User login
NIH director expresses concern over CRISPR-cas9 baby claim
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
Transcription factor plays key role in AML gene regulatory networks
The AP-1 transcription factor family, important in many tumor types, plays a major role in acute myeloid leukemia, according to researchers who conducted a comprehensive global analysis of gene regulatory networks involved in this disease.
This observation suggests new opportunities for targeted treatment of AML, according to the researchers, led by Peter N. Cockerill, PhD, and Constanze Bonifer, PhD, with the Institute of Cancer and Genomic Sciences, University of Birmingham, England.
“Induced and aberrantly expressed transcription factors are not bystanders, but are important for network maintenance and leukemic growth,” the investigators wrote in Nature Genetics.
Investigators combined data obtained via several different analytic techniques to construct transcription factor networks in normal CD34+ cells and cells from specific subgroups of subjects with defined mutations, including RUNX1 mutations, t(8;21) translocations, mutations of both alleles of the CEBPA gene, and FLT3-ITD with or without NPM1 mutation.
The AP-1 family network was of “high regulatory relevance” for all AML subtypes evaluated, the investigators reported.
Previous work revealed the existence of gene regulatory networks in different types of AML classified by gene expression and DNA-methylation patterns.
“Our work now defines these networks in detail, and shows that leukemic drivers determine the regulatory phenotype by establishing and maintaining specific gene regulatory and signaling networks that are distinct from those in normal cells,” the authors said in their report.
Follow-up in vitro and in vivo studies confirmed the importance of AP-1 for different AML subtypes.
In the in vitro study, investigators transduced AML cells with a doxycycline-inducible version of a dominant negative FOS protein.
“AP-1 is a heterodimer formed by members of the FOS, JUN, ATF, CREB and JDP families of transcription factors, thus it is challenging to target by defined RNA interference approaches,” the investigators explained.
Results of the in vitro study showed that induction of that protein, mediated by doxycycline, inhibited proliferation and colony-forming ability in AML cell lines.
To evaluate the relevance of AP-1 for leukemia propagation in vivo, they transplanted two different types of cells expressing inducible dominant negative FOS protein in immunodeficient mice.
For the first cell type, granulosarcomas developed in six out of seven mice in a control group, but in only two mice treated with doxycycline, neither of which expressed the inducible protein, suggesting that the transgene was silenced, according to the investigators. For the second cell type, doxycycline inhibited leukemia development, while untreated mice rapidly developed tumors.
“Taken together, these findings demonstrate the importance of AP-1 for several AML subtypes and emphasize the potential of transcriptional network analyses to predict transcription factors crucial for malignant propagation,” the investigators wrote.
They declared no competing interests related to their research, which was funded by Bloodwise, Cancer Research UK, a Kay Kendall Clinical Training Fellowship and a MRC/Leuka Clinical Training Fellowship.
SOURCE: Assi SA et al. Nat Genet. 2018 Nov 12. doi: 10.1038/s41588-018-0270-1.
The AP-1 transcription factor family, important in many tumor types, plays a major role in acute myeloid leukemia, according to researchers who conducted a comprehensive global analysis of gene regulatory networks involved in this disease.
This observation suggests new opportunities for targeted treatment of AML, according to the researchers, led by Peter N. Cockerill, PhD, and Constanze Bonifer, PhD, with the Institute of Cancer and Genomic Sciences, University of Birmingham, England.
“Induced and aberrantly expressed transcription factors are not bystanders, but are important for network maintenance and leukemic growth,” the investigators wrote in Nature Genetics.
Investigators combined data obtained via several different analytic techniques to construct transcription factor networks in normal CD34+ cells and cells from specific subgroups of subjects with defined mutations, including RUNX1 mutations, t(8;21) translocations, mutations of both alleles of the CEBPA gene, and FLT3-ITD with or without NPM1 mutation.
The AP-1 family network was of “high regulatory relevance” for all AML subtypes evaluated, the investigators reported.
Previous work revealed the existence of gene regulatory networks in different types of AML classified by gene expression and DNA-methylation patterns.
“Our work now defines these networks in detail, and shows that leukemic drivers determine the regulatory phenotype by establishing and maintaining specific gene regulatory and signaling networks that are distinct from those in normal cells,” the authors said in their report.
Follow-up in vitro and in vivo studies confirmed the importance of AP-1 for different AML subtypes.
In the in vitro study, investigators transduced AML cells with a doxycycline-inducible version of a dominant negative FOS protein.
“AP-1 is a heterodimer formed by members of the FOS, JUN, ATF, CREB and JDP families of transcription factors, thus it is challenging to target by defined RNA interference approaches,” the investigators explained.
Results of the in vitro study showed that induction of that protein, mediated by doxycycline, inhibited proliferation and colony-forming ability in AML cell lines.
To evaluate the relevance of AP-1 for leukemia propagation in vivo, they transplanted two different types of cells expressing inducible dominant negative FOS protein in immunodeficient mice.
For the first cell type, granulosarcomas developed in six out of seven mice in a control group, but in only two mice treated with doxycycline, neither of which expressed the inducible protein, suggesting that the transgene was silenced, according to the investigators. For the second cell type, doxycycline inhibited leukemia development, while untreated mice rapidly developed tumors.
“Taken together, these findings demonstrate the importance of AP-1 for several AML subtypes and emphasize the potential of transcriptional network analyses to predict transcription factors crucial for malignant propagation,” the investigators wrote.
They declared no competing interests related to their research, which was funded by Bloodwise, Cancer Research UK, a Kay Kendall Clinical Training Fellowship and a MRC/Leuka Clinical Training Fellowship.
SOURCE: Assi SA et al. Nat Genet. 2018 Nov 12. doi: 10.1038/s41588-018-0270-1.
The AP-1 transcription factor family, important in many tumor types, plays a major role in acute myeloid leukemia, according to researchers who conducted a comprehensive global analysis of gene regulatory networks involved in this disease.
This observation suggests new opportunities for targeted treatment of AML, according to the researchers, led by Peter N. Cockerill, PhD, and Constanze Bonifer, PhD, with the Institute of Cancer and Genomic Sciences, University of Birmingham, England.
“Induced and aberrantly expressed transcription factors are not bystanders, but are important for network maintenance and leukemic growth,” the investigators wrote in Nature Genetics.
Investigators combined data obtained via several different analytic techniques to construct transcription factor networks in normal CD34+ cells and cells from specific subgroups of subjects with defined mutations, including RUNX1 mutations, t(8;21) translocations, mutations of both alleles of the CEBPA gene, and FLT3-ITD with or without NPM1 mutation.
The AP-1 family network was of “high regulatory relevance” for all AML subtypes evaluated, the investigators reported.
Previous work revealed the existence of gene regulatory networks in different types of AML classified by gene expression and DNA-methylation patterns.
“Our work now defines these networks in detail, and shows that leukemic drivers determine the regulatory phenotype by establishing and maintaining specific gene regulatory and signaling networks that are distinct from those in normal cells,” the authors said in their report.
Follow-up in vitro and in vivo studies confirmed the importance of AP-1 for different AML subtypes.
In the in vitro study, investigators transduced AML cells with a doxycycline-inducible version of a dominant negative FOS protein.
“AP-1 is a heterodimer formed by members of the FOS, JUN, ATF, CREB and JDP families of transcription factors, thus it is challenging to target by defined RNA interference approaches,” the investigators explained.
Results of the in vitro study showed that induction of that protein, mediated by doxycycline, inhibited proliferation and colony-forming ability in AML cell lines.
To evaluate the relevance of AP-1 for leukemia propagation in vivo, they transplanted two different types of cells expressing inducible dominant negative FOS protein in immunodeficient mice.
For the first cell type, granulosarcomas developed in six out of seven mice in a control group, but in only two mice treated with doxycycline, neither of which expressed the inducible protein, suggesting that the transgene was silenced, according to the investigators. For the second cell type, doxycycline inhibited leukemia development, while untreated mice rapidly developed tumors.
“Taken together, these findings demonstrate the importance of AP-1 for several AML subtypes and emphasize the potential of transcriptional network analyses to predict transcription factors crucial for malignant propagation,” the investigators wrote.
They declared no competing interests related to their research, which was funded by Bloodwise, Cancer Research UK, a Kay Kendall Clinical Training Fellowship and a MRC/Leuka Clinical Training Fellowship.
SOURCE: Assi SA et al. Nat Genet. 2018 Nov 12. doi: 10.1038/s41588-018-0270-1.
FROM NATURE GENETICS
Key clinical point:
Major finding: The AP-1 factor family gene regulatory network was of high regulatory relevance in multiple subtypes of AML with defined mutations.
Study details: Analysis of normal CD34+ cells and cells from AML subjects.
Disclosures: Funding came from Bloodwise and Cancer Research UK, among other sources. The researchers reported having no competing financial interests.
Source: Assi SA et al. Nat Genet. 2018 Nov 12. doi: 10.1038/s41588-018-0270-1.
Aberrant RNA editing linked to aggressive myeloma
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
FROM BLOOD
Key clinical point:
Major finding: ADAR1-mediated editing of NEIL1 leads to a weakened DNA base excision repair mechanism.
Study details: Experimental series using plasma samples from healthy volunteers and patients with multiple myeloma.
Disclosures: The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
Source: Teoh PJ et al. Blood. 2018;132(12):1304-17.
CDK8 inhibitor shows activity against AML
DUBROVNIK, CROATIA – The (AML), but the agent’s mechanism of action is still unclear.
Researchers found that several AML cell lines were “highly sensitive” to SEL120, and the inhibitor was active in primary patient samples. SEL120 also reduced tumor growth in mouse models of AML and demonstrated synergy with venetoclax.
The researchers suggest that SEL120 works by affecting the maintenance of AML cells and leukemic stem cells (LSCs), inducing differentiation and, sometimes, apoptosis. However, the mechanism is not well defined.
Eliza Majewska, PhD, of Selvita S.A. in Krakow, Poland, discussed research on SEL120 at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Majewska explained that CDK8 is a transcriptional kinase working in the context of the Mediator complex, and previous research indicated that CDK8 drives oncogenic transcription in AML (Nature. 2015 Oct 8;526[7572]:273-6).
In a prior study, researchers found that SEL120 inhibits CDK8 activity in AML cells with high levels of STAT phosphorylation (Oncotarget. 2017 May 16;8[20]:33779-95).
Dr. Majewska said the MV4-11 cell line responds particularly well to SEL120, and other sensitive cell lines include SKNO-1, Oci-AML5, GDM-1, KG-1, MOLM-16, and Oci-AML3.
“The fact that STAT signaling was upregulated in those cell lines that were very sensitive to SEL120 gave us the hint that perhaps we are looking at a mechanism of action of the compound that has something to do with leukemic stem cells,” Dr. Majewska said.
In fact, she and her colleagues found that cell lines sensitive to SEL120 had upregulation of genes linked to LSCs and high levels of CD34 surface expression.
Experiments in CD34+ TEX cells showed that SEL120 specifically depletes CD34+ cells, leads to downregulation of stemness-related genes, and induces myeloid differentiation.
After 6 days of treatment with SEL120, TEX cells showed decreased expression of the LSC-linked genes MEIS1 and LILRB2, enrichment of gene sets downregulated in LSCs and linked to differentiation, and increased expression of differentiation markers and immune response genes.
SEL120 also demonstrated antileukemic activity in vivo. The researchers tested SEL120 in a CD34+ model of AML (KG-1) and a FLT3-ITD model of AML (MV4-11).
In both models, SEL120 induced “significant tumor regression” of about 80%. In some cases, the researchers observed apoptosis.
Toxicities observed in the mice included weight loss and upregulation of inflammation.
The researchers also found that SEL120 was synergistic with venetoclax. In fact, the combination of these drugs resulted in “almost complete remission cures” in the MV4-11 model, according to Dr. Majewska.
Finally, she and her colleagues discovered that SEL120 was active against primary patient cells. Samples from three of four patients had a significant reduction in cell numbers after 7 days of treatment with SEL120. For one patient, there were no viable cells on day 7.
Dr. Majewska said a phase 1 trial of SEL120 is planned for 2019 or 2020, and SEL120’s mechanism of action is still under investigation.
“The mechanism of action ... is, in our mind – at least in some cases – linked to the fact that CDK8 functions within the context of the Mediator complex, which contributes to gene expression related to leukemic stem cells,” Dr. Majewska said.
“And when we inhibit this specific transcription, of course, the Mediator complex still works because this is just one of the components of the complex. However, the function that it has is suddenly very different, and it’s actually linked to lack of maintenance of leukemic stem cells, resulting in differentiation [and], in some cases, the induction of apoptosis, but we do not fully understand the mechanism of this induction.”
Dr. Majewska works for Selvita, the company developing SEL120. This research was funded by Selvita, the Leukemia & Lymphoma Society, and the National Centre for Research and Development.
The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
DUBROVNIK, CROATIA – The (AML), but the agent’s mechanism of action is still unclear.
Researchers found that several AML cell lines were “highly sensitive” to SEL120, and the inhibitor was active in primary patient samples. SEL120 also reduced tumor growth in mouse models of AML and demonstrated synergy with venetoclax.
The researchers suggest that SEL120 works by affecting the maintenance of AML cells and leukemic stem cells (LSCs), inducing differentiation and, sometimes, apoptosis. However, the mechanism is not well defined.
Eliza Majewska, PhD, of Selvita S.A. in Krakow, Poland, discussed research on SEL120 at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Majewska explained that CDK8 is a transcriptional kinase working in the context of the Mediator complex, and previous research indicated that CDK8 drives oncogenic transcription in AML (Nature. 2015 Oct 8;526[7572]:273-6).
In a prior study, researchers found that SEL120 inhibits CDK8 activity in AML cells with high levels of STAT phosphorylation (Oncotarget. 2017 May 16;8[20]:33779-95).
Dr. Majewska said the MV4-11 cell line responds particularly well to SEL120, and other sensitive cell lines include SKNO-1, Oci-AML5, GDM-1, KG-1, MOLM-16, and Oci-AML3.
“The fact that STAT signaling was upregulated in those cell lines that were very sensitive to SEL120 gave us the hint that perhaps we are looking at a mechanism of action of the compound that has something to do with leukemic stem cells,” Dr. Majewska said.
In fact, she and her colleagues found that cell lines sensitive to SEL120 had upregulation of genes linked to LSCs and high levels of CD34 surface expression.
Experiments in CD34+ TEX cells showed that SEL120 specifically depletes CD34+ cells, leads to downregulation of stemness-related genes, and induces myeloid differentiation.
After 6 days of treatment with SEL120, TEX cells showed decreased expression of the LSC-linked genes MEIS1 and LILRB2, enrichment of gene sets downregulated in LSCs and linked to differentiation, and increased expression of differentiation markers and immune response genes.
SEL120 also demonstrated antileukemic activity in vivo. The researchers tested SEL120 in a CD34+ model of AML (KG-1) and a FLT3-ITD model of AML (MV4-11).
In both models, SEL120 induced “significant tumor regression” of about 80%. In some cases, the researchers observed apoptosis.
Toxicities observed in the mice included weight loss and upregulation of inflammation.
The researchers also found that SEL120 was synergistic with venetoclax. In fact, the combination of these drugs resulted in “almost complete remission cures” in the MV4-11 model, according to Dr. Majewska.
Finally, she and her colleagues discovered that SEL120 was active against primary patient cells. Samples from three of four patients had a significant reduction in cell numbers after 7 days of treatment with SEL120. For one patient, there were no viable cells on day 7.
Dr. Majewska said a phase 1 trial of SEL120 is planned for 2019 or 2020, and SEL120’s mechanism of action is still under investigation.
“The mechanism of action ... is, in our mind – at least in some cases – linked to the fact that CDK8 functions within the context of the Mediator complex, which contributes to gene expression related to leukemic stem cells,” Dr. Majewska said.
“And when we inhibit this specific transcription, of course, the Mediator complex still works because this is just one of the components of the complex. However, the function that it has is suddenly very different, and it’s actually linked to lack of maintenance of leukemic stem cells, resulting in differentiation [and], in some cases, the induction of apoptosis, but we do not fully understand the mechanism of this induction.”
Dr. Majewska works for Selvita, the company developing SEL120. This research was funded by Selvita, the Leukemia & Lymphoma Society, and the National Centre for Research and Development.
The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
DUBROVNIK, CROATIA – The (AML), but the agent’s mechanism of action is still unclear.
Researchers found that several AML cell lines were “highly sensitive” to SEL120, and the inhibitor was active in primary patient samples. SEL120 also reduced tumor growth in mouse models of AML and demonstrated synergy with venetoclax.
The researchers suggest that SEL120 works by affecting the maintenance of AML cells and leukemic stem cells (LSCs), inducing differentiation and, sometimes, apoptosis. However, the mechanism is not well defined.
Eliza Majewska, PhD, of Selvita S.A. in Krakow, Poland, discussed research on SEL120 at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Majewska explained that CDK8 is a transcriptional kinase working in the context of the Mediator complex, and previous research indicated that CDK8 drives oncogenic transcription in AML (Nature. 2015 Oct 8;526[7572]:273-6).
In a prior study, researchers found that SEL120 inhibits CDK8 activity in AML cells with high levels of STAT phosphorylation (Oncotarget. 2017 May 16;8[20]:33779-95).
Dr. Majewska said the MV4-11 cell line responds particularly well to SEL120, and other sensitive cell lines include SKNO-1, Oci-AML5, GDM-1, KG-1, MOLM-16, and Oci-AML3.
“The fact that STAT signaling was upregulated in those cell lines that were very sensitive to SEL120 gave us the hint that perhaps we are looking at a mechanism of action of the compound that has something to do with leukemic stem cells,” Dr. Majewska said.
In fact, she and her colleagues found that cell lines sensitive to SEL120 had upregulation of genes linked to LSCs and high levels of CD34 surface expression.
Experiments in CD34+ TEX cells showed that SEL120 specifically depletes CD34+ cells, leads to downregulation of stemness-related genes, and induces myeloid differentiation.
After 6 days of treatment with SEL120, TEX cells showed decreased expression of the LSC-linked genes MEIS1 and LILRB2, enrichment of gene sets downregulated in LSCs and linked to differentiation, and increased expression of differentiation markers and immune response genes.
SEL120 also demonstrated antileukemic activity in vivo. The researchers tested SEL120 in a CD34+ model of AML (KG-1) and a FLT3-ITD model of AML (MV4-11).
In both models, SEL120 induced “significant tumor regression” of about 80%. In some cases, the researchers observed apoptosis.
Toxicities observed in the mice included weight loss and upregulation of inflammation.
The researchers also found that SEL120 was synergistic with venetoclax. In fact, the combination of these drugs resulted in “almost complete remission cures” in the MV4-11 model, according to Dr. Majewska.
Finally, she and her colleagues discovered that SEL120 was active against primary patient cells. Samples from three of four patients had a significant reduction in cell numbers after 7 days of treatment with SEL120. For one patient, there were no viable cells on day 7.
Dr. Majewska said a phase 1 trial of SEL120 is planned for 2019 or 2020, and SEL120’s mechanism of action is still under investigation.
“The mechanism of action ... is, in our mind – at least in some cases – linked to the fact that CDK8 functions within the context of the Mediator complex, which contributes to gene expression related to leukemic stem cells,” Dr. Majewska said.
“And when we inhibit this specific transcription, of course, the Mediator complex still works because this is just one of the components of the complex. However, the function that it has is suddenly very different, and it’s actually linked to lack of maintenance of leukemic stem cells, resulting in differentiation [and], in some cases, the induction of apoptosis, but we do not fully understand the mechanism of this induction.”
Dr. Majewska works for Selvita, the company developing SEL120. This research was funded by Selvita, the Leukemia & Lymphoma Society, and the National Centre for Research and Development.
The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
EXPERT ANALYSIS FROM LEUKEMIA AND LYMPHOMA 2018
Eltrombopag irons out kinks in hematopoiesis
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Eltrombopag stimulates hematopoiesis through iron-chelating effects at the stem cell level, independent of its effect on the thrombopoietin receptor.
Study details: Basic science experiments in mouse models, human bone marrow cells lines, and samples from patients with immune thrombocytopenia.
Disclosures: The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis and serving as consultants for Novartis. Two of the coauthors are employees of Novartis.
Source: Kao Y-R et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
New hematologic, cardiovascular system link may have therapeutic implications
ATLANTA – An intriguing link between the sex steroid hormonal milieu and platelet mitochondria has potential implications for reducing thrombosis risk.
The link, which involves a mitochondrial protein known as optic atrophy 1 (OPA1), appears to play a role in the regulation of thrombosis, and provides a possible explanation for the marked differences in cardiovascular risks between men and women, according to E. Dale Abel, MD, chair of the department of internal medicine, and director of the Fraternal Order of Eagles Diabetes Research Center at the University of Iowa, Iowa City.
The findings could lead to risk-stratification strategies and the identification of therapeutic targets, Dr. Abel said in an interview.
OPA1 is an inner mitochondrial membrane protein involved in mitochondrial fusion, he explained.
“My laboratory, for a very long time, has been interested in the cardiovascular complications of diabetes, and a lot of our work has focused on the heart and on the relationship between changes in metabolism and mitochondrial biology in those complications. We got interested in platelets because of a collaboration that actually started with Dr. [Andrew] Weyrich when my lab was at the University of Utah. There was a request for proposals from the National Heart, Lung, and Blood Institute for projects that would seek to understand the increased risk of thrombosis that occurs in people with diabetes,” he said.
Specifically, Dr. Weyrich had some preliminary data showing a backup of intermediates of glucose metabolism occurring in the platelets of diabetics.
“This suggested either that there was increased import of glucose into those cells or a decreased ability of those cells to metabolize glucose,” Dr. Abel said, adding that a closer look at the expression of certain genes in platelets as they related to the risk of thrombosis showed that a number of mitochondrial genes were involved, including OPA1.
Since Dr. Abel’s lab was already involved with studying glucose metabolism and mitochondrial metabolism, and had created a number of tools for modifying alleles, which would enable the targeting of expression of some of these genes, he and his colleagues began to look closer at the role of OPA1.
“The relationship between OPA1 and platelet biology, at least based on epidemiological studies from Dr. [Jane] Freedman’s analysis of platelet RNA expression in the Framingham cohort, really seemed to suggest that this had more to do with events in females rather than males,” Dr. Abel said.
He and his colleagues then generated a mouse model in which OPA1 levels in platelets could be manipulated. The goal was to determine if such manipulation would affect platelet function or platelet biology, and also to see if the effects differed between males and females.
“Initially, we didn’t have an expectation that we would see a difference between males and females, but in retrospect, it actually fits very nicely with what the epidemiological data in humans would suggest,” he said, referring to the differences in thrombosis risk between men and women.
Mitochondria go through a process of fusion and fission; OPA1 is involved in the fusion of the inner mitochondrial membrane, which has many folds known as cristae.
“These cristae are very important in the ability of mitochondria to generate energy, and OPA1 plays a very important role in maintaining the structure of these cristae,” he explained.
He and his colleagues generated mice that lacked OPA1 specifically in platelets. They then characterized the mitochondria and platelet function in these knockout mice.
“We saw that there was a difference between males and females in terms of how they responded to OPA1 deletion. Specifically, the males appeared to get more overt mitochondrial damage in terms of their structure and function, whereas the mitochondria appeared remarkably normal in females,” he said.
A look at platelet function showed that platelets in males were somewhat hyperactive, while in females they were somewhat underactive.
When the researchers used a model of deep venous thrombosis (DVT), more than 90% of male knockout mice developed a DVT versus 50% of wild-type controls. In contrast, there was no increase in DVT in female knockout mice relative to wild-type controls.
“So they were really opposite phenotypes in terms of platelet activity, and whenever one sees a difference between sexes in any biological variable or phenotype, you wonder if this is because of sex hormones,” he said.
This question led to a number of additional experiments.
In one of those experiments, Dr. Abel and his colleagues used a mouse model in which platelets were depleted and replaced via transfusion with platelets from another animal.
“We took male mice that were wild type and we depleted their platelets, and then we took platelets from an OPA1 deficient female and transfused these back into male mice, and took OPA1 deficient platelets from males and transfused them back into platelet-depleted female hosts. The really interesting thing in those experiments was that the phenotype switched,” he said.
That is, platelets in male mice with OPA1 deficiency, which had increased platelet activation in the male mice, became hypoactive when they were transfused into female mice. Similarly, hypoactive platelets from female mice became hyperactive when transfused into platelet-depleted male mice.
“What this told us then, is that the hormonal milieu interacts with OPA1 deficiency to modulate the function of the platelets,” he said.
Additional hormonal manipulations, involving orchiectomy in male mice to lower testosterone levels and increase estrogen levels, and ovariectomy in female mice to lower estrogen levels, showed that this could also modify platelet response.
“So we have discovered that somehow the amount of OPA1 in platelets interacts with circulating estrogens to modify the activity of platelets. This is not a trivial issue, because, as in the epidemiological study, the relationship is something that seems to be particularly true in females, and it also turned out that the OPA1 tended to track with increased cardiovascular events,” he said.
Preliminary studies involving pregnant women, looking at both the first and third trimester (when estrogen levels spike), also showed a correlation between increased platelet activity in the third trimester and higher levels of OPA1 in their platelets.
“It seems there is a relationship between OPA1 and platelets in women and estrogen levels that may then increase the risk of thrombosis. Maybe our mouse model phenotype is explained by the fact that we did the opposite: We reduced OPA1 in the platelets of females, and we actually saw that this was protective,” he said.
The findings are generating excitement, according to Dr. Weyrich, professor of internal medicine and vice president for research at the University of Utah, Salt Lake City, who was involved in the earlier studies that led Dr. Abel and his team to delve into the OPA1 research.
During a presentation of Dr. Abel’s findings at the annual meeting of the American Society of Hematology, Dr. Weyrich called the work “really, really striking,” and said the gender-specific findings are of particular importance.
“It’s something we often overlook and don’t think about, but I think it’s something that’s probably going to be more and more important as we begin to understand all types of diseases both in benign and malignant hematology,” he said.
Dr. Abel and his team plan to do their part to further that understanding. They are awaiting word on a new National Institutes of Health grant that will allow for expansion of their mouse studies into humans. Specifically, those studies will look at correlations between levels of OPA1 expression in platelets in women and history of/risk for developing a thrombotic event.
“Thrombosis is a significant problem in women who are exposed to estrogens ... and with the exception of a small number of specific genetic disorders of platelets, very little is known about what the risk factors are for this estrogen dependent increase in thrombotic risk,” he said.
What needs to be uncovered, Dr. Abel said, is whether women with the highest levels of OPA1 carry the highest risk of thrombosis.
“If we understand that, we may be in a position to stratify these women based on thrombosis risk in the setting of estrogen exposure. I think the other thing that will come out of the work, as we begin to understand the mechanisms for this relationship, is the identification of targets that we could therapeutically modulate to reduce this risk,” he added.
Eventually, as more is learned about the mechanisms that underlie the relationship between OPA1 and platelet activation, the findings might also lead to new approaches for reducing the risk of thrombosis in men, he noted.
Dr. Abel and Dr. Weyrich reported having no relevant financial disclosures.
ATLANTA – An intriguing link between the sex steroid hormonal milieu and platelet mitochondria has potential implications for reducing thrombosis risk.
The link, which involves a mitochondrial protein known as optic atrophy 1 (OPA1), appears to play a role in the regulation of thrombosis, and provides a possible explanation for the marked differences in cardiovascular risks between men and women, according to E. Dale Abel, MD, chair of the department of internal medicine, and director of the Fraternal Order of Eagles Diabetes Research Center at the University of Iowa, Iowa City.
The findings could lead to risk-stratification strategies and the identification of therapeutic targets, Dr. Abel said in an interview.
OPA1 is an inner mitochondrial membrane protein involved in mitochondrial fusion, he explained.
“My laboratory, for a very long time, has been interested in the cardiovascular complications of diabetes, and a lot of our work has focused on the heart and on the relationship between changes in metabolism and mitochondrial biology in those complications. We got interested in platelets because of a collaboration that actually started with Dr. [Andrew] Weyrich when my lab was at the University of Utah. There was a request for proposals from the National Heart, Lung, and Blood Institute for projects that would seek to understand the increased risk of thrombosis that occurs in people with diabetes,” he said.
Specifically, Dr. Weyrich had some preliminary data showing a backup of intermediates of glucose metabolism occurring in the platelets of diabetics.
“This suggested either that there was increased import of glucose into those cells or a decreased ability of those cells to metabolize glucose,” Dr. Abel said, adding that a closer look at the expression of certain genes in platelets as they related to the risk of thrombosis showed that a number of mitochondrial genes were involved, including OPA1.
Since Dr. Abel’s lab was already involved with studying glucose metabolism and mitochondrial metabolism, and had created a number of tools for modifying alleles, which would enable the targeting of expression of some of these genes, he and his colleagues began to look closer at the role of OPA1.
“The relationship between OPA1 and platelet biology, at least based on epidemiological studies from Dr. [Jane] Freedman’s analysis of platelet RNA expression in the Framingham cohort, really seemed to suggest that this had more to do with events in females rather than males,” Dr. Abel said.
He and his colleagues then generated a mouse model in which OPA1 levels in platelets could be manipulated. The goal was to determine if such manipulation would affect platelet function or platelet biology, and also to see if the effects differed between males and females.
“Initially, we didn’t have an expectation that we would see a difference between males and females, but in retrospect, it actually fits very nicely with what the epidemiological data in humans would suggest,” he said, referring to the differences in thrombosis risk between men and women.
Mitochondria go through a process of fusion and fission; OPA1 is involved in the fusion of the inner mitochondrial membrane, which has many folds known as cristae.
“These cristae are very important in the ability of mitochondria to generate energy, and OPA1 plays a very important role in maintaining the structure of these cristae,” he explained.
He and his colleagues generated mice that lacked OPA1 specifically in platelets. They then characterized the mitochondria and platelet function in these knockout mice.
“We saw that there was a difference between males and females in terms of how they responded to OPA1 deletion. Specifically, the males appeared to get more overt mitochondrial damage in terms of their structure and function, whereas the mitochondria appeared remarkably normal in females,” he said.
A look at platelet function showed that platelets in males were somewhat hyperactive, while in females they were somewhat underactive.
When the researchers used a model of deep venous thrombosis (DVT), more than 90% of male knockout mice developed a DVT versus 50% of wild-type controls. In contrast, there was no increase in DVT in female knockout mice relative to wild-type controls.
“So they were really opposite phenotypes in terms of platelet activity, and whenever one sees a difference between sexes in any biological variable or phenotype, you wonder if this is because of sex hormones,” he said.
This question led to a number of additional experiments.
In one of those experiments, Dr. Abel and his colleagues used a mouse model in which platelets were depleted and replaced via transfusion with platelets from another animal.
“We took male mice that were wild type and we depleted their platelets, and then we took platelets from an OPA1 deficient female and transfused these back into male mice, and took OPA1 deficient platelets from males and transfused them back into platelet-depleted female hosts. The really interesting thing in those experiments was that the phenotype switched,” he said.
That is, platelets in male mice with OPA1 deficiency, which had increased platelet activation in the male mice, became hypoactive when they were transfused into female mice. Similarly, hypoactive platelets from female mice became hyperactive when transfused into platelet-depleted male mice.
“What this told us then, is that the hormonal milieu interacts with OPA1 deficiency to modulate the function of the platelets,” he said.
Additional hormonal manipulations, involving orchiectomy in male mice to lower testosterone levels and increase estrogen levels, and ovariectomy in female mice to lower estrogen levels, showed that this could also modify platelet response.
“So we have discovered that somehow the amount of OPA1 in platelets interacts with circulating estrogens to modify the activity of platelets. This is not a trivial issue, because, as in the epidemiological study, the relationship is something that seems to be particularly true in females, and it also turned out that the OPA1 tended to track with increased cardiovascular events,” he said.
Preliminary studies involving pregnant women, looking at both the first and third trimester (when estrogen levels spike), also showed a correlation between increased platelet activity in the third trimester and higher levels of OPA1 in their platelets.
“It seems there is a relationship between OPA1 and platelets in women and estrogen levels that may then increase the risk of thrombosis. Maybe our mouse model phenotype is explained by the fact that we did the opposite: We reduced OPA1 in the platelets of females, and we actually saw that this was protective,” he said.
The findings are generating excitement, according to Dr. Weyrich, professor of internal medicine and vice president for research at the University of Utah, Salt Lake City, who was involved in the earlier studies that led Dr. Abel and his team to delve into the OPA1 research.
During a presentation of Dr. Abel’s findings at the annual meeting of the American Society of Hematology, Dr. Weyrich called the work “really, really striking,” and said the gender-specific findings are of particular importance.
“It’s something we often overlook and don’t think about, but I think it’s something that’s probably going to be more and more important as we begin to understand all types of diseases both in benign and malignant hematology,” he said.
Dr. Abel and his team plan to do their part to further that understanding. They are awaiting word on a new National Institutes of Health grant that will allow for expansion of their mouse studies into humans. Specifically, those studies will look at correlations between levels of OPA1 expression in platelets in women and history of/risk for developing a thrombotic event.
“Thrombosis is a significant problem in women who are exposed to estrogens ... and with the exception of a small number of specific genetic disorders of platelets, very little is known about what the risk factors are for this estrogen dependent increase in thrombotic risk,” he said.
What needs to be uncovered, Dr. Abel said, is whether women with the highest levels of OPA1 carry the highest risk of thrombosis.
“If we understand that, we may be in a position to stratify these women based on thrombosis risk in the setting of estrogen exposure. I think the other thing that will come out of the work, as we begin to understand the mechanisms for this relationship, is the identification of targets that we could therapeutically modulate to reduce this risk,” he added.
Eventually, as more is learned about the mechanisms that underlie the relationship between OPA1 and platelet activation, the findings might also lead to new approaches for reducing the risk of thrombosis in men, he noted.
Dr. Abel and Dr. Weyrich reported having no relevant financial disclosures.
ATLANTA – An intriguing link between the sex steroid hormonal milieu and platelet mitochondria has potential implications for reducing thrombosis risk.
The link, which involves a mitochondrial protein known as optic atrophy 1 (OPA1), appears to play a role in the regulation of thrombosis, and provides a possible explanation for the marked differences in cardiovascular risks between men and women, according to E. Dale Abel, MD, chair of the department of internal medicine, and director of the Fraternal Order of Eagles Diabetes Research Center at the University of Iowa, Iowa City.
The findings could lead to risk-stratification strategies and the identification of therapeutic targets, Dr. Abel said in an interview.
OPA1 is an inner mitochondrial membrane protein involved in mitochondrial fusion, he explained.
“My laboratory, for a very long time, has been interested in the cardiovascular complications of diabetes, and a lot of our work has focused on the heart and on the relationship between changes in metabolism and mitochondrial biology in those complications. We got interested in platelets because of a collaboration that actually started with Dr. [Andrew] Weyrich when my lab was at the University of Utah. There was a request for proposals from the National Heart, Lung, and Blood Institute for projects that would seek to understand the increased risk of thrombosis that occurs in people with diabetes,” he said.
Specifically, Dr. Weyrich had some preliminary data showing a backup of intermediates of glucose metabolism occurring in the platelets of diabetics.
“This suggested either that there was increased import of glucose into those cells or a decreased ability of those cells to metabolize glucose,” Dr. Abel said, adding that a closer look at the expression of certain genes in platelets as they related to the risk of thrombosis showed that a number of mitochondrial genes were involved, including OPA1.
Since Dr. Abel’s lab was already involved with studying glucose metabolism and mitochondrial metabolism, and had created a number of tools for modifying alleles, which would enable the targeting of expression of some of these genes, he and his colleagues began to look closer at the role of OPA1.
“The relationship between OPA1 and platelet biology, at least based on epidemiological studies from Dr. [Jane] Freedman’s analysis of platelet RNA expression in the Framingham cohort, really seemed to suggest that this had more to do with events in females rather than males,” Dr. Abel said.
He and his colleagues then generated a mouse model in which OPA1 levels in platelets could be manipulated. The goal was to determine if such manipulation would affect platelet function or platelet biology, and also to see if the effects differed between males and females.
“Initially, we didn’t have an expectation that we would see a difference between males and females, but in retrospect, it actually fits very nicely with what the epidemiological data in humans would suggest,” he said, referring to the differences in thrombosis risk between men and women.
Mitochondria go through a process of fusion and fission; OPA1 is involved in the fusion of the inner mitochondrial membrane, which has many folds known as cristae.
“These cristae are very important in the ability of mitochondria to generate energy, and OPA1 plays a very important role in maintaining the structure of these cristae,” he explained.
He and his colleagues generated mice that lacked OPA1 specifically in platelets. They then characterized the mitochondria and platelet function in these knockout mice.
“We saw that there was a difference between males and females in terms of how they responded to OPA1 deletion. Specifically, the males appeared to get more overt mitochondrial damage in terms of their structure and function, whereas the mitochondria appeared remarkably normal in females,” he said.
A look at platelet function showed that platelets in males were somewhat hyperactive, while in females they were somewhat underactive.
When the researchers used a model of deep venous thrombosis (DVT), more than 90% of male knockout mice developed a DVT versus 50% of wild-type controls. In contrast, there was no increase in DVT in female knockout mice relative to wild-type controls.
“So they were really opposite phenotypes in terms of platelet activity, and whenever one sees a difference between sexes in any biological variable or phenotype, you wonder if this is because of sex hormones,” he said.
This question led to a number of additional experiments.
In one of those experiments, Dr. Abel and his colleagues used a mouse model in which platelets were depleted and replaced via transfusion with platelets from another animal.
“We took male mice that were wild type and we depleted their platelets, and then we took platelets from an OPA1 deficient female and transfused these back into male mice, and took OPA1 deficient platelets from males and transfused them back into platelet-depleted female hosts. The really interesting thing in those experiments was that the phenotype switched,” he said.
That is, platelets in male mice with OPA1 deficiency, which had increased platelet activation in the male mice, became hypoactive when they were transfused into female mice. Similarly, hypoactive platelets from female mice became hyperactive when transfused into platelet-depleted male mice.
“What this told us then, is that the hormonal milieu interacts with OPA1 deficiency to modulate the function of the platelets,” he said.
Additional hormonal manipulations, involving orchiectomy in male mice to lower testosterone levels and increase estrogen levels, and ovariectomy in female mice to lower estrogen levels, showed that this could also modify platelet response.
“So we have discovered that somehow the amount of OPA1 in platelets interacts with circulating estrogens to modify the activity of platelets. This is not a trivial issue, because, as in the epidemiological study, the relationship is something that seems to be particularly true in females, and it also turned out that the OPA1 tended to track with increased cardiovascular events,” he said.
Preliminary studies involving pregnant women, looking at both the first and third trimester (when estrogen levels spike), also showed a correlation between increased platelet activity in the third trimester and higher levels of OPA1 in their platelets.
“It seems there is a relationship between OPA1 and platelets in women and estrogen levels that may then increase the risk of thrombosis. Maybe our mouse model phenotype is explained by the fact that we did the opposite: We reduced OPA1 in the platelets of females, and we actually saw that this was protective,” he said.
The findings are generating excitement, according to Dr. Weyrich, professor of internal medicine and vice president for research at the University of Utah, Salt Lake City, who was involved in the earlier studies that led Dr. Abel and his team to delve into the OPA1 research.
During a presentation of Dr. Abel’s findings at the annual meeting of the American Society of Hematology, Dr. Weyrich called the work “really, really striking,” and said the gender-specific findings are of particular importance.
“It’s something we often overlook and don’t think about, but I think it’s something that’s probably going to be more and more important as we begin to understand all types of diseases both in benign and malignant hematology,” he said.
Dr. Abel and his team plan to do their part to further that understanding. They are awaiting word on a new National Institutes of Health grant that will allow for expansion of their mouse studies into humans. Specifically, those studies will look at correlations between levels of OPA1 expression in platelets in women and history of/risk for developing a thrombotic event.
“Thrombosis is a significant problem in women who are exposed to estrogens ... and with the exception of a small number of specific genetic disorders of platelets, very little is known about what the risk factors are for this estrogen dependent increase in thrombotic risk,” he said.
What needs to be uncovered, Dr. Abel said, is whether women with the highest levels of OPA1 carry the highest risk of thrombosis.
“If we understand that, we may be in a position to stratify these women based on thrombosis risk in the setting of estrogen exposure. I think the other thing that will come out of the work, as we begin to understand the mechanisms for this relationship, is the identification of targets that we could therapeutically modulate to reduce this risk,” he added.
Eventually, as more is learned about the mechanisms that underlie the relationship between OPA1 and platelet activation, the findings might also lead to new approaches for reducing the risk of thrombosis in men, he noted.
Dr. Abel and Dr. Weyrich reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM ASH 2017
The enemy of good
“But no perfection is so absolute,
That some impurity doth not pollute.”
– William Shakespeare
While lounging in the ivory tower of academia, we frequently find ourselves condemning the peasantry who fail to grasp limitations of clinical trials. We deride the ignorant masses who insist on flaunting the inclusion criteria of the latest study and extrapolate the results to the ineligible patient sitting in front of them. The disrespect heaped on the “referring doctor” for treating their patients in the absence of evidence from prospective, randomized, multi-institutional trials is routine in conference rooms across the National Cancer Institute’s designated cancer centers.
The introduction of third-party insurers decades ago warped the economics of health care to the point that modern patients generally expect to pay little or nothing for pretty much any medical intervention. As a result, physicians tend to prescribe treatments without regard to cost. Predictably, this results in a steady increase in costs, which have now become unsustainable for our nation. Those rising costs have resulted in many proposals for control, including the Affordable Care Act and the efforts to reverse it. Many see a single payer, government administered system as the only viable way forward.
No matter the final system our society settles on, it will have to account for the almost miraculous results from modern therapeutics, which seem to be announced more and more frequently.
As I write this column, the annual meeting of the American Society of Hematology is being held in Atlanta. The presentations recount studies of new agents alone, or in combination, that report unprecedented response and survival rates. In particular, cellular immunotherapy with chimeric antigen receptor T cells (CAR T cells) has captured the attention of physicians, patients, and investors. Simultaneously – and recognizing this revolution in oncologic therapeutics – the New England Journal of Medicine prepublished two papers presenting the results of CAR T-cell therapy for diffuse large B-cell lymphoma (DLBCL). The results are impressive, and earlier this year, the Food and Drug Administration approved axicabtagene ciloleucel for the treatment of relapsed or refractory DLBCL based on these data. An approval for tisagenlecleucel exists for the treatment of B-cell acute lymphoblastic leukemia, but approval for DLBCL is likely forthcoming, too.
These are wonderful developments. Patients with incurable lymphoma may now be offered potentially curative treatment. Hematology News has covered the development of these treatments closely.
Yet, there is a glaring problem that has also attracted attention: CAR T-cell therapy is incredibly expensive. The potentially mitigating effect of competing products on cost will be canceled by the demand, as well as by geographic scarcity, because only certain large centers will provide this treatment. Remember that the price of imatinib went up over time even though competitors entered the market.
Entering CAR T-cell treatments into the nation’s formulary for some patients will lead to rising premiums for all patients. Disturbingly, CAR T cells are just a treatment for hematology patients at present. What about the equally impressive new – and expensive – technologies in cardiology, neurology, surgery, and every other medical subspecialty? Our system is already struggling to accommodate rapidly rising costs as our population ages and demands more and more medical care.
Many believe that our society will ultimately require strict controls on access to these expensive treatments. While the idea of rationing care is abhorrent to clinicians, “evidence-based” restrictions to access appear not to be. For example, rituximab is effective for immune thrombocytopenic purpura (ITP), but is not FDA approved for it. Despite the restriction, rituximab is frequently used for ITP and generally reimbursed. Venetoclax is a useful agent for patients in relapse of chronic lymphocytic leukemia, but the FDA only approved it for those harboring a deletion of 17p. While insurers seem willing to reimburse the use of rituximab for ITP, they balk at covering venetoclax for off-label indications. More recently, and more ominously for the implications, the FDA approval for tisagenlecleucel in the treatment of B-cell acute lymphoblastic leukemia only extends to those up to age 25. That could mean a 26-year-old in relapse after an allogeneic transplant would be denied coverage for potentially curative CAR T-cell therapy.
The federal government is not the only bureaucracy with a financial interest in limiting access to expensive treatments. Commercial insurers have a fiduciary duty to their shareholders, not to the patients who consume their services. They employ thousands, among them physicians, tasked with reviewing our treatment recommendations to determine whether treatments will be paid for, often citing FDA approvals. Preauthorization for coverage results in innumerable treatment delays and added administrative costs that frustrate us and anger our patients. The insurers defend this incessant obstructionism by claiming they are protecting patients from unnecessary or unhelpful care. Like the FDA, they invoke our own penchant for evidence-based medicine or declare that some care pathway is the ultimate arbiter of truth in coverage determination. Therein lies the danger.
Where do you suppose the evidence and care pathways the FDA and insurers rely on come from? They come from academics like many of this publication’s readers. We gladly provide them with the data needed to restrict care. Through published studies in “major” journals, consensus guidelines promulgated through national organizations, and care pathways generated by our own institutions, we provide the fodder that feeds the regulatory apparatus that decides whose care is approved and paid for. As Walt Kelly’s Pogo stated in 1970, “We have met the enemy and he is us.”
In the interest of science and in the interest of safety – but mostly in the interest of ensuring regulatory approval – clinical trials of new agents often restrict eligibility. Our group recently found that randomized trials routinely exclude patients for rather arbitrary organ dysfunction (Leukemia. 2017 Aug;31[8]:1808-15).
Another recent study concluded, “Current oncology clinical trials stipulate many inclusion and exclusion criteria that specifically define the patient population under study. Although eligibility criteria are needed to define the study population and improve safety, overly restrictive eligibility criteria limit participation in clinical trials, cause the study population to be unrepresentative of the general population of patients with cancer, and limit patient access to new treatments.” (J Clin Oncol. 2017 Nov 20;35[33]:3745-52).
Federal and private agencies will necessarily become stricter in their interpretations of studies and policies in order to control costs. They will happily cite the data we produce in order to do so. For the vast majority of patients who do not meet stringent inclusion criteria, access to new treatments may well be denied. To ensure that patients are provided with the best and most economical care, I am an advocate for evidence-based medicine and care pathways to standardize practice. However, I am progressively more wary of their potential to restrict the availability of innovative remedies to our patients who are not fortunate enough to meet exacting inclusion criteria. Faced with complex patients for whom no study applies, our colleagues in the fields who feed us need flexibility to provide the best care for their patients. Those of us in the ivory tower who determine such inclusion criteria should not let perfect be the enemy of good and must do everything we can to help them and our patients.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at kalaycm@ccf.org.
“But no perfection is so absolute,
That some impurity doth not pollute.”
– William Shakespeare
While lounging in the ivory tower of academia, we frequently find ourselves condemning the peasantry who fail to grasp limitations of clinical trials. We deride the ignorant masses who insist on flaunting the inclusion criteria of the latest study and extrapolate the results to the ineligible patient sitting in front of them. The disrespect heaped on the “referring doctor” for treating their patients in the absence of evidence from prospective, randomized, multi-institutional trials is routine in conference rooms across the National Cancer Institute’s designated cancer centers.
The introduction of third-party insurers decades ago warped the economics of health care to the point that modern patients generally expect to pay little or nothing for pretty much any medical intervention. As a result, physicians tend to prescribe treatments without regard to cost. Predictably, this results in a steady increase in costs, which have now become unsustainable for our nation. Those rising costs have resulted in many proposals for control, including the Affordable Care Act and the efforts to reverse it. Many see a single payer, government administered system as the only viable way forward.
No matter the final system our society settles on, it will have to account for the almost miraculous results from modern therapeutics, which seem to be announced more and more frequently.
As I write this column, the annual meeting of the American Society of Hematology is being held in Atlanta. The presentations recount studies of new agents alone, or in combination, that report unprecedented response and survival rates. In particular, cellular immunotherapy with chimeric antigen receptor T cells (CAR T cells) has captured the attention of physicians, patients, and investors. Simultaneously – and recognizing this revolution in oncologic therapeutics – the New England Journal of Medicine prepublished two papers presenting the results of CAR T-cell therapy for diffuse large B-cell lymphoma (DLBCL). The results are impressive, and earlier this year, the Food and Drug Administration approved axicabtagene ciloleucel for the treatment of relapsed or refractory DLBCL based on these data. An approval for tisagenlecleucel exists for the treatment of B-cell acute lymphoblastic leukemia, but approval for DLBCL is likely forthcoming, too.
These are wonderful developments. Patients with incurable lymphoma may now be offered potentially curative treatment. Hematology News has covered the development of these treatments closely.
Yet, there is a glaring problem that has also attracted attention: CAR T-cell therapy is incredibly expensive. The potentially mitigating effect of competing products on cost will be canceled by the demand, as well as by geographic scarcity, because only certain large centers will provide this treatment. Remember that the price of imatinib went up over time even though competitors entered the market.
Entering CAR T-cell treatments into the nation’s formulary for some patients will lead to rising premiums for all patients. Disturbingly, CAR T cells are just a treatment for hematology patients at present. What about the equally impressive new – and expensive – technologies in cardiology, neurology, surgery, and every other medical subspecialty? Our system is already struggling to accommodate rapidly rising costs as our population ages and demands more and more medical care.
Many believe that our society will ultimately require strict controls on access to these expensive treatments. While the idea of rationing care is abhorrent to clinicians, “evidence-based” restrictions to access appear not to be. For example, rituximab is effective for immune thrombocytopenic purpura (ITP), but is not FDA approved for it. Despite the restriction, rituximab is frequently used for ITP and generally reimbursed. Venetoclax is a useful agent for patients in relapse of chronic lymphocytic leukemia, but the FDA only approved it for those harboring a deletion of 17p. While insurers seem willing to reimburse the use of rituximab for ITP, they balk at covering venetoclax for off-label indications. More recently, and more ominously for the implications, the FDA approval for tisagenlecleucel in the treatment of B-cell acute lymphoblastic leukemia only extends to those up to age 25. That could mean a 26-year-old in relapse after an allogeneic transplant would be denied coverage for potentially curative CAR T-cell therapy.
The federal government is not the only bureaucracy with a financial interest in limiting access to expensive treatments. Commercial insurers have a fiduciary duty to their shareholders, not to the patients who consume their services. They employ thousands, among them physicians, tasked with reviewing our treatment recommendations to determine whether treatments will be paid for, often citing FDA approvals. Preauthorization for coverage results in innumerable treatment delays and added administrative costs that frustrate us and anger our patients. The insurers defend this incessant obstructionism by claiming they are protecting patients from unnecessary or unhelpful care. Like the FDA, they invoke our own penchant for evidence-based medicine or declare that some care pathway is the ultimate arbiter of truth in coverage determination. Therein lies the danger.
Where do you suppose the evidence and care pathways the FDA and insurers rely on come from? They come from academics like many of this publication’s readers. We gladly provide them with the data needed to restrict care. Through published studies in “major” journals, consensus guidelines promulgated through national organizations, and care pathways generated by our own institutions, we provide the fodder that feeds the regulatory apparatus that decides whose care is approved and paid for. As Walt Kelly’s Pogo stated in 1970, “We have met the enemy and he is us.”
In the interest of science and in the interest of safety – but mostly in the interest of ensuring regulatory approval – clinical trials of new agents often restrict eligibility. Our group recently found that randomized trials routinely exclude patients for rather arbitrary organ dysfunction (Leukemia. 2017 Aug;31[8]:1808-15).
Another recent study concluded, “Current oncology clinical trials stipulate many inclusion and exclusion criteria that specifically define the patient population under study. Although eligibility criteria are needed to define the study population and improve safety, overly restrictive eligibility criteria limit participation in clinical trials, cause the study population to be unrepresentative of the general population of patients with cancer, and limit patient access to new treatments.” (J Clin Oncol. 2017 Nov 20;35[33]:3745-52).
Federal and private agencies will necessarily become stricter in their interpretations of studies and policies in order to control costs. They will happily cite the data we produce in order to do so. For the vast majority of patients who do not meet stringent inclusion criteria, access to new treatments may well be denied. To ensure that patients are provided with the best and most economical care, I am an advocate for evidence-based medicine and care pathways to standardize practice. However, I am progressively more wary of their potential to restrict the availability of innovative remedies to our patients who are not fortunate enough to meet exacting inclusion criteria. Faced with complex patients for whom no study applies, our colleagues in the fields who feed us need flexibility to provide the best care for their patients. Those of us in the ivory tower who determine such inclusion criteria should not let perfect be the enemy of good and must do everything we can to help them and our patients.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at kalaycm@ccf.org.
“But no perfection is so absolute,
That some impurity doth not pollute.”
– William Shakespeare
While lounging in the ivory tower of academia, we frequently find ourselves condemning the peasantry who fail to grasp limitations of clinical trials. We deride the ignorant masses who insist on flaunting the inclusion criteria of the latest study and extrapolate the results to the ineligible patient sitting in front of them. The disrespect heaped on the “referring doctor” for treating their patients in the absence of evidence from prospective, randomized, multi-institutional trials is routine in conference rooms across the National Cancer Institute’s designated cancer centers.
The introduction of third-party insurers decades ago warped the economics of health care to the point that modern patients generally expect to pay little or nothing for pretty much any medical intervention. As a result, physicians tend to prescribe treatments without regard to cost. Predictably, this results in a steady increase in costs, which have now become unsustainable for our nation. Those rising costs have resulted in many proposals for control, including the Affordable Care Act and the efforts to reverse it. Many see a single payer, government administered system as the only viable way forward.
No matter the final system our society settles on, it will have to account for the almost miraculous results from modern therapeutics, which seem to be announced more and more frequently.
As I write this column, the annual meeting of the American Society of Hematology is being held in Atlanta. The presentations recount studies of new agents alone, or in combination, that report unprecedented response and survival rates. In particular, cellular immunotherapy with chimeric antigen receptor T cells (CAR T cells) has captured the attention of physicians, patients, and investors. Simultaneously – and recognizing this revolution in oncologic therapeutics – the New England Journal of Medicine prepublished two papers presenting the results of CAR T-cell therapy for diffuse large B-cell lymphoma (DLBCL). The results are impressive, and earlier this year, the Food and Drug Administration approved axicabtagene ciloleucel for the treatment of relapsed or refractory DLBCL based on these data. An approval for tisagenlecleucel exists for the treatment of B-cell acute lymphoblastic leukemia, but approval for DLBCL is likely forthcoming, too.
These are wonderful developments. Patients with incurable lymphoma may now be offered potentially curative treatment. Hematology News has covered the development of these treatments closely.
Yet, there is a glaring problem that has also attracted attention: CAR T-cell therapy is incredibly expensive. The potentially mitigating effect of competing products on cost will be canceled by the demand, as well as by geographic scarcity, because only certain large centers will provide this treatment. Remember that the price of imatinib went up over time even though competitors entered the market.
Entering CAR T-cell treatments into the nation’s formulary for some patients will lead to rising premiums for all patients. Disturbingly, CAR T cells are just a treatment for hematology patients at present. What about the equally impressive new – and expensive – technologies in cardiology, neurology, surgery, and every other medical subspecialty? Our system is already struggling to accommodate rapidly rising costs as our population ages and demands more and more medical care.
Many believe that our society will ultimately require strict controls on access to these expensive treatments. While the idea of rationing care is abhorrent to clinicians, “evidence-based” restrictions to access appear not to be. For example, rituximab is effective for immune thrombocytopenic purpura (ITP), but is not FDA approved for it. Despite the restriction, rituximab is frequently used for ITP and generally reimbursed. Venetoclax is a useful agent for patients in relapse of chronic lymphocytic leukemia, but the FDA only approved it for those harboring a deletion of 17p. While insurers seem willing to reimburse the use of rituximab for ITP, they balk at covering venetoclax for off-label indications. More recently, and more ominously for the implications, the FDA approval for tisagenlecleucel in the treatment of B-cell acute lymphoblastic leukemia only extends to those up to age 25. That could mean a 26-year-old in relapse after an allogeneic transplant would be denied coverage for potentially curative CAR T-cell therapy.
The federal government is not the only bureaucracy with a financial interest in limiting access to expensive treatments. Commercial insurers have a fiduciary duty to their shareholders, not to the patients who consume their services. They employ thousands, among them physicians, tasked with reviewing our treatment recommendations to determine whether treatments will be paid for, often citing FDA approvals. Preauthorization for coverage results in innumerable treatment delays and added administrative costs that frustrate us and anger our patients. The insurers defend this incessant obstructionism by claiming they are protecting patients from unnecessary or unhelpful care. Like the FDA, they invoke our own penchant for evidence-based medicine or declare that some care pathway is the ultimate arbiter of truth in coverage determination. Therein lies the danger.
Where do you suppose the evidence and care pathways the FDA and insurers rely on come from? They come from academics like many of this publication’s readers. We gladly provide them with the data needed to restrict care. Through published studies in “major” journals, consensus guidelines promulgated through national organizations, and care pathways generated by our own institutions, we provide the fodder that feeds the regulatory apparatus that decides whose care is approved and paid for. As Walt Kelly’s Pogo stated in 1970, “We have met the enemy and he is us.”
In the interest of science and in the interest of safety – but mostly in the interest of ensuring regulatory approval – clinical trials of new agents often restrict eligibility. Our group recently found that randomized trials routinely exclude patients for rather arbitrary organ dysfunction (Leukemia. 2017 Aug;31[8]:1808-15).
Another recent study concluded, “Current oncology clinical trials stipulate many inclusion and exclusion criteria that specifically define the patient population under study. Although eligibility criteria are needed to define the study population and improve safety, overly restrictive eligibility criteria limit participation in clinical trials, cause the study population to be unrepresentative of the general population of patients with cancer, and limit patient access to new treatments.” (J Clin Oncol. 2017 Nov 20;35[33]:3745-52).
Federal and private agencies will necessarily become stricter in their interpretations of studies and policies in order to control costs. They will happily cite the data we produce in order to do so. For the vast majority of patients who do not meet stringent inclusion criteria, access to new treatments may well be denied. To ensure that patients are provided with the best and most economical care, I am an advocate for evidence-based medicine and care pathways to standardize practice. However, I am progressively more wary of their potential to restrict the availability of innovative remedies to our patients who are not fortunate enough to meet exacting inclusion criteria. Faced with complex patients for whom no study applies, our colleagues in the fields who feed us need flexibility to provide the best care for their patients. Those of us in the ivory tower who determine such inclusion criteria should not let perfect be the enemy of good and must do everything we can to help them and our patients.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at kalaycm@ccf.org.
FDA authorizes next-generation sequencing test for tumor profiling
The Food and Drug Administration has authorized a new tumor profiling test that can identify a larger number of genetic mutations than available in any other test previously reviewed, the agency has announced.
The tumor profiling test, developed at Memorial Sloan Kettering Cancer Center and known as MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), is a custom targeted sequencing platform that uses exon capture and sequencing, so-called next-generation sequencing, to identify point mutations, small insertions and deletions, and microsatellite instability in tumor specimens. The assay involves hybridization capture and deep sequencing of all protein coding exons of 468 cancer-associated genes, as well as molecular changes in a tumor’s genomic makeup, according to the FDA announcement.
Unlike cancer diagnostic tests designed to determine the presence of one cancer biomarker for use with a single drug, the IMPACT test compares tumor tissue to a “normal” tissue or cell sample from the same patient to find genetic alterations that could potentially guide treatment options. However, the FDA said, the results of IMPACT are “not conclusive” for choosing a corresponding treatment.
Next-generation sequencing technologies can examine “hundreds, if not millions, of DNA variants at a time,” Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in the announcement. “We are only at the beginning of realizing the true potential for these devices to assist patients and their health care providers in learning about the genetic underpinnings of their disease.”
Evaluations of IMPACT suggest the assay is “highly accurate” with a greater than 99% capability of detecting a mutation at a frequency of approximately 5%, according to the FDA.
In addition, detection of molecular changes, including microsatellite instability, were concordant more than 92% of the time when compared with traditional detection methods, the agency said.
Along with the marketing authorization for IMPACT, which was granted to Memorial Sloan Kettering Cancer Center, the agency announced that the New York State Department of Health has been accredited as an FDA third-party reviewer of in vitro diagnostics similar to IMPACT.
That action “paves the way” for efficient review and availability of other next-generation sequencing–based cancer profiling tools.
Allowing third parties to review next-generation sequencing–based tumor profiling tests will “reduce the burden on test developers and streamline the regulatory assessment of these types of innovative products,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
The Food and Drug Administration has authorized a new tumor profiling test that can identify a larger number of genetic mutations than available in any other test previously reviewed, the agency has announced.
The tumor profiling test, developed at Memorial Sloan Kettering Cancer Center and known as MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), is a custom targeted sequencing platform that uses exon capture and sequencing, so-called next-generation sequencing, to identify point mutations, small insertions and deletions, and microsatellite instability in tumor specimens. The assay involves hybridization capture and deep sequencing of all protein coding exons of 468 cancer-associated genes, as well as molecular changes in a tumor’s genomic makeup, according to the FDA announcement.
Unlike cancer diagnostic tests designed to determine the presence of one cancer biomarker for use with a single drug, the IMPACT test compares tumor tissue to a “normal” tissue or cell sample from the same patient to find genetic alterations that could potentially guide treatment options. However, the FDA said, the results of IMPACT are “not conclusive” for choosing a corresponding treatment.
Next-generation sequencing technologies can examine “hundreds, if not millions, of DNA variants at a time,” Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in the announcement. “We are only at the beginning of realizing the true potential for these devices to assist patients and their health care providers in learning about the genetic underpinnings of their disease.”
Evaluations of IMPACT suggest the assay is “highly accurate” with a greater than 99% capability of detecting a mutation at a frequency of approximately 5%, according to the FDA.
In addition, detection of molecular changes, including microsatellite instability, were concordant more than 92% of the time when compared with traditional detection methods, the agency said.
Along with the marketing authorization for IMPACT, which was granted to Memorial Sloan Kettering Cancer Center, the agency announced that the New York State Department of Health has been accredited as an FDA third-party reviewer of in vitro diagnostics similar to IMPACT.
That action “paves the way” for efficient review and availability of other next-generation sequencing–based cancer profiling tools.
Allowing third parties to review next-generation sequencing–based tumor profiling tests will “reduce the burden on test developers and streamline the regulatory assessment of these types of innovative products,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
The Food and Drug Administration has authorized a new tumor profiling test that can identify a larger number of genetic mutations than available in any other test previously reviewed, the agency has announced.
The tumor profiling test, developed at Memorial Sloan Kettering Cancer Center and known as MSK-IMPACT (Integrated Mutation Profiling of Actionable Cancer Targets), is a custom targeted sequencing platform that uses exon capture and sequencing, so-called next-generation sequencing, to identify point mutations, small insertions and deletions, and microsatellite instability in tumor specimens. The assay involves hybridization capture and deep sequencing of all protein coding exons of 468 cancer-associated genes, as well as molecular changes in a tumor’s genomic makeup, according to the FDA announcement.
Unlike cancer diagnostic tests designed to determine the presence of one cancer biomarker for use with a single drug, the IMPACT test compares tumor tissue to a “normal” tissue or cell sample from the same patient to find genetic alterations that could potentially guide treatment options. However, the FDA said, the results of IMPACT are “not conclusive” for choosing a corresponding treatment.
Next-generation sequencing technologies can examine “hundreds, if not millions, of DNA variants at a time,” Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in the announcement. “We are only at the beginning of realizing the true potential for these devices to assist patients and their health care providers in learning about the genetic underpinnings of their disease.”
Evaluations of IMPACT suggest the assay is “highly accurate” with a greater than 99% capability of detecting a mutation at a frequency of approximately 5%, according to the FDA.
In addition, detection of molecular changes, including microsatellite instability, were concordant more than 92% of the time when compared with traditional detection methods, the agency said.
Along with the marketing authorization for IMPACT, which was granted to Memorial Sloan Kettering Cancer Center, the agency announced that the New York State Department of Health has been accredited as an FDA third-party reviewer of in vitro diagnostics similar to IMPACT.
That action “paves the way” for efficient review and availability of other next-generation sequencing–based cancer profiling tools.
Allowing third parties to review next-generation sequencing–based tumor profiling tests will “reduce the burden on test developers and streamline the regulatory assessment of these types of innovative products,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
Gene editing aims to recreate beneficial mutation in SCD, beta-thalassemia
MADRID – With some genetic sleight-of-hand, investigators hope to mimic a rare, naturally occurring mutation that protects some patients with beta-thalassemia or sickle-cell disease (SCD) from becoming symptomatic.
Although human studies have yet to begin, investigators in a biotech company report that they can use CRISPR/Cas9 gene editing to recreate the rare condition known as hereditary persistence of fetal hemoglobin, or HPFH, which causes some patients with SCD or beta-thalassemia to continue to produce the fully functional fetal rather than adult form of hemoglobin into adulthood.
To date, there have been no detectable undesirable off-target genetic modifications seen by targeted deep sequencing for the two leading guide RNAs (gRNA) in development, he said at the annual congress of the European Hematology Association.
“Patients with sickle-cell disease and beta-thalassemia are not sick when they are first born, but symptoms develop shortly after birth as the fetal hemoglobin levels decline, and as adult hemoglobin rises,” Dr. Lundberg said.
Fetal hemoglobin has been shown to reduce the risk of sickle events in SCD, and reduce symptoms and morbidity of beta-thalassemia.
“Modest amounts of fetal hemoglobin are beneficial, and more appears to be better,” he said.
In rare instances, the genetic switch to turn off fetal hemoglobin fails, leading to HPFH. It is this rare circumstance that the investigators hope to copy.
CRISPR/Cas9 technology copies a bacterial defense mechanism using clustered regularly interspaced short palindromic (CRISPR) repeats of DNA as a template for adaptive immunity against viruses and plasmids. The system allows bacteria to prevent the activation of invading nucleic acids by effectively snipping out target sequences of foreign DNA.
The investigators plan to harvest hematopoietic stem cells from patients with SCD and beta-thalassemia and use CRISPR/Cas9 technology to modify the cells to express the fetal form of hemoglobin. The reintroduced stem cells would, ideally, proliferate and help protect patients against painful crises and debilitating symptoms of the hemoglobinopathies.
Dr. Lundberg said that to date they have been able to edit blood stem cells with more than 80% on-target efficiency, and that the editing leads to “clinically meaningful” levels of protective fetal hemoglobin, in the range of 30%.
As noted, the investigators have to date seen no evidence of off-target editing that could lead to undesirable or dangerous complications. When introduced into an immunodeficient mouse model (NOD scid gamma, or NSG mice), the edited human cells persisted for long periods.
Finally, the investigators have been able to demonstrate that the modified stem cells are able to differentiate and reconstitute different types of cells in blood.
The company plans to submit a clinical trial application in 2017, and start clinical trials in 2018, Dr. Lundberg said.
At a media briefing where he discussed his research prior to his presentation of data in a symposium, Dr. Lundberg said that to date they have worked only with mouse models and with cells from healthy donors.
He pointed out, however, that there are many thousands of patients with inherited hemoglobin disorders worldwide and beta-thalassemia, and asked “how do you proceed to implement this very expensive treatment?”
Dr. Lundberg acknowledged that the diseases are common in both the developing world and in wealthy countries. He said that the technique relies as much as possible on existing technologies, and pointed out that if the treatment is successful, it’s costs could be at least partially offset by reducing the costs of other forms of therapy.
The work is supported by CRISPR Therapeutics. Dr. Lundberg is an employee and shareholder in the company. Dr. Hagenbeek reported having no relevant conflicts of interest.
MADRID – With some genetic sleight-of-hand, investigators hope to mimic a rare, naturally occurring mutation that protects some patients with beta-thalassemia or sickle-cell disease (SCD) from becoming symptomatic.
Although human studies have yet to begin, investigators in a biotech company report that they can use CRISPR/Cas9 gene editing to recreate the rare condition known as hereditary persistence of fetal hemoglobin, or HPFH, which causes some patients with SCD or beta-thalassemia to continue to produce the fully functional fetal rather than adult form of hemoglobin into adulthood.
To date, there have been no detectable undesirable off-target genetic modifications seen by targeted deep sequencing for the two leading guide RNAs (gRNA) in development, he said at the annual congress of the European Hematology Association.
“Patients with sickle-cell disease and beta-thalassemia are not sick when they are first born, but symptoms develop shortly after birth as the fetal hemoglobin levels decline, and as adult hemoglobin rises,” Dr. Lundberg said.
Fetal hemoglobin has been shown to reduce the risk of sickle events in SCD, and reduce symptoms and morbidity of beta-thalassemia.
“Modest amounts of fetal hemoglobin are beneficial, and more appears to be better,” he said.
In rare instances, the genetic switch to turn off fetal hemoglobin fails, leading to HPFH. It is this rare circumstance that the investigators hope to copy.
CRISPR/Cas9 technology copies a bacterial defense mechanism using clustered regularly interspaced short palindromic (CRISPR) repeats of DNA as a template for adaptive immunity against viruses and plasmids. The system allows bacteria to prevent the activation of invading nucleic acids by effectively snipping out target sequences of foreign DNA.
The investigators plan to harvest hematopoietic stem cells from patients with SCD and beta-thalassemia and use CRISPR/Cas9 technology to modify the cells to express the fetal form of hemoglobin. The reintroduced stem cells would, ideally, proliferate and help protect patients against painful crises and debilitating symptoms of the hemoglobinopathies.
Dr. Lundberg said that to date they have been able to edit blood stem cells with more than 80% on-target efficiency, and that the editing leads to “clinically meaningful” levels of protective fetal hemoglobin, in the range of 30%.
As noted, the investigators have to date seen no evidence of off-target editing that could lead to undesirable or dangerous complications. When introduced into an immunodeficient mouse model (NOD scid gamma, or NSG mice), the edited human cells persisted for long periods.
Finally, the investigators have been able to demonstrate that the modified stem cells are able to differentiate and reconstitute different types of cells in blood.
The company plans to submit a clinical trial application in 2017, and start clinical trials in 2018, Dr. Lundberg said.
At a media briefing where he discussed his research prior to his presentation of data in a symposium, Dr. Lundberg said that to date they have worked only with mouse models and with cells from healthy donors.
He pointed out, however, that there are many thousands of patients with inherited hemoglobin disorders worldwide and beta-thalassemia, and asked “how do you proceed to implement this very expensive treatment?”
Dr. Lundberg acknowledged that the diseases are common in both the developing world and in wealthy countries. He said that the technique relies as much as possible on existing technologies, and pointed out that if the treatment is successful, it’s costs could be at least partially offset by reducing the costs of other forms of therapy.
The work is supported by CRISPR Therapeutics. Dr. Lundberg is an employee and shareholder in the company. Dr. Hagenbeek reported having no relevant conflicts of interest.
MADRID – With some genetic sleight-of-hand, investigators hope to mimic a rare, naturally occurring mutation that protects some patients with beta-thalassemia or sickle-cell disease (SCD) from becoming symptomatic.
Although human studies have yet to begin, investigators in a biotech company report that they can use CRISPR/Cas9 gene editing to recreate the rare condition known as hereditary persistence of fetal hemoglobin, or HPFH, which causes some patients with SCD or beta-thalassemia to continue to produce the fully functional fetal rather than adult form of hemoglobin into adulthood.
To date, there have been no detectable undesirable off-target genetic modifications seen by targeted deep sequencing for the two leading guide RNAs (gRNA) in development, he said at the annual congress of the European Hematology Association.
“Patients with sickle-cell disease and beta-thalassemia are not sick when they are first born, but symptoms develop shortly after birth as the fetal hemoglobin levels decline, and as adult hemoglobin rises,” Dr. Lundberg said.
Fetal hemoglobin has been shown to reduce the risk of sickle events in SCD, and reduce symptoms and morbidity of beta-thalassemia.
“Modest amounts of fetal hemoglobin are beneficial, and more appears to be better,” he said.
In rare instances, the genetic switch to turn off fetal hemoglobin fails, leading to HPFH. It is this rare circumstance that the investigators hope to copy.
CRISPR/Cas9 technology copies a bacterial defense mechanism using clustered regularly interspaced short palindromic (CRISPR) repeats of DNA as a template for adaptive immunity against viruses and plasmids. The system allows bacteria to prevent the activation of invading nucleic acids by effectively snipping out target sequences of foreign DNA.
The investigators plan to harvest hematopoietic stem cells from patients with SCD and beta-thalassemia and use CRISPR/Cas9 technology to modify the cells to express the fetal form of hemoglobin. The reintroduced stem cells would, ideally, proliferate and help protect patients against painful crises and debilitating symptoms of the hemoglobinopathies.
Dr. Lundberg said that to date they have been able to edit blood stem cells with more than 80% on-target efficiency, and that the editing leads to “clinically meaningful” levels of protective fetal hemoglobin, in the range of 30%.
As noted, the investigators have to date seen no evidence of off-target editing that could lead to undesirable or dangerous complications. When introduced into an immunodeficient mouse model (NOD scid gamma, or NSG mice), the edited human cells persisted for long periods.
Finally, the investigators have been able to demonstrate that the modified stem cells are able to differentiate and reconstitute different types of cells in blood.
The company plans to submit a clinical trial application in 2017, and start clinical trials in 2018, Dr. Lundberg said.
At a media briefing where he discussed his research prior to his presentation of data in a symposium, Dr. Lundberg said that to date they have worked only with mouse models and with cells from healthy donors.
He pointed out, however, that there are many thousands of patients with inherited hemoglobin disorders worldwide and beta-thalassemia, and asked “how do you proceed to implement this very expensive treatment?”
Dr. Lundberg acknowledged that the diseases are common in both the developing world and in wealthy countries. He said that the technique relies as much as possible on existing technologies, and pointed out that if the treatment is successful, it’s costs could be at least partially offset by reducing the costs of other forms of therapy.
The work is supported by CRISPR Therapeutics. Dr. Lundberg is an employee and shareholder in the company. Dr. Hagenbeek reported having no relevant conflicts of interest.
AT EHA 2017
Key clinical point: The fetal form of hemoglobin is protective against symptoms of sickle-cell disease (SCD) and beta-thalassemia.
Major finding: Human blood stem cells modified by CRISPR/Cas9 gene editing produced fetal hemoglobin without observable off-target effects.
Data source: Summary of preclinical studies with blood from healthy human volunteers and mouse models.
Disclosures: The work is supported by CRISPR Therapeutics. Dr. Lundberg is an employee and shareholder in the company. Dr. Hagenbeek reported having no relevant conflicts of interest.
Two SNPs linked to survival in R-CHOP–treated DLBCL
Two variations of the BCL2 gene are linked with the survival prospects of patients with diffuse large B-cell lymphoma (DLBCL) who are treated with the R-CHOP regimen, based on a study published in Haematologica.
In the population-based, case-control study of patients with non-Hodgkin’s lymphoma across the British Columbia province, Morteza Bashash, PhD, of the Dalla Lana School of Public Health, Toronto, and researchers at the British Columbia Cancer Agency analyzed 217 germline DLBCL samples, excluding those with primary mediastinal large B-cell lymphoma, specifically looking at nine single nucleotide polymorphisms (SNPs).
Patients receiving R-CHOP who had the AA genotype at rs7226979 had a risk of death that was four times higher than that of those with a G allele, researchers said (P less than .01). The same pattern was seen for PFS, with AA carriers having twice the risk of an event, compared with the other genotypes (P less than .05).
For those with rs4456611, patients with the GG genotype had a risk of death that was 3 times greater than that of those with an A allele (P less than .01), but there was no association with PFS for that SNP.
In an analysis of an independent cohort, only the associations that were seen with rs7226979 – and not those with rs4456611 – were able to be replicated.
The researchers noted that, while most predictive markers that are used to guide clinical treatment are drawn from actual tumor material, host-related factors could also be important.
“Compared to genetic analysis of the tumor, the patient’s constitutional genetic profile is relatively easy to obtain and can be assessed before treatment is started,” they wrote. “Our result has the potential to be useful as a complementary tool to predict the outcome of patients treated with R-CHOP and enhance clinical decision-making after confirmation by further studies.”
Two variations of the BCL2 gene are linked with the survival prospects of patients with diffuse large B-cell lymphoma (DLBCL) who are treated with the R-CHOP regimen, based on a study published in Haematologica.
In the population-based, case-control study of patients with non-Hodgkin’s lymphoma across the British Columbia province, Morteza Bashash, PhD, of the Dalla Lana School of Public Health, Toronto, and researchers at the British Columbia Cancer Agency analyzed 217 germline DLBCL samples, excluding those with primary mediastinal large B-cell lymphoma, specifically looking at nine single nucleotide polymorphisms (SNPs).
Patients receiving R-CHOP who had the AA genotype at rs7226979 had a risk of death that was four times higher than that of those with a G allele, researchers said (P less than .01). The same pattern was seen for PFS, with AA carriers having twice the risk of an event, compared with the other genotypes (P less than .05).
For those with rs4456611, patients with the GG genotype had a risk of death that was 3 times greater than that of those with an A allele (P less than .01), but there was no association with PFS for that SNP.
In an analysis of an independent cohort, only the associations that were seen with rs7226979 – and not those with rs4456611 – were able to be replicated.
The researchers noted that, while most predictive markers that are used to guide clinical treatment are drawn from actual tumor material, host-related factors could also be important.
“Compared to genetic analysis of the tumor, the patient’s constitutional genetic profile is relatively easy to obtain and can be assessed before treatment is started,” they wrote. “Our result has the potential to be useful as a complementary tool to predict the outcome of patients treated with R-CHOP and enhance clinical decision-making after confirmation by further studies.”
Two variations of the BCL2 gene are linked with the survival prospects of patients with diffuse large B-cell lymphoma (DLBCL) who are treated with the R-CHOP regimen, based on a study published in Haematologica.
In the population-based, case-control study of patients with non-Hodgkin’s lymphoma across the British Columbia province, Morteza Bashash, PhD, of the Dalla Lana School of Public Health, Toronto, and researchers at the British Columbia Cancer Agency analyzed 217 germline DLBCL samples, excluding those with primary mediastinal large B-cell lymphoma, specifically looking at nine single nucleotide polymorphisms (SNPs).
Patients receiving R-CHOP who had the AA genotype at rs7226979 had a risk of death that was four times higher than that of those with a G allele, researchers said (P less than .01). The same pattern was seen for PFS, with AA carriers having twice the risk of an event, compared with the other genotypes (P less than .05).
For those with rs4456611, patients with the GG genotype had a risk of death that was 3 times greater than that of those with an A allele (P less than .01), but there was no association with PFS for that SNP.
In an analysis of an independent cohort, only the associations that were seen with rs7226979 – and not those with rs4456611 – were able to be replicated.
The researchers noted that, while most predictive markers that are used to guide clinical treatment are drawn from actual tumor material, host-related factors could also be important.
“Compared to genetic analysis of the tumor, the patient’s constitutional genetic profile is relatively easy to obtain and can be assessed before treatment is started,” they wrote. “Our result has the potential to be useful as a complementary tool to predict the outcome of patients treated with R-CHOP and enhance clinical decision-making after confirmation by further studies.”
FROM HAEMATOLOGICA
Key clinical point: Two SNPs were found to be linked to survival prospects in patients with diffuse large B-cell lymphoma who receive primary R-CHOP therapy.
Major finding: For the rs7226979 SNP, those with the AA genotype had a four times higher risk of death than those with a G allele.
Data source: A population-based, case-control study of patients with non-Hodgkin’s lymphoma in British Columbia, with DNA samples analyzed for 9nine SNPs among the DLBCL patients, excluding those with primary mediastinal large B-cell lymphoma.
Disclosures: Some of the study authors reported institutional research funding from Roche; honoraria from Roche/Genentech, Janssen Pharmaceuticals and Celgene; and/or consultant or advisory roles with Roche/Genentech, Janssen Pharmaceuticals, Celgene, and NanoString Technologies.






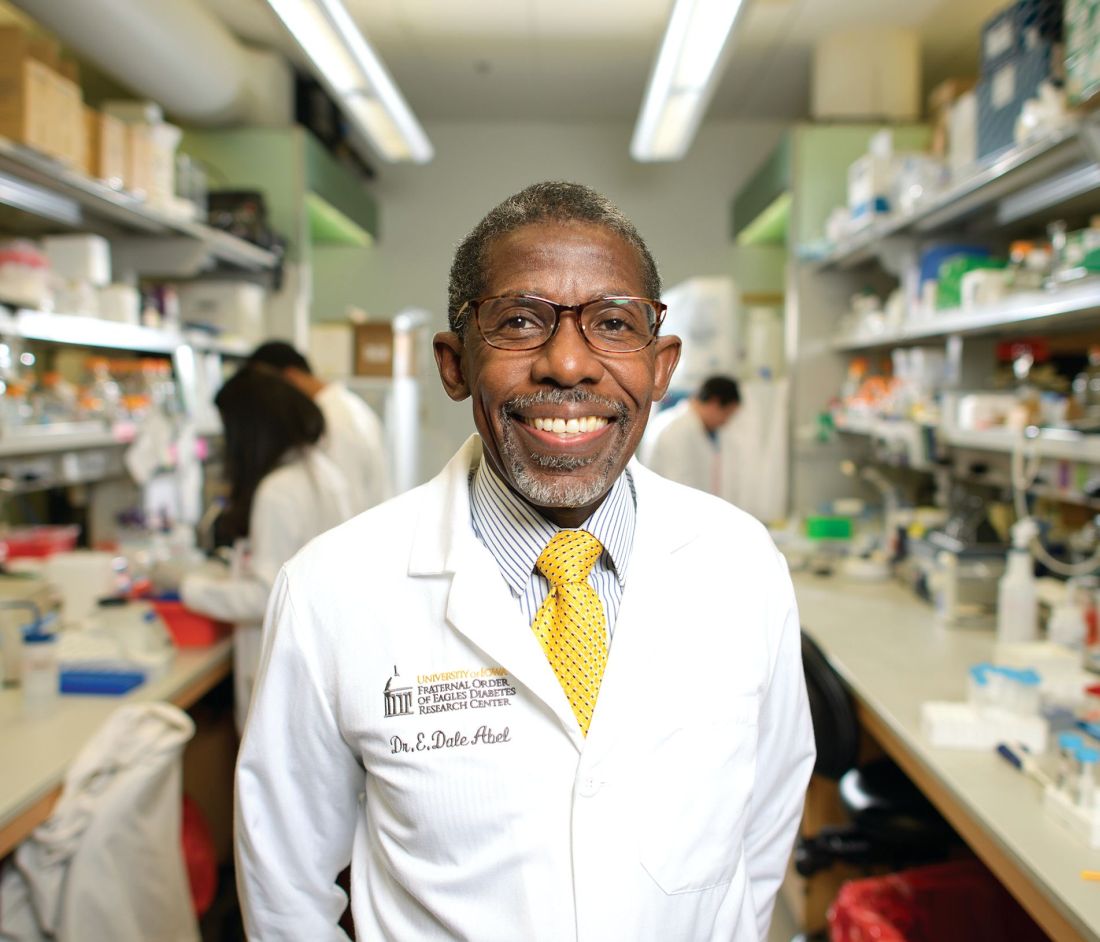





![Micrograph of a 'diffuse large B cell lymphoma. Lymph node FNA specimen. Field stain.(http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](https://cdn.mdedge.com/files/s3fs-public/styles/medium/public/Image/June-2017/DLBCL_web.jpg?itok=LAQhMuwC)
![Micrograph of a 'diffuse large B cell lymphoma. Lymph node FNA specimen. Field stain.(http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](https://cdn.mdedge.com/files/s3fs-public/Image/June-2017/DLBCL_web.jpg)