User login
Assessing benefits and risks of hormone therapy in 2008: New evidence, especially with regard to the heart
Physicians and their women patients have faced a continuous, confusing mix of information about the risks and benefits of hormone therapy (HT) for perimenopausal and postmenopausal women, most of it without respect to age or the timing of HT relative to menopause. Initial data from the Women’s Health Initiative (WHI) estrogen + progestin (E+P) trial, a prevention study conducted predominantly in older postmenopausal women without menopausal symptoms,1 resulted in questioning of the role of HT (unfortunately and inappropriately in younger symptomatic women). Cumulative trial data and further analyses of the WHI have refined and added to our understanding of the effects of HT, particularly with regard to cardiovascular health. This review will update physicians on the latest data on the risks and benefits of HT, with a particular focus on the heart, and will put the risks of HT into appropriate clinical context.
HORMONE THERAPY AND CARDIOVASCULAR DISEASE: A HISTORICAL PERSPECTIVE
Observational studies conducted prior to the WHI found consistently that women who self-selected to use HT had a reduction in mortality and in the incidence of cardiovascular disease relative to women who did not choose to use HT.2–8 This reduction in risk was apparent whether the HT users had taken ET (estrogen therapy) or EPT (estrogen-progestogen therapy). In contrast, randomized controlled trials failed to confirm these findings from observational studies. However, the findings from randomized controlled trials were derived from older postmenopausal women who were many years past menopause. Often overlooked is the WHI observational study of ET and EPT,9,10 in which women who chose to use HT had a reduction in the risk of coronary heart disease (CHD) similar to that observed among the HT users in other observational studies.
RECENT REPORTS FROM THE WHI
Since the original publication of the WHI E+P trial in 2002,1 an extensive collection of data have been published in piecemeal fashion, contributing to the confusion and misperception of the effects of HT on risks and benefits. It is important to note that the WHI consists of both randomized and observational components, as detailed below, and that data have come from both. Together, these data help clarify the misperceptions generated from the first WHI report of 2002,1 particularly misperceptions regarding the timing of HT initiation relative to menopause and the effect of HT duration on cardiovascular disease outcomes. In most instances, the conclusions drawn from this recent research run counter to the inaccurate but prevalent perception that HT use at any time and at any age is associated with cardiovascular harm, a perception that has unfortunately prevailed since the initial publication of the WHI E+P trial findings in 2002.
The WHI randomized trials and combined analysis
The WHI trials enrolled 27,347 postmenopausal women aged 50 to 79 years at baseline; almost two-thirds of the women enrolled were 60 years of age or older, and the majority of women were more than 10 years past menopause. WHI actually comprised two parallel randomized trials:
- One among 16,608 women who had not undergone hysterectomy (ie, with uterus intact), who were randomized to EPT or placebo (ie, WHI E+P trial) 1
- One among 10,739 women who had undergone hysterectomy, who were randomized to ET or placebo.11
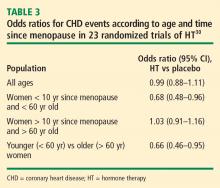
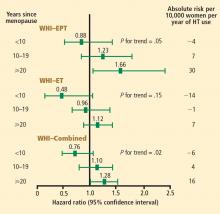
Recent analyses from the WHI, published in 2007, assessed the cardiovascular effects of ET and EPT independently and combined, both overall and according to subject age and years since menopause when randomized.12 Other analyses following the initial WHI E+P trial publication have analyzed the effects of HT according to duration of HT use and according to secondary end points. Many of these analyses have presented risks and benefits in terms of both nominal and adjusted confidence intervals (CIs). Nominal 95% CIs describe the variability in risk estimates that would arise from a simple trial for a single end point. Although nominal CIs are traditionally used, they do not take into account the multiple statistical testing issues (across time and across outcome categories) that occur in a trial. In contrast, adjusted 95% CIs correct for these stastical testing issues. From a clinical perspective, it is most appropriate to look at the adjusted CIs.
WHI: EPT vs placebo
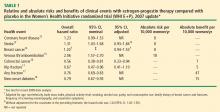
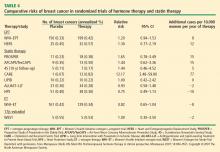
CHD. Although the point estimate for CHD is increased, the 95% CI indicates that EPT has a non-significant effect on CHD outcome relative to placebo among all women randomized in the WHI E+P trial (mean age, 63 years).12 This is a very important point for cardiologists and primary care physicians to note.
In a 2008 analysis of the WHI E+P trial that included a 2.4-year open-label follow-up subsequent to the randomized trial,19 the randomized trial data reported were again different than in previous reports, but remained nonsignificant. The hazard ratio (HR) reported for CHD in the 2008 analysis for the randomized portion of the trial was 1.22 (95% CI, 0.99 to 1.51), as compared with 1.23 (95% CI, 0.99 to 1.53) reported in 200712 (Table 1), 1.24 (95% CI, 1.00 to 1.54) reported in 2003,20 and 1.29 (95% CI, 1.02 to 1.63) reported in 2002.1 In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens (EPT or placebo), the HR for CHD between the original randomized treatment groups was nonsignificant at 0.95 (95% CI, 0.73 to 1.26) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Stroke. The risk of stroke was increased significantly (by an additional 8 events per 10,000 women treated per year) in the EPT arm versus the placebo arm in the nominal analysis,12 but this difference was nonsignificant after adjustment.13
In the 2008 WHI E+P analysis, the HR reported for stroke during the randomized trial phase was different than in previous reports—1.34 (95% CI, 1.05 to 1.71)19 versus 1.31 (95% CI, 1.03 to 1.68) reported in 200712 (Table 1)—and the adjusted analysis was not reported. In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens, the HR for stroke between the original randomized treatment groups was nonsignifi-cant at 1.16 (95% CI, 0.83 to 1.61) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Breast cancer. Breast cancer risk was originally reported to be increased significantly (by an additional 8 cases per 10,000 women per year) in the EPT arm versus the placebo arm with the nominal statistic, but this increase was nonsignificant after adjustment.1 This risk estimate was revised in a follow-up publication 1 year after the original data were reported, and the increase in risk in the EPT arm was still no longer significant in the adjusted analysis.21 Importantly, another subsequent analysis that adjusted for baseline risk factors for breast cancer resulted in a further revision of the risk estimate, which again showed a nonsignificant increase in the EPT arm relative to the placebo arm.14 This is very important since it is commonly accepted that EPT increases the risk of breast cancer when this has not been definitively proven in any randomized controlled trial.
Unfortunately, the most recent breast cancer data14 (Table 1) were not used in the 2008 WHI E+P analysis.19 However, even using the unadjusted data in the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR for breast cancer between the original randomized treatment groups was nonsignificant and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Venous thromboembolism (VTE). EPT was associated with a doubling of the risk of VTE (ie, deep vein thrombosis and pulmonary embolism) compared with placebo, resulting in an excess of 18 VTE events per 10,000 women per year of therapy.15 The risk of VTE was significant across the entire cohort of women (mean age, 63 years).
In the 2008 WHI E+P analysis, the HR reported for VTE during the randomized phase was different than in previous reports—1.98 (95% CI, 1.52 to 2.59)19 versus 2.06 (95% CI, 1.57 to 2.70) reported in 200415 (Table 1)—and the HR during the 2.4-year open-label follow-up, in which women were no longer on their randomized regimens, was no longer significant (HR = 0.95; 95% CI, 0.63 to 1.44). This change in the HR over time from the randomized phase to the open-label phase was statistically significant.19
Fracture. The risk of hip fracture was reduced by 33% with EPT relative to placebo, which was statistically significant in the nominal analysis but not in the adjusted analysis.17 The risk of any fracture was reduced by 24% in women randomized to EPT compared with placebo, which was statistically significant and translated to 47 fewer fractures per 10,000 women per year of therapy.17 Clinically, these results are most impressive given that women randomized in the WHI were not selected on the basis of risk for osteoporosis or fracture. This claim cannot be made for any other therapy.
In the 2008 WHI E+P analysis of the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR between the original randomized treatment groups was nonsignificant for hip fracture and any fracture—0.92 (95% CI, 0.64 to 1.34) and 0.91 (95% CI, 0.78 to 1.06), respectively—and the change in the HR over time from the randomized phase to the open-label phase was not significant for either fracture outcome.19
Diabetes. The risk of new-onset diabetes was reduced by a statistically significant 21% in women randomized to EPT compared with placebo.18
WHI: ET vs placebo
CHD. Importantly, no significant difference was found between the ET and placebo arms with respect to CHD events in the overall cohort of women, whose average age was 64 years.12
Stroke. The risk of stroke was greater with ET than with placebo in the nominal analysis, but importantly, the difference in event rates (11 per 10,000 women per year of therapy) failed to reach significance in the adjusted analysis.11,12
Breast cancer. A strong but nonsignificant trend toward a reduction in breast cancer risk was apparent in the ET arm (8 fewer breast cancer cases per 10,000 women per year of therapy). Among women who actually were adherent to their study regimen (ie, consuming ≥ 80% of their study medication), there was a statistically significant 33% reduction in breast cancer risk with ET relative to placebo.22 Importantly, the reduction in breast cancer risk relative to placebo was found across all the age ranges studied.11
VTE. The excess risk of VTE with ET versus placebo (32%) was less than the excess risk of VTE associated with EPT (Table 1). Importantly, the risk of VTE associated with ET was not statistically significant.11,23
Fracture. The risk of any fracture (hip or vertebral) was reduced significantly in the ET arm compared with the placebo arm.11
Diabetes. In a nominal analysis, there was a trend toward a reduction in the risk of new-onset diabetes in women randomized to ET relative to placebo, which nearly achieved statistical significance.24
WHAT EXPLAINS THE DISCORDANCE BETWEEN OBSERVATIONAL AND RANDOMIZED TRIALS OF HT?
How can the perceived discordance between the results from observational studies and those from randomized controlled trials be explained? There are currently three hypotheses:
- The populations differ in the two types of study designs (observational studies and randomized controlled trials)
- The duration of HT use differs
- The timing of HT initiation differs in relation to age, time since menopause, and stage of atherosclerosis.
Population characteristics
One obvious difference between randomized trials and observational studies of HT is the presence of menopausal symptoms. To maintain blinding, women with hot flashes were predominantly excluded from randomized trials of HT, whereas the presence of hot flashes is the predominant menopausal symptom of women included in observational studies and the main reason women seek HT from their providers.
Other consistent and possibly explanatory differences between clinical trials and observational studies of HT are patient age at enrollment, years since menopause, and body mass index (BMI). Comparing randomized controlled trials with observational studies, age at enrollment was much higher in the clinical trials (mean age ≥ 63 years) than in the observational studies (range of 30 to 55 years). Similarly, women enrolled in randomized trials were more than 10 years beyond menopause, whereas those in observational studies were less than 5 years beyond menopause. In fact, more than 80% of HT users in observational studies initiated HT within 1 or 2 years of menopause.
Additionally, women in randomized trials of HT tend to have higher BMIs than their counterparts in observational studies. For example, mean BMI was considerably higher in the WHI randomized trials (28.5 kg/m2 and 30.1 kg/m2)1,11 than in the observational Nurses’ Health Study (25.8 kg/m2),25 and a full third (34%) of women in the WHI randomized trials were severely obese (BMI ≥ 30 kg/m2).
This point about BMI is noteworthy in light of findings on the effect of BMI on breast cancer risk from an analysis of the WHI observational study among 85,917 women aged 50 to 79 years old at enrollment.26 This analysis found that BMI was unrelated to breast cancer risk among women who had used HT; however, among nonusers of HT, a baseline BMI greater than 31.1 kg/m2 was associated with a 2.52 relative risk of breast cancer compared with a baseline BMI less than 22.6 kg/m2. The risk of breast cancer with increasing BMI was most pronounced in younger postmenopausal women. One interpretation is that high endogenous estrogen levels in postmenopausal women with an elevated BMI serve to increase breast cancer risk to a level beyond which HT adds no further risk. Alternatively, conjugated equine estrogens may act through a selective estrogen receptor modulator mechanism to block any potential adverse breast tissue effects of elevated endogenous estrone and estradiol levels.
Duration of HT
Another hypothesis for the discordant findings between observational and randomized studies of HT focuses on differences in duration of HT use between the two types of studies. Duration of HT use has been substantially longer in observational studies, ranging from 10 years to 40 years, compared with no more than 7 or 8 years in randomized trials to date. Moreover, the results from observational studies have suggested that the longer the duration of HT use, the greater the benefit in terms of CHD risk.
For example, a case-control study by Chilvers et al showed that HT protected against nonfatal myocardial infarction only when used for more than 60 months.27 Analysis of data on EPT use from the Heart and Estrogen/progestin Replacement Study (HERS),28 the randomized WHI E+P trial,20 and the WHI observational study9 reveals an interesting and consistent trend: rates of CHD events increased during the first year of EPT therapy (compared with placebo or nonuse) but then declined over time, ending up below the rates of CHD events in placebo recipients or nonusers of HT after approximately 5 years of therapy. This trend was not as pronounced with ET use in either the WHI randomized trial29 or the WHI observational study,10 but the incidence of CHD events did decline over time with ET use in both studies, and in the WHI observational study, greater than 5 years of ET use was associated with a significant 27% reduction (HR, 0.73; 95% CI, 0.61 to 0.84) in CHD events compared with nonuse.10
Timing of HT initiation
A third hypothesis for the discordance between randomized and observational studies of HT concerns the timing of HT initiation relative to patient age, time since menopause, and stage of atherosclerosis. As noted above, women enrolled in randomized trials have tended to be considerably older and further from menopause compared with their counterparts in observational studies. The effects of differences in timing of HT initiation on specific clinical end points, particularly in relation to cardiovascular health, are reviewed below.
Early and continued HT use may interrupt the pathogenic sequence of vascular aging, potentially preventing progression of atherosclerosis to the late stage at which plaque rupture and clinical events occur. In contrast, late intervention with HT may have little effect on established plaque and, in the case of EPT, may actually predispose to plaque rupture. This concept has been demonstrated in a pair of sister studies, the Women’s Estrogen-Progestin Lipid-Lowering Hormone Atherosclerosis Regression Trial (WELLHART)31 and the Estrogen Prevention Atherosclerosis Trial (EPAT).32
Mortality. The same Stanford University researchers who performed the above meta-analysis of CHD events also assessed odd ratios for overall mortality in a meta-analysis of 30 randomized trials of HT versus placebo that included a total of 26,708 postmenopausal women (representing 119,118 patient-years).33 They found the timing of HT initiation to have an effect on mortality similar to its effect on CHD events. In the overall cohort of women, the odds of death were not different between the HT and placebo groups, but among women younger than 60 years (mean, 54 years), those randomized to HT had a significant 39% reduction in the risk of death (HR = 0.61; 95% CI, 0.39 to 0.95) compared with those randomized to placebo. HT had no effect on mortality among women older than 60 years (mean, 66 years) in this analysis.
These mortality data are consistent with those from the WHI randomized trials, in which both EPT and ET were associated with a 30% reduction in overall mortality relative to placebo among women 50 to 59 years old.12 When both the EPT and ET portions of the WHI were combined to increase the sample size, HT was associated with a significant 30% reduction in mortality (HR = 0.70; 95% CI, 0.51 to 0.96) compared with placebo among women 50 to 59 years old.12
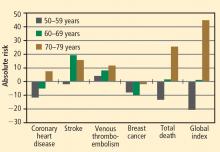
Stroke. The most recent WHI data indicate that stroke is not increased with ET in women 50 to 59 years of age, as there were 2 fewer events per 10,000 women per year of ET relative to placebo.12 In this same age group, the risk of stroke from EPT was increased by 5 events per 10,000 women per year of therapy relative to placebo.12 Among women randomized within 5 years of menopause, stroke risk was increased by 3 events per 10,000 women per year of EPT relative to placebo.13
VTE. Although age was not a significant contributing factor to the risk of VTE from HT in the WHI, the absolute risk of VTE was lower in younger versus older women. The additional absolute risk for VTE events per 10,000 women per year of EPT use was 11 events for women 50 to 59 years old at randomization, 16 events for women 60 to 69 years old at randomization, and 35 events for women 70 to 79 years old at randomization.15 The additional absolute risk for VTE events per 10,000 women per year of ET use was 4 events for women 50 to 59 years old at randomization, 7 events for women 60 to 69 years old at randomization, and 11 events for women 70 to 79 years old at randomization.23 A history of a prior thromboembolic event increases the risk of VTE with postmenopausal HT use, which should be considered before HT is initiated.
HORMONE THERAPY IN CLINICAL PERSPECTIVE
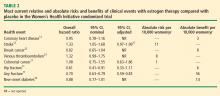
Comparative effects of lipid-lowering therapy and HT
Examination of the evidence regarding lipid-lowering therapy for prevention of CHD, as well as its effects on breast cancer risk and coronary artery calcium scores in women, can add some much-needed perspective and context to the HT data reviewed above.
CHD prevention. Walsh and Pignone examined six randomized controlled trials (N = 11,435) of primary prevention with lipid-lowering medication in women and found no significant effect on CHD events, nonfatal myocardial infarction, CHD mortality, or total mortality.34 In eight randomized controlled trials of secondary prevention (N = 8,272), lipid-lowering therapy in women resulted in significant reductions in CHD end points but had no effect on total mortality.34
Atherosclerosis progression. In three randomized controlled trials, 1 to 4 years of statin therapy had no effect on the progression of coronary artery calcium compared with placebo.41–43 Among 1,064 women 50 to 59 years old who participated in a WHI substudy called the WHI Coronary Artery Calcium Study (WHI-CACS), those who were randomized to ET had significantly less coronary artery calcium at year 7 compared with those assigned to placebo.44 The mean Agatston coronary artery calcium scores were 83.1 with ET versus 123.1 with placebo (P = .02).
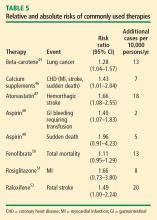
Comparing risk of HT with risk of other therapies
Other comparisons yield similar conclusions.35 For instance, a comparison of the ET arm of the WHI randomized trial with raloxifene in the Raloxifene Use for the Heart (RUTH) trial52 reveals similar effects on CHD, stroke, VTE, pulmonary embolism, deep vein thrombosis, and breast cancer, with the only large difference being a greater reduction in bone fracture risk with ET compared with raloxifene.35 Finally, in putting the risk of VTE with HT into perspective, consider that the risk of thromboembolic events with selective estrogen receptor modulators52 and with the fibric acid derivative fenofibrate in diabetics50 is of similar magnitude as the risk with HT.
Risk must be viewed in light of age at HT initiation
CONCLUSIONS FROM RANDOMIZED TRIALS
HT’s effects on CHD and mortality: Timing is everything
Cumulative data from randomized trials indicate that in the overall population of women studied, HT, aspirin, and lipid-lowering therapy each have a null effect on the incidence of CHD and mortality. However, within this overall null effect, early initiation of HT (in terms of time from menopause [< 10 years] and age at initiation [< 60 years]) is associated with reductions in total mortality and CHD incidence. Additionally, a duration of HT use beyond 5 years is associated with a reduction in the incidence of CHD.9,10,20,28,29 These effects of the timing and duration of therapy are unique to HT. Unopposed ET may have an advantageous profile relative to EPT for reducing the incidence of CHD and mortality in postmenopausal women.
Gaining perspective on risks
The risks of stroke and VTE associated with HT are low for women overall and lower still for women who are within 10 years of menopause or younger than age 60 when they start HT. With respect to stroke, fewer cases of stroke developed in users of ET compared with placebo in women who started HT before age 60. The risks of EPT are comparable to those of other medications commonly used in this population of women. More broadly, the magnitude and types of risk associated with HT are similar to those associated with other commonly used therapies.
In addition, the underappreciated benefits of HT, such as potential prevention of diabetes mellitus (15 fewer cases of incident diabetes per 10,000 women per year with EPT and 14 fewer cases with ET), need to be recognized and discussed with our patients. These data are consistent in both observational studies and randomized trials.
The bottom line
As data from randomized trials of HT accumulate, the results are clearly similar to those from the more than 20 observational studies indicating that young, symptomatic postmenopausal women who use HT for long periods have lower rates of CHD and total mortality compared with postmenopausal women who do not use HT. Consistent with these data, the American Association of Clinical Endocrinologists issued a position statement in 2008 concluding that for symptomatic menopausal women under the age of 60, the benefits of HT exceed the risks.53
Nevertheless, the bottom line remains that the estrogen-cardioprotective hypothesis has yet to be studied, since randomized trials have not been conducted in the same population of women from which the hypothesis was generated. This hypothesis will be directly evaluated, however, in the ongoing Early versus Late Intervention Trial with Estradiol (ELITE). This randomized trial, funded by the National Institute on Aging, is designed to determine the effects of 17β-estradiol on the progression of atherosclerosis, cognition, and other postmenopausal health issues in recently menopausal (< 6 years) and remotely menopausal (≥ 10 years) women with no history of cardiovascular disease or diabetes. Until data from trials like ELITE emerge, guidelines such as those from the North American Menopause Society54 (reviewed in the next article in this supplement) are reasonable for clinical practice.
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 2002; 288:321–333.
- Rosenberg L, Palmer JR, Shapiro S. A case-control study of myocardial infarction in relation to use of estrogen supplements. Am J Epidemiol 1993; 137:54–63.
- Mann RD, Lis Y, Chukwujindu J, Chanter DO. A study of the association between hormone replacement therapy, smoking and the occurrence of myocardial infarction in women. J Clin Epidemiol 1994; 47:307–312.
- Psaty B, Heckbert SR, Atkins D, et al. The risk of myocardial infarction associated with the combined use of estrogens and progestins in postmenopausal women. Arch Intern Med 1994; 154:1333–1339.
- Sidney S, Petitti DB, Quisenberry CP Jr. Myocardial infarction and the use of estrogen and estrogen-progestogen in postmenopausal women. Ann Intern Med 1997; 127:501–508.
- Grodstein F, Stampfer MJ, Falkeborn M, Naessen T, Persson I. Postmenopausal hormone therapy and risk of cardiovascular disease and hip fracture in a cohort of Swedish women. Epidemiology 1999; 10:476–480.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Varas-Lorenzo C, García-Rodríguez LA, Perez-Gutthann S, Duque-Oliart A. Hormone replacement therapy and incidence of acute myocardial infarction. A population-based nested case-control study. Circulation 2000; 101:2572–2578.
- Prentice RL, Langer R, Stefanick ML, et al. Combined postmenopausal hormone therapy and cardiovascular disease: toward resolving the discrepancy between observational studies and the Women’s Health Initiative clinical trial. Am J Epidemiol 2005; 162:404–414.
- Prentice RL, Langer RD, Stefanick ML, et al. Combined analysis of Women’s Health Initiative observational and clinical trial data on postmenopausal hormone treatment and cardiovascular disease. Am J Epidemiol 2006; 163:589–599.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Rossouw JE, Prentice RL, Manson JE, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA 2007; 297:1465–1477.
- Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA 2003; 289:2673–2684.
- Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen plus progestin. Maturitas 2006; 55:103–115.
- Cushman M, Kuller LH, Prentice R, et al. Estrogen plus progestin and risk of venous thrombosis. JAMA 2004; 292:1573–1580.
- Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, et al. Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med 2004; 350:991–1004.
- Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA 2003; 290:1729–1738.
- Margolis KL, Bonds DE, Rodabough RJ, et al. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia 2004; 47:1175–1187.
- Heiss G, Wallace R, Anderson GL, et al, for the WHI investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA 2008; 299:1036–1045.
- Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003; 349:523–534.
- Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA 2003; 289:3243–3253.
- Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in post-menopausal women with hysterectomy. JAMA 2006; 295:1647–1657.
- Curb JD, Prentice RL, Bray PF, et al. Venous thrombosis and conjugated equine estrogen in women without a uterus. Arch Intern Med 2006; 166:772–780.
- Bonds DE, Lasser N, Qi L, et al. The effect of conjugated equine oestrogen on diabetes incidence: the Women’s Health Initiative randomised trial. Diabetologia 2006; 49:459–468.
- Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med 1996; 335:453–461.
- Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control 2002; 13:741–751.
- Chilvers CE, Knibb RC, Armstrong SJ, Woods KL, Logan RF. Postmenopausal hormone replacement therapy and risk of acute myocardial infarction—a case control study of women in the East Midlands, UK. Eur Heart J 2003; 24:2197–2205.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med 2006; 166:357–365.
- Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med 2006; 21:363–366.
- Hodis HN, Mack WJ, Lobo RA, et al. Hormone therapy and progression of coronary-artery atherosclerosis in postmenopausal women. N Engl J Med 2003; 349:535–545.
- Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.
- Walsh JM, Pignone M. Drug treatment of hyperlipidemia in women. JAMA 2004; 291:2243–2252.
- Hodis HN, Mack WJ. Postmenopausal hormone therapy in clinical perspective. Menopause 2007; 14:944–957.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996; 335:1001–1009.
- Dale KM, Coleman CI, Henyan NN, Kluger J, White CM. Statins and cancer risk: a meta-analysis. JAMA 2006; 295:74–80.
- Bonovas S, Filioussi K, Tsavaris N, Sitaras NM. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol 2005; 23:8606–8612.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267–1278.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial. Circulation 2006; 113:427–437.
- Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES). Circulation 2005; 112:563–571.
- Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol 2005; 46:166–172.
- Manson JE, Allison MA, Rossouw JE, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med 2007; 356:2591–2602.
- Omenn GS, Goodman GE, Thornquist MD, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 1996; 334:1150–1155.
- Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 2008; 336:262–266.
- Amarenco P, Bogousslavsky J, Callahan A III, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005; 352:1293–1304.
- Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med 1989; 321:129–135.
- Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005; 366:1849–1861.
- DREAM (Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication) Trial Investigators. Effect of rosiglita-zone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: randomised controlled trial. Lancet 2006; 368:1096–1105.
- Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med 2006; 355:125–137.
- American Association of Clinical Endocrinologists (AACE) position statement on hormone replacement therapy (HRT) and cardiovascular risk. American Association of Clinical Endocrinologists Web site. www.aace.com/pub/pdf/guidelines/HRTCVRISKposition_ statement.pdf. Accessed March 5, 2008.
- Estrogen and progestogen use in peri- and postmenopausal women: March 2007 position statement of The North American Menopause Society. Menopause 2007; 14:168–182.
Physicians and their women patients have faced a continuous, confusing mix of information about the risks and benefits of hormone therapy (HT) for perimenopausal and postmenopausal women, most of it without respect to age or the timing of HT relative to menopause. Initial data from the Women’s Health Initiative (WHI) estrogen + progestin (E+P) trial, a prevention study conducted predominantly in older postmenopausal women without menopausal symptoms,1 resulted in questioning of the role of HT (unfortunately and inappropriately in younger symptomatic women). Cumulative trial data and further analyses of the WHI have refined and added to our understanding of the effects of HT, particularly with regard to cardiovascular health. This review will update physicians on the latest data on the risks and benefits of HT, with a particular focus on the heart, and will put the risks of HT into appropriate clinical context.
HORMONE THERAPY AND CARDIOVASCULAR DISEASE: A HISTORICAL PERSPECTIVE
Observational studies conducted prior to the WHI found consistently that women who self-selected to use HT had a reduction in mortality and in the incidence of cardiovascular disease relative to women who did not choose to use HT.2–8 This reduction in risk was apparent whether the HT users had taken ET (estrogen therapy) or EPT (estrogen-progestogen therapy). In contrast, randomized controlled trials failed to confirm these findings from observational studies. However, the findings from randomized controlled trials were derived from older postmenopausal women who were many years past menopause. Often overlooked is the WHI observational study of ET and EPT,9,10 in which women who chose to use HT had a reduction in the risk of coronary heart disease (CHD) similar to that observed among the HT users in other observational studies.
RECENT REPORTS FROM THE WHI
Since the original publication of the WHI E+P trial in 2002,1 an extensive collection of data have been published in piecemeal fashion, contributing to the confusion and misperception of the effects of HT on risks and benefits. It is important to note that the WHI consists of both randomized and observational components, as detailed below, and that data have come from both. Together, these data help clarify the misperceptions generated from the first WHI report of 2002,1 particularly misperceptions regarding the timing of HT initiation relative to menopause and the effect of HT duration on cardiovascular disease outcomes. In most instances, the conclusions drawn from this recent research run counter to the inaccurate but prevalent perception that HT use at any time and at any age is associated with cardiovascular harm, a perception that has unfortunately prevailed since the initial publication of the WHI E+P trial findings in 2002.
The WHI randomized trials and combined analysis
The WHI trials enrolled 27,347 postmenopausal women aged 50 to 79 years at baseline; almost two-thirds of the women enrolled were 60 years of age or older, and the majority of women were more than 10 years past menopause. WHI actually comprised two parallel randomized trials:
- One among 16,608 women who had not undergone hysterectomy (ie, with uterus intact), who were randomized to EPT or placebo (ie, WHI E+P trial) 1
- One among 10,739 women who had undergone hysterectomy, who were randomized to ET or placebo.11
Recent analyses from the WHI, published in 2007, assessed the cardiovascular effects of ET and EPT independently and combined, both overall and according to subject age and years since menopause when randomized.12 Other analyses following the initial WHI E+P trial publication have analyzed the effects of HT according to duration of HT use and according to secondary end points. Many of these analyses have presented risks and benefits in terms of both nominal and adjusted confidence intervals (CIs). Nominal 95% CIs describe the variability in risk estimates that would arise from a simple trial for a single end point. Although nominal CIs are traditionally used, they do not take into account the multiple statistical testing issues (across time and across outcome categories) that occur in a trial. In contrast, adjusted 95% CIs correct for these stastical testing issues. From a clinical perspective, it is most appropriate to look at the adjusted CIs.
WHI: EPT vs placebo
CHD. Although the point estimate for CHD is increased, the 95% CI indicates that EPT has a non-significant effect on CHD outcome relative to placebo among all women randomized in the WHI E+P trial (mean age, 63 years).12 This is a very important point for cardiologists and primary care physicians to note.
In a 2008 analysis of the WHI E+P trial that included a 2.4-year open-label follow-up subsequent to the randomized trial,19 the randomized trial data reported were again different than in previous reports, but remained nonsignificant. The hazard ratio (HR) reported for CHD in the 2008 analysis for the randomized portion of the trial was 1.22 (95% CI, 0.99 to 1.51), as compared with 1.23 (95% CI, 0.99 to 1.53) reported in 200712 (Table 1), 1.24 (95% CI, 1.00 to 1.54) reported in 2003,20 and 1.29 (95% CI, 1.02 to 1.63) reported in 2002.1 In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens (EPT or placebo), the HR for CHD between the original randomized treatment groups was nonsignificant at 0.95 (95% CI, 0.73 to 1.26) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Stroke. The risk of stroke was increased significantly (by an additional 8 events per 10,000 women treated per year) in the EPT arm versus the placebo arm in the nominal analysis,12 but this difference was nonsignificant after adjustment.13
In the 2008 WHI E+P analysis, the HR reported for stroke during the randomized trial phase was different than in previous reports—1.34 (95% CI, 1.05 to 1.71)19 versus 1.31 (95% CI, 1.03 to 1.68) reported in 200712 (Table 1)—and the adjusted analysis was not reported. In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens, the HR for stroke between the original randomized treatment groups was nonsignifi-cant at 1.16 (95% CI, 0.83 to 1.61) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Breast cancer. Breast cancer risk was originally reported to be increased significantly (by an additional 8 cases per 10,000 women per year) in the EPT arm versus the placebo arm with the nominal statistic, but this increase was nonsignificant after adjustment.1 This risk estimate was revised in a follow-up publication 1 year after the original data were reported, and the increase in risk in the EPT arm was still no longer significant in the adjusted analysis.21 Importantly, another subsequent analysis that adjusted for baseline risk factors for breast cancer resulted in a further revision of the risk estimate, which again showed a nonsignificant increase in the EPT arm relative to the placebo arm.14 This is very important since it is commonly accepted that EPT increases the risk of breast cancer when this has not been definitively proven in any randomized controlled trial.
Unfortunately, the most recent breast cancer data14 (Table 1) were not used in the 2008 WHI E+P analysis.19 However, even using the unadjusted data in the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR for breast cancer between the original randomized treatment groups was nonsignificant and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Venous thromboembolism (VTE). EPT was associated with a doubling of the risk of VTE (ie, deep vein thrombosis and pulmonary embolism) compared with placebo, resulting in an excess of 18 VTE events per 10,000 women per year of therapy.15 The risk of VTE was significant across the entire cohort of women (mean age, 63 years).
In the 2008 WHI E+P analysis, the HR reported for VTE during the randomized phase was different than in previous reports—1.98 (95% CI, 1.52 to 2.59)19 versus 2.06 (95% CI, 1.57 to 2.70) reported in 200415 (Table 1)—and the HR during the 2.4-year open-label follow-up, in which women were no longer on their randomized regimens, was no longer significant (HR = 0.95; 95% CI, 0.63 to 1.44). This change in the HR over time from the randomized phase to the open-label phase was statistically significant.19
Fracture. The risk of hip fracture was reduced by 33% with EPT relative to placebo, which was statistically significant in the nominal analysis but not in the adjusted analysis.17 The risk of any fracture was reduced by 24% in women randomized to EPT compared with placebo, which was statistically significant and translated to 47 fewer fractures per 10,000 women per year of therapy.17 Clinically, these results are most impressive given that women randomized in the WHI were not selected on the basis of risk for osteoporosis or fracture. This claim cannot be made for any other therapy.
In the 2008 WHI E+P analysis of the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR between the original randomized treatment groups was nonsignificant for hip fracture and any fracture—0.92 (95% CI, 0.64 to 1.34) and 0.91 (95% CI, 0.78 to 1.06), respectively—and the change in the HR over time from the randomized phase to the open-label phase was not significant for either fracture outcome.19
Diabetes. The risk of new-onset diabetes was reduced by a statistically significant 21% in women randomized to EPT compared with placebo.18
WHI: ET vs placebo
CHD. Importantly, no significant difference was found between the ET and placebo arms with respect to CHD events in the overall cohort of women, whose average age was 64 years.12
Stroke. The risk of stroke was greater with ET than with placebo in the nominal analysis, but importantly, the difference in event rates (11 per 10,000 women per year of therapy) failed to reach significance in the adjusted analysis.11,12
Breast cancer. A strong but nonsignificant trend toward a reduction in breast cancer risk was apparent in the ET arm (8 fewer breast cancer cases per 10,000 women per year of therapy). Among women who actually were adherent to their study regimen (ie, consuming ≥ 80% of their study medication), there was a statistically significant 33% reduction in breast cancer risk with ET relative to placebo.22 Importantly, the reduction in breast cancer risk relative to placebo was found across all the age ranges studied.11
VTE. The excess risk of VTE with ET versus placebo (32%) was less than the excess risk of VTE associated with EPT (Table 1). Importantly, the risk of VTE associated with ET was not statistically significant.11,23
Fracture. The risk of any fracture (hip or vertebral) was reduced significantly in the ET arm compared with the placebo arm.11
Diabetes. In a nominal analysis, there was a trend toward a reduction in the risk of new-onset diabetes in women randomized to ET relative to placebo, which nearly achieved statistical significance.24
WHAT EXPLAINS THE DISCORDANCE BETWEEN OBSERVATIONAL AND RANDOMIZED TRIALS OF HT?
How can the perceived discordance between the results from observational studies and those from randomized controlled trials be explained? There are currently three hypotheses:
- The populations differ in the two types of study designs (observational studies and randomized controlled trials)
- The duration of HT use differs
- The timing of HT initiation differs in relation to age, time since menopause, and stage of atherosclerosis.
Population characteristics
One obvious difference between randomized trials and observational studies of HT is the presence of menopausal symptoms. To maintain blinding, women with hot flashes were predominantly excluded from randomized trials of HT, whereas the presence of hot flashes is the predominant menopausal symptom of women included in observational studies and the main reason women seek HT from their providers.
Other consistent and possibly explanatory differences between clinical trials and observational studies of HT are patient age at enrollment, years since menopause, and body mass index (BMI). Comparing randomized controlled trials with observational studies, age at enrollment was much higher in the clinical trials (mean age ≥ 63 years) than in the observational studies (range of 30 to 55 years). Similarly, women enrolled in randomized trials were more than 10 years beyond menopause, whereas those in observational studies were less than 5 years beyond menopause. In fact, more than 80% of HT users in observational studies initiated HT within 1 or 2 years of menopause.
Additionally, women in randomized trials of HT tend to have higher BMIs than their counterparts in observational studies. For example, mean BMI was considerably higher in the WHI randomized trials (28.5 kg/m2 and 30.1 kg/m2)1,11 than in the observational Nurses’ Health Study (25.8 kg/m2),25 and a full third (34%) of women in the WHI randomized trials were severely obese (BMI ≥ 30 kg/m2).
This point about BMI is noteworthy in light of findings on the effect of BMI on breast cancer risk from an analysis of the WHI observational study among 85,917 women aged 50 to 79 years old at enrollment.26 This analysis found that BMI was unrelated to breast cancer risk among women who had used HT; however, among nonusers of HT, a baseline BMI greater than 31.1 kg/m2 was associated with a 2.52 relative risk of breast cancer compared with a baseline BMI less than 22.6 kg/m2. The risk of breast cancer with increasing BMI was most pronounced in younger postmenopausal women. One interpretation is that high endogenous estrogen levels in postmenopausal women with an elevated BMI serve to increase breast cancer risk to a level beyond which HT adds no further risk. Alternatively, conjugated equine estrogens may act through a selective estrogen receptor modulator mechanism to block any potential adverse breast tissue effects of elevated endogenous estrone and estradiol levels.
Duration of HT
Another hypothesis for the discordant findings between observational and randomized studies of HT focuses on differences in duration of HT use between the two types of studies. Duration of HT use has been substantially longer in observational studies, ranging from 10 years to 40 years, compared with no more than 7 or 8 years in randomized trials to date. Moreover, the results from observational studies have suggested that the longer the duration of HT use, the greater the benefit in terms of CHD risk.
For example, a case-control study by Chilvers et al showed that HT protected against nonfatal myocardial infarction only when used for more than 60 months.27 Analysis of data on EPT use from the Heart and Estrogen/progestin Replacement Study (HERS),28 the randomized WHI E+P trial,20 and the WHI observational study9 reveals an interesting and consistent trend: rates of CHD events increased during the first year of EPT therapy (compared with placebo or nonuse) but then declined over time, ending up below the rates of CHD events in placebo recipients or nonusers of HT after approximately 5 years of therapy. This trend was not as pronounced with ET use in either the WHI randomized trial29 or the WHI observational study,10 but the incidence of CHD events did decline over time with ET use in both studies, and in the WHI observational study, greater than 5 years of ET use was associated with a significant 27% reduction (HR, 0.73; 95% CI, 0.61 to 0.84) in CHD events compared with nonuse.10
Timing of HT initiation
A third hypothesis for the discordance between randomized and observational studies of HT concerns the timing of HT initiation relative to patient age, time since menopause, and stage of atherosclerosis. As noted above, women enrolled in randomized trials have tended to be considerably older and further from menopause compared with their counterparts in observational studies. The effects of differences in timing of HT initiation on specific clinical end points, particularly in relation to cardiovascular health, are reviewed below.
Early and continued HT use may interrupt the pathogenic sequence of vascular aging, potentially preventing progression of atherosclerosis to the late stage at which plaque rupture and clinical events occur. In contrast, late intervention with HT may have little effect on established plaque and, in the case of EPT, may actually predispose to plaque rupture. This concept has been demonstrated in a pair of sister studies, the Women’s Estrogen-Progestin Lipid-Lowering Hormone Atherosclerosis Regression Trial (WELLHART)31 and the Estrogen Prevention Atherosclerosis Trial (EPAT).32
Mortality. The same Stanford University researchers who performed the above meta-analysis of CHD events also assessed odd ratios for overall mortality in a meta-analysis of 30 randomized trials of HT versus placebo that included a total of 26,708 postmenopausal women (representing 119,118 patient-years).33 They found the timing of HT initiation to have an effect on mortality similar to its effect on CHD events. In the overall cohort of women, the odds of death were not different between the HT and placebo groups, but among women younger than 60 years (mean, 54 years), those randomized to HT had a significant 39% reduction in the risk of death (HR = 0.61; 95% CI, 0.39 to 0.95) compared with those randomized to placebo. HT had no effect on mortality among women older than 60 years (mean, 66 years) in this analysis.
These mortality data are consistent with those from the WHI randomized trials, in which both EPT and ET were associated with a 30% reduction in overall mortality relative to placebo among women 50 to 59 years old.12 When both the EPT and ET portions of the WHI were combined to increase the sample size, HT was associated with a significant 30% reduction in mortality (HR = 0.70; 95% CI, 0.51 to 0.96) compared with placebo among women 50 to 59 years old.12
Stroke. The most recent WHI data indicate that stroke is not increased with ET in women 50 to 59 years of age, as there were 2 fewer events per 10,000 women per year of ET relative to placebo.12 In this same age group, the risk of stroke from EPT was increased by 5 events per 10,000 women per year of therapy relative to placebo.12 Among women randomized within 5 years of menopause, stroke risk was increased by 3 events per 10,000 women per year of EPT relative to placebo.13
VTE. Although age was not a significant contributing factor to the risk of VTE from HT in the WHI, the absolute risk of VTE was lower in younger versus older women. The additional absolute risk for VTE events per 10,000 women per year of EPT use was 11 events for women 50 to 59 years old at randomization, 16 events for women 60 to 69 years old at randomization, and 35 events for women 70 to 79 years old at randomization.15 The additional absolute risk for VTE events per 10,000 women per year of ET use was 4 events for women 50 to 59 years old at randomization, 7 events for women 60 to 69 years old at randomization, and 11 events for women 70 to 79 years old at randomization.23 A history of a prior thromboembolic event increases the risk of VTE with postmenopausal HT use, which should be considered before HT is initiated.
HORMONE THERAPY IN CLINICAL PERSPECTIVE
Comparative effects of lipid-lowering therapy and HT
Examination of the evidence regarding lipid-lowering therapy for prevention of CHD, as well as its effects on breast cancer risk and coronary artery calcium scores in women, can add some much-needed perspective and context to the HT data reviewed above.
CHD prevention. Walsh and Pignone examined six randomized controlled trials (N = 11,435) of primary prevention with lipid-lowering medication in women and found no significant effect on CHD events, nonfatal myocardial infarction, CHD mortality, or total mortality.34 In eight randomized controlled trials of secondary prevention (N = 8,272), lipid-lowering therapy in women resulted in significant reductions in CHD end points but had no effect on total mortality.34
Atherosclerosis progression. In three randomized controlled trials, 1 to 4 years of statin therapy had no effect on the progression of coronary artery calcium compared with placebo.41–43 Among 1,064 women 50 to 59 years old who participated in a WHI substudy called the WHI Coronary Artery Calcium Study (WHI-CACS), those who were randomized to ET had significantly less coronary artery calcium at year 7 compared with those assigned to placebo.44 The mean Agatston coronary artery calcium scores were 83.1 with ET versus 123.1 with placebo (P = .02).
Comparing risk of HT with risk of other therapies
Other comparisons yield similar conclusions.35 For instance, a comparison of the ET arm of the WHI randomized trial with raloxifene in the Raloxifene Use for the Heart (RUTH) trial52 reveals similar effects on CHD, stroke, VTE, pulmonary embolism, deep vein thrombosis, and breast cancer, with the only large difference being a greater reduction in bone fracture risk with ET compared with raloxifene.35 Finally, in putting the risk of VTE with HT into perspective, consider that the risk of thromboembolic events with selective estrogen receptor modulators52 and with the fibric acid derivative fenofibrate in diabetics50 is of similar magnitude as the risk with HT.
Risk must be viewed in light of age at HT initiation
CONCLUSIONS FROM RANDOMIZED TRIALS
HT’s effects on CHD and mortality: Timing is everything
Cumulative data from randomized trials indicate that in the overall population of women studied, HT, aspirin, and lipid-lowering therapy each have a null effect on the incidence of CHD and mortality. However, within this overall null effect, early initiation of HT (in terms of time from menopause [< 10 years] and age at initiation [< 60 years]) is associated with reductions in total mortality and CHD incidence. Additionally, a duration of HT use beyond 5 years is associated with a reduction in the incidence of CHD.9,10,20,28,29 These effects of the timing and duration of therapy are unique to HT. Unopposed ET may have an advantageous profile relative to EPT for reducing the incidence of CHD and mortality in postmenopausal women.
Gaining perspective on risks
The risks of stroke and VTE associated with HT are low for women overall and lower still for women who are within 10 years of menopause or younger than age 60 when they start HT. With respect to stroke, fewer cases of stroke developed in users of ET compared with placebo in women who started HT before age 60. The risks of EPT are comparable to those of other medications commonly used in this population of women. More broadly, the magnitude and types of risk associated with HT are similar to those associated with other commonly used therapies.
In addition, the underappreciated benefits of HT, such as potential prevention of diabetes mellitus (15 fewer cases of incident diabetes per 10,000 women per year with EPT and 14 fewer cases with ET), need to be recognized and discussed with our patients. These data are consistent in both observational studies and randomized trials.
The bottom line
As data from randomized trials of HT accumulate, the results are clearly similar to those from the more than 20 observational studies indicating that young, symptomatic postmenopausal women who use HT for long periods have lower rates of CHD and total mortality compared with postmenopausal women who do not use HT. Consistent with these data, the American Association of Clinical Endocrinologists issued a position statement in 2008 concluding that for symptomatic menopausal women under the age of 60, the benefits of HT exceed the risks.53
Nevertheless, the bottom line remains that the estrogen-cardioprotective hypothesis has yet to be studied, since randomized trials have not been conducted in the same population of women from which the hypothesis was generated. This hypothesis will be directly evaluated, however, in the ongoing Early versus Late Intervention Trial with Estradiol (ELITE). This randomized trial, funded by the National Institute on Aging, is designed to determine the effects of 17β-estradiol on the progression of atherosclerosis, cognition, and other postmenopausal health issues in recently menopausal (< 6 years) and remotely menopausal (≥ 10 years) women with no history of cardiovascular disease or diabetes. Until data from trials like ELITE emerge, guidelines such as those from the North American Menopause Society54 (reviewed in the next article in this supplement) are reasonable for clinical practice.
Physicians and their women patients have faced a continuous, confusing mix of information about the risks and benefits of hormone therapy (HT) for perimenopausal and postmenopausal women, most of it without respect to age or the timing of HT relative to menopause. Initial data from the Women’s Health Initiative (WHI) estrogen + progestin (E+P) trial, a prevention study conducted predominantly in older postmenopausal women without menopausal symptoms,1 resulted in questioning of the role of HT (unfortunately and inappropriately in younger symptomatic women). Cumulative trial data and further analyses of the WHI have refined and added to our understanding of the effects of HT, particularly with regard to cardiovascular health. This review will update physicians on the latest data on the risks and benefits of HT, with a particular focus on the heart, and will put the risks of HT into appropriate clinical context.
HORMONE THERAPY AND CARDIOVASCULAR DISEASE: A HISTORICAL PERSPECTIVE
Observational studies conducted prior to the WHI found consistently that women who self-selected to use HT had a reduction in mortality and in the incidence of cardiovascular disease relative to women who did not choose to use HT.2–8 This reduction in risk was apparent whether the HT users had taken ET (estrogen therapy) or EPT (estrogen-progestogen therapy). In contrast, randomized controlled trials failed to confirm these findings from observational studies. However, the findings from randomized controlled trials were derived from older postmenopausal women who were many years past menopause. Often overlooked is the WHI observational study of ET and EPT,9,10 in which women who chose to use HT had a reduction in the risk of coronary heart disease (CHD) similar to that observed among the HT users in other observational studies.
RECENT REPORTS FROM THE WHI
Since the original publication of the WHI E+P trial in 2002,1 an extensive collection of data have been published in piecemeal fashion, contributing to the confusion and misperception of the effects of HT on risks and benefits. It is important to note that the WHI consists of both randomized and observational components, as detailed below, and that data have come from both. Together, these data help clarify the misperceptions generated from the first WHI report of 2002,1 particularly misperceptions regarding the timing of HT initiation relative to menopause and the effect of HT duration on cardiovascular disease outcomes. In most instances, the conclusions drawn from this recent research run counter to the inaccurate but prevalent perception that HT use at any time and at any age is associated with cardiovascular harm, a perception that has unfortunately prevailed since the initial publication of the WHI E+P trial findings in 2002.
The WHI randomized trials and combined analysis
The WHI trials enrolled 27,347 postmenopausal women aged 50 to 79 years at baseline; almost two-thirds of the women enrolled were 60 years of age or older, and the majority of women were more than 10 years past menopause. WHI actually comprised two parallel randomized trials:
- One among 16,608 women who had not undergone hysterectomy (ie, with uterus intact), who were randomized to EPT or placebo (ie, WHI E+P trial) 1
- One among 10,739 women who had undergone hysterectomy, who were randomized to ET or placebo.11
Recent analyses from the WHI, published in 2007, assessed the cardiovascular effects of ET and EPT independently and combined, both overall and according to subject age and years since menopause when randomized.12 Other analyses following the initial WHI E+P trial publication have analyzed the effects of HT according to duration of HT use and according to secondary end points. Many of these analyses have presented risks and benefits in terms of both nominal and adjusted confidence intervals (CIs). Nominal 95% CIs describe the variability in risk estimates that would arise from a simple trial for a single end point. Although nominal CIs are traditionally used, they do not take into account the multiple statistical testing issues (across time and across outcome categories) that occur in a trial. In contrast, adjusted 95% CIs correct for these stastical testing issues. From a clinical perspective, it is most appropriate to look at the adjusted CIs.
WHI: EPT vs placebo
CHD. Although the point estimate for CHD is increased, the 95% CI indicates that EPT has a non-significant effect on CHD outcome relative to placebo among all women randomized in the WHI E+P trial (mean age, 63 years).12 This is a very important point for cardiologists and primary care physicians to note.
In a 2008 analysis of the WHI E+P trial that included a 2.4-year open-label follow-up subsequent to the randomized trial,19 the randomized trial data reported were again different than in previous reports, but remained nonsignificant. The hazard ratio (HR) reported for CHD in the 2008 analysis for the randomized portion of the trial was 1.22 (95% CI, 0.99 to 1.51), as compared with 1.23 (95% CI, 0.99 to 1.53) reported in 200712 (Table 1), 1.24 (95% CI, 1.00 to 1.54) reported in 2003,20 and 1.29 (95% CI, 1.02 to 1.63) reported in 2002.1 In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens (EPT or placebo), the HR for CHD between the original randomized treatment groups was nonsignificant at 0.95 (95% CI, 0.73 to 1.26) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Stroke. The risk of stroke was increased significantly (by an additional 8 events per 10,000 women treated per year) in the EPT arm versus the placebo arm in the nominal analysis,12 but this difference was nonsignificant after adjustment.13
In the 2008 WHI E+P analysis, the HR reported for stroke during the randomized trial phase was different than in previous reports—1.34 (95% CI, 1.05 to 1.71)19 versus 1.31 (95% CI, 1.03 to 1.68) reported in 200712 (Table 1)—and the adjusted analysis was not reported. In the 2.4-year open-label follow-up period in which women were no longer on their randomized regimens, the HR for stroke between the original randomized treatment groups was nonsignifi-cant at 1.16 (95% CI, 0.83 to 1.61) and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Breast cancer. Breast cancer risk was originally reported to be increased significantly (by an additional 8 cases per 10,000 women per year) in the EPT arm versus the placebo arm with the nominal statistic, but this increase was nonsignificant after adjustment.1 This risk estimate was revised in a follow-up publication 1 year after the original data were reported, and the increase in risk in the EPT arm was still no longer significant in the adjusted analysis.21 Importantly, another subsequent analysis that adjusted for baseline risk factors for breast cancer resulted in a further revision of the risk estimate, which again showed a nonsignificant increase in the EPT arm relative to the placebo arm.14 This is very important since it is commonly accepted that EPT increases the risk of breast cancer when this has not been definitively proven in any randomized controlled trial.
Unfortunately, the most recent breast cancer data14 (Table 1) were not used in the 2008 WHI E+P analysis.19 However, even using the unadjusted data in the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR for breast cancer between the original randomized treatment groups was nonsignificant and the change in the HR over time from the randomized phase to the open-label phase was not significant.19
Venous thromboembolism (VTE). EPT was associated with a doubling of the risk of VTE (ie, deep vein thrombosis and pulmonary embolism) compared with placebo, resulting in an excess of 18 VTE events per 10,000 women per year of therapy.15 The risk of VTE was significant across the entire cohort of women (mean age, 63 years).
In the 2008 WHI E+P analysis, the HR reported for VTE during the randomized phase was different than in previous reports—1.98 (95% CI, 1.52 to 2.59)19 versus 2.06 (95% CI, 1.57 to 2.70) reported in 200415 (Table 1)—and the HR during the 2.4-year open-label follow-up, in which women were no longer on their randomized regimens, was no longer significant (HR = 0.95; 95% CI, 0.63 to 1.44). This change in the HR over time from the randomized phase to the open-label phase was statistically significant.19
Fracture. The risk of hip fracture was reduced by 33% with EPT relative to placebo, which was statistically significant in the nominal analysis but not in the adjusted analysis.17 The risk of any fracture was reduced by 24% in women randomized to EPT compared with placebo, which was statistically significant and translated to 47 fewer fractures per 10,000 women per year of therapy.17 Clinically, these results are most impressive given that women randomized in the WHI were not selected on the basis of risk for osteoporosis or fracture. This claim cannot be made for any other therapy.
In the 2008 WHI E+P analysis of the 2.4-year open-label follow-up in which women were no longer on their randomized regimens, the HR between the original randomized treatment groups was nonsignificant for hip fracture and any fracture—0.92 (95% CI, 0.64 to 1.34) and 0.91 (95% CI, 0.78 to 1.06), respectively—and the change in the HR over time from the randomized phase to the open-label phase was not significant for either fracture outcome.19
Diabetes. The risk of new-onset diabetes was reduced by a statistically significant 21% in women randomized to EPT compared with placebo.18
WHI: ET vs placebo
CHD. Importantly, no significant difference was found between the ET and placebo arms with respect to CHD events in the overall cohort of women, whose average age was 64 years.12
Stroke. The risk of stroke was greater with ET than with placebo in the nominal analysis, but importantly, the difference in event rates (11 per 10,000 women per year of therapy) failed to reach significance in the adjusted analysis.11,12
Breast cancer. A strong but nonsignificant trend toward a reduction in breast cancer risk was apparent in the ET arm (8 fewer breast cancer cases per 10,000 women per year of therapy). Among women who actually were adherent to their study regimen (ie, consuming ≥ 80% of their study medication), there was a statistically significant 33% reduction in breast cancer risk with ET relative to placebo.22 Importantly, the reduction in breast cancer risk relative to placebo was found across all the age ranges studied.11
VTE. The excess risk of VTE with ET versus placebo (32%) was less than the excess risk of VTE associated with EPT (Table 1). Importantly, the risk of VTE associated with ET was not statistically significant.11,23
Fracture. The risk of any fracture (hip or vertebral) was reduced significantly in the ET arm compared with the placebo arm.11
Diabetes. In a nominal analysis, there was a trend toward a reduction in the risk of new-onset diabetes in women randomized to ET relative to placebo, which nearly achieved statistical significance.24
WHAT EXPLAINS THE DISCORDANCE BETWEEN OBSERVATIONAL AND RANDOMIZED TRIALS OF HT?
How can the perceived discordance between the results from observational studies and those from randomized controlled trials be explained? There are currently three hypotheses:
- The populations differ in the two types of study designs (observational studies and randomized controlled trials)
- The duration of HT use differs
- The timing of HT initiation differs in relation to age, time since menopause, and stage of atherosclerosis.
Population characteristics
One obvious difference between randomized trials and observational studies of HT is the presence of menopausal symptoms. To maintain blinding, women with hot flashes were predominantly excluded from randomized trials of HT, whereas the presence of hot flashes is the predominant menopausal symptom of women included in observational studies and the main reason women seek HT from their providers.
Other consistent and possibly explanatory differences between clinical trials and observational studies of HT are patient age at enrollment, years since menopause, and body mass index (BMI). Comparing randomized controlled trials with observational studies, age at enrollment was much higher in the clinical trials (mean age ≥ 63 years) than in the observational studies (range of 30 to 55 years). Similarly, women enrolled in randomized trials were more than 10 years beyond menopause, whereas those in observational studies were less than 5 years beyond menopause. In fact, more than 80% of HT users in observational studies initiated HT within 1 or 2 years of menopause.
Additionally, women in randomized trials of HT tend to have higher BMIs than their counterparts in observational studies. For example, mean BMI was considerably higher in the WHI randomized trials (28.5 kg/m2 and 30.1 kg/m2)1,11 than in the observational Nurses’ Health Study (25.8 kg/m2),25 and a full third (34%) of women in the WHI randomized trials were severely obese (BMI ≥ 30 kg/m2).
This point about BMI is noteworthy in light of findings on the effect of BMI on breast cancer risk from an analysis of the WHI observational study among 85,917 women aged 50 to 79 years old at enrollment.26 This analysis found that BMI was unrelated to breast cancer risk among women who had used HT; however, among nonusers of HT, a baseline BMI greater than 31.1 kg/m2 was associated with a 2.52 relative risk of breast cancer compared with a baseline BMI less than 22.6 kg/m2. The risk of breast cancer with increasing BMI was most pronounced in younger postmenopausal women. One interpretation is that high endogenous estrogen levels in postmenopausal women with an elevated BMI serve to increase breast cancer risk to a level beyond which HT adds no further risk. Alternatively, conjugated equine estrogens may act through a selective estrogen receptor modulator mechanism to block any potential adverse breast tissue effects of elevated endogenous estrone and estradiol levels.
Duration of HT
Another hypothesis for the discordant findings between observational and randomized studies of HT focuses on differences in duration of HT use between the two types of studies. Duration of HT use has been substantially longer in observational studies, ranging from 10 years to 40 years, compared with no more than 7 or 8 years in randomized trials to date. Moreover, the results from observational studies have suggested that the longer the duration of HT use, the greater the benefit in terms of CHD risk.
For example, a case-control study by Chilvers et al showed that HT protected against nonfatal myocardial infarction only when used for more than 60 months.27 Analysis of data on EPT use from the Heart and Estrogen/progestin Replacement Study (HERS),28 the randomized WHI E+P trial,20 and the WHI observational study9 reveals an interesting and consistent trend: rates of CHD events increased during the first year of EPT therapy (compared with placebo or nonuse) but then declined over time, ending up below the rates of CHD events in placebo recipients or nonusers of HT after approximately 5 years of therapy. This trend was not as pronounced with ET use in either the WHI randomized trial29 or the WHI observational study,10 but the incidence of CHD events did decline over time with ET use in both studies, and in the WHI observational study, greater than 5 years of ET use was associated with a significant 27% reduction (HR, 0.73; 95% CI, 0.61 to 0.84) in CHD events compared with nonuse.10
Timing of HT initiation
A third hypothesis for the discordance between randomized and observational studies of HT concerns the timing of HT initiation relative to patient age, time since menopause, and stage of atherosclerosis. As noted above, women enrolled in randomized trials have tended to be considerably older and further from menopause compared with their counterparts in observational studies. The effects of differences in timing of HT initiation on specific clinical end points, particularly in relation to cardiovascular health, are reviewed below.
Early and continued HT use may interrupt the pathogenic sequence of vascular aging, potentially preventing progression of atherosclerosis to the late stage at which plaque rupture and clinical events occur. In contrast, late intervention with HT may have little effect on established plaque and, in the case of EPT, may actually predispose to plaque rupture. This concept has been demonstrated in a pair of sister studies, the Women’s Estrogen-Progestin Lipid-Lowering Hormone Atherosclerosis Regression Trial (WELLHART)31 and the Estrogen Prevention Atherosclerosis Trial (EPAT).32
Mortality. The same Stanford University researchers who performed the above meta-analysis of CHD events also assessed odd ratios for overall mortality in a meta-analysis of 30 randomized trials of HT versus placebo that included a total of 26,708 postmenopausal women (representing 119,118 patient-years).33 They found the timing of HT initiation to have an effect on mortality similar to its effect on CHD events. In the overall cohort of women, the odds of death were not different between the HT and placebo groups, but among women younger than 60 years (mean, 54 years), those randomized to HT had a significant 39% reduction in the risk of death (HR = 0.61; 95% CI, 0.39 to 0.95) compared with those randomized to placebo. HT had no effect on mortality among women older than 60 years (mean, 66 years) in this analysis.
These mortality data are consistent with those from the WHI randomized trials, in which both EPT and ET were associated with a 30% reduction in overall mortality relative to placebo among women 50 to 59 years old.12 When both the EPT and ET portions of the WHI were combined to increase the sample size, HT was associated with a significant 30% reduction in mortality (HR = 0.70; 95% CI, 0.51 to 0.96) compared with placebo among women 50 to 59 years old.12
Stroke. The most recent WHI data indicate that stroke is not increased with ET in women 50 to 59 years of age, as there were 2 fewer events per 10,000 women per year of ET relative to placebo.12 In this same age group, the risk of stroke from EPT was increased by 5 events per 10,000 women per year of therapy relative to placebo.12 Among women randomized within 5 years of menopause, stroke risk was increased by 3 events per 10,000 women per year of EPT relative to placebo.13
VTE. Although age was not a significant contributing factor to the risk of VTE from HT in the WHI, the absolute risk of VTE was lower in younger versus older women. The additional absolute risk for VTE events per 10,000 women per year of EPT use was 11 events for women 50 to 59 years old at randomization, 16 events for women 60 to 69 years old at randomization, and 35 events for women 70 to 79 years old at randomization.15 The additional absolute risk for VTE events per 10,000 women per year of ET use was 4 events for women 50 to 59 years old at randomization, 7 events for women 60 to 69 years old at randomization, and 11 events for women 70 to 79 years old at randomization.23 A history of a prior thromboembolic event increases the risk of VTE with postmenopausal HT use, which should be considered before HT is initiated.
HORMONE THERAPY IN CLINICAL PERSPECTIVE
Comparative effects of lipid-lowering therapy and HT
Examination of the evidence regarding lipid-lowering therapy for prevention of CHD, as well as its effects on breast cancer risk and coronary artery calcium scores in women, can add some much-needed perspective and context to the HT data reviewed above.
CHD prevention. Walsh and Pignone examined six randomized controlled trials (N = 11,435) of primary prevention with lipid-lowering medication in women and found no significant effect on CHD events, nonfatal myocardial infarction, CHD mortality, or total mortality.34 In eight randomized controlled trials of secondary prevention (N = 8,272), lipid-lowering therapy in women resulted in significant reductions in CHD end points but had no effect on total mortality.34
Atherosclerosis progression. In three randomized controlled trials, 1 to 4 years of statin therapy had no effect on the progression of coronary artery calcium compared with placebo.41–43 Among 1,064 women 50 to 59 years old who participated in a WHI substudy called the WHI Coronary Artery Calcium Study (WHI-CACS), those who were randomized to ET had significantly less coronary artery calcium at year 7 compared with those assigned to placebo.44 The mean Agatston coronary artery calcium scores were 83.1 with ET versus 123.1 with placebo (P = .02).
Comparing risk of HT with risk of other therapies
Other comparisons yield similar conclusions.35 For instance, a comparison of the ET arm of the WHI randomized trial with raloxifene in the Raloxifene Use for the Heart (RUTH) trial52 reveals similar effects on CHD, stroke, VTE, pulmonary embolism, deep vein thrombosis, and breast cancer, with the only large difference being a greater reduction in bone fracture risk with ET compared with raloxifene.35 Finally, in putting the risk of VTE with HT into perspective, consider that the risk of thromboembolic events with selective estrogen receptor modulators52 and with the fibric acid derivative fenofibrate in diabetics50 is of similar magnitude as the risk with HT.
Risk must be viewed in light of age at HT initiation
CONCLUSIONS FROM RANDOMIZED TRIALS
HT’s effects on CHD and mortality: Timing is everything
Cumulative data from randomized trials indicate that in the overall population of women studied, HT, aspirin, and lipid-lowering therapy each have a null effect on the incidence of CHD and mortality. However, within this overall null effect, early initiation of HT (in terms of time from menopause [< 10 years] and age at initiation [< 60 years]) is associated with reductions in total mortality and CHD incidence. Additionally, a duration of HT use beyond 5 years is associated with a reduction in the incidence of CHD.9,10,20,28,29 These effects of the timing and duration of therapy are unique to HT. Unopposed ET may have an advantageous profile relative to EPT for reducing the incidence of CHD and mortality in postmenopausal women.
Gaining perspective on risks
The risks of stroke and VTE associated with HT are low for women overall and lower still for women who are within 10 years of menopause or younger than age 60 when they start HT. With respect to stroke, fewer cases of stroke developed in users of ET compared with placebo in women who started HT before age 60. The risks of EPT are comparable to those of other medications commonly used in this population of women. More broadly, the magnitude and types of risk associated with HT are similar to those associated with other commonly used therapies.
In addition, the underappreciated benefits of HT, such as potential prevention of diabetes mellitus (15 fewer cases of incident diabetes per 10,000 women per year with EPT and 14 fewer cases with ET), need to be recognized and discussed with our patients. These data are consistent in both observational studies and randomized trials.
The bottom line
As data from randomized trials of HT accumulate, the results are clearly similar to those from the more than 20 observational studies indicating that young, symptomatic postmenopausal women who use HT for long periods have lower rates of CHD and total mortality compared with postmenopausal women who do not use HT. Consistent with these data, the American Association of Clinical Endocrinologists issued a position statement in 2008 concluding that for symptomatic menopausal women under the age of 60, the benefits of HT exceed the risks.53
Nevertheless, the bottom line remains that the estrogen-cardioprotective hypothesis has yet to be studied, since randomized trials have not been conducted in the same population of women from which the hypothesis was generated. This hypothesis will be directly evaluated, however, in the ongoing Early versus Late Intervention Trial with Estradiol (ELITE). This randomized trial, funded by the National Institute on Aging, is designed to determine the effects of 17β-estradiol on the progression of atherosclerosis, cognition, and other postmenopausal health issues in recently menopausal (< 6 years) and remotely menopausal (≥ 10 years) women with no history of cardiovascular disease or diabetes. Until data from trials like ELITE emerge, guidelines such as those from the North American Menopause Society54 (reviewed in the next article in this supplement) are reasonable for clinical practice.
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 2002; 288:321–333.
- Rosenberg L, Palmer JR, Shapiro S. A case-control study of myocardial infarction in relation to use of estrogen supplements. Am J Epidemiol 1993; 137:54–63.
- Mann RD, Lis Y, Chukwujindu J, Chanter DO. A study of the association between hormone replacement therapy, smoking and the occurrence of myocardial infarction in women. J Clin Epidemiol 1994; 47:307–312.
- Psaty B, Heckbert SR, Atkins D, et al. The risk of myocardial infarction associated with the combined use of estrogens and progestins in postmenopausal women. Arch Intern Med 1994; 154:1333–1339.
- Sidney S, Petitti DB, Quisenberry CP Jr. Myocardial infarction and the use of estrogen and estrogen-progestogen in postmenopausal women. Ann Intern Med 1997; 127:501–508.
- Grodstein F, Stampfer MJ, Falkeborn M, Naessen T, Persson I. Postmenopausal hormone therapy and risk of cardiovascular disease and hip fracture in a cohort of Swedish women. Epidemiology 1999; 10:476–480.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Varas-Lorenzo C, García-Rodríguez LA, Perez-Gutthann S, Duque-Oliart A. Hormone replacement therapy and incidence of acute myocardial infarction. A population-based nested case-control study. Circulation 2000; 101:2572–2578.
- Prentice RL, Langer R, Stefanick ML, et al. Combined postmenopausal hormone therapy and cardiovascular disease: toward resolving the discrepancy between observational studies and the Women’s Health Initiative clinical trial. Am J Epidemiol 2005; 162:404–414.
- Prentice RL, Langer RD, Stefanick ML, et al. Combined analysis of Women’s Health Initiative observational and clinical trial data on postmenopausal hormone treatment and cardiovascular disease. Am J Epidemiol 2006; 163:589–599.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Rossouw JE, Prentice RL, Manson JE, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA 2007; 297:1465–1477.
- Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA 2003; 289:2673–2684.
- Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen plus progestin. Maturitas 2006; 55:103–115.
- Cushman M, Kuller LH, Prentice R, et al. Estrogen plus progestin and risk of venous thrombosis. JAMA 2004; 292:1573–1580.
- Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, et al. Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med 2004; 350:991–1004.
- Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA 2003; 290:1729–1738.
- Margolis KL, Bonds DE, Rodabough RJ, et al. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia 2004; 47:1175–1187.
- Heiss G, Wallace R, Anderson GL, et al, for the WHI investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA 2008; 299:1036–1045.
- Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003; 349:523–534.
- Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA 2003; 289:3243–3253.
- Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in post-menopausal women with hysterectomy. JAMA 2006; 295:1647–1657.
- Curb JD, Prentice RL, Bray PF, et al. Venous thrombosis and conjugated equine estrogen in women without a uterus. Arch Intern Med 2006; 166:772–780.
- Bonds DE, Lasser N, Qi L, et al. The effect of conjugated equine oestrogen on diabetes incidence: the Women’s Health Initiative randomised trial. Diabetologia 2006; 49:459–468.
- Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med 1996; 335:453–461.
- Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control 2002; 13:741–751.
- Chilvers CE, Knibb RC, Armstrong SJ, Woods KL, Logan RF. Postmenopausal hormone replacement therapy and risk of acute myocardial infarction—a case control study of women in the East Midlands, UK. Eur Heart J 2003; 24:2197–2205.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med 2006; 166:357–365.
- Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med 2006; 21:363–366.
- Hodis HN, Mack WJ, Lobo RA, et al. Hormone therapy and progression of coronary-artery atherosclerosis in postmenopausal women. N Engl J Med 2003; 349:535–545.
- Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.
- Walsh JM, Pignone M. Drug treatment of hyperlipidemia in women. JAMA 2004; 291:2243–2252.
- Hodis HN, Mack WJ. Postmenopausal hormone therapy in clinical perspective. Menopause 2007; 14:944–957.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996; 335:1001–1009.
- Dale KM, Coleman CI, Henyan NN, Kluger J, White CM. Statins and cancer risk: a meta-analysis. JAMA 2006; 295:74–80.
- Bonovas S, Filioussi K, Tsavaris N, Sitaras NM. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol 2005; 23:8606–8612.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267–1278.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial. Circulation 2006; 113:427–437.
- Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES). Circulation 2005; 112:563–571.
- Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol 2005; 46:166–172.
- Manson JE, Allison MA, Rossouw JE, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med 2007; 356:2591–2602.
- Omenn GS, Goodman GE, Thornquist MD, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 1996; 334:1150–1155.
- Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 2008; 336:262–266.
- Amarenco P, Bogousslavsky J, Callahan A III, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005; 352:1293–1304.
- Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med 1989; 321:129–135.
- Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005; 366:1849–1861.
- DREAM (Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication) Trial Investigators. Effect of rosiglita-zone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: randomised controlled trial. Lancet 2006; 368:1096–1105.
- Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med 2006; 355:125–137.
- American Association of Clinical Endocrinologists (AACE) position statement on hormone replacement therapy (HRT) and cardiovascular risk. American Association of Clinical Endocrinologists Web site. www.aace.com/pub/pdf/guidelines/HRTCVRISKposition_ statement.pdf. Accessed March 5, 2008.
- Estrogen and progestogen use in peri- and postmenopausal women: March 2007 position statement of The North American Menopause Society. Menopause 2007; 14:168–182.
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 2002; 288:321–333.
- Rosenberg L, Palmer JR, Shapiro S. A case-control study of myocardial infarction in relation to use of estrogen supplements. Am J Epidemiol 1993; 137:54–63.
- Mann RD, Lis Y, Chukwujindu J, Chanter DO. A study of the association between hormone replacement therapy, smoking and the occurrence of myocardial infarction in women. J Clin Epidemiol 1994; 47:307–312.
- Psaty B, Heckbert SR, Atkins D, et al. The risk of myocardial infarction associated with the combined use of estrogens and progestins in postmenopausal women. Arch Intern Med 1994; 154:1333–1339.
- Sidney S, Petitti DB, Quisenberry CP Jr. Myocardial infarction and the use of estrogen and estrogen-progestogen in postmenopausal women. Ann Intern Med 1997; 127:501–508.
- Grodstein F, Stampfer MJ, Falkeborn M, Naessen T, Persson I. Postmenopausal hormone therapy and risk of cardiovascular disease and hip fracture in a cohort of Swedish women. Epidemiology 1999; 10:476–480.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Varas-Lorenzo C, García-Rodríguez LA, Perez-Gutthann S, Duque-Oliart A. Hormone replacement therapy and incidence of acute myocardial infarction. A population-based nested case-control study. Circulation 2000; 101:2572–2578.
- Prentice RL, Langer R, Stefanick ML, et al. Combined postmenopausal hormone therapy and cardiovascular disease: toward resolving the discrepancy between observational studies and the Women’s Health Initiative clinical trial. Am J Epidemiol 2005; 162:404–414.
- Prentice RL, Langer RD, Stefanick ML, et al. Combined analysis of Women’s Health Initiative observational and clinical trial data on postmenopausal hormone treatment and cardiovascular disease. Am J Epidemiol 2006; 163:589–599.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Rossouw JE, Prentice RL, Manson JE, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA 2007; 297:1465–1477.
- Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA 2003; 289:2673–2684.
- Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen plus progestin. Maturitas 2006; 55:103–115.
- Cushman M, Kuller LH, Prentice R, et al. Estrogen plus progestin and risk of venous thrombosis. JAMA 2004; 292:1573–1580.
- Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, et al. Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med 2004; 350:991–1004.
- Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA 2003; 290:1729–1738.
- Margolis KL, Bonds DE, Rodabough RJ, et al. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia 2004; 47:1175–1187.
- Heiss G, Wallace R, Anderson GL, et al, for the WHI investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA 2008; 299:1036–1045.
- Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003; 349:523–534.
- Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA 2003; 289:3243–3253.
- Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in post-menopausal women with hysterectomy. JAMA 2006; 295:1647–1657.
- Curb JD, Prentice RL, Bray PF, et al. Venous thrombosis and conjugated equine estrogen in women without a uterus. Arch Intern Med 2006; 166:772–780.
- Bonds DE, Lasser N, Qi L, et al. The effect of conjugated equine oestrogen on diabetes incidence: the Women’s Health Initiative randomised trial. Diabetologia 2006; 49:459–468.
- Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med 1996; 335:453–461.
- Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control 2002; 13:741–751.
- Chilvers CE, Knibb RC, Armstrong SJ, Woods KL, Logan RF. Postmenopausal hormone replacement therapy and risk of acute myocardial infarction—a case control study of women in the East Midlands, UK. Eur Heart J 2003; 24:2197–2205.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med 2006; 166:357–365.
- Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med 2006; 21:363–366.
- Hodis HN, Mack WJ, Lobo RA, et al. Hormone therapy and progression of coronary-artery atherosclerosis in postmenopausal women. N Engl J Med 2003; 349:535–545.
- Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.
- Walsh JM, Pignone M. Drug treatment of hyperlipidemia in women. JAMA 2004; 291:2243–2252.
- Hodis HN, Mack WJ. Postmenopausal hormone therapy in clinical perspective. Menopause 2007; 14:944–957.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996; 335:1001–1009.
- Dale KM, Coleman CI, Henyan NN, Kluger J, White CM. Statins and cancer risk: a meta-analysis. JAMA 2006; 295:74–80.
- Bonovas S, Filioussi K, Tsavaris N, Sitaras NM. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol 2005; 23:8606–8612.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267–1278.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial. Circulation 2006; 113:427–437.
- Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES). Circulation 2005; 112:563–571.
- Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol 2005; 46:166–172.
- Manson JE, Allison MA, Rossouw JE, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med 2007; 356:2591–2602.
- Omenn GS, Goodman GE, Thornquist MD, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 1996; 334:1150–1155.
- Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 2008; 336:262–266.
- Amarenco P, Bogousslavsky J, Callahan A III, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005; 352:1293–1304.
- Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med 1989; 321:129–135.
- Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005; 366:1849–1861.
- DREAM (Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication) Trial Investigators. Effect of rosiglita-zone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: randomised controlled trial. Lancet 2006; 368:1096–1105.
- Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med 2006; 355:125–137.
- American Association of Clinical Endocrinologists (AACE) position statement on hormone replacement therapy (HRT) and cardiovascular risk. American Association of Clinical Endocrinologists Web site. www.aace.com/pub/pdf/guidelines/HRTCVRISKposition_ statement.pdf. Accessed March 5, 2008.
- Estrogen and progestogen use in peri- and postmenopausal women: March 2007 position statement of The North American Menopause Society. Menopause 2007; 14:168–182.
Case studies and clinical considerations in menopausal management
Dr. Holly Thacker: In light of the updates that Drs. Hodis and Gass have presented on hormone therapy (HT) for menopausal women and that Drs. Jenkins and Sikon have presented on nonhormonal options for menopausal management, let’s start our roundtable by considering a couple of case studies that will give us the chance to apply the latest data in a practical way.
CASE 1: A SYMPTOMATIC 67-YEAR-OLD IN WHOM HORMONE THERAPY WAS ABRUPTLY STOPPED
Dr. Margaret McKenzie: A 67-year-old menopausal woman presents for the evaluation of hot flashes, vaginal dryness causing dyspareunia, and decreased libido. She was previously on estrogen-progestogen therapy (EPT), consisting of daily conjugated equine estrogens and medroxyprogesterone acetate, for 15 years starting at the time of natural menopause. Her gynecologist discontinued this HT abruptly at the time of the initial release of data from the Women’s Health Initiative trial, and the patient is now seeking another opinion about resuming HT. When she presents, she has been off HT for less than 6 months. Would you restart HT in this patient?
Dr. Andrea Sikon: The abrupt discontinuation certainly contributes to her symptoms. The short duration of time off HT is important, and would lead me to restart HT after an updated review of risk factors. She had been on it for 15 years and has done fine, so she appears to be an ideal candidate to restart.
Dr. McKenzie: What specific questions would you ask when doing your risk assessment? How would you evaluate this patient to determine whether she is a good candidate to continue HT?
Dr. Thacker: I would obtain a family history. Using a population-based risk assessment such as the Gail model, I would calculate her absolute risk of breast cancer based on her duration of EPT use. I might offer her a lower-dose regimen. A conjugated equine estrogen dosage of 0.3 mg/day may be as effective in a 67-year-old woman as 0.625 mg/day is in a younger woman in terms of relieving vasomotor symptoms, depending on individual metabolism. We do have evidence from the HOPE trial that 0.3 mg/day is effective for relief of vasomotor symptoms.1 In addition, data from the Nurses’ Health Study show no increased risk of stroke with 0.3 mg/day, as opposed to the increased risk with 0.625 mg/day, and there are other data showing that the risk of stroke is possibly related to dosage.2
At the same time, we do not yet have long-term data to show that the lower dose is necessarily safer and we do not have data on bone fracture risk with the lower dose, so I would want to know this patient’s bone mineral density (BMD). I would also want to know about her cardiovascular risk profile, including her lipid profile, and I would want more details about her sexual function.
Dr. McKenzie: I will supply a few more case details. This patient’s body mass index (BMI) was 24 kg/m2. She exercised regularly. Her BMD was normal for her age. She was taking a statin to treat hyperlipidemia. She was a nonsmoker, and her family history was unremarkable. Does any of this information change the way that you would counsel her?
Dr. Howard Hodis: Knowing her BMI and that she was on a statin, I would have even less of a problem reinitiating HT.
Case continued
Dr. McKenzie: Well, EPT was reinitiated in this patient at a lower dose (0.45/1.5 mg), and she was satisfied. At her most recent visit, several years later, the possibility of reducing her dose of HT was offered; however, the patient is happy with her quality of life and accepts whatever risk that continued HT may bring. She inquired about transdermal testosterone to restore her sex drive, and it was agreed that if it receives US marketing approval for women with decreased libido, a 24-week trial would be attempted.
Dr. Hodis: If you look at the data, this patient not only may enhance her quality of life by continuing HT but might extend it as well.
Dr. Thacker: Many patients inquire about using testosterone only, without estrogen, for treating dyspareunia and low libido. Clinicians must understand that testosterone is aromatized to estrogen. If a patient is on a high dose of oral estrogen, I would consider switching to transdermal estrogen before trying testosterone, whose use in women remains off-label in the United States. But the patient in our case has been doing well for several years on low-dose estrogen and she still has her ovaries.
Dr. Margery Gass: Some colleagues and I completed a study, which was presented at a recent Endocrine Society meeting,3 in which transdermal testosterone was just as effective without estrogen in increasing libido. But this remains moot for general clinical practice unless the transdermal testosterone patch is approved in this country (as it is already approved for use in women in Europe).
Dr. Hodis: Would any of you be worried about this patient’s fracture risk after having HT stopped following 15 years of use? Data show that the rate of bone loss after abrupt cessation of HT is just as great as when a woman is going through menopause.
Dr. Gass: Yes, and that is exactly the point. The woman should be assessed under these circumstances just as she would be at menopause, using the same risk factors.
Dr. Thacker: I think that underscores that there is risk in stopping treatment, just as there is in taking treatment or not taking treatment, and all of these risks should be considered. Many times, once a patient is off HT, some clinicians forget to check the patient’s BMD or to do a complete genital examination.
Dr. Sikon: Many providers who do not specialize in women’s health may forget that when HT is stopped, it is as if a newly menopausal state is being created. Providers need to think about ensuing changes in bone and genitourinary status as well as quality-of-life concerns.
Dr. McKenzie: In today’s clinical environment, there is awareness of the importance of long-term bone health because patients are living longer. The use of BMD measurements in practice is clearly expanding.
Dr. Thacker: It is worth noting that all of the drugs used to treat osteoporosis have been studied primarily in women who already have osteoporosis. The therapy with the most data to support a reduction in the risk of all types of fracture is HT. These data are very impressive, and although fracture prevention would not be the sole reason for using HT, it can make the overall risk-benefit assessment easier, particularly if it can be determined whether or not an individual patient is at high risk of venous thromboembolism (VTE).
CASE 2: A SYMPTOMATIC 47-YEAR-OLD WITH A HISTORY OF BREAST CANCER
Dr. McKenzie: A 47-year-old postmenopausal woman with a 7-year history of breast cancer presents for the management of hot flashes, irritability, and reduced sleep. In addition, recent onset of vaginal dryness is causing dyspareunia that is not alleviated by lubricants. Her breast cancer was estrogen receptor (ER)/progesterone receptor (PR)–positive, and she received tamoxifen therapy for 5 years (now completed) following the initial diagnosis and management. How would you approach the management of this patient?
Dr. Marjorie Jenkins: I would first try to determine the severity of her hot flashes and how much her symptoms are affecting her quality of life. She may say that she is still having hot flashes, but how frequent are they? Do they cause nighttime awakening and subsequent fatigue?
Dr. McKenzie: The reason this patient presented was to ask for some form of relief because her symptoms were affecting her quality of life. Her dyspareunia was getting worse. She was trying various lubricants without success. At the same time, she expressed fear because her tumor was ER/PR-positive. Most cancer survivors have recurrence in the back of their mind even though they are in remission.
Dr. Jenkins: Was she asking specifically about HT or about help to relieve her symptoms?
Dr. McKenzie: She was asking for help for her symptoms.
Dr. Jenkins: I would consider low-dose vaginal estrogen to address her dyspareunia. I would also consider a serotonin-norepinephrine reuptake inhibitor, such as venlafaxine, to treat her hot flashes and irritability, along with lifestyle modifications, although the latter do not have evidence-based support. If these measures failed to offer relief, I would reconsider the risks and benefits of low-dose HT. I would call her oncologist for input if I planned to start vaginal estrogen, low-dose topical testosterone, or any type of hormonal treatment. I would make sure that the patient knew that her oncologist was working as part of the team responsible for her management.
Dr. Thacker: I concur. When I see hormonally sensitive breast cancer patients with vaginal symptoms, particularly when they are taking tamoxifen, I often talk to them about local estrogen before vaginal atrophy becomes severe. Once the atrophy becomes severe, local estrogen, even in low doses, may be absorbed systemically (increasing the risk of endometrial hyperplasia) until the the vagina becomes re-estrogenized and stratified with healthy squamous epithelium. Once this restratification takes place, there are generally no systemic hormonal effects with low-dose local vaginal estrogen, but it is best to avoid severe atrophy in the first place. I like to start local estrogen early if I know that the oncologist wants to use an aromatase inhibitor in a breast cancer survivor. I prescribe the low-dose vaginal form frequently in my practice, and order transvaginal ultrasonography liberally if there is concern about the endometrium.
Additionally, I would offer this patient venlafaxine or, more specifically, desvenlafaxine, as the literature has shown that the latter agent is associated with an improvement in sleep.4 (Currently, desvenlafaxine has been approved by the US Food and Drug Administration [FDA] solely to treat major depression; however, it has been studied in nondepressed women with hot flashes and is expected to be the first nonhormonal agent to receive FDA approval specifically to treat hot flashes.)
Dr. Gass: This patient still has her uterus in place. Data show that estrogens have a first-pass uterine effect, and this gives me pause because estrogen levels could well be higher in the uterus than in the bloodstream. Because of those data, as well as the absence of long-term safety data, the use of estrogen in this patient would cause me concern.
With breast cancer patients in particular, I try everything else to treat vaginal dryness before adding estrogen. I believe that if a patient is having dyspareunia despite the use of adequate lubricants, something else is the problem. In many cases these women have not had intercourse for months because they have been undergoing treatment for breast cancer, and they can have hallmark pain syndromes or constriction of the vagina that may require treatments besides just estrogen. If all else failed, I would prescribe vaginal estrogen on a temporary basis. Women who stay sexually active after menopause can do perfectly fine without treatment, but those who have periods of abstinence and then try to resume sexual activity typically run into problems.
Dr. Hodis: Would you have concern about breast cancer recurrence with estrogen reinitiation, based on the literature?
Dr. Gass: I have seen recurrences out to 20 years after the initial cancer. If the cancer does recur, the woman will always have a nagging doubt that it could have been avoided if she had not used estrogen.
Dr. Thacker: We have many breast cancer survivors in our practice. It is an easier decision to give estrogen to women who have had bilateral mastectomy with reconstruction for a stage I breast cancer and have already had a hysterectomy or bilateral salpingooophorectomy. But we otherwise try to avoid it unless the patient has first tried everything else and is miserable from her vaginal symptoms.
Dr. Gass: When a patient is diagnosed with breast cancer, I gently encourage her to continue sexual activity through the course of treatment, explaining that she may be far better off later. It may avoid a lot of problems if we can proactively get that message across.
Dr. Jenkins: That is a great point, and there is evidence that increased sexual activity decreases vaginal atrophy and assists in maintaining vaginal elasticity and the ability of urogenital congestion with arousal. Although lubricants and moisturizers do work well, they may require repeated application, and inelasticity is still a problem for some patients. It is somewhat of a “use it or lose it” proposition.
Dr. Thacker: Recurrent urinary tract infections (UTIs) are a problem as well. Patients see urologists, undergo multiple endoscopies, and are treated with antibiotics, sometimes chronically, yet often they are not even offered local vaginal estrogen, which reduces recurrent UTIs. Local estrogen should be considered in any woman with vaginal atrophy and recurrent UTIs.
Case continued
Dr. McKenzie: To return to our case, this patient’s vagina was, in fact, severely constricted because she had not been sexually active for a while. Her BMI was initially greater than 25 kg/m2, but she lost weight and became more symptomatic as she did so. She then stopped having sex because it was painful.
When she presented initially, she had a package of black cohosh with her and was willing to try it for her symptoms but was apprehensive after reading the disclaimers in the package. A 47-year-old who has already been diagnosed with ER-positive breast cancer is generally anxious about using any therapies that may be associated with an increased risk of breast cancer.
After examination of her vagina, her oncologist was consulted and suggested that her serum estradiol levels be measured; they were less than 20 pg/mL. We then agreed to a trial of estradiol vaginal tablets, vaginal dilators, and an increase in her sexual activity. She has been on vaginal estradiol for 2 years and is functioning very well. Her hot flashes improved spontaneously as her body adapted to her new weight.
BEYOND THE CASES: OTHER CHALLENGES IN MENOPAUSAL MANAGEMENT
HT discontinuation, dose reduction in real-world practice
Dr. Thacker: The first case we covered touched on both discontinuation of HT and HT dosage reduction. These are issues that come up often in clinical practice; what lessons does the panel have to share on these issues?
Dr. Gass: I find that there is a small subset of women who are highly symptomatic and are probably always going to be miserable whenever they try to go off HT. For some, if they are highly symptomatic at menopause, they tend to stay that way. They may try to go off, but a year later, they come back and say, “I am just too miserable.”
Dr. McKenzie: In my practice, I have noticed patients who end up staying on higher doses of HT for a long period because they do not tolerate weaning. If you take them down to 0.625 mg of estrogen, their hot flashes resume, so they seem to require 0.9 mg.
Dr. Thacker: I have a very small subset of those women too. I wonder if their metabolism is different; maybe 0.9 mg of conjugated equine estrogens is to them what 0.3 mg is to other women. As women get older, perhaps metabolic changes are one reason that many can reduce their hormone dosage. It is very challenging. I tell my students that it is much easier trying to determine how much thyroid hormone replacement to give a patient than how much estrogen.
When does transdermal estrogen make sense?
Dr. Sikon: I would be interested in the rest of the panel’s views on management of a woman in her early postmenopausal years who is symptomatic and has been on oral HT and is also a smoker. Would you switch her to transdermal estrogen or continue her oral HT and continue aggressive smoking cessation counseling?
Dr. Thacker: Many practitioners think that a smoker cannot take any type of HT because they equate it to oral/hormonal contraceptives, which increase the risk of heart attack in smokers over age 35, but hormonal contraceptives are different in that they involve a much higher dose of hormone. In my practice, the cases when I will offer transdermal estrogen are generally when a patient has gastrointestinal upset, known gallbladder disease, elevated triglycerides, or a prior deep vein thrombosis (DVT), even though I will tell the patient that the HT-associated risks are still possible with transdermal therapies. Many women are inappropriately and inaccurately told that compounded transdermal therapies are “risk free.”
Dr. McKenzie: Transdermal estrogen is also an option for patients who are poor pill takers or are already taking too many pills. Many of my patients are on transdermal estrogen for the convenience that it offers. It is unfortunate that transdermal progesterone cream does not protect the endometrium in all patients; for women with a uterus, an oral progestogen needs to be prescribed. However, two transdermal patches containing progestogens have been shown to be efficacious in protecting the endometrium.
How should a history of DVT affect decision-making?
Dr. McKenzie: What do you do when a patient has a history of postoperative DVT and is already on HT? How many of the panel would discontinue the HT as opposed to continuing it?
Dr. Hodis: If it were a history of spontaneous DVT, I would feel uncomfortable continuing HT. A few years ago, a clinical trial was stopped early because women with a prior spontaneous DVT who were randomized to HT had a substantial increase in DVT incidence relative to those randomized to placebo.5 In the case of provoked or postoperative DVT, it may be a tougher call.
Dr. Thacker: I think that DVT is the greatest risk with HT, even though the media are more focused on breast cancer risk. The risk of breast cancer with estrogen alone is debatable, at least with oral conjugated estrogen, which was associated with a decreased risk in women who had undergone hysterectomy in the Women’s Health Initiative (WHI).6
When I see a woman with a history of DVT in my practice, I check her homocysteine levels and check for factor V Leiden and prothrombin gene mutation. If I find an inherited hypercoagulability disorder, I tell the patient that her risk of DVT with any type of hormone product is not just multiplicative, it is logarithmic. If the patient already requires lifelong anticoagulation, then I am a bit more comfortable with prescribing HT and I usually will try the transdermal route first; however, I always consider nonhormonal treatment alternatives first.
Dr. Gass: The WHI was supposed to have excluded women with a history of DVT, but a few such women were enrolled, and it was demonstrated that they were at higher risk of DVT recurrence if randomized to HT. The majority of DVT episodes in the WHI were spontaneous, not related to surgical procedures.
Dr. Jenkins: I have a patient who had been on low-dose HT for 30 years and underwent lumbar spine surgery. She had a somewhat prolonged recovery, so her lack of mobility and her age clearly increased her risk of DVT. So she was taken off HT and became miserable from the resulting hot flashes and sleep disturbance. We thoroughly discussed the risks and benefits of restarting HT, and because she was taking warfarin, we felt comfortable restarting the HT.
Women with spontaneous DVT are a different case, however, and I have an issue with restarting oral or transdermal HT in those cases. However, if we discuss the data with these patients and document the significant risks of HT in their cases, some may want to accept the increased risk in order to improve their quality of life, and that may be reasonable if they are truly fully informed.
Dr. Thacker: What about a woman who has been on oral contraceptives for several years and has not had a DVT? Is the safe use of oral/ hormonal contraceptives something you take into account, Dr. Gass, in your decision whether to prescribe HT?
Dr. Gass: Yes, that can be reassuring. Twenty-seven percent of EPT participants and 49% of estrogen therapy (ET) participants in the WHI randomized trial had used hormones in the past, so it was as if they were already tested for an early risk of blood clots.7
What role for SERMs (estrogen agonists/antagonists)?
Dr. Thacker: I would like to discuss the use of estrogen agonists/estogen antagonists, formerly known as selective estrogen receptor modulators (SERMs), such as raloxifene. Raloxifene now has an indication for breast cancer prevention as well as for reduction of vertebral fractures. I don’t know if there is adequate recognition among practitioners that SERMs appear to be associated with the same risk of DVT that estrogen is, and a greater risk of fatal stroke.
Dr. Jenkins: I find the lack of hip fracture data with raloxifene concerning, because hip fracture carries the highest 5-year mortality of any type of fracture. Raloxifene therefore is not a first-line agent for bone loss in my practice. But we also have to consider the patient’s risk of breast cancer and whether or not she has been on tamoxifen and now needs an agent to protect her against fracture. The question is whether we should consider starting these patients on raloxifene versus a bisphosphonate.
Dr. Thacker: Dr. Gass, do you think that raloxifene is safe for the endometrium? For years, we did not know the full effects of tamoxifen on the endometrium; it took experience with millions of patients to find out that tamoxifen increases the risk of endometrial cancer.
Dr. Gass: I do think that raloxifene is safer. I use it in my practice primarily for women younger than age 65 who are not yet at high risk for hip fracture but are still concerned about breast cancer. Although this concern diminishes as women age without having developed breast cancer, for younger women, who may see their friends getting breast cancer, it is a major concern. So if a patient is a good candidate for a bone loss agent and also has concern about breast cancer, raloxifene can be a good option, especially since we do not know what the implications are of taking bisphosphonates for 30 years. Questions about that are starting to be raised, so I think it is good to consider a sequential approach for some of these patients. A sequential approach might involve use of HT in a symptomatic menopausal woman, followed by use of raloxifene after the woman no longer has menopausal symptoms but is concerned about spine fracture protection and breast cancer risk reduction, followed by bisphosphonate use as she gets older and is at increased risk for stroke/VTE and for hip fracture.
The challenge of educating younger doctors about HT
Dr. Thacker: I think we need to find ways to translate the data on HT to younger generations of physicians, because the closer one is to graduating from medical school, the less likely he or she is to offer HT to an otherwise healthy, severely symptomatic woman younger than age 60.
Dr. McKenzie: Absolutely, and I think the real challenge is to reach younger physicians who go into private practice, who generally have the fewest opportunities to stay on top of the latest evidence. We must offer evidence-based education programs on this topic to physicians in the community to ensure that they are equipped to understand and explain the real risks and benefits of HT in order to individualize treatment decisions.
As a physician at a tertiary care center, I am surprised at the number of women referred to me who should have already been on HT for menopausal symptoms, but their physicians were unduly influenced by the initial WHI publication. They need to thoroughly evaluate their patients, assess their risks, assess any new medical problems, try to educate them, and then tailor therapy to improve their patients’ quality of life.
Correcting misperceptions: WHI was not a treatment trial
Dr. Thacker: I believe that many practitioners and especially students do not realize that the WHI was a trial designed to assess prevention of chronic diseases. It was not a menopausal treatment trial, and often its data are being misapplied to women who are different from the ones enrolled in the WHI, in that they are younger and more symptomatic.
Dr. Gass: It is correct that the WHI was not a treatment trial, but that was how HT was being used by some physicians and patients prior to the WHI. Physicians in this country were giving some 65-year-old women HT for osteoporosis and dementia. These practices needed to be supported with data, and that was the impetus behind the trial. Along the same lines, it is important how we present the risks to patients. If HT is being used as a therapy for a woman suffering from menopausal symptoms, she might be willing to accept more risk than if it is being used like a vitamin pill, to promote general health, in which case the risks should be virtually nil because the woman is healthy and without complaints.
Dr. Thacker: Yes, and that is why I think the earlier discussion of comparable risks of breast cancer, stroke, and VTE with aspirin, SERMs, fibric acid derivatives, and statins helps to put the risks of HT in perspective. It appears that physicians and patients tolerate very similar risks with commonly used nonhormonal medicines in women but do not tolerate any risks with HT, even in symptomatic women. In my opinion, this is a medical travesty. It is important to recognize that there are few absolutes in medicine that apply to all patients. The only universal recommendations I make to all patients are to wear seatbelts and not to smoke.
Dr. Hodis: What I find notable is that with HT we see a reduction in mortality regardless of the risks that we have described. As the observational data show, if we start HT and continue it, there is a reduction in mortality of 30% or even greater, and the clinical trial data tend to support this benefit. So why do we shy away from HT? Because we are worried about a small increase in breast cancer diagnoses or a small increase in DVT? That is an issue I am grappling with.
Dr. Thacker: Similarly, how do you reconcile the observational data with aspirin? In the Nurses’ Health Study, the aspirin users had lower mortality, but in all of the randomized controlled trials in midlife women, we do not see a reduction in cardiovascular risk with aspirin, let alone a reduction in mortality. So, the people who self-select for treatment are obviously different from those enrolled in randomized trials. The randomized controlled trial may be our gold standard, but it is not necessarily the only evidence to consider.
Dr. Hodis: But there is a concordance between observational studies and randomized trials with respect to overall mortality and HT. The data from a meta-analysis of 30 randomized trials8 are consistent with the data from observational studies, even though they do identify risks. I wonder how many more women would select HT if we told them about the 30% reduction in mortality despite the possibility of breast cancer diagnosis and DVT risks.
Dr. Gass: Women will select according to their own agenda.
Dr. Hodis: Yes, in the end, it is all individualized.
Dr. Gass: Indeed, because women have specific concerns, such as breast cancer, fracture risk, or Alzheimer disease, and they base their personal decisions on these specific concerns. I educate them about the risks and benefits, and they pretty much decide for themselves. They know their priorities.
Age and the risk-benefit assessment with HT
Dr. Thacker: Does the panel have any comments on the recent position statement from the American Association of Clinical Endocrinologists concluding that the benefits of HT exceed the risks in symptomatic women younger than age 60?
Dr. Hodis: My only comment is to ask why it took them so long to come to that conclusion.
Dr. Thacker: We could say the same for the North American Menopause Society (NAMS). It was not until its 2007 position statement on the use of ET and EPT in perimenopausal and postmenopausal women that NAMS moved beyond the issue of a time limit for HT—the “lowest dose for the shortest amount of time” mantra—and recommended the type of reevaluation used with any other treatment.
It seems as if practitioners are less willing to tolerate the risks of HT in older women than to tolerate the risks of hormonal contraceptives in younger women. Perhaps that is because hormonal contraceptives prevent pregnancy and the risks associated with it, yet this same value is not afforded to the symptoms and other effects suffered by postmenopausal women. I think we did afford HT similar value as hormonal contraceptives in the 1980s and 1990s, when we were trying to promote the potential health benefits of HT before we had bisphosphonates and statins and before we realized the risks of VTE with HT, risks that were identified much sooner with hormonal contraceptives. Since then the medical community has overcorrected by too often dismissing HT, overemphasizing the risks and ignoring very important quality-of-life issues, including sex and sleep disturbances, in the process.
Dr. Jenkins: Also, too many people associate menopause only with hot flashes, without taking into account the increased risk of serious diseases that may occur at this time, such as osteoporosis and heart disease.
Dr. Thacker: That may be because menopause is a normal event. It can be a great time of life for many women; in fact, it is associated with lower rates of depression, unless there is a prolonged symptomatic perimenopause. Menopause is certainly not a disease, and NAMS has been very good at recognizing and promoting it as a normal phase of life. But to neglect treating a woman going through menopausal symptoms just because menopause is a normal life event would be akin to withholding assistance for women during childbirth, which is another natural event.
We fail from a medical perspective if we do not take care of symptomatic women, because they will then turn to people who are not physicians and who offer unregulated therapies. These people may deliver the right message—that menopausal women deserve to feel well and look good—but the way they tell women to treat menopausal symptoms is not science-based.
At one time, we were overtreating women and not individualizing therapy, but to me it is even more worrisome to withhold therapies unless women are so highly symptomatic that they consider ending their life. We are continuing to discover the risks and benefits of HT and how to further tailor it. We have many newer, lower-dose HT options, and we are expecting the first nonhormonal therapy for menopausal vasomotor symptoms, desvenlafaxine. We are fortunate to have bone agents and local vaginal therapies for women without vasomotor symptoms. With both hormonal and nonhormonal options, we must keep the risks and benefits of any therapy in perspective.
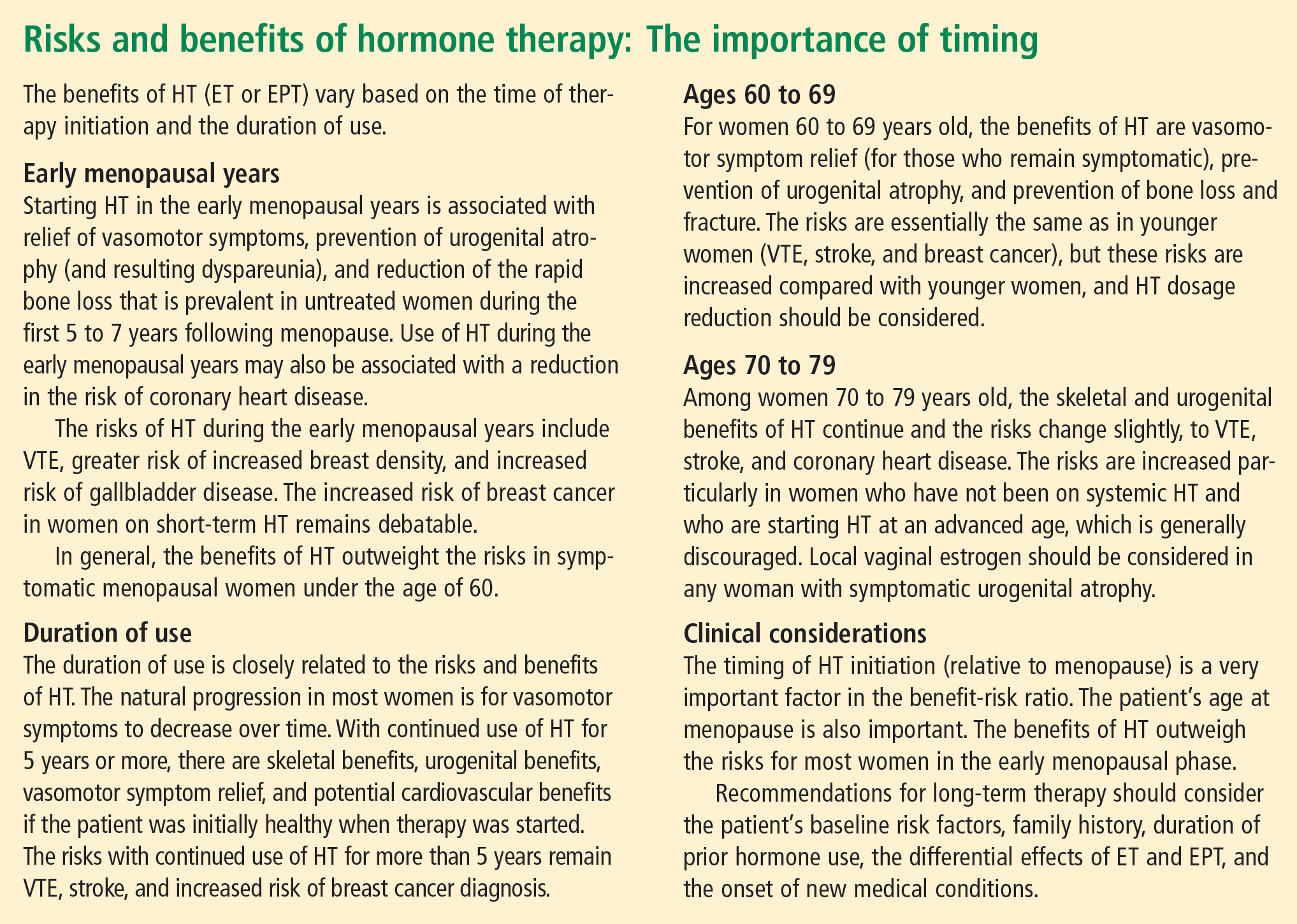
CONCLUSIONS
Dr. Thacker: This has been a great discussion, and although we do not all agree on every point, I would like to conclude by summarizing some key points on which I think we do all agree (see sidebar above). Menopause is a normal life event, but for some women who are symptomatic, and for a smaller percentage who will be symptomatic for the rest of their lives, HT is the gold standard, although it does not treat all symptoms and has some well-defined risks. We do have other options on the horizon for relief of vasomotor symptoms, for bone health, and for urogenital atrophy.
Following the data on the effects of HT on cardiovascular health will be particularly interesting. Although there is not support for using HT specifically for cardiovascular prevention, there are provocative data that in the symptomatic woman who has self-selected it, HT has cardiovascular benefit and reduces the risk of diabetes.
A woman on HT who has not had “early harm” does not need to arbitrarily discontinue therapy based on any time limit, as long as she is being periodically reevaluated and is offered individualized options.
- Utian WH, Shoupe D, Backmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril 2001; 75:1065–1079.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Davis S, Studd J, Bouchard C, Kroll R, Moufarege A, Von Schoultz B. The effect of a testosterone transdermal system on hypoactive sexual desire disorder in postmenopausal women not receiving systemic estrogen therapy, the APHRODITE study. Abstract presented at: 86th Annual Meeting of the Endocrine Society; June 16–19, 2004; New Orleans, LA.
- Speroff L, Gass M, Constantine G, Olivier S; Study 315 Investigators. Efficacy and tolerability of desvenlafaxine succinate treatment for menopausal vasomotor symptoms: a randomized controlled trial. Obstet Gynecol 2008; 111:77–87.
- Høibraaten E, Qvigstad E, Arnesen H, Larsen S, Wickstrøm E, Sandset PM. Increased risk of recurrent venous thromboembolism during hormone replacement therapy: results of the randomized, double-blind, placebo-controlled Estrogen in Venous Thromboembolism Trial (EVTET). Thromb Haemost 2000; 84:961–967.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Stefanick ML, Cochrane BB, Hsia J, Barad DH, Liu JH, Johnson SR. The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiol 2003; 13:S78–S86.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.
Dr. Holly Thacker: In light of the updates that Drs. Hodis and Gass have presented on hormone therapy (HT) for menopausal women and that Drs. Jenkins and Sikon have presented on nonhormonal options for menopausal management, let’s start our roundtable by considering a couple of case studies that will give us the chance to apply the latest data in a practical way.
CASE 1: A SYMPTOMATIC 67-YEAR-OLD IN WHOM HORMONE THERAPY WAS ABRUPTLY STOPPED
Dr. Margaret McKenzie: A 67-year-old menopausal woman presents for the evaluation of hot flashes, vaginal dryness causing dyspareunia, and decreased libido. She was previously on estrogen-progestogen therapy (EPT), consisting of daily conjugated equine estrogens and medroxyprogesterone acetate, for 15 years starting at the time of natural menopause. Her gynecologist discontinued this HT abruptly at the time of the initial release of data from the Women’s Health Initiative trial, and the patient is now seeking another opinion about resuming HT. When she presents, she has been off HT for less than 6 months. Would you restart HT in this patient?
Dr. Andrea Sikon: The abrupt discontinuation certainly contributes to her symptoms. The short duration of time off HT is important, and would lead me to restart HT after an updated review of risk factors. She had been on it for 15 years and has done fine, so she appears to be an ideal candidate to restart.
Dr. McKenzie: What specific questions would you ask when doing your risk assessment? How would you evaluate this patient to determine whether she is a good candidate to continue HT?
Dr. Thacker: I would obtain a family history. Using a population-based risk assessment such as the Gail model, I would calculate her absolute risk of breast cancer based on her duration of EPT use. I might offer her a lower-dose regimen. A conjugated equine estrogen dosage of 0.3 mg/day may be as effective in a 67-year-old woman as 0.625 mg/day is in a younger woman in terms of relieving vasomotor symptoms, depending on individual metabolism. We do have evidence from the HOPE trial that 0.3 mg/day is effective for relief of vasomotor symptoms.1 In addition, data from the Nurses’ Health Study show no increased risk of stroke with 0.3 mg/day, as opposed to the increased risk with 0.625 mg/day, and there are other data showing that the risk of stroke is possibly related to dosage.2
At the same time, we do not yet have long-term data to show that the lower dose is necessarily safer and we do not have data on bone fracture risk with the lower dose, so I would want to know this patient’s bone mineral density (BMD). I would also want to know about her cardiovascular risk profile, including her lipid profile, and I would want more details about her sexual function.
Dr. McKenzie: I will supply a few more case details. This patient’s body mass index (BMI) was 24 kg/m2. She exercised regularly. Her BMD was normal for her age. She was taking a statin to treat hyperlipidemia. She was a nonsmoker, and her family history was unremarkable. Does any of this information change the way that you would counsel her?
Dr. Howard Hodis: Knowing her BMI and that she was on a statin, I would have even less of a problem reinitiating HT.
Case continued
Dr. McKenzie: Well, EPT was reinitiated in this patient at a lower dose (0.45/1.5 mg), and she was satisfied. At her most recent visit, several years later, the possibility of reducing her dose of HT was offered; however, the patient is happy with her quality of life and accepts whatever risk that continued HT may bring. She inquired about transdermal testosterone to restore her sex drive, and it was agreed that if it receives US marketing approval for women with decreased libido, a 24-week trial would be attempted.
Dr. Hodis: If you look at the data, this patient not only may enhance her quality of life by continuing HT but might extend it as well.
Dr. Thacker: Many patients inquire about using testosterone only, without estrogen, for treating dyspareunia and low libido. Clinicians must understand that testosterone is aromatized to estrogen. If a patient is on a high dose of oral estrogen, I would consider switching to transdermal estrogen before trying testosterone, whose use in women remains off-label in the United States. But the patient in our case has been doing well for several years on low-dose estrogen and she still has her ovaries.
Dr. Margery Gass: Some colleagues and I completed a study, which was presented at a recent Endocrine Society meeting,3 in which transdermal testosterone was just as effective without estrogen in increasing libido. But this remains moot for general clinical practice unless the transdermal testosterone patch is approved in this country (as it is already approved for use in women in Europe).
Dr. Hodis: Would any of you be worried about this patient’s fracture risk after having HT stopped following 15 years of use? Data show that the rate of bone loss after abrupt cessation of HT is just as great as when a woman is going through menopause.
Dr. Gass: Yes, and that is exactly the point. The woman should be assessed under these circumstances just as she would be at menopause, using the same risk factors.
Dr. Thacker: I think that underscores that there is risk in stopping treatment, just as there is in taking treatment or not taking treatment, and all of these risks should be considered. Many times, once a patient is off HT, some clinicians forget to check the patient’s BMD or to do a complete genital examination.
Dr. Sikon: Many providers who do not specialize in women’s health may forget that when HT is stopped, it is as if a newly menopausal state is being created. Providers need to think about ensuing changes in bone and genitourinary status as well as quality-of-life concerns.
Dr. McKenzie: In today’s clinical environment, there is awareness of the importance of long-term bone health because patients are living longer. The use of BMD measurements in practice is clearly expanding.
Dr. Thacker: It is worth noting that all of the drugs used to treat osteoporosis have been studied primarily in women who already have osteoporosis. The therapy with the most data to support a reduction in the risk of all types of fracture is HT. These data are very impressive, and although fracture prevention would not be the sole reason for using HT, it can make the overall risk-benefit assessment easier, particularly if it can be determined whether or not an individual patient is at high risk of venous thromboembolism (VTE).
CASE 2: A SYMPTOMATIC 47-YEAR-OLD WITH A HISTORY OF BREAST CANCER
Dr. McKenzie: A 47-year-old postmenopausal woman with a 7-year history of breast cancer presents for the management of hot flashes, irritability, and reduced sleep. In addition, recent onset of vaginal dryness is causing dyspareunia that is not alleviated by lubricants. Her breast cancer was estrogen receptor (ER)/progesterone receptor (PR)–positive, and she received tamoxifen therapy for 5 years (now completed) following the initial diagnosis and management. How would you approach the management of this patient?
Dr. Marjorie Jenkins: I would first try to determine the severity of her hot flashes and how much her symptoms are affecting her quality of life. She may say that she is still having hot flashes, but how frequent are they? Do they cause nighttime awakening and subsequent fatigue?
Dr. McKenzie: The reason this patient presented was to ask for some form of relief because her symptoms were affecting her quality of life. Her dyspareunia was getting worse. She was trying various lubricants without success. At the same time, she expressed fear because her tumor was ER/PR-positive. Most cancer survivors have recurrence in the back of their mind even though they are in remission.
Dr. Jenkins: Was she asking specifically about HT or about help to relieve her symptoms?
Dr. McKenzie: She was asking for help for her symptoms.
Dr. Jenkins: I would consider low-dose vaginal estrogen to address her dyspareunia. I would also consider a serotonin-norepinephrine reuptake inhibitor, such as venlafaxine, to treat her hot flashes and irritability, along with lifestyle modifications, although the latter do not have evidence-based support. If these measures failed to offer relief, I would reconsider the risks and benefits of low-dose HT. I would call her oncologist for input if I planned to start vaginal estrogen, low-dose topical testosterone, or any type of hormonal treatment. I would make sure that the patient knew that her oncologist was working as part of the team responsible for her management.
Dr. Thacker: I concur. When I see hormonally sensitive breast cancer patients with vaginal symptoms, particularly when they are taking tamoxifen, I often talk to them about local estrogen before vaginal atrophy becomes severe. Once the atrophy becomes severe, local estrogen, even in low doses, may be absorbed systemically (increasing the risk of endometrial hyperplasia) until the the vagina becomes re-estrogenized and stratified with healthy squamous epithelium. Once this restratification takes place, there are generally no systemic hormonal effects with low-dose local vaginal estrogen, but it is best to avoid severe atrophy in the first place. I like to start local estrogen early if I know that the oncologist wants to use an aromatase inhibitor in a breast cancer survivor. I prescribe the low-dose vaginal form frequently in my practice, and order transvaginal ultrasonography liberally if there is concern about the endometrium.
Additionally, I would offer this patient venlafaxine or, more specifically, desvenlafaxine, as the literature has shown that the latter agent is associated with an improvement in sleep.4 (Currently, desvenlafaxine has been approved by the US Food and Drug Administration [FDA] solely to treat major depression; however, it has been studied in nondepressed women with hot flashes and is expected to be the first nonhormonal agent to receive FDA approval specifically to treat hot flashes.)
Dr. Gass: This patient still has her uterus in place. Data show that estrogens have a first-pass uterine effect, and this gives me pause because estrogen levels could well be higher in the uterus than in the bloodstream. Because of those data, as well as the absence of long-term safety data, the use of estrogen in this patient would cause me concern.
With breast cancer patients in particular, I try everything else to treat vaginal dryness before adding estrogen. I believe that if a patient is having dyspareunia despite the use of adequate lubricants, something else is the problem. In many cases these women have not had intercourse for months because they have been undergoing treatment for breast cancer, and they can have hallmark pain syndromes or constriction of the vagina that may require treatments besides just estrogen. If all else failed, I would prescribe vaginal estrogen on a temporary basis. Women who stay sexually active after menopause can do perfectly fine without treatment, but those who have periods of abstinence and then try to resume sexual activity typically run into problems.
Dr. Hodis: Would you have concern about breast cancer recurrence with estrogen reinitiation, based on the literature?
Dr. Gass: I have seen recurrences out to 20 years after the initial cancer. If the cancer does recur, the woman will always have a nagging doubt that it could have been avoided if she had not used estrogen.
Dr. Thacker: We have many breast cancer survivors in our practice. It is an easier decision to give estrogen to women who have had bilateral mastectomy with reconstruction for a stage I breast cancer and have already had a hysterectomy or bilateral salpingooophorectomy. But we otherwise try to avoid it unless the patient has first tried everything else and is miserable from her vaginal symptoms.
Dr. Gass: When a patient is diagnosed with breast cancer, I gently encourage her to continue sexual activity through the course of treatment, explaining that she may be far better off later. It may avoid a lot of problems if we can proactively get that message across.
Dr. Jenkins: That is a great point, and there is evidence that increased sexual activity decreases vaginal atrophy and assists in maintaining vaginal elasticity and the ability of urogenital congestion with arousal. Although lubricants and moisturizers do work well, they may require repeated application, and inelasticity is still a problem for some patients. It is somewhat of a “use it or lose it” proposition.
Dr. Thacker: Recurrent urinary tract infections (UTIs) are a problem as well. Patients see urologists, undergo multiple endoscopies, and are treated with antibiotics, sometimes chronically, yet often they are not even offered local vaginal estrogen, which reduces recurrent UTIs. Local estrogen should be considered in any woman with vaginal atrophy and recurrent UTIs.
Case continued
Dr. McKenzie: To return to our case, this patient’s vagina was, in fact, severely constricted because she had not been sexually active for a while. Her BMI was initially greater than 25 kg/m2, but she lost weight and became more symptomatic as she did so. She then stopped having sex because it was painful.
When she presented initially, she had a package of black cohosh with her and was willing to try it for her symptoms but was apprehensive after reading the disclaimers in the package. A 47-year-old who has already been diagnosed with ER-positive breast cancer is generally anxious about using any therapies that may be associated with an increased risk of breast cancer.
After examination of her vagina, her oncologist was consulted and suggested that her serum estradiol levels be measured; they were less than 20 pg/mL. We then agreed to a trial of estradiol vaginal tablets, vaginal dilators, and an increase in her sexual activity. She has been on vaginal estradiol for 2 years and is functioning very well. Her hot flashes improved spontaneously as her body adapted to her new weight.
BEYOND THE CASES: OTHER CHALLENGES IN MENOPAUSAL MANAGEMENT
HT discontinuation, dose reduction in real-world practice
Dr. Thacker: The first case we covered touched on both discontinuation of HT and HT dosage reduction. These are issues that come up often in clinical practice; what lessons does the panel have to share on these issues?
Dr. Gass: I find that there is a small subset of women who are highly symptomatic and are probably always going to be miserable whenever they try to go off HT. For some, if they are highly symptomatic at menopause, they tend to stay that way. They may try to go off, but a year later, they come back and say, “I am just too miserable.”
Dr. McKenzie: In my practice, I have noticed patients who end up staying on higher doses of HT for a long period because they do not tolerate weaning. If you take them down to 0.625 mg of estrogen, their hot flashes resume, so they seem to require 0.9 mg.
Dr. Thacker: I have a very small subset of those women too. I wonder if their metabolism is different; maybe 0.9 mg of conjugated equine estrogens is to them what 0.3 mg is to other women. As women get older, perhaps metabolic changes are one reason that many can reduce their hormone dosage. It is very challenging. I tell my students that it is much easier trying to determine how much thyroid hormone replacement to give a patient than how much estrogen.
When does transdermal estrogen make sense?
Dr. Sikon: I would be interested in the rest of the panel’s views on management of a woman in her early postmenopausal years who is symptomatic and has been on oral HT and is also a smoker. Would you switch her to transdermal estrogen or continue her oral HT and continue aggressive smoking cessation counseling?
Dr. Thacker: Many practitioners think that a smoker cannot take any type of HT because they equate it to oral/hormonal contraceptives, which increase the risk of heart attack in smokers over age 35, but hormonal contraceptives are different in that they involve a much higher dose of hormone. In my practice, the cases when I will offer transdermal estrogen are generally when a patient has gastrointestinal upset, known gallbladder disease, elevated triglycerides, or a prior deep vein thrombosis (DVT), even though I will tell the patient that the HT-associated risks are still possible with transdermal therapies. Many women are inappropriately and inaccurately told that compounded transdermal therapies are “risk free.”
Dr. McKenzie: Transdermal estrogen is also an option for patients who are poor pill takers or are already taking too many pills. Many of my patients are on transdermal estrogen for the convenience that it offers. It is unfortunate that transdermal progesterone cream does not protect the endometrium in all patients; for women with a uterus, an oral progestogen needs to be prescribed. However, two transdermal patches containing progestogens have been shown to be efficacious in protecting the endometrium.
How should a history of DVT affect decision-making?
Dr. McKenzie: What do you do when a patient has a history of postoperative DVT and is already on HT? How many of the panel would discontinue the HT as opposed to continuing it?
Dr. Hodis: If it were a history of spontaneous DVT, I would feel uncomfortable continuing HT. A few years ago, a clinical trial was stopped early because women with a prior spontaneous DVT who were randomized to HT had a substantial increase in DVT incidence relative to those randomized to placebo.5 In the case of provoked or postoperative DVT, it may be a tougher call.
Dr. Thacker: I think that DVT is the greatest risk with HT, even though the media are more focused on breast cancer risk. The risk of breast cancer with estrogen alone is debatable, at least with oral conjugated estrogen, which was associated with a decreased risk in women who had undergone hysterectomy in the Women’s Health Initiative (WHI).6
When I see a woman with a history of DVT in my practice, I check her homocysteine levels and check for factor V Leiden and prothrombin gene mutation. If I find an inherited hypercoagulability disorder, I tell the patient that her risk of DVT with any type of hormone product is not just multiplicative, it is logarithmic. If the patient already requires lifelong anticoagulation, then I am a bit more comfortable with prescribing HT and I usually will try the transdermal route first; however, I always consider nonhormonal treatment alternatives first.
Dr. Gass: The WHI was supposed to have excluded women with a history of DVT, but a few such women were enrolled, and it was demonstrated that they were at higher risk of DVT recurrence if randomized to HT. The majority of DVT episodes in the WHI were spontaneous, not related to surgical procedures.
Dr. Jenkins: I have a patient who had been on low-dose HT for 30 years and underwent lumbar spine surgery. She had a somewhat prolonged recovery, so her lack of mobility and her age clearly increased her risk of DVT. So she was taken off HT and became miserable from the resulting hot flashes and sleep disturbance. We thoroughly discussed the risks and benefits of restarting HT, and because she was taking warfarin, we felt comfortable restarting the HT.
Women with spontaneous DVT are a different case, however, and I have an issue with restarting oral or transdermal HT in those cases. However, if we discuss the data with these patients and document the significant risks of HT in their cases, some may want to accept the increased risk in order to improve their quality of life, and that may be reasonable if they are truly fully informed.
Dr. Thacker: What about a woman who has been on oral contraceptives for several years and has not had a DVT? Is the safe use of oral/ hormonal contraceptives something you take into account, Dr. Gass, in your decision whether to prescribe HT?
Dr. Gass: Yes, that can be reassuring. Twenty-seven percent of EPT participants and 49% of estrogen therapy (ET) participants in the WHI randomized trial had used hormones in the past, so it was as if they were already tested for an early risk of blood clots.7
What role for SERMs (estrogen agonists/antagonists)?
Dr. Thacker: I would like to discuss the use of estrogen agonists/estogen antagonists, formerly known as selective estrogen receptor modulators (SERMs), such as raloxifene. Raloxifene now has an indication for breast cancer prevention as well as for reduction of vertebral fractures. I don’t know if there is adequate recognition among practitioners that SERMs appear to be associated with the same risk of DVT that estrogen is, and a greater risk of fatal stroke.
Dr. Jenkins: I find the lack of hip fracture data with raloxifene concerning, because hip fracture carries the highest 5-year mortality of any type of fracture. Raloxifene therefore is not a first-line agent for bone loss in my practice. But we also have to consider the patient’s risk of breast cancer and whether or not she has been on tamoxifen and now needs an agent to protect her against fracture. The question is whether we should consider starting these patients on raloxifene versus a bisphosphonate.
Dr. Thacker: Dr. Gass, do you think that raloxifene is safe for the endometrium? For years, we did not know the full effects of tamoxifen on the endometrium; it took experience with millions of patients to find out that tamoxifen increases the risk of endometrial cancer.
Dr. Gass: I do think that raloxifene is safer. I use it in my practice primarily for women younger than age 65 who are not yet at high risk for hip fracture but are still concerned about breast cancer. Although this concern diminishes as women age without having developed breast cancer, for younger women, who may see their friends getting breast cancer, it is a major concern. So if a patient is a good candidate for a bone loss agent and also has concern about breast cancer, raloxifene can be a good option, especially since we do not know what the implications are of taking bisphosphonates for 30 years. Questions about that are starting to be raised, so I think it is good to consider a sequential approach for some of these patients. A sequential approach might involve use of HT in a symptomatic menopausal woman, followed by use of raloxifene after the woman no longer has menopausal symptoms but is concerned about spine fracture protection and breast cancer risk reduction, followed by bisphosphonate use as she gets older and is at increased risk for stroke/VTE and for hip fracture.
The challenge of educating younger doctors about HT
Dr. Thacker: I think we need to find ways to translate the data on HT to younger generations of physicians, because the closer one is to graduating from medical school, the less likely he or she is to offer HT to an otherwise healthy, severely symptomatic woman younger than age 60.
Dr. McKenzie: Absolutely, and I think the real challenge is to reach younger physicians who go into private practice, who generally have the fewest opportunities to stay on top of the latest evidence. We must offer evidence-based education programs on this topic to physicians in the community to ensure that they are equipped to understand and explain the real risks and benefits of HT in order to individualize treatment decisions.
As a physician at a tertiary care center, I am surprised at the number of women referred to me who should have already been on HT for menopausal symptoms, but their physicians were unduly influenced by the initial WHI publication. They need to thoroughly evaluate their patients, assess their risks, assess any new medical problems, try to educate them, and then tailor therapy to improve their patients’ quality of life.
Correcting misperceptions: WHI was not a treatment trial
Dr. Thacker: I believe that many practitioners and especially students do not realize that the WHI was a trial designed to assess prevention of chronic diseases. It was not a menopausal treatment trial, and often its data are being misapplied to women who are different from the ones enrolled in the WHI, in that they are younger and more symptomatic.
Dr. Gass: It is correct that the WHI was not a treatment trial, but that was how HT was being used by some physicians and patients prior to the WHI. Physicians in this country were giving some 65-year-old women HT for osteoporosis and dementia. These practices needed to be supported with data, and that was the impetus behind the trial. Along the same lines, it is important how we present the risks to patients. If HT is being used as a therapy for a woman suffering from menopausal symptoms, she might be willing to accept more risk than if it is being used like a vitamin pill, to promote general health, in which case the risks should be virtually nil because the woman is healthy and without complaints.
Dr. Thacker: Yes, and that is why I think the earlier discussion of comparable risks of breast cancer, stroke, and VTE with aspirin, SERMs, fibric acid derivatives, and statins helps to put the risks of HT in perspective. It appears that physicians and patients tolerate very similar risks with commonly used nonhormonal medicines in women but do not tolerate any risks with HT, even in symptomatic women. In my opinion, this is a medical travesty. It is important to recognize that there are few absolutes in medicine that apply to all patients. The only universal recommendations I make to all patients are to wear seatbelts and not to smoke.
Dr. Hodis: What I find notable is that with HT we see a reduction in mortality regardless of the risks that we have described. As the observational data show, if we start HT and continue it, there is a reduction in mortality of 30% or even greater, and the clinical trial data tend to support this benefit. So why do we shy away from HT? Because we are worried about a small increase in breast cancer diagnoses or a small increase in DVT? That is an issue I am grappling with.
Dr. Thacker: Similarly, how do you reconcile the observational data with aspirin? In the Nurses’ Health Study, the aspirin users had lower mortality, but in all of the randomized controlled trials in midlife women, we do not see a reduction in cardiovascular risk with aspirin, let alone a reduction in mortality. So, the people who self-select for treatment are obviously different from those enrolled in randomized trials. The randomized controlled trial may be our gold standard, but it is not necessarily the only evidence to consider.
Dr. Hodis: But there is a concordance between observational studies and randomized trials with respect to overall mortality and HT. The data from a meta-analysis of 30 randomized trials8 are consistent with the data from observational studies, even though they do identify risks. I wonder how many more women would select HT if we told them about the 30% reduction in mortality despite the possibility of breast cancer diagnosis and DVT risks.
Dr. Gass: Women will select according to their own agenda.
Dr. Hodis: Yes, in the end, it is all individualized.
Dr. Gass: Indeed, because women have specific concerns, such as breast cancer, fracture risk, or Alzheimer disease, and they base their personal decisions on these specific concerns. I educate them about the risks and benefits, and they pretty much decide for themselves. They know their priorities.
Age and the risk-benefit assessment with HT
Dr. Thacker: Does the panel have any comments on the recent position statement from the American Association of Clinical Endocrinologists concluding that the benefits of HT exceed the risks in symptomatic women younger than age 60?
Dr. Hodis: My only comment is to ask why it took them so long to come to that conclusion.
Dr. Thacker: We could say the same for the North American Menopause Society (NAMS). It was not until its 2007 position statement on the use of ET and EPT in perimenopausal and postmenopausal women that NAMS moved beyond the issue of a time limit for HT—the “lowest dose for the shortest amount of time” mantra—and recommended the type of reevaluation used with any other treatment.
It seems as if practitioners are less willing to tolerate the risks of HT in older women than to tolerate the risks of hormonal contraceptives in younger women. Perhaps that is because hormonal contraceptives prevent pregnancy and the risks associated with it, yet this same value is not afforded to the symptoms and other effects suffered by postmenopausal women. I think we did afford HT similar value as hormonal contraceptives in the 1980s and 1990s, when we were trying to promote the potential health benefits of HT before we had bisphosphonates and statins and before we realized the risks of VTE with HT, risks that were identified much sooner with hormonal contraceptives. Since then the medical community has overcorrected by too often dismissing HT, overemphasizing the risks and ignoring very important quality-of-life issues, including sex and sleep disturbances, in the process.
Dr. Jenkins: Also, too many people associate menopause only with hot flashes, without taking into account the increased risk of serious diseases that may occur at this time, such as osteoporosis and heart disease.
Dr. Thacker: That may be because menopause is a normal event. It can be a great time of life for many women; in fact, it is associated with lower rates of depression, unless there is a prolonged symptomatic perimenopause. Menopause is certainly not a disease, and NAMS has been very good at recognizing and promoting it as a normal phase of life. But to neglect treating a woman going through menopausal symptoms just because menopause is a normal life event would be akin to withholding assistance for women during childbirth, which is another natural event.
We fail from a medical perspective if we do not take care of symptomatic women, because they will then turn to people who are not physicians and who offer unregulated therapies. These people may deliver the right message—that menopausal women deserve to feel well and look good—but the way they tell women to treat menopausal symptoms is not science-based.
At one time, we were overtreating women and not individualizing therapy, but to me it is even more worrisome to withhold therapies unless women are so highly symptomatic that they consider ending their life. We are continuing to discover the risks and benefits of HT and how to further tailor it. We have many newer, lower-dose HT options, and we are expecting the first nonhormonal therapy for menopausal vasomotor symptoms, desvenlafaxine. We are fortunate to have bone agents and local vaginal therapies for women without vasomotor symptoms. With both hormonal and nonhormonal options, we must keep the risks and benefits of any therapy in perspective.
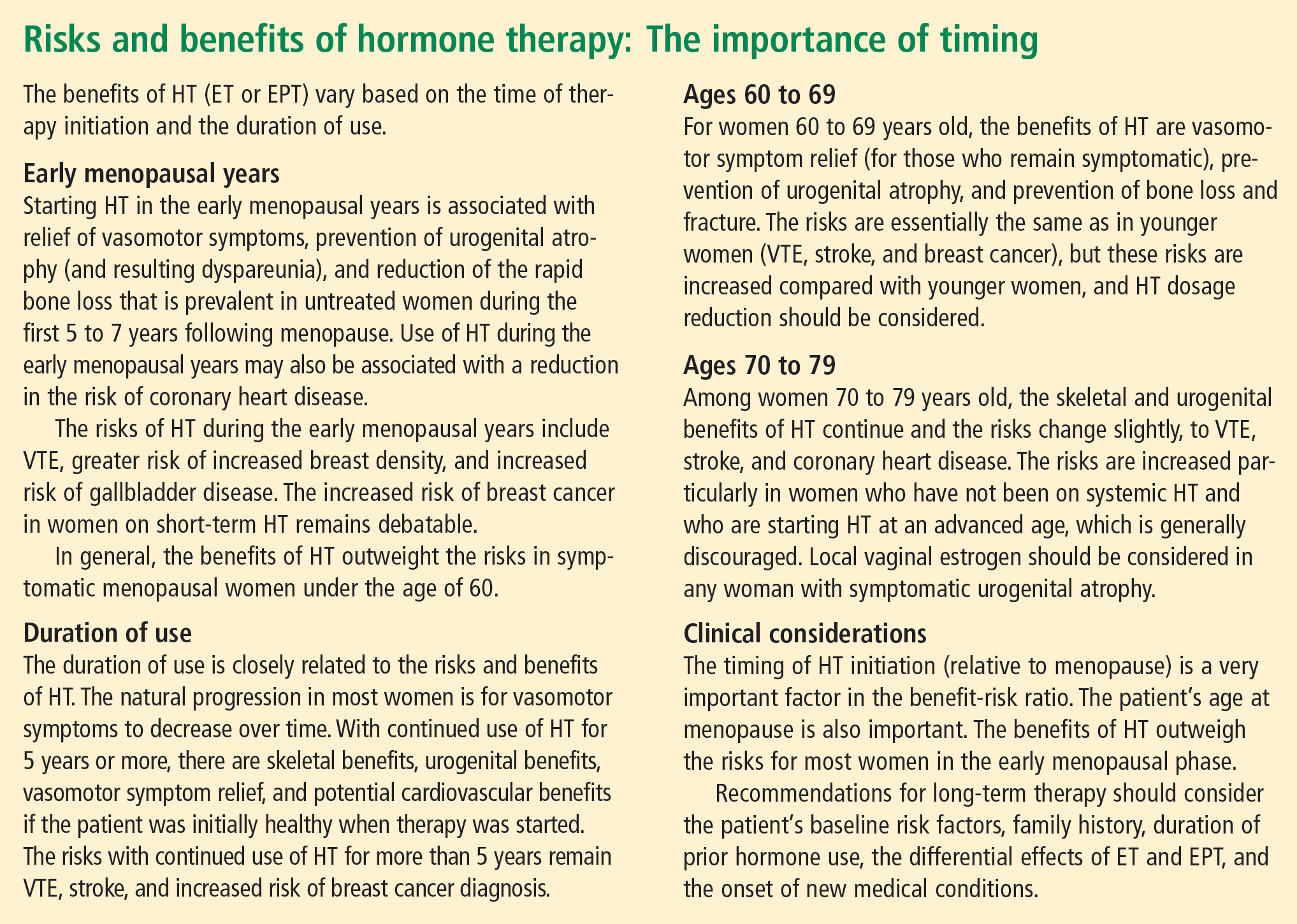
CONCLUSIONS
Dr. Thacker: This has been a great discussion, and although we do not all agree on every point, I would like to conclude by summarizing some key points on which I think we do all agree (see sidebar above). Menopause is a normal life event, but for some women who are symptomatic, and for a smaller percentage who will be symptomatic for the rest of their lives, HT is the gold standard, although it does not treat all symptoms and has some well-defined risks. We do have other options on the horizon for relief of vasomotor symptoms, for bone health, and for urogenital atrophy.
Following the data on the effects of HT on cardiovascular health will be particularly interesting. Although there is not support for using HT specifically for cardiovascular prevention, there are provocative data that in the symptomatic woman who has self-selected it, HT has cardiovascular benefit and reduces the risk of diabetes.
A woman on HT who has not had “early harm” does not need to arbitrarily discontinue therapy based on any time limit, as long as she is being periodically reevaluated and is offered individualized options.
Dr. Holly Thacker: In light of the updates that Drs. Hodis and Gass have presented on hormone therapy (HT) for menopausal women and that Drs. Jenkins and Sikon have presented on nonhormonal options for menopausal management, let’s start our roundtable by considering a couple of case studies that will give us the chance to apply the latest data in a practical way.
CASE 1: A SYMPTOMATIC 67-YEAR-OLD IN WHOM HORMONE THERAPY WAS ABRUPTLY STOPPED
Dr. Margaret McKenzie: A 67-year-old menopausal woman presents for the evaluation of hot flashes, vaginal dryness causing dyspareunia, and decreased libido. She was previously on estrogen-progestogen therapy (EPT), consisting of daily conjugated equine estrogens and medroxyprogesterone acetate, for 15 years starting at the time of natural menopause. Her gynecologist discontinued this HT abruptly at the time of the initial release of data from the Women’s Health Initiative trial, and the patient is now seeking another opinion about resuming HT. When she presents, she has been off HT for less than 6 months. Would you restart HT in this patient?
Dr. Andrea Sikon: The abrupt discontinuation certainly contributes to her symptoms. The short duration of time off HT is important, and would lead me to restart HT after an updated review of risk factors. She had been on it for 15 years and has done fine, so she appears to be an ideal candidate to restart.
Dr. McKenzie: What specific questions would you ask when doing your risk assessment? How would you evaluate this patient to determine whether she is a good candidate to continue HT?
Dr. Thacker: I would obtain a family history. Using a population-based risk assessment such as the Gail model, I would calculate her absolute risk of breast cancer based on her duration of EPT use. I might offer her a lower-dose regimen. A conjugated equine estrogen dosage of 0.3 mg/day may be as effective in a 67-year-old woman as 0.625 mg/day is in a younger woman in terms of relieving vasomotor symptoms, depending on individual metabolism. We do have evidence from the HOPE trial that 0.3 mg/day is effective for relief of vasomotor symptoms.1 In addition, data from the Nurses’ Health Study show no increased risk of stroke with 0.3 mg/day, as opposed to the increased risk with 0.625 mg/day, and there are other data showing that the risk of stroke is possibly related to dosage.2
At the same time, we do not yet have long-term data to show that the lower dose is necessarily safer and we do not have data on bone fracture risk with the lower dose, so I would want to know this patient’s bone mineral density (BMD). I would also want to know about her cardiovascular risk profile, including her lipid profile, and I would want more details about her sexual function.
Dr. McKenzie: I will supply a few more case details. This patient’s body mass index (BMI) was 24 kg/m2. She exercised regularly. Her BMD was normal for her age. She was taking a statin to treat hyperlipidemia. She was a nonsmoker, and her family history was unremarkable. Does any of this information change the way that you would counsel her?
Dr. Howard Hodis: Knowing her BMI and that she was on a statin, I would have even less of a problem reinitiating HT.
Case continued
Dr. McKenzie: Well, EPT was reinitiated in this patient at a lower dose (0.45/1.5 mg), and she was satisfied. At her most recent visit, several years later, the possibility of reducing her dose of HT was offered; however, the patient is happy with her quality of life and accepts whatever risk that continued HT may bring. She inquired about transdermal testosterone to restore her sex drive, and it was agreed that if it receives US marketing approval for women with decreased libido, a 24-week trial would be attempted.
Dr. Hodis: If you look at the data, this patient not only may enhance her quality of life by continuing HT but might extend it as well.
Dr. Thacker: Many patients inquire about using testosterone only, without estrogen, for treating dyspareunia and low libido. Clinicians must understand that testosterone is aromatized to estrogen. If a patient is on a high dose of oral estrogen, I would consider switching to transdermal estrogen before trying testosterone, whose use in women remains off-label in the United States. But the patient in our case has been doing well for several years on low-dose estrogen and she still has her ovaries.
Dr. Margery Gass: Some colleagues and I completed a study, which was presented at a recent Endocrine Society meeting,3 in which transdermal testosterone was just as effective without estrogen in increasing libido. But this remains moot for general clinical practice unless the transdermal testosterone patch is approved in this country (as it is already approved for use in women in Europe).
Dr. Hodis: Would any of you be worried about this patient’s fracture risk after having HT stopped following 15 years of use? Data show that the rate of bone loss after abrupt cessation of HT is just as great as when a woman is going through menopause.
Dr. Gass: Yes, and that is exactly the point. The woman should be assessed under these circumstances just as she would be at menopause, using the same risk factors.
Dr. Thacker: I think that underscores that there is risk in stopping treatment, just as there is in taking treatment or not taking treatment, and all of these risks should be considered. Many times, once a patient is off HT, some clinicians forget to check the patient’s BMD or to do a complete genital examination.
Dr. Sikon: Many providers who do not specialize in women’s health may forget that when HT is stopped, it is as if a newly menopausal state is being created. Providers need to think about ensuing changes in bone and genitourinary status as well as quality-of-life concerns.
Dr. McKenzie: In today’s clinical environment, there is awareness of the importance of long-term bone health because patients are living longer. The use of BMD measurements in practice is clearly expanding.
Dr. Thacker: It is worth noting that all of the drugs used to treat osteoporosis have been studied primarily in women who already have osteoporosis. The therapy with the most data to support a reduction in the risk of all types of fracture is HT. These data are very impressive, and although fracture prevention would not be the sole reason for using HT, it can make the overall risk-benefit assessment easier, particularly if it can be determined whether or not an individual patient is at high risk of venous thromboembolism (VTE).
CASE 2: A SYMPTOMATIC 47-YEAR-OLD WITH A HISTORY OF BREAST CANCER
Dr. McKenzie: A 47-year-old postmenopausal woman with a 7-year history of breast cancer presents for the management of hot flashes, irritability, and reduced sleep. In addition, recent onset of vaginal dryness is causing dyspareunia that is not alleviated by lubricants. Her breast cancer was estrogen receptor (ER)/progesterone receptor (PR)–positive, and she received tamoxifen therapy for 5 years (now completed) following the initial diagnosis and management. How would you approach the management of this patient?
Dr. Marjorie Jenkins: I would first try to determine the severity of her hot flashes and how much her symptoms are affecting her quality of life. She may say that she is still having hot flashes, but how frequent are they? Do they cause nighttime awakening and subsequent fatigue?
Dr. McKenzie: The reason this patient presented was to ask for some form of relief because her symptoms were affecting her quality of life. Her dyspareunia was getting worse. She was trying various lubricants without success. At the same time, she expressed fear because her tumor was ER/PR-positive. Most cancer survivors have recurrence in the back of their mind even though they are in remission.
Dr. Jenkins: Was she asking specifically about HT or about help to relieve her symptoms?
Dr. McKenzie: She was asking for help for her symptoms.
Dr. Jenkins: I would consider low-dose vaginal estrogen to address her dyspareunia. I would also consider a serotonin-norepinephrine reuptake inhibitor, such as venlafaxine, to treat her hot flashes and irritability, along with lifestyle modifications, although the latter do not have evidence-based support. If these measures failed to offer relief, I would reconsider the risks and benefits of low-dose HT. I would call her oncologist for input if I planned to start vaginal estrogen, low-dose topical testosterone, or any type of hormonal treatment. I would make sure that the patient knew that her oncologist was working as part of the team responsible for her management.
Dr. Thacker: I concur. When I see hormonally sensitive breast cancer patients with vaginal symptoms, particularly when they are taking tamoxifen, I often talk to them about local estrogen before vaginal atrophy becomes severe. Once the atrophy becomes severe, local estrogen, even in low doses, may be absorbed systemically (increasing the risk of endometrial hyperplasia) until the the vagina becomes re-estrogenized and stratified with healthy squamous epithelium. Once this restratification takes place, there are generally no systemic hormonal effects with low-dose local vaginal estrogen, but it is best to avoid severe atrophy in the first place. I like to start local estrogen early if I know that the oncologist wants to use an aromatase inhibitor in a breast cancer survivor. I prescribe the low-dose vaginal form frequently in my practice, and order transvaginal ultrasonography liberally if there is concern about the endometrium.
Additionally, I would offer this patient venlafaxine or, more specifically, desvenlafaxine, as the literature has shown that the latter agent is associated with an improvement in sleep.4 (Currently, desvenlafaxine has been approved by the US Food and Drug Administration [FDA] solely to treat major depression; however, it has been studied in nondepressed women with hot flashes and is expected to be the first nonhormonal agent to receive FDA approval specifically to treat hot flashes.)
Dr. Gass: This patient still has her uterus in place. Data show that estrogens have a first-pass uterine effect, and this gives me pause because estrogen levels could well be higher in the uterus than in the bloodstream. Because of those data, as well as the absence of long-term safety data, the use of estrogen in this patient would cause me concern.
With breast cancer patients in particular, I try everything else to treat vaginal dryness before adding estrogen. I believe that if a patient is having dyspareunia despite the use of adequate lubricants, something else is the problem. In many cases these women have not had intercourse for months because they have been undergoing treatment for breast cancer, and they can have hallmark pain syndromes or constriction of the vagina that may require treatments besides just estrogen. If all else failed, I would prescribe vaginal estrogen on a temporary basis. Women who stay sexually active after menopause can do perfectly fine without treatment, but those who have periods of abstinence and then try to resume sexual activity typically run into problems.
Dr. Hodis: Would you have concern about breast cancer recurrence with estrogen reinitiation, based on the literature?
Dr. Gass: I have seen recurrences out to 20 years after the initial cancer. If the cancer does recur, the woman will always have a nagging doubt that it could have been avoided if she had not used estrogen.
Dr. Thacker: We have many breast cancer survivors in our practice. It is an easier decision to give estrogen to women who have had bilateral mastectomy with reconstruction for a stage I breast cancer and have already had a hysterectomy or bilateral salpingooophorectomy. But we otherwise try to avoid it unless the patient has first tried everything else and is miserable from her vaginal symptoms.
Dr. Gass: When a patient is diagnosed with breast cancer, I gently encourage her to continue sexual activity through the course of treatment, explaining that she may be far better off later. It may avoid a lot of problems if we can proactively get that message across.
Dr. Jenkins: That is a great point, and there is evidence that increased sexual activity decreases vaginal atrophy and assists in maintaining vaginal elasticity and the ability of urogenital congestion with arousal. Although lubricants and moisturizers do work well, they may require repeated application, and inelasticity is still a problem for some patients. It is somewhat of a “use it or lose it” proposition.
Dr. Thacker: Recurrent urinary tract infections (UTIs) are a problem as well. Patients see urologists, undergo multiple endoscopies, and are treated with antibiotics, sometimes chronically, yet often they are not even offered local vaginal estrogen, which reduces recurrent UTIs. Local estrogen should be considered in any woman with vaginal atrophy and recurrent UTIs.
Case continued
Dr. McKenzie: To return to our case, this patient’s vagina was, in fact, severely constricted because she had not been sexually active for a while. Her BMI was initially greater than 25 kg/m2, but she lost weight and became more symptomatic as she did so. She then stopped having sex because it was painful.
When she presented initially, she had a package of black cohosh with her and was willing to try it for her symptoms but was apprehensive after reading the disclaimers in the package. A 47-year-old who has already been diagnosed with ER-positive breast cancer is generally anxious about using any therapies that may be associated with an increased risk of breast cancer.
After examination of her vagina, her oncologist was consulted and suggested that her serum estradiol levels be measured; they were less than 20 pg/mL. We then agreed to a trial of estradiol vaginal tablets, vaginal dilators, and an increase in her sexual activity. She has been on vaginal estradiol for 2 years and is functioning very well. Her hot flashes improved spontaneously as her body adapted to her new weight.
BEYOND THE CASES: OTHER CHALLENGES IN MENOPAUSAL MANAGEMENT
HT discontinuation, dose reduction in real-world practice
Dr. Thacker: The first case we covered touched on both discontinuation of HT and HT dosage reduction. These are issues that come up often in clinical practice; what lessons does the panel have to share on these issues?
Dr. Gass: I find that there is a small subset of women who are highly symptomatic and are probably always going to be miserable whenever they try to go off HT. For some, if they are highly symptomatic at menopause, they tend to stay that way. They may try to go off, but a year later, they come back and say, “I am just too miserable.”
Dr. McKenzie: In my practice, I have noticed patients who end up staying on higher doses of HT for a long period because they do not tolerate weaning. If you take them down to 0.625 mg of estrogen, their hot flashes resume, so they seem to require 0.9 mg.
Dr. Thacker: I have a very small subset of those women too. I wonder if their metabolism is different; maybe 0.9 mg of conjugated equine estrogens is to them what 0.3 mg is to other women. As women get older, perhaps metabolic changes are one reason that many can reduce their hormone dosage. It is very challenging. I tell my students that it is much easier trying to determine how much thyroid hormone replacement to give a patient than how much estrogen.
When does transdermal estrogen make sense?
Dr. Sikon: I would be interested in the rest of the panel’s views on management of a woman in her early postmenopausal years who is symptomatic and has been on oral HT and is also a smoker. Would you switch her to transdermal estrogen or continue her oral HT and continue aggressive smoking cessation counseling?
Dr. Thacker: Many practitioners think that a smoker cannot take any type of HT because they equate it to oral/hormonal contraceptives, which increase the risk of heart attack in smokers over age 35, but hormonal contraceptives are different in that they involve a much higher dose of hormone. In my practice, the cases when I will offer transdermal estrogen are generally when a patient has gastrointestinal upset, known gallbladder disease, elevated triglycerides, or a prior deep vein thrombosis (DVT), even though I will tell the patient that the HT-associated risks are still possible with transdermal therapies. Many women are inappropriately and inaccurately told that compounded transdermal therapies are “risk free.”
Dr. McKenzie: Transdermal estrogen is also an option for patients who are poor pill takers or are already taking too many pills. Many of my patients are on transdermal estrogen for the convenience that it offers. It is unfortunate that transdermal progesterone cream does not protect the endometrium in all patients; for women with a uterus, an oral progestogen needs to be prescribed. However, two transdermal patches containing progestogens have been shown to be efficacious in protecting the endometrium.
How should a history of DVT affect decision-making?
Dr. McKenzie: What do you do when a patient has a history of postoperative DVT and is already on HT? How many of the panel would discontinue the HT as opposed to continuing it?
Dr. Hodis: If it were a history of spontaneous DVT, I would feel uncomfortable continuing HT. A few years ago, a clinical trial was stopped early because women with a prior spontaneous DVT who were randomized to HT had a substantial increase in DVT incidence relative to those randomized to placebo.5 In the case of provoked or postoperative DVT, it may be a tougher call.
Dr. Thacker: I think that DVT is the greatest risk with HT, even though the media are more focused on breast cancer risk. The risk of breast cancer with estrogen alone is debatable, at least with oral conjugated estrogen, which was associated with a decreased risk in women who had undergone hysterectomy in the Women’s Health Initiative (WHI).6
When I see a woman with a history of DVT in my practice, I check her homocysteine levels and check for factor V Leiden and prothrombin gene mutation. If I find an inherited hypercoagulability disorder, I tell the patient that her risk of DVT with any type of hormone product is not just multiplicative, it is logarithmic. If the patient already requires lifelong anticoagulation, then I am a bit more comfortable with prescribing HT and I usually will try the transdermal route first; however, I always consider nonhormonal treatment alternatives first.
Dr. Gass: The WHI was supposed to have excluded women with a history of DVT, but a few such women were enrolled, and it was demonstrated that they were at higher risk of DVT recurrence if randomized to HT. The majority of DVT episodes in the WHI were spontaneous, not related to surgical procedures.
Dr. Jenkins: I have a patient who had been on low-dose HT for 30 years and underwent lumbar spine surgery. She had a somewhat prolonged recovery, so her lack of mobility and her age clearly increased her risk of DVT. So she was taken off HT and became miserable from the resulting hot flashes and sleep disturbance. We thoroughly discussed the risks and benefits of restarting HT, and because she was taking warfarin, we felt comfortable restarting the HT.
Women with spontaneous DVT are a different case, however, and I have an issue with restarting oral or transdermal HT in those cases. However, if we discuss the data with these patients and document the significant risks of HT in their cases, some may want to accept the increased risk in order to improve their quality of life, and that may be reasonable if they are truly fully informed.
Dr. Thacker: What about a woman who has been on oral contraceptives for several years and has not had a DVT? Is the safe use of oral/ hormonal contraceptives something you take into account, Dr. Gass, in your decision whether to prescribe HT?
Dr. Gass: Yes, that can be reassuring. Twenty-seven percent of EPT participants and 49% of estrogen therapy (ET) participants in the WHI randomized trial had used hormones in the past, so it was as if they were already tested for an early risk of blood clots.7
What role for SERMs (estrogen agonists/antagonists)?
Dr. Thacker: I would like to discuss the use of estrogen agonists/estogen antagonists, formerly known as selective estrogen receptor modulators (SERMs), such as raloxifene. Raloxifene now has an indication for breast cancer prevention as well as for reduction of vertebral fractures. I don’t know if there is adequate recognition among practitioners that SERMs appear to be associated with the same risk of DVT that estrogen is, and a greater risk of fatal stroke.
Dr. Jenkins: I find the lack of hip fracture data with raloxifene concerning, because hip fracture carries the highest 5-year mortality of any type of fracture. Raloxifene therefore is not a first-line agent for bone loss in my practice. But we also have to consider the patient’s risk of breast cancer and whether or not she has been on tamoxifen and now needs an agent to protect her against fracture. The question is whether we should consider starting these patients on raloxifene versus a bisphosphonate.
Dr. Thacker: Dr. Gass, do you think that raloxifene is safe for the endometrium? For years, we did not know the full effects of tamoxifen on the endometrium; it took experience with millions of patients to find out that tamoxifen increases the risk of endometrial cancer.
Dr. Gass: I do think that raloxifene is safer. I use it in my practice primarily for women younger than age 65 who are not yet at high risk for hip fracture but are still concerned about breast cancer. Although this concern diminishes as women age without having developed breast cancer, for younger women, who may see their friends getting breast cancer, it is a major concern. So if a patient is a good candidate for a bone loss agent and also has concern about breast cancer, raloxifene can be a good option, especially since we do not know what the implications are of taking bisphosphonates for 30 years. Questions about that are starting to be raised, so I think it is good to consider a sequential approach for some of these patients. A sequential approach might involve use of HT in a symptomatic menopausal woman, followed by use of raloxifene after the woman no longer has menopausal symptoms but is concerned about spine fracture protection and breast cancer risk reduction, followed by bisphosphonate use as she gets older and is at increased risk for stroke/VTE and for hip fracture.
The challenge of educating younger doctors about HT
Dr. Thacker: I think we need to find ways to translate the data on HT to younger generations of physicians, because the closer one is to graduating from medical school, the less likely he or she is to offer HT to an otherwise healthy, severely symptomatic woman younger than age 60.
Dr. McKenzie: Absolutely, and I think the real challenge is to reach younger physicians who go into private practice, who generally have the fewest opportunities to stay on top of the latest evidence. We must offer evidence-based education programs on this topic to physicians in the community to ensure that they are equipped to understand and explain the real risks and benefits of HT in order to individualize treatment decisions.
As a physician at a tertiary care center, I am surprised at the number of women referred to me who should have already been on HT for menopausal symptoms, but their physicians were unduly influenced by the initial WHI publication. They need to thoroughly evaluate their patients, assess their risks, assess any new medical problems, try to educate them, and then tailor therapy to improve their patients’ quality of life.
Correcting misperceptions: WHI was not a treatment trial
Dr. Thacker: I believe that many practitioners and especially students do not realize that the WHI was a trial designed to assess prevention of chronic diseases. It was not a menopausal treatment trial, and often its data are being misapplied to women who are different from the ones enrolled in the WHI, in that they are younger and more symptomatic.
Dr. Gass: It is correct that the WHI was not a treatment trial, but that was how HT was being used by some physicians and patients prior to the WHI. Physicians in this country were giving some 65-year-old women HT for osteoporosis and dementia. These practices needed to be supported with data, and that was the impetus behind the trial. Along the same lines, it is important how we present the risks to patients. If HT is being used as a therapy for a woman suffering from menopausal symptoms, she might be willing to accept more risk than if it is being used like a vitamin pill, to promote general health, in which case the risks should be virtually nil because the woman is healthy and without complaints.
Dr. Thacker: Yes, and that is why I think the earlier discussion of comparable risks of breast cancer, stroke, and VTE with aspirin, SERMs, fibric acid derivatives, and statins helps to put the risks of HT in perspective. It appears that physicians and patients tolerate very similar risks with commonly used nonhormonal medicines in women but do not tolerate any risks with HT, even in symptomatic women. In my opinion, this is a medical travesty. It is important to recognize that there are few absolutes in medicine that apply to all patients. The only universal recommendations I make to all patients are to wear seatbelts and not to smoke.
Dr. Hodis: What I find notable is that with HT we see a reduction in mortality regardless of the risks that we have described. As the observational data show, if we start HT and continue it, there is a reduction in mortality of 30% or even greater, and the clinical trial data tend to support this benefit. So why do we shy away from HT? Because we are worried about a small increase in breast cancer diagnoses or a small increase in DVT? That is an issue I am grappling with.
Dr. Thacker: Similarly, how do you reconcile the observational data with aspirin? In the Nurses’ Health Study, the aspirin users had lower mortality, but in all of the randomized controlled trials in midlife women, we do not see a reduction in cardiovascular risk with aspirin, let alone a reduction in mortality. So, the people who self-select for treatment are obviously different from those enrolled in randomized trials. The randomized controlled trial may be our gold standard, but it is not necessarily the only evidence to consider.
Dr. Hodis: But there is a concordance between observational studies and randomized trials with respect to overall mortality and HT. The data from a meta-analysis of 30 randomized trials8 are consistent with the data from observational studies, even though they do identify risks. I wonder how many more women would select HT if we told them about the 30% reduction in mortality despite the possibility of breast cancer diagnosis and DVT risks.
Dr. Gass: Women will select according to their own agenda.
Dr. Hodis: Yes, in the end, it is all individualized.
Dr. Gass: Indeed, because women have specific concerns, such as breast cancer, fracture risk, or Alzheimer disease, and they base their personal decisions on these specific concerns. I educate them about the risks and benefits, and they pretty much decide for themselves. They know their priorities.
Age and the risk-benefit assessment with HT
Dr. Thacker: Does the panel have any comments on the recent position statement from the American Association of Clinical Endocrinologists concluding that the benefits of HT exceed the risks in symptomatic women younger than age 60?
Dr. Hodis: My only comment is to ask why it took them so long to come to that conclusion.
Dr. Thacker: We could say the same for the North American Menopause Society (NAMS). It was not until its 2007 position statement on the use of ET and EPT in perimenopausal and postmenopausal women that NAMS moved beyond the issue of a time limit for HT—the “lowest dose for the shortest amount of time” mantra—and recommended the type of reevaluation used with any other treatment.
It seems as if practitioners are less willing to tolerate the risks of HT in older women than to tolerate the risks of hormonal contraceptives in younger women. Perhaps that is because hormonal contraceptives prevent pregnancy and the risks associated with it, yet this same value is not afforded to the symptoms and other effects suffered by postmenopausal women. I think we did afford HT similar value as hormonal contraceptives in the 1980s and 1990s, when we were trying to promote the potential health benefits of HT before we had bisphosphonates and statins and before we realized the risks of VTE with HT, risks that were identified much sooner with hormonal contraceptives. Since then the medical community has overcorrected by too often dismissing HT, overemphasizing the risks and ignoring very important quality-of-life issues, including sex and sleep disturbances, in the process.
Dr. Jenkins: Also, too many people associate menopause only with hot flashes, without taking into account the increased risk of serious diseases that may occur at this time, such as osteoporosis and heart disease.
Dr. Thacker: That may be because menopause is a normal event. It can be a great time of life for many women; in fact, it is associated with lower rates of depression, unless there is a prolonged symptomatic perimenopause. Menopause is certainly not a disease, and NAMS has been very good at recognizing and promoting it as a normal phase of life. But to neglect treating a woman going through menopausal symptoms just because menopause is a normal life event would be akin to withholding assistance for women during childbirth, which is another natural event.
We fail from a medical perspective if we do not take care of symptomatic women, because they will then turn to people who are not physicians and who offer unregulated therapies. These people may deliver the right message—that menopausal women deserve to feel well and look good—but the way they tell women to treat menopausal symptoms is not science-based.
At one time, we were overtreating women and not individualizing therapy, but to me it is even more worrisome to withhold therapies unless women are so highly symptomatic that they consider ending their life. We are continuing to discover the risks and benefits of HT and how to further tailor it. We have many newer, lower-dose HT options, and we are expecting the first nonhormonal therapy for menopausal vasomotor symptoms, desvenlafaxine. We are fortunate to have bone agents and local vaginal therapies for women without vasomotor symptoms. With both hormonal and nonhormonal options, we must keep the risks and benefits of any therapy in perspective.
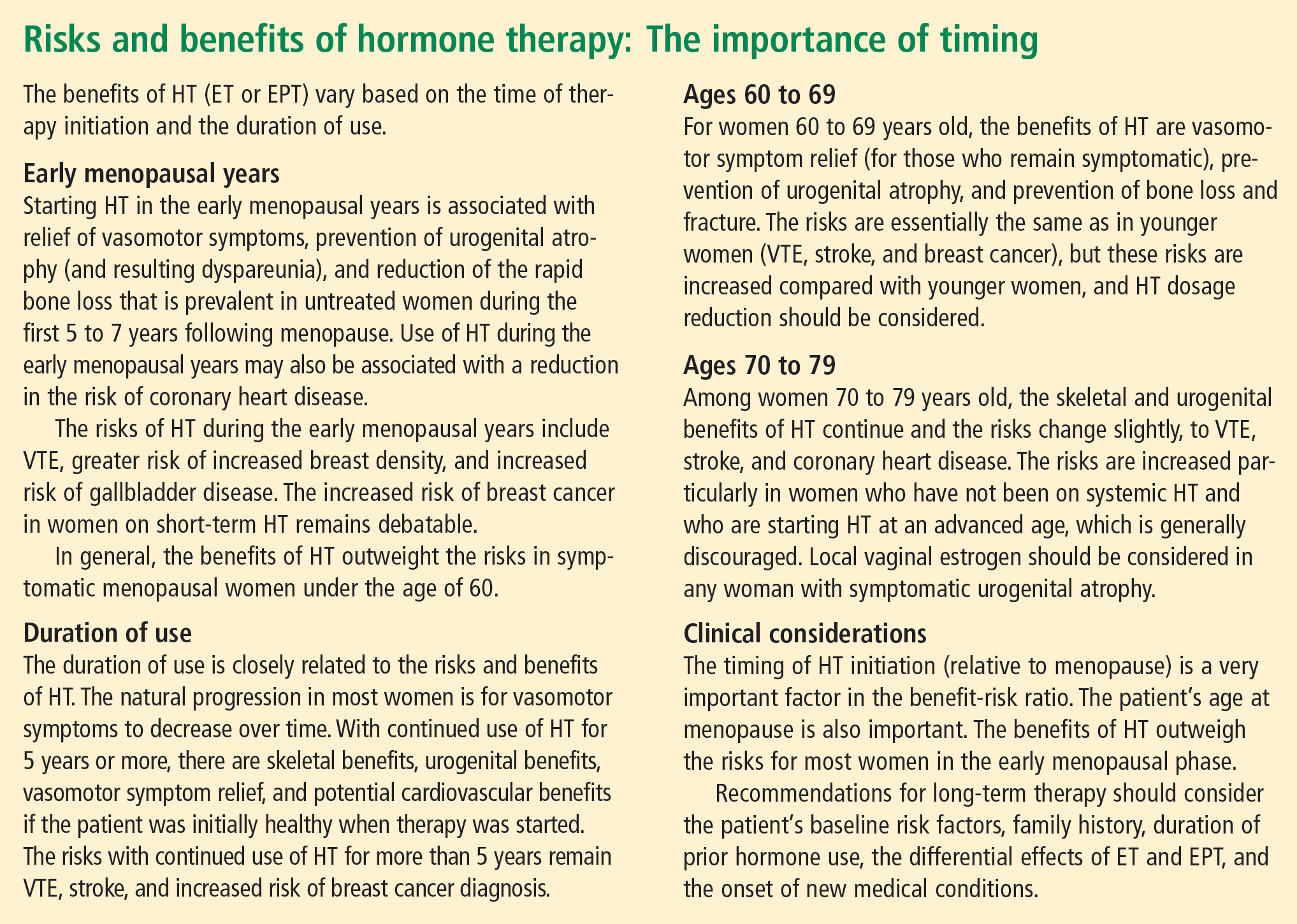
CONCLUSIONS
Dr. Thacker: This has been a great discussion, and although we do not all agree on every point, I would like to conclude by summarizing some key points on which I think we do all agree (see sidebar above). Menopause is a normal life event, but for some women who are symptomatic, and for a smaller percentage who will be symptomatic for the rest of their lives, HT is the gold standard, although it does not treat all symptoms and has some well-defined risks. We do have other options on the horizon for relief of vasomotor symptoms, for bone health, and for urogenital atrophy.
Following the data on the effects of HT on cardiovascular health will be particularly interesting. Although there is not support for using HT specifically for cardiovascular prevention, there are provocative data that in the symptomatic woman who has self-selected it, HT has cardiovascular benefit and reduces the risk of diabetes.
A woman on HT who has not had “early harm” does not need to arbitrarily discontinue therapy based on any time limit, as long as she is being periodically reevaluated and is offered individualized options.
- Utian WH, Shoupe D, Backmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril 2001; 75:1065–1079.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Davis S, Studd J, Bouchard C, Kroll R, Moufarege A, Von Schoultz B. The effect of a testosterone transdermal system on hypoactive sexual desire disorder in postmenopausal women not receiving systemic estrogen therapy, the APHRODITE study. Abstract presented at: 86th Annual Meeting of the Endocrine Society; June 16–19, 2004; New Orleans, LA.
- Speroff L, Gass M, Constantine G, Olivier S; Study 315 Investigators. Efficacy and tolerability of desvenlafaxine succinate treatment for menopausal vasomotor symptoms: a randomized controlled trial. Obstet Gynecol 2008; 111:77–87.
- Høibraaten E, Qvigstad E, Arnesen H, Larsen S, Wickstrøm E, Sandset PM. Increased risk of recurrent venous thromboembolism during hormone replacement therapy: results of the randomized, double-blind, placebo-controlled Estrogen in Venous Thromboembolism Trial (EVTET). Thromb Haemost 2000; 84:961–967.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Stefanick ML, Cochrane BB, Hsia J, Barad DH, Liu JH, Johnson SR. The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiol 2003; 13:S78–S86.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.
- Utian WH, Shoupe D, Backmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril 2001; 75:1065–1079.
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933–941.
- Davis S, Studd J, Bouchard C, Kroll R, Moufarege A, Von Schoultz B. The effect of a testosterone transdermal system on hypoactive sexual desire disorder in postmenopausal women not receiving systemic estrogen therapy, the APHRODITE study. Abstract presented at: 86th Annual Meeting of the Endocrine Society; June 16–19, 2004; New Orleans, LA.
- Speroff L, Gass M, Constantine G, Olivier S; Study 315 Investigators. Efficacy and tolerability of desvenlafaxine succinate treatment for menopausal vasomotor symptoms: a randomized controlled trial. Obstet Gynecol 2008; 111:77–87.
- Høibraaten E, Qvigstad E, Arnesen H, Larsen S, Wickstrøm E, Sandset PM. Increased risk of recurrent venous thromboembolism during hormone replacement therapy: results of the randomized, double-blind, placebo-controlled Estrogen in Venous Thromboembolism Trial (EVTET). Thromb Haemost 2000; 84:961–967.
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 2004; 291:1701–1712.
- Stefanick ML, Cochrane BB, Hsia J, Barad DH, Liu JH, Johnson SR. The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiol 2003; 13:S78–S86.
- Salpeter SR, Walsh JM, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women: a meta-analysis. J Gen Intern Med 2004; 19:791–804.