User login
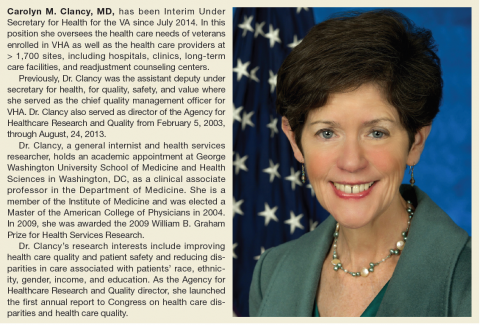
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.