User login
Personalized Health Planning in Primary Care Settings
Health care has become increasingly unaffordable in the U.S., yet it remains ineffective in preventing or effectively treating chronic diseases.1,2 Given the increasing burden of chronic disease on the American health care system, there is an effort to shift the practice of medicine away from its reactive, disease-oriented approach to a more sustainable proactive model.3-5
Personalized health care (PHC) is an approach to the practice of medicine where prediction, prevention, intense patient engagement, shared health care decision making, and coordination of care are essential to cost effectively facilitate better outcomes.3,5-7 Greater collaboration between patient and clinician replaces the traditional clinician-dominated dialogue with more effective patient-clinician partnerships.8,9 Patients’ knowledge, skills, and confidence to manage their health care have been linked to improved health outcomes, lower costs, and greater satisfaction with health care experiences.10,11
Personalized health care has been proposed as a means to achieve better patient engagement as part of an aligned, proactive clinical approach. At the heart of PHC is personalized health planning, wherein the patient and clinician develop shared health-related goals and a plan to achieve them.3
The VHA, the largest integrated health care system in the country, is on the vanguard of incorporating tenets of PHC into its delivery model. In 2011, the Office of Patient Centered Care and Cultural Transformation (OPCC&CT) was founded to “oversee the VHA’s cultural transformation to patient-centered care.”12 This undertaking represents “one of the most massive changes in the philosophy and process for health care delivery ever undertaken by an organized health care system.”13
The primary goal of the VHA’s strategic plan for 2013 to 2018 is to provide veterans personalized, proactive, patient-driven health care.14 The intention of this approach is to engage and inspire veterans to their highest possible level of health and well-being. A personalized approach requires a dynamic customization of care that is specifically relevant to the individual, based on factors such as medical conditions, genome, needs, values, and circumstances. In addition to being personalized, this approach must be proactive, and therefore, preventive and include strategies to strengthen the person’s innate capacity for enhancing health.
The third distinction of this new model health care is that it is patient-driven, rooted in and driven by that which matters most to people in their lives and aligns their health care with their day-to-day and long-term life goals.15 The latter may be the most critical of the 3 tenets, because a personalized, proactive approach that is not driven by an engaged and inspired individual will be unlikely to achieve adherence, let alone the highest level of health and well-being.
The VHA is uniquely positioned to optimize health and well-being for veterans due in part to a systemwide emphasis on training providers to promote and support behavior change through approaches including health coaching and motivational interviewing. These synergistic approaches used widely by clinicians throughout the VHA are influenced by the transtheoretical model (ie, the stages of change theory), which considers patients holistically and helps them identify intrinsic motivation to improve their health behaviors.16,17 The transformation occurring in the VHA is intended to shift the current disease-centric medical model to an approach that optimizes the health of veterans through patient-clinician engagement, health risk assessment (HRA), shared health goal creation, and a coordinated plan to attain them.12,13
Personalized Health Planning
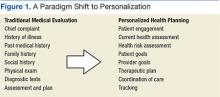
In recognition of the need to deliver care that emphasizes prevention and coordination, the patient-centered medical home, patient-aligned care teams (PACTs), and the chronic care model were developed. All of these embrace concepts of patient engagement, shared decision making, and team-based care. However, none of these approaches have outlined a clinical workflow that systematically and proactively operationalizes these concepts with the creation of a risk-based personalized care approach. Personalized health planning provides a clinical workflow that operationalizes all these features (Figure 1).
Of central importance is the creation of a personalized health plan (PHP), which the patient and clinician develop collaboratively. The plan serves to organize and coordinate care while engaging the patient in the process of care delivery and appropriate self-management of health.3,5 This approach promotes personalized and proactive care that values the individual and fosters meaningful patient self-awareness and engagement through shared decision making.7
The personalized health planning process is composed of several key components (Figure 2).
With this information, the clinician develops a preliminary therapeutic plan to meet these goals and discusses this plan with the patient. The next component is the synthesis of the clinician’s goals and/or treatment plan with the priorities of the patient to establish shared clinician-patient goals. This is followed by the establishment of the PHP, which consists of the agreed upon shared clinician and patient goals, a therapeutic and wellness plan to meet them, metrics for tracking progress, consults and referrals, and a time frame for the patient to achieve the health goals.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
The final component is coordination of care and a formalized follow-up system in which the health care team monitors the patient’s progress and provides support by revisiting or updating the PHP at intervals determined by the provider, based on the level of monitoring required by the patient’s health status. This approach invites the patient to become an empowered member of the care team by creating a patient-clinician partnership and providing a model for delivering personalized, proactive, patient-driven care to individuals with a diverse range of needs.4,5,18
Design and Implementation
This project qualified as exempt through the Duke University Institutional Review Board. The primary aim of this pilot was to examine the feasibility of implementing personalized health planning into primary care settings and to develop a workable process that is scalable and customizable to inpatient and outpatient clinics of varying sizes for different patient populations within the VHA. The pilot included 5 clinics in 2 geographic areas that were selected for their facility’s leadership support and desire to participate.
The VA Boston Healthcare System implemented personalized health planning at 3 primary care clinics: Jamaica Plain Primary Care, Jamaica Plain Women’s Health, and Quincy Primary Care. Three distinct PACTs participated in Boston, each composed of a medical doctor or doctor of osteopathy, a registered nurse (RN) or health technician, and a medical support assistant. The Sam Rayburn Memorial Veterans Center in Bonham, Texas, implemented personalized health planning at 2 clinics: the Hypertension Shared Medical Appointment and the Domiciliary Inpatient Primary Care. At Bonham, a medical doctor, pharmacist, RN, and an integrated mental health provider led the shared medical appointment (SMA) with guest presenters for individual appointments, depending on the topic covered. A RN and social worker implemented personalized health planning in the domiciliary.
After receiving training in the personalized health planning process, each of the clinics’ multidisciplinary PACTs incorporated their custom personalized health planning workflow into patient encounters. During the intake process of the clinic visit, the patient received a Personal Health Inventory (PHI) to determine health care priorities. The OPCC&CT developed the PHI as a whole-health self-assessment tool to help patients reflect on their health and lives, including core values, disparities between current and desired states, and preparedness to make behavioral changes to promote health.
The PHI assisted with framing this whole health approach to clinical care by expanding the definition of health to include more holistic elements of well-being, such as spirituality, personal relationships, emotional health, and personal development. A visual representation of the whole health domains termed The Circle of Health introduced this concept to the patient and assisted with goal setting (Figure 3).12
The PHI organized the patient’s input and was provided to the clinician to contribute to the development of the shared therapeutic goals and a final treatment plan. The PHP provided the tool to organize the goals, plans, and care following the visit and to connect the patient to additional resources within the VHA to support goal attainment through skill building and support. Each clinical site developed a mechanism to follow up with these patients either telephonically or with additional clinic appointments. The participating clinics implemented their customized version of personalized health planning for an average of 3 months.
Personalized health planning and accompanying tools were used primarily in routine ambulatory care visits. They were also used in the Bonham domiciliary clinic, which provides care for veterans with mental illnesses or addictive disorders who require additional structure and support. The purpose of the pilot was to determine whether personalized health planning could be used within this population. Given the small sample size and incompleteness of data collected, the Bonham domiciliary group was not included in the participating patient total. Across the other 4 clinics a total of 153 patients participated in the 3-month pilot study by establishing shared health goals and plans to meet them.
Results and Evaluation
Using a structured interview guide, a total of 6 small group interviews with participating clinicians were held (3 in Boston and 3 in Bonham, N = 18). Qualitative methods for research and evaluation were used to capture the depth of responses and to provide complex descriptions of the clinicians’ perspectives on the implementation of the personalized health planning process. Two researchers reviewed the transcripts to identify and code themes, and a third researcher reviewed the transcripts to confirm themes and resolve any discrepancies.
Analysis of the interview data revealed 9 core themes related to the feasibility, effectiveness, and future dissemination of personalized health planning. These themes, described below with exemplar data, include (a) patient engagement; (b) clinical assessment; (c) goal setting; (d) clinical workflow; (e) resources and support for veterans and clinicians; (f) Computerized Patient Record System (CPRS) integration; (g) patient-clinician relationship; (h) clinical outcomes; and (i) patient satisfaction.
The purpose of this study was to evaluate the feasibility of introducing personalized health planning within the workflows of the clinics that were participating. As a consequence of this, interviews were held with clinic staff rather than patients. However, the authors did obtain patient satisfaction data from 10 patients who received care from the hypertension SMA and responded to TruthPoint questions after their visit (Table).
Patient Engagement
A central tenant of personalized health planning is to engage patients in their health and health care. Findings revealed that clinicians at both sites perceived the PHP as an effective tool for integrating patients as robust members of the care team. Clinicians noted that by asking patients what was important to them, the patients felt more empowered to actively engage in the clinical encounter and to take responsibility for their health decisions. One pharmacist noted, “Patients are more empowered…when you change how you’re having your conversation with them that helps people start to recognize that they are an active participant [sic] and they can have an impact and can help with minimizing medicines or trying other things.”
Clinicians reported that including patients as active members in their care created a level of buy-in that motivated behavioral changes, because the patients identified behaviors they wanted to change vs the clinician telling them what they should or should not do. A nurse manager reported, “The key is that (the health goal) is coming from the patient…. Once it comes out of their mouth, they’re thinking about it and it’s not the clinician telling them what they should or shouldn’t do, but it’s helping them…identify something that’s important that will keep them into staying the way they want to, for the reasons that they want to.”
Clinical Assessment
The HRA tools are a vital part of the personalized health planning process, as they focus on preventive strategies that are most important for the patient.4 Clinicians reported using the PHI and additional HRA tools as part of the pilot program. The PHI is a self-assessment tool designed to identify psychosocial, behavioral, and environmental issues that can impact the patient’s care and health status. Most clinicians found that the PHI helped to solicit patients’ input on what was important to them and their health status while introducing the new approach to care. One nurse commented, “I found [PHI] very effective if I could actually sit down and review it with them to see what it was that was truly important to them and explain that this new approach is for a better understanding.”
Clinicians also found that the PHI helped focus the patient’s attention toward self-care areas that facilitated the shared goal setting process with the clinician. It moved the clinical encounter away from the chief health problems and toward identifying what is important to the patient and leveraging his or her intrinsic motivation to support health promotion via lifestyle modification.
Goal Setting
Shared goal setting is a critical component of personalized health planning. The clinician and patient must agree about realistic goals to improve the patient’s health. Clinicians reported that the goal setting stage was most successful when patients were invited to guide the process and offered the goals themselves; ie, when it was not just patient-centered but patient-driven.
“Setting a goal with a patient is pretty easy because people have an idea of what they should be doing and what they want to be doing,” one clinician reported. “They know their goal. So it’s a matter of just listening, really listening, and seeing what they want…. It’s not incongruous to get the medical goal and the patient goal to match.”
Patients were amenable to this collaborative approach to goal setting, and there was often commonality between the clinician’s goals and what was important to the patient. Occasionally, the patient set goals in seemingly unrelated areas that facilitated chronic disease management.
“One of our hypertensive patients wanted to work on things that are external that they felt are stressors that actually caused their blood pressure to be high,” a pharmacist recalled. “At the end of the day they wanted to control their environment better so that they could see if they could then be off of antihypertensives altogether. It appears that may be the case right now. That this individual has been able to accomplish that, which I thought was amazing, and since it’s still new, I’m still a little bit skeptical.... Is that possible? But if at the end of the day that is an outcome that we see from doing this, I think that’s wonderful.”
Clinicians reported that follow-up with the patient was a critical aspect of goal setting, because it improved accountability and helped track progress and health outcomes. However, due to the 3-month time limit of the pilot, there was insufficient time to get uniform data on the formalized follow-up systems developed by each clinic.
Clinical Workflow
Examining the feasibility of creating a process to incorporate personalized health planning into a busy primary care clinic was one of the major aims of this pilot. As such, issues of time, staff responsibilities, and use of the CPRS and other systems to facilitate the process were challenges that each clinic addressed in slightly different ways and with varying success. One method was to leverage the SMA for a group of patients with a common diagnosis to discuss their goals, provide accountability, and improve access to a medical team.
Another innovative approach was utilizing medical support administrators and health technicians to front-load some of the introductory information and patient education in the waiting room or during the intake process. Despite these efforts, some clinicians thought that the personalized health planning process might take longer than the traditional clinical encounter. One nurse manager commented, “I think it did affect the length of visits…it has made them a little bit longer.”
Resources and Support
The VHA has been undergoing a shift from an emphasis on tertiary care to include a greater focus on primary care. Part of this shift has been an investment in complementary and alternative medicine (CAM). The PHP helped clinicians explore what resources existed at their facility to support veterans in accomplishing their goals, including CAM. One nurse reported, “It made us look into other avenues that were actually available at the VHA that we didn’t even know we had…the acupuncture, the qigong, the voluntary services getting the veterans involved.”
Clinicians also identified the need for patient education in the concepts of whole health, personalized care, and patient involvement as necessary for moving the piloted approach forward. A nurse noted that “for [personalized health planning] to work well, [the patients] need more orientation and education upfront systemwide so that when they get into an appointment with us, we’re not starting at explaining the whole world view of partnership and doing things differently.”
Resources for clinicians were just as critical as resources for patients in facilitating the personalized health planning process. Specifically, most clinicians identified their own education and training in techniques to engage the patient in a meaningful way via motivational interviewing and health coaching complemented the personalized approach to care, particularly for shared goal setting,
CPRS Integration
The CPRS is an integrated, electronic patient record system that provides a single interface for clinicians to manage patient care as well as an efficient means for others to access and use patient information.19 The most commonly cited challenge in the pilot was the lack of available staff and time in the patient visit to complete the PHP while completing documentation requirements in CPRS.
One clinician stated, “For clinicians, the barriers…it’s time to get through the reminders and preventatives.” Clinicians reported that the process and the CPRS documentation were misaligned and lacked integration to coordinate care or support health planning. Moreover, clinicians reported that the data being collected did not support patient-centered care.
Patient-Clinician Relationship
A significant strength of personalized health planning was that it fostered a beneficial patient-clinician relationship that promoted greater depth of care. One clinician noted, “I think that it adds a more personalized dimension to the whole patient visit.” In addition to experiencing a deeper relationship with their patients, clinicians also expressed having higher levels of job satisfaction and relished the opportunity to connect with their patients in a more personal way.
Clinicians also reported that patients seemed more satisfied with the experience. One nurse commented, “They really respond to it very well when they figure out that you care about them as a whole… it’s not just about the disease process anymore.”
Clinical Outcomes
Clinicians reported a number of positive health outcomes during the pilot. One physician reported, “I have a patient, he had a follow-up today, a 29-year-old veteran, who was 260 pounds 5 months ago, and he’s 230 pounds today. He comes in monthly to see the nurse to let us know he’s doing it.”
The same physician also shared a similar transformation in a patient as a result of personalized health planning. “We had another one yesterday, 4 months ago his [hemoglobin] A1c was 10.3%. It was 7.2% yesterday, and [his weight was] down 20 pounds.” In addition to positive clinical outcomes, patients made changes in areas of their health that they identified as important through the PHI, although these areas are not typically discussed in a clinical visit.
Patient Satisfaction
Although the overall goal of this pilot was to determine the feasibility of a clinical workflow embracing personalized health planning, data on patient satisfaction were collected from patients receiving care in the Hypertension Shared Medical Appointments Program at Bohnam. Ten patients were seen over the course of 5 visits. At each visit, they were asked to rate their satisfaction (Table).
Overall, patients were highly satisfied with their experience and the care they received: 91.7% reported exploring what they wanted for their health and setting shared goals; 100% reported that their providers truly listened to their needs and treated them with respect and dignity; and 97.2% reported that their experience was better than a traditional office visit. One participating physician noted that higher levels of patient and provider satisfaction are a product of this type of patient engagement. “I also think that looking at patient and provider satisfaction, the visits feel more meaningful, and there’s a better relationship built through this discussion,” he noted. These findings demonstrating increased satisfaction further suggest the benefits of personalized health planning approach.
Discussion
In 2012, the VHA National Leadership Council convened a Strategic Planning Summit to set goals and objectives to help the VHA be at the vanguard of a movement toward a more proactive health care delivery model. The first of 3 goals developed was to provide veterans personalized, proactive, patient-driven health care.13 It is becoming increasingly clear that truly affecting health and health outcomes requires motivated, engaged, and informed patients with a care delivery approach that provides ample opportunities for patient involvement and input in health care decision making.10,11
The OPCC&CT has ongoing initiatives driving innovation, research, education, and deployment across the system to set the stage for personalized, proactive, patient-driven care.20 Some of these innovations include clinician education in the concept of whole health; health coaching; group-based, peer-led approaches; and the expansion of CAM such as mind-body approaches, qi-gong, massage therapy, yoga, and acupuncture.21
The primary aim of the Whole Health in Primary Care Project was to determine the feasibility of using personalized health planning as the operational model to deliver personalized, proactive, patient-driven care. The decision was made to integrate personalized health planning into ongoing clinical operations rather than design clinical pilots de novo. This had the advantage of speed in starting the project but limited the ability to create an optimal workflow from scratch. Given the time and resources available for this study, it was not possible to obtain quantitative data particularly as it related to quantifying clinical outcomes.
Despite these limitations, early indications suggest that the personalized health planning process can serve as the operational clinical working model to enable personalized, proactive, patient-driven care in a variety of primary care settings. As noted by one nurse manager, preparing the personalized health plan made the initial visit “a bit longer.” However, after the first visit, monitoring health risk abatement and goal achievement is akin to what is currently done by reviewing problem lists. Thus, although the personalized health planning experience is just beginning, clinicians noted that it fostered a beneficial patient-clinician relationship. This deeper relationship between the patient and the clinician may be the most powerful signal that the process is worthwhile.
This pilot provided valuable information related to the implementation of a clinical workflow redesign, an initial step toward developing an optimized operational model of the PHP process. Additionally, although it is not yet possible to quantify the clinical impact of the personalized health planning, anecdotal evidence suggests its positive potential. Clinicians reported that patients were successful in managing a multitude of common chronic diseases, including weight loss, high blood pressure management, reduction of A1c, and improved sleep habits.
These findings compare with studies using similar approaches that demonstrated their value in the treatment of congestive heart failure, cardiovascular disease risk, type 2 diabetes, and postpartum weight retention.22-25 A growing body of evidence continues to affirm that a primary care model designed to deliver individualized care focused on improving health and an augmented patient-clinician relationship results in significant savings, primarily from reduced medical expenditures.26
This pilot provided an important opportunity to learn how to improve the effectiveness of personalized health planning and how to scale it. The experiences in Boston and Bonham demonstrated that personalized health planning can be integrated into diverse primary care settings with PACTs. The authors suggest that the knowledge gained from this project should be incorporated into new pilots at various clinical settings to determine the usefulness of the PHP for clinical indications beyond primary care. Specialty care clinics, home-based primary care services, and telehealth programs would be potential clinical applications for such pilots.
New pilots should be designed de novo and be of sufficient length to gain quantitative data on patient activation and clinical outcomes. Furthermore, future studies of personalized health planning should obtain input from the patient using Likert scales, surveys, and focus groups to gauge and quantify patient satisfaction and outcomes with the approach. Since patient engagement and better understanding of patients’ holistic needs are central to development of the PHP, patients need to be educated about this new approach to care and their active role in it.
The choice of the tools, including the HRA instrument, materials for orienting patients to their more active role in their care, the PHI, the PHP template to document shared goals, and other avenues used to engage patients, require refinement to improve their clarity, effectiveness of conveying the intended information, and ease of use. These studies demonstrated the vital need to address the best means to engage patients in understanding the value of their health to them since the clinician visit is likely to be an opportune teaching moment. Initial observations suggested that patients respond with different degrees of enthusiasm when given the opportunity to be more engaged in their care. Future pilots should clarify whether these differences stem from (a) how the invitation is presented; (b) individual differences in personality and preferences; (c) perceived clinical needs; or (d) unfamiliarity with the collaborative personalized health planning process.
The alignment of personalized health planning with outcomes data in the CPRS is essential for widespread adoption. Importantly, incentives and performance metrics will need to be redesigned to support the intended outcomes of using personalized health planning in clinical care. To that end, further investigation into the potential for cost savings associated with personalized health planning use is warranted, especially given studies that suggest high levels of patient engagement result in lower health care utilization expenditures.27
Additionally, wherever personalized health planning is initiated, employees across all levels of the system would benefit from training in patient engagement techniques and other means of attaining behavioral change. This would facilitate more effective use of time during the clinical visit and improve both the patient’s and the clinician’s satisfaction. Indeed, preliminary data indicate that this approach in a SMA setting is greatly valued by the patients.
Conclusions
The Whole Health in Primary Care Project was conducted to determine the feasibility of personalized health planning as the basis for primary care designed to facilitate personalized, proactive, patient-driven care. The pilot demonstrated that personalized health planning could be operational in VHA clinical settings and used to enhance patient-clinician engagement, establish shared health goals, and increase patient satisfaction. The personalized health planning process also provides a framework for the rational introduction of new capabilities to enhance prediction, clinical tracking, coordination of ancillary services, and clinical data collection. Future research should validate the efficacy of personalized health planning within both the VHA and health systems nationwide. Such research has the potential to refine this process so it becomes a key part of a personalized, proactive, patient-driven delivery approach.
Acknowledgements
We gratefully acknowledge the assistance of Cindy Mitchell at Duke University Medical Center with the editing and preparation of this manuscript. We also gratefully acknowledge the participation of the providers and patients at VA Boston Healthcare System and Sam Rayburn Memorial Veterans Center. Funding for this project was provided by VA777-12-C-002 to the Pacific Institute for Research and Evaluation through subcontracts to Ralph Snyderman, MD, and to the Duke University School of Nursing (Simmons PI.)
1. Anderson G. Chronic care: making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
2. Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119(3):263-270.
3. Dinan MA, Simmons LA, Snyderman R. Commentary: Personalized health planning and the Patient Protection and Affordable Care Act: an opportunity for academic medicine to lead health care reform. Acad Med. 2010;85(11):1665-1668.
4. Snyderman R, Yoediono Z. Prospective care: a personalized, preventative approach to medicine. Pharmacogenomics. 2006;7(1):5-9.
5. Snyderman R. Personalized health care: from theory to practice. Biotechnol. 2012;7(8):973-979.
6. Burnette R, Simmons LA, Snyderman R. Personalized health care as a pathway for the adoption of genomic medicine. J Pers Med. 2012;2(4):232-240.
7. Simmons LA, Dinan MA, Robinson TJ, Snyderman R. Personalized medicine is more than genomic medicine: confusion over terminology impedes progress towards personalized healthcare. J Pers Med. 2012;9(1):85-91.
8. Pelletier LR, Stichler JF. Patient-centered care and engagement: nurse leaders' imperative for health reform. J Nurs Adm. 2014;44(9):473-480.
9. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
10. Simmons LA, Wolever RQ, Bechard EM, Snyderman R. Patient engagement as a risk factor in personalized health care: a systematic review of the literature on chronic disease. Genome Med. 2014;6(2):16.
11. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520-526.
12. U.S. Department of Veterans Affairs. VA Patient Centered Care. U.S. Department of Veterans Affairs Website. http://www.va.gov/patientcenteredcare. Updated October 30, 2015. Accessed December 3, 2015.
13. Gaudet T. The Transformation of Healthcare. Paper presented at: 27th Annual Voluntary Health Leadership Conference; 2014; Tucson, Arizona.
14. U.S. Department of Veterans Affairs. VHA Strategic Plan FY 2013-2018. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_STRATEGIC_PLAN_FY2013-2018.pdf. Accessed December 3, 2015.
15. U.S. Department of Veterans Affairs. Blueprint for excellence. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed December 3, 2015.
16. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38-48.
17. Simmons LA, Wolever RQ. Integrative health coaching and motivational interviewing: synergistic approaches to behavior change in healthcare. Glob Adv Health Med. 2013;2(4):28-35.
18. Snyderman R, Dinan MA. Improving health by taking it personally. JAMA. 2010;303(4):363-364.
19. U.S. Department of Veterans Affairs. Computerized Patient Record System (CPRS) User Guide: GUI version. U.S Department of Veterans Affairs Website. http://www.va.gov/vdl/documents/Clinical/Comp_Patient_Recrd_Sys_(CPRS)/cprsguium.pdf. Published November 2015. Accessed December 3, 2015.
20. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Healthc Pap. 2005;5(4):10-24.
21. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. JRRD. 2011;48(9):1119-1128.
22. Whellan DJ, Gaulden L, Gattis WA, et al. The benefit of implementing a heart failure disease management program. Arch Intern Med. 2001;161(18):2223-2228.
23. Edelman D, Oddone EZ, Liebowitz RS, et al. A multidimensional integrative medicine intervention to improve cardiovascular risk. J Gen Intern Med. 2006;21(7):728-734.
24. Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36(4):629-639.
25. Yang NY, Wroth S, Parham C, Strait M, Simmons LA. Personalized health planning with integrative health coaching to reduce obesity risk among women gaining excess weight during pregnancy. Glob Adv Health Med. 2013;2(4):72-77.
26. Musich S, Klemes A, Kubica MA, Wang S, Hawkins K. Personalized preventive care reduces healthcare expenditures among Medicare advantage beneficiaries. Am J Manag Care. 2014;20(8):613-620.
27. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients' 'scores.' Health Aff. 2013;32(2):216-222.
Health care has become increasingly unaffordable in the U.S., yet it remains ineffective in preventing or effectively treating chronic diseases.1,2 Given the increasing burden of chronic disease on the American health care system, there is an effort to shift the practice of medicine away from its reactive, disease-oriented approach to a more sustainable proactive model.3-5
Personalized health care (PHC) is an approach to the practice of medicine where prediction, prevention, intense patient engagement, shared health care decision making, and coordination of care are essential to cost effectively facilitate better outcomes.3,5-7 Greater collaboration between patient and clinician replaces the traditional clinician-dominated dialogue with more effective patient-clinician partnerships.8,9 Patients’ knowledge, skills, and confidence to manage their health care have been linked to improved health outcomes, lower costs, and greater satisfaction with health care experiences.10,11
Personalized health care has been proposed as a means to achieve better patient engagement as part of an aligned, proactive clinical approach. At the heart of PHC is personalized health planning, wherein the patient and clinician develop shared health-related goals and a plan to achieve them.3
The VHA, the largest integrated health care system in the country, is on the vanguard of incorporating tenets of PHC into its delivery model. In 2011, the Office of Patient Centered Care and Cultural Transformation (OPCC&CT) was founded to “oversee the VHA’s cultural transformation to patient-centered care.”12 This undertaking represents “one of the most massive changes in the philosophy and process for health care delivery ever undertaken by an organized health care system.”13
The primary goal of the VHA’s strategic plan for 2013 to 2018 is to provide veterans personalized, proactive, patient-driven health care.14 The intention of this approach is to engage and inspire veterans to their highest possible level of health and well-being. A personalized approach requires a dynamic customization of care that is specifically relevant to the individual, based on factors such as medical conditions, genome, needs, values, and circumstances. In addition to being personalized, this approach must be proactive, and therefore, preventive and include strategies to strengthen the person’s innate capacity for enhancing health.
The third distinction of this new model health care is that it is patient-driven, rooted in and driven by that which matters most to people in their lives and aligns their health care with their day-to-day and long-term life goals.15 The latter may be the most critical of the 3 tenets, because a personalized, proactive approach that is not driven by an engaged and inspired individual will be unlikely to achieve adherence, let alone the highest level of health and well-being.
The VHA is uniquely positioned to optimize health and well-being for veterans due in part to a systemwide emphasis on training providers to promote and support behavior change through approaches including health coaching and motivational interviewing. These synergistic approaches used widely by clinicians throughout the VHA are influenced by the transtheoretical model (ie, the stages of change theory), which considers patients holistically and helps them identify intrinsic motivation to improve their health behaviors.16,17 The transformation occurring in the VHA is intended to shift the current disease-centric medical model to an approach that optimizes the health of veterans through patient-clinician engagement, health risk assessment (HRA), shared health goal creation, and a coordinated plan to attain them.12,13
Personalized Health Planning
In recognition of the need to deliver care that emphasizes prevention and coordination, the patient-centered medical home, patient-aligned care teams (PACTs), and the chronic care model were developed. All of these embrace concepts of patient engagement, shared decision making, and team-based care. However, none of these approaches have outlined a clinical workflow that systematically and proactively operationalizes these concepts with the creation of a risk-based personalized care approach. Personalized health planning provides a clinical workflow that operationalizes all these features (Figure 1).
Of central importance is the creation of a personalized health plan (PHP), which the patient and clinician develop collaboratively. The plan serves to organize and coordinate care while engaging the patient in the process of care delivery and appropriate self-management of health.3,5 This approach promotes personalized and proactive care that values the individual and fosters meaningful patient self-awareness and engagement through shared decision making.7
The personalized health planning process is composed of several key components (Figure 2).
With this information, the clinician develops a preliminary therapeutic plan to meet these goals and discusses this plan with the patient. The next component is the synthesis of the clinician’s goals and/or treatment plan with the priorities of the patient to establish shared clinician-patient goals. This is followed by the establishment of the PHP, which consists of the agreed upon shared clinician and patient goals, a therapeutic and wellness plan to meet them, metrics for tracking progress, consults and referrals, and a time frame for the patient to achieve the health goals.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
The final component is coordination of care and a formalized follow-up system in which the health care team monitors the patient’s progress and provides support by revisiting or updating the PHP at intervals determined by the provider, based on the level of monitoring required by the patient’s health status. This approach invites the patient to become an empowered member of the care team by creating a patient-clinician partnership and providing a model for delivering personalized, proactive, patient-driven care to individuals with a diverse range of needs.4,5,18
Design and Implementation
This project qualified as exempt through the Duke University Institutional Review Board. The primary aim of this pilot was to examine the feasibility of implementing personalized health planning into primary care settings and to develop a workable process that is scalable and customizable to inpatient and outpatient clinics of varying sizes for different patient populations within the VHA. The pilot included 5 clinics in 2 geographic areas that were selected for their facility’s leadership support and desire to participate.
The VA Boston Healthcare System implemented personalized health planning at 3 primary care clinics: Jamaica Plain Primary Care, Jamaica Plain Women’s Health, and Quincy Primary Care. Three distinct PACTs participated in Boston, each composed of a medical doctor or doctor of osteopathy, a registered nurse (RN) or health technician, and a medical support assistant. The Sam Rayburn Memorial Veterans Center in Bonham, Texas, implemented personalized health planning at 2 clinics: the Hypertension Shared Medical Appointment and the Domiciliary Inpatient Primary Care. At Bonham, a medical doctor, pharmacist, RN, and an integrated mental health provider led the shared medical appointment (SMA) with guest presenters for individual appointments, depending on the topic covered. A RN and social worker implemented personalized health planning in the domiciliary.
After receiving training in the personalized health planning process, each of the clinics’ multidisciplinary PACTs incorporated their custom personalized health planning workflow into patient encounters. During the intake process of the clinic visit, the patient received a Personal Health Inventory (PHI) to determine health care priorities. The OPCC&CT developed the PHI as a whole-health self-assessment tool to help patients reflect on their health and lives, including core values, disparities between current and desired states, and preparedness to make behavioral changes to promote health.
The PHI assisted with framing this whole health approach to clinical care by expanding the definition of health to include more holistic elements of well-being, such as spirituality, personal relationships, emotional health, and personal development. A visual representation of the whole health domains termed The Circle of Health introduced this concept to the patient and assisted with goal setting (Figure 3).12
The PHI organized the patient’s input and was provided to the clinician to contribute to the development of the shared therapeutic goals and a final treatment plan. The PHP provided the tool to organize the goals, plans, and care following the visit and to connect the patient to additional resources within the VHA to support goal attainment through skill building and support. Each clinical site developed a mechanism to follow up with these patients either telephonically or with additional clinic appointments. The participating clinics implemented their customized version of personalized health planning for an average of 3 months.
Personalized health planning and accompanying tools were used primarily in routine ambulatory care visits. They were also used in the Bonham domiciliary clinic, which provides care for veterans with mental illnesses or addictive disorders who require additional structure and support. The purpose of the pilot was to determine whether personalized health planning could be used within this population. Given the small sample size and incompleteness of data collected, the Bonham domiciliary group was not included in the participating patient total. Across the other 4 clinics a total of 153 patients participated in the 3-month pilot study by establishing shared health goals and plans to meet them.
Results and Evaluation
Using a structured interview guide, a total of 6 small group interviews with participating clinicians were held (3 in Boston and 3 in Bonham, N = 18). Qualitative methods for research and evaluation were used to capture the depth of responses and to provide complex descriptions of the clinicians’ perspectives on the implementation of the personalized health planning process. Two researchers reviewed the transcripts to identify and code themes, and a third researcher reviewed the transcripts to confirm themes and resolve any discrepancies.
Analysis of the interview data revealed 9 core themes related to the feasibility, effectiveness, and future dissemination of personalized health planning. These themes, described below with exemplar data, include (a) patient engagement; (b) clinical assessment; (c) goal setting; (d) clinical workflow; (e) resources and support for veterans and clinicians; (f) Computerized Patient Record System (CPRS) integration; (g) patient-clinician relationship; (h) clinical outcomes; and (i) patient satisfaction.
The purpose of this study was to evaluate the feasibility of introducing personalized health planning within the workflows of the clinics that were participating. As a consequence of this, interviews were held with clinic staff rather than patients. However, the authors did obtain patient satisfaction data from 10 patients who received care from the hypertension SMA and responded to TruthPoint questions after their visit (Table).
Patient Engagement
A central tenant of personalized health planning is to engage patients in their health and health care. Findings revealed that clinicians at both sites perceived the PHP as an effective tool for integrating patients as robust members of the care team. Clinicians noted that by asking patients what was important to them, the patients felt more empowered to actively engage in the clinical encounter and to take responsibility for their health decisions. One pharmacist noted, “Patients are more empowered…when you change how you’re having your conversation with them that helps people start to recognize that they are an active participant [sic] and they can have an impact and can help with minimizing medicines or trying other things.”
Clinicians reported that including patients as active members in their care created a level of buy-in that motivated behavioral changes, because the patients identified behaviors they wanted to change vs the clinician telling them what they should or should not do. A nurse manager reported, “The key is that (the health goal) is coming from the patient…. Once it comes out of their mouth, they’re thinking about it and it’s not the clinician telling them what they should or shouldn’t do, but it’s helping them…identify something that’s important that will keep them into staying the way they want to, for the reasons that they want to.”
Clinical Assessment
The HRA tools are a vital part of the personalized health planning process, as they focus on preventive strategies that are most important for the patient.4 Clinicians reported using the PHI and additional HRA tools as part of the pilot program. The PHI is a self-assessment tool designed to identify psychosocial, behavioral, and environmental issues that can impact the patient’s care and health status. Most clinicians found that the PHI helped to solicit patients’ input on what was important to them and their health status while introducing the new approach to care. One nurse commented, “I found [PHI] very effective if I could actually sit down and review it with them to see what it was that was truly important to them and explain that this new approach is for a better understanding.”
Clinicians also found that the PHI helped focus the patient’s attention toward self-care areas that facilitated the shared goal setting process with the clinician. It moved the clinical encounter away from the chief health problems and toward identifying what is important to the patient and leveraging his or her intrinsic motivation to support health promotion via lifestyle modification.
Goal Setting
Shared goal setting is a critical component of personalized health planning. The clinician and patient must agree about realistic goals to improve the patient’s health. Clinicians reported that the goal setting stage was most successful when patients were invited to guide the process and offered the goals themselves; ie, when it was not just patient-centered but patient-driven.
“Setting a goal with a patient is pretty easy because people have an idea of what they should be doing and what they want to be doing,” one clinician reported. “They know their goal. So it’s a matter of just listening, really listening, and seeing what they want…. It’s not incongruous to get the medical goal and the patient goal to match.”
Patients were amenable to this collaborative approach to goal setting, and there was often commonality between the clinician’s goals and what was important to the patient. Occasionally, the patient set goals in seemingly unrelated areas that facilitated chronic disease management.
“One of our hypertensive patients wanted to work on things that are external that they felt are stressors that actually caused their blood pressure to be high,” a pharmacist recalled. “At the end of the day they wanted to control their environment better so that they could see if they could then be off of antihypertensives altogether. It appears that may be the case right now. That this individual has been able to accomplish that, which I thought was amazing, and since it’s still new, I’m still a little bit skeptical.... Is that possible? But if at the end of the day that is an outcome that we see from doing this, I think that’s wonderful.”
Clinicians reported that follow-up with the patient was a critical aspect of goal setting, because it improved accountability and helped track progress and health outcomes. However, due to the 3-month time limit of the pilot, there was insufficient time to get uniform data on the formalized follow-up systems developed by each clinic.
Clinical Workflow
Examining the feasibility of creating a process to incorporate personalized health planning into a busy primary care clinic was one of the major aims of this pilot. As such, issues of time, staff responsibilities, and use of the CPRS and other systems to facilitate the process were challenges that each clinic addressed in slightly different ways and with varying success. One method was to leverage the SMA for a group of patients with a common diagnosis to discuss their goals, provide accountability, and improve access to a medical team.
Another innovative approach was utilizing medical support administrators and health technicians to front-load some of the introductory information and patient education in the waiting room or during the intake process. Despite these efforts, some clinicians thought that the personalized health planning process might take longer than the traditional clinical encounter. One nurse manager commented, “I think it did affect the length of visits…it has made them a little bit longer.”
Resources and Support
The VHA has been undergoing a shift from an emphasis on tertiary care to include a greater focus on primary care. Part of this shift has been an investment in complementary and alternative medicine (CAM). The PHP helped clinicians explore what resources existed at their facility to support veterans in accomplishing their goals, including CAM. One nurse reported, “It made us look into other avenues that were actually available at the VHA that we didn’t even know we had…the acupuncture, the qigong, the voluntary services getting the veterans involved.”
Clinicians also identified the need for patient education in the concepts of whole health, personalized care, and patient involvement as necessary for moving the piloted approach forward. A nurse noted that “for [personalized health planning] to work well, [the patients] need more orientation and education upfront systemwide so that when they get into an appointment with us, we’re not starting at explaining the whole world view of partnership and doing things differently.”
Resources for clinicians were just as critical as resources for patients in facilitating the personalized health planning process. Specifically, most clinicians identified their own education and training in techniques to engage the patient in a meaningful way via motivational interviewing and health coaching complemented the personalized approach to care, particularly for shared goal setting,
CPRS Integration
The CPRS is an integrated, electronic patient record system that provides a single interface for clinicians to manage patient care as well as an efficient means for others to access and use patient information.19 The most commonly cited challenge in the pilot was the lack of available staff and time in the patient visit to complete the PHP while completing documentation requirements in CPRS.
One clinician stated, “For clinicians, the barriers…it’s time to get through the reminders and preventatives.” Clinicians reported that the process and the CPRS documentation were misaligned and lacked integration to coordinate care or support health planning. Moreover, clinicians reported that the data being collected did not support patient-centered care.
Patient-Clinician Relationship
A significant strength of personalized health planning was that it fostered a beneficial patient-clinician relationship that promoted greater depth of care. One clinician noted, “I think that it adds a more personalized dimension to the whole patient visit.” In addition to experiencing a deeper relationship with their patients, clinicians also expressed having higher levels of job satisfaction and relished the opportunity to connect with their patients in a more personal way.
Clinicians also reported that patients seemed more satisfied with the experience. One nurse commented, “They really respond to it very well when they figure out that you care about them as a whole… it’s not just about the disease process anymore.”
Clinical Outcomes
Clinicians reported a number of positive health outcomes during the pilot. One physician reported, “I have a patient, he had a follow-up today, a 29-year-old veteran, who was 260 pounds 5 months ago, and he’s 230 pounds today. He comes in monthly to see the nurse to let us know he’s doing it.”
The same physician also shared a similar transformation in a patient as a result of personalized health planning. “We had another one yesterday, 4 months ago his [hemoglobin] A1c was 10.3%. It was 7.2% yesterday, and [his weight was] down 20 pounds.” In addition to positive clinical outcomes, patients made changes in areas of their health that they identified as important through the PHI, although these areas are not typically discussed in a clinical visit.
Patient Satisfaction
Although the overall goal of this pilot was to determine the feasibility of a clinical workflow embracing personalized health planning, data on patient satisfaction were collected from patients receiving care in the Hypertension Shared Medical Appointments Program at Bohnam. Ten patients were seen over the course of 5 visits. At each visit, they were asked to rate their satisfaction (Table).
Overall, patients were highly satisfied with their experience and the care they received: 91.7% reported exploring what they wanted for their health and setting shared goals; 100% reported that their providers truly listened to their needs and treated them with respect and dignity; and 97.2% reported that their experience was better than a traditional office visit. One participating physician noted that higher levels of patient and provider satisfaction are a product of this type of patient engagement. “I also think that looking at patient and provider satisfaction, the visits feel more meaningful, and there’s a better relationship built through this discussion,” he noted. These findings demonstrating increased satisfaction further suggest the benefits of personalized health planning approach.
Discussion
In 2012, the VHA National Leadership Council convened a Strategic Planning Summit to set goals and objectives to help the VHA be at the vanguard of a movement toward a more proactive health care delivery model. The first of 3 goals developed was to provide veterans personalized, proactive, patient-driven health care.13 It is becoming increasingly clear that truly affecting health and health outcomes requires motivated, engaged, and informed patients with a care delivery approach that provides ample opportunities for patient involvement and input in health care decision making.10,11
The OPCC&CT has ongoing initiatives driving innovation, research, education, and deployment across the system to set the stage for personalized, proactive, patient-driven care.20 Some of these innovations include clinician education in the concept of whole health; health coaching; group-based, peer-led approaches; and the expansion of CAM such as mind-body approaches, qi-gong, massage therapy, yoga, and acupuncture.21
The primary aim of the Whole Health in Primary Care Project was to determine the feasibility of using personalized health planning as the operational model to deliver personalized, proactive, patient-driven care. The decision was made to integrate personalized health planning into ongoing clinical operations rather than design clinical pilots de novo. This had the advantage of speed in starting the project but limited the ability to create an optimal workflow from scratch. Given the time and resources available for this study, it was not possible to obtain quantitative data particularly as it related to quantifying clinical outcomes.
Despite these limitations, early indications suggest that the personalized health planning process can serve as the operational clinical working model to enable personalized, proactive, patient-driven care in a variety of primary care settings. As noted by one nurse manager, preparing the personalized health plan made the initial visit “a bit longer.” However, after the first visit, monitoring health risk abatement and goal achievement is akin to what is currently done by reviewing problem lists. Thus, although the personalized health planning experience is just beginning, clinicians noted that it fostered a beneficial patient-clinician relationship. This deeper relationship between the patient and the clinician may be the most powerful signal that the process is worthwhile.
This pilot provided valuable information related to the implementation of a clinical workflow redesign, an initial step toward developing an optimized operational model of the PHP process. Additionally, although it is not yet possible to quantify the clinical impact of the personalized health planning, anecdotal evidence suggests its positive potential. Clinicians reported that patients were successful in managing a multitude of common chronic diseases, including weight loss, high blood pressure management, reduction of A1c, and improved sleep habits.
These findings compare with studies using similar approaches that demonstrated their value in the treatment of congestive heart failure, cardiovascular disease risk, type 2 diabetes, and postpartum weight retention.22-25 A growing body of evidence continues to affirm that a primary care model designed to deliver individualized care focused on improving health and an augmented patient-clinician relationship results in significant savings, primarily from reduced medical expenditures.26
This pilot provided an important opportunity to learn how to improve the effectiveness of personalized health planning and how to scale it. The experiences in Boston and Bonham demonstrated that personalized health planning can be integrated into diverse primary care settings with PACTs. The authors suggest that the knowledge gained from this project should be incorporated into new pilots at various clinical settings to determine the usefulness of the PHP for clinical indications beyond primary care. Specialty care clinics, home-based primary care services, and telehealth programs would be potential clinical applications for such pilots.
New pilots should be designed de novo and be of sufficient length to gain quantitative data on patient activation and clinical outcomes. Furthermore, future studies of personalized health planning should obtain input from the patient using Likert scales, surveys, and focus groups to gauge and quantify patient satisfaction and outcomes with the approach. Since patient engagement and better understanding of patients’ holistic needs are central to development of the PHP, patients need to be educated about this new approach to care and their active role in it.
The choice of the tools, including the HRA instrument, materials for orienting patients to their more active role in their care, the PHI, the PHP template to document shared goals, and other avenues used to engage patients, require refinement to improve their clarity, effectiveness of conveying the intended information, and ease of use. These studies demonstrated the vital need to address the best means to engage patients in understanding the value of their health to them since the clinician visit is likely to be an opportune teaching moment. Initial observations suggested that patients respond with different degrees of enthusiasm when given the opportunity to be more engaged in their care. Future pilots should clarify whether these differences stem from (a) how the invitation is presented; (b) individual differences in personality and preferences; (c) perceived clinical needs; or (d) unfamiliarity with the collaborative personalized health planning process.
The alignment of personalized health planning with outcomes data in the CPRS is essential for widespread adoption. Importantly, incentives and performance metrics will need to be redesigned to support the intended outcomes of using personalized health planning in clinical care. To that end, further investigation into the potential for cost savings associated with personalized health planning use is warranted, especially given studies that suggest high levels of patient engagement result in lower health care utilization expenditures.27
Additionally, wherever personalized health planning is initiated, employees across all levels of the system would benefit from training in patient engagement techniques and other means of attaining behavioral change. This would facilitate more effective use of time during the clinical visit and improve both the patient’s and the clinician’s satisfaction. Indeed, preliminary data indicate that this approach in a SMA setting is greatly valued by the patients.
Conclusions
The Whole Health in Primary Care Project was conducted to determine the feasibility of personalized health planning as the basis for primary care designed to facilitate personalized, proactive, patient-driven care. The pilot demonstrated that personalized health planning could be operational in VHA clinical settings and used to enhance patient-clinician engagement, establish shared health goals, and increase patient satisfaction. The personalized health planning process also provides a framework for the rational introduction of new capabilities to enhance prediction, clinical tracking, coordination of ancillary services, and clinical data collection. Future research should validate the efficacy of personalized health planning within both the VHA and health systems nationwide. Such research has the potential to refine this process so it becomes a key part of a personalized, proactive, patient-driven delivery approach.
Acknowledgements
We gratefully acknowledge the assistance of Cindy Mitchell at Duke University Medical Center with the editing and preparation of this manuscript. We also gratefully acknowledge the participation of the providers and patients at VA Boston Healthcare System and Sam Rayburn Memorial Veterans Center. Funding for this project was provided by VA777-12-C-002 to the Pacific Institute for Research and Evaluation through subcontracts to Ralph Snyderman, MD, and to the Duke University School of Nursing (Simmons PI.)
Health care has become increasingly unaffordable in the U.S., yet it remains ineffective in preventing or effectively treating chronic diseases.1,2 Given the increasing burden of chronic disease on the American health care system, there is an effort to shift the practice of medicine away from its reactive, disease-oriented approach to a more sustainable proactive model.3-5
Personalized health care (PHC) is an approach to the practice of medicine where prediction, prevention, intense patient engagement, shared health care decision making, and coordination of care are essential to cost effectively facilitate better outcomes.3,5-7 Greater collaboration between patient and clinician replaces the traditional clinician-dominated dialogue with more effective patient-clinician partnerships.8,9 Patients’ knowledge, skills, and confidence to manage their health care have been linked to improved health outcomes, lower costs, and greater satisfaction with health care experiences.10,11
Personalized health care has been proposed as a means to achieve better patient engagement as part of an aligned, proactive clinical approach. At the heart of PHC is personalized health planning, wherein the patient and clinician develop shared health-related goals and a plan to achieve them.3
The VHA, the largest integrated health care system in the country, is on the vanguard of incorporating tenets of PHC into its delivery model. In 2011, the Office of Patient Centered Care and Cultural Transformation (OPCC&CT) was founded to “oversee the VHA’s cultural transformation to patient-centered care.”12 This undertaking represents “one of the most massive changes in the philosophy and process for health care delivery ever undertaken by an organized health care system.”13
The primary goal of the VHA’s strategic plan for 2013 to 2018 is to provide veterans personalized, proactive, patient-driven health care.14 The intention of this approach is to engage and inspire veterans to their highest possible level of health and well-being. A personalized approach requires a dynamic customization of care that is specifically relevant to the individual, based on factors such as medical conditions, genome, needs, values, and circumstances. In addition to being personalized, this approach must be proactive, and therefore, preventive and include strategies to strengthen the person’s innate capacity for enhancing health.
The third distinction of this new model health care is that it is patient-driven, rooted in and driven by that which matters most to people in their lives and aligns their health care with their day-to-day and long-term life goals.15 The latter may be the most critical of the 3 tenets, because a personalized, proactive approach that is not driven by an engaged and inspired individual will be unlikely to achieve adherence, let alone the highest level of health and well-being.
The VHA is uniquely positioned to optimize health and well-being for veterans due in part to a systemwide emphasis on training providers to promote and support behavior change through approaches including health coaching and motivational interviewing. These synergistic approaches used widely by clinicians throughout the VHA are influenced by the transtheoretical model (ie, the stages of change theory), which considers patients holistically and helps them identify intrinsic motivation to improve their health behaviors.16,17 The transformation occurring in the VHA is intended to shift the current disease-centric medical model to an approach that optimizes the health of veterans through patient-clinician engagement, health risk assessment (HRA), shared health goal creation, and a coordinated plan to attain them.12,13
Personalized Health Planning
In recognition of the need to deliver care that emphasizes prevention and coordination, the patient-centered medical home, patient-aligned care teams (PACTs), and the chronic care model were developed. All of these embrace concepts of patient engagement, shared decision making, and team-based care. However, none of these approaches have outlined a clinical workflow that systematically and proactively operationalizes these concepts with the creation of a risk-based personalized care approach. Personalized health planning provides a clinical workflow that operationalizes all these features (Figure 1).
Of central importance is the creation of a personalized health plan (PHP), which the patient and clinician develop collaboratively. The plan serves to organize and coordinate care while engaging the patient in the process of care delivery and appropriate self-management of health.3,5 This approach promotes personalized and proactive care that values the individual and fosters meaningful patient self-awareness and engagement through shared decision making.7
The personalized health planning process is composed of several key components (Figure 2).
With this information, the clinician develops a preliminary therapeutic plan to meet these goals and discusses this plan with the patient. The next component is the synthesis of the clinician’s goals and/or treatment plan with the priorities of the patient to establish shared clinician-patient goals. This is followed by the establishment of the PHP, which consists of the agreed upon shared clinician and patient goals, a therapeutic and wellness plan to meet them, metrics for tracking progress, consults and referrals, and a time frame for the patient to achieve the health goals.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
The final component is coordination of care and a formalized follow-up system in which the health care team monitors the patient’s progress and provides support by revisiting or updating the PHP at intervals determined by the provider, based on the level of monitoring required by the patient’s health status. This approach invites the patient to become an empowered member of the care team by creating a patient-clinician partnership and providing a model for delivering personalized, proactive, patient-driven care to individuals with a diverse range of needs.4,5,18
Design and Implementation
This project qualified as exempt through the Duke University Institutional Review Board. The primary aim of this pilot was to examine the feasibility of implementing personalized health planning into primary care settings and to develop a workable process that is scalable and customizable to inpatient and outpatient clinics of varying sizes for different patient populations within the VHA. The pilot included 5 clinics in 2 geographic areas that were selected for their facility’s leadership support and desire to participate.
The VA Boston Healthcare System implemented personalized health planning at 3 primary care clinics: Jamaica Plain Primary Care, Jamaica Plain Women’s Health, and Quincy Primary Care. Three distinct PACTs participated in Boston, each composed of a medical doctor or doctor of osteopathy, a registered nurse (RN) or health technician, and a medical support assistant. The Sam Rayburn Memorial Veterans Center in Bonham, Texas, implemented personalized health planning at 2 clinics: the Hypertension Shared Medical Appointment and the Domiciliary Inpatient Primary Care. At Bonham, a medical doctor, pharmacist, RN, and an integrated mental health provider led the shared medical appointment (SMA) with guest presenters for individual appointments, depending on the topic covered. A RN and social worker implemented personalized health planning in the domiciliary.
After receiving training in the personalized health planning process, each of the clinics’ multidisciplinary PACTs incorporated their custom personalized health planning workflow into patient encounters. During the intake process of the clinic visit, the patient received a Personal Health Inventory (PHI) to determine health care priorities. The OPCC&CT developed the PHI as a whole-health self-assessment tool to help patients reflect on their health and lives, including core values, disparities between current and desired states, and preparedness to make behavioral changes to promote health.
The PHI assisted with framing this whole health approach to clinical care by expanding the definition of health to include more holistic elements of well-being, such as spirituality, personal relationships, emotional health, and personal development. A visual representation of the whole health domains termed The Circle of Health introduced this concept to the patient and assisted with goal setting (Figure 3).12
The PHI organized the patient’s input and was provided to the clinician to contribute to the development of the shared therapeutic goals and a final treatment plan. The PHP provided the tool to organize the goals, plans, and care following the visit and to connect the patient to additional resources within the VHA to support goal attainment through skill building and support. Each clinical site developed a mechanism to follow up with these patients either telephonically or with additional clinic appointments. The participating clinics implemented their customized version of personalized health planning for an average of 3 months.
Personalized health planning and accompanying tools were used primarily in routine ambulatory care visits. They were also used in the Bonham domiciliary clinic, which provides care for veterans with mental illnesses or addictive disorders who require additional structure and support. The purpose of the pilot was to determine whether personalized health planning could be used within this population. Given the small sample size and incompleteness of data collected, the Bonham domiciliary group was not included in the participating patient total. Across the other 4 clinics a total of 153 patients participated in the 3-month pilot study by establishing shared health goals and plans to meet them.
Results and Evaluation
Using a structured interview guide, a total of 6 small group interviews with participating clinicians were held (3 in Boston and 3 in Bonham, N = 18). Qualitative methods for research and evaluation were used to capture the depth of responses and to provide complex descriptions of the clinicians’ perspectives on the implementation of the personalized health planning process. Two researchers reviewed the transcripts to identify and code themes, and a third researcher reviewed the transcripts to confirm themes and resolve any discrepancies.
Analysis of the interview data revealed 9 core themes related to the feasibility, effectiveness, and future dissemination of personalized health planning. These themes, described below with exemplar data, include (a) patient engagement; (b) clinical assessment; (c) goal setting; (d) clinical workflow; (e) resources and support for veterans and clinicians; (f) Computerized Patient Record System (CPRS) integration; (g) patient-clinician relationship; (h) clinical outcomes; and (i) patient satisfaction.
The purpose of this study was to evaluate the feasibility of introducing personalized health planning within the workflows of the clinics that were participating. As a consequence of this, interviews were held with clinic staff rather than patients. However, the authors did obtain patient satisfaction data from 10 patients who received care from the hypertension SMA and responded to TruthPoint questions after their visit (Table).
Patient Engagement
A central tenant of personalized health planning is to engage patients in their health and health care. Findings revealed that clinicians at both sites perceived the PHP as an effective tool for integrating patients as robust members of the care team. Clinicians noted that by asking patients what was important to them, the patients felt more empowered to actively engage in the clinical encounter and to take responsibility for their health decisions. One pharmacist noted, “Patients are more empowered…when you change how you’re having your conversation with them that helps people start to recognize that they are an active participant [sic] and they can have an impact and can help with minimizing medicines or trying other things.”
Clinicians reported that including patients as active members in their care created a level of buy-in that motivated behavioral changes, because the patients identified behaviors they wanted to change vs the clinician telling them what they should or should not do. A nurse manager reported, “The key is that (the health goal) is coming from the patient…. Once it comes out of their mouth, they’re thinking about it and it’s not the clinician telling them what they should or shouldn’t do, but it’s helping them…identify something that’s important that will keep them into staying the way they want to, for the reasons that they want to.”
Clinical Assessment
The HRA tools are a vital part of the personalized health planning process, as they focus on preventive strategies that are most important for the patient.4 Clinicians reported using the PHI and additional HRA tools as part of the pilot program. The PHI is a self-assessment tool designed to identify psychosocial, behavioral, and environmental issues that can impact the patient’s care and health status. Most clinicians found that the PHI helped to solicit patients’ input on what was important to them and their health status while introducing the new approach to care. One nurse commented, “I found [PHI] very effective if I could actually sit down and review it with them to see what it was that was truly important to them and explain that this new approach is for a better understanding.”
Clinicians also found that the PHI helped focus the patient’s attention toward self-care areas that facilitated the shared goal setting process with the clinician. It moved the clinical encounter away from the chief health problems and toward identifying what is important to the patient and leveraging his or her intrinsic motivation to support health promotion via lifestyle modification.
Goal Setting
Shared goal setting is a critical component of personalized health planning. The clinician and patient must agree about realistic goals to improve the patient’s health. Clinicians reported that the goal setting stage was most successful when patients were invited to guide the process and offered the goals themselves; ie, when it was not just patient-centered but patient-driven.
“Setting a goal with a patient is pretty easy because people have an idea of what they should be doing and what they want to be doing,” one clinician reported. “They know their goal. So it’s a matter of just listening, really listening, and seeing what they want…. It’s not incongruous to get the medical goal and the patient goal to match.”
Patients were amenable to this collaborative approach to goal setting, and there was often commonality between the clinician’s goals and what was important to the patient. Occasionally, the patient set goals in seemingly unrelated areas that facilitated chronic disease management.
“One of our hypertensive patients wanted to work on things that are external that they felt are stressors that actually caused their blood pressure to be high,” a pharmacist recalled. “At the end of the day they wanted to control their environment better so that they could see if they could then be off of antihypertensives altogether. It appears that may be the case right now. That this individual has been able to accomplish that, which I thought was amazing, and since it’s still new, I’m still a little bit skeptical.... Is that possible? But if at the end of the day that is an outcome that we see from doing this, I think that’s wonderful.”
Clinicians reported that follow-up with the patient was a critical aspect of goal setting, because it improved accountability and helped track progress and health outcomes. However, due to the 3-month time limit of the pilot, there was insufficient time to get uniform data on the formalized follow-up systems developed by each clinic.
Clinical Workflow
Examining the feasibility of creating a process to incorporate personalized health planning into a busy primary care clinic was one of the major aims of this pilot. As such, issues of time, staff responsibilities, and use of the CPRS and other systems to facilitate the process were challenges that each clinic addressed in slightly different ways and with varying success. One method was to leverage the SMA for a group of patients with a common diagnosis to discuss their goals, provide accountability, and improve access to a medical team.
Another innovative approach was utilizing medical support administrators and health technicians to front-load some of the introductory information and patient education in the waiting room or during the intake process. Despite these efforts, some clinicians thought that the personalized health planning process might take longer than the traditional clinical encounter. One nurse manager commented, “I think it did affect the length of visits…it has made them a little bit longer.”
Resources and Support
The VHA has been undergoing a shift from an emphasis on tertiary care to include a greater focus on primary care. Part of this shift has been an investment in complementary and alternative medicine (CAM). The PHP helped clinicians explore what resources existed at their facility to support veterans in accomplishing their goals, including CAM. One nurse reported, “It made us look into other avenues that were actually available at the VHA that we didn’t even know we had…the acupuncture, the qigong, the voluntary services getting the veterans involved.”
Clinicians also identified the need for patient education in the concepts of whole health, personalized care, and patient involvement as necessary for moving the piloted approach forward. A nurse noted that “for [personalized health planning] to work well, [the patients] need more orientation and education upfront systemwide so that when they get into an appointment with us, we’re not starting at explaining the whole world view of partnership and doing things differently.”
Resources for clinicians were just as critical as resources for patients in facilitating the personalized health planning process. Specifically, most clinicians identified their own education and training in techniques to engage the patient in a meaningful way via motivational interviewing and health coaching complemented the personalized approach to care, particularly for shared goal setting,
CPRS Integration
The CPRS is an integrated, electronic patient record system that provides a single interface for clinicians to manage patient care as well as an efficient means for others to access and use patient information.19 The most commonly cited challenge in the pilot was the lack of available staff and time in the patient visit to complete the PHP while completing documentation requirements in CPRS.
One clinician stated, “For clinicians, the barriers…it’s time to get through the reminders and preventatives.” Clinicians reported that the process and the CPRS documentation were misaligned and lacked integration to coordinate care or support health planning. Moreover, clinicians reported that the data being collected did not support patient-centered care.
Patient-Clinician Relationship
A significant strength of personalized health planning was that it fostered a beneficial patient-clinician relationship that promoted greater depth of care. One clinician noted, “I think that it adds a more personalized dimension to the whole patient visit.” In addition to experiencing a deeper relationship with their patients, clinicians also expressed having higher levels of job satisfaction and relished the opportunity to connect with their patients in a more personal way.
Clinicians also reported that patients seemed more satisfied with the experience. One nurse commented, “They really respond to it very well when they figure out that you care about them as a whole… it’s not just about the disease process anymore.”
Clinical Outcomes
Clinicians reported a number of positive health outcomes during the pilot. One physician reported, “I have a patient, he had a follow-up today, a 29-year-old veteran, who was 260 pounds 5 months ago, and he’s 230 pounds today. He comes in monthly to see the nurse to let us know he’s doing it.”
The same physician also shared a similar transformation in a patient as a result of personalized health planning. “We had another one yesterday, 4 months ago his [hemoglobin] A1c was 10.3%. It was 7.2% yesterday, and [his weight was] down 20 pounds.” In addition to positive clinical outcomes, patients made changes in areas of their health that they identified as important through the PHI, although these areas are not typically discussed in a clinical visit.
Patient Satisfaction
Although the overall goal of this pilot was to determine the feasibility of a clinical workflow embracing personalized health planning, data on patient satisfaction were collected from patients receiving care in the Hypertension Shared Medical Appointments Program at Bohnam. Ten patients were seen over the course of 5 visits. At each visit, they were asked to rate their satisfaction (Table).
Overall, patients were highly satisfied with their experience and the care they received: 91.7% reported exploring what they wanted for their health and setting shared goals; 100% reported that their providers truly listened to their needs and treated them with respect and dignity; and 97.2% reported that their experience was better than a traditional office visit. One participating physician noted that higher levels of patient and provider satisfaction are a product of this type of patient engagement. “I also think that looking at patient and provider satisfaction, the visits feel more meaningful, and there’s a better relationship built through this discussion,” he noted. These findings demonstrating increased satisfaction further suggest the benefits of personalized health planning approach.
Discussion
In 2012, the VHA National Leadership Council convened a Strategic Planning Summit to set goals and objectives to help the VHA be at the vanguard of a movement toward a more proactive health care delivery model. The first of 3 goals developed was to provide veterans personalized, proactive, patient-driven health care.13 It is becoming increasingly clear that truly affecting health and health outcomes requires motivated, engaged, and informed patients with a care delivery approach that provides ample opportunities for patient involvement and input in health care decision making.10,11
The OPCC&CT has ongoing initiatives driving innovation, research, education, and deployment across the system to set the stage for personalized, proactive, patient-driven care.20 Some of these innovations include clinician education in the concept of whole health; health coaching; group-based, peer-led approaches; and the expansion of CAM such as mind-body approaches, qi-gong, massage therapy, yoga, and acupuncture.21
The primary aim of the Whole Health in Primary Care Project was to determine the feasibility of using personalized health planning as the operational model to deliver personalized, proactive, patient-driven care. The decision was made to integrate personalized health planning into ongoing clinical operations rather than design clinical pilots de novo. This had the advantage of speed in starting the project but limited the ability to create an optimal workflow from scratch. Given the time and resources available for this study, it was not possible to obtain quantitative data particularly as it related to quantifying clinical outcomes.
Despite these limitations, early indications suggest that the personalized health planning process can serve as the operational clinical working model to enable personalized, proactive, patient-driven care in a variety of primary care settings. As noted by one nurse manager, preparing the personalized health plan made the initial visit “a bit longer.” However, after the first visit, monitoring health risk abatement and goal achievement is akin to what is currently done by reviewing problem lists. Thus, although the personalized health planning experience is just beginning, clinicians noted that it fostered a beneficial patient-clinician relationship. This deeper relationship between the patient and the clinician may be the most powerful signal that the process is worthwhile.
This pilot provided valuable information related to the implementation of a clinical workflow redesign, an initial step toward developing an optimized operational model of the PHP process. Additionally, although it is not yet possible to quantify the clinical impact of the personalized health planning, anecdotal evidence suggests its positive potential. Clinicians reported that patients were successful in managing a multitude of common chronic diseases, including weight loss, high blood pressure management, reduction of A1c, and improved sleep habits.
These findings compare with studies using similar approaches that demonstrated their value in the treatment of congestive heart failure, cardiovascular disease risk, type 2 diabetes, and postpartum weight retention.22-25 A growing body of evidence continues to affirm that a primary care model designed to deliver individualized care focused on improving health and an augmented patient-clinician relationship results in significant savings, primarily from reduced medical expenditures.26
This pilot provided an important opportunity to learn how to improve the effectiveness of personalized health planning and how to scale it. The experiences in Boston and Bonham demonstrated that personalized health planning can be integrated into diverse primary care settings with PACTs. The authors suggest that the knowledge gained from this project should be incorporated into new pilots at various clinical settings to determine the usefulness of the PHP for clinical indications beyond primary care. Specialty care clinics, home-based primary care services, and telehealth programs would be potential clinical applications for such pilots.
New pilots should be designed de novo and be of sufficient length to gain quantitative data on patient activation and clinical outcomes. Furthermore, future studies of personalized health planning should obtain input from the patient using Likert scales, surveys, and focus groups to gauge and quantify patient satisfaction and outcomes with the approach. Since patient engagement and better understanding of patients’ holistic needs are central to development of the PHP, patients need to be educated about this new approach to care and their active role in it.
The choice of the tools, including the HRA instrument, materials for orienting patients to their more active role in their care, the PHI, the PHP template to document shared goals, and other avenues used to engage patients, require refinement to improve their clarity, effectiveness of conveying the intended information, and ease of use. These studies demonstrated the vital need to address the best means to engage patients in understanding the value of their health to them since the clinician visit is likely to be an opportune teaching moment. Initial observations suggested that patients respond with different degrees of enthusiasm when given the opportunity to be more engaged in their care. Future pilots should clarify whether these differences stem from (a) how the invitation is presented; (b) individual differences in personality and preferences; (c) perceived clinical needs; or (d) unfamiliarity with the collaborative personalized health planning process.
The alignment of personalized health planning with outcomes data in the CPRS is essential for widespread adoption. Importantly, incentives and performance metrics will need to be redesigned to support the intended outcomes of using personalized health planning in clinical care. To that end, further investigation into the potential for cost savings associated with personalized health planning use is warranted, especially given studies that suggest high levels of patient engagement result in lower health care utilization expenditures.27
Additionally, wherever personalized health planning is initiated, employees across all levels of the system would benefit from training in patient engagement techniques and other means of attaining behavioral change. This would facilitate more effective use of time during the clinical visit and improve both the patient’s and the clinician’s satisfaction. Indeed, preliminary data indicate that this approach in a SMA setting is greatly valued by the patients.
Conclusions
The Whole Health in Primary Care Project was conducted to determine the feasibility of personalized health planning as the basis for primary care designed to facilitate personalized, proactive, patient-driven care. The pilot demonstrated that personalized health planning could be operational in VHA clinical settings and used to enhance patient-clinician engagement, establish shared health goals, and increase patient satisfaction. The personalized health planning process also provides a framework for the rational introduction of new capabilities to enhance prediction, clinical tracking, coordination of ancillary services, and clinical data collection. Future research should validate the efficacy of personalized health planning within both the VHA and health systems nationwide. Such research has the potential to refine this process so it becomes a key part of a personalized, proactive, patient-driven delivery approach.
Acknowledgements
We gratefully acknowledge the assistance of Cindy Mitchell at Duke University Medical Center with the editing and preparation of this manuscript. We also gratefully acknowledge the participation of the providers and patients at VA Boston Healthcare System and Sam Rayburn Memorial Veterans Center. Funding for this project was provided by VA777-12-C-002 to the Pacific Institute for Research and Evaluation through subcontracts to Ralph Snyderman, MD, and to the Duke University School of Nursing (Simmons PI.)
1. Anderson G. Chronic care: making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
2. Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119(3):263-270.
3. Dinan MA, Simmons LA, Snyderman R. Commentary: Personalized health planning and the Patient Protection and Affordable Care Act: an opportunity for academic medicine to lead health care reform. Acad Med. 2010;85(11):1665-1668.
4. Snyderman R, Yoediono Z. Prospective care: a personalized, preventative approach to medicine. Pharmacogenomics. 2006;7(1):5-9.
5. Snyderman R. Personalized health care: from theory to practice. Biotechnol. 2012;7(8):973-979.
6. Burnette R, Simmons LA, Snyderman R. Personalized health care as a pathway for the adoption of genomic medicine. J Pers Med. 2012;2(4):232-240.
7. Simmons LA, Dinan MA, Robinson TJ, Snyderman R. Personalized medicine is more than genomic medicine: confusion over terminology impedes progress towards personalized healthcare. J Pers Med. 2012;9(1):85-91.
8. Pelletier LR, Stichler JF. Patient-centered care and engagement: nurse leaders' imperative for health reform. J Nurs Adm. 2014;44(9):473-480.
9. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
10. Simmons LA, Wolever RQ, Bechard EM, Snyderman R. Patient engagement as a risk factor in personalized health care: a systematic review of the literature on chronic disease. Genome Med. 2014;6(2):16.
11. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520-526.
12. U.S. Department of Veterans Affairs. VA Patient Centered Care. U.S. Department of Veterans Affairs Website. http://www.va.gov/patientcenteredcare. Updated October 30, 2015. Accessed December 3, 2015.
13. Gaudet T. The Transformation of Healthcare. Paper presented at: 27th Annual Voluntary Health Leadership Conference; 2014; Tucson, Arizona.
14. U.S. Department of Veterans Affairs. VHA Strategic Plan FY 2013-2018. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_STRATEGIC_PLAN_FY2013-2018.pdf. Accessed December 3, 2015.
15. U.S. Department of Veterans Affairs. Blueprint for excellence. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed December 3, 2015.
16. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38-48.
17. Simmons LA, Wolever RQ. Integrative health coaching and motivational interviewing: synergistic approaches to behavior change in healthcare. Glob Adv Health Med. 2013;2(4):28-35.
18. Snyderman R, Dinan MA. Improving health by taking it personally. JAMA. 2010;303(4):363-364.
19. U.S. Department of Veterans Affairs. Computerized Patient Record System (CPRS) User Guide: GUI version. U.S Department of Veterans Affairs Website. http://www.va.gov/vdl/documents/Clinical/Comp_Patient_Recrd_Sys_(CPRS)/cprsguium.pdf. Published November 2015. Accessed December 3, 2015.
20. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Healthc Pap. 2005;5(4):10-24.
21. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. JRRD. 2011;48(9):1119-1128.
22. Whellan DJ, Gaulden L, Gattis WA, et al. The benefit of implementing a heart failure disease management program. Arch Intern Med. 2001;161(18):2223-2228.
23. Edelman D, Oddone EZ, Liebowitz RS, et al. A multidimensional integrative medicine intervention to improve cardiovascular risk. J Gen Intern Med. 2006;21(7):728-734.
24. Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36(4):629-639.
25. Yang NY, Wroth S, Parham C, Strait M, Simmons LA. Personalized health planning with integrative health coaching to reduce obesity risk among women gaining excess weight during pregnancy. Glob Adv Health Med. 2013;2(4):72-77.
26. Musich S, Klemes A, Kubica MA, Wang S, Hawkins K. Personalized preventive care reduces healthcare expenditures among Medicare advantage beneficiaries. Am J Manag Care. 2014;20(8):613-620.
27. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients' 'scores.' Health Aff. 2013;32(2):216-222.
1. Anderson G. Chronic care: making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
2. Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119(3):263-270.
3. Dinan MA, Simmons LA, Snyderman R. Commentary: Personalized health planning and the Patient Protection and Affordable Care Act: an opportunity for academic medicine to lead health care reform. Acad Med. 2010;85(11):1665-1668.
4. Snyderman R, Yoediono Z. Prospective care: a personalized, preventative approach to medicine. Pharmacogenomics. 2006;7(1):5-9.
5. Snyderman R. Personalized health care: from theory to practice. Biotechnol. 2012;7(8):973-979.
6. Burnette R, Simmons LA, Snyderman R. Personalized health care as a pathway for the adoption of genomic medicine. J Pers Med. 2012;2(4):232-240.
7. Simmons LA, Dinan MA, Robinson TJ, Snyderman R. Personalized medicine is more than genomic medicine: confusion over terminology impedes progress towards personalized healthcare. J Pers Med. 2012;9(1):85-91.
8. Pelletier LR, Stichler JF. Patient-centered care and engagement: nurse leaders' imperative for health reform. J Nurs Adm. 2014;44(9):473-480.
9. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
10. Simmons LA, Wolever RQ, Bechard EM, Snyderman R. Patient engagement as a risk factor in personalized health care: a systematic review of the literature on chronic disease. Genome Med. 2014;6(2):16.
11. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520-526.
12. U.S. Department of Veterans Affairs. VA Patient Centered Care. U.S. Department of Veterans Affairs Website. http://www.va.gov/patientcenteredcare. Updated October 30, 2015. Accessed December 3, 2015.
13. Gaudet T. The Transformation of Healthcare. Paper presented at: 27th Annual Voluntary Health Leadership Conference; 2014; Tucson, Arizona.
14. U.S. Department of Veterans Affairs. VHA Strategic Plan FY 2013-2018. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_STRATEGIC_PLAN_FY2013-2018.pdf. Accessed December 3, 2015.
15. U.S. Department of Veterans Affairs. Blueprint for excellence. U.S. Department of Veterans Affairs Website. http://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf. Published September 21, 2014. Accessed December 3, 2015.
16. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38-48.
17. Simmons LA, Wolever RQ. Integrative health coaching and motivational interviewing: synergistic approaches to behavior change in healthcare. Glob Adv Health Med. 2013;2(4):28-35.
18. Snyderman R, Dinan MA. Improving health by taking it personally. JAMA. 2010;303(4):363-364.
19. U.S. Department of Veterans Affairs. Computerized Patient Record System (CPRS) User Guide: GUI version. U.S Department of Veterans Affairs Website. http://www.va.gov/vdl/documents/Clinical/Comp_Patient_Recrd_Sys_(CPRS)/cprsguium.pdf. Published November 2015. Accessed December 3, 2015.
20. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Healthc Pap. 2005;5(4):10-24.
21. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. JRRD. 2011;48(9):1119-1128.
22. Whellan DJ, Gaulden L, Gattis WA, et al. The benefit of implementing a heart failure disease management program. Arch Intern Med. 2001;161(18):2223-2228.
23. Edelman D, Oddone EZ, Liebowitz RS, et al. A multidimensional integrative medicine intervention to improve cardiovascular risk. J Gen Intern Med. 2006;21(7):728-734.
24. Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36(4):629-639.
25. Yang NY, Wroth S, Parham C, Strait M, Simmons LA. Personalized health planning with integrative health coaching to reduce obesity risk among women gaining excess weight during pregnancy. Glob Adv Health Med. 2013;2(4):72-77.
26. Musich S, Klemes A, Kubica MA, Wang S, Hawkins K. Personalized preventive care reduces healthcare expenditures among Medicare advantage beneficiaries. Am J Manag Care. 2014;20(8):613-620.
27. Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients' 'scores.' Health Aff. 2013;32(2):216-222.