECIST v1.1 and nonprogressive disease per irRC, and progressive disease per both criteria were 77.6%, 37.5%, and 17.3%, respectively.
Conventional response criteria such as RECIST might underestimate benefit of immune checkpoint blockade, such as ipilimumab and pembrolizumab, because objective response and prolonged disease stabilization can occur after an initial increase in tumor burden or new lesions. To better characterize atypical response patterns observed in trials of ipilimumab in melanoma, irRC were developed, where the initial evidence of disease progression is handled differently. The current study retrospectively examined responses from KEYNOTE-001 melanoma expansion cohorts, which enrolled 655 patients with advanced melanoma; 327 had 28 weeks or more of imaging follow up and were eligible for atypical response analysis.
In total, 24 of 327 patients (7.3%) had atypical responses, including 15 (4.5%) with early pseudoprogression and nine (2.8%) with delayed pseudoprogression. Patterns of atypical response included regression of tumor burden and stable disease despite the development of new lesions, and initial increases in the size of target lesions followed by decreases without evidence of new lesions.
The irRC uses bidimensional tumor measurements, which introduce greater variability than unidimensional measurements. In addition, the investigators note that irRC may not fully capture all patterns of clinical response to immunotherapies.
“Given the rapid development of effective immuno-oncology agents in multiple cancers, there is a growing effort to develop new standard response criteria for patients treated with immunotherapy to provide for robust clinical end points in evaluating these new treatments,” the investigators wrote.
Certain patients with advanced melanoma treated with pembrolizumab had unique response patterns, such as early or delayed tumor pseudoprogression, and Response Evaluation Criteria in Solid Tumors (RECIST) criteria might underestimate the immunotherapy benefit in this subset.
Among 592 patients who survived 12 weeks or more, 84 (14%) had progressive disease per RECIST v1.1 but nonprogressive disease per immune-related response criteria (irRC). Overall survival (OS) was longer in this group compared with the 177 patients who had progressive disease per both RECIST v1.1 and irRC: median OS was 22.5 months (95% CI, 16.5 to not yet reached) vs. 8.4 months (95% CI, 6.6 to 9.9), investigators reported (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.0391).
“RECIST v1.1 might underestimate the benefit of pembrolizumab in approximately 15% of patients. These data suggest that patients may benefit from receiving treatment beyond initial evidence of radiographic progression and thus support the use of modified response criteria on the basis of immune-related response patterns. Furthermore, clinicians aware to these criteria might be able to avoid otherwise premature termination of potentially effective treatment,” wrote Dr. F. Stephen Hodi Jr., director of immuno-oncology at Dana Farber Cancer Institute, Boston, and colleagues.
Two-year OS rates for patients with nonprogressive disease per both criteria, progressive disease per RECIST v1.1 and nonprogressive disease per irRC, and progressive disease per both criteria were 77.6%, 37.5%, and 17.3%, respectively.
Conventional response criteria such as RECIST might underestimate benefit of immune checkpoint blockade, such as ipilimumab and pembrolizumab, because objective response and prolonged disease stabilization can occur after an initial increase in tumor burden or new lesions. To better characterize atypical response patterns observed in trials of ipilimumab in melanoma, irRC were developed, where the initial evidence of disease progression is handled differently. The current study retrospectively examined responses from KEYNOTE-001 melanoma expansion cohorts, which enrolled 655 patients with advanced melanoma; 327 had 28 weeks or more of imaging follow up and were eligible for atypical response analysis.
In total, 24 of 327 patients (7.3%) had atypical responses, including 15 (4.5%) with early pseudoprogression and nine (2.8%) with delayed pseudoprogression. Patterns of atypical response included regression of tumor burden and stable disease despite the development of new lesions, and initial increases in the size of target lesions followed by decreases without evidence of new lesions.
The irRC uses bidimensional tumor measurements, which introduce greater variability than unidimensional measurements. In addition, the investigators note that irRC may not fully capture all patterns of clinical response to immunotherapies.
“Given the rapid development of effective immuno-oncology agents in multiple cancers, there is a growing effort to develop new standard response criteria for patients treated with immunotherapy to provide for robust clinical end points in evaluating these new treatments,” the investigators wrote.
Certain patients with advanced melanoma treated with pembrolizumab had unique response patterns, such as early or delayed tumor pseudoprogression, and Response Evaluation Criteria in Solid Tumors (RECIST) criteria might underestimate the immunotherapy benefit in this subset.
Among 592 patients who survived 12 weeks or more, 84 (14%) had progressive disease per RECIST v1.1 but nonprogressive disease per immune-related response criteria (irRC). Overall survival (OS) was longer in this group compared with the 177 patients who had progressive disease per both RECIST v1.1 and irRC: median OS was 22.5 months (95% CI, 16.5 to not yet reached) vs. 8.4 months (95% CI, 6.6 to 9.9), investigators reported (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.0391).
“RECIST v1.1 might underestimate the benefit of pembrolizumab in approximately 15% of patients. These data suggest that patients may benefit from receiving treatment beyond initial evidence of radiographic progression and thus support the use of modified response criteria on the basis of immune-related response patterns. Furthermore, clinicians aware to these criteria might be able to avoid otherwise premature termination of potentially effective treatment,” wrote Dr. F. Stephen Hodi Jr., director of immuno-oncology at Dana Farber Cancer Institute, Boston, and colleagues.
Two-year OS rates for patients with nonprogressive disease per both criteria, progressive disease per RECIST v1.1 and nonprogressive disease per irRC, and progressive disease per both criteria were 77.6%, 37.5%, and 17.3%, respectively.
Conventional response criteria such as RECIST might underestimate benefit of immune checkpoint blockade, such as ipilimumab and pembrolizumab, because objective response and prolonged disease stabilization can occur after an initial increase in tumor burden or new lesions. To better characterize atypical response patterns observed in trials of ipilimumab in melanoma, irRC were developed, where the initial evidence of disease progression is handled differently. The current study retrospectively examined responses from KEYNOTE-001 melanoma expansion cohorts, which enrolled 655 patients with advanced melanoma; 327 had 28 weeks or more of imaging follow up and were eligible for atypical response analysis.
In total, 24 of 327 patients (7.3%) had atypical responses, including 15 (4.5%) with early pseudoprogression and nine (2.8%) with delayed pseudoprogression. Patterns of atypical response included regression of tumor burden and stable disease despite the development of new lesions, and initial increases in the size of target lesions followed by decreases without evidence of new lesions.
The irRC uses bidimensional tumor measurements, which introduce greater variability than unidimensional measurements. In addition, the investigators note that irRC may not fully capture all patterns of clinical response to immunotherapies.
“Given the rapid development of effective immuno-oncology agents in multiple cancers, there is a growing effort to develop new standard response criteria for patients treated with immunotherapy to provide for robust clinical end points in evaluating these new treatments,” the investigators wrote.
Key clinical point: Approximately 15% of patients with advanced melanoma treated with pembrolizumab had unique response patterns, and RECIST criteria may underestimate the immunotherapy benefit in this subset.
Major finding: Among 592 patients, 84 (14%) had progressive disease per RECIST v1.1 but nonprogressive disease per immune-related response criteria (irRC); overall survival was longer in this group compared with patients who had progressive disease per both RECIST v1.1 and irRC (median OS 22.5 vs. 8.4 months, respectively).
Data sources: The KEYNOTE-001 expansion cohorts included 655 patients with advanced melanoma; 327 had 28 weeks or more of imaging follow up for atypical response analysis.
Disclosures: Dr. Hodi reported financial ties to Merck, Novartis, Bristol-Myers Squibb, Genentech, and Dana-Farber Cancer Institute (intellectual property). Several of his coauthors reported financial ties to industry sources.
Mets to liver linked with lowest survival in men with CRPC
The baseline presence of visceral disease was a negative prognostic factor in men with castration-resistant prostate cancer (CRPC), and the site of metastasis impacted survival: Overall survival (OS) was worse with liver metastasis than lung metastasis, which, in turn, was worse than bone metastasis with or without lymph node (LN) involvement.
Median OS for men with metastasis in the liver was 13.5 months (95% confidence interval, 12.7-14.4); in the lung, 19.4 months (17.8-20.7); and in the bone, 21.3 months (20.8-21.9). Men with liver vs. lung metastasis had a significantly increased risk of death, with a pooled multivariable hazard ratio of 1.52 (95% CI, 1.35-1.73; P = .0001). Men with lung vs. bone metastasis had a significantly increased risk of death, with a pooled multivariable HR of 1.14 (95% CI, 1.04-1.25; P = .007), investigators reported online in the Journal of Clinical Oncology.
The authors observed little variability in OS across trials for each metastatic site, and suggested that differences observed in median OS from trial to trial could be explained by the relative proportion of metastatic subsets in each trial.
“The heterogeneity of men with (metastatic) CRPC enrolled into trials and the substantially different outcomes among these subgroups highlight the importance of reporting OS by disease location,” wrote Dr. Susan Halabi of Duke University Medical Center and colleagues. They added, “These data suggest that the distribution of patients across the following categories should be routinely reported: LN-only disease, bone with or without LN involvement with no visceral metastases, any lung metastases (but no liver), and any liver metastases.” (J Clin Oncol. 2016 Mar 7. doi: 10.1200/JCO.2015.65.7270).
The meta-analysis evaluated nine randomized, controlled, phase III trials published from 2004 to 2015, including 8,736 men with metastatic CRPC who received docetaxel with or without an experimental agent. The median age of patients was 68 years. The median follow-up time was 21.8 months (range, 0-91.2 months), and there were 5,470 deaths.
Most patients had bone metastasis (6,356; 72.8%); visceral disease was observed in 1,815 patients (20.8%); and LN-only disease was present in 565 patients (6.4%). Of those with visceral disease, 791 (9.1%) had lung metastasis and 752 (8.6%) had liver metastasis (173 had both lung and liver metastases and were included in the liver category).
The authors noted as a limitation of the study that abiraterone acetate or enzalutamide, now generally administered before chemotherapy, was not used in most of the studies evaluated.
The baseline presence of visceral disease was a negative prognostic factor in men with castration-resistant prostate cancer (CRPC), and the site of metastasis impacted survival: Overall survival (OS) was worse with liver metastasis than lung metastasis, which, in turn, was worse than bone metastasis with or without lymph node (LN) involvement.
Median OS for men with metastasis in the liver was 13.5 months (95% confidence interval, 12.7-14.4); in the lung, 19.4 months (17.8-20.7); and in the bone, 21.3 months (20.8-21.9). Men with liver vs. lung metastasis had a significantly increased risk of death, with a pooled multivariable hazard ratio of 1.52 (95% CI, 1.35-1.73; P = .0001). Men with lung vs. bone metastasis had a significantly increased risk of death, with a pooled multivariable HR of 1.14 (95% CI, 1.04-1.25; P = .007), investigators reported online in the Journal of Clinical Oncology.
The authors observed little variability in OS across trials for each metastatic site, and suggested that differences observed in median OS from trial to trial could be explained by the relative proportion of metastatic subsets in each trial.
“The heterogeneity of men with (metastatic) CRPC enrolled into trials and the substantially different outcomes among these subgroups highlight the importance of reporting OS by disease location,” wrote Dr. Susan Halabi of Duke University Medical Center and colleagues. They added, “These data suggest that the distribution of patients across the following categories should be routinely reported: LN-only disease, bone with or without LN involvement with no visceral metastases, any lung metastases (but no liver), and any liver metastases.” (J Clin Oncol. 2016 Mar 7. doi: 10.1200/JCO.2015.65.7270).
The meta-analysis evaluated nine randomized, controlled, phase III trials published from 2004 to 2015, including 8,736 men with metastatic CRPC who received docetaxel with or without an experimental agent. The median age of patients was 68 years. The median follow-up time was 21.8 months (range, 0-91.2 months), and there were 5,470 deaths.
Most patients had bone metastasis (6,356; 72.8%); visceral disease was observed in 1,815 patients (20.8%); and LN-only disease was present in 565 patients (6.4%). Of those with visceral disease, 791 (9.1%) had lung metastasis and 752 (8.6%) had liver metastasis (173 had both lung and liver metastases and were included in the liver category).
The authors noted as a limitation of the study that abiraterone acetate or enzalutamide, now generally administered before chemotherapy, was not used in most of the studies evaluated.
The baseline presence of visceral disease was a negative prognostic factor in men with castration-resistant prostate cancer (CRPC), and the site of metastasis impacted survival: Overall survival (OS) was worse with liver metastasis than lung metastasis, which, in turn, was worse than bone metastasis with or without lymph node (LN) involvement.
Median OS for men with metastasis in the liver was 13.5 months (95% confidence interval, 12.7-14.4); in the lung, 19.4 months (17.8-20.7); and in the bone, 21.3 months (20.8-21.9). Men with liver vs. lung metastasis had a significantly increased risk of death, with a pooled multivariable hazard ratio of 1.52 (95% CI, 1.35-1.73; P = .0001). Men with lung vs. bone metastasis had a significantly increased risk of death, with a pooled multivariable HR of 1.14 (95% CI, 1.04-1.25; P = .007), investigators reported online in the Journal of Clinical Oncology.
The authors observed little variability in OS across trials for each metastatic site, and suggested that differences observed in median OS from trial to trial could be explained by the relative proportion of metastatic subsets in each trial.
“The heterogeneity of men with (metastatic) CRPC enrolled into trials and the substantially different outcomes among these subgroups highlight the importance of reporting OS by disease location,” wrote Dr. Susan Halabi of Duke University Medical Center and colleagues. They added, “These data suggest that the distribution of patients across the following categories should be routinely reported: LN-only disease, bone with or without LN involvement with no visceral metastases, any lung metastases (but no liver), and any liver metastases.” (J Clin Oncol. 2016 Mar 7. doi: 10.1200/JCO.2015.65.7270).
The meta-analysis evaluated nine randomized, controlled, phase III trials published from 2004 to 2015, including 8,736 men with metastatic CRPC who received docetaxel with or without an experimental agent. The median age of patients was 68 years. The median follow-up time was 21.8 months (range, 0-91.2 months), and there were 5,470 deaths.
Most patients had bone metastasis (6,356; 72.8%); visceral disease was observed in 1,815 patients (20.8%); and LN-only disease was present in 565 patients (6.4%). Of those with visceral disease, 791 (9.1%) had lung metastasis and 752 (8.6%) had liver metastasis (173 had both lung and liver metastases and were included in the liver category).
The authors noted as a limitation of the study that abiraterone acetate or enzalutamide, now generally administered before chemotherapy, was not used in most of the studies evaluated.
Key clinical point: In men with castration-resistant prostate cancer treated with docetaxel, overall survival was worse with liver metastasis than lung metastasis, which, in turn, was worse than bone metastasis with or without lymph node involvement.
Major finding: Median OS for men with metastasis in the liver was 13.5 months (95% CI, 12.7-14.4); lung, 19.4 (17.8-20.7); and bone, 21.3 (20.8-21.9).
Data sources: A meta-analysis of nine randomized, controlled, phase III trials published from 2004 to 2015, including 8,736 men with metastatic CRPC who received docetaxel with or without an experimental agent.
Disclosures: Dr. Halabi reported financial ties to Dendreon, Sanofi-Aventis, Bayer, Novartis, Medivation, Janssen Biotech, Pfizer, Bristol-Myers Squibb, KangLaiTe, Janssen Oncology, Astellas Pharma, and ImClone Systems. Several of his coauthors reported financial ties to industry sources.
PFS a surrogate for overall survival in soft tissue sarcoma trials
The use of progression-free survival and response rate as surrogates for overall survival were supported by significant correlations between the endpoints, in randomized trials of advanced soft tissue sarcoma.
However, 3-month progression-free survival (PFS) and 6-month PFS were not significantly correlated with overall survival (OS) and were not recommended as surrogates for OS, according to the researchers.
Significant correlations were observed between overall survival and PFS (correlation coefficient, 0.61) and overall survival and response rate (0.51). Correlations between 3-month PFS and 6-month PFS with overall survival (0.27 and 0.31, respectively) were not significant.
“In soft tissue sarcoma, trial design is particularly challenging, owing to the rarity and heterogeneity of this disease. Time-based endpoints including PFS, 3-month PFS, and 6-month PFS are gaining popularity as primary endpoints in phase III RCTs [randomized controlled trials], despite the fact that current data support their use only to screen for effective drugs in phase II trials,” wrote Dr. Alona Zer of Princess Margaret Cancer Centre and the University of Toronto and colleagues (J Clin Oncol. 2016 March 7. Doi: 10.1200/JCO.2016.66.4581).
“Data show that the assessment of outcomes as a single point in time … only rarely mirrors the hazards of the same endpoint. … As such, the odds ratio for 3-month PFS or 6-month PFS likely do not approximate the hazard ratio for PFS, making it difficult to justify the use of these endpoints in definitive phase III trials.”
PFS and overall survival have shown poor correlation in other cancer types, and evidence suggests that survival post progression may influence the association, with weaker correlations at longer survival post progression. The majority of soft tissue sarcoma reports had survival post progression of less than 12 months, likely explaining the high correlation between PFS and overall survival.
The investigators performed a systematic review of 52 randomized controlled trials, published from 1974 to 2014, that included 9,762 patients who received systemic therapy for advanced/metastatic soft tissue sarcoma.
Comprehensive toxicity assessment was included in just 20 studies (47%) and poorly reported in 6 studies (14%). Few studies included quality of life as a secondary endpoint. The authors noted that in the soft tissue sarcoma setting in which the purpose of systemic treatment may be palliation of symptoms, this is a concern.
Over the 4 decades represented by the systematic review, several trends appeared. Overall, a low proportion of studies included intent-to-treat analyses and clearly defined primary endpoints, but these characteristics improved over time. Endpoint selection has shifted away from response rate in favor of time-based events, including PFS, 3-month PFS, and 6-month PFS. Overall survival was the primary endpoint in just 4% of studies. Studies published in the last 2 decades were more likely to be supported by industry (5% vs. 35%).
Dr. Zer and coauthors reported having no relevant financial disclosures.
In evaluating drug efficacy in oncology clinical trials, overall survival is considered the most reliable and meaningful endpoint because it is objective, precise, and easy to measure. However, it requires a large sample size, prolonged follow-up, and may be confounded by postprogression therapies. Given these drawbacks, surrogate markers are especially useful for rare diseases and diseases with effective subsequent-line therapies.
For a practical definition of surrogate endpoints, researchers use criteria that describe the association between surrogate and clinical endpoints at the individual level and trial level as requirements for validation.
In their systematic review, Zer et al. investigated trial-level surrogacy of progression-free survival and response rate for overall survival in advanced soft tissue sarcoma, concluding that PFS and response rate are appropriate surrogates of overall survival. For trial-level surrogacy analysis, the effective sample size is the number of trials, which should be large enough to reliably estimate the correlation between treatment effects on the surrogate and clinical endpoints. Of note in this review, the sample size was 13 trials.
The influence of postprogression survival on the association between PFS and overall survival is important in this analysis. The median postprogression survival was less than 12 months in most of the studies included, and this figure might improve when more effective drugs become available. Longer postprogression survival may translate to a lower correlation between PFS and overall survival.
Another challenge to the surrogacy of an endpoint may come from new treatments in which the mode of action is substantially different from that used to validate the surrogate. Caution is required in generalizing the validation of surrogate endpoints.
In general, time-to-event outcomes assessed at a single time point (for example, 3-month and 6-month PFS) may be misleading. This is also true of the median value of a time-to-event outcome, such as median PFS. For trial-level surrogacy validation, the hazard ratio is the most appropriate measure for time-to-event outcomes.
Efforts to improve the validation of surrogate endpoints are important in this era of personalized medicine and rapid development of oncology drugs. Surrogate markers usually allow for smaller trials and shorter completion times.
Fengman Zhao, Ph.D., is a biostatistician at Dana-Farber Cancer Institute, Boston. These remarks were part of an editorial accompanying the report by Zer et al. (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.3437).
In evaluating drug efficacy in oncology clinical trials, overall survival is considered the most reliable and meaningful endpoint because it is objective, precise, and easy to measure. However, it requires a large sample size, prolonged follow-up, and may be confounded by postprogression therapies. Given these drawbacks, surrogate markers are especially useful for rare diseases and diseases with effective subsequent-line therapies.
For a practical definition of surrogate endpoints, researchers use criteria that describe the association between surrogate and clinical endpoints at the individual level and trial level as requirements for validation.
In their systematic review, Zer et al. investigated trial-level surrogacy of progression-free survival and response rate for overall survival in advanced soft tissue sarcoma, concluding that PFS and response rate are appropriate surrogates of overall survival. For trial-level surrogacy analysis, the effective sample size is the number of trials, which should be large enough to reliably estimate the correlation between treatment effects on the surrogate and clinical endpoints. Of note in this review, the sample size was 13 trials.
The influence of postprogression survival on the association between PFS and overall survival is important in this analysis. The median postprogression survival was less than 12 months in most of the studies included, and this figure might improve when more effective drugs become available. Longer postprogression survival may translate to a lower correlation between PFS and overall survival.
Another challenge to the surrogacy of an endpoint may come from new treatments in which the mode of action is substantially different from that used to validate the surrogate. Caution is required in generalizing the validation of surrogate endpoints.
In general, time-to-event outcomes assessed at a single time point (for example, 3-month and 6-month PFS) may be misleading. This is also true of the median value of a time-to-event outcome, such as median PFS. For trial-level surrogacy validation, the hazard ratio is the most appropriate measure for time-to-event outcomes.
Efforts to improve the validation of surrogate endpoints are important in this era of personalized medicine and rapid development of oncology drugs. Surrogate markers usually allow for smaller trials and shorter completion times.
Fengman Zhao, Ph.D., is a biostatistician at Dana-Farber Cancer Institute, Boston. These remarks were part of an editorial accompanying the report by Zer et al. (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.3437).
In evaluating drug efficacy in oncology clinical trials, overall survival is considered the most reliable and meaningful endpoint because it is objective, precise, and easy to measure. However, it requires a large sample size, prolonged follow-up, and may be confounded by postprogression therapies. Given these drawbacks, surrogate markers are especially useful for rare diseases and diseases with effective subsequent-line therapies.
For a practical definition of surrogate endpoints, researchers use criteria that describe the association between surrogate and clinical endpoints at the individual level and trial level as requirements for validation.
In their systematic review, Zer et al. investigated trial-level surrogacy of progression-free survival and response rate for overall survival in advanced soft tissue sarcoma, concluding that PFS and response rate are appropriate surrogates of overall survival. For trial-level surrogacy analysis, the effective sample size is the number of trials, which should be large enough to reliably estimate the correlation between treatment effects on the surrogate and clinical endpoints. Of note in this review, the sample size was 13 trials.
The influence of postprogression survival on the association between PFS and overall survival is important in this analysis. The median postprogression survival was less than 12 months in most of the studies included, and this figure might improve when more effective drugs become available. Longer postprogression survival may translate to a lower correlation between PFS and overall survival.
Another challenge to the surrogacy of an endpoint may come from new treatments in which the mode of action is substantially different from that used to validate the surrogate. Caution is required in generalizing the validation of surrogate endpoints.
In general, time-to-event outcomes assessed at a single time point (for example, 3-month and 6-month PFS) may be misleading. This is also true of the median value of a time-to-event outcome, such as median PFS. For trial-level surrogacy validation, the hazard ratio is the most appropriate measure for time-to-event outcomes.
Efforts to improve the validation of surrogate endpoints are important in this era of personalized medicine and rapid development of oncology drugs. Surrogate markers usually allow for smaller trials and shorter completion times.
Fengman Zhao, Ph.D., is a biostatistician at Dana-Farber Cancer Institute, Boston. These remarks were part of an editorial accompanying the report by Zer et al. (J Clin Oncol. 2016 March 7. doi: 10.1200/JCO.2015.64.3437).
The use of progression-free survival and response rate as surrogates for overall survival were supported by significant correlations between the endpoints, in randomized trials of advanced soft tissue sarcoma.
However, 3-month progression-free survival (PFS) and 6-month PFS were not significantly correlated with overall survival (OS) and were not recommended as surrogates for OS, according to the researchers.
Significant correlations were observed between overall survival and PFS (correlation coefficient, 0.61) and overall survival and response rate (0.51). Correlations between 3-month PFS and 6-month PFS with overall survival (0.27 and 0.31, respectively) were not significant.
“In soft tissue sarcoma, trial design is particularly challenging, owing to the rarity and heterogeneity of this disease. Time-based endpoints including PFS, 3-month PFS, and 6-month PFS are gaining popularity as primary endpoints in phase III RCTs [randomized controlled trials], despite the fact that current data support their use only to screen for effective drugs in phase II trials,” wrote Dr. Alona Zer of Princess Margaret Cancer Centre and the University of Toronto and colleagues (J Clin Oncol. 2016 March 7. Doi: 10.1200/JCO.2016.66.4581).
“Data show that the assessment of outcomes as a single point in time … only rarely mirrors the hazards of the same endpoint. … As such, the odds ratio for 3-month PFS or 6-month PFS likely do not approximate the hazard ratio for PFS, making it difficult to justify the use of these endpoints in definitive phase III trials.”
PFS and overall survival have shown poor correlation in other cancer types, and evidence suggests that survival post progression may influence the association, with weaker correlations at longer survival post progression. The majority of soft tissue sarcoma reports had survival post progression of less than 12 months, likely explaining the high correlation between PFS and overall survival.
The investigators performed a systematic review of 52 randomized controlled trials, published from 1974 to 2014, that included 9,762 patients who received systemic therapy for advanced/metastatic soft tissue sarcoma.
Comprehensive toxicity assessment was included in just 20 studies (47%) and poorly reported in 6 studies (14%). Few studies included quality of life as a secondary endpoint. The authors noted that in the soft tissue sarcoma setting in which the purpose of systemic treatment may be palliation of symptoms, this is a concern.
Over the 4 decades represented by the systematic review, several trends appeared. Overall, a low proportion of studies included intent-to-treat analyses and clearly defined primary endpoints, but these characteristics improved over time. Endpoint selection has shifted away from response rate in favor of time-based events, including PFS, 3-month PFS, and 6-month PFS. Overall survival was the primary endpoint in just 4% of studies. Studies published in the last 2 decades were more likely to be supported by industry (5% vs. 35%).
Dr. Zer and coauthors reported having no relevant financial disclosures.
The use of progression-free survival and response rate as surrogates for overall survival were supported by significant correlations between the endpoints, in randomized trials of advanced soft tissue sarcoma.
However, 3-month progression-free survival (PFS) and 6-month PFS were not significantly correlated with overall survival (OS) and were not recommended as surrogates for OS, according to the researchers.
Significant correlations were observed between overall survival and PFS (correlation coefficient, 0.61) and overall survival and response rate (0.51). Correlations between 3-month PFS and 6-month PFS with overall survival (0.27 and 0.31, respectively) were not significant.
“In soft tissue sarcoma, trial design is particularly challenging, owing to the rarity and heterogeneity of this disease. Time-based endpoints including PFS, 3-month PFS, and 6-month PFS are gaining popularity as primary endpoints in phase III RCTs [randomized controlled trials], despite the fact that current data support their use only to screen for effective drugs in phase II trials,” wrote Dr. Alona Zer of Princess Margaret Cancer Centre and the University of Toronto and colleagues (J Clin Oncol. 2016 March 7. Doi: 10.1200/JCO.2016.66.4581).
“Data show that the assessment of outcomes as a single point in time … only rarely mirrors the hazards of the same endpoint. … As such, the odds ratio for 3-month PFS or 6-month PFS likely do not approximate the hazard ratio for PFS, making it difficult to justify the use of these endpoints in definitive phase III trials.”
PFS and overall survival have shown poor correlation in other cancer types, and evidence suggests that survival post progression may influence the association, with weaker correlations at longer survival post progression. The majority of soft tissue sarcoma reports had survival post progression of less than 12 months, likely explaining the high correlation between PFS and overall survival.
The investigators performed a systematic review of 52 randomized controlled trials, published from 1974 to 2014, that included 9,762 patients who received systemic therapy for advanced/metastatic soft tissue sarcoma.
Comprehensive toxicity assessment was included in just 20 studies (47%) and poorly reported in 6 studies (14%). Few studies included quality of life as a secondary endpoint. The authors noted that in the soft tissue sarcoma setting in which the purpose of systemic treatment may be palliation of symptoms, this is a concern.
Over the 4 decades represented by the systematic review, several trends appeared. Overall, a low proportion of studies included intent-to-treat analyses and clearly defined primary endpoints, but these characteristics improved over time. Endpoint selection has shifted away from response rate in favor of time-based events, including PFS, 3-month PFS, and 6-month PFS. Overall survival was the primary endpoint in just 4% of studies. Studies published in the last 2 decades were more likely to be supported by industry (5% vs. 35%).
Dr. Zer and coauthors reported having no relevant financial disclosures.
Key clinical point: In randomized trials of advanced soft tissue sarcoma, intermediate endpoints of progression-free survival and response rate were significantly correlated with overall survival; 3-month PFS and 6-month PFS were not significantly correlated with overall survival.
Major finding: The correlation coefficient between overall survival and PFS was 0.61; overall survival and response rate, 0.51; overall survival and 3-month PFS, 0.27; and overall survival and 6-month PFS, 0.31.
Data sources: A systematic review of 52 randomized controlled trials published from 1974 to 2014 involving 9,762 patients who received systemic therapy for advanced/metastatic soft tissue sarcoma.
Disclosures: Dr. Zer and coauthors reported having no relevant financial disclosures.
HDAC inhibition may reverse anthracycline resistance in patients with sarcoma
In patients with advanced solid tumors, including sarcoma, the combination of panobinostat, a histone deacetylase (HDAC) inhibitor, and the anthracycline epirubicin demonstrated a correlation between neutropenia, peripheral blood mononucleocyte (PBMC) histone acetylation, and clinical benefit. Acquired topoisomerase resistance was reversed in 8 of 14 patients, suggesting HDAC inhibition reverses resistance.
In 37 evaluable patients, 4 (11%) had partial responses and 17 (46%) had stable disease. The median time to progression and median overall survival were 3.1 (95% CI, 1.8 to 4.6) months and 7.3 (5.9 to 10.3) months, respectively. All four patients with objective partial response had progressed on previous topoisomerase II inhibitors.
“The potential for prolonged treatment with an anthracycline in combination with an HDAC inhibitor speaks to the tolerability of this regimen. This study suggests that further investigation of HDAC inhibition in combination with DNA-damaging agents in defined advanced sarcoma subtypes to validate these preliminary findings is warranted,” wrote Dr. Scott Thomas of the Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, and colleagues (Ann Oncol. 2016 Feb 21. doi: 10.1093/annonc/mdw044).
HDACs regulate protein acetylation, thereby modulating protein activity and gene expression. Preclinical studies showed that HDAC inhibitors potentiate DNA damaging activity of anthracyclines in various cancer types, including sarcoma.
The phase I trial enrolled patients with metastatic solid tumors in dose escalation cohorts, and 20 patients with advanced sarcoma in the dose expansion cohort at the maximum tolerated dose of 50 mg/day of panobinostat on days 1, 3, and 5, and 75 mg/m2 of epirubicin on day 5.
In total, 24 patients (60%) had at least one grade 3 or 4 adverse event, including neutropenia (45%), leukopenia (35%), lymphopenia (22.5%), thrombocytopenia (17.5%), anemia (15%), and febrile neutropenia (7.5%). Major nonhematologic toxicities of panobinostat were myelotoxicity, nausea/vomiting, and fatigue, which required dose modification in 26% of patients.
In patients with advanced solid tumors, including sarcoma, the combination of panobinostat, a histone deacetylase (HDAC) inhibitor, and the anthracycline epirubicin demonstrated a correlation between neutropenia, peripheral blood mononucleocyte (PBMC) histone acetylation, and clinical benefit. Acquired topoisomerase resistance was reversed in 8 of 14 patients, suggesting HDAC inhibition reverses resistance.
In 37 evaluable patients, 4 (11%) had partial responses and 17 (46%) had stable disease. The median time to progression and median overall survival were 3.1 (95% CI, 1.8 to 4.6) months and 7.3 (5.9 to 10.3) months, respectively. All four patients with objective partial response had progressed on previous topoisomerase II inhibitors.
“The potential for prolonged treatment with an anthracycline in combination with an HDAC inhibitor speaks to the tolerability of this regimen. This study suggests that further investigation of HDAC inhibition in combination with DNA-damaging agents in defined advanced sarcoma subtypes to validate these preliminary findings is warranted,” wrote Dr. Scott Thomas of the Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, and colleagues (Ann Oncol. 2016 Feb 21. doi: 10.1093/annonc/mdw044).
HDACs regulate protein acetylation, thereby modulating protein activity and gene expression. Preclinical studies showed that HDAC inhibitors potentiate DNA damaging activity of anthracyclines in various cancer types, including sarcoma.
The phase I trial enrolled patients with metastatic solid tumors in dose escalation cohorts, and 20 patients with advanced sarcoma in the dose expansion cohort at the maximum tolerated dose of 50 mg/day of panobinostat on days 1, 3, and 5, and 75 mg/m2 of epirubicin on day 5.
In total, 24 patients (60%) had at least one grade 3 or 4 adverse event, including neutropenia (45%), leukopenia (35%), lymphopenia (22.5%), thrombocytopenia (17.5%), anemia (15%), and febrile neutropenia (7.5%). Major nonhematologic toxicities of panobinostat were myelotoxicity, nausea/vomiting, and fatigue, which required dose modification in 26% of patients.
In patients with advanced solid tumors, including sarcoma, the combination of panobinostat, a histone deacetylase (HDAC) inhibitor, and the anthracycline epirubicin demonstrated a correlation between neutropenia, peripheral blood mononucleocyte (PBMC) histone acetylation, and clinical benefit. Acquired topoisomerase resistance was reversed in 8 of 14 patients, suggesting HDAC inhibition reverses resistance.
In 37 evaluable patients, 4 (11%) had partial responses and 17 (46%) had stable disease. The median time to progression and median overall survival were 3.1 (95% CI, 1.8 to 4.6) months and 7.3 (5.9 to 10.3) months, respectively. All four patients with objective partial response had progressed on previous topoisomerase II inhibitors.
“The potential for prolonged treatment with an anthracycline in combination with an HDAC inhibitor speaks to the tolerability of this regimen. This study suggests that further investigation of HDAC inhibition in combination with DNA-damaging agents in defined advanced sarcoma subtypes to validate these preliminary findings is warranted,” wrote Dr. Scott Thomas of the Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, and colleagues (Ann Oncol. 2016 Feb 21. doi: 10.1093/annonc/mdw044).
HDACs regulate protein acetylation, thereby modulating protein activity and gene expression. Preclinical studies showed that HDAC inhibitors potentiate DNA damaging activity of anthracyclines in various cancer types, including sarcoma.
The phase I trial enrolled patients with metastatic solid tumors in dose escalation cohorts, and 20 patients with advanced sarcoma in the dose expansion cohort at the maximum tolerated dose of 50 mg/day of panobinostat on days 1, 3, and 5, and 75 mg/m2 of epirubicin on day 5.
In total, 24 patients (60%) had at least one grade 3 or 4 adverse event, including neutropenia (45%), leukopenia (35%), lymphopenia (22.5%), thrombocytopenia (17.5%), anemia (15%), and febrile neutropenia (7.5%). Major nonhematologic toxicities of panobinostat were myelotoxicity, nausea/vomiting, and fatigue, which required dose modification in 26% of patients.
FROM ANNALS OF ONCOLOGY
Key clinical point: Despite prior exposure to multiple regimens, clinical benefit was observed in several patients with advanced solid tumors, including some with sarcoma, who received panobinostat and epirubicin.
Major finding: In 37 evaluable patients, 4 (11%) had partial responses and 17 (46%) had stable disease; acquired topoisomerase resistance was reversed in 8 of 14 patients.
Data source: Phase I trial of 20 patients with metastatic solid tumors in dose escalation cohorts, and 20 patients with advanced sarcoma in the dose expansion cohort.
Disclosures: Research was supported in part by Novartis International AG. Dr. Thomas reported having no disclosures. Dr. Munster received research support from Novartis for this and other clinical trials.
Radiotherapy for prostate cancer linked to higher risk of secondary malignancies
Radiotherapy for prostate cancer may result in an increased risk of secondary malignancies of the bladder, colon, and rectum, according to findings of a systematic review and meta-analysis.
The unadjusted odds ratios for secondary bladder, colorectal, and rectal cancers in patients exposed to radiotherapy, compared with those not exposed, were 1.39 (95% CI, 1.12-1.71), 1.68 (1.33-2.12), and 1.62 (1.26-2.08), respectively. Differences in absolute risks for cases and controls were low, ranging from –0.9 to 1.9 cancers per 100 patients, and arose from variation in type of radiotherapy, comparator group, and lag time.
The findings, based on a relatively small number of studies with limited adjustments made for confounders, point to the need for future studies, according to the investigators. They described the implications of the findings for making treatment decisions with patients.
“In particular, for patients with a long life expectancy of 20 years or more, the possibility of secondary malignancy related to radiation needs to be included in management discussions. We acknowledge, however, that further studies are required before conclusive implication of the association between radiotherapy and secondary malignancy in these patients,” wrote Dr. Christopher J.D. Wallis of the University of Toronto and his colleagues (BMJ 2016 March 2. doi: 10.1136/bmj.i851).
Evidence suggests that irradiation of the prostate may contribute to carcinogenesis outside the irradiated area by radiation scatter, as well as the bystander effect, described as changes in gene expression due to an increase in reactive oxygen species. The researchers examined the association between radiotherapy and secondary malignancies of the bladder, colorectal tract, lung, and hematologic systems, and found no consistent evidence for associations with lung and hematologic cancers.
The systematic review and meta-analysis involved 9 studies (n = 555,873) for bladder cancer, 10 (n = 228,965) for colorectal cancer, and 8 (n = 157,239) for rectal cancer. Of the 21 reports total, 18 were multi-institutional and 3 were single-center studies. The lag period before outcome determination varied considerably, as did the comparator groups, with 13 studies (62%) designating patients treated with surgery as comparators, and 8 studies designating patients with no radiation or no radiation and no surgery as controls.
The results were similar when the analysis was restricted to studies with 5-year or 10-year lag periods. Notably, for bladder and rectal cancers, risk increased with longer lag time: from 1.3 to 1.89 for a 5-year and 10-year period, respectively, for bladder cancer and from 1.68 to 2.2 for rectal cancer.
Risks associated with brachytherapy were lower than for external beam radiotherapy.
The comprehensive systematic review and meta-analysis by Wallis et al. suggests an increased risk of bladder (odds ratio, 1.39), rectal (OR, 1.62), and colorectal (OR, 1.68) cancers subsequent to radiotherapy for prostate cancer. Despite the increased relative risks, absolute risk remains small, and discovered cancers, while still requiring treatment, might not be lethal. Indeed, there appears to be no survival difference between men with bladder cancers linked to previous prostate cancer treated with radiation vs. prostate cancer treated with surgery.
 |
Dr. Anthony L. Zietman |
The current study found that brachytherapy (high radiation dose to a small volume of tissue) was not associated with an increased risk for secondary malignancies, which supports the move toward even more tightly targeted external radiation techniques.
As for real world implications of the findings, the observed increase in risk may have a bigger influence in treatment decisions for young patients with few comorbidities than it would for older patients or those with competing health risks.
“This study confirms our belief that second malignancy should be added to the already long list of avoidable hazards associated with treatment for those men with low-risk prostate cancer who simply need no treatment at all. Concern about second malignancies should not, however, stand in the way of an effective and well-studied treatment being given to men with higher-grade, lethal prostate cancer for whom the potential benefit simply dwarfs the risk,” wrote Dr. Christine E. Eyler and Dr. Anthony L. Zietman.
Dr. Eyler is a clinical fellow in radiation oncology at Massachusetts General Hospital, Boston. Dr. Zietman is professor of radiation oncology at Massachusetts General Hospital. These remarks were part of an editorial accompanying a report in the British Medical Journal (2016 March 2. doi: 10.1136/bmj.i1073).
The comprehensive systematic review and meta-analysis by Wallis et al. suggests an increased risk of bladder (odds ratio, 1.39), rectal (OR, 1.62), and colorectal (OR, 1.68) cancers subsequent to radiotherapy for prostate cancer. Despite the increased relative risks, absolute risk remains small, and discovered cancers, while still requiring treatment, might not be lethal. Indeed, there appears to be no survival difference between men with bladder cancers linked to previous prostate cancer treated with radiation vs. prostate cancer treated with surgery.
 |
Dr. Anthony L. Zietman |
The current study found that brachytherapy (high radiation dose to a small volume of tissue) was not associated with an increased risk for secondary malignancies, which supports the move toward even more tightly targeted external radiation techniques.
As for real world implications of the findings, the observed increase in risk may have a bigger influence in treatment decisions for young patients with few comorbidities than it would for older patients or those with competing health risks.
“This study confirms our belief that second malignancy should be added to the already long list of avoidable hazards associated with treatment for those men with low-risk prostate cancer who simply need no treatment at all. Concern about second malignancies should not, however, stand in the way of an effective and well-studied treatment being given to men with higher-grade, lethal prostate cancer for whom the potential benefit simply dwarfs the risk,” wrote Dr. Christine E. Eyler and Dr. Anthony L. Zietman.
Dr. Eyler is a clinical fellow in radiation oncology at Massachusetts General Hospital, Boston. Dr. Zietman is professor of radiation oncology at Massachusetts General Hospital. These remarks were part of an editorial accompanying a report in the British Medical Journal (2016 March 2. doi: 10.1136/bmj.i1073).
The comprehensive systematic review and meta-analysis by Wallis et al. suggests an increased risk of bladder (odds ratio, 1.39), rectal (OR, 1.62), and colorectal (OR, 1.68) cancers subsequent to radiotherapy for prostate cancer. Despite the increased relative risks, absolute risk remains small, and discovered cancers, while still requiring treatment, might not be lethal. Indeed, there appears to be no survival difference between men with bladder cancers linked to previous prostate cancer treated with radiation vs. prostate cancer treated with surgery.
 |
Dr. Anthony L. Zietman |
The current study found that brachytherapy (high radiation dose to a small volume of tissue) was not associated with an increased risk for secondary malignancies, which supports the move toward even more tightly targeted external radiation techniques.
As for real world implications of the findings, the observed increase in risk may have a bigger influence in treatment decisions for young patients with few comorbidities than it would for older patients or those with competing health risks.
“This study confirms our belief that second malignancy should be added to the already long list of avoidable hazards associated with treatment for those men with low-risk prostate cancer who simply need no treatment at all. Concern about second malignancies should not, however, stand in the way of an effective and well-studied treatment being given to men with higher-grade, lethal prostate cancer for whom the potential benefit simply dwarfs the risk,” wrote Dr. Christine E. Eyler and Dr. Anthony L. Zietman.
Dr. Eyler is a clinical fellow in radiation oncology at Massachusetts General Hospital, Boston. Dr. Zietman is professor of radiation oncology at Massachusetts General Hospital. These remarks were part of an editorial accompanying a report in the British Medical Journal (2016 March 2. doi: 10.1136/bmj.i1073).
Radiotherapy for prostate cancer may result in an increased risk of secondary malignancies of the bladder, colon, and rectum, according to findings of a systematic review and meta-analysis.
The unadjusted odds ratios for secondary bladder, colorectal, and rectal cancers in patients exposed to radiotherapy, compared with those not exposed, were 1.39 (95% CI, 1.12-1.71), 1.68 (1.33-2.12), and 1.62 (1.26-2.08), respectively. Differences in absolute risks for cases and controls were low, ranging from –0.9 to 1.9 cancers per 100 patients, and arose from variation in type of radiotherapy, comparator group, and lag time.
The findings, based on a relatively small number of studies with limited adjustments made for confounders, point to the need for future studies, according to the investigators. They described the implications of the findings for making treatment decisions with patients.
“In particular, for patients with a long life expectancy of 20 years or more, the possibility of secondary malignancy related to radiation needs to be included in management discussions. We acknowledge, however, that further studies are required before conclusive implication of the association between radiotherapy and secondary malignancy in these patients,” wrote Dr. Christopher J.D. Wallis of the University of Toronto and his colleagues (BMJ 2016 March 2. doi: 10.1136/bmj.i851).
Evidence suggests that irradiation of the prostate may contribute to carcinogenesis outside the irradiated area by radiation scatter, as well as the bystander effect, described as changes in gene expression due to an increase in reactive oxygen species. The researchers examined the association between radiotherapy and secondary malignancies of the bladder, colorectal tract, lung, and hematologic systems, and found no consistent evidence for associations with lung and hematologic cancers.
The systematic review and meta-analysis involved 9 studies (n = 555,873) for bladder cancer, 10 (n = 228,965) for colorectal cancer, and 8 (n = 157,239) for rectal cancer. Of the 21 reports total, 18 were multi-institutional and 3 were single-center studies. The lag period before outcome determination varied considerably, as did the comparator groups, with 13 studies (62%) designating patients treated with surgery as comparators, and 8 studies designating patients with no radiation or no radiation and no surgery as controls.
The results were similar when the analysis was restricted to studies with 5-year or 10-year lag periods. Notably, for bladder and rectal cancers, risk increased with longer lag time: from 1.3 to 1.89 for a 5-year and 10-year period, respectively, for bladder cancer and from 1.68 to 2.2 for rectal cancer.
Risks associated with brachytherapy were lower than for external beam radiotherapy.
Radiotherapy for prostate cancer may result in an increased risk of secondary malignancies of the bladder, colon, and rectum, according to findings of a systematic review and meta-analysis.
The unadjusted odds ratios for secondary bladder, colorectal, and rectal cancers in patients exposed to radiotherapy, compared with those not exposed, were 1.39 (95% CI, 1.12-1.71), 1.68 (1.33-2.12), and 1.62 (1.26-2.08), respectively. Differences in absolute risks for cases and controls were low, ranging from –0.9 to 1.9 cancers per 100 patients, and arose from variation in type of radiotherapy, comparator group, and lag time.
The findings, based on a relatively small number of studies with limited adjustments made for confounders, point to the need for future studies, according to the investigators. They described the implications of the findings for making treatment decisions with patients.
“In particular, for patients with a long life expectancy of 20 years or more, the possibility of secondary malignancy related to radiation needs to be included in management discussions. We acknowledge, however, that further studies are required before conclusive implication of the association between radiotherapy and secondary malignancy in these patients,” wrote Dr. Christopher J.D. Wallis of the University of Toronto and his colleagues (BMJ 2016 March 2. doi: 10.1136/bmj.i851).
Evidence suggests that irradiation of the prostate may contribute to carcinogenesis outside the irradiated area by radiation scatter, as well as the bystander effect, described as changes in gene expression due to an increase in reactive oxygen species. The researchers examined the association between radiotherapy and secondary malignancies of the bladder, colorectal tract, lung, and hematologic systems, and found no consistent evidence for associations with lung and hematologic cancers.
The systematic review and meta-analysis involved 9 studies (n = 555,873) for bladder cancer, 10 (n = 228,965) for colorectal cancer, and 8 (n = 157,239) for rectal cancer. Of the 21 reports total, 18 were multi-institutional and 3 were single-center studies. The lag period before outcome determination varied considerably, as did the comparator groups, with 13 studies (62%) designating patients treated with surgery as comparators, and 8 studies designating patients with no radiation or no radiation and no surgery as controls.
The results were similar when the analysis was restricted to studies with 5-year or 10-year lag periods. Notably, for bladder and rectal cancers, risk increased with longer lag time: from 1.3 to 1.89 for a 5-year and 10-year period, respectively, for bladder cancer and from 1.68 to 2.2 for rectal cancer.
Risks associated with brachytherapy were lower than for external beam radiotherapy.
FROM BRITISH MEDICAL JOURNAL
Key clinical point: Radiotherapy for prostate cancer was associated with a higher risk of secondary malignancies of the bladder, colon, and rectum.
Major finding: The unadjusted odds ratios for secondary bladder, colorectal, and rectal cancers in patients exposed to radiotherapy, compared with those not exposed, were 1.39 (95% CI, 1.12-1.71), 1.68 (1.33-2.12), and 1.62 (1.26-2.08), respectively.
Data sources: The systematic review and meta-analysis of 21 reports involved 9 studies (n = 555,873) for bladder cancer, 10 (n = 228,965) for colorectal cancer, and 8 (n = 157,239) for rectal cancer.
Disclosures: Dr. Wallis and coauthors reported having no relevant financial disclosures.
Ki-67 bests cytology, growth pattern as prognostic factor for MCL
Evaluating routinely available histopathological prognostic features from more than 500 MCL patients in prospective trials, researchers found that the Ki-67 index is a better prognostic factor than are cytology and growth pattern in mantle-cell lymphoma (MCL). In addition, the combination of the Ki-67 index with the Mantle Cell Lymphoma International Prognostic Index [MIPI] defined four prognostic groups with better discrimination than did MIPI or the two-category biologic MIPI (MIPI-b) alone.
Higher Ki-67 index was associated with poorer overall survival (OS) (hazard ratio [HR], 1.24 per 10% increase; P less than .001) and progression-free survival (PFS) (HR, 1.17; P less than .001). Consistent with an earlier, population-based study, results showed prognostic value for a 30% cutoff of the Ki-67 index. Quantitative levels below 30% provided no additional prognostic information.
“The Ki-67 index remains the only routinely available independent prognostic factor in addition to MIPI. In contrast to cytology and growth pattern, the Ki-67 evaluation has been standardized for routine application,” wrote Dr. Eva Hoster of University Hospital Munich, and colleagues. “The modified combination of Ki-67 index and MIPI integrates the most important clinical and biologic markers currently available in clinical routine and was shown to allow a simple and powerful risk stratification superior to MIPI and MIPI-b in our evaluation,” they added (J Clin Oncol. 2016 Feb. 29. doi: 10.1200/jco.63.8387).
Blastoid cytology was associated with inferior 5-year OS compared with nonblastoid cytology (35% vs. 68%; HR, 2.35; P less than .001) and PFS (29% vs. 44%; HR, 1.58; P = .007), but the effect was largely accounted for by a generally higher Ki-67 index in blastoid MCL. Diffuse growth pattern was associated slightly worse 5-year OS (61% vs. 72%; HR, 1.38; P = .048) and PFS (38% vs. 49%; HR, 1.25; P = .087), but the effect was largely explained by MIPI score.
Combining dichotomized Ki-67 (above or below 30%) with MIPI risk groups defined four prognostic groups by the sum of weights (total 0 to 3): Ki-67 of 30% or more (weight 1), intermediate-risk MIPI (weight 1), and high-risk MIPI (weight 2). The 5-year OS rates for the four groups ranged from 17% to 85%, with OS hazard ratios greater than 2 between adjacent risk groups.
The study analyzed pooled data from two randomized trials initiated in 2004 by the European Mantle Cell Lymphoma Network, MCL Younger and MCL Elderly. In total, 508 patients of median age 62 years were included. The proportion of low-risk, intermediate-risk, and high-risk MIPI were 41%, 35%, and 24%, respectively.
Research was supported in part by Roche. Dr. Hoster reported receiving funding from Roche Pharma AG and Celgene. Several of her coauthors reported ties to industry.
Evaluating routinely available histopathological prognostic features from more than 500 MCL patients in prospective trials, researchers found that the Ki-67 index is a better prognostic factor than are cytology and growth pattern in mantle-cell lymphoma (MCL). In addition, the combination of the Ki-67 index with the Mantle Cell Lymphoma International Prognostic Index [MIPI] defined four prognostic groups with better discrimination than did MIPI or the two-category biologic MIPI (MIPI-b) alone.
Higher Ki-67 index was associated with poorer overall survival (OS) (hazard ratio [HR], 1.24 per 10% increase; P less than .001) and progression-free survival (PFS) (HR, 1.17; P less than .001). Consistent with an earlier, population-based study, results showed prognostic value for a 30% cutoff of the Ki-67 index. Quantitative levels below 30% provided no additional prognostic information.
“The Ki-67 index remains the only routinely available independent prognostic factor in addition to MIPI. In contrast to cytology and growth pattern, the Ki-67 evaluation has been standardized for routine application,” wrote Dr. Eva Hoster of University Hospital Munich, and colleagues. “The modified combination of Ki-67 index and MIPI integrates the most important clinical and biologic markers currently available in clinical routine and was shown to allow a simple and powerful risk stratification superior to MIPI and MIPI-b in our evaluation,” they added (J Clin Oncol. 2016 Feb. 29. doi: 10.1200/jco.63.8387).
Blastoid cytology was associated with inferior 5-year OS compared with nonblastoid cytology (35% vs. 68%; HR, 2.35; P less than .001) and PFS (29% vs. 44%; HR, 1.58; P = .007), but the effect was largely accounted for by a generally higher Ki-67 index in blastoid MCL. Diffuse growth pattern was associated slightly worse 5-year OS (61% vs. 72%; HR, 1.38; P = .048) and PFS (38% vs. 49%; HR, 1.25; P = .087), but the effect was largely explained by MIPI score.
Combining dichotomized Ki-67 (above or below 30%) with MIPI risk groups defined four prognostic groups by the sum of weights (total 0 to 3): Ki-67 of 30% or more (weight 1), intermediate-risk MIPI (weight 1), and high-risk MIPI (weight 2). The 5-year OS rates for the four groups ranged from 17% to 85%, with OS hazard ratios greater than 2 between adjacent risk groups.
The study analyzed pooled data from two randomized trials initiated in 2004 by the European Mantle Cell Lymphoma Network, MCL Younger and MCL Elderly. In total, 508 patients of median age 62 years were included. The proportion of low-risk, intermediate-risk, and high-risk MIPI were 41%, 35%, and 24%, respectively.
Research was supported in part by Roche. Dr. Hoster reported receiving funding from Roche Pharma AG and Celgene. Several of her coauthors reported ties to industry.
Evaluating routinely available histopathological prognostic features from more than 500 MCL patients in prospective trials, researchers found that the Ki-67 index is a better prognostic factor than are cytology and growth pattern in mantle-cell lymphoma (MCL). In addition, the combination of the Ki-67 index with the Mantle Cell Lymphoma International Prognostic Index [MIPI] defined four prognostic groups with better discrimination than did MIPI or the two-category biologic MIPI (MIPI-b) alone.
Higher Ki-67 index was associated with poorer overall survival (OS) (hazard ratio [HR], 1.24 per 10% increase; P less than .001) and progression-free survival (PFS) (HR, 1.17; P less than .001). Consistent with an earlier, population-based study, results showed prognostic value for a 30% cutoff of the Ki-67 index. Quantitative levels below 30% provided no additional prognostic information.
“The Ki-67 index remains the only routinely available independent prognostic factor in addition to MIPI. In contrast to cytology and growth pattern, the Ki-67 evaluation has been standardized for routine application,” wrote Dr. Eva Hoster of University Hospital Munich, and colleagues. “The modified combination of Ki-67 index and MIPI integrates the most important clinical and biologic markers currently available in clinical routine and was shown to allow a simple and powerful risk stratification superior to MIPI and MIPI-b in our evaluation,” they added (J Clin Oncol. 2016 Feb. 29. doi: 10.1200/jco.63.8387).
Blastoid cytology was associated with inferior 5-year OS compared with nonblastoid cytology (35% vs. 68%; HR, 2.35; P less than .001) and PFS (29% vs. 44%; HR, 1.58; P = .007), but the effect was largely accounted for by a generally higher Ki-67 index in blastoid MCL. Diffuse growth pattern was associated slightly worse 5-year OS (61% vs. 72%; HR, 1.38; P = .048) and PFS (38% vs. 49%; HR, 1.25; P = .087), but the effect was largely explained by MIPI score.
Combining dichotomized Ki-67 (above or below 30%) with MIPI risk groups defined four prognostic groups by the sum of weights (total 0 to 3): Ki-67 of 30% or more (weight 1), intermediate-risk MIPI (weight 1), and high-risk MIPI (weight 2). The 5-year OS rates for the four groups ranged from 17% to 85%, with OS hazard ratios greater than 2 between adjacent risk groups.
The study analyzed pooled data from two randomized trials initiated in 2004 by the European Mantle Cell Lymphoma Network, MCL Younger and MCL Elderly. In total, 508 patients of median age 62 years were included. The proportion of low-risk, intermediate-risk, and high-risk MIPI were 41%, 35%, and 24%, respectively.
Research was supported in part by Roche. Dr. Hoster reported receiving funding from Roche Pharma AG and Celgene. Several of her coauthors reported ties to industry.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The Ki-67 index was superior to cytology and growth pattern as a prognostic factor in mantle-cell lymphoma (MCL).
Major finding: Higher Ki-67 index was associated with poorer overall survival (hazard ratio [HR], 1.24 per 10% increase; P less than .001) and progression-free survival (HR, 1.17; P less than .001).
Data source: Pooled data from two randomized trials initiated in 2004 by the European Mantle Cell Lymphoma Network, MCL Younger and MCL Elderly, included 508 patients.
Disclosures: Research was supported in part by Roche. Dr. Hoster reported receiving funding from Roche Pharma AG and Celgene. Several of her coauthors reported ties to industry.
Prospective study confirms chemo not needed after low Recurrence Score
Patients with hormone receptor-positive breast cancer at high risk for recurrence by traditional parameters, but with a low 21-gene Recurrence Score (RS) can safely avoid chemotherapy, according to results of the phase III PlanB trial.
In this prospective trial, patients with intermediate to high risk breast cancer receiving adjuvant chemotherapy based on RS and those receiving no adjuvant chemotherapy based on RS of 11 or less had similar 3-year disease-free survival (DFS) rates.
In patients with pN0 to 1 breast cancer, 3-year DFS was 98.4% (95% CI, 97.0% to 99.8%) for patients with RS of 11 or less (no adjuvant chemotherapy); 97.5% (95% CI, 95.9% to 99.0%) for RS of 12 to 25 (with adjuvant chemotherapy); and 94.9% (95% CI, 91.4% to 98.4%) for RS greater than 25 (with adjuvant chemotherapy) (P = .05 for RS greater than 25 vs. others).
“The most important finding in our study is the high 3-year DFS (98%) in patients with low RS (11 or less) and no chemotherapy, despite being high risk by traditional parameters. Even with an only 3-year follow-up, such a high rate of DFS almost excludes possible benefit from adjuvant chemotherapy,” wrote Dr. Oleg Gluz of the West German Study Group, Breast Center Niederrhein, Evangelical Hospital Bethesda, Germany, and colleagues (J Clin Oncol 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383).
Univariate analysis showed RS to be a prognostic factor for DFS, along with nodal status, grade, concentration of the Ki-67 protein encoded by the MKI67 gene, estrogen and progesterone receptor status, and tumor size. In multivariate analysis, fractionally ranked RS was associated with DFS (hazard ratio [HR], 1.68; 95% CI, 1.04 to 2.74; P = .035), as were node status (pN1-3 vs. pN0: HR, 2.45; 95% CI, 1.39 to 4.29, P = .001) and centrally-determined grade (G3 vs. G1 and G2: HR, 2.27; 95% CI, 1.28 to 4.02; P = .005).
The study demonstrated substantial disagreement in grade assessment by central vs. local pathology reviews, with 44% discordance in locally HR-positive tumors. Investigators suggest that use of RS may help to make treatment decisions more homogeneous and reliable, regardless of where patients are treated.
The results suggest that patients N0 to N1 breast cancer with low RS scores derive little benefit from adjuvant chemotherapy, but benefits for patients with intermediate RS scores (12 to 25) are unclear. Prospective trials are underway to address this question.
The prospective, randomized PlanB trial recruited 3,198 patients from 93 German centers from 2009 to 2011. RS scores were available for 2,568 patients with HR-positive, HER2-negative, intermediate to high risk breast cancer. In total, 18.1% had RS of 11 or less, 60.4% had RS from 12 to 25, and 21.6% had RS greater than 25.
Research was supported by Genomic Health, Sanofi Aventis, and Amgen. Dr. Gluz reported consulting or advisory roles with Genomic Health and NanoString Technologies. Several of his coauthors reported ties to industry sources.
Patients with hormone receptor-positive breast cancer at high risk for recurrence by traditional parameters, but with a low 21-gene Recurrence Score (RS) can safely avoid chemotherapy, according to results of the phase III PlanB trial.
In this prospective trial, patients with intermediate to high risk breast cancer receiving adjuvant chemotherapy based on RS and those receiving no adjuvant chemotherapy based on RS of 11 or less had similar 3-year disease-free survival (DFS) rates.
In patients with pN0 to 1 breast cancer, 3-year DFS was 98.4% (95% CI, 97.0% to 99.8%) for patients with RS of 11 or less (no adjuvant chemotherapy); 97.5% (95% CI, 95.9% to 99.0%) for RS of 12 to 25 (with adjuvant chemotherapy); and 94.9% (95% CI, 91.4% to 98.4%) for RS greater than 25 (with adjuvant chemotherapy) (P = .05 for RS greater than 25 vs. others).
“The most important finding in our study is the high 3-year DFS (98%) in patients with low RS (11 or less) and no chemotherapy, despite being high risk by traditional parameters. Even with an only 3-year follow-up, such a high rate of DFS almost excludes possible benefit from adjuvant chemotherapy,” wrote Dr. Oleg Gluz of the West German Study Group, Breast Center Niederrhein, Evangelical Hospital Bethesda, Germany, and colleagues (J Clin Oncol 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383).
Univariate analysis showed RS to be a prognostic factor for DFS, along with nodal status, grade, concentration of the Ki-67 protein encoded by the MKI67 gene, estrogen and progesterone receptor status, and tumor size. In multivariate analysis, fractionally ranked RS was associated with DFS (hazard ratio [HR], 1.68; 95% CI, 1.04 to 2.74; P = .035), as were node status (pN1-3 vs. pN0: HR, 2.45; 95% CI, 1.39 to 4.29, P = .001) and centrally-determined grade (G3 vs. G1 and G2: HR, 2.27; 95% CI, 1.28 to 4.02; P = .005).
The study demonstrated substantial disagreement in grade assessment by central vs. local pathology reviews, with 44% discordance in locally HR-positive tumors. Investigators suggest that use of RS may help to make treatment decisions more homogeneous and reliable, regardless of where patients are treated.
The results suggest that patients N0 to N1 breast cancer with low RS scores derive little benefit from adjuvant chemotherapy, but benefits for patients with intermediate RS scores (12 to 25) are unclear. Prospective trials are underway to address this question.
The prospective, randomized PlanB trial recruited 3,198 patients from 93 German centers from 2009 to 2011. RS scores were available for 2,568 patients with HR-positive, HER2-negative, intermediate to high risk breast cancer. In total, 18.1% had RS of 11 or less, 60.4% had RS from 12 to 25, and 21.6% had RS greater than 25.
Research was supported by Genomic Health, Sanofi Aventis, and Amgen. Dr. Gluz reported consulting or advisory roles with Genomic Health and NanoString Technologies. Several of his coauthors reported ties to industry sources.
Patients with hormone receptor-positive breast cancer at high risk for recurrence by traditional parameters, but with a low 21-gene Recurrence Score (RS) can safely avoid chemotherapy, according to results of the phase III PlanB trial.
In this prospective trial, patients with intermediate to high risk breast cancer receiving adjuvant chemotherapy based on RS and those receiving no adjuvant chemotherapy based on RS of 11 or less had similar 3-year disease-free survival (DFS) rates.
In patients with pN0 to 1 breast cancer, 3-year DFS was 98.4% (95% CI, 97.0% to 99.8%) for patients with RS of 11 or less (no adjuvant chemotherapy); 97.5% (95% CI, 95.9% to 99.0%) for RS of 12 to 25 (with adjuvant chemotherapy); and 94.9% (95% CI, 91.4% to 98.4%) for RS greater than 25 (with adjuvant chemotherapy) (P = .05 for RS greater than 25 vs. others).
“The most important finding in our study is the high 3-year DFS (98%) in patients with low RS (11 or less) and no chemotherapy, despite being high risk by traditional parameters. Even with an only 3-year follow-up, such a high rate of DFS almost excludes possible benefit from adjuvant chemotherapy,” wrote Dr. Oleg Gluz of the West German Study Group, Breast Center Niederrhein, Evangelical Hospital Bethesda, Germany, and colleagues (J Clin Oncol 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383).
Univariate analysis showed RS to be a prognostic factor for DFS, along with nodal status, grade, concentration of the Ki-67 protein encoded by the MKI67 gene, estrogen and progesterone receptor status, and tumor size. In multivariate analysis, fractionally ranked RS was associated with DFS (hazard ratio [HR], 1.68; 95% CI, 1.04 to 2.74; P = .035), as were node status (pN1-3 vs. pN0: HR, 2.45; 95% CI, 1.39 to 4.29, P = .001) and centrally-determined grade (G3 vs. G1 and G2: HR, 2.27; 95% CI, 1.28 to 4.02; P = .005).
The study demonstrated substantial disagreement in grade assessment by central vs. local pathology reviews, with 44% discordance in locally HR-positive tumors. Investigators suggest that use of RS may help to make treatment decisions more homogeneous and reliable, regardless of where patients are treated.
The results suggest that patients N0 to N1 breast cancer with low RS scores derive little benefit from adjuvant chemotherapy, but benefits for patients with intermediate RS scores (12 to 25) are unclear. Prospective trials are underway to address this question.
The prospective, randomized PlanB trial recruited 3,198 patients from 93 German centers from 2009 to 2011. RS scores were available for 2,568 patients with HR-positive, HER2-negative, intermediate to high risk breast cancer. In total, 18.1% had RS of 11 or less, 60.4% had RS from 12 to 25, and 21.6% had RS greater than 25.
Research was supported by Genomic Health, Sanofi Aventis, and Amgen. Dr. Gluz reported consulting or advisory roles with Genomic Health and NanoString Technologies. Several of his coauthors reported ties to industry sources.
Key clinical point: Patients with hormone-receptor–positive (HR-positive) breast cancer at high risk for recurrence by traditional parameters, but with 21-gene Recurrence Score (RS) of 11 or less, did not receive adjuvant chemotherapy and had excellent 3-year survival.
Major finding: In patients with pN0 to 1 breast cancer, 3-year disease-free survival (DFS) was 98.4% (95% CI, 97.0% to 99.8%) for patients with RS of 11 or less (no adjuvant chemotherapy); 97.5% (95% CI, 95.9% to 99.0%) for RS of 12 to 25 (with adjuvant chemotherapy); and 94.9% (95% CI, 91.4% to 98.4%) for RS greater than 25 (with adjuvant chemotherapy) (P = .05 for RS greater than 25 vs. others).
Data source: The prospective, randomized PlanB trial included 2,568 HR-positive, HER2-negative patients with intermediate to high risk breast cancer.
Disclosures: Research was supported by Genomic Health, Sanofi Aventis, and Amgen. Dr. Gluz reported consulting or advisory roles with Genomic Health and NanoString Technologies. Several of his coauthors reported ties to industry sources.
Occult micrometastases in N2 lymph nodes correlated with shorter survival in NSCLC
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
In patients with non–small cell lung cancer (NSCLC) designated stage I by conventional histopathology, occult metastases were detected by immunohistochemistry (IHC) staining of cytokeratin in 14% of patients and by reverse transcriptase polymerase chain reaction (RT-PCR) for carcinoembryonic antigen in 69% of patients; however, only IHC-positivity within N2 nodes was correlated with overall survival.
Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive patients compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017. Patients who were IHC-positive within N1 nodes had survival similar to that of IHC-negative patients.
Although the majority of patients in the study (69%) had occult metastases by RT-PCR, no relationship between PCR status and overall survival or disease-free survival emerged from the data.
Surgical resection in early stage NSCLC yields unpredictable outcomes, and one explanation for this is the presence of occult metastases in regional nodes.
“The presence of (occult metastases) is a logical explanation for tumors that are classified as stage I by conventional histopathology to demonstrate a worse prognosis. However, the current rigorously designed and executed prospective study only showed a significant difference in survival when N2 nodes demonstrated positivity by IHC, but not by RT-PCR,” wrote Dr. Linda W. Martin of the University of Maryland, Baltimore, and colleagues (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.4543).
“Clearly RT-PCR is more sensitive, but perhaps (carcinoembryonic antigen) is not as specific for NSCLC and thus the clinical impact is insignificant,” they wrote. RT-PCR data showed poor concordance with IHC data in the study, and did not correlate with outcomes, pointing to a lack of clinical utility for RT-PCR in NSCLC, the authors stated.
The Cancer and Leukemia Group B (CALGB) 9761 trial accrued 501 patients from 1997 to 2002, 304 of whom had stage 1A or 1B NSCLC. Median follow up was 8.4 years (range: 0.97 to 11.4 years). Local only recurrence occurred in 24 patients, local and distant in 18, and distant only in 27.
Dr. Martin and coauthors had no disclosures.
Key clinical point: Micrometastasis detected by immunohistochemistry (IHC) staining for cytokeratin (AE1/AE3) in the lymph nodes of patients with non–small cell lung cancer (NSCLC), designated stage I or N0 by standard techniques, correlated with decreased overall survival.
Major finding: Patients who were IHC-positive within an N2 node had worse overall survival than did IHC-negative patients (HR, 2.04; 95% CI, 1.14 to 3.66); 5-year survival for N2 IHC-positive compared with IHC-negative patients was 50% (95% CI, 29.1% to 67.8%) vs. 66.9% (60.9% to 72.2%), P = .017.
Data source: The Cancer and Leukemia Group B (CALGB) 9761 trial of 304 patients with stage 1A or 1B NSCLC.
Disclosures: Dr. Martin and coauthors had no disclosures.