User login
Breaking Bad News
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
Broadly defined, bad news is any information that negatively alters a person's expectation about the present and the future.1 Importantly, news is defined as bad based on the patient's perspective about the information. Providers must remember that it will not always be obvious what patients will interpret as bad news. Although all would agree that the diagnosis of a new cancer would qualify as bad news, to some patients discovering hypertension would be deeply disturbing. Delivering bad news is difficult and stressful to all involved. Substantial data are now available describing patient preferences in these interactions, the impact on physicians who participate in these conversations, and specific recommendations for the delivery of bad news.
Hospitalists face additional challenges: lacking long‐standing relationships with patients and dealing with discontinuity in patient care and patient handoffs on a regular basis. Using an actual case as an example, this article examines the patient/family perspective and the provider perspective and reviews practical advice, actual phrases, useful mnemonics, and communication techniques to make these conversations more successful and less stressful. Opportunities to increase training in this area of palliative care are discussed. Adequate preparation, effective communication skills, empathy, and planned follow‐up are essential steps to assure that the goals for these difficult interactions are met.2, 3
CASE
The following scenario is based on an actual patient. The details and initials have been changed to maintain anonymity.
A 52‐year‐old Latino man, JR, was admitted with new‐onset ascites. He had a known diagnosis of end‐stage liver disease from prior alcohol use. Paracentesis revealed spontaneous bacterial peritonitis, and appropriate antibiotics were started. The fluid was sent for cytological analysis; the final diagnosis reported adenocarcinoma. A subsequent workup including PSA and CT of the abdomen/pelvis did not reveal the primary site of this malignancy.
JR had a supportive family and an established primary care physician. His spouse was no longer involved in his life, but his 2 daughters provided strong social support. His primary language was Spanish.
During the first 3 days of JR's hospital stay, he developed increasing abdominal pain, requiring escalating doses of narcotics. On the fourth day, the team received the cytology results, and the medical resident discussed the new diagnosis of cancer with JR. This conversation was not supervised by an attending, no interpreter was present, and no family members were in the room.
On entering the room, the resident said to the patient, I have bad news for you, JR.
The patient turned and said, Yes.
The resident continued, JR, you have cancer, and we don't know where it originated from.
The patient was silent and without expression. Unclear about how to proceed, the resident went on to say, The oncologist will be coming by later to discuss options with you. As there was no response, verbal or otherwise, the resident exited the room. The resident reported that the patient was unexpectedly calm after the news.
Provider Perspective
The responsibility of breaking bad news to patients weighs heavily on clinicians. As in this case, most providers' first experience with breaking bad news occurs with patients they have known for only a few hours or days. Even for the more experienced, this part of the job is rated as at least moderately stressful. Notably, most also feel that this stress lasts beyond the encounter, despite their perceived ability to manage their own stress during these situations.4 Additional training on clinicians' own coping skills may alleviate some of the emotional burden.
Provider's awareness and management of distress may enhance ability to provide comfort to patients or to specifically address their needs. Medical providers may try to suppress personal thoughts and feelings in these situations, but they bring emotional attachments to almost all encounters with patients.5 Emotional preparation by the provider is an important step prior to delivering bad news. Self‐reflection helps to identify personal emotions of sadness, anger, fear, or guilt and will help the provider not to disengage from the delivery of bad news.6 It is normal to have strong feelings, especially in difficult situations. Encouraging and validating these emotions personally will lead to a more therapeutic presence during a patient's time of need.7
Clinicians' perceptions of their interactions with patients when discussing bad news are probably more strongly influenced by the content of the discussion rather than the process itself. When asked to analyze their own videotaped consultations, doctors thought performance was worse when discussing palliative therapy than when discussing curative therapy.8
Traditionally, greatest emphasis has been placed on the acquisition and assessment of medical knowledge in medical training, and thus the focus on content is understandable. But more recently, efforts have been made at all levels of medical education to shift this focus toward encompassing many other competencies including professionalism and communication skills, which should translate into equal emphasis on the quality of these interactions.
As many hospitalists work closely with trainees, they are in the ideal position to serve as mentors and role models for communication. The case discussed in this article provides an example of a missed teaching opportunity. Ideally, the attending would have gone through the steps of preparation with the resident prior to the meeting, reviewed one or several of the suggested approaches discussed below, and observed the conversation and provided immediate feedback and a forum for processing afterward. It is especially helpful when first developing this skill to be familiar with helpful phrases to open the conversation, clarify patient preferences for communication, and convey empathy. It is also helpful to be aware of phrases that should be avoided (Table 1).
| Phrases to consider |
|---|
| To start a conversation |
| I am sorry to have to tell you this. |
| I know this is not good news. |
| I wish I had better news. |
| To elicit patient preferences |
| Would you like your family here when we talk about this? |
| Would you rather I speak with you about this or your daughter? |
| Some people want to be very involved in making decisions about their medical care, and some people want their doctor to just give them a recommendationhow do you feel about that? |
| To facilitate empathy |
| I can see how upsetting this is. |
| Is it okay if I hold your hand? |
| Phrases to avoid |
| There is nothing more we can do for you. |
| I know what this must be like. |
| I understand what you are going through. |
CASE
The following morning the attending physician, medical resident, and oncology fellow met with the patient and his daughter for a more extensive discussion. The goals of this discussion were to review the diagnosis and discuss the prognosis and future approaches to care. The entire discussion was conducted via a professional Spanish interpreter.
The attending physician began the conversation by asking, What do you remember about what the resident doctor told you, JR? pointing to the resident.
JR replied, I don't remember, and then went on to say, Please talk to my daughter, who was sitting across the room.
Family/Patient Perspective
As patient preferences for receiving bad news vary widely, it is these preferences that should determine the approach to the delivery, content, and context in which the news will be received. Some patients want information, and some do not; this needs to be clarified before beginning the discussion. The amount of detail should be negotiated in advance as well. As suggested by Back et al., soliciting patient preference prior to a discussion is important.9 These authors recommended using an approach called asktellask. This approach emphasizes the importance of asking questions to assess a patient's needs, telling the patient the information that meets those needs, and asking again to assess the patient's understanding.
Patients will rarely raise the issue of bad news with providers. In general, the provider must initiate the discussion.10 Surveys of patient preferences for delivery of bad news lend insight into this process and help guide providers during this challenging time. Patients report poor delivery is often characterized by bluntness, a lack of hope, and initiation of this serious conversation at an inappropriate time or place.11 Patients prefer providers to speak in clear, simple terms, being careful not to use technical jargon.12 Clinicians often use euphemisms to soften the blow of bad news, but this can lead to ambiguity. In addition to the clarity of the message, privacy, the attitude of the doctor, and the ability to answer questions are most important to patients and families receiving bad news.13 Although most would encourage touching in these difficult situations, it has been reported that up to a third of patients surveyed do not want physical contact.
Contrary to what providers may believe, diagnostic disclosure is not the most important part of a bad‐news discussion. Many patients believe it is most important to receive information on prognosis and treatment options. Often, patients want to discuss life expectancy. However, physicians are hesitant to address this issue. One study revealed that despite these requests, 22% of physicians would not provide any estimates at all, and when they did, 36% offered an overestimate.14 The authors hypothesized that how confident physicians are in this prognostic estimate and how much and what type of practice experience they have may influence their willingness to communicate a frank survival estimate.
The traditional dilemma of balancing hope with realism is reframed by Hagerty et al., who found that 98% of the patients they surveyed preferred a realistic and individualized approach.15 Use of euphemism and apparent unease of the provider actually decreases hope. Clayton et al. added that nurturing hope can also be facilitated by emphasizing what can be done, such as symptomatic management, emotional support, and practical support, particularly in terms of day‐to‐day living.16
In the case discussed in this article, preparation should have included asking the patient (1) whom he wanted present during the meeting, (2) how much information he and his family wanted to know, and (3) how involved he wanted his family to be. The informational needs of patients and their families will evolve over time as they process and accept the news. Thus, the asktellask approach remains a key concept to keep in mind as the dialogue continues beyond the initial encounter.
CASE
The attending physician attempted to continue the discussion by addressing both patient and daughter. He restated, JR, you have cancer in the fluid in your belly, and it is likely widespread throughout your body.
At that moment, the daughter became very tearful and emotional. There were several minutes of silence. The patient began to sob as well. The oncology fellow broke the silence by adding, Unfortunately, there is nothing that can be done when cancer is so widespread. The daughter broke into audible sobs; the patient looked away from the team and gazed through the window into the distance. The team fell silent and quietly left the room.
Importance of Empathy
The team failed in its inability to respond to emotion in this case. The emotional turmoil was apparent, but the team members made no attempt to acknowledge this emotion or to arrange additional emotional support. This could, at least in part, be a result of the providers' inability to process and manage their own emotions. A preparatory meeting beforehand and a debriefing session afterward for all the team members may have helped. Awareness of patients' coping strategies and various effective responses to these coping strategies may have better prepared the team to react and validate this patient's emotions. The role that psychology and emotion play cannot be overemphasized and clearly are important considerations. A useful mnemonic highlighting the components of the empathetic response is NURSE: naming, understanding, respect, supporting, and exploring.9 Using this technique, the provider starts by naming the emotion (anger, fear, disbelief); confirms a clear understanding of the patient's feelings; expresses respect verbally or nonverbally, letting the patient know the emotion is important; uses supporting statements that may express concern, reiterate understanding, or indicate a willingness to help; and closes by exploring additional concerns.
Certain phrases such as the one uttered by the fellowThere is nothing that can be doneshould be avoided.
Cultural Issues
Cultural diversity is increasingly common in contemporary medical practice in the United States. Some have suggested the Western value of autonomy is not embraced by all cultures. It has been suggested that non‐English‐speaking patients may receive less optimal end‐of‐life care than their English‐speaking counterparts.17 Beyond the language barrier, this observation may be a reflection of associated cultural barriers as well. Effective strategies for key issues of truth telling, language, family involvement, and decision making may help effective cross‐cultural communication and understanding and thus be effective patient‐centered care.18
A study of Korean patients and family members revealed a marked discordance between family and patients in the desire for disclosure.19 Almost all patients wanted to be informed that they had terminal illness, whereas a quarter of family members did not want physicians to relay this bad news to the patient. Interestingly, this study found patients would prefer to be told by the physician, whereas their family members would prefer to be the ones to deliver the news.
In some cultures it is believed that disclosure of bad news may cause patients to lose hope and hasten death. Physicians in these cultures may be more likely to honor family wishes. Language barriers may make a difficult situation even more complex. It is important to ascertain early on in what language patients and their families want to hold discussions. A medical interpreter should always be utilized for discussions with patients and their families. Dependence on a family member to interpret is not advised because the objective point of view may be lost in the interpretation. In addition, this places an enormous burden on the family member to be the bearer of bad news, which could have a lasting emotional impact. Although in the case discussed in this article, the patient's daughter was bilingual and could have translated, an interpreter should have been present for all discussions with this patient. Again, the importance of soliciting the patient's preference is critical.
Prior knowledge of the language requirement and of the patient's need for his daughter's involvement would also aid in the planning process. Because the patient's primary care physician (PCP) shared JR's Hispanic heritage, consultation with this PCP might have provided important insight, resulting in better preparation and planning.
How to Deliver Bad News
A number of guidelines are available to help physicians structure their conversations.2022 Baile and Buckman outline a 6‐step approach (Table 2). Rabow and Mcphee recommend the ABCDE mnemonic to help providers remember techniques for delivering bad news (Table 3). These recommendations are largely based on the literature to date. Both these approaches first emphasize preparations and planning. A private and quiet space, the presence of significant others if desired, arrangement to minimize interruptions, and provider emotional preparations are all prerequisites for the success of this type of encounter before the actual dialogue begins. As the encounter begins, it is key to assess a patient's needs if not already done before conveying information. Unidirectional transfer of information most likely will fail to satisfy the patient. The resident's initial conversation suffered in this key aspect.
| Setting up interview | Maintain privacy, involve significant others, sit down, make a connection, minimize interruptions. |
| Assessing patient perceptions | What have you been told about your illness? |
| Obtaining patient's invitation | How would you like me to give the information about your test results? |
| Giving knowledge and information to patient | Begin with warning statement, avoid jargon, avoid excessive bluntness. |
| Addressing patient's emotions | Listen, observe, acknowledge the emotion. |
| Providing strategy and summary | Give prognosis and treatment options and address symptoms. |
| Advance preparation |
|---|
| Ask what the patient already knows and understands. |
| Arrange for the presence of a support person and appropriate family. |
| Arrange a time and place that will be undisturbed (hand off beeper). |
| Prepare emotionally. |
| Decide which words and phrases to use (write down a script). |
| Practice delivering the news. |
| Build a therapeutic environment/relationship |
| Arrange a private, quiet place without interruptions. |
| Provide adequate seating for all. |
| Sit close enough to touch if appropriate. |
| Reassure about pain, suffering, abandonment. |
| Communicate well |
| Be direct (I am sorry, I have bad news). |
| Do not use euphemisms, jargon, or acronyms. |
| Do say cancer or death. |
| Allow for silence. |
| Use touch appropriately. |
| Ask patient to repeat his or her understanding of the news. |
| Arrange additional meetings. |
| Use repetition and written explanations of reminders. |
| Deal with patient and family reactions |
| Assess patient reaction |
| Physiologic responses: flight/fight, conservation/withdrawal; |
| Cognitive coping strategies: denial, blame, intellectualization, disbelief, acceptance; |
| Affective responses: anger/rage, fear/terror, anxiety, helplessness, hopelessness, shame, relief, guilt, sadness, anticipatory grief; |
| Listen actively, explore feelings, express empathy. |
| Encourage and validate emotions |
| Correct distortions. |
| Offer to tell others on behalf of the patient. |
| Evaluate the effects of the news. |
| Explore what the news means to the patient. |
| Address further needs, determine the patient's immediate and near‐term plans, assess suicidality. |
| Make appropriate referrals for more support, provide written materials, and arrange follow up. |
| Process your own feelings. |
Armed with knowledge of a patient's individual preferences, it is then possible to effectively convey information in a clear manner without jargon, using a direct but not blunt style. Both the SPIKES and ABCDE approaches similarly emphasize the asktellask approach. The attending physician was fairly effective in applying this communication approach in the subsequent encounter. However, the team left the room without providing a summary and follow‐up plan. Even though the patient and his daughter were quite emotional, acknowledging their reactions and appropriately ending the meeting with a summary and plans for the next steps would have been helpful in this continuing dialogue.
Hospitalist‐Specific Issues
Hospitalists may face special challenges when delivering bad news to patients. Without the benefit of preexisting longitudinal relationships with their patients, they lack prior understanding of a patient's values, family support system, and other cultural, spiritual, and social issues. Thus, preparation for these conversations is more difficult, and establishing rapport is more time‐consuming. There are no data available to describe the impact that not having a previous relationship with a patient has on these encounters. It is possible that the newness of the hospitalistpatient relationship may allow more candid, transparent communication than would be possible with established providers, who may themselves be struggling with the news and how it reflects on their care or the emotional impact of the impending loss.
Handoffs are a frequent part of the care the hospitalist provides, but communicating bad news is often a longitudinal process. One hospitalist may have the initial conversation regarding the patient's disease and prognosis, but the follow‐up often falls to a different hospitalist. Continuity of communication and awareness about what has been said previously are critical. It is important to explicitly document these conversations and their content in the medical record. In additional, summaries of pivotal conversations should be included in sign‐out. At discharge, whether patients are transitioning to postacute care or back to the outpatient arena, the hospitalist should carefully and vigilantly communicate critical conversations and predictions about patients' emotional needs.
Hospitalists do have some advantages when it comes to communication with patients. Unlike in outpatient practice, where clinicians are under pressure to keep up with a heavily loaded patient schedule, the hospitalist often has the flexibility and ability to allot time to each patient according to that patient's need. In addition, by definition, a hospitalist is in a hospital; this availability allows for more timely meetings, minimal delay in delivery of news, and accommodating the schedules of other people the patient may want included in any conversations.
CASE
A subsequent meeting occurred between the patient, his daughter, and the team, this time including a social worker and a hospice nurse.
The social worker began this discussion by stating, I understand you were quite upset last time and understandably so, and then inquired, What questions can we help you answer?
The patient and his daughter appropriately asked about alternatives to the usual aggressive treatment, and he made clear his desire to eventually spend his last days at home with family.
Through the translator, the hospice nurse succinctly explained the concept of palliative care with emphasis on symptomatic management as an alternative to aggressive curative therapy. JR and his daughter chose this palliative approach to care. This decision to focus on palliation was conveyed to JR's PCP. JR was eventually discharged to a short‐term postacute facility for rehabilitation and palliative care.
The health care team was finally able to acknowledge and validate JR's emotions with the help of the additional expertise of a social worker and a hospice nurse. This multidisciplinary approach allows team members to complement each other's strengths and weaknesses. Further, the patient had time to process his feelings and articulate his questions, values, and desires. Time often is required for this type of news to be more fully understood and eventually accepted. Breaking bad news is not a single event but a continuing dialogue and ultimately a relationship. Thus, proper delivery of bad news not only requires planning, effective communication, and empathy, but also deliberate follow‐up.
Training
What can be done to improve the effectiveness and satisfaction of these interactions for patients, providers, and families? Awareness of guidelines and effective strategies is a start but is unlikely to really change behavior or improve skills. Communication skills must be practiced, implemented, and observed with opportunity for feedback.23 Graduate and postgraduate training is probably the best time to develop these skills, and formal training in this area should be incorporated in a curriculum. Workshops on communicating bad news are offered frequently to oncologists and oncology fellows at various regional and national meetings. Ideally, these workshops would be offered at CME meetings specifically designed for hospitalists already in practice. Comprehensive palliative care training and materials, including specific modules and live workshops for delivering bad news, are available via the Education in Palliative and End‐of‐Life Care Project (EPEC) and the End‐of‐Life/Palliative Education Resource Center (EPERC) at the University of Wisconsin.
Hospitalists and trainees fortunate enough to practice in an institution with a palliative care service have the opportunity to learn from a multidisciplinary team, often including social workers, nursing staff, physicians and spiritual leaders. This interdisciplinary model is likely a more effective way to address the diverse physical, emotional, social, and spiritual needs of patients receiving difficult news and provides an ideal framework for this training.
CONCLUSIONS
Hospitalists are frequently called on to deliver bad news. A specific skills set is needed to be an effective communicator, especially in these stressful situations. Familiarity with an evidence‐based approach to this process and incorporation of the key steps into each of these encounters will likely improve patient and provider satisfaction as well as patient care during these critical times. Patient and family preferences for communication vary; so communication should be adjusted for each patient using the asktellask approach. Providers must remember to respond empathetically to emotion expressed by the patient and family and should keep the NURSE mnemonic in mind to guide the discussion. Providers should seek hands‐on training opportunities, which include supervision and feedback. Medical educators should incorporate training on the communication of bad news into curricula for students and trainees. Hospitalists may take a leadership role in teaching these skills at their institutions.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
- .Breaking bad news: why is it still so difficult?BMJ.1984;288:1597–1599.
- ,.Bad news: delivery, dialogue, and dilemmas.Arch Intern Med.1991;151:463–468.
- ,.Beyond breaking bad news: how to help patients who suffer.WJM.1999;171:260–263.
- ,,,.Breaking bad news to patients: physicians' perception of the process.Support Care Cancer.1999;7:113–120.
- ..Giving bad news to cancer patients: matching process and content.J Clin Oncol.2001;19:2575–2577.
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263.
- .Breaking bad news.Am Fam Physician.2001;64:1975–1978
- ,,.Truth may hurt but deceit hurts more: communication in palliative care.Palliat Med.2002;16:297–303.
- ,,, et al.Approaching difficult communication tasks in oncology.CA Cancer J Clin.2005;55:164–177.
- ,,,.Enhancing physician‐patient communication.Hematology Am Soc Hematol Educ Program.2002;464–483.
- ,,,,,.Communicating with dying patients within the spectrum of care from terminal diagnosis to death.Arch Intern Med.2001;161:868–874.
- ,,,.Communicating prognosis in early breast cancer: do women understand the language used?Med J Aust.1999;171:290–294.
- ,,,.Giving bad news: the family perspective.J Trauma.2000;48:865–870
- ,.Prognostic disclosure to patients with cancer near the end of life.Ann Intern Med.2001;134:1096–1105.
- ,,, et al.Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis.J Clin Oncol.2005;23:1278–1288.
- ,,, et al.Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers.Cancer.2005;103:1965–1975.
- ,.Comparison of palliative care needs of English and non‐English‐speaking patients.J Palliat Care.1999;15(1):26–30
- ,.Negotiating cross‐cultural issues at the end of life.JAMA.2001;286:2993–3001
- ,,,,,.The attitudes of cancer patients and their families towards disclosure of terminal illness.J Clin Oncol.2004;22:307–314.
- ,.Breaking bad news:consensus guidelines for medical practitioners.J Clin Oncol.1995;13:2449–2456
- ,,, et al.SPIKES—a six step protocol for delivering bad news: application to the patient with cancer.Oncologist.2000;5:302–311
- ,.Beyond breaking bad news:how to help patients who suffer.West J Med.1999;171:260–263
- ,,.Communication skills training for health professionals working with cancer patients, their families, and/or careers.Cochrane Database Syst Rev.2003;2:CD003751.
Physician Attitudes and Use of Computerized Order Entry
It is widely acknowledged that the U.S. health care system is plagued by error and inefficiency and that these factors contribute to as many as 44,000‐98,000 deaths each year in U.S. hospitals. In To Err Is Human: Building a Safer Health System, the Institute of Medicine1 outlined the critical role that information technology can play in improving patient safety and highlighted computerized physician order entry (CPOE) systems for their potential to reduce the frequency of medication errors and to improve the quality of medical care.
Computerized physician order entry systems are specialized software applications that allow physicians to place orders directly into a computer. This process has a number of potential advantages over traditional handwritten ordering, including the ability to structure the ordering process to ensure the completeness of individual orders, to provide clinical decision support through diagnosis‐based order sets, and to automatically check orders for potential drugallergy, drugdrug, and drugfood interactions.2 Finally, entering orders directly into a computer eliminates the problem of transcription‐related errors that stem from the difficulty of interpreting handwriting. In clinical trials, the introduction of CPOE has been shown to reduce the frequency of medication errors, to improve the use of preventive services, and to reduce costs.36 Recognition of the benefits of these systems has not been confined to the medical community. The Leapfrog Organization, a coalition of large businesses in the United States, has chosen CPOE as one of its 3 initial safety leaps and has established a threshold that 70% of medication orders should be entered directly by physicians.7
Although the benefits of CPOE systems are widely recognized, few hospitals have implemented these systems successfully.8, 9 Those that have, have often developed the applications internally, and many have relied on house staff to do most or all of the actual ordering.10 However, most hospitals do not have the expertise for internal development and instead rely on commercially available products. Moreover, most patients hospitalized in the United States are cared for by attending physicians working without the assistance of house staff.11 In light of the importance of successfully implementing CPOE systems in such settings, we assessed the adoption of CPOE by attending physicians at 2 community hospitals where its use was voluntary and examined the characteristics and attitudes associated with use of the system to place orders.
METHODS
Setting and Participants
Baystate Medical Center is a 600‐bed teaching hospital in Springfield, Massachusetts, where approximately 50% of patients are cared for with the assistance of house staff. Franklin Medical Center is a 125‐bed community hospital in rural Greenfield, Massachusetts, and is not a house staff training site. Medical staff membership at the 2 hospitals is largely voluntary. Both institutions share a vendor‐supplied computerized order entry system that was implemented in the early 1990s (E7000, Eclipsys Corporation, Boca Raton, FL). The system provides a structured format for the creation of medication, laboratory, and radiology orders and contains thousands of preconstructed medication order sentences and hundreds of order sets designed to standardize ordering for common diagnoses and procedures. Pharmacists are alerted of potential drugallergy and drugdrug interactions and use clinical judgment about whether to communicate this information to the physician. Although the house staff at Baystate Medical Center is mandated to place orders in the system, attending physicians have no such requirement at either institution. Access to the system is provided though the many fixed workstations located on nursing units, in operating rooms, and in the health sciences library. On a typical medical‐surgical patient care unit most computers are behind the nurses' station, though some are distributed along hallways and in physician charting rooms. No computers are in patient rooms. Although the number varies slightly across units, the average ratio of computers to patient beds is roughly 1 to 1.
Survey
In June 2003 we mailed a 20‐item survey to attending physicians who had been responsible for a minimum of 25 orders during the preceding month at either Baystate or Franklin Medical Center. Orders counted toward this minimum if they had been written, given verbally in person or by phone, or entered directly into the computer by the physician. The survey consisted of 20 questions focused on the topic of computerized order entry. In addition to collecting information about sex and specialty, we asked respondents to describe their use of CPOE during training, their use of computers at home, and, where applicable, their use of computers in their outpatient practices. The survey included questions about how often respondents used the order entry system when caring for hospitalized patients and which features of the system they used. To assess physician attitudes about the order entry process, we asked respondents to consider whether it was faster to place orders directly into the system than it was by handwriting them, whether orders placed in the system were carried out more rapidly, whether placing orders in the system led to fewer medication and other errors, whether order sets were important for the efficient use of the system, whether order sets helped to ensure that important aspects of care did not slip through the cracks, whether the system's user interface supported their work flow, and whether the encouragement of nurses was an important factor in their use of the system. Questions that assessed physician attitudes were presented on a 5‐point Likert scale. Nonrespondents were sent reminder letters along with duplicate surveys twice, approximately 1 and 2 months after the initial mailing. No financial incentive was offered for participation. The study protocol was approved by the Institutional Review Board of Baystate Health System.
Order Entry Rates
Regardless of whether an order is placed directly by a physician into a computer, given verbally, or handwritten, all orders are ultimately entered into the CPOE system. Working with our hospitals' Departments of Information Services, we developed a report that provided physician‐specific information about order entry patterns. For each physician in the study, we determined the total number of orders generated during the month preceding the initial June mailing, as well as the absolute number and percentage of orders of each of the following categories: directly entered, telephone, verbal, and written. Because verbal and telephone orders are required during urgent situations and when physicians give orders from outside the hospital, we calculated and report an adjusted order entry rate as the total number of orders placed directly into the system divided by the sum of the orders entered directly and the number of written orders.
Analysis
Summary statistics for the overall sample were constructed using simple frequencies and proportions for categorical variables and medians and interquartile ranges for continuous variables. We compared characteristics of respondents from the 2 hospitals using chi‐square tests of association for categorical factors and Wilcoxon rank‐sum tests for continuous scale data. We compared the total number of orders placed during the study month and the order entry rates of responders and nonresponders using the Wilcoxon rank‐sum test. We categorized physicians as low (20%), intermediate (21%‐79%), and high (80%) users of the system based on their calculated order entry rate. Responses to each of the attitude questions in the survey were tabulated, and the responses strongly agree and agree were combined for analyses comparing responses. Demographic variables and physician attitudes were tested for associations with order entry rate categories via the Pearson chi‐square for categorical factors, the Mantel‐Haenszel chi‐square for ordered factors, and Kruskal‐Wallis analysis of variance for continuous variables. Initial analyses were stratified by hospital; where no differences in association were found across strata, the data were combined. Statistical tests were performed using SAS version 9.1 (SAS Institute, Cary, NC)
RESULTS
During the study period the target group of physicians placed a total of 135,692 orders, of which 69,654 (51%) were placed directly into the CPOE system, 38,878 (29%) were made using pen and paper, 7,208 (5%) were made verbally, and 19,952 (15%) were placed by telephone. Three hundred and fifty‐six (71%) of the 502 surveys sent out to physicians at the 2 hospitals were returned. Thirteen surveys were excluded from analysis because the respondent was not a physician, and 2 because we were unable to match the survey to system usage data, leaving a total of 341 surveys for analysis. Order entry rates were not computed for an additional 3 physicians who only placed verbal and telephone orders during the study period. Response rates did not differ by clinician specialty (P = .53); compared to those of nonresponders, respondents had a similar median total number of orders (111 vs. 101, P = .67) and a higher median order entry rate (66% vs. 48%, P = .03).
Characteristics of Respondents
Seventy‐two percent of physicians who completed the survey were men; half had graduated from medical school at least 20 years ago, and the median duration of practice at the study institution was 11 years (Table 1). Forty percent practiced internal medicine, 18% were surgeons, and 16% were pediatricians. Thirty‐five percent completed training at an institution that had computerized physician order entry, and 86% cared for patients primarily at Baystate Medical Center. More than half reported they used the system many times each day for patient care, and the features they used most commonly were retrieval of results (95%), placing of orders (78%), and viewing and printing of patient lists (75%). Among those with outpatient practices, 81% used computers in their outpatient practice, and more than half used computers for personal activities at home at least once a day. On average, respondents from Franklin Medical Center had graduated from medical school farther in the past and reported less reliance on the system to carry out all activities other than viewing results.
| Overall n (%) | Baystate n (%) 293 (85.9) | Franklin n (%) 48 (14.1) | Chi square P value | |
|---|---|---|---|---|
| ||||
| Sex | .64 | |||
| Male | 244 (71.6) | 211 (72.0) | 33 (68.8) | |
| Specialty | .24 | |||
| Anesthesia | 23 (6.7) | 23 (7.9) | 0 (0.0) | |
| Internal medicine | 135 (39.6) | 112 (38.2) | 23 (47.9) | |
| Medicine/pediatrics | 13 (3.8) | 6 (2.0) | 7 (14.6) | |
| OB/GYN | 36 (10.6) | 30 (10.2) | 6 (12.5) | |
| Pediatrics | 54 (15.8) | 51 (17.4) | 3 (6.3) | |
| Surgery | 61 (17.9) | 55 (18.8) | 6 (12.5) | |
| Other | 19 (5.6) | 16 (5.5) | 3 (6.3) | |
| Use of CPOE systema | .09 | |||
| Many times a day | 176 (52.2) | 160 (55.0) | 16 (34.8) | |
| At least once a day | 77 (22.9) | 61 (21.0) | 16 (34.8) | |
| A few times a week | 55 (16.3) | 45 (15.5) | 10 (21.7) | |
| Once a week or less | 29 (8.6) | 25 (8.6) | 4 (8.7) | |
| Features useda | ||||
| Viewing and printing patient lists | 254 (75.2) | 212 (72.6) | 42 (91.3) | .01 |
| Looking up results | 320 (94.7) | 277 (94.9) | 43 (93.5) | .70 |
| Viewing current medications | 218 (64.5) | 204 (69.9) | 14 (30.4) | < .01 |
| Placing orders | 263 (77.8) | 244 (83.6) | 19 (41.3) | < .01 |
| Entering discharge summaries | 72 (21.3) | 70 (24.0) | 2 (4.4) | < .01 |
| Use of order setsa | ||||
| Rarely or never | 98 (29.0) | 74 (25.3) | 24 (52.2) | < .01 |
| Minority of patients | 92 (27.2) | 78 (26.7) | 14 (30.4) | |
| Majority of patients | 104 (30.8) | 97 (33.2) | 7 (15.2) | |
| For all or nearly all patients | 44 (13.0) | 43 (14.7) | 1 (2.2) | |
| Percentage of orders placed using order setsa | < .01 | |||
| None | 46 (13.7) | 26 (9.0) | 20 (44.4) | |
| 1%‐25% | 62 (18.5) | 50 (17.2) | 12 (26.7) | |
| 26%‐50% | 29 (8.7) | 23 (7.9) | 6 (13.3) | |
| 51%‐75% | 45 (13.4) | 43 (14.9) | 2 (4.4) | |
| 76%‐99% | 103 (30.8) | 98 (33.8) | 5 (11.1) | |
| All | 50 (14.9) | 50 (17.2) | 0 (0.0) | |
| Use of computer in outpatient practiceab | 243 (81.3) | 206 (80.8) | 37 (84.1) | .60 |
| Personal computer usea | .47 | |||
| At least once a day | 209 (61.7) | 185 (63.4) | 24 (51.1) | |
| Several times a week | 84 (24.8) | 67 (23.0) | 17 (36.2) | |
| A few times a month | 21 (6.2) | 18 (6.2) | 3 (6.4) | |
| Rarely | 25 (7.4) | 22 (7.5) | 3 (6.4) | |
| Training at an institution that had CPOE | 117 (34.7) | 105 (36.1) | 12 (26.1) | 0.19 |
| Use of system to enter orders should be mandatorya | ||||
| Yes | 113 (35.2) | 106 (38.4) | 7 (15.6) | <.01 |
| Median (IQR) | Median (IQR) | Median (IQR) | WilcoxonPvalue | |
| Years since medical school graduationa | 20 (13, 26) | 20 (13, 26) | 24 (17, 28) | .02 |
| Years in practice at study institutiona | 11 (5, 18) | 11 (5, 18) | 13 (7, 19) | .39 |
| Orders directly enteredc | 23 (2, 99) | 27 (5, 108) | 1 (0, 27) | < .01 |
| Orders placed by telephonec | 14 (5, 49) | 12 (3, 38) | 49.5 (16, 123.5) | < .01 |
| Orders placed verballyc | 2 (0, 11) | 3 (0, 13) | 1 (0,3) | < .01 |
| Orders placed in writingc | 21 (4, 73) | 14 (3, 45) | 220 (106.5, 391) | < .01 |
| CPOE ratebc | 66% (3%, 94%) | 76% (19%, 96%) | 0.25% (0%, 17%) | < .01 |
Attitudes Toward Computerized Physician Order Entry
Physicians who completed the survey offered diverse opinions about the impact of computerized order entry on work flow, patient safety, and quality of care. Only 22% believed the system's user interface supported their work flow (Q7), 34% believed it was faster to enter orders directly into the system than to handwrite them (Q1), and 41% believed orders placed into the system were carried out more rapidly (Q2) (Table 2). On the other hand, 63% of respondents believed that placing orders directly into the system led to fewer medication errors (Q3), and 51% stated the system generally reduced medical errors (Q4). Sixty‐nine percent stated order sets were important for efficient use of the system (Q5), and 71% believed order sets served an important decision support role (Q6). Twenty‐six percent stated that the encouragement of nurses was an important factor in their use of the system (Q8). Finally, 35% of attending physicians believed use of the system to place orders should be mandatory.
Characteristics and Attitudes of High, Intermediate, and Low Users
The median order entry rate of respondents was 66%. One hundred and forty‐one (42%) placed at least 80% of their orders directly into the system, whereas 109 (32%) placed no more than 20% of their orders directly in the system (Fig. 1). There was not a significant difference between the low, intermediate, and high use groups in the total number of orders that each physician placed during the study period (Table 3). Sex, years since graduation from medical school, years in practice at the study institution, and use of computers in the outpatient setting were not meaningfully different between the 3 categories of users (Table 3). On the other hand, medical specialty was strongly associated with use of the system, with anesthesiologists, pediatricians, and surgeons the specialties with the largest proportion of high users. Furthermore, physicians who were trained in a CPOE environment and those who reported daily use of computers for personal activities showed the highest levels of adoption. Physicians at Franklin Medical Center showed lower levels of order entry than their counterparts at Baystate.
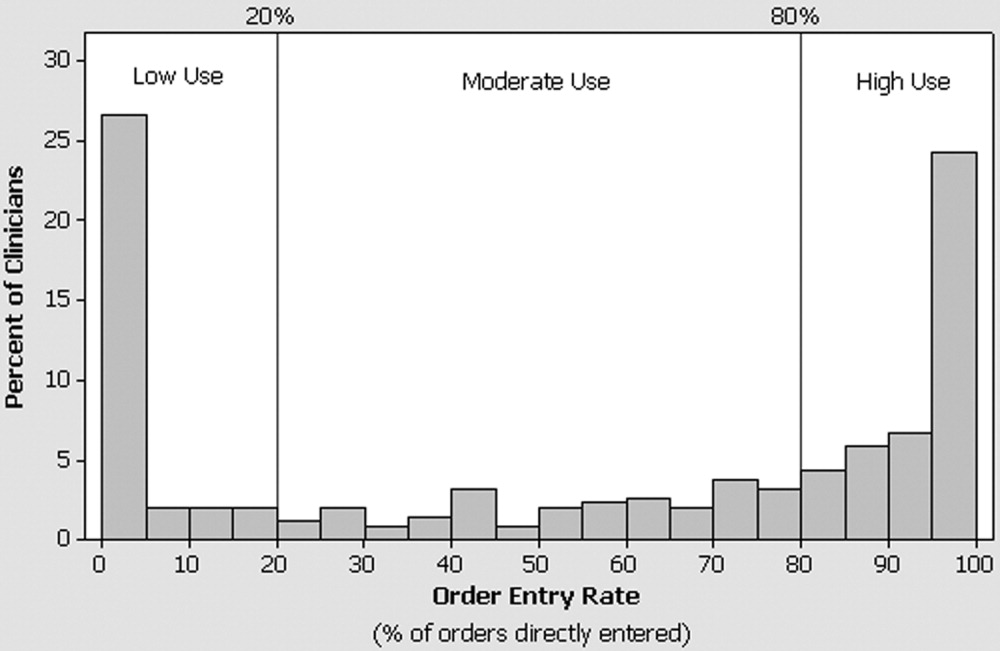
| Low (20%) n (row %) | Intermediate (20%‐79%) n (row %) | High (80%) n (row %) | P value | |
|---|---|---|---|---|
| ||||
| n = 109 | n = 88 | n = 141 | ||
| Hospital | < .01c | |||
| Baystate | 73 (25) | 79 (27) | 138 (48) | |
| Franklin | 36 (75) | 9 (19) | 3 (6) | |
| Sex | .69c | |||
| Female | 28 (29) | 24 (25) | 43 (45) | |
| Male | 81 (33) | 64 (26) | 98 (40) | |
| Specialty | .0001c | |||
| Anesthesia | 8 (35) | 3 (13) | 12 (52) | |
| Internal medicine | 45 (33) | 37 (27) | 53 (39) | |
| Medicine/pediatrics | 6 (46) | 5 (38) | 2 (15) | |
| OB/GYN | 20 (56) | 12 (33) | 4 (11) | |
| Pediatrics | 13 (24) | 9 (17) | 32 (59) | |
| Surgery | 14 (23) | 21 (34) | 26 (43) | |
| Other | 3 (19) | 1 (6) | 12 (75) | |
| Do you use a computer in your outpatient practice?a | ||||
| Yes | 75 (31) | 61 (25) | 105 (44) | .22c |
| No | 20 (36) | 18 (33) | 17 (31) | |
| Level of personal computer useb | .045d | |||
| Rarely | 11 (44) | 8 (32) | 6 (24) | |
| A few times a month | 7 (33) | 4 (19) | 10 (48) | |
| Several times a week | 28 (35) | 25 (31) | 28 (35) | |
| At least once a day | 62 (30) | 50 (24) | 97 (46) | |
| Training at an institution that had CPOE | .037c | |||
| Yes | 30 (26) | 40 (34) | 46 (40) | |
| No | 76 (35) | 48 (22) | 94 (43) | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Years since graduation from medical school | 21 (16, 28) | 18 (14, 25) | 19 (12, 25) | .06e |
| Years in practice at study institution | 12 (5, 19) | 12 (6, 19) | 12 (6, 17) | .84e |
| Total number of orders placed | 112 (45, 306) | 105 (56, 254) | 113 (44, 382) | .92e |
Use of the system was highly associated with physician attitudes toward CPOE, with the views of intermediate and high users consistently different than those of low users (Fig. 2). The associations found held true regardless of hospital: low, intermediate, and high users from Franklin had similar responses to those from Baystate (P > .05 for all questions), and the data from the 2 hospitals therefore were combined for presentation. Although few physicians believed that the user interface of the system supported their work flow, high and intermediate users were 3 times as likely to share this view than were low users (Q7; Fig. 2). Similarly, 19% of low users, 31% of intermediate users, and 45% of high users believed that entering orders into the system was faster than writing orders (Q1). High and intermediate users of the system were more likely than low users to believe that orders entered into the system were carried out more rapidly (Q2) and led to fewer medication (Q3) and nonmedication (Q4) errors. Regardless of their utilization pattern, most physicians believed that order sets played an important role in promoting efficiency and quality.
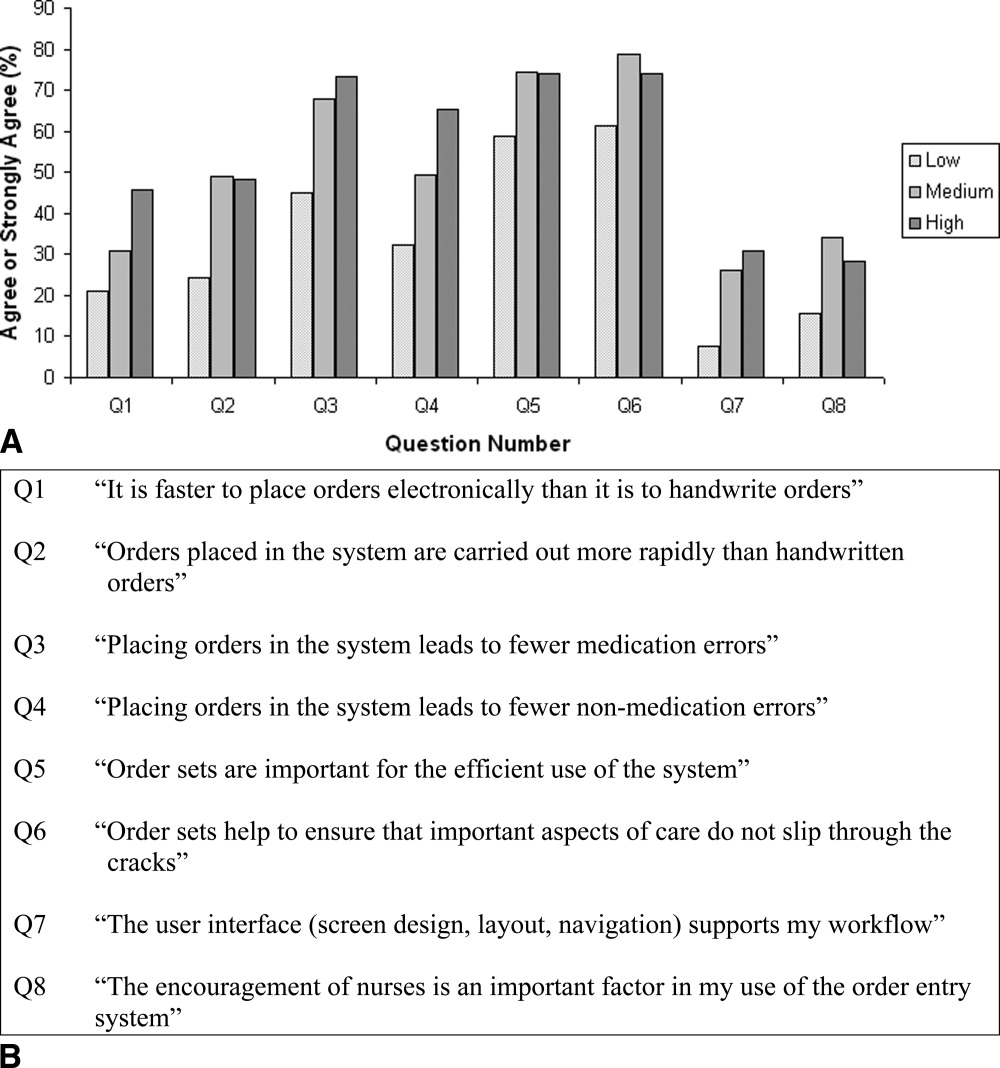
DISCUSSION
In this study of the clinical computing practices of physicians at 2 community hospitals, we observed wide variation in the adoption of CPOE by individual attendings. Although roughly one‐third rarely placed orders directly into the system, 42% had an order entry rate of at least 80%. Contrary to our initial expectation, we found little association between a physician's order entry rate with years in practice, duration of exposure to CPOE, or use of computers in the outpatient setting. On the other hand, we observed marked differences in use of the CPOE system across specialty lines and found that physicians who were exposed to CPOE during training and those who were regular users of computers for personal activities were more likely to embrace this technology. Further, we observed important differences between physicians who used the system to place some or most of their orders and those who did so only rarely in their beliefs and attitudes about the impact and benefits of CPOE. Physicians with higher order entry rates were more likely than their colleagues to believe that placing orders electronically was faster than handwriting and that use of the system led to fewer medical errors. These findings should be encouraging to hospitals hoping to implement CPOE because they suggest that successful adoption of CPOE is not limited to physicians who have just completed their residencies or to hospitals with the capability of designing and building their own systems. On the contrary, we documented that women, older physicians, and those with limited CPOE experience were as likely to be frequent users, especially if they perceived CPOE to be safer than handwriting and if they believed the user interface supported the efficient entering of orders.
On the basis of these results we recommend that in addition to purchasing systems that meet physician work‐flow needs and support the efficient entry of orders, hospital leaders should emphasize the quality and safety benefits of CPOE as part of a comprehensive change management strategy. The differences we observed in order entry rates across specialties may have resulted from several factors, including inherent differences in personality type associated with choice of specialty and in the level of customization of a system reflected in which and how many order sets are included. Such findings suggest that when it comes to CPOE, one size does not fit all, and implementation planning should be carried out at the specialty level. Finally, our observation that physicians who had exposure to CPOE during training were more likely to use the system to place orders suggests that the nation's training institutions will play an important role in fostering universal adoption of this technology.
Several earlier studies have reported on physician experiences with CPOE systems. Murff and Kannry12 surveyed 94 internal medicine house staff to compare experiences with 2 CPOE systems: the Department of Veterans Affairs Computerized Patient Record System (CPRS) and a commercially available product. They found striking differences in user satisfaction with numerous aspects of the systems, however they did not address attitudes toward safety or quality, and because house staff were required to place orders electronically they were unable to correlate responses with actual usage patterns. Weiner et al.13 compared the opinions of internal medicine house staff, attendings, fellows, and nurses about the benefits and challenges of using a computerized provider order entry system. In contrast to the findings from our study, Weiner et al. reported that more than half of physicians believed that provider order entry led to a greater number of errors, and only a minority believed the system increased quality of care overall. Finally, Lee et al.14 surveyed medical and surgical house officers and nurses at a large academic medical center about their satisfaction with a locally developed order entry system. They found that attitudes about the impact of the system on productivity and ease of use were more strongly associated with overall satisfaction than having undergone training or experience with personal computers. These findings are congruous with our own observation that beliefs about the speed with which orders are placed are closely associated with actual use of the system. They reported, as have we, that physicians placed a high value on order sets.
Our study had a number of strengths. First, we were able to offer insight into the attitudes and behaviors of a previously neglected, but critically important groupattending physicians who care for patients at community hospitals without the assistance of house staff. Second, whereas previous studies primarily assessed physician satisfaction with CPOE, we explored how physician attitudes about the impact of CPOE on work flow and on safety were associated with actual ordering habits. Information about ordering was obtained directly from the order entry system and not through self‐report. We conducted the study at 2 hospitals, a large urban community teaching hospital and a smaller rural hospital, and focused on a CPOE system that is in use at many institutions throughout the country, thereby increasing the generalizability of our findings. Although adoption of the system by physicians at the 2 hospitals differed, factors that associated with the use of CPOE to place orders were similar. Finally, we surveyed a large number of physicians, had a high response rate, and found only small differences in the utilization patterns of responders and nonresponders, suggesting that our portrayal of the attitudes of physicians was representative of the views of physicians practicing in our community.
The study had a number of weaknesses. First, we cannot be sure whether preexisting beliefs about the benefits of CPOE directly influenced physicians' use of the system or, conversely, if these attitudes developed in response to experience as users. Nevertheless, it seems practical to suggest that hospitals focus on purchasing systems that support the efficient entering of orders while simultaneously adopting a communication and change management strategy that emphasizes the safety and quality benefits of CPOE more broadly. Second, we did not attempt to validate the opinions expressed by physicians about the usability or safety benefits of the system. That said, the purpose of the study was to determine whether physician attitudes toward these issues was associated with the use of the system to place orders. Whether or not this particular CPOE system actually prevented medication errors, most physicians believed it did, a belief strongly associated with the observed order entry rates. Third, we studied a single CPOE system implemented approximately 10 years ago that does not reflect state‐of‐the‐art user interface design or functionality. Nevertheless, our observation about the importance of the user experience is probably no less relevant today. Fourth, we were unable to ascertain every order given by physicians, as some so‐called MD to RN orders may never have made it into the system. Finally, there is a small risk that some written, telephone, and verbal orders may have been randomly or systematically assigned to incorrect physicians, which would have led us to calculate inaccurate utilization rates.
CONCLUSIONS
In a voluntary community hospital environment the adoption of CPOE by attending physicians varies widely. While placing a premium on the purchase of systems that meet the work‐flow needs of physicians and support the efficient entry of orders, hospital leaders can enhance physician adoption of this technology by communicating the role of CPOE in improving quality and safety.
Acknowledgements
The authors thank Gilad Kuperman, MD, PhD, for his thoughtful comments on an earlier version of the manuscript.
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press,2000.
- ,.Computer physician order entry: benefits, costs, and issues.Ann Intern Med.2003;139:31–39.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,,,,.A computerized reminder system to increase the use of preventive care for hospitalized patients.N Engl J Med.2001;345:965–970.
- ,,,.A randomized trial of “corollary orders” to prevent errors of omission.J Am Med Inform Assoc.1997;4:364–375.
- ,,, et al.A computer‐assisted management program for antibiotics and other antiinfective agents.N Engl J Med.1998;338:232–238.
- The Leapfrog Group. Patient Safety Fact Sheet. Available at: http://www.leapfroggroup.org/FactSheets/LF_FactSheet.pdf. Accessed October 6,2004.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,.U.S. adoption of computerized physician order entry systems.Health Aff.2005;24:1654–1663.
- ,,.Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review.Arch Intern Med.2003;163:1409–1416.
- HCUPnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 6,2004.
- ,.Physician satisfaction with two order entry systems.J Am Med Inform Assoc.2001;8:499–509.
- ,,, et al.Contrasting views of physicians and nurses about an inpatient computer‐based provider order‐entry system.J Am Med Inform Assoc.1999;6:234–244.
- ,,,.Implementation of physician order entry: user satisfaction and self‐reported usage patterns.J Am Med Inform Assoc.1996;3:42–55.
It is widely acknowledged that the U.S. health care system is plagued by error and inefficiency and that these factors contribute to as many as 44,000‐98,000 deaths each year in U.S. hospitals. In To Err Is Human: Building a Safer Health System, the Institute of Medicine1 outlined the critical role that information technology can play in improving patient safety and highlighted computerized physician order entry (CPOE) systems for their potential to reduce the frequency of medication errors and to improve the quality of medical care.
Computerized physician order entry systems are specialized software applications that allow physicians to place orders directly into a computer. This process has a number of potential advantages over traditional handwritten ordering, including the ability to structure the ordering process to ensure the completeness of individual orders, to provide clinical decision support through diagnosis‐based order sets, and to automatically check orders for potential drugallergy, drugdrug, and drugfood interactions.2 Finally, entering orders directly into a computer eliminates the problem of transcription‐related errors that stem from the difficulty of interpreting handwriting. In clinical trials, the introduction of CPOE has been shown to reduce the frequency of medication errors, to improve the use of preventive services, and to reduce costs.36 Recognition of the benefits of these systems has not been confined to the medical community. The Leapfrog Organization, a coalition of large businesses in the United States, has chosen CPOE as one of its 3 initial safety leaps and has established a threshold that 70% of medication orders should be entered directly by physicians.7
Although the benefits of CPOE systems are widely recognized, few hospitals have implemented these systems successfully.8, 9 Those that have, have often developed the applications internally, and many have relied on house staff to do most or all of the actual ordering.10 However, most hospitals do not have the expertise for internal development and instead rely on commercially available products. Moreover, most patients hospitalized in the United States are cared for by attending physicians working without the assistance of house staff.11 In light of the importance of successfully implementing CPOE systems in such settings, we assessed the adoption of CPOE by attending physicians at 2 community hospitals where its use was voluntary and examined the characteristics and attitudes associated with use of the system to place orders.
METHODS
Setting and Participants
Baystate Medical Center is a 600‐bed teaching hospital in Springfield, Massachusetts, where approximately 50% of patients are cared for with the assistance of house staff. Franklin Medical Center is a 125‐bed community hospital in rural Greenfield, Massachusetts, and is not a house staff training site. Medical staff membership at the 2 hospitals is largely voluntary. Both institutions share a vendor‐supplied computerized order entry system that was implemented in the early 1990s (E7000, Eclipsys Corporation, Boca Raton, FL). The system provides a structured format for the creation of medication, laboratory, and radiology orders and contains thousands of preconstructed medication order sentences and hundreds of order sets designed to standardize ordering for common diagnoses and procedures. Pharmacists are alerted of potential drugallergy and drugdrug interactions and use clinical judgment about whether to communicate this information to the physician. Although the house staff at Baystate Medical Center is mandated to place orders in the system, attending physicians have no such requirement at either institution. Access to the system is provided though the many fixed workstations located on nursing units, in operating rooms, and in the health sciences library. On a typical medical‐surgical patient care unit most computers are behind the nurses' station, though some are distributed along hallways and in physician charting rooms. No computers are in patient rooms. Although the number varies slightly across units, the average ratio of computers to patient beds is roughly 1 to 1.
Survey
In June 2003 we mailed a 20‐item survey to attending physicians who had been responsible for a minimum of 25 orders during the preceding month at either Baystate or Franklin Medical Center. Orders counted toward this minimum if they had been written, given verbally in person or by phone, or entered directly into the computer by the physician. The survey consisted of 20 questions focused on the topic of computerized order entry. In addition to collecting information about sex and specialty, we asked respondents to describe their use of CPOE during training, their use of computers at home, and, where applicable, their use of computers in their outpatient practices. The survey included questions about how often respondents used the order entry system when caring for hospitalized patients and which features of the system they used. To assess physician attitudes about the order entry process, we asked respondents to consider whether it was faster to place orders directly into the system than it was by handwriting them, whether orders placed in the system were carried out more rapidly, whether placing orders in the system led to fewer medication and other errors, whether order sets were important for the efficient use of the system, whether order sets helped to ensure that important aspects of care did not slip through the cracks, whether the system's user interface supported their work flow, and whether the encouragement of nurses was an important factor in their use of the system. Questions that assessed physician attitudes were presented on a 5‐point Likert scale. Nonrespondents were sent reminder letters along with duplicate surveys twice, approximately 1 and 2 months after the initial mailing. No financial incentive was offered for participation. The study protocol was approved by the Institutional Review Board of Baystate Health System.
Order Entry Rates
Regardless of whether an order is placed directly by a physician into a computer, given verbally, or handwritten, all orders are ultimately entered into the CPOE system. Working with our hospitals' Departments of Information Services, we developed a report that provided physician‐specific information about order entry patterns. For each physician in the study, we determined the total number of orders generated during the month preceding the initial June mailing, as well as the absolute number and percentage of orders of each of the following categories: directly entered, telephone, verbal, and written. Because verbal and telephone orders are required during urgent situations and when physicians give orders from outside the hospital, we calculated and report an adjusted order entry rate as the total number of orders placed directly into the system divided by the sum of the orders entered directly and the number of written orders.
Analysis
Summary statistics for the overall sample were constructed using simple frequencies and proportions for categorical variables and medians and interquartile ranges for continuous variables. We compared characteristics of respondents from the 2 hospitals using chi‐square tests of association for categorical factors and Wilcoxon rank‐sum tests for continuous scale data. We compared the total number of orders placed during the study month and the order entry rates of responders and nonresponders using the Wilcoxon rank‐sum test. We categorized physicians as low (20%), intermediate (21%‐79%), and high (80%) users of the system based on their calculated order entry rate. Responses to each of the attitude questions in the survey were tabulated, and the responses strongly agree and agree were combined for analyses comparing responses. Demographic variables and physician attitudes were tested for associations with order entry rate categories via the Pearson chi‐square for categorical factors, the Mantel‐Haenszel chi‐square for ordered factors, and Kruskal‐Wallis analysis of variance for continuous variables. Initial analyses were stratified by hospital; where no differences in association were found across strata, the data were combined. Statistical tests were performed using SAS version 9.1 (SAS Institute, Cary, NC)
RESULTS
During the study period the target group of physicians placed a total of 135,692 orders, of which 69,654 (51%) were placed directly into the CPOE system, 38,878 (29%) were made using pen and paper, 7,208 (5%) were made verbally, and 19,952 (15%) were placed by telephone. Three hundred and fifty‐six (71%) of the 502 surveys sent out to physicians at the 2 hospitals were returned. Thirteen surveys were excluded from analysis because the respondent was not a physician, and 2 because we were unable to match the survey to system usage data, leaving a total of 341 surveys for analysis. Order entry rates were not computed for an additional 3 physicians who only placed verbal and telephone orders during the study period. Response rates did not differ by clinician specialty (P = .53); compared to those of nonresponders, respondents had a similar median total number of orders (111 vs. 101, P = .67) and a higher median order entry rate (66% vs. 48%, P = .03).
Characteristics of Respondents
Seventy‐two percent of physicians who completed the survey were men; half had graduated from medical school at least 20 years ago, and the median duration of practice at the study institution was 11 years (Table 1). Forty percent practiced internal medicine, 18% were surgeons, and 16% were pediatricians. Thirty‐five percent completed training at an institution that had computerized physician order entry, and 86% cared for patients primarily at Baystate Medical Center. More than half reported they used the system many times each day for patient care, and the features they used most commonly were retrieval of results (95%), placing of orders (78%), and viewing and printing of patient lists (75%). Among those with outpatient practices, 81% used computers in their outpatient practice, and more than half used computers for personal activities at home at least once a day. On average, respondents from Franklin Medical Center had graduated from medical school farther in the past and reported less reliance on the system to carry out all activities other than viewing results.
| Overall n (%) | Baystate n (%) 293 (85.9) | Franklin n (%) 48 (14.1) | Chi square P value | |
|---|---|---|---|---|
| ||||
| Sex | .64 | |||
| Male | 244 (71.6) | 211 (72.0) | 33 (68.8) | |
| Specialty | .24 | |||
| Anesthesia | 23 (6.7) | 23 (7.9) | 0 (0.0) | |
| Internal medicine | 135 (39.6) | 112 (38.2) | 23 (47.9) | |
| Medicine/pediatrics | 13 (3.8) | 6 (2.0) | 7 (14.6) | |
| OB/GYN | 36 (10.6) | 30 (10.2) | 6 (12.5) | |
| Pediatrics | 54 (15.8) | 51 (17.4) | 3 (6.3) | |
| Surgery | 61 (17.9) | 55 (18.8) | 6 (12.5) | |
| Other | 19 (5.6) | 16 (5.5) | 3 (6.3) | |
| Use of CPOE systema | .09 | |||
| Many times a day | 176 (52.2) | 160 (55.0) | 16 (34.8) | |
| At least once a day | 77 (22.9) | 61 (21.0) | 16 (34.8) | |
| A few times a week | 55 (16.3) | 45 (15.5) | 10 (21.7) | |
| Once a week or less | 29 (8.6) | 25 (8.6) | 4 (8.7) | |
| Features useda | ||||
| Viewing and printing patient lists | 254 (75.2) | 212 (72.6) | 42 (91.3) | .01 |
| Looking up results | 320 (94.7) | 277 (94.9) | 43 (93.5) | .70 |
| Viewing current medications | 218 (64.5) | 204 (69.9) | 14 (30.4) | < .01 |
| Placing orders | 263 (77.8) | 244 (83.6) | 19 (41.3) | < .01 |
| Entering discharge summaries | 72 (21.3) | 70 (24.0) | 2 (4.4) | < .01 |
| Use of order setsa | ||||
| Rarely or never | 98 (29.0) | 74 (25.3) | 24 (52.2) | < .01 |
| Minority of patients | 92 (27.2) | 78 (26.7) | 14 (30.4) | |
| Majority of patients | 104 (30.8) | 97 (33.2) | 7 (15.2) | |
| For all or nearly all patients | 44 (13.0) | 43 (14.7) | 1 (2.2) | |
| Percentage of orders placed using order setsa | < .01 | |||
| None | 46 (13.7) | 26 (9.0) | 20 (44.4) | |
| 1%‐25% | 62 (18.5) | 50 (17.2) | 12 (26.7) | |
| 26%‐50% | 29 (8.7) | 23 (7.9) | 6 (13.3) | |
| 51%‐75% | 45 (13.4) | 43 (14.9) | 2 (4.4) | |
| 76%‐99% | 103 (30.8) | 98 (33.8) | 5 (11.1) | |
| All | 50 (14.9) | 50 (17.2) | 0 (0.0) | |
| Use of computer in outpatient practiceab | 243 (81.3) | 206 (80.8) | 37 (84.1) | .60 |
| Personal computer usea | .47 | |||
| At least once a day | 209 (61.7) | 185 (63.4) | 24 (51.1) | |
| Several times a week | 84 (24.8) | 67 (23.0) | 17 (36.2) | |
| A few times a month | 21 (6.2) | 18 (6.2) | 3 (6.4) | |
| Rarely | 25 (7.4) | 22 (7.5) | 3 (6.4) | |
| Training at an institution that had CPOE | 117 (34.7) | 105 (36.1) | 12 (26.1) | 0.19 |
| Use of system to enter orders should be mandatorya | ||||
| Yes | 113 (35.2) | 106 (38.4) | 7 (15.6) | <.01 |
| Median (IQR) | Median (IQR) | Median (IQR) | WilcoxonPvalue | |
| Years since medical school graduationa | 20 (13, 26) | 20 (13, 26) | 24 (17, 28) | .02 |
| Years in practice at study institutiona | 11 (5, 18) | 11 (5, 18) | 13 (7, 19) | .39 |
| Orders directly enteredc | 23 (2, 99) | 27 (5, 108) | 1 (0, 27) | < .01 |
| Orders placed by telephonec | 14 (5, 49) | 12 (3, 38) | 49.5 (16, 123.5) | < .01 |
| Orders placed verballyc | 2 (0, 11) | 3 (0, 13) | 1 (0,3) | < .01 |
| Orders placed in writingc | 21 (4, 73) | 14 (3, 45) | 220 (106.5, 391) | < .01 |
| CPOE ratebc | 66% (3%, 94%) | 76% (19%, 96%) | 0.25% (0%, 17%) | < .01 |
Attitudes Toward Computerized Physician Order Entry
Physicians who completed the survey offered diverse opinions about the impact of computerized order entry on work flow, patient safety, and quality of care. Only 22% believed the system's user interface supported their work flow (Q7), 34% believed it was faster to enter orders directly into the system than to handwrite them (Q1), and 41% believed orders placed into the system were carried out more rapidly (Q2) (Table 2). On the other hand, 63% of respondents believed that placing orders directly into the system led to fewer medication errors (Q3), and 51% stated the system generally reduced medical errors (Q4). Sixty‐nine percent stated order sets were important for efficient use of the system (Q5), and 71% believed order sets served an important decision support role (Q6). Twenty‐six percent stated that the encouragement of nurses was an important factor in their use of the system (Q8). Finally, 35% of attending physicians believed use of the system to place orders should be mandatory.
Characteristics and Attitudes of High, Intermediate, and Low Users
The median order entry rate of respondents was 66%. One hundred and forty‐one (42%) placed at least 80% of their orders directly into the system, whereas 109 (32%) placed no more than 20% of their orders directly in the system (Fig. 1). There was not a significant difference between the low, intermediate, and high use groups in the total number of orders that each physician placed during the study period (Table 3). Sex, years since graduation from medical school, years in practice at the study institution, and use of computers in the outpatient setting were not meaningfully different between the 3 categories of users (Table 3). On the other hand, medical specialty was strongly associated with use of the system, with anesthesiologists, pediatricians, and surgeons the specialties with the largest proportion of high users. Furthermore, physicians who were trained in a CPOE environment and those who reported daily use of computers for personal activities showed the highest levels of adoption. Physicians at Franklin Medical Center showed lower levels of order entry than their counterparts at Baystate.
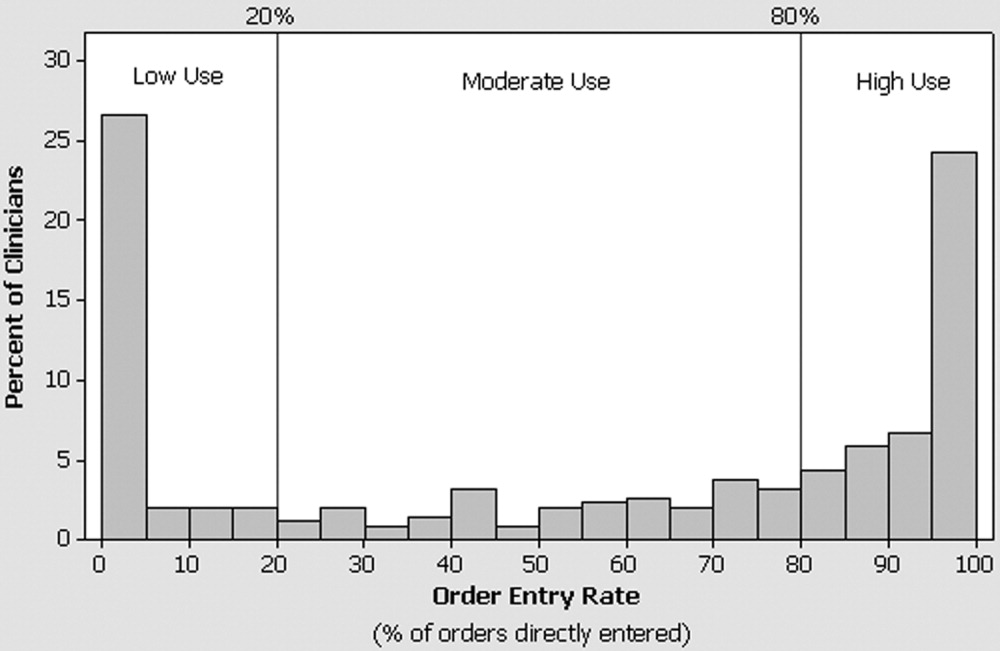
| Low (20%) n (row %) | Intermediate (20%‐79%) n (row %) | High (80%) n (row %) | P value | |
|---|---|---|---|---|
| ||||
| n = 109 | n = 88 | n = 141 | ||
| Hospital | < .01c | |||
| Baystate | 73 (25) | 79 (27) | 138 (48) | |
| Franklin | 36 (75) | 9 (19) | 3 (6) | |
| Sex | .69c | |||
| Female | 28 (29) | 24 (25) | 43 (45) | |
| Male | 81 (33) | 64 (26) | 98 (40) | |
| Specialty | .0001c | |||
| Anesthesia | 8 (35) | 3 (13) | 12 (52) | |
| Internal medicine | 45 (33) | 37 (27) | 53 (39) | |
| Medicine/pediatrics | 6 (46) | 5 (38) | 2 (15) | |
| OB/GYN | 20 (56) | 12 (33) | 4 (11) | |
| Pediatrics | 13 (24) | 9 (17) | 32 (59) | |
| Surgery | 14 (23) | 21 (34) | 26 (43) | |
| Other | 3 (19) | 1 (6) | 12 (75) | |
| Do you use a computer in your outpatient practice?a | ||||
| Yes | 75 (31) | 61 (25) | 105 (44) | .22c |
| No | 20 (36) | 18 (33) | 17 (31) | |
| Level of personal computer useb | .045d | |||
| Rarely | 11 (44) | 8 (32) | 6 (24) | |
| A few times a month | 7 (33) | 4 (19) | 10 (48) | |
| Several times a week | 28 (35) | 25 (31) | 28 (35) | |
| At least once a day | 62 (30) | 50 (24) | 97 (46) | |
| Training at an institution that had CPOE | .037c | |||
| Yes | 30 (26) | 40 (34) | 46 (40) | |
| No | 76 (35) | 48 (22) | 94 (43) | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Years since graduation from medical school | 21 (16, 28) | 18 (14, 25) | 19 (12, 25) | .06e |
| Years in practice at study institution | 12 (5, 19) | 12 (6, 19) | 12 (6, 17) | .84e |
| Total number of orders placed | 112 (45, 306) | 105 (56, 254) | 113 (44, 382) | .92e |
Use of the system was highly associated with physician attitudes toward CPOE, with the views of intermediate and high users consistently different than those of low users (Fig. 2). The associations found held true regardless of hospital: low, intermediate, and high users from Franklin had similar responses to those from Baystate (P > .05 for all questions), and the data from the 2 hospitals therefore were combined for presentation. Although few physicians believed that the user interface of the system supported their work flow, high and intermediate users were 3 times as likely to share this view than were low users (Q7; Fig. 2). Similarly, 19% of low users, 31% of intermediate users, and 45% of high users believed that entering orders into the system was faster than writing orders (Q1). High and intermediate users of the system were more likely than low users to believe that orders entered into the system were carried out more rapidly (Q2) and led to fewer medication (Q3) and nonmedication (Q4) errors. Regardless of their utilization pattern, most physicians believed that order sets played an important role in promoting efficiency and quality.
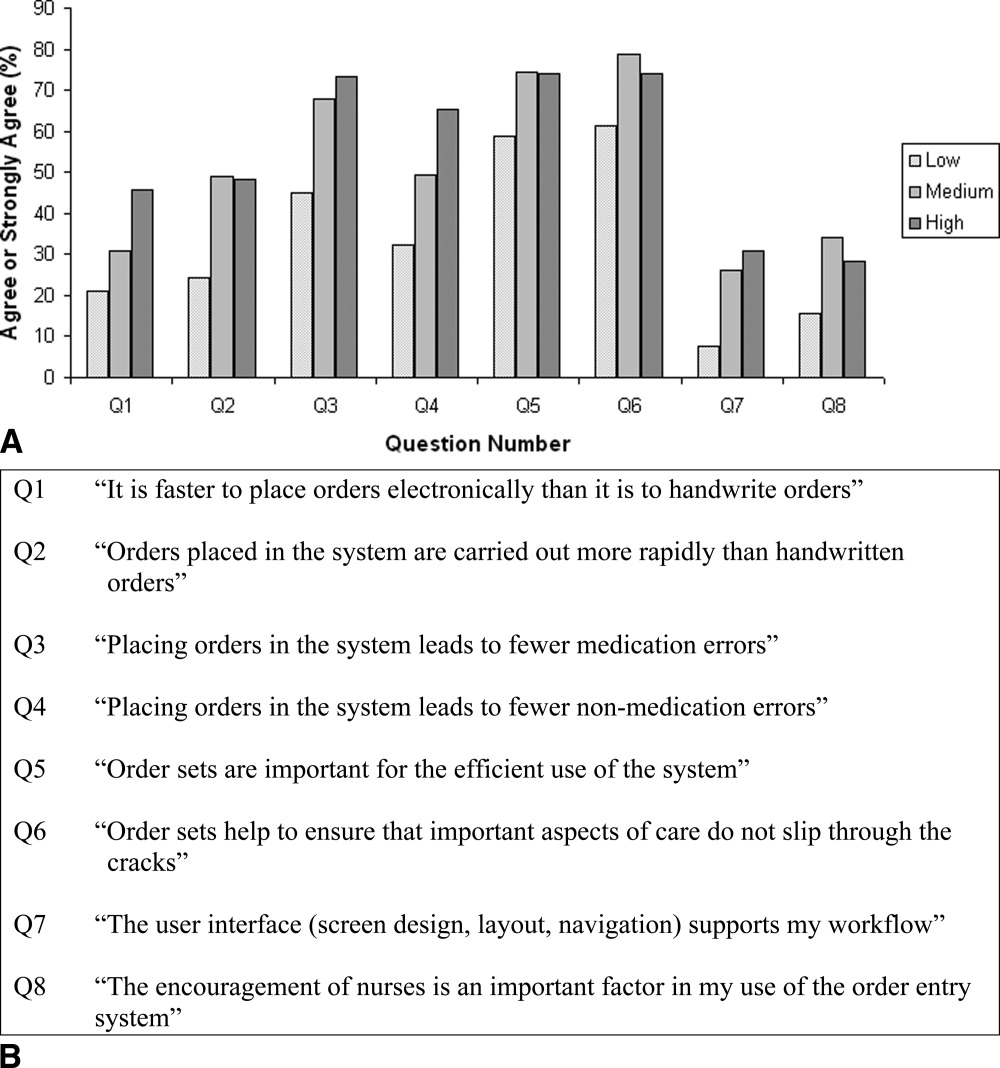
DISCUSSION
In this study of the clinical computing practices of physicians at 2 community hospitals, we observed wide variation in the adoption of CPOE by individual attendings. Although roughly one‐third rarely placed orders directly into the system, 42% had an order entry rate of at least 80%. Contrary to our initial expectation, we found little association between a physician's order entry rate with years in practice, duration of exposure to CPOE, or use of computers in the outpatient setting. On the other hand, we observed marked differences in use of the CPOE system across specialty lines and found that physicians who were exposed to CPOE during training and those who were regular users of computers for personal activities were more likely to embrace this technology. Further, we observed important differences between physicians who used the system to place some or most of their orders and those who did so only rarely in their beliefs and attitudes about the impact and benefits of CPOE. Physicians with higher order entry rates were more likely than their colleagues to believe that placing orders electronically was faster than handwriting and that use of the system led to fewer medical errors. These findings should be encouraging to hospitals hoping to implement CPOE because they suggest that successful adoption of CPOE is not limited to physicians who have just completed their residencies or to hospitals with the capability of designing and building their own systems. On the contrary, we documented that women, older physicians, and those with limited CPOE experience were as likely to be frequent users, especially if they perceived CPOE to be safer than handwriting and if they believed the user interface supported the efficient entering of orders.
On the basis of these results we recommend that in addition to purchasing systems that meet physician work‐flow needs and support the efficient entry of orders, hospital leaders should emphasize the quality and safety benefits of CPOE as part of a comprehensive change management strategy. The differences we observed in order entry rates across specialties may have resulted from several factors, including inherent differences in personality type associated with choice of specialty and in the level of customization of a system reflected in which and how many order sets are included. Such findings suggest that when it comes to CPOE, one size does not fit all, and implementation planning should be carried out at the specialty level. Finally, our observation that physicians who had exposure to CPOE during training were more likely to use the system to place orders suggests that the nation's training institutions will play an important role in fostering universal adoption of this technology.
Several earlier studies have reported on physician experiences with CPOE systems. Murff and Kannry12 surveyed 94 internal medicine house staff to compare experiences with 2 CPOE systems: the Department of Veterans Affairs Computerized Patient Record System (CPRS) and a commercially available product. They found striking differences in user satisfaction with numerous aspects of the systems, however they did not address attitudes toward safety or quality, and because house staff were required to place orders electronically they were unable to correlate responses with actual usage patterns. Weiner et al.13 compared the opinions of internal medicine house staff, attendings, fellows, and nurses about the benefits and challenges of using a computerized provider order entry system. In contrast to the findings from our study, Weiner et al. reported that more than half of physicians believed that provider order entry led to a greater number of errors, and only a minority believed the system increased quality of care overall. Finally, Lee et al.14 surveyed medical and surgical house officers and nurses at a large academic medical center about their satisfaction with a locally developed order entry system. They found that attitudes about the impact of the system on productivity and ease of use were more strongly associated with overall satisfaction than having undergone training or experience with personal computers. These findings are congruous with our own observation that beliefs about the speed with which orders are placed are closely associated with actual use of the system. They reported, as have we, that physicians placed a high value on order sets.
Our study had a number of strengths. First, we were able to offer insight into the attitudes and behaviors of a previously neglected, but critically important groupattending physicians who care for patients at community hospitals without the assistance of house staff. Second, whereas previous studies primarily assessed physician satisfaction with CPOE, we explored how physician attitudes about the impact of CPOE on work flow and on safety were associated with actual ordering habits. Information about ordering was obtained directly from the order entry system and not through self‐report. We conducted the study at 2 hospitals, a large urban community teaching hospital and a smaller rural hospital, and focused on a CPOE system that is in use at many institutions throughout the country, thereby increasing the generalizability of our findings. Although adoption of the system by physicians at the 2 hospitals differed, factors that associated with the use of CPOE to place orders were similar. Finally, we surveyed a large number of physicians, had a high response rate, and found only small differences in the utilization patterns of responders and nonresponders, suggesting that our portrayal of the attitudes of physicians was representative of the views of physicians practicing in our community.
The study had a number of weaknesses. First, we cannot be sure whether preexisting beliefs about the benefits of CPOE directly influenced physicians' use of the system or, conversely, if these attitudes developed in response to experience as users. Nevertheless, it seems practical to suggest that hospitals focus on purchasing systems that support the efficient entering of orders while simultaneously adopting a communication and change management strategy that emphasizes the safety and quality benefits of CPOE more broadly. Second, we did not attempt to validate the opinions expressed by physicians about the usability or safety benefits of the system. That said, the purpose of the study was to determine whether physician attitudes toward these issues was associated with the use of the system to place orders. Whether or not this particular CPOE system actually prevented medication errors, most physicians believed it did, a belief strongly associated with the observed order entry rates. Third, we studied a single CPOE system implemented approximately 10 years ago that does not reflect state‐of‐the‐art user interface design or functionality. Nevertheless, our observation about the importance of the user experience is probably no less relevant today. Fourth, we were unable to ascertain every order given by physicians, as some so‐called MD to RN orders may never have made it into the system. Finally, there is a small risk that some written, telephone, and verbal orders may have been randomly or systematically assigned to incorrect physicians, which would have led us to calculate inaccurate utilization rates.
CONCLUSIONS
In a voluntary community hospital environment the adoption of CPOE by attending physicians varies widely. While placing a premium on the purchase of systems that meet the work‐flow needs of physicians and support the efficient entry of orders, hospital leaders can enhance physician adoption of this technology by communicating the role of CPOE in improving quality and safety.
Acknowledgements
The authors thank Gilad Kuperman, MD, PhD, for his thoughtful comments on an earlier version of the manuscript.
It is widely acknowledged that the U.S. health care system is plagued by error and inefficiency and that these factors contribute to as many as 44,000‐98,000 deaths each year in U.S. hospitals. In To Err Is Human: Building a Safer Health System, the Institute of Medicine1 outlined the critical role that information technology can play in improving patient safety and highlighted computerized physician order entry (CPOE) systems for their potential to reduce the frequency of medication errors and to improve the quality of medical care.
Computerized physician order entry systems are specialized software applications that allow physicians to place orders directly into a computer. This process has a number of potential advantages over traditional handwritten ordering, including the ability to structure the ordering process to ensure the completeness of individual orders, to provide clinical decision support through diagnosis‐based order sets, and to automatically check orders for potential drugallergy, drugdrug, and drugfood interactions.2 Finally, entering orders directly into a computer eliminates the problem of transcription‐related errors that stem from the difficulty of interpreting handwriting. In clinical trials, the introduction of CPOE has been shown to reduce the frequency of medication errors, to improve the use of preventive services, and to reduce costs.36 Recognition of the benefits of these systems has not been confined to the medical community. The Leapfrog Organization, a coalition of large businesses in the United States, has chosen CPOE as one of its 3 initial safety leaps and has established a threshold that 70% of medication orders should be entered directly by physicians.7
Although the benefits of CPOE systems are widely recognized, few hospitals have implemented these systems successfully.8, 9 Those that have, have often developed the applications internally, and many have relied on house staff to do most or all of the actual ordering.10 However, most hospitals do not have the expertise for internal development and instead rely on commercially available products. Moreover, most patients hospitalized in the United States are cared for by attending physicians working without the assistance of house staff.11 In light of the importance of successfully implementing CPOE systems in such settings, we assessed the adoption of CPOE by attending physicians at 2 community hospitals where its use was voluntary and examined the characteristics and attitudes associated with use of the system to place orders.
METHODS
Setting and Participants
Baystate Medical Center is a 600‐bed teaching hospital in Springfield, Massachusetts, where approximately 50% of patients are cared for with the assistance of house staff. Franklin Medical Center is a 125‐bed community hospital in rural Greenfield, Massachusetts, and is not a house staff training site. Medical staff membership at the 2 hospitals is largely voluntary. Both institutions share a vendor‐supplied computerized order entry system that was implemented in the early 1990s (E7000, Eclipsys Corporation, Boca Raton, FL). The system provides a structured format for the creation of medication, laboratory, and radiology orders and contains thousands of preconstructed medication order sentences and hundreds of order sets designed to standardize ordering for common diagnoses and procedures. Pharmacists are alerted of potential drugallergy and drugdrug interactions and use clinical judgment about whether to communicate this information to the physician. Although the house staff at Baystate Medical Center is mandated to place orders in the system, attending physicians have no such requirement at either institution. Access to the system is provided though the many fixed workstations located on nursing units, in operating rooms, and in the health sciences library. On a typical medical‐surgical patient care unit most computers are behind the nurses' station, though some are distributed along hallways and in physician charting rooms. No computers are in patient rooms. Although the number varies slightly across units, the average ratio of computers to patient beds is roughly 1 to 1.
Survey
In June 2003 we mailed a 20‐item survey to attending physicians who had been responsible for a minimum of 25 orders during the preceding month at either Baystate or Franklin Medical Center. Orders counted toward this minimum if they had been written, given verbally in person or by phone, or entered directly into the computer by the physician. The survey consisted of 20 questions focused on the topic of computerized order entry. In addition to collecting information about sex and specialty, we asked respondents to describe their use of CPOE during training, their use of computers at home, and, where applicable, their use of computers in their outpatient practices. The survey included questions about how often respondents used the order entry system when caring for hospitalized patients and which features of the system they used. To assess physician attitudes about the order entry process, we asked respondents to consider whether it was faster to place orders directly into the system than it was by handwriting them, whether orders placed in the system were carried out more rapidly, whether placing orders in the system led to fewer medication and other errors, whether order sets were important for the efficient use of the system, whether order sets helped to ensure that important aspects of care did not slip through the cracks, whether the system's user interface supported their work flow, and whether the encouragement of nurses was an important factor in their use of the system. Questions that assessed physician attitudes were presented on a 5‐point Likert scale. Nonrespondents were sent reminder letters along with duplicate surveys twice, approximately 1 and 2 months after the initial mailing. No financial incentive was offered for participation. The study protocol was approved by the Institutional Review Board of Baystate Health System.
Order Entry Rates
Regardless of whether an order is placed directly by a physician into a computer, given verbally, or handwritten, all orders are ultimately entered into the CPOE system. Working with our hospitals' Departments of Information Services, we developed a report that provided physician‐specific information about order entry patterns. For each physician in the study, we determined the total number of orders generated during the month preceding the initial June mailing, as well as the absolute number and percentage of orders of each of the following categories: directly entered, telephone, verbal, and written. Because verbal and telephone orders are required during urgent situations and when physicians give orders from outside the hospital, we calculated and report an adjusted order entry rate as the total number of orders placed directly into the system divided by the sum of the orders entered directly and the number of written orders.
Analysis
Summary statistics for the overall sample were constructed using simple frequencies and proportions for categorical variables and medians and interquartile ranges for continuous variables. We compared characteristics of respondents from the 2 hospitals using chi‐square tests of association for categorical factors and Wilcoxon rank‐sum tests for continuous scale data. We compared the total number of orders placed during the study month and the order entry rates of responders and nonresponders using the Wilcoxon rank‐sum test. We categorized physicians as low (20%), intermediate (21%‐79%), and high (80%) users of the system based on their calculated order entry rate. Responses to each of the attitude questions in the survey were tabulated, and the responses strongly agree and agree were combined for analyses comparing responses. Demographic variables and physician attitudes were tested for associations with order entry rate categories via the Pearson chi‐square for categorical factors, the Mantel‐Haenszel chi‐square for ordered factors, and Kruskal‐Wallis analysis of variance for continuous variables. Initial analyses were stratified by hospital; where no differences in association were found across strata, the data were combined. Statistical tests were performed using SAS version 9.1 (SAS Institute, Cary, NC)
RESULTS
During the study period the target group of physicians placed a total of 135,692 orders, of which 69,654 (51%) were placed directly into the CPOE system, 38,878 (29%) were made using pen and paper, 7,208 (5%) were made verbally, and 19,952 (15%) were placed by telephone. Three hundred and fifty‐six (71%) of the 502 surveys sent out to physicians at the 2 hospitals were returned. Thirteen surveys were excluded from analysis because the respondent was not a physician, and 2 because we were unable to match the survey to system usage data, leaving a total of 341 surveys for analysis. Order entry rates were not computed for an additional 3 physicians who only placed verbal and telephone orders during the study period. Response rates did not differ by clinician specialty (P = .53); compared to those of nonresponders, respondents had a similar median total number of orders (111 vs. 101, P = .67) and a higher median order entry rate (66% vs. 48%, P = .03).
Characteristics of Respondents
Seventy‐two percent of physicians who completed the survey were men; half had graduated from medical school at least 20 years ago, and the median duration of practice at the study institution was 11 years (Table 1). Forty percent practiced internal medicine, 18% were surgeons, and 16% were pediatricians. Thirty‐five percent completed training at an institution that had computerized physician order entry, and 86% cared for patients primarily at Baystate Medical Center. More than half reported they used the system many times each day for patient care, and the features they used most commonly were retrieval of results (95%), placing of orders (78%), and viewing and printing of patient lists (75%). Among those with outpatient practices, 81% used computers in their outpatient practice, and more than half used computers for personal activities at home at least once a day. On average, respondents from Franklin Medical Center had graduated from medical school farther in the past and reported less reliance on the system to carry out all activities other than viewing results.
| Overall n (%) | Baystate n (%) 293 (85.9) | Franklin n (%) 48 (14.1) | Chi square P value | |
|---|---|---|---|---|
| ||||
| Sex | .64 | |||
| Male | 244 (71.6) | 211 (72.0) | 33 (68.8) | |
| Specialty | .24 | |||
| Anesthesia | 23 (6.7) | 23 (7.9) | 0 (0.0) | |
| Internal medicine | 135 (39.6) | 112 (38.2) | 23 (47.9) | |
| Medicine/pediatrics | 13 (3.8) | 6 (2.0) | 7 (14.6) | |
| OB/GYN | 36 (10.6) | 30 (10.2) | 6 (12.5) | |
| Pediatrics | 54 (15.8) | 51 (17.4) | 3 (6.3) | |
| Surgery | 61 (17.9) | 55 (18.8) | 6 (12.5) | |
| Other | 19 (5.6) | 16 (5.5) | 3 (6.3) | |
| Use of CPOE systema | .09 | |||
| Many times a day | 176 (52.2) | 160 (55.0) | 16 (34.8) | |
| At least once a day | 77 (22.9) | 61 (21.0) | 16 (34.8) | |
| A few times a week | 55 (16.3) | 45 (15.5) | 10 (21.7) | |
| Once a week or less | 29 (8.6) | 25 (8.6) | 4 (8.7) | |
| Features useda | ||||
| Viewing and printing patient lists | 254 (75.2) | 212 (72.6) | 42 (91.3) | .01 |
| Looking up results | 320 (94.7) | 277 (94.9) | 43 (93.5) | .70 |
| Viewing current medications | 218 (64.5) | 204 (69.9) | 14 (30.4) | < .01 |
| Placing orders | 263 (77.8) | 244 (83.6) | 19 (41.3) | < .01 |
| Entering discharge summaries | 72 (21.3) | 70 (24.0) | 2 (4.4) | < .01 |
| Use of order setsa | ||||
| Rarely or never | 98 (29.0) | 74 (25.3) | 24 (52.2) | < .01 |
| Minority of patients | 92 (27.2) | 78 (26.7) | 14 (30.4) | |
| Majority of patients | 104 (30.8) | 97 (33.2) | 7 (15.2) | |
| For all or nearly all patients | 44 (13.0) | 43 (14.7) | 1 (2.2) | |
| Percentage of orders placed using order setsa | < .01 | |||
| None | 46 (13.7) | 26 (9.0) | 20 (44.4) | |
| 1%‐25% | 62 (18.5) | 50 (17.2) | 12 (26.7) | |
| 26%‐50% | 29 (8.7) | 23 (7.9) | 6 (13.3) | |
| 51%‐75% | 45 (13.4) | 43 (14.9) | 2 (4.4) | |
| 76%‐99% | 103 (30.8) | 98 (33.8) | 5 (11.1) | |
| All | 50 (14.9) | 50 (17.2) | 0 (0.0) | |
| Use of computer in outpatient practiceab | 243 (81.3) | 206 (80.8) | 37 (84.1) | .60 |
| Personal computer usea | .47 | |||
| At least once a day | 209 (61.7) | 185 (63.4) | 24 (51.1) | |
| Several times a week | 84 (24.8) | 67 (23.0) | 17 (36.2) | |
| A few times a month | 21 (6.2) | 18 (6.2) | 3 (6.4) | |
| Rarely | 25 (7.4) | 22 (7.5) | 3 (6.4) | |
| Training at an institution that had CPOE | 117 (34.7) | 105 (36.1) | 12 (26.1) | 0.19 |
| Use of system to enter orders should be mandatorya | ||||
| Yes | 113 (35.2) | 106 (38.4) | 7 (15.6) | <.01 |
| Median (IQR) | Median (IQR) | Median (IQR) | WilcoxonPvalue | |
| Years since medical school graduationa | 20 (13, 26) | 20 (13, 26) | 24 (17, 28) | .02 |
| Years in practice at study institutiona | 11 (5, 18) | 11 (5, 18) | 13 (7, 19) | .39 |
| Orders directly enteredc | 23 (2, 99) | 27 (5, 108) | 1 (0, 27) | < .01 |
| Orders placed by telephonec | 14 (5, 49) | 12 (3, 38) | 49.5 (16, 123.5) | < .01 |
| Orders placed verballyc | 2 (0, 11) | 3 (0, 13) | 1 (0,3) | < .01 |
| Orders placed in writingc | 21 (4, 73) | 14 (3, 45) | 220 (106.5, 391) | < .01 |
| CPOE ratebc | 66% (3%, 94%) | 76% (19%, 96%) | 0.25% (0%, 17%) | < .01 |
Attitudes Toward Computerized Physician Order Entry
Physicians who completed the survey offered diverse opinions about the impact of computerized order entry on work flow, patient safety, and quality of care. Only 22% believed the system's user interface supported their work flow (Q7), 34% believed it was faster to enter orders directly into the system than to handwrite them (Q1), and 41% believed orders placed into the system were carried out more rapidly (Q2) (Table 2). On the other hand, 63% of respondents believed that placing orders directly into the system led to fewer medication errors (Q3), and 51% stated the system generally reduced medical errors (Q4). Sixty‐nine percent stated order sets were important for efficient use of the system (Q5), and 71% believed order sets served an important decision support role (Q6). Twenty‐six percent stated that the encouragement of nurses was an important factor in their use of the system (Q8). Finally, 35% of attending physicians believed use of the system to place orders should be mandatory.
Characteristics and Attitudes of High, Intermediate, and Low Users
The median order entry rate of respondents was 66%. One hundred and forty‐one (42%) placed at least 80% of their orders directly into the system, whereas 109 (32%) placed no more than 20% of their orders directly in the system (Fig. 1). There was not a significant difference between the low, intermediate, and high use groups in the total number of orders that each physician placed during the study period (Table 3). Sex, years since graduation from medical school, years in practice at the study institution, and use of computers in the outpatient setting were not meaningfully different between the 3 categories of users (Table 3). On the other hand, medical specialty was strongly associated with use of the system, with anesthesiologists, pediatricians, and surgeons the specialties with the largest proportion of high users. Furthermore, physicians who were trained in a CPOE environment and those who reported daily use of computers for personal activities showed the highest levels of adoption. Physicians at Franklin Medical Center showed lower levels of order entry than their counterparts at Baystate.
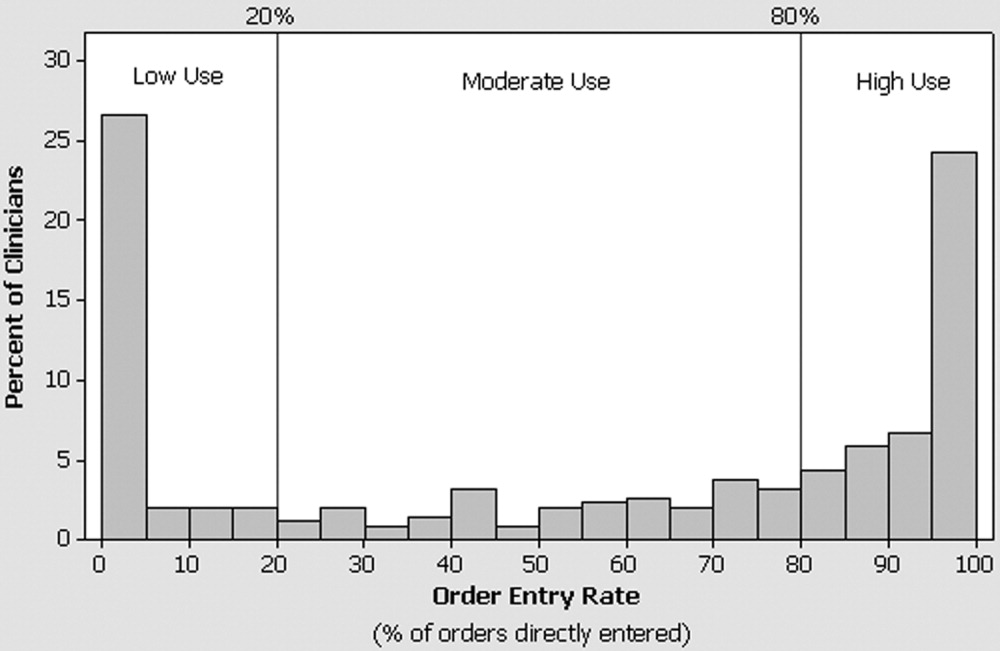
| Low (20%) n (row %) | Intermediate (20%‐79%) n (row %) | High (80%) n (row %) | P value | |
|---|---|---|---|---|
| ||||
| n = 109 | n = 88 | n = 141 | ||
| Hospital | < .01c | |||
| Baystate | 73 (25) | 79 (27) | 138 (48) | |
| Franklin | 36 (75) | 9 (19) | 3 (6) | |
| Sex | .69c | |||
| Female | 28 (29) | 24 (25) | 43 (45) | |
| Male | 81 (33) | 64 (26) | 98 (40) | |
| Specialty | .0001c | |||
| Anesthesia | 8 (35) | 3 (13) | 12 (52) | |
| Internal medicine | 45 (33) | 37 (27) | 53 (39) | |
| Medicine/pediatrics | 6 (46) | 5 (38) | 2 (15) | |
| OB/GYN | 20 (56) | 12 (33) | 4 (11) | |
| Pediatrics | 13 (24) | 9 (17) | 32 (59) | |
| Surgery | 14 (23) | 21 (34) | 26 (43) | |
| Other | 3 (19) | 1 (6) | 12 (75) | |
| Do you use a computer in your outpatient practice?a | ||||
| Yes | 75 (31) | 61 (25) | 105 (44) | .22c |
| No | 20 (36) | 18 (33) | 17 (31) | |
| Level of personal computer useb | .045d | |||
| Rarely | 11 (44) | 8 (32) | 6 (24) | |
| A few times a month | 7 (33) | 4 (19) | 10 (48) | |
| Several times a week | 28 (35) | 25 (31) | 28 (35) | |
| At least once a day | 62 (30) | 50 (24) | 97 (46) | |
| Training at an institution that had CPOE | .037c | |||
| Yes | 30 (26) | 40 (34) | 46 (40) | |
| No | 76 (35) | 48 (22) | 94 (43) | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Years since graduation from medical school | 21 (16, 28) | 18 (14, 25) | 19 (12, 25) | .06e |
| Years in practice at study institution | 12 (5, 19) | 12 (6, 19) | 12 (6, 17) | .84e |
| Total number of orders placed | 112 (45, 306) | 105 (56, 254) | 113 (44, 382) | .92e |
Use of the system was highly associated with physician attitudes toward CPOE, with the views of intermediate and high users consistently different than those of low users (Fig. 2). The associations found held true regardless of hospital: low, intermediate, and high users from Franklin had similar responses to those from Baystate (P > .05 for all questions), and the data from the 2 hospitals therefore were combined for presentation. Although few physicians believed that the user interface of the system supported their work flow, high and intermediate users were 3 times as likely to share this view than were low users (Q7; Fig. 2). Similarly, 19% of low users, 31% of intermediate users, and 45% of high users believed that entering orders into the system was faster than writing orders (Q1). High and intermediate users of the system were more likely than low users to believe that orders entered into the system were carried out more rapidly (Q2) and led to fewer medication (Q3) and nonmedication (Q4) errors. Regardless of their utilization pattern, most physicians believed that order sets played an important role in promoting efficiency and quality.
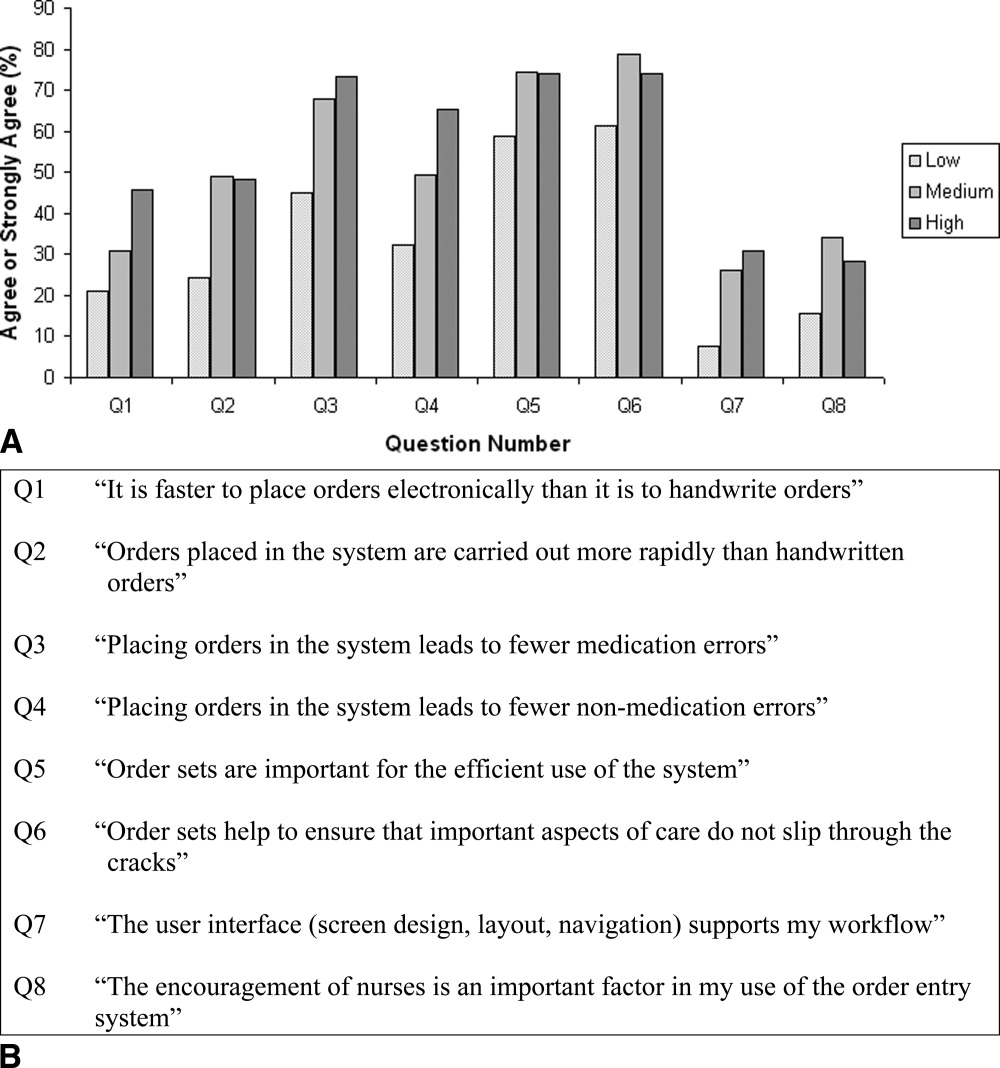
DISCUSSION
In this study of the clinical computing practices of physicians at 2 community hospitals, we observed wide variation in the adoption of CPOE by individual attendings. Although roughly one‐third rarely placed orders directly into the system, 42% had an order entry rate of at least 80%. Contrary to our initial expectation, we found little association between a physician's order entry rate with years in practice, duration of exposure to CPOE, or use of computers in the outpatient setting. On the other hand, we observed marked differences in use of the CPOE system across specialty lines and found that physicians who were exposed to CPOE during training and those who were regular users of computers for personal activities were more likely to embrace this technology. Further, we observed important differences between physicians who used the system to place some or most of their orders and those who did so only rarely in their beliefs and attitudes about the impact and benefits of CPOE. Physicians with higher order entry rates were more likely than their colleagues to believe that placing orders electronically was faster than handwriting and that use of the system led to fewer medical errors. These findings should be encouraging to hospitals hoping to implement CPOE because they suggest that successful adoption of CPOE is not limited to physicians who have just completed their residencies or to hospitals with the capability of designing and building their own systems. On the contrary, we documented that women, older physicians, and those with limited CPOE experience were as likely to be frequent users, especially if they perceived CPOE to be safer than handwriting and if they believed the user interface supported the efficient entering of orders.
On the basis of these results we recommend that in addition to purchasing systems that meet physician work‐flow needs and support the efficient entry of orders, hospital leaders should emphasize the quality and safety benefits of CPOE as part of a comprehensive change management strategy. The differences we observed in order entry rates across specialties may have resulted from several factors, including inherent differences in personality type associated with choice of specialty and in the level of customization of a system reflected in which and how many order sets are included. Such findings suggest that when it comes to CPOE, one size does not fit all, and implementation planning should be carried out at the specialty level. Finally, our observation that physicians who had exposure to CPOE during training were more likely to use the system to place orders suggests that the nation's training institutions will play an important role in fostering universal adoption of this technology.
Several earlier studies have reported on physician experiences with CPOE systems. Murff and Kannry12 surveyed 94 internal medicine house staff to compare experiences with 2 CPOE systems: the Department of Veterans Affairs Computerized Patient Record System (CPRS) and a commercially available product. They found striking differences in user satisfaction with numerous aspects of the systems, however they did not address attitudes toward safety or quality, and because house staff were required to place orders electronically they were unable to correlate responses with actual usage patterns. Weiner et al.13 compared the opinions of internal medicine house staff, attendings, fellows, and nurses about the benefits and challenges of using a computerized provider order entry system. In contrast to the findings from our study, Weiner et al. reported that more than half of physicians believed that provider order entry led to a greater number of errors, and only a minority believed the system increased quality of care overall. Finally, Lee et al.14 surveyed medical and surgical house officers and nurses at a large academic medical center about their satisfaction with a locally developed order entry system. They found that attitudes about the impact of the system on productivity and ease of use were more strongly associated with overall satisfaction than having undergone training or experience with personal computers. These findings are congruous with our own observation that beliefs about the speed with which orders are placed are closely associated with actual use of the system. They reported, as have we, that physicians placed a high value on order sets.
Our study had a number of strengths. First, we were able to offer insight into the attitudes and behaviors of a previously neglected, but critically important groupattending physicians who care for patients at community hospitals without the assistance of house staff. Second, whereas previous studies primarily assessed physician satisfaction with CPOE, we explored how physician attitudes about the impact of CPOE on work flow and on safety were associated with actual ordering habits. Information about ordering was obtained directly from the order entry system and not through self‐report. We conducted the study at 2 hospitals, a large urban community teaching hospital and a smaller rural hospital, and focused on a CPOE system that is in use at many institutions throughout the country, thereby increasing the generalizability of our findings. Although adoption of the system by physicians at the 2 hospitals differed, factors that associated with the use of CPOE to place orders were similar. Finally, we surveyed a large number of physicians, had a high response rate, and found only small differences in the utilization patterns of responders and nonresponders, suggesting that our portrayal of the attitudes of physicians was representative of the views of physicians practicing in our community.
The study had a number of weaknesses. First, we cannot be sure whether preexisting beliefs about the benefits of CPOE directly influenced physicians' use of the system or, conversely, if these attitudes developed in response to experience as users. Nevertheless, it seems practical to suggest that hospitals focus on purchasing systems that support the efficient entering of orders while simultaneously adopting a communication and change management strategy that emphasizes the safety and quality benefits of CPOE more broadly. Second, we did not attempt to validate the opinions expressed by physicians about the usability or safety benefits of the system. That said, the purpose of the study was to determine whether physician attitudes toward these issues was associated with the use of the system to place orders. Whether or not this particular CPOE system actually prevented medication errors, most physicians believed it did, a belief strongly associated with the observed order entry rates. Third, we studied a single CPOE system implemented approximately 10 years ago that does not reflect state‐of‐the‐art user interface design or functionality. Nevertheless, our observation about the importance of the user experience is probably no less relevant today. Fourth, we were unable to ascertain every order given by physicians, as some so‐called MD to RN orders may never have made it into the system. Finally, there is a small risk that some written, telephone, and verbal orders may have been randomly or systematically assigned to incorrect physicians, which would have led us to calculate inaccurate utilization rates.
CONCLUSIONS
In a voluntary community hospital environment the adoption of CPOE by attending physicians varies widely. While placing a premium on the purchase of systems that meet the work‐flow needs of physicians and support the efficient entry of orders, hospital leaders can enhance physician adoption of this technology by communicating the role of CPOE in improving quality and safety.
Acknowledgements
The authors thank Gilad Kuperman, MD, PhD, for his thoughtful comments on an earlier version of the manuscript.
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press,2000.
- ,.Computer physician order entry: benefits, costs, and issues.Ann Intern Med.2003;139:31–39.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,,,,.A computerized reminder system to increase the use of preventive care for hospitalized patients.N Engl J Med.2001;345:965–970.
- ,,,.A randomized trial of “corollary orders” to prevent errors of omission.J Am Med Inform Assoc.1997;4:364–375.
- ,,, et al.A computer‐assisted management program for antibiotics and other antiinfective agents.N Engl J Med.1998;338:232–238.
- The Leapfrog Group. Patient Safety Fact Sheet. Available at: http://www.leapfroggroup.org/FactSheets/LF_FactSheet.pdf. Accessed October 6,2004.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,.U.S. adoption of computerized physician order entry systems.Health Aff.2005;24:1654–1663.
- ,,.Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review.Arch Intern Med.2003;163:1409–1416.
- HCUPnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 6,2004.
- ,.Physician satisfaction with two order entry systems.J Am Med Inform Assoc.2001;8:499–509.
- ,,, et al.Contrasting views of physicians and nurses about an inpatient computer‐based provider order‐entry system.J Am Med Inform Assoc.1999;6:234–244.
- ,,,.Implementation of physician order entry: user satisfaction and self‐reported usage patterns.J Am Med Inform Assoc.1996;3:42–55.
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press,2000.
- ,.Computer physician order entry: benefits, costs, and issues.Ann Intern Med.2003;139:31–39.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,,,,.A computerized reminder system to increase the use of preventive care for hospitalized patients.N Engl J Med.2001;345:965–970.
- ,,,.A randomized trial of “corollary orders” to prevent errors of omission.J Am Med Inform Assoc.1997;4:364–375.
- ,,, et al.A computer‐assisted management program for antibiotics and other antiinfective agents.N Engl J Med.1998;338:232–238.
- The Leapfrog Group. Patient Safety Fact Sheet. Available at: http://www.leapfroggroup.org/FactSheets/LF_FactSheet.pdf. Accessed October 6,2004.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,.U.S. adoption of computerized physician order entry systems.Health Aff.2005;24:1654–1663.
- ,,.Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review.Arch Intern Med.2003;163:1409–1416.
- HCUPnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/data/hcup/hcupnet.htm. Accessed October 6,2004.
- ,.Physician satisfaction with two order entry systems.J Am Med Inform Assoc.2001;8:499–509.
- ,,, et al.Contrasting views of physicians and nurses about an inpatient computer‐based provider order‐entry system.J Am Med Inform Assoc.1999;6:234–244.
- ,,,.Implementation of physician order entry: user satisfaction and self‐reported usage patterns.J Am Med Inform Assoc.1996;3:42–55.
Copyright © 2006 Society of Hospital Medicine
Editorial
Despite the widespread availability of potent anti-infective agents, infectious diseases remain formidable and common problems in hospitalized patients. In this issue of The Hospitalist, hospitalists and infectious disease specialists provide state-of-the-art reviews of common infectious disease syndromes encountered in hospital medicine. This should be required reading for hospitalists, given the severity of illness of many patients with these syndromes, and the rapidly evolving developments in optimal diagnosis and management in many of these areas.
Hospitalists and infectious disease practitioners share similar challenges and should be natural allies in improving patient care. To name a few, these challenges include the prompt recognition and management of new and emerging infectious diseases; the rising incidence of drug-resistant pathogens; the prevention, prompt recognition, and effective management of nosocomial and opportunistic infections in hospitalized patients, including outbreaks; the implementation of clinical practice guidelines for common infectious disease problems; and the vaccination of high-risk hospitalized patients.
New and emerging infectious diseases have been recognized with increasing frequency, and hospitalists are among those physicians most likely to encounter them. In the past two years alone, these have included SARS (1), monkeypox (2), tanapox (3), and American Boutonneuse fever (4). Drug-resistant pathogens have become increasingly common. Methicillin-resistant Staphylococcus aureus (MRSA) now accounts for more than 50% of Staphylococcus aureus isolates in many hospitals. Until recently, MRSA has afflicted mainly hospitalized patients or those with significant underlying comorbidities. Recent reports, however, have described MRSA in previously healthy patients admitted from the community (5,6) Even more ominously, isolates of Staphylococcus aureus with intermediate or high-level resistance to vancomycin have been reported (7,8).
Drug-resistant Streptococcus pneumoniae is common in many parts of the United States; many isolates are resistant to multiple common antibiotics, and fluoroquinolone resistance, though still uncommon, has been reported (9,10). Vancomycin-resistant enterococci have emerged over the past decade and now account for up to 15% of enterococcal isolates in many centers. Macrolide-resistance in Treponema pallidum was recently described (11). The emergence of drug-resistant pathogens has important implications for hospitalists, who are typically at the front line in choosing empiric or pathogen-specific antimicrobial therapy for hospitalized patients. Knowledge about local trends in antimicrobial resistance is essential for making informed antibiotic selections, and prevention of spread of these organisms within hospitals is crucial.
How have hospitalists partnered with infectious disease specialists in tackling these problems? Surprisingly, very little has been written. In our review of the literature we were able to identify only 3 studies addressing the role of hospitalists and infectious disease physicians in the management of infectious diseases (12-14). Reddy et al. compared the impact of a clinical practice guideline introduced at the University of California San Francisco Moffitt-Long Hospital in 1996 with that of a hospitalist-based reorganization of their medical service in the management of patients with community-acquired pneumonia (CAP) (12). Following implementation of the guideline, average cost per case and length of stay declined similarly among patients cared for by hospitalists versus those cared for by attending physicians on the traditional medical service. Mortality remained unchanged despite shorter length of stay, and readmission rates fell. However, hospitalists achieved statistically greater reductions in cost per case and length of stay for all other diagnoses compared with their traditional attending counterparts. This study therefore concluded that the implementation of a clinical practice guideline was the key driver in improving resource utilization in hospitalized patients with CAP, rather than physician model of care.
In a similar study, Rifkin et al. compared outcomes and resource utilization in hospitalized patients with CAP at Long Island Jewish Medical Center cared for by hospitalists (185 patients) versus primary care physicians (270 patients) (13). No local clinical practice guideline was in place, although appropriateness of therapy was evaluated based upon guidelines disseminated by the American Thoracic Society and the Infectious Disease Society of America at the time. Compared with hospitalists, primary care physicians obtained more subspecialty consultations and administered antibiotics in a more timely fashion. Nevertheless, hospitalist care was associated with shorter length of stay, lower cost per case, more rapid transition from parenteral to oral antibiotic therapy, and improved survival. Hospitalist patients were more likely to be discharged with an unstable vital sign, but 15- and 30-day readmission rates were similar to patients cared for by primary care physicians. This study implies that, absent an enforced clinical practice guideline, hospitalist care of patients with CAP is associated with decreased resource utilization and better outcome.
Finally, in a case-control study, Eron and Passos examined the performance of hospitalists versus infectious disease consultants in the care of hospitalized patients with CAP, cellulitis, or pyelonephritis (14). One hundred eleven patients cared for by infectious disease consultants were compared with 112 historical controls cared for by hospitalists. Patients receiving care from infectious disease specialists had higher patient satisfaction, shorter length of stay, no readmissions, and more rapid return to activities of daily living. The benefits of specialty care were attributable to more frequent use of early outpatient parenteral antibiotic therapy (OPAT) in patients with cellulitis and more rapid switching from parenteral to oral therapy in patients with pyelonephritis and CAP by infectious disease specialists compared with hospitalists. This study has several implications. First, selected inpatients may benefit from early infectious disease consultation. And second, hospitalists may be able to learn from their subspecialty colleagues about the safety and efficacy of early switch therapy and OPAT in selected patient populations.
These limited data suggest that patients with selected infectious diseases may benefit from care provided by hospitalists and infectious disease specialists and that such care is associated with better outcomes and decreased resource utilization. No studies have examined what we believe to be the true potential for improved patient care through the partnership of these 2 disciplines working in collaboration. In the absence of data, we offer several suggestions for areas of fruitful collaboration and further study. First, with the increasing incidence of drug-resistant pathogens and the increasing severity of illness of hospitalized patients with infectious diseases, hospitalists and infectious disease specialists can work together to ensure optimal use of empiric and pathogen-specific antimicrobial therapy and the development and implementation of evidence-based practice guidelines. Second, early infectious disease consultation should be strongly considered in critically ill patients, in those with suspected or confirmed drug-resistant pathogens, and in those with unusual or complicated infectious disease problems. Third, hospitalists, in collaboration with infectious disease specialists, can and should help to improve basic infection control practices, such as hand hygiene and the appropriate use of indwelling devices such as Foley catheters and vascular access devices, which predispose to nosocomial infection. Fourth, hospitalists can facilitate the appropriate immunization of at-risk hospitalized patients against influenza and S. pneumoniae. Finally, hospitalists can partner with their infectious disease colleagues to optimize the use of OPAT and early switch therapy in patients with selected infectious diseases so as to maximize outcome while at the same time reducing hospital length of stay and resource utilization.
In a demonstration project, the Center for Medicare and Medicaid Services has now linked quality measures to reimbursement in several areas of infectious diseases. These include timeliness of antibiotic administration in patients with CAP, blood culture collection prior to antibiotic therapy in patients with CAP, and screening and administering influenza and pneumococcal immunizations to at-risk patients. This trend of linking reimbursement to performance in infectious disease management and prevention is likely to continue.
There are therefore many reasons to encourage partnership and collaboration between these disciplines. These include better quality of care, improved resource utilization, and, hopefully, better reimbursement for hospitals. Through leadership, teamwork, and a multidisciplinary approach, hospitalists and infectious disease physicians should together drive change to realize these goals.
References
- Pieris JSM, Lai ST, Poon LLM, et al. Coronavirus as a cause of severe acute respiratory syndrome. Lancet. 2003;361:1319-25.
- Reed KD, Melski JW, Graham MB, et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med. 2004;350:342-50.
- Dhar AD, Werchniak AE, Li Y, et al. Tanapox infection in a college student. N Engl J Med. 2004;350;361-6.
- Paddock CD, Sumner JW, Comer JA, et al. Rickettsia parkeri: a newly recognized cause of spotted fever rickettsiosis in the United States. Clin Infect Dis. 2004;38: 805-11.
- Fridkin SK., Hageman JC, Morrison M, et al. Methicillin resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-44.
- Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med. 2005;352:1445-53.
- Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004;39:539-45.
- Whitener CJ, Park SY, Browne FA, et al. Vancomycin resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin Infect Dis. 2004;38:1049-55.
- Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343: 1917-24.
- Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-50.
- Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004;351:154-8.
- Reddy JC, Katz PP, Goldman L, Wachter RM. A pneumonia practice guideline and a hospitalist-based reorganization lead to equivalent efficiency gains. Am J Manag Care. 2001;7:1142-8.
- Rifkin WD, Connor D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Eron LJ, Passos S: Early discharge of infected patients through appropriate antibiotic use. Arch Intern Med. 2001;161:61-5.
Despite the widespread availability of potent anti-infective agents, infectious diseases remain formidable and common problems in hospitalized patients. In this issue of The Hospitalist, hospitalists and infectious disease specialists provide state-of-the-art reviews of common infectious disease syndromes encountered in hospital medicine. This should be required reading for hospitalists, given the severity of illness of many patients with these syndromes, and the rapidly evolving developments in optimal diagnosis and management in many of these areas.
Hospitalists and infectious disease practitioners share similar challenges and should be natural allies in improving patient care. To name a few, these challenges include the prompt recognition and management of new and emerging infectious diseases; the rising incidence of drug-resistant pathogens; the prevention, prompt recognition, and effective management of nosocomial and opportunistic infections in hospitalized patients, including outbreaks; the implementation of clinical practice guidelines for common infectious disease problems; and the vaccination of high-risk hospitalized patients.
New and emerging infectious diseases have been recognized with increasing frequency, and hospitalists are among those physicians most likely to encounter them. In the past two years alone, these have included SARS (1), monkeypox (2), tanapox (3), and American Boutonneuse fever (4). Drug-resistant pathogens have become increasingly common. Methicillin-resistant Staphylococcus aureus (MRSA) now accounts for more than 50% of Staphylococcus aureus isolates in many hospitals. Until recently, MRSA has afflicted mainly hospitalized patients or those with significant underlying comorbidities. Recent reports, however, have described MRSA in previously healthy patients admitted from the community (5,6) Even more ominously, isolates of Staphylococcus aureus with intermediate or high-level resistance to vancomycin have been reported (7,8).
Drug-resistant Streptococcus pneumoniae is common in many parts of the United States; many isolates are resistant to multiple common antibiotics, and fluoroquinolone resistance, though still uncommon, has been reported (9,10). Vancomycin-resistant enterococci have emerged over the past decade and now account for up to 15% of enterococcal isolates in many centers. Macrolide-resistance in Treponema pallidum was recently described (11). The emergence of drug-resistant pathogens has important implications for hospitalists, who are typically at the front line in choosing empiric or pathogen-specific antimicrobial therapy for hospitalized patients. Knowledge about local trends in antimicrobial resistance is essential for making informed antibiotic selections, and prevention of spread of these organisms within hospitals is crucial.
How have hospitalists partnered with infectious disease specialists in tackling these problems? Surprisingly, very little has been written. In our review of the literature we were able to identify only 3 studies addressing the role of hospitalists and infectious disease physicians in the management of infectious diseases (12-14). Reddy et al. compared the impact of a clinical practice guideline introduced at the University of California San Francisco Moffitt-Long Hospital in 1996 with that of a hospitalist-based reorganization of their medical service in the management of patients with community-acquired pneumonia (CAP) (12). Following implementation of the guideline, average cost per case and length of stay declined similarly among patients cared for by hospitalists versus those cared for by attending physicians on the traditional medical service. Mortality remained unchanged despite shorter length of stay, and readmission rates fell. However, hospitalists achieved statistically greater reductions in cost per case and length of stay for all other diagnoses compared with their traditional attending counterparts. This study therefore concluded that the implementation of a clinical practice guideline was the key driver in improving resource utilization in hospitalized patients with CAP, rather than physician model of care.
In a similar study, Rifkin et al. compared outcomes and resource utilization in hospitalized patients with CAP at Long Island Jewish Medical Center cared for by hospitalists (185 patients) versus primary care physicians (270 patients) (13). No local clinical practice guideline was in place, although appropriateness of therapy was evaluated based upon guidelines disseminated by the American Thoracic Society and the Infectious Disease Society of America at the time. Compared with hospitalists, primary care physicians obtained more subspecialty consultations and administered antibiotics in a more timely fashion. Nevertheless, hospitalist care was associated with shorter length of stay, lower cost per case, more rapid transition from parenteral to oral antibiotic therapy, and improved survival. Hospitalist patients were more likely to be discharged with an unstable vital sign, but 15- and 30-day readmission rates were similar to patients cared for by primary care physicians. This study implies that, absent an enforced clinical practice guideline, hospitalist care of patients with CAP is associated with decreased resource utilization and better outcome.
Finally, in a case-control study, Eron and Passos examined the performance of hospitalists versus infectious disease consultants in the care of hospitalized patients with CAP, cellulitis, or pyelonephritis (14). One hundred eleven patients cared for by infectious disease consultants were compared with 112 historical controls cared for by hospitalists. Patients receiving care from infectious disease specialists had higher patient satisfaction, shorter length of stay, no readmissions, and more rapid return to activities of daily living. The benefits of specialty care were attributable to more frequent use of early outpatient parenteral antibiotic therapy (OPAT) in patients with cellulitis and more rapid switching from parenteral to oral therapy in patients with pyelonephritis and CAP by infectious disease specialists compared with hospitalists. This study has several implications. First, selected inpatients may benefit from early infectious disease consultation. And second, hospitalists may be able to learn from their subspecialty colleagues about the safety and efficacy of early switch therapy and OPAT in selected patient populations.
These limited data suggest that patients with selected infectious diseases may benefit from care provided by hospitalists and infectious disease specialists and that such care is associated with better outcomes and decreased resource utilization. No studies have examined what we believe to be the true potential for improved patient care through the partnership of these 2 disciplines working in collaboration. In the absence of data, we offer several suggestions for areas of fruitful collaboration and further study. First, with the increasing incidence of drug-resistant pathogens and the increasing severity of illness of hospitalized patients with infectious diseases, hospitalists and infectious disease specialists can work together to ensure optimal use of empiric and pathogen-specific antimicrobial therapy and the development and implementation of evidence-based practice guidelines. Second, early infectious disease consultation should be strongly considered in critically ill patients, in those with suspected or confirmed drug-resistant pathogens, and in those with unusual or complicated infectious disease problems. Third, hospitalists, in collaboration with infectious disease specialists, can and should help to improve basic infection control practices, such as hand hygiene and the appropriate use of indwelling devices such as Foley catheters and vascular access devices, which predispose to nosocomial infection. Fourth, hospitalists can facilitate the appropriate immunization of at-risk hospitalized patients against influenza and S. pneumoniae. Finally, hospitalists can partner with their infectious disease colleagues to optimize the use of OPAT and early switch therapy in patients with selected infectious diseases so as to maximize outcome while at the same time reducing hospital length of stay and resource utilization.
In a demonstration project, the Center for Medicare and Medicaid Services has now linked quality measures to reimbursement in several areas of infectious diseases. These include timeliness of antibiotic administration in patients with CAP, blood culture collection prior to antibiotic therapy in patients with CAP, and screening and administering influenza and pneumococcal immunizations to at-risk patients. This trend of linking reimbursement to performance in infectious disease management and prevention is likely to continue.
There are therefore many reasons to encourage partnership and collaboration between these disciplines. These include better quality of care, improved resource utilization, and, hopefully, better reimbursement for hospitals. Through leadership, teamwork, and a multidisciplinary approach, hospitalists and infectious disease physicians should together drive change to realize these goals.
References
- Pieris JSM, Lai ST, Poon LLM, et al. Coronavirus as a cause of severe acute respiratory syndrome. Lancet. 2003;361:1319-25.
- Reed KD, Melski JW, Graham MB, et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med. 2004;350:342-50.
- Dhar AD, Werchniak AE, Li Y, et al. Tanapox infection in a college student. N Engl J Med. 2004;350;361-6.
- Paddock CD, Sumner JW, Comer JA, et al. Rickettsia parkeri: a newly recognized cause of spotted fever rickettsiosis in the United States. Clin Infect Dis. 2004;38: 805-11.
- Fridkin SK., Hageman JC, Morrison M, et al. Methicillin resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-44.
- Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med. 2005;352:1445-53.
- Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004;39:539-45.
- Whitener CJ, Park SY, Browne FA, et al. Vancomycin resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin Infect Dis. 2004;38:1049-55.
- Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343: 1917-24.
- Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-50.
- Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004;351:154-8.
- Reddy JC, Katz PP, Goldman L, Wachter RM. A pneumonia practice guideline and a hospitalist-based reorganization lead to equivalent efficiency gains. Am J Manag Care. 2001;7:1142-8.
- Rifkin WD, Connor D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Eron LJ, Passos S: Early discharge of infected patients through appropriate antibiotic use. Arch Intern Med. 2001;161:61-5.
Despite the widespread availability of potent anti-infective agents, infectious diseases remain formidable and common problems in hospitalized patients. In this issue of The Hospitalist, hospitalists and infectious disease specialists provide state-of-the-art reviews of common infectious disease syndromes encountered in hospital medicine. This should be required reading for hospitalists, given the severity of illness of many patients with these syndromes, and the rapidly evolving developments in optimal diagnosis and management in many of these areas.
Hospitalists and infectious disease practitioners share similar challenges and should be natural allies in improving patient care. To name a few, these challenges include the prompt recognition and management of new and emerging infectious diseases; the rising incidence of drug-resistant pathogens; the prevention, prompt recognition, and effective management of nosocomial and opportunistic infections in hospitalized patients, including outbreaks; the implementation of clinical practice guidelines for common infectious disease problems; and the vaccination of high-risk hospitalized patients.
New and emerging infectious diseases have been recognized with increasing frequency, and hospitalists are among those physicians most likely to encounter them. In the past two years alone, these have included SARS (1), monkeypox (2), tanapox (3), and American Boutonneuse fever (4). Drug-resistant pathogens have become increasingly common. Methicillin-resistant Staphylococcus aureus (MRSA) now accounts for more than 50% of Staphylococcus aureus isolates in many hospitals. Until recently, MRSA has afflicted mainly hospitalized patients or those with significant underlying comorbidities. Recent reports, however, have described MRSA in previously healthy patients admitted from the community (5,6) Even more ominously, isolates of Staphylococcus aureus with intermediate or high-level resistance to vancomycin have been reported (7,8).
Drug-resistant Streptococcus pneumoniae is common in many parts of the United States; many isolates are resistant to multiple common antibiotics, and fluoroquinolone resistance, though still uncommon, has been reported (9,10). Vancomycin-resistant enterococci have emerged over the past decade and now account for up to 15% of enterococcal isolates in many centers. Macrolide-resistance in Treponema pallidum was recently described (11). The emergence of drug-resistant pathogens has important implications for hospitalists, who are typically at the front line in choosing empiric or pathogen-specific antimicrobial therapy for hospitalized patients. Knowledge about local trends in antimicrobial resistance is essential for making informed antibiotic selections, and prevention of spread of these organisms within hospitals is crucial.
How have hospitalists partnered with infectious disease specialists in tackling these problems? Surprisingly, very little has been written. In our review of the literature we were able to identify only 3 studies addressing the role of hospitalists and infectious disease physicians in the management of infectious diseases (12-14). Reddy et al. compared the impact of a clinical practice guideline introduced at the University of California San Francisco Moffitt-Long Hospital in 1996 with that of a hospitalist-based reorganization of their medical service in the management of patients with community-acquired pneumonia (CAP) (12). Following implementation of the guideline, average cost per case and length of stay declined similarly among patients cared for by hospitalists versus those cared for by attending physicians on the traditional medical service. Mortality remained unchanged despite shorter length of stay, and readmission rates fell. However, hospitalists achieved statistically greater reductions in cost per case and length of stay for all other diagnoses compared with their traditional attending counterparts. This study therefore concluded that the implementation of a clinical practice guideline was the key driver in improving resource utilization in hospitalized patients with CAP, rather than physician model of care.
In a similar study, Rifkin et al. compared outcomes and resource utilization in hospitalized patients with CAP at Long Island Jewish Medical Center cared for by hospitalists (185 patients) versus primary care physicians (270 patients) (13). No local clinical practice guideline was in place, although appropriateness of therapy was evaluated based upon guidelines disseminated by the American Thoracic Society and the Infectious Disease Society of America at the time. Compared with hospitalists, primary care physicians obtained more subspecialty consultations and administered antibiotics in a more timely fashion. Nevertheless, hospitalist care was associated with shorter length of stay, lower cost per case, more rapid transition from parenteral to oral antibiotic therapy, and improved survival. Hospitalist patients were more likely to be discharged with an unstable vital sign, but 15- and 30-day readmission rates were similar to patients cared for by primary care physicians. This study implies that, absent an enforced clinical practice guideline, hospitalist care of patients with CAP is associated with decreased resource utilization and better outcome.
Finally, in a case-control study, Eron and Passos examined the performance of hospitalists versus infectious disease consultants in the care of hospitalized patients with CAP, cellulitis, or pyelonephritis (14). One hundred eleven patients cared for by infectious disease consultants were compared with 112 historical controls cared for by hospitalists. Patients receiving care from infectious disease specialists had higher patient satisfaction, shorter length of stay, no readmissions, and more rapid return to activities of daily living. The benefits of specialty care were attributable to more frequent use of early outpatient parenteral antibiotic therapy (OPAT) in patients with cellulitis and more rapid switching from parenteral to oral therapy in patients with pyelonephritis and CAP by infectious disease specialists compared with hospitalists. This study has several implications. First, selected inpatients may benefit from early infectious disease consultation. And second, hospitalists may be able to learn from their subspecialty colleagues about the safety and efficacy of early switch therapy and OPAT in selected patient populations.
These limited data suggest that patients with selected infectious diseases may benefit from care provided by hospitalists and infectious disease specialists and that such care is associated with better outcomes and decreased resource utilization. No studies have examined what we believe to be the true potential for improved patient care through the partnership of these 2 disciplines working in collaboration. In the absence of data, we offer several suggestions for areas of fruitful collaboration and further study. First, with the increasing incidence of drug-resistant pathogens and the increasing severity of illness of hospitalized patients with infectious diseases, hospitalists and infectious disease specialists can work together to ensure optimal use of empiric and pathogen-specific antimicrobial therapy and the development and implementation of evidence-based practice guidelines. Second, early infectious disease consultation should be strongly considered in critically ill patients, in those with suspected or confirmed drug-resistant pathogens, and in those with unusual or complicated infectious disease problems. Third, hospitalists, in collaboration with infectious disease specialists, can and should help to improve basic infection control practices, such as hand hygiene and the appropriate use of indwelling devices such as Foley catheters and vascular access devices, which predispose to nosocomial infection. Fourth, hospitalists can facilitate the appropriate immunization of at-risk hospitalized patients against influenza and S. pneumoniae. Finally, hospitalists can partner with their infectious disease colleagues to optimize the use of OPAT and early switch therapy in patients with selected infectious diseases so as to maximize outcome while at the same time reducing hospital length of stay and resource utilization.
In a demonstration project, the Center for Medicare and Medicaid Services has now linked quality measures to reimbursement in several areas of infectious diseases. These include timeliness of antibiotic administration in patients with CAP, blood culture collection prior to antibiotic therapy in patients with CAP, and screening and administering influenza and pneumococcal immunizations to at-risk patients. This trend of linking reimbursement to performance in infectious disease management and prevention is likely to continue.
There are therefore many reasons to encourage partnership and collaboration between these disciplines. These include better quality of care, improved resource utilization, and, hopefully, better reimbursement for hospitals. Through leadership, teamwork, and a multidisciplinary approach, hospitalists and infectious disease physicians should together drive change to realize these goals.
References
- Pieris JSM, Lai ST, Poon LLM, et al. Coronavirus as a cause of severe acute respiratory syndrome. Lancet. 2003;361:1319-25.
- Reed KD, Melski JW, Graham MB, et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med. 2004;350:342-50.
- Dhar AD, Werchniak AE, Li Y, et al. Tanapox infection in a college student. N Engl J Med. 2004;350;361-6.
- Paddock CD, Sumner JW, Comer JA, et al. Rickettsia parkeri: a newly recognized cause of spotted fever rickettsiosis in the United States. Clin Infect Dis. 2004;38: 805-11.
- Fridkin SK., Hageman JC, Morrison M, et al. Methicillin resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-44.
- Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med. 2005;352:1445-53.
- Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004;39:539-45.
- Whitener CJ, Park SY, Browne FA, et al. Vancomycin resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin Infect Dis. 2004;38:1049-55.
- Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343: 1917-24.
- Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-50.
- Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004;351:154-8.
- Reddy JC, Katz PP, Goldman L, Wachter RM. A pneumonia practice guideline and a hospitalist-based reorganization lead to equivalent efficiency gains. Am J Manag Care. 2001;7:1142-8.
- Rifkin WD, Connor D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Eron LJ, Passos S: Early discharge of infected patients through appropriate antibiotic use. Arch Intern Med. 2001;161:61-5.
Other Literature of Interest
1. Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 352:1305-16.
This is the first prospective study comparing antithrombotic therapies for patients with atherosclerotic stenosis of major intracranial arteries. This multicenter, NINDS-sponsored, placebo-controlled, blinded study randomized 569 patients to aspirin (650 mg twice daily) or warfarin (initially 5 mg daily, titrated to achieve an INR of 2.0–3.0) and followed them for nearly 2 years. The study was terminated early over safely concerns about patients in the warfarin group. Baseline characteristics between the 2 groups were not significantly different. Warfarin was not more effective than aspirin in its effect on the primary endpoints of ischemic stroke, brain hemorrhage, or vascular death other than from stroke (as defined in the study protocol). However, major cardiac events (myocardial infarction or sudden death) were significantly higher in the warfarin group, and major hemorrhage (defined as any intracranial or systemic hemorrhage requiring hospitalization, transfusion, or surgical intervention) was also significantly higher in the warfarin group. The authors note the difficulty maintaining the INR in the target range (achieved only 63.1 % of the time during the maintenance period, an observation in line with other anticoagulation studies). In an accompanying editorial, Dr. Koroshetz of the stroke service at the Massachusetts General Hospital also observed that difficulties in achieving the therapeutic goal with warfarin could have impacted the results. The authors also note that the dose of aspirin employed in this study is somewhat higher than in previous trials. Nevertheless, until other data emerge, this investigation’s results favor aspirin in preference to warfarin for this high-risk condition.
2. Cornish PL, Knowles, SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission Arch Intern Med. 2005;165:424-9
Of the various types of medical errors, medication errors are believed to be the most common. At the time of hospital admission, medication discrepancies may lead to unintended drug interactions, toxicity, or interruption of appropriate drug therapies. These investigators performed a prospective study to identify unintended medication discrepancies between the patient’s home medications and those ordered at the time of the patient’s admission and to evaluate the potential clinical significance of these discrepancies.
This study was conducted at a 1,000-bed tertiary care hospital in Canada on the general medicine teaching service. A member of the study team reviewed each medical record to ascertain the physician-recorded medication history, the nurse-recorded medication history, the admission medication orders, and demographic information. A comprehensive list of all of the patient’s prescription or nonprescription drugs was compiled by interviewing patients, families, and pharmacists, and by inspecting the bottles. A discrepancy was defined as any difference between this comprehensive list and the admission medication orders. These were categorized into omission or addition of a medication, substitution of an agent within the same drug class, and change in dose, route, and frequency of administration of an agent. The medical team caring for the patient was then asked whether or not these discrepancies were intended. The team then reconciled any unintended discrepancies. These unintended discrepancies were further classified according to their potential for harm by 3 medical hospitalists into Class 1, 2, 3, in increasing order of potential harm. One hundred fifty-one patients were included in the analysis. A total of 140 errors occurred in 81 patients (54%). The overall error rate was 0.93 per patient. Of the errors, 46% consisted of omission of a regularly prescribed medication, 25% involved discrepant doses, 17.1% involved discrepant frequency, and 11.4% were actually incorrect drugs. Breakdown of error severity resulted in designation of 61% as Class 1, 33% as Class 2, and 5.7% as Class 3. The interrater agreement was a kappa of 0.26. These discrepancies were not found to be associated with night or weekend admissions, high patient volume, or high numbers of medications.
Real-time clinical correlation with the responsible physicians allowed distinction of intended from unintended discrepancies. This presumably improved the accuracy of the error rate measurement. This study confirmed the relatively high rate previously reported. Further study can focus on possible intervention to minimize these errors.
3. Liperoti R, Gambassi G, Lapane KL, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest Arch Intern Med. 2005;165:696-701.
As the number of hospitalized elderly and demented patients increases, use of both typical and atypical antipsychotics has become prevalent. QT prolongation, ventricular arrhythmia, and cardiac arrest are more commonly associated with the older conventional antipsychotics than with newer atypical agents. This case-control study was conducted to estimate the effect of both conventional and atypical antipsychotics use on the risk of hospital admission for ventricular arrhythmia or cardiac arrest.
The patient population involved consisted of elderly nursing home residents in 6 US states. The investigators utilized Systematic Assessment of Geriatric Drug Use via Epidemiology database that contains data from minimum data set (MDS), a standardized data set required of all certified nursing homes in the United States. Case patients were selected by ICD-9 codes for cardiac arrest or ventricular arrhythmia. Control patients were selected via ICD-9 codes of 6 other common inpatient diagnoses. Antipsychotic exposure was determined by use of the most recent assessment in the nursing homes prior to admission. Exposed patients were those who received atypical antipsychotics such as risperidone, olanzapine, quetiapine, and clozapine, and those who used conventional agents such as haloperidol and others. After control for potential confounders, users of conventional antipsychotics showed an 86% increase in the risk of hospitalization for ventricular arrhythmias or cardiac arrest (OR: 1.86) compared with nonusers. No increased risk was reported for users of atypical antipsychotics. (OR: 0.87). When compared with atypical antipsychotic use, conventional antipsychotic use carries an OR of 2.13 for these cardiac outcomes. In patients using conventional antipsychotics, the presence and absence of cardiac diseases were 3.27 times and 2.05 times, respectively, more likely to be associated with hospitalization for ventricular arrhythmias and cardiac arrest, compared with nonusers without cardiac diseases.
These results suggest that atypical antipsychotics may carry less cardiac risk than conventional agents. In an inpatient population with advancing age and increasing prevalence of dementia and cardiac disease, use of atypical antipsychotic agents may be safer than older, typical agents.
4. Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 352:777-85.
This placebo-controlled, double-blind, multicenter, industry-sponsored trial of early treatment of hemorrhagic stroke with rFVIIa at 3 escalating doses, evaluated stroke hematoma growth, mortality, and functional outcomes up to 90 days. The authors note the substantial mortality and high morbidity of this condition, which currently lacks definitive treatment. Patients within 3 hours of symptoms with intracerebral hemorrhage on CT and who met study criteria were randomized to receive either placebo or a single intravenous dose of 40, 80, or 160 mcg/kg of rFVIIa within 1 hour of baseline CT and no more than 4 hours after symptoms. Follow-up CTs at 24 and 72 hours were obtained and functional assessments were performed serially at frequent intervals throughout the study period. Three hundred ninety-nine patients were analyzed and were found similar in their baseline characteristics. Lesion volume was significantly less with treatment, in a dose-dependent fashion. Mortality at 3 months was significantly less (29% vs. 18%) with treatment, and all 4 of the global functional outcome scales utilized were favorable, 3 of them (modified Rankin Scale for all doses, NIH Stroke Scale for all doses, and the Barthel Index at the 80 and 160 mcg/kg doses) in a statistically significant fashion. However, the authors noted an increase in serious thromboembolic events in the treatment groups, with a statistically significant increased frequency of arterial thromboembolic events. These included myocardial ischemic events and cerebral infarction, and most occurred within 3 days of rFVIIa treatment. Of note, the majority of patients who suffered these events made recovery from their complications, and the overall rates of fatal or disabling thromboembolic occurrences between the treatment and placebo groups were similar. This study offers new and exciting insights into potential therapy for this serious form of stroke, although safety concerns merit further study.
5. Siguret V, Gouin I, Debray M, et al. Initiation of warfarin therapy in elderly medical inpatients: a safe and accurate regimen. Am J Med. 2005; 118:137-142.
Warfarin therapy is widely used in geriatric populations. Sometimes over-anticoagulation occurs when warfarin therapy is initiated based on standard loading and maintenance dose in the hospital setting. This is mainly due to decreased hepatic clearance and polypharmacy in the geriatric population. A recent study in France demonstrated a useful and simple low-dose regimen for starting warfarin therapy (target INR: 2.0–3.0) in the elderly without over-anticoagulation. The patients enrolled in this study were typical geriatric patients with multiple comorbid conditions. These patients also received concomitant medications known to potentiate the effect of warfarin. One hundred six consecutive inpatients (age %70, mean age of 85 years) were given a 4-mg induction dose of warfarin for 3 days, and INR levels were measured on the 4th day. From this point, the daily warfarin dose was adjusted according to an algorithm (see Table 1), and INR values were obtained every 2–3 days until actual maintenance doses were determined. The maintenance dose was defined as the amount of warfarin required to yield an INR in 2.0 to 3.0 range on 2 consecutive samples obtained 48–72 hours apart in the absence of any dosage change for at least 4 days. Based on this algorithm, the predicted daily warfarin dose (3.1 ± 1.6 mg/day) correlated closely with the actual maintenance dose (3.2 ± 1.7 mg/day). The average time needed to achieve a therapeutic INR was 6.7 ± 3.3 days. None of the patients had an INR >4.0 during the induction period. This regimen also required fewer INR measurements.
Intracranial hemorrhage and gastrointestinal bleeding are serious complications of over-anticoagulation. The majority of gastrointestinal bleeding episodes respond to withholding warfarin and reversing anticoagulation. However, intracranial hemorrhage frequently leads to devastating outcomes. A recent report suggested that an age over 85 and INR of 3.5 or greater were associated with increased risk of intracranial hemorrhage. The warfarin algorithm proposed in this study provides a simple, safe, and effective tool to predict warfarin dosing in elderly hospitalized patients without over-anticoagulation. Although this regimen still needs to be validated in a large patient population in the future, it can be incorporated into computer-based dosing entry programs in the hospital setting to guide physicians in initiating warfarin therapy.
6. Wisnivesky JP, Henschke C, Balentine J, Willner, C, Deloire AM, McGinn TG. Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis. Arch Intern Med. 2005;165:453-7.
Whether to isolate a patient for suspected pulmonary tuberculosis (TB) is often a balancing act between clinical risk assessment and optimal hospital resource utilitization. Practitioners need a relatively simple but sophisticated tool that they can use at the bedside to more precisely assess the likelihood of TB for more efficient and effective triage.
These authors previously developed such a tool with a sensitivity of 98% and specificity of 46%. (See Table 2 for details) This study was designed to validate this decision rule in a new set of patients. Patients were enrolled in 2 tertiary-care hospitals in New York City area over a 21-month period. They were all admitted and isolated because of clinical suspicion for pulmonary TB, not utilizing the decision rule under study. Study team members collected demographic, clinical risk factors, presenting symptoms, and signs, laboratory, and radiographic findings. Chest x-ray findings were reviewed by investigators who were blinded to the other clinical and demographical information. The gold standard of diagnosis was at least 1 sputum culture that was positive for Mycobacterium tuberculosis.
A total of 516 patients were enrolled in this study. Of the 516, 19 (3.7%) were found to have culture-proven pulmonary TB. Univariate analyses showed that history of positive PPD, higher (98% vs. 95%) oxygen saturation, upper-lobe consolidation (not upper lobe cavity), and lymphadenopathy (hilar, mediastinal, or paratracheal) were all associated with the presence of pulmonary TB. Shortness of breath was associated with the absence of TB. A total score of 1 or higher in the prediction rule had a sensitivity of 95% for pulmonary TB, and score of less than 1 had a specificity of 35%. The investigators estimated a prevalence of 3.7%, thereby yielding a positive predictive value of 9.6% but a negative predictive value of 99.7%. They estimated that 35% of patients isolated would not have been with this prediction rule.
Though validated scientifically, this tool still has a false-negative rate of 5%. In a less endemic area, the false-negative rate would be correspondingly lower and thus more acceptable from a public health perspective. This is one step closer to a balance of optimal bed utilization and reasoned clinical assessment.
1. Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 352:1305-16.
This is the first prospective study comparing antithrombotic therapies for patients with atherosclerotic stenosis of major intracranial arteries. This multicenter, NINDS-sponsored, placebo-controlled, blinded study randomized 569 patients to aspirin (650 mg twice daily) or warfarin (initially 5 mg daily, titrated to achieve an INR of 2.0–3.0) and followed them for nearly 2 years. The study was terminated early over safely concerns about patients in the warfarin group. Baseline characteristics between the 2 groups were not significantly different. Warfarin was not more effective than aspirin in its effect on the primary endpoints of ischemic stroke, brain hemorrhage, or vascular death other than from stroke (as defined in the study protocol). However, major cardiac events (myocardial infarction or sudden death) were significantly higher in the warfarin group, and major hemorrhage (defined as any intracranial or systemic hemorrhage requiring hospitalization, transfusion, or surgical intervention) was also significantly higher in the warfarin group. The authors note the difficulty maintaining the INR in the target range (achieved only 63.1 % of the time during the maintenance period, an observation in line with other anticoagulation studies). In an accompanying editorial, Dr. Koroshetz of the stroke service at the Massachusetts General Hospital also observed that difficulties in achieving the therapeutic goal with warfarin could have impacted the results. The authors also note that the dose of aspirin employed in this study is somewhat higher than in previous trials. Nevertheless, until other data emerge, this investigation’s results favor aspirin in preference to warfarin for this high-risk condition.
2. Cornish PL, Knowles, SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission Arch Intern Med. 2005;165:424-9
Of the various types of medical errors, medication errors are believed to be the most common. At the time of hospital admission, medication discrepancies may lead to unintended drug interactions, toxicity, or interruption of appropriate drug therapies. These investigators performed a prospective study to identify unintended medication discrepancies between the patient’s home medications and those ordered at the time of the patient’s admission and to evaluate the potential clinical significance of these discrepancies.
This study was conducted at a 1,000-bed tertiary care hospital in Canada on the general medicine teaching service. A member of the study team reviewed each medical record to ascertain the physician-recorded medication history, the nurse-recorded medication history, the admission medication orders, and demographic information. A comprehensive list of all of the patient’s prescription or nonprescription drugs was compiled by interviewing patients, families, and pharmacists, and by inspecting the bottles. A discrepancy was defined as any difference between this comprehensive list and the admission medication orders. These were categorized into omission or addition of a medication, substitution of an agent within the same drug class, and change in dose, route, and frequency of administration of an agent. The medical team caring for the patient was then asked whether or not these discrepancies were intended. The team then reconciled any unintended discrepancies. These unintended discrepancies were further classified according to their potential for harm by 3 medical hospitalists into Class 1, 2, 3, in increasing order of potential harm. One hundred fifty-one patients were included in the analysis. A total of 140 errors occurred in 81 patients (54%). The overall error rate was 0.93 per patient. Of the errors, 46% consisted of omission of a regularly prescribed medication, 25% involved discrepant doses, 17.1% involved discrepant frequency, and 11.4% were actually incorrect drugs. Breakdown of error severity resulted in designation of 61% as Class 1, 33% as Class 2, and 5.7% as Class 3. The interrater agreement was a kappa of 0.26. These discrepancies were not found to be associated with night or weekend admissions, high patient volume, or high numbers of medications.
Real-time clinical correlation with the responsible physicians allowed distinction of intended from unintended discrepancies. This presumably improved the accuracy of the error rate measurement. This study confirmed the relatively high rate previously reported. Further study can focus on possible intervention to minimize these errors.
3. Liperoti R, Gambassi G, Lapane KL, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest Arch Intern Med. 2005;165:696-701.
As the number of hospitalized elderly and demented patients increases, use of both typical and atypical antipsychotics has become prevalent. QT prolongation, ventricular arrhythmia, and cardiac arrest are more commonly associated with the older conventional antipsychotics than with newer atypical agents. This case-control study was conducted to estimate the effect of both conventional and atypical antipsychotics use on the risk of hospital admission for ventricular arrhythmia or cardiac arrest.
The patient population involved consisted of elderly nursing home residents in 6 US states. The investigators utilized Systematic Assessment of Geriatric Drug Use via Epidemiology database that contains data from minimum data set (MDS), a standardized data set required of all certified nursing homes in the United States. Case patients were selected by ICD-9 codes for cardiac arrest or ventricular arrhythmia. Control patients were selected via ICD-9 codes of 6 other common inpatient diagnoses. Antipsychotic exposure was determined by use of the most recent assessment in the nursing homes prior to admission. Exposed patients were those who received atypical antipsychotics such as risperidone, olanzapine, quetiapine, and clozapine, and those who used conventional agents such as haloperidol and others. After control for potential confounders, users of conventional antipsychotics showed an 86% increase in the risk of hospitalization for ventricular arrhythmias or cardiac arrest (OR: 1.86) compared with nonusers. No increased risk was reported for users of atypical antipsychotics. (OR: 0.87). When compared with atypical antipsychotic use, conventional antipsychotic use carries an OR of 2.13 for these cardiac outcomes. In patients using conventional antipsychotics, the presence and absence of cardiac diseases were 3.27 times and 2.05 times, respectively, more likely to be associated with hospitalization for ventricular arrhythmias and cardiac arrest, compared with nonusers without cardiac diseases.
These results suggest that atypical antipsychotics may carry less cardiac risk than conventional agents. In an inpatient population with advancing age and increasing prevalence of dementia and cardiac disease, use of atypical antipsychotic agents may be safer than older, typical agents.
4. Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 352:777-85.
This placebo-controlled, double-blind, multicenter, industry-sponsored trial of early treatment of hemorrhagic stroke with rFVIIa at 3 escalating doses, evaluated stroke hematoma growth, mortality, and functional outcomes up to 90 days. The authors note the substantial mortality and high morbidity of this condition, which currently lacks definitive treatment. Patients within 3 hours of symptoms with intracerebral hemorrhage on CT and who met study criteria were randomized to receive either placebo or a single intravenous dose of 40, 80, or 160 mcg/kg of rFVIIa within 1 hour of baseline CT and no more than 4 hours after symptoms. Follow-up CTs at 24 and 72 hours were obtained and functional assessments were performed serially at frequent intervals throughout the study period. Three hundred ninety-nine patients were analyzed and were found similar in their baseline characteristics. Lesion volume was significantly less with treatment, in a dose-dependent fashion. Mortality at 3 months was significantly less (29% vs. 18%) with treatment, and all 4 of the global functional outcome scales utilized were favorable, 3 of them (modified Rankin Scale for all doses, NIH Stroke Scale for all doses, and the Barthel Index at the 80 and 160 mcg/kg doses) in a statistically significant fashion. However, the authors noted an increase in serious thromboembolic events in the treatment groups, with a statistically significant increased frequency of arterial thromboembolic events. These included myocardial ischemic events and cerebral infarction, and most occurred within 3 days of rFVIIa treatment. Of note, the majority of patients who suffered these events made recovery from their complications, and the overall rates of fatal or disabling thromboembolic occurrences between the treatment and placebo groups were similar. This study offers new and exciting insights into potential therapy for this serious form of stroke, although safety concerns merit further study.
5. Siguret V, Gouin I, Debray M, et al. Initiation of warfarin therapy in elderly medical inpatients: a safe and accurate regimen. Am J Med. 2005; 118:137-142.
Warfarin therapy is widely used in geriatric populations. Sometimes over-anticoagulation occurs when warfarin therapy is initiated based on standard loading and maintenance dose in the hospital setting. This is mainly due to decreased hepatic clearance and polypharmacy in the geriatric population. A recent study in France demonstrated a useful and simple low-dose regimen for starting warfarin therapy (target INR: 2.0–3.0) in the elderly without over-anticoagulation. The patients enrolled in this study were typical geriatric patients with multiple comorbid conditions. These patients also received concomitant medications known to potentiate the effect of warfarin. One hundred six consecutive inpatients (age %70, mean age of 85 years) were given a 4-mg induction dose of warfarin for 3 days, and INR levels were measured on the 4th day. From this point, the daily warfarin dose was adjusted according to an algorithm (see Table 1), and INR values were obtained every 2–3 days until actual maintenance doses were determined. The maintenance dose was defined as the amount of warfarin required to yield an INR in 2.0 to 3.0 range on 2 consecutive samples obtained 48–72 hours apart in the absence of any dosage change for at least 4 days. Based on this algorithm, the predicted daily warfarin dose (3.1 ± 1.6 mg/day) correlated closely with the actual maintenance dose (3.2 ± 1.7 mg/day). The average time needed to achieve a therapeutic INR was 6.7 ± 3.3 days. None of the patients had an INR >4.0 during the induction period. This regimen also required fewer INR measurements.
Intracranial hemorrhage and gastrointestinal bleeding are serious complications of over-anticoagulation. The majority of gastrointestinal bleeding episodes respond to withholding warfarin and reversing anticoagulation. However, intracranial hemorrhage frequently leads to devastating outcomes. A recent report suggested that an age over 85 and INR of 3.5 or greater were associated with increased risk of intracranial hemorrhage. The warfarin algorithm proposed in this study provides a simple, safe, and effective tool to predict warfarin dosing in elderly hospitalized patients without over-anticoagulation. Although this regimen still needs to be validated in a large patient population in the future, it can be incorporated into computer-based dosing entry programs in the hospital setting to guide physicians in initiating warfarin therapy.
6. Wisnivesky JP, Henschke C, Balentine J, Willner, C, Deloire AM, McGinn TG. Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis. Arch Intern Med. 2005;165:453-7.
Whether to isolate a patient for suspected pulmonary tuberculosis (TB) is often a balancing act between clinical risk assessment and optimal hospital resource utilitization. Practitioners need a relatively simple but sophisticated tool that they can use at the bedside to more precisely assess the likelihood of TB for more efficient and effective triage.
These authors previously developed such a tool with a sensitivity of 98% and specificity of 46%. (See Table 2 for details) This study was designed to validate this decision rule in a new set of patients. Patients were enrolled in 2 tertiary-care hospitals in New York City area over a 21-month period. They were all admitted and isolated because of clinical suspicion for pulmonary TB, not utilizing the decision rule under study. Study team members collected demographic, clinical risk factors, presenting symptoms, and signs, laboratory, and radiographic findings. Chest x-ray findings were reviewed by investigators who were blinded to the other clinical and demographical information. The gold standard of diagnosis was at least 1 sputum culture that was positive for Mycobacterium tuberculosis.
A total of 516 patients were enrolled in this study. Of the 516, 19 (3.7%) were found to have culture-proven pulmonary TB. Univariate analyses showed that history of positive PPD, higher (98% vs. 95%) oxygen saturation, upper-lobe consolidation (not upper lobe cavity), and lymphadenopathy (hilar, mediastinal, or paratracheal) were all associated with the presence of pulmonary TB. Shortness of breath was associated with the absence of TB. A total score of 1 or higher in the prediction rule had a sensitivity of 95% for pulmonary TB, and score of less than 1 had a specificity of 35%. The investigators estimated a prevalence of 3.7%, thereby yielding a positive predictive value of 9.6% but a negative predictive value of 99.7%. They estimated that 35% of patients isolated would not have been with this prediction rule.
Though validated scientifically, this tool still has a false-negative rate of 5%. In a less endemic area, the false-negative rate would be correspondingly lower and thus more acceptable from a public health perspective. This is one step closer to a balance of optimal bed utilization and reasoned clinical assessment.
1. Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 352:1305-16.
This is the first prospective study comparing antithrombotic therapies for patients with atherosclerotic stenosis of major intracranial arteries. This multicenter, NINDS-sponsored, placebo-controlled, blinded study randomized 569 patients to aspirin (650 mg twice daily) or warfarin (initially 5 mg daily, titrated to achieve an INR of 2.0–3.0) and followed them for nearly 2 years. The study was terminated early over safely concerns about patients in the warfarin group. Baseline characteristics between the 2 groups were not significantly different. Warfarin was not more effective than aspirin in its effect on the primary endpoints of ischemic stroke, brain hemorrhage, or vascular death other than from stroke (as defined in the study protocol). However, major cardiac events (myocardial infarction or sudden death) were significantly higher in the warfarin group, and major hemorrhage (defined as any intracranial or systemic hemorrhage requiring hospitalization, transfusion, or surgical intervention) was also significantly higher in the warfarin group. The authors note the difficulty maintaining the INR in the target range (achieved only 63.1 % of the time during the maintenance period, an observation in line with other anticoagulation studies). In an accompanying editorial, Dr. Koroshetz of the stroke service at the Massachusetts General Hospital also observed that difficulties in achieving the therapeutic goal with warfarin could have impacted the results. The authors also note that the dose of aspirin employed in this study is somewhat higher than in previous trials. Nevertheless, until other data emerge, this investigation’s results favor aspirin in preference to warfarin for this high-risk condition.
2. Cornish PL, Knowles, SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission Arch Intern Med. 2005;165:424-9
Of the various types of medical errors, medication errors are believed to be the most common. At the time of hospital admission, medication discrepancies may lead to unintended drug interactions, toxicity, or interruption of appropriate drug therapies. These investigators performed a prospective study to identify unintended medication discrepancies between the patient’s home medications and those ordered at the time of the patient’s admission and to evaluate the potential clinical significance of these discrepancies.
This study was conducted at a 1,000-bed tertiary care hospital in Canada on the general medicine teaching service. A member of the study team reviewed each medical record to ascertain the physician-recorded medication history, the nurse-recorded medication history, the admission medication orders, and demographic information. A comprehensive list of all of the patient’s prescription or nonprescription drugs was compiled by interviewing patients, families, and pharmacists, and by inspecting the bottles. A discrepancy was defined as any difference between this comprehensive list and the admission medication orders. These were categorized into omission or addition of a medication, substitution of an agent within the same drug class, and change in dose, route, and frequency of administration of an agent. The medical team caring for the patient was then asked whether or not these discrepancies were intended. The team then reconciled any unintended discrepancies. These unintended discrepancies were further classified according to their potential for harm by 3 medical hospitalists into Class 1, 2, 3, in increasing order of potential harm. One hundred fifty-one patients were included in the analysis. A total of 140 errors occurred in 81 patients (54%). The overall error rate was 0.93 per patient. Of the errors, 46% consisted of omission of a regularly prescribed medication, 25% involved discrepant doses, 17.1% involved discrepant frequency, and 11.4% were actually incorrect drugs. Breakdown of error severity resulted in designation of 61% as Class 1, 33% as Class 2, and 5.7% as Class 3. The interrater agreement was a kappa of 0.26. These discrepancies were not found to be associated with night or weekend admissions, high patient volume, or high numbers of medications.
Real-time clinical correlation with the responsible physicians allowed distinction of intended from unintended discrepancies. This presumably improved the accuracy of the error rate measurement. This study confirmed the relatively high rate previously reported. Further study can focus on possible intervention to minimize these errors.
3. Liperoti R, Gambassi G, Lapane KL, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest Arch Intern Med. 2005;165:696-701.
As the number of hospitalized elderly and demented patients increases, use of both typical and atypical antipsychotics has become prevalent. QT prolongation, ventricular arrhythmia, and cardiac arrest are more commonly associated with the older conventional antipsychotics than with newer atypical agents. This case-control study was conducted to estimate the effect of both conventional and atypical antipsychotics use on the risk of hospital admission for ventricular arrhythmia or cardiac arrest.
The patient population involved consisted of elderly nursing home residents in 6 US states. The investigators utilized Systematic Assessment of Geriatric Drug Use via Epidemiology database that contains data from minimum data set (MDS), a standardized data set required of all certified nursing homes in the United States. Case patients were selected by ICD-9 codes for cardiac arrest or ventricular arrhythmia. Control patients were selected via ICD-9 codes of 6 other common inpatient diagnoses. Antipsychotic exposure was determined by use of the most recent assessment in the nursing homes prior to admission. Exposed patients were those who received atypical antipsychotics such as risperidone, olanzapine, quetiapine, and clozapine, and those who used conventional agents such as haloperidol and others. After control for potential confounders, users of conventional antipsychotics showed an 86% increase in the risk of hospitalization for ventricular arrhythmias or cardiac arrest (OR: 1.86) compared with nonusers. No increased risk was reported for users of atypical antipsychotics. (OR: 0.87). When compared with atypical antipsychotic use, conventional antipsychotic use carries an OR of 2.13 for these cardiac outcomes. In patients using conventional antipsychotics, the presence and absence of cardiac diseases were 3.27 times and 2.05 times, respectively, more likely to be associated with hospitalization for ventricular arrhythmias and cardiac arrest, compared with nonusers without cardiac diseases.
These results suggest that atypical antipsychotics may carry less cardiac risk than conventional agents. In an inpatient population with advancing age and increasing prevalence of dementia and cardiac disease, use of atypical antipsychotic agents may be safer than older, typical agents.
4. Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 352:777-85.
This placebo-controlled, double-blind, multicenter, industry-sponsored trial of early treatment of hemorrhagic stroke with rFVIIa at 3 escalating doses, evaluated stroke hematoma growth, mortality, and functional outcomes up to 90 days. The authors note the substantial mortality and high morbidity of this condition, which currently lacks definitive treatment. Patients within 3 hours of symptoms with intracerebral hemorrhage on CT and who met study criteria were randomized to receive either placebo or a single intravenous dose of 40, 80, or 160 mcg/kg of rFVIIa within 1 hour of baseline CT and no more than 4 hours after symptoms. Follow-up CTs at 24 and 72 hours were obtained and functional assessments were performed serially at frequent intervals throughout the study period. Three hundred ninety-nine patients were analyzed and were found similar in their baseline characteristics. Lesion volume was significantly less with treatment, in a dose-dependent fashion. Mortality at 3 months was significantly less (29% vs. 18%) with treatment, and all 4 of the global functional outcome scales utilized were favorable, 3 of them (modified Rankin Scale for all doses, NIH Stroke Scale for all doses, and the Barthel Index at the 80 and 160 mcg/kg doses) in a statistically significant fashion. However, the authors noted an increase in serious thromboembolic events in the treatment groups, with a statistically significant increased frequency of arterial thromboembolic events. These included myocardial ischemic events and cerebral infarction, and most occurred within 3 days of rFVIIa treatment. Of note, the majority of patients who suffered these events made recovery from their complications, and the overall rates of fatal or disabling thromboembolic occurrences between the treatment and placebo groups were similar. This study offers new and exciting insights into potential therapy for this serious form of stroke, although safety concerns merit further study.
5. Siguret V, Gouin I, Debray M, et al. Initiation of warfarin therapy in elderly medical inpatients: a safe and accurate regimen. Am J Med. 2005; 118:137-142.
Warfarin therapy is widely used in geriatric populations. Sometimes over-anticoagulation occurs when warfarin therapy is initiated based on standard loading and maintenance dose in the hospital setting. This is mainly due to decreased hepatic clearance and polypharmacy in the geriatric population. A recent study in France demonstrated a useful and simple low-dose regimen for starting warfarin therapy (target INR: 2.0–3.0) in the elderly without over-anticoagulation. The patients enrolled in this study were typical geriatric patients with multiple comorbid conditions. These patients also received concomitant medications known to potentiate the effect of warfarin. One hundred six consecutive inpatients (age %70, mean age of 85 years) were given a 4-mg induction dose of warfarin for 3 days, and INR levels were measured on the 4th day. From this point, the daily warfarin dose was adjusted according to an algorithm (see Table 1), and INR values were obtained every 2–3 days until actual maintenance doses were determined. The maintenance dose was defined as the amount of warfarin required to yield an INR in 2.0 to 3.0 range on 2 consecutive samples obtained 48–72 hours apart in the absence of any dosage change for at least 4 days. Based on this algorithm, the predicted daily warfarin dose (3.1 ± 1.6 mg/day) correlated closely with the actual maintenance dose (3.2 ± 1.7 mg/day). The average time needed to achieve a therapeutic INR was 6.7 ± 3.3 days. None of the patients had an INR >4.0 during the induction period. This regimen also required fewer INR measurements.
Intracranial hemorrhage and gastrointestinal bleeding are serious complications of over-anticoagulation. The majority of gastrointestinal bleeding episodes respond to withholding warfarin and reversing anticoagulation. However, intracranial hemorrhage frequently leads to devastating outcomes. A recent report suggested that an age over 85 and INR of 3.5 or greater were associated with increased risk of intracranial hemorrhage. The warfarin algorithm proposed in this study provides a simple, safe, and effective tool to predict warfarin dosing in elderly hospitalized patients without over-anticoagulation. Although this regimen still needs to be validated in a large patient population in the future, it can be incorporated into computer-based dosing entry programs in the hospital setting to guide physicians in initiating warfarin therapy.
6. Wisnivesky JP, Henschke C, Balentine J, Willner, C, Deloire AM, McGinn TG. Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis. Arch Intern Med. 2005;165:453-7.
Whether to isolate a patient for suspected pulmonary tuberculosis (TB) is often a balancing act between clinical risk assessment and optimal hospital resource utilitization. Practitioners need a relatively simple but sophisticated tool that they can use at the bedside to more precisely assess the likelihood of TB for more efficient and effective triage.
These authors previously developed such a tool with a sensitivity of 98% and specificity of 46%. (See Table 2 for details) This study was designed to validate this decision rule in a new set of patients. Patients were enrolled in 2 tertiary-care hospitals in New York City area over a 21-month period. They were all admitted and isolated because of clinical suspicion for pulmonary TB, not utilizing the decision rule under study. Study team members collected demographic, clinical risk factors, presenting symptoms, and signs, laboratory, and radiographic findings. Chest x-ray findings were reviewed by investigators who were blinded to the other clinical and demographical information. The gold standard of diagnosis was at least 1 sputum culture that was positive for Mycobacterium tuberculosis.
A total of 516 patients were enrolled in this study. Of the 516, 19 (3.7%) were found to have culture-proven pulmonary TB. Univariate analyses showed that history of positive PPD, higher (98% vs. 95%) oxygen saturation, upper-lobe consolidation (not upper lobe cavity), and lymphadenopathy (hilar, mediastinal, or paratracheal) were all associated with the presence of pulmonary TB. Shortness of breath was associated with the absence of TB. A total score of 1 or higher in the prediction rule had a sensitivity of 95% for pulmonary TB, and score of less than 1 had a specificity of 35%. The investigators estimated a prevalence of 3.7%, thereby yielding a positive predictive value of 9.6% but a negative predictive value of 99.7%. They estimated that 35% of patients isolated would not have been with this prediction rule.
Though validated scientifically, this tool still has a false-negative rate of 5%. In a less endemic area, the false-negative rate would be correspondingly lower and thus more acceptable from a public health perspective. This is one step closer to a balance of optimal bed utilization and reasoned clinical assessment.