User login
Coding Changes for 2016
New Codes for 2016
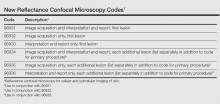
In 2016, noninvasive imaging in dermatology finally received recognition at the Current Procedural Terminology (CPT) level with the publication of 6 new Category I codes for reflectance confocal microscopy.1 These new codes are classified under the “Special Dermatological Procedures” section of CPT where codes do not have technical and professional payment splits, unlike pathology codes (Table). Currently, the new codes for reflectance confocal microscopy can only be implemented when using the VivaScope 1500 (Caliber I.D.) reflectance confocal imaging system and not with any other devices. At present, these codes are priced by each insurer and should be payable, as they are Category I codes that meet all criteria for widely used procedures that are well supported by strong evidence.
Additionally, MelaFind (MELA Sciences) has received 2 Category III CPT codes in 2016: 0400T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [1–5 lesions]; 0401T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [≥6 lesions]).
The CPT Professional Edition notes that Category III codes are a set of temporary codes for emerging technology, services, and procedures that allow data collection for these services and procedures.1 Inclusion implies nothing about safety, efficacy, frequency of use, or payment. These codes are used to differentiate emerging technology from the widely accepted Category I codes and use of alphanumeric characters instead of 5-digit codes. If reading this paragraph makes you giddy all over, pay a visit to the American Medical Association website to learn more about the process by which CPT codes come to life.2
Policy and Coding Changes
Last year saw much sturm and drang with the passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).3 The MACRA repealed the Sustainable Growth Rate formula and established annual positive or flat-fee updates for 10 years. A 2-tracked fee update was instituted afterward. It also established the Merit-Based Incentive Payment System, which consolidates existing Medicare fee-for-service physician incentive programs, establishes a pathway for physicians to participate in alternative payment models including the patient-centered medical home, and makes a bunch of other changes to existing Medicare physician payment statutes. It is too early to say if and how it will work and if it will change dermatology. It could fail miserably or it could be a brave new world; stay tuned.3
On the coding front, MACRA prohibits across-the-board elimination of global periods that the Centers for Medicare & Medicaid Services (CMS) had previously announced.4 Instead, the CMS must develop and implement a process to gather data on services furnished during global periods based on a representative sample of physician data. The CMS can delay up to 5% of payments if it does not get the data it asks for and must work through the rulemaking process, which will impact medicine in 2019. Among our codes with nonzero global periods, the premalignant destruction codes 17000 and 17004, each of which contains the value of a 99212 established patient visit, are at the very apex of the hit list. It is not clear if the CMS will retrospectively pull medical records to evaluate the occurrence of the global visit or will prospectively have us use 99024, the code for a “[p]ostoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure.”1 This code is not used unless your practice needs a “filler” code for nonreportable visits but that may change. Is this another unfunded mandate? Yes.
Clarifications also have been made for reporting superficial radiation therapy.1 Treatment delivery using energies below 1 MV are to be reported with CPT code 77401 and cannot be combined with radiation treatment delivery codes (77402, 77407, 77412), clinical treatment planning codes (77261–77263), treatment device development codes (77332–77334), isodose planning codes (77306, 77307, 77316–77318), radiation treatment management codes (77427, 77431, 77432, 77435, 77469, 77470, 77499), continuing medical physics consultation code (77336), and special physics consultation code (77370). Evaluation and management services may still be reported separately, when appropriate, in cases in which only superficial radiation therapy services (ie, 77401) are provided.1
Electronic brachytherapy for skin cancer has a new Category III tracking code (0394T [high-dose-rate electronic brachytherapy, skin surface application, per fraction, includes basic dosimetry, when performed]) that is priced by the insurer. Noridian Healthcare Solutions pulled the plug on what many perceived as astronomical payments, but changes may be afoot, as its URL for their new policy was down at the time of publication, and there is still great variability in how payment is being made for these codes. For those interested in learning about perception, a visit to http://forums.studentdoctor.net/threads/electronic-brachy.1132531/ is in order, as the economic drivers to the utilization of this therapy are discussed in detail from the perspective of students and young physicians.
Although there are new telehealth codes for inpatient services and end-stage renal disease management, there are still none that are relevant to dermatology.
Place of service codes have been updated. Place of service code 19 refers to “off campus outpatient hospital” settings while place of service code 22 has been revised to “on campus outpatient hospital.” If your practice is a facility, consult the Medicare Claims Processing Manual (20.4.2) on the site of service payment differential for further enlightenment.5 Do note that CMS is increasingly interested in physicians who use wrong place of service codes.
Incident to billing rules are somewhat clearer. The physician or other practitioner who bills must be the supervising physician or practitioner. Services cannot be provided by individuals who have been excluded from Medicare, Medicaid, or other federal programs, nor can they be provided by an individual who has had Medicare enrollment revoked. State laws that are more restrictive take precedence.
Of course, the Relative Value Scale Update Committee (RUC) process moves on as always and you likely will receive 1 or more surveys in the near future. If you get one of these surveys, do not delete it. The surveys are the currency of the RUC, and if you give your RUC team bad or no data, the specialty will suffer cuts in valuation of what we do. If you have questions about the survey, contact the American Academy of Dermatology staff as listed in the survey. If you want to learn more about RUC, visit the American Medical Association website.6 To see the current relative value units for what dermatologists do and the typical time for these procedures, visit the CMS website, which provides resources that supply tremendous amounts of data on code valuation including documents detailing relative value units for every CPT code.7 You also can access current time values for preservice work, intraservice work, and postservice work times for all CPT codes in the entire CPT Professional Edition. They are based on typical times and are the major determinants of what you get paid. Happy reading.
1. Current Procedural Terminology 2016, Professional Edition. Chicago, IL: American Medical Association; 2015.
2. CPT–Current Procedural Terminology. American Medical Association website. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt/cpt-editorial-panel.page. Accessed March 23, 2016.
3. The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs). Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Accessed March 23, 2016.
4. Text of the Medicare Access and CHIP Reauthorization Act of 2015. GovTrack website. https://www.govtrack.us/congress/bills/114/hr2/text. Accessed March 23, 2016.
5. Physicians/Nonphysician Practitioners. Medicare Claims Processing Manual. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed March 23, 2016.
6. American Medical Association. The RVS update committee. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/medicare/the-resource-based-relative-value-scale/the-rvs-update-committee.page?. Accessed March 23, 2016.
7. Details for title: CMS-1631-FC. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Physician FeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1631-FC.html. Published November 16, 2015. Accessed March 23, 2016.
New Codes for 2016
In 2016, noninvasive imaging in dermatology finally received recognition at the Current Procedural Terminology (CPT) level with the publication of 6 new Category I codes for reflectance confocal microscopy.1 These new codes are classified under the “Special Dermatological Procedures” section of CPT where codes do not have technical and professional payment splits, unlike pathology codes (Table). Currently, the new codes for reflectance confocal microscopy can only be implemented when using the VivaScope 1500 (Caliber I.D.) reflectance confocal imaging system and not with any other devices. At present, these codes are priced by each insurer and should be payable, as they are Category I codes that meet all criteria for widely used procedures that are well supported by strong evidence.
Additionally, MelaFind (MELA Sciences) has received 2 Category III CPT codes in 2016: 0400T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [1–5 lesions]; 0401T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [≥6 lesions]).
The CPT Professional Edition notes that Category III codes are a set of temporary codes for emerging technology, services, and procedures that allow data collection for these services and procedures.1 Inclusion implies nothing about safety, efficacy, frequency of use, or payment. These codes are used to differentiate emerging technology from the widely accepted Category I codes and use of alphanumeric characters instead of 5-digit codes. If reading this paragraph makes you giddy all over, pay a visit to the American Medical Association website to learn more about the process by which CPT codes come to life.2
Policy and Coding Changes
Last year saw much sturm and drang with the passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).3 The MACRA repealed the Sustainable Growth Rate formula and established annual positive or flat-fee updates for 10 years. A 2-tracked fee update was instituted afterward. It also established the Merit-Based Incentive Payment System, which consolidates existing Medicare fee-for-service physician incentive programs, establishes a pathway for physicians to participate in alternative payment models including the patient-centered medical home, and makes a bunch of other changes to existing Medicare physician payment statutes. It is too early to say if and how it will work and if it will change dermatology. It could fail miserably or it could be a brave new world; stay tuned.3
On the coding front, MACRA prohibits across-the-board elimination of global periods that the Centers for Medicare & Medicaid Services (CMS) had previously announced.4 Instead, the CMS must develop and implement a process to gather data on services furnished during global periods based on a representative sample of physician data. The CMS can delay up to 5% of payments if it does not get the data it asks for and must work through the rulemaking process, which will impact medicine in 2019. Among our codes with nonzero global periods, the premalignant destruction codes 17000 and 17004, each of which contains the value of a 99212 established patient visit, are at the very apex of the hit list. It is not clear if the CMS will retrospectively pull medical records to evaluate the occurrence of the global visit or will prospectively have us use 99024, the code for a “[p]ostoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure.”1 This code is not used unless your practice needs a “filler” code for nonreportable visits but that may change. Is this another unfunded mandate? Yes.
Clarifications also have been made for reporting superficial radiation therapy.1 Treatment delivery using energies below 1 MV are to be reported with CPT code 77401 and cannot be combined with radiation treatment delivery codes (77402, 77407, 77412), clinical treatment planning codes (77261–77263), treatment device development codes (77332–77334), isodose planning codes (77306, 77307, 77316–77318), radiation treatment management codes (77427, 77431, 77432, 77435, 77469, 77470, 77499), continuing medical physics consultation code (77336), and special physics consultation code (77370). Evaluation and management services may still be reported separately, when appropriate, in cases in which only superficial radiation therapy services (ie, 77401) are provided.1
Electronic brachytherapy for skin cancer has a new Category III tracking code (0394T [high-dose-rate electronic brachytherapy, skin surface application, per fraction, includes basic dosimetry, when performed]) that is priced by the insurer. Noridian Healthcare Solutions pulled the plug on what many perceived as astronomical payments, but changes may be afoot, as its URL for their new policy was down at the time of publication, and there is still great variability in how payment is being made for these codes. For those interested in learning about perception, a visit to http://forums.studentdoctor.net/threads/electronic-brachy.1132531/ is in order, as the economic drivers to the utilization of this therapy are discussed in detail from the perspective of students and young physicians.
Although there are new telehealth codes for inpatient services and end-stage renal disease management, there are still none that are relevant to dermatology.
Place of service codes have been updated. Place of service code 19 refers to “off campus outpatient hospital” settings while place of service code 22 has been revised to “on campus outpatient hospital.” If your practice is a facility, consult the Medicare Claims Processing Manual (20.4.2) on the site of service payment differential for further enlightenment.5 Do note that CMS is increasingly interested in physicians who use wrong place of service codes.
Incident to billing rules are somewhat clearer. The physician or other practitioner who bills must be the supervising physician or practitioner. Services cannot be provided by individuals who have been excluded from Medicare, Medicaid, or other federal programs, nor can they be provided by an individual who has had Medicare enrollment revoked. State laws that are more restrictive take precedence.
Of course, the Relative Value Scale Update Committee (RUC) process moves on as always and you likely will receive 1 or more surveys in the near future. If you get one of these surveys, do not delete it. The surveys are the currency of the RUC, and if you give your RUC team bad or no data, the specialty will suffer cuts in valuation of what we do. If you have questions about the survey, contact the American Academy of Dermatology staff as listed in the survey. If you want to learn more about RUC, visit the American Medical Association website.6 To see the current relative value units for what dermatologists do and the typical time for these procedures, visit the CMS website, which provides resources that supply tremendous amounts of data on code valuation including documents detailing relative value units for every CPT code.7 You also can access current time values for preservice work, intraservice work, and postservice work times for all CPT codes in the entire CPT Professional Edition. They are based on typical times and are the major determinants of what you get paid. Happy reading.
New Codes for 2016
In 2016, noninvasive imaging in dermatology finally received recognition at the Current Procedural Terminology (CPT) level with the publication of 6 new Category I codes for reflectance confocal microscopy.1 These new codes are classified under the “Special Dermatological Procedures” section of CPT where codes do not have technical and professional payment splits, unlike pathology codes (Table). Currently, the new codes for reflectance confocal microscopy can only be implemented when using the VivaScope 1500 (Caliber I.D.) reflectance confocal imaging system and not with any other devices. At present, these codes are priced by each insurer and should be payable, as they are Category I codes that meet all criteria for widely used procedures that are well supported by strong evidence.
Additionally, MelaFind (MELA Sciences) has received 2 Category III CPT codes in 2016: 0400T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [1–5 lesions]; 0401T, multispectral digital skin lesion analysis of clinically atypical cutaneous pigmented lesions for detection of melanomas and high-risk melanocytic atypia [≥6 lesions]).
The CPT Professional Edition notes that Category III codes are a set of temporary codes for emerging technology, services, and procedures that allow data collection for these services and procedures.1 Inclusion implies nothing about safety, efficacy, frequency of use, or payment. These codes are used to differentiate emerging technology from the widely accepted Category I codes and use of alphanumeric characters instead of 5-digit codes. If reading this paragraph makes you giddy all over, pay a visit to the American Medical Association website to learn more about the process by which CPT codes come to life.2
Policy and Coding Changes
Last year saw much sturm and drang with the passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).3 The MACRA repealed the Sustainable Growth Rate formula and established annual positive or flat-fee updates for 10 years. A 2-tracked fee update was instituted afterward. It also established the Merit-Based Incentive Payment System, which consolidates existing Medicare fee-for-service physician incentive programs, establishes a pathway for physicians to participate in alternative payment models including the patient-centered medical home, and makes a bunch of other changes to existing Medicare physician payment statutes. It is too early to say if and how it will work and if it will change dermatology. It could fail miserably or it could be a brave new world; stay tuned.3
On the coding front, MACRA prohibits across-the-board elimination of global periods that the Centers for Medicare & Medicaid Services (CMS) had previously announced.4 Instead, the CMS must develop and implement a process to gather data on services furnished during global periods based on a representative sample of physician data. The CMS can delay up to 5% of payments if it does not get the data it asks for and must work through the rulemaking process, which will impact medicine in 2019. Among our codes with nonzero global periods, the premalignant destruction codes 17000 and 17004, each of which contains the value of a 99212 established patient visit, are at the very apex of the hit list. It is not clear if the CMS will retrospectively pull medical records to evaluate the occurrence of the global visit or will prospectively have us use 99024, the code for a “[p]ostoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure.”1 This code is not used unless your practice needs a “filler” code for nonreportable visits but that may change. Is this another unfunded mandate? Yes.
Clarifications also have been made for reporting superficial radiation therapy.1 Treatment delivery using energies below 1 MV are to be reported with CPT code 77401 and cannot be combined with radiation treatment delivery codes (77402, 77407, 77412), clinical treatment planning codes (77261–77263), treatment device development codes (77332–77334), isodose planning codes (77306, 77307, 77316–77318), radiation treatment management codes (77427, 77431, 77432, 77435, 77469, 77470, 77499), continuing medical physics consultation code (77336), and special physics consultation code (77370). Evaluation and management services may still be reported separately, when appropriate, in cases in which only superficial radiation therapy services (ie, 77401) are provided.1
Electronic brachytherapy for skin cancer has a new Category III tracking code (0394T [high-dose-rate electronic brachytherapy, skin surface application, per fraction, includes basic dosimetry, when performed]) that is priced by the insurer. Noridian Healthcare Solutions pulled the plug on what many perceived as astronomical payments, but changes may be afoot, as its URL for their new policy was down at the time of publication, and there is still great variability in how payment is being made for these codes. For those interested in learning about perception, a visit to http://forums.studentdoctor.net/threads/electronic-brachy.1132531/ is in order, as the economic drivers to the utilization of this therapy are discussed in detail from the perspective of students and young physicians.
Although there are new telehealth codes for inpatient services and end-stage renal disease management, there are still none that are relevant to dermatology.
Place of service codes have been updated. Place of service code 19 refers to “off campus outpatient hospital” settings while place of service code 22 has been revised to “on campus outpatient hospital.” If your practice is a facility, consult the Medicare Claims Processing Manual (20.4.2) on the site of service payment differential for further enlightenment.5 Do note that CMS is increasingly interested in physicians who use wrong place of service codes.
Incident to billing rules are somewhat clearer. The physician or other practitioner who bills must be the supervising physician or practitioner. Services cannot be provided by individuals who have been excluded from Medicare, Medicaid, or other federal programs, nor can they be provided by an individual who has had Medicare enrollment revoked. State laws that are more restrictive take precedence.
Of course, the Relative Value Scale Update Committee (RUC) process moves on as always and you likely will receive 1 or more surveys in the near future. If you get one of these surveys, do not delete it. The surveys are the currency of the RUC, and if you give your RUC team bad or no data, the specialty will suffer cuts in valuation of what we do. If you have questions about the survey, contact the American Academy of Dermatology staff as listed in the survey. If you want to learn more about RUC, visit the American Medical Association website.6 To see the current relative value units for what dermatologists do and the typical time for these procedures, visit the CMS website, which provides resources that supply tremendous amounts of data on code valuation including documents detailing relative value units for every CPT code.7 You also can access current time values for preservice work, intraservice work, and postservice work times for all CPT codes in the entire CPT Professional Edition. They are based on typical times and are the major determinants of what you get paid. Happy reading.
1. Current Procedural Terminology 2016, Professional Edition. Chicago, IL: American Medical Association; 2015.
2. CPT–Current Procedural Terminology. American Medical Association website. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt/cpt-editorial-panel.page. Accessed March 23, 2016.
3. The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs). Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Accessed March 23, 2016.
4. Text of the Medicare Access and CHIP Reauthorization Act of 2015. GovTrack website. https://www.govtrack.us/congress/bills/114/hr2/text. Accessed March 23, 2016.
5. Physicians/Nonphysician Practitioners. Medicare Claims Processing Manual. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed March 23, 2016.
6. American Medical Association. The RVS update committee. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/medicare/the-resource-based-relative-value-scale/the-rvs-update-committee.page?. Accessed March 23, 2016.
7. Details for title: CMS-1631-FC. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Physician FeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1631-FC.html. Published November 16, 2015. Accessed March 23, 2016.
1. Current Procedural Terminology 2016, Professional Edition. Chicago, IL: American Medical Association; 2015.
2. CPT–Current Procedural Terminology. American Medical Association website. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt/cpt-editorial-panel.page. Accessed March 23, 2016.
3. The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs). Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Accessed March 23, 2016.
4. Text of the Medicare Access and CHIP Reauthorization Act of 2015. GovTrack website. https://www.govtrack.us/congress/bills/114/hr2/text. Accessed March 23, 2016.
5. Physicians/Nonphysician Practitioners. Medicare Claims Processing Manual. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c12.pdf. Accessed March 23, 2016.
6. American Medical Association. The RVS update committee. http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/medicare/the-resource-based-relative-value-scale/the-rvs-update-committee.page?. Accessed March 23, 2016.
7. Details for title: CMS-1631-FC. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Physician FeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1631-FC.html. Published November 16, 2015. Accessed March 23, 2016.
Practice Points
- Many dermatology codes are in the “Special Dermatological Procedures” section of the Current Procedural Terminology (CPT) manual.
- Physicians should purchase a new CPT manual every year, as accurate coding is critical for accurate reimbursement.